Abstract
Technological advances now permit self-management strategies using mobile applications which could greatly benefit patient care. The purpose of this study was to investigate whether the use of the inflammatory bowel disease (IBD) digital health monitoring platform, HealthPROMISE, leads to better quality of care and improved health outcomes in IBD patients. IBD patients were recruited in gastroenterology clinics and asked to install the HealthPROMISE application onto their smartphones. Patient satisfaction, quality of care, quality of life, patient symptoms, and resource utilization metrics were collected throughout the study and sent directly to their healthcare teams. Patients with abnormal symptom/SIBDQ scores were flagged for their physicians to follow up. After one-year, patient outcome metrics were compared to baseline values. Overall, out of 59 patients enrolled in the study, 32 patients (54%) logged into the application at least once during the study period. The number of IBD-related ER visits/hospitalizations in the year of use compared to the prior year demonstrated a significant decrease from 25% of patients (8/32) to 3% (1/32) (p = 0.03). Patients also reported an increase in their understanding of the nature/causes of their condition after using the application (p = 0.026). No significant changes were observed in the number of quality indicators met (p = 0.67) or in SIBDQ scores (p = 0.48). Given the significant burden of IBD, there is a need to develop effective management strategies. This study demonstrated that digital health monitoring platforms may aid in reducing the number of ER visits and hospitalizations in IBD patients.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10916-021-01706-x.
Keywords: Inflammatory bowel disease, IBD, Digital health monitoring, eHealth, Telemedicine, HealthPROMISE
Introduction
Inflammatory bowel disease (IBD) is comprised of Crohn’s disease (CD) and ulcerative colitis (UC), which are conditions involving chronic inflammation in the gastrointestinal tract [1]. Patients with IBD may experience diarrhea, abdominal pain, weight loss, bloody stools, and various extra-intestinal manifestations. Further, IBD is often associated with mood disorders, such as anxiety and depression, and may cause significant emotional distress [2]. Patients with IBD consistently report lower quality of life scores, higher rates of healthcare use, and decreases in productivity [3, 4].
The exact etiology of IBD remains unknown, however, it is speculated that genetically susceptible individuals may exhibit abnormal immune responses to triggers that subsequently lead to intestinal inflammation [5]. As a result, IBD is typically a chronic, lifelong condition where patients fluctuate between remissions and relapses. Therefore, current treatments are largely focused on symptom management and prevention of relapses.
To avoid urgent care, hospitalizations, and surgery, proactive care through ‘Treat to Target’ strategies aimed at the normalization of a patient’s symptoms and inflammatory markers are now considered best practice [6]. In spite of these evidence-based recommendations, these strategies are difficult to implement in regular clinical practice where patients are only seen every few months and ultimately leads to increased variation in the standards of care for patients with IBD [7]. Therefore, it is important for healthcare providers to provide patients with effective self-management strategies to complement outpatient care.
With the rapid rise of smart phones, electronic health (eHealth) monitoring platforms may be a promising medium to achieve a ‘Treat to Target’ goal. eHealth involves the use of technologies that facilitate health-related communication between patients and health care providers. It also provides patients with a means of tracking their medical information, learning about their condition, and getting their questions answered. A study by Wang et al found that patients who use smartphone applications (apps) to monitor their medical conditions felt more secure about their condition, participated in their health more, and felt like they were well taken care of outside of the clinical setting [8]. Further, the use of mobile health applications has been associated with decreases in cost and increases in convenience, productivity, and efficiency [9].
Studies investigating health monitoring platforms created for other chronic diseases such diabetes, cardiovascular diseases, asthma, and digestive diseases show promising improvements in clinical outcomes in some but not all studies [10, 11]. Further, studies have noted that research for digestive disease-specific applications are limited compared to other chronic diseases and that the majority of applications suffer from a lack of professional medical involvement [12]. Consequently, the evidence supporting IBD-specific health monitoring platforms, particularly those that include medical involvement, is limited [13].
The purpose of this study was to investigate the effect of implementing the IBD health monitoring platform, HealthPROMISE, in clinical practice and to evaluate whether its use leads to better quality of care and improved health outcomes.
Methods
HealthPROMISE health monitoring platform
HealthPROMISE is a cloud-based digital therapeutics and IBD monitoring application developed within the Sinai AppLab at the Icahn School of Medicine in Mount Sinai (New York, NY) in conjunction with healthcare providers treating IBD patients [14]. The application is now licensed to Rx.Health (Rx.Health, Inc., New York, NY) and available as part of American Gastroenterological Association Digital Transformation Network.
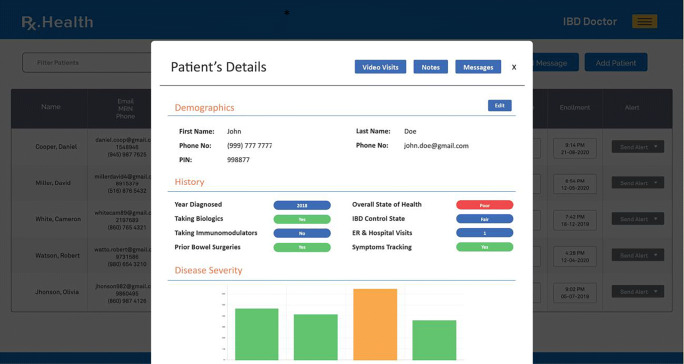
HealthPROMISE was developed based on patient input and designed to promote patient participation. Its creation was guided by a study that found three parameters that characterized the needs of IBD patients [15]. The investigators noted that patients complained of a lack of information dissemination by their providers, struggles with the social impacts of IBD, and called for a tool that facilitates symptom monitoring with physician feedback to patient input. Through the application, patients are able to track their symptoms, medications, quality of life scores (measured by Short Inflammatory Bowel Disease Questionnaire (SIBDQ), quality of care scores (measured by IBD quality indicators developed by the Canadian Association of Gastroenterology), visits with physicians, emergency room (ER) visits, or hospitalizations. They can then access their personal data through an individual patient dashboard where they can view the details of their different ePRO domains and their longitudinal trends (Fig. 1). Their physicians are also able to keep track of the data, suggest changes in lifestyle or treatment, or facilitate a clinic visit. Further, the application also permits the flagging of patients with suboptimal disease control, medication non-adherence, or extra-intestinal complications which may require further attention.
Fig. 1.
Individual patient view of the HealthPROMISE live dashboard showing details of all domains within ePROs (collected from the app) with longitudinal trends (courtesy Rx.Health, All4IBD program)
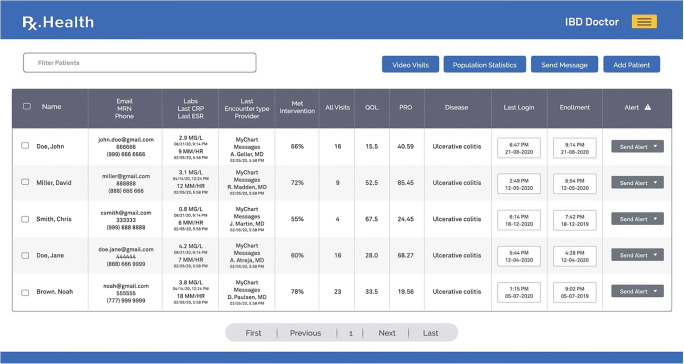
Within the HIPAA compliant HealthPROMISE dashboard, structured information and ePROs coming from the application are uploaded in real-time. With the recent integration of electronic health records, the dashboard now contains data columns related to C-reactive protein, erythrocyte sedimentation rate, and recent medical visits, next to ePRO columns to provide a 360-degree view of patients’ symptomology and inflammatory markers in one snapshot (Fig. 2). During COVID, we have also built in automation tools within the live dashboard to efficiently manage entire populations at IBD centres. A snapshot view of the application shows all the patients who are enrolled with alerts next to patients whose thresholds for ePROs are exceeded. From this view, care teams can select all patients with alerts and send them an individual or “bulk” messages using text or a chat feature with a link to an automated program for patients to request in-person or video visits appointments (instead of waiting on phone lines).
Fig. 2.
Population-level view of the HealthPROMISE live dashboard with columns for ePROs (collected from the app), inflammatory markers (collected from electronic health records) and alerting feature (based on clinical logic and best practices). The care teams can sort patients at highest risk and send them texts, chat links, or initiate video visits from the dashboard itself (courtesy Rx.Health, All4IBD program)
Study protocol
Participants were recruited from March 1, 2018 to September 30, 2018 at the gastroenterology clinics at McMaster University Medical Centre (Hamilton, Ontario). Eligible patients were 18 years or older, diagnosed with IBD, and have access to the application (via mobile phone, tablet, computer, etc). Exclusion criteria included the inability to communicate with investigators, comply with the study requirements, or the presence of any condition that may make it difficult to use the HealthPROMISE application, such as dementia.
Once enrolled in the study, patients received a quick briefing of HealthPROMISE, a walkthrough of the app, and access to a training video. Patients then completed a series of baseline questionnaires and were asked to fill out the symptom score indices in the application once every 2 weeks. The data entered was made visible through a secure online dashboard that is monitored by the healthcare provider’s team, including the most responsible physician and a nurse practitioner. Follow up was completed after 52 weeks and patients were asked to complete a series of end-of-study questionnaires. Patients who were not completing study questionnaires as expected were reminded monthly through a notification from the app. Meanwhile, there is a physician dashboard that sends periodic notifications to the healthcare team to remind them to contact the patient and provide feedback on patient inputs.
Study instruments
A combination of quality indicators, symptom score indices, and study questionnaires were used to evaluate patients during this study.
Quality indicators
A Canadian Association of Gastroenterology consensus meeting of gastroenterologists, surgeons, nurses, and patients identified forty-five quality indicators that IBD Centres of Excellence in Canada should aspire to achieve [16]. The number of quality indicators met serves as a proxy for the quality of care score of IBD patients. Patient-specific quality indicators from this meeting were implemented into the Canadian version of HealthPROMISE and can be found in the Supplementary Material (Table S1). Patients were asked to update their quality indicator checklist every 3 months.
Disease specific quality of life questionnaire and symptom score indices
The Short Inflammatory Bowel Disease Questionnaire (SIBDQ) is a validated tool for the measurement of health-related quality of life in adult patients with IBD [17]. The questionnaire is based on four domains: bowel symptoms, emotional health, systemic systems, and social function. Furthermore, patient reported outcome (PRO) scores were used to monitor Crohn’s disease and ulcerative colitis activity. For Crohn’s disease, patients were asked components of the Harvey-Bradshaw Index including the severity of their abdominal pain and the average number of liquid bowel movements they’ve had in the past week [18]. Meanwhile, for ulcerative colitis, patients were asked components of the Mayo score including their stool frequency and the presence of rectal bleeding [19]. The SIBDQ and patient reported outcome scores are fully integrated within the HealthPROMISE application and patients are asked to complete them every 2 weeks. Based on their bi-weekly responses, clinicians can identify patients who are not in good control of their condition who may need additional interventions or referrals. Patients were also asked to complete a baseline SIBDQ and an end-of-study SIBDQ at 52 weeks to determine overall quality of life improvements after HealthPROMISE use.
Patient satisfaction with care
To evaluate patient satisfaction, their perceptions regarding their understanding of IBD, and their relationship with their healthcare team, a satisfaction questionnaire was administered at baseline and after 52 weeks of using HealthPROMISE. A patient satisfaction questionnaire that was previously validated for chronic disease management in an outpatient setting was adapted for this study and can be found in the Supplementary Material (Table S2) [20]. Responses were recorded on a five-point Likert-type scale ranging from strongly disagree to strongly agree for the endorsement of each statement.
Statistical analysis
All patient data were collected through their electronic health records (EHRs), the HealthPROMISE dashboard, and study questionnaires. Data were then analyzed using GraphPad Prism (version 5.03, GraphPad Software, San Diego, CA, USA) and SAS 9.4 (Cary, NC, USA). Comparisons of means, such as the number of hospitalizations/ER visits prior to and after 52 weeks of HealthPROMISE use, were analyzed with the Student’s t test. SIBDQ and quality indicator scores were compared using the Wilcoxon signed rank test given these were not normally distributed. Meanwhile, patient satisfaction was dichotomized into patients satisfied with care versus those who are not, and a comparison was made between the percentage of patients satisfied prior and after the use of HealthPROMISE using the chi-square test. Alpha was set to 0.05 and p-values of <0.05 were considered statistically significant.
Ethics statement
This study was approved by the Hamilton Integrated Research Ethics Board. Written informed consent was obtained from all participants before enrolling in the study.
Results
Participants
A total of 59 patients were enrolled into the study. 32 (54%) of these patients logged into the HealthPROMISE application at least once over the 12-month follow up period (median 6 logins, range 1–52). Out of the 32 participants, 37.5% were female (n = 12) with a median age of 28.5 years (Table 1). From the 27 patients that did not use the application, the reasons provided at the end of the study period included: technical difficulties (6), forgot their password (5), lost interest (5), were too busy (4), felt their condition was adequately controlled (2), and 5 patients did not respond. These patients were excluded from the analysis.
Table 1.
Patient demographics
| Characteristics | N = 32 |
| Age (years), median (IQR) | 28.5 (22–38) |
| Sex, n (%) | |
|
Male Female |
20 (62.5) 12 (37.5) |
| Diagnosis, n (%) | |
|
Crohn’s disease Ulcerative colitis |
23 (71.9) 9 (28.1) |
| Smoking status, n (%) | |
|
Active smoker Past smoker Non-smoker |
5 (15.6) 5 (15.6) 22 (68.8) |
Quality indicators and health-related quality of life
Analysis of the PACE IBD quality indicators revealed that there was no significant difference in the number of indicators met after one year of HealthPROMISE use (median = 7.5, IQR 3–10.75) compared to the year prior to use (median = 7.5, IQR 6.25–10.75) (p = 0.67).
Further, analysis of SIBDQ scores as a proxy measurement for health-related quality of life and symptom control revealed no significant difference in baseline scores (median = 21, IQR 17.5–43.5) compared to end-of-study scores (median = 22, IQR 12.75–38.5) (p = 0.48).
Patient satisfaction
Patient satisfaction questionnaires administered at baseline and after 1 year of using the HealthPROMISE platform revealed a significant increase in the number of patients who strongly agree or agree with the statement, “I am satisfied that I understand the nature and causes of my health condition” (74.2% versus 96.8%, p = 0.026) (Table 2). Satisfaction scores regarding the relationship that patients have with their physicians and patient knowledge of disease prevention/treatment showed no significant differences after 1 year.
Table 2.
Patient satisfaction at baseline and after 1 year of HealthPROMISE use
| Question | Number of patients who strongly agreed or agreed at baseline | Number of patients who strongly agreed or agreed after 1 year of HealthPROMISE use | p value |
|---|---|---|---|
| I am satisfied with the patient education at McMaster University Medical Centre | 30/31 | 29/31 | 1.0 |
| I am satisfied that my doctor told me about my condition, the treatment options and how I can stay healthy. | 31/31 | 31/31 | 1.0 |
| I am satisfied that I understand the nature and causes of my health condition | 23/31 | 30/31 | 0.026 |
| I am satisfied that I know the different medical treatment options available for my health condition | 28/31 | 30/31 | 0.61 |
| I am satisfied that I know how to prevent further problems with my health condition | 23/31 | 28/31 | 0.18 |
Hospitalizations and emergency room visits
Over the course of follow-up, 13 patients (40.6%) were called by their healthcare team due to a high SIBDQ or partial Harvey Bradshaw Index score indicating sub-optimal management of their disease. Meanwhile, 7 patients (21.9%) had an expedited clinic visit scheduled to discuss their condition and 8 patients (25%) had their management and treatment plans changed to better control their condition. 1 patient (3%) was sent to the hospital by their healthcare practitioner as a result of symptoms consistent with a bowel obstruction.
Over the course of the study, there was 1 IBD-related hospitalization/ER visit in the year of using HealthPROMISE (3%) with a mean number of visits per patient of 0.03 (SD = 0.18). This is a significant decrease compared to the 8 IBD-related hospitalizations/ER visits in the year prior to use of HealthPROMISE (25%) with a mean number of visits per patient of 0.25 (SD = 0.51) (p = 0.03) (Fig. 3).
Fig. 3.
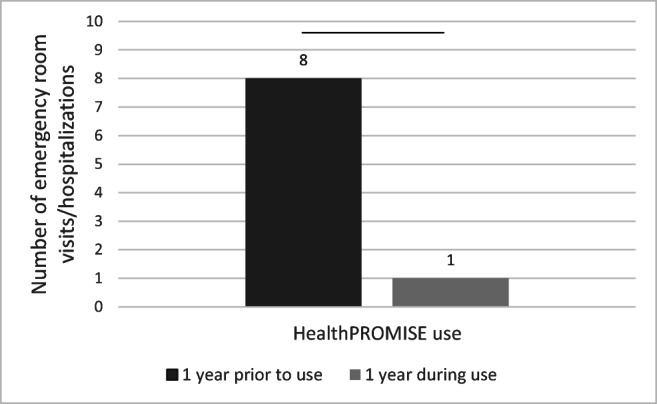
IBD-related ER/hospitalization utilization in the year prior to enrollment and the year post-enrollment into HealthPROMISE
Discussion
Due to the nature of IBD, patients often require medication adjustments or outpatient clinic visits, and have high healthcare utilization rates [21]. Consequently, IBD strains medical resources, leads to long wait lists for specialist care, and may disproportionately affect individuals that have barriers to care [22]. Therefore, patient engagement, with the guidance of their healthcare team, may provide an effective method to target key drivers of IBD flare-ups such as smoking and medication non-adherence [23]. Thus, this study sought to assess the impact of HealthPROMISE use on the quality of life, quality of care, and healthcare utilization of IBD patients.
Notably, the significant decrease from a 25% to 3% yearly ER/hospitalization rate after HealthPROMISE implementation represents a promising practical benefit of health monitoring applications (p = 0.03). This decrease is likely to be a direct result of the interventions that were prompted by concerning questionnaire scores on the application. Therefore, the use of a secure provider dashboard allows the team to be earlier informed and subsequently earlier address a patient who may be deteriorating. These results directly support published literature that demonstrate a decrease in hospitalizations in heart failure patients and chronic obstructive pulmonary disease (COPD) patients using mobile monitoring technologies [24, 25]. Further, while booking clinic visits or virtual visits to frequently follow-up with IBD patients regardless of their management status may be slow, ineffective, and low yield, with a steady stream of patient information from the application, physicians can quickly notice trends in symptomatology and effectively triage those who may need more urgent care. Additionally, the application provides a medium for both continuous and on-demand access to healthcare which is advantageous compared to the sporadic nature of clinic visits or virtual visits where patients may wait weeks to months for care and may forget about the course and severity of their symptoms. Further, where patients may pay out-of-pocket for healthcare, digital health applications could provide a more affordable and accessible means of communicating with their healthcare team [26].
We did not note any significant differences in IBD quality indicator or SIBDQ scores after HealthPROMISE implementation. These findings contribute to the mixed evidence of eHealth in other chronic health conditions. Numerous systematic reviews of mobile health monitoring in diabetes mellitus, cardiovascular disease, chronic lung disease, digestive diseases, and IBD found that approximately half of all included studies demonstrated statistically significant improvements in clinical outcome measures [10, 11, 21]. In an interim analysis of 320 IBD patients enrolled in a pragmatic randomized controlled trial of the HealthPROMISE application, Atreja et al. showed that the application led to significant improvement in quality indicators (15% vs 34%, P < 0.05), however, they found no improvements in quality of life scores [27]. Our findings could be attributed to a variety of factors in addition to differences in measurement and attribution. One consideration is that a number of factors are one-time considerations, for instance, having tuberculosis and hepatitis B screening conducted prior to initiation of advanced IBD therapy. Patients who started the study with tests already completed in the past would continue to answer that these tests were done throughout the study. Another factor would be that not all quality indicators are relevant to all participants. For example, the quality indicator encompassing smoking cessation advice would only be relevant to patients who smoke.
Previous studies have suggested that the majority of IBD patients felt their knowledge about their condition was inadequate and would like more information [28]. As a result, IBD-specific educational material is included in the HealthPROMISE application and patients are encouraged to explore the articles. Our study found that at baseline, IBD patients are generally very satisfied with the education they receive from their healthcare team. However, patients were more satisfied with their knowledge about the nature and causes of their health condition after HealthPROMISE use. These findings could be attributable to the nature of traditional out-patient encounters which often involves a heavy emphasis on diagnosis, treatment, and prevention. As a result, patients are often not well-informed about the epidemiology, symptoms, and causes of their medical condition, which often are multi-factorial and not very well understood. However, we acknowledge the subjectivity from self-assessments of an individual’s understanding of IBD. Future studies using objective measurements, such as a short quiz, could provide more objective results.
Our study participants were relatively young, with a median age of 28.5 years (IQR 22–38). As younger individuals are more likely to use technology for non-health related purposes when compared to older adults, they may be more likely to adopt eHealth applications [29]. The key challenge of most eHealth applications is its high attrition rate. As such, many eHealth studies have demonstrated that as few as 10% to 25% of recruited participants enter data by the end of the study [30]. This is consistent with our study which noted an attrition rate of 45.8% (27/59) despite the use of monthly reminders sent to participants and continuous testing/adjustments to improve the interface and navigation within the app. However, another similar review noted that no studies found any significant differences in the demographics or clinical features between the groups that dropped out and those who did not [10]. Therefore, the risk of attrition bias in this study is assumed to be minimal. Nevertheless, factors that have been found to enhance engagement with eHealth applications and could be included in future studies include decreasing the frequency of data collection, increasing the frequency of follow ups, and ensuring adequate study/technological support [30].
Overall, HealthPROMISE differentiates itself from many of the IBD-specific mobile health applications through the use of validated measurement tools, such as the SIBDQ, and a physician dashboard that connects the healthcare team with patients. However, there are several limitations to our study. First, our sample size was relatively small and combined with high rates of attrition, while consistent with other eHealth studies, potentially introduce a risk of attrition bias and reduced our ability to assess changes in outcomes. Further, as with many studies that involve mobile health applications, there may be selection bias as mainly participants that have the appropriate device, internet, and are comfortable with technology, will enroll in the study. Lastly, as participants were recruited from a single medical centre and geographical demographics were not collected, we could not investigate whether participants were more likely to use the application if they lived further from the medical centre or in rural communities. However, previous studies on eHealth have found that remote monitoring is an effective and reliable way to increase access to services to patients in remote and rural communities [31]. Future studies should involve a large sample size with diverse subsets of participants to investigate the generalizability of findings. Further, investigations evaluating acceptability and costs would help determine the feasibility of widely implementing mobile health applications in the management of IBD.
Conclusion
Health applications can provide an efficient, reliable, and consistent stream for the collection of clinical data and allows for more physician-patient interaction time to be directed towards counselling. Medical conditions that require frequent medical care, such as IBD, may benefit most from eHealth technologies involving proactive symptom management. This study demonstrated that HealthPROMISE, may increase levels of patient education and improve patient outcomes through reducing ER visits and hospitalizations. Health monitoring platforms, like HealthPROMISE, have the potential to scale, could be incorporated into electronic health records, and with the changing landscape of virtual care brought about by the COVID-19 pandemic, could become an essential part of healthcare.
Supplementary Information
(DOCX 39 kb)
Acknowledgements
The authors would like to acknowledge Ms. Cindy James for her efforts in patient recruitment and training.
Author contributions
Jamie Zhen - data interpretation; drafting of the manuscript;
John K. Marshall – study concept and design; data interpretation; drafting of the manuscript.
Geoffrey Nguyen - study concept and design; drafting of the manuscript.
Ashish Atreja - study concept and design; drafting of the manuscript.
Neeraj Narula - study concept and design; acquisition and compilation of data; statistical analysis; data interpretation; drafting of the manuscript;
Funding
This study was funded using a grant obtained from Crohn’s and Colitis Canada through the Promoting Access and Care through Centres of Excellence (PACE) initiative.
Compliance with ethical standards
No other author has any relevant conflicts of interest.
Conflict of interest
The RxUniverse software platform and HealthPROMISE digital therapeutic are licensed technologies from Icahn School of Medicine at Mount Sinai to Rx.Health, Inc. (New York, NY). Ashish Atreja owns stock in Rx.Health and have recused himself from data analysis. Neeraj Narula holds a McMaster University Department of Medicine Internal Career Award. Neeraj Narula has received honoraria from Janssen, Abbvie, Takeda, Pfizer, Merck, Sandoz, Novartis, and Ferring.
John Marshall receives honoraria as a speaker and/or consultant from AbbVie, Allergan, Amgen, Bristol Myers Squibb, Ferring, Fresenius Kabi, Janssen, Lilly, Lupin, Novartis, Paladin, Pfizer, Pharmascience, Procter & Gamble, Roche, Shire, Takeda, and Teva.
Footnotes
This article is part of the Topical Collection on Mobile and Wireless Health
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fakhoury M, Negrulj R, Mooranian A, Al-Salami H. Inflammatory bowel disease: clinical aspects and treatments. J Inflamm Res. 2014;7:113–20. doi: 10.2147/JIR.S65979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Byrne G, Rosenfeld G, Leung Y, Qian H, Raudzus J, Nunez C, et al. Prevalence of Anxiety and Depression in Patients with Inflammatory Bowel Disease. Can J Gastroenterol Hepatol. 2017;2017:6496727. doi: 10.1155/2017/6496727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernklev T, Jahnsen J, Lygren I, Henriksen M, Vatn M, Moum B. Health-related quality of life in patients with inflammatory bowel disease measured with the short form-36: psychometric assessments and a comparison with general population norms. Inflamm Bowel Dis. 2005;11(10):909–18. doi: 10.1097/01.mib.0000179467.01748.99. [DOI] [PubMed] [Google Scholar]
- 4.Cohen R, Skup M, Ozbay AB, Rizzo J, Yang M, Diener M, et al. Direct and indirect healthcare resource utilization and costs associated with ulcerative colitis in a privately-insured employed population in the US. J Med Econ. 2015;18(6):447–56. doi: 10.3111/13696998.2015.1021353. [DOI] [PubMed] [Google Scholar]
- 5.Guan Q. A Comprehensive Review and Update on the Pathogenesis of Inflammatory Bowel Disease. J Immunol Res. 2019;2019:7247238. doi: 10.1155/2019/7247238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atreja A. Smarter Care for Patients With Inflammatory Bowel Disease: A Necessity for IBD Home, Value-Based Health Care and Treat-to-Target Strategies. Inflamm Bowel Dis. 242018. p. 1460-1. [DOI] [PMC free article] [PubMed]
- 7.Riaz MS, Atreja A. Personalized Technologies in Chronic Gastrointestinal Disorders: Self-monitoring and Remote Sensor Technologies. Clin Gastroenterol Hepatol. 2016;14(12):1697–705. doi: 10.1016/j.cgh.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang J, Wang Y, Wei C, Yao NA, Yuan A, Shan Y, et al. Smartphone interventions for long-term health management of chronic diseases: an integrative review. Telemed J E Health. 2014;20(6):570–83. doi: 10.1089/tmj.2013.0243. [DOI] [PubMed] [Google Scholar]
- 9.Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P t. 2014;39(5):356–64. [PMC free article] [PubMed] [Google Scholar]
- 10.Whitehead L, Seaton P. The Effectiveness of Self-Management Mobile Phone and Tablet Apps in Long-term Condition Management: A Systematic Review. J Med Internet Res. 2016;18(5):e97. doi: 10.2196/jmir.4883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Helsel BC, Williams JE, Lawson K, Liang J, Markowitz J. Telemedicine and Mobile Health Technology Are Effective in the Management of Digestive Diseases: A Systematic Review. Dig Dis Sci. 2018;63(6):1392–408. doi: 10.1007/s10620-018-5054-z. [DOI] [PubMed] [Google Scholar]
- 12.Con D, De Cruz P. Mobile Phone Apps for Inflammatory Bowel Disease Self-Management: A Systematic Assessment of Content and Tools. JMIR Mhealth Uhealth. 2016;4(1):e13. doi: 10.2196/mhealth.4874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ullman TA, Atreja A. Building evidence for care beyond the medical centre. Lancet. 2017;390(10098):919–20. doi: 10.1016/S0140-6736(17)31857-3. [DOI] [PubMed] [Google Scholar]
- 14.Atreja A, Khan S, Rogers JD, Otobo E, Patel NP, Ullman T, et al. Impact of the Mobile HealthPROMISE Platform on the Quality of Care and Quality of Life in Patients With Inflammatory Bowel Disease: Study Protocol of a Pragmatic Randomized Controlled Trial. JMIR Res Protoc. 2015;4(1):e23. doi: 10.2196/resprot.4042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khan S, Dasrath F, Farghaly S, Otobo E, Riaz MS, Rogers J, et al. Unmet Communication and Information Needs for Patients with IBD: Implications for Mobile Health Technology. Br J Med Med Res. 2016;12(3). [DOI] [PMC free article] [PubMed]
- 16.Bitton A, Vutcovici M, Lytvyak E, Kachan N, Bressler B, Jones J, et al. Selection of Quality Indicators in IBD: Integrating Physician and Patient Perspectives. Inflamm Bowel Dis. 2019;25(2):403–9. doi: 10.1093/ibd/izy259. [DOI] [PubMed] [Google Scholar]
- 17.Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn's Relapse Prevention Trial. Am J Gastroenterol. 1996;91(8):1571–8. [PubMed] [Google Scholar]
- 18.Vermeire S, Schreiber S, Sandborn WJ, Dubois C, Rutgeerts P. Correlation between the Crohn's disease activity and Harvey-Bradshaw indices in assessing Crohn's disease severity. Clin Gastroenterol Hepatol. 2010;8(4):357–63. doi: 10.1016/j.cgh.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Lewis JD, Chuai S, Nessel L, Lichtenstein GR, Aberra FN, Ellenberg JH. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008;14(12):1660–6. doi: 10.1002/ibd.20520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siddharthan T, Rabin T, Canavan ME, Nassali F, Kirchhoff P, Kalyesubula R, et al. Implementation of Patient-Centered Education for Chronic-Disease Management in Uganda: An Effectiveness Study. PLoS One. 2016;11(11):e0166411. doi: 10.1371/journal.pone.0166411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson BD, Gray K, Knowles SR, De Cruz P. EHealth Technologies in Inflammatory Bowel Disease: A Systematic Review. J Crohns Colitis. 2016;10(9):1103–21. doi: 10.1093/ecco-jcc/jjw059. [DOI] [PubMed] [Google Scholar]
- 22.Longobardi T, Bernstein CN. Health care resource utilization in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2006;4(6):731–43. doi: 10.1016/j.cgh.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 23.Feagins LA, Iqbal R, Spechler SJ. Case-control study of factors that trigger inflammatory bowel disease flares. World J Gastroenterol. 2014;20(15):4329–34. doi: 10.3748/wjg.v20.i15.4329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park C, Otobo E, Ullman J, Rogers J, Fasihuddin F, Garg S, et al. Impact on Readmission Reduction Among Heart Failure Patients Using Digital Health Monitoring: Feasibility and Adoptability Study. JMIR Med Inform. 2019;7(4):e13353. doi: 10.2196/13353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang F, Wang Y, Yang C, Hu H, Xiong Z. Mobile health applications in self-management of patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis of their efficacy. BMC Pulm Med. 2018;18(1):147. doi: 10.1186/s12890-018-0671-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cassatly S, Cassatly M. The Affordable Care Act and Digital Health Applications. J Med Pract Manage. 2016;32(3):198–201. [PubMed] [Google Scholar]
- 27.Atreja, et al. App Monitoring Improves Quality of IBD Care GI & Hepatology News, 2018. Available at https://www.mdedge.com/gihepnews/article/167149/gastroenterology/app-monitoring-improves-quality-ibd-care. Accessed Aug 5, 2020).
- 28.Schölmerich J, Sedlak P, Hoppe-Seyler P, Gerok W. The information needs and fears of patients with inflammatory bowel disease. Hepatogastroenterology. 1987;34(4):182–5. [PubMed] [Google Scholar]
- 29.Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, et al. Factors predicting the use of technology: findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE) Psychol Aging. 2006;21(2):333–52. doi: 10.1037/0882-7974.21.2.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Druce KL, Dixon WG, McBeth J. Maximizing Engagement in Mobile Health Studies: Lessons Learned and Future Directions. Rheum Dis Clin North Am. 2019;45(2):159–72. doi: 10.1016/j.rdc.2019.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Banbury A, Roots A, Nancarrow S. Rapid review of applications of e-health and remote monitoring for rural residents. Aust J Rural Health. 2014;22(5):211–22. doi: 10.1111/ajr.12127. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 39 kb)