Abstract
Purpose
We examined self‐reported financial toxicity and out‐of‐pocket expenses among adult women with breast cancer.
Methods
Patients spoke English, Spanish, or Mandarin Chinese, were aged 18+ years, had stage I–IIIA breast cancer, and were eligible for breast‐conserving and mastectomy surgery. Participants completed surveys about out‐of‐pocket costs and financial toxicity at 1 week, 12 weeks, and 1 year postsurgery.
Results
Three hundred ninety‐five of 448 eligible patients (88.2%) from the parent trial completed surveys. Excluding those reporting zero costs, crude mean ± SD out‐of‐pocket costs were $1,512 ± $2,074 at 1 week, $2,609 ± $6,369 at 12 weeks, and $3,308 ± $5,000 at 1 year postsurgery. Controlling for surgery, cancer stage, and demographics with surgeon and clinic as random effects, higher out‐of‐pocket costs were associated with higher financial toxicity 1 week and 12 weeks postsurgery (p < .001). Lower socioeconomic status (SES) was associated with lower out‐of‐pocket costs at each time point (p = .002–.013). One week postsurgery, participants with lower SES reported financial toxicity scores 1.02 points higher than participants with higher SES (95% confidence interval [CI], 0.08–1.95). Black and non‐White/non‐Black participants reported financial toxicity scores 1.91 (95% CI, 0.46–3.37) and 2.55 (95% CI, 1.11–3.99) points higher than White participants. Older (65+ years) participants reported financial toxicity scores 2.58 points lower than younger (<65 years) participants (95% CI, −3.41, −1.74). Younger participants reported significantly higher financial toxicity at each time point.
Discussion
Younger age, non‐White race, and lower SES were associated with higher financial toxicity regardless of costs. Out‐of‐pocket costs increased over time and were positively associated with financial toxicity. Future work should reduce the impact of cancer care costs among vulnerable groups.
Implications for Practice
This study was one of the first to examine out‐of‐pocket costs and financial toxicity up to 1 year after breast cancer surgery. Younger age, Black race, race other than Black or White, and lower socioeconomic status were associated with higher financial toxicity. Findings highlight the importance of addressing patients’ financial toxicity in several ways, particularly for groups vulnerable to its effects.
Keywords: Financial toxicity, Breast cancer, Costs of care
Short abstract
The term “financial toxicity” describes both the financial hardship and the psychological distress associated with health care costs. This article examines financial toxicity of women diagnosed with breast cancer at three time points up to 1 year post‐surgery, assessing demographic and clinical variables associated with higher financial toxicity and higher out‐of‐pocket expenses.
Introduction
Improvements in cancer treatments have led to higher out‐of‐pocket costs for patients [1, 2, 3, 4, 5]. These out‐of‐pocket costs substantially impact patients’ financial stability and health outcomes [6, 7, 8, 9, 10]. Financial toxicity [11, 12] describes both the financial hardship and psychological distress associated with health care costs. Many patients report depleting their savings to pay for needed cancer care [13]. Others describe rationing medication [4] and delaying or avoiding needed care because of costs [8, 14, 15, 16, 17]. Patients with cancer also report worry and anxiety about paying their medical bills [18]. Financial toxicity can thus lower patients’ quality of life and affect cancer outcomes [11, 19, 20] regardless of demographic characteristic or cancer type [21, 22, 23].
Financial toxicity survey questions ask patients about the impact of care costs on their life [1]. Few studies have explored the relationship between financial toxicity and out‐of‐pocket expenses and how those two factors relate to each other. In addition, survey questions are typically assessed at a single point in time or use a different set of respondents randomly selected at each time point. The relationship between out‐of‐pocket costs and financial toxicity over time is complex. Some patients might feel greater burden from costs over time, as costs could increase with additional treatment [24]. Others might feel a lower burden over time; they could anticipate care needs, prepare for potential costs, identify resources to offset costs, or even change insurance plans during open enrollment. In studies that have explored out‐of‐pocket expenses longitudinally among Medicare beneficiaries, costs initially rose after diagnosis, stabilized around 1 to 2 years after diagnosis, and rose again if patients approached the end of life [24]. However, younger adults or those with insurance other than Medicare might shoulder the cost burden differently, depending on their plan type and overall health status. Young adults often report higher financial toxicity after cancer than their older counterparts [25], but the burden of these costs over time and how other demographic and clinical factors affect this burden have not yet been examined.
Measurable direct and indirect expenses associated with care could lead to high levels of financial toxicity. Additional patient characteristics and experiences could compound this hardship. For example, those with lower incomes and poor insurance coverage might report more financial hardship after a cancer diagnosis [18]. Understanding how these characteristics interact with financial toxicity and out‐of‐pocket expenses might help clinicians better support patients at risk for financial distress.
The purpose of this study was to examine financial toxicity and out‐of‐pocket expenses of adult women recently diagnosed with breast cancer at three time points: 1 week after primary surgery for breast cancer, 12 weeks after surgery, and 1 year after surgery (Aim 1). We assessed demographic and clinical variables associated with both higher financial toxicity and higher out‐of‐pocket expenses at each time point (Aim 2). We also explored whether financial toxicity correlated with out‐of‐pocket expenses at each time point (Aim 3).
Materials and Methods
Procedure
We conducted secondary data analysis of a parent randomized trial examining whether the use of paper‐based encounter decision aids used during clinical consultations supported women's decisions about breast cancer surgery across socioeconomic strata. The full details of the trial are published and available by open access [26]. The study was conducted at four National Cancer Institute–designated cancer centers in the U.S., located in geographically diverse regions with racially and ethnically diverse patient populations. Surgeons were randomized to one of two encounter decision aids or usual care; eligible patients who were seen by one of the 16 surgeons were included. Baseline data were collected over the course of 18 months, from September 2017 to February 2019; follow‐up continued through May 2019. Patients completed surveys before the clinic visit, immediately after the visit, 1 week postsurgery, and 12 weeks postsurgery. For all participants who received surgery before May 2018, we also measured costs and financial toxicity 1 year postsurgery. The data analyzed in this paper are from measures collected 1 week postsurgery, 12 weeks postsurgery, and 1 year postsurgery, along with demographics collected at baseline.
Participants
Patients were eligible if they spoke English, Spanish, or Mandarin Chinese, were at least 18 years of age, had a confirmed diagnosis of stage I–IIIA breast cancer, and were eligible for both breast‐conserving surgery and mastectomy based on medical records and clinicians’ judgment. We excluded transgender men and women, women who had undergone prophylactic mastectomy, women with visual impairment who might have difficulty viewing study materials, women with severe mental illness or severe dementia, and women with inflammatory breast carcinoma. Enrollment of women receiving neoadjuvant therapy was limited to the first 9 months of the trial to allow completion of follow‐up assessments before the trial terminated.
Measures
Socioeconomic status (SES) was categorized by examining (a) insurance status (obtained via the electronic health record), (b) highest educational attainment (self‐reported), and (c) federal poverty level (as determined by the Census Bureau in that calendar year and calculated using self‐reported household income and family size). Together, these three socioeconomic factors composed a composite SES variable. As defined in this study, those of lower SES met at least two of the following criteria: (a) public insurance (Medicaid, Medicare without supplemental) or uninsured, (b) lower educational attainment (less than a Bachelor's degree), and (c) below the federal poverty level (as defined above).
We included four items from a validated measure of financial toxicity, the COST measure [20]. In order to reduce participant burden, we consulted the scale developer and reviewed the development paper [27] to select a subset of items. We selected the items with the highest importance score within each of the three themes (resources, financial, affect) and the item with the overall highest loading in the factor analysis (“I feel financially stressed.”). Our goal with this approach was to purposefully select items that would reflect both direct and indirect costs (even if they did not have the highest loading in the factor). We consulted with our patient partners, patient associates, and community advisory board to ensure understanding and relevance of the items. We also received approval to use only these four questions from the scale developer. As in the original scale, each item is scored from 0 to 4 (total score 0 to 16), and higher scores indicate higher financial toxicity.
We asked participants to estimate the out‐of‐pocket portion of their medical expenses at three time points: about 1 week after surgery, about 12 weeks after surgery, and about 1 year after surgery. At each time point, they were asked to estimate their medical expenses since their last study survey. We also created a separate dichotomous out‐of‐pocket variable, comparing those with no reported costs with those with any costs reported. Self‐report measures of out‐of‐pocket cancer costs within the past year are used in many national surveys and can provide reasonable estimates of the care cost burden on patients [27, 28, 29].
Analyses
Analyses Corresponding to Aim 1
We used descriptive statistics to examine participants’ crude financial toxicity scores and self‐reported out‐of‐pocket medical expenses at each time point.
Analyses Corresponding to Aim 2
For inferential analyses in Aims 2 and 3, we included specific demographic, societal, and clinical variables pertinent to our outcomes of interest, including SES (dichotomous), age (65 years and older versus younger than 65; we used age 65 to dichotomize age because of Medicare insurance eligibility starting at age 65), race (categorical), surgery choice (breast‐conserving surgery vs. mastectomy), and cancer stage (stage I, II, or III). For all time points, the out‐of‐pocket costs variable was highly skewed to the right, so we used log‐transformed values for this variable in our analysis.
We used one‐way ANOVAs, two‐sample t tests, and simple regressions to examine the relationship between each selected patient variable, financial toxicity scores, and out‐of‐pocket costs. We used mixed‐effects logistic regression to examine the relationship between the dichotomous out‐of‐pocket variable (dependent variable) with all patient variables as independent predictors at each time point. We used mixed‐effects linear regression to examine this relationship with the log of the continuous out‐of‐pocket variable at each time point, which we favored over the use of a single longitudinal model because of differences in the way that out‐of‐pocket costs were asked across the three time points (e.g., costs since the last survey).
Analyses Corresponding to Aim 3
We used simple linear regression to examine the relationship between financial toxicity scores (dependent variable) and out‐of‐pocket costs (independent variable) at each time point. We used mixed‐effects linear regression to examine this relationship while adjusting for all patient variables as independent predictors at each time point.
In the parent trial, there were 16 surgeons within seven clinics across the four participating sites. For all adjusted analyses, we included study site as a fixed effect and surgeon and clinic as random effects to control for potential impact of surgeon‐ and clinic‐level clusters in our outcomes of interest.
Sensitivity Analyses
Finally, to check the robustness of the results, we concatenated the data across the three time points and estimated a longitudinal multivariable model allowing time‐by‐covariate interactions (i.e., distinct effects at each time point), treating patient as a random effect to account for repeated measurements of patients’ financial toxicity and out‐of‐pocket costs across time. This analysis has the advantage of being able to evaluate the overall strength of association between predictors and the outcome as well as being able to test whether the associations differ significantly between the follow‐up times.
Results
Participants
A total of 622 patients were recruited into the parent trial at baseline; 395 of 448 eligible patients (88.2%) from the parent trial completed measures relevant to this analysis (Fig. 1). Of those with missing data in these analyses, some participants skipped the question or responded that they did not know their costs, some became ineligible upon imaging or after receiving neoadjuvant chemotherapy, some were unreachable, and some were not followed at 1 year postsurgery because the study had ended. The majority of our sample in this analysis (n = 395) was of higher SES (n = 259, 65.6%), younger than age 65 (n = 231, 58.5%), and White (n = 254, 64.3%). Most had stage I breast cancer (n = 270, 68.3%) and chose breast‐conserving surgery (n = 313, 79.2%). There were few statistical differences between patients reporting out‐of‐pocket costs compared with those who did not know or did not report their out‐of‐pocket costs (Table 1). Differences occurred only at 1 year postsurgery when participants who were White and of higher SES were less likely to have missing out‐of‐pocket costs.
Figure 1.
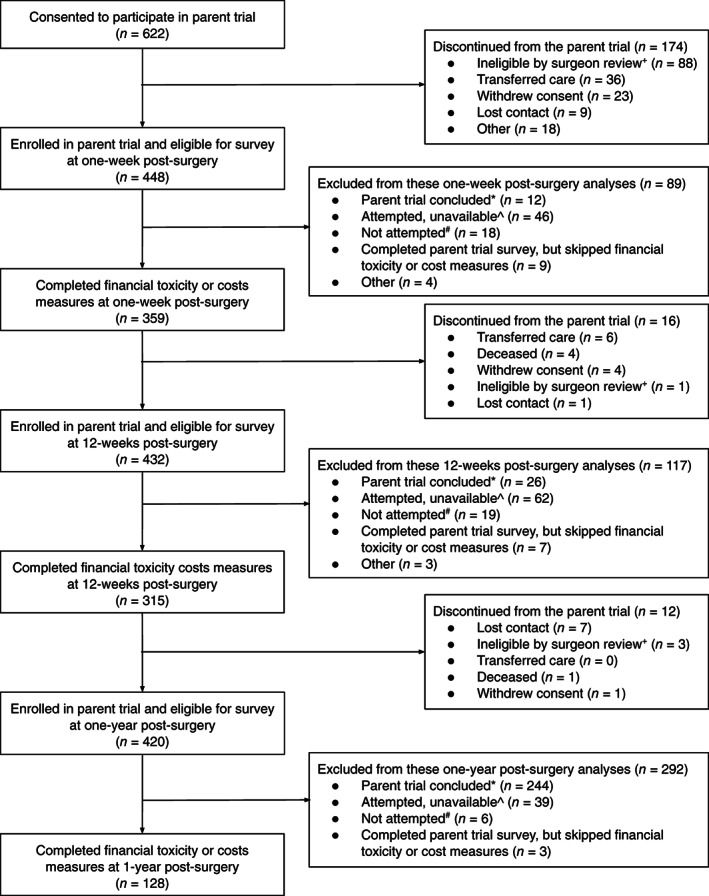
Patient flow and data collection. ^, Attempted, unavailable: we reached out to participants a maximum of five times via phone or email (according to patient preference); *, Parent trial concluded: we collected follow‐up data through 6/1/2019, not all participants received surgery within a timeframe that allowed for follow‐up before this date; #, Not attempted: this includes research team turnover, issues with follow‐up reminders, and holidays; +, Ineligible by surgeon review: participant was deemed ineligible after consent based on surgeon review. This was most often the case because their cancer stage changed after additional imaging or the participant no longer had a choice between breast conserving surgery and mastectomy.
Table 1.
Participant characteristics stratified by whether they reported OOP costs or did not report OOP costs, by time point
| Characteristic, n (%) | Overall (n = 395) | 1 week postsurgery | 12 weeks postsurgery | 1 year postsurgery | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Missing OOP (n = 171) | Reported OOP (n = 268) | p value a | Missing OOP (n = 152) | Reported OOP (n = 257) | p value a | Missing OOP (n = 89) | Reported OOP (n = 94) | p value a | ||
| Socioeconomic status | .97 | .95 | .01 | |||||||
| Lower | 136 (34.4) | 59 (34.5) | 92 (34.3) | 51 (33.6) | 87 (33.9) | 40 (45.0) | 25 (27.0) | |||
| Higher | 259 (65.6) | 112 (65.5) | 176 (65.7) | 101 (66.4) | 170 (66.1) | 49 (55.0) | 69 (73.0) | |||
| Age | .57 | .90 | .67 | |||||||
| Less than 65 | 231 (58.5) | 98 (57.3) | 161 (60.1) | 92 (60.5) | 154 (59.9) | 52 (58.0) | 52 (55.0) | |||
| 65 and older | 164 (41.5) | 73 (42.7) | 107 (39.9) | 60 (40.5) | 103 (40.1) | 37 (42.0) | 42 (45.0) | |||
| Race | .71 | .94 | .001 | |||||||
| White, non‐Hispanic | 254 (64.3) | 111 (64.9) | 175 (65.3) | 102 (67.1) | 172 (66.9) | 53 (60.0) | 75 (80.0) | |||
| Black, non‐Hispanic | 55 (13.9) | 21 (12.3) | 38 (14.2) | 20 (13.2) | 33 (12.8) | 8 (9.0) | 10 (11.0) | |||
| Other | 78 (19.7) | 36 (21.1) | 49 (18.3) | 26 (17.1) | 48 (18.7) | 26 (29.0) | 8 (9.0) | |||
| Missing | 8 (2.0) | 3 (1.8) | 6 (2.2) | 4 (2.6) | 4 (1.6) | 2 (2.0) | 1 (1.0) | |||
| Surgery choice | .83 | .21 | .40 | |||||||
| Lumpectomy | 313 (79.2) | 121 (70.8) | 213 (79.5) | 104 (68.4) | 209 (81.3) | 72 (81.0) | 82 (87.0) | |||
| Mastectomy | 80 (20.3) | 33 (19.3) | 55 (20.5) | 33 (21.7) | 48 (18.7) | 15 (17.0) | 12 (13.0) | |||
| Missing | 2 (0.5) | 17 (9.9) | 0 (0.0) | 15 (9.9) | 0 (0.0) | (2.0) | 0 (0.0) | |||
| Cancer stage | .57 | .10 | .53 | |||||||
| Stage I | 270 (68.4) | 109 (63.0) | 188 (70.1) | 95 (62.5) | 183 (71.2) | 62 (70.0) | 73 (78.0) | |||
| Stage II | 109 (27.6) | 49 (28.7) | 72 (26.9) | 50 (32.9) | 65 (25.3) | 25 (28.0) | 20 (21.0) | |||
| Stage III | 10 (2.5) | 5 (2.9) | 5 (1.9) | 1 (0.7) | 6 (2.3) | 1 (1.0) | 1 (1.0) | |||
| Missing | 6 (1.5) | 8 (4.7) | 3 (1.1) | 6 (3.9) | 3 (1.2) | 1 (1.0) | 0 (0.0) | |||
Does not include participants who discontinued before specified time point or participants where this follow‐up was due after data collection ended.
Chi‐square tests were used to test for statistical differences between groups.
Abbreviation: OOP, out‐of‐pocket.
Aim 1: Out‐of‐Pocket Costs and Financial Toxicity at Each Time Point
Mean ± SD self‐reported out‐of‐pocket costs were $1,027 ± $1,856 at 1 week postsurgery, $1,944 ± $5,610 at 12 weeks postsurgery, and $2,533 ± $4,590 at 1 year postsurgery. Excluding those who reported zero costs (n = 86; 32.1%, 66; 25.7%, 22; 23.4% at 1 week, 12 weeks, 1 year postsurgery), mean ± SD self‐reported out‐of‐pocket costs were $1,512 ± $2,074 at 1 week postsurgery, $2,609 ± $6,369 at 12 weeks postsurgery, and $3,308 ± $5,000 at 1 year postsurgery. Mean ± SD financial toxicity scores were 6.4/16 ± 4.2 at 1 week postsurgery, 6.2/16 ± 4.3 at 12 weeks postsurgery, and 6.2/16 ± 4.8 at 1 year postsurgery. There were no significant differences in financial toxicity scores across time points.
Aim 2. Relationship Between Patient Attributes, Out‐of‐Pocket Expenses, and Financial Toxicity
In bivariate analyses, out‐of‐pocket costs were significantly associated with SES, age, and race at 1 week and 12 weeks postsurgery. At 1 year postsurgery, only age was significantly associated with out‐of‐pocket costs (supplemental online Table 1). In the mixed‐effects multivariable linear regression, controlling for surgery, cancer stage, demographic variables, and surgeon‐ and clinic‐level clusters, being of lower SES (t1‐week = −2.81, p = .005) and 65 years or older (t 1‐week = −6.31, p < .001) were significantly associated with lower out‐of‐pocket costs at 1 week postsurgery. These relationships were similar across time points, but only lower SES and being 65 years or older related to lower out‐of‐pocket costs at all three time points. Being Black was significantly associated with higher out‐of‐pocket costs at 1 year postsurgery (t = 2.12, p = .034; supplemental online Table 1).
In the mixed‐effects multivariable logistic regression using the binary out‐of‐pocket variable, participants of lower SES (Z1‐week = −2.46, p = .014) and aged at least 65 (Z1‐week = −4.23, p < .001) were more likely to report zero out‐of‐pocket costs at 1 week postsurgery. This held at 12 weeks postsurgery; however, lower SES was the only variable associated with zero out‐of‐pocket costs reported at 1 year postsurgery (Z1‐week = −2.35, p = .019). Table 2 shows the crude and adjusted results of the out‐of‐pocket regression analyses.
Table 2.
Adjusted logistic regression odds ratios examining the relationship between zero versus nonzero out‐of‐pocket costs at each time point
| 1 week postsurgery | 12 weeks postsurgery | 1 year postsurgery | ||||
|---|---|---|---|---|---|---|
| Crude OR (95% CI) | Adjusted a OR (95% CI) | Crude OR (95% CI) | Adjusted a OR (95% CI) | Crude OR (95% CI) | Adjusted a OR (95% CI) | |
| Lower SES (vs. higher SES) | 0.31 (0.18–0.54) b | 0.45 (0.24–0.85) b | 0.28 (0.16–0.50) b | 0.39 (0.20–0.80) b | 0.41 (0.15–1.14) | 0.26 (0.08–0.85) b |
| 65 years and older (vs. <65) | 0.32 (0.19–0.55) b | 0.27 (0.15–0.50) b | 0.53 (0.30–0.94) b | 0.45 (0.23–0.88) b | 0.47 (0.18–1.23) | 0.34 (0.11–1.03) |
| Race/ethnicity | ||||||
| White, non‐Hispanic | referent | referent | referent | referent | referent | referent |
| Black, non‐Hispanic | 0.82 (0.38–1.80) | 1.43 (0.47–4.38) | 0.45 (0.19–1.04) | 1.01 (0.32–3.12) | 3.05 (0.36–25.7) | 8.67 (0.58–130.12) |
| Other | 0.25 (0.13–0.49) b | 0.55 (0.19–1.57) | 0.15 (0.08–0.30) | 0.50 (0.18–1.36) | 1.02 (0.19–5.48) | 3.51 (0.36–34.12) |
| Mastectomy (vs. lumpectomy) | 1.50 (0.77–2.92) | 1.67 (0.73–3.81) | 0.71 (0.36–1.41) | 1.06 (0.43–2.63) | 0.16 (0.33–7.99) | 1.35 (0.17–10.94) |
| Stage (I, II, or III) | ||||||
| Stage I | referent | referent | referent | referent | referent | referent |
| Stage II | 1.34 (0.77–2.43) | 1.11 (0.55–2.25) | 1.03 (0.53–1.98) | 0.98 (0.44–2.17) | 0.65 (0.22–1.98) | 0.62 (0.15–2.46) |
| Stage III | 0.77 (0.13–4.75) | 0.34 (0.04–3.17) | 0.67 (0.12–3.79) | 1.18 (0.15–9.27) | [small cell size] | [small cell size] |
| Site | ||||||
| Site 1 | — | referent | — | referent | — | referent |
| Site 2 | — | 0.56 (0.19–1.70) | — | 0.30 (0.10–0.90) b | — | 0.13 (0.01–1.13) |
| Site 3 | — | 0.33 (0.10–1.16) | — | 0.23 (0.06–0.81) b | — | 0.51 (0.07–3.54) |
| Site 4 | — | 1.20 (0.54–2.65) | — | 1.33 (0.51–3.49) | — | 0.75 (0.21–2.71) |
| Random effect SD estimates (SE) | ||||||
| Clinic | — | 8.57e‐12 (0.17) | — | 1.53e‐07 (0.18) | — | 7.62e‐5 (0.27) |
| Surgeon | — | 2.45e‐12 (0.21) | — | 2.34e‐07 (0.31) | — | 2.31e‐4 (1.88) |
Adjusted for each of the following, exclusive of the variable of being compared: participant SES (high vs. low), age (≥65 vs. less than 65), race (White vs. Black vs. other), surgery choice (breast‐conserving surgery vs. mastectomy), cancer stage (I vs. II vs. III), and study site as fixed effects and surgeon and clinic as random effects.
p < .05.
Abbreviations: CI, confidence interval; OR, odds ratio; SES, socioeconomic status.
In the bivariate analysis, financial toxicity scores were significantly associated with lower SES, age, race, and more advanced breast cancer stage at all three time points (Table 3). In the mixed‐effects multivariable linear regression analyses at 1 week postsurgery, controlling for cancer stage, surgery, demographics, and surgeon‐ and clinic‐level clusters, participants of lower SES had an average financial toxicity score 1.02 points higher than participants of higher SES (95% confidence interval [CI], 0.08–1.95). Participants 65 years and older had an average financial toxicity score 2.58 points lower than participants under 65 (95% CI, −3.41, −1.74). Participants identifying as Black or as a race other than Black or White had an average financial toxicity score 1.91 points (95% CI, 0.46–3.37) and 2.55 points (95% CI, 1.11–3.99) higher, respectively, than participants who self‐reported as White. These results were similar at 12 weeks postsurgery, except that being a race other than White or Black was not significantly associated with financial toxicity at 12 weeks postsurgery. Being younger than 65 years and of lower SES was associated with higher financial toxicity scores at 1 year postsurgery. Table 3 shows crude and adjusted results of the financial toxicity analysis.
Table 3.
Bivariate statistics and adjusted coefficients from linear regressions examining financial toxicity scores
| 1 week postsurgery | 12 weeks postsurgery | 1 year postsurgery | ||||
|---|---|---|---|---|---|---|
| Bivariate statistic, p value | Adjusted coeff. a (95% CI) | Bivariate statistic, p value | Adjusted coeff. a (95% CI) | Bivariate statistic, p value | Adjusted coeff. a (95% CI) | |
| Lower SES (vs. higher SES) | t = −3.50, p = .0005 | 1.02 (0.08, 1.95) b | t = −2.94, p = .004 | 1.04 (0.05, 2.06) b | t = −2.73, p = .007 | 2.17 (0.49, 3.85) b |
| 65 years and older (vs. <65) | t = 5.99, p < .0001 | −2.58 (−3.41, −1.74) b | t = 5.82, p < .0001 | −2.57 (−3.48, −1.67) b | t = 4.27, p < .0001 | −3.57 (−5.08, −2.05) b |
| Race | F = 11.65, p < .0001 | — | F = 4.58, p = .011 | — | F = 3.70, p = .028 | — |
| White | — | referent | — | referent | — | referent |
| Black | — | 1.91 (0.46, 3.37) b | — | 2.59 (1.04, 4.15) b | — | 2.48 (−0.73, 5.69) |
| Other | — | 2.55 (1.11, 3.99) b | — | 1.27 (−0.32, 2.86) | — | 0.13 (−2.42, 2.67) |
| Mastectomy (vs. Lumpectomy) | t = −0.77, p = .44 | −0.25 (−1.29, 0.79) | t = 0.12, p = .90 | −0.46 (−1.66, 0.74) | t = −1.05, p = .30 | −0.76 (−3.12, 1.60) |
| Stage (I, II, or III) | F = 3.57, p = 0.03 | — | F = 3.66, p = .027 | — | F = 3.30, p = .040 | — |
| Stage I | — | referent | — | referent | — | referent |
| Stage II | — | 0.44 (−0.49, 1.37) | — | 1.17 (0.16, 2.19) b | — | 1.15 (−0.60, 2.90) |
| Stage III | — | 3.31 (0.32, 6.29) b | — | 1.26 (−2.10, 4.62) | — | 9.32 (0.31, 18.3) b |
| Site | ||||||
| Site 1 | — | referent | — | referent | — | referent |
| Site 2 | — | −1.86 (−3.34, −0.38) b | — | −2.24 (−3.83, −0.65) b | — | 0.09 (−3.43, 3.61) |
| Site 3 | — | −1.93 (−3.67, −0.20) b | — | −0.95 (−2.87, 0.98) | — | −1.28 (−4.51, 1.96) |
| Site 4 | — | −1.33 (−2.38, −0.28) b | — | −1.30 (−2.41, −0.19) | — | −0.58 (−2.89, 1.74) |
| Random effect SD estimates (SE) | ||||||
| Clinic | — | 3.51e‐20 (4.98e‐19) | — | 3.35e‐19 (6.12e‐18) | — | 1.03e‐17 (NA) |
| Surgeon | — | 2.00e‐19 (1.91e‐18) | — | 2.02e‐19 (2.18e‐18) | — | 0.82 (2.27) |
Adjusted for participant SES (high vs. low), age (≥65 vs. less than 65), race (White vs. Black vs. other), surgery choice (breast‐conserving surgery vs. mastectomy), cancer stage (I vs. II vs. III), and study site as fixed effects and surgeon and clinic as random effects.
p < .05.
Abbreviations: CI, confidence interval; coeff., coefficient; SES, socioeconomic status.
Aim 3. Correlation Between Financial Toxicity and Out‐of‐Pocket Expenses
In simple linear regression analyses, financial toxicity and out‐of‐pocket medical expenses were positively associated at all three time points (p < .001). In the mixed‐effects multivariable linear regression analyses, the relationship remained significant at 1 week and 12 weeks postsurgery (p < .001) while controlling for cancer stage, surgery, demographics, and surgeon‐ and clinic‐level clusters. In this model, for every 10% increase in out‐of‐pocket costs, financial toxicity scores were 0.04 higher at 1 week postsurgery (95% CI, 0.02–0.05) and 0.05 points higher at 12 weeks postsurgery (95% CI, 0.03–0.06). In multivariable linear regression analyses, out‐of‐pocket costs and financial toxicity were not significantly correlated at 1 year postsurgery. Table 4 shows the crude and adjusted linear regression results.
Table 4.
Crude and adjusted linear regression coefficients assessing the relationship between financial toxicity and self‐reported out‐of‐pocket costs by time point
| 1 week postsurgery | 12 weeks postsurgery | 1 year postsurgery | ||||
|---|---|---|---|---|---|---|
| Crude coeff. | Adjusted coeff. a | Crude coeff. | Adjusted coeff. a | Crude coeff. | Adjusted coeff. a | |
| OOP costs, b mean ± SD | $1,027 ± $1,856 | — | $1,944 ± $5,610 | — | $2,533 ± $4,590 | — |
| Financial toxicity, mean ± SD | 6.4 ± 4.2 | — | 6.2 ± 4.3 | — | 6.2 ± 4.8 | — |
| OOP costs coefficient (95% CI) | 0.03 (0.01, 0.06) | 0.04 (0.02, 0.05) | 0.04 (0.02, 0.05) | 0.05 (0.03, 0.06) | 0.06 (0.04, 0.09) | 0.01 (−0.0004, 0.03) |
| z‐score | 3.69 | 5.03 | 5.37 | 7.23 | 5.26 | 1.92 |
| p value | <.001 | <.001 | <.001 | <.001 | <.001 | .055 |
| n | 268 | 259 | 257 | 250 | 94 | 74 |
Adjusted for participant SES (high vs. low), age (≥65 vs. less than 65), race (White vs. Black vs. other), surgery choice (breast‐conserving surgery vs. mastectomy), cancer stage (I vs. II vs. III), and study site as fixed effects and surgeon and clinic as random effects. Transformed out of log version for interpretation using the following formula: coefficient*log(1.10) to look for a difference based on 10% increase in out‐of‐pocket costs.
Self‐reported out‐of‐pocket costs related to breast cancer care.
Abbreviations: CI, confidence interval; coeff., coefficient; OOP, out‐of‐pocket.
Sensitivity Analysis with Patients as a Random Effect
In the sensitivity analyses adding patient as a random effect to the multilevel models, results remained consistent except that there was no longer an association between out‐of‐pocket costs and race. Higher out‐of‐pocket costs remained associated with lower SES and being 65 years or older. Reporting zero out‐of‐pocket costs remained associated with lower SES and being aged at least 65 years. Higher financial toxicity scores remained associated with lower SES, being aged less than 65 years, and being of Black race or a race other than Black or White. Financial toxicity and out‐of‐pocket costs were also associated with having stage II cancer versus stage I cancer. Financial toxicity and out‐of‐pocket costs remained associated with each other (Z = 8.29, p < .001; supplemental online Table 2).
Discussion
To our knowledge, this study was one of the first to examine the impact of breast cancer on patients’ out‐of‐pocket costs and financial toxicity at multiple time points, up to 1 year postsurgery. In multilevel regression analyses controlling for patient demographic and clinical characteristics, lower SES, older age (65+), and surgeon‐ and clinic‐level clusters were associated with lower out‐of‐pocket costs at each time point. Younger age, Black race, race other than Black or White, and lower socioeconomic status were associated with higher financial toxicity. Higher out‐of‐pocket costs were significantly related to higher financial toxicity at 1 week and 12 weeks postsurgery.
Findings highlight the importance of addressing patients’ financial toxicity in several ways, particularly for groups vulnerable to its effects. Lowering out‐of‐pocket costs for patients with breast cancer should be the first priority when intervening to reduce financial toxicity, given the positive relationship between the two variables in our analyses. For example, clinicians could change logistics of care such that care can be consolidated on days convenient for patients and their employment or life responsibilities [4, 30, 31], such as scheduling multidisciplinary care team appointments on the same day. Clinicians could also prescribe generic versus brand‐name medications, change dosages or frequency of dosages of medications, provide medication samples, facilitate copay assistance, and or even change treatment plans if it helps patients adhere to an evidence‐informed care plan [4, 30, 31]. Lowering patients’ out‐of‐pocket costs could better support adherence to needed cancer care; many patients report delaying or avoiding needed care because of costs [17, 32, 33], which can impact cancer outcomes and quality of life [34].
For some groups (e.g., those of lower SES), however, lowering some out‐of‐pocket costs might not be enough to lower financial toxicity. In this study, lower SES related to both lower out‐of‐pocket costs and higher financial toxicity. Those of lower SES might carry more burden from any increase in out‐of‐pocket costs. In addition, younger age consistently related to higher out‐of‐pocket expenses and higher financial toxicity at each time point. Insurance status could explain some of these findings. Being covered by private insurance with high deductibles or copayments, which we characterized as a higher‐SES trait in our SES composite variable, could lead to higher out‐of‐pocket costs [35]. Similarly, Medicaid health coverage for low‐income individuals may be responsible for the lower out‐of‐pocket costs reported in the low‐SES group. The lower out‐of‐pocket expenses reported by individuals aged 65 years and older are consistent with that group's access to Medicare health coverage.
Those of a race other than White also reported higher financial toxicity. This finding is consistent with the racial wealth gap in the U.S. [36], a persistent disparity perpetuated by political, social, and institutional factors [37] that may better allow White patients to absorb financial shocks such as those resulting from costs of cancer care. Screening for financial toxicity could identify vulnerable patients who could benefit from a referral to support staff to discuss care cost information [38]. Cancer centers could include resources either internally (e.g., financial navigators [39], which have been shown to reduce patients’ financial burden and anxiety and are recommended as part of treatment planning [40, 41]) or in in the region (e.g., certified application counselors or health insurance navigators) to discuss insurance options with patients [38, 42, 43]. For groups that are vulnerable to increased burden from care costs, facilitating insurance choices [35, 42, 43, 44] to best match their needs and providing broader social services could be needed. These services could be particularly relevant given the coronavirus pandemic and the high rates of unemployment, insurance loss, and subsequent financial hardship in the U.S. [45].
This study had several key strengths, including examining the relationship between financial toxicity and out‐of‐pocket expenses up to 1 year postsurgery, the diverse sample recruited from several geographic regions in the U.S., the analyses collected over time up to 1 year postsurgery, and the robust analysis plan to account for potential surgeon‐ and clinic‐level clusters.
Findings should be interpreted within the context of some study limitations. Participants self‐reported out‐of‐pocket costs, but we did not examine insurance claims data to verify true costs. Large national surveys such as the Medical Expenditure Panel Survey and National Health Interview Survey ask participants to self‐report out‐of‐pocket expenses [28, 29], but these might be subject to recall bias. Some participants reported zero costs, which could have indicated that they could not estimate their out‐of‐pocket costs accurately. Answering “I don't know” was a possible response but was not selected by participants who reported zero costs. We examined results with and without those reporting zero costs, and results did not change. We controlled for clinical stage of disease but did not have information about whether or not patients had chemotherapy, which can be associated with high care costs. SES was calculated using a combination of insurance status, income (federal poverty level), and educational attainment, but future studies could examine other ways to measure and calculate this construct. Including insurance as one part of SES meant we could not look at individual constructs that made up this variable, such as insurance status. To check the robustness of our SES variable, we added insurance as a covariate to our models; in our analyses, we kept SES the way we originally calculated it when results largely remained consistent. Future studies should examine how both insurance and SES relate to costs and financial toxicity. Moreover, not all patients completed surveys at each time point. Study attrition at the first analysis point (1 week postsurgery) largely occurred when patients were no longer eligible for the parent study after consent (50.6%) or because they transferred care to another center (20.7%). Attrition at 1 year postsurgery mostly occurred because we did not contact all study participants given the grant timeline (83.6% of those who were not included at 1 year postsurgery). Finally, these data are secondary analyses of a parent randomized trial; we included clinic and surgeon in our adjusted analyses to control for the potential impact of surgeon‐ and clinic‐level clusters on our outcomes of interest. We also conducted a robustness check to account for repeated measurements.
Conclusion
This study was one of the first to examine out‐of‐pocket costs and financial toxicity up to 1 year after breast cancer surgery. Future studies could examine these findings in a larger sample of women with varying demographic and clinical risk factors for financial toxicity, using claims data to verify out‐of‐pocket costs. Studies could also examine ways to offset high costs of cancer care to lower financial toxicity among women vulnerable to experiencing high burden of cancer care costs; this, in turn, could support adherence to cancer care, clinical outcomes, and patients’ quality of life.
Author Contributions
Conception/design: Mary C. Politi, Renata W. Yen, Glyn Elwyn, Marie‐Anne Durand
Collection and/or assembly of data: Renata W. Yen, Catherine H. Saunders, Danielle Schubbe
Data analysis and interpretation: Mary C. Politi, Renata W. Yen, Glyn Elwyn, A. James O'Malley, Marie‐Anne Durand
Manuscript writing: Mary C. Politi, Renata W. Yen, Glyn Elwyn, A. James O'Malley, Catherine H. Saunders, Danielle Schubbe, Rachel Forcino, Marie‐Anne Durand
Final approval of manuscript: Mary C. Politi, Renata W. Yen, Glyn Elwyn, A. James O'Malley, Catherine H. Saunders, Danielle Schubbe, Rachel Forcino, Marie‐Anne Durand
Disclosures
Mary C. Politi: Merck (RF); Glyn Elwyn: EBSCO Health (C/A); Catherine H. Saunders: consideRATE suite of tools for serious illness (IP); Marie‐Anne Durand: EBSCO Health (C/A). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
Supporting information
See http://www.TheOncologist.com for supplemental material available online.
Supplementary Tables
Acknowledgments
Financial support for this study was provided by a grant from Patient‐Centered Outcomes Research Institute (PCORI; 1511‐32875). The statements presented in this article are solely the responsibility of the authors and do not necessarily represent the views of the Patient‐Centered Outcomes Research Institute, its Board of Governors, or its Methodology Committee.
Disclosures of potential conflicts of interest may be found at the end of this article.
References
- 1. Witte J, Mehlis K, Surmann B et al. Methods for measuring financial toxicity after cancer diagnosis and treatment: A systematic review and its implications. Ann Oncol 2019;30:1061–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shih YCT, Smieliauskas F, Geynisman DM et al. Trends in the cost and use of targeted cancer therapies for the privately insured nonelderly: 2001 to 2011. J Clin Oncol 2015;33:2190–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Azzani M, Roslani AC, Su TT. The perceived cancer‐related financial hardship among patients and their families: A systematic review. Support Care Cancer 2015;23:889–898. [DOI] [PubMed] [Google Scholar]
- 4. Bestvina CM, Zullig LL, Rushing C et al. Patient‐oncologist cost communication, financial distress, and medication adherence. J Oncol Pract 2014;10:162–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McGuire A, Drummond M, Martin M et al. End of life or end of the road? Are rising cancer costs sustainable? Is it time to consider alternative incentive and funding schemes? Expert Rev Pharmacoecon Outcomes Res 2015;15:599–605. [DOI] [PubMed] [Google Scholar]
- 6. Kale HP, Carroll NV. Self‐reported financial burden of cancer care and its effect on physical and mental health‐related quality of life among US cancer survivors. Cancer 2016;122:283–289. [DOI] [PubMed] [Google Scholar]
- 7. Fenn KM, Evans SB, McCorkle R et al. Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract 2014;10:332–338. [DOI] [PubMed] [Google Scholar]
- 8. Jan S, Kimman M, Peters S et al. Financial catastrophe, treatment discontinuation and death associated with surgically operable cancer in South‐East Asia: Results from the ACTION study. Surgery 2015;157:971–982. [DOI] [PubMed] [Google Scholar]
- 9. Ramsey SD, Bansal A, Fedorenko CR et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol 2016;34:980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gilligan AM, Alberts DS, Roe DJ et al. Death or debt? National estimates of financial toxicity in persons with newly‐diagnosed cancer. Am J Med 2018;131:1187–1199.e5. [DOI] [PubMed] [Google Scholar]
- 11. Zafar SY. Financial toxicity of cancer care: It's time to intervene. J Natl Cancer Inst 2015;108:djv370. [DOI] [PubMed] [Google Scholar]
- 12. Zafar SY, Peppercorn JM, Schrag D et al. The financial toxicity of cancer treatment: A pilot study assessing out‐of‐pocket expenses and the insured cancer patient's experience. The Oncologist 2013;18:381–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chino F, Peppercorn JM, Rushing C et al. Out‐of‐pocket costs, financial distress, and underinsurance in cancer care. JAMA Oncol 2017;3:1582–1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kaisaeng N, Harpe SE, Carroll NV. Out‐of‐pocket costs and oral cancer medication discontinuation in the elderly. J Manag Care Spec Pharm 2014;20:669–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Smith KT, Monti D, Mir N et al. Access is necessary but not sufficient: Factors influencing delay and avoidance of health care services. MDM Policy Pract 2018;3:2381468318760298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Abelson R. Women with breast cancer delay care when faced with high deductibles. New York Times, May 4, 2018. Available at https://www.nytimes.com/2018/05/04/health/breast-cancer-insurance-deductibles.html. . [Google Scholar]
- 17. Kent EE, Forsythe LP, Yabroff KR et al. Are survivors who report cancer‐related financial problems more likely to forgo or delay medical care? Cancer 2013;119:3710–3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Han X, Zhao J, Zheng Z et al. Medical financial hardship intensity and financial sacrifice associated with cancer in the United States. Cancer Epidemiol Biomarkers Prev 2020;29:308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ramsey SD, Bansal A, Fedorenko CR et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol 2016;34:980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. De Souza JA, Yap BJ, Wroblewski K et al. Measuring financial toxicity as a clinically relevant patient‐reported outcome: The validation of the Comprehensive Score for financial Toxicity (COST). Cancer 2017;123:476–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mady LJ, Lyu L, Owoc MS et al. Understanding financial toxicity in head and neck cancer survivors. Oral Oncol 2019;95:187–193. [DOI] [PubMed] [Google Scholar]
- 22. Bouberhan S, Shea M, Kennedy A et al. Financial toxicity in gynecologic oncology. Gynecol Oncol 2019;154:8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Huntington SF, Weiss BM, Vogl DT et al. Financial toxicity in insured patients with multiple myeloma: a cross‐sectional pilot study. Lancet Haematol 2015;2:e408–e416. [DOI] [PubMed] [Google Scholar]
- 24. Narang AK, Nicholas LH. Out‐of‐pocket spending and financial burden among Medicare beneficiaries with cancer. JAMA Oncol 2017;3:757–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Morello RJ, Bramley TJ, Hennenfent K et al. Cancer‐Related Financial Toxicity and Its Pervasive Effects on Patients and Families: Solving a National Health and Economic Crisis Hiding in Plain Sight. Boston, MA: FamilyReach, 2018. [Google Scholar]
- 26. Durand MA, Yen RW, O'Malley AJ et al. What matters most: Protocol for a randomized controlled trial of breast cancer surgery encounter decision aids across socioeconomic strata. BMC Public Health 2018;18:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. de Souza JA, Yap BJ, Hlubocky FJ et al. The development of a financial toxicity patient‐reported outcome in cancer: The COST measure. Cancer 2014;120:3245–3253. [DOI] [PubMed] [Google Scholar]
- 28. National Health Interview Survey . Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention.
- 29. Medical Expenditure Panel Survey . Rockville, MD: Agency for Healthcare Research and Quality. [PubMed]
- 30. Tina SYC, Chun‐Ru C. A review of cost communication in oncology: Patient attitude, provider acceptance, and outcome assessment. Cancer 2017;123:928–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zafar SY, Chino F, Ubel PA et al. The utility of cost discussions between patients with cancer and oncologists. Am J Manag Care 2015;21:607–615. [PubMed] [Google Scholar]
- 32. Tipirneni R, Politi MC, Kullgren JT et al. Association between health insurance literacy and avoidance of health care services owing to cost. JAMA Network Open 2018;1:e184796–e184796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Farias AJ, Hansen RN, Zeliadt SB et al. The association between out‐of‐pocket costs and adherence to adjuvant endocrine therapy among newly diagnosed breast cancer patients. Am J Clin Oncol 2018;41:708–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tran G, Zafar SY. Financial toxicity and implications for cancer care in the era of molecular and immune therapies. Ann Transl Med 2018;6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wharam JF, Zhang F, Wallace J et al. Vulnerable and less vulnerable women in high‐deductible health plans experienced delayed breast cancer care. Health Aff (Millwood) 2019;38:408–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Urban Institute . Nine charts about wealth inequality in America. 2017. Available at http://apps.urban.org/features/wealth‐inequality‐charts/. Accessed May 10, 2020.
- 37. Dickman SL, Himmelstein DU, Woolhandler S. Inequality and the health‐care system in the USA. Lancet 2017;389:1431–1441. [DOI] [PubMed] [Google Scholar]
- 38. Association of Community Cancer Centers . ACCC Financial Advocacy Network Shared Decision Making Summit Executive Summary. Washington, DC: Association of Community Cancer Centers, 2018. [Google Scholar]
- 39. Shankaran V, Leahy T, Steelquist J et al. Pilot feasibility study of an oncology financial navigation program. J Oncol Pract 2018;14:e122–e129. [DOI] [PubMed] [Google Scholar]
- 40. Gesme DH, Wiseman M. A financial counselor on the practice staff: A win‐win. J Oncol Pract 2011;7:273–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Van Dyck G. Financial counselors: A must have in oncology. In: Association of Community Cancer Centers 2017 Patient Assistance and Reimbursement Guide, 2017. Available at https://www.accc‐cancer.org/docs/documents/publications/patient‐assistance‐guide‐2017‐article.pdf?sfvrsn=213d0e80_6. Accessed September 27, 2020.
- 42. Politi MC, Kuzemchak MD, Liu J et al. Show me my health plans: Using a decision aid to improve decisions in the federal health insurance marketplace. MDM Policy Pract 2016;1:2381468316679998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. George N, Grant R, James A et al. Burden associated with selecting and using health insurance to manage care costs: Results of a qualitative study of nonelderly cancer survivors. Med Care Res Rev 2018. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 44. Politi MC, Grant RL, George NP et al. Improving cancer patients’ insurance choices (I Can PIC): A randomized trial of a personalized health insurance decision aid. The Oncologist 2020;25:609–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Garfield R, Claxton G, Damico A et al. Eligibility for ACA Health Coverage Following Job Loss. San Francisco, CA: Kaiser Family Foundation, 2020. Available at https://www.kff.org/coronavirus‐covid‐19/issue‐brief/eligibility‐for‐aca‐health‐coverage‐following‐job‐loss/. Accessed October 5, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
See http://www.TheOncologist.com for supplemental material available online.
Supplementary Tables


