IL-6: a nexus for immune responses and disease
Keywords: cytokine storm of COVID-19, IL-6 amplifier, local initiation model, NF-κB, STAT3
Abstract
IL-6 is involved both in immune responses and in inflammation, hematopoiesis, bone metabolism and embryonic development. IL-6 plays roles in chronic inflammation (closely related to chronic inflammatory diseases, autoimmune diseases and cancer) and even in the cytokine storm of corona virus disease 2019 (COVID-19). Acute inflammation during the immune response and wound healing is a well-controlled response, whereas chronic inflammation and the cytokine storm are uncontrolled inflammatory responses. Non-immune and immune cells, cytokines such as IL-1β, IL-6 and tumor necrosis factor alpha (TNFα) and transcription factors nuclear factor-kappa B (NF-κB) and signal transducer and activator of transcription 3 (STAT3) play central roles in inflammation. Synergistic interactions between NF-κB and STAT3 induce the hyper-activation of NF-κB followed by the production of various inflammatory cytokines. Because IL-6 is an NF-κB target, simultaneous activation of NF-κB and STAT3 in non-immune cells triggers a positive feedback loop of NF-κB activation by the IL-6–STAT3 axis. This positive feedback loop is called the IL-6 amplifier (IL-6 Amp) and is a key player in the local initiation model, which states that local initiators, such as senescence, obesity, stressors, infection, injury and smoking, trigger diseases by promoting interactions between non-immune cells and immune cells. This model counters dogma that holds that autoimmunity and oncogenesis are triggered by the breakdown of tissue-specific immune tolerance and oncogenic mutations, respectively. The IL-6 Amp is activated by a variety of local initiators, demonstrating that the IL-6–STAT3 axis is a critical target for treating diseases.
Introduction
Cytokines function in many fundamental processes for life and disease including immunity, inflammation, embryonic development, regeneration, angiogenesis, metabolism, obesity, aging and so on. Among these diverse functions, their roles in inflammation have attracted attention in relation to disease development and treatment.
Inflammation is involved in homeostasis and regenerative processes such as wound healing. It is also involved in acute-phase reactions and immune responses against pathogens. In these cases, inflammation is well controlled. On the other hand, chronic inflammation and cytokine storm are uncontrolled forms of inflammation. The former plays crucial roles in the development of many complex diseases and disorders such as chronic inflammatory diseases, including metabolic syndrome, neurodegenerative diseases and cardiovascular diseases, along with autoimmune diseases and cancer (1–11). Cytokine storm has received a great deal of attention in connection with the pathology of corona virus disease 2019 (COVID-19) (12–17). Cytokine storm is considered a type of inflammation where the massive production of inflammatory cytokines is acutely induced in a dysregulated manner in response to infection, trauma, chimeric antigen-receptor T-cell (CAR-T) therapy and so on. In this regard, inflammation is a double-edged sword in that it is dependent on the context, location and timing, making it difficult to develop therapeutics.
Inflammation is a complex process in which a variety of cells, including B lymphocytes, T lymphocytes, myeloid cells, epithelial cells, fibroblasts, endothelial cells, muscle cells and adipocytes, interact with each other through membrane-associated molecules, matrix metalloproteases (MMPs) and soluble factors, such as cytokines, chemokines and growth factors. Pro-inflammatory cytokines such as IL-1β, tumor necrosis factor alpha (TNFα) and IL-6 play crucial roles in inflammation. Among them, IL-6 is a major player in chronic inflammatory diseases, autoimmune diseases, cancer and cytokine storm (1, 3, 10–26).
IL-6, which was discovered in 1986 (27), is a pleiotropic cytokine involved not only in immune responses but also in inflammation, hematopoiesis, bone metabolism, embryonic development and other fundamental processes (1, 21, 28–32). IL-6 is a prototypical member of the IL-6 family of cytokines, which is composed of 10 members including IL-6, IL-11, IL-27, oncostatin M (OSM), leukemia inhibitory factor (LIF), ciliary neurotrophic factor (CNTF), cardiotrophin 1 (CT-1), cardiotrophin-like cytokine factor 1 (CLCF1), IL-35 and IL-39 (33). It was originally identified as B-cell stimulating factor-2 (BSF-2), an inducer of immunoglobulin production (27). Several other proteins including IFNβ2 (34), IL-1-induced 26-kDa protein (35), plasmacytoma/hybridoma/myeloma growth factor (36–38) and hepatocyte-stimulating factor (39, 40) were found to be identical to BSF-2 and thus IL-6 (41). These studies indicated that IL-6 has a variety of functions not only in health but also in diseases, such as plasmacytoma and myeloma.
Studies in the 1980s also showed that IL-6 is produced by cardiac myxoma cells (42) and Castleman’s germinal center cells (43) and is present at high amounts in the synovial fluid of rheumatoid arthritis (RA) patients (44, 45), suggesting its role in autoimmune diseases and chronic inflammatory diseases (1). Accordingly, a working hypothesis explaining the possible mechanisms of chronic inflammatory diseases and autoimmune diseases was proposed (1, 46). The original hypothesis has since been updated and is here called the local initiation model, which emphasizes the importance of local initiators, such as infection, injury and stress in the promotion of interactions between non-immune cells and immune cells in disease. A similar hypothesis was proposed for local lesions triggering these interactions rather than the breakdown of tissue-specific immune tolerance (47, 48). Consistently, evidence has indicated that interactions between immune cells and non-immune tissues play critical roles in chronic inflammatory diseases and autoimmune diseases (3, 41, 49–51). Furthermore, tissue property-dependent events (49), microbleeding (52, 53), neural stimulation (54, 55), cell senescence (56, 57) and oncogenic mutations in pre-neoplastic cells have been shown to trigger these interactions.
Additionally, interactions between a tumor and its microenvironment through the immune system are critical for tumor development and progression (2, 6, 9, 58–60), and aging is related with cancer progression as well as inflammation and autoimmunity. Notably, IL-6 is involved in cell senescence, is produced by senescent cells and is critically involved in senescence-induced inflammation and age-dependent pathologies and cancer (7). IL-6 is also a key factor in inflammation, autoimmunity and cancer, with its effect mainly exerted through the IL-6–signal transducer and activator of transcription 3 (STAT3) pathway (18–26, 61–65).
The IL-6 amplifier (IL-6 Amp) is an amplification mechanism for the production of IL-6 and a variety of other cytokines and chemokines through a synergic interaction between STAT3 and nuclear factor-kappa B (NF-κB). It too plays a key role in inflammatory diseases including cytokine storm syndromes, autoimmune diseases and cancer (10, 11, 15, 41, 66–68), providing a link for STAT3 and NF-κB in these disorders (67).
Considering the properties of IL-6, an anti-IL-6 therapy against multiple myeloma was tried in the 1990s (69). Although anti-IL-6 murine monoclonal antibody (MoAb) inhibited the proliferation of myeloma cells and production of C-reactive protein (CRP), the effect was limited, most likely because of the increase of the IL-6 half-life (70). Instead of murine MoAb against IL-6, a humanized MoAb against IL-6 receptor (IL-6R), tocilizumab, has proven successful for treating RA and Castleman’s disease (71–75). The IL-6–STAT3 pathway is now considered a major target for the treatment of inflammatory diseases (15, 19, 21, 24–26, 76).
In this review, the central roles of IL-6 and the local initiation model in inflammation, autoimmunity and cancer are summarized and discussed.
IL-6 expression, IL-6 receptor and its mode of action and signaling
The IL-6 gene contains several elements for transcription factor binding, including NF-κB, activator protein 1 (AP-1), CCAAT/enhancer-binding protein beta (C/EBPβ), cyclic adenosine monophosphate (cAMP)-responsive elements and STAT3 (77–84). IL-6 transcription is induced by a variety of stimuli, such as Toll-like receptor (TLR) ligands, IL-1, TNFα, reactive oxygen species (ROS) and zinc (Zn) and also depends on epigenetic regulation (33, 82, 84–86). Post-transcriptional control of IL-6 mRNA affects the IL-6 expression level. Regnase-1 degrades IL-6 mRNA (87), while Arid5a protects IL-6 mRNA from Regnase-1-mediated degradation (88). Lin 28 induced by NF-κB activation prevents IL-6 mRNA degradation by inhibiting microRNA let-7 (89). STAT3-induced microRNA (miR)-21 and miR-181b-1 activate NF-κB, resulting in the induction of IL-6 gene expression (90). Finally, MiR-26a inhibits hepatocellular carcinoma growth and metastasis by inhibiting IL-6 expression (91).
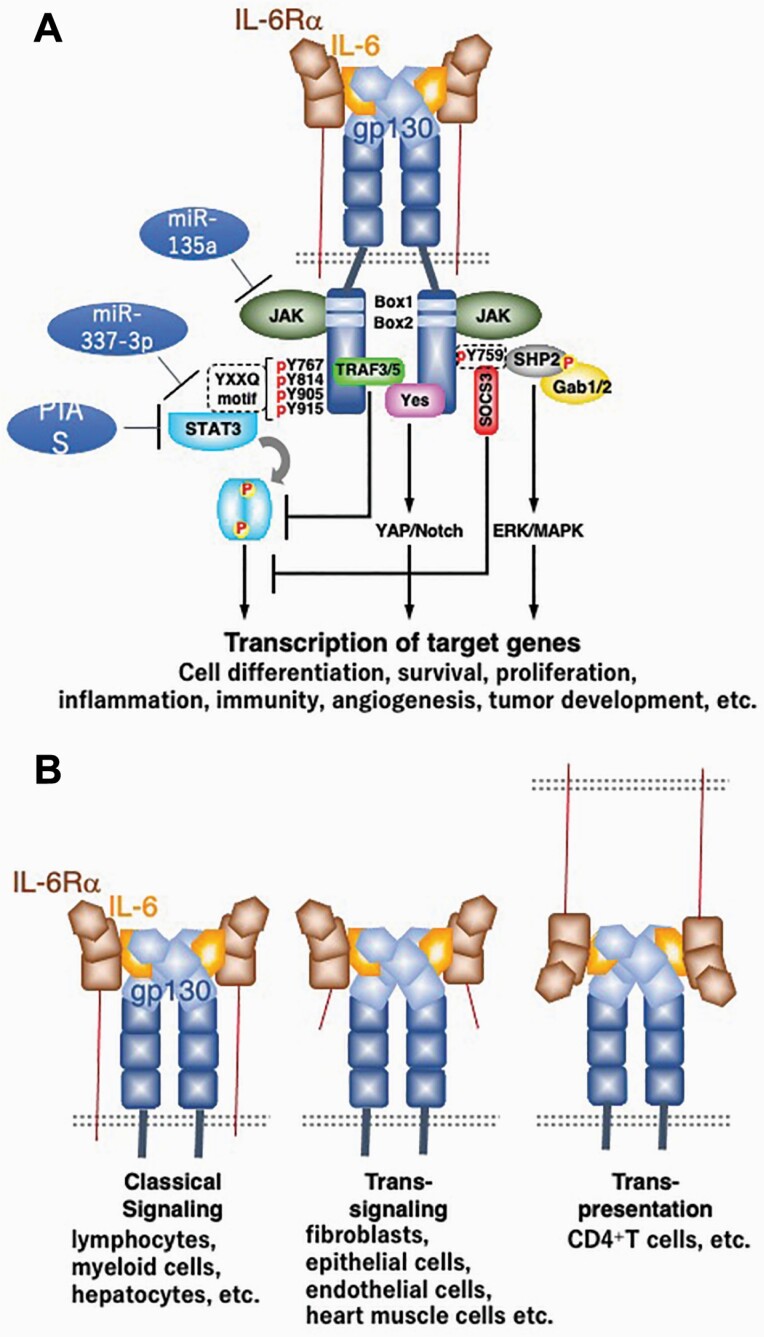
The IL-6R is composed of an IL-6-binding receptor molecule (IL-6Rα) and a signal transducer, gp130, which is shared among the IL-6 family of cytokines (Fig. 1A) (33). For IL-6 activity, the expression of both IL-6Rα and gp130 on the cell surface is required, which limits the number of target cells on which IL-6 acts to lymphocytes, myeloid cells and hepatocytes (33). However, IL-6 complexed with the soluble form of IL-6Rα (sIL-6Rα) can act on cells expressing only gp130, such as heart muscle cells. Double transgenic mice expressing both IL-6 and IL-6Rα, but not transgenic mice expressing either IL-6 or IL-6Rα alone, show myocardial hypertrophy (92). In the early 1990s, it was found that IL-12 is composed of a disulfide heterodimer that included p40 and p35 subunits, resembling IL-6 and sIL-6Rα, respectively (93). Additionally, IL-12 acts through IL-12R, which is closely related to gp130 (94). The complex of CNTF and the soluble form of CNTF receptor alpha acts on cells expressing LIFRβ and gp130 (95). These early studies show that there is a mechanism by which a cytokine acquires different target specificity through complex formation with the ligand and the soluble form of the cytokine receptor subunit. Through this mechanism, a cytokine acquires a novel function, namely cytokine-soluble receptor complex function, to act as a novel cytokine on target cells (1). This mode of IL-6 action is now called the trans-signaling mode, while the original membrane type is called the classic mode (Fig. 1B) (96). The trans-signaling mode expands the range of cells that respond to IL-6, because gp130 is expressed in a wide range of cells, including endothelial cells and fibroblasts, explaining one of the mechanisms by which IL-6 acts on a wide range of cells and tissues to exert a pleiotropic function. Indeed, this mode plays crucial roles in chronic inflammation (33, 96). One example has IL-6 together with sIL-6Rα acting on endothelial cells that express only gp130 to induce STAT3 activation, chemokine expression and the augmentation of ICAM-1, thus contributing to local inflammation by activating leukocyte recruitment (97). In addition, IL-6 and sIL-6Rα induce a transition between the early predominantly neutrophilic stage of an infection and the more sustained mononuclear cell influx, contributing to the switch from acute to chronic inflammation (98). Further, they act on fibroblasts and endothelial cells to recruit T helper 17 (Th17) cells, leading to an RA-like joint disease (F759 arthritis) and experimental autoimmune encephalomyelitis (EAE) (54, 66, 99).
Fig. 1.
IL-6 receptor and signaling. (A) IL-6 binding induces a hexameric complex composed of two molecules of IL-6, IL-6Rα and gp130 each, leading to the activation of JAKs associated with gp130 at Box1 and Box2. The phosphorylation of tyrosine 759 of gp130 is required for the gp130-mediated ERK–MAPK pathway via SHP2 and GAB adaptor molecules and essential for the SOCS3-mediated negative feedback loop. The distal four tyrosine residues of gp130 (Y767, Y814, Y905 and Y915) form a YXXQ motif, which is required for STAT3 activation. The YAP–Notch pathway is triggered by Yes. TRAF is associated with gp130 and inhibits the STAT3 signaling pathway. MiR-135a and miR-337-3p down-regulate JAK2 and STAT3, respectively. PIAS directly inhibits STAT3. All amino acid positions are of human gp130. (B) Three modes of gp130-mediated signaling. IL-6 acts on cells expressing both IL-6Rα and gp130 (classical signaling). The complex of IL-6 and sIL-6Rα acts like a novel cytokine on cells expressing only gp130 (trans-signaling). In the trans-presentation mode, IL-6 bound to IL-6Rα expressed on one type of cell acts on another cell type expressing gp130.
sIL-6Rα is generated mainly by proteolysis by ADAM17 and to a minor extent by alternative splicing in humans. Notably, sIL-6Rα is increased in several diseases, indicating that trans-signaling plays important roles in the progression of inflammation in many diseases including severe COVID-19 (15, 96).
In certain cases, IL-6 bound to cell surface IL-6Rα can act on another cell that expresses gp130 in a manner consistent with the IL-6–sIL-6Rα complex. For example, IL-6 bound to IL-6Rα expressed on dendritic cells (DCs) directly acts on CD4(+) T cells through gp130 to induce Th17 cells (100). The signal transduction by this trans-presentation (Fig. 1B) might differ from trans-signaling, since the soluble form of gp130 efficiently inhibits trans-signaling, but not trans-presentation or classical signaling (101).
IL-6 activates Janus kinase (JAK) family tyrosine kinases through gp130, leading to the activation of STAT family transcription factors, mainly STAT3, as well as src homology region 2 domain-containing phosphatase 2 (SHP-2), GRB2-associated-binding protein (GAB), extracellular signal-regulated kinase (ERK) and mitogen-activated protein kinase (MAPK) signaling pathways (Fig. 1A). Activated JAK phosphorylates tyrosine residues in the cytoplasmic domain of gp130 (30, 31, 61, 62, 102, 103).
Utilizing chimeric receptors carrying the intracellular region of human gp130, it was shown that Y767, Y814, Y905 and Y915, which all have YXXQ moieties, are required for STAT3 activation in vitro, and that Y759 is an SHP-2-binding site (104, 105). The binding of SHP-2 to Y759 mediates activation of the ERK–MAPK cascade via the adaptor molecules GAB1 and GAB2 (106, 107). Gp130 signaling is also mediated by the Src family kinase, Yes, which directly associates with gp130 via amino acid residues 812–827 (108). IL-6 activates the Yes-associated protein (YAP)-Notch pathway through Yes, stimulates epithelial cell proliferation and confers regeneration capacity in injured intestinal epithelia. The IL-6–Notch-3 pathway is also involved in cell growth and the promotion of a hypoxia-resistant/invasive phenotype in breast cancer development (109).
These pathways affect each other and are negatively regulated by several molecules. The gp130-mediated activation of STAT3 is involved in the cell-cycle transition through the up-regulation of cyclins D2, D3 and A, and cdc25A, and the concomitant down-regulation of p21 and p27, while p21 is induced when STAT3 activation is suppressed, indicating the balance of contradictory signals determines the final output (110). Similarly, defective STAT3 activation enhances SHP-2–ERK–MAPK activation pathways, most likely through an impaired STAT3-mediated induction of suppressor of cytokine signaling 3 (SOCS3) (111, 112). Phosphorylated Y759 (human gp130) or Y757 (murine gp130) serves as a binding site for SOCS3 and SHP-2. In fact, knock-in mice expressing human gp130 with Y759F mutation (F759 mice) (113) or mice expressing murine gp130 with Y757F mutation (64) display splenomegaly, lymphadenopathy, an enhanced acute-phase reaction and prolonged STAT3 activation. The enhanced STAT3 activation was initially considered the result of an inability to recruit SHP-2, a negative regulator having tyrosine phosphatase activity (113–115). However, this site is also a recruitment motif for SOCS3, and it was found that the F759/F757-dependent negative regulation is mainly dependent on the recruitment of SOCS3 (116, 117). SOCS3 is induced by STAT3 and considered to regulate a major negative feedback loop of a gp130-mediated signaling pathway (118–120). In addition, TNF receptor-associated factor 5 (TRAF5) negatively regulates IL-6–gp130-mediated STAT3 activation in naive CD4(+) T cells to suppress the Th17 differentiation (121), while TRAF3 facilitates the association of protein tyrosine phosphatase non-receptor type 22 (PTPN22), inhibiting STAT3 activation in B cells (122). MiR-135a and miR-337-3p down-regulate JAK2 and STAT3, respectively (123, 124). A protein inhibitor of activated STAT (PIAS) is also known to be a direct inhibitor of STAT3 (125).
These multiple signal transduction pathways intimately regulate cell survival, proliferation, inflammation, immunity, angiogenesis, and tumor development and progression through the expression of several genes (1, 19, 21, 26, 31).
IL-6 signaling in cell survival, proliferation, metastasis and angiogenesis
Concerning cell survival and proliferation, two signals through gp130 are involved. One is the SHP-2–ERK–MAPK pathway and the other is STAT3–bcl-2-mediated cell survival (104). STAT3 is involved not only in bcl-2 induction, but also in the induction of c-myc, cyclins and Pim1/2 kinase to regulate cell survival and cell cycle progression in a pre-B-cell line (110, 126, 127). STAT3 activation by IL-6 is required for intestinal epithelial cell survival and cell-cycle progression during colitis-induced tumorigenesis (20).
The proto-oncogene serine/threonine-protein (Pim) kinases, Pim-1 and Pim-2, are targets of STAT3 and involved in cell proliferation and cell survival together with c-myc (127). The IL-6–STAT3–Pim kinase axis is involved in the development and cell growth of pancreatic cancer (128, 129). In fact, Pim-1 expression in pancreatic cancer tissues and plasma Pim-1 levels are increased, and a high expression level is negatively associated with prognosis. Furthermore, high plasma Pim-1 expression is an independent adverse prognostic factor for pancreatic cancer (129) and also for breast cancer (130). The IL-6–STAT3 pathway is involved in the epithelial–mesenchymal transition (EMT) (131, 132), tumor migration (133), cancer stemness (130, 134, 135) and the induction of hypoxia-inducible factor-1α (HIF-1α) and vascular endothelial growth factor (VEGF), two key players for angiogenesis (136–140). Furthermore, oncogenic miR-21 and miR-181b are targets of IL-6–STAT3, leading to the activation of NF-κB (90, 141). An increased expression of miR-200 family members is associated with both tumor initiation in STAT3-dependent murine gastric cancer and early-stage gastric cancer in patient cohorts (142).
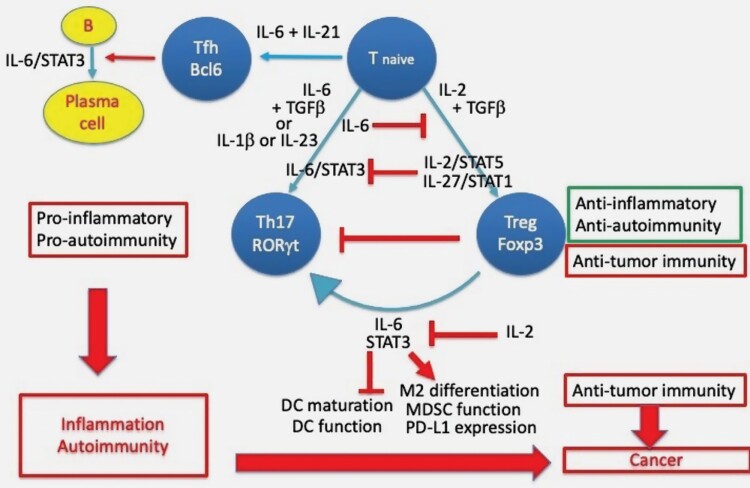
IL-6–STAT3 signaling in immunity
IL-6 was originally cloned as a factor acting on B cells to induce immunoglobulin production (27) and having a role in B-cell abnormality (42). Indeed, IL-6 promotes antibody production by directly acting on plasma cells and by indirectly promoting Bcl6-dependent follicular CD4(+) T (Tfh) cell differentiation together with IL-21 (Fig. 2) (143–146). IL-6 transgenic mice show severe plasmacytosis with hypergammaglobulinemia (147), while IL-6-deficient mice are defective in immunoglobulin production (148, 149). Moreover, mice reconstituted with hematopoietic stem cells carrying mutant gp130 lacking STAT3-binding sites show lower serum immunoglobulin levels (113), and conditional knockout of Stat3 in mouse B cells results in a loss of T-cell-dependent plasma cells (150). STAT3 is also required for human plasma cell differentiation by up-regulating BLIMP1 and down-regulating BCL6 (151). STAT3 loss-of-function (LOF) patients have impaired antigen-specific antibody responses (152, 153). IL-6-induced STAT3 activation is critical for in vivo plasma cell survival and immunoglobulin secretion in humans (154). Consistently, TRAF3 inhibits IL-6–STAT3 signaling in B cells and reduces plasma cell development (122). In addition to the aforementioned role of IL-6 on Tfh cells, IL-6 is known to direct the differentiation of IL-4-producing T helper type 2 (Th2) cells, while it inhibits the differentiation of IFNγ-producing Th1 cells (155). T-cell responses against tumors are mediated by CD8(+) effector T cells (Teff), of which differentiation is dependent on IFNγ-secreting Th1 cells. It was shown that myeloid-derived sIL-6R complexed with IL-6 inhibits Th1 responses through STAT3-induced c-Maf. This is considered to be one of mechanisms by which IL-6 inhibits T-cell immunity against tumors (156). However, the effect of IL-6 on the diversity of Th1 and Th2 cells is not simple: IL-6 induced by repeated inflammation is responsible for Th1 cell responses in peritoneal fibrosis (157).
Fig. 2.
IL-6/STAT3 in immunity. IL-6 promotes antibody production by either directly acting on plasma cells or indirectly promoting Tfh cell differentiation. IL-6/STAT3 together with TGFβ or IL-1β and IL-23 induces Th17 cells, while IL-6 inhibits the TGFβ/IL-2-induced generation of Treg cells. IL-2/STAT5 or IL-27/STAT1 inhibits the IL-6/STAT3-induced differentiation of Th17 cells. IL-6/STAT3 induces the conversion of Treg cells to Th17 cells, and this process is inhibited by IL-2. The IL-6/TGFβ and IL-2/TGFβ axes regulate the balance of Th17 and Treg cells; the former is pro-inflammatory and the latter anti-inflammatory. IL-6/STAT3 induces the differentiation of M2 macrophages and activates MDSCs, both of which have anti-tumor immunity effects. In addition, IL-6/STAT3 inhibits DC maturation and function. Finally, IL-6/STAT3 induces PD-L1 expression.
IL-17-producing Th17 cells have been shown to have a crucial role in autoimmunity and a still-controversial role in cancer (pro-tumorigenic or anti-tumorigenic), whereas regulatory T (Treg) cells inhibit autoimmunity and tumor immunity (158–163). IL-6 together with TGFβ induces Th17 cells (Fig. 2) (164). RAR-related orphan receptor gamma t (RORγt) is the key transcription factor for IL-6 and TGFβ-induced Th17 cell differentiation (165). On the other hand, IL-6 inhibits the TGFβ-induced generation of Treg cells (166). This inhibition by IL-6 is a direct action on naive T cells (167). However, IL-6-mediated inhibition is restricted to inducible Treg cells and has no effect on natural Treg cells (168).
The requirement for human naive T cells in Th17 cell differentiation differs from that of mice, since human T cells in the presence of IL-1β with IL-6 or IL-23 can differentiate to Th17 cells without TGFβ (169, 170). However, even in the absence of TGFβ, the combination of IL-1β, IL-6 and IL-23 induces pathogenic Th17 cells from mouse naive T cells in vitro and in vivo, suggesting an alternate mode of Th17 cell differentiation (171). Th17 cells generated without TGFβ express both RORγt and T-bet, while Th17 cells generated in the presence of TGFβ express only RORγt. IL-6 up-regulates IL-23R expression in a manner dependent on STAT3, and IL-23 further enhances its own receptor expression to increase the pathogenic potential of Th17 cells (171). Consistently, IL-23R is essential for the terminal differentiation of Th17 cells that are capable of inducing EAE in vivo (172). IL-6-activated STAT3 promotes Th17 cell pathogenicity by up-regulating IL-1R through miR-183c induction (173).
The IL-6–STAT3 pathway in CD4(+) T cells is essential for Th17 cell development and for the expression of RORγt (174, 175), while IL-27, a member of the IL-6 family of cytokines and activator of STAT3, inhibits Th17 cell differentiation in a manner dependent on STAT1 (Fig. 2) (176, 177). This effect suggests that STAT1 inhibits STAT3-induced Th17 cell differentiation. In fact, it was shown that IL-27 induces Th17 cell differentiation in the absence of STAT1 and that Th17 cell differentiation is dependent on the ratio of activated STAT3 and STAT1. The ratio induced by IL-6 is more than 1, whereas that induced by IL-27 is less than 1 (178). Of note is that both STAT3 LOF and STAT1 gain-of-function (GOF) mutations in patients show defects in Th17 cell differentiation (179, 180). Hyperactivated STAT1-mediated inhibition of Th17 cell differentiation is most likely due to a STAT1-induced up-regulation of PD-L1 in naive T cells (181), since the PD-L1–PD-1 interaction in naive T cells impairs Th17 cell differentiation (182). The critical role of STAT3 for Th17 cell differentiation is also supported by the fact that n-3 fatty acid docosahexaenoic acid and platelet factor 4, both of which induce SOCS3, inhibit Th17 cell differentiation and tumor growth (183, 184). Further, Zn, which is an essential trace element and affects the immune response and oncogenesis by either pro-inflammatory or anti-inflammatory effects in a context dependent manner (185), inhibits Th17 cell differentiation through the inhibition of IL-6-induced STAT3 activation (186).
TGFβ and IL-6 together induce Th17 cells, while TGFβ together with IL-2 induces Treg cells. IL-2-activated STAT5 inhibits Th17 cell differentiation (187), while IL-6 reduces Foxp3 expression, which inhibits RORγt-mediated IL-17A promoter activation (188). Furthermore, opposing regulation of the locus encoding IL-17 through the reciprocal actions of STAT3 and STAT5 suggest the balance between IL-6–STAT3 and IL-2–STAT5 regulates the development of Th17 cells and Treg cells from naive CD4(+)T cells (189).
Furthermore, there is Th17/Treg cell plasticity (Fig. 2). Treg cells when stimulated with IL-6 differentiate into Th17 cells (190). IL-6 down-regulates Foxp3 expression through STAT3 and together with IL-1 induces the genetic reprogramming of Treg cells to express Th17 cell function (191). Such a conversion of Treg to IL-17-producing Th17 cells is induced by IL-6 derived from synovial fibroblasts in mice suffering collagen-induced arthritis. Th17 cells converted from Treg cells are more potently osteoclastogenic than conventional Th17 cells (192). The IL-6-induced conversion of Treg cells to Th17 cells is inhibited by miR-125a-5p, which is induced by IL-2 and down-regulates the expression of IL-6R and STAT3 in Treg cells (193). IL-6 further inhibits the suppressive activity of Treg cells. The microbial induction of IL-6 through TLRs inhibits Treg cell activity (194). IL-6–STAT3 signaling prevents the Treg cell-mediated suppression of Teff cells in patients with psoriasis and multiple sclerosis (MS) (195, 196).
All evidence supports the idea that the immune system tightly regulates Th17/Treg cell homeostasis through the IL-6–IL-2 axis, and the disturbance of this balance in the presence of TGFβ causes inflammation and autoimmunity (Fig. 2). Treg cell dysfunction due to Foxp3 mutation causes a lethal autoimmunity known as immunodysregulation, polyendocrinopathy, enteropathy and X-linked (IPEX) syndrome (197), and defects of IL-2 signaling induce severe autoimmunity (198). Accordingly, low-dose IL-2 therapy for autoimmune and inflammatory diseases is under development (199). On the other hand, the enhancement of IL-6–STAT3 signaling causes IL-17A-dependent autoimmune arthritis in mice (41, 63, 66). In line with these findings, several inflammatory and autoimmune diseases, including RA, MS and inflammatory bowel disease show a bias for Th17 cells over Treg cells (163). Anti-IL-6R therapy in RA restores the homeostasis, suggesting one of possible mechanisms by which the therapy functions (200).
DCs present antigens to T cells to initiate immune responses and inflammation against infectious pathogens, organ transplants and tumors (201). Much evidence has accumulated to show that STAT3 functions as an inhibitor for DC differentiation, maturation and antigen-presenting ability, and therefore STAT3 inhibits tumor immunity by interfering with DC functions (Fig. 2) (25). The requirement for STAT3 in hematopoietic stem cell commitment to the DC lineage has also been shown (202), but TLR4-induced DC maturation is inhibited by IL-6 (203). Further, IL-6–STAT3 signaling inhibits the LPS-induced maturation of DCs and DC-mediated activation of T cells in vivo (204). In line with this observation, IL-6–STAT3 signaling reduces intracellular MHC class II levels in DCs by increasing cathepsin S activity (205). STAT3 activated through TLR9 in myeloid cells inhibits DC maturation and tumor immunity (206). The enhanced expression of IL-6 in tumor-infiltrating DCs from colorectal cancer patients correlates with a decrease in the expression of HLA-DR and CD86 on DCs and attenuation of DCs’ T-cell-stimulating ability (207). Accordingly, mammary tumor-derived exosomes block the differentiation of DCs in vitro through IL-6 (208). Versican is a soluble tumor-derived factor that induces DC dysfunction by up-regulating IL-6 and IL-10 receptor signaling (209).
Classically activated M1 macrophages produce nitric oxide synthase, IL-12 and TNFα and promote Th1 cell responses, while activated M2 macrophages produce arginase-1, IL-10 and TGFβ and relate with the Th2 cell response. M1 macrophages are pro-inflammatory, while M2 macrophages are anti-inflammatory (210). Tumor-associated M2 macrophages not only promote tumor progression and metastasis by producing tumor growth factor and angiogenic factors, such as epidermal growth factor (EGF), VEGF and IL-6, but also inhibit tumor immunity by arginase-1, IL-10 and TGFβ (211–214). IL-6 and IL-10 are abundant in tumor microenvironments originated from myeloid cells, fibroblasts and tumor cells, and they further induce M2 macrophage differentiation through STAT3 (215, 216). Breast cancer-derived exosomes that contain gp130 induce IL-6 production and activate gp130–STAT3 signaling to induce phenotypic changes in bone marrow-derived macrophages toward M2 macrophages (217).
Myeloid-derived suppressor cells (MDSCs), which are abundant in tumor microenvironments, inhibit T-cell activation to suppress tumor immunity by producing IL-10 and TGFβ (218). MDSC function is dependent on STAT3 (25). Tumor-derived Hsp72 mediates the MDSC suppressive activity of tumor growth in a manner dependent on STAT3 activation through the autocrine production of IL-6 (Fig. 2) (219).
Inhibitors of immune checkpoints, such as inhibitors of CTLA-4 and PD-1 and their ligands, have been shown to be effective to treat several cancers such as melanoma (25, 220). PD-L1, which is a ligand of PD-1, is expressed in tumor microenvironments and tumors in a manner dependent on STAT3. For example, the STAT3-dependent expression of PD-L1 in pancreatic carcinoma and head and neck squamous carcinoma was reported (221, 222). The direct binding of STAT3 to the PD-L1 promoter was also shown (223). PD-L1 is expressed in non-small-cell lung cancer cells through EGF receptor (EGFR)-mediated IL-6–STAT3 activation (224). Cancer-associated fibroblasts induce PD-L1 in neutrophils in an IL-6–STAT3-dependent manner (225). In addition, glioblastoma and tumor-associated stromal myofibroblasts induce PD-L1 expression in DCs through IL-6–STAT3 signaling (Fig. 2) (226, 227).
All evidence indicates that IL-6–STAT3 signaling determines the homeostasis of Th17 cells and Treg cells. Th17 cells are favored for inflammation and autoimmunity, while Treg cells suppress these responses. Interestingly, the suppressive activity of Treg cells is observed in several autoimmune diseases (163, 228). IL-6 makes Teff cells resistant to the suppressive effect of Treg cells (195, 196). In addition, IL-6–STAT3 signaling induces the conversion of Treg cells to Th17 cells, which are pro-inflammatory, and induces the differentiation of M2 macrophages and MDSCs, both of which suppress tumor immunity. IL-6 further inhibits DC maturation and up-regulates PD-L1 through STAT3 to suppress T-cell activation against tumors. Moreover, IL-6 itself is an autocrine and paracrine growth factor as well as a survival factor for a variety of cancers and promotes cancer development and progression by inducing angiogenesis and metastasis. Overall, accumulating evidence supports the intimate relationship of IL-6 with inflammation, autoimmunity and cancer (Fig. 2).
Involvement of IL-6 in chronic inflammation, autoimmune diseases and cancer
Chronic inflammation is often accompanied with autoimmune disease and cancer (2, 4, 9). Autoimmune diseases are thought to result from a breakdown in self-tolerance and/or dysregulation of immune responses. However, true pathogenic antigens causing the breakdown have not been identified for many autoimmune diseases, including RA and other tissue-specific disorders (229–231). This raises the possibility that a breakdown in tolerance to a tissue-specific antigen is not always required for localized autoimmune diseases. Instead, hyper-activation of the immune system to the target tissue may be a consequent event that is initiated by local initiators in non-immune target tissue in a manner dependent on genetic and/or environmental factors (1, 47, 48, 50). This view highlights the importance of local initiators in the target tissue as a trigger of autoimmunity (49, 51, 52, 57, 232). Even in cancer development, it is now known that only 5–10% of all cancers are due to an inherited gene defect, and the remaining 90–95% have their roots in an environment and lifestyle that are intimately related with chronic inflammation (233). Therefore, rather than the dogma that oncogenesis is intrinsically triggered in pre-neoplastic cells, environmental factors, such as infection, stress, obesity, aging and smoking, each of which can induce chronic inflammation, could be a major cause of oncogenesis (4, 6, 9, 233).
Just after the molecular cloning of IL-6, cardiac myxoma cells were found to produce IL-6 (42). Patients with cardiac myxoma show a variety of autoimmune symptoms, including hypergammaglobulinemia, auto-antibodies and increased acute-phase proteins. These symptoms disappear after surgical resection of the tumor, suggesting the intimate relationship between cardiac myxoma cells and autoimmune symptoms. In addition, it was found that synovial fluid obtained from patients with RA contains high amounts of IL-6 (44, 45), and serum IL-6 levels in RA patients correlate with clinical and laboratory indices of the disease (234). In addition, serum IL-6 levels are increased and correlate with the poor prognosis of multiple myeloma patients (235). Taking the above together with the fact that IL-6 is a growth factor for plasmacytoma and myeloma (28, 37) and the production of IL-6 in Castleman’s germinal center (43) suggests that IL-6 is involved in inflammation, autoimmunity and B-cell malignancies. Of note is that the pleural effusion cells of patients with pulmonary tuberculosis produce a large amount of factors inducing immunoglobulin production (236); one of the factors was partially purified as a TRF-like factor with similar properties to IL-6 (237). Importantly, an intimate relationship between tuberculosis and autoimmunity and B-cell malignancies was reported (238–240). Furthermore, pristane and mineral oil, strong inducers of chronic inflammation and later found to induce IL-6 production, develop plasmacytoma, arthritis and auto-antibody production in mice (241–245). Accordingly, IL-6 transgenic mice develop polyclonal plasmacytosis and monoclonal plasmacytoma in C57BL/6 and BALB/c genetic backgrounds, respectively (147, 246). Moreover, IL-6 induces CRP and fever (247, 248). All these early studies more than 25 years ago support the idea that IL-6 is involved in diseases (1, 80). In 1994, Kopf et al. showed that IL-6-deficient mice have impaired immune responses against vaccinia virus and Listeria monocytogenes, T-cell-dependent antibody responses against vesicular stomatitis virus and inflammatory acute-phase responses after tissue damage or infection (148), confirming the pleiotropic function of IL-6 and its role in immune responses as well as inflammation. By utilizing IL-6-deficient mice, it was shown that IL-6 is required for type II collagen-induced arthritis (249), antigen-induced arthritis (AIA) (250), EAE (251, 252), pristane-induced autoantibody production (253) and plasmacytoma (254), further showing that IL-6 is involved in experimental autoimmune diseases and B-cell malignancies. However, experimental autoimmune disease models usually utilize autoantigens in the presence of adjuvants as an inducer of the disease, making it difficult to interpret the results obtained from these experiments in relation to naturally occurring diseases. From this point of view, F759 mice are an ideal murine model of RA, which show an increased activation of STAT3 through gp130 because of the lack of negative regulation exerted by SOCS3 (63, 113). Of note is that F759 mice spontaneously develop IL-6-dependent and CD4(+) T-cell-dependent F759 arthritis in a manner dependent on age, supporting the idea that enhanced but dysregulated IL-6–STAT3 signaling is involved in age-related inflammatory autoimmune diseases, such as RA. Furthermore, F759 arthritis is enhanced by human T-cell lymphotropic virus 1 (HTLV-1) pX gene, which encodes Tax, a transcriptional trans-activator of NF-κB, showing the synergistic effect of STAT3 and NF-κB (255).
Another knock-in mouse strain (gp130Y757F/Y757F mice) having the point mutation Y759F in murine gp130 also shows the hyper-activation of STAT3 and develops gastric hyperplasia resembling human early-stage gastric cancer (64, 256). Further, the mice show a similar expression pattern of STAT3-dependent miR-200 family members with that of early stage gastric cancer patients (142). Gp130Y757F/Y757F mice show enhanced colitis-associated tumorigenesis in a manner dependent on the enhanced activation of STAT3 (20). The requirement of IL-6 and STAT3 for activated mutant EGFR-induced lung cancer and colitis-associated cancer has also been demonstrated (18, 257). Taken together with the fact that the development of pristane or mineral oil-induced plasmacytoma and obesity-related hepatocellular carcinoma (HCC), both of which are related to inflammation, are dependent on IL-6 (254, 258), all studies indicate the intimate link between inflammation and tumorigenesis via IL-6–STAT3 signaling.
The reason why different phenotypes are observed between F759 mice and gp130Y757F/Y757F mice is not known, but the reason could be due to the difference of gp130; the former is human gp130 and the latter is mouse gp130. In fact, it takes about 1 year for F759 mice to develop arthritis, while gp130Y757F/Y757F mice show hyperproliferative lesions in the stomach mucosa as early as 6 weeks (256). It has not yet been reported whether gp130Y757F/Y757F mice spontaneously develop arthritis as F759 mice do, but AIA, which is also IL-6-dependent, is enhanced in gp130Y757F/Y757F mice in a manner dependent on STAT3 (259). Thus, it seems the IL-6–STAT3 axis is involved in inflammation, autoimmunity and cancer and that they are all intimately related to each other.
In line with this notion, there is a correlation between IL-6 and the severity of RA and other inflammatory and autoimmune diseases (3, 260, 261). In addition, the correlation between IL-6 and the prognosis of 23 different cancer types was demonstrated (262). Genome-wide association studies (GWAS), meta-analysis, exome analysis and single nucleotide polymorphism (SNP) mapping have associated IL-6, IL-6R and gp130 with inflammatory diseases such as RA and coronary artery disease (263–269). It was also reported that IL-6R is associated with asthma and atopic dermatitis (270, 271). Somatic GOF mutations in gp130 that activate gp130–STAT3 signaling lead to inflammatory hepatocellular tumors (272). LOF mutations of TRAF3, a negative regulator of IL-6–STAT3 signaling, are observed in B-cell lymphoma and multiple myeloma patients (122, 273, 274). On the other hand, the frequency of a polymorphism at the 5’ flanking region of the IL-6 gene that is correlated with lower levels of plasma IL-6 is reduced in systemic-onset juvenile chronic arthritis (275). Further, a non-conservative SNP in the gp130, Gly148Arg, which has low IL-6 responsiveness, is associated with a decreased risk of myocardial infarction in a hypertensive population (276).
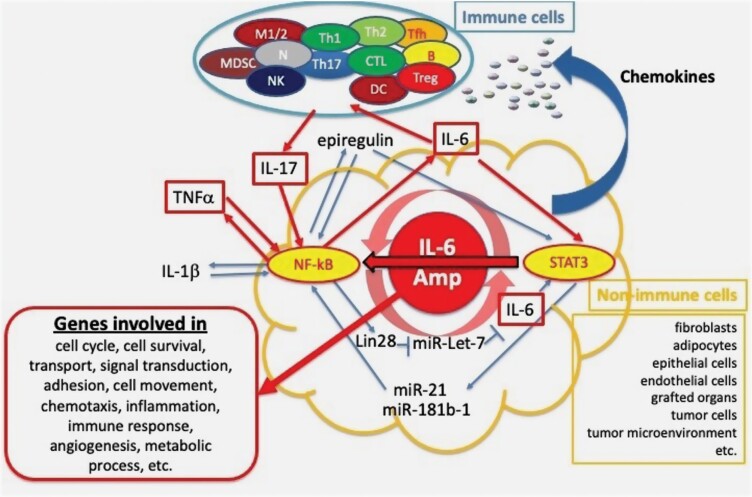
Cross-talk between non-immune cells and immune cells through the IL-6 Amp
Although the development of F759 arthritis is dependent on Th17 cells, the F759 mutation is required in non-immune cells but not immune cells, clearly indicating that the interaction between non-immune cells and immune cells is crucial for arthritis development in F759 mice (66, 99). In fact, a mutated gp130-mediated excessive production of cytokines and chemokines in non-immune cells in F759 mice is necessary for CD4(+) T-cell proliferation, Th17 cell accumulation in the lesion and the arthritis development (66, 99). The effects of non-immune cells in F759 arthritis is explained by the capability of these cells to produce large amounts of chemokines, growth factors and IL-6 under the situation where gp130-mediated STAT3 activation is enhanced. Furthermore, IL-6 and IL-17 or TNFα synergistically enhance the production of various pro-inflammatory mediators including IL-6 from non-immune cells in a manner dependent on STAT3 and NF-κB (66). The produced IL-6 further induces Th17 cell differentiation through STAT3 in the presence of TGFβ, IL-1β and IL-23, all of which are rich in inflammatory lesions and tumor microenvironments (164, 166, 169–171, 174, 175). Therefore, there is an in vivo positive-feedback amplification loop of IL-6 production via Th17 cell differentiation and their interaction with non-immune cells, such as fibroblasts (41). In addition, the enhanced production of epiregulin and TNFα is induced by the activation of the IL-6 Amp, and these molecules further activate NF-κB alone or STAT3 as well (10). Therefore, amplification of the IL-6–STAT3 axis is augmented by several pathways after the induction of other STAT3 and NF-κB activators during inflammation processes (Fig. 3) (41, 66). Of note is that the IL-6 Amp enhances NF-κB activity by STAT3 through the interaction of these two molecules. Therefore, the IL-6 Amp amplifies not only IL-6 but also a variety of pro-inflammatory cytokines and growth factors that are targets and/or activators of the NF-κB pathway. STAT3 activation is also augmented through enhanced IL-6 production. Consistent with the concept that IL-6 Amp activation in non-immune cells plays a pivotal role in the development of autoimmune diseases, mice devoid of STAT3 or gp130 in non-immune cells like type-1 collagen positive cells are highly resistant to F759 arthritis and EAE (54, 66).
Fig. 3.
The IL-6 Amp. STAT3 activators (e.g. IL-6) and NF-κB activators (e.g. IL-17 or TNFα) synergistically enhance the production of various pro-inflammatory mediators including IL-6 from non-immune cells in a manner dependent on STAT3 and NF-κB. This amplification mechanism is called the IL-6 amplifier (IL-6 Amp). The IL-6 Amp recruits immune cells such as activated T cells into the lesion by chemokines. The interaction between immune cells and non-immune cells further strengthens the IL-6 Amp. The IL-6 Amp enhances the expression of many genes involved in cell proliferation, survival, movement, inflammation, angiogenesis and so on.
The IL-6 Amp could be exerted by several mechanisms. For example, STAT3 prolongs NF-κB nuclear retention through acetyltransferase p300-mediated RelA acetylation, thereby interfering with NF-κB nuclear export in both cancer cells and tumor-associated hematopoietic cells (277). The cooperative role of NF-κB and STAT3 recruitment to ICAM-1 intronic consensus elements in the invasion and migration of radiation-induced glioma was also reported (278). STAT3 directly binds to the IL-6 promoter to induce IL-6 gene expression (82, 83). In addition, STAT3 activates NF-κB through the direct induction of miR-21 and miR-181b-1, leading to IL-6 gene expression (90). NF-κB also increases IL-6 levels by inhibiting let-7 expression (89).
As described above, the IL-6 Amp is a mechanism by which the regional production of a variety of cytokines and growth factors is augmented through the interaction between NF-κB and STAT3, both of which are activated not only in inflammatory lesions but also in tumor microenvironments and neoplastic tumor cells. Furthermore, NF-κB and STAT3 play crucial roles in cancer development and progression (19, 25, 67, 279). Thus, the IL-6 Amp plays a crucial role in not only chronic inflammatory and autoimmune diseases but also cancer. In fact, a comparative analysis between GWAS data and the targets or regulatory genes of the IL-6 Amp revealed that 202 out of 1700 screened genes show over 490 indications of association not only with autoimmune diseases but also with metabolic syndromes, neurodegenerative diseases and other chronic inflammatory diseases, including RA, lupus, pancreatitis, thyroiditis/Graves’ diseases, type 1 diabetes (T1D) and type 2 diabetes (T2D), MS, cardiovascular diseases/atherosclerosis/systemic sclerosis, Alzheimer’s disease/hippocampal atrophy, pulmonary disease/asthma/cystic fibrosis, hepatitis, inflammatory bowel disease/colitis, stroke and nephropathy/glomerulonephritis (10). Furthermore, many cancer-associated genes were identified as regulators or target genes of the IL-6 Amp (11). Ingenuity Pathways Analysis (IPA) showed that these genes are related with multiple biologic processes, such as cell development, cell cycle, transport, signal transduction, adhesion, cell movement, chemotaxis, immune response, angiogenesis and metabolic process. Moreover, the IL-6 Amp is related with various types of cancer, including hematologic malignancies, tumors in lung, and colorectal/intestinal, urinary/bladder/vulvar, breast, stomach and liver cancers (11).
The IL-6 Amp, which is activated not only in non-immune cells such as fibroblasts and endothelial cells but also in grafted organs and tumor cells, acts as a linker between these cells and immune cells by attracting immune cells through the production of a variety of chemokines. Accumulated immune cells interact with non-immune cells in inflammatory lesions and tumor microenvironments as well as with tumor cells to further enhance the IL-6 Amp by producing not only IL-6 but also a variety of IL-6 Amp stimulators such as IL-17, TNFα, IL-1 and epiregulin. Target molecules of the IL-6 Amp include EGFR, c-Myc, Pim1, VEGFα, hypoxia-inducible factor 1-alpha (HIF1-α), MMPs and many pro-inflammatory cytokines and growth factors involved in cell survival, proliferation, angiogenesis and metastasis (Fig. 3) (10, 11).
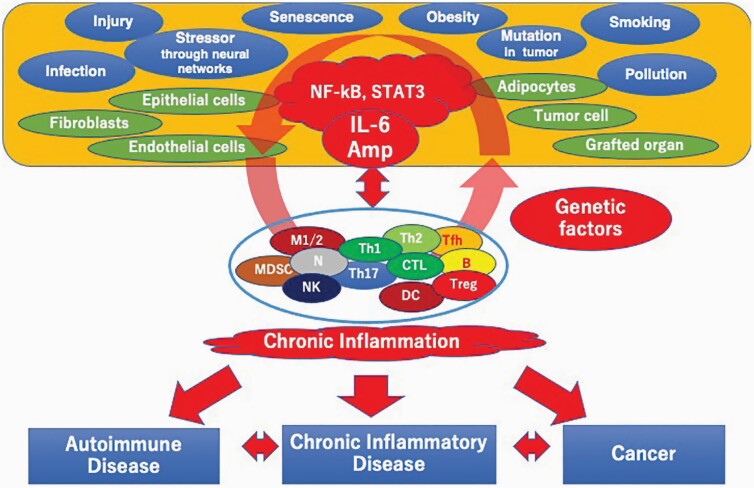
The local initiation model
In 1964, Boyden pointed out the importance of local initiators such as injury or infection as triggers of inflammation followed by the destruction of the target tissues (47). Decades later, Wilkin proposed the primary lesion theory, in which a primary lesion triggers autoimmunity, rather than the popular view, which held the primary cause of autoimmunity was the breakdown of self-tolerance (48).
Patients with RA show a variety of symptoms, including polyclonal plasmacytosis accompanied by the production of rheumatoid factor, enhanced bone resorption and increases in the amount of acute-phase proteins, agalactosyl IgG and platelet numbers. None of these phenotypes at first glance appear related to each other, suggesting that complex factors are involved in RA. However, the pleiotropic nature of IL-6, which induces B-cell differentiation with immunoglobulin production (27), osteoclast activation (280, 281), the production of acute-phase proteins (39, 40), the increase of agalactosyl immunoglobulin (282) and megakaryocyte differentiation (281, 283, 284), suggested an intimate relationship between IL-6 and RA. Assuming that the same cause can induce both RA and IL-6 expression, such an intimate relationship could be explained. This possibility led to a working hypothesis (1, 46), the updated version of which is called the local initiation model (Fig. 4). In this model, NF-κB and STAT3 are activated by a variety of local initiators, including injury, infection, stressors, age-related events in senescent cells and oncogenic mutation in pre-neoplastic cells, leading to the activation of the IL-6 Amp in non-immune cells, such as fibroblasts, epithelial cells, endothelial cells and adipocytes. The IL-6 Amp enhances the production of a variety of pro-inflammatory cytokines and chemokines, resulting in the recruitment of immune cells, such as activated T cells into the lesion. The interaction between immune cells, in particularly activated T cells, further strengthens the IL-6 Amp. The IL-6 Amp can become dysregulated depending on the genetic background and other factors including local initiators, leading to inflammatory diseases and autoimmune diseases. Because initial events occur in non-immune cells or tissues, this model strengthens the importance of both local initiators in the target tissue and the interaction between non-immune and immune systems in the disease onset and progression. The local initiation model is similar to the primary lesion theory proposed by Wilkin (48), but the former clearly shows the key role of transcription factors, such as NF-κB and STAT3, which can simultaneously induce multiple actions and be activated by a variety of local initiators. Therefore, the local initiation model could be applied not only to chronic inflammatory diseases and autoimmune diseases, but also to age-related diseases and cancer (Fig. 4).
Fig. 4.
Local initiation model. A variety of local initiators, such as infection, injury, stressors acting through neural networks, senescence, obesity, smoking and oncogenic mutations, activate both STAT3 and NF-κB, leading to activation of the IL-6 Amp in non-immune cells such as fibroblasts, epithelial cells, endothelial cells and adipocytes. The IL-6 Amp amplifies the production of IL-6 and other pro-inflammatory cytokines and growth factors. Chemokines produced by the IL-6 Amp recruit immune cells such as activated T cells to the lesion to interact with non-immune cells, leading to further activation of the IL-6 Amp. The IL-6 Amp becomes dysregulated depending on the genetic background and or other factors including the properties of local initiators, leading to chronic inflammatory diseases, autoimmune diseases and cancer.
One clear piece of evidence supporting the local initiation model has been obtained from F759 mice. F759 mice bred by mating T-cell antigen-receptor transgenic mice and Rag2-KO mice to express only one T-cell antigen-receptor on CD4(+) T cells still develop arthritis. These results suggest even T-cell-dependent tissue-specific autoimmune diseases do not necessarily require antigen-specific T cells (52). The question is, what determines the tissue specificity of the autoimmune disease without tissue-specific CD4(+) T cells? Murakami et al. demonstrated that local initiators such as microbleeding induce the accumulation of T cells in the joints through CCL20 production (52). The disease induction requires IL-17A production by transferred T cells, IL-6 and CCL20 expression and STAT3 signaling in type I collagen-expressing cells. This is consistent with the IL-6 Amp being involved in the disease.
Persistent local initiator activity, such as chronic infections, with or without genetic factors leads to chronic activation of the IL-6 Amp. This effect induces the manifestation of inflammatory diseases and autoimmune diseases (232). This scenario highlights the importance of local initiators and supports the local initiation model (Fig. 4). It is also consistent with the fact that many chronic inflammatory diseases are dependent on aging and accompanied by the activation of polyclonal T cells and an increase of IL-6 (285).
Local initiators activating the IL-6 Amp in chronic inflammation
A variety of stressors, such as pain, light and gravity are sensed by a sensory–sympathetic neural network. Neuroinflammation is associated with the invasion of various immune cells in the central nervous system (CNS) followed by the dysregulation of homeostasis in the brain and spinal cord. However, the CNS is protected by the blood–brain barrier, which tightly limits the traffic of substances and immune cells from the blood. In an adoptive transfer model of EAE using myelin-specific autoreactive CD4(+) T cells, it was found that the initial invasion site of these cells is determined by specific neural activation through the sensory–sympathetic pathway stimulated by gravity (54). This neural pathway, which is now called the gateway reflex (286, 287), activates the IL-6 Amp through beta-adrenergic receptors in the dorsal vessels of the fifth lumbar cord, allowing for autoreactive T-cell accumulation and disease onset (54). Further, pain sensation induces a relapse of EAE by activating the IL-6 Amp through another sensory–sympathetic neural network (55). Consistent with this, it was reported that adrenergic receptor stimulation not only activates STAT3 in an ovarian cancer cell line (288) but also enhances the IL-6 production that is induced by IL-1β, an NF-κB activator in cardiomyocytes, to induce cardiac hypertrophy (289). Additionally, it was shown that acute stress induces a systemic increase of IL-6 secreted from brown adipocytes in a beta-3-adrenergic-receptor-dependent manner in mouse models (290).
These studies provide evidence supporting the claim that a variety of stressors, such as gravity and pain, act as local initiators through specific neural pathways, resulting in activation of the IL-6 Amp, linking inflammation and autoimmunity and possibly affecting cancer development and progression.
Age-related changes in senescent cells also act as local initiators. Senescent fibroblasts secrete high levels of several MMPs, EGF and inflammatory cytokines, resembling fibroblasts undergoing a wound response or associations with cancer. Of note, the local low-grade inflammation that characterizes aging is triggered by senescent cells and is intimately related to age-related diseases such as cardiovascular diseases and cancer (5, 291, 292). It might also be associated with the cytokine storm in COVID-19 (293, 294). These mediators maintain and propagate the senescence process to neighboring cells and then recruit immune cells to clear the senescent cells. In this scenario, Campisi proposed a model in which senescent cells by themselves contribute to the disruption of normal tissues through the production of degradative enzymes as well as inflammatory cytokines, while senescent cells help pre-neoplastic mutated cells to proliferate by producing inflammatory cytokines (5). NF-κB-regulated and C/EBPβ-regulated cytokines such as IL-6 and CXCR2-binding chemokines including IL-8, which are produced by senescent cells, play crucial roles in the senescence process (7, 8). IL-6–STAT3–PIM-1 signaling is involved in cytokine-induced senescence (295). Importantly, senescent cells and tissues contribute to age-related pathologies including cancer by producing inflammatory cytokines such as IL-6, which act as autocrine and paracrine factors (7). Consistently, IL-6 levels increase with age (296, 297). Concerning age-related diseases, senescent cells themselves are critically involved in T1D and T2D, and the deletion of senescent beta cells prevents diabetes (57, 298), indicating that even in T1D in which tissue-specific T cells are involved (299–301), local initiators originating from senescent beta cells play critical roles. This process is consistent with the idea that the primary cause of T1D may be a senescence-induced local initiator that can activate the IL-6 Amp rather than the breakdown of self-tolerance.
Obesity causes chronic low-grade inflammation and is closely related with chronic inflammatory diseases, such as cardiovascular diseases and T2D and some cancers, such as breast, liver and colon cancers (233, 302–304). The enlargement of adipose tissue in obesity induces mechanical stress, ER stress and hypoxia in adipocytes, resulting in the release of free fatty acids (FFAs) and inflammatory cytokines such as IL-6 and TNFα and chemokines (303–305), suggesting activation of the IL-6 Amp. Consistently, these events recruit macrophages, which further produce IL-6 and TNFα, major players involved in obesity-induced low-grade inflammation and cancer development (303, 304). Shi et al. showed that FFA activates TLR4 signaling and that mice lacking TLR4 are partially protected against high fat diet-induced insulin resistance (306). In line with these findings, FFA activates NF-κB through TLR4, leading to the expression of monocyte chemotactic protein-1 (MCP-1) to recruit macrophages, which further produce IL-6 and TNFα (307, 308). IL-6–STAT3 signaling in adipocytes is known to be involved in adipocyte-induced EMT in breast cancer cells (23) and obesity-promoted HCC (258). Lysophospholipid sphingosine-1-phosphate (S1P), a lipid metabolite, activates STAT3 through its G protein-coupled receptor, S1P receptor-1 (309). Intracellular S1P induces IL-6 production through NF-κB activation, resulting in the activation of both STAT3 and NF-κB, major players of the IL-6 Amp. This process is critically involved in colitis-associated cancer (310). These findings support the idea that obesity-induced mechanical and/or ER stress and lipid metabolites act as local initiators in the target tissue to trigger chronic activation of the IL-6 Amp.
Pre-neoplastic cells or cancer cells by themselves act as local initiators much like senescent cells do. Either or both of STAT3 and NF-κB are activated in a variety of tumors, including lung, breast, pancreatic and prostate cancers (67). Additionally, either or both are activated in cells transformed with HTLV-1 (311), v-src (312), abl (313), bcr-abl or v-eyk (314). K-RAS mutation is often observed in many cancers, such as lung cancer and pancreatic cancer. Mutated K-RAS activates NF-κB in a mouse model of lung cancer (315), and the K-RAS-induced activation of NF-κB is required for pancreatic cancer development (316), which depends on IL-6 trans-signaling-mediated STAT3 activation (317). Mesothelin (MSLN) is up-regulated following K-RAS, p53 and p16 mutations in pancreatic cancer (318). MSLN is also suggested to be involved in the progression of breast cancer, ovarian cancer and pancreatic cancer. It confers pancreatic cancer cell resistance to TNFα-induced apoptosis through NF-κB activation and the enhanced expression of IL-6 (319). MSLN also promotes pancreatic cancer cell proliferation through autocrine IL-6 trans-signaling (320). Similarly, activated mutant EGFR in lung cancer induces IL-6 gene expression to activate constitutive IL-6–STAT3 signaling in a paracrine and autocrine manner (257). HER2 overexpression occurs in approximately 25% of breast cancers. Its expression in breast cancer activates an IL-6 autocrine signaling loop to activate STAT3, which is critical for tumorigenesis (321). The loss of p53 alone is insufficient to initiate intestinal tumorigenesis but markedly enhances carcinogen-induced tumor incidence, the progression of which is associated with increased intestinal permeability, causing the formation of a NF-κB-dependent inflammatory microenvironment (322). Another oncogenic molecule, BRAFE600, induces IL-6 and IL-1, a NF-κB activator, through C/EBPβ (7).
All the above results are in line with cancer cells activating the IL-6 Amp through the direct or indirect activation of NF-κB and STAT3, likely resulting in the recruitment of Th17 cells and/or myeloid cells to further enhance the IL-6 Amp. RANTES and MCP-1 secreted by tumor cells and tumor-derived fibroblasts mediate the recruitment of Th17 cells (159). Exosomal miR-1247-3p secreted by hepatocellular carcinoma activates beta1-integrin–NF-κB signaling in fibroblasts, resulting in the production of pro-inflammatory cytokines, including IL-6 and IL-8 (323). The IL-6 Amp at the leading edge could play a critical role in tumor progression. Indeed, Chang et al. showed that IL-6–STAT3 signaling is increased at the leading edge of breast tumors to promote MDSC recruitment, angiogenesis, fibroblast infiltration and metastases (83).
Infection is a local initiator that triggers and maintains inflammation, leading to chronic inflammatory diseases and cancer. For the initial detection of microbes, the immune system utilizes pattern-recognition receptors (PRRs), such as TLRs to activate MyD88-dependent signaling and ultimately activate NF-κB (324). In addition to NF-κB activation, TLRs such as TLR2, TLR4, TLR7 and TLR9 activate STAT3 (206, 325). TLR stimulation also induces IL-6 production and other pro-inflammatory cytokines through NF-κB, leading to activation of the IL-6 Amp. Therefore, infection is one trigger of the IL-6 Amp. Indeed, a human colonic bacterium, enterotoxigenic Bacteroides fragilis (ETBF)-derived toxin, which triggers colitis and induces colonic tumors in mice, activates the STAT3 and Th17 response (326). Helicobacter pylori, which induces gastritis and is related to gastric cancer, activates STAT3 in epithelial cells (327). Both hepatitis B and hepatitis C viruses, which induce hepatitis and cause hepatocellular carcinoma, activate STAT3 (328–330), while HTLV-I, Epstein–Barr virus and papilloma virus activate STAT3 and NF-κB (311, 331, 332).
Cytokine storm, uncontrolled acute inflammation
COVID-19, which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is now a pandemic. The life-threatening phenotype of COVID-19 is severe acute respiratory distress syndrome (ARDS) (333). ARDS is a lethal syndrome induced by mechanical injury and infection such as pneumonia, sepsis and trauma (334). ARDS in COVID-19 is considered the result of cytokine storm (12–17), resembling the disease caused by SARS-CoV-1 and Middle East respiratory syndrome coronavirus (MERS-CoV) (335). Cytokine storm is uncontrolled and rapidly progressing inflammation accompanied by the massive production of pro-inflammatory cytokines, chemokines and growth factors. Consistent with the notion that severe COVID-19 is a cytokine storm syndrome (12–17, 336), the severity of COVID-19 is associated with an increased level of inflammatory cytokines, such as IL-6, granulocyte macrophage colony-stimulating factor (GM-CSF) and TNFα (333, 337). Among the elevated inflammatory mediators, the blood IL-6 level is highly correlated with the disease mortality (293, 338) and predicts the need for mechanical ventilation (339). Notably, IL-6 and TNFα serum levels are known to be significant predictors of disease severity and death (340).
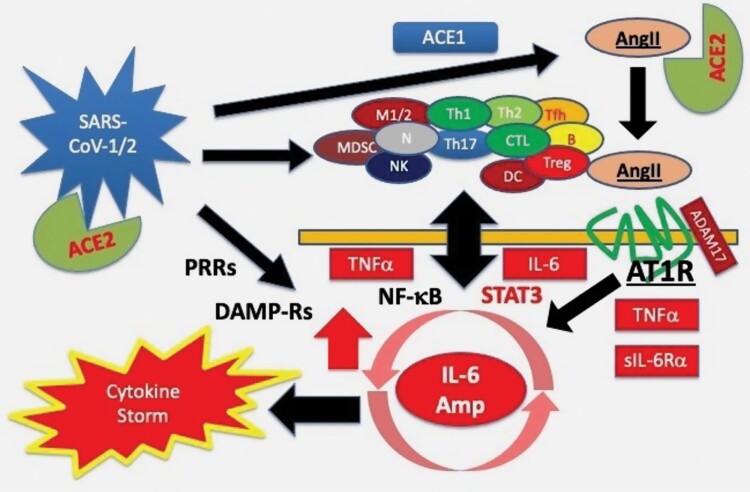
SARS-CoV-1 and MERS-CoV activate NF-κB in a manner dependent on MyD88 through PRRs, such as retinoic acid-inducible gene I protein (RIG-I) and melanoma differentiation-associated protein 5 (MDA5), leading to the activation of a variety of pro-inflammatory cytokines, including IL-6, TNFα, IL-8 and CC-chemokine ligand 2 (CCL2) (335). In addition to this PRR-mediated activation of NF-κB, the nucleocapsid protein of SARS-CoV-1 activates IL-6 expression through NF-κB by facilitating the translocation of NF-κB from the cytosol to the nucleus (341). Since SARS-CoV-2 uses angiotensin-converting enzyme (ACE) 2 as a receptor (342, 343), it is speculated that SARS-CoV-2 induces pro-inflammatory cytokines through angiotensin II (AngII)/angiotensin type 1 receptor (AT1R) (15) as SARS-CoV-1 does (344–346).
The AngII–AT1R axis activates the NF-κB pathway through various growth factors and pro-inflammatory cytokines (347, 348). This axis activates ADAM17, which generates the mature form of EGFR ligand and TNFα, two NF-κB stimulators (346). Furthermore, ADAM17 increases sIL-6Rα, which activates STAT3 through gp130 on a variety of non-immune cells including fibroblasts, endothelial cells and epithelial cells (33, 96). Therefore, it is likely that the AngII–AT1R axis is involved in the ARDS induced by SARS-CoV-2 infection (15), which is like SARS-CoV-1-induced ARDS in a mouse model (344).
Therefore, SARS-CoV-1 and SARS-CoV-2 infection activate both NF-κB and STAT3, key elements of the IL-6 Amp, to cause cytokine storm (12, 13, 15, 349, 350). Since an activated IL-6 Amp enhances the production of chemokines to recruit lymphoid cells and myeloid cells including Th17 cells in the lesion, the IL-6 Amp could be further enhanced (66).
Cytokine storm also occurs in CAR-T treatment, which is used to treat leukemia. It is triggered by the activation of CAR-T cells that recognize cognate antigens expressed by tumor cells, leading to the release of cytokines and chemokines, including IL-6 in parallel with the release of pro-inflammatory cytokines and chemokines by monocytes and/or macrophages (351, 352). IL-1 and IL-6 are involved in the lethal cytokine storm sometimes seen in CAR-T treatment (353, 354).
The massive cell death commonly observed in cytokine storm, regardless of the inducer type, activates damage-associated molecular pattern (DAMP) receptor-mediated signaling pathways and/or TLR-mediated ones. These events further induce pro-inflammatory cytokines including IL-6 through NF-κB activation.
Taking together all the evidence described above, a possible mechanism of SARS-CoV-1-induced and SARS-CoV-2-induced cytokine storm is illustrated in Fig. 5. This model could be applied to ARDS induced by other causes. ARDS with a cytokine storm occurs in viral infections such as MERS-CoV, influenza virus and sepsis. Furthermore, it also occurs due to lung damage caused by gastric acid or inappropriate operation of a ventilator, like aspiration pneumonia (334). The AngII–AT1R signaling system plays an important role not only in pneumonia but also in ARDS model mice (345), indicating that lung injury itself activates the AngII–AT1R signaling. Macrophage activation via TLR4, a type of PRR, is also involved in gastric acid-induced ARDS and mouse ARDS models induced by SARS-CoV-1 or influenza virus H5N1 (355). Furthermore, it has been shown that ARDS and renal dysfunction induced in a sepsis rat model are suppressed by anti-IL-6R antibody through the suppression of NF-κB activation (356). Interestingly, ACE1 gene polymorphisms are involved in the development and severity of ARDS (357). Furthermore, the ACE1 II genotype is protective against COVID-19 as compared to the ACE1 DD genotype (358), and serum levels of ACE1 are higher in the DD genotype compared with the II genotype (359).
Fig. 5.
A possible mechanism of SARS-CoV-1/2-induced cytokine storm. Because SARS-CoV-1/2 utilizes ACE2 as a receptor, virus infection decreases the cell surface expression of ACE2, which is a peptidase of angiotensin II (AngII), resulting in an increase of AngII. In addition, virus-induced lung injury activates ACE1, further increasing serum AngII levels. As a result, AT1R-mediated signaling is enhanced. In turn, so too is the inflammatory response, including TNFα and sIL-6Rα via ADAM17 activation. Virus infection itself activates signaling through pattern-recognition receptors (PRRs). Furthermore, virus-induced massive cell death can activate DAMP receptor-mediated signaling pathways. Moreover, virus infection activates and/or recruits lymphoid cells and myeloid cells in the lesion. All these events synergistically activate the IL-6 Amp through the interaction of STAT3 and NF-κB, leading to cytokine storm.
Consistent with animal models, it was reported that AngII–AT1R axis inhibitors may be beneficial for COVID-19 patients (360–363) to decrease serum IL-6 levels (360). The anti-IL-6R antibody tocilizumab is effective at treating patients with CAR-T-induced cytokine release syndrome (CRS) (352, 364) and is being considered for treating ARDS in COVID-19 patients (365–368). Baricitinib, an inhibitor of JAK1 and JAK2, is reported to prevent COVID-19 severity followed by lowering IL-6 and TNFα levels (369). In addition, dexamethasone reduces the death rate of patients with severe COVID-19 (370).
Of note, aging, obesity and inflammation-related diseases such as diabetes and cardiovascular diseases have been shown to be risk factors for the severity of COVID-19 (293, 371–373). As discussed in this manuscript, these risk factors are all associated with chronic inflammation, which could decrease the threshold of the activation of the IL-6 Amp to induce cytokine storm.
Conclusion and perspectives
At the time of its discovery in 1986, IL-6 was considered just one of many cytokines. It has since been clarified that IL-6 is a critical factor in inflammation, autoimmunity and cancer, and its inhibitors are used as therapeutic agents for several diseases already, with the potential of being expanded to more in the future. The anti-IL-6R antibodies tocilizumab and sarilumab are used to treat RA, Castleman’s disease and CAR-T-induced CRS (71–75, 352, 364) and have promise for treating the severe form of COVID-19 (365–367). Other inhibitors against the IL-6–STAT3 signaling pathway are under development (19, 21, 24–26, 76, 374).
One possible explanation for why inhibiting IL-6 activity is effective against inflammation-related diseases, in spite of the many cytokines involved, is that in inflammation IL-6 is the major stimulator of STAT3, which plays important roles in inflammation and oncogenesis together with NF-κB, which expresses IL-6 as a target. Therefore, NF-κB and STAT3 are the basis of the IL-6 Amp which is the amplification mechanism of IL-6 itself and other pro-inflammatory molecules, such as cytokines, chemokines and growth factors. A variety of local initiators, such as infection, stressors, injury, senescence, obesity, pre-neoplastic mutation, cell death and smoking can activate the IL-6 Amp, which mediates the interaction between non-immune cells and immune cells, leading to the manifestation of inflammatory and autoimmune diseases and cancer. These observations have led to a strategy targeting the IL-6–STAT3 signaling axis to treat related diseases.
However, many questions remain. One of the reasons why IL-6 is a key cytokine in inflammation is that it has a wide range of target cells because of its trans-signaling mechanism. IL-6 usually acts on lymphoid and myeloid immune cells expressing both IL-6Rα and gp130, but it acts on a wide range of non-immune cells as well, including fibroblasts and endothelial cells that express gp130 during inflammation. For this action, sIL-6Rα is required. Therefore, more study of the mechanism by which sIL-6Rα is generated is required to understand inflammation and develop therapeutics (96). Another question concerns the mechanism of the synergistic action of STAT3 and NF-κB. STAT3 and NF-κB are involved in a wide range of inflammatory diseases and cancer development and, more importantly, their interaction is central to activation of the IL-6 Amp. More study on the synergistic activation would also open the way to new therapeutics.
Since the IL-6 Amp is deeply involved in uncontrolled inflammation, it is critical to elucidate the genetic and environmental factors that destabilize it. Defects in the negative feedback mechanism mediated by SOCS3 observed in F759 mice is one factor worth investigating. So too are the transcriptional factors and microRNAs that cause STAT3 and NF-κB to indirectly interact.
To realize a healthy aging society, it is crucial to prevent and cure age-related diseases. The list of diseases is long and includes autoimmune diseases, diabetes, cardiovascular diseases, dementia, pneumonia and cancer, all of which are related to uncontrolled inflammation. Uncontrolled inflammation is triggered by a variety of local initiators, including senescence, obesity, stressors through regional neural pathways, and infection through activation of the IL-6 Amp. More research on the effects of each initiator, either individually or synergistically with other initiators, on the inflammatory process and the IL-6 Amp would give deeper insights on inflammation, its prevention and cures.
Inflammatory diseases, autoimmune diseases and cancer are induced by complex interactions between non-immune cells and immune cells via the IL-6 Amp. Therefore, the expression and/or functions of IL-6 Amp-related molecules could be used to predict diseases initiated by local initiators. However, current knowledge is insufficient for predicting the end stage or detailed process of the disease. Furthermore, there are many pro-inflammatory molecules that determine the state of the IL-6 Amp as well as inflammation. The modes of interactions between these molecules too require more study. Improvements in detection technology and systems biology research for age- and inflammation-related diseases driven by artificial intelligence (AI) would be helpful (375).
Several inhibitors of IL-6 are now clinically used, but in order to develop small peptides or compounds with higher specificity and efficacy against diseases, high-resolution structural analysis of the ligand–receptor complex is needed. We can study the steady state of molecular interactions at the molecular level, but it is difficult to analyze in real time the dynamic changes of the molecular state of the receptor complexes and signaling molecules. Here, quantum life sciences in the field of inflammation will be helpful (376, 377).
Acknowledgements
I appreciate Dr P. Karagiannis (CiRA, Kyoto University, Kyoto, Japan) for critical reading the manuscript.
Conflicts of interest statement: the authors declared no conflicts of interest.
References
- 1. Hirano, T. 1998. Interleukin 6 and its receptor: ten years later. Int. Rev. Immunol. 16:249. [DOI] [PubMed] [Google Scholar]
- 2. Balkwill, F. and Mantovani, A. 2001. Inflammation and cancer: back to Virchow? Lancet 357:539. [DOI] [PubMed] [Google Scholar]
- 3. Ishihara, K. and Hirano, T. 2002. IL-6 in autoimmune disease and chronic inflammatory proliferative disease. Cytokine Growth Factor Rev. 13:357. [DOI] [PubMed] [Google Scholar]
- 4. Coussens, L. M. and Werb, Z. 2002. Inflammation and cancer. Nature 420:860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Campisi, J. 2005. Senescent cells, tumor suppression, and organismal aging: good citizens, bad neighbors. Cell 120:513. [DOI] [PubMed] [Google Scholar]
- 6. Mantovani, A., Allavena, P., Sica, A. and Balkwill, F. 2008. Cancer-related inflammation. Nature 454:436. [DOI] [PubMed] [Google Scholar]
- 7. Kuilman, T., Michaloglou, C., Vredeveld, L. C.et al. 2008. Oncogene-induced senescence relayed by an interleukin-dependent inflammatory network. Cell 133:1019. [DOI] [PubMed] [Google Scholar]
- 8. Acosta, J. C., O’Loghlen, A., Banito, A.et al. 2008. Chemokine signaling via the CXCR2 receptor reinforces senescence. Cell 133:1006. [DOI] [PubMed] [Google Scholar]
- 9. Grivennikov, S. I., Greten, F. R. and Karin, M. 2010. Immunity, inflammation, and cancer. Cell 140:883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Murakami, M., Harada, M., Kamimura, D.et al. 2013. Disease-association analysis of an inflammation-related feedback loop. Cell Rep. 3:946. [DOI] [PubMed] [Google Scholar]
- 11. Atsumi, T., Singh, R., Sabharwal, L.et al. 2014. Inflammation amplifier, a new paradigm in cancer biology. Cancer Res. 74:8. [DOI] [PubMed] [Google Scholar]
- 12. Mehta, P., McAuley, D. F., Brown, M., Sanchez, E., Tattersall, R. S. and Manson, J. J.; HLH Across Speciality Collaboration, UK . 2020. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 395:1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mahmudpour, M., Roozbeh, J., Keshavarz, M., Farrokhi, S. and Nabipour, I. 2020. COVID-19 cytokine storm: the anger of inflammation. Cytokine 133:155151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hu, B., Huang, S., and Yin, L. 2021. The cytokine storm and COVID-19. J. Med. Virol. 93:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hirano, T. and Murakami, M. 2020. COVID-19: a new virus, but a familiar receptor and cytokine release syndrome. Immunity 52:731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. García, L. F. 2020. Immune response, inflammation, and the clinical spectrum of COVID-19. Front. Immunol. 11:1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vabret, N., Britton, G. J., Gruber, C.et al. ; Sinai Immunology Review Project. 2020. Immunology of COVID-19: current state of the science. Immunity 52:910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grivennikov, S., Karin, E., Terzic, J.et al. 2009. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell 15:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yu, H., Pardoll, D. and Jove, R. 2009. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat. Rev. Cancer 9:798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bollrath, J., Phesse, T. J., von Burstin, V. A.et al. 2009. gp130-mediated Stat3 activation in enterocytes regulates cell survival and cell-cycle progression during colitis-associated tumorigenesis. Cancer Cell 15:91. [DOI] [PubMed] [Google Scholar]
- 21. Hunter, C. A. and Jones, S. A. 2015. IL-6 as a keystone cytokine in health and disease. Nat. Immunol. 16:448. [DOI] [PubMed] [Google Scholar]
- 22. Masjedi, A., Hashemi, V., Hojjat-Farsangi, M.et al. 2018. The significant role of interleukin-6 and its signaling pathway in the immunopathogenesis and treatment of breast cancer. Biomed. Pharmacother. 108:1415. [DOI] [PubMed] [Google Scholar]
- 23. Gyamfi, J., Lee, Y. H., Eom, M. and Choi, J. 2018. Interleukin-6/STAT3 signalling regulates adipocyte induced epithelial-mesenchymal transition in breast cancer cells. Sci. Rep. 8:8859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jones, S. A. and Jenkins, B. J. 2018. Recent insights into targeting the IL-6 cytokine family in inflammatory diseases and cancer. Nat. Rev. Immunol. 18:773. [DOI] [PubMed] [Google Scholar]
- 25. Rebe, C. and Ghiringhelli, F. 2019. STAT3, a master regulator of anti-tumor immune response. Cancer 11:1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Johnson, D. E., O’Keefe, R. A. and Grandis, J. R. 2018. Targeting the IL-6/JAK/STAT3 signalling axis in cancer. Nat. Rev. Clin. Oncol. 15:234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hirano, T., Yasukawa, K., Harada, H.et al. 1986. Complementary DNA for a novel human interleukin (BSF-2) that induces B lymphocytes to produce immunoglobulin. Nature 324:73. [DOI] [PubMed] [Google Scholar]
- 28. Van Snick, J. 1990. Interleukin-6: an overview. Annu. Rev. Immunol. 8:253. [DOI] [PubMed] [Google Scholar]
- 29. Hirano, T. and Kishimoto, T. 1990. Interleukin-6. In Sporn, M. B. and Roberts, A. B., eds., Peptide Growth Factors and Their Receptors I, p. 633. Springer, Berlin, Germany. [Google Scholar]
- 30. Heinrich, P. C., Behrmann, I., Haan, S., Hermanns, H. M., Müller-Newen, G. and Schaper, F. 2003. Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochem. J. 374(Pt 1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kamimura, D., Ishihara, K. and Hirano, T. 2003. IL-6 signal transduction and its physiological roles: the signal orchestration model. Rev. Physiol. Biochem. Pharmacol. 149:1. [DOI] [PubMed] [Google Scholar]
- 32. Hasegawa, H., Mizoguchi, I., Chiba, Y., Ohashi, M., Xu, M. and Yoshimoto, T. 2016. Expanding diversity in molecular structures and functions of the IL-6/IL-12 heterodimeric cytokine family. Front. Immunol. 7:479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Murakami, M., Kamimura, D. and Hirano, T. 2019. Pleiotropy and specificity: insights from the interleukin 6 family of cytokines. Immunity 50:812. [DOI] [PubMed] [Google Scholar]
- 34. Zilberstein, A., Ruggieri, R., Korn, J. H. and Revel, M. 1986. Structure and expression of cDNA and genes for human interferon-beta-2, a distinct species inducible by growth-stimulatory cytokines. EMBO J. 5:2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Haegeman, G., Content, J., Volckaert, G., Derynck, R., Tavernier, J. and Fiers, W. 1986. Structural analysis of the sequence coding for an inducible 26-kDa protein in human fibroblasts. Eur. J. Biochem. 159:625. [DOI] [PubMed] [Google Scholar]
- 36. Van Damme, J., Cayphas, S., Van Snick, J.et al. 1987. Purification and characterization of human fibroblast-derived hybridoma growth factor identical to T-cell-derived B-cell stimulatory factor-2 (interleukin-6). Eur. J. Biochem. 168:543. [DOI] [PubMed] [Google Scholar]
- 37. Kawano, M., Hirano, T., Matsuda, T.et al. 1988. Autocrine generation and requirement of BSF-2/IL-6 for human multiple myelomas. Nature 332:83. [DOI] [PubMed] [Google Scholar]
- 38. Van Snick, J., Cayphas, S., Szikora, J. P.et al. 1988. cDNA cloning of murine interleukin-HP1: homology with human interleukin 6. Eur. J. Immunol. 18:193. [DOI] [PubMed] [Google Scholar]
- 39. Andus, T., Geiger, T., Hirano, T.et al. 1987. Recombinant human B cell stimulatory factor 2 (BSF-2/IFN-beta 2) regulates beta-fibrinogen and albumin mRNA levels in Fao-9 cells. FEBS Lett. 221:18. [DOI] [PubMed] [Google Scholar]
- 40. Gauldie, J., Richards, C., Harnish, D., Lansdorp, P. and Baumann, H. 1987. Interferon beta 2/B-cell stimulatory factor type 2 shares identity with monocyte-derived hepatocyte-stimulating factor and regulates the major acute phase protein response in liver cells. Proc. Natl Acad. Sci. USA 84:7251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hirano, T. 2010. Interleukin 6 in autoimmune and inflammatory diseases: a personal memoir. Proc. Jpn Acad. Ser. B. Phys. Biol. Sci. 86:717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hirano, T., Taga, T., Yasukawa, K.et al. 1987. Human B-cell differentiation factor defined by an anti-peptide antibody and its possible role in autoantibody production. Proc. Natl Acad. Sci. USA 84:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yoshizaki, K., Matsuda, T., Nishimoto, N.et al. 1989. Pathogenic significance of interleukin-6 (IL-6/BSF-2) in Castleman’s disease. Blood 74:1360. [PubMed] [Google Scholar]
- 44. Hirano, T., Matsuda, T., Turner, M.et al. 1988. Excessive production of interleukin 6/B cell stimulatory factor-2 in rheumatoid arthritis. Eur. J. Immunol. 18:1797. [DOI] [PubMed] [Google Scholar]
- 45. Houssiau, F. A., Devogelaer, J. P., Van Damme, J., de Deuxchaisnes, C. N. and Van Snick, J. 1988. Interleukin-6 in synovial fluid and serum of patients with rheumatoid arthritis and other inflammatory arthritides. Arthritis Rheum. 31:784. [DOI] [PubMed] [Google Scholar]
- 46. Hirano, T. 1992. Interleukin-6 and its relation to inflammation and disease. Clin. Immunol. Immunopathol. 62(1 Pt 2):S60. [DOI] [PubMed] [Google Scholar]
- 47. Boyden, S. 1964. Autoimmunity and inflammation. Nature 201:200. [DOI] [PubMed] [Google Scholar]
- 48. Wilkin, T. J. 1990. The primary lesion theory of autoimmunity: a speculative hypothesis. Autoimmunity 7:225. [DOI] [PubMed] [Google Scholar]
- 49. Matsumoto, I., Maccioni, M., Lee, D. M.et al. 2002. How antibodies to a ubiquitous cytoplasmic enzyme may provoke joint-specific autoimmune disease. Nat. Immunol. 3:360. [DOI] [PubMed] [Google Scholar]
- 50. Marrack, P., Kappler, J. and Kotzin, B. L. 2001. Autoimmune disease: why and where it occurs. Nat. Med. 7:899. [DOI] [PubMed] [Google Scholar]
- 51. Hirano, T. 2002. Revival of the autoantibody model in rheumatoid arthritis. Nat. Immunol. 3:342. [DOI] [PubMed] [Google Scholar]
- 52. Murakami, M., Okuyama, Y., Ogura, H.et al. 2011. Local microbleeding facilitates IL-6- and IL-17-dependent arthritis in the absence of tissue antigen recognition by activated T cells. J. Exp. Med. 208:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Leavy, O. 2011. Autoimmunity: joint damage without antigen. Nat. Rev. Immunol. 11:75. [DOI] [PubMed] [Google Scholar]
- 54. Arima, Y., Harada, M., Kamimura, D.et al. 2012. Regional neural activation defines a gateway for autoreactive T cells to cross the blood-brain barrier. Cell 148:447. [DOI] [PubMed] [Google Scholar]
- 55. Arima, Y., Kamimura, D., Atsumi, T.et al. 2015. A pain-mediated neural signal induces relapse in murine autoimmune encephalomyelitis, a multiple sclerosis model. Elife 4:e08733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Okano, S., Yasui, A., Kanno, S. I., Satoh, K., Igarashi, M. and Nakajima, O. 2019. Karyopherin alpha 2-expressing pancreatic duct glands and intra-islet ducts in aged diabetic C414A-mutant-CRY1 transgenic mice. J. Diabetes Res. 2019:7234549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Thompson, P. J., Shah, A., Ntranos, V., Van Gool, F., Atkinson, M. and Bhushan, A. 2019. Targeted elimination of senescent beta cells prevents type 1 diabetes. Cell Metab. 29:1045.e10. [DOI] [PubMed] [Google Scholar]
- 58. Hirano, T. 1991. Interleukin 6 (IL-6) and its receptor: their role in plasma cell neoplasias. Int. J. Cell Cloning 9:166. [DOI] [PubMed] [Google Scholar]
- 59. Tricot, G. 2000. New insights into role of microenvironment in multiple myeloma. Lancet 355:248. [DOI] [PubMed] [Google Scholar]
- 60. Chen, D. S. and Mellman, I. 2013. Oncology meets immunology: the cancer-immunity cycle. Immunity 39:1. [DOI] [PubMed] [Google Scholar]
- 61. Bromberg, J. and Darnell, J. E.Jr. 2000. The role of STATs in transcriptional control and their impact on cellular function. Oncogene 19:2468. [DOI] [PubMed] [Google Scholar]
- 62. Hirano, T., Ishihara, K. and Hibi, M. 2000. Roles of STAT3 in mediating the cell growth, differentiation and survival signals relayed through the IL-6 family of cytokine receptors. Oncogene 19:2548. [DOI] [PubMed] [Google Scholar]
- 63. Atsumi, T., Ishihara, K., Kamimura, D.et al. 2002. A point mutation of Tyr-759 in interleukin 6 family cytokine receptor subunit gp130 causes autoimmune arthritis. J. Exp. Med. 196:979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Jenkins, B. J., Grail, D., Nheu, T.et al. 2005. Hyperactivation of Stat3 in gp130 mutant mice promotes gastric hyperproliferation and desensitizes TGF-beta signaling. Nat. Med. 11:845. [DOI] [PubMed] [Google Scholar]
- 65. Jenkins, B. J., Roberts, A. W., Greenhill, C. J.et al. 2007. Pathologic consequences of STAT3 hyperactivation by IL-6 and IL-11 during hematopoiesis and lymphopoiesis. Blood 109:2380. [DOI] [PubMed] [Google Scholar]
- 66. Ogura, H., Murakami, M., Okuyama, Y.et al. 2008. Interleukin-17 promotes autoimmunity by triggering a positive-feedback loop via interleukin-6 induction. Immunity 29:628. [DOI] [PubMed] [Google Scholar]
- 67. Grivennikov, S. I. and Karin, M. 2010. Dangerous liaisons: STAT3 and NF-kappaB collaboration and crosstalk in cancer. Cytokine Growth Factor Rev. 21:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Yoon, S., Woo, S. U., Kang, J. H.et al. 2012. NF-κB and STAT3 cooperatively induce IL6 in starved cancer cells. Oncogene 31:3467. [DOI] [PubMed] [Google Scholar]
- 69. Bataille, R., Barlogie, B., Lu, Z. Y.et al. 1995. Biologic effects of anti-interleukin-6 murine monoclonal antibody in advanced multiple myeloma. Blood 86:685. [PubMed] [Google Scholar]
- 70. Lu, Z. Y., Brailly, H., Wijdenes, J., Bataille, R., Rossi, J. F. and Klein, B. 1995. Measurement of whole body interleukin-6 (IL-6) production: prediction of the efficacy of anti-IL-6 treatments. Blood 86:3123. [PubMed] [Google Scholar]
- 71. Choy, E. H., Isenberg, D. A., Garrood, T.et al. 2002. Therapeutic benefit of blocking interleukin-6 activity with an anti-interleukin-6 receptor monoclonal antibody in rheumatoid arthritis: a randomized, double-blind, placebo-controlled, dose-escalation trial. Arthritis Rheum. 46:3143. [DOI] [PubMed] [Google Scholar]
- 72. Nishimoto, N., Kanakura, Y., Aozasa, K.et al. 2005. Humanized anti-interleukin-6 receptor antibody treatment of multicentric Castleman disease. Blood 106:2627. [DOI] [PubMed] [Google Scholar]
- 73. Maini, R., Taylor, P., Szechinski, J.et al. 2006. Double-blind randomized controlled clinical trial of the interleukin-6 receptor antagonist, tocilizumab, in European patients with rheumatoid arthritis who had an incomplete response to methotrexate. Arthritis Rheum. 54:2817. [DOI] [PubMed] [Google Scholar]
- 74. Genovese, M. C., McKay, J. D., Nasonov, E. L.et al. 2008. Interleukin-6 receptor inhibition with tocilizumab reduces disease activity in rheumatoid arthritis with inadequate response to disease-modifying antirheumatic drugs: the tocilizumab in combination with traditional disease-modifying antirheumatic drug therapy study. Arthritis Rheum. 58:2968. [DOI] [PubMed] [Google Scholar]
- 75. Jones, G., Sebba, A., Gu, J.et al. 2010. Comparison of tocilizumab monotherapy versus methotrexate monotherapy in patients with moderate to severe rheumatoid arthritis: the AMBITION study. Ann. Rheum. Dis. 69:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Taher, M. Y., Davies, D. M. and Maher, J. 2018. The role of the interleukin (IL)-6/IL-6 receptor axis in cancer. Biochem. Soc. Trans. 46:1449. [DOI] [PubMed] [Google Scholar]
- 77. Yasukawa, K., Hirano, T., Watanabe, Y.et al. 1987. Structure and expression of human B cell stimulatory factor-2 (BSF-2/IL-6) gene. EMBO J. 6:2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Libermann, T. A. and Baltimore, D. 1990. Activation of interleukin-6 gene expression through the NF-kappa B transcription factor. Mol. Cell. Biol. 10:2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Akira, S., Isshiki, H., Sugita, T.et al. 1990. A nuclear factor for IL-6 expression (NF-IL6) is a member of a C/EBP family. EMBO J. 9:1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Hirano, T., Akira, S., Taga, T. and Kishimoto, T. 1990. Biological and clinical aspects of interleukin 6. Immunol. Today 11:443. [DOI] [PubMed] [Google Scholar]
- 81. Muraoka, O., Kaisho, T., Tanabe, M. and Hirano, T. 1993. Transcriptional activation of the interleukin-6 gene by HTLV-1 p40tax through an NF-kappa B-like binding site. Immunol. Lett. 37:159. [DOI] [PubMed] [Google Scholar]
- 82. Yoon, S., Woo, S. U., Kang, J. H.et al. 2010. STAT3 transcriptional factor activated by reactive oxygen species induces IL6 in starvation-induced autophagy of cancer cells. Autophagy 6:1125. [DOI] [PubMed] [Google Scholar]
- 83. Chang, Q., Bournazou, E., Sansone, P.et al. 2013. The IL-6/JAK/Stat3 feed-forward loop drives tumorigenesis and metastasis. Neoplasia 15:848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Wolf, J., Rose-John, S. and Garbers, C. 2014. Interleukin-6 and its receptors: a highly regulated and dynamic system. Cytokine 70:11. [DOI] [PubMed] [Google Scholar]
- 85. Nishida, K., Hasegawa, A., Yamasaki, S.et al. 2019. Mast cells play role in wound healing through the ZnT2/GPR39/IL-6 axis. Sci. Rep. 9:10842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Hu, L., Yu, Y., Huang, H.et al. 2016. Epigenetic regulation of interleukin 6 by histone acetylation in macrophages and its role in paraquat-induced pulmonary fibrosis. Front. Immunol. 7:696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Maeda, K. and Akira, S. 2017. Regulation of mRNA stability by CCCH-type zinc-finger proteins in immune cells. Int. Immunol. 29:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Masuda, K., Ripley, B., Nishimura, R.et al. 2013. Arid5a controls IL-6 mRNA stability, which contributes to elevation of IL-6 level in vivo. Proc. Natl Acad. Sci. USA 110:9409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Iliopoulos, D., Hirsch, H. A. and Struhl, K. 2009. An epigenetic switch involving NF-kappaB, Lin28, Let-7 MicroRNA, and IL6 links inflammation to cell transformation. Cell 139:693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Iliopoulos, D., Jaeger, S. A., Hirsch, H. A., Bulyk, M. L. and Struhl, K. 2010. STAT3 activation of miR-21 and miR-181b-1 via PTEN and CYLD are part of the epigenetic switch linking inflammation to cancer. Mol. Cell 39:493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Yang, X., Liang, L., Zhang, X. F.et al. 2013. MicroRNA-26a suppresses tumor growth and metastasis of human hepatocellular carcinoma by targeting interleukin-6-Stat3 pathway. Hepatology 58:158. [DOI] [PubMed] [Google Scholar]
- 92. Hirota, H., Yoshida, K., Kishimoto, T. and Taga, T. 1995. Continuous activation of gp130, a signal-transducing receptor component for interleukin 6-related cytokines, causes myocardial hypertrophy in mice. Proc. Natl Acad. Sci. USA 92:4862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Gearing, D. P. and Cosman, D. 1991. Homology of the p40 subunit of natural killer cell stimulatory factor (NKSF) with the extracellular domain of the interleukin-6 receptor. Cell 66:9. [DOI] [PubMed] [Google Scholar]
- 94. Chua, A. O., Chizzonite, R., Desai, B. B.et al. 1994. Expression cloning of a human IL-12 receptor component. A new member of the cytokine receptor superfamily with strong homology to gp130. J. Immunol. 153:128. [PubMed] [Google Scholar]
- 95. Davis, S., Aldrich, T. H., Ip, N. Y.et al. 1993. Released form of CNTF receptor alpha component as a soluble mediator of CNTF responses. Science 259:1736. [DOI] [PubMed] [Google Scholar]
- 96. Rose-John, S. 2017. The soluble interleukin 6 receptor: advanced therapeutic options in inflammation. Clin. Pharmacol. Ther. 102:591. [DOI] [PubMed] [Google Scholar]
- 97. Romano, M., Sironi, M., Toniatti, C.et al. 1997. Role of IL-6 and its soluble receptor in induction of chemokines and leukocyte recruitment. Immunity 6:315. [DOI] [PubMed] [Google Scholar]
- 98. Hurst, S. M., Wilkinson, T. S., McLoughlin, R. M.et al. 2001. Il-6 and its soluble receptor orchestrate a temporal switch in the pattern of leukocyte recruitment seen during acute inflammation. Immunity 14:705. [DOI] [PubMed] [Google Scholar]
- 99. Sawa, S., Kamimura, D., Jin, G. H.et al. 2006. Autoimmune arthritis associated with mutated interleukin (IL)-6 receptor gp130 is driven by STAT3/IL-7-dependent homeostatic proliferation of CD4+ T cells. J. Exp. Med. 203:1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Heink, S., Yogev, N., Garbers, C.et al. 2017. Trans-presentation of IL-6 by dendritic cells is required for the priming of pathogenic TH17 cells. Nat. Immunol. 18:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Jostock, T., Müllberg, J., Ozbek, S.et al. 2001. Soluble gp130 is the natural inhibitor of soluble interleukin-6 receptor transsignaling responses. Eur. J. Biochem. 268:160. [DOI] [PubMed] [Google Scholar]
- 102. Zhong, Z., Wen, Z. and Darnell, J. E.Jr. 1994. Stat3: a STAT family member activated by tyrosine phosphorylation in response to epidermal growth factor and interleukin-6. Science 264:95. [DOI] [PubMed] [Google Scholar]
- 103. Stark, G. R. and Darnell, J. E.Jr. 2012. The JAK-STAT pathway at twenty. Immunity 36:503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Fukada, T., Hibi, M., Yamanaka, Y.et al. 1996. Two signals are necessary for cell proliferation induced by a cytokine receptor gp130: involvement of STAT3 in anti-apoptosis. Immunity 5:449. [DOI] [PubMed] [Google Scholar]
- 105. Yamanaka, Y., Nakajima, K., Fukada, T., Hibi, M. and Hirano, T. 1996. Differentiation and growth arrest signals are generated through the cytoplasmic region of gp130 that is essential for Stat3 activation. EMBO J. 15:1557. [PMC free article] [PubMed] [Google Scholar]
- 106. Takahashi-Tezuka, M., Yoshida, Y., Fukada, T.et al. 1998. Gab1 acts as an adapter molecule linking the cytokine receptor gp130 to ERK mitogen-activated protein kinase. Mol. Cell. Biol. 18:4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Nishida, K., Yoshida, Y., Itoh, M.et al. 1999. Gab-family adapter proteins act downstream of cytokine and growth factor receptors and T- and B-cell antigen receptors. Blood 93:1809. [PubMed] [Google Scholar]
- 108. Taniguchi, K., Wu, L. W., Grivennikov, S. I.et al. 2015. A gp130-Src-YAP module links inflammation to epithelial regeneration. Nature 519:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Sansone, P., Storci, G., Tavolari, S.et al. 2007. IL-6 triggers malignant features in mammospheres from human ductal breast carcinoma and normal mammary gland. J. Clin. Invest. 117:3988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Fukada, T., Ohtani, T., Yoshida, Y.et al. 1998. STAT3 orchestrates contradictory signals in cytokine-induced G1 to S cell-cycle transition. EMBO J. 17:6670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Ernst, M., Inglese, M., Waring, P.et al. 2001. Defective gp130-mediated signal transducer and activator of transcription (STAT) signaling results in degenerative joint disease, gastrointestinal ulceration, and failure of uterine implantation. J. Exp. Med. 194:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Jenkins, B. J., Grail, D., Inglese, M.et al. 2004. Imbalanced gp130-dependent signaling in macrophages alters macrophage colony-stimulating factor responsiveness via regulation of c-fms expression. Mol. Cell. Biol. 24:1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Ohtani, T., Ishihara, K., Atsumi, T.et al. 2000. Dissection of signaling cascades through gp130 in vivo: reciprocal roles for STAT3- and SHP2-mediated signals in immune responses. Immunity 12:95. [DOI] [PubMed] [Google Scholar]
- 114. Kim, H., Hawley, T. S., Hawley, R. G. and Baumann, H. 1998. Protein tyrosine phosphatase 2 (SHP-2) moderates signaling by gp130 but is not required for the induction of acute-phase plasma protein genes in hepatic cells. Mol. Cell. Biol. 18:1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Schaper, F., Gendo, C., Eck, M.et al. 1998. Activation of the protein tyrosine phosphatase SHP2 via the interleukin-6 signal transducing receptor protein gp130 requires tyrosine kinase Jak1 and limits acute-phase protein expression. Biochem. J. 335 (Pt 3):557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Lehmann, U., Schmitz, J., Weissenbach, M.et al. 2003. SHP2 and SOCS3 contribute to Tyr-759-dependent attenuation of interleukin-6 signaling through gp130. J. Biol. Chem. 278:661. [DOI] [PubMed] [Google Scholar]
- 117. Fairlie, W. D., De Souza, D., Nicola, N. A. and Baca, M. 2003. Negative regulation of gp130 signalling mediated through tyrosine-757 is not dependent on the recruitment of SHP2. Biochem. J. 372(Pt 2):495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Kubo, M., Hanada, T. and Yoshimura, A. 2003. Suppressors of cytokine signaling and immunity. Nat. Immunol. 4:1169. [DOI] [PubMed] [Google Scholar]
- 119. Nicholson, S. E., De Souza, D., Fabri, L. J.et al. 2000. Suppressor of cytokine signaling-3 preferentially binds to the SHP-2-binding site on the shared cytokine receptor subunit gp130. Proc. Natl Acad. Sci. USA 97:6493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Schmitz, J., Weissenbach, M., Haan, S., Heinrich, P. C. and Schaper, F. 2000. SOCS3 exerts its inhibitory function on interleukin-6 signal transduction through the SHP2 recruitment site of gp130. J. Biol. Chem. 275:12848. [DOI] [PubMed] [Google Scholar]
- 121. Nagashima, H., Okuyama, Y., Asao, A.et al. 2014. The adaptor TRAF5 limits the differentiation of inflammatory CD4(+) T cells by antagonizing signaling via the receptor for IL-6. Nat. Immunol. 15:449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Lin, W. W., Yi, Z., Stunz, L. L., Maine, C. J., Sherman, L. A. and Bishop, G. A. 2015. The adaptor protein TRAF3 inhibits interleukin-6 receptor signaling in B cells to limit plasma cell development. Sci. Signal. 8:ra88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Navarro, A., Diaz, T., Martinez, A.et al. 2009. Regulation of JAK2 by miR-135a: prognostic impact in classic Hodgkin lymphoma. Blood 114:2945. [DOI] [PubMed] [Google Scholar]
- 124. Du, L., Subauste, M. C., DeSevo, C.et al. 2012. miR-337-3p and its targets STAT3 and RAP1A modulate taxane sensitivity in non-small cell lung cancers. PLoS ONE 7:e39167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Chung, C. D., Liao, J., Liu, B.et al. 1997. Specific inhibition of Stat3 signal transduction by PIAS3. Science 278:1803. [DOI] [PubMed] [Google Scholar]
- 126. Kiuchi, N., Nakajima, K., Ichiba, M.et al. 1999. STAT3 is required for the gp130-mediated full activation of the c-myc gene. J. Exp. Med. 189:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Shirogane, T., Fukada, T., Muller, J. M., Shima, D. T., Hibi, M. and Hirano, T. 1999. Synergistic roles for Pim-1 and c-Myc in STAT3-mediated cell cycle progression and antiapoptosis. Immunity 11:709. [DOI] [PubMed] [Google Scholar]
- 128. Block, K. M., Hanke, N. T., Maine, E. A. and Baker, A. F. 2012. IL-6 stimulates STAT3 and Pim-1 kinase in pancreatic cancer cell lines. Pancreas 41:773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Xu, J., Xiong, G., Cao, Z.et al. 2016. PIM-1 contributes to the malignancy of pancreatic cancer and displays diagnostic and prognostic value. J. Exp. Clin. Cancer Res. 35:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Gao, X., Liu, X., Lu, Y.et al. 2019. PIM1 is responsible for IL-6-induced breast cancer cell EMT and stemness via c-myc activation. Breast Cancer 26:663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Sullivan, N. J., Sasser, A. K., Axel, A. E.et al. 2009. Interleukin-6 induces an epithelial-mesenchymal transition phenotype in human breast cancer cells. Oncogene 28:2940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Yadav, A., Kumar, B., Datta, J., Teknos, T. N. and Kumar, P. 2011. IL-6 promotes head and neck tumor metastasis by inducing epithelial-mesenchymal transition via the JAK-STAT3-SNAIL signaling pathway. Mol. Cancer Res. 9:1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Barbieri, I., Pensa, S., Pannellini, T.et al. 2010. Constitutively active Stat3 enhances neu-mediated migration and metastasis in mammary tumors via upregulation of Cten. Cancer Res. 70:2558. [DOI] [PubMed] [Google Scholar]
- 134. Tang, Y., Kitisin, K., Jogunoori, W.et al. 2008. Progenitor/stem cells give rise to liver cancer due to aberrant TGF-beta and IL-6 signaling. Proc. Natl Acad. Sci. USA 105:2445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Islam, M., Sharma, S. and Teknos, T. N. 2014. RhoC regulates cancer stem cells in head and neck squamous cell carcinoma by overexpressing IL-6 and phosphorylation of STAT3. PLoS ONE 9:e88527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Niu, G., Wright, K. L., Huang, M.et al. 2002. Constitutive Stat3 activity up-regulates VEGF expression and tumor angiogenesis. Oncogene 21:2000. [DOI] [PubMed] [Google Scholar]
- 137. Wei, L. H., Kuo, M. L., Chen, C. A.et al. 2003. Interleukin-6 promotes cervical tumor growth by VEGF-dependent angiogenesis via a STAT3 pathway. Oncogene 22:1517. [DOI] [PubMed] [Google Scholar]
- 138. Xu, Q., Briggs, J., Park, S.et al. 2005. Targeting Stat3 blocks both HIF-1 and VEGF expression induced by multiple oncogenic growth signaling pathways. Oncogene 24:5552. [DOI] [PubMed] [Google Scholar]
- 139. Adachi, Y., Aoki, C., Yoshio-Hoshino, N., Takayama, K., Curiel, D. T. and Nishimoto, N. 2006. Interleukin-6 induces both cell growth and VEGF production in malignant mesotheliomas. Int. J. Cancer 119:1303. [DOI] [PubMed] [Google Scholar]
- 140. Yeh, H. H., Lai, W. W., Chen, H. H., Liu, H. S. and Su, W. C. 2006. Autocrine IL-6-induced Stat3 activation contributes to the pathogenesis of lung adenocarcinoma and malignant pleural effusion. Oncogene 25:4300. [DOI] [PubMed] [Google Scholar]
- 141. Löffler, D., Brocke-Heidrich, K., Pfeifer, G.et al. 2007. Interleukin-6 dependent survival of multiple myeloma cells involves the Stat3-mediated induction of microRNA-21 through a highly conserved enhancer. Blood 110:1330. [DOI] [PubMed] [Google Scholar]
- 142. Yu, L., Wu, D., Gao, H.et al. 2018. Clinical utility of a STAT3-regulated miRNA-200 family signature with prognostic potential in early gastric cancer. Clin. Cancer Res. 24:1459. [DOI] [PubMed] [Google Scholar]
- 143. Muraguchi, A., Hirano, T., Tang, B.et al. 1988. The essential role of B cell stimulatory factor 2 (BSF-2/IL-6) for the terminal differentiation of B cells. J. Exp. Med. 167:332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Jego, G., Palucka, A. K., Blanck, J. P., Chalouni, C., Pascual, V. and Banchereau, J. 2003. Plasmacytoid dendritic cells induce plasma cell differentiation through type I interferon and interleukin 6. Immunity 19:225. [DOI] [PubMed] [Google Scholar]
- 145. Cassese, G., Arce, S., Hauser, A. E.et al. 2003. Plasma cell survival is mediated by synergistic effects of cytokines and adhesion-dependent signals. J. Immunol. 171:1684. [DOI] [PubMed] [Google Scholar]
- 146. Vinuesa, C. G., Linterman, M. A., Yu, D. and MacLennan, I. C. 2016. Follicular helper T cells. Annu. Rev. Immunol. 34:335. [DOI] [PubMed] [Google Scholar]
- 147. Suematsu, S., Matsuda, T., Aozasa, K.et al. 1989. IgG1 plasmacytosis in interleukin 6 transgenic mice. Proc. Natl Acad. Sci. USA 86:7547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Kopf, M., Baumann, H., Freer, G.et al. 1994. Impaired immune and acute-phase responses in interleukin-6-deficient mice. Nature 368:339. [DOI] [PubMed] [Google Scholar]
- 149. Ramsay, A. J., Husband, A. J., Ramshaw, I. A.et al. 1994. The role of interleukin-6 in mucosal IgA antibody responses in vivo. Science 264:561. [DOI] [PubMed] [Google Scholar]
- 150. Fornek, J. L., Tygrett, L. T., Waldschmidt, T. J., Poli, V., Rickert, R. C. and Kansas, G. S. 2006. Critical role for Stat3 in T-dependent terminal differentiation of IgG B cells. Blood 107:1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Diehl, S. A., Schmidlin, H., Nagasawa, M.et al. 2008. STAT3-mediated up-regulation of BLIMP1 is coordinated with BCL6 down-regulation to control human plasma cell differentiation. J. Immunol. 180:4805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Leung, D. Y., Ambrosino, D. M., Arbeit, R. D., Newton, J. L. and Geha, R. S. 1988. Impaired antibody responses in the hyperimmunoglobulin E syndrome. J. Allergy Clin. Immunol. 81:1082. [DOI] [PubMed] [Google Scholar]
- 153. Meyer-Bahlburg, A., Renner, E. D., Rylaarsdam, S.et al. 2012. Heterozygous signal transducer and activator of transcription 3 mutations in hyper-IgE syndrome result in altered B-cell maturation. J. Allergy Clin. Immunol. 129:559, 562.e1. [DOI] [PubMed] [Google Scholar]
- 154. Rodríguez-Bayona, B., Ramos-Amaya, A., López-Blanco, R., Campos-Caro, A. and Brieva, J. A. 2013. STAT-3 activation by differential cytokines is critical for human in vivo-generated plasma cell survival and Ig secretion. J. Immunol. 191:4996. [DOI] [PubMed] [Google Scholar]
- 155. Rincón, M., Anguita, J., Nakamura, T., Fikrig, E. and Flavell, R. A. 1997. Interleukin (IL)-6 directs the differentiation of IL-4-producing CD4+ T cells. J. Exp. Med. 185:461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Tsukamoto, H., Fujieda, K., Hirayama, M.et al. 2017. Soluble IL6R expressed by myeloid cells reduces tumor-specific Th1 differentiation and drives tumor progression. Cancer Res. 77:2279. [DOI] [PubMed] [Google Scholar]
- 157. Fielding, C. A., Jones, G. W., McLoughlin, R. M.et al. 2014. Interleukin-6 signaling drives fibrosis in unresolved inflammation. Immunity 40:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Korn, T., Bettelli, E., Oukka, M. and Kuchroo, V. K. 2009. IL-17 and Th17 cells Annu. Rev. Immunol. 27:485. [DOI] [PubMed] [Google Scholar]
- 159. Su, X., Ye, J., Hsueh, E. C., Zhang, Y., Hoft, D. F. and Peng, G. 2010. Tumor microenvironments direct the recruitment and expansion of human Th17 cells. J. Immunol. 184:1630. [DOI] [PubMed] [Google Scholar]
- 160. Young, M. R. 2016. Th17 cells in protection from tumor or promotion of tumor progression. J. Clin. Cell. Immunol. 7:431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Sakaguchi, S. 2004. Naturally arising CD4+ regulatory T cells for immunologic self-tolerance and negative control of immune responses. Annu. Rev. Immunol. 22:531. [DOI] [PubMed] [Google Scholar]
- 162. Tanaka, A. and Sakaguchi, S. 2019. Targeting Treg cells in cancer immunotherapy. Eur. J. Immunol. 49:1140. [DOI] [PubMed] [Google Scholar]
- 163. Knochelmann, H. M., Dwyer, C. J., Bailey, S. R.et al. 2018. When worlds collide: Th17 and Treg cells in cancer and autoimmunity. Cell. Mol. Immunol. 15:458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Veldhoen, M., Hocking, R. J., Atkins, C. J., Locksley, R. M. and Stockinger, B. 2006. TGFbeta in the context of an inflammatory cytokine milieu supports de novo differentiation of IL-17-producing T cells. Immunity 24:179. [DOI] [PubMed] [Google Scholar]
- 165. Ivanov, I. I., McKenzie, B. S., Zhou, L.et al. 2006. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell 126:1121. [DOI] [PubMed] [Google Scholar]
- 166. Bettelli, E., Carrier, Y., Gao, W.et al. 2006. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature 441:235. [DOI] [PubMed] [Google Scholar]
- 167. Korn, T., Mitsdoerffer, M., Croxford, A. L.et al. 2008. IL-6 controls Th17 immunity in vivo by inhibiting the conversion of conventional T cells into Foxp3+ regulatory T cells. Proc. Natl Acad. Sci. USA 105:18460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Fujimoto, M., Nakano, M., Terabe, F.et al. 2011. The influence of excessive IL-6 production in vivo on the development and function of Foxp3+ regulatory T cells. J. Immunol. 186:32. [DOI] [PubMed] [Google Scholar]
- 169. Acosta-Rodriguez, E. V., Napolitani, G., Lanzavecchia, A. and Sallusto, F. 2007. Interleukins 1beta and 6 but not transforming growth factor-beta are essential for the differentiation of interleukin 17-producing human T helper cells. Nat. Immunol. 8:942. [DOI] [PubMed] [Google Scholar]
- 170. Wilson, N. J., Boniface, K., Chan, J. R.et al. 2007. Development, cytokine profile and function of human interleukin 17-producing helper T cells. Nat. Immunol. 8:950. [DOI] [PubMed] [Google Scholar]
- 171. Ghoreschi, K., Laurence, A., Yang, X. P.et al. 2010. Generation of pathogenic T(H)17 cells in the absence of TGF-β signalling. Nature 467:967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. McGeachy, M. J., Chen, Y., Tato, C. M.et al. 2009. The interleukin 23 receptor is essential for the terminal differentiation of interleukin 17-producing effector T helper cells in vivo. Nat. Immunol. 10:314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Ichiyama, K., Gonzalez-Martin, A., Kim, B. S.et al. 2016. The MicroRNA-183-96-182 cluster promotes T helper 17 cell pathogenicity by negatively regulating transcription factor Foxo1 expression. Immunity 44:1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Nishihara, M., Ogura, H., Ueda, N.et al. 2007. IL-6-gp130-STAT3 in T cells directs the development of IL-17+ Th with a minimum effect on that of Treg in the steady state. Int. Immunol. 19:695. [DOI] [PubMed] [Google Scholar]
- 175. Harris, T. J., Grosso, J. F., Yen, H. R.et al. 2007. Cutting edge: an in vivo requirement for STAT3 signaling in TH17 development and TH17-dependent autoimmunity. J. Immunol. 179:4313. [DOI] [PubMed] [Google Scholar]
- 176. Stumhofer, J. S., Laurence, A., Wilson, E. H.et al. 2006. Interleukin 27 negatively regulates the development of interleukin 17-producing T helper cells during chronic inflammation of the central nervous system. Nat. Immunol. 7:937. [DOI] [PubMed] [Google Scholar]
- 177. Neufert, C., Becker, C., Wirtz, S.et al. 2007. IL-27 controls the development of inducible regulatory T cells and Th17 cells via differential effects on STAT1. Eur. J. Immunol. 37:1809. [DOI] [PubMed] [Google Scholar]
- 178. Peters, A., Fowler, K. D., Chalmin, F., Merkler, D., Kuchroo, V. K. and Pot, C. 2015. IL-27 induces Th17 differentiation in the absence of STAT1 signaling. J. Immunol. 195:4144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Milner, J. D., Brenchley, J. M., Laurence, A.et al. 2008. Impaired T(H)17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature 452:773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Liu, L., Okada, S., Kong, X. F.et al. 2011. Gain-of-function human STAT1 mutations impair IL-17 immunity and underlie chronic mucocutaneous candidiasis. J. Exp. Med. 208:1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Zhang, Y., Ma, C. A., Lawrence, M. G.et al. 2017. PD-L1 up-regulation restrains Th17 cell differentiation in STAT3 loss- and STAT1 gain-of-function patients. J. Exp. Med. 214:2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Hirahara, K., Ghoreschi, K., Yang, X. P.et al. 2012. Interleukin-27 priming of T cells controls IL-17 production in trans via induction of the ligand PD-L1. Immunity 36:1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Berger, H., Végran, F., Chikh, M.et al. 2013. SOCS3 transactivation by PPARγ prevents IL-17-driven cancer growth. Cancer Res. 73:3578. [DOI] [PubMed] [Google Scholar]
- 184. Fang, S., Liu, B., Sun, Q., Zhao, J., Qi, H. and Li, Q. 2014. Platelet factor 4 inhibits IL-17/Stat3 pathway via upregulation of SOCS3 expression in melanoma. Inflammation 37:1744. [DOI] [PubMed] [Google Scholar]
- 185. Fukada, T., Yamasaki, S., Nishida, K., Murakami, M. and Hirano, T. 2011. Zinc homeostasis and signaling in health and diseases: zinc signaling. J. Biol. Inorg. Chem. 16:1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Kitabayashi, C., Fukada, T., Kanamoto, M.et al. 2010. Zinc suppresses Th17 development via inhibition of STAT3 activation. Int. Immunol. 22:375. [DOI] [PubMed] [Google Scholar]
- 187. Laurence, A., Tato, C. M., Davidson, T. S.et al. 2007. Interleukin-2 signaling via STAT5 constrains T helper 17 cell generation. Immunity 26:371. [DOI] [PubMed] [Google Scholar]
- 188. Ichiyama, K., Yoshida, H., Wakabayashi, Y.et al. 2008. Foxp3 inhibits RORgammat-mediated IL-17A mRNA transcription through direct interaction with RORgammat. J. Biol. Chem. 283:17003. [DOI] [PubMed] [Google Scholar]
- 189. Yang, X. P., Ghoreschi, K., Steward-Tharp, S. M.et al. 2011. Opposing regulation of the locus encoding IL-17 through direct, reciprocal actions of STAT3 and STAT5. Nat. Immunol. 12:247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Xu, L., Kitani, A., Fuss, I. and Strober, W. 2007. Cutting edge: regulatory T cells induce CD4+CD25-Foxp3- T cells or are self-induced to become Th17 cells in the absence of exogenous TGF-beta. J. Immunol. 178:6725. [DOI] [PubMed] [Google Scholar]
- 191. Yang, X. O., Nurieva, R., Martinez, G. J.et al. 2008. Molecular antagonism and plasticity of regulatory and inflammatory T cell programs. Immunity 29:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Komatsu, N., Okamoto, K., Sawa, S.et al. 2014. Pathogenic conversion of Foxp3+ T cells into TH17 cells in autoimmune arthritis. Nat. Med. 20:62. [DOI] [PubMed] [Google Scholar]
- 193. Li, D., Kong, C., Tsun, A.et al. 2015. MiR-125a-5p decreases the sensitivity of Treg cells toward IL-6-mediated conversion by inhibiting IL-6R and STAT3 expression. Sci. Rep. 5:14615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Pasare, C. and Medzhitov, R. 2003. Toll pathway-dependent blockade of CD4+CD25+ T cell-mediated suppression by dendritic cells. Science 299:1033. [DOI] [PubMed] [Google Scholar]
- 195. Goodman, W. A., Levine, A. D., Massari, J. V., Sugiyama, H., McCormick, T. S. and Cooper, K. D. 2009. IL-6 signaling in psoriasis prevents immune suppression by regulatory T cells. J. Immunol. 183:3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Schneider, A., Long, S. A., Cerosaletti, K.et al. 2013. In active relapsing-remitting multiple sclerosis, effector T cell resistance to adaptive T(regs) involves IL-6-mediated signaling. Sci. Transl. Med. 5:170ra15. [DOI] [PubMed] [Google Scholar]
- 197. van der Vliet, H. J. and Nieuwenhuis, E. E. 2007. IPEX as a result of mutations in FOXP3. Clin. Dev. Immunol. 2007:89017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Suzuki, H., Kündig, T. M., Furlonger, C.et al. 1995. Deregulated T cell activation and autoimmunity in mice lacking interleukin-2 receptor beta. Science 268:1472. [DOI] [PubMed] [Google Scholar]
- 199. Klatzmann, D. and Abbas, A. K. 2015. The promise of low-dose interleukin-2 therapy for autoimmune and inflammatory diseases. Nat. Rev. Immunol. 15:283. [DOI] [PubMed] [Google Scholar]
- 200. Samson, M., Audia, S., Janikashvili, N.et al. 2012. Brief report: inhibition of interleukin-6 function corrects Th17/Treg cell imbalance in patients with rheumatoid arthritis. Arthritis Rheum. 64:2499. [DOI] [PubMed] [Google Scholar]
- 201. Steinman, R. M. 1991. The dendritic cell system and its role in immunogenicity. Annu. Rev. Immunol. 9:271. [DOI] [PubMed] [Google Scholar]
- 202. Laouar, Y., Welte, T., Fu, X. Y. and Flavell, R. A. 2003. STAT3 is required for Flt3L-dependent dendritic cell differentiation. Immunity 19:903. [DOI] [PubMed] [Google Scholar]
- 203. Hegde, S., Pahne, J. and Smola-Hess, S. 2004. Novel immunosuppressive properties of interleukin-6 in dendritic cells: inhibition of NF-kappaB binding activity and CCR7 expression. FASEB J. 18:1439. [DOI] [PubMed] [Google Scholar]
- 204. Park, S. J., Nakagawa, T., Kitamura, H.et al. 2004. IL-6 regulates in vivo dendritic cell differentiation through STAT3 activation. J. Immunol. 173:3844. [DOI] [PubMed] [Google Scholar]
- 205. Kitamura, H., Kamon, H., Sawa, S.et al. 2005. IL-6-STAT3 controls intracellular MHC class II alphabeta dimer level through cathepsin S activity in dendritic cells. Immunity 23:491. [DOI] [PubMed] [Google Scholar]
- 206. Kortylewski, M., Kujawski, M., Herrmann, A.et al. 2009. Toll-like receptor 9 activation of signal transducer and activator of transcription 3 constrains its agonist-based immunotherapy. Cancer Res. 69:2497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Ohno, Y., Kitamura, H., Takahashi, N.et al. 2016. IL-6 down-regulates HLA class II expression and IL-12 production of human dendritic cells to impair activation of antigen-specific CD4(+) T cells. Cancer Immunol. Immunother. 65:193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Yu, S., Liu, C., Su, K.et al. 2007. Tumor exosomes inhibit differentiation of bone marrow dendritic cells. J. Immunol. 178:6867. [DOI] [PubMed] [Google Scholar]
- 209. Tang, M., Diao, J., Gu, H., Khatri, I., Zhao, J. and Cattral, M. S. 2015. Toll-like receptor 2 activation promotes tumor dendritic cell dysfunction by regulating IL-6 and IL-10 receptor signaling. Cell Rep. 13:2851. [DOI] [PubMed] [Google Scholar]
- 210. Martinez, F. O., Helming, L. and Gordon, S. 2009. Alternative activation of macrophages: an immunologic functional perspective. Annu. Rev. Immunol. 27:451. [DOI] [PubMed] [Google Scholar]
- 211. Sica, A., Schioppa, T., Mantovani, A. and Allavena, P. 2006. Tumour-associated macrophages are a distinct M2 polarised population promoting tumour progression: potential targets of anti-cancer therapy. Eur. J. Cancer 42:717. [DOI] [PubMed] [Google Scholar]
- 212. Lewis, C. E. and Pollard, J. W. 2006. Distinct role of macrophages in different tumor microenvironments. Cancer Res. 66:605. [DOI] [PubMed] [Google Scholar]
- 213. Italiani, P. and Boraschi, D. 2014. From monocytes to M1/M2 macrophages: phenotypical vs. functional differentiation. Front. Immunol. 5:514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Wan, S., Zhao, E., Kryczek, I.et al. 2014. Tumor-associated macrophages produce interleukin 6 and signal via STAT3 to promote expansion of human hepatocellular carcinoma stem cells. Gastroenterology 147:1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Solís-Martínez, R., Cancino-Marentes, M., Hernández-Flores, G.et al. 2018. Regulation of immunophenotype modulation of monocytes-macrophages from M1 into M2 by prostate cancer cell-culture supernatant via transcription factor STAT3. Immunol. Lett. 196:140. [DOI] [PubMed] [Google Scholar]
- 216. Fu, X. L., Duan, W., Su, C. Y.et al. 2017. Interleukin 6 induces M2 macrophage differentiation by STAT3 activation that correlates with gastric cancer progression. Cancer Immunol. Immunother. 66:1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Ham, S., Lima, L. G., Chai, E. P. Z.et al. 2018. Breast cancer-derived exosomes alter macrophage polarization via gp130/STAT3 signaling. Front. Immunol. 9:871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Gabrilovich, D. I., Bronte, V., Chen, S. H.et al. 2007. The terminology issue for myeloid-derived suppressor cells. Cancer Res. 67:425; author reply 426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Chalmin, F., Ladoire, S., Mignot, G.et al. 2010. Membrane-associated Hsp72 from tumor-derived exosomes mediates STAT3-dependent immunosuppressive function of mouse and human myeloid-derived suppressor cells. J. Clin. Invest. 120:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. Chowdhury, P. S., Chamoto, K. and Honjo, T. 2018. Combination therapy strategies for improving PD-1 blockade efficacy: a new era in cancer immunotherapy. J. Intern. Med. 283:110. [DOI] [PubMed] [Google Scholar]
- 221. Bu, L. L., Yu, G. T., Wu, L.et al. 2017. STAT3 induces immunosuppression by upregulating PD-1/PD-L1 in HNSCC. J. Dent. Res. 96:1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Lu, C., Talukder, A., Savage, N. M., Singh, N. and Liu, K. 2017. JAK-STAT-mediated chronic inflammation impairs cytotoxic T lymphocyte activation to decrease anti-PD-1 immunotherapy efficacy in pancreatic cancer. Oncoimmunology 6:e1291106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Wölfle, S. J., Strebovsky, J., Bartz, H.et al. 2011. PD-L1 expression on tolerogenic APCs is controlled by STAT-3. Eur. J. Immunol. 41:413. [DOI] [PubMed] [Google Scholar]
- 224. Zhang, N., Zeng, Y., Du, W.et al. 2016. The EGFR pathway is involved in the regulation of PD-L1 expression via the IL-6/JAK/STAT3 signaling pathway in EGFR-mutated non-small cell lung cancer. Int. J. Oncol. 49:1360. [DOI] [PubMed] [Google Scholar]
- 225. Cheng, Y., Li, H., Deng, Y.et al. 2018. Cancer-associated fibroblasts induce PDL1+ neutrophils through the IL6-STAT3 pathway that foster immune suppression in hepatocellular carcinoma. Cell Death Dis. 9:422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Lamano, J. B., Lamano, J. B., Li, Y. D.et al. 2019. Glioblastoma-derived IL6 induces immunosuppressive peripheral myeloid cell PD-L1 and promotes tumor growth. Clin. Cancer Res. 25:3643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Spary, L. K., Salimu, J., Webber, J. P., Clayton, A., Mason, M. D. and Tabi, Z. 2014. Tumor stroma-derived factors skew monocyte to dendritic cell differentiation toward a suppressive CD14+ PD-L1+ phenotype in prostate cancer. Oncoimmunology 3:e955331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Jones, B. E., Maerz, M. D. and Buckner, J. H. 2018. IL-6: a cytokine at the crossroads of autoimmunity. Curr. Opin. Immunol. 55:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Inshaw, J. R. J., Cutler, A. J., Burren, O. S., Stefana, M. I. and Todd, J. A. 2018. Approaches and advances in the genetic causes of autoimmune disease and their implications. Nat. Immunol. 19:674. [DOI] [PubMed] [Google Scholar]
- 230. Rothhammer, V. and Quintana, F. J. 2016. Environmental control of autoimmune inflammation in the central nervous system. Curr. Opin. Immunol. 43:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. Mathis, D. and Benoist, C. 2004. Back to central tolerance. Immunity 20:509. [DOI] [PubMed] [Google Scholar]
- 232. Murakami, M. and Hirano, T. 2011. A four-step model for the IL-6 amplifier, a regulator of chronic inflammations in tissue-specific MHC class II-associated autoimmune diseases. Front. Immunol. 2:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Anand, P., Kunnumakkara, A. B., Kunnumakara, A. B.et al. 2008. Cancer is a preventable disease that requires major lifestyle changes. Pharm. Res. 25:2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Madhok, R., Crilly, A., Watson, J. and Capell, H. A. 1993. Serum interleukin 6 levels in rheumatoid arthritis: correlations with clinical and laboratory indices of disease activity. Ann. Rheum. Dis. 52:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Ludwig, H., Nachbaur, D. M., Fritz, E., Krainer, M. and Huber, H. 1991. Interleukin-6 is a prognostic factor in multiple myeloma. Blood 77:2794. [PubMed] [Google Scholar]
- 236. Hirano, T., Teranishi, T., Toba, H., Sakaguchi, N., Fukukawa, T. and Tsuyuguchi, I. 1981. Human helper T cell factor(s) (ThF). I. Partial purification and characterization. J. Immunol. 126:517. [PubMed] [Google Scholar]
- 237. Teranishi, T., Hirano, T., Arima, N. and Onoue, K. 1982. Human helper T cell factor(s) (ThF). II. Induction of IgG production in B lymphoblastoid cell lines and identification of T cell-replacing factor- (TRF) like factor(s). J. Immunol. 128:1903. [PubMed] [Google Scholar]
- 238. Sela, O., el-Roeiy, A., Pick, A. I. and Shoenfeld, Y. 1987. Serum immunoglobulin levels in patients with active pulmonary tuberculosis and patients with Klebsiella infection. Immunol. Lett. 15:117. [DOI] [PubMed] [Google Scholar]
- 239. Shoenfeld, Y. and Isenberg, D. A. 1988. Mycobacteria and autoimmunity. Immunol. Today 9:178. [DOI] [PubMed] [Google Scholar]
- 240. Falagas, M. E., Kouranos, V. D., Athanassa, Z. and Kopterides, P. 2010. Tuberculosis and malignancy. QJM 103:461. [DOI] [PubMed] [Google Scholar]
- 241. Potter, M. and Boyce, C. R. 1962. Induction of plasma-cell neoplasms in strain BALB/c mice with mineral oil and mineral oil adjuvants. Nature 193:1086. [DOI] [PubMed] [Google Scholar]
- 242. Anderson, P. N. and Potter, M. 1969. Induction of plasma cell tumours in BALB-c mice with 2,6,10,14-tetramethylpentadecane (pristane). Nature 222:994. [DOI] [PubMed] [Google Scholar]
- 243. Potter, M. and Wax, J. S. 1981. Genetics of susceptibility to pristane-induced plasmacytomas in BALB/cAn: reduced susceptibility in BALB/cJ with a brief description of pristane-induced arthritis. J. Immunol. 127:1591. [PubMed] [Google Scholar]
- 244. Nordan, R. P. and Potter, M. 1986. A macrophage-derived factor required by plasmacytomas for survival and proliferation in vitro. Science 233:566. [DOI] [PubMed] [Google Scholar]
- 245. Satoh, M. and Reeves, W. H. 1994. Induction of lupus-associated autoantibodies in BALB/c mice by intraperitoneal injection of pristane. J. Exp. Med. 180:2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Suematsu, S., Matsusaka, T., Matsuda, T.et al. 1992. Generation of plasmacytomas with the chromosomal translocation t(12;15) in interleukin 6 transgenic mice. Proc. Natl Acad. Sci. USA 89:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Heinrich, P. C., Castell, J. V. and Andus, T. 1990. Interleukin-6 and the acute phase response. Biochem. J. 265:621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Lesnikov, V. A., Efremov, O. M., Korneva, E. A., Van Damme, J. and Billiau, A. 1991. Fever produced by intrahypothalamic injection of interleukin-1 and interleukin-6. Cytokine 3:195. [DOI] [PubMed] [Google Scholar]
- 249. Alonzi, T., Fattori, E., Lazzaro, D.et al. 1998. Interleukin 6 is required for the development of collagen-induced arthritis. J. Exp. Med. 187:461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Ohshima, S., Saeki, Y., Mima, T.et al. 1998. Interleukin 6 plays a key role in the development of antigen-induced arthritis. Proc. Natl Acad. Sci. USA 95:8222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251. Eugster, H. P., Frei, K., Kopf, M., Lassmann, H. and Fontana, A. 1998. IL-6-deficient mice resist myelin oligodendrocyte glycoprotein-induced autoimmune encephalomyelitis. Eur. J. Immunol. 28:2178. [DOI] [PubMed] [Google Scholar]
- 252. Samoilova, E. B., Horton, J. L., Hilliard, B., Liu, T. S. and Chen, Y. 1998. IL-6-deficient mice are resistant to experimental autoimmune encephalomyelitis: roles of IL-6 in the activation and differentiation of autoreactive T cells. J. Immunol. 161:6480. [PubMed] [Google Scholar]
- 253. Richards, H. B., Satoh, M., Jennette, J. C., Okano, T., Kanwar, Y. S. and Reeves, W. H. 1999. Disparate T cell requirements of two subsets of lupus-specific autoantibodies in pristane-treated mice. Clin. Exp. Immunol. 115:547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Lattanzio, G., Libert, C., Aquilina, M.et al. 1997. Defective development of pristane-oil-induced plasmacytomas in interleukin-6-deficient BALB/c mice. Am. J. Pathol. 151:689. [PMC free article] [PubMed] [Google Scholar]
- 255. Ishihara, K., Sawa, S., Ikushima, H.et al. 2004. The point mutation of tyrosine 759 of the IL-6 family cytokine receptor gp130 synergizes with HTLV-1 pX in promoting rheumatoid arthritis-like arthritis. Int. Immunol. 16:455. [DOI] [PubMed] [Google Scholar]
- 256. Tebbutt, N. C., Giraud, A. S., Inglese, M.et al. 2002. Reciprocal regulation of gastrointestinal homeostasis by SHP2 and STAT-mediated trefoil gene activation in gp130 mutant mice. Nat. Med. 8:1089. [DOI] [PubMed] [Google Scholar]
- 257. Gao, S. P., Mark, K. G., Leslie, K.et al. 2007. Mutations in the EGFR kinase domain mediate STAT3 activation via IL-6 production in human lung adenocarcinomas. J. Clin. Invest. 117:3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Park, E. J., Lee, J. H., Yu, G. Y.et al. 2010. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression. Cell 140:197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Nowell, M. A., Williams, A. S., Carty, S. A.et al. 2009. Therapeutic targeting of IL-6 trans signaling counteracts STAT3 control of experimental inflammatory arthritis. J. Immunol. 182:613. [DOI] [PubMed] [Google Scholar]
- 260. de Benedetti, F., Massa, M., Robbioni, P., Ravelli, A., Burgio, G. R. and Martini, A. 1991. Correlation of serum interleukin-6 levels with joint involvement and thrombocytosis in systemic juvenile rheumatoid arthritis. Arthritis Rheum. 34:1158. [DOI] [PubMed] [Google Scholar]
- 261. Reinisch, W., Gasché, C., Tillinger, W.et al. 1999. Clinical relevance of serum interleukin-6 in Crohn’s disease: single point measurements, therapy monitoring, and prediction of clinical relapse. Am. J. Gastroenterol. 94:2156. [DOI] [PubMed] [Google Scholar]
- 262. Lippitz, B. E. and Harris, R. A. 2016. Cytokine patterns in cancer patients: a review of the correlation between interleukin 6 and prognosis. Oncoimmunology 5:e1093722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263. Dar, S. A., Haque, S., Mandal, R. K.et al. 2017. Interleukin-6-174G > C (rs1800795) polymorphism distribution and its association with rheumatoid arthritis: a case-control study and meta-analysis. Autoimmunity 50:158. [DOI] [PubMed] [Google Scholar]
- 264. Hou, H., Wang, C., Sun, F., Zhao, L., Dun, A. and Sun, Z. 2015. Association of interleukin-6 gene polymorphism with coronary artery disease: an updated systematic review and cumulative meta-analysis. Inflamm. Res. 64:707. [DOI] [PubMed] [Google Scholar]
- 265. Interleukin-6 Receptor Mendelian Randomisation Analysis (IL6R MR) Consortium; Swerdlow, D. I., Holmes, M. V., Kuchenbaecker, K. B.et al. 2012. The interleukin-6 receptor as a target for prevention of coronary heart disease: a Mendelian randomisation analysis. Lancet 379:1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266. Li, F., Xu, J., Zheng, J.et al. 2014. Association between interleukin-6 gene polymorphisms and rheumatoid arthritis in Chinese Han population: a case-control study and a meta-analysis. Sci. Rep. 4:5714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267. Luchtefeld, M., Schunkert, H., Stoll, M.et al. 2007. Signal transducer of inflammation gp130 modulates atherosclerosis in mice and man. J. Exp. Med. 204:1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268. Okada, Y., Wu, D., Trynka, G.et al. ; RACI Consortium; GARNET Consortium. 2014. Genetics of rheumatoid arthritis contributes to biology and drug discovery. Nature 506:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. Stahl, E. A., Raychaudhuri, S., Remmers, E. F.et al. ; BIRAC Consortium; YEAR Consortium. 2010. Genome-wide association study meta-analysis identifies seven new rheumatoid arthritis risk loci. Nat. Genet. 42:508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270. Ferreira, M. A., Matheson, M. C., Duffy, D. L.et al. ; Australian Asthma Genetics Consortium. 2011. Identification of IL6R and chromosome 11q13.5 as risk loci for asthma. Lancet 378:1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271. Esparza-Gordillo, J., Schaarschmidt, H., Liang, L.et al. 2013. A functional IL-6 receptor (IL6R) variant is a risk factor for persistent atopic dermatitis. J. Allergy Clin. Immunol. 132:371. [DOI] [PubMed] [Google Scholar]
- 272. Rebouissou, S., Amessou, M., Couchy, G.et al. 2009. Frequent in-frame somatic deletions activate gp130 in inflammatory hepatocellular tumours. Nature 457:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Annunziata, C. M., Davis, R. E., Demchenko, Y.et al. 2007. Frequent engagement of the classical and alternative NF-kappaB pathways by diverse genetic abnormalities in multiple myeloma. Cancer Cell 12:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Keats, J. J., Fonseca, R., Chesi, M.et al. 2007. Promiscuous mutations activate the noncanonical NF-kappaB pathway in multiple myeloma. Cancer Cell 12:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275. Fishman, D., Faulds, G., Jeffery, R.et al. 1998. The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J. Clin. Invest. 102:1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Benrick, A., Jirholt, P., Wernstedt, I.et al. 2008. A non-conservative polymorphism in the IL-6 signal transducer (IL6ST)/gp130 is associated with myocardial infarction in a hypertensive population. Regul. Pept. 146:189. [DOI] [PubMed] [Google Scholar]
- 277. Lee, H., Herrmann, A., Deng, J. H.et al. 2009. Persistently activated Stat3 maintains constitutive NF-kappaB activity in tumors. Cancer Cell 15:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278. Kesanakurti, D., Chetty, C., Rajasekhar Maddirela, D., Gujrati, M. and Rao, J. S. 2013. Essential role of cooperative NF-κB and Stat3 recruitment to ICAM-1 intronic consensus elements in the regulation of radiation-induced invasion and migration in glioma. Oncogene 32:5144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279. Taniguchi, K. and Karin, M. 2018. NF-κB, inflammation, immunity and cancer: coming of age. Nat. Rev. Immunol. 18:309. [DOI] [PubMed] [Google Scholar]
- 280. Ishimi, Y., Miyaura, C., Jin, C. H.et al. 1990. IL-6 is produced by osteoblasts and induces bone resorption. J. Immunol. 145:3297. [PubMed] [Google Scholar]
- 281. Poli, V., Balena, R., Fattori, E.et al. 1994. Interleukin-6 deficient mice are protected from bone loss caused by estrogen depletion. EMBO J. 13:1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282. Suzuki, H., Raska, M., Yamada, K.et al. 2014. Cytokines alter IgA1 O-glycosylation by dysregulating C1GalT1 and ST6GalNAc-II enzymes. J. Biol. Chem. 289:5330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283. Ishibashi, T., Kimura, H., Uchida, T., Kariyone, S., Friese, P. and Burstein, S. A. 1989. Human interleukin 6 is a direct promoter of maturation of megakaryocytes in vitro. Proc. Natl Acad. Sci. USA 86:5953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284. Ishibashi, T., Kimura, H., Shikama, Y.et al. 1989. Interleukin-6 is a potent thrombopoietic factor in vivo in mice. Blood 74:1241. [PubMed] [Google Scholar]
- 285. Ershler, W. B., Sun, W. H., Binkley, N.et al. 1993. Interleukin-6 and aging: blood levels and mononuclear cell production increase with advancing age and in vitro production is modifiable by dietary restriction. Lymphokine Cytokine Res. 12:225. [PubMed] [Google Scholar]
- 286. Kamimura, D., Ohki, T., Arima, Y. and Murakami, M. 2018. Gateway reflex: neural activation-mediated immune cell gateways in the central nervous system. Int. Immunol. 30:281. [DOI] [PubMed] [Google Scholar]
- 287. Pavlov, V. A., Chavan, S. S. and Tracey, K. J. 2018. Molecular and functional neuroscience in immunity. Annu. Rev. Immunol. 36:783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288. Landen, C. N.Jr, Lin, Y. G., Armaiz Pena, G. N.et al. 2007. Neuroendocrine modulation of signal transducer and activator of transcription-3 in ovarian cancer. Cancer Res. 67:10389. [DOI] [PubMed] [Google Scholar]
- 289. Szabo-Fresnais, N., Lefebvre, F., Germain, A., Fischmeister, R. and Pomérance, M. 2010. A new regulation of IL-6 production in adult cardiomyocytes by beta-adrenergic and IL-1 beta receptors and induction of cellular hypertrophy by IL-6 trans-signalling. Cell. Signal. 22:1143. [DOI] [PubMed] [Google Scholar]
- 290. Qing, H., Desrouleaux, R., Israni-Winger, K.et al. 2020. Origin and function of stress-induced IL-6 in murine models. Cell 182:372.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291. Lasry, A. and Ben-Neriah, Y. 2015. Senescence-associated inflammatory responses: aging and cancer perspectives. Trends Immunol. 36:217. [DOI] [PubMed] [Google Scholar]
- 292. Franceschi, C., Garagnani, P., Vitale, G., Capri, M. and Salvioli, S. 2017. Inflammaging and ‘Garb-aging’. Trends Endocrinol. Metab. 28:199. [DOI] [PubMed] [Google Scholar]
- 293. Zhou, F., Yu, T., Du, R.et al. 2020. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395:1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294. Akbar, A. N. and Gilroy, D. W. 2020. Aging immunity may exacerbate COVID-19. Science 369:256. [DOI] [PubMed] [Google Scholar]
- 295. Jin, B., Wang, Y., Wu, C. L., Liu, K. Y., Chen, H. and Mao, Z. B. 2014. PIM-1 modulates cellular senescence and links IL-6 signaling to heterochromatin formation. Aging Cell. 13:879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Daynes, R. A., Araneo, B. A., Ershler, W. B., Maloney, C., Li, G. Z. and Ryu, S. Y. 1993. Altered regulation of IL-6 production with normal aging. Possible linkage to the age-associated decline in dehydroepiandrosterone and its sulfated derivative. J. Immunol. 150:5219. [PubMed] [Google Scholar]
- 297. Hong, D. S., Angelo, L. S. and Kurzrock, R. 2007. Interleukin-6 and its receptor in cancer: implications for translational therapeutics. Cancer 110:1911. [DOI] [PubMed] [Google Scholar]
- 298. Aguayo-Mazzucato, C., Andle, J., Lee, T. B.Jret al. 2019. Acceleration of β cell aging determines diabetes and senolysis improves disease outcomes. Cell Metab. 30:129.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299. Bluestone, J. A., Herold, K. and Eisenbarth, G. 2010. Genetics, pathogenesis and clinical interventions in type 1 diabetes. Nature 464:1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300. Wållberg, M. and Cooke, A. 2013. Immune mechanisms in type 1 diabetes. Trends Immunol. 34:583. [DOI] [PubMed] [Google Scholar]
- 301. Christoffersson, G., Rodriguez-Calvo, T., and von Herrath, M. 2016. Recent advances in understanding type 1 diabetes. F1000Res. 5:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302. Haslam, D. W. and James, W. P. 2005. Obesity. Lancet 366:1197. [DOI] [PubMed] [Google Scholar]
- 303. Ghosh, S. and Ashcraft, K. 2013. An IL-6 link between obesity and cancer. Front. Biosci. (Elite Ed.) 5:461. [DOI] [PubMed] [Google Scholar]
- 304. Kern, L., Mittenbuhler, M. J., Vesting, A. J., Ostermann, A. L., Wunderlich, C. M., and Wunderlich, F. T. 2019. Obesity-induced TNFalpha and IL-6 signaling: the missing link between obesity and inflammation-driven liver and colorectal cancers. Cancers 11:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305. Trayhurn, P., Wang, B. and Wood, I. S. 2008. Hypoxia in adipose tissue: a basis for the dysregulation of tissue function in obesity? Br. J. Nutr. 100:227. [DOI] [PubMed] [Google Scholar]
- 306. Shi, H., Kokoeva, M. V., Inouye, K., Tzameli, I., Yin, H. and Flier, J. S. 2006. TLR4 links innate immunity and fatty acid-induced insulin resistance. J. Clin. Invest. 116:3015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307. Davis, J. E., Gabler, N. K., Walker-Daniels, J. and Spurlock, M. E. 2008. Tlr-4 deficiency selectively protects against obesity induced by diets high in saturated fat. Obesity (Silver Spring) 16:1248. [DOI] [PubMed] [Google Scholar]
- 308. Schaeffler, A., Gross, P., Buettner, R.et al. 2009. Fatty acid-induced induction of Toll-like receptor-4/nuclear factor-kappaB pathway in adipocytes links nutritional signalling with innate immunity. Immunology 126:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309. Lee, H., Deng, J., Kujawski, M.et al. 2010. STAT3-induced S1PR1 expression is crucial for persistent STAT3 activation in tumors. Nat. Med. 16:1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310. Liang, J., Nagahashi, M., Kim, E. Y.et al. 2013. Sphingosine-1-phosphate links persistent STAT3 activation, chronic intestinal inflammation, and development of colitis-associated cancer. Cancer Cell. 23:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311. Migone, T. S., Lin, J. X., Cereseto, A.et al. 1995. Constitutively activated Jak-STAT pathway in T cells transformed with HTLV-I. Science 269:79. [DOI] [PubMed] [Google Scholar]
- 312. Yu, C. L., Meyer, D. J., Campbell, G. S.et al. 1995. Enhanced DNA-binding activity of a Stat3-related protein in cells transformed by the Src oncoprotein. Science 269:81. [DOI] [PubMed] [Google Scholar]
- 313. Hilbert, D. M., Migone, T. S., Kopf, M., Leonard, W. J. and Rudikoff, S. 1996. Distinct tumorigenic potential of abl and raf in B cell neoplasia: abl activates the IL-6 signaling pathway. Immunity 5:81. [DOI] [PubMed] [Google Scholar]
- 314. Besser, D., Bromberg, J. F., Darnell, J. E.Jr and Hanafusa, H. 1999. A single amino acid substitution in the v-Eyk intracellular domain results in activation of Stat3 and enhances cellular transformation. Mol. Cell. Biol. 19:1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315. Bassères, D. S., Ebbs, A., Levantini, E. and Baldwin, A. S. 2010. Requirement of the NF-kappaB subunit p65/RelA for K-Ras-induced lung tumorigenesis. Cancer Res. 70:3537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316. Ling, J., Kang, Y., Zhao, R.et al. 2012. KrasG12D-induced IKK2/β/NF-κB activation by IL-1α and p62 feedforward loops is required for development of pancreatic ductal adenocarcinoma. Cancer Cell 21:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317. Lesina, M., Kurkowski, M. U., Ludes, K.et al. 2011. Stat3/Socs3 activation by IL-6 transsignaling promotes progression of pancreatic intraepithelial neoplasia and development of pancreatic cancer. Cancer Cell 19:456. [DOI] [PubMed] [Google Scholar]
- 318. Koorstra, J. B., Hustinx, S. R., Offerhaus, G. J. and Maitra, A. 2008. Pancreatic carcinogenesis. Pancreatology 8:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319. Bharadwaj, U., Marin-Muller, C., Li, M., Chen, C. and Yao, Q. 2011. Mesothelin confers pancreatic cancer cell resistance to TNF-α-induced apoptosis through Akt/PI3K/NF-κB activation and IL-6/Mcl-1 overexpression. Mol. Cancer 10:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320. Bharadwaj, U., Marin-Muller, C., Li, M., Chen, C. and Yao, Q. 2011. Mesothelin overexpression promotes autocrine IL-6/sIL-6R trans-signaling to stimulate pancreatic cancer cell proliferation. Carcinogenesis 32:1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321. Hartman, Z. C., Yang, X. Y., Glass, O.et al. 2011. HER2 overexpression elicits a proinflammatory IL-6 autocrine signaling loop that is critical for tumorigenesis. Cancer Res. 71:4380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322. Schwitalla, S., Ziegler, P. K., Horst, D.et al. 2013. Loss of p53 in enterocytes generates an inflammatory microenvironment enabling invasion and lymph node metastasis of carcinogen-induced colorectal tumors. Cancer Cell 23:93. [DOI] [PubMed] [Google Scholar]
- 323. Fang, T., Lv, H., Lv, G.et al. 2018. Tumor-derived exosomal miR-1247-3p induces cancer-associated fibroblast activation to foster lung metastasis of liver cancer. Nat. Commun. 9:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324. Kawai, T. and Akira, S. 2010. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat. Immunol. 11:373. [DOI] [PubMed] [Google Scholar]
- 325. Yu, H., Lee, H., Herrmann, A., Buettner, R. and Jove, R. 2014. Revisiting STAT3 signalling in cancer: new and unexpected biological functions. Nat. Rev. Cancer 14:736. [DOI] [PubMed] [Google Scholar]
- 326. Wu, S., Rhee, K. J., Albesiano, E.et al. 2009. A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat. Med. 15:1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327. Bronte-Tinkew, D. M., Terebiznik, M., Franco, A.et al. 2009. Helicobacter pylori cytotoxin-associated gene A activates the signal transducer and activator of transcription 3 pathway in vitro and in vivo. Cancer Res. 69:632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328. Yoshida, T., Hanada, T., Tokuhisa, T.et al. 2002. Activation of STAT3 by the hepatitis C virus core protein leads to cellular transformation. J. Exp. Med. 196:641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329. Choudhari, S. R., Khan, M. A., Harris, G.et al. 2007. Deactivation of Akt and STAT3 signaling promotes apoptosis, inhibits proliferation, and enhances the sensitivity of hepatocellular carcinoma cells to an anticancer agent, Atiprimod. Mol. Cancer Ther. 6:112. [DOI] [PubMed] [Google Scholar]
- 330. Xiong, Q., Wu, S., Wang, J.et al. 2017. Hepatitis B virus promotes cancer cell migration by downregulating miR-340-5p expression to induce STAT3 overexpression. Cell Biosci. 7:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331. Muromoto, R., Ikeda, O., Okabe, K.et al. 2009. Epstein-Barr virus-derived EBNA2 regulates STAT3 activation. Biochem. Biophys. Res. Commun. 378:439. [DOI] [PubMed] [Google Scholar]
- 332. Sun, S. and Steinberg, B. M. 2002. PTEN is a negative regulator of STAT3 activation in human papillomavirus-infected cells. J. Gen. Virol. 83(Pt 7):1651. [DOI] [PubMed] [Google Scholar]
- 333. Huang, C., Wang, Y., Li, X.et al. 2020. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334. Thompson, B. T., Chambers, R. C. and Liu, K. D. 2017. Acute respiratory distress syndrome. N. Engl. J. Med. 377:1904. [DOI] [PubMed] [Google Scholar]
- 335. de Wit, E., van Doremalen, N., Falzarano, D. and Munster, V. J. 2016. SARS and MERS: recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 14:523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336. Mangalmurti, N. and Hunter, C. A. 2020. Cytokine storms: understanding COVID-19. Immunity 53:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337. Chen, N., Zhou, M., Dong, X.et al. 2020. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395:507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338. Liu, B., Li, M., Zhou, Z., Guan, X. and Xiang, Y. 2020. Can we use interleukin-6 (IL-6) blockade for coronavirus disease 2019 (COVID-19)-induced cytokine release syndrome (CRS)? J. Autoimmun. 111:102452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339. Herold, T., Jurinovic, V., Arnreich, C.et al. 2020. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J. Allergy Clin. Immunol. 146:128.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340. Del Valle, D. M., Kim-Schulze, S., Huang, H. H.et al. 2020. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 26:1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341. Zhang, X., Wu, K., Wang, D.et al. 2007. Nucleocapsid protein of SARS-CoV activates interleukin-6 expression through cellular transcription factor NF-kappaB. Virology 365:324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342. Zhou, P., Yang, X. L., Wang, X. G.et al. 2020. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343. Hoffmann, M., Kleine-Weber, H., Schroeder, S.et al. 2020. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181:271.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344. Kuba, K., Imai, Y., Rao, S.et al. 2005. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat. Med. 11:875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345. Imai, Y., Kuba, K., Rao, S.et al. 2005. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature 436:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346. Eguchi, S., Kawai, T., Scalia, R. and Rizzo, V. 2018. Understanding angiotensin II type 1 receptor signaling in vascular pathophysiology. Hypertension 71:804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347. Brasier, A. R., Recinos, A.3rd and Eledrisi, M. S. 2002. Vascular inflammation and the renin-angiotensin system. Arterioscler. Thromb. Vasc. Biol. 22:1257. [DOI] [PubMed] [Google Scholar]
- 348. Hunyady, L. and Catt, K. J. 2006. Pleiotropic AT1 receptor signaling pathways mediating physiological and pathogenic actions of angiotensin II. Mol. Endocrinol. 20:953. [DOI] [PubMed] [Google Scholar]
- 349. Moore, J. B. and June, C. H. 2020. Cytokine release syndrome in severe COVID-19. Science 368:473. [DOI] [PubMed] [Google Scholar]
- 350. McGonagle, D., Sharif, K., O’Regan, A. and Bridgewood, C. 2020. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun. Rev. 19:102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351. June, C. H., O’Connor, R. S., Kawalekar, O. U., Ghassemi, S. and Milone, M. C. 2018. CAR T cell immunotherapy for human cancer. Science 359:1361. [DOI] [PubMed] [Google Scholar]
- 352. Neelapu, S. S., Tummala, S., Kebriaei, P.et al. 2018. Chimeric antigen receptor T-cell therapy—assessment and management of toxicities. Nat. Rev. Clin. Oncol. 15:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353. Norelli, M., Camisa, B., Barbiera, G.et al. 2018. Monocyte-derived IL-1 and IL-6 are differentially required for cytokine-release syndrome and neurotoxicity due to CAR T cells. Nat. Med. 24:739. [DOI] [PubMed] [Google Scholar]
- 354. Giavridis, T., van der Stegen, S. J. C., Eyquem, J., Hamieh, M., Piersigilli, A. and Sadelain, M. 2018. CAR T cell-induced cytokine release syndrome is mediated by macrophages and abated by IL-1 blockade. Nat. Med. 24:731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355. Imai, Y., Kuba, K., Neely, G. G.et al. 2008. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell 133:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356. Ibrahim, Y. F., Moussa, R. A., Bayoumi, A. M. A. and Ahmed, A. F. 2020. Tocilizumab attenuates acute lung and kidney injuries and improves survival in a rat model of sepsis via down-regulation of NF-κB/JNK: a possible role of P-glycoprotein. Inflammopharmacology 28:215. [DOI] [PubMed] [Google Scholar]
- 357. Marshall, R. P., Webb, S., Bellingan, G. J.et al. 2002. Angiotensin converting enzyme insertion/deletion polymorphism is associated with susceptibility and outcome in acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 166:646. [DOI] [PubMed] [Google Scholar]
- 358. Yamamoto, N., Ariumi, Y., Nishida, N.et al. 2020. SARS-CoV-2 infections and COVID-19 mortalities strongly correlate with ACE1 I/D genotype. Gene 758:144944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359. Rigat, B., Hubert, C., Alhenc-Gelas, F., Cambien, F., Corvol, P. and Soubrier, F. 1990. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J. Clin. Invest. 86:1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360. Meng, J., Xiao, G., Zhang, J.et al. 2020. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Emerg. Microbes Infect. 9:757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361. Zhang, P., Zhu, L., Cai, J.et al. 2020. Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ. Res. 126:1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362. Matsuzawa, Y., Ogawa, H., Kimura, K.et al. 2020. Renin-angiotensin system inhibitors and the severity of coronavirus disease 2019 in Kanagawa, Japan: a retrospective cohort study. Hypertens. Res. 43:1257. [DOI] [PubMed] [Google Scholar]
- 363. Caldeira, D., Alves, M., Gouveia E Melo, R.et al. 2020. Angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers and the risk of COVID-19 infection or severe disease: systematic review and meta-analysis. Int. J. Cardiol. Heart Vasc. 31:100627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364. Maude, S. L., Frey, N., Shaw, P. A.et al. 2014. Chimeric antigen receptor T cells for sustained remissions in leukemia. N. Engl. J. Med. 371:1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365. Xu, X., Han, M., Li, T.et al. 2020. Effective treatment of severe COVID-19 patients with tocilizumab. Proc. Natl Acad. Sci. USA 117:10970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366. Luo, P., Liu, Y., Qiu, L., Liu, X., Liu, D. and Li, J. 2020. Tocilizumab treatment in COVID-19: a single center experience. J. Med. Virol. 92:814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367. Alattar, R., Ibrahim, T. B. H., Shaar, S. H.et al. 2020. Tocilizumab for the treatment of severe coronavirus disease 2019. J. Med. Virol. 92:2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368. Narain, S., Stefanov, D. G., Chau, A. S.et al. 2021. Comparative survival analysis of immunomodulatory therapy for coronavirus disease 2019 cytokine storm. Chest. doi: 10.1016/j.chest.2020.09.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369. Bronte, V., Ugel, S., Tinazzi, E.et al. 2020. Baricitinib restrains the immune dysregulation in patients with severe COVID-19. J. Clin. Invest. 130:6409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370. Group, R. C., Horby, P., Lim, W. S.et al. 2021. Dexamethasone in hospitalized patients with Covid-19—preliminary report. N Engl J Med. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371. Zheng, K. I., Gao, F., Wang, X. B.et al. 2020. Letter to the Editor: obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease. Metabolism 108:154244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372. Guo, W., Li, M., Dong, Y.et al. 2020. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab. Res. Rev. 36:e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373. Clerkin, K. J., Fried, J. A., Raikhelkar, J.et al. 2020. COVID-19 and cardiovascular disease. Circulation 141:1648. [DOI] [PubMed] [Google Scholar]
- 374. Kang, S., Tanaka, T., Narazaki, M. and Kishimoto, T. 2019. Targeting interleukin-6 signaling in clinic. Immunity 50:1007. [DOI] [PubMed] [Google Scholar]
- 375. Topol, E. J. 2019. High-performance medicine: the convergence of human and artificial intelligence. Nat. Med. 25:44. [DOI] [PubMed] [Google Scholar]
- 376. Ball, P. 2011. Physics of life: the dawn of quantum biology. Nature 474:272. [DOI] [PubMed] [Google Scholar]
- 377. Marais, A., Adams, B., Ringsmuth, A. K.et al. 2018. The future of quantum biology. J. R. Soc. Interface 15:e0640. [DOI] [PMC free article] [PubMed] [Google Scholar]