To the Editor:
Atopic dermatitis (AD) is an itchy, inflammatory skin condition associated with multiple comorbidities. Observational epidemiology suggests an increased prevalence of obesity in patients with AD, but (1) whether there is a causal effect and (2) whether obesity leads to AD or vice versa remain unclear. Genetic predisposition to obesity has been shown to promote psoriasis,1 but dermatologic disorders can also lead to reduced participation in physical activity, resulting in weight gain. We aimed to investigate evidence of causality in the association of AD with elevated body mass index (BMI).
We meta-analyzed 33 published studies examining the association between obesity or elevated BMI and AD to summarize available observational data (see Fig E1 in this article’s Online Repository at www.jacionline.org). The odds ratio (OR) for AD in overweight individuals was 1.05 (95% CI = 0.94-1.19) in adults (n = 51,008) and 1.08 (95% CI = 1.00-1.16) in children (n = 506,202) (see Fig E2 in this article’s Online Repository at www.jacionline.org). For obese individuals, the OR for having AD was 1.19 (95% CI = 0.95-1.49) in adults (n = 1,400,679) and 1.20 (95% = CI 1.11-1.30) in children (n = 796,514) (see Fig E3 in this article’s Online Repository at www.jacionline.org); the methods and results are detailed in the Methods and Results sections of the Online Repository (at www.jacionline.org). We extended the observational analysis by using 2 large population-based studies from the United Kingdom and Norway2,3 (for details, see the Online Repository and Tables E1-E4). Among overweight individuals (BMI of 25-30 kg/m2), the OR of AD was 1.02 per each 1-kg/m2 increase in BMI (95% CI = 1.00-1.04; P = .07; 4,820 cases and 130,776 controls); a similar estimate was found among obese individuals (BMI >30 kg/m2) (ie, OR =1.02 [95% CI = 1.01-1.03; P = 3.3 × 10–4] in a sample of 2,741 cases and 73,907 controls) (see Fig E4 in this article’s Online Repository at www.jacionline.org).
Observational epidemiology has several limitations, including bias from confounding and reverse causation; this restricts its utility for causal inference. However, causality and the direction of effect can be investigated by mendelian randomization (MR). MR uses genetic variants as a proxy for the exposure (eg, BMI) to estimate the effect on an outcome (eg, AD). Genetic variants are randomly allocated at fertilization, therefore avoiding confounding; they are not affected by outcomes later in life, thus avoiding reverse causation. Genome-wide association studies (GWASs) have identified single-nucleotide polymorphisms (SNPs) associated with BMI (≤941 loci4,5) and AD (24 loci in European populations6). These SNPs can be combined into a genetic risk score (GRS) or “genetic instrument” that acts as a proxy for the specified trait during MR.
We conducted MR analysis by using data from the largest population-based studies in the United Kingdom (UK Biobank2) and Norway (Nord-Trøndelag Health Study, Norway3 [HUNT, 2006-08]) along with the largest published GWASs for BMI4,5 and AD6 to date, representing a total of 742,611 individuals (see Table E5 in this article's Online Repository at www.jacionline.org). One-sample MR was performed in the UK Biobank and HUNT data sets with the individuals’ BMI SNPs, measured BMI, and AD status. Two-sample MR using published GWAS data4, 5, 6 was performed and meta-analyzed with the 1-sample estimate to obtain an overall causal estimate. Similarly, reverse MR was conducted to investigate the effect of AD genetic risk on BMI. Methodologic details and sensitivity analysis are described in the Online Repository, including Fig E5.
The BMI GRS was strongly associated with BMI in both the UK Biobank and HUNT data sets (see Figs E6 and E7 in this article’s Online Repository at www.jacionline.org), supporting its use as a genetic instrument. Potential confounders of the GRS-BMI association were detected (see Figs E6-E9), but the magnitudes were minimal in comparison with the strength of association with BMI. Similarly, the AD GRS was a good predictor of AD in both the UK Biobank (OR = 1.26 [95% CI = 1.23-1.28]; F-statistic = 2036; R2 = 0.7%) and HUNT (OR = 1.15 [95% CI = 1.11-1.21]; F-statistic = 97; R2 = 0.4%) data sets, despite lacking an FLG null genotype (R501X/rs61816761), which is known to show strong association with AD.
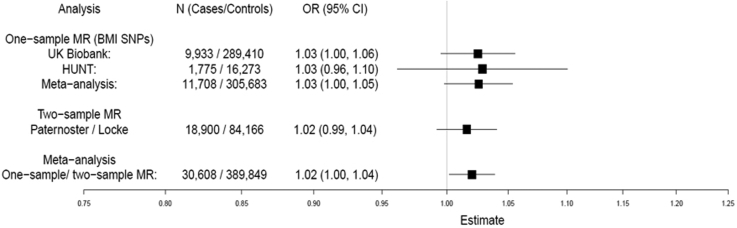
Meta-analyzed 1- and 2-sample MRs show evidence of a small causal effect of higher BMI increasing the risk of AD (OR = 1.02 [95% CI = 1.00-1.04]; P = .03) (Fig 1). This represents an increase in AD risk by approximately 2% for each 1-kg/m2 increase in BMI, which is remarkably similar to the observational estimate (see Figs E2 and E3 in the Online Repository). Importantly, sensitivity analyses showed little evidence of pleiotropy (for details, see the Sensitivity Analysis section, Table E6, Fig E10, and Fig E11 in this article’s Online Repository at www.jacionline.org) or heterogeneity among the individual SNP effect estimates (UK Biobank Q = 101.07 [P = .32]; HUNT Q = 100.04 [P = .37]). Two-sample MR using the larger number of recently published BMI SNP estimates (941 SNPs)4 gave similar evidence of a causal effect on AD risk (OR = 1.08 [95% CI = 1.01-1.16]; P =.02).
Fig 1.
MR analysis of the causal effect of BMI on AD. Meta-analysis of 1-sample and 2-sample MR estimates using individual BMI SNPs as instruments. Estimates are given per 1-kg/m2 increase in BMI.
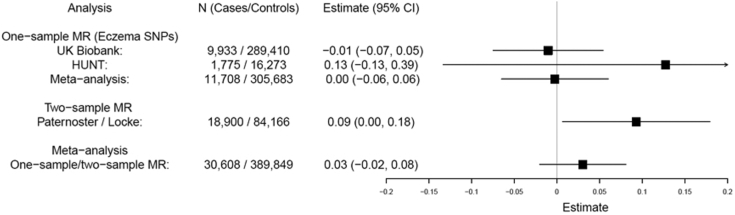
In the reverse direction, meta-analysis gave weak evidence of a very small causal effect (Fig 2): a 0.03-kg/m2 change in BMI per doubling odds of AD (95% CI = –0.02 to 0.08; P = .24). There was little evidence of pleiotropy but modest heterogeneity among the individual SNP effects (see Fig E12 and Table E7 in in this article’s Online Repository at www.jacionline.org). The difference in BMI between patients with AD and controls estimated in 1-sample MR (0.15 kg/m2, 95% CI -1.97 to 2.27) was small compared with observational estimates (see Tables E1 and E2), indicating that the association is mainly explained by the causal effect of BMI on AD.
Fig 2.
Reverse direction MR analysis: effect of AD genetic risk on BMI. Meta-analysis of 1-sample and 2-sample MR estimates using individual AD SNPs as instrumental variables. Estimates represent change in BMI (kg/m2) per doubling odds of AD.
The association of obesity with cardiometabolic disease and systemic inflammation is now well recognized, and clinical guidelines recommend screening patients with psoriasis for obesity. The presence of a causal effect and the direction of effect are both clinically relevant, to define a primary target (ie, obesity) for intervention. Our MR analysis shows evidence that higher BMI increases the risk of AD (ie, a 2% increase in disease risk for each 1-kg/m2 increase in BMI). Conversely, there was no strong evidence of a causal effect of AD genetic risk on BMI; the estimate of 0.03 kg/m2 suggests that genetic risk for AD has little meaningful influence on an individual’s BMI. These findings may be compared with the causal effect of BMI on psoriasis and lack of effect of psoriasis genetic risk on BMI.1 The effect of BMI on AD is more modest than the effect size observed in psoriasis, but the high prevalence of obesity (in more than one-third of US adults) and AD (in ≤10% of adults) demonstrate the potential importance of this causal effect on a population scale.
The molecular mechanisms by which obesity contributes to skin inflammation remain unclear. Excess adipose tissue secretes proinflammatory cytokines and hormones,7 and atopic inflammation may be promoted by disruption of the epidermal barrier in obese individuals.8 Changes in the adipocytes and lymphatic vessels may also contribute to obesity-related skin inflammation.8 Research to define mechanisms underlying the causal relationship demonstrated by MR may identify novel therapeutic targets.
Our MR analyses have various strengths as well as weaknesses. The large sample size is powerful, and the genetic instruments are strong. The 2-sample analysis included an overlap of data sources (from the HUNT study), which has the potential to bias the causal estimate, but this bias would be in the direction of the null. There is the possibility of misclassification of AD, and because AD often shows remission in childhood, this phenotype may be particularly susceptible to recall bias in adult studies; however, this would likely drive any estimate toward the null. It is also important to note that the MR methodology applied here does not define temporal relationship. Genetic risk has a lifetime effect and therefore predates disease onset, but a causal effect determined by MR does not rely on obesity occurring before the onset of AD. However, when we attempted to mitigate this issue by repeating the MR analyses using SNPs that are strongly associated with childhood BMI,9 a causal estimate with the same direction of effect was obtained (OR = 1.04; 95% CI = 1.01-1.07; P = .01). Nevertheless, replication of these analyses within pediatric cohorts with large sample sizes would be valuable future work.
In conclusion, we have found evidence of a small but potentially important causal effect of BMI on AD. Clinical trials have shown that interventions to promote weight loss can lead to improvement in psoriasis, but this approach has not been tested in AD. The results of our study provide support for the investigation of obesity management strategies and/or targeting of the adipocyte-keratinocyte cross-talk as therapeutic opportunities for AD. This may contribute to the prevention of AD, as well as to a reduction in the population prevalence of this chronic disease.
Acknowledgments
This research was conducted by using data from the UK Biobank Resource (application number 10074) and the Nord-Trøndelag Health Study (the HUNT Study). Details of patient and public involvement in the UK Biobank are available online (http://www.ukbiobank.ac.uk/about-biobank-uk/ and https://www.ukbiobank.ac.uk/wp-content/uploads/2011/07/Summary-EGF-consultation.pdf?phpMyAdmin=trmKQlYdjjnQIgJ%2CfAzikMhEnx6). The UK Biobank data set used to conduct the research in this article is available via application directly to the UK Biobank. Applications are assessed for meeting the required criteria for access, including legal and ethics standards. More information regarding data access can be found at the following website: http://www.ukbiobank.ac.uk/scientists-3/. Data from the HUNT Study used in research projects will, when reasonably requested by others, be made available on request to the HUNT Data Access Committee (hunt@medisin.ntnu.no). The HUNT data access information (available at: http://www.ntnu.edu/hunt/data) describes in detail the policy regarding data availability. No patients were specifically involved in setting the research question or the outcome measures, nor were they involved in developing plans for recruitment, design, or implementation of this study. No patients were asked to advise on interpretation or writing up of results. There are no specific plans to disseminate the results of the research to study participants, but the UK Biobank and the HUNT Study disseminate key findings from projects on their websites. The HUNT Study is a collaboration between HUNT Research Centre (Faculty of Medicine and Health Sciences, NTNU, Norwegian University of Science and Technology), Nord-Trøndelag County Council, Central Norway Regional Health Authority, and the Norwegian Institute of Public Health. We acknowledge the permission of the EAGLE consortium (including 23andMe) to use results from their previous GWAS of AD (Paternoster et al6).
Footnotes
A.B-A. is funded by a grant awarded to L.P. by the British Skin Foundation (8010 Innovative Project). A.B-A, L.P., S.W., and G.D.S. work in a research unit funded by the UK Medical Research Council (MC_UU_00011/1). B.B., M.L., L.G.F., and B.O.A. work in a research unit funded by Stiftelsen Kristian Gerhard Jebsen, Faculty of Medicine and Health Sciences, NTNU; The Liaison Committee for Education, Research, and Innovation in Central Norway; and the Joint Research Committee between St. Olav's Hospital and the Faculty of Medicine and Health Sciences, NTNU. J.T. is supported by an Academy of Medical Sciences Springboard award, which is supported by the Academy of Medical Sciences, the Wellcome Trust, GCRF, the Government Department of Business, Energy and Industrial strategy, the British Heart Foundation, and Diabetes UK. E.H.M. was supported by a research grant from the Liaison Committee for Education, Research and Innovation in Central Norway. G.A.V. is supported by a research grant from the Norwegian Research Council (grant 250335). M.L. is supported by research grants from the Liaison Committee for Education, Research and Innovation in Central Norway. J.B.N. was supported by grants from the Danish Heart Foundation and the Lundbeck Foundation. L.P. is supported by an Academy of Medical Sciences Springboard Award, which is supported by the Wellcome Trust, the Government Department for Business, Energy and Industrial Strategy, the Global Challenges Research Fund, and the British Heart Foundation [SBF003/1094]. S.J.B. holds a Wellcome Trust Senior Research Fellowship in Clinical Science (106865/Z/15/Z) and a British Skin Foundation large project grant. The genotyping in HUNT was financed by the National Institutes of Health; the University of Michigan; the Research Council of Norway; the Liaison Committee for Education, Research, and Innovation in Central Norway; and the Joint Research Committee between St. Olav's Hospital and the Faculty of Medicine and Health Sciences, NTNU. The funders had no influence on study design, data collection and analysis, decision to publish, or preparation of the article.
Disclosure of potential conflict of interest: L. Paternoster has received personal fees from Merck for Scientific Input Engagement related to MR methodology. The rest of the authors declare that they have no relevant conflicts of interest.
Supplementary data
References
- 1.Budu-Aggrey A., Brumpton B., Tyrrell J., Watkins S., Modalsli E.H., Celis-Morales C. Evidence of a causal relationship between body mass index and psoriasis: a mendelian randomization study. PLoS Med. 2019;16 doi: 10.1371/journal.pmed.1002739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sudlow C., Gallacher J., Allen N., Beral V., Burton P., Danesh J. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12 doi: 10.1371/journal.pmed.1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krokstad S., Langhammer A., Hveem K., Holmen T.L., Midthjell K., Stene T.R. Cohort profile: the HUNT study, Norway. Int J Epidemiol. 2013;42:968–977. doi: 10.1093/ije/dys095. [DOI] [PubMed] [Google Scholar]
- 4.Yengo L., Sidorenko J., Kemper K.E., Zheng Z., Wood A.R., Weedon M.N. Meta-analysis of genome-wide association studies for height and body mass index in approximately 700000 individuals of European ancestry. Hum Mol Genet. 2018;27:3641–3649. doi: 10.1093/hmg/ddy271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Locke A.E., Kahali B., Berndt S.I., Justice A.E., Pers T.H., Day F.R. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206. doi: 10.1038/nature14177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paternoster L., Standl M., Waage J., Baurecht H., Hotze M., Strachan D.P. Multi-ancestry genome-wide association study of 21,000 cases and 95,000 controls identifies new risk loci for atopic dermatitis. Nat Genet. 2015;47:1449–1456. doi: 10.1038/ng.3424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakamizo S., Honda T., Kabashima K. Obesity and inflammatory skin diseases. Trends Immunother. 2017;1:67–74. [Google Scholar]
- 8.Yosipovitch G., DeVore A., Dawn A. Obesity and the skin: skin physiology and skin manifestations of obesity. J Am Acad Dermatol. 2007;56:901–916. doi: 10.1016/j.jaad.2006.12.004. [quiz 17-20] [DOI] [PubMed] [Google Scholar]
- 9.Felix J.F., Bradfield J.P., Monnereau C., van der Valk R.J., Stergiakouli E., Chesi A. Genome-wide association analysis identifies three new susceptibility loci for childhood body mass index. Hum Mol Genet. 2016;25:389–403. doi: 10.1093/hmg/ddv472. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.