Leaning point for clinicians
Recent reports have shown that patients with COVID-19 also present with acute kidney injury and are associated with increased morbidity and mortality. Collapsing glomerulopathy (CG) seems to be an emerging manifestation of COVID-19, and a trial of steroids and lisinopril along with resolution of the infection seems to improve outcomes.
Introduction
Collapsing glomerulopathy (CG) seems to be an emerging manifestation of coronavirus disease 2019 (COVID-19), and it could result from immune dysregulation-mediated podocytopathy in genetically predisposed patients. We present a case of COVID-19 who developed CG.
Case
A 63-year-old African American female with a history of chronic kidney disase (CKD) stage 3aA1, systemic lupus erythematosus and antiphospholipid syndrome presented to the emergency department with dry cough and diarrhea. She had dry mucous membranes on exam. Workup revealed positive COVID-19, elevated serum creatinine (Scr) 2.69 mg/dl (peak 4.6 mg/dl, baseline 1.33 mg/dl), new-onset nephrotic range proteinuria of 6.8 g on urine protein-creatinine ratio (UPCR), normal C3/C4 complement levels and negative serologies for anti-PLA2R antibody, HIV, Hepatitis B and C. Renal ultrasound and subsequent abdominal computed tomography (CT) scan showed atrophied left kidney (Figure 1A). A high-risk right kidney biopsy showed CG involving 15% of glomeruli amid a background of severe arteriosclerosis and arteriolosclerosis with generalized chronic ischemic glomerular and tubular injury (Figure 1B). There was no evidence of immune complex glomerulonephritis or thrombotic microangiopathy. Immunofluorescence had nonspecific staining. Ultrastructure showed diffuse podocyte foot process fusion (Figure 1C). Genotyping for APOL1 was positive for heterozygous haplotypes G1 and G2. After two negative COVID-19 results, the patient was discharged on steroid taper and lisinopril with improvement in Scr 2.1 mg/dl and UPCR 3.8 g on 3 weeks follow-up.
Figure 1.
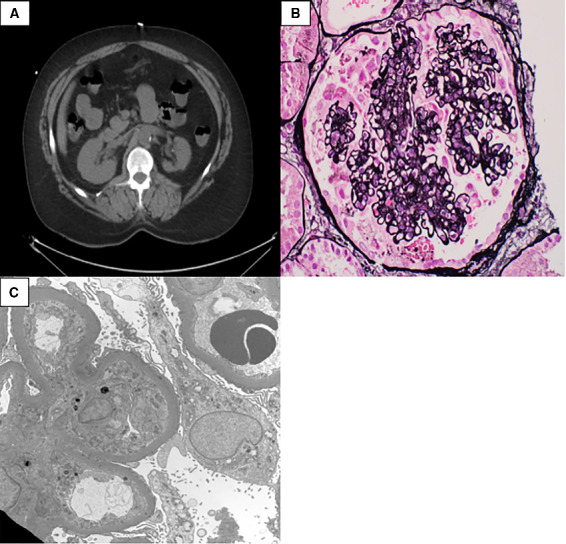
(A) Transverse CT scan of abdomen showing atrophy of the left kidney. (B) Light microscopy of glomeruli with 15% of glomeruli showing collapsing lesions and background of severe arteriosclerosis and arteriolosclerosis with generalized chronic ischemic glomerular change and tubular injury consistent with ischemic injury. (C) Electron microscopy with immunofluorescence showing nonspecific trace staining and Ultrastructure showing diffuse podocyte foot process fusion.
Discussion
Collapsing glomerulopathy is a distinct pathological entity of glomerular basement membrane collapse and podocytopathy from visceral epithelial proliferation resulting in a hyperplastic phenotype. Overtime dysfunctional repair leads to progressive fibrosis. Host factors including genetic predisposition, dysfunctional immune response to environmental triggers including medications and infections have been noted to be associated with CG.1 CGN is a rapidly progressive glomerulopathy that can present with abrupt onset of acute renal failure, nephrotic range proteinuria and can progress to end-stage renal disease. Patients presenting predominantly with proteinuria may have varying degrees of response to immunosuppressive treatments.
Data and information about kidney pathology and long-term sequelae of COVID-19 infection on the kidneys are limited. There are only a handful of case reports of CGN associated with COVID-19 reported in the literature.2–4 High-risk APOL1 allele variants may increase the risk of CG in African American patients.Previous studies have suggested homozygosity for APOL1 high-risk alleles leading to increased risk of developing CG. Our patient's unique clinical characteristics and genetic testing suggest that even heterozygous APOL1 high-risk alleles can lead to CG with COVID-19. Her Scr and proteinuria improved on a trial of steroids and lisinopril. Whether this could be due to the resolution of infection and subsequent improvement or primary treatment-induced response remain a matter of further research. Further studies are needed to establish optimum treatment strategies and assess the long-term prognosis of CG as a manifestation of COVID-19 in patients with high-risk APOL1 alleles.
Conflict of interest. None declared.
Contributor Information
G J Hoilat, From the Department of Medicine, USA.
G Das, Department of Nephrology, USA.
M Shahnawaz, From the Department of Medicine, USA.
P Shanley, Department of Pathology, State University of New York Upstate Medical University, Syracuse, NY, USA.
S H Bukhari, Department of Nephrology, USA.
References
- 1. Nicholas Cossey L, Larsen CP, Liapis H. Collapsing glomerulopathy: a 30-year perspective and single, large center experience. Clin Kidney J 2017; 10:443–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Larsen CP, Bourne TD, Wilson JD, Saqqa O, Sharshir MA. Collapsing glomerulopathy in a patient with COVID-19. Kidney Int Rep 2020; 5:935–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Peleg Y, Kudose S, D’Agati V, Siddall E, Ahmad S, Nickolas T, et al. Acute kidney injury due to collapsing glomerulopathy following COVID-19 infection. Kidney Int Rep 2020; 5:940–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kissling S, Rotman S, Gerber C, Halfon M, Lamoth F, Comte D, et al. Collapsing glomerulopathy in a COVID-19 patient. Kidney Int 2020; 98:228–31. [DOI] [PMC free article] [PubMed] [Google Scholar]


