Abstract
Objective
To evaluate the impact of a care bundle (antenatal information to women, manual perineal protection and mediolateral episiotomy when indicated) on obstetric anal sphincter injury (OASI) rates.
Design
Multicentre stepped‐wedge cluster design.
Setting
Sixteen maternity units located in four regions across England, Scotland and Wales.
Population
Women with singleton live births between October 2016 and March 2018.
Methods
Stepwise region by region roll‐out every 3 months starting January 2017. The four maternity units in a region started at the same time. Multi‐level logistic regression was used to estimate the impact of the care bundle, adjusting for time trend and case‐mix factors (age, ethnicity, body mass index, parity, birthweight and mode of birth).
Main outcome measures
Obstetric anal sphincter injury in singleton live vaginal births.
Results
A total of 55 060 singleton live vaginal births were included (79% spontaneous and 21% operative). Median maternal age was 30 years (interquartile range 26–34 years) and 46% of women were primiparous. The OASI rate decreased from 3.3% before to 3.0% after care bundle implementation (adjusted odds ratio 0.80, 95% CI 0.65–0.98, P = 0.03). There was no evidence that the effect of the care bundle differed according to parity (P = 0.77) or mode of birth (P = 0.31). There were no significant changes in caesarean section (P = 0.19) or episiotomy rates (P = 0.16) during the study period.
Conclusions
The implementation of this care bundle reduced OASI rates without affecting caesarean section rates or episiotomy use. These findings demonstrate its potential for reducing perineal trauma during childbirth.
Tweetable abstract
OASI Care Bundle reduced severe perineal tear rates without affecting caesarean section rates or episiotomy use.
Keywords: Obstetric anal sphincter injury, perineal tear, quality improvement
Tweetable abstract
OASI Care Bundle reduced severe perineal tear rates without affecting caesarean section rates or episiotomy use.
Introduction
An obstetric anal sphincter injury (OASI), graded as a third‐ or fourth‐degree perineal tear, is a severe complication of vaginal childbirth. 1 Long‐term outcomes of OASI include chronic pain, sexual dysfunction and urinary or anal incontinence. 2 OASI rates are increasing in many countries. In the English National Health Service (NHS), reported OASI rates tripled among primiparous women over a decade, from 1.8% in 2000 to 5.9% in 2011, 3 with similar trends in many other countries. 4 , 5 , 6 , 7 The rise in OASI rates is likely to be linked to improved recognition of tears, changes in the characteristics of women giving birth as well as to changes in practice, such as an increased use of a ‘hands‐poised/hands‐off’ approach, opposed to a ‘hands‐on’ approach to protect the perineum, 8 , 9 , 10 a reluctance to perform an episiotomy 9 and gaps in the training of midwives and obstetricians. 11 , 12 , 13
Evidence from studies carried out in Scandinavian countries suggests that training to improve intrapartum techniques with focus on slowing down the birth of the head can significantly decrease OASI rates. 14 , 15 , 16 , 17 , 18 However, similar studies carried out elsewhere did not confirm these results. 19 , 20 A multidisciplinary team of national UK experts, supported by national professional organisations, developed a ‘care bundle’, which is a set of interventions likely to improve outcomes when implemented together. This OASI Care Bundle includes information provision to women during the antenatal period, manual perineal protection and use of mediolateral episiotomy when clinically indicated at 60‐degree angle. The care bundle also included the requirement that the perineum should be carefully checked following birth, including a per rectum examination, to improve detection of perineal injuries and instigate prompt repair.
A quality improvement project was initiated to implement the OASI Care Bundle following a stepped‐wedge design in 16 maternity units across the NHS in England, Scotland and Wales. The implementation strategy was informed by a detailed ‘theory of change’ that highlighted the need for ongoing project team support to participating units and local communications and awareness campaigns. 21 In this paper, we report the impact of the quality improvement project on OASI rates as well as on caesarean section rates and use of episiotomy.
Methods
Study design and participants
The OASI Care Bundle was evaluated in 16 maternity units between 1 October 2016 and 31 March 2018, using a multicentre study with a stepped‐wedge design. All women who had singleton live births were eligible for inclusion.
The participating units were located in four regions with four units in each region. A stepwise region‐by‐region roll‐out was instigated. At each step, the maternity units in a region started at the same time. The regional roll‐out minimised contamination across units and facilitated the delivery of the skills development module and site visits by the project team.
The eligibility and section criteria for the participating units have been previously reported. 21 Briefly, 91 units that had expressed an interest in participating in a pilot study in 2015 were eligible for inclusion. For each of the four regions, units were purposively selected from different areas in the region, aiming to include units of various sizes and types (obstetric‐led, alongside midwifery unit and freestanding midwifery unit) in each region.
Women who expected to give birth after the introduction of the care bundle were given a sheet that explained that the care bundle did not affect their choice about how or in what position they would like to give birth. As a consequence, manual perineal protection was not used when a woman had different preferences and the per rectum check following birth was only performed with consent.
Sequential roll‐out
The order of the four regions in the stepwise region‐by‐region roll‐out was determined by a member of the project team (IGU) using computer‐generated random numbers before the start of the roll‐out. The maternity units and their local clinical champions were informed of their allocation 2 months before the start of the roll‐out period in their region to allow for preparation time.
The roll‐out took place in three phases. For each region, a ‘baseline phase’ was used to determine the OASI rates before implementation of the care bundle. The care bundle was implemented in the maternity units during a 3‐month ‘transition phase’. An ‘evaluation phase’ was used to determine the OASI rates after implementation. The duration of the baseline and evaluation phases depended on the place in the order of the sequential roll‐out (see Supplementary material, Figure S1). Births that took place during the transition phase were excluded from the analysis.
The roll‐out of the OASI Care Bundle started in the first region in January 2017. It has to be noted that the OASI Project was retrospectively registered on the ISCTRN database in September 2017. However, the project team engaged in an extensive publicity campaign throughout 2016 and the study protocol, describing the project in detail, was available on the Royal College of Obstetricians and Gynaecologists website from January 2017.
Intervention
The OASI Care Bundle was developed following recommendations from existing UK guidelines 22 by a multidisciplinary team of national experts. The three components of the care bundle are listed in Figure 1 and a full description can be found on the project website. 23
Figure 1.
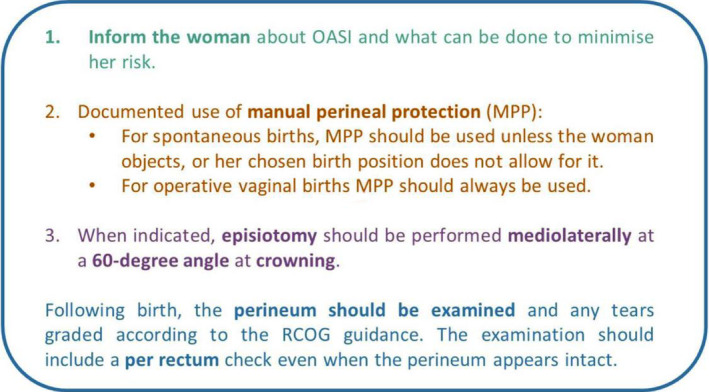
OASI Care Bundle components.
The first component of the care bundle is a leaflet providing information about perineal trauma during childbirth, its risk factors and the OASI Care Bundle. This was given to women in the antenatal period between 32 and 36 weeks of gestation.
The second component is the use of manual perineal protection for all singleton vaginal births, unless a woman objects or if her chosen birth position does not allow it (e.g. water birth or use of birthing stool). This component of the care bundle advises manual perineal protection using a specific technique (‘Finnish grip’). 16
The third component is the use of episiotomy when clinically indicated, performed at a 60‐degree angle at crowning. The recognised indications for episiotomy in this context are fetal distress, delayed second stage of labour, operative vaginal birth and cases when a severe perineal tear is judged to be imminent (e.g. thick inelastic perineum). For operative vaginal birth, episiotomy should be used for all forceps births, regardless of parity, and for all vacuum‐assisted births in primiparous women. In multiparous women, episiotomy could be omitted for vacuum‐assisted births after considering the woman’s OASI risk.
The care bundle also includes the requirement to carry out a thorough perineal examination following all vaginal births, including a per rectum examination. 24 Whereas the first three components of the care bundle contribute to the primary prevention of OASI, the per rectum examination is a secondary prevention measure, which may have improved detection rates after the implementation of the care bundle.
The implementation of the OASI Care Bundle in each unit was led by local midwives and obstetricians. These clinical champions received central multidisciplinary training on key elements of the care bundle at designated ‘skills development days’ at the start of the transition period. Project clinical leads visited all units during the study period to provide further training, support and advice.
Clinical data
Patient‐level data were extracted from local electronic maternity information systems for 15 units in England, Scotland and Wales, and from the Scottish Morbidity Record 02 and Scottish Birth Record for one unit in Scotland. The maternity information systems, available in almost all English units, captured detailed demographic and clinical information related to maternity care and outcomes with the data entered by midwives and support staff. Scottish Morbidity Record 02 collects data submitted by maternity units to the Information Services Division Scotland since 1975 for all women admitted to Scottish maternity units. 25
Outcomes
The primary outcome was OASI in women who had singleton live vaginal births with episiotomy as a secondary outcome. Another secondary outcome was caesarean section in all women who had a singleton live birth.
Statistical analysis
The study’s sample size was calculated based on the approach proposed by Hussey and Hughes. 26 There were on average 912 vaginal births in a 3‐monthly period (‘step’) for the participating units (with a range of 339–1617) between 1 April 2014 and 31 March 2015. The baseline OASI rate (3.2%) and the intra‐cluster correlation (ρ 0.006) were calculated from English data for births that took place between 1 April 2013 and 31 March 2014. 27 Based on these numbers, and a 5% significance level, the statistical power of the study to detect a 25% reduction in OASI rate (from 3.2 to 2.4%) was estimated to be 0.92.
We used multi‐level logistic regression to estimate adjusted odds ratios (aOR) that represent relative differences in the odds of OASI before and after implementation of the care bundle. To adjust for the small number of clusters, we estimated the model using adaptive Gaussian–Hermite approximation to the likelihood. 28 The regression model included a linear term for calendar time in 3‐monthly intervals to account for temporal confounding, a random effect to account for clustering at both region and unit levels 26 and individual case‐mix factors (maternal age, ethnicity, body mass index, parity, mode of birth and birthweight). 3 The case‐mix factors were categorised as listed in Table 2. Multiple imputation was used to deal with missing values for age (missing for 3.0% of women), ethnicity (12.8%), body mass index (9.7%), parity (1.2%), birthweight (0.6%) with statistical coefficients obtained from ten imputed data sets, pooled using Rubin’s rules.
Table 2.
Characteristics of the included 55 060 vaginal births
| Baseline phase without OASI Care Bundle | Evaluation phase with OASI Care Bundle | All | |
|---|---|---|---|
| Number of births | 27 668 | 27 392 | 55 060 |
| Age (years), median (interquartile range) | 30 (26–34) | 30 (26–34) | 30 (26–34) |
| Age categories (years) | |||
| <25 | 5191 (19.0) | 5177 (19.9) | 10 368 (19.4) |
| 25–29 | 7752 (28.3) | 7597 (29.2) | 15 349 (28.7) |
| 30–34 | 8651 (31.6) | 7998 (30.7) | 16 649 (31.2) |
| >35 | 5771 (21.1) | 5269 (20.2) | 11 040 (20.7) |
| Missing (n = 1654, 3.0%) | |||
| Ethnicity | |||
| White | 18 100 (75.0) | 18 100 (75.9) | 36 200 (75.4) |
| Asian | 2918 (12.1) | 3038 (12.7) | 5956 (12.4) |
| Black | 1271 (5.3) | 1075 (4.5) | 2346 (4.9) |
| Other | 1860 (7.7) | 1640 (6.9) | 3500 (7.3) |
| Missing (n = 7058, 12.8%) | |||
| Body mass index (kg/m2) | |||
| <18 | 945 (3.6) | 728 (3.1) | 1673 (3.4) |
| 18–25 | 13 771 (52.9) | 12 009 (50.7) | 25 780 (51.9) |
| 25–30 | 6700 (25.7) | 6307 (26.7) | 13 007 (26.2) |
| >30 | 4633 (17.8) | 4620 (19.5) | 9253 (18.6) |
| Missing (n = 5347, 9.7%) | |||
| Parity | |||
| Primiparous | 12 662 (46.0) | 12 153 (45.2) | 24 815 (46.5) |
| Multiparous | 14 853 (54.0) | 14 759 (54.8) | 29 612 (55.4) |
| Missing (n = 633, 1.2%) | |||
| Birthweight (g) | |||
| <3500 | 6162 (22.4) | 6243 (23.0) | 12 405 (22.7) |
| 3500–3999 | 10 542 (38.3) | 10 434 (38.4) | 20 976 (38.3) |
| ≥4000 | 10 818 (39.3) | 10 510 (38.7) | 21 328 (39) |
| Missing (n = 351, 0.6%) | |||
| Mode of birth | |||
| Spontaneous | 22 006 (79.5) | 21 651 (79.0) | 43 657 (79.3) |
| Forceps | 3660 (13.2) | 3644 (13.3) | 7304 (13.3) |
| Vacuum‐assisted | 2002 (7.3) | 2097 (7.7) | 4099 (7.4) |
| Episiotomy | 6934 (25.1) | 6719 (24.5) | 13 653 (24.8) |
Data are number or number (%), unless otherwise indicated.
The analysis was carried out following the intention‐to‐treat principle, with births analysed according to whether they took place during the baseline or evaluation periods, irrespective of whether or not all aspects of the care bundle could be implemented. Differences with a P value <0.05 were considered to be statistically significant.
Although not defined in the published protocol, subgroup analyses of the care bundle effect were carried out according to parity and mode of birth (spontaneous, forceps or vacuum‐assisted). 21 The Wald test was used to test for significance of interactions.
A first sensitivity analysis was performed to examine whether or not results were affected if time was included as a categorical variable (in 3‐monthly period). A second sensitivity analysis estimated the impact of the care bundle using a model that included a random interaction between phase (baseline versus evaluation) and maternity unit with an unstructured covariance matrix that allowed the impact of the care bundle to vary between maternity units. 29
Patient and public involvement
The OASI Project had patient and public involvement throughout inception, implementation and evaluation stages to ensure that care bundle development and implementation were informed by the perspective of women. The project was supported by an Independent Advisory Group, including lay representatives. The antenatal information sheet (first component of the OASI Care Bundle) was developed together with patient and public involvement groups in order to ensure that the material was appropriate. Patient and public involvement representatives were present at all skills development days.
Results
The characteristics of the 16 participating units are described in Table 1. In total, 80 339 singleton live vaginal births were included, 40 475 in the baseline phase (before the implementation of the care bundle) and 39 864 in the evaluation phase (after the implementation of the care bundle).
Table 1.
Characteristics of the 16 participating maternity units during the baseline phase before the implementation of the OASI Care Bundle by region
| Number and characteristics of participating units | Unit size* | All singleton live births, n | Vaginal births | Caesarean sections | |||
|---|---|---|---|---|---|---|---|
| All vaginal births, n (% all births) | Forceps and vacuum births, n (% all vaginal) | Episiotomy, n (% all vaginal) | OASI, n (% all vaginal) | n (% all birth) | |||
| Region 1 | |||||||
| 2 OU + AMU | 1 small | 4494 | 3101 (69.0) | 657 (21.2) | 675 (21.8) | 96 (3.1) | 1393 (31.0) |
| 1 OU + FMU | 2 medium | ||||||
| 1 OU + AMU+FMU | 1 large | ||||||
| Region 2 | |||||||
| 1 OU | 2 medium | 7638 | 5401 (70.7) | 1106 (20.5) | 1402 (26.0) | 187 (3.5) | 2237 (29.3) |
| 2 OU + AMU | 2 large | ||||||
| 1 OU + AMU+FMU | |||||||
| Region 3 | |||||||
| 4 OU + AMU | 2 small | 9612 | 6093 (63.4) | 1385 (22.7) | 1288 (21.1) | 201 (3.3) | 3519 (36.6) |
| 1 medium | |||||||
| 1 large | |||||||
| Region 4 | |||||||
| 2 OU | 1 small | 18 731 | 13 073 (69.8) | 2514 (19.2) | 3569 (27.3) | 427 (3.3) | 5658 (30.2) |
| 2 OU + AMU | 1 medium | ||||||
| 2 large | |||||||
| All | 40 475 | 27 668 (68.4) | 5662 (20.5) | 6934 (25.1) | 911 (3.3) | 12 807 (31.6) | |
AMU, alongside midwifery unit; FMU, freestanding midwifery unit; OU, obstetric unit.
Small unit: <3500 vaginal births per year; Medium size unit: between 3500 and 5000 vaginal births; Large unit: >5000 vaginal births.
Of the 40 475 singleton live births during the baseline phase, 27 668 (68.4%) were vaginal births and 12 807 (31.6%) were caesarean sections with some variation between the four regions (Table 1).
Of the 39 864 singleton live births that took place during the evaluation phase, 27 932 (68.7%) were vaginal births and 12 472 (31.3%) were caesarean sections. There was no evidence of differences in the caesarean section rate in the baseline and the evaluation phase (aOR 0.96, 95% CI 0.89–1.02, P = 0.19).
A total of 55 060 vaginal births were included in the analysis: 27 668 births (50.3%) in the baseline phase and 27 392 births (49.7%) in the evaluation phase (Table 2). The median maternal age was 30 years (interquartile range 26–34 years) and 46% of the women were primiparous. Of the vaginal births, 79.3% were spontaneous and 20.7% were operative. The characteristics of the women included in the baseline and evaluation phases were similar.
Table 3 shows that the OASI rate decreased significantly from 3.3% in the baseline phase to 3.0% in the evaluation phase (aOR 0.80, 95% CI 0.65–0.98). There was no statistically significant evidence for a time trend in OASI rates (linear trend, aOR 1.04 per 3‐monthly interval, 95% CI 0.99–1.09, P = 0.16).
Table 3.
Effect of implementation of care bundle on OASI rates
| Baseline OASI rate number (%) | Evaluation OASI rate | Adjusted* OR (95% CI) | P‐value | |
|---|---|---|---|---|
| Number of births | 27 668 | 27 392 | ||
| OASI | 911 (3.3) | 817 (3.0) | 0.80 (0.65–0.98) | 0.03 |
| Subgroup analysis according to parity | ||||
| Primiparous | ||||
| Number of births | 12 662 | 12 153 | ||
| OASI | 663 (5.2) | 597 (4.9) | 0.81 (0.65–1.00) | 0.05 |
| Multiparous | ||||
| Number of births | 14 853 | 14 759 | ||
| OASI | 248 (1.7) | 220 (1.5) | 0.78 (0.61–1.01) | 0.06 |
| Interaction care bundle and parity | 0.77 | |||
| Subgroup analysis according to mode of birth | ||||
| Spontaneous | ||||
| Number of births | 22 006 | 21 651 | ||
| OASI | 579 (2.6) | 484 (2.2) | 0.75 (0.60–0.93) | 0.01 |
| Forceps | ||||
| Number of birth | 3660 | 3644 | ||
| OASI | 278 (7.6) | 278 (7.6) | 0.88 (0.69–1.14) | 0.34 |
| Vacuum‐assisted | ||||
| Number of births | 2002 | 2097 | ||
| OASI | 540 (2.7) | 550 (2.6) | 0.82 (0.54–1.25) | 0.36 |
| Interaction care bundle and mode of birth | 0.31 | |||
Adjusted for time trend and case‐mix factors (age, ethnicity, body mass index, parity, mode of birth and birthweight).
Subgroup analyses showed that there was no evidence that the effect of the care bundle was different for primiparous women (decrease of OASI from 5.2 to 4.9%; aOR 0.81, 95% CI 0.65–1.00) and multiparous women (decrease from 1.7 to 1.5%; aOR 0.78, 95% CI 0.78–1.01; P for interaction 0.77).
Neither was there evidence that the effect of the care bundle differed between women who had a spontaneous vaginal birth (OASI rate 2.6% before and 2.2% after implementation; aOR 0.75, 95%CI 0.60–0.93), those who had a forceps (OASI rate of 7.6% in both periods; aOR 0.88, 95%CI 0.69–1.14) and those who had a vacuum‐assisted birth (OASI rate 2.7% before and 2.6% after implementation; aOR 0.82, 95%CI 0.54–1.25; P for interaction 0.31).
The episiotomy rate decreased slightly from 25.1% in the baseline phase to 24.5% in evaluation phase, but this decrease was not statistically significant (aOR 0.99, 95% CI 0.88–1.12, P = 0.90).
A sensitivity analysis with calendar time included as a categorical variable did not alter the estimated decrease in the OASI rate results following care bundle implementation (aOR 0.81, 95% CI 0.65–0.996, P = 0.046). Neither did we find a substantial change in the estimated decrease in the OASI rates in another sensitivity analysis including a random interaction between phase and maternity unit in the model (aOR 0.79, 95% CI 0.63–0.996, P = 0.047).
Discussion
Main findings
This study including 55 060 singleton live vaginal births found a reduction of 20% in the case‐mix‐adjusted risk of severe perineal injury after the introduction of the OASI Care Bundle. Subgroup analyses did not provide evidence that the care bundle had different effects according to parity or mode of birth. The implementation of the care bundle did not affect caesarean section or episiotomy rates.
Strengths and limitations
We used a stepped‐wedge design to evaluate the effects of the care bundle. Stepped‐wedge designs are pragmatic and often used when logistical constraints require a sequential roll‐out. However, they are susceptible to selection bias and temporal confounding. 30 , 31 We aimed to mitigate these biases by including all eligible births and by controlling for a time trend in the analysis using both a linear term in the main analysis as well as a categorical variable in the sensitivity analysis to represent calendar time.
In our study, we randomised the order of the roll out of the OASI Care Bundle in four regions. This implies that there were only four randomisation units. As a consequence, it cannot be simply assumed that the characteristics of the women who gave birth before the implementation of the care bundle were similar to those of women who gave birth after the implementation. However, the characteristics of the women included in the baseline and evaluation phases were similar as well as the mode of birth and the babies’ birthweight, which provides support for the validity of the comparison. In addition, the impact of the implementation of the care bundle that we report is adjusted for a time trend and a range of case‐mix factors (age, ethnicity, body mass index, parity, birthweight and mode of birth), also including additional sensitivity analyses exploring different model assumptions.
The development and implementation of the care bundle was supported by the two relevant national professional bodies in the UK, representing obstetricians and midwives, and promoted multidisciplinary teams to work together. The intervention was multifaceted and informed by a detailed theory of change. 21 Women were involved in all stages of the quality improvement project, which ensured that the implementation of the care bundle supported women’s choices of birth position and the importance of communication during labour, but their involvement in the design of the care bundle itself was limited.
Our quality improvement project was designed as a pragmatic study only using routinely collected clinical data. Therefore, we could not measure the ‘coverage’ (compliance rate for all eligible births) and the ‘fidelity’ (extent to which the care bundle was applied as intended) of the intervention, which limits our ability to determine to what extent the effect of the OASI Care Bundle can be further increased through enhancing its uptake.
We could not control for some of the main risk factors for OASI, most notably shoulder dystocia, epidural use and length of second stage of labour. However, shoulder dystocia accounts for <1% of births and it is unlikely that the rates of other major risk factors changed before and after implementation of the care bundle. Therefore, it is unlikely that these risk factors had a major confounding effect on our results.
Interpretation
A ‘package of interventions’ to reduce the rate of OASI was developed for the first time in Norway, in response to observations that the rates of OASI were consistently lower in Finland than in other Scandinavian countries. 14 , 16 , 17 The difference between these countries was attributed to the ongoing and consistent practice of slowing down the birth of the head using a specific manual perineal protection technique, the so‐called ‘Finnish grip’, 8 and episiotomy when clinically indicated, explicitly avoiding a median cut.
An observational study in five Norwegian units using a structured training programme to implement this approach showed a reduction in the OASI rates from 4–5% to 1–2%. 16 , 17 Subsequently, this approach was implemented in Denmark, 32 , 33 Holland, 20 England 34 and the USA. 19 The results of the Danish studies matched those seen in Norway, but the reductions in OASI rates observed in the other countries were smaller, and not statistically significant because of small sample sizes. Possible explanations for these differences include the extent to which the intervention to reduce OASI rates was fully adopted by the clinical teams 35 as well as methodological issues, including improved detection rates of perineal and anal injuries after implementation of the intervention. 36
One might argue that the reduction in OASI rates that was found after the implementation of the OASI Care Bundle is relatively small and that the extra effort linked to the implementation process may outweigh the benefits. However, our OASI Care Bundle also requires a careful check of the perineum following birth, ensuring accurate diagnoses, which may have increased the OASI detection rate after the implementation of the care bundle. Therefore, the reduction of OASI rates that we found after implementation of the OASI Care Bundle is likely to be an underestimate of its true effect.
Our study was not powered to study the effect of the OASI Care Bundle in specific groups. However, the lack of subgroup differences in our study is in line with the results of studies from Norway and Denmark with respect to parity 16 , 32 , 33 and studies from the Netherlands and Denmark with respect to mode of birth. 20 , 33
Concerns have been raised about the impact of interventions similar to the OASI Care Bundle on episiotomy and caesarean section rates. For example, increases in episiotomy rates were observed for subgroups of women or some participating units in Norway and Denmark, 14 , 16 , 17 , 33 but not in the Netherlands 20 or the USA. 19 Our study did not find any indication that the implementation of the care bundle affected caesarean section or episiotomy rates, albeit that the episiotomy rates that we observed (25.1% in the baseline phase and 24.5% in the evaluation phase) were higher than the corresponding episiotomy rate of 21.9% reported by the National Maternity and Perinatal Audit for vaginal singleton cephalic births at term between April 2016 and March 2017 in England, Scotland and Wales.
Our results represent the effect of a combination of interventions. It has been argued that interventions such as manual perineal protection should not be considered in isolation but always as part of a combination of interventions that can be implemented together because the causes of OASI are complex. 37 This would explain, in addition to their limited statistical power and heterogeneity, why meta‐analyses of randomised controlled trials of manual perineal protection 37 , 38 did not find evidence of a protective effect.
Conversely, a single‐centre study in the UK of 10 370 vaginal births evaluating the impact of an OASI prevention programme, including encouraging an upright birthing position, effective communication to slow down birth of the fetal head, and a hand placed on the head to judge speed of birth, but without manual perineal protection, found a reduction in OASI rate from 2.8 to 1.7%. 39 Study authors argue that the key to success of their programme is that it not only focuses on how the second stage of labour is conducted but includes a multifaceted campaign increasing awareness and engagement among healthcare professionals, which echoes the theory of change underpinning the approach used in our study.
Conclusion
These findings from a large‐scale quality improvement project across the NHS in England, Scotland and Wales demonstrate the potential of the care bundle to improve perineal care during childbirth.
Disclosure of interests
All authors have completed the Unified Competing Interests form (available on request from the corresponding author). NS reports grants from National Institute for Health Research and personal fees from London Safety and Training Solutions Ltd, during the conduct of the study, and grants from Sanofi Pasteur and King’s Health Partners, outside the submitted work. IGU, PB, NS, LS, VN, AH, RT and JvdM report a grant from the Health Foundation Scaling Up Improvement Programme during the conduct of the study. RF has nothing to disclose.
Completed disclosure of interests forms are available to view online as supporting information.
Contribution to authorship
The study was conceived and designed by all authors. IGU and JvdM performed the statistical analyses. RT, RF, LS, NS, VN and AH assisted with the interpretation of results. IGU, PB and JvdM wrote the manuscript, with input from all other authors. The joint senior authors (RT and JvdM) have made an equal contribution to this study and manuscript.
Details of ethics approval
This quality improvement intervention was reviewed by NHS Health Research Authority in October 2016 and approved as a service evaluation (Ref: 60/86/81). Relevant local approvals were obtained from the participating units’ research and development departments, namely: Bedford Hospital, Birmingham Women’s Hospital, Calderdale Royal Hospital, Chelsea & Westminster Hospital, Epsom General Hospital, Milton Keynes University Hospital, Nottingham University Hospital, Poole Hospital, Queen Elizabeth University Hospital, Royal Gwent Hospital, Royal United Hospital Bath, Saint Mary's Hospital, St Richard’s Hospital, St John’s Hospital, University Hospital of North Tees and Warrington Hospital. We also obtained Caldicott Guardian Approval from each of these units for the clinical data we receive.
Funding
The OASI Project was funded by The Health Foundation Scaling Up Improvement Programme (award number 7674). The funders of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report. NS’ research is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration (ARC) South London at King’s College Hospital NHS Foundation Trust. NS is a member of King’s Improvement Science, which offers co‐funding to the NIHR ARC South London and comprises a specialist team of improvement scientists and senior researchers based at King’s College London. Its work is funded by King’s Health Partners (Guy’s and St Thomas’ NHS Foundation Trust, King’s College Hospital NHS Foundation Trust, King’s College London and South London and Maudsley NHS Foundation Trust), Guy’s and St Thomas’ Charity and the Maudsley Charity.
Acknowledgements
We are grateful to the obstetric and midwifery champions at each of the 16 maternity units, for their hard work and dedication to improving outcomes for women.
Supporting information
Figure S1. Consort flow diagram.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Gurol-Urganci I, Bidwell P, Sevdalis N, Silverton L, Novis V, Freeman R, Hellyer A, van der Meulen J, Thakar R. Impact of a quality improvement project to reduce the rate of obstetric anal sphincter injury: a multicentre study with a stepped-wedge design. BJOG 2021; 128:584–592.
van der Meulen and Thakar are joint senior authors.
Study registration: The OASI Project was retrospectively registered on the ISCTRN database: date assigned 03/10/2017 (#12143325, http://www.isrctn.com/ISRCTN12143325).
Linked article: This article is commented on by S Alexander and J Langhoff‐Roos, p. 593 in this issue. To view this mini commentary visit https://doi.org/10.1111/1471-0528.16560.
References
- 1. Sultan A. Obstetric perineal injury and anal incontinence. Clinical Risk 1999;5:193–6. [Google Scholar]
- 2. LaCross A, Groff M, Smaldone A. Obstetric anal sphincter injury and anal incontinence following vaginal birth: a systematic review and meta‐analysis. J Midwifery Womens Health 2015;60:37–47. [DOI] [PubMed] [Google Scholar]
- 3. Gurol‐Urganci I, Cromwell DA, Edozien LC, Mahmood TA, Adams EJ, Richmond DH, et al. Third‐ and fourth‐degree perineal tears among primiparous women in England between 2000 and 2012: time trends and risk factors. BJOG 2013;120:1516–25. [DOI] [PubMed] [Google Scholar]
- 4. Ampt AJ, Patterson JA, Roberts CL, Ford JB. Obstetric anal sphincter injury rates among primiparous women with different modes of vaginal delivery. Int J Gynecol Obstet 2015;131:260–4. [DOI] [PubMed] [Google Scholar]
- 5. Chi Wai T, Cecilia CW, Anny TWM, Hau YL. Incidence and risk factors of obstetric anal sphincter injuries after various modes of vaginal deliveries in Chinese women. Chin Med J 2015;128:2420–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McLeod NL, Gilmour DT, Joseph KS, Farrell SA, Luther ER. Trends in major risk factors for anal sphincter lacerations: a 10‐year study. J Obstet Gynaecol Canada 2003;25:586–93. [DOI] [PubMed] [Google Scholar]
- 7. Marschalek ML, Worda C, Kuessel L, Koelbl H, Oberaigner W, Leitner H, et al. Risk and protective factors for obstetric anal sphincter injuries: a retrospective nationwide study. Birth (Berkeley, Calif) 2018;45(4):409–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Laine K, Gissler M, Pirhonen J. Changing incidence of anal sphincter tears in four Nordic countries through the last decades. Eur J Obstet Gynecol Reprod Biol 2009;146:71–5. [DOI] [PubMed] [Google Scholar]
- 9. Trochez R, Waterfield M, Freeman RM. Hands on or hands off the perineum: a survey of care of the perineum in labour (HOOPS). Int Urogynecol J 2011;22:1279–85. [DOI] [PubMed] [Google Scholar]
- 10. Ismail KM, Paschetta E, Papoutsis D, Freeman RM. Perineal support and risk of obstetric anal sphincter injuries: a Delphi survey. Acta Obstet Gynecol Scand 2015;94:165–74. [DOI] [PubMed] [Google Scholar]
- 11. Tincello DG, Williams A, Fowler GE, Adams EJ, Richmond DH, Alfirevic Z. Differences in episiotomy technique between midwives and doctors. BJOG 2003;110:1041–4. [PubMed] [Google Scholar]
- 12. Naidu M, Kapoor DS, Evans S, Vinayakarao L, Thakar R, Sultan AH. Cutting an episiotomy at 60 degrees: how good are we? Int Urogynecol J 2015;26:813–6. [DOI] [PubMed] [Google Scholar]
- 13. East CE, Lau R, Biro MA. Midwives' and doctors' perceptions of their preparation for and practice in managing the perineum in the second stage of labour: a cross‐sectional survey. Midwifery 2015;31:122–31. [DOI] [PubMed] [Google Scholar]
- 14. Laine K, Skjeldestad FE, Sandvik L, Staff AC. Incidence of obstetric anal sphincter injuries after training to protect the perineum: cohort study. BMJ Open 2012;2:e001649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rasmussen O, Yding A, Anhoj J, Anderson C, Boris J. Reducing the incidence of Obstetric Sphincter Injuries using a hands‐on technique: an interventional quality improvement project. BMJ Quality 2016;5:u217936.w7106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Laine K, Pirhonen T, Rolland R, Pirhonen J. Decreasing the incidence of anal sphincter tears during delivery. Obstet Gynecol 2008;111:1053–7. [DOI] [PubMed] [Google Scholar]
- 17. Hals E, Oian P, Pirhonen T, Gisller M, Hjelle S, Nilsen E. A multicenter interventional program to reduce the incidence of anal sphincter tears. Obstet Gynaecol 2010;116:901–8. [DOI] [PubMed] [Google Scholar]
- 18. Stedenfeldt M, Oian P, Gissler M, Blix E, Pirhonen J. Risk factors for obstetric anal sphincter injury after a successful multicentre interventional programme. BJOG 2014;121:83–91. [DOI] [PubMed] [Google Scholar]
- 19. Yeung J, Stecher A, Crisp C, Mazloomdoost D, Smith B, Kleeman S, et al. Incidence of obstetric anal sphincter injuries after training to protect the perineum. Female Pelvic Med Reconstr Surg 2018;24:126–9. [DOI] [PubMed] [Google Scholar]
- 20. De Meutter L, van Heesewijk AD, van der Woerdt‐Eltink I, de Leeuw JW. Implementation of a perineal support programme for reduction of the incidence of obstetric anal sphincter injuries and the effect of non‐compliance. Eur J Obstet Gynecol Reprod Biol. 2018;230:119–23. [DOI] [PubMed] [Google Scholar]
- 21. Bidwell P, Thakar R, Sevdalis N, Silverton L, Novis V, Hellyer A, et al. A multi‐centre quality improvement project to reduce the incidence of obstetric anal sphincter injury (OASI): study protocol. BMC Pregnancy Childbirth 2018;18:331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Royal College of Obstetricians and Gynaecologists . The management of third and fourth‐degree perineal tears. RCOG Green‐top Guideline No. 29. London: RCOG, 2015. [https://www.rcog.org.uk/globalassets/documents/guidelines/gtg‐29.pdf]. Accessed 3 August 2020. [Google Scholar]
- 23. OASI Care Bundle Project Team . OASI Care Bundle Project materials. 2019. [https://www.rcog.org.uk/en/guidelines‐research‐services/audit‐quality‐improvement/oasi‐care‐bundle/materials/]. Accessed 24 July 2020.
- 24. Sultan AH, Kettle C. Diagnosis of perineal trauma In: Sultan AH, Thakar R, Fenner D, editors. Perineal and anal sphincter trauma. London: Springer; 2007:13–9. [Google Scholar]
- 25. Information Services Division Scotland . Births in Scottish Hospitals. Year ending 31 March 2018. 2018. [Google Scholar]
- 26. Hussey MA, Hughes JP. Design and analysis of stepped wedge cluster randomized trials. Contemporary Clin Trials 2007;28:182–91. [DOI] [PubMed] [Google Scholar]
- 27. Royal College of Obstetricians & Gynaecologists . Patterns of maternity care in English NHS trusts 2013/14. London, UK: 2016. [Google Scholar]
- 28. Austin PC. Estimating multilevel logistic regression models when the number of clusters is low: a comparison of different statistical software procedures. Int J Biostat 2010;6:Article 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hemming K, Taljaard M, Forbes A. Analysis of cluster randomised stepped wedge trials with repeated cross‐sectional samples. Trials 2017;18(1):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Haines TP, Hemming K. Stepped‐wedge cluster‐randomised trials: level of evidence, feasibility and reporting. J Physiother 2018;64:63–6. [DOI] [PubMed] [Google Scholar]
- 31. Copas AJ, Lewis JJ, Thompson JA, Davey C, Baio G, Hargreaves JR. Designing a stepped wedge trial: three main designs, carry‐over effects and randomisation approaches. Trials 2015;16:352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rasmussen OB, Yding A, Anh OJ, Sander Andersen C, Boris J. Reducing the incidence of obstetric sphincter injuries using a hands‐on technique: an interventional quality improvement project. BMJ Qual Improv Rep 2016;5:u217936.w7106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Leenskjold S, Hoj L, Pirhonen J. Manual protection of the perineum reduces the risk of obstetric anal sphincter ruptures. Dan Med J 2015;62:A5075 [PubMed] [Google Scholar]
- 34. Naidu M, Sultan A, Thakar R. Reducing obstetric anal sphincter injuries using perineal support a preliminary experience. Female Pelvic Med Reconstr Surg 2014;20:S1–40. [Google Scholar]
- 35. Rasmussen OB, Yding A, Lauszus F, Andersen CS, Anhoj J, Boris J. Importance of individual elements for perineal protection in childbirth: an interventional prospective trial. AJP Rep 2018;8:e289–e294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal sphincter injuries – myth or reality? BJOG 2006;113:195–200. [DOI] [PubMed] [Google Scholar]
- 37. Bulchandani S, Watts E, Sucharitha A, Yates D, Ismail KM. Manual perineal support at the time of childbirth: a systematic review and meta‐analysis. BJOG 2015;122:1157–65. [DOI] [PubMed] [Google Scholar]
- 38. Aasheim V, Nilsen ABV, Reinar LM, Lukasse M. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev 2017;6:CD006672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Basu M, Smith D. Long‐term outcomes of the Stop Traumatic OASI Morbidity Project (STOMP). Int J Gynaecol Obstet 2018;142:295–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Consort flow diagram.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material


