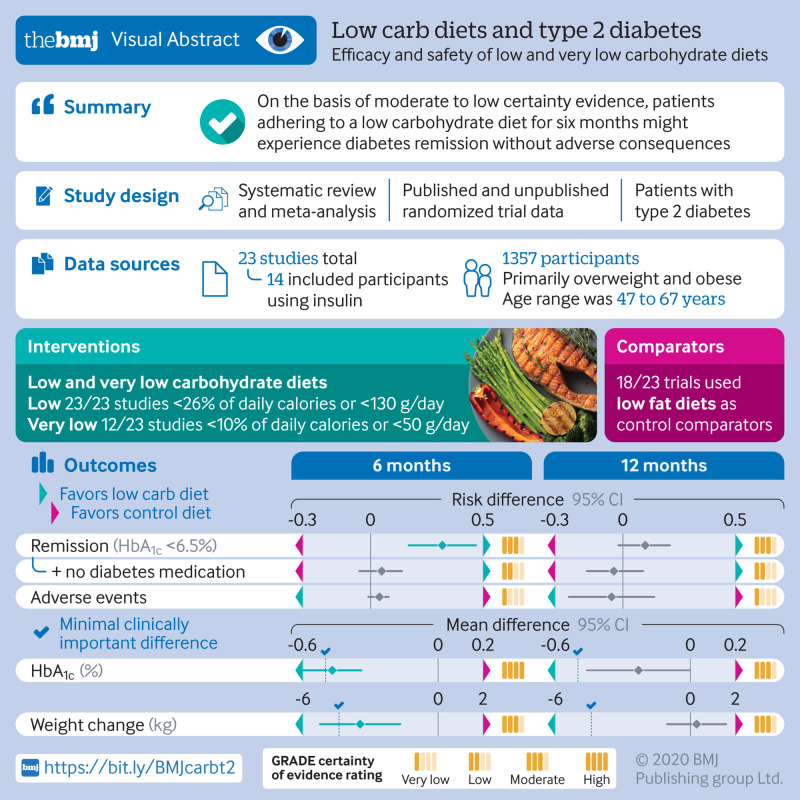
Abstract
Objective
To determine the efficacy and safety of low carbohydrate diets (LCDs) and very low carbohydrate diets (VLCDs) for people with type 2 diabetes.
Design
Systematic review and meta-analysis.
Data sources
Searches of CENTRAL, Medline, Embase, CINAHL, CAB, and grey literature sources from inception to 25 August 2020.
Study selection
Randomized clinical trials evaluating LCDs (<130 g/day or <26% of a 2000 kcal/day diet) and VLCDs (<10% calories from carbohydrates) for at least 12 weeks in adults with type 2 diabetes were eligible.
Data extraction
Primary outcomes were remission of diabetes (HbA1c <6.5% or fasting glucose <7.0 mmol/L, with or without the use of diabetes medication), weight loss, HbA1c, fasting glucose, and adverse events. Secondary outcomes included health related quality of life and biochemical laboratory data. All articles and outcomes were independently screened, extracted, and assessed for risk of bias and GRADE certainty of evidence at six and 12 month follow-up. Risk estimates and 95% confidence intervals were calculated using random effects meta-analysis. Outcomes were assessed according to a priori determined minimal important differences to determine clinical importance, and heterogeneity was investigated on the basis of risk of bias and seven a priori subgroups. Any subgroup effects with a statistically significant test of interaction were subjected to a five point credibility checklist.
Results
Searches identified 14 759 citations yielding 23 trials (1357 participants), and 40.6% of outcomes were judged to be at low risk of bias. At six months, compared with control diets, LCDs achieved higher rates of diabetes remission (defined as HbA1c <6.5%) (76/133 (57%) v 41/131 (31%); risk difference 0.32, 95% confidence interval 0.17 to 0.47; 8 studies, n=264, I2=58%). Conversely, smaller, non-significant effect sizes occurred when a remission definition of HbA1c <6.5% without medication was used. Subgroup assessments determined as meeting credibility criteria indicated that remission with LCDs markedly decreased in studies that included patients using insulin. At 12 months, data on remission were sparse, ranging from a small effect to a trivial increased risk of diabetes. Large clinically important improvements were seen in weight loss, triglycerides, and insulin sensitivity at six months, which diminished at 12 months. On the basis of subgroup assessments deemed credible, VLCDs were less effective than less restrictive LCDs for weight loss at six months. However, this effect was explained by diet adherence. That is, among highly adherent patients on VLCDs, a clinically important reduction in weight was seen compared with studies with less adherent patients on VLCDs. Participants experienced no significant difference in quality of life at six months but did experience clinically important, but not statistically significant, worsening of quality of life and low density lipoprotein cholesterol at 12 months. Otherwise, no significant or clinically important between group differences were found in terms of adverse events or blood lipids at six and 12 months.
Conclusions
On the basis of moderate to low certainty evidence, patients adhering to an LCD for six months may experience remission of diabetes without adverse consequences. Limitations include continued debate around what constitutes remission of diabetes, as well as the efficacy, safety, and dietary satisfaction of longer term LCDs.
Systematic review registration
PROSPERO CRD42020161795.
Introduction
Diabetes is a common, deadly, and expensive medical condition. It is estimated that 1 in 11 adults worldwide have diabetes and that it is responsible for 11% of deaths annually, costing $760bn (£570bn; €626bn) in direct costs alone.1 Type 2 diabetes is the most common form of diabetes, accounting for 90-95% of cases, and for decades has been a rapidly growing international concern.2 Type 2 diabetes is characterized by insulin resistance driven by chronic hyperglycemia and is commonly diagnosed by measures of glycemia such as fasting blood glucose concentrations of 7.0 mmol/L or above or glycated hemoglobin (HbA1c) values of 6.5% (48 mmol/mol) or above.3 It is associated with several risk factors including genetics and lifestyle influences, but by far the most common risk factor is obesity.1
Structured dietary interventions are commonly recommended for patients with diabetes, with varied recommendations from authoritative organizations.4 Before the discovery of insulin, diets emphasizing carbohydrate restriction had been used extensively in the management of diabetes, but more recently they have fallen out of favor.5 Because a key underlying mechanism of type 2 diabetes is insulin resistance driven in part by chronic hyperglycemia, lowering dietary intake of carbohydrate, most of which is absorbed as glucose or fructose, has been suggested to improve blood glucose control and outcomes of type 2 diabetes.6 Structured diets with carbohydrate restriction have been variably described in the research literature but have been commonly grouped into three categories: 20-50 g/day carbohydrates or less than 10% of the 2000 kcal/day diet that is generally sufficient to induce ketosis; less than 130 g/day or less than 26% of the 2000 kcal/day diet; and less than 45% of the 2000 kcal/day diet.7 8 For the purposes of this review, we refer to diets with less than 130 g/day or less than 26% of calories from carbohydrates based on 2000 kcal/day as a low carbohydrate diet (LCD).
Type 2 diabetes remains a significant and worsening problem worldwide, despite many pharmaceutical developments and a global emphasis on glycemic control.9 Structured diets are recognized as an essential component of treating diabetes,10 but confusion remains about which diet to choose.11 Systematic reviews and meta-analyses to date have attempted to pool carbohydrate restricted diets for diabetic populations, reporting mixed results.12 13 14 Among the limitations, as a whole, the systematic reviews and meta-analyses have included interventions with moderate carbohydrate intake that may dilute the effect of LCDs. Other limitations include an exclusive focus on surrogate outcomes (for example, blood lipids), with the largest systematic reviews and meta-analysis to date identifying only 10 trials that meet strict eligibility criteria of LCDs three months or more in length, limiting the certainty and precision in effect estimates.15 Furthermore, no review to date has attempted to report the effect of LCDs on rates of remission of diabetes,16 and no review has presented effect estimates with consideration of minimal important difference thresholds, thresholds that will assist patients and clinicians with interpreting the magnitude of treatment effects.17 18 We aimed to systematically assess the efficacy, safety, and certainty of estimates for both surrogate outcomes and outcomes important to patients of strict LCDs for people with type 2 diabetes.
Methods
Search strategy and selection criteria
On the basis of an a priori and publicly available protocol (PROSPERO CRD42020161795), we did a systematic review with meta-analysis of randomized controlled trials assessing the efficacy and safety of LCDs among adult patients with a diagnosis of type 2 diabetes. We included people with or without cardiovascular conditions regardless of medication use or glucose concentration and HbA1c level.
We included trials comparing LCDs with any wait list controls or any active controls including competing dietary programs higher in carbohydrates (≥26%), with or without exercise, lifestyle, and behavioral recommendations. No language, date, or publication restrictions were applied. We sought unpublished data from investigators of published and unpublished trials.
To meet inclusion criteria, studies had to investigate allocation to an LCD (<26% calories from carbohydrates or <130 g/day) for a defined period (12 weeks or longer), with or without exercise (for example, walking, jogging, strength training) or lifestyle and behavioral recommendations (for example, cognitive therapy, group support). Primary outcomes of interest, based on our a priori protocol,16 were remission of type 2 diabetes (dichotomously defined as HbA1c <6.5% or fasting glucose <7.0 mmol/L), with or without the use of diabetes medication. Additional primary outcomes were weight loss, HbA1c, fasting glucose, and adverse events (total and serious adverse events). Secondary outcomes were health related quality of life, reduction of medication, and biochemical laboratory data including total cholesterol, low density lipoprotein cholesterol, high density lipoprotein cholesterol, triglycerides, homeostasis model assessment of insulin resistance (HOMA-IR), and inflammatory markers (C reactive protein).
We searched the following databases from inception to 25 August 2020 to identify studies: Cochrane Central Register of Controlled Trials (CENTRAL), Medline via PubMed, Embase, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Commonwealth Agricultural Bureaux (CAB) abstracts. With the assistance of an expert clinical librarian, search strategies were customized, including the use of a Cochrane recommended filter for the identification of randomized controlled trials in PubMed.19 The Medline search strategy is reported in supplementary table A. On the basis of our study protocol, we also searched three trial registries (for example, clinicaltrials.gov) and four additional grey literature sources (for example, BIOSIS Citation Index, ProQuest Dissertations & Theses Global).16
Two authors, independently and in duplicate, screened titles and abstracts and subsequently full text articles. Disagreements were resolved by consensus.
Data analysis
Data extraction was done independently and in duplicate using a pilot tested extraction form. Domains for extraction included study design factors, population, intervention, comparator, and surrogate and health outcomes (variables listed in supplementary table B). All outcomes were extracted and reported at six months (±3 months) and 12 months (±3 months). We used version 2.0 of the Cochrane Risk-of-Bias (RoB) instrument for randomized trials and assessed each of the RoB domains as “high,” “low,” or “some concern” using the Excel file provided by the RoB 2.0 development team.20
We used Revman software (version 5.3) and the “meta” package in R (version 3.6.1) to do meta-analyses. For dichotomous outcomes, we calculated the pooled risk difference, risk ratio, and number needed to treat for an additional beneficial outcome (NNT) with 95% confidence intervals. For continuous outcomes, we combined endpoint or change data; when both endpoint and change data were reported, we prioritized endpoint data.21 We calculated the pooled mean difference and/or standardized mean difference with corresponding 95% confidence intervals. We pooled studies that measured continuous health related quality of life with different instruments if the underlying construct was the same or similar. To improve interpretability for readers, we followed published guidance and presented effect estimates in two ways.22 Firstly, we pooled the effect estimates as standardized mean differences. Secondly, we converted scores of the different health related quality of life instruments to units of the most commonly used reference instrument and presented the mean difference.22 23 24 Where possible, we presented the effect size on the basis of known or estimated minimal clinically important difference (MCID) thresholds for all outcomes (supplementary table C). We rated the overall certainty (quality) of evidence for each of our outcomes by using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach, wherein randomized trials began as high certainty evidence but could be rated down by one or more levels on the basis of five categories of limitations: risk of bias, inconsistency, indirectness, imprecision, and publication bias.25 26 We assessed the RoB and GRADE independently and in duplicate, with disagreement resolved by consensus. After a request from referees, we also did a sensitivity analysis comparing the certainty of evidence using GRADE versus NutriGRADE.27
Following published guidance, we chose to use data from complete cases for our primary analysis.28 When studies had missing outcome data and reported a complete case analysis, we did sensitivity analyses and applied increasingly stringent but plausible assumptions to this data,24 28 29 using Excel files made available from the authors of the GRADE guidance on missing outcome data.24 For assessing the effect of missing outcome data on risk of bias, we did these sensitivity assessments at the study level to best integrate with Cochrane RoB 2.0.20
We assessed and reported heterogeneity quantitatively using the I2 statistic and did a χ2 test for homogeneity according to guidelines from the Cochrane Handbook (for example, 50% to 90% may represent substantial heterogeneity; 75% to 100% may represent considerable heterogeneity).30
We investigated heterogeneity and the possibility of effect modification for our primary outcomes on the basis of risk of bias and seven a priori subgroups,16 with any subgroup effects with a statistically significant test of interaction subjected to a five point credibility checklist.31 Subgroups were very low carbohydrate diets (VLCD) (<10% calories from carbohydrates) versus diets with between 10% and 26% of calories from carbohydrates; trials that provided behavioral support versus those that did not; LCDs versus comparator diets (for example, low fat diets, Mediterranean diets); trials in which caloric intake did not significantly differ between groups (iso-caloric) versus those in which it did; LCD trials that used caloric restriction versus those that did not; trials that included patients who used insulin versus those that did not; trials in which the intervention group showed adequate adherence (determined by three a priori criteria: 3-β-hydroxybutyrate, measured carbohydrate intake, and author definitions16) versus those that did not. Furthermore, for each outcome, we investigated the effect on the point estimate when we restricted the analysis to studies at low risk of bias; if the risk of bias sensitivity analysis was credible,16 we focused our results on those studies at low risk.
To assess for the possibility of publication bias, we visually inspected funnel plots when 10 or more trials were included. We further assessed for publication bias by using Egger's regression test for continuous outcomes and the Harbord score for dichotomous outcomes.32 33
Patient and public involvement
Given the nature of secondary data capture and analysis, patients and the public were not involved in the design or interpretation of this study.
Results
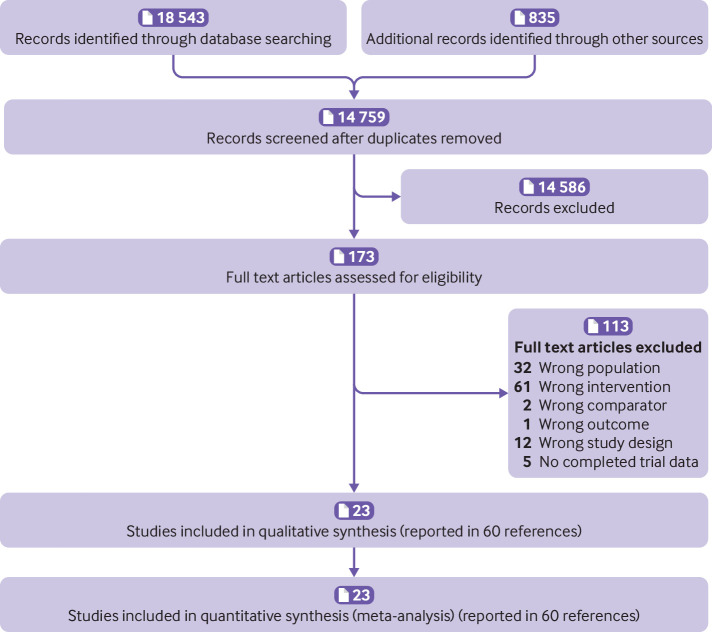
Our search yielded 14 759 records, of which 23 studies (1357 participants) met the inclusion criteria (fig 1). Table 1 shows characteristics of the clinical trials. In short, trials primarily included overweight and obese patients with type 2 diabetes, with 14/23 (61%) studies including participants using insulin. Trial size ranged from 12 to 144 participants with a mean age range of 47 to 67 years. Studies used various carbohydrate restriction thresholds with 12/23 (52%) meeting our criteria for very low carbohydrate diets (<10% daily calories from carbohydrates or <50 g/d). Trials primarily used low fat diets as control comparators (18/23; 78%). Duration of treatment ranged from three months to two years. Dropouts were common in the included studies. Eighteen (78%) of 23 studies reported missing participant outcome data, with 10 reporting more than 20% of data being missing. In studies with reported missing data, we assessed the robustness of reported effect estimates by using increasingly stringent assumptions about the missing data and incorporated this into the overall assessment for risk of bias.24 Overall, 59.4% of outcomes were rated as having some concern or high risk of bias, and 40.6% of outcomes were rated as having low risk of bias (fig 2). The randomization process was the risk of bias domain that had the poorest reporting, with just over 40% of trials having “some concerns.”
Fig 1.
PRISMA study flow
Table 1.
Characteristics of included trials
| Trial | BMI; HbA1C range; insulin dependent inclusive? | Mean age (years: (intervention/control); % female | Carbohydrate intake; caloric restriction; intense behavioral support | Comparator (diet, iso-caloric) | Adherence | Missing participant outcome data | Duration of intervention (months) |
|---|---|---|---|---|---|---|---|
| Dyson et al (2010)34 | BMI >25; did not include patients receiving insulin (n=12) | 54 | <40 g/d; calorically restricted; intense behavioral support | Low fat | Adequate | 17% | 3 |
| Morris et al (2019)35 | BMI >30; did not include patients receiving insulin (n=33) | 69/64; 55% female | <26% carbohydrate/d; calorically restricted | Low fat | Adequate | 0% | 3 |
| Saslow et al (2014)36 * | BMI ≥25; did not include patients receiving insulin (n=34) | 65/55; 74% female | “A very low carbohydrate, high fat, non calorie-restricted diet whose goal is to induce nutritional ketosis”; intense behavioral support | Low fat; iso-caloric (per intake not per goal) | Adequate | 11% | 12 |
| Saslow et al (2017)37 | BMI≥25; did not include patients receiving insulin (n=25) | 53/58; 56% female | 20-50 g/d | Low fat; iso-caloric | Adequate | 24% | 8 |
| Yamada et al (2014)38 | Did include patients receiving insulin (n=24) | 63/63; 50% female | 70-130 g/d | Low fat; iso-caloric (per intake not per goal) | Adequate | 0% | 6 |
| Tay et al (2014)39 | BMI 26-45; HbA1c≥7.0% or taking diabetes medication; did include patients receiving insulin (n=131) | 58/58; 37% female | 50-70 g/d target; calorically restricted; intense behavioral support | Low glycemic index; iso-caloric | Adequate | 29% | 24 |
| Jönsson et al (2009)40 | HbA1c>5.5%; did not include patients receiving insulin (n=17) | 66/63; 24% female | <130 g/d | Low fat | Adequate | 18% | 6 (crossover study; first 3 month comparison used in analysis) |
| Sato et al (2017)41 | BMI >23; HbA1c>7.5%; did include patients receiving insulin (n=66) | 61/58; 23% female | 130 g/d target | Low fat | Adequate | 6% | 6 |
| Goldstein et al (2011)42 | BMI 30-40; HbA1C>7%; did not include patients receiving insulin (n=52) | 57/55; 48% female | 25-40 g/d; intense behavioral support | Low fat (ADA 2000); iso-caloric | Adherent at VLCD level | 42% | 12 |
| Guldbrand et al (2012)43 | Did include patients receiving insulin (n=61) | 61/62; 56% female | 20%; calorically restricted | Low fat; iso-caloric | Adequate | 0% | 24 |
| Iqbal et al (2010)44 | BMI≥30; did include patients receiving insulin (n=144) | 60/60; 11% female | <30 g/d; intense behavioral support | Low fat | Not adequate | 47% | 24 |
| Nishimori et al (2018)45 | NAFLD in addition; did include patients receiving insulin (n=28) | 49/50; 36% female | 70-130 g/d; goal was for restriction but was not seen with intake | Low fat; iso-caloric (per intake not per goal) | Adequate | 0% | 3 |
| Vlachos et al (2011)46 | BMI >30; did include patients receiving insulin (n=79) | NA | “Low-carbohydrate and protein sparing modified fast”; calorically restricted | Low glycemic | NA | 22% | 6 |
| Westman et al (2008)47 | BMI 27-50; did include patients receiving insulin (n=97) | 52/52; 78% female | <20 g/d; intense behavioral support | Low glycemic; iso-caloric (per intake not per goal) | Adequate | 48% | 6 |
| Zadeh et al (2018)48 | BMI 30-38; did include patients receiving insulin (n=42) | 46.5 | 20%; intense behavioral support; calorically restricted | Low fat; high fat; moderate fat; probably iso-caloric (three control arms) | NA | 7% | 6 |
| Daly et al (2006)49 | Obese, poorly controlled T2D; did include patients receiving insulin (n=102) | 58/59; 52% female | <7 0 g/d | Low fat; iso-caloric | Adequate | 23% | 3 |
| Davis et al (2009)50 | BMI>25; A1C 6-11%; did include patients receiving insulin (n=105) | 54/53; 50% female | 20-25 g/d × 2 weeks + 5 g/wk; calorically restricted | Low fat; iso-caloric | Adherent at VLCD level | 20% | 12 |
| Yancy et al (2010)51 | BMI 27-30 plus obesity related disease, or BMI≥30; did include patients receiving insulin (n=46) | 57/55; 13% female | ≤20 g/d; intense behavioral support | Low fat + orlistat | Adequate | 11% | 12 |
| Samaha et al (2003)52 | BMI >35; did include patients receiving insulin (n=52) | NA | <30 g/d; intense behavioral support | Low fat | NA | 42% | 12 |
| Shai et al (2008)53 | BMI≥27 or coronary heart disease; did include patients receiving insulin (n=46) | NA | 20 g/d × 2 months with gradual increase to maximum 120 g/d | Low fat; Mediterranean (two control arms) | NA | 22% | 24 |
| Lee et al (2013)54 | BMI 30-65 (n=105) | NA | <70 g/d | Low fat | NA | 25% | 6 |
| Breukelman et al (2019)55 | BMI 38.9 (mean) (n=39) | 55/58; 60% female | <50 g/d | No treatment control | NA | 10% | 4 |
| Perna et al (2019)56 | BMI 24.9-34.9; A1c≤7.5% taking metformin; did not include patients receiving insulin (n=17) | 59.5/67.8; 65% female | <125 g/d; calorically restricted | “Standard” calorically restricted + metformin | NA | 0% | 3 |
ADA=American Diabetes Association; BMI=body mass index; HbA1c=glycated hemoglobin; NA=not available; NAFLD=non-alcoholic fatty liver disease; T2D=type 2 diabetes; VLCD=very low calorie diet.
Saslow 2014 met inclusion criteria but included 4/34 randomized participants who had pre-diabetes, not type 2 diabetes (>88% diabetic population). Contact with authors for diabetes specific data was unsuccessful. Although this situation was not considered a priori, research team decided to include this study on basis that any study with >80% of population having diabetes would be eligible; this scenario was not relevant in any other cases. This decision was made before results of study were reviewed.
Fig 2.
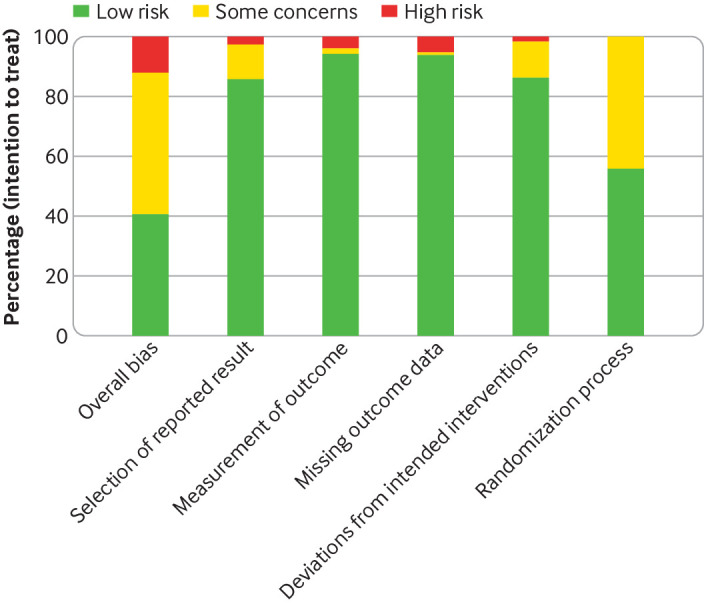
Risk of bias by outcome (percentage)
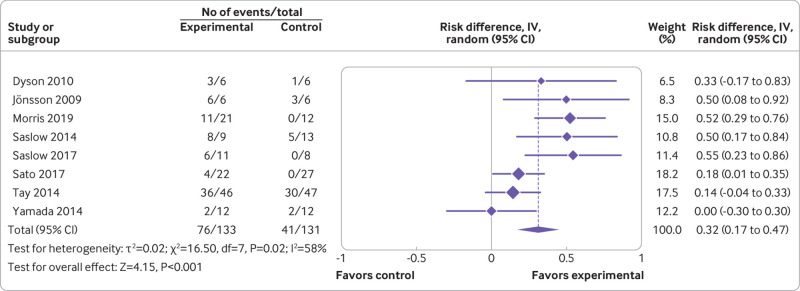
Eight studies reported on remission of diabetes at six months.34 35 36 37 38 39 40 41 Pooled analysis showed that when remission was defined by an HbA1c level below 6.5% independent of medication use, LCDs increased remissions by an additional 32 per 100 patients followed (risk difference 0.32, 95% confidence interval 0.17 to 0.47; 8 studies, n=264; GRADE=moderate) (fig 3; table 2). When remission was defined by an HbA1c level below 6.5% and the absence of diabetes medication, LCDs increased remissions at a lower rate (risk difference 0.05, –0.05 to 0.14; 5 studies, n=199; GRADE=low) (table 2). Three studies reported on remission at 12 months.35 39 41 When remission was defined independently of medication use, LCDs increased remission (risk difference 0.10, –0.02 to 0.21; 3 studies, n=171; GRADE=moderate), but they lowered the remission rate when the definition of remission included absence of diabetes medication (risk difference –0.04, –0.16 to 0.09; 2 studies, n=126; GRADE=low) (table 2).
Fig 3.
Remission (HbA1c <6.5%) at six months
Table 2.
Summary of findings for primary outcomes
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of evidence (GRADE) | |
|---|---|---|---|---|---|
| Risk with control | Risk with LCD | ||||
| Remission (HbA1c <6.5%) at 6 months | 31 per 100 | 59 (37 to 93) per 100 | RR 1.87 (1.18 to 2.97) | 264 (8 RCTs) | Moderatea,b |
| Remission (HbA1c <6.5% + no diabetes medication) at 6 months | 13 per 100 | 16 (9 to 32) per 100 | RR 1.24 (0.65 to 2.38) | 199 (5 RCTs) | Lowb,c |
| Remission (HbA1c <6.5%) at 12 months | 38 per 100 | 49 (38 to 63) per 100 | RR 1.27 (0.99 to 1.64) | 171 (3 RCTs) | Moderateb |
| Remission (HbA1c <6.5% + no diabetes medication) at 12 months | 16 per 100 | 13 (6 to 27) per 100 | RR 0.79 (0.36 to 1.73) | 126 (2 RCTs) | Lowb,c |
| Weight loss at 6 months | - | MD 3.46 kg lower (5.25 lower to 1.67 lower) | - | 882 (18 RCTs) | Moderated,e,f,g |
| Weight loss at 12 months | - | MD 0.29 kg higher (1.02 lower to 1.6 higher) | - | 499 (7 RCTs) | Moderateh |
| HbA1c at 6 months | - | MD 0.47% lower (0.60 lower to 0.34 lower) | - | 747 (17 RCTs) | High |
| HbA1c at 12 months | - | MD 0.23% lower (0.46 lower to 0 ) | - | 489 (8 RCTs) | Moderatei |
| Fasting glucose at 6 months | - | MD 0.73 (mmol/L) lower (1.19 lower to 0.27 lower) | - | 611 (14 RCTs) | Moderatej |
| Fasting glucose at 12 months | - | MD 0.06 mmol/L higher (0.37 lower to 0.48 higher) | - | 365 (6 RCTs) | Moderatei |
| Adverse events at 6 months | 5 per 100 | 8 (4 to 15) per 100 | RR 1.55 (0.76 to 3.15) | 423 (9 RCTs) | Very lowc,k,l |
| Serious adverse events at 6 months | 2 per 100 | 1 (0 to 8) per 100 | RR 0.79 (0.14 to 4.47) | 448 (8 RCTs) | Lowc,k |
| Adverse events at 12 months | 24 per 100 | 18 (10 to 32) per 100 | RR 0.72 (0.39 to 1.33) | 156 (2 RCTs) | Very lowb,c,l |
| Serious adverse events at 12 months | 4 per 100 | 3 (0 to 22) per 100 | RR 0.78 (0.10 to 6.13) | 217 (3 RCTs) | Very lowc,k |
For more information on GRADE, see https://gdt.gradepro.org/app/handbook/handbook.html.
HbA1c=glycated hemoglobin; MD=mean difference; RCT=randomized controlled trial; RD=risk difference; RR=risk ratio.
No statistically significant heterogeneity with RR meta-analysis (I2=34%, P=0.16); significant heterogeneity with RD (I2=58%, P=0.02). Did not rate down for heterogeneity as used RR for GRADE analyses and RD heterogeneity is explained by a priori subgroup analyses of those studies that included participants using versus not using insulin (I2=0%, P=0.97 for those not using insulin).
Rated down for imprecision because optimal information size (OIS) was not met.
Rated down for imprecision because of very wide confidence interval.
Evidence of subgroup differences by methodological quality, with low risk of bias studies showing larger effect than high risk of bias studies, surpassing MCID (4.4 kg) (mean difference –7.41, –9.75 to –5.08; 6 studies, n=171; test for subgroup differences P<0.001).
Statistically significant heterogeneity (I2=66%, P<0.001) explained by risk of bias; lower risk of bias shows larger effect with I2=0%, so not rated down.
95%CI is precise and sample size meets OIS; did not rate down.
Rated down for “other considerations” because visual inspection and Egger’s plot were suggestive of publication bias (P=0.02).
Visual inspection of funnel plot and statistical analysis for 6 months suggestive of publication bias, so rated down; analysis for publication bias at 12 months was underpowered (k<10), but cautiously rated down for 12 month data as well.
Rated down for imprecision because 95%CI includes small effect, no effect, and small worsening.
Rated down for inconsistency because of statistically significant unexplained heterogeneity (I2=68%, P<0.001).
Rated down for risk of bias because few included studies reported adverse events, suggesting selective outcome reporting bias.
Rated down for indirectness because studies used varied definitions of adverse events for their reported counts.
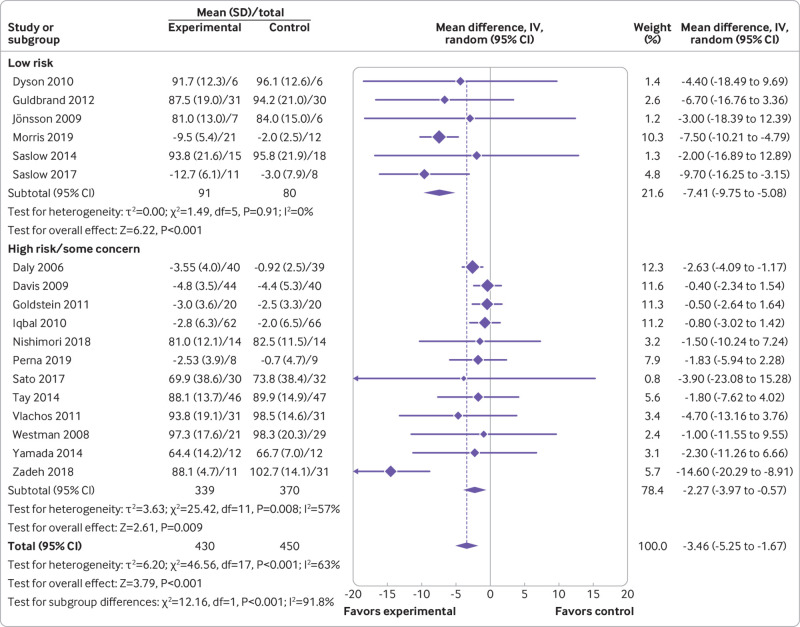
Eighteen studies reported on weight loss at six months.34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 56 Pooled analysis showed that patients on LCDs achieved greater weight loss compared with control (mean difference –3.46, 95% confidence interval –5.25 to –1.67; n=882; GRADE=moderate) (table 2). On the basis of subgroup credibility testing, we found that in studies at low risk of bias, LCDs achieved 7.41 kg greater weight loss compared with controls (mean difference –7.41, –9.75 to –5.08; 6 studies, n=171; test for subgroup differences P<0.001) (fig 4). Seven studies reported on weight loss at 12 months,36 39 42 43 44 50 51 with our pooled analysis showing that any benefit over control diets was trivial and non-significant (mean difference 0.29 (–1.02 to 1.60) kg; n=499; GRADE=moderate) (table 2).
Fig 4.
Weight loss at six months
Seventeen studies reported on HbA1c levels at six months.34 35 36 37 38 40 41 42 43 44 45 46 47 49 50 52 56 LCDs achieved greater reductions in HbA1c than did control diets (mean difference –0.47%, –0.60 to –0.34; n=747; GRADE=high) (table 2). At 12 months, eight studies reported on HbA1c levels, showing that the effect size had decreased by around half (mean difference –0.23%, –0.46% to 0.00%; n=489; GRADE=moderate) (table 2).
Fourteen studies reported on fasting glucose at six months.35 36 38 39 40 42 44 45 46 47 48 52 53 56 Pooled analysis showed that LCDs achieved an average 0.73 mmol/L greater reduction in glucose concentrations compared with control diets (mean difference –0.73, –1.19 to –0.27; n=611; GRADE=moderate) (table 2). Six studies reported on fasting glucose at 12 months,39 42 44 51 52 53 with little or no difference observed between the comparator diets (mean difference 0.06, –0.37 to 0.48; n=365; GRADE=moderate) (table 2).
Eleven studies reported total adverse events or serious adverse events at six months.34 35 37 38 39 41 43 44 45 47 52 Pooled analysis suggested a trivial and non-significant increase in total adverse events among patients on LCDs (risk difference 0.04, –0.01 to 0.08; 9 studies, n=423; GRADE=very low) and similarly little or no effect on serious adverse events (risk difference 0.00, –0.03 to 0.02; 8 studies, n=448; GRADE=low) (table 2). Three studies reported on total adverse events or serious adverse events at 12 months,39 43 44 with pooled estimates showing that LCDs were associated with a small, non-significant decrease in total adverse events (risk difference –0.05, –0.24 to 0.14; 2 studies, n=156; GRADE=very low) and a trivial, non-significant decrease in serious adverse events (risk difference –0.01, –0.06 to 0.04; 3 studies, n=217; GRADE=low) (table 2).
Table 3 shows secondary outcomes. Briefly, pooled analyses showed that LCDs led to greater reductions in diabetes medication and clinically important benefits threefold greater than the MCID estimate for triglycerides and insulin resistance (HOMA-IR) at six and 12 months. LCDs had clinically important harms on quality of life and low density lipoprotein cholesterol at 12 months, with little to no effect observed at six months. LCDs had little or no effect on total and high density lipoprotein cholesterol concentrations or C reactive protein related inflammation at six and 12 months.
Table 3.
Secondary outcomes
| Outcome | Endpoint | Participants (studies) | Effect estimate (95% CI) | Clinically important? (≥MCID for continuous outcomes) | GRADE |
|---|---|---|---|---|---|
| Quality of life—diabetes specific overall score (DDS and PAID) | 6 months | 169 (4 studies) | SMD –0.63 (–1.41 to 0.16) | NA | Low |
| 12 months | 116 (1 study) | MD 3.10 (–2.03 to 8.23) | Yes (harm) (MCID=1) | Low | |
| Quality of life—diabetes specific overall score (PAID, converted) | 6 months | 169 (4 studies) | MD –0.97 (–2.68 to 0.73) | No (MCID=1) | Low |
| 12 months | 116 (1 study) | MD 3.10 (–2.03 to 8.23) | Yes (harm) (MCID=1) | Low | |
| Medication reduction (No of participants who reduced diabetes medication) | 6 months | 240 (7 studies) | RD 0.24 (0.12 to 0.35) | NA | Moderate |
| 12 months | 148 (3 studies) | RD 0.33 (–0.00 to 0.66) | NA | Low | |
| Total cholesterol (mmol/L) | 6 months | 576 (12 studies) | MD –0.10 (–0.41 to 0.20) | No (MCID=0.26) | Moderate |
| 12 months | 430 (6 studies) | MD 0.11 (–0.05 to 0.27) | No (MCID=0.26) | Moderate | |
| LDL cholesterol (mmol/L) | 6 months | 672 (15 studies) | MD 0.02 (–0.09 to 0.12) | No (MCID=0.10) | High |
| 12 months | 429 (6 studies) | MD 0.14 (–0.00 to 0.28) | Yes (harm) (MCID=0.10) | Moderate | |
| HDL cholesterol (mmol/L) | 6 months | 647 (16 studies) | MD 0.06 (0.01 to 0.10) | No (MCID=0.10) | High |
| 12 months | 458 (7 studies) | MD 0.04 (–0.00 to 0.08) | No (MCID=0.10) | High | |
| Triglycerides (mmol/L) | 6 months | 860 (19 studies) | MD –0.30 (–0.43 to –0.17) | Yes (benefit) (MCID=0.09) | High |
| 12 months | 459 (7 studies) | MD –0.32 (–0.51, –0.12) | Yes (benefit) (MCID=0.09) | High | |
| Insulin resistance (HOMA-IR) | 6 months | 241 (6 studies) | MD –0.14 (–0.51 to 0.23) | Yes (benefit) (MCID=0.05) | Very low |
| 12 months | 135 (2 studies) | MD –0.13 (–0.39 to 0.13) | Yes (benefit) (MCID=0.05) | Very low | |
| Inflammation (C reactive protein, mg/L) | 6 months | 359 (7 studies) | MD 0.16 (–0.27 to 0.59) | No (MCID=0.5) | Moderate |
| 12 months | 141 (2 studies) | MD 0.37 (–0.44 to 1.18) | No (MCID=0.5) | Very low |
DDS=diabetes distress scale; HDL=high density lipoprotein; HOMA-IR=homeostasis model assessment of insulin resistance; LDL=low density lipoprotein; MCID=minimal clinically important difference; MD=mean difference; NA=not available; PAID=problem areas in diabetes; RD=risk difference; SMD=standardized mean difference.
We did subgroup assessments (level of carbohydrate restriction, behavioral support intensity, comparator diet, iso-caloric comparator, caloric restriction, inclusion of patients who used insulin, and adherence) for each of our five primary outcomes. Most subgroup observations were not deemed credible; however, three credible subgroups were identified on the basis of meeting four of five credibility criteria. Specifically, for these subgroups, statistical analysis suggested that chance could not explain the apparent subgroup effect, the effect was consistent across studies, the subgroup hypothesis was one of a small number of hypotheses developed a priori with direction specified, and strong pre-existing biological support existed (supplementary table D). Studies that included patients using insulin had fewer remissions for both definitions of remission (HbA1c <6.5%; HbA1c <6.5% and no diabetes medication) at six months (risk difference 0.14, 0.03 to 0.25; 0.00, –0.07 to 0.07) compared with studies that did not (risk difference 0.51, 0.36 to 0.65; 0.20, 0.03 to 0.38) (test for subgroup difference P<0.001; P=0.03). Diets with very low carbohydrates (<10% of daily calories from carbohydrates) led to smaller weight loss at six months (mean difference –1.05, –2.27 to 0.17) than did less restrictive diets (mean difference –5.22, –8.33 to –2.11) (test for subgroup difference P=0.01). However, on the basis of our third subgroup that was judged to be credible,16 this effect was explained by diet adherence. That is, among VLCDs to which the patients were highly adherent, a larger clinically important weight loss occurred (mean difference –4.47, –8.21 to –0.73) compared with patients less adherent to VLCDs (mean difference –0.55, –1.76 to 0.66) (test for subgroup difference P=0.05).
We did a post hoc sensitivity analysis comparing the certainty of evidence using GRADE versus NutriGRADE (supplementary table E). NutriGRADE analysis resulted in 16/30 (53%) outcomes with the same rating as GRADE; 10 (33%) of outcomes were upgraded compared with GRADE ratings (mainly our secondary outcomes), and 4 (13%) were downgraded.
Discussion
Among 23 studies comparing LCDs with mostly low fat control diets in patients with type 2 diabetes, on the basis of moderate to low certainty evidence, patients on LCDs achieved higher diabetes remission rates at six months (HbA1c <6.5%: NNT=3; HbA1c <6.5% and no diabetes medication: NNT=20). On the basis of very low to high certainty evidence, no statistically significant and clinically important detrimental effects on cardiovascular risk factors (for example, lipids, C reactive protein) or adverse events were detected with LCDs. However, we observed a trend for clinically important increases in low density lipoprotein cholesterol at 12 months. Additionally, LCDs increased weight loss, reduced medication use, and improved triglyceride concentrations at six months. In general, most benefits diminished at 12 months, a finding consistent with previous reviews.15 57
Sensitivity and subgroup analyses
We did sensitivity analyses based on risk of bias for all outcomes, but only one outcome, weight loss, showed a credible subgroup effect between studies with higher and lower risk of bias. Studies with lower risk of bias showed more dramatic increases in weight loss, findings that were both statistically and clinically significant, supporting our overall findings.
Subgroup analyses, based on credibility testing,16 27 suggested that patients not using insulin, compared with those that did, had increased diabetes remission rates at six months. For patients not using insulin, the NNT was 2 for remission defined as HbA1c below 6.5% and 5 for remission defined as HbA1c below 6.5 without diabetes medication. Furthermore, on the basis of our subgroup testing, VLCDs underperformed compared with less restrictive LCDs for weight loss at six months. However, this difference was negated when we considered patients highly adherent to VLCDs. Of note, the limited number of studies with 12 month outcome data providing differing levels of support and having highly adherent versus less adherent intervention arms precluded subgroup analyses that explicitly explored the effects of adherence at 12 months. Although improvements noted at six months diminished by 12 months, determining with any certainty whether this is related to intensity of intervention and/or dietary adherence beyond six months is difficult.
Strengths of study
Our systematic review has several important strengths. Firstly, we did a thorough literature search and contacted authors of all studies for any unpublished data on remission of diabetes. Although only three included studies previously published HbA1c threshold criteria and medication use to determine diabetes remission, our successful contact with authors yielded trial data from five additional studies to determine remission rates,34 38 39 40 58 increasing the precision and overall certainty of the effect estimates.13 15 57 59 Recent systematic reviews conducted by Sainsbury, van Zuuren, and Snorgaard have shown important reductions in mean HbA1c values with low and very low carbohydrate diets,13 15 59 but no previous review has summarized HbA1c as a dichotomous outcome informed by the suggested American Diabetes Association remission definitions (for example, <6.5% HbA1c threshold).16 60 We believe that our meta-analytic summary of published and unpublished data from eight randomized controlled trials using HbA1c thresholds, a first in the literature, will lead to more informed clinical decision making in the management of type 2 diabetes.
Secondly, on the basis of a publicly available protocol,16 we used robust evidence synthesis methods including the use of Cochrane’s Risk of Bias instrument 2.0,20 missing participant outcome data sensitivity analyses,24 and subgroup credibility assessments based on a priori stated effect modifiers.31 Missing data for participants is particularly important in nutrition research in general given the often dramatic losses to follow-up in diet based clinical trials (>20% among 10/23 (43%) of trials included in this analysis) and the corresponding risk of bias due to losses to follow-up.61 Subgroup credibility assessment is of particular interest to researchers in this field given that some have advocated for subgroup elucidation when considering LCDs for treating diabetes.62 63 Whereas previous reviews have focused on one or two potential modifiers—for example, Korsmo et al, who explored subgroups on length of follow-up and carbohydrate intake,57 and Naude et al, who explored calorically matched controls14—in our protocol driven approach, we explored seven actively debated potential effect modifiers by using published, explicit subgroup credibility criteria.
Thirdly, the use of GRADE for rating the certainty of evidence in systematic reviews of nutrition studies has been questioned,27 with some calling for a methodological approach specific to nutrition studies. However, we believe the logic of scientific inquiry demands consistent standards for casual inference across health claims, preferably using GRADE, a more conservative rating approach than the alternative systems suggested by the nutrition community.64 65 66 67 Nevertheless, we did a sensitivity analysis comparing GRADE ratings with NutriGRADE ratings (supplementary table E). NutriGRADE analysis resulted in 16/30 (53%) outcomes with the same rating as GRADE; 10 (33%) of outcomes were judged to be of higher certainty using NutriGRADE, and 4 (13%) were judged to be of lower certainty using NutriGRADE. Overall, the certainty of evidence using NutriGRADE indicates, on average, a higher degree of confidence in the efficacy and safety of LCDs across outcomes, particularly our primary outcomes including diabetes remission and fasting glucose, and higher certainty in the evidence for little to no short term risk of adverse events with LCDs.
Fourthly, our interpretations of estimates for continuous outcomes were based on a priori estimates of the minimal clinically important differences (supplementary table C). To our knowledge, no previous review on this topic has attempted to present effect estimates while considering MCID thresholds, thresholds that will help clinicians and patients to better interpret the magnitude of treatment effect.30 Among 10 continuous outcomes, two showed improvements that met or surpassed the MCID at six months (triglycerides, insulin resistance) with no detrimental effects. At 12 months, two had improvements that surpassed the MCID (triglycerides, insulin resistance) and two had a clinically important worsening (quality of life, low density lipoprotein cholesterol), although neither was statistically significant (P=0.24 and P=0.05).
Limitations of study
Our study is not without limitations. Firstly, the definition of remission of diabetes is the subject of considerable debate, specifically with regards to threshold levels of HbA1c/fasting glucose, use of diabetes medication, and the length of follow-up time meeting these criteria.60 We attempted to overcome this by using multiple a priori definitions of remission (both with and without the use of diabetes medication) at both of our predetermined endpoints (six months and 12 months).
Secondly, safety concerns have been raised with LCDs.68 Although no significant or clinically important increase in total or serious adverse events was identified, these outcomes were poorly reported among trials and the certainty of evidence for safety ranges from low to very low. By contrast, we have moderate to high certainty that surrogate markers for cardiovascular disease risk, such as blood lipids, do not worsen, whereas triglycerides significantly improved in a clinically meaningful way. One exception was low density lipoprotein cholesterol concentrations at 12 months’ follow-up, which seemed to worsen, surpassing the MCID. Thirdly, 18/23 (78%) studies used low fat diets as a comparator, limiting the applicability of our results to other dietary regimens such as a Mediterranean-style diet.
Fourthly, an important concern with LCDs is the potential confounding factor of caloric restriction. Restricting carbohydrates, which tends to reduce hunger,69 would mean that whether any purported benefit was due to carbohydrate restriction or caloric restriction was unclear. For this reason, as part of our a priori planned subgroup analysis, we investigated the effect of calorically matched controls (as assessed by follow-up dietary questionnaires). On the basis of 18 studies providing adequate data, we identified no evidence of credible effect modification based on caloric matching or lack thereof. However, self-reported dietary intake data are prone to measurement error, particularly in dietary trials in which participants are not blinded.70 71
Fifthly, we made a pragmatic a priori decision to assess our endpoints at six and 12 months (±3 months). Whereas trials informing our 12 month endpoint were all reported at this time point, those informing our six month endpoint varied between three months and eight months. Of the 14 trials informing our six month pooled estimates, 7/14 (50%) reported data at three to less than six months (3 months: 6 trials; 4 months: 1 trial), and 7/14 (50%) trials reported at six to nine months (6 months: 6 trials; 8 months: 1 trial). On the basis of comments from peer reviewers, we did a post hoc analysis on remission at six (±3) months. Evidence suggested larger treatment effects for LCDs in shorter term trials (3 to <6 months), suggesting that shorter term trials may be an effect modifier. For the definition of remission of HbA1c below 6.5%, the risk difference was 0.49 (95% confidence interval 0.30 to 0.68) for trials of three to less than six months in length compared with 0.25 (0.08 to 0.42) for trials of between six and nine months. Similarly, for the definition of remission of HbA1c below 6.5% and no diabetes medication use, the risk difference was 0.20 (0.03 to 0.38) for trials of three to less than six months compared with 0.00 (–0.07 to 0.07) for trials of between six and nine months.
Sixthly, our protocol driven results are limited to short term markers of remission of diabetes, adverse events, and related cardiometabolic outcomes.16 Future long term, well designed, calorie controlled randomized trials are needed to determine the effects of LCD on sustained weight loss and remission of diabetes, as well as cardiovascular mortality and major morbidity.
Seventhly, our review focused on studies defined by macronutrient quantity. Macronutrient quality may also be important, and, although we were unable to consider the characteristics of dietary quality given the lack of reporting in our 23 eligible trials, future trials should better document dietary quality (for example, processed versus unprocessed foods) using optimally validated questionnaires together with emerging objective biomarkers using microbiomics, metabolomics, or other high dimensional platforms.72
Finally, the limited number of trials allowing patients to reduce their medication use impeded our ability to assess remission of diabetes when defined as HbA1c below 6.5% without diabetes medication. Only 7/23 (30%) of eligible trials permitted reduction of medication and reported usable medication data. Future trials should allow for, and adequately report on, reduction of medication while closely monitoring blood glucose concentrations.58 LCDs seem to promote important reductions in HbA1c, potentially increasing risk for hypoglycemic episodes, including severe syncope, if the dosage of diabetes medications is not adjusted accordingly. Because blinding is not possible in these studies, these adjustments should be applied using a priori algorithms that help to guide medication management.47 Reductions in medication may blunt the effect on mean HbA1c levels, biasing results towards the null and masking any effect; however, any improvement can still be captured if reduction of medication is included as an outcome of interest.
Conclusions
Moderate to low certainty evidence suggests that patients adhering to LCDs for six months may experience greater rates of remission of diabetes without adverse consequences compared with other diets commonly recommended for management of type 2 diabetes (for example, low fat diets). These benefits diminished at 12 months, and, although LCDs seem to improve triglycerides in a clinically meaningful way, some evidence shows clinical worsening of quality of life and low density lipoprotein cholesterol. Considering this and a recent systematic review of cohort studies suggesting that long term LCDs are associated with increased mortality,73 clinicians might consider short term LCDs for management of type 2 diabetes, while actively monitoring and adjusting diabetes medication as needed.
What is already known on this topic
Previous systematic reviews have used broad definitions of low carbohydrate (eg, <45% of calories from carbohydrates) and have not systematically assessed remission of diabetes
Results from reviews based on a subgroup of 10 randomized trials assessing low carbohydrate diets (LCDs) (<26-45% of daily calories from carbohydrate) have been encouraging
What this study adds
This systematic review of the effect of LCDs on remission of type 2 diabetes included 23 trials, including unpublished HbA1c and medication use data from five trials
Compared with (mostly low fat) control diets, on the basis of moderate certainty evidence at six months, LCDs were associated with a large (32%) increase in remission of diabetes
According to a priori determined minimal important difference estimates, large and clinically important improvements in weight loss, triglycerides, and insulin resistance were also seen, without adverse events
Acknowledgments
We thank Pamela Dyson for sharing unpublished data and Paria Tajallipour for her assistance with our literature search.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary tables
Contributors: JZG and BCJ conceived the study. JZG, LT, and BCJ designed the study. JZG, JJ, and BCJ developed a priori estimates of the minimal clinically important difference. JB designed and executed the search. JG and AD selected the articles and extracted the data. JZG, AD, and BCJ analyzed the data. JZG and BCJ wrote the first draft of the manuscript. GB, JS, SY, and TJ provided unpublished trial data and reviewed and interpreted the data of the draft manuscript. JZG, BCJ, AD, JB, LT, GB, JS, SY, TJ, and JJ interpreted the data and contributed to the writing of the final version of the manuscript. All authors agreed with the results and conclusions of this article. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. JZG and BCJ are the guarantors.
Funding: This study was funded in part by Texas A&M University. The university had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: support from Texas A&M University; BCJ receives funds from Texas A&M AgriLife Research to support investigator initiated research related to saturated and polyunsaturated fats for a separate research project, as part of his recent recruitment to Texas A&M University (support from Texas A&M AgriLife institutional funds are from interest and investment earnings, not a sponsoring organization, industry, or company); GB is author of the CSIRO Low Carb Diet Book that aims to translate clinical research outcomes of low carbohydrate diet studies for the general public in Australia, but he does not personally receive any financial royalties or funds either directly or indirectly from this publication, and any royalties received by his employment institution (CSIRO) do not contribute to his salary, nor have they been used to execute this work; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not needed. All the work was developed using aggregate level data.
Data sharing: Further data are available on request through the corresponding author at bradley.johnston@tamu.edu.
The lead and senior authors (manuscript’s guarantors) affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: We plan to reach out to diabetes and obesity patient advocacy groups (eg, Obesity Canada) as well as professional medical, nutrition, and agricultural organizations (eg, Practice-based Evidence in Nutrition, Royal Australian College of General Practitioners, USDA) to help to disseminate this work. Additionally, all authors will work with their home institutions to leverage their unique dissemination platforms including social media communication and organizational websites.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 2018;14:88-98. 10.1038/nrendo.2017.151 [DOI] [PubMed] [Google Scholar]
- 2. DeFronzo RA, Ferrannini E, Groop L, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers 2015;1:15019. 10.1038/nrdp.2015.19 [DOI] [PubMed] [Google Scholar]
- 3. American Diabetes Association 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020 . Diabetes Care 2020;43(Suppl 1):S14-31. 10.2337/dc20-S002 [DOI] [PubMed] [Google Scholar]
- 4. Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: A consensus report. Diabetes Care 2019;42:731-54. 10.2337/dci19-0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Westman EC, Vernon MC. Has carbohydrate-restriction been forgotten as a treatment for diabetes mellitus? A perspective on the ACCORD study design. Nutr Metab (Lond) 2008;5:10. 10.1186/1743-7075-5-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Volek JS, Fernandez ML, Feinman RD, Phinney SD. Dietary carbohydrate restriction induces a unique metabolic state positively affecting atherogenic dyslipidemia, fatty acid partitioning, and metabolic syndrome. Prog Lipid Res 2008;47:307-18. 10.1016/j.plipres.2008.02.003 [DOI] [PubMed] [Google Scholar]
- 7. Feinman RD, Pogozelski WK, Astrup A, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition 2015;31:1-13. 10.1016/j.nut.2014.06.011 [DOI] [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention (CDC) Trends in intake of energy and macronutrients--United States, 1971-2000. MMWR Morb Mortal Wkly Rep 2004;53:80-2. [PubMed] [Google Scholar]
- 9.International Diabetes Federation. Diabetes Atlas. 9th edition. 2019. https://diabetesatlas.org/en/.
- 10. Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014;37(Suppl 1):S120-43. 10.2337/dc14-S120 [DOI] [PubMed] [Google Scholar]
- 11. Mozaffarian D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016;133:187-225. 10.1161/CIRCULATIONAHA.115.018585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr 2013;97:505-16. 10.3945/ajcn.112.042457 [DOI] [PubMed] [Google Scholar]
- 13. Snorgaard O, Poulsen GM, Andersen HK, Astrup A. Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res Care 2017;5:e000354. 10.1136/bmjdrc-2016-000354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Naude CE, Schoonees A, Senekal M, Young T, Garner P, Volmink J. Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: a systematic review and meta-analysis. PLoS One 2014;9:e100652. 10.1371/journal.pone.0100652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sainsbury E, Kizirian NV, Partridge SR, Gill T, Colagiuri S, Gibson AA. Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: A systematic review and meta-analysis. Diabetes Res Clin Pract 2018;139:239-52. 10.1016/j.diabres.2018.02.026 [DOI] [PubMed] [Google Scholar]
- 16.Goldenberg JZ, Day A, Beardsley J, Thabane L, Johnston BC. Very low carbohydrate diets for type 2 diabetes: a systematic review and meta-analysis. 2020. https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=161795. [DOI] [PMC free article] [PubMed]
- 17. Guyatt GH, Juniper EF, Walter SD, Griffith LE, Goldstein RS. Interpreting treatment effects in randomised trials. BMJ 1998;316:690-3. 10.1136/bmj.316.7132.690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Johnston BC, Alonso-Coello P, Friedrich JO, et al. Do clinicians understand the size of treatment effects? A randomized survey across 8 countries. CMAJ 2016;188:25-32. 10.1503/cmaj.150430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 Cochrane Collaboration, 2011. [Google Scholar]
- 20. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 21. da Costa BR, Nüesch E, Rutjes AW, et al. Combining follow-up and change data is valid in meta-analyses of continuous outcomes: a meta-epidemiological study. J Clin Epidemiol 2013;66:847-55. 10.1016/j.jclinepi.2013.03.009 [DOI] [PubMed] [Google Scholar]
- 22. Thorlund K, Walter SD, Johnston BC, Furukawa TA, Guyatt GH. Pooling health-related quality of life outcomes in meta-analysis-a tutorial and review of methods for enhancing interpretability. Res Synth Methods 2011;2:188-203. 10.1002/jrsm.46 [DOI] [PubMed] [Google Scholar]
- 23. Guyatt GH, Thorlund K, Oxman AD, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles-continuous outcomes. J Clin Epidemiol 2013;66:173-83. 10.1016/j.jclinepi.2012.08.001 [DOI] [PubMed] [Google Scholar]
- 24. Guyatt GH, Ebrahim S, Alonso-Coello P, et al. GRADE guidelines 17: assessing the risk of bias associated with missing participant outcome data in a body of evidence. J Clin Epidemiol 2017;87:14-22. 10.1016/j.jclinepi.2017.05.005 [DOI] [PubMed] [Google Scholar]
- 25. Guyatt GH, Oxman AD, Vist GE, et al. GRADE Working Group GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924-6. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schünemann H, Brożek J, Guyatt G, Oxman A. Handbook for Grading the Quality of Evidence And the Strength of Recommendation Using the GRADE Approach. 2013. https://gdt.gradepro.org/app/handbook/handbook.html.
- 27. Schwingshackl L, Knüppel S, Schwedhelm C, et al. Perspective: NutriGrade: A scoring system to assess and judge the meta-evidence of randomized controlled trials and cohort studies in nutrition research. Adv Nutr 2016;7:994-1004. 10.3945/an.116.013052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ebrahim S, Akl EA, Mustafa RA, et al. Addressing continuous data for participants excluded from trial analysis: a guide for systematic reviewers. J Clin Epidemiol 2013;66:1014-1021.e1. 10.1016/j.jclinepi.2013.03.014 [DOI] [PubMed] [Google Scholar]
- 29. Akl EA, Kahale LA, Agoritsas T, et al. Handling trial participants with missing outcome data when conducting a meta-analysis: a systematic survey of proposed approaches. Syst Rev 2015;4:98. 10.1186/s13643-015-0083-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Higgins JPT, Thomas J, Chandler J, et al. , eds. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed Wiley Blackwell, 2019. 10.1002/9781119536604 . [DOI] [Google Scholar]
- 31. Sun X, Ioannidis JPA, Agoritsas T, Alba AC, Guyatt G. How to use a subgroup analysis: users’ guide to the medical literature. JAMA 2014;311:405-11. 10.1001/jama.2013.285063 [DOI] [PubMed] [Google Scholar]
- 32. Harbord RM, Egger M, Sterne JAC. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med 2006;25:3443-57. 10.1002/sim.2380 [DOI] [PubMed] [Google Scholar]
- 33. Sterne JAC, Sutton AJ, Ioannidis JPA, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002. 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 34.Dyson PA. Dietary advice for people with diabetes: the role of carbohydrate in dietary treatment and an assessment of video education. 2010. https://radar.brookes.ac.uk/radar/items/c0e6a243-1e36-4820-806d-d3a1c1724266/1/.
- 35. Morris E, Aveyard P, Dyson P, et al. A food-based, low-energy, low-carbohydrate diet for people with type 2 diabetes in primary care: A randomized controlled feasibility trial. Diabetes Obes Metab 2020;22:512-20. 10.1111/dom.13915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Saslow LR, Kim S, Daubenmier JJ, et al. A randomized pilot trial of a moderate carbohydrate diet compared to a very low carbohydrate diet in overweight or obese individuals with type 2 diabetes mellitus or prediabetes. PLoS One 2014;9:e91027. 10.1371/journal.pone.0091027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Saslow LR, Mason AE, Kim S, et al. An online intervention comparing a very low-carbohydrate ketogenic diet and lifestyle recommendations versus a plate method diet in overweight individuals with type 2 diabetes: A randomized controlled trial. J Med Internet Res 2017;19:e36. 10.2196/jmir.5806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yamada Y, Uchida J, Izumi H, et al. A non-calorie-restricted low-carbohydrate diet is effective as an alternative therapy for patients with type 2 diabetes. Intern Med 2014;53:13-9. 10.2169/internalmedicine.53.0861 [DOI] [PubMed] [Google Scholar]
- 39. Tay J, Luscombe-Marsh ND, Thompson CH, et al. A very low-carbohydrate, low-saturated fat diet for type 2 diabetes management: a randomized trial. Diabetes Care 2014;37:2909-18. 10.2337/dc14-0845 [DOI] [PubMed] [Google Scholar]
- 40. Jönsson T, Granfeldt Y, Ahrén B, et al. Beneficial effects of a Paleolithic diet on cardiovascular risk factors in type 2 diabetes: a randomized cross-over pilot study. Cardiovasc Diabetol 2009;8:35. 10.1186/1475-2840-8-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sato J, Kanazawa A, Makita S, et al. A randomized controlled trial of 130 g/day low-carbohydrate diet in type 2 diabetes with poor glycemic control. Clin Nutr 2017;36:992-1000. 10.1016/j.clnu.2016.07.003 [DOI] [PubMed] [Google Scholar]
- 42. Goldstein T, Kark JD, Berry EM, Adler B, Ziv E, Raz I. The effect of a low carbohydrate energy-unrestricted diet on weight loss in obese type 2 diabetes patients - A randomized controlled trial. e-SPEN 2011;6:e178-86 10.1016/j.eclnm.2011.04.003 . [DOI] [Google Scholar]
- 43. Guldbrand H, Dizdar B, Bunjaku B, et al. In type 2 diabetes, randomisation to advice to follow a low-carbohydrate diet transiently improves glycaemic control compared with advice to follow a low-fat diet producing a similar weight loss. Diabetologia 2012;55:2118-27. 10.1007/s00125-012-2567-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Iqbal N, Vetter ML, Moore RH, et al. Effects of a low-intensity intervention that prescribed a low-carbohydrate vs. a low-fat diet in obese, diabetic participants. Obesity (Silver Spring) 2010;18:1733-8. 10.1038/oby.2009.460 [DOI] [PubMed] [Google Scholar]
- 45. Nishimori E, Tetsu O, Takasugi K, et al. Carbohydrate-restricted diet is a non-alcoholic fatty liver disease associated with type 2 diabetes Improve calorie-restricted diet. Diabetes 2018;61:297-306. [Google Scholar]
- 46. Vlachos D, Ganotopoulou A, Stathi C, et al. A low-carbohydrate protein sparing modified fast diet compared with a low glycaemic index reduced calorie diet in obese type 2 diabetic patients. Diabetologia 2011;54(supplement 1):S355. [Google Scholar]
- 47. Westman EC, Yancy WS, Jr, Mavropoulos JC, Marquart M, McDuffie JR. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab (Lond) 2008;5:36. 10.1186/1743-7075-5-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Asle Mohammadi Zadeh M, Kargarfard M, Marandi SM, Habibi A. Diets along with interval training regimes improves inflammatory & anti-inflammatory condition in obesity with type 2 diabetes subjects. J Diabetes Metab Disord 2018;17:253-67. 10.1007/s40200-018-0368-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Daly ME, Paisey R, Paisey R, et al. Short-term effects of severe dietary carbohydrate-restriction advice in Type 2 diabetes--a randomized controlled trial. Diabet Med 2006;23:15-20. 10.1111/j.1464-5491.2005.01760.x [DOI] [PubMed] [Google Scholar]
- 50. Davis NJ, Tomuta N, Schechter C, et al. Comparative study of the effects of a 1-year dietary intervention of a low-carbohydrate diet versus a low-fat diet on weight and glycemic control in type 2 diabetes. Diabetes Care 2009;32:1147-52. 10.2337/dc08-2108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yancy WS, Jr, Westman EC, McDuffie JR, et al. A randomized trial of a low-carbohydrate diet vs orlistat plus a low-fat diet for weight loss. Arch Intern Med 2010;170:136-45. 10.1001/archinternmed.2009.492 [DOI] [PubMed] [Google Scholar]
- 52. Samaha FF, Iqbal N, Seshadri P, et al. A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med 2003;348:2074-81. 10.1056/NEJMoa022637 [DOI] [PubMed] [Google Scholar]
- 53. Shai I, Schwarzfuchs D, Henkin Y, et al. Dietary Intervention Randomized Controlled Trial (DIRECT) Group Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med 2008;359:229-41. 10.1056/NEJMoa0708681 [DOI] [PubMed] [Google Scholar]
- 54. Lee P, Paisey R, Waterson M, et al. Reduction in High Sensitivity C-reactive Protein levels in type 2 diabetes after low carbohydrate but not energy deficit diet. Diabet Med 2013;30(Suppl 1):47. [Google Scholar]
- 55. Breukelman GJ, Basson AK, Djarova TG, Du Preez CJ, Shaw I, Shaw BS. Combination low carbohydrate, high fat diet and physical activity intervention on lipoprotein-lipids in type 2 diabetics. Asian J Sports Med 2019;10:e86905 10.5812/asjsm.86905 . [DOI] [Google Scholar]
- 56. Perna S, Alalwan TA, Gozzer C, et al. Effectiveness of a hypocaloric and low-carbohydrate diet on visceral adipose tissue and glycemic control in overweight and obese patients with type 2 diabetes. Bahrain Med Bull 2019;41:159-64. [Google Scholar]
- 57. Korsmo-Haugen HK, Brurberg KG, Mann J, Aas AM. Carbohydrate quantity in the dietary management of type 2 diabetes: A systematic review and meta-analysis. Diabetes Obes Metab 2019;21:15-27. 10.1111/dom.13499 [DOI] [PubMed] [Google Scholar]
- 58. Sato J, Kanazawa A, Hatae C, et al. One year follow-up after a randomized controlled trial of a 130 g/day low-carbohydrate diet in patients with type 2 diabetes mellitus and poor glycemic control. PLoS One 2017;12:e0188892. 10.1371/journal.pone.0188892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. van Zuuren EJ, Fedorowicz Z, Kuijpers T, Pijl H. Effects of low-carbohydrate- compared with low-fat-diet interventions on metabolic control in people with type 2 diabetes: a systematic review including GRADE assessments. Am J Clin Nutr 2018;108:300-31. 10.1093/ajcn/nqy096 [DOI] [PubMed] [Google Scholar]
- 60. Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care 2009;32:2133-5. 10.2337/dc09-9036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Johnston BC, Guyatt GH. Best (but oft-forgotten) practices: intention-to-treat, treatment adherence, and missing participant outcome data in the nutrition literature. Am J Clin Nutr 2016;104:1197-201. 10.3945/ajcn.115.123315 [DOI] [PubMed] [Google Scholar]
- 62. Batterham MJ, Tapsell LC, Charlton KE. Analyzing weight loss intervention studies with missing data: which methods should be used? Nutrition 2013;29:1024-9. 10.1016/j.nut.2013.01.017 [DOI] [PubMed] [Google Scholar]
- 63. Tay J, de Bock MI, Mayer-Davis EJ. Low-carbohydrate diets in type 2 diabetes. Lancet Diabetes Endocrinol 2019;7:331-3. 10.1016/S2213-8587(18)30368-1 [DOI] [PubMed] [Google Scholar]
- 64. Meerpohl JJ, Naude CE, Garner P, Mustafa RA, Schünemann HJ. Comment on “Perspective: NutriGrade: A Scoring System to Assess and Judge the Meta-Evidence of Randomized Controlled Trials and Cohort Studies in Nutrition Research”. Adv Nutr 2017;8:789-90. 10.3945/an.117.016188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Giovannucci E, Rimm E. Red and processed meat consumption and risk for all-cause mortality and cardiometabolic outcomes. Ann Intern Med 2020;172:510-1. 10.7326/L20-0069 [DOI] [PubMed] [Google Scholar]
- 66. Schwingshackl L, Knüppel S, Schwedhelm C, et al. Reply to JJ Meerpohl et al. Adv Nutr 2017;8:790-1. 10.3945/an.117.016469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Giovannucci E, Rimm E. Red and processed meat consumption and risk for all-cause mortality and cardiometabolic outcomes. Ann Intern Med 2020;172:510-1. 10.7326/L20-0069 [DOI] [PubMed] [Google Scholar]
- 68. Crowe TC. Safety of low-carbohydrate diets. Obes Rev 2005;6:235-45. 10.1111/j.1467-789X.2005.00196.x [DOI] [PubMed] [Google Scholar]
- 69. Gibson AA, Seimon RV, Lee CMY, et al. Do ketogenic diets really suppress appetite? A systematic review and meta-analysis. Obes Rev 2015;16:64-76. 10.1111/obr.12230 [DOI] [PubMed] [Google Scholar]
- 70. Archer E, Marlow ML, Lavie CJ. Controversy and debate: Memory-Based Methods Paper 1: the fatal flaws of food frequency questionnaires and other memory-based dietary assessment methods. J Clin Epidemiol 2018;104:113-24. 10.1016/j.jclinepi.2018.08.003 [DOI] [PubMed] [Google Scholar]
- 71. Brakenhoff TB, van Smeden M, Visseren FLJ, Groenwold RHH. Random measurement error: Why worry? An example of cardiovascular risk factors. PLoS One 2018;13:e0192298. 10.1371/journal.pone.0192298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Prentice RL. Dietary assessment and opportunities to enhance nutritional epidemiology evidence. Ann Intern Med 2020;172:354-5. 10.7326/M19-3290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Seidelmann SB, Claggett B, Cheng S, et al. Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. Lancet Public Health 2018;3:e419-28. 10.1016/S2468-2667(18)30135-X [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary tables