Abstract
Study Design:
The COrona VIrus Disease-19 (COVID-19) pandemic has disrupted craniomaxillofacial (CMF) surgeons practice worldwide. We implemented a cross-sectional study and enrolled a sample of CMF surgeons who completed a survey.
Objective:
To measure the impact that COVID-19 has had on CMF surgeons by (1) identifying variations that may exist by geographic region and specialty and (2) measuring access to adequate personal protective equipment (PPE) and identify factors associated with limited access to adequate PPE.
Methods:
Primary outcome variable was availability of adequate PPE for health-care workers (HCWs) in the front line and surgeons. Descriptive and analytic statistics were computed. Level of statistical significance was set at P < .05. Binary logistic regression models were created to identify variables associated with PPE status (adequate or inadequate).
Results:
Most of the respondents felt that hospitals did not provide adequate PPE to the HCWs (57.3%) with significant regional differences (P = .04). Most adequate PPE was available to surgeons in North America with the least offered in Africa. Differences in PPE adequacy per region (P < .001) and per country (P < .001) were significant. In Africa and South America, regions reporting previous virus outbreaks, the differences in access to adequate PPE evaporated compared to Europe (P = .18 and P = .15, respectively).
Conclusion:
The impact of COVID-19 among CMF surgeons is global and adversely affects both clinical practice and personal lives of CMF surgeons. Future surveys should capture what the mid- and long-term impact of the COVID-19 crisis will look like.
Keywords: COVID-19, impact, global, craniomaxillofacial, AO CMF, surgeons
Introduction
The pandemic due to severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2 virus) has profoundly affected the way we conduct health services.1 The virus causes COrona VIrus Disease-19 (COVID-19), which encompasses minor symptoms like fever, coughing, and/or dyspnea, but may cause serious health problems in the form of a severe acute respiratory syndrome (SARS) as well.2 COVID-19 presents all health-care workers (HCWs) with complex challenges ranging from occupational exposure to the virus, to complications in treating patients, and changes to established treatment protocols. As the world responds to this crisis with behavior modifications such as social distancing, lockdowns, school closures, and quarantine of suspected cases, HCWs are at the front line to counter coronavirus.3–5
In general, all elective surgical procedures should have been canceled and rescheduled after safe strategies to limit occupational exposure have been identified. For surgeons working in the craniomaxillofacial (CMF) field, the surgical procedures should be limited to those involving emergent airway management, bleeding, infection, surgical management of facial fractures, and oncologic procedures in which a delay in management could affect ultimate outcome.6 CMF surgeons are at high risks of coronavirus exposure because they work in the nasal/nasopharyngeal area, where the highest viral load is located and the SARS-CoV-2 virus (SC-2) is believed to replicate continuously.7 When using power or diathermic instruments, CMF surgeons create aerosols contaminated with viral particles making them vulnerable to aerosol transmissible diseases by way of droplet or particle transmission associated with aerosol-generating procedures (AGPs).8
“Arbeitsgemeinschaft für Osteosynthesefragen” (AO) CMF is a global leading organization that exists to serve surgeons and health-care professionals across the world working in the CMF field. AO CMF is acutely aware of the difficult circumstances the membership faces. AO CMF leadership created an international task force tasked to develop and disseminate recommendations for best surgical practices during the COVID-19 pandemic. The Task Force has already published a guideline with clear recommendations for CMF surgeons including which personal protective equipment (PPE) should be used for AGPs.6
Recently, AO Spine conducted a survey among their members to measure the effect of COVID-19 on practice and provider welfare. The survey has 8 domains, that is, general demographics, personal impact of COVID-19, patient care, governmental and policy actions, financial impact of COVID-19, conduction of research during the COVID-19 crisis, future challenges, and personal well-being, chosen to capture the effect of SC-2 on the individual and community.
The purpose of this study was to measure and describe how COVID-19 has changed and disrupted CMF patient care and to determine if there are geographic differences. A secondary purpose was to measure the adequacy of PPE and identify factors that may limit access to adequate PPE. We hypothesize that most CMF surgeons will not have access to adequate PPE and there will be one or more factors identified associated with inability to access to adequate PPE. By identifying those factors, we hope that addressing those factors will mitigate the inability to access adequate PPE. The specific aims of this study were to design, disseminate, and collect a survey among CMF surgeons, estimate changes in practice, and to compare and contrast changes among geographic regions. We specifically are interested in the availability of PPE, realizing that limited PPE could increase the risk for occupational exposure to SC-2 and development of COVID-19.
Materials and Methods
Ethical Approval
The study protocol has been approved by the medical ethical committee of the Erasmus Medical Centre in Rotterdam, the Netherlands (MEC-2020-0330). The study is conducted following the guidelines proposed by the World Medical Association of Helsinki.9
Study Design
This study is designed as a cross-sectional survey study.
Survey Population and Sample
All surgeons registered in the database of AO CMF, that is, AO CMF community, were eligible to participate in the survey. On April 8, 2020, the AO CMF community (N = 21 491) received an invitation via an eblast-mail from AO CMF headquarters in Davos, Switzerland, to participate in the survey. On April 11, 2020, the survey was sent a second time. The survey was closed on April 12, 2020. The final sample was composed of CMF surgeons who submitted surveys. By completion of the survey the participants gave written informed consent to use their anonymized data for research, according to the ICMJE Recommendations for the Protection of Research Participants.
Survey Administration
AO CMF staff in Davos, Switzerland, collected, deidentified, and registered the completed surveys and sent the data to the Department of Oral and Maxillofacial Surgery, Erasmus Medical Centre, Rotterdam, the Netherlands, for statistical analysis.
Survey Construction and Variables
For this study, the investigators adapted a survey developed by the AO Spine used to evaluate the global impact of COVID-19 on the spine surgeons. The final AO CMF survey contained 77 questions and is available in Online Supplemental Material 1.
The questions surveyed 8 domains: general demographics, personal impact of COVID-19, patient care, governmental and policy actions, financial impact of COVID-19, conduction of research during the COVID-19 crisis, future challenges, and personal well-being. Most were asked as a multiple-choice question. The complete survey is available in Online Supplemental Material 1.
The primary outcome variable was defined as the respondent’s perception of whether there is adequate PPE availability for HCWs in the front line and surgeons coded as yes/no. All variables used for this study are specified below.
Domain—General Demographics
The respondent’s sex was categorized as male or female. Age was grouped into 5 levels: 25 to 34 years, 35 to 44 years, 45 to 54 years, 55 to 64 years, and more than 65 years of age. Geographic region of their practice was classified as Europe, Africa, Asia, Australia, Middle East, North America, and South America. Furthermore, surgeons were asked about the estimated population of where they practice and grouped this variable as <100 000, 100 000 to 500 000, 500 000 to 1 000 000, 1 000 000 to 2 000 000, and >2 000 000 citizens. The respondents could choose from different specialties; Oral and Maxillofacial Surgery, Plastic and Reconstructive Surgery, Ear, Nose, and Throat (ENT), Head and Neck Surgery, Orthopedics, and Other. Moreover, they were asked about previous virus outbreaks in their country and the responses were coded as None, SARS, Swine Flu, or Both. Other questions included coronavirus test status (positive, negative, untested), were performing elective procedures (yes/no), and whether they were following COVID-19 management guidelines (yes/no). The guidelines were further categorized as only the hospital guideline, only the local government guideline, only the national association, only the AO CMF guideline, only the dental association guideline, or two or more guidelines were followed. At last, the respondents were asked about the maximal available PPE. The PPE choices were surgical and/or FFP1 masks only, up to N95/FFP2 masks, or up to FFP3 masks, and/or powered-air purifying respirators (PAPR) systems.
Statistical Analyses
Descriptive statistics were computed for each study variable. Bivariate analysis was computed to measure the association between study variables and the availability of adequate PPE for frontline HCWs and surgeons. For this purpose, a χ2 test or a Fisher’s exact test (Monte Carlo method with a confidence interval of 99%), if the cell count was lower than 5, was used. The level of significance was set at a P value <.05. Sample characteristics are presented per category with their corresponding number of participants and their respective percentages, based on the number of valid cases. Furthermore, the availability of adequate PPE, the guidelines used, the maximal mask protection, and whether elective surgery was performed were graphically visualized in a bar plot by stratifying on region of practice. Differences in distribution were tested by either a χ2 test or a Fisher’s exact test. The same was performed by stratifying on country if there were 10 or more respondents available from the respective country. Next to the country, the place on the list of most confirmed COVID-19 cases per country is depicted, which is retrieved from the data provided by Dong et al.10 Binary logistic regression models were built to assess the influence of region on the own view of adequate availability of PPE for HCWs and surgeons. In the first model, we did not adjust for any other variable. In the second model, the association was adjusted for the maximum mask protection availability, to which guideline was adhered to and to whether there have been previous virus outbreaks in the region. Selection of the variables was based on a discussion between 2 authors on which variables would likely influence or confound the association. Missing data of the included variables were imputed using a multiple imputation method (10 imputations), except for the exposure and outcome variables of the model. The results of the logistic regression were pooled from the imputed data sets and are presented as odds ratios (ORs) with their 95% confidence intervals (95% CIs). The analyses were performed, and the graphs were plotted with the statistical software package Statistical Package for Social Sciences (SPSS) version 25.0, released 2017 (IBM Corp) for Windows. P values ≤.05 were considered statistically significant.
Results
The sample was composed of 511 subjects (2.48%) of the AO CMF community who responded to the survey. Descriptive characteristics of the sample are presented in Table 1. In total, more than two-third of the respondents were male (n = 358, 70.9%), 412 (81.6%) respondents were oral and maxillofacial surgeons, 68% were aged between 25 and 44 years (n = 345). The respondents came from Africa (n = 24, 4.70%), Asia (n = 135, 26.4%), Australia (n = 5, 0.98%), Europe (n = 124, 24.3%), Middle East (n = 28, 5.48%), North America (n = 59, 11.5%), or South America (n = 124, 24.3%).
Table 1.
Characteristics of the survey respondents (n = 511).a
| Total, n (%) | Missing, n (%) | |
|---|---|---|
| Sex | ||
| Male | 358 (70.9) | 6 (1.17) |
| Female | 147 (29.1) | |
| Age | ||
| 25-34 | 171 (33.7) | 3 (0.59) |
| 35-44 | 174 (34.3) | |
| 45-54 | 95 (18.7) | |
| 55-64 | 56 (11.0) | |
| 65+ | 12 (2.36) | |
| Region of practice | ||
| Africa | 24 (4.70) | 12 (2.35) |
| Asia | 135 (26.4) | |
| Australia | 5 (0.98) | |
| Europe | 124 (24.3) | |
| Middle East | 28 (5.48) | |
| North America | 59 (11.5) | |
| South America | 124 (24.3) | |
| City population size | ||
| <100 000 | 39 (7.63) | 4 (0.78) |
| 100 000-500 000 | 105 (20.5) | |
| 500 000-1 000 000 | 95 (18.6) | |
| 1 000 000-2 000 000 | 81 (15.9) | |
| >2 000 000 | 187 (36.6) | |
| Specialty | ||
| Oral and Maxillofacial Surgery | 412 (81.6) | 6 (1.17) |
| Plastic and Reconstructive Surgery | 54 (10.7) | |
| ENT | 25 (4.95 | |
| Head and Neck Surgery | 4 (0.79) | |
| Orthopedics | 4 (0.79) | |
| Other | 6 (1.18) | |
| Previous virus outbreak | ||
| None | 321 (62.8) | 26 (5.09) |
| SARS | 23 (4.50) | |
| Swine Flu | 100 (19.6) | |
| Both | 41 (8.02) | |
| Positive test for COVID-19 | ||
| Yes | 6 (1.33) | 59 (11.5) |
| No | 446 (98.7) | |
| Performing elective CMF surgery | ||
| Yes | 57 (13.3) | 83 (16.2) |
| No | 371 (86.7) | |
| Adequate PPE provision | ||
| Yes | 191 (42.6) | 63 (12.3) |
| No | 257 (57.3) | |
| Impact on research activity | ||
| Increase in productivity | 38 (9.74) | 121 (23.7) |
| No change | 47 (12.1) | |
| Decrease in productivity | 101 (25.9) | |
| Complete stop | 73 (18.7) | |
| I do not engage in research | 131 (33.6) | |
| Are guidelines followed for patient management? | ||
| Yes | 427 (95.7) | 65 (12.7) |
| No | 19 (4.26) |
Abbreviations: CMF, craniomaxillofacial; COVID-19, COrona VIrus Disease-19; PPE, personal protective equipment.
a Percentages are based on the number of valid cases.
What Is the Adequacy of PPE and What Factors Are Associated With Adequate PPE?
Of the respondents, 42.6% (n = 191) reported to have access to adequate PPE (n = 191; Online Supplement Table S1). Details of the bivariate analyses used to identify factors associated with adequate PPE are summarized in Table 2. The availability of PPE among HCWs and surgeons was significantly different by region of practice (P = .041). Moreover, respondents believed the availability of PPE among HCWs and surgeons to be more adequate as the level of maximal protection increased (P < .001). HCWs and surgeons from Africa were less likely to report adequate PPE when compared to their counterparts in Europe (OR 0.31, 95% CI [0.11-0.88]). A similar trend was seen for HCWs and surgeons from South America compared to those from Europe (OR 0.63, 95% CI [0.33-1.02]), although this association was not significant. After adjusting for previous virus outbreaks in that region, adherence to guidelines, and availability of maximal mask protection, the difference between availability of adequate PPE for African and South American surgeons compared to European surgeons was no longer statistically significant (OR 0.45, 95% CI [0.14-1.44] and OR 0.63, 95% CI [0.33-1.18], respectively).
Table 2.
Binary logistic regression for the association between adequate PPE availability and region of practice.a
| Region of practice (n = 441) (adequate PPE/no adequate PPE) |
Model 1b (OR [95% CI]) | Model 2c (OR [95% CI]) |
|---|---|---|
| Adequate PPE | Adequate PPE | |
| Europe (52/61) | Reference | Reference |
| Africa (5/19) | 0.31 [0.11-0.88] | 0.45 [0.14-1.44] |
| Asia (57/67) | 1.00 [0.60-1.66] | 1.18 [0.66-2.12] |
| Australia (3/2) | 1.76 [0.28-10.9] | 1.53 [0.23-10.1] |
| Middle East (15/11) | 1.60 [0.68-3.79] | 2.61 [0.97-7.00] |
| North America (23/24) | 1.12 [0.57-2.22] | 0.98 [0.48-1.99] |
| South America (34/68) | 0.59 [0.34-1.02] | 0.63 [0.33-1.18] |
Abbreviations: CMF, craniomaxillofacial; COVID-19, COrona VIrus Disease-19; HCW: health-care worker; OR: odds ratio; PPE, personal protective equipment.
a Significant associations are bold.
b Unadjusted model.
c Additionally adjusted for previous virus outbreaks, which guidelines are used, which type of maximal mask protection is available for HCWs.
Is Adequate PPE Available for Frontline HCWs?
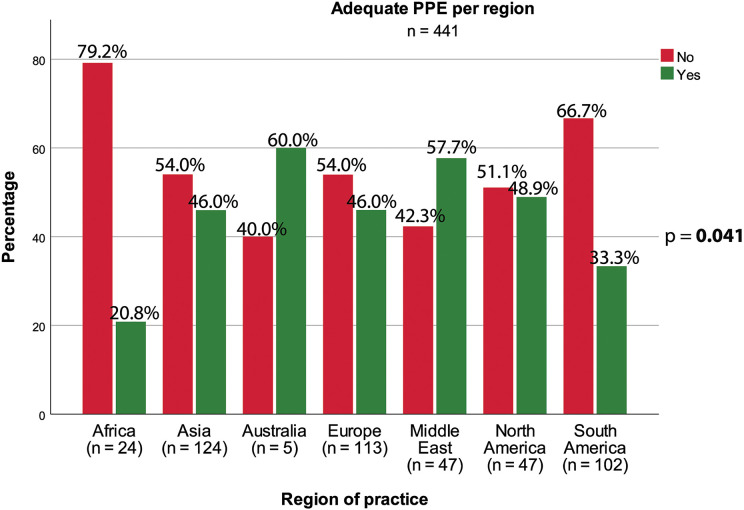
Overall, the vast majority of the AO CMF community globally feels the hospitals do not provide adequate PPE to the frontline HCWs, although regional differences exist (Figure 1). In Africa (79.2%), Asia (54.0%), Europe (54.0%), and South America (66.7%), the majority of the surgeons indicate the hospitals do not provide their frontline HCWs adequate PPE, whereas in Australia (60.0%) and the Middle East (57.7%), the surgeons report their HCWs do receive adequate PPE. Of note, Australia had 5 respondents to the survey and the results should be interpreted cautiously. In North America, the respondents reported that PPE adequacy was similar between HCWs and surgeons (51.0% vs 49.0%, respectively).
Figure 1.
Availability of adequate PPE for HCWs and surgeons per region. HCW indicates health-care worker; PPE, personal protective equipment.
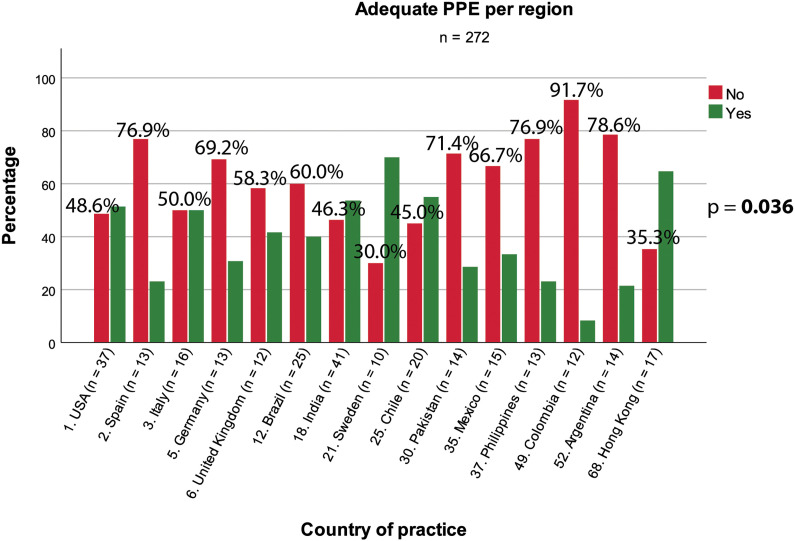
When stratified by country, similar finding as to regions was noted (Figure 2). In all countries, most surgeons believe the hospital do not provide adequate PPE. The percentage of surgeons per country, who report inadequate PPE, was inversely related to the number of confirmed COVID-19 cases per country. The availability of PPE among HCWs and surgeons differed significantly between regions and countries (P = .041 and P = .036, respectively).
Figure 2.
Availability of adequate PPE for HCWs and surgeons per country. Percentages are presented for the category “No Adequate PPE.” HCW indicates health-care worker; PPE, personal protective equipment.
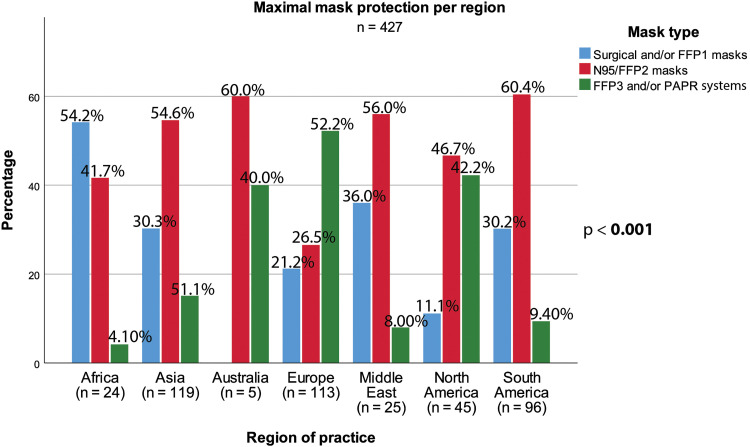
The perceived availability of adequate PPE for HCWs and surgeons significantly differed among regions of practice (see Figure 1) but was associated with the availability of maximal mask protection (P = .041 and P < .001, respectively) (Online Supplemental Table S1). This perception, however, was not dependent on guideline use (P = .083), the city population size (P = .83), previous virus outbreaks (P = .26), or whether elective surgery was performed (P = .43) (see Figure 3 and Online Supplemental Table S2 for details).
Figure 3.
Maximal mask protection for surgeon per region. Percentages are presented for the category “FFP3 and/or PAPR systems.” PAPR indicates powered-air purifying respirators.
What Is the Quality of PPE Offered to the Surgeons?
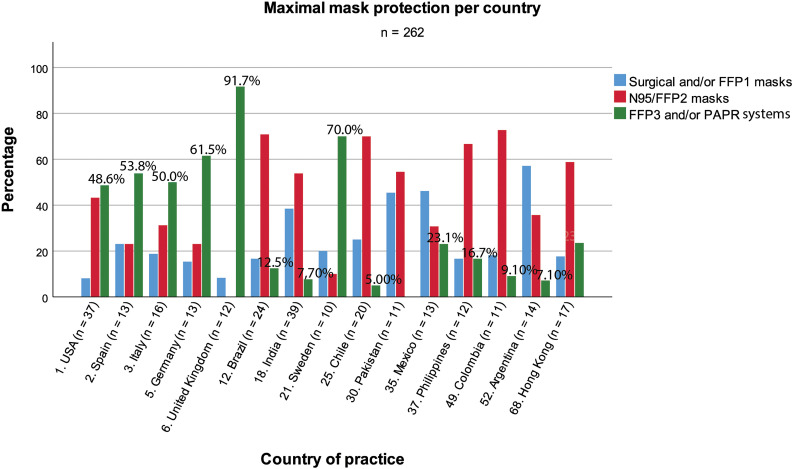
The best protection offered to the surgeons is in Australia, where surgeons can work with N95/FFP2 masks (60.0%) or PAPR systems (40.0%), followed by North America reporting availability of N95/FFP2 masks (47.7%) and PAPR systems (42.2%) (Figure 4). At the other extreme, in Africa, the vast majority of the surgeons have access to only surgical masks as the maximum protection when treating COVID-19 patients. In addition, we also see in other regions that a relatively high percentage of surgeons (Asia 30.3%, Europe 24.2%, Middle East 36.0%, North America 11.1%, and South America 30.2%) have to rely on surgical masks for protection.
Figure 4.
Maximal mask protection for surgeon per country.
Per country most surgeons can rely on either N95/FFP2 masks and/or FFP3/PAPR systems (Figure 3). However, as with the perception of availability of adequate PPE, the quality of maximal mask protection decreases as the ranking of confirmed COVID-19 cases per country decreases. Between both regions and countries, the maximal available protection significantly differed (P < .001 for regions and countries).
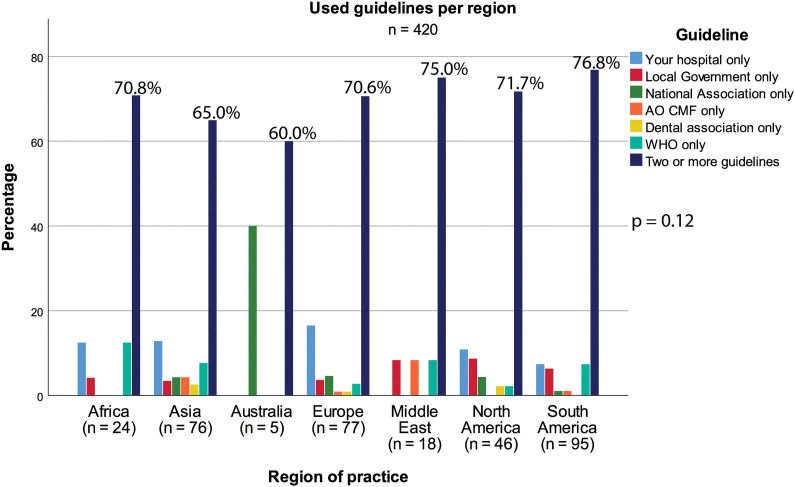
To What Guideline Do Surgeons Adhere?
Most surgeons from all around the globe adhere to more than 1 guideline (Figure 5). In Australia, 40% of the surgeons use the guidelines from their national association, which is high compared to other regions. In Europe, the surgeons are using the guideline provided by their hospital, whereas in North America a mix of guidelines is used, from their hospital, local governments, and national associations. The guideline of the World Health Organization (WHO) is used in Africa, Asia, Middle East, and South Africa. In the Middle East, AO CMF guidelines were preferred. The differences among the regions, however, were not significantly different (P = .12).
Figure 5.
Used guidelines per region. Percentages are presented for the category “Two or more guidelines.”
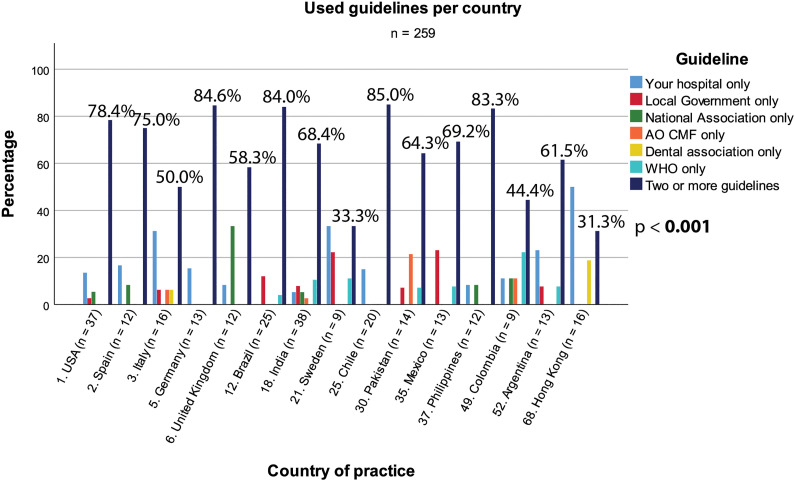
When stratifying by country, most surgeons adhere to more than 1 guideline (Figure 6). Noteworthy, may be the relatively high percentage of surgeons in Hong Kong that adhere to only the hospital guidelines (50.0%, n = 8). Guideline use was significantly different among countries (P < .001).
Figure 6.
Used guidelines per country. Percentages are presented for the category “Two or more guidelines.”
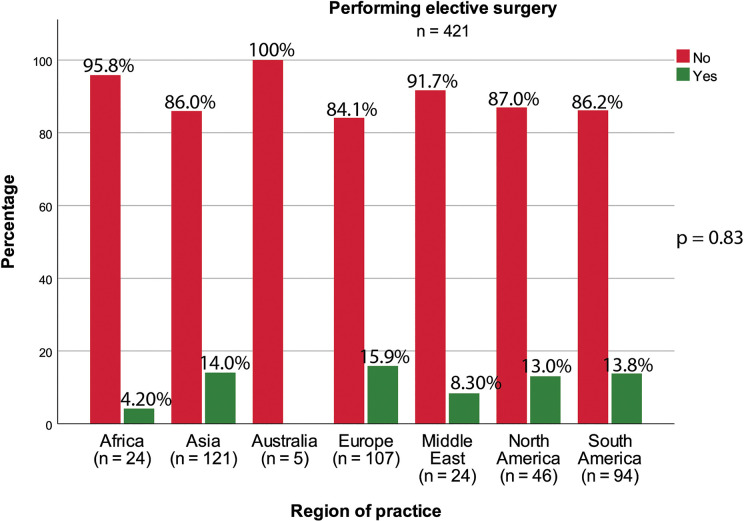
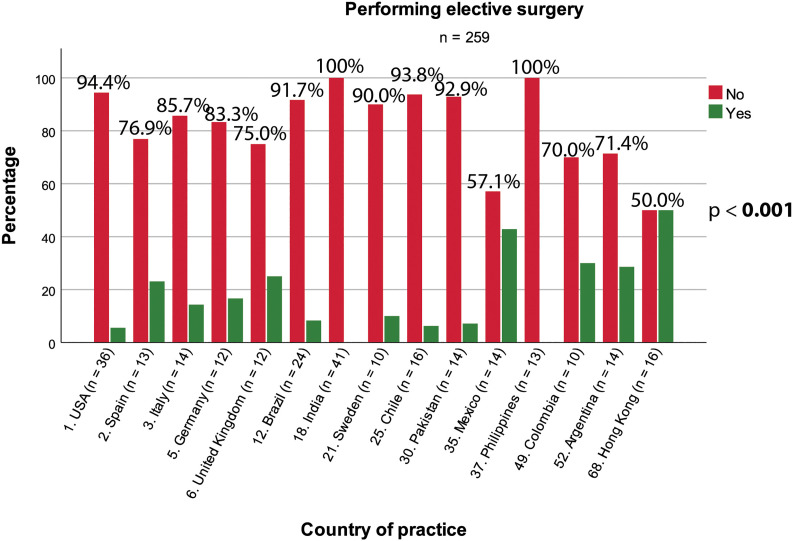
What Is the Effect on Clinical Practice?
More than 80% of all surgeons in the different regions stopped performing elective surgery (Figure 7). No significant differences among the regions were observed (P = .83). Similar findings were noted when stratifying by country. However, half of the respondents from Hong Kong performed elective surgery at the time of the survey (Figure 8). Moreover, the countries differed significantly in the number of surgeons who continued elective surgery (P < .001).
Figure 7.
Continuation of elective surgery per region.
Figure 8.
Continuation of elective surgery per country. Percentages are presented for the category “No elective surgery.”
Discussion
The purposes of this study were to (1) describe the effects of COVID on CMF surgeons and their practices and (2) to estimate the adequacy of access to PPE and to identify factors that may be barriers to accessing adequate PPE.
Main Outcomes
There were 5 main findings of this survey. First, the vast majority of CMF surgeons feel the hospitals do not provide adequate PPE to the frontline HCWs, though we see regional differences. Second, the availability of PPE under HCWs and surgeons considerably varies per region. Third, after adjusting for multiple variables, the region of practice seems not to be associated with the issue of inadequate PPE availability under HCWs and surgeons. Fourth, in all 7 regions, most surgeons are using more than 1 guideline how to manage patients under the COVID-19 pandemic. Lastly, the vast majority of the CMF surgeons stopped performing elective surgery.
Do Hospitals Provide Adequate PPE to the Frontline HCWs?
Health workers are at the front line of the COVID-19 outbreak response and are exposed to hazards that put them at risk of infection. As proposed by WHO, one may assume overall responsibility to ensure that all necessary preventive and protective measures are taken to minimize occupational safety and health risks.11 Therefore, it is remarkable to notice that from this survey the majority of CMF surgeons feel the hospitals do not provide adequate PPE to the frontline HCWs. As expected, we see regional differences. The best protection offered to the surgeons is in Australia, although from this region only 5 responses were received, followed by North America where N95/FFP2 and PAPR systems are provided. On the other side of the spectrum of PPE availability, we see that in Africa the majority of the surgeons can only use surgical/FFP1 masks as the maximum protection for the treatment of COVID-19 positive patients. As the disease progresses geographically over the regions and over time, the hospitals are struggling to keep enough supplies available. The WHO expects disruptions in the global supply chain of PPE. While the current global stockpile of PPE is insufficient, particularly for medical masks and respirators, the supply of gowns and goggles is soon expected to be insufficient as well. The capacity to expand PPE production is limited, and the present demand for respirators and masks cannot be met. For the near future, widespread inappropriate and unnecessary use of PPE continues.11 Compounding the issue is that the price for PPE has gone up as a result of the increased demand for fixed or limited PPE.12 In many countries, consortium-based approaches were initiated to increase their purchasing power and decrease competition at a hospital, local, and/or national level. Furthermore, new initiatives to produce PPE locally instead of purchasing the PPE from foreign suppliers were embraced. Under all circumstances, the hospitals must adhere to the guidelines to safeguard their HCWs and staff including CMF surgeons from unnecessary occupational exposure to SC-2.
What Is the Level of PPE Offered to Surgeons?
Surgical procedures in the CMF area involving the nasal–oral–endotracheal mucosal region are high risk for exposure to SC-2 due to anatomic proximity to the upper airway and due to aerosolization of the virus. SC-2 is known to be in high concentration in these areas when compared to swabs from the lower respiratory tract.7 Therefore, we were disappointed to see that lack of adequate PPE in various regions putting our colleagues and indirectly others at risk. The best protection offered to the surgeons is probably in Australia, where surgeons can work with N95/FFP2 masks or PAPR systems, followed by North America where N95/FFP2 masks and PAPR systems are provided. In marked contrast, in Africa, the vast majority of the surgeons only have surgical masks for maximum protection when treating COVID-19 patients. In addition, we also see in Asia, Europe, Middle East, South America, the surgeons still have to rely on surgical masks.
Furthermore, we found that as the number of confirmed COVID-19 cases per country decreases, adequate amount and quality of PPE for the HCWs and surgeons decreases. This is a troubling finding, since countries with low numbers of confirmed COVID-19 cases (Pakistan, Mexico, the Philippines, Colombia, and Argentina) are probably more at risk for further spread of SC-2 making access to adequate PPE even more important. However, whether this finding is a result of late availability of adequate PPE in countries with low COVID-19 cases or is a result of structural mismanagement cannot be ascertained from these cross-sectional data. Overall, it is alarming to hear our colleagues around the globe have to deal with unsafe situations, as the protective quality of a surgical mask may be insufficient.6 Luckily, the number of surgeons who were tested positive for SC-2 was low in this survey. Due to this small numbers, however, we determine if SC-2 exposure was due to the lack of adequate PPE availability or community spread. We also do not know if this number will increase over time.
Meanwhile, WHO published general recommendations to increase availability of PPE summarized in 3 main points.11 First, the need of PPE should be minimized by protecting HCWs and others from exposure to SC-2 in health-care settings. Secondly, the use of PPE should be rational and appropriate. It is obvious that the type of PPE used when caring for COVID-19 patients will vary according to the setting and type of personnel and activity. For CMF surgeons, appropriate PPE should be worn for surgical procedures and urgent ambulatory visits which includes N95/FFP2/full face shield or PAPR systems.6 Thirdly, the PPE supply chain should be coordinated and managed through essential national and international consortium-based initiatives.
To What Guideline Do Surgeons Adhere?
From the current survey, it is noteworthy that all surgeons from around the globe use more than 1 guideline when managing COVID-19 patients. In Asia, Africa, Europe, North America, and South America, the surgeons mostly adhere to the guidelines of their hospital, whereas in Australia and Middle East, the hospitals seem to play no role in guiding their staff. WHO guidelines are specifically used in Africa, Asia, Middle East, and South Africa. The AO CMF guideline is used in the Middle East.
Currently, little good information on COVID-19 is available. As such, following more than 1 guideline permits surgeons to be exposed to a number of different global, national, and local authorities (including hospitals) to develop patient care recommendations and opportunities to limit occupational exposure to SC-2. It must be stressed that formulating guidelines with evidence-based information on COVID-19 testing, PPE for management of COVID-19 negative and positive patients including AGPs is complex mainly due to the limited amount of available literature. It is critical that international societies, such as AO CMF, supported by data provided by the WHO, national health authorities, and other scientific societies take the lead in disseminating the best information we have available. As such, the AO CMF International Task Force has launched their first version of recommendations and will continue to distribute updates as more clinical information on the disease and PPE becomes available.6
Are Surgeons Still Doing Elective Surgery?
On March 11, 2020, WHO declared the novel COVID-19 as a global pandemic, classifying the outbreak as an international emergency.13 Subsequent to this declaration, in many countries, the recommendation to cancel elective operations appeared. Elective procedures could potentially contribute to the spreading of the coronavirus within the hospital facilities and consume medical resources needed to manage COVID-19 patients. From the results of this survey, it is clear CMF surgeons followed this advice and stopped elective surgery. As confirmed with this survey (data not shown here), the vast majority of the CMF surgeons are suffering from severe negative economic consequences. At present, various countries are experiencing a drop in the number of COVID-19 cases and will plan to restart elective surgical care again. Interestingly, surgeons from Hong Kong seem to have restarted elective surgery since the same number of surgeons were performing and not performing elective surgery. Specifically, for CMF surgeons must understand and limit the role they play in spreading of the disease.
Strengths and Limitations
A great strength of this study is the large number of survey respondents. As such, we can compare CMF surgeons from different regions and countries. Furthermore, the questions were extensive and the percentage of missing data per analyzed variable were low. A limitation of this survey is the relatively low response rate potentially leading to a response bias. Since no information about the nonresponders is known, we can only speculate on how this may have affected our findings. Another limitation is that we were not able to determine which guidelines the respondents adhered to if two or more guidelines were followed. This may weaken our ability to determine which guideline was found to be most important to CMF surgeons. Moreover, the cross-sectional setting and the early timepoint in the COVID-19 pandemic of the survey limits the ability to assess and measure the effects of COVID-19 over the long term.
Conclusion
In conclusion, this survey outlines adverse effects of COVID-19 on CMF surgeons globally, by limiting care to urgent or emergent cases and limited access to adequate PPE. Major findings from the survey are (1) the vast majority of CMF surgeons feel the hospitals do not provide adequate PPE to the frontline HCWs; (2) the availability of the PPE among HCWs and surgeons considerably varies per region; (3) after adjusting for multiple variables, the region of practice seems not to be associated with the issue of inadequate PPE availability under HCWs and surgeons; (4) most CMF surgeons are using more than 1 guideline how to manage patients under the COVID-19 pandemic; and (5) the vast majority of CMF surgeons stopped elective surgery. Future surveys via the AO CMF network should capture what the mid- and long-term impact of the COVID-19 crisis on CMF surgery and surgeons will look like.
Supplemental Material
Supplemental_Material_S1 for The Global Impact of COVID-19 on Craniomaxillofacial Surgeons by Justin van der Tas, Thomas Dodson, Daniel Buchbinder, Stefano Fusetti, Michael Grant, Yiu Yan Leung, Erich Roethlisberger, Gregorio Sánchez Aniceto, Alexander Schramm, Edward Bradley Strong and Eppo Wolvius in Craniomaxillofacial Trauma & Reconstruction
Supplemental_Tables_S1_and_S2 for The Global Impact of COVID-19 on Craniomaxillofacial Surgeons by Justin van der Tas, Thomas Dodson, Daniel Buchbinder, Stefano Fusetti, Michael Grant, Yiu Yan Leung, Erich Roethlisberger, Gregorio Sánchez Aniceto, Alexander Schramm, Edward Bradley Strong and Eppo Wolvius in Craniomaxillofacial Trauma & Reconstruction
Acknowledgments
The authors acknowledge AO Spine (Dr Dino Samartzis and Dr Phil Louie) for generously reaching out to the other clinical divisions of the AO Foundation including the AO CMF Research & Development Commission to participate in their initiative of this COVID-19 survey.
Authors’ Note: All of the authors are members of the AO CMF International COVID-19 Task Force, with the exception of Justin van der Tas.
Author Contributions: All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. All authors were involved in drafting the article or critically revising it for important intellectual content. And, finally, all authors approved of the version to be published.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Stefano Fusetti  https://orcid.org/0000-0002-5861-5046
https://orcid.org/0000-0002-5861-5046
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus Disease 19 (COVID-19): implications for clinical dental care. J Endod. 2020;46(5):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhou M, Zhang X, Qu J. Coronavirus disease 2019 (COVID-19): a clinical update. Front Med. 2020;14(2):126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Viner RM, Russell SJ, Croker H, et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4(5):P397–P404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8(4):e488–e496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cowling BJ, Aiello AE. Public health measures to slow community spread of coronavirus disease 2019. J Infect Dis. 2020;221(11):1749–1751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grant M, Schramm A, Strong B, et al. AO CMF International Task Force recommendations on best practices for maxillofacial procedures during COVID-19 pandemic 2020. Accessed April 13, 2020 https://aocmf3.aofoundation.org/-/media/project/aocmf/aocmf/files/covid-19/ao_cmf_covid-19_task_force_guidelines.pdf?la=en&hash=C2B89E1E6E9AB72EBF386C747D3BC74CF1009C1E. [DOI] [PMC free article] [PubMed]
- 7. Zou L, Ruan F, Huang M, et al. SARS-CoV-2 Viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zimmermann M, Nkenke E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J Craniomaxillofac Surg. 2020;48(5):521–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. [DOI] [PubMed] [Google Scholar]
- 10. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):P533–P534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. WHOTeam. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19). 2020. Accessed April 19, 2020 https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf.
- 12. Zimmet M, Silverberg J, Stawis A, Greenfield M. The society for healthcare organization procurement professionals. 2020. Accessed April 21, 2020 http://cdn.cnn.com/cnn/2020/images/04/16/shopp.covid.ppd.costs.analysis_.pdf.
- 13. McKay B, Calfas J, Ansari T. Wall St J. 2020. Accessed April 24, 2020 https://www.wsj.com/articles/u-s-coronavirus-cases-top-1-000-11583917794.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental_Material_S1 for The Global Impact of COVID-19 on Craniomaxillofacial Surgeons by Justin van der Tas, Thomas Dodson, Daniel Buchbinder, Stefano Fusetti, Michael Grant, Yiu Yan Leung, Erich Roethlisberger, Gregorio Sánchez Aniceto, Alexander Schramm, Edward Bradley Strong and Eppo Wolvius in Craniomaxillofacial Trauma & Reconstruction
Supplemental_Tables_S1_and_S2 for The Global Impact of COVID-19 on Craniomaxillofacial Surgeons by Justin van der Tas, Thomas Dodson, Daniel Buchbinder, Stefano Fusetti, Michael Grant, Yiu Yan Leung, Erich Roethlisberger, Gregorio Sánchez Aniceto, Alexander Schramm, Edward Bradley Strong and Eppo Wolvius in Craniomaxillofacial Trauma & Reconstruction