Abstract
Objective:
Compare the 2016 Federal Motor Carrier Safety Administration (FMCSA) and 2006 Joint Task Force (JTF) Guidelines for commercial drivers’ obstructive sleep apnea (OSA) screening.
Methods:
Retrospective review of all commercial driver medical examinations performed in 2017 at an academic occupational medicine clinic. Screening criteria from both the JTF and FMCSA were applied, separately, and jointly. Statistical tests were applied as appropriate.
Results:
Applying the FMCSA or JTF criteria separately to 706 commercial drivers, the positive OSA screening yields were 15.7% and 16.9%, respectively. Using both criteria produced an overall positive OSA screen yield of 20.1%. Positive predictive values for applying both guidelines ranged from 72.7% to 95.5%.
Conclusions:
The combined use of the 2016 FMCSA and 2006 JTF OSA screening criteria in series has a higher screening yield than using either guideline individually.
Keywords: DOT medical examinations, Federal Motor Carrier Safety Administration, obstructive sleep apnea, obstructive sleep apnea screening
Obstructive sleep apnea (OSA) is characterized by repetitive cessations (apnea) or decrements (hypopnea) in airflow through the upper airways during sleep, resulting in a variety of physiological and metabolic disturbances, including frequent arousals from sleep and less deep sleep.1,2 Accordingly, OSA has been shown to increase the risk of diabetes, hypertension, metabolic syndrome, coronary heart disease, cognitive decline, and even sudden cardiac death.3–8
Due to the constant sleep disruptions caused by apneic and hypopneic episodes, OSA decreases both sleep quality and quantity. Therefore, OSA may be associated with both excessive daytime sleepiness and impaired vigilance/attention, which significantly increase the occupational risks for safety-sensitive positions such as commercial driving.9–13
It is estimated that 7% to 20% of all large truck crashes are due to fatigued drivers,9,14 and OSA is the most common medical cause of fatigue among these operators.15 There are robust data demonstrating that untreated OSA is associated with a 2 to 7-fold increase in the risk of motor vehicle accidents among primarily non-commercial drivers,10–12 a doubling of workplace accidents in general,13 and a 4 to 5-fold increase in preventable crashes among commercial drivers.9 Moreover, because OSA is closely associated with obesity and more common in middle-aged men, the prevalence of OSA among United States commercial drivers may be as high or higher than 28%, which equates to approximately 1.1 million commercial drivers with OSA.16 Furthermore, there are additional good data supporting that adequate treatment of OSA reduces the risk of motor vehicle crashes to control levels.9,10,17 Thus, the current body of medical and public health evidence strongly supports that commercial drivers should be screened for OSA during Federal Motor Carrier Safety Administration (FMCSA)—mandated commercial driver medical examinations.18
According to the FMCSA’s “Physical Qualifications for Drivers” 49 CFR 391.41(b),5 OSA, if present and not treated, is a disqualifying condition for operating a commercial vehicle.19 However, the current FMCSA regulations do not specify required methods for OSA screening during commercial driver medical examinations (CDME) other than a driver self-reported question.
Given the absence of formal FMCSA regulations to guide OSA screening, occupational medicine practitioners may choose from more recent OSA 2016 screening recommendations from the FMCSA’s Medical Review Board (MRB)20 or the 2006 Consensus Guidelines, put together by a Joint Task Force (JTF) comprised of representatives from the American College of Occupational and Environmental Medicine, the American College of Chest Physicians, and the National Sleep Foundation.21 The latter JTF guidelines have been viewed by many occupational medicine professionals as the minimum community standard for OSA screening for commercial drivers.22
Early cohort studies by Talmage et al23 and Parks et al1 demonstrated the efficacy and high positive predictive value of the JTF consensus criteria. However, to our knowledge, no previous study has examined the comparative efficacy of the 2006 JTF Consensus Guidelines with those of the newer 2016 FMCSA MRB recommendations. The aim of this study was to retrospectively compare the screening yields and positive predictive values of the 2016 FMCSA MRB Recommendations and the 2006 Joint Task Force’s Consensus Guidelines. Additionally, we examined the effect of using both sets of guidelines in tandem.
METHODS
Study Population and Setting
A retrospective cohort record review study was conducted at a busy academic occupational medicine clinic in the greater Boston area. We examined all CDME examination records of commercial drivers (truck, bus, and other drivers subject to the FMCSA-regulated medical certification examinations) who presented for CDME from January 2, 2017 through December 31, 2017. We continued to monitor and update follow up data for these drivers until January, 2020. A total of four FMCSA-certified medical examiners worked at this clinic during the study period. The study protocol was approved by the Institutional Review Board of Cambridge Health Alliance.
Screening Protocol and Data Collection
The clinic has screened commercial drivers for OSA as a standard practice since 2007 using the 2006 JTF Consensus Guidelines criteria. The current clinical protocol used in this clinic was modified and implemented in January 2017 and utilizes both the 2006 JTF Consensus Guidelines and the 2016 FMCSA MRB Recommendations. A summary of the two screening criteria and the clinic’s screening form can be found in Supplemental Digital Content 1, http://links.lww.com/JOM/A779.
Inclusion criteria were commercial drivers defined as truck, bus, and other drivers subject to the FMCSA-mandated examinations during the study period. We excluded drivers such as school bus drivers that presented for state-required physical examination clearances that were not FMCSA-regulated. When the same driver presented multiple times during the year, only the first CDME during the study period was used for the study, and subsequent visits were evaluated for follow-up outcomes. Sleep study referrals that were not completed with results returned before 3 months after the completion of the record review period were considered to be noncompliant with the request of the Medical Examiner.
The process of each CDME visit at the study clinic is summarized as below. At the beginning of the visit, the commercial driver answered questions on the federal CDME form which included a yes or no answer to a sleep disorder question asking if the driver “has a sleep disorder, pauses in breathing while asleep, daytime sleepiness, or loud snoring.” In addition, the driver also completed an Epworth Sleepiness Scale (ESS) on a separate form.24 The medical assistant then collected anthropometric data including height, weight, neck circumference, and resting blood pressure. Height and neck circumference were measured to the nearest half inch and weight was measured to the nearest pound wearing only light clothing. Body mass index (BMI) was then calculated by the medical assistant. Resting blood pressure was taken while the driver was seated and repeated up to one time if the initial reading was more than or equal to 140/90 mmHg. The driver then completed other CDME requirements, including urinalysis, vison, and hearing screening, prior to being seen by the medical examiner. During the examination, the medical examiner clarified any inconsistencies and/or asked additional questions, performed a physical examination, and then determined if the driver met either the JTF Consensus Guidelines or the FMCSA Recommendations OSA screening criteria. A printed summary and checklist containing the two screening guidelines were included in each driver’s chart during the examination. The medical examiners were recommended to document positive findings per the two guidelines on the CDME form. (Supplemental Digital Content 1, http://links.lww.com/JOM/A779).
While the use of the screening form was required by clinic policy, the medical examiner ultimately determined the certification result using the two screening criteria and his/her own clinical judgement. If the medical examiner determined the driver warranted a sleep study, a letter to the driver’s primary care physician would be provided to the driver requesting a referral preferably for in-laboratory, attended polysomnography (PSG), which is the gold standard for OSA diagnosis.25 Drivers who screened positive on either one or both sets of criteria generally received a shorter certification and were requested to return for re-examination after receiving a diagnostic test for OSA. If the driver had a prior OSA diagnosis or a positive OSA diagnostic test following screening, evidence of effective OSA treatment adherence (ie, compliance with Continuous, auto, or bilevel Positive Airway Pressure [CPAP, aPAP, or bPAP hereto forward “PAP”] therapy was requested required prior to further CDME certification and defined as at least 4 hours per night on >/=70% of nights).26
There was no required timeline for the subsequent sleep study and follow-up process other than the expiration of the medical certificate issued. The driver was responsible to coordinate the sleep study with his or her primary care physician. While an in-laboratory PSG was preferred, the type of sleep study (in-lab or home sleep apnea test) was determined by the driver’s primary care physician and health insurance. The driver was not obligated to return to our clinic for re-evaluation unless required by their employer.
Supporting documents, such as the ESS form, sleep study results, and at least 2 weeks of PAP adherence reports, were scanned into the electronic medical record and attached to the CDME form as part of the record. If a driver indicated use of PAP, adherence was determined through printed recent PAP usage report brought by the driver. If a report was not provided during the visit or within 1 week after the visit, the driver was determined to be non-compliant for the purpose for CDME. Non-compliant drivers were allowed to return for re-certification at a later date if they could provide subsequent documented PAP adherence.
Data Extraction
We conducted a case-by-case electronic chart review of all drivers that presented for CDME during the study period. We reviewed and recorded all data for eligible drivers regardless of the final certification disposition by the medical examiner. We extracted demographic, anthropometrics, and medical examination findings relevant to both screening criteria into a computerized database. BMI (kg/m2) was recalculated using the standard formula prior to recording for accuracy. The ESS score was recalculated based on the scanned form and entered into the database if available. We defined uncontrolled hypertension as resting blood pressure greater than or equal to 140/90 mmHg.27
We categorized and reported the final OSA screening decision as follows: (1) lower risk of OSA/excessive daytime sleepiness (EDS) and does not meet screening criteria; (2) OSA screen positive with no current evidence of EDS and can be given a conditional certification for up to 3 months; (3) significant risk of OSA with EDS and is disqualified until evaluated and treated; (4) OSA treatment compliant requiring no further referral; (5) OSA treatment non-compliant and given time to produce PAP compliance data or new sleep study; and (6) OSA on PAP but compliance not determined (usually due to another disqualifying medical condition making compliance irrelevant).
Medical charts of all drivers presented for CDME during the study period were reviewed including any subsequent visit(s). Additionally, Apnea-hypopnea Index (AHI) (or Respiratory Disturbance Index [RDI] or Respiratory Event Index [REI]) results were extracted from any prior sleep studies if scanned into the driver’s chart. In our clinic, an AHI or similar index more than or equal to 5 is considered probable OSA and an AHI more than 10 is considered definite OSA.26,30
Primary data extractions were performed and completed, and then verified during a second review by an independent set of reviewers. Disagreements on any categorization were resolved by an attending physician who is board-certified in occupational medicine and certified as an FMCSA medical examiner. A complete list of extracted variables and their definitions can be found in Supplemental Digital Content 2, http://links.lww.com/JOM/A776.
Statistical Analysis
Analyses were performed to evaluate the relationships between multiple OSA-related factors and the two screening criteria. According to the FMCSA MRB Recommendations, drivers were stratified by BMI as BMI more than or equal to 40 mg/kg2, and BMI more than or equal to 33 and less than 40 mg/kg2. We compared the yields of each set of screening criteria in isolation: positive OSA screens, negative OSA screens, among the positive OSA screens the proportion and characteristics of those subsequently determined to have a definitive diagnosis of OSA, and range of positive predictive values of the two different criteria within limitations. To further compare these two criteria, we further divided the participants based on their test results: positive for each criterion, positive for both criteria, and positive for only one criterion.
For the estimations of positive predictive values, we created three scenarios based conservatively on prior studies of commercial driver OSA screening28–30: best, intermediate, and worst-case scenario, defined as follow. For best case scenario, we excluded all drivers that lost follow-up during the study period or who were not referred for PSG by the provider. For intermediate case scenario, those subjects without defined follow-up we assumed: 1. If men with BMI less than 30 or women with any BMI, all were categorized as negative PSG; 2. If men with BMI 30 to 31.99, 50% of subjects in this group were assumed to have positive OSA diagnosis by PSG; 3. If men with BMI 32 to 39.99, 75% of subjects in this group were assumed to have positive OSA diagnosis by PSG; 4. If men with BMI more than or equal to 40, 100% of subjects in this group were assumed to have positive OSA diagnosis by PSG. For worst case scenario, we assumed all drivers that lost follow-up during the study period would have a negative OSA result by PSG.
Independent t tests were used for the comparison of continuous variables, and Chi-squared and Fisher exact tests were used for the comparison of categorical variables, as appropriate. All tests assumed unequal variances. All P values were two sided with a level of significance P < 0.05. Analyses were conducted using Stata 15.1 software (StataCorps LLC, College Station, TX).
RESULTS
General Characteristics of Study Population
A total of 706 eligible commercial drivers (242 were self-employed drivers, 137 drivers were referred through a third-party administrator providing occupational examination referrals, and the remainder came from 81 unique employers) presented to our clinic during the study period for FMCSA-mandated CDMEs and were included in this study (Table 1). The majority of drivers were men and age 42 and older. With an average BMI of 30.15, most of the drivers in our study were overweight, 42.9% were obese (BMI more than or equal to 30) and 6.1% were morbidly obese (BMI more than or equal to 40). Hypertension was present in 30.2% of the drivers, while 8.5% reported diabetes mellitus, and 6.9% of drivers checked “yes” to the sleep disorder question on the CDME form.
TABLE 1.
General Characteristics of Commercial Truck Drivers Presented for DOT Mandated CDME During Study Period in 2017
| Characteristics | All Drivers Examined n = 706 |
|---|---|
| Men, n (%) | 675 (95.6) |
| Age range, yr | 18–84 |
| Age 42 and above, n (%) | 456 (64.6) |
| Mean age, yr (±SD) | 46.66 (12.6) |
| Mean BMI, kg/m2 (±SD) | 30.15 (5.6) |
| BMI ≥40 mg/kg2, n (%) | 43 (6.1) |
| BMI ≥33 mg/kg2 and <40 mg/kg2, n (%) | 119 (16.9) |
| Mean NC, inches (±SD) | 15.73 (1.3) |
| NC >17 in. (male), 15.5 in. (female) | 87 (12.3) |
| Mean SBP, mmHg (±SD) | 121.39 (12.6) |
| Mean DBP, mmHg (±SD) | 75.55 (9.4) |
| Hypertension (treated or untreated), n (%) | 213 (30.2) |
| Mean ESS (±SD) | 1.90 (4.3) (n = 671) |
| ESS >10 | 5 (0.71%) (n = 671) |
| Answered “yes” to sleep-related question on the CDME form using JTF criteria*, n (%) | 49 (6.9) |
| Type 2 diabetes (treated or untreated), n (%) | 60 (8.5) |
| History of stroke, coronary artery disease, or arrhythmias, n (%) | 27 (3.8) |
Do you have “sleep disorders, pauses in breathing while asleep, daytime sleepiness, loud snoring?”
BMI, body mass index; CDME, Commercial Driver Medical Examination; DBP, diastolic blood pressure; ESS, Epworth sleepiness scale; mmHg, millimeters of mercury; NC, neck circumference; SBP, systolic blood pressure; SD, standard deviation.
Driver Characteristics Stratified by Screening Criteria
By using the JTF criteria or the FMCSA criteria alone, 119 drivers and 111 drivers screened positive for OSA, which translates to yields of 16.9% and 15.7%, respectively. A total of 142 (20.1%) drivers screened OSA positive by either the JTF or the FMCSA criteria (Fig. 1). The combined yield 1.19 times higher (1.11 to 1.28 95% CI); 1.28 times higher (1.17 to 1.39 95% CI), higher than screening by JTF or FMCSA criteria in isolation respectively. Of the total 142 OSA positive screens, 88 (62.0%) were positive on both the JTF and the FMCSA criteria. Of the 142 drivers identified as OSA screen positive, 74 (52%) were drivers with a pre-existing diagnosis of OSA (see results, next section below).
FIGURE 1.
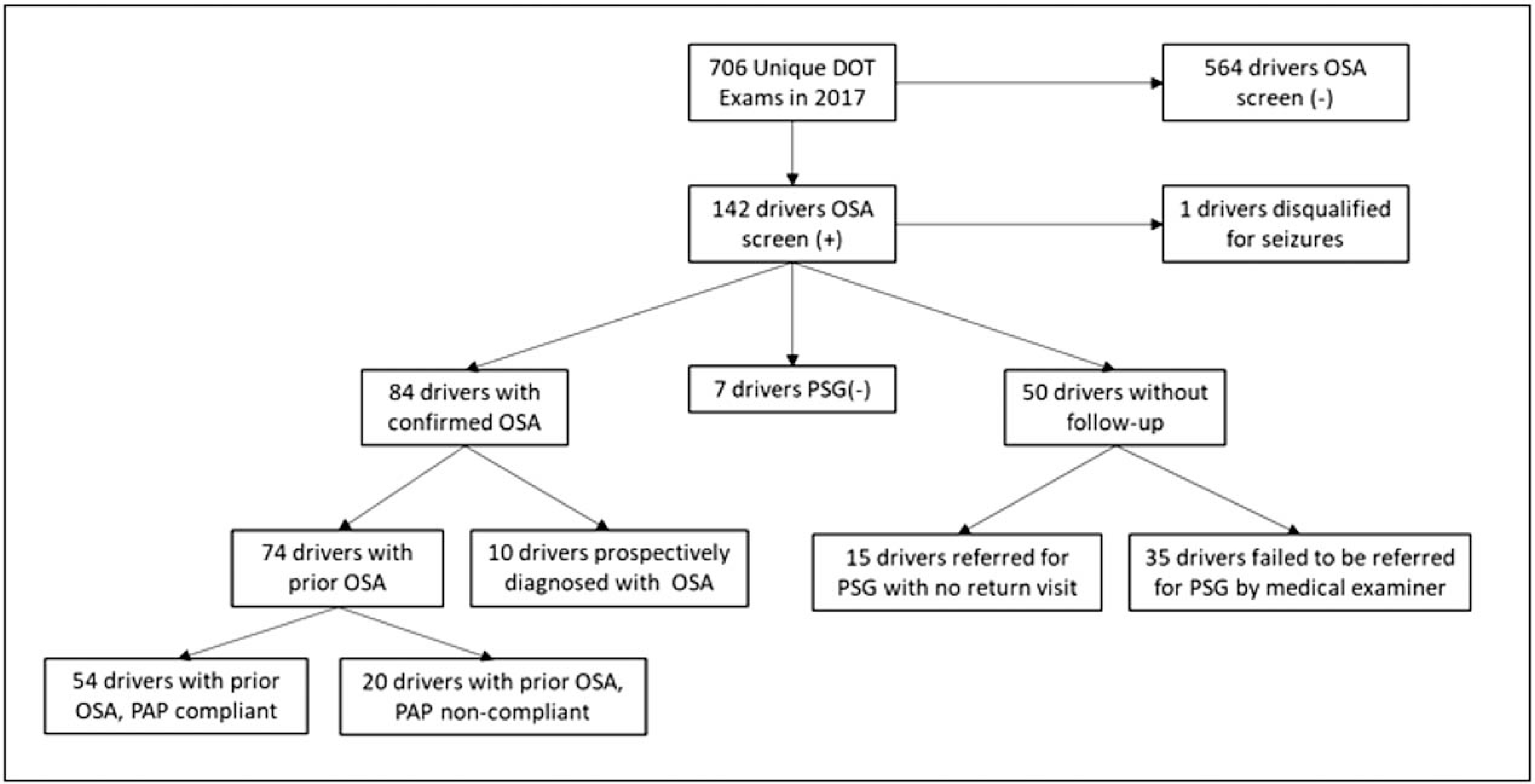
Flowchart of OSA screening during commercial drivers' medical examination of those screened positive with either the JTF criteria or the FMCSA criteria. FMCSA, Federal Motor Carrier Safety Administration; JTF, Joint Task Force; OSA, obstructive sleep apnea; PAP, positive airway pressure, PSG, polysomnography.
The drivers’ characteristics as stratified according to their screening results for the two OSA screening criteria are presented in Table 2. Comparing the values of population characteristics of the positive screening groups to the remainder of the population resulted in statistically significant differences in all of the tabulated measures except for driver sex and ESS score.
TABLE 2.
Study Population Characteristics Stratified by Screening Results of the Two OSA Screening Criteria
| Characteristics | Screened (−) for OSA JTF Criteria* n = 587 (83.1%) | Screened (+) for OSA JTF Criteria* n = 119 (16.9%) | P | Screened (−) for OSA FMCSA MRB Criteria† n = 595 (84.3%) | Screened (+) for OSA FMCSA MRB Criteria† n = 111 (15.7%) | P | Screened (−) for Either Criteria n = 564 | Screened (+) for Both Criteria n = 88 | P |
|---|---|---|---|---|---|---|---|---|---|
| Men, n (%) | 559 (95.2) | 116 (97.5) | 0.336 | 568 (95.5) | 107 (96.4) | 0.659 | 538 (95.4) | 86 (97.7) | 0.409 |
| Age range, yr | 18–84 | 19–68 | 18–84 | 25–67 | 18–84 | 25–67 | |||
| Age 42 and above, n (%) | 356 (60.7) | 100 (84.0) | <0.001 | 362 (60.8) | 94 (84.7) | <0.001 | 341 (60.5) | 79 (89.8) | <0.001 |
| Mean age, yr (± SD) | 45.57 (12.8) | 52.03 (10.0) | <0.0001 | 45.72 (12.9) | 51.70 (9.5) | <0.0001 | 45.50 (12.9) | 52.84 (8.7) | <0.0001 |
| Mean BMI, kg/m2 (±SD) | 28.57 (3.9) | 37.96 (6.2) | <0.0001 | 28.40 (3.6) | 39.51 (5.1) | <0.0001 | 28.25 (3.5) | 40.33 (5.0) | <0.0001 |
| BMI ≥40 mg/kg2, n (%) | 4 (0.7) | 39 (32.8) | <0.001 | 0 (0) | 43 (38.7) | <0.001 | 0 (0.00) | 39 (44.3) | <0.001 |
| BMI ≥33 mg/kg2 and <40 mg/kg2, n (%) | 62 (10.6) | 57 (47.9) | <0.001 | 51 (8.6) | 68 (61.3) | <0.001 | 43 (7.6) | 49 (55.7) | <0.001 |
| Mean NC, inches (±SD) | 15.41 (1.0) | 17.34 (1.4) | <0.0001 | 15.42 (1.0) | 17.44 (1.3) | <0.0001 | 15.37 (1.0) | 17.74 (1.2) | <0.0001 |
| NC >17 in. (male), 15.5 in. (female) | 20 (3.4) | 67 (57.3) | <0.001 | 23 (3.7) | 64 (57.7) | <0.001 | 17 (3.0) | 61 (69.3) | <0.001 |
| Mean SBP, mmHg (±SD) | 120.40 (12.5) | 126.27 (11.9) | <0.0001 | 120.41 (12.6) | 126.63 (11.2) | <0.0001 | 120.36 (12.7) | 128.02 (11.5) | <0.0001 |
| Mean DBP, mmHg (±SD) | 75.12 (9.5) | 77.68 (8.2) | 0.0065 | 75.14 (9.5) | 77.78 (8.1) | 0.0026 | 75.12 (9.7) | 78.50 (8.4) | 0.0020 |
| Hypertension (treated or untreated), n (%) | 146 (24.9) | 67 (56.3) | <0.001 | 144 (24.2) | 69 (62.2) | <0.001 | 131 (23.2) | 54 (61.4) | <0.001 |
| Mean ESS (±SD) | 1.88 (4.6) (n = 561) | 2.05 (2.7) (n = 110) | 0.7058 | 1.97 (4.6) (n = 568) | 1.52 (1.8) (n = 103) | 0.0843 | 1.90 (4.7) (n = 539) | 1.57 (1.8) (n = 81) | 0.5279 |
| Answered “yes” to sleep-related question on the CDME form using JTF criteria,‡ n (%) | 0 (0) | 49 (41.2) | <0.001 | 13 (2.2) | 36 (32.4) | <0.001 | 15 (2.7) | 36 (40.9) | <0.001 |
| Type 2 diabetes (treated or untreated), n (%) | 39 (6.6) | 21 (17.7) | <0.001 | 40 (6.7) | 20 (18.0) | <0.001 | 34 (6.0) | 15 (17.1) | <0.001 |
| History of stroke, coronary artery disease, or arrhythmias, n (%) | 16 (2.7) | 11 (9.2) | 0.001 | 17 (2.8) | 10 (9.0) | 0.002 | 15 (2.7) | 9 (10.2) | 0.001 |
According to JTF Guidelines and clinical judgement.
According to FMCSA MRB Guidelines and clinical judgement.
Do you have “sleep disorders, pauses in breathing while asleep, daytime sleepiness, loud snoring?”
BMI, body mass index; CDME, Commercial Driver Medical Examination; DBP, diastolic blood pressure; ESS, Epworth sleepiness scale; mmHg, millimeters of mercury; NC, neck circumference; SBP, systolic blood pressure; SD, standard deviation.
We further compared the characteristics of drivers who screened positive for only one OSA screening criteria but screened negative for the other OSA screening criteria (Supplemental Digital Content 3, http://links.lww.com/JOM/A777). There were 31 drivers who screened positive by JTF criteria only and 23 drivers who screened positive by FMCSA criteria only. The two groups were similar comparing mean age, mean neck circumference, blood pressure and past medical history such as hypertension, diabetes, or stroke. However, drivers that were only positive by FMCSA criteria had a statistically higher average BMI compared with drivers that were only positive by the JTF criteria (36.39 vs 31.22, P < 0.01). Additionally, among the drivers that only screened positive by JTF criteria, eight (25.81%) drivers had a BMI more than or equal to 33 kg/m2 and less than 40 kg/m2, compared with 19 (82.61%) drivers that only screened positive by FMCSA criteria (P < 0.001). The lower BMI in the JTF screen positive only group was due primarily to the presence of less obese drivers who had a prior history of OSA or an abnormal ESS.
Epworth Sleepiness Scale and FMCSA Sleep Self-Report Question
We evaluated ESS and sleep disorder self-assessment question on the CDME form to the driver’s history of OSA and adherence with PAP (Table 3). Only about 58% of drivers with a prior OSA diagnosis provided accurate self-reports of a sleep disorder based on their answers to the CDME form sleep question, the remainder were identified by the clinic’s screening protocol. PAP-adherent drivers were more likely to self-report their OSA diagnosis (65.5%) as compared with non-PAP-adherent drivers (35.0%) (P = 0.017). ESS scores were all low (means less than 2), and there were no statistically significant differences in ESS among the different groups.
TABLE 3.
Comparison of Mean Epworth Sleepiness Scale and Self-Assessed Sleep Disorder Question on CDME Form Between PAP-Compliant Versus Non-Compliant Drivers Previously Diagnosed with OSA
| All Drivers n = 706 | Drivers With Past Diagnosis of OSA n = 78 | Drivers With OSA Who Were Non-compliant With PAP Use n = 20 (25.6%) | Drivers with OSA Who Were Compliant With PAP Use n = 58 (74.4%) | P | |
|---|---|---|---|---|---|
| Mean ESS (±SD) | 1.90 (4.32) (n = 671) | 1.72 (1.92) (n = 71) | 1.88 (1.58) (n = 17) | 1.70 (2.07) (n = 54) | 0.724 |
| Answered “yes” to sleep-related question on the CDME form using JTF criteria*, n (%) | 49 (6.9) | 45 (57.7) | 7 (35.0) | 38 (65.5) | 0.017 |
Do you have “sleep disorders, pauses in breathing while asleep, daytime sleepiness, loud snoring?”
ESS, Epworth sleepiness scale; SD, standard deviation; PAP, positive airway pressure.
Driver Characteristics Stratified by Confirmed OSA, Lost Follow-Up, or not Referred for a Sleep Study
In Table 4, we compared drivers that were screened positive for OSA by either the JTF or the FMCSA criteria and were subsequently confirmed with OSA by a sleep study versus those drivers that were referred for a sleep study but lost follow-up with our clinic or drivers that were not referred due to provider’s clinical judgment. Drivers that were not referred for a sleep study by the clinician had lower BMI (P = 0.0029) and drivers that were referred for a sleep study but lost follow-up were younger (P = 0.0001). There was no significant difference between other risk factor characteristics, such as office blood pressure, neck circumference, diabetes, or hypertension status.
TABLE 4.
Comparison of Confirmed OSA Drivers and Those Who Failed to Follow-up or Were Not Referred for OSA After Screening (+)
| Screened (+) for OSA but Diagnosis Unconfirmed* |
||||
|---|---|---|---|---|
| Characteristics | Screened (+) for OSA and Diagnosis Confirmed* (n = 84) | Referred for PSG but Lost to Follow-Up† (n = 15) | Not referred for PSG† (n = 35) | P |
| Men, n (%) | 83 (98.8) | 15 (100.0) | 32 (91.4) | 0.075 |
| Age range, yr | 31–68 | 25–63 | 19–66 | |
| Age ≥42, n (%) | 77 (91.7) | 9 (60.0) | 25 (71.4) | 0.001 |
| Mean age, yr (±SD) | 54.37 (8.2) | 43.46 (11.7) | 47.63 (11.5) | 0.0001 |
| Mean BMI, kg/m2 (±SD) | 38.57 (6.5) | 40.01 (4.4) | 34.63 (4.1) | 0.0029 |
| BMI ≥40 mg/kg2, n (%) | 32 (38.1) | 7 (46.7) | 3 (8.6) | 0.003 |
| BMI ≥33 mg/kg2 and <40 mg/kg2, n (%) | 36 (42.7) | 9 (60.0) | 26 (74.3) | 0.006 |
| Mean NC, in. (±SD) | 17.44 (1.4) | 17.07 (0.8) | 16.69 (1.6) | 0.0466 |
| NC >17 in. (male), 15.5 in. (female), n (%) | 45 (53.6) | 8 (53.3) | 16 (45.7) | 0.728 |
| Mean SBP, mmHg (±SD) | 126.12 (10.2) | 129.2 (13.0) | 122.11 (13.4) | 0.1867 |
| Mean DBP, mmHg (± SD) | 77.00 (7.9) | 78.93 (6.9) | 76.80 (9.2) | 0.7681 |
| Hypertension (treated or untreated), n (%) | 50 (59.5) | 9 (60.0) | 19 (54.3) | 0.860 |
| Type 2 diabetes (treated or untreated), n (%) | 15 (17.9) | 4 (26.7) | 4 (11.4) | 0.408 |
| History of stroke, coronary artery disease, or arrhythmias, n (%) | 11 (13.1) | 0 (0.0) | 1 (2.9) | 0.089 |
BMI, body mass index; DBP, diastolic blood pressure; mmHg, millimeters of mercury; NC, neck circumference; PSG polysomnography or other sleep study; SBP, systolic blood pressure; SD, standard deviation.
According to JTF Guidelines and clinical judgement.
According to FMCSA MRB Guidelines and clinical judgement.
There were some differences in referrals associated with nonmedical factors. Of the four examiners in our clinic during the study period, one failed to refer drivers for a sleep study on 23 occasions during 349 examinations, while the other three combined failed to refer only 12 times in 357 examinations (P = 0.048). Among the 67 drivers who should have been referred for a sleep study, 25/39 (64%) of company/government-employed received physician referrals, compared with 7/25 (28%) of self-employed drivers who were referred (P = 0.012).
Positive Predictive Values of the Two Screening Criteria
In Table 5, we compared the positive predictive values (PPV) of using one of the two screening guidelines versus using both guidelines in series. The PPV of the JTF tended to be higher than that of the FMCSA, while all PPV in the intermediate and best-case scenarios were 84% or greater.
TABLE 5.
Estimation of Positive Predictive Value (PPV) of OSA Screening Criteria
| Criteria Used | Positive Diagnosis for OSA | Positive Screening for OSA | PPV |
|---|---|---|---|
| Either JTF or FMCSA | |||
| Best case scenario | 84 | 91 | 92% |
| Intermediate case scenario | 118 | 141 | 84% |
| Worst case scenario | 84 | 141 | 60% |
| JTF | |||
| Best case scenario | 83 | 86 | 97% |
| Intermediate case scenario | 105 | 118 | 89% |
| Worst case scenario | 83 | 118 | 70% |
| FMCSA | |||
| Best case scenario | 65 | 72 | 90% |
| Intermediate case scenario | 94 | 111 | 85% |
| Worst case scenario | 65 | 111 | 59% |
| Both JTF/FMCSA | |||
| Best case scenario | 64 | 67 | 96% |
| Intermediate case scenario | 81 | 88 | 92% |
| Worst case scenario | 64 | 88 | 73% |
F/U, follow-up; PPV, positive predictive value.
DISCUSSION
This retrospective study reviewed the medical records of 706 consecutive commercial truck drivers who presented to an academic occupational medicine clinic in Boston during 2017 for the DOTmandated medical examinations and compared two currently recommended OSA screening criteria. To the best of our knowledge, our study is the first to compare the screening yield rates and positive predictive values of the 2006 JTF Consensus Guidelines and the 2016 FMCSA MRB Recommendations. The results of this study not only reinforce the value of using evidence-based and primarily objective OSA screening criteria during commercial driver medical exams, but further demonstrate the significantly higher yield of utilizing both screening criteria in series.
Currently there is no FMCSA regulation requiring medical examiners to use OSA screening guidelines during CDMEs beyond the examination form, and the choice of which guideline or any to use for screening commercial drivers is based on medical examiner’s clinical judgement.31 The current research, consistent with previous studies, demonstrates that additional screening beyond the FMCSA-examination form is necessary to identify the majority of drivers who already have an OSA diagnosis or who will go on to have one confirmed. Furthermore, the benefits of such screening outweigh the risks for two reasons. First, research has already demonstrated the increased rates of preventable accidents among drivers with OSA who are not adequately treated, as well as the reduction of accident risk with proper treatment adherence.9,10,12,13 Second, the estimated PPV of utilizing the recommended criteria in realistic scenarios are 84% or greater. False-positives were only 5% of those screening positive and most were ruled out based on an existing prior sleep study so that the inconvenience was minimal. In fact, loss to follow-up, likely due to doctor-shopping by OSA screen positive drivers for more lenient examiners is a greater issue.
The PPVs estimated in this study are very consistent with the best case scenarios in previous studies of the JTF of 95% to 100%.1,23 In our current study, the worst-case scenario PPV under the JTF criteria was 70.3%, in which we assumed all drivers lost to follow-up were OSA negative. This worst-case scenario PPV is higher than the worst case scenario PPV result (37.7%) reported by Parks et al1 because the proportion of drivers screening positive and then lost to follow-up was lower in this study. The main reason for this is that so many drivers in the current study had already been diagnosed with OSA, suggesting that greater awareness of OSA screening during CDME by medical examiners over the past decade has resulted in more drivers being diagnosed and treated.
This secular change over time is supported by the following comparison of the previous study1 and the current study done in the same clinic, which both yielded OSA screen positive rates of 17% for the JTF. In the prior study,1 only 9% of drivers screening OSA positive were subsequently found to have a past diagnosis of OSA, whereas 55% of those screening positive in the present study were confirmed to have a past OSA diagnosis. Additionally, in the original study, only a single driver (5%) demonstrated adequate PAP adherence at follow-up, while in the present study, about 75% of those with pre-existing OSA were treatment adherent.
Our study underlines the import of continuing to use objective OSA screening criteria. Without our clinic’s screening protocols, only 58% of these drivers would have been self-identified by the questions mandated by FMCSA. This underlines the crucial point that without evidence-based protocols that rely objective measures beyond self-reports, many drivers will continue to under-report their medical conditions.32 Although few drivers endorse abnormal ESS scores, it is important to employ the ESS and sleepiness questions for medico-legal reasons to identify drivers that require out-of-service sleep studies. As expected, those compliant with PAP in our cohort were significantly more likely to answer yes on the self-assessed sleep disorder question (66% vs 35%). But again, even among those PAP-adherent drivers, roughly one-third of drivers did not initially report their sleep disorder to the examiner.
Our study does have several limitations. First, 47% (15/32) of drivers referred for sleep study did not return to our clinic for subsequent follow-up. This rate is consistent with observations from previous publications.1,23
Second, in our current study, 25% (35/142) of all drivers who screened positive for OSA were not referred for a sleep study by the medical examiner. We reviewed these drivers’ examinations and compared them to those with positive screening who were subsequently confirmed to have OSA. Drivers not referred for a sleep study were statistically younger in age with a lower average BMI (Table 4). However, there was no difference in other characteristics between the two groups, such as neck circumference, blood pressure, hypertension, or diabetes. This limitation is similar to prior studies.1,23 Given the resistance of drivers to OSA screening, some examiners will provide leeway to younger drivers and those who are seen as meeting the screening criteria in “borderline” fashion. This was also observed in the prior study at the same clinic.1
Another limitation of our study is some missing data. The current CDME form (FMCSA Form MCSA-5875) does not mandate the collection of several key items used in the two OSA screening guidelines, including history of motor vehicle accident; history of motor vehicle accident related to OSA; presence or absence of micrognathia or retrognathia; mallampati classification; or history of untreated hypothyroidism. The documentation of these conditions relied on medical examiners free-texting into the driver health history review section. However, except for micrognathia, retrognathia, and mallampati classification, the other items also rely on drivers’ self-reports and would be subject to under-reporting. It was also not possible for our study to directly determine the number of drivers with OSA who are missed by the screening criteria.
Our study also has several important strengths. We reviewed a large sample of consecutive CDME at a single clinic where standardized protocols were employed. Our thorough and multiple reviews of all driver CDME records ensured the accuracy of our findings. Even with the limitations as discussed, our study demonstrated high diagnostic yields and high PPV across varying sets of assumptions.
CONCLUSION
The combined use of the 2016 FMCSA OSA screening criteria with the 2006 JTF Consensus Guidelines has a higher screening yield compared with using either guideline individually. Although a greater proportion of drivers have been diagnosed with OSA and adequately treated with PAP over the last decade, many drivers continue to under-report OSA. The present study supports the use of OSA screening criteria beyond the FMCSA mandated form.
Supplementary Material
Acknowledgments
Source of funding: Harvard College Research Program to Ms Hyun.
Footnotes
The authors report no conflicts of interest.
Disclosure: Dr Kales has served as a medicolegal consultant and expert witness on cases involving commercial drivers. The views expressed in this article are those of the author(s) and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government. Dr. Wilcox’s disclaimer: Lt. Cmdr. Wilcox is a military service member. This work was prepared as part of my official duties. Title 17, USC, §105 provides that copyright protection under this title is not available for any work of the U.S. Government. Title 17, USC, §101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
Clinical Significance: The 2016 FMCSA and 2006 JTF OSA screening recommendations for commercial drivers have similar yields and predictive values. However, using the two screening criteria synergistically is superior to using either guideline alone. When the guidelines were used in combination, the overall screening yield increased from 16% OSA-positive screens to 20%.
Supplemental digital contents are available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.joem.org).
Contributor Information
Clifton Wilcox, Environmental & Occupational Medicine & Epidemiology Program, Department of Environmental Health Harvard T.H. Chan School of Public Health; Occupational Medicine, Cambridge Health Alliance/Harvard Medical School; Occupational Medicine, Naval Hospital Jacksonville, Jacksonville, Florida.
Justin Yang, Environmental & Occupational Medicine & Epidemiology Program, Department of Environmental Health Harvard T.H. Chan School of Public Health; Occupational Medicine, Cambridge Health Alliance/Harvard Medical School; Department of Medicine, Boston University School of Medicine, Boston; Manet Community Health Center, North Quincy.
Robert Filler, Environmental & Occupational Medicine & Epidemiology Program, Department of Environmental Health Harvard T.H. Chan School of Public Health; Occupational Medicine, Cambridge Health Alliance/Harvard Medical School.
Po-Hua Chen, Occupational Medicine, Cambridge Health Alliance/Harvard Medical School.
Yoo Jin Hyun, Environmental & Occupational Medicine & Epidemiology Program, Department of Environmental Health Harvard T.H. Chan School of Public Health; Harvard College, Cambridge, Massachusetts..
Albert Rielly, Environmental & Occupational Medicine & Epidemiology Program, Department of Environmental Health Harvard T.H. Chan School of Public Health; Occupational Medicine, Cambridge Health Alliance/Harvard Medical School.
Stefanos N. Kales, Environmental & Occupational Medicine & Epidemiology Program, Department of Environmental Health Harvard T.H. Chan School of Public Health; Occupational Medicine, Cambridge Health Alliance/Harvard Medical School.
REFERENCES
- 1.Parks P, Durand G, Tsismenakis AJ, Vela-Bueno A, Kales S. Screening for obstructive sleep apnea during commercial driver medical examinations. J Occup Environ Med. 2009;51:275–282. [DOI] [PubMed] [Google Scholar]
- 2.Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3:310–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307:2169–2176.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gami AS, Howard DE, Olson EJ, Somers VK. Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med. 2005;352:1206–1214. [DOI] [PubMed] [Google Scholar]
- 5.Romero-Corral A, Caples SM, Lopez-Jimenez F, Somers VK. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest. 2010;137:711–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tasali E, Ip MS. Obstructive sleep apnea and metabolic syndrome: alterations in glucose metabolism and inflammation. Proc Am Thorac Soc. 2008;5:207–217.. [DOI] [PubMed] [Google Scholar]
- 7.Bilyukov RG, Nikolov MS, Pencheva VP, et al. Cognitive impairment and affective disorders in patients with obstructive sleep apnea syndrome. Front Psychiatry. 2018;9:357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai C, Strange C, Bachman D. Neurocognitive impairment in obstructive sleep apnea. Chest. 2012;141:1601–1610. [DOI] [PubMed] [Google Scholar]
- 9.Burks SV, Anderson JE, Bombyk M, et al. Nonadherence with employermandated sleep apnea treatment and increased risk of serious truck crashes. Sleep. 2016;39:967–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. 2009;5:573–581. [PMC free article] [PubMed] [Google Scholar]
- 11.Ward KL, Hillman DR, James A, et al. Excessive daytime sleepiness increases the risk of motor vehicle crash in obstructive sleep apnea. J Clin Sleep Med. 2013;9:1013–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ellen RLB, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M. Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med. 2006;2:193–200. [PubMed] [Google Scholar]
- 13.Garbarino S, Guglielmi O, Sanna A, Mancardi GL, Magnavita N. Risk of occupational accidents in workers with obstructive sleep apnea: systematic review and meta-analysis. Sleep. 2016;39:1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akerstedt T. Consensus statement: fatigue and accidents in transport operations. J Sleep Res. 2000;9:395. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine Committee on Sleep M, Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006. [PubMed] [Google Scholar]
- 16.Kales SN, Straubel MG. Obstructive sleep apnea in North American commercial drivers. Ind Health. 2014;52:13–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karimi M, Hedner J, Habel H, Nerman O, Grote L. Sleep apnea-related risk of motor vehicle accidents is reduced by continuous positive airway pressure: Swedish Traffic Accident Registry data. Sleep. 2015;38:341–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kales SN, Czeisler CA. Obstructive sleep apnea and work accidents: time for action. Sleep. 2016;39:1171–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.FMCSA. Federal Motor Carrier Safety Administration (FMCSA) Medical Examiner Handbook. In: Transportation Do, ed. Washington DC. [Google Scholar]
- 20.Board MR. Final MRB Task 16–01 Letter Report from MCSAC. In: Transportation Do, ed. Washington DC: Federal Motor Carrier Safety Administration; 2016. [Google Scholar]
- 21.Hartenbaum N, Collop N, Rosen IM, et al. Sleep apnea and commercial motor vehicle operators: statement from the joint Task Force of the American College of Chest Physicians, American College of Occupational and Environmental Medicine, and the National Sleep Foundation. J Occup Environ Med. 2006;48:S4–S37. [DOI] [PubMed] [Google Scholar]
- 22.Gurubhagavatula I, Patil S, Meoli A, et al. Sleep apnea evaluation of commercial motor vehicle operators. J Clin Sleep Med. 2015;12:285–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Talmage JB, Hudson TB, Hegmann KT, Thiese MS. Consensus criteria for screening commercial drivers for obstructive sleep apnea: evidence of efficacy. J Occup Environ Med. 2008;50:324–329. [DOI] [PubMed] [Google Scholar]
- 24.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. [DOI] [PubMed] [Google Scholar]
- 25.Collop NA, Tracy SL, Kapur V, et al. Obstructive sleep apnea devices for out-of-center (OOC) testing: technology evaluation. J Clinical Sleep Med. 2011;7:531–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang C, Berger M, Rielly A, Malhotra A, Kales SN. Chapter 79 obstructive sleep apnea in the workplace In: Kryger M, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. Philadelphia, PA: Elsevier; 2017. [Google Scholar]
- 27.Armstrong C, Joint National C. JNC8 guidelines for the management of hypertension in adults. Am Fam Physician. 2014;90:503–504. [PubMed] [Google Scholar]
- 28.Dagan Y, Doljansky JT, Green A, Weiner A. Body Mass Index (BMI) as a first-line screening criterion for detection of excessive daytime sleepiness among professional drivers. Traffic Inj Prev. 2006;7:44–48. [DOI] [PubMed] [Google Scholar]
- 29.Gurubhagavatula I, Maislin G, Nkwuo JE, Pack AL Occupational screening for obstructive sleep apnea in commercial drivers. Am J Respir Crit Care Med. 2004;170:371–376. [DOI] [PubMed] [Google Scholar]
- 30.Berger M, Varvarigou V, Rielly A, Czeisler CA, Malhotra A, Kales SN. Employer-mandated sleep apnea screening and diagnosis in commercial drivers. J Occup Environ Med. 2012;54:1017–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hartenbaum NP. Withdrawal of advanced notice of proposed rulemaking (ANPRM) on obstructive sleep apnea (OSA) does not mean examiners and employers should ignore safety risks. J Occup Environ Med. 2017;59: e374–e376. [DOI] [PubMed] [Google Scholar]
- 32.Burks SV, Anderson JE, Panda B, et al. The Pre-Registry Commercial Driver’s Medical Exam: screening sensitivity and certification lengths for two safetyrelated medical conditions. J Occup Environ Med. 2020;62:237–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


