Abstract
Objectives:
The social determinants of health affect a wide range of health outcomes and risks. To date, there have been no studies evaluating the impact of social determinants of health on laryngotracheal stenosis (LTS). We sought to describe the social determinants in a cohort of LTS patients and explore their association with treatment outcome.
Methods:
Subjects diagnosed with LTS undergoing surgical procedures between 2013– 2018 were identified. Matched controls were identified from intensive care unit (ICU) patients who underwent intubation for greater than 24 hours. Medical comorbidities, stenosis characteristics, and patient demographics were abstracted from the clinical record. Tracheostomy at last follow-up was recorded from the medical record and phone calls. Socioeconomic data was obtained from the American Community Survey.
Results:
122 cases met inclusion criteria. Cases had significantly lower education compared to Tennessee (p=0.009) but similar education rates as ICU controls. Cases had significantly higher body mass index (OR: 1.04, p=0.035), duration of intubation (OR: 1.21, p<0.001), and tobacco use (OR: 1.21, p=0.006) in adjusted analysis when compared to controls. Tracheostomy dependence within the case cohort was significantly associated with public insurance (OR:1.33, p=0.016) and chronic obstructive pulmonary disease (OR: 1.34, p=0.018) in adjusted analysis.
Conclusion:
Intubation practices, medical comorbidities and social determinants of health may influence the development of LTS and tracheostomy dependence after treatment. Identification of at-risk populations in ICUs may allow for prevention of tracheostomy dependence through the use of early tracheostomy and specialized follow-up.
Keywords: social determinants of health, laryngotracheal stenosis, endotracheal intubation, tracheostomy dependence, intensive care unit
INTRODUCTION
Social determinants of health is an umbrella term used to describe the demographic and socioeconomic factors within a patient’s environment that contribute to disease development, management, and outcomes.1 The study of these social determinants, such as income, education, race, nutrition, and insurance is gaining momentum as a promising method to decrease the burden of disease and achieve health equity.1,2 Disparities in these factors have been documented in multiple otolaryngologic diseases,1,3–5 and several studies have employed zipcode-based analysis to describe sociodemographic factors as well as geographic clustering of patients.5–7 A recent study utilizing zipcode-based analysis demonstrated higher sociodemographic status patients have higher utilization rates for chronic rhinosinusitis treatment.7 Despite the impact of social determinants of health on several otolaryngologic diseases, the study of these factors in laryngotracheal stenosis has not been explored.
Laryngotracheal stenosis (LTS) denotes a fixed extra-pulmonary airway narrowing that can have a significant impact on quality of life, ventilation, and phonation.8 LTS can occur after endotracheal intubation (termed iatrogenic), although it can also arise in the setting of vasculitis or without antecedent event (termed idiopathic).9 Of these, iatrogenic LTS obtained after prolonged intubation in intensive care units (ICU) represents the majority of LTS cases.10 Several studies have examined the medical comorbidities, intubation practices, and demographics of the iatrogenic LTS population in hopes of reducing its incidence and improving outcomes.10–13 However, to the best of our knowledge, no prior study has described social determinants of health such as income, education, and insurance status in this patient population.
We present a case-control study of 122 patients who underwent procedures for airway stenosis at a tertiary care center. This study seeks to characterize the social determinants of health in the iatrogenic LTS population in comparison to age-matched ICU controls. We additionally sought to explore the association of the social determinants of health with treatment outcomes in LTS and describe the geographic clustering of LTS cases through zipcode analysis.
MATERIALS AND METHODS
This retrospective study was performed in accordance with the Declaration of Helsinki, Good Clinical Practice and was approved by the Vanderbilt University Medical Center Institutional Review Board (IRB 140429).
Clinical Data
Adult patients (≥18 years of age) undergoing treatment for benign LTS at a tertiary care hospital were included (2013–2018). Patients were identified via current procedural terminology (CPT) codes (31580, 31587, 31588, 31582, 31592, 31780, 31800). Patients were included regardless of the type of intervention, which ranged from open surgical intervention to endoscopic approaches. Those with a history of tracheal malignancy or non-iatrogenic laryngeal trauma were excluded. For each patient, operation type, time of intubation, sociodemographic data, disease characteristics, follow-up duration, medical comorbidities, and tracheostomy at last follow-up (primary outcome) were extracted from the electronic medical record. Cases were staged according to the McCaffrey classification system.14. This staging system was utilized because a prior study found that McCaffrey staging has a more linear association with increasing tracheostomy dependence as compared to other staging systems.10 Patients were contacted via telephone with an IRB approved script to assess their current tracheostomy status as well as location of intubation. Location of intubation was defined as the first documented place of endotracheal intubation during the patient’s episode of prolonged intubation.
Age-matched controls were identified as ICU patients who underwent prolonged intubation at a tertiary hospital between 2001–2018 (International Classification of Diseases, Ninth Revision [ICD-9]: 96.70, 96.71, 96.72). These ICU controls lacked a diagnosis of airway stenosis and were defined by the absence of an otolaryngology consultation or a documented negative laryngeal exam.
Outcomes
Presence of a tracheostomy at last follow-up was the primary outcome within the case cohort. This represented failure of surgical management to correct airway narrowing.
Socioeconomic Data
Socioeconomic data was obtained from 2016 5-year estimates from the American Community Survey (ACS). Patient 5-digit zipcodes were used to obtain neighborhood median household income and percent college educated. Percent college educated was defined as obtaining a bachelor degree or greater. The ACS was additionally used to obtain Tennessee’s average age, race, sex, median household income, percent public insured, percent privately insured, percent uninsured, and percent college educated. Chart review was used to obtain individual patient insurance status. Insurance status was grouped into public, comprised of Medicaid and Medicare, private, and uninsured, which was defined as no insurance documented in the chart.
Prevalence of diabetes, obesity, and smoking in Tennessee (TN) was obtained from the Centers for Disease Control and Prevention. The CDC’s Behavioral Risk Factor Surveillance System and the US Renal Data System were used to obtain state-level data for estimates of diagnosed diabetes, risk factors, and complications. The TN rate of adult diabetes mellitus was estimated as 11.4% from 2015 data.15 The CDC’s National Center for Chronic Disease Prevention and Health Promotion was used to obtain the prevalence of obesity in TN, which was estimated at 34.8% in 2016.16 The CDC’s Office of on Smoking and Health was used to obtain estimates for tobacco use in Tennessee. In 2016, the CDC estimates that 22.1% of adults in Tennessee smoked cigarettes.17
Statistical Analysis
Data analysis was done in R (RStudio. Version 1.1.447. Vienna, Australia: R Foundation for Statistical Computing; 2018). Wilcoxon Rank Sum, Chi-Squared, and Fisher-Exact tests were used for univariate analysis as appropriate. Multivariable logistic regression was used for multivariable analysis. As per convention, statistical significance was reported as p<0.05. Geographic Analysis was done with the publicly available SatScan software (SatScan. Version 9.6. Calverton, Maryland: Boston and Informational Management Services Inc; 2018). The purely spatial discrete Poisson scan statistic was used to determine if there were geographic clusters with either a high or low proportion of cases at a statistical significance level of p<0.05 (supplementary information S1).
RESULTS
122 LTS patients met inclusion criteria. 62.3% of these patients underwent open surgical intervention. The remaining 37.7% underwent endoscopic procedures. Patients hospital of intubation was obtained from the medical record and phone calls. The location of intubation was determined for 92 of the 122 patients. 42 of these patients were intubated and managed by Vanderbilt University Medical Center (VUMC). The remaining 50 were intubated at outside hospitals (Figure 1).
Figure 1;
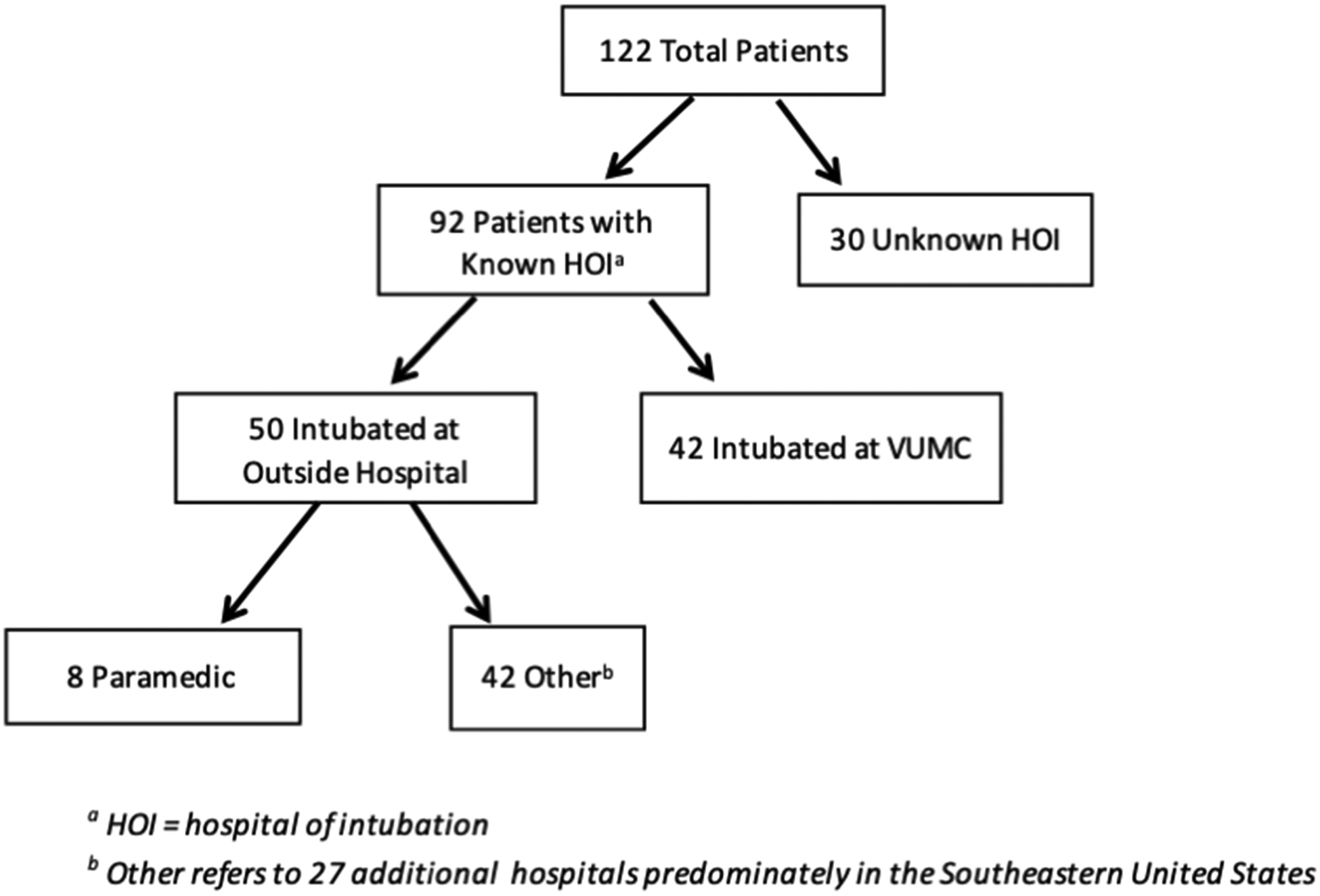
Flowchart of LTS endotracheal intubation: An illustration of the breakdown of hospital of intubation for the study population
Geographic Analysis of LTS Population
Patients zipcodes mapped predominately to the greater Nashville and Knoxville areas, reflecting referral patterns for VUMC. No statistically significant geographic clusters were found with SatScan software. Instead the density of LTS patients appeared to directly correlate with the population density in those areas (supplementary information S2).
Sociodemographics of LTS Population as compared to Tennessee
The study population of LTS patients was compared to the total population of Tennessee in order to place the case cohort in context of its larger surrounding community (Table 1). Percent college educated was significantly lower in the LTS study population as compared to Tennessee (19.1% vs 25.4%, p=0.009). The LTS population had significantly higher prevalence of tobacco use (49.2% vs 22.1%, p<0.001), obesity (50.5% vs 34.8%, p=0.032), and diabetes (30.3% vs 11.4%, p=0.001) compared to the population of Tennessee.
Table 1;
Demographics, socioeconomic status, and comorbidities of LTS population: The characteristics of the LTS population compared to the greater surrounding population of TN
| LTS Study Population (n=122) | Tennessee (n=6,548,009) | Significance (p) | |
|---|---|---|---|
| Demographics | |||
| Age, Median years (IQR†) | 53.0 (24.3–81.8) | 38.5‡ (38.4–38.6) | <0.001 |
| Sex, Male, N (%) | 65 (52.9) | 3188880 (48.7) | 0.651 |
| Race, Caucasian, N (%) | 102 (83.1) | 5094351 (77.8) | 0.355 |
| Socioeconomic Status and Comorbidities | |||
| Median Household Income, dollars, Median (IQR) | 46014 (28846–63183) | 46574 (46780–46368) | 0.831 |
| Coverage Type, Public, N (%) | 76 (65.5) | 4275849 (65.3) | 1.000 |
| Uninsured, N (%) | 6 (4.9) | 772665 (11.8) | 0.082 |
| Percent College Educated, Median (IQR) | 19.1 (0.8–37.4) | 25.4 (25.2–25.6) | 0.009 |
| Obesity, N (%) | 55 (50.5) | 2278707 (34.8) | 0.032 |
| Tobacco Use, N (%) | 58 (49.2) | 1440562 (22.1) | <0.001 |
| Type II Diabetes Mellitus, N (%) | 37 (30.3) | 746473 (11.4) | 0.001 |
IQR = Interquartile Range
does not exclude population <18
Sociodemographics of LTS Population as compared to ICU Controls
ICU controls had comparable sex, age, and race to cases. College education was not significantly different between controls and cases (19.1% vs 18.4%, p=0.733). Cases had significantly higher body mass index (30.3 vs. 26.1, p=0.006) and time of intubation (10.0 vs. 3.0 days, p<0.001) compared to controls. Cases had significantly higher prevalence of tobacco use (49.2% vs 30.9%, p=0.010) and diabetes (30.3% vs 16.1%, p=0.014) compared to controls (Table 2).
Table 2;
Demographics, socioeconomic status, and comorbidities of LTS cases versus ICU controls: A comparison of the LTS population to age-matched controls who underwent prolonged intubation without the development of stenosis
| LTS Study Population (n=122) | VUMC ICU (n=118) | Significance (p) | |
|---|---|---|---|
| Demographics | |||
| Age, Median years (IQR†) | 53.0 (24.3–81.8) | 54.0 (22.6–85.4) | 0.282 |
| Sex, Male, N (%) | 65 (52.9) | 67 (56.8) | 0.678 |
| Race, Caucasian, N (%) | 102 (83.1) | 87 (73.7) | 0.087 |
| Socioeconomic Status and Comorbidities | |||
| Median Household Income, dollars, Median (IQR) | 46014 (28846–63183) | 44583 (31948–57217) | 0.469 |
| Coverage Type, Public, N (%) | 76 (65.5) | 60 (59.4) | 0.431 |
| Percent College Educated, Median (IQR) | 19.1 (0.8–37.4) | 18.4 (0.1–36.8) | 0.733 |
| BMI, kg/m2, Median (IQR) | 30.3 (17.1–43.5) | 26.1 (15.9–36.3) | 0.006 |
| Tobacco Use, N (%) | 58 (49.2) | 30 (30.9) | 0.010 |
| Type II Diabetes Mellitus, N (%) | 37 (30.3) | 19 (16.1) | 0.014 |
| Intubation | |||
| Time of Intubation, Days, Median (IQR) | 10.0 (3.0–17.0) | 3.0 (1.0–5.0) | <0.001 |
IQR = Interquartile Range
Multivariable Analysis of Cases and Controls
Multivariable logistic regression was performed to determine if sociodemographic factors, medical comorbidities, and time of intubation were independently associated with LTS development. Tobacco use (OR: 1.21, p=0.006), body mass index (OR: 1.04, p=0.035), and time of intubation (OR: 1.21, p<0.001) continued to be significantly associated with the LTS population (Table 3).
Table 3;
Multivariable analysis of cases and controls: A multivariable logistic regression assessing the difference between insurance status, diabetes, age, income, tobacco use, intubation, and BMI between cases and controls.
| Unadjusted Analysis | Adjusted Analysis | |||||
|---|---|---|---|---|---|---|
| Factors | UOR† | 95% CI | p | AOR‡ | 95% CI | p |
| Insurance Status, public vs. private | 1.07 | 0.93–1.22 | 0.356 | 1.04 | 0.90–1.20 | 0.570 |
| Age, 10 year units | 1.02 | 0.99–1.05 | 0.248 | 0.97 | 0.94–1.01 | 0.207 |
| Median Household Income, 10k units | 1.03 | 0.99–1.06 | 0.165 | 1.01 | 0.97–1.04 | 0.713 |
| Diabetes Mellitus II | 1.22 | 1.05–1.41 | 0.009 | 1.07 | 0.91–1.26 | 0.437 |
| Tobacco Use | 1.21 | 1.05–1.38 | 0.007 | 1.21 | 1.06–1.39 | 0.006 |
| Body Mass Index, 5kg/m2 units | 1.05 | 1.02–1.09 | 0.005 | 1.04 | 1.00–1.08 | 0.035 |
| Time of Intubation, 5 day units | 1.24 | 1.19–1.30 | <0.001 | 1.21 | 1.15–1.26 | <0.001 |
UOR = unadjusted odds ratio
AOR = adjusted odds ratio
Univariate Analysis of Case Outcomes
Univariate analysis was done within the case cohort to determine if social determinants of health had an association with the primary outcome of tracheostomy dependence (Table 4). Tracheostomy dependent patients had significantly higher prevalence of public insurance (84.0% vs. 53.0%, p=0.001) and diabetes (43.1% vs 21.1%, p=0.016). Time of intubation (14.0 vs. 8.0 days, p=0.043) and McCaffrey stage (4.0 vs. 3.0, p=0.015) were higher in the tracheostomy dependent group. The non-tracheostomy dependent group had higher prevalence of open surgical intervention (74.6% vs. 45.1%, p=0.002). No difference was found in tobacco use, body mass index (BMI), median household income, or college education. We additionally assessed the prevalence of chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), myocardial infarction (MI), and transient ischemic attack or stroke by case outcome (supplementary information S3). We found COPD to be significantly higher in the tracheostomy dependent group (58.8% vs. 18.3%, p<0.001).
Table 4;
Analysis of social determinants of health on LTS outcomes: Subgroup analysis of the case cohort comparing tracheostomy dependent and non-tracheostomy dependent patients
| Tracheostomy (n=51) | No Tracheostomy (n=71) | Significance (p) | |
|---|---|---|---|
| Demographics | |||
| Age, Median years (IQR†) | 54 (23.0–85.0) | 50 (22.5–77.5) | 0.288 |
| Sex, Male, N (%) | 22 (43.1) | 43 (60.6) | 0.086 |
| Race, Caucasian, N (%) | 39 (76.5) | 63 (88.7) | 0.120 |
| Socioeconomic Status and Comorbidities | |||
| Median Household Income, dollars, Median (IQR) | 46780 (25886–67674) | 44195 (27657–60733) | 0.540 |
| Coverage Type, Public, N (%) | 42 (84.0) | 35 (53.0) | 0.001 |
| Uninsured, N (%) | 1 (2.0) | 5 (7.0) | 0.392 |
| Percent College Educated, Median (IQR) | 20.0 (0.4–39.6) | 18.4 (1.7–35.0) | 0.289 |
| BMI, kg/m2, Median (IQR) | 32.6 (18.7–46.5) | 28.8 (16.2–41.4) | 0.278 |
| Tobacco Use, N (%) | 27 (54.0) | 31 (45.6) | 0.469 |
| Type II Diabetes Mellitus, N (%) | 22 (43.1) | 15 (21.1) | 0.016 |
| Intubation and Surgical Intervention | |||
| Open Surgical Intervention, N (%) | 23 (45.1) | 53 (74.6) | 0.002 |
| Time of Intubation, Days, Median (IQR) | 14.0 (4.8–23.3) | 8.0 (0.0–16.0) | 0.043 |
| Stage of Disease | |||
| McCaffrey Stage, Median (IQR) | 4.0 (3.0–5.0) | 3.0 (1.0–5.0) | 0.015 |
IQR = Interquartile Range
Multivariable Analysis of Case Outcomes
Multivariable regression analysis was performed to determine if social determinants of health, operation type, medical comorbidities, and severity of disease were independent predictors of tracheostomy at last follow-up (Table 5). Public insurance status (OR: 1.33, p=0.016) and COPD (OR: 1.34, p=0.018) remained significantly independently associated with tracheostomy dependence in multivariable logistic regression even when adjusting for age, operation type, time of intubation, stage of disease, diabetes, and income.
Table 5;
Multivariable analysis of predictors of tracheostomy dependence: A multivariate analysis assessing insurance status, diabetes mellitus, age, disease severity, and income on tracheostomy dependence at last known follow-up.
| Unadjusted Analysis | Adjusted Analysis | |||||
|---|---|---|---|---|---|---|
| Factors | UOR† | 95% CI | p | AOR‡ | 95% CI | p |
| Insurance Status, public vs. private | 1.42 | 1.19–1.70 | <0.001 | 1.33 | 1.06–1.66 | 0.016 |
| Age, 10 year units | 1.03 | 0.98–1.08 | 0.272 | 1.02 | 0.96–1.08 | 0.598 |
| Median Household Income, 10k units | 1.02 | 0.97–1.07 | 0.501 | 1.00 | 0.95–1.05 | 0.880 |
| Surgical Intervention, open vs. noninvasive | 0.74 | 0.62–0.88 | <0.001 | 0.90 | 0.71–1.13 | 0.357 |
| Diabetes Mellitus II | 1.29 | 1.07–1.55 | 0.009 | 1.12 | 0.88–1.43 | 0.354 |
| Chronic Obstructive Pulmonary Disease | 1.54 | 1.30–1.82 | <0.001 | 1.34 | 1.06–1.69 | 0.018 |
| Time of Intubation, 5 day units | 1.04 | 0.97–1.12 | 0.244 | 1.03 | 0.97–1.10 | 0.355 |
| McCaffrey Stage | 1.11 | 1.00–1.21 | 0.045 | 1.05 | 0.94–1.19 | 0.390 |
UOR = unadjusted odds ratio
AOR = adjusted odds ratio
DISCUSSION
This is the first study to describe the social determinants of health in the LTS patient population and explore the association of those variables with disease development and treatment outcome. Our data suggests that low social determinants of health are associated with critical illness requiring intubation and mechanical ventilation in the ICU but not necessarily with LTS development. Once intubated in the ICU, patient specific comorbidities, health behaviors, and procedural factors (i.e. length of intubation) are associated with LTS development. After the development of LTS, low social determinants of health are associated with negative treatment outcomes. Treatment outcome was also negatively impacted by comorbid COPD.
When comparing the population of LTS to the surrounding community, we found a higher prevalence of obesity (p=0.032), tobacco use (p<0.001), and diabetes (p=0.001) in the LTS population. Additionally, we found lower prevalence of college education (p=0.009). Yet, when comparing LTS cases to age-matched ICU controls we found comparable rates of college education but higher prevalence of tobacco use (p=0.010) and diabetes (p=0.014) along with higher median BMI (p=0.006). These findings suggest that while the LTS population has lower social determinants of health compared to the surrounding community, these social determinants are less important in distinguishing which ICU patients will develop stenosis. However, it is difficult to precisely unravel the effect of medical comorbidities and health behaviors as they are also closely tied to the social determinants of health.
In geographic analysis, we found no statistically significant clusters of LTS patients, but rather the density of LTS patients correlated with the population of that zipcode. The lack of geographic clustering argues against the concept that a single hospital’s intubation practices are adding significantly to the burden of LTS in the community. However, the limits of administrative data prevent a definitive answer to this question and this will be an area of active research in the future.
The social determinants of health affect a wide range of health-related outcomes and play a significant role in the health disparities of America. Higher income, for example, has been found to associate with greater life expectancy.18 Meanwhile, lower socioeconomic status has been associated with higher post-discharge mortality among elderly patients.19 While social determinants such as education, race, and income have been associated with disease development and outcomes,19–22 they are also intricately associated with each other as well as additional social determinants, health behaviors, and medical comorbidities.23–25 Thus, the causality of a single social determinant on disease outcome is difficult to identify but rather several social determinants often work together to influence disease development.
Various studies have explored the role of social determinants on intensive care unit admissions, disease severity, and patient outcomes.26–29 Epstein et al. 2014 found that lower income, Latino race, and children with government insurance were all associated with higher disease severity at the time of admission to the ICU. Some studies have focused on the impact of social determinants on asthma ICU admissions, but with conflicting results.27,28,30 Moghaddas et al. 2016 found asthmatic patients admitted to the ICU had a lower socioeconomic index when compared to those admitted to the general ward. McDowell et al. 2016, on the other hand, found intrinsic disease factors, such as allergic sensitization, were more important for ICU admission among asthmatic patients. Other studies have investigated the impact of social determinants on ICU procedures and outcomes.29,31,32 Fowler et al. 2010 concluded that critically ill patients who were uninsured were less likely to receive critical care services, and once admitted to the ICU were less likely to have procedures and more likely to have life support withdrawn. It is possible patients with lower social determinants of health present with increased disease severity and consequently require longer durations of intubation. However, there does not appear to be a significant difference in the social determinants among prolonged intubation patients who subsequently develop LTS and those who do not.
Open surgical intervention was associated with a lower risk of tracheostomy dependence when compared to endoscopic treatment alone in univariate analysis (74.6% vs. 45.1%, p=0.002). This finding did not persist in multivariable analysis, although this may be due to the limited sample size of our study. Several prior studies that have demonstrated more invasive procedures are associated with higher rates of decannulation.33–35 For this reason, the majority of airway surgeons reserve more invasive procedures (open resections) for patients who fail to respond to conservative measures.33
Finally, public insurance was significantly associated with tracheostomy dependence in multivariable analysis when adjusting for age, operation type, income, diabetes, COPD, time of intubation, and stage of disease. Insurance status is a well-recognized social determinant of health that impacts several health outcomes. Uninsured and underinsured adults experience barriers to utilizing healthcare and therefore do not obtain preventative health measures such as flu vaccines.36 Medicaid patients also experience barriers with timely access to primary care and more often utilize emergency departments.37 Public insurance may represent a barrier to healthcare either within the intensive care unit itself or with specialized follow-up after discharge. Additional studies that differentiate among Medicare and Medicaid patients would be needed to fully understand the impact of public insurance on LTS treatment outcomes.
An in-depth understanding of the social determinants of health is critical for managing and preventing chronic illness.38 Iatrogenic LTS represents the most common etiology of LTS and creates a significant burden on the healthcare system and patients.9,10 This subgroup of LTS is also more likely to suffer from worse long-term outcomes such as tracheostomy dependence.10,11 Our study suggests that the social determinants of health are associated with poor long-term treatment outcomes in LTS. By recognizing risk factors for poor treatment outcome, these patients can be pre-emptively identified in the ICU for airway monitoring and follow-up with an airway specialist after discharge. Larger endotracheal tubes have been associated with increased risk of airway injury,12,39 and early tracheostomy has been shown to shorten ICU stays and prevent complications such as pneumonia, acute respiratory distress syndrome, and airway injury.40,41 Early follow-up allows for management of acute inflammatory lesions and prevention of mature scar tissue.42 Therefore, early identification of these patients may allow for personalized care through smaller endotracheal tubes, early tracheostomy, and close airway follow-up. Moreover, scheduled post-ICU visits with an airway specialist may prevent patients from being lost to follow-up after their ICU stay.
While we report novel results that may be further explored with additional studies, there are inherent limitations to our study. We are limited in sample size in part due to the prevalence of LTS and the loss of these patients to follow-up. This affected our power and it is possible that with increased sample size we would find that factors such as income also impacted LTS and its complications. Additionally, the majority of our control population was defined by a lack of otolaryngologic consult rather than a negative laryngeal exam, and it is possible that some control patients had underlying LTS. Despite this, we were able to find significant differences between these two groups. While we acknowledge that the use of tracheostomy dependence as a primary treatment outcome in LTS has limitations (as other disease processes can affect this outcome), it remains an outcome with high patient-perceived value. Our assessment of additional medical comorbidities that may be associated with tracheostomy dependence (COPD, MI, CHF, stroke) support this contention. We found that COPD was significantly associated with tracheostomy at last follow-up. However even when accounting for this variable in multivariable logistic regression public insurance status remained significantly associated with worse outcome. In future studies, patient-reported quality of life metrics may also be utilized for a more nuanced outcome assessment.
Moreover, similar to prior studies, we utilized zipcodes to obtain socioeconomic information for patient neighborhoods via the ACS. This causes us to lose data granularity and introduces the error of making judgements for the individual based on the group. Nonetheless, we were able to both reinforce known associations with LTS development and outcome as well as discover a potentially new association that warrants additional research. Further investigation into the impact of the social determinants of health on LTS development and therapy may facilitate patient-centered-care and improve long-term functional outcomes.
Conclusion
Lower social determinants of health may play a role in ICU admission and care but are less important for the development of stenosis after prolonged intubation. Lower social determinants and poor pulmonary function are associated with tracheostomy dependence after LTS treatment. Identification of at-risk populations in ICUs may allow for disease prevention and enhanced outcomes. Future mechanistic studies are needed to explore the causality of these relationships.
Supplementary Material
Acknowledgments
All authors have no disclosures. All authors had full access to the data and take responsibility for the integrity and accuracy of the data analysis.
Footnotes
Meeting Information: Combined Otolaryngology Spring Meeting, Austin, TX, USA, May 1–5th 2019
Funding and Conflicts of Interest: None
References
- 1.Bergmark RW, Sedaghat AR. Disparities in health in the United States: An overview of the social determinants of health for otolaryngologists. Laryngoscope Investigative Otolaryngology. 2017;2(4):187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: Addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283(19):2579–2584. [DOI] [PubMed] [Google Scholar]
- 3.Scangas GA, Ishman SL, Bergmark RW, Cunningham MJ, Sedaghat AR. Emergency department presentation for uncomplicated acute rhinosinusitis is associated with poor access to healthcare. The Laryngoscope. 2015;125(10):2253–2258. [DOI] [PubMed] [Google Scholar]
- 4.Daraei P, Moore CE. Racial Disparity Among the Head and Neck Cancer Population. J Cancer Educ. 2015;30(3):546–551. [DOI] [PubMed] [Google Scholar]
- 5.Xie DX, Wang RY, Penn EB, Chinnadurai S, Shannon CN, Wootten CT. Understanding sociodemographic factors related to health outcomes in pediatric obstructive sleep apnea. International Journal of Pediatric Otorhinolaryngology. 2018;111:138–141. [DOI] [PubMed] [Google Scholar]
- 6.Lieu TA, Ray GT, Klein NP, Chung C, Kulldorff M. Geographic clusters in underimmunization and vaccine refusal. Pediatrics. 2015;135(2):280–289. [DOI] [PubMed] [Google Scholar]
- 7.Samuelson MB, Chandra RK, Turner JH, Russell PT, Francis DO. The relationship between social determinants of health and utilization of tertiary rhinology care. Am J Rhinol Allergy. 2017;31(6):376–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Naunheim MR, Paddle PM, Husain I, Wangchalabovorn P, Rosario D, Franco RA Jr., Quality-of-Life Metrics Correlate With Disease Severity in Idiopathic Subglottic Stenosis. Laryngoscope. 2018. [DOI] [PubMed] [Google Scholar]
- 9.de la Fuente J, Garrett CG, Ossoff R, Vinson K, Francis DO, Gelbard A. A Case Series of the Probability Density and Cumulative Distribution of Laryngeal Disease in a Tertiary Care Voice Center. Ann Otol Rhinol Laryngol. 2017;126(11):748–754. [DOI] [PubMed] [Google Scholar]
- 10.Gelbard A, Francis DO, Sandulache VC, Simmons JC, Donovan DT, Ongkasuwan J. Causes and consequences of adult laryngotracheal stenosis. The Laryngoscope. 2014;125(5):1137–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gadkaree SK, Pandian V, Best S, et al. Laryngotracheal Stenosis: Risk Factors for Tracheostomy Dependence and Dilation Interval. Otolaryngol Head Neck Surg. 2017;156(2):321–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hillel AT, Karatayli-Ozgursoy S, Samad I, et al. Predictors of Posterior Glottic Stenosis: A Multi-Institutional Case-Control Study. Ann Otol Rhinol Laryngol. 2016;125(3):257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koshkareva Y, Gaughan JP, Soliman AM. Risk factors for adult laryngotracheal stenosis: a review of 74 cases. Ann Otol Rhinol Laryngol. 2007;116(3):206–210. [DOI] [PubMed] [Google Scholar]
- 14.McCaffrey VT. Classification of laryngotracheal stenosis. The Laryngoscope. 1992;102(12):1335–1340. [DOI] [PubMed] [Google Scholar]
- 15.Data & Statistics Diabetes. 2018; https://www.cdc.gov/diabetes/data/. Accessed November 17, 2018.
- 16.Data, Trend and Maps. https://www.cdc.gov/nccdphp/dnpao/data-trends-maps/index.html. Accessed Dec 06, 2018.
- 17.Extinguishing the tobacco epidemic in Tennessee. 2018; https://www.cdc.gov/tobacco/about/osh/state-fact-sheets/tennessee/. Accwessed November 17, 2018.
- 18.Chetty R, Stepner M, Abraham S, et al. The association between income and life expectancy in the united states, 2001–2014. JAMA. 2016;315(16):1750–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu L, Sullivan DH. Relationship between social demographic factors and survival within one year of hospital discharge in a cohort of elderly male patients. J Epidemiol. 2003;13(4):203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coffey PM, Ralph AP, Krause VL. The role of social determinants of health in the risk and prevention of group A streptococcal infection, acute rheumatic fever and rheumatic heart disease: A systematic review. PLoS neglected tropical diseases. 2018;12(6):e0006577–e0006577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rönkä S, Karjalainen K, Martikainen P, Mäkelä P. Social determinants of drug-related mortality in a general population. Drug and Alcohol Dependence. 2017;181:37–43. [DOI] [PubMed] [Google Scholar]
- 22.Borschuk AP, Everhart RS. Health disparities among youth with type 1 diabetes: A systematic review of the current literature. Fam Syst Health. 2015;33(3):297–313. [DOI] [PubMed] [Google Scholar]
- 23.Adler NE, Glymour M, Fielding J. Addressing social determinants of health and health inequalities. JAMA. 2016;316(16):1641–1642. [DOI] [PubMed] [Google Scholar]
- 24.Babey SH, Hastert TA, Wolstein J, Diamant AL. Income disparities in obesity trends among California adolescents. American journal of public health. 2010;100(11):2149–2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pampel FC, Denney JT. Cross-national sources of health inequality: education and tobacco use in the World Health Survey. Demography. 2011;48(2):653–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Epstein D, Reibel M, Unger JB, et al. The effect of neighborhood and individual characteristics on pediatric critical illness. Journal of community health. 2014;39(4):753–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moghaddas F, Smith C, Pilcher D, O’Hehir R, Hew M, Dabscheck E. Need for intensive care in patients admitted for asthma: Red flags from the social history. Respirology. 2016;21(7):1251–1254. [DOI] [PubMed] [Google Scholar]
- 28.McDowell KM, Kercsmar CM, Huang B, Guilbert TW, Kahn RS. Medical and Social Determinants of Health Associated with Intensive Care Admission for Asthma in Children. Ann Am Thorac Soc. 2016;13(7):1081–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fowler RA, Noyahr L-A, Thornton JD, et al. An Official American Thoracic Society Systematic Review: The Association between Health Insurance Status and Access, Care Delivery, and Outcomes for Patients Who Are Critically Ill. American Journal of Respiratory and Critical Care Medicine. 2010;181(9):1003–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Belessis Y, Dixon S, Thomsen A, et al. Risk factors for an intensive care unit admission in children with asthma. Pediatr Pulmonol. 2004;37(3):201–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kumar G, Taneja A, Majumdar T, et al. The association of lacking insurance with outcomes of severe sepsis: retrospective analysis of an administrative database*. Critical care medicine. 2014;42(3):583–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lyon SM, Benson NM, Cooke CR, Iwashyna TJ, Ratcliffe SJ, Kahn JM. The effect of insurance status on mortality and procedural use in critically ill patients. Am J Respir Crit Care Med. 2011;184(7):809–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gadkaree SK, Gelbard A, Best SR, Akst LM, Brodsky M, Hillel AT. Outcomes in Bilateral Vocal Fold Immobility: A Retrospective Cohort Analysis. Otolaryngology–Head and Neck Surgery. 2018;159(6):1020–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamamoto K, Kojima F, Tomiyama K-i, Nakamura T, Hayashino Y. Meta-Analysis of Therapeutic Procedures for Acquired Subglottic Stenosis in Adults. The Annals of Thoracic Surgery. 2011;91(6):1747–1753. [DOI] [PubMed] [Google Scholar]
- 35.Terra RM, Minamoto H, Carneiro F, Pego-Fernandes PM, Jatene FB. Laryngeal split and rib cartilage interpositional grafting: treatment option for glottic/subglottic stenosis in adults. J Thorac Cardiovasc Surg. 2009;137(4):818–823. [DOI] [PubMed] [Google Scholar]
- 36.Villarroel MA, Cohen RA. Health insurance continuity and health care access and utilization, 2014. Age. 2016;7:2. [PubMed] [Google Scholar]
- 37.Cheung PT, Wiler JL, Lowe RA, Ginde AA. National Study of Barriers to Timely Primary Care and Emergency Department Utilization Among Medicaid Beneficiaries. Annals of Emergency Medicine. 2012;60(1):4–10.e12. [DOI] [PubMed] [Google Scholar]
- 38.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52. [DOI] [PubMed] [Google Scholar]
- 39.Schiff BA. The Relationship between Body Mass, Tracheal Diameter, Endotracheal Tube Size, and Tracheal Stenosis. Int Anesthesiol Clin. 2017;55(1):42–51. [DOI] [PubMed] [Google Scholar]
- 40.Mahafza T, Batarseh S, Bsoul N, Massad E, Qudaisat I, Al-Layla AEe. Early vs. late tracheostomy for the ICU patients: Experience in a referral hospital. Saudi journal of anaesthesia. 2012;6(2):152–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Möller MG, Slaikeu JD, Bonelli P, Davis AT, Hoogeboom JE, Bonnell BW. Early tracheostomy versus late tracheostomy in the surgical intensive care unit. The American Journal of Surgery. 2005;189(3):293–296. [DOI] [PubMed] [Google Scholar]
- 42.Nouraei SAR, Singh A, Patel A, Ferguson C, Howard DJ, Sandhu GS. Early Endoscopic Treatment of Acute Inflammatory Airway Lesions Improves the Outcome of Postintubation Airway Stenosis. The Laryngoscope. 2006;116(8):1417–1421. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


