Learning objectives.
By reading this article, you should be able to:
-
•
Explain the factors that put a patient at increased risk of a delayed return of consciousness after anaesthesia.
-
•
Use a structured approach to managing such a case in the post-anaesthesia care unit.
-
•
Identify the potential causes for a delayed return in consciousness.
Key points.
-
•
There is no agreed unifying definition of delayed recovery of consciousness: the diagnosis is based on clinical evaluation and the exact incidence is not known.
-
•
Most cases of delayed return of consciousness are rapidly treatable, although rarer and potentially catastrophic pathologies exist.
-
•
A wide range of patient-related, pharmacological and surgical factors can contribute to the risk of a delayed return of consciousness.
-
•
Identification of the patient at risk is paramount.
Clinical scenario.
A 75-yr-old man with well-controlled hypertension and mild chronic obstructive pulmonary disease has undergone a robotic total prostatectomy. The procedure was long and technically difficult, with a total operating time of 5 h. The patient received a total i.v. general anaesthetic with an infusion of atracurium, and was given morphine 10 mg i.v., 30 min before the end of the procedure. Sixty minutes after the end of anaesthesia, the patient is not rousable but is breathing spontaneously through a tracheal tube; his observations are stable, he has no apparent focal neurology, but he is not regaining consciousness. An arterial blood gas shows a Paco2 of 6.3 kPa but all other values are within normal reference ranges.
Introduction
Adequate recovery from general anaesthesia has been defined as ‘a state of consciousness of an individual when they awaken or become rousable and aware of their surroundings and identity’.1 For the majority of patients this occurs soon after the end of anaesthesia, but when this is delayed it represents a diagnostic challenge and potentially, a serious occurrence. This article aims to highlight the importance of the early identification of patients at increased risk of a delayed return of consciousness, review the potential causes and provide a structured approach if such an event should occur. An algorithm is presented to help the anaesthetist faced with a patient exhibiting delayed return of consciousness.
There is scarce research and very little published on delayed return of consciousness after general anaesthesia. There is no set time threshold for the expected return of consciousness. It is vital, therefore, that each patient is assessed individually to determine if their time taken to return to consciousness is outside that which would be normally anticipated in similar patients. However, even after a lengthy procedure in a deep plane of anaesthesia, we would suggest that most patients would normally be rousable without the need for an artificial airway within 60 min of sedative medications being stopped.
Risk factors for delayed return of consciousness
Risk factors for delayed return of consciousness can be divided into those related to the patient and their existing comorbidities, and those related to the type of surgery (Table 1, Table 2). Patients who exhibit a delayed return of consciousness often have multiple risk factors.
Table 1.
Risk factors for delayed return of consciousness
| Patient factors | Anaesthetic/surgical factors |
|---|---|
| Extremes of age | CNS surgery |
| Genetic variation | Cardiac surgery |
| Body habitus | Long duration of anaesthesia/surgery |
| Comorbidities present |
Table 2.
Comorbidities predisposing to increased risk of delayed return of consciousness
| Respiratory | Hepatic | Renal | Endocrine |
|---|---|---|---|
Reduced central drive:
|
Acute hepatic failure | Acute kidney injury | Hypothyroidism |
Neuromuscular disorder:
|
Chronic hepatic failure | Chronic renal failure | |
Pulmonary pathology:
|
Patient-related factors
Ageing
Ageing affects pharmacokinetics because of an accumulation of deficits across organ systems. This increases the risk of a delayed return of consciousness after general anaesthesia: elderly or frail patients are more sensitive to drugs commonly used during general anaesthesia, including i.v. and inhalational anaesthetic agents, benzodiazepines and opioids. The reasons for this are multifactorial and include declining CNS function leading to an increased response to drugs acting on the CNS; changes in body composition with reduced muscle mass; an increase in adipose tissue; and a reduction in total body water. As a result, lipophilic agents have a larger volume of distribution, which may prolong their duration of action, and hydrophilic agents have higher peak plasma concentrations. Ageing also reduces renal mass, glomerular filtration rates and phase one hepatic metabolism, which may impair renal and hepatic clearance and therefore the duration of action of agents dependent on these pathways for excretion.2
Infants
Infants are more sensitive to the effects of general anaesthetic agents. Again, the reasons for this are multifactorial and include immature Phases I and II hepatic processes, reduced plasma protein binding and increased volumes of distribution; this results in a relative increase in dose requirements coupled with an increased pharmacodynamic sensitivity to the effects of sedative drugs. Drug metabolism may also be delayed if hypothermia is present, which is more common during general anaesthesia in infants as a result of their increased surface area to volume ratio. Also, the immature blood–brain barrier permits smaller molecules to enter the CNS. In addition, infants are more prone to hypoglycaemia because of reduced hepatic glycogen stores and a higher metabolic rate, which can itself cause unconsciousness. Hypoglycaemia must be excluded promptly in the event of delayed return of consciousness, particularly in infants.3
Genetic variation
Advances in pharmacogenetics have enabled a better understanding of the genetic factors influencing the response to drugs used during anaesthesia. The majority of anaesthetic agents are initially metabolised via Phase I CYP450 enzyme superfamilies and subsequently via Phase II enzymes, many of which show significant genetic polymorphism of their isoforms. The interindividual variability of the CYP2D6 gene involved in the metabolism of opioids is known to increase the risk of a delayed return of consciousness as a result of central respiratory depression and hypercapnia.4 It is also recognised that a number of CYP enzymes, including CYP2B6 and CYP2C9, and the Phase II uridine diphosphate-glucuronosyltransferase enzymes all play a role in the metabolism of propofol and therefore may affect individual response, including delaying return of consciousness.5
Body habitus
Body composition can play a significant role in the speed of recovery after general anaesthesia. Most drug doses should be administered based on lean body weight, but increased body fat in the obese may mean that relatively higher doses have to be given to attain the same peak plasma concentration compared with an individual with less body fat. This results predominantly from redistribution of the lipid-soluble anaesthetic agents in body fat. At the termination of anaesthesia, this lipid sink of anaesthetic agent diffuses into the plasma compartment, resulting in a slower rate of reduction of plasma concentration and therefore, a slower return of consciousness. The Society for Bariatric Anaesthesia has produced a useful guideline for appropriate dosing of multiple anaesthetic drugs in obese individuals to reduce this risk of ‘overdosing’.6 Underweight patients were shown to be at a higher risk of slower recovery after peripheral vascular or coronary artery bypass graft surgery in one large observational study, but no mechanism was proposed and this has not been investigated or explored further in the literature.7
Comorbidities
Preexisting comorbidities may play a role in delaying return of consciousness after anaesthesia. Respiratory comorbidity, whether related to central drive, neuromuscular function or pulmonary pathology, can increase the risk of delayed return of consciousness after anaesthesia because of hypoxia, hypercarbia or slower clearance of inhalational agents. This is compounded by drugs known to reduce minute volume such as opioids and inhalational anaesthetic agents. Congestive heart failure can cause a slower wash-out of anaesthetic agents as a result of increased lung water and low cardiac output.
Acute and chronic hepatic disease can cause significant alterations in the pharmacokinetics of a number of anaesthetic drugs and therefore, can increase the risk of delayed emergence if doses are not altered accordingly. Of particular note, a reduction in plasma proteins increases the unbound fraction of thiopental, prolonging its half-life and therefore duration of action. Similarly, the risk of accumulation of opioids is higher in patients with liver cirrhosis as a result of reduced hepatic blood flow, reduced extraction ratios, reduced plasma protein binding and increases in volumes of distribution.8
Acute and chronic renal disease influences the pharmacokinetics of various agents used in general anaesthesia, increasing risk of delayed return of consciousness. As with hepatic disease, a failure to alter drug doses accordingly may result in an increased duration of drug action. Thiopental requires a dose reduction in patients with renal impairment as a result of reduced plasma protein binding and an increased volume of distribution. Opioids including fentanyl, alfentanil, oxycodone and morphine require dose reductions in patients with renal failure to ensure avoidance of excessive sedation. This is particularly relevant in the case of morphine, as its potent metabolite morphine-6-glucuronide is entirely excreted via the kidney.9 Hypothyroidism has multisystem effects including decreased spontaneous minute ventilation, reduced plasma volume, hyponatraemia and impaired hepatic drug metabolism, all of which can increase the risk of delayed return in consciousness after anaesthesia. Myxoedema coma is a recognised cause of delayed return of consciousness and it has been reported that subclinical hypothyroidism has presented as a delayed return in consciousness after anaesthesia.10
Factors related to anaesthesia and surgery
The nature of surgery can predispose to a slower return of consciousness. Operations on the brain and vasculature of the CNS are particularly associated with delayed awakening and are also associated with a higher risk of postoperative stroke (either ischaemic or haemorrhagic depending on the nature of surgery).11 Stroke is a potentially catastrophic cause of failure to regain consciousness after anaesthesia.
Other surgical risk factors that may increase the risk of a delayed return of consciousness include:
-
(i)
Operations where a steep Trendelenburg position is used (e.g. robotic prostate surgery): the resulting cerebral oedema may not become apparent until the cessation of anaesthesia when delayed or even a failed return of consciousness becomes apparent.
-
(ii)
Operations where hypotonic irrigation fluids are able to enter the circulation (e.g. transurethral resections of the prostate): mechanisms for delayed recovery of consciousness include cerebral oedema and electrolyte disturbance after absorption of hypotonic glycine into the intravascular compartment together with the direct central inhibitory action of glycine.
-
(iii)
Cardiac surgery with cardiopulmonary bypass. Complications include hypothermia, haemorrhagic stroke from anticoagulation, cerebral ischaemia resulting from microemboli and the change from pulsatile to linear blood flow through the brain.
Causes of delayed return of consciousness
The potential causes of a delayed return of consciousness after anaesthesia can be subdivided into pharmacological, patient and metabolic factors (Table 3).
Table 3.
Medical and pharmacological causes of delayed return of consciousness
| Pharmacological | Metabolic | Rare causes |
|---|---|---|
| Serotonin syndrome | Hypoglycaemia/hyperglycaemia | Seizures (including non-convulsive status epilepticus) |
| Opioids | Hypo/hypernatraemia | Myxoedema coma |
| Neuromuscular blockers | Hypothermia | Functional coma |
| I.V. anaesthetic agents | Brainstem stroke | |
| Volatile anaesthetic agents | ||
| Central anticholinergic syndrome |
Pharmacological causes
Intravenous anaesthetic agents
Induction doses of i.v. anaesthetic agents are highly unlikely to delay return of consciousness after anaesthesia, but the use of infusions to maintain anaesthesia may carry a risk of delayed emergence. The time taken for plasma concentrations to decrease after termination of an infusion depends on the duration, or context, of that infusion. It is important to be aware of the varying context-sensitive half-times (CSHT) of drugs given as an infusion during anaesthesia. Propofol has only a very minor increase in CSHT with increasing duration of infusion from 3 min for a very short infusion to 18 min after a 12-h infusion. This relatively small variation occurs because propofol is excreted from the central compartment more rapidly than it is redistributed from peripheral compartments. However, CSHT describes the time taken for the plasma concentration to decrease to 50% of the value at the time of stopping the infusion, which does not necessarily relate to the point at which recovery of consciousness will occur. Therefore, if high rates of propofol infusion have been required for a lengthy and stimulating surgery, plasma propofol concentrations may exceed those at which the patient is expected to wake up for some time after the infusion has been stopped.12
Volatile anaesthetic agents
Emergence from general anaesthesia with volatile anaesthetic agents can be delayed by alveolar hypoventilation. At a pharmacokinetic level, volatile anaesthetic agents with a higher blood–gas partition coefficient are taken up to a greater extent into the pulmonary circulation and may prolong recovery from anaesthesia. Patients who are obese are at a greater risk of delayed return of consciousness when agents with a higher oil:gas partition coefficient, such as isoflurane, are used for a prolonged time.13
Opioids
Opioids may contribute to a delayed return of consciousness through two mechanisms—direct sedation via opioid receptor activity or as a result of respiratory depression causing hypercarbia. The use of naloxone should be considered when recovery is delayed and opioids have been used, particularly in patients who are elderly, frail or have impaired hepatic or renal function. Alfentanil and fentanyl infusions must be used with caution, as both have highly variable CSHTs that depend on the duration of infusion. For infusions of short durations (fewer than 2 h), fentanyl has a shorter CSHT than alfentanil. However, if a longer duration of infusion occurs, the CSHT of fentanyl begins to rapidly increase because of its high rates of redistribution, which maintain plasma concentrations despite a rapid excretion.12
Benzodiazepines
Benzodiazepines have anxiolytic, hypnotic and anticonvulsant properties and are therefore commonly used as a coinduction agents or premedication in patients undergoing general anaesthesia. Although unlikely to cause a delayed return of consciousness when used in isolation, the use of flumazenil as an antidote should be considered in patients at higher risk of excessive sedation.14
Neuromuscular blocking agents
Neuromuscular blocking drugs do not directly delay return of consciousness after anaesthesia. However, delayed recovery of consciousness may be mimicked by patients with residual neuromuscular block. If a patient has inadequate respiratory muscle function at the termination of anaesthesia as a result of residual paralysis, hypoventilation and hypercapnia, slower clearance of inhalation agents or an impaired ventilatory response to hypoxia may result, all of which may contribute to delayed return of consciousness. The risk of prolonged neuromuscular blockade is increased in patients with preexisting neuromuscular disorders and in certain metabolic states including hypothermia, acidosis, hypermagnesaemia and hypokalaemia. Aminoglycoside antibiotics also increase the duration of action of neuromuscular blocking drugs. This is a class effect, reported as a magnesium-like effect on the neuromuscular junction. Objective monitoring is recommended for all patients receiving neuromuscular blocking drugs and a patient should not be considered to have satisfactorily recovered from neuromuscular block until a train-of–four ratio >0.9 has returned. If rocuronium bromide or vecuronium bromide has been used, consideration should be given to administering the chelating antidote sugammadex. Acquired and inherited abnormalities of plasma cholinesterase may cause a significant prolongation of the action of suxamethonium. The incidence of significant abnormal metabolism of suxamethonium is estimated at one in 2800.15
Serotonin syndrome
The diagnosis of serotonin syndrome is clinical and includes a change in conscious state (including coma, seizures and lethargy resulting in delayed emergence), autonomic dysfunction (including diaphoresis and dilated, unreactive pupils) and neuromuscular changes (e.g. hyperreflexia, rigidity and nystagmus). Perioperative serotonin syndrome has been reviewed recently in this journal.16
Patients at risk are those taking drugs with serotonergic effects who then receive drugs common to anaesthesia and surgery that also have serotonergic effects (e.g. methylthioninium chloride ['methylene blue'], metoclopramide, ondansetron, fentanyl, tramadol). Treatment is largely supportive and involves cessation of serotonergic drugs, organ support as required and the consideration of serotonin receptor antagonists.16
Central anticholinergic syndrome
A wide range of drugs have been implicated in cases of central anticholinergic syndrome. Anticholinergic medications such as atropine or hyoscine, antihistamine, antiparkinsonian and antidepressant medications have been reported most, but other anaesthetic and analgesic drugs such as ketamine, propofol and fentanyl have also been implicated. Symptoms include stupor and coma, which could manifest as delayed emergence from anaesthesia. Peripheral signs and symptoms include tachycardia, dry mouth and urinary retention. Treatment includes organ support and the use of acetylcholinesterase inhibitors such as physostigmine.17
Metabolic causes
Hypo/hyperglycaemia
As an obligate glucose consumer, the brain is susceptible to hypoglycaemia and this may present as a delayed return of consciousness after anaesthesia. Those at increased risk of hypoglycaemia include: infants; diabetic patients (particularly those taking insulin or oral hypoglycaemic medications); patients with hepatic failure or heavy alcohol use/abuse; and those who have undergone prolonged starvation. Hyperglycaemia may result in a delayed recovery of consciousness after anaesthesia. Diabetic patients undergoing surgery with a significant stress response or receiving i.v. steroids during general anaesthesia may be at particular risk.
Hypo/hypernatraemia
Hyponatraemia may occur as a result of surgery or anaesthesia. This is particularly relevant in neurosurgical patients who can develop syndrome of inappropriate antidiuretic hormone secretion or cerebral salt wasting.18 Hyponatraemia is also seen in transurethral resection syndrome, as described above.
Hypernatraemia is a rare cause of delayed return of consciousness after anaesthesia that has been associated with surgery on hydatid liver cysts.19 The use of hypertonic saline during anaesthesia necessitates strict monitoring of sodium concentrations to reduce the risk of iatrogenic hypernatraemia.
Hypothermia
All general anaesthetic agents produce a dose-dependent reduction in body temperature. Hypothermia causes reduced CNS activity, impairs drug metabolism and reduces minimum alveolar concentration. Temperature should be measured and recorded in all patients receiving general anaesthesia of greater than 30 min duration.20
An approach to the patient with delayed return of consciousness
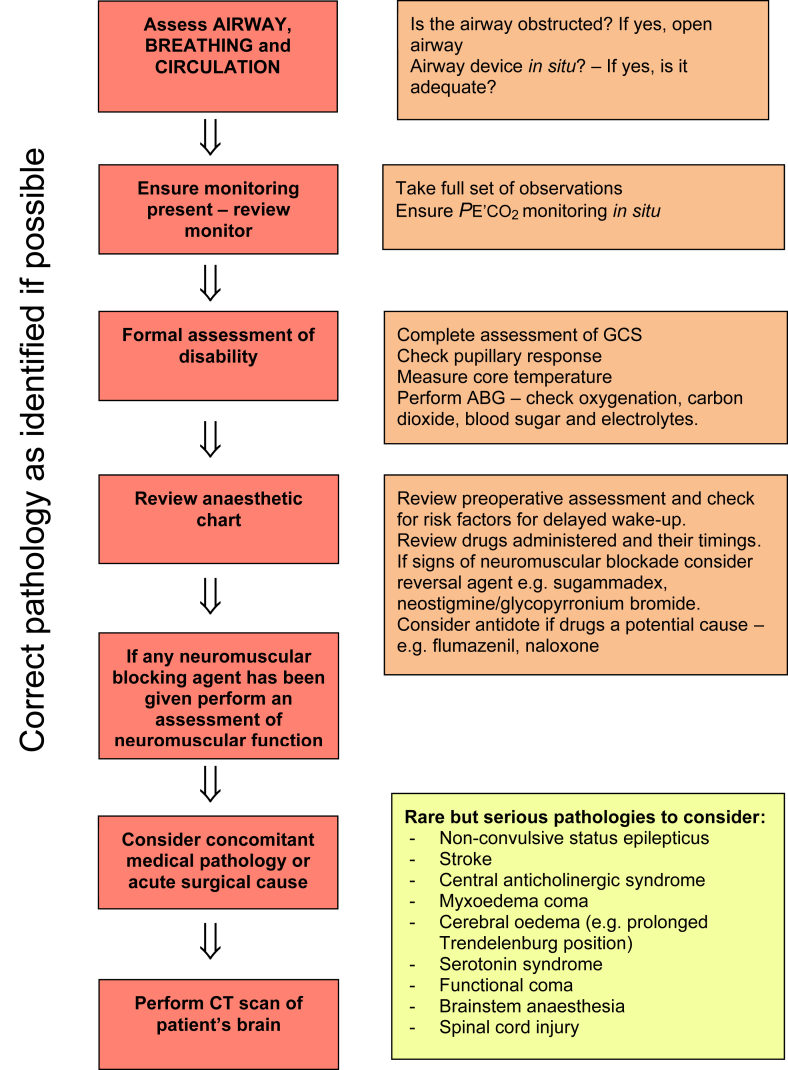
The algorithm in Fig. 1 should allow identification of readily correctable underlying conditions and allow consideration of the rarer pathologies. It starts with a focussed ‘ABC’ assessment—though an airway problem itself would in itself not cause a delay in return of consciousness after general anaesthesia, an evaluation of the airway and its adequacy is appropriate, as in all patients who are unwell.
Figure 1.
Algorithm for approaching the patient with a delayed return of consciousness.
If after completion of the algorithm there is no resolution or identification of the underlying cause for delayed return of consciousness, the potential for a significant medical or surgical pathology should be considered. An early request for a CT brain scan should be made to determine if there is acute pathology within the CNS.
If a CT scan fails to demonstrate the cause, the patient's airway should be protected with a tracheal tube if not already in place, and the patient should be transferred to the ICU where organ support can be delivered whilst further diagnostic tests such as an MRI scan or EEG can be performed.
Modern technology and mitigating the risk
The availability of enhanced monitoring and near patient testing can potentially reduce the risk of a delayed return of consciousness after anaesthesia. The increasing availability of arterial blood gas machines with a wider range of available assays should help to enable a rapid diagnosis of respiratory compromise, electrolyte abnormalities and hypoglycaemia.
The use of processed EEG-based depth of anaesthesia monitoring (bispectral index) has been examined in a recent Cochrane review. Bispectral index demonstrated a faster wake-up by a matter of minutes compared with clinical signs (but not end-tidal anaesthetic gas monitoring). The Cochrane review provides some encouraging findings regarding the use of processed EEG in reducing the risk of delayed recovery, but more research is needed.21
Rare events
The following is a summary of case reports identified in the literature, which present rare causes of delayed return of consciousness after general anaesthesia.
Brainstem stroke
Perioperative stroke is a potentially devastating complication with an incidence of 0.1–0.6% in non-cardiac surgery.22 Approximately 10% of strokes affect the brainstem. Brainstem stroke can present with complex symptoms including a decreased level of consciousness and can be particularly difficult to diagnose. The deficit may be life threatening and input from a stroke specialist is beneficial.
Non-convulsive status epilepticus
Seizures under anaesthesia are rare, although a small number of case reports have established non-convulsive status epilepticus (NCSE) as a cause for delayed return of consciousness after anaesthesia. NCSE is defined as EEG evidence of uncontrolled seizure activity without clinically apparent tonic-clonic convulsions.23 NCSE often results from underlying neurological conditions such as encephalitis, hypoxic brain injury or post-cardiac arrest. Early input from a specialist in neurology is vital.
Myxoedema coma
Myxoedema coma is a life-threatening complication of hypothyroidism that has been cited as an unusual cause of delayed return of consciousness after anaesthesia. It has been reported in patients with previously undiagnosed hypothyroidism and may present with signs including hypothermia, coma, bradycardia, hypercarbia and hyponatraemia.10 Treatment includes organ support and i.v. thyroxine.
Functional coma
A functional coma is loss of consciousness, stupor or coma not attributable to a general medical condition. It is also referred to as dissociative coma or psychogenic coma. Approximately half the cases described occur in the perioperative setting. This is a diagnosis of exclusion and should only be made after all organic causes have been ruled out. Physical examination can assist diagnosis including passive resistance to eye opening or avoidance of the face with arm drop. Episodes have been reported lasting from 45 min to 4 days. Treatment includes supportive management and careful psychological input.24
Conclusions
Delayed return of consciousness after general anaesthesia is a potentially serious occurrence. The exact incidence is not currently known. At present there is no agreed unifying definition. The diagnosis is based on a stepwise clinical evaluation as proposed in the attached algorithm. A wide range of patient-related, pharmacological and surgical factors can contribute to a patient's risk of delayed return in consciousness and most cases are rapidly treatable having been identified. A number of rare and catastrophic causes should be considered if simple assessment and management do not solve the problem.
Declaration of interests
The authors declare that they have no conflicts of interest.
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Elizabeth Thomas FRCA FFICM is a consultant in anaesthesia and intensive care medicine at Stepping Hill Hospital, Stockport, UK. Dr Thomas has written an article on pharmacokinetics and with Dr Martin and others, a revision textbook for trainees preparing for the final FRCA examination.
Fiona Martin FRCA is a specialty registrar in anaesthesia in the North West of England.
Brian Pollard BPharm MD FRCA is emeritus professor of medical education and of anaesthesia at the University of Manchester and was honorary consultant in anaesthesia and intensive care at Manchester Royal Infirmary. Professor Pollard has written 10 textbooks on anaesthesia, has been editor-in-chief of three international journals and has undertaken research on measuring consciousness and xenon anaesthesia.
Matrix codes: 1A02, 2A06, 2C01, 3I00
References
- 1.Sinclair R., Faleiro R.J. Delayed recovery of consciousness after anaesthesia. Contin Educ Anaesth Crit Care Pain. 2006;6:1248. [Google Scholar]
- 2.Eusuf D.V., Thomas E. Pharmacokinetic variation. Anaesth Intensive Care. 2019;2:126–129. [Google Scholar]
- 3.Meyer H., Kemp K. Neonatal anaesthesia. Update Anesth. 2015;30:123–132. [Google Scholar]
- 4.Sweeney B.P. Do genes influence outcome from anaesthesia? Brit J Anaesth. 2003;90:725–727. doi: 10.1093/bja/aeg103. [DOI] [PubMed] [Google Scholar]
- 5.Yonekura H., Murayama N., Yamazaki H., Sobue K. A case of delayed emergence after propofol anesthesia: genetic analysis. A A Case Rep. 2016;11:243–246. doi: 10.1213/XAA.0000000000000397. [DOI] [PubMed] [Google Scholar]
- 6.Society for Obesity and Bariatric Anaesthesia . 2020. Anaesthesia for the obese patient.https://www.sobauk.co.uk/guidelines-1?lightbox=dataItem-iit6ri461 [Google Scholar]
- 7.Tsai H.J., Chen C.C., Chang K.Y. Patients and surgery-related factors that affect time to recovery of consciousness in adult patients undergoing elective cardiac surgery. Chin Med Assoc. 2011;74:345–349. doi: 10.1016/j.jcma.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Vaia R., McNicol L., Sisley I. Anaesthesia for patients with liver disease. Contin Educ Anaesth Crit Care Pain. 2010;10:15–19. [Google Scholar]
- 9.Craig R.G., Hunter J.M. Recent developments in the perioperative management of adult patients with chronic kidney disease. Br J Anaesth. 2008;101:296–310. doi: 10.1093/bja/aen203. [DOI] [PubMed] [Google Scholar]
- 10.Kumar V., Kaimar P. Subclinical hypothyroidism: a cause for delayed recovery from anaesthesia? Indian J Anaesth. 2011;55:433–434. doi: 10.4103/0019-5049.84836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mashour G.A., Woodrum D.T., Avidan M.S. Neurological complications of surgery and anaesthesia. Br J Anaesth. 2015;114:194–203. doi: 10.1093/bja/aeu296. [DOI] [PubMed] [Google Scholar]
- 12.Hill S.A. Pharmacokinetics of drug infusions. Contin Educ Anaesth Crit Care Pain. 2004;4:76–80. [Google Scholar]
- 13.Khan K.S., Hayes I., Buggy D.J. Pharmacology of anaesthetic agents II: inhalation anaesthetic agents. Contin Educ Anaesth Crit Care Pain. 2014;14:106–111. [Google Scholar]
- 14.Fredman B., Lahay M., Zohar E., Golod M., Pruta I., Jedeikin R. The effect of midazolam premedication on mental and psychomotor recovery in geriatric patients undergoing brief surgical procedures. Anesth Analg. 1999;89:1161–1166. [PubMed] [Google Scholar]
- 15.Royal College of Anaesthetists factsheet – suxamethonuim apnoea. 2018. https://www.rcoa.ac.uk/sites/default/files/documents/2019-11/Factsheet-Suxapnoeaweb.pdf [Google Scholar]
- 16.Bartakke A., Corredor C., van Rensburg A. Serotonin syndrome in the perioperative period. BJA Educ. 2020;20:10–17. doi: 10.1016/j.bjae.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cook B., Spence A.A. Post-operative central anticholinergic syndrome. Eur J Anaesthesiol. 1997;14:1–2. doi: 10.1046/j.1365-2346.1997.00074.x. [DOI] [PubMed] [Google Scholar]
- 18.Upadhyay U.M., Gormley W.B. Etiology and management of hyponatremia in neurosurgical patients. J Intensive Care Med. 2012;27:139–144. doi: 10.1177/0885066610395489. [DOI] [PubMed] [Google Scholar]
- 19.Grati L., Toumi S., Gahbiche M. Failure to recover after anaesthesia for surgery of a liver hydatid cyst assigned to hypernatremia. Ann Fr Anaesth Reanim. 2009;28:261–262. doi: 10.1016/j.annfar.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Sessler D.I. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008;109:318–338. doi: 10.1097/ALN.0b013e31817f6d76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lewis S.R., Pritchard M.W., Fawcett L.J., Punjasawadwong Y. Bispectral index for improving intraoperative awareness and early postoperative recovery in adults. Cochrane Database Syst Rev. 2019;9:CD003843. doi: 10.1002/14651858.CD003843.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sanders R.D., Jørgensen M.E., Mashour G.A. Perioperative stroke: a question of timing? Br J Anaesth. 2015;115:11–13. doi: 10.1093/bja/aev031. [DOI] [PubMed] [Google Scholar]
- 23.Carter E.L., Adapa R.M. Adult epilepsy and anaesthesia. Contin Educ Anaesth Crit Care Pain. 2015;15:111–117. [Google Scholar]
- 24.Ryznar E., Wilcox D. Functional Coma: two case reports and a review of the literature. Psychosomatics. 2019;60:343–351. doi: 10.1016/j.psym.2019.03.005. [DOI] [PubMed] [Google Scholar]