Abstract
Vitamin D deficiency is a major public health concern of pregnant women and neonates worldwide, affecting more than half of neonates. Studies report inconsistent and inconclusive effects of vitamin D treatment on neonatal sepsis. This study aimed to provide conclusive evidence regarding the effect of maternal and cord blood vitamin D levels on neonatal sepsis. Data were retrieved from the electronic database (Web of Science, Scopus, CINAHL [EBSCOhost], ProQuest, EMBASE [Ovid], PubMed, Emcare, MEDLINE [Ovid], and gray literature sources [World cat, Mednar, Google scholar and Google]). Joanna Briggs Institute quality assessment tool was utilized for quality assessment while analysis was performed using Open Meta‐analyst, Comprehensive Meta‐analysis version 3.3.070, and Review Manager version 5.3 software. From the 18 studies included in the study, the overall prevalence of vitamin D deficiency among neonates was 61% (95% CI: 44.3, 77.7); 79.4% (95% CI: 71.6, 87.3) of neonates with sepsis were vitamin D deficient as were 43.7% (23.4, 63.9) of sepsis‐free neonates. Neonates born from mothers with low vitamin D levels were at greater risk of developing neonatal sepsis with a weighed mean difference of −8.57 ng/ml (95% CI: −13.09, −4.05). Similarly, neonates with low cord vitamin D levels were at risk for neonatal sepsis with a mean difference of −8.78 ng/ml (95% CI:‐11.58, −5.99). The incidence of EONS in full‐term newborns was significantly associated with low maternal and cord blood vitamin D levels with weighed mean differences of −11.55ng/ml (95% CI: −17.63, −5.46) & −11.59 ng/ml (95% CI:‐16.65, −6.53), respectively. Low levels of vitamin D both in the cord blood and maternal blood were significantly associated with neonatal sepsis. Hence, vitamin D supplementation for pregnant women and newborns could decrease neonatal sepsis.
Keywords: 25‐hydroxyvitamin D, neonatal infections, newborn, vitamin D deficiency
This is a systematic review and meta‐analysis about the effect of low level of maternal and cord blood vitamin D levels on neonatal sepsis. It is found that low vitamin D levels are risky for neonatal sepsis.

Key messages.
Low levels of vitamin D are common in the general neonatal population and are significantly higher in neonates with sepsis.
Low levels of cord blood and maternal vitamin D are associated with neonatal sepsis.
Maternal periconceptional and postpartum supplementation of vitamin D could prevent this life‐threatening burden of newborns.
1. BACKGROUND
Neonatal sepsis is a systemic infection in the first 28 days of life including bloodstream infections, meningitis, and pneumonia (Moraga & Collaborators, G. C. o. D. 2017). Despite advancements in newborn care, sepsis remains a significant cause of morbidity and mortality globally. The neonatal mortality rate ranges between 11% and 19% of which sepsis contributes to 3 million newborn morbidities (Fleischmann‐Struzek et al., 2018). Globally, sepsis increased neonatal mortality by 1% to 5% and severe sepsis by 9% to 20% (Fleischmann‐Struzek et al., 2018; Hug et al., 2019). The burden is relatively high in Asia and sub‐Saharan Africa (Liu et al., 2015) with the magnitude of neonatal mortality being uneven distributed in sub‐Saharan Africa (29/1000 live births) (You et al., 2015).
Many factors contribute to neonatal sepsis, both maternal and neonatal in origin (Adatara et al., 2019; Oliveira et al., 2016; Hammad & Zainab, 2018; Mugadza et al., 2017; Murthy et al., 2019; Thorne‐Lyman & Fawzi, 2012). An estimated three out of ten neonatal deaths worldwide are thought to be associated with neonatal sepsis secondary to resistant pathogens (Laxminarayan et al., 2016). Annually, around one million newborn deaths are expected to be associated with maternal infections (Black et al., 20166).
Low vitamin D levels in maternal blood during pregnancy and in cord blood are mentioned as risk factors associated with neonatal sepsis. This is explained by vitamin D immune modulation effects which can stimulate the inflammatory mediators and boost the innate immunity (Clancy et al., 2013). It also activates lymphocyte subsets and enhances T‐lymphocyte activation (Youssef et al., 2019). Vitamin D deficiency is common in the general pediatric population and frequently seen in the neonatal period, mainly in the low birthweight and preterm newborns of which neonatal sepsis is more prevalent (McCarthy et al., 2009). Vitamin D deficiency among newborn population ranges from 73% (Khuri‐Bulos et al., 2014) to 94% (Swai et al., 2006), revealing that vitamin D deficiency is a public health problem affecting neonates in several ways. Although low vitamin D levels both in the maternal blood and in the cord blood are associated with newborn infections, there are some studies reporting that this association is insignificant. Thus, these original studies reported inconsistent findings regarding the effects of cord blood and maternal vitamin D levels and the association of neonatal sepsis.
Therefore, the aim of this study was to determine the effects of maternal and newborn cord blood vitamin D levels and the association of neonatal sepsis and to compute the pooled prevalence of cord blood vitamin D deficiency from primary case–control and prospective cohort studies. The pooled estimates were computed using mean and standard deviation of either maternal or cord blood vitamin D levels. The findings of this study will be crucial for policymakers and program planners who are in charge of designing preventive strategies of neonatal sepsis. The findings will have a particular implication for the developing world, where sepsis is the main predictor of newborn deaths (Amare et al., 2019; Cooper, 2014; Rudd et al., 2020).
2. METHODS
2.1. Searching strategies
The preferred reporting items for systematic review and meta‐analysis (PRISMA) guideline were followed to prepare this systematic review and meta‐analysis (Moher et al., 2009). Searching was conducted by three authors (ZWB, TW, and AA) who were trained in systematic review methods. During the searching process, we consulted a senior librarian working at St. Paul's Hospital Millennium Medical College, Ethiopia. The systematic searches were conducted from electronic and other literature sources in the following databases: Web of Science, Emcare (Ovid), MEDLINE (Ovid), CINAHL (EBSCOhost), EMBASE (Ovid), PubMed, ProQuest and Scopus. Mednar, Google scholar, World cat, and Google were explored for gray literature. In addition, we communicated via personal email exploring unpublished articles as well as information of articles with incomplete reports. The reference lists of included articles were crosschecked for articles which fit the searching criteria and if found treated according to PRISMA guidelines. The searches were conducted using indexed terms, combined with key terms, text words, and search strings taken from the review questions. Advanced search strategies were applied in major databases by three authors (ZWB, TW, and AA) independently. The following were used for searching terms: effect OR impact OR association AND “cord blood” OR “maternal blood” AND vitamin D AND “neonatal sepsis.” The searching terms were checked for being indexed term in each of electronic database before proceeding to the actual search. The Boolean operators such as “AND” or “OR” were used accordingly (See Appendix S1). EndNote X8 reference manager was utilized to manage the searched literature (See Appendix S2).
2.2. Inclusion and exclusion criteria
2.2.1. Inclusion criteria
All observational studies (cohort and case–control studies) fulfilling the following criteria were included.
2.2.2. Population
All neonates with neonatal sepsis and their mothers.
2.2.3. Intervention
Vitamin D levels (cord blood and maternal blood vitamin D).
2.2.4. Comparators
Neonates free from neonatal sepsis and their mothers.
2.2.5. Outcome
Neonatal sepsis.
2.2.6. Study designs
Case–control and cohort studies.
2.2.7. Study period
Studies conducted from inception to December 2019 were reviewed and included, accordingly.
2.3. Exclusion criteria
The studies fulfilling the following criteria were excluded:
Articles with irrelevant/incongruent outcomes
Articles with abstract only and when it was difficult to access the full texts after communicating with the corresponding author(s).
Articles without mean and standard deviation scores of vitamin D blood levels.
Finally, 18 cohort and case–control studies that compared either maternal or cord blood vitamin D levels with neonatal sepsis were included. The details are presented using the PRISMA flow diagram (Figure 1).
FIGURE 1.
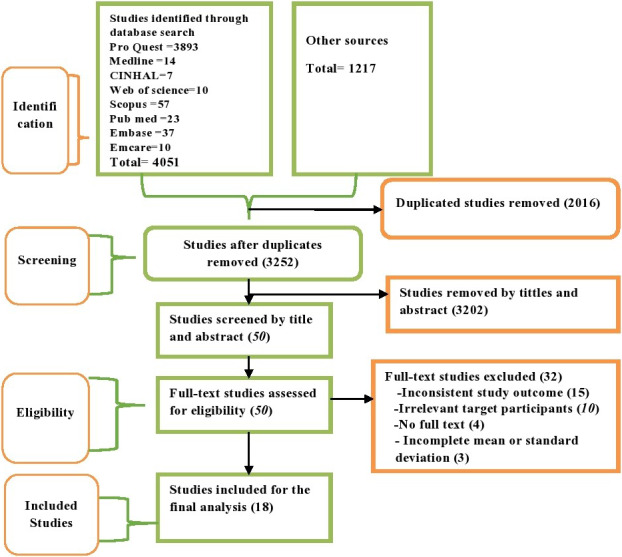
The PRISMA flowchart showing study selection process
2.4. Study selection procedure
The EndNote X8 citation manager was used to import studies extracted from several sources, and duplicates were removed. Titles and abstracts were screened by two investigators (ZWB and TW) based on the predefined inclusion criteria. The full texts were collected and evaluated for eligibility for final inclusion considering study subjects, study design, language, methodologic quality, and outcome by two authors (ZWB and AA), independently. Finally, of the eligible articles, the entirety of each article was reviewed by all investigators.
2.5. Critical appraisal and data abstraction of the studies
Pretested and structured extraction checklist was used to extract the data, and two investigators (ZWB and TW) performed data extraction. Data (author‐year‐country, study population, gestational age in weeks, study design, sample size, vitamin D deficiency (newborns), neonatal vitamin D level (ng/ml), maternal blood vitamin D levels (ng/ml), and type of neonatal sepsis) were extracted and summarized in Microsoft word 2016 (Table 1). Next, the data were stored in Microsoft excel, 2016 by two authors (ZWB and TW) independently. Finally, the data were cleaned and made ready for the final analysis using the excel spreadsheet. Disagreements between the two authors were resolved by the third author (AA). Joana Briggs Institute checklists of cross‐sectional and cohort studies were used for critical appraisal of the included studies (Munn et al., 2015). Critical appraisal was completed by the two authors (ZWB and AA) independently. The tool has yes, no, unclear, and not applicable options. One was given for yes and zero for all other options. The scores were added up and changed into percentages. In this meta‐analysis, articles with > 50% were included in the final analysis (See Appendix S3). After the critical appraisals were completed, the inter‐rater reliability or inter‐rater agreements were computed prior to the final decision of inclusion of the studies in this systematic review and meta‐analysis. The inter‐rater agreements were computed for both cohort and case–control studies using Cohen's kappa coefficient (κ). The findings revealed that there was substantial agreement (Belur et al., 2018) between the two raters in both case–control (κ = 0.67, p ≤ .001) and cohort studies (κ = 0.70, p = .024).
TABLE 1.
Characteristics of studies used to compute the association between low vitamin D levels and neonatal sepsis, 2019
| Author(year) country | Study Population | GA(wks) | Study design | Sample | Cord Vit.D deficiency | Neonatal Vitamin D level (ng/ml) | Maternal Vitamin D level | Type of neonatal sepsis | Quality score | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Controls | Cases (Event/total) | Control (Event/total) | Cases | Controls | Cases | Controls | ||||||
| Sarwade (2019) Sarwade, 2019, India | 30 | 30 | Both | Case–control | 60 | NA | NA | 13.43 ± 3.43 | 21.53 ± 6.6 | NA | NA | EONS | medium |
| Agrawal et al. (2019) (Agrawal et al., 2019), India | 175 | 50 | Term | Case–control | 225 | 151/175 | 37/50 | 12.28 ± 6.11 | 14.88 ± 7.2 | NA | NA | LONS | high |
| Aye et al. (2018) (Aye et al., 2018), Myanmar | 40 | 40 | Term | Case–control | 80 | 40/40 | 26/40 | 9.82 ± 2.65 | 18.47 ± 4.37 | NA | NA | EONS | medium |
| Cetinkaya et al. (2015) (Cetinkaya et al., 2015), Turkey | 50 | 50 | Term | Cohort | 100 | 42/50 | 1/50 | 8.6 ± 3.1 | 19.0 ± 4.8 | 22.2 ± 6.8 | 36.2 ± 1.8 | EONS | medium |
| Dhandai et al. (2018) (Dhandai et al., 2018),India | 60 | 60 | Term | Cohort | 120 | 55/60 | 52/60 | 15.37 ± 10 | 21.37 + 9.53 | 17.87 ± 11.89 | 23.65 ± l (9.55 | LONS | medium |
| Kumar et al. (2019) (Kumar et al., 2019), India | 100 | 100 | Term | Cohort | 200 | 77/100 | 41/100 | NA | NA | NA | NA | EONS | low |
| Ozdemir and Cag (2019) (Ozdemir & Cag, 2019),Turkey | 51 | 56 | Term | Cohort | 107 | 31/51 | 30/56 | 11 ± 5.5 | 13.8 ± 10.6 | 10.8 ± 5.6 | 14.9 ± 10 | LONS | medium |
| Gad et al. (2015) (Gad et al., 2015), Egypt | 30 | 30 | Term | Case–control | 60 | 15/30 | 2/30 | 34.83 ± 18.16 | 93.20 ± 36.12 | NA | NA | EONS | medium |
| Gamal et al. (2017) (Gamal et al., 2017), Egypt | 50 | 30 | Both | Case–control | 80 | NA | NA | 2.56 ± 0.72 | 9.84 ± 0.88 | 17 ± 8.28 | 20.16 ± 8.56 | EONS | medium |
| Tayel et al. (2018) (Tayel et al., 2018), Egypt | 40 | 40 | Term | Case–control | 80 | NA | NA | 8.7 ± 0.7 | 19.1 ± 4.7 | 21.4 ± 4.8 | 36.9 ± 4.2 | EONS | medium |
| Cizmeci et al. (2015) (Cizmeci et al., 2015), Turkey | 40 | 43 | Term | Case–control | 83 | 28/40 | 22/43 | 26.8 ± 18.95 | 40.5 ± 28.25 | NA | NA | EONS | medium |
| Say et al.(2017) (Say et al., 2017), Turkey | 59 | 41 | Preterm | Case–control | 100 | 52/59 | 7/41 | NA | NA | NA | NA | Both | medium |
| Çekmez et al.(2014) (Çekmez et al., 2014),Turkey | 40 | 20 | Term | Case–control | 60 | NA | NA | 49 ± 6.4 | 35 ± 19 | NA | NA | EONS | medium |
| Dinlen et al.(2016) (Dinlen et al., 2016), Turkey | 30 | 30 | Term | Case–control | 60 | 26/30 | 17/30 | NA | NA | NA | NA | LONS | medium |
| El‐Kader et al.(2018) (El‐Kader et al., 2018), Egypt | 25 | 25 | Term | Cohort | 50 | NA | NA | 8.562 ± 2.18 | 28.55 ± 3.046 | 22.3 ± 5.047 | 36.047 ± 1.243 | EONS | medium |
| Mokhtar et al.(2018) (Mokhtar et al., 2018), Egypt | 80 | 80 | Term | Case–control | 160 | 52/80 | 23/80 | NA | NA | NA | NA | EONS | medium |
| Uday et al.(2016) (Uday et al., 2016), India | 39 | 39 | Both | Cohort | 78 | NA | NA | 14.69 ± 4.45 | 26.46 ± 22.01 | NA | NA | ENOS | medium |
| Yang et al.(2016) (Yang et al., 2016), China | 78 | 60 | Term | Case–control | 138 | NA | NA | 10 ± 4 | 14 ± 5 | 24 + 5 | 27 + 5 | EONS | medium |
Y = yes, N = no, U = unclear, NA = not applicable, <60% = low, 60%–80% = medium, >80% = high quality, GA = gestational age, WKS = weeks, Vit.D = vitamin D.
2.6. Summary measures
The primary outcome of this systematic review and meta‐analysis was the weighed mean difference of vitamin D levels among neonates with neonatal sepsis and their sepsis‐free neonate counterparts. The pooled prevalence of vitamin D deficiency among neonates with sepsis and control groups was the second outcome. The vitamin D level was measured from both maternal blood and newborn cord blood. The mean vitamin D levels were reported in ng/ml with standard deviations. Then, mean differences were computed from vitamin D levels of both maternal blood and newborn blood. This was used to verify the association between vitamin D levels and neonatal sepsis among neonates. In this study, cases were neonates with sepsis and the counterpart sepsis‐free neonates were considered the control groups. The pooled estimates were presented with 95% CI. The effect sizes were pooled mean differences of vitamin D levels and the prevalence of vitamin D deficiency among neonates with sepsis and the control groups.
2.7. Assessment of certainty in the findings and data analysis
The extracted data were exported to OpenMeta‐analyst software to compute the pooled prevalence of cord blood vitamin D deficiency. Review Manager Software was used to analyze the effects of maternal blood and cord blood vitamin D levels on neonatal sepsis. Comprehensive meta‐analysis (CMA) version 3.3.070 software was used to identify publication bias. The pooled estimates were presented using forest plot. The I2 test statistic was used to identify heterogeneities between the included studies. The I2 values were interpreted as 25% (low), 50% (medium) and 75% (high) heterogeneity. In this study, heterogeneity was declared and justified when I 2 ≥ 50% with a p‐value of ≤0.05. Subgroup and sensitivity analyses were performed to identify the source of heterogeneity and to minimize it. Besides, fixed and random‐effect models were used alternatively in the analyses. Significant heterogeneity was observed between the studies included in computing pooled estimates. Hence, the DerSimonian and Laird random‐effect model (DerSimonian & Laird, 1986) were used to report the pooled estimates. The presence or absence of neonatal sepsis was considered in the subgroup analysis of vitamin D levels in the two groups. Also, an association between maternal and cord blood vitamin D levels with early‐onset neonatal sepsis (EONS) among term neonates was assessed as part of the subgroup analysis. The funnel plot was checked for asymmetry, and Egger's regression test (p ≤ .05) (Sterne & Egger, 2001) was used for declaring the presence of publication bias.
3. RESULTS
3.1. Selection of eligible studies
4,051 articles were retrieved through electronic searching, and 1,217 studies found from gray literature sources. Out of the total articles, 2016 articles were duplicates and removed accordingly. Using titles and abstracts, 3,252 articles were chosen and 3,202 were excluded due to the fact they were not consistent with the study criteria. Next, full texts of the 50 articles were reviewed for eligibility and 32 studies were excluded due to incomplete or inconsistent outcome and study population. Of the excluded studies, 15 (Abbasian et al., 2016; Belderbos et al., 2011; Boskabadi et al., 2019; Camargo et al., 2011; Gharehbaghi et al., 2018; Karras et al., 2016; Liao et al., 2016; Magnus et al., 2013; Mohamed Hegazy et al., 2018; Nageshu et al., 2016; Panda et al., 2019; Puthuraya et al., 2018; Youssef et al., 2019; Zhang et al., 2019; Zheng et al., 2018) were excluded due to irrelevant/incongruent outcomes and ten studies (Ahmed et al., 2015; Binks et al., 2016; Inamo et al., 2011; Khakshour et al., 2015; Łuczyńska et al., 2014; Mansy et al., 2019; McNally et al., 2009; Mohamed & Al‐Shehri, 2013; Roth et al., 2009; Wayse et al., 2004) were excluded due to differences in study participants. The others were excluded because of incompleteness of the mean or standard(Grant, 2010; Prasad et al., 2018; Pulmano, 2018; Tekgunduz et al., 2015) and the absence of full texts(Das et al., 2016; Saboute et al., 2019; Seliem et al., 2016). Finally, a total of 18 articles (Agrawal et al., 2019; Aye et al., 2018; Çekmez et al., 2014; Cetinkaya et al., 2015; Cizmeci et al., 2015; Dhandai et al., 2018; Dinlen et al., 2016; El‐Kader et al., 2018; Gad et al., 2015; Gamal et al., 2017; Kumar et al., 2019; Mokhtar et al., 2018; Ozdemir & Cag, 2019; Sarwade, 2019; Say et al., 2017; Tayel et al., 2018; Uday et al., 2016; Yang et al., 2016) were included in this systematic review and meta‐analysis (Table 1 and Figure 1).
3.2. Characteristics of the original studies
In the current study, 12 case–control (Agrawal et al., 2019; Aye et al., 2018; Çekmez et al., 2014; Cizmeci et al., 2015; Dinlen et al., 2016; Gad et al., 2015; Gamal et al., 2017; Mokhtar et al., 2018; Sarwade, 2019; Say et al., 2017; Tayel et al., 2018; Yang et al., 2016) and six cohort (Cetinkaya et al., 2015; Dhandai et al., 2018; El‐Kader et al., 2018; Kumar et al., 2019; Ozdemir & Cag, 2019; Uday et al., 2016) studies were included. Out of the included studies, six were from Turkey (Çekmez et al., 2014; Cetinkaya et al., 2015; Cizmeci et al., 2015; Dinlen et al., 2016; Ozdemir & Cag, 2019; Say et al., 2017), 10 studies were from Egypt (El‐Kader et al., 2018; Gad et al., 2015; Gamal et al., 2017; Mokhtar et al., 2018; Tayel et al., 2018) and India (Agrawal et al., 2019; Dhandai et al., 2018; Kumar et al., 2019; Sarwade, 2019; Uday et al., 2016). The rest were conducted in Myanmar (Aye et al., 2018) and China (Yang et al., 2016). Although articles were searched from inception to 2019, articles published from 2014 to 2019 were eligible for the final analysis of this study. Regarding the quality scores of the studies, most had medium quality (Aye et al., 2018; Çekmez et al., 2014; Cetinkaya et al., 2015; Cizmeci et al., 2015; Dhandai et al., 2018; Dinlen et al., 2016; El‐Kader et al., 2018; Gad et al., 2015; Gamal et al., 2017; Mokhtar et al., 2018; Ozdemir & Cag, 2019; Sarwade, 2019; Say et al., 2017; Tayel et al., 2018; Uday et al., 2016; Yang et al., 2016), whereas one was classified under the low (Kumar et al., 2019) and high (Agrawal et al., 2019) quality category each.
3.3. The prevalence of vitamin D deficiency among neonates
In the present study, vitamin D deficiency was declared when cord blood was less than 20ng/ml (Chang & Lee, 2019). Eleven studies (Agrawal et al., 2019; Aye et al., 2018; Cetinkaya et al., 2015; Cizmeci et al., 2015; Dhandai et al., 2018; Dinlen et al., 2016; Gad et al., 2015; Kumar et al., 2019; Mokhtar et al., 2018; Ozdemir & Cag, 2019; Say et al., 2017) were eligible to compute the pooled vitamin D deficiency among neonates with sepsis and the control groups. From the selected studies, vitamin D deficiency among neonates with neonatal sepsis ranged from 50% (Gad et al., 2015) to 98.8% (Aye et al., 2018), whereas vitamin D deficiency among the controls ranged from 2% (Cetinkaya et al., 2015) to 86.7% (Dhandai et al., 2018). In this meta‐analysis, the pooled estimate of vitamin D deficiency among neonates was 61% (95% CI: 44, 77). In the subgroup analysis, 79.4% (95% CI: 71, 87) of neonates with neonatal sepsis and 43.7% (95% CI: 23.4, 63.9) in the control group had vitamin D deficiency. The heterogeneity test for the pooled estimate was significantly high with I2 = 98.9% & p ≤ .001. Subgroup analysis and sensitivity analysis were performed to identify the source of heterogeneity. However, all studies were found to have similar contributions for heterogeneity among the included studies. The pooled estimates were also computed for both random and fixed models. However, there was remarkable heterogeneity among the included studies. Hence, DerSimonian and Laird random‐effect model was used in this analysis (Figure 2).
FIGURE 2.
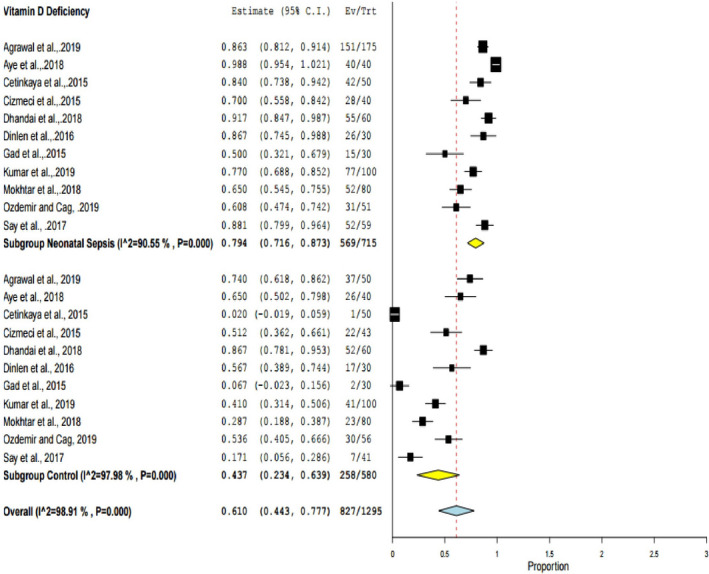
The pooled prevalence of vitamin D deficiency among neonates, 2019
3.4. Effect of maternal Vitamin D Level on Neonatal Sepsis
Seven studies (Cetinkaya et al., 2015; Dhandai et al., 2018; El‐Kader et al., 2018; Gamal et al., 2017; Ozdemir & Cag, 2019; Tayel et al., 2018; Yang et al., 2016) involving 675 participants were included in computing the effect of maternal vitamin D levels on the occurrence of neonatal sepsis. In this study, it was found that there was a significant association between maternal vitamin D levels and neonatal sepsis. Neonates born from mothers having low vitamin D levels were at greater risk of developing neonatal sepsis with a weighed mean difference (MD) of −8.57 ng/ml (95% CI: −13.09, −40.5). The heterogeneity was found to be high (I2 = 96%, p = .000). Due to this, the DerSimonian and Laird random‐effect model was employed in the final report (Figure 3). In addition, the association of maternal vitamin D levels during pregnancy with the incidence of EONS was checked among term newborns using four eligible studies (Cetinkaya et al., 2015; El‐Kader et al., 2018; Tayel et al., 2018; Yang et al., 2016). It was found that the maternal vitamin D level of newborns with ENOS was significantly lower than the vitamin D levels of control groups (MD=−11.55, 95% CI: −17.63, −5.46 ng/ml; I2 = 98% & p ≤ .001) (Figure 4).
FIGURE 3.
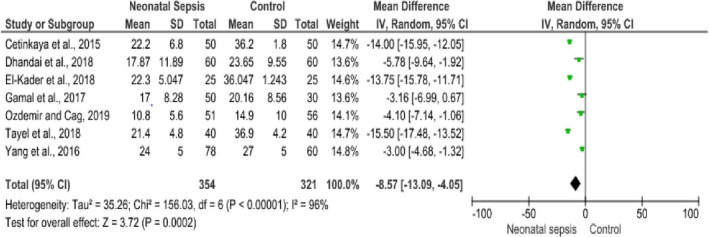
Forest plot showing the association between maternal vitamin D levels with neonatal sepsis, 2019
FIGURE 4.
Forest plot showing the association between maternal vitamin D level and early‐onset neonatal sepsis among term neonates, 2019
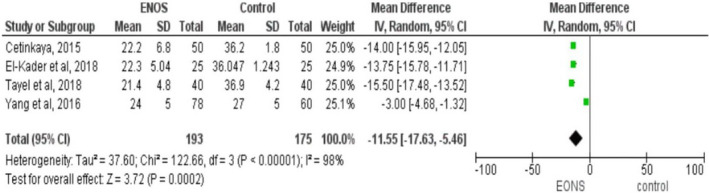
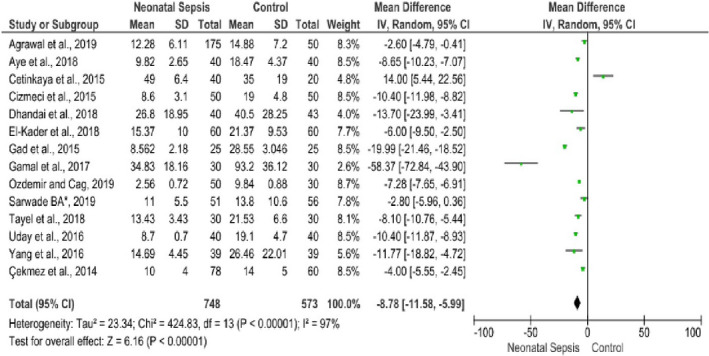
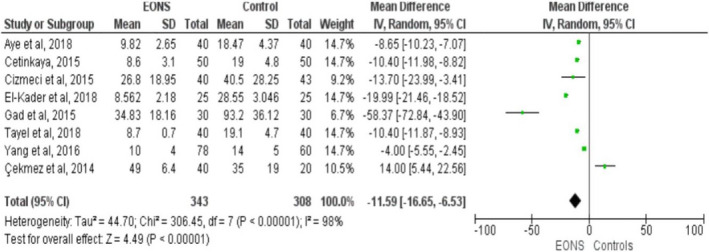
3.5. Effect cord blood vitamin D levels on neonatal sepsis
Fourteen studies reported the relationship of cord blood vitamin D level and neonatal sepsis (Agrawal et al., 2019; Aye et al., 2018; Çekmez et al., 2014; Cetinkaya et al., 2015; Cizmeci et al., 2015; Dhandai et al., 2018; El‐Kader et al., 2018; Gad et al., 2015; Gamal et al., 2017; Ozdemir & Cag, 2019; Sarwade, 2019; Tayel et al., 2018; Uday et al., 2016; Yang et al., 2016) involving 748 neonates with sepsis and 573 controls. From these, thirteen studies (Agrawal et al., 2019; Aye et al., 2018; Çekmez et al., 2014; Cizmeci et al., 2015; Dhandai et al., 2018; El‐Kader et al., 2018; Gad et al., 2015; Gamal et al., 2017; Ozdemir & Cag, 2019; Sarwade, 2019; Tayel et al., 2018; Uday et al., 2016; Yang et al., 2016) revealed that low cord blood vitamin D levels were significantly associated with the incidence of neonatal sepsis. In contrast, one study (Cetinkaya et al., 2015) reported the opposite finding with a weighed mean difference of 14 (95% CI: 5.44, 25.5). The overall finding implied that vitamin D levels in neonates’ cord blood with sepsis were lower than the control groups. The pooled MD was −8.78 ng/ml (95% CI: −11.58, −5.99) with remarkable heterogeneity among the included studies (I2 = 97%, p ≤ .001). Sensitivity and subgroup analyses were conducted to identify the possible sources of heterogeneity among the included studies. Nonetheless, no significant difference was observed in the pooled estimates. Finally, publication bias was checked using a funnel plot (Figure 5). On the inspection of the funnel plot, publication bias was suspected. To confirm the suspicion, Egger's regression test was performed and the result showed publication bias (the intercept (B0) is −11.733, (95% CI: −17.388, −6.078), with t = 4.52, df = 12.000. The p‐value (1‐tailed) was 0.00035, and the p‐value (2‐tailed) was 0.0007). Hence, DerSimonian and Laird random‐effect model was used in computing the final MD (Figure 6). Specifically, the association between cord blood vitamin D levels with EONS in term neonates was assessed using eight studies fulfilling the inclusion criteria (Aye et al., 2018; Çekmez et al., 2014; Cetinkaya et al., 2015; Cizmeci et al., 2015; El‐Kader et al., 2018; Gad et al., 2015; Tayel et al., 2018; Yang et al., 2016). Vitamin D levels in cord blood of term neonates with EONS were significantly lower as compared to neonates free from EONS (MD=−11.59, 95%CI: −16.65, −6.53 ng/ml; I2 = 98% & p ≤ .001) (Figure 7).
FIGURE 5.
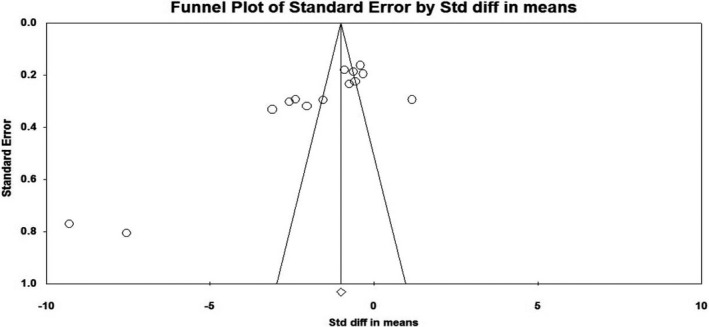
Forest plot showing the association between cord blood Vitamin D levels and neonatal sepsis, 2019
FIGURE 6.
Forest plot showing the association between cord blood vitamin D level and early‐onset neonatal sepsis among term neonates, 2019
FIGURE 7.
Funnel plot showing publication bias of the included studies for the analysis of the effect of cord Vitamin D level on the neonatal sepsis, 2019
4. DISCUSSION
The current systemic review and meta‐analysis presented the pooled prevalence of cord blood vitamin D deficiency and the effect of low maternal and cord vitamin D levels on the occurrence of neonatal sepsis. To generate conclusive evidence in this area, prospective cohort and case–control studies were included. A total of 18 studies have been included to compute the respective pooled estimates. The pooled estimates were presented in the random‐effect model due to the presence of considerable heterogeneity among the included studies. The presence of high heterogeneity could be attributed to differences in the study settings, sample size differences, and discrepancies during the measurement of vitamin D levels by the original studies.
Vitamin D levels during pregnancy and the perinatal period are a crucial factor which determines health outcomes of neonates. According to this study, vitamin D deficiency continues to remains high among neonates without much attention to tackle the problem. The pooled prevalence of vitamin D deficiency is high among neonates and significantly higher among neonates with neonatal sepsis. On the other side, vitamin D deficiency among neonates without neonatal sepsis is confirmed to be low. In the present study, the pooled prevalence of vitamin D deficiency among all neonates was 61%. The prevalence was significantly higher (79.4%) among neonates with sepsis as compared to neonates without sepsis (43.7%). This finding was relatively lower than a study conducted in India, where the prevalence of vitamin D deficiency among neonates with sepsis was 91.7% and 86.7% in the control group (sepsis‐free neonates) (Dhandai et al., 2018). However, these findings are higher than a study conducted in Egypt, where 50% and 6.7% of cases and controls were vitamin D deficient, respectively (Gad et al., 2015). The possible elucidation for the discrepancies could be associated with sample size differences, geospatial variations, and differences in the study setting of the original studies.
In this study, vitamin D levels in the maternal blood and cord blood were significantly associated with neonatal sepsis incidence. So that it is possible to infer that neonates born from mothers having a low vitamin D level are at greater risk of developing neonatal sepsis. Similarly, low levels of vitamin D in newborns’ cord blood were found to have a significant association with neonatal sepsis. Despite this, vitamin D is not part of the standard care of pregnant women in many countries. This is supported by a systematic review and meta‐analysis of four studies on the association between vitamin D levels and neonatal early‐onset sepsis (Lee et al., 2018), which revealed that neonatal sepsis was significantly associated with low vitamin D levels in the maternal blood and cord blood. According to this study, the weighted mean difference in vitamin D levels in neonates with early‐onset sepsis and controls was −7.27 ng/ml (95% CI:‐7.62, 6.92). The weighted mean difference in maternal vitamin D levels of neonates with neonatal sepsis was −7.24 ng/ml (95% CI: −8.45, −6.03). Similarly, another systemic review also supports our finding that vitamin D supplementation decreases respiratory tract infections (OR = 0.582, 95% CI: 0.417,0.812) (Charan et al., 2012). Besides, our finding is supported by a recent meta‐analysis finding which showed a significant association between vitamin D deficiency/lower 25(OH)D levels and sepsis in neonates and children (Xiao et al., 2020). A cohort study conducted in India was also in line with these present findings (Behera et al., 2020). Thus, supplementation of vitamin D during pregnancy can increase the mother and the offspring's vitamin D levels. This could boost the immune system of neonates and can decrease neonatal mortality that might be associated with neonatal sepsis (Bi et al., 2018; Karras et al., 2016).
In this study, the relationship between cord blood and maternal vitamin D levels with EONS among term newborns was also analyzed. The likelihood of EONS in term newborns was found to be significantly associated with low levels of both maternal and cord blood vitamin D. The weighed mean difference between maternal vitamin D levels of term newborns with EONS and controls is −11.55 ng/ml. Likewise, the weighed mean difference between cord blood vitamin D levels in term newborns with EONS and controls is −11.59 ng/ml. The possible elucidation is that vitamin D could prevent bacterial infections due to its’ immunomodulation effects which decrease chemokine production, T‐cell activation, and inhibit dendritic cell activation (Karras et al., 2016). Therefore, we recommend periconceptional supplementation of vitamin D especially in African countries where the magnitude of sepsis in neonates is significantly higher (Belachew & Tewabe, 2020; Seale et al., 2013). The studies included in this meta‐analysis are limited to some countries, and thus, additional primary studies could unfold the strong association of vitamin D deficiency with neonatal sepsis and related neonatal disorders.
4.1. Strengths and Limitations
The strengths of this study were multiple databases were explored, and all possible analyses were done to compute the pooled estimates. To our knowledge, this study is the first of its type in estimating the pooled vitamin D levels in both maternal blood and cord blood by using a relatively large number of studies globally. Thus, these findings will pave the wave to conduct controlled clinical trials in the future. However, this study has limitations such as differences in the units of measurements, incompleteness of the findings, and in some studies, the vitamin D levels were reported with different measures of central tendency. Hence, some studies were excluded due to those discrepancies and this could affect the pooled estimates of this systematic review and meta‐analysis.
5. CONCLUSION
Vitamin D has multiple effects on neonatal health including the prevention of neonatal sepsis. Low levels of vitamin D both in pregnant mothers and in the cord blood of newborns were significantly associated with neonatal sepsis. Specifically, early‐onset neonatal sepsis in term newborns was also associated with low levels of both maternal and cord blood vitamin D. Therefore, it is recommended to supplement vitamin D during pregnancy to decrease sepsis in neonates. To clearly identify the timing, the dosage and mode of vitamin D supplementation, comprehensive randomized controlled trial studies are recommended.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
ETHICS APPROVAL
Not applicable in this study.
Supporting information
Appendix S1
Appendix S2
Appendix S3
ACKNOWLEDGMENT
We would like to address our deepest gratitude to the authors of the included studies for this systematic review and meta‐analysis. Our deepest gratitude also goes to staffs of St. Paul's Hospital Millennium Medical College who gave us technical support.
Workneh Bitew Z, Worku T, Alemu A. Effects of vitamin D on neonatal sepsis: A systematic review and meta‐analysis. Food Sci Nutr.2021;9:375–388. 10.1002/fsn3.2003
Funding information
All costs of this work were covered by the authors.
DATA AVAILABILITY STATEMENT
All important data are included with in the manuscript, and others can be obtained upon request of the corresponding author.
REFERENCES
- Abbasian, M. , Chaman, R. , Amiri, M. , Ajami, M. E. , Jafari‐Koshki, T. , Rohani, H. , & Raei, M. (2016). Vitamin D Deficiency in Pregnant Women and Their Neonates. Global Journal of Health science, 8(9), 54008 10.5539/gjhs.v8n9p83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adatara, P. , Afaya, A. , Salia, S. M. , Afaya, R. A. , Konlan, K. D. , Agyabeng‐Fandoh, E. , … & Boahene, I. G. (2019). Risk Factors Associated with Neonatal Sepsis: A Case Study at a Specialist Hospital in Ghana. The Scientific World Journal, 2019 10.1155/2019/9369051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal, A. , Gupta, A. , & Shrivastava, J. (2019). Role of vitamin‐D deficiency in term neonates with late‐onset sepsis: A case‐control study. Journal of Tropical Pediatrics, 65(6), 609‐616. 10.1093/tropej/fmz021 [DOI] [PubMed] [Google Scholar]
- Ahmed, P. , Babaniyi, I. B. , Yusuf, K. K. , Dodd, C. , Langdon, G. , Steinhoff, M. , & Dawodu, A. (2015). Vitamin D status and hospitalisation for childhood acute lower respiratory tract infections in Nigeria. Paediatrics and International Child Health, 35(2), 151–156. 10.1179/2046905514y.0000000148 [DOI] [PubMed] [Google Scholar]
- Amare, D. , Mela, M. , & Dessie, G. (2019). Unfinished agenda of the neonates in developing countries: Magnitude of neonatal sepsis: Systematic review and meta‐analysis. Heliyon, 5(9), e02519 10.1016/j.heliyon.2019.e02519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aye, A. , Yu, Y. , Khaing, K. , & Wai, L. (2018). Serum vitamin D levels in term neonates with early onset sepsis. Pediatr Neonat Biol, 3(3), 124. [Google Scholar]
- Behera, C. K. , Sahoo, J. P. , Patra, S. D. , & Jena, P. K. (2020). Is Lower Vitamin D Level Associated with Increased Risk of Neonatal Sepsis? A Prospective Cohort Study. Indian Journal of Pediatrics, 87(6), 427–432. 10.1007/s12098-020-03188-0 [DOI] [PubMed] [Google Scholar]
- Belachew, A. , & Tewabe, T. (2020). Neonatal sepsis and its association with birth weight and gestational age among admitted neonates in Ethiopia: Systematic review and meta‐analysis. BMC Pediatrics, 20(1), 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belderbos, M. E. , Houben, M. L. , Wilbrink, B. , Lentjes, E. , Bloemen, E. M. , Kimpen, J. L. , & Bont, L. (2011). Cord blood vitamin D deficiency is associated with respiratory syncytial virus bronchiolitis. Pediatrics, 127(6), e1513–e1520. [DOI] [PubMed] [Google Scholar]
- Belur, J. , Tompson, L. , Thornton, A. , & Simon, M. (2018). Interrater reliability in systematic review methodology: Exploring variation in coder decision‐making. Sociological Methods & Research, 20(10), 1–29. [Google Scholar]
- Bi, W. G. , Nuyt, A. M. , Weiler, H. , Leduc, L. , Santamaria, C. , & Wei, S. Q. (2018). Association between vitamin D supplementation during pregnancy and offspring growth, morbidity, and mortality: A systematic review and meta‐analysis. JAMA Pediatrics, 172(7), 635–645. 10.1001/jamapediatrics.2018.0302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binks, M. J. , Smith‐Vaughan, H. C. , Marsh, R. , Chang, A. B. , & Andrews, R. M. (2016). Cord blood vitamin D and the risk of acute lower respiratory infection in Indigenous infants in the Northern Territory. Medical Journal of Australia, 204(6), 238 10.5694/mja15.00798 [DOI] [PubMed] [Google Scholar]
- Black, R. E. , Laxminarayan, R. , Temmerman, M. , & Walker, N. (2016). Reproductive maternal newborn and child health. Disease control priorities (vol 2). [PubMed] [Google Scholar]
- Boskabadi, H. , Maamouri, G. , Hemmatipour, A. , Parvini, Z. , Ramazani, A. , & Bagheri, F. (2019). Comparison of serum vitamin D in the umbilical cord of survived with not survived premature infants. Iran Journal of Pediatrics, 29(3), 10.5812/ijp.84798 [DOI] [Google Scholar]
- Camargo, C. A. Jr , Ingham, T. , Wickens, K. , Thadhani, R. , Silvers, K. M. , Epton, M. J. , & Crane, J. (2011). Cord‐blood 25‐hydroxyvitamin D levels and risk of respiratory infection, wheezing, and asthma. Pediatrics, 127(1), e180–e187. 10.1542/peds.2010-0442 [DOI] [PubMed] [Google Scholar]
- Çekmez, F. , Aydemir, G. , Yildirim, Ş. , Bulut, Ö. , Tunç, T. , Kul, M. , & Çoban, A. (2014). Diagnostic value of 25‐hydroxyvitamin D level and new cytokines in neonatal sepsis. European Journal of Inflammation, 12(2), 297–304. 10.1177/1721727X1401200209 [DOI] [Google Scholar]
- Cetinkaya, M. , Cekmez, F. , Buyukkale, G. , Erener‐Ercan, T. , Demir, F. , Tunc, T. , & Aydemir, G. (2015). Lower vitamin D levels are associated with increased risk of early‐onset neonatal sepsis in term infants. Journal of Perinatology, 35(1), 39–45. 10.1038/jp.2014.146 [DOI] [PubMed] [Google Scholar]
- Chang, S.‐W. , & Lee, H.‐C. (2019). Vitamin D and health‐The missing vitamin in humans. Pediatrics & Neonatology, 60(3), 237–244. [DOI] [PubMed] [Google Scholar]
- Charan, J. , Goyal, J. P. , Saxena, D. , & Yadav, P. (2012). Vitamin D for prevention of respiratory tract infections: A systematic review and meta‐analysis. Journal of Pharmacology and Pharmacotherapeutics, 3(4), 300–303. 10.4103/0976-500X.103685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cizmeci, M. N. , Kanburoglu, M. K. , Akelma, A. Z. , Ayyildiz, A. , Kutukoglu, I. , Malli, D. D. , & Tatli, M. M. (2015). Cord‐blood 25‐hydroxyvitamin D levels and risk of early‐onset neonatal sepsis: A case–control study from a tertiary care center in Turkey. European Journal of Pediatrics, 174(6), 809–815. [DOI] [PubMed] [Google Scholar]
- Clancy, N. , Onwuneme, C. , Carroll, A. , McCarthy, R. , McKenna, M. , Murphy, N. , & Molloy, E. (2013). Vitamin D and neonatal immune function. The Journal of Maternal‐Fetal & Neonatal Medicine, 26(7), 639–646. [DOI] [PubMed] [Google Scholar]
- Cooper, P. A. (2014). The challenge of reducing neonatal mortality in low‐and middle‐income countries. Pediatrics, 133(1), 4–6. [DOI] [PubMed] [Google Scholar]
- Das, B. , Patra, S. , Behera, C. , & Suar, M. (2016). Genotyping of vitamin D receptor gene polymorphisms using mismatched amplification mutation assay in neonatal sepsis patients of Odisha, eastern India. Infection, Genetics and Evolution, 45, 40–47. 10.1016/j.meegid.2016.08.013 [DOI] [PubMed] [Google Scholar]
- de Oliveira, C. O. P. , Souza, J. R. S. , Machado, R. C. , Feijão, A. R. , & de Souza, N. L. (2016). Risk factors for neonatal sepsis in neonatal intensive care unit: Evidence study. Cogitare Enferm, 21(2), 1–9. [Google Scholar]
- DerSimonian, R. , & Laird, N. (1986). Meta‐analysis in clinical trials. Controlled Clinical Trials, 7(3), 177–188. [DOI] [PubMed] [Google Scholar]
- Dhandai, R. , Jajoo, M. , Singh, A. , Mandal, A. , & Jain, R. (2018). Association of vitamin D deficiency with an increased risk of late‐onset neonatal sepsis. Paediatrics and International Child Health, 38(3), 193–197. 10.1080/20469047.2018.1477388 [DOI] [PubMed] [Google Scholar]
- Dinlen, N. , Zenciroglu, A. , Beken, S. , Dursun, A. , Dilli, D. , & Okumus, N. (2016). Association of vitamin D deficiency with acute lower respiratory tract infections in newborns. Expanded Journal of Maternal‐Fetal & Neonatal Medicine, 29(6), 928–932. 10.3109/14767058.2015.1023710 [DOI] [PubMed] [Google Scholar]
- El‐Kader, M. A. A. , El‐Azab, G. A. E. K. , & El‐Rifaey, S. M. (2018). Relation between vitamin D level and some inflammatory cytokines in full‐term newborns with early onset sepsis. International Journal of Pharmaceutical Sciences Review and Research, 49(2), 64–70. [Google Scholar]
- Fleischmann‐Struzek, C. , Goldfarb, D. M. , Schlattmann, P. , Schlapbach, L. J. , Reinhart, K. , & Kissoon, N. (2018). The global burden of paediatric and neonatal sepsis: A systematic review. The Lancet Respiratory Medicine, 6(3), 223–230. 10.1016/s2213-2600(18)30063-8 [DOI] [PubMed] [Google Scholar]
- Gad, G. I. , Abushady, N. M. , Fathi, M. S. , & Elsaadany, W. (2015). Diagnostic value of anti‐microbial peptide, cathelicidin in congenital pneumonia. Journal of Maternal‐Fetal & Neonatal Medicine, 28(18), 2197–2200. 10.3109/14767058.2014.981806 [DOI] [PubMed] [Google Scholar]
- Gamal, T. , Madiha, A.‐A. , Hanan, M. , Abdel‐Azeem, M. , & Marian, G. (2017). Neonatal and maternal 25‐OH vitamin D serum levels in neonates with early‐onset sepsis. Children, 4(5), 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gharehbaghi, M. , Ghergherechi, R. , & Karimi, B. (2018). Vitamin D deficiency and lower respiratory tract infections in Newborn infants. Hong Kong Journal of Paediatrics, 23(1), 20–24. [Google Scholar]
- Grant, W. B. (2010). Vitamin D supplementation of mother and infant could reduce risk of sepsis in premature infants. Early Human Development, 86(2), 133 10.1016/j.earlhumdev.2010.02.003 [DOI] [PubMed] [Google Scholar]
- Hammad, E. , & Zainab, M. (2018). Meta‐analysis on factors influencing early onset neonatal sepsis. Scholar Journal of Applied Sciences and Research, 1(8), 20–22. [Google Scholar]
- Hug, L. , Alexander, M. , You, D. , & Alkema, L. (2019). National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario‐based projections to 2030: A systematic analysis. Lancet Glob Health, 7(6), e710–e720. 10.1016/s2214-109x(19)30163-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inamo, Y. , Hasegawa, M. , Saito, K. , Hayashi, R. , Ishikawa, T. , Yoshino, Y. , & Fuchigami, T. (2011). Serum vitamin D concentrations and associated severity of acute lower respiratory tract infections in Japanese hospitalized children. Pediatrics International, 53(2), 199–201. [DOI] [PubMed] [Google Scholar]
- Karras, S. N. , Fakhoury, H. , Muscogiuri, G. , Grant, W. B. , van den Ouweland, J. M. , Colao, A. M. , & Kotsa, K. (2016). Maternal vitamin D levels during pregnancy and neonatal health: Evidence to date and clinical implications. Therapeutic Advances in Musculoskeletal Disease, 8(4), 124–135. 10.1177/1759720X16656810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khakshour, A. , Farhat, A. S. , Mohammadzadeh, A. , Zadeh, F. K. , & Kamali, H. (2015). The association between 25‐dehydroxy vitamin D and lower respiratory infection in children aged less than "5" years in Imam Reza hospital, Bojnurd, Iran. Journal of Pakistan Medical Association, 65(11), 1153–1155. [PubMed] [Google Scholar]
- Khuri‐Bulos, N. , Lang, R. D. , Blevins, M. , Kudyba, K. , Lawrence, L. , Davidson, M. , & Halasa, N. B. (2014). Vitamin D deficiency among newborns in Amman, Jordan. Global Journal of Health Science, 6(1), 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, A. , Narang, G. S. , Singh, G. , & Virk, N. (2019). Association of vitamin D deficiency with early onset sepsis in term neonates. International Journal of Contemporary Pediatrics, 6(2), 440–444. 10.18203/2349-3291.ijcp20190500 [DOI] [Google Scholar]
- Laxminarayan, R. , Matsoso, P. , Pant, S. , Brower, C. , Røttingen, J.‐A. , Klugman, K. , & Davies, S. (2016). Access to effective antimicrobials: A worldwide challenge. The Lancet, 387(10014), 168–175. [DOI] [PubMed] [Google Scholar]
- Lee, S. Y. , Kim, H. E. , & An, S. H. (2018). The Association between Vitamin D Levels and Neonatal Early‐onset Sepsis : A Systematic Review and Meta‐analysis. Korean Journal of Clinical Pharmacy, 28(1), 10–16. 10.24304/kjcp.2018.28.1.10 [DOI] [Google Scholar]
- Liao, S. L. , Lai, S. H. , Tsai, M. H. , Hua, M. C. , Yeh, K. W. , Su, K. W. , & Huang, J. L. (2016). Maternal Vitamin D Level Is Associated with Viral Toll‐Like Receptor Triggered IL‐10 Response but Not the Risk of Infectious Diseases in Infancy. Mediators of Inflammation, 2016, 8175898 10.1155/2016/8175898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, L. , Oza, S. , Hogan, D. , Perin, J. , Rudan, I. , Lawn, J. E. , & Black, R. E. (2015). Global, regional, and national causes of child mortality in 2000–13, with projections to inform post‐2015 priorities: An updated systematic analysis. The Lancet, 385(9966), 430–440. [DOI] [PubMed] [Google Scholar]
- Łuczyńska, A. , Logan, C. , Nieters, A. , Elgizouli, M. , Schöttker, B. , Brenner, H. , & Rothenbacher, D. (2014). Cord blood 25(OH)D levels and the subsequent risk of lower respiratory tract infections in early childhood: The Ulm birth cohort. European Journal of Epidemiology, 29(8), 585–594. [DOI] [PubMed] [Google Scholar]
- Magnus, M. C. , Stene, L. C. , Håberg, S. E. , Nafstad, P. , Stigum, H. , London, S. J. , & Nystad, W. (2013). Prospective Study of Maternal Mid‐pregnancy 25‐hydroxyvitamin D Level and Early Childhood Respiratory Disorders. PPE Paediatric and Perinatal Epidemiology, 27(6), 532–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansy, W. , Ibrahim, N. H. , Al‐Gawhary, S. , Alsubaie, S. S. , Abouelkheir, M. M. , Fatani, A. , & Zakaria, E. A. (2019). Vitamin D status and vitamin D receptor gene polymorphism in Saudi children with acute lower respiratory tract infection. Molecular Biology Reports, 46(2), 1955–1962. 10.1007/s11033-019-04645-6 [DOI] [PubMed] [Google Scholar]
- McCarthy, R. , McCallion, N. , Harrison, G. , & Molloy, E. (2009). Relationship between vitamin D and alkaline phosphatase in very‐low‐birthweight infants. Archives of Disease in Childhood‐Fetal and Neonatal Edition, 94(1), F77–F78. [DOI] [PubMed] [Google Scholar]
- McNally, J. D. , Leis, K. , Matheson, L. A. , Karuananyake, C. , Sankaran, K. , & Rosenberg, A. M. (2009). Vitamin D deficiency in young children with severe acute lower respiratory infection. Pediatric Pulmonology, 44(10), 981–988. 10.1002/ppul.21089 [DOI] [PubMed] [Google Scholar]
- Mohamed Hegazy, A. , Mohamed Shinkar, D. , Refaat Mohamed, N. , & Abdalla Gaber, H. (2018). Association between serum 25 (OH) vitamin D level at birth and respiratory morbidities among preterm neonates. The Journal of Maternal‐Fetal & Neonatal Medicine, 31(20), 2649–2655. [DOI] [PubMed] [Google Scholar]
- Mohamed, W. A. , & Al‐Shehri, M. A. (2013). Cord blood 25‐hydroxyvitamin D levels and the risk of acute lower respiratory tract infection in early childhood. Journal of Tropical Pediatrics, 59(1), 29–35. 10.1093/tropej/fms042 [DOI] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269. [DOI] [PubMed] [Google Scholar]
- Mokhtar, W. A. , Mohamed, A. F. , Allam, R. M. , Zidan, N. I. , Mokhtar, G. A. , Malek, M. M. , & Hamed, M. S. (2018). Vitamin D deficiency and vitamin D receptor gene polymorphisms as a risk factor for severe early‐onset neonatal sepsis. Alexandria Journal of Pediatrics, 31(2), 82. [Google Scholar]
- Moraga, P. , & Collaborators, G. C. o. D. (2017). Global, regional, and national age‐sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 390(10100), 1151–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugadza, G. , Zvinavashe, M. , Gumbo, F. Z. , & Pedersen, B. S. (2017). Early breastfeeding initiation and incidence of neonatal sepsis in Chipinge District Zimbabwe. International Journal of Contemporary Pediatrics, 5(1), 1 10.18203/2349-3291.ijcp20175564 [DOI] [Google Scholar]
- Munn, Z. , Moola, S. , Lisy, K. , Riitano, D. , & Tufanaru, C. (2015). Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. International Journal of Evidence‐Based Healthcare, 13, 147–153. [DOI] [PubMed] [Google Scholar]
- Murthy, S. , Godinho, M. A. , Guddattu, V. , Lewis, L. E. S. , & Nair, N. S. (2019). Risk factors of neonatal sepsis in India: A systematic review and meta‐analysis. PLoS One, 14(4), e0215683 10.1371/journal.pone.0215683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nageshu, S. , Krishna, K. L. K. , Bhat, B. , Suma, H. , & Reddy, S. (2016). A study of prevalence of Vitamin D deficiency among pregnant women and its impact on feto maternal outcome. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 5(4), 1174–1180, 10.18203/2320-1770.ijrcog20160880 [DOI] [Google Scholar]
- Ozdemir, A. A. , & Cag, Y. (2019). Neonatal Vitamin D status and the risk of neonatal sepsis. Pakistan Journal of Medical, 35(2), 420–425. 10.12669/pjms.35.2.342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda, M. , McIntosh, J. , Chaudhari, T. , & Kent, A. L. (2019). Do Maternal Vitamin D Levels Influence Vitamin D Levels in Preterm Neonates? International Journal of Pediatric, 2019, 8613414 10.1155/2019/8613414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad, R. , Shanataram, B. , Kiran, B. , & Dsa, S. (2018). Vitamin d levels in late pre‐term neonates and its association with sepsis. Indian Journal of Public Health Research and Development, 9(10), 128–132. 10.5958/0976-5506.2018.01327.X [DOI] [Google Scholar]
- Pulmano, C. B. (2018). Association of breastfeeding practices and selected clinical outcomes of patients aged 3 months to 2 years old diagnosed with pcap c in a tertiary government hospital in manila from January 2013‐ January 2016. Pediatrics & Therapeutics, 8, 10.4172/2161-0665-c2-055 [DOI] [Google Scholar]
- Puthuraya, S. , Karnati, S. , Kazzi, S. N. J. , Qureshi, F. , Jacques, S. M. , & Thomas, R. (2018). Does vitamin D deficiency affect placental inflammation or infections among very low birth weight infants? The Journal of Maternal‐Fetal & Neonatal Medicine, 31(14), 1906–1912. [DOI] [PubMed] [Google Scholar]
- Roth, D. E. , Jones, A. B. , Prosser, C. , Robinson, J. L. , & Vohra, S. (2009). Vitamin D status is not associated with the risk of hospitalization for acute bronchiolitis in early childhood. European Journal of Clinical Nutrition, 63(2), 297–299. 10.1038/sj.ejcn.1602946 [DOI] [PubMed] [Google Scholar]
- Rudd, K. E. , Johnson, S. C. , Agesa, K. M. , Shackelford, K. A. , Tsoi, D. , Kievlan, D. R. , & Naghavi, M. (2020). Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. The Lancet, 395(10219), 200–211. 10.1016/S0140-6736(19)32989-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saboute, M. , Yavar, R. , Kashaki, M. , Khaledi, F. K. , Khalesi, N. , & Rohani, F. (2019). Investigation of association between maternal 25‐OH vitamin D serum levels and neonatal early onset sepsis in newborns by evaluating key factors. Lipids in Health and Disease, 18(1), 153 10.1186/s12944-019-1095-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarwade, B. A. (2019). Vitamin D levels in early onset neonatal sepsis without maternal risk factors: A case‐control study. Vitam Miner, 8(2), 1000183. [Google Scholar]
- Say, B. , Uras, N. , Sahin, S. , Degirmencioglu, H. , Oguz, S. S. , & Canpolat, F. E. (2017). Effects of cord blood vitamin D levels on the risk of neonatal sepsis in premature infants. Korean Journal of Pediatrics, 60(8), 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seale, A. C. , Blencowe, H. , Zaidi, A. , Ganatra, H. , Syed, S. , Engmann, C. , & Cousens, S. N. (2013). Neonatal severe bacterial infection impairment estimates in South Asia, sub‐Saharan Africa, and Latin America for 2010. Pediatric Research, 74(S1), 73–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seliem, M. S. , Abdel Haie, O. M. , Mansour, A. I. , & Salama, S. S. M. E. (2016). The relation between vitamin D level and increased risk for early‐onset neonatal sepsis in full‐term infants. Medical Research Journal, 15(1), 16–21. [Google Scholar]
- Sterne, J. A. , & Egger, M. (2001). Funnel plots for detecting bias in meta‐analysis: Guidelines on choice of axis. Journal of Clinical Epidemiology, 54(10), 1046–1055. [DOI] [PubMed] [Google Scholar]
- Swai, R. O. , Matee, M. I. , Killewo, J. , Lyamuya, E. F. , Kwesigabo, G. , Tulli, T. , & Ndayongeje, J. (2006). Surveillance of HIV and syphilis infections among antenatal clinic attendees in Tanzania‐2003/2004. BMC Public Health, 6(1), 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tayel, S. I. , Soliman, S. E. , & Elsayed, H. M. (2018). Vitamin D deficiency and vitamin D receptor variants in mothers and their neonates are risk factors for neonatal sepsis. Steroids, 134, 37–42. 10.1016/j.steroids.2018.03.003 [DOI] [PubMed] [Google Scholar]
- Tekgunduz, K. S. , Alp, H. , & Akkar, M. K. (2015). Is vitamin D deficiency alone sufficient to increase the incidence of neonatal sepsis? European Journal of Pediatrics, 174(6), 817–818. 10.1007/s00431-014-2486-0 [DOI] [PubMed] [Google Scholar]
- Thorne‐Lyman, A. , & Fawzi, W. W. (2012). Vitamin D during pregnancy and maternal, neonatal and infant health outcomes: A systematic review and meta‐analysis. Paediatric and Perinatal Epidemiology, 26(Suppl 1), 75–90. 10.1111/j.1365-3016.2012.01283.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uday, K. , Ashwin, K. , & Srinivas, G. (2016). Association between vitamin D levels and early onset sepsis in infants: A prospective observational study. International Journal of Contemporary Pediatrics, 3(4), 1189–1192. [Google Scholar]
- Wayse, V. , Yousafzai, A. , Mogale, K. , & Filteau, S. (2004). Association of subclinical vitamin D deficiency with severe acute lower respiratory infection in Indian children under 5 y. European Journal of Clinical Nutrition, 58(4), 563–567. 10.1038/sj.ejcn.1601845 [DOI] [PubMed] [Google Scholar]
- Xiao, D. , Zhang, X. , Ying, J. , Zhou, Y. , Li, X. , Mu, D. , & Qu, Y. (2020). Association between vitamin D status and sepsis in children: A meta‐analysis of observational studies. Clinical Nutrition, 39(6), 1735–1741. 10.1016/j.clnu.2019.08.010 [DOI] [PubMed] [Google Scholar]
- Yang, L. R. , Li, H. , Yang, T. Y. , Zhang, T. , & Zhao, R. C. (2016). Relationship between vitamin D deficiency and early‐onset neonatal sepsis. Zhongguo Dang Dai Er Ke Za Zhi, 18(9), 791–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- You, D. , Hug, L. , Ejdemyr, S. , & Beise, J. (2015). Levels and trends in child mortality. Estimates developed by the UN Inter‐agency Group for Child Mortality Estimation (IGME). Report 2015. [Google Scholar]
- Youssef, M. A. M. , Zahran, A. M. , Hussien, A. M. , Elsayh, K. I. , Askar, E. A. , & Farghaly, H. S. (2019). In neonates with vitamin D deficiency, low lymphocyte activation markers are risk factors for infection. Paediatrics and international child health, 39(2), 111–118. 10.1080/20469047.2018.1528755 [DOI] [PubMed] [Google Scholar]
- Zhang, Q. , Chen, H. , Wang, Y. , Zhang, C. , Tang, Z. , Li, H. , Liu, Z. (2019). Severe vitamin D deficiency in the first trimester is associated with placental inflammation in high‐risk singleton pregnancy. Clinical Nutrition, 38(4), 1921–1926. [DOI] [PubMed] [Google Scholar]
- Zheng, G. , Pan, M. , Li, Z. , Xiang, W. , & Jin, W. (2018). Effects of vitamin D on apoptosis of T‐lymphocyte subsets in neonatal sepsis. Experimental and Therapeutic Medicine, 16(2), 629–634. 10.3892/etm.2018.6215 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Appendix S2
Appendix S3
Data Availability Statement
All important data are included with in the manuscript, and others can be obtained upon request of the corresponding author.


