Key Points
Question
Does surgical treatment of wrist fractures with volar-locking plates in patients 60 years and older provide superior patient-reported wrist pain and function at 12 months after treatment compared with nonsurgical treatment?
Findings
In this randomized clinical trial and parallel observational study of 300 participants (166 who were randomized to surgical or nonsurgical treatment and 134 who declined randomization), no clinically important difference was found in wrist pain and function at 12 months in those who received surgical vs nonsurgical treatment.
Meaning
In older patients, surgical treatment with volar-locking plates provided no important functional advantages over nonsurgical treatment at 12 months.
Abstract
Importance
The burden of injury and costs of wrist fractures are substantial. Surgical treatment became popular without strong supporting evidence.
Objective
To assess whether current surgical treatment for displaced distal radius fractures provided better patient-reported wrist pain and function than nonsurgical treatment in patients 60 years and older.
Design, Setting, and Participants
In this multicenter randomized clinical trial and parallel observational study, 300 eligible patients were screened from 19 centers in Australia and New Zealand from December 1, 2016, until December 31, 2018. A total of 166 participants were randomized to surgical or nonsurgical treatment and followed up at 3 and 12 months by blinded assessors. Those 134 individuals who declined randomization were included in a parallel observational cohort with the same treatment options and follow-up. The primary analysis was intention to treat; sensitivity analyses included as-treated and per-protocol analyses.
Intervention
Surgical treatment was open reduction and internal fixation using a volar-locking plate (VLP). Nonsurgical treatment was closed reduction and cast immobilization (CR).
Main Outcomes and Measures
The primary outcome was the Patient-Rated Wrist Evaluation score at 12 months. Secondary outcomes were Disabilities of Arm, Shoulder, and Hand questionnaire score, health-related quality of life, pain, major complications, patient-reported treatment success, bother with appearance, and therapy use.
Results
In the 300 study participants (mean [SD] age, 71.2 [7.5] years; 269 [90%] female; 166 [81 VLP and 85 CR] in the randomized clinical trial sample and 134 [32 VLP and 102 CR] in the observational sample), no clinically important between-group difference in 12-month Patient-Rated Wrist Evaluation scores (mean [SD] score of 19.8 [21.1] for VLP and 21.5 [24.3] for CR; mean difference, 1.7 points; 95% CI −5.4 to 8.8) was observed. No clinically important differences were found in quality of life, wrist pain, or bother at 3 and 12 months. No significant difference was found in total complications between groups (12 of 84 [14%] for the CR group vs 6 of 80 [8%] for the VLP group; risk ratio [RR], 0.53; 95% CI, 0.21-1.33). Patient-reported treatment success favored the VLP group at 12 months (very successful or successful: 70 [89%] vs 57 [70%]; RR, 1.26; 95% CI, 1.07-1.48; P = .005). There was greater use of postoperative physical therapy in the VLP group (56 [72%] vs 44 [54%]; RR, 1.32; 95% CI, 1.04-1.69; P = 0.02).
Conclusions and Relevance
This randomized clinical trial found no between-group differences in improvement in wrist pain or function at 12 months from VLP fixation over CR for displaced distal radius fractures in older people.
Trial Registration
http://anzctr.org.au identifier: ACTRN12616000969460
This randomized clinical trial and parallel observational study assesses whether current surgical treatment for displaced distal radius fractures provided better patient-reported wrist pain and function than nonsurgical treatment in patients 60 years and older.
Introduction
Wrist fractures are 1 of the most common fracture types.1 Incidence peaks in older people because of osteoporosis and increased risk of falls, and the incidence is increasing.1,2 Wrist fractures in older people represent a patient and societal burden by way of functional decline3 and cost to health systems. In Australia, annual direct costs from osteoporotic wrist fractures have been estimated to be more than A$130 million dollars.4 In the US, Medicare alone paid $170 million in wrist fracture–related payments for older patients in 2007.5
The 2 most common treatments for wrist fracture are nonsurgical treatment by closed reduction and cast immobilization (CR) and surgical treatment by open reduction and fracture fixation using a volar-locking plate (VLP).6 Volar-locking plate fixation has become the most common surgical treatment,7 with the rate of use in older people increasing substantially in the past 2 decades.1,5,7,8,9 The increase in VLP fixation has coincided with considerable practice variation in the management of wrist fractures in older people,6,8,10,11,12 with choice of treatment as likely to be determined by surgeon preference and patient expectations as by best available evidence.12 The cost differential between VLP fixation and CR has been estimated to be 10-fold.7 The cost burden is expected to accelerate with an aging population and increasing use of surgical treatment.5
Although research suggests no significant advantages for some forms of surgical fixation over CR and no differences among surgical techniques,13,14,15,16,17,18,19,20,21,22,23,24 evidence exclusively comparing CR with VLP fixation in older patients is limited.14,25,26,27 Studies16,28 comparing the safety of surgical and nonsurgical treatments of wrist fracture in older patients have found significantly higher rates of major complications with surgical treatments. Two recent systematic reviews28,29 comparing CR with VLP fixation found no clinically important difference in functional outcomes at 12 months. High-level evidence is required to guide treatment that provides the best clinical outcome and that justifies or avoids treatment costs and risks of harm.
The primary aim of this study was to assess whether, for adults 60 years or older with dorsally angulated, displaced distal radius fractures, VLP fixation was superior to CR with respect to patient-reported pain and function at 12 months after treatment. Secondary aims were to determine whether VLP fixation was superior to CR at 3 months and whether there were between-group differences in safety, treatment success, bother, and therapy use.
Methods
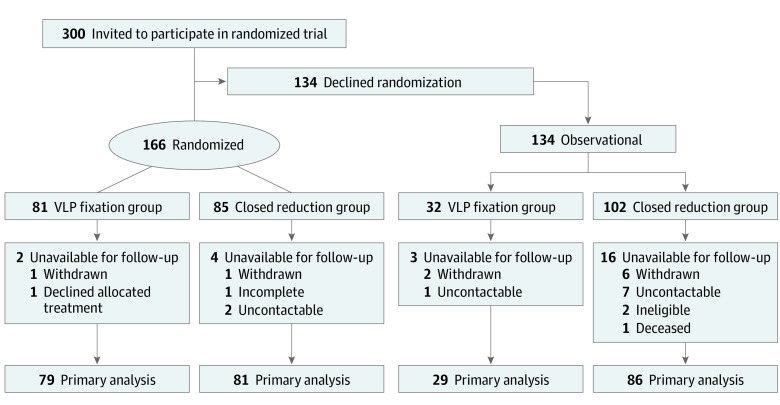
From December 1, 2016, until December 31, 2018, we screened 300 eligible patients; 166 consented to the randomized clinical trial (RCT) and 134 consented to be included in the observational cohort. The CONSORT flowchart is presented in Figure 1. This study, the Combined Randomised and Observational Study of Surgery for Fractures in the Distal Radius in the Elderly (CROSSFIRE), was approved by the Hunter New England Human Research Ethics Committee. The trial was prospectively registered, the protocol was published in 2017,30 and the statistical analysis plan was published in 2020.31 (The study protocol is available in Supplement 1, and the statistical analysis plan is available in Supplement 2.) The Australia and New Zealand Musculoskeletal (ANZMUSC) Clinical Trials Network endorsed the trial. The ANZMUSC Scientific Advisory Committee and Consumer Advisory Group reviewed and approved the protocol. Separately, 3 patients with wrist fracture (not study participants) were interviewed regarding what posttreatment information was most relevant and important to such patients. All study participants provided written informed consent. The data set was deidentified. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines.32
Figure 1. CONSORT Flow Diagram .
VLP indicates volar-locking plate.
Design
We conducted a pragmatic, multicenter study that recruited participants from 19 sites across Australia and New Zealand. Eligible patients were invited to participate in the RCT. Treatment was randomized to surgical (VLP) fixation or nonsurgical treatment (CR) at a 1:1 ratio; those who declined participation in the RCT were invited to join an observational cohort. Participants in the observational cohort received 1 of the 2 treatments in the RCT according to patient and surgeon preference, and follow-up was identical to that in the RCT. The inclusion of an observational cohort was to investigate potential sampling bias and provide information on the generalizability of the RCT results.33 This study design has been used in surgical trials34,35 and has been recommended as a model for trials of surgery vs nonsurgical treatment in which recruitment rates are expected to be lower than for other RCTs.36
Participants
Potential participants presenting to 1 of our recruitment sites for the treatment of a wrist fracture were eligible if they were 60 years or older; presented within 1 week of injury with a distal radius fracture, classified according to the Association for the Study of Internal Fixation/Orthopaedic Trauma Association (AO/OTA)37 23A (extra-articular) or 23C (complete articular); demonstrated initial fracture displacement greater than 10° dorsal angulation, greater than 3-mm shortening, or greater than 2-mm articular step; were medically fit for surgery; were living independently; had a low-energy injury (fall from <1 m); and were available for follow-up. Patients were ineligible if they met any of the following criteria: inability to provide informed consent (because of cognitive capacity or English proficiency), fracture with volar angulation or diaphyseal extension or partial articular fracture (AO/OTA 23B), associated injury in any other body part that affected the use of the involved wrist, open fracture, or previous ipsilateral wrist fracture.
Randomization and Blinding
Eligible consenting participants were randomized using an automated telephone-based computerized randomization system. Randomization was stratified by site, using the technique of minimization,38 to balance sex and age (≤74 and >74 years).
Surgeon investigators (Z.J.B., P.S., R.M., P.Y., B.R., G.S., S.A., I.E., W.K., J.S., K.Latendresse., J.W., S.V., K.Landale., H.D., P.T., R.P., S.B., J.M., I.I., M.K., B.S., T.L., A.H., and A.O.) and participants were not blinded. Collection of outcomes was performed by telephone by blinded researchers (A.L. and S.C.). The statistician and the investigators (A.L., W.X., and I.A.H.) conducting the analysis remained blinded to treatment groups. Treatment allocation was masked using dummy intervention group names. Masking of treatment allocation was maintained until statistical analysis and interpretation was agreed to by all authors.
Interventions
The intervention was surgical treatment by open reduction and VLP fixation, performed within 2 weeks of initial injury according to the usual protocol of the participating institution, with an orthopedic surgeon in attendance. Surgical technique and type of plate (make and length) were per surgeon preference. A plaster splint was applied postoperatively for no longer than 2 weeks. Active finger movement was encouraged postoperatively. Participants were reviewed approximately 2 weeks (range, 10-17 days) after surgery; the wound was reviewed, the splint removed, and sutures removed where necessary.
The control was CR within 2 weeks of initial injury. The CR was performed by a member of the orthopedic service in the emergency department with the patient under sedation and local anesthetic infiltration administered into the fracture (hematoma block) where possible; otherwise, the CR was performed in an operating room. Casting avoided wrist flexion, consistent with standard casting practice, to reduce the risk of posttreatment complications, such as complex regional pain syndrome (CRPS). The best reduction achievable was accepted. Active finger movement and light hand use were encouraged immediately. The cast was removed at a mean of 6 (±1) weeks from the initial reduction.
In both groups, participants were provided with a printed home-exercise program (eAppendix 1 in Supplement 3). Although the evidence that supports ongoing physical therapy is uncertain,39,40 referral to outpatient therapy was not routinely provided but was permitted.
Outcome Variables
Baseline data included age, sex, fracture type (AO/OTA 23A or 23C), fracture healing risk factors (Table 1 and eAppendix 2 in Supplement 3), treatment preference, and quality of life (Table 1). Data collection was paper based, and collected data were forwarded to the study coordinator (A.V.) for direct electronic data entry into a central electronic database (Research Electronic Data Capture [REDCap]).41
Table 1. Baseline Characteristics for the Randomized Clinical Trial Cohorta .
| Characteristic | CR (n = 85) | VLP fixation (n = 81) |
|---|---|---|
| Age, mean (SD) [range], y | 71.3 (7.6) [60-90] | 70.5 (7.0) [60-86] |
| Female | 75 (88) | 70 (86) |
| Fracture type | ||
| 23A | 49 (58) | 55 (68) |
| 23C | 35 (42) | 26 (32) |
| Comorbidities | ||
| Diabetes | 9 (11) | 10 (12) |
| Smoker | 3 (4) | 1 (1) |
| Glucocorticoid treatment | 10 (12) | 10 (12) |
| Osteoporosis treatment | 10 (12) | 10 (12) |
| Treatment preference | ||
| Surgery | 5 (6) | 10 (13) |
| CR | 24 (28) | 25 (32) |
| No preference | 56 (66) | 44 (56) |
| EQ-5D-5L score, mean (SD) | ||
| Index | 0.89 (0.14) | 0.85 (0.19) |
| EQ-VAS | 83.6 (14.4) | 81.1 (17.4) |
Abbreviations: CR, closed reduction and cast immobilization; EQ-5D-5L, EuroQol 5-dimension 5-level; EQ-VAS, EuroQol visual analog scale; VLP, volar-locking plate.
Data are presented as number (percentage) of patients unless otherwise indicated.
The primary outcome was the score on the Patient-Rated Wrist Evaluation (PRWE) questionnaire administered 12 (±1) months after injury. The PRWE is a wrist-specific, 15-item, patient-reported measure of pain and function. It uses a continuous score converted to a 0- to 100-point scale, with higher scores indicating poorer outcomes.42 It is commonly used, was developed with patient input, and has been validated for use in patients with distal radius fractures.43 We considered 14 points on the PRWE to be the minimal clinically important difference (MCID) necessary to justify the additional costs and risks of surgery compared with nonsurgical treatment.44
Secondary outcomes are as follows (eAppendix 2 in Supplement 3), with a full description of each outcome provided in the published protocol29: PRWE score at 3 months; Disability of Arm, Shoulder, and Hand questionnaire score at 12 months (MCID, 10 points)44; utility-based quality of life at 3 and 12 months based on the EuroQol 5-dimension 5-level (EQ-5D-5L) score, with baseline EQ-5D-5L assessed in retrospect of the initial injury (retrospective use of EQ-5D-5L has been validated45; MCID, 0.074 for EQ utility index scores and 10.8 points for EQ visual analogue scores46); wrist pain using a numeric rating scale (scale of 0-10 points, with 0 indicating no pain and 10 indicating maximal pain) at 3 and 12 months (MCID, 1.7 points based on the median of a systematic review of MCIDs for pain scales)47; patient-reported treatment success at 3 and 12 months measured on a Likert scale, ranging from very successful to very unsuccessful (eAppendix 3 in Supplement 3); patient-rated bother with appearance at 12 months (eAppendix 3 in Supplement 3) (the bother question has been assessed for reliability in wrist fractures48); complications (including deep infection, reoperation, neuropathy, tendon irritation that required treatment, tendon rupture, fracture nonunion at 6 months, implant failure, CRPS, and death) at 3 and 12 months (CRPS was defined according to the International Association for the Study of Pain clinical diagnosis criteria,49 and we report risk ratios [RRs] instead of [the planned] odds ratios because these are more readily understood and interpreted); and physical therapy use up to 3 months (yes/no) and continuing at 3 months (yes/no). Outcomes were used to conduct 2 separate analyses: an economic analysis and an analysis of radiographic findings. Participant follow-up at 3 months (±1 week) and 12 months (±1 month) was conducted by telephone.
Statistical Analysis
A sample size of 160 patients (80 in each group) would provide 90% power to detect a mean (SD) difference of 14.0 (22.7) points on the PRWE scale at a significance level of P < .05, allowing 20% unavailability for follow-up. Two previous RCTs14,25 had published results at the time of our sample size calculation, and each reported unavailability for follow-up rates of 19%. The observational cohort included all eligible patients not consenting to randomization. The RCT and observational cohorts were analyzed separately.
Data were analyzed on an intention-to-treat (ITT) principle, and sensitivity analyses were performed using as-treated and per-protocol analyses. Further details of the statistical analysis are provided in the statistical analysis plan31 (also see Supplement 2). Data were analyzed with SAS statistical software (SAS Institute Inc) and R statistical computing software (R Foundation for Statistical Computing).50
Results
A total of 300 patients (mean [SD] age, 71.2 [7.5] years; 269 [90%] female; 166 [81 VLP and 85 CR] in the RCT sample and 134 [32 VLP and 102 CR] in the observational sample) participated in this study. Baseline characteristics of the 2 treatment groups in the RCT were similar (Table 1). The ITT analysis for the RCT is reported below. Sensitivity analyses are in eAppendix 4 in Supplement 3.
Patient-Reported Outcomes
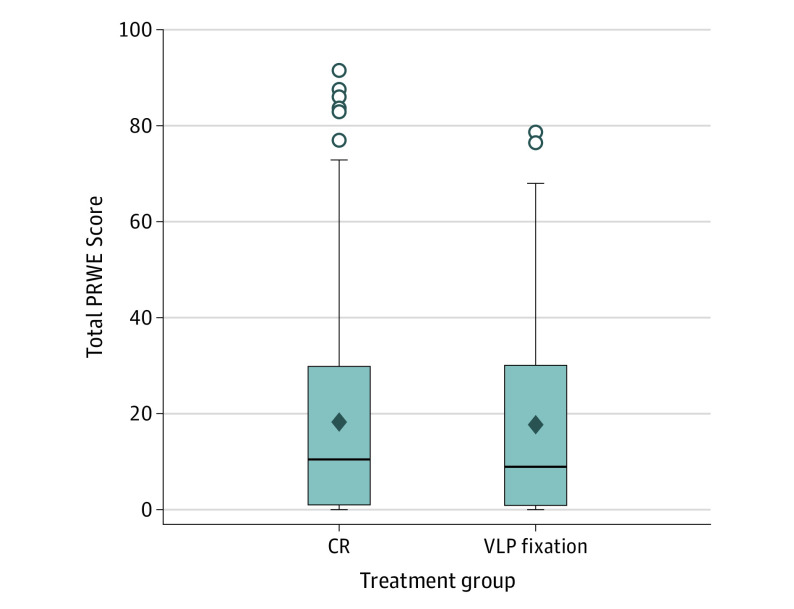
Data were not imputed because the follow-up rate (96%) was above the prespecified threshold. In the RCT, no clinically important between-group difference was found in patient-reported wrist pain and function at 3 and 12 months. At 12 months, mean (SD) PRWE scores were 19.8 (21.1) for VLP fixation compared with 21.5 (24.3) for CR (mean difference [MD], 1.7 points; 95% CI, –5.4 to 8.8 points) (Table 2 and Figure 2). In the multivariate analysis, adjustment for age and sex revealed no significant difference in PRWE score at 12 months between the 2 groups. In addition, no difference in pain was found on the numerical rating scale at 12 months: mean (SD), 1.1 (2.2) for VLP and 1.0 (2.1) for CR; MD, −0.1; 95% CI, −0.8 to 0.6. At 3 months, mean (SD) PRWE scores were 28.1 (23.1) for VLP fixation and 37.1 (22.3) for CR (MD, 9 points; 95% CI, 1.8-16.2) (Table 2 and eAppendix 5 in Supplement 3).
Table 2. Primary and Secondary Outcomes at 3 and 12 Months for the Randomized Clinical Trial Cohorta.
| Outcome | 3 mo | 12 mo | ||||
|---|---|---|---|---|---|---|
| CR (n = 85) | VLP fixation (n = 79) | MD (95% CI), RRb (95% CI), or P value | CR (n = 85) | VLP fixation (n = 79) | MD (95% CI), RRb (95% CI), or P value | |
| PRWE score, mean (SD) | 37.1 (22.3) | 28.1 (23.1) | 9 (1.8 to 16.2) | 21.5 (24.3) | 19.8 (21.1) | 1.7 (–5.4 to 8.8) |
| DASH score, mean (SD) | NA | NA | NA | 19.6 (21) | 18.7 (20.1) | 0.9 (–5.6 to 7.4) |
| EQ-5D-5L score, mean (SD) | ||||||
| Index | 0.70 (0.24) | 0.74 (0.24) | –0.03 (–0.10 to 0.04) | 0.70 (0.23) | 0.69 (0.22) | 0.01 (–0.06 to 0.08) |
| EQ-VAS | 76.0 (17.7) | 74.2 (21.2) | 1.8 (–4.3 to 7.9) | 73.9 (21.5) | 72.6 (19.3) | 1.4 (−5.0 to 7.7) |
| Pain on NRS (0- to 10-point scale) | 1.5 (2.5) | 1.1 (1.9) | 0.5 (−0.2 to 1.1) | 1.0 (2.1) | 1.1 (2.2) | –0.1 (–0.8 to 0.6) |
| Patient-reported treatment success | ||||||
| Very successful | 21 (26) | 33 (44) | .10 | 27 (33) | 42 (53) | .03 |
| Successful | 33 (41) | 28 (37) | 30 (37) | 28 (35) | ||
| Neutral | 14 (18) | 5 (7) | 9 (11) | 4 (5) | ||
| Unsuccessful | 6 (8) | 5 (7) | 12 (15) | 5 (6) | ||
| Very unsuccessful | 6 (8) | 4 (5) | 3 (4) | 0 | ||
| Patient-reported bother with appearance | ||||||
| Not at all | NA | NA | NA | 64 (79) | 69 (90) | .16 |
| Bothered a little | NA | NA | NA | 10 (12) | 7 (9) | |
| Bothered moderately | NA | NA | NA | 6 (8) | 1 (1) | |
| Very bothered | NA | NA | NA | 1 (1) | 0 | |
| Extremely bothered | NA | NA | NA | 0 | 0 | |
| Therapy use | ||||||
| Up to 3 mo | 44 (54) | 56 (72) | 1.32 (1.04 to 1.69) | NA | NA | NA |
| At 3 mo | 26 (59) | 22 (39) | 0.65 (0.43 to 0.98) | NA | NA | NA |
Abbreviations: CR, closed reduction and cast immobilization; DASH, Disabilities of Arm, Shoulder, and Hand; EQ-5D-5L, EuroQol 5-dimension 5-level; EQ-VAS, EuroQol visual analog scale; MD, mean difference; NA, not applicable; NRS, numerical rating scale; PRWE, Patient-Rated Wrist Evaluation; RR, risk ratio; VLP, volar-locking plate.
Data are presented as number (percentage) of patients unless otherwise indicated.
Risk ratios are expressed as VLP fixation vs CR.
Figure 2. Distribution of Patient-Rated Wrist Evaluation (PRWE) Scores at 12 Months .
Horizontal line indicates median; error bars, interquartile ranges; open circles, outlier PRWE scores; and open diamonds, mean PRWE scores. CR indicates closed reduction and cast immobilization; VLP, volar-locking plate.
Patient-reported treatment success favored VLP fixation at 12 months (27 [33%] in the CR group vs 42 [53%] in the VLP group; P = .03) (Table 2). Overall treatment success (very successful and successful) was higher for VLP fixation at 3 months: 61 (81%) vs 54 (67%); RR, 1.2; 95% CI, 1.00-1.45; P = .05, and at 12 months: 70 (89%) vs 57 (70%); RR, 1.26; 95% CI, 1.07-1.48; P = .005 (eAppendix 6 in Supplement 3). No other significant between-group differences were found in any other clinical outcomes.
A significant difference was found between treatment groups in the rate of therapy use in the 3 months after treatment, with 56 (72%) of the VLP fixation group receiving therapy compared with 44 (54%) in the CR treatment group (RR, 1.32; 95% CI, 1.04-1.69) (Table 2).
Complications
A total of 12 complications occurred in the CR group compared with 6 in the VLP fixation group (RR, 0.53; 95% CI, 0.21-1.33) (Table 3). Complications led to additional operations in 8 participants, 6 in the CR group and 2 in the VLP fixation group (RR, 0.35; 95% CI, 0.07-1.68). The incidence of fracture nonunion at 6 months was higher with CR (4 cases, 3 of which required further surgery, compared with none in the VLP group). The incidence of neuropathy and tendon injury was similar between treatment groups. Incidence of other complications, including deep infection, implant failure, and CRPS, was very low, and each favored VLP fixation. Notably, deep infection and implant failure complications occurred in patients allocated to CR who had crossed over to VLP fixation.
Table 3. Complications for the Randomized Clinical Trial Cohort.
| Complication | No. (%) of patients | Risk ratioa (95% CI) | |
|---|---|---|---|
| CR (n = 84) | VLP fixation (n = 80) | ||
| Any complications | 12 (14) | 6 (8) | 0.53 (0.21-1.33) |
| Deep infection | 1 (1)b | 0 | NA |
| Additional operation | 6 (7)c | 2 (3)d | 0.35 (0.07-1.68) |
| Neuropathy | 3 (4) | 3 (4) | 1.05 (0.22-5.05) |
| Tendon irritation requiring treatment | 0 | 1 (1) | NA |
| Tendon rupture | 1 (1) | 1 (1) | 1.05 (0.07-16.50) |
| Fracture nonunion at 6 mo | 4 (5) | 0 | NA |
| Implant failure | 1 (1)b | 0 | NA |
| Complex regional pain syndrome | 2 (2) | 1 (1) | 0.53 (0.05-5.68) |
| Death | 0 | 0 | NA |
Abbreviations: CR, closed reduction and cast immobilization; NA, not applicable; VLP, volar-locking plate.
Risk ratios are expressed as VLP fixation vs CR.
These complications occurred after these participants had crossed over to VLP fixation.
Additional operations were for carpal tunnel release (n = 1), fracture nonunion requiring plating (n = 1), hardware failure after early crossover to surgery (n = 1), postoperative infection requiring surgical washout after crossing over to surgery (n = 1), and osteotomy at 6 months after initial treatment (n = 2).
Additional operations were for removal of hardware after metal allergy (n = 1) and removal of hardware after tendon irritation at 3 months after initial treatment.
Observational Cohort
The age and sex of the participants were similar in the RCT and the observational cohorts (eAppendix 7 in Supplement 3). A significant difference was found in the incidence of self-reported osteoporosis between cohorts (11.5% for the RCT cohort and 20.9% for the observational cohort, P = .04), but little difference was found between cohorts for other comorbidities. A significantly higher proportion of participants in the RCT expressed no treatment preference compared with participants in the observational group (100 [61%] vs 12 [9%], P < .001) (eAppendix 7 in Supplement 3), who preferred CR (94 [71%]) over VLP fixation (27 [20%]).
Findings in the observational cohort were similar to findings in the RCT. For patient-reported pain and function, mean (SD) PRWE scores were 12.1 (16.7) for VLP fixation compared with 15.3 (18.6) for CR (MD, 3.3; 95% CI, –4.4 to 10.9). There was an MD of 0.7 (95% CI, –6.9 to 8.2; P = .86) points on the Disabilities of Arm, Shoulder, and Hand questionnaire, favoring VLP fixation. There was little between-group difference for the other outcomes at 12 months (eAppendix 8 in Supplement 3). At 3 months, there was an MD in PRWE of 10.3 points (95% CI, –0.2 to 20.9; P = .06). No between-group differences were found in other outcomes at 3 months or in the rate of any complications (eAppendix 8 in Supplement 3).
Sensitivity Analysis
In the RCT, there were 5 participants who crossed over treatment groups before surgery, all within 6 weeks: 3 from CR to VLP fixation and 2 from VLP fixation to CR. We conducted sensitivity analyses to investigate the impact of crossover. Results of each analysis are compared and displayed in eAppendix 4 in Supplement 3. The as-treated and per-protocol analyses (eAppendix 4 in Supplement 3) produced similar results to the ITT analysis.
Discussion
In this randomized clinical trial, VLP fixation provided a small but clinically unimportant benefit over CR for wrist pain and function at 3 months, and no difference was found at 12 months after treatment. Participants receiving VLP fixation were more likely to rate their treatment as successful.
The incidence of all complications was generally low and similar between groups. Previous systematic reviews showed no between-group differences29 or higher major complication rates28 in the surgical groups. Although complication rates in this study were not significantly different between treatment groups and overall rates were low, these differences may be more important when extrapolated to a population level.
The RCT and observational cohorts were similar in baseline characteristics and outcomes, which indicates that the results from the RCT are generalizable to patients who declined randomization and this patient population generally. A difference was found between cohorts in treatment preference, expressed at baseline. Most participants (91%) in the observational cohort expressed a treatment preference compared with 39% in the RCT cohort. Participants with no treatment preference were more likely to participate in the RCT.
Our findings are in accord with recent systematic reviews.28,29 To provide a visual comparison of our results with similar RCTs,14,25,26,27 we added our functional outcomes to this meta-analysis (eAppendix 9 in Supplement 3). However, in 2 of these similar RCTs,25,27 crossover from CR to VLP fixation was high (41% and 38%, respectively). These 2 studies25,27 were conducted according to a treatment regimen by which patients received initial CR with reassessment at 2 weeks to determine stability. In many countries (and in our study), the treatment practice is that fracture stability and treatment are determined based on initial radiographs. Consequently, the rate of crossover in our RCT was low by comparison.
Earlier functional recovery with VLP fixation was a consistent finding in the literature7,14,16,25,26,27,28,29 and in the current study. Surgery may have a role in older patients for whom speed of recovery is important, such as people in paid employment or people who live independently.
Two clinical practice guidelines for the treatment of wrist fractures have recently been published by professional organizations and are based largely on the outcomes of 2 RCTs.14,25 A Norwegian guideline made a weak recommendation for surgical treatment of patients 65 years and older.51 In contrast, a British guideline recommended CR as the primary treatment option after careful consideration of patient characteristics.52 More recent evidence suggests that there are no clinically important advantages to surgical treatment over nonsurgical treatment of displaced distal radius fractures in older patients with respect to patient-reported outcomes. There is now sufficient high-quality evidence to review and revise clinical practice guidelines concerning the treatment of wrist fractures in older patients.
Strengths and Limitations
This study has strengths, including low unavailability for follow-up (RCT, 4%) and a low rate of crossover (3%). Because attrition was very low, the difference between the per-protocol and the ITT analyses of the primary outcome was negligible. Comparison studies reported follow-up rates of 81%14,25 and 85%.26,27 In these studies,14,25,26,27 follow-up was conducted by face-to-face clinic appointment compared with the telephone follow-up used in this study.
Other strengths relate to study design. Confounding was minimized by using a central computer–based randomization process that incorporated minimization. Apart from treatment preference and incidence of self-reported osteoporosis, little difference was found in baseline characteristics between the RCT and the parallel observational cohort, suggesting minimal sampling bias and improving the generalizability of findings. Detection bias was minimized by using a blinded investigator (A.L.) to gather 3- and 12-month outcomes by telephone. Selective reporting was mitigated by using blinded investigators (A.L., W.X., and I.A.H.) to conduct the statistical analysis and interpretation and by prespecifying the statistical analysis.31
This study also has limitations. Given that it compared surgical with nonsurgical treatment, this study could have been at risk of performance bias, although this would likely overestimate the benefit of surgery. Furthermore, there was potential for unblinding, particularly when ascertaining complications; this detection bias risk was minimized by collecting complication outcomes last. Because local recruitment depended on the local surgical teams, it is likely that not all eligible patients were offered participation, and no screening log was used, potentially leading to sampling bias.
Conclusions
These findings support those of other recent studies28,29 that found that VLP fixation offers no clinically important advantage over CR in the treatment of wrist fractures in older patients at 12 months. These results should encourage practitioners to carefully consider the indications and cost implications for surgical treatment in this context.
Trial Protocol
Statistical Analysis Plan
eAppendix 1. Printed Patient Information
eAppendix 2. Study Outcomes
eAppendix 3. Nonstandard Outcome Measures
eAppendix 4. Boxplot of PRWE Scores for the RCT at 3 Months
eAppendix 5. Patient-Reported Treatment Success for the RCT
eAppendix 6. Comparison of RCT With Observational Cohort
eAppendix 7. Observational Cohort Outcomes
eAppendix 8. Sensitivity Analysis
eAppendix 9. Comparison With Other Studies
Data Sharing Statement
References
- 1.Nellans KW, Kowalski E, Chung KC. The epidemiology of distal radius fractures. Hand Clin. 2012;28(2):113-125. doi: 10.1016/j.hcl.2012.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bengnér U, Johnell O. Increasing incidence of forearm fractures: a comparison of epidemiologic patterns 25 years apart. Acta Orthop Scand. 1985;56(2):158-160. doi: 10.3109/17453678508994345 [DOI] [PubMed] [Google Scholar]
- 3.Edwards BJ, Song J, Dunlop DD, Fink HA, Cauley JA. Functional decline after incident wrist fractures: study of osteoporotic fractures: prospective cohort study. BMJ. 2010;341:c3324. doi: 10.1136/bmj.c3324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Watts JJ, Abimanyi-Ochom J, Sanders KM. Osteoporosis Costing All Australians: A New Burden of Disease Analysis—2012 to 2022. Osteoporosis Australia; 2013. [Google Scholar]
- 5.Shauver MJ, Yin H, Banerjee M, Chung KC. Current and future national costs to Medicare for the treatment of distal radius fracture in the elderly. J Hand Surg Am. 2011;36(8):1282-1287. doi: 10.1016/j.jhsa.2011.05.017 [DOI] [PubMed] [Google Scholar]
- 6.Ansari U, Adie S, Harris IA, Naylor JM. Practice variation in common fracture presentations: a survey of orthopaedic surgeons. Injury. 2011;42(4):403-407. doi: 10.1016/j.injury.2010.11.011 [DOI] [PubMed] [Google Scholar]
- 7.Mellstrand Navarro C, Brolund A, Ekholm C, et al. Treatment of radius or ulna fractures in the elderly: a systematic review covering effectiveness, safety, economic aspects and current practice. PLoS One. 2019;14(3):e0214362. doi: 10.1371/journal.pone.0214362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91(8):1868-1873. doi: 10.2106/JBJS.H.01297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhat SB, Liss FE, Beredjiklian PK. Economic analysis of the cost of implants used for treatment of distal radius fractures. Arch Bone Jt Surg. 2018;6(5):371-375. [PMC free article] [PubMed] [Google Scholar]
- 10.Fanuele J, Koval KJ, Lurie J, Zhou W, Tosteson A, Ring D. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg Am. 2009;91(6):1313-1319. doi: 10.2106/JBJS.H.00448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walenkamp MMJ, Mulders MAM, Goslings JC, Westert GP, Schep NWL. Analysis of variation in the surgical treatment of patients with distal radial fractures in the Netherlands. J Hand Surg Eur Vol. 2017;42(1):39-44. doi: 10.1177/1753193416651577 [DOI] [PubMed] [Google Scholar]
- 12.Mauck BM, Swigler CW. Evidence-based review of distal radius fractures. Orthop Clin North Am. 2018;49(2):211-222. doi: 10.1016/j.ocl.2017.12.001 [DOI] [PubMed] [Google Scholar]
- 13.Chan YH, Foo TL, Yeo CJ, Chew WY. Comparison between cast immobilization versus volar locking plate fixation of distal radius fractures in active elderly patients, the Asian perspective. Hand Surg. 2014;19(1):19-23. doi: 10.1142/S021881041450004X [DOI] [PubMed] [Google Scholar]
- 14.Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93(23):2146-2153. [DOI] [PubMed] [Google Scholar]
- 15.Belloti JC, Tamaoki MJ, Atallah AN, Albertoni WM, dos Santos JB, Faloppa F. Treatment of reducible unstable fractures of the distal radius in adults: a randomised controlled trial of De Palma percutaneous pinning versus bridging external fixation. BMC Musculoskelet Disord. 2010;11:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diaz-Garcia RJ, Chung KC. Common myths and evidence in the management of distal radius fractures. Hand Clin. 2012;28(2):127-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egol K, Walsh M, Tejwani N, McLaurin T, Wynn C, Paksima N. Bridging external fixation and supplementary Kirschner-wire fixation versus volar locked plating for unstable fractures of the distal radius: a randomised, prospective trial. J Bone Joint Surg Br. 2008;90(9):1214-1221. [DOI] [PubMed] [Google Scholar]
- 18.Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92(9):1851-1857. [DOI] [PubMed] [Google Scholar]
- 19.Gradl G, Gradl G, Wendt M, Mittlmeier T, Kundt G, Jupiter JB. Non-bridging external fixation employing multiplanar K-wires versus volar locked plating for dorsally displaced fractures of the distal radius. Arch Orthop Trauma Surg. 2013;133(5):595-602. [DOI] [PubMed] [Google Scholar]
- 20.Grewal R, MacDermid JC, King GJ, Faber KJ. Open reduction internal fixation versus percutaneous pinning with external fixation of distal radius fractures: a prospective, randomized clinical trial. J Hand Surg Am. 2011;36(12):1899-1906. [DOI] [PubMed] [Google Scholar]
- 21.Harley BJ, Scharfenberger A, Beaupre LA, Jomha N, Weber DW. Augmented external fixation versus percutaneous pinning and casting for unstable fractures of the distal radius: a prospective randomized trial. J Hand Surg Am. 2004;29(5):815-824. [DOI] [PubMed] [Google Scholar]
- 22.Kreder HJ, Agel J, McKee MD, Schemitsch EH, Stephen D, Hanel DP. A randomized, controlled trial of distal radius fractures with metaphyseal displacement but without joint incongruity: closed reduction and casting versus closed reduction, spanning external fixation, and optional percutaneous K-wires. J Orthop Trauma. 2006;20(2):115-121. [DOI] [PubMed] [Google Scholar]
- 23.Margaliot Z, Haase SC, Kotsis SV, Kim HM, Chung KC. A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J Hand Surg Am. 2005;30(6):1185-1199. [DOI] [PubMed] [Google Scholar]
- 24.Young CF, Nanu AM, Checketts RG. Seven-year outcome following Colles’ type distal radial fracture: a comparison of two treatment methods. J Hand Surg Br. 2003;28(5):422-426. [DOI] [PubMed] [Google Scholar]
- 25.Bartl C, Stengel D, Bruckner T, Gebhard F; ORCHID Study Group . The treatment of displaced intra-articular distal radius fractures in elderly patients. Dtsch Arztebl Int. 2014;111(46):779-787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saving J, Severin Wahlgren S, Olsson K, et al. Nonoperative treatment compared with volar locking plate fixation for dorsally displaced distal radial fractures in the elderly: a randomized controlled trial. J Bone Joint Surg Am. 2019;101(11):961-969. [DOI] [PubMed] [Google Scholar]
- 27.Sirniö K, Leppilahti J, Ohtonen P, Flinkkilä T. Early palmar plate fixation of distal radius fractures may benefit patients aged 50 years or older: a randomized trial comparing 2 different treatment protocols. Acta Orthop. 2019;90(2):123-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen Y, Chen X, Li Z, Yan H, Zhou F, Gao W. Safety and efficacy of operative versus nonsurgical management of distal radius fractures in elderly patients: a systematic review and meta-analysis. J Hand Surg Am. 2016;41(3):404-413. doi: 10.1016/j.jhsa.2015.12.008 [DOI] [PubMed] [Google Scholar]
- 29.Stephens AR, Presson AP, McFarland MM, et al. Volar locked plating versus closed reduction and casting for acute, displaced distal radial fractures in the elderly: a systematic review and meta-analysis of randomized controlled trials. J Bone Joint Surg Am. 2020;102(14):1280-1288. doi: 10.2106/JBJS.19.01442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harris IA, Naylor JM, Lawson A, et al. A Combined Randomised and Observational Study of Surgery for Fractures in the Distal Radius in the Elderly (CROSSFIRE): a study protocol. BMJ Open. 2017;7(6):e016100. doi: 10.1136/bmjopen-2017-016100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lawson A, Naylor J, Buchbinder R, et al. A Combined Randomised and Observational Study of Surgery for Fractures in the Distal Radius in the Elderly (CROSSFIRE): a statistical analyses plan. Trials. 2020;21(1):651. doi: 10.1186/s13063-020-4228-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schulz KF, Altman DG, Moher D; CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Torgerson DJ, Sibbald B. Understanding controlled trials: what is a patient preference trial? BMJ. 1998;316(7128):360. doi: 10.1136/bmj.316.7128.360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grant AM, Wileman SM, Ramsay CR, et al. ; REFLUX Trial Group . Minimal access surgery compared with medical management for chronic gastro-oesophageal reflux disease: UK collaborative randomised trial. BMJ. 2008;337:a2664. doi: 10.1136/bmj.a2664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mittal R, Harris IA, Adie S, Naylor JM; CROSSBAT Study Group . Surgery for type B ankle fracture treatment: a Combined Randomised and Observational Study (CROSSBAT). BMJ Open. 2017;7(3):e013298. doi: 10.1136/bmjopen-2016-013298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Blazeby JM, Barham CP, Donovan JL. Randomised trials of surgical and non-surgical treatment: a role model for the future. BMJ. 2008;337:a2747. doi: 10.1136/bmj.a2747 [DOI] [PubMed] [Google Scholar]
- 37.Muller ME, Nazarian S, Koch P, Schatzker J. The Comprehensive Classification of Fractures of Long Bones. Springer-Verlag; 1990. doi: 10.1007/978-3-642-61261-9 [DOI] [Google Scholar]
- 38.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31(1):103-115. doi: 10.2307/2529712 [DOI] [PubMed] [Google Scholar]
- 39.Handoll HHG, Elliott J. Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev. 2015;(9):CD003324. doi: 10.1002/14651858.CD003324.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ziebart C, Nazari G, MacDermid JC. Therapeutic exercise for adults post-distal radius fracture: an overview of systematic reviews of randomized controlled trials. Hand Ther. 2019;24:69-81. doi: 10.1177/1758998319865751 [DOI] [Google Scholar]
- 41.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577-586. doi: 10.1097/00005131-199811000-00009 [DOI] [PubMed] [Google Scholar]
- 43.Kleinlugtenbelt YV, Nienhuis RW, Bhandari M, Goslings JC, Poolman RW, Scholtes VA. Are validated outcome measures used in distal radial fractures truly valid? a critical assessment using the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) checklist. Bone Joint Res. 2016;5(4):153-161. doi: 10.1302/2046-3758.54.2000462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38(4):641-649. doi: 10.1016/j.jhsa.2012.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lawson A, Tan AC, Naylor J, Harris IA. Is retrospective assessment of health-related quality of life valid? BMC Musculoskelet Disord. 2020;21(1):415. doi: 10.1186/s12891-020-03434-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res. 2005;14(6):1523-1532. doi: 10.1007/s11136-004-7713-0 [DOI] [PubMed] [Google Scholar]
- 47.Olsen MF, Bjerre E, Hansen MD, et al. Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Med. 2017;15(1):35. doi: 10.1186/s12916-016-0775-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lawson A, Santhakumar P, Naylor JM et al. Wrist deformity, bother and function following wrist fracture in the elderly. BMC Res Notes. 2002;13:169. doi:10.1186/s13104-020-05013-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harden RN, Bruehl S, Perez RS, et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for complex regional pain syndrome. Pain. 2010;150(2):268-274. doi: 10.1016/j.pain.2010.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.R Core Team . R: A Language and Environment for Statistical Computing. Version 3.4.4. R Foundation for Statistical Computing; 2018. https://www.R-project.org/
- 51.Kvernmo HB, Hove LM, Frønsdal KB, Harboe I, Odinsson A, Krukhaug Y. Treatment of distal radius fractures in adults. Norwegian Orthopaedic Association and The Norwegian Medical Association. Accessed November 10, 2020. https://files.magicapp.org/guideline/ac10868f-c18b-462d-978d-cb53a5959fd5/2_6/pdf/published_guideline_551-2_6.pdf
- 52.British Orthopaedic Association and British Society for Surgery of the Hand Blue Book Committee . Best practice for management of distal radial fractures. Published 2018. Accessed November 10, 2020. https://www.bssh.ac.uk/_userfiles/pages/files/professionals/Radius/Blue Book DRF Final Document.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
Statistical Analysis Plan
eAppendix 1. Printed Patient Information
eAppendix 2. Study Outcomes
eAppendix 3. Nonstandard Outcome Measures
eAppendix 4. Boxplot of PRWE Scores for the RCT at 3 Months
eAppendix 5. Patient-Reported Treatment Success for the RCT
eAppendix 6. Comparison of RCT With Observational Cohort
eAppendix 7. Observational Cohort Outcomes
eAppendix 8. Sensitivity Analysis
eAppendix 9. Comparison With Other Studies
Data Sharing Statement