Abstract
Background and aims
Probiotics can support the body’s systems in fighting viral infections. This review is aimed to focus current knowledge about the use of probiotics as adjuvant therapy for COVID-19 patients.
Methods
We performed an extensive research using the PubMed-LitCovid, Cochrane Library, Embase databases, and conducting manual searches on Google Scholar, Elsevier Connect, Web of Science about this issue.
Results
We have found several papers reporting data about the potential role of probiotics as well as contrasting experimental data about it.
Conclusions
Most data show good results demonstrating that probiotics can play a significant role in fighting SARS-CoV-2 infection, also compared with their use in the past for various diseases. They seem effective in lowering inflammatory status, moreover in patients with chronic comorbidities such as cancer and diabetes, improving clinical outcomes.
Keywords: SARS-Cov-2, Human microbiota, Dysbiosis, Probiotics, Pharmacological effects
1. Introduction
A beneficial association of microorganisms in the human body was first established by Döderlein in 1892. Then, bacteria from fermented milk products have been tested for their health-promoting properties by Metchnikoff in 1908. Much progress has been made in microbiology with technological advances, especially regarding genetic analysis. In 2001, the Nobel laureate Joshua Lederberg introduced the term “microbiome”, including the entire genetic patrimony of all living microorganisms in the human body (gastrointestinal system, skin, respiratory system, urogenital system etc.). Instead, the term “microbiota” refers to the specific and unique composition (genera/species) of this microbial population, differs from one person to another, and influences human health (Table 1 ) [[1], [2], [3]]. While the microbiota remains largely unchanged throughout life and very similar between two individuals, microbiome constantly changes and differs significantly between individuals, even if they are homozygous twins. Hence, microbiome has its own biological importance and should be studied as a part of the entire human genome [1,2].
Table 1.
Main bacterial composition of the human microbiota in the various body areas. It is noted that the Bacteroides are present in airways, mouth and gastrointestinal tract, instead Firmicutes is present in all.
|
Prevailing Bacteria | |
|---|---|
| Body sites | Phyla |
| Skin | Actinobacteria, Firmicutes, Proteobacteria |
| Oral | Bacteroides,Firmicutes,Fusobacteria,Proteobacteria |
| Airways | Bacteroides, Firmicutes, Proteobacteria |
| Gastrointestinal | Bacteroides, Firmicutes, Actinobacteria |
| Urogenital | Firmicutes |
To understand the central relationship between microbes and the human body many investigations have been made, particularly for a better comprehension of its role in human health. In 2008, an international project, the so called “Human Microbiome Project”, was designed by the US National Institutes of Health (NIH) [1,3].
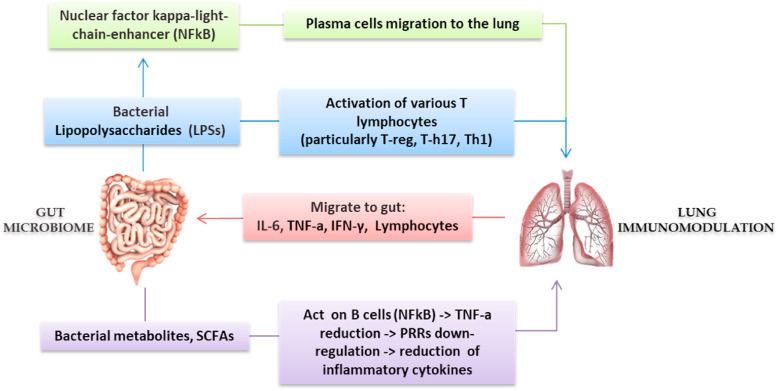
Human microbiome must be considered as a “metabolic system” that interacts with the host and performs many necessary functions for human health. Continuous and reciprocal relationships (crosstalk) between the host and all the microbiota sites define several axes, such as the gut/lung or gut/brain or gut/skin. For instance, through the mesenteric lymphatic system, intact bacteria and their metabolites enter the systemic circulation and influence the pulmonary immune response (gut/lung axis). Through this way intestinal metabolites, mainly produced by bacterial fermentation of dietary fiber, such as short-chain fatty acids (SCFAs), significantly influence local gut immunity but also distant organs. SCFAs derived from gut are able to suppress lung inflammation [[4], [5], [6], [7], [8]]. Dendritic cells (DCs), the antigen-presenting cells of the mammalian immune system, stimulate T-cells subpopulations in mesenteric lymph nodes and gut lymphatic tissue to produce regulatory cytokines. After airways immune-stimulation, these T-cells move from the gut to the respiratory system, providing protection and stimulating an anti-inflammatory response In fact, gut microbiota rebalancing has been shown to reduce ventilator-associated enteritis and pneumonia [4,7,9].
Opposite to the healthy condition of eubiosis is the so called dysbiosis. The altered bacterial balance causes the translocation of cytokines, endotoxins and microbial metabolites in the general circulation to other organs, such as the lung. Conversely, respiratory inflammation (due to many causes, e.g., respiratory viral infections due to SARS-CoV-2), causes local dysbiosis and, in turn, the translocation of microbial metabolites and toxins to other organs, such as the gut (Fig. 1 ). Physiological changes in the human microbiota with age leads to a “physiological dysbiosis”, with less diversification in microbial composition, aggravated in case of comorbidity (hypertension, diabetes, chronic inflammatory bowel diseases, etc.) [[9], [10], [11]]. Therefore, to establish the condition of eubiosis, “good” bacteria are required. The concept of probiotics as a food with positive effects was firstly used by Parker RB in 1974 and then recognized by the Food and Agriculture Organization (FAO), and more recently by the Word Health Organization (WHO) [4,7,11].
Fig. 1.
Gut/Lung axis: the hypothesis that the intestinal microbiota can modulate the immunological activity of the lung and vice versa: Lipopolysaccharides (LPSs) promote the activation of nuclear factor kappa-light chain-enhancer (NFkb) and plasma cells with various T cells, in particular regulatory T or suppressor T cells (Treg cells), T helper 17 (T-h17), T helper 1 (Th1) migrating later to the lung through the bloodstream. The bacterial metabolites, in particular short chain fatty acids (SCFAs) act directly on the nuclear factor kappa-light-chain-enhancer of activated B cells (NFkB), reducing production of tumor necrosis factor alpha (TNF-α) and the downregulation of the pattern recognition receptors (PRRs). This will lead to the reduction of the inflammatory cytokines and lung immunomodulation. Then, interleukin-6 (IL-6), tumor necrosis factor alpha (TNF-α), interferon gamma (IFNγ) and lymphocytes migrate to the gut .
On December 31, 2019, a novel Coronavirus strain was reported in Wuhan, China, subsequently identified as a new Coronavirus beta strain ß-CoV from Group 2B, with a genetic similarity of approximately 70% to SARS-CoV. It was denominated “Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)”, which is the cause of COVID-19, the pandemic ongoing till date. On December 20, 2020, more than 50-million SARS-Cov-2 infections have been confirmed worldwide. Our efforts are to investigate alternative/supporting therapeutic remedies in the fighting against this virus. Particularly, we think that SARS-CoV-2 infection course could influenced by many factors, including intestinal dysbiosis. In this document we analyze available data on the association between SARS-CoV-2 and human microbiota [12,13].
2. The SARS-CoV-2 action on microbiota
COVID-19 symptoms are on average non-specific, especially in children and young adults. Fever, body aches, nasal congestion, dry cough and sore throat are the most frequent. About 5–10% of patients suffer from gastrointestinal symptoms (nausea, vomiting, diarrhea, abdominal pain). Less frequent symptoms are hyposmia or anosmia, ageusia, neurological symptoms (encephalopathy and encephalitis), cerebrovascular events (ischemic stroke, intracerebral hemorrhages, and more), neuropsychiatric symptoms (psychosis, dementia, affective disorders etc.) and skin manifestations (maculo-papular or papulovesicular rash, urticarious lesions, livedo reticularis) [[14], [15], [16], [17]]. Furthermore, patients with oncologic and metabolic disorders may experience worse clinical course.
SARS-CoV-2 pro-inflammatory response can cause a pulmonary hyper-inflammatory scenario, leading to acute respiratory distress syndrome (ARDS) and diffused alveolar destruction (DAD) [15,[18], [19], [20]]. It damages bronchiolar structures and disrupts surfactant, the protective film produced by type II pneumocytes [15,18,19]. The structural protein SARS-CoV-2 spike (S) binds the angiotensin converting enzyme 2 receptor on human cells (ACE2), using it as a “gateway” to penetrate the cell and to replicate. This receptor is expressed on endothelial cells, on airways epithelial cells, but also on intestinal cells. ACE2 is one of the central enzymes in the renin-angiotensin system (RAS) that regulates blood pressure, fluid and electrolyte balance, but also vascular local and systemic resistances.
In the lungs, local RAS activation contributes to lung damage throughout multiple mechanisms, such as increasing permeability and causing alveolar epithelial alterations. The cascade starts with the activation of the renin, which cleaves angiotensinogen generating angiotensin I (Ang-I, decapeptide hormone, inactive). The ACE converts angiotensin I to angiotensin II (Ang II, an octapeptide hormone, active). This exerts vasoactive effects by binding two types of receptors, AT1 and AT2 [14,18,21]. ACE2 is present in the gut, so this must make us aware of its possible involvement in the pathophysiology of the disease. It physiologically contributes to regulating amino acid transports. When its activity is altered, a decrease in tryptophan occurs which leads to a reduction in the activity of the mTOR (mammalian target of rapamycin) pathway, causing an altered expression of antimicrobial peptides on Paneth’s intestinal cells. This alteration modifies the composition of the intestinal microbiota, both qualitatively and quantitatively. In turn, this influences the gut/lung crosstalk [14,18,[21], [22], [23], [24]].
In various pathological situations, such as that of SARS-Cov-2 infection, the loss of equilibrium between IL-10 and IL-17 has been observed. In fact, one of the main pathogenic mechanisms causing pulmonary acute damage is the “cytokine storm”. IL-6 is one of the main pro-inflammatory markers in this sense [9,18,24,25].
Since the presence of gastrointestinal symptoms, in many cases in those with a severe prognosis, we can hypothesize that SARS-Cov-2 interacts with the gut microbiota via the gut/lung axis. Contemporary, we believe it could be responsible of neuropsychiatric and cutaneous manifestations through the gut/brain and gut/skin, and skin/brain axes [8,12]. SCAFs are able to inhibit the myelin synthesis in the prefrontal cortex, inhibiting the action of the transcription factor Sox10 in oligodendrocytes. Myelin loss is associated with anxiety, depression, and decreased sociability. Perhaps this is a probable explanation for the neuropsychiatric manifestations [18,26,27].
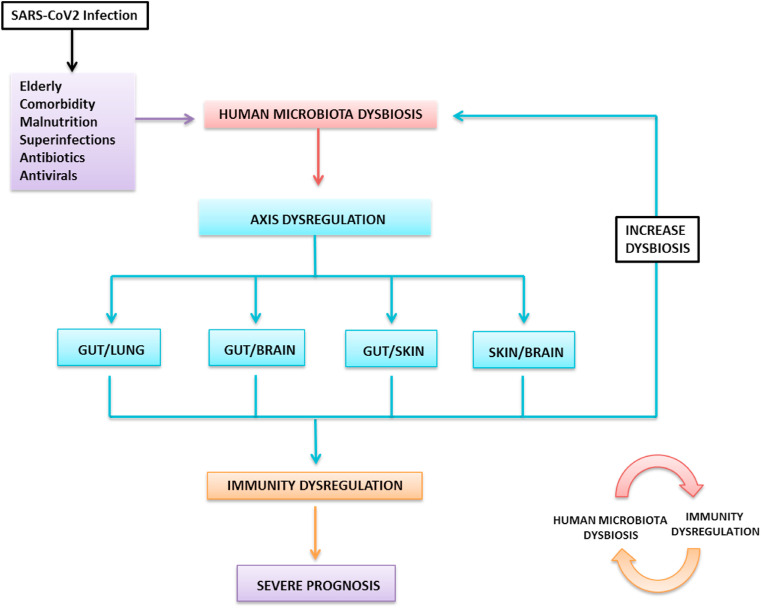
In the setting of COVID-19, it is also important to consider that antibiotics and antivirals are often given to patients with SARS-Cov-2 infection, which could result in further gut microbiota dysbiosis. Therefore, dysregulated inflammation and intestinal dysbiosis is caused not only by the infection itself. Indeed, comorbidities or the patient’s age may be the causes that lead to a greater severity of the disease and poor results in therapy. This may be one of the reasons for the increased severity of COVID-19 due to the direct regulation of crosstalk between the intestine, lung, brain, and skin, which increases immune dysregulation. (Fig. 2 ) [14,[28], [29], [30]]. Therefore, all this leads to the translocation of pathogenic organisms through the intestinal mucosa and secondary bacterial infections. Consequently, the increased inflammatory response leads to multi-organ dysfunction with poor clinical outcome [14,23,31,32]. Indeed, in the SARS-Cov-2 was observed, in several studies, that the intestinal microbiome presented bacterial diversity. It is reported that there is a higher number of opportunistic pathogenic population, such as Actinomyces, Streptococcus, Rothia, Veillonella, Clostridium hathewayi, Actinomyces viscosus, Bacteroides nordii and reduced Eubacterium ventriosum, Faecalibacterium, Lachnospiraceae. It is also noted that the excessive presence of Coprobacillus, Clostridium ramosum and Clostridium hathewayi related to the severity of the prognosis. Instead, there is an inverse relationship between the excessive presence of Faecalibacterium prausnitzii, acting as inflammatory activator, and the severity of the infection [31]. In other studies, in the fecal microbiome was found that Lactobacillus, Bifidobacterium, Streptococcus, Clostridium, Firmicutes, Corynebacterium, Ruthenibacterium were over represented, and the Lactobacillus, Bifidobacterium, Coprococcus, Parabacteroides, Roseburia, Faecalibacterium and Bacteroidetes were inferior [32,33]. Firmicutes has a potential influence on the intestinal ACE2 expression, and Bacteroides dorei, Bacteroides thetaiotaomicron, Bacteroides massiliensis and Bacteroides ovatus, have shown an inverse correlation with the fecal load of SARS-Cov-2 and a protective effect against inflammation [31,33,34].
Fig. 2.
The “immunity dysregulation dysbiosis cycle” (IDDC) hypothesis in SARS-CoV-2 patients: in the context of SARS-Cov-2 infection, it is important to consider the patient’s age, comorbidities, malnutrition, superinfections, antibiotics and antivirals which could result in further microbiota dysbiosis. This will lead to direct dysregulation of the human microbiota and of the intestinal, pulmonary, brain and skin axes. Consequently, immune dysregulation will increase leading to continuous increased microbiota dysbiosis and immune dysregulation. All this can contribute to a severe prognosis for the patients.
Finally, the bidirectional link between intestinal microbiota and the skin contributes to skin allostasis and homeostasis after an inflammatory process also based on its role in innate and adaptive immunity. It has been noted that pro-inflammatory cytokines produced in excess further aggravate the barrier damage in the intestine. This triggers in turn a vicious circle that leads to systemic low-grade inflammation with also involvement of the skin and development of pathologies such as acne, atopic dermatitis, and psoriasis [1,8,35]. A SARS-Cov-2 patient also presents skin symptoms, as we have previously mentioned. The discovered alterations of the gut microbiota in these patients could partly justify their presence thanks to this immune process of gut/skin crosstalk, that still are undergoing further studies [[12], [13], [14]].In fact, in alterations of the composition of the intestinal microbiota there is an increase in the production of free phenol and p-cresol, which are the final product of the metabolism of aromatic amino acids by Clostridium difficile. The passage of these substances into the bloodstream can induce their accumulation in the skin with alteration of epidermal differentiation and of the skin barrier, capable of causing skin dehydration and alterations of keratinization. So, there is an alteration of intestinal permeability induced by dysbiosis capable of altering the relationship between Teff and Treg lymphocytes in the intestine (and not only) with involvement of the skin [23,35,36].
3. SARS-CoV-2 infection and the role of probiotics in microbiota dysbiosis
Many evidences demonstrated significant effects of probiotics in strengthen and modulate the immune system against diseases [11,[37], [38], [39]]. In case of dysbiosis, probiotics contribute to repopulate gut with “good” bacteria, avoiding pathogens proliferation and establishing a condition of eubiosis [9,39].
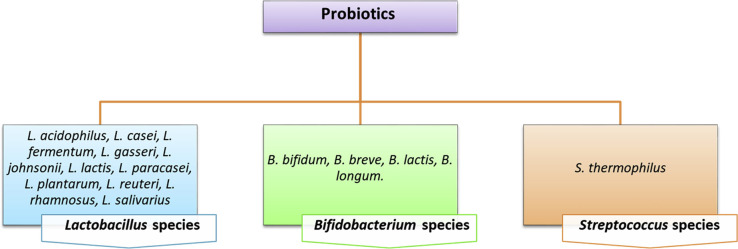
The term probiotics include many species, such as Lactobacillus spp. (L. acidophilus, L. casei, L. rhamnosus), Bifidobacterium spp (B. bifidum, B. longum, B. lactis), Enterococcus spp (E. faecalis, E. faecium), and Saccharomyces spp (S. boulardii, S. cerevisiae), Leuconostoc, Pediococcus. The Lactobacillus spp. (L. rhamnosus) and Bifidobacterium spp. (B. lactis HN019) are commonly taken by fermented products, such as yogurts and cheeses. (Table 2 ) [11,[40], [41], [42]]. The Lactobacillus spp. and Bifidobacterium spp. are the main conventional probiotics that can really be used for the balance of a diversified intestinal ecosystem in the fight against SARS-Cov-2. The rationale for using probiotics to treat SARS-CoV-2 comes from some experimental studies and indirect evidences. Probiotics, such as Lactobacillus can, through an antiviral action, lead to a condition of eubiosis in the intestinal microbiota and thus can contribute an anti-inflammatory effect and to the prevention of super-infections.
Table 2.
Main probiotics strains Lactobacillus, Bifidobacterium and Streptoccocus spp. used as food and adjuvant therapy. The bacteriotherapy already in the past had demonstrated its anti-inflammatory efficacy and immune-stimulatory effects in various diseases, such as the viral ones. They are also easy to administer and usually have no side effects.
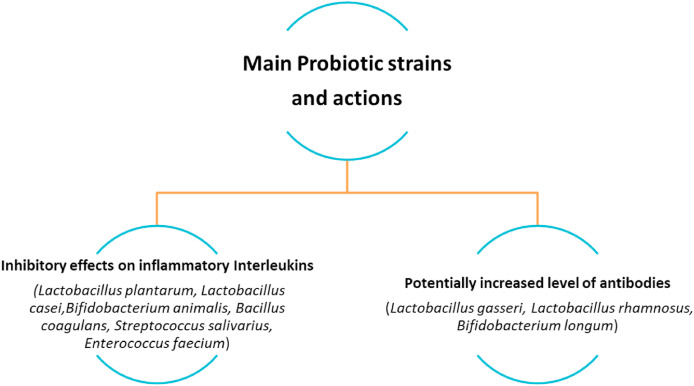
It is recommendable the use of probiotics, and their metabolites SCFAs, to reinforce innate and adaptive immunity in SARS-CoV-2 patients, as an adjuvant strategy against complications. The rationale for this approach comes from different experimental evidences [[43], [44], [45], [46], [47]]. Probiotics detain anti-inflammatory properties during viral infections and contribute to prevent bacterial super-infections. Butyrate, a probiotics’ metabolite, has been found in the portal circulation. It binds a G protein coupled receptor (free fatty acid receptor 2) on leucocytes, stimulating pulmonary macrophages proliferation and dendritic cells translocation. In the lungs, they contribute to stimulate a Th2 immune response. Contemporary, probiotics show an immunomodulating role in the cytokine storm (IL-1B, IL-6, IL-15, IL-15, IL-17 IFN-γ, TNF-α) [34,[48], [49], [50]].
Beneficial properties of probiotics in viral infections have been documented in antibiotic-associated diarrhea, different gastrointestinal infections, but also in modulating inflammation during high and low airways infections and sepsis, both in children and adults. The administration of multilayered probiotics tablets (L. paracasei, L. plantarum, L. acidophilus, L. delbrueckii, B. longum, B. infantis, B. breve, S. salivarius) to children admitted to the intensive care unit (ICU) with severe sepsis was useful to increase anti-inflammatory cytokines (TGF-ß1, IL-10) and to decrease pro-inflammatory cytokines levels (TNF-a, IL-6, IL-12p70, IL-17) [14,29,51]. The administration of more than twenty probiotics has demonstrated to improve anti-inflammatory interleukins levels and anti-viral antibodies production, reducing the viral load [[51], [52], [53], [54]]. For instance, Lactobacillus delbrueckii ssp. bulgaricus OLL1073R-1 and L. plantarum L-137 reduced the viral load of influenza and influenza H1N1 (modified strain) viruses in infected mices, respectively. On the other hand, the administration of Enterococcus faecalis FK-23 in HCV patients reduced liver enzymes, but without reducing the viral load [44,55].
In COVID-19 patients, probiotics could help to restore the altered gut microbiota, contributing to a healthy gut-lung axis. They could also reduce pathogens translocation through the intestinal mucosa, avoiding overlapping infections.
Hence, the immunomodulatory effects of probiotics could be relevant to prevent major complications in COVID-19 patients, such as ARDS with DAD and multi-organ dysfunction syndrome (MOF). Moreover, probiotics could interfere with the virus entry into the host cells and with its replication. Bifidobacterium animalis inhibits coronaviruses replication with an anti-interleukin effect. Lactobacillus casei ATCC 39392 stimulates IL-17 expression during coronavirus gastroenteritis. Some hypotheses have indicated that oral administration of Streptococcus salivarius K12 strain, through a still not perfectly clear molecular mechanism, reduce IL-8 plasma concentrations and increase interferon-γ salivary levels. Coronaviruses can also be vulnerable to probiotics, and in experimental models they have shown that Enterococcus faecium NCIMB 10415 increases nitric oxide (NO), and this leads to increased expression of IL-6 and IL-8. Instead, E. faecium HDRf1 is able to modify pro-inflammatory cytokines levels (TNF-a, IL-1, IL-6, IL-8, IL-12, IL-17) [18,56,57].
Two meta-analyses of twelve and thirteen randomized controlled trials, demonstrated clinical benefits of Lactobacillus and Bifidobacterium administration in mechanically ventilated patients in ICU, showing a lower incidence of upper respiratory tract infections and ventilator-associated pneumonia. Another study showed a better prognosis in 28 of 70 symptomatic patients taking probiotics (L. acidophilus DSM 32241, L. helveticus DSM 32242, L. paracasei DSM 32243, L. plantarum DSM 32244, L. brevis DSM 27961, B. lactis DSM 32246, B. lactis DSM 32247, 2400 billion bacteria per day), reducing the risk of admission in ICU. All these actions would be useful in reducing SARS-CoV-2 dissemination in the respiratory tract and gut, reinforcing both anti-inflammatory responses and immune defenses (Fig. 3 ) [14,32,47].
Fig. 3.
The various bacteria strains with the two different action ability. In general, probiotics can (a) compete with pathogens for sites of attachment to the mucosa; (b) modulate and strengthen the expression of genes that code for the proteins of the junctions themselves; (c) produce low molecular weight organic acids (lactic acid and acetic acid) and bacteriocins (proteinaceous or peptidic toxins for some pathogenic bacteria) and (d) modulate the immune system for the benefit of the persons or patients, mainly through the increase of antibodies level and inhibitory effects on inflammatory interleukins.
4. Conclusions
The SARS-CoV-2 pandemic made patient’s management difficult, especially regarding therapy. Different factors (age, comorbidities, therapeutics, etc.) dysregulate the four communication axes of the gut/lung, gut/brain, and gut/skin and skin/brain microbiota, leading to microbial imbalance in those patients. We can define this new hypothesis as the “immunity dysregulation dysbiosis cycle” (IDDC). The proven efficacy of probiotics was already demonstrated in the past in various diseases, including the viral ones, specially their anti-inflammatory and immune-stimulatory effects. Immunomodulatory benefits are particularly relevant for people at risk of developing SARS-CoV-2 severe disease. In this case, they exhibit excessive inflammatory responses and complications, especially in case of comorbidities. Moreover, probiotics are available and not expensive, easy to administer orally, without side effects or therapeutic interferences. Hence, they are a potential therapeutic strategy that must considered in supporting moderate and severe cases of SARS-CoV-2. Some authors also recommend their administration in mechanically ventilated patients and in advance for a better prognosis and outcome.
Authors contribution
All the authors equally conceived and designed this review. Dr. Charitos has written the original draft, Dr. Di Cosola revised it. All the authors have read and approved the final version, also approving the choice for journal submission.
Funding
No funds or grants available for this paper.
Ethical issues
Not applicable.
Acknowledgments
The authors thanks Giuseppe Divittorio and Michelangelo Ferri for their valuable help in data collection.
References
- 1.Ursell L.K., Metcalf J.L., Parfrey L.W., Knight R. Defining the human microbiome. Nutr Rev. 2012;70(1):S38–S44. doi: 10.1111/j.1753-4887.2012.00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sender R., Fuchs S., Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 2016 Aug 19;14(8) doi: 10.1371/journal.pbio.1002533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Human Microbiome Project Consortium Structure, function and diversity of the healthy human microbiome. Nature. 2012;486(7402):207–214. doi: 10.1038/nature11234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bottalico L., Castellaneta F., Charitos I.A. From hydrotherapy to the discovery of the gut microbiota: the historical gastrointestinal health concept. Pharmacophore. 2020;11(2):82–90. [Google Scholar]
- 5.Ballini A., Dipalma G., Isacco C.G., Boccellino M., Di Domenico M., Santacroce L. Oral microbiota and immune system crosstalk: a translational research. Biology (Basel) 2020;9(6):131. doi: 10.3390/biology9060131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rhee S.H., Pothoulakis C., Mayer E.A. Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat Rev Gastroenterol Hepatol. 2009;6(5):306–314. doi: 10.1038/nrgastro.2009.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santacroce L., Charitos I.A., Ballini A., Inchingolo F., Luperto P., De Nitto E. The human respiratory system and its microbiome at a glimpse. Biology (Basel) 2020;1;9(10):E318. doi: 10.3390/biology9100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salem I., Ramser A., Isham N., Ghannoum M.A. The gut microbiome as a major regulator of the gut-skin Axis. Front Microbiol. 2018;10;9:1459. doi: 10.3389/fmicb.2018.01459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samuelson D.R., Welsh D.A., Shellito J.E. Regulation of lung immunity and host defense by the intestinal microbiota. Front Microbiol. 2015;7(6):1085. doi: 10.3389/fmicb.2015.01085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Belkaid Y., Hand T.W. Role of the microbiota in immunity and inflammation. Cell. 2014;157(1):121–141. doi: 10.1016/j.cell.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santacroce L., Charitos I.A., Bottalico L. A successful history: probiotics and their potential as antimicrobials. Expert Rev Anti Infect Ther. 2019;17(8):635–645. doi: 10.1080/14787210.2019.1645597. [DOI] [PubMed] [Google Scholar]
- 12.Charitos I.A., Ballini A., Bottalico L., Cantore S., Passarelli P.C., Inchingolo F. Special features of SARS-CoV-2 in daily practice. World J Clin Cases. 2020 Sep 26;8(18):3920–3933. doi: 10.12998/wjcc.v8.i18.3920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santacroce L., Charitos I.A., Del Prete R. COVID-19 in Italy: an overview from the first case to date. Electron J Gen Med. 2020;17(6) doi: 10.29333/ejgm/7926. [DOI] [Google Scholar]
- 14.Angurana S.K., Bansal A. Probiotics and COVID-19: think about the link. Br J Nutr. 2020:1–26. doi: 10.1017/S000711452000361X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Machhi J., Herskovitz J., Senan A.M., Dutta D., Nath B., Oleynikov M.D. The natural history, pathobiology, and clinical manifestations of SARS-CoV-2 infections. J Neuroimmune Pharmacol. 2020;21:1–28. doi: 10.1007/s11481-020-09944-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cazzolla A.P., Lovero R., Lo Muzio L., Testa N.F., Schirinzi A., Palmieri G. Taste and smell disorders in COVID-19 patients: role of Interleukin-6. ACS Chem Neurosci. 2020 doi: 10.1021/acschemneuro.0c00447. [DOI] [PubMed] [Google Scholar]
- 17.Santacroce L., Bottalico L., Charitos I.A. The impact of COVID-19 on Italy: a lesson for the future. Int J Occup Environ Med. 1984:2020. doi: 10.34172/ijoem.2020.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Santacroce L., Charitos I.A., Carretta D.M., De Nitto E., Lovero R. The human coronaviruses (HCoVs) and the molecular mechanisms of SARS-CoV-2 infection. J Mol Med (Berl) 2020 Dec 2 doi: 10.1007/s00109-020-02012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grosse C., Grosse A., Salzer H.J.F., Dünser M.W., Motz R., Langer R. Analysis of cardiopulmonary findings in COVID-19 fatalities: high incidence of pulmonary artery thrombi and acute suppurative bronchopneumonia. Cardiovasc Pathol. 2020;49 doi: 10.1016/j.carpath.2020.107263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ni W., Yang X., Yang D., Bao J., Li R., Xiao Y. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;24(1):422. doi: 10.1186/s13054-020-03120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drosten C., Günther S., Preiser W., van der Werf S., Brodt H.R., Becker S. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348(20):1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 22.Schirinzi A., Cazzolla A.P., Lovero R., Lo Muzio L., Testa N.F., Ciavarella D. New insights in laboratory testing for COVID-19 patients: looking for the role and predictive value of Human epididymis secretory protein 4 (HE4) and the innate immunity of the oral cavity and respiratory tract. Microorganisms. 2020;8(11):E1718. doi: 10.3390/microorganisms8111718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dhar D., Mohanty A. Gut microbiota and Covid-19- possible link and implications. Virus Res. 2020;285:198018. doi: 10.1016/j.virusres.2020.198018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Conte L., Toraldo D.M. Targeting the gut-lung microbiota axis by means of a high-fibre diet and probiotics may have anti-inflammatory effects in COVID-19 infection. Ther Adv Respir Dis. 2020;14 doi: 10.1177/1753466620937170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Costela-Ruiz V.J., Illescas-Montes R., Puerta-Puerta J.M., Ruiz C., Melguizo-Rodríguez L. SARS-CoV-2 infection: the role of cytokines in COVID-19 disease. Cytokine Growth Factor Rev. 2020;54:62–75. doi: 10.1016/j.cytogfr.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaves Andrade M., Souza de Faria R., Avelino Mota Nobre S. COVID-19: can the symptomatic SARS-CoV-2 infection affect the homeostasis of the gut-brain-microbiota axis? Med Hypotheses. 2020;144:110206. doi: 10.1016/j.mehy.2020.110206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mayer E.A., Tillisch K., Gupta A. Gut/brain axis and the microbiota. J Clin Invest. 2015;125(3):926–938. doi: 10.1172/JCI76304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riphagen S., Gomez X., Gonzalez-Martinez C., Wilkinson N., Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607–1608. doi: 10.1016/S0140-6736(20)31094-1. 10237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. China medical treatment expert Group for covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gu S., Chen Y., Wu Z., Chen Y., Gao H., Lv L. Alterations of the gut microbiota in patients with COVID-19 or H1N1 influenza. Clin Infect Dis. 2020;4:ciaa709. doi: 10.1093/cid/ciaa709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zuo T., Zhang F., Lui G.C.Y., Yeoh Y.K., Li A.Y.L., Zhan H. Alterations in gut microbiota of patients with COVID-19 during time of hospitalization. Gastroenterology. 2020;159(3):944–955.e8. doi: 10.1053/j.gastro.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tao W, Zhu S, Zhang G,Wang X,Guo M, Zeng W et al. Analysis of the intestinal microbiota in COVID-19 patients and its correlation with the inflammatory factor IL-18 and SARS-CoV-2-specific IgA medRxiv 2020; 20173781; doi: 10.1101/2020.08.12.20173781. [DOI] [PMC free article] [PubMed]
- 33.d’Ettorre G., Ceccarelli G., Marazzato M., Campagna G., Pinacchio C., Alessandri F. Challenges in the management of SARS-CoV2 infection: the role of oral bacteriotherapy as complementary therapeutic strategy to avoid the progression of COVID-19. Front Med (Lausanne) 2020;7:389. doi: 10.3389/fmed.2020.00389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morais A.H.A., Aquino J.S., da Silva-Maia J.K., Vale S.H.L., Maciel B.L.L., Passos T.S. Nutritional status, diet and viral respiratory infections: perspectives for severe acute respiratory syndrome coronavirus 2. Br J Nutr. 2020 Aug 26:1–12. doi: 10.1017/S0007114520003311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Neill C.A., Monteleone G., McLaughlin J.T., Paus R. The gut-skin axis in health and disease: a paradigm with therapeutic implications. Bioessays. 2016;38(11):1167–1176. doi: 10.1002/bies.201600008. [DOI] [PubMed] [Google Scholar]
- 36.Miyazaki K., Masuoka N., Kano M., Iizuka R. Bifidobacterium fermented milk and galacto-oligosaccharides lead to improved skin health by decreasing phenols production by gut microbiota. Benef Microbes. 2014;5(2):121–128. doi: 10.3920/BM2012.0066. [DOI] [PubMed] [Google Scholar]
- 37.Signorini L., De Leonardis F., Santacroce L., Haxhirexha K., Topi S., Fumarola L. Probiotics may modulate the impact of aging on adults. J Biol Regul Homeost Agents. 2020;34(4):1601–1606. doi: 10.23812/20-393-L. [DOI] [PubMed] [Google Scholar]
- 38.Ballini A., Santacroce L., Cantore S., Bottalico L., Dipalma G., Topi S. Probiotics efficacy on oxidative stress values in inflammatory bowel disease: a randomized double-blinded placebo-controlled pilot study. Endocr Metab Immune Disord - Drug Targets. 2019;19(3):373–381. doi: 10.2174/1871530319666181221150352. [DOI] [PubMed] [Google Scholar]
- 39.Shi L.H., Balakrishnan K., Thiagarajah K., Mohd Ismail N.I., Yin O.S. Beneficial properties of probiotics. Trop Life Sci Res. 2016;27(2):73–90. doi: 10.21315/tlsr2016.27.2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Santacroce L., Sardaro N., Topi S., Pettini F., Bottalico L., Cantore S. The pivotal role of oral microbiota in health and disease. J Biol Regul Homeost Agents. 2020;34(2):733–737. doi: 10.23812/20-127-L-45. [DOI] [PubMed] [Google Scholar]
- 41.Inchingolo F., Santacroce L., Cantore S., Ballini A., Del Prete R., Topi S. Probiotics and EpiCor® in human health. J Biol Regul Homeost Agents. 2019;33(6):1973–1979. doi: 10.23812/19-543-L. [DOI] [PubMed] [Google Scholar]
- 42.Ballini A., Santacroce L., Cantore S., Bottalico L., Dipalma G., Vito D. Probiotics improve urogenital health in women. Open Access Maced J Med Sci. 2018;6(10):1845–1850. doi: 10.3889/oamjms.2018.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Santacroce L. Letter in response to the article "Enhancing immunity in viral infections, with special emphasis on COVID-19: a review" (Jayawardena et al.) Diabetes Metab Syndr. 2020;14(5):927. doi: 10.1016/j.dsx.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kanauchi O., Andoh A., AbuBakar S., Yamamoto N. Probiotics and paraprobiotics in viral infection: clinical application and effects on the innate and acquired immune systems. Curr Pharmaceut Des. 2018;24(6):710–717. doi: 10.2174/1381612824666180116163411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Olaimat A.N., Aolymat I., Al-Holy M., Ayyash M., Abu Ghoush M., Al-Nabulsi A.A., Osaili T., Apostolopoulos V., Liu S.Q., Shah N.P. The potential application of probiotics and prebiotics for the prevention and treatment of COVID-19. NPJ Sci Food. 2020 Oct 5;4:17. doi: 10.1038/s41538-020-00078-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Inchingolo F., Dipalma G., Cirulli N., Cantore S., Saini R.S., Altini V. Microbiological results of improvement in periodontal condition by administration of oral probiotics. J Biol Regul Homeost Agents. 2018;32(5):1323–1328. [PubMed] [Google Scholar]
- 47.Morais A.H.A., Passos T.S., Maciel B.L.L., da Silva-Maia J.K. Can probiotics and diet promote beneficial immune modulation and purine control in coronavirus infection? Nutrients. 2020;12(6):1737. doi: 10.3390/nu12061737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baud D., Dimopoulou Agri V., Gibson G.R., Reid G., Giannoni E. Using probiotics to flatten the curve of coronavirus disease COVID-2019 pandemic. Front Publ Health. 2020;8:186. doi: 10.3389/fpubh.2020.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mack D.R., Michail S., Wei S., McDougall L., Hollingsworth M.A. Probiotics inhibit enteropathogenic E. coli adherence in vitro by inducing intestinal mucin gene expression. Am J Physiol. 1999;276(4):G941–G950. doi: 10.1152/ajpgi.1999.276.4.G941. [DOI] [PubMed] [Google Scholar]
- 50.Liu M., Zhu H., He Y., Zhu Y., Hu X., Zeng Y. Probiotics for treating novel coronavirus with diarrhea: a protocol for systematic review and meta-analysis. Medicine (Baltim) 2020;99(38) doi: 10.1097/MD.0000000000021617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang G., Wen J., Xu L., Zhou S., Gong M., Wen P. Effect of enteral nutrition and ecoimmunonutrition on bacterial translocation and cytokine production in patients with severe acute pancreatitis. J Surg Res. 2013;183(2):592–597. doi: 10.1016/j.jss.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 52.Isacco C.G., Ballini A., De Vito D., Nguyen K.C.D., Cantore S., Bottalico L. Rebalance the oral microbiota as efficacy tool in endocrine, metabolic, and immune disorders. Endocr Metab Immune Disord - Drug Targets. 2020 doi: 10.2174/1871530320666200729142504. [DOI] [PubMed] [Google Scholar]
- 53.Mahooti M., Miri S.M., Abdolalipour E., Ghaemi A. The immunomodulatory effects of probiotics on respiratory viral infections: a hint for COVID-19 treatment? Microb Pathog. 2020;148 doi: 10.1016/j.micpath.2020.104452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ballini A., Gnoni A., De Vito D., Dipalma G., Cantore S., Gargiulo I.C. Effect of probiotics on the occurrence of nutrition absorption capacities in healthy children: a randomized double-blinded placebo-controlled pilot study. Eur Rev Med Pharmacol Sci. 2019 Oct;23(19):8645–8657. doi: 10.26355/eurrev_201910_19182. [DOI] [PubMed] [Google Scholar]
- 55.Baud D., Dimopoulou Agri V., Gibson G.R., Reid G., Giannoni E. Using probiotics to flatten the curve of coronavirus disease COVID-2019 pandemic. Front Publ Health. 2020;8:186. doi: 10.3389/fpubh.2020.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Walton G.E., Gibson G.R., Hunter K.A. Mechanisms linking the human gut microbiome to prophylactic and treatment strategies for COVID-19. Br J Nutr. 2020 Oct 9:1–36. doi: 10.1017/S0007114520003980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Morais A.H.A., Passos T.S., Maciel B.L.L., da Silva-Maia J.K. Can probiotics and diet promote beneficial immune modulation and purine control in coronavirus infection? Nutrients. 2020;12(6):1737. doi: 10.3390/nu12061737. [DOI] [PMC free article] [PubMed] [Google Scholar]