Abstract
Background
Tai Chi (TC) mind-body exercise has been shown to reduce falls and improve balance and gait, however, few studies have evaluated the role of lower extremity muscle activation patterns in the observed benefits of TC on mobility.
Purpose
To perform an exploratory analysis of the association between TC training and levels of lower extremity muscle co-contraction in healthy adults during walking under single-task (ST) and cognitive dual-task (DT) conditions.
Methods
Surface electromyography of the anterior tibialis and lateral gastrocnemius muscles was recorded during 90 sec trials of overground ST (walking normally) and DT (walking with verbalized serial subtractions) walking. A mean co-contraction index (CCI), across all strides, was calculated based on the percentage of total muscle activity when antagonist muscles were simultaneously activated. A hybrid study design investigated long-term effects of TC via a cross-sectional comparison of 27 TC experts and 60 age-matched TC-naïve older adults. A longitudinal comparison assessed the shorter-term effects of TC; TC-naïve participants were randomly allocated to either 6 months of TC training or to usual care.
Results
Across all participants at baseline, greater CCI was correlated with slower gait speed under DT (β(95% CI) = -26.1(-48.6, -3.7)) but not ST (β(95% CI) = -15.4(-38.2, 7.4)) walking. Linear models adjusting for age, gender, BMI and other factors that differed at baseline indicated that TC experts exhibited lower CCI compared to TC naives under DT, but not ST conditions (ST: mean difference (95% CI) = -7.1(-15.2, 0.97); DT: mean difference (95% CI) = -10.1(-18.1, -2.4)). No differences were observed in CCI for TC-naive adults randomly assigned to 6 months of TC vs. usual care.
Conclusion
Lower extremity muscle co-contraction may play a role in the observed benefit of longer-term TC training on gait and postural control. Longer-duration and adequately powered randomized trials are needed to evaluate the effect of TC on neuromuscular coordination and its impact on postural control.
Trial registration
The randomized trial component of this study was registered at ClinicalTrials.gov (NCT01340365).
Introduction
Healthy gait and postural control require the effective function and coordination of lower extremity and trunk muscles [1–3]. Muscle co-contraction measured using electromyography (EMG), and defined as the simultaneous activation of agonist and antagonist muscle groups, can serve as an informative clinical marker of mobility health [4]. Relatively high muscle co-contraction is associated with joint degeneration, fatigue, reduced physical performance, and increased falls [2, 5–7], as well as a higher energy cost of walking [8, 9]. Increased co-contraction in older adults is associated with reduced joint mobility and has been hypothesized as a strategy to compensate for decreased postural control and sensory processing [10]. Muscle co-contraction has also been shown to positively correlate with aging from adulthood into senescence [11–13]. For these reasons, strategies that reduce lower-extremity co-contraction may be particularly advantageous for the promotion of safe, independent mobility and physical activity in older adults [11–13].
Tai Chi is an increasingly popular multi-modal mind-body exercise used to enhance mobility and function in older adults [14]. Tai Chi has been shown to reduce falls [15–18] and improve clinical measures of balance [15, 19–22] and gait (e.g., velocity, stride length, single-leg stance time, and stride time variability) [23–25]. Recent studies suggest that the benefits of Tai Chi’s mind-body training on gait may be more pronounced during “dual-task” challenges that require attention shifting between cognitive and motor tasks [25, 26]. Surprisingly, few studies have evaluated the potential role of lower extremity muscle activation patterns in contributing to the observed benefits of Tai Chi on mobility and postural control [27, 28].
To inform the potential of Tai Chi to effect lower extremity co-contraction, this exploratory analysis of secondary outcomes reports on the effect of both long- and short-term Tai Chi training on EMG-assessed co-contraction of the anterior tibialis and lateral gastrocnemius muscles during both undisturbed single-task, and dual-task overground walking in healthy older adults. Because previous work has shown that co-contraction of this pair of muscles is sensitive to dual-task challenges during overground walking [29], may be mediated in part by executive cognitive impairment, and that Tai Chi's benefits to gait health are more pronounced during dual-task challenges, we anticipated that: 1) Age-matched Tai Chi experts with long-term training experience would exhibit lower levels of co-contraction when compared Tai Chi naive older adults, particularly under dual-task challenges; 2) Dual-task walking would increase the levels of co-contraction more in Tai Chi naive than Tai Chi expert older adults; and 3) Tai Chi naive adults randomized to 6 months of Tai Chi training (vs. a waitlist no treatment control) would show reduced levels of co-contraction, particularly during dual-task walking.
Methods
Study design
The data presented here are part of a larger study evaluating physiological outcomes associated with long- and short-term Tai Chi training in healthy older adults. Measures of EMG during gait were secondary outcomes. Details of the study design and population characteristics are reported elsewhere [14, 25, 30–32] and are briefly summarized below. We employed a hybrid study design that included a cross-sectional observational study followed by a two-arm randomized clinical trial. The Institutional Review Boards at Beth Israel Deaconess Medical Center and Brigham and Women’s Hospital, Boston, Massachusetts, approved this study. The randomized clinical trial was registered at ClinicalTrials.gov (NCT01340365).
The cross-sectional study was designed to assess the association between long-term Tai Chi training on single and dual-task gait performance, including co-contraction during gait, by comparing Tai Chi-naive older adults with age-matched Tai Chi experts. The Tai Chi-naïve group was comprised of sixty healthy older subjects, age 50–79 years, who lived in the Greater Boston area and reported no regular Tai Chi practice within the past 5 years. Individuals were excluded if they had: 1) a chronic medical condition including cardiovascular disease, stroke, active cancer, neurological conditions, or significant neuromuscular or musculoskeletal conditions requiring chronic use of pain medication; 2) an acute medical condition requiring hospitalization within the past 6 months; 3) a self-reported inability to walk continuously for 15 minutes unassisted; or 4) regular participation in physical exercise on average 4 or more times per week. The Tai Chi expert group consisted of 27 subjects (age 50–79) who had been practicing Tai Chi regularly for at least 5 years prior to being enrolled (mean experience = 24.2 y). There was no limitation on the style of Tai Chi being practiced. With the exception of a regular Tai Chi practice, the other exclusion criteria and screening for the Tai Chi expert group were identical to that of the naïve group. Interested and eligible individuals were asked to sign an informed consent form.
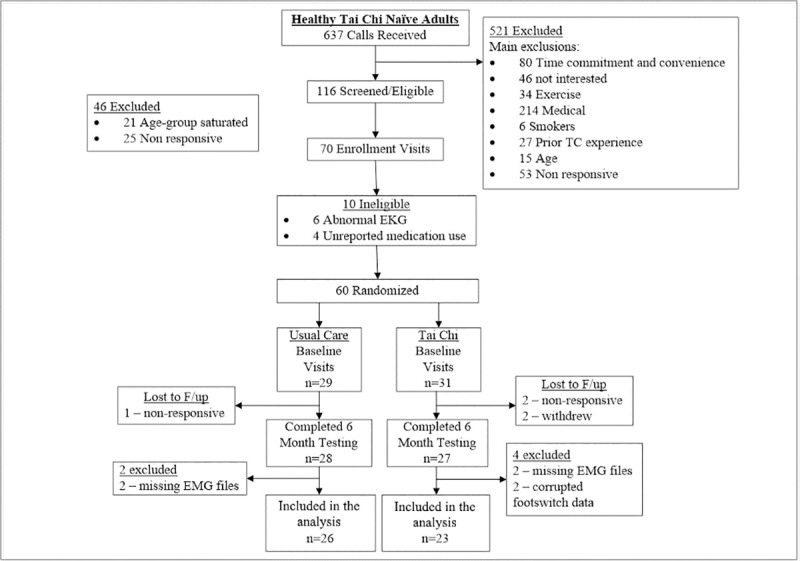
To assess the effects of shorter-term Tai Chi training on gait performance and lower extremity co-contraction, following baseline assessments, subjects in the Tai Chi-naïve group were randomized 1:1 to 6 months of Tai Chi in addition to their usual routine health care vs. to usual health care alone, see Fig 1. Those who were randomized to usual care alone were offered a complimentary 3 month Tai Chi course upon completion of the study. Randomization was stratified by age (50–59, 60–69, 70–79 years) and used a permuted blocks scheme with randomly varying block sizes. Randomization was performed by the study statistician. The staff members performing the gait assessments were blinded to group assignments. Tai Chi interventions were pragmatically administered at one location chosen from five pre-screened Tai Chi schools within the Greater Boston area that met certain guidelines as described elsewhere [14, 33]. Instructors were asked to teach using the same Tai Chi style, approach, and protocols that they use for non-study community participants. Study participants were asked to attend two classes per week (on average) over the 6 month intervention. They were asked to practice for at least 30 minutes on two additional days per week. Outcomes were assessed at baseline and at 6 months.
Fig 1. Participant flow through the randomized trial sub-study.
All outcomes were assessed at the Syncope and Falls in the Elderly (i.e. SAFE) laboratory at Beth Israel Deaconess Medical Center. The outcomes reported on here were part of a larger battery of tests that lasted approximately 3.5 hours per visit.
Measurement of muscle co-contraction
Co-contraction was assessed during overground walking in a straight 5m wide hallway. Subjects were instructed to walk at their normal preferred pace and make wide turns at the end of the hallway. Trials of 90 seconds of walking were performed under two conditions; walking without a cognitive task, referred to as a single-task (ST), and walking while performing serial subtraction, referred to as a dual-task (DT). The serial subtraction task consisted of counting backward from 500 by threes. The first 5 seconds of the walks were not included in the analysis as to avoid any differences in co-contraction associated with walking initiation.
EMG electrodes were placed on the anterior tibialis and lateral gastrocnemius muscles. EMG data were sampled at 1500Hz using a Noraxon data acquisition system (Noraxon, Scottsdale, USA) with a selectable low pass filter of 500Hz. The EMG sensors had a 1st order high pass filter set to 10Hz. Wireless force-sensitive resistor footswitches were placed under the subject’s toes and heels to record toe and heel strikes. The footswitches were also sampled at 1500Hz.
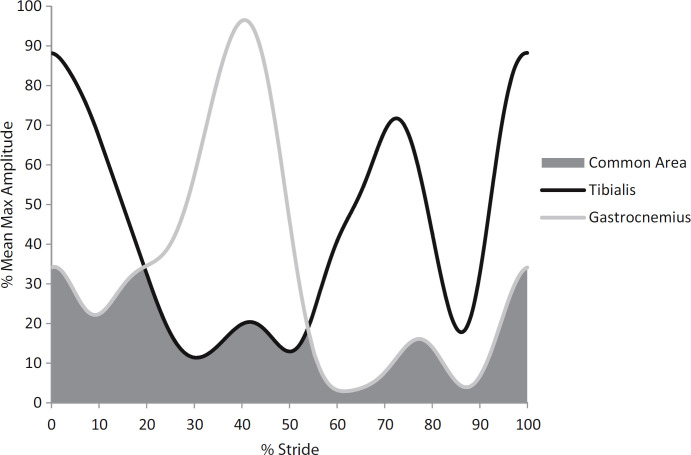
Data were processed using MATLAB (Mathworks, Natick, USA). Walking stride cycles were determined from footswitch data. A stride was defined as the time from a heel strike on a given leg to the subsequent heel strike on the same leg. Stride time variability was calculated from the stride time time-series as the coefficient of variation (%CV, 100 multiplied by the standard deviation of the stride times divided by the mean of each subject’s stride times). EMG data were bandpass filtered from 20 – 400Hz using a 4th order Butterworth filter, full-wave rectified, and subsequently low pass filtered at 6 Hz using a 4th order Butterworth, similar to Hallal et. al. [2]. Each stride was resampled to 1000 points. We used EMG to calculate co-contraction between two muscles during the entire walking bout by performing the following steps. First, the maximum EMG signal amplitude for each muscle group for all strides in a trial was noted and the mean of these maximums was calculated. Next, the EMG signals from each stride were averaged across all strides in a subject’s walk to get a mean EMG stride pattern. Next, the mean EMG stride pattern for each muscle group was then normalized as a percentage of the mean maximum amplitude to get the overall EMG stride pattern [29]. A co-contraction index (CCI) was then quantified based on this overall EMG stride pattern. The co-contraction index was defined as the percentage of mean total muscle activity when antagonist muscles (anterior tibialis and lateral gastrocnemius) were simultaneously activated, as derived from the following formula [2]:
Area A was defined as the area under the EMG curve of muscle A, and area B as the area under the curve for muscle B. The common area A & B was defined as the overlapping area between muscle A and muscle B on the mean EMG curve (Fig 2).
Fig 2. Calculation of lower limb muscle co-contraction index.
The EMG signals of the anterior tibialis and lateral gastrocnemius muscles were extracted from each stride of each walking trial, then averaged, and then normalized relative to the mean of the maximum EMG amplitudes for all strides. The common area is the overlapping region under the curves of the EMG signals and represents the muscle co-contraction index. Adapted from Lo et. al. 2017 [29].
Statistical analysis
General statistical analysis considerations
Our goal in this exploratory study was not to definitively test the efficacy of Tai Chi on co-contraction, but rather to generate preliminary data relevant to our proposed mechanisms. Given that these are exploratory analyses, we anticipated that we would not have sufficient power to formally test for interactions between our exposure and task (single versus dual). Instead, we stratified our analyses by task to explore if the tasks condition may impact the exposure-outcome association.
Subjects who had missing or corrupted data at their baseline or 6 month visit were excluded from analysis, see Fig 1 for details. All analyses were performed in SAS (version 9.3, SAS Institute, Cary, NC, USA).
Associations between co-contraction and markers of gait performance
Associations between co-contraction and both gait speed and stride time variability across all subjects at baseline for a given task were estimated with a linear regression model. An unadjusted model along with an age, gender, BMI, education, physical activity, and hall length adjusted model are presented. Age was a priori defined as a potential confounder. Gender, BMI, education, physical activity, and an executive function Z-score were added to the model due to observed differences between the groups at baseline. Executive function was assessed with two widely used measures, Category Fluency and the Trail Making Test [34, 35]. Results of these two outcomes were combined to create a composite executive function (EF) Z-score using methods described elsewhere [31]. Midway through our study testing, we changed the hallway location in which walking was evaluated. Hallway length changed from 48m to 23m. The ratio of Tai Chi experts tested on the shorter hallways was higher than the Tai Chi naives. We also checked our assumption that these potential associations would be independent of group by comparing the slope differences between experts and naives for each task with these unadjusted and adjusted models.
Muscle co-contraction in Tai Chi expert vs. Tai Chi naïve adults
Cross-sectional comparisons of co-contraction between Tai Chi experts and Tai Chi naïves were assessed with linear models assuming equal variance across groups. Analyses were conducted with both unadjusted models, and with models controlling for age, gender, BMI, education, physical activity, hall length, and executive function Z-score. Reasoning for the inclusion of these confounders are mentioned in the paragraph above.
The effect of short-term Tai Chi training on muscle co-contraction
Longitudinal changes in co-contraction over the 6-month intervention were compared between initially Tai Chi-naïve participants randomized to Tai Chi or usual care using a random-slopes model with shared baseline. The model included fixed effect of time, time x treatment, age, and time x age and random participant-specific intercepts and slopes with unstructured covariance. The shared baseline assumption, enforced by omitting a treatment main-effect term, properly reflects the true state of the population sampled prior to randomization and has the advantage of adjusting for any chance differences at baseline [36]. Treatment-group differences and adjusted means for a participant with mean age were estimated as well as their 95% confidence intervals.
Results
Baseline characteristics and study flow
Tai Chi expert and naïve subjects were well matched with respect to mean age. Relative to the naïve participants, the expert group had fewer females, lower BMI, a higher number of education years, and more self-reported physical activity (Table 1). Tai Chi experts also appeared to have modestly better cognitive ability as reflected in their higher executive function Z-score. Tai Chi experts reported a mean of 24.2±12 years of Tai Chi training experience (median: 20 years, range 10–50 years). Approximately equal numbers reported Yang (n = 12) and Wu (n = 14) style Tai Chi as their primary training systems.
Table 1. Baseline characteristics.
| Observational groups | Randomized groups | ||||
|---|---|---|---|---|---|
| Tai Chi experts (n = 26) | Tai Chi naives (n = 49) | Usual care (n = 26) | Tai Chi (n = 23) | ||
| Age | 62.96 ± 7.66 | 64.61 ± 7.58 | 64.92 ± 7.55 | 64.26 ± 7.77 | |
| Gender | Male | 12 (46.2%) | 16 (32.7%) | 8 (30.7%) | 8 (34.8%) |
| Female | 14 (53.8%) | 33 (67.3%) | 18 (69.3%) | 15 (65.2%) | |
| BMI | 22.89 ± 2.35 | 26.21 ± 5.34 | 26.51 ± 5.93 | 25.86 ± 4.68 | |
| Physical activity level a | 5.73 ± 2.03 | 4.35 ± 2.28 | 4.08 ± 2.33 | 4.65 ± 2.23 | |
| Education (years) | 18.46 ± 3.41 | 16.73 ± 2.92 | 16.22 ± 3.06 | 17.32 ± 2.73 | |
| Mini mental state exam (MMSE) | 29.03 ± 1.11 | 29.12 ± 1.07 | 29.15 ± 0.83 | 29.09 ± 1.31 | |
| Executive function Z-score b | 0.034 ± 0.19 | -0.018 ± 0.21 | - | - | |
| Exposure to Tai-Chi hours (% of subjects) | |||||
| Compliant subjects c | - | - | - | 89 (65%) | |
| Non-compliant subjects c | - | - | - | 45 (35%) | |
Unless otherwise noted values are provided as mean ± standard deviation.
a 4 = Run about 1 mile/week OR walk about 1.3 miles/week OR spend about 30 min/week in comparable physical activity; 5 = Run about 1 to 5 miles per week OR walk 1.3 to 6 miles per week OR spend 30 to 60 minutes per week in comparable physical activity; 6 = run about 6–10 miles/week OR walk 7–13 miles/week OR spend 1–3h/week in comparable physical activity.
b Executive function Z-score was calculated from the ratio of the standardized Trail Making and COWAT tests. More specifically the ratio of Trail Making B to Trail Making A and Category Fluency were used to generate an Executive function Z-score.
c Participants that attended a minimum of 70% of all classes (two 1 hour classes per week) and completed 70% or more of prescribed home practice (two 30 minute sessions per week) were considered compliant.
Baseline characteristics for Tai Chi naïve subjects randomized to Tai Chi plus usual care or to usual care alone were comparable (Table 1). A CONSORT flowchart detailing study recruitment, randomization, and retention for the randomized trial component of the study is shown in Fig 1. Recruitment spanned from March 2011 to March 2013. All follow up procedures were completed by September 2013.
A total of 4 non-serious adverse events were reported throughout study. All events were reported by participants randomized to the Tai Chi group. Only 2 of the 4 events were determined to be related to the Tai Chi intervention (both minor musculoskeletal injuries (one wrist, one ankle)).
Associations between co-contraction and markers of gait performance
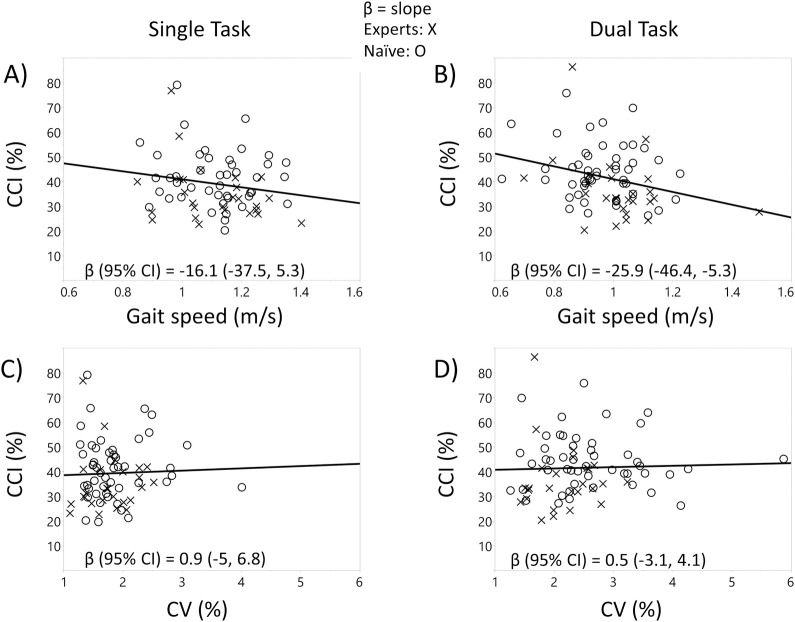
Regression models revealed that participants with greater CCI exhibited slower gait speed. This negative association was apparent under the dual-task condition in both the unadjusted model (β (95% CI) = -25.9 (-46.4, -5.3)) and the age, gender, BMI, physical activity, education, hallway length, and executive function Z-score adjusted model (β (95% CI) = -26.1 (-48.6, -3.7)). β indicates the slope change in CCI per unit in gait speed (shown above) or stride time variability (further below). Gait speed was measured in meters per second. Formal definitions for CCI and stride time variability are given above in the section on the measurement of muscle co-contraction. The correlation was not as apparent, however, under the single-task condition in the unadjusted model (β (95% CI) = -16.1 (-37.5, 5.3)) or adjusted model (β (95% CI) = -15.4 (-38.2, 7.4)). Associations between co-contraction and stride time variability (%CV) were weaker under single and dual-task conditions in the unadjusted model (ST: β (95% CI) = 0.9 (-5, 6.8); DT: β (95% CI) = 0.5 (-3.1, 4.1)) and adjusted model (ST: β (95% CI) = -0.47(-7.3, 6.3); DT: β (95% CI) = 0.25 (-3.5, 4.0)). The association between CCI and either gait speed or stride time variability were similar for the Tai Chi experts and the Tai Chi naïve subjects in an unadjusted model under DT (gait speed: expert β (95% CI) = -30.8 (-66.9, 5.4), naïve β (95% CI) = -14.1 (-40, 11.8); %CV: expert β (95% CI) = -1.7 (-13, 9.7), naïve β (95% CI) = -0.6 (-4.3, 3.1)) and ST conditions (gait speed: expert β (95% CI) = -26 (-59.6, 7.6), naïve β (95% CI) = -10.2 (-37.6, 17.3); %CV: expert β (95% CI) = 0.6 (-11.7, 12.9), naïve β (95% CI) = 0.3 (-6.4, 7.1)). Similar results were seen for an age, gender, BMI, physical activity, education, hallway length, and executive function Z-score adjusted model (DT gait speed: expert β (95% CI) = -30.9 (-81, 19.3), naïve β (95% CI) = -6.5 (-35.3, 22.3); DT %CV: expert β (95% CI) = -1.5 (-14.4, 11.4), naïve β (95% CI) = -1.8 (-5.4, 1.9); ST gait speed: expert β (95% CI) = -33.6 (-74, 6.8), naïve β (95% CI) = -12.9 (-45.8, 20.1); ST %CV: expert β (95% CI) = -1.4 (-16.7, 14), naïve β (95% CI) = -0.8(-8.9, 7.2)) (see Fig 3).
Fig 3.
Unadjusted associations between co-contraction vs. gait speed and stride time variability (%CV) across all subjects at baseline (solid line). A) Gait speed vs. co-contraction index (CCI) association under the single-task condition, B) gait speed vs. CCI association under the dual-task condition, C) CV vs. CCI association under the single-task condition, D) CV vs. CCI under the dual-task condition.
Muscle co-contraction in Tai Chi expert vs. Tai Chi naïve adults
Tai Chi experts (n = 26) exhibited lower CCI compared to Tai Chi naives (n = 49) under both ST and DT conditions (ST: mean difference (95% CI) = -6.5 (-12.4, -0.6); DT: mean difference (95% CI) = -7.44 (-13.2, -1.7)) in unadjusted models. Similar trends were observed in the age, gender, BMI, physical activity, education, hallway length, and executive function Z-score adjusted model (ST: mean difference (95% CI) = -7.1 (-15.2, 0.97); DT: mean difference (95% CI) = -10.1 (-18.1, -2.4)). Compared to ST walking, co-contraction trended toward being higher during DT walking in both the Tai Chi expert (ST = 34.5 ± 2.9, DT = 34.8 ± 2.8 [mean ± SE]) and Tai Chi naïve (ST = 41.6 ± 2.0, DT = 45.1 ± 2 [mean ± SE]) groups in the adjusted model (see Fig 4).
Fig 4. Co-contraction for age-matched Tai Chi expert and naïve older adults.
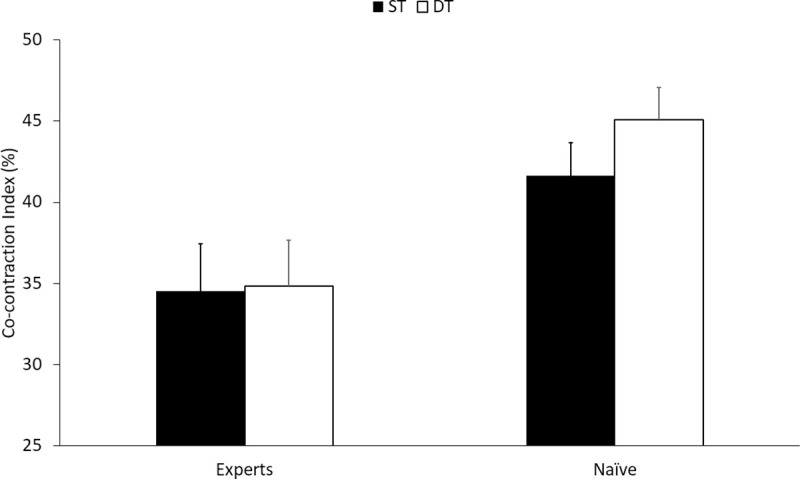
Comparison between naïve and experts with age, gender, BMI, activity, education, hallway length, and executive function Z-score adjusted mean values and standard errors, shown under single-task (ST) and dual-task (DT).
The effect of short-term Tai Chi training on muscle co-contraction
Subjects randomized to Tai Chi plus usual care and to usual care alone both showed a reduction in co-contraction in an age adjusted model between their baseline and six-month visits under DT (Tai Chi: Δbl-6mo mean (95% CI) = -3.8 (-7.6, -0.04), usual care: Δbl-6mo mean (95% CI) = -3.7 (-7.2, -0.14)) and to a lesser extent under ST (Tai Chi: Δbl-6mo mean (95% CI) = -2.2 (-6.3, 2), usual care: Δbl-6mo mean (95% CI) = -3.4(7.3, 0.5)). This age-adjusted random-slopes model with a shared baseline did not indicate any differences across time between groups (ST: mean difference (95% CI) = 1.2 (-3.8, 6.2); DT: mean difference (95% CI) = -0.1 (-4.7, 4.5)) (Table 2).
Table 2. Co-contraction for the usual care and randomized to Tai Chi groups at their baseline and 6 month visits.
| Outcome Measure | Tai Chi (n = 23) | Usual Care (n = 26) | Group x Time | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 Month | Baseline | 6 Month | ST | DT | |||||
| ST* | DT* | ST* | DT* | ST* | DT* | ST* | DT* | Mean difference (95% CI) | Mean difference (95% CI) | |
| Co-contraction index (%) | 41.3 (37.8, 44.9) | 43.9 (40.7, 47.1) | 39.2 (35.2, 43.2) | 40.1 (36.4, 43.8) | 41.3 (37.8, 44.9) | 43.9 (40.7, 47.1) | 38.0 (34.1, 41.8) | 40.2 (36.7, 43.7) | 1.2 (-3.8, 6.2) | -0.1 (-4.7, 4.5) |
Age-adjusted random-slopes model with a shared baseline.
*ST and DT provided as age adjusted mean (95% CI)
Discussion
Compared to healthy Tai Chi naive adults, age-matched Tai Chi experts exhibited lower CCI as measured with EMG during walking. Of note, this effect was more pronounced under dual-task conditions, including in models accounting for multiple potential confounders. Moreover, across both Tai Chi experts and naïve subjects, there was a negative association between levels of CCI and DT gait speed. In contrast to longer-term associations with Tai Chi training, shorter-term Tai Chi training had relatively smaller effects on CCI. Taken together, these preliminary results suggest that lower extremity co-contraction during overground walking may contribute to Tai Chi’s beneficial effect on gait health, and is a topic worthy of further exploration, particularly with a longer intervention than the 6 months used in this study.
Surprisingly few studies to date have employed EMG to evaluate the effect of Tai Chi on any aspect of gait or postural control [27, 37–40]. Observational studies have used EMG to characterize the activity of lower extremity muscles during the performance of choreographed Tai Chi sequences versus normal overground walking [41–43]. Not surprisingly, the less linear Tai Chi movements performed more slowly and with a relatively flexed knee and ankle stance resulted in higher levels of co-contraction [42]. Other studies have employed EMG to assess reaction to unpredictable postural perturbations, and reported that Tai Chi training was associated with shorter latencies in lower extremity muscles including the tibilais anterior and gastrocnemius [40, 44]. Gatts and Woolacott [28] conducted a randomized controlled trial evaluating short-term Tai Chi training (3 weeks) which employed an array of EMG sensors to evaluate lower extremity muscle responses during experimental balance recovery tasks (i.e., shifting force plates on heel strikes). Tai Chi subjects, but not controls, significantly reduced the tibialis anterior response time to these balance perturbations, as well as the occurrence of co-contraction of the tibilais anterior and gastrocnemius of the perturbed leg. That study also reported that Tai Chi subjects exhibited significant improvements in multiple clinical balance measures [28]. To our knowledge, our study is the first to inform how long- or short-term Tai Chi training may influence lower extremity co-contraction during single- and dual-task overground walking.
We observed that the lower levels of muscle co-contraction exhibited by Tai Chi experts, as compared to Tai Chi naïve counterparts, was more pronounced during dual-task walking. Increasing evidence from epidemiological studies and clinical trials support that cognition and gait health are interrelated in older adults [45–47]. In particular, executive function—which describes an array of higher-level cognitive functions such as attention, task switching, judgment of external and internal cues, and goal setting—is highly associated with multiple parameters of gait health including speed and stride time variability in older adults. Recent studies employing dual-task paradigms also suggest that the widely-reported benefits of Tai Chi for gait, balance and fall prevention may result, in part, from enhanced executive function and cognitive-motor integration [48–50]. More generally, studies identifying gait related risk factors for falls have reported greater discrimination during dual- vs. single-task observations [51, 52]. However, few studies to date have employed EMG to understand the effect of dual-task cognitive distractions on co-contraction of lower extremity antagonistic muscles during gait, or if Tai Chi could ameliorate the effect of a cognitive distraction on muscle coordination. Whether the differential benefits of Tai Chi for lower extremity muscle function and gait observed under single- versus dual-task are due to Tai Chi's enhancement of executive function [31, 53–55], motor control [56–58], or other processes warrants additional study.
In the cross-sectional component of this study, we observed a trend towards higher levels of co-contraction during DT vs. ST walking. Lo and colleagues also evaluated EMG response’s under dual- versus single-task walking and explored how interactions between cognitive and motor processes effect lower extremity neuromuscular function [29]. They did not observe a significant difference in co-contraction under DT vs. ST. However, paralleling our findings of an association between CCI and DT gait speed, they did report that CCI was associated with gait speed and stride time under dual-task but not single-task conditions. They also reported an association between executive function and co-contraction during both normal and dual-task walking. Given that prior studies have suggested that Tai Chi affects both cognitive and motor skills [22, 25, 31, 53, 59], further investigation into EMG outcomes (co-contraction, reaction time) with long-term Tai Chi interventions may be warranted, especially under dual-task conditions.
In contrast to cross-sectional comparisons between Tai Chi experts and naives, we observed only small effects of short-term Tai Chi training on levels of co-contraction. This observation parallels other clinical and phsyiological outcomes previously reported in the same study population [30–32]. The small effect observed in the cross-sectional comparison may be due to many factors including that 6 months of Tai Chi training is an insufficient dose to effect change. It is also possible that because our eligibility criteria, which targeted and resulted in a very healthy population, responses to Tai Chi were limited due to ceiling effects. Indeed, mean CCI values in our study population were markedly lower than those reported for the older and more frail population studied by Lo and colleagues [29].
This study has a number of limitations. As an exploratory study of secondary outcomes, sample sizes in both the cross-sectional and randomized studies were small and these analyses may be underpowered to detect differences between the groups. In the cross-sectional study, although we corrected for multiple potential confounders, observed between-group differences may have been confounded by other factors which we did not assess. In our cross-sectional comparison, we observed modest between-group differences in physical activity which were partially accounted for in adjusted models. Nevertheless, future studies should better control for overall physical activity levels. In our randomized trial, both the short-duration of exposure (6 months) as well as the very high levels of health of participants at baseline may have contributed to the null effect of Tai Chi on CCI. Finally, we only assessed EMG on one pair of lower extremity muscles and during short periods of relatively simple overground walking tasks. Assements of a larger array of lower extremity and trunk muscles during more diverse and challenging motor and cognitive tasks may better inform the effect of Tai Chi on mobility and postural control.
Conclusions
Our results from the cross-sectional, and to a lesser extent, randomized group comparisons suggest that reduced co-contraction may play a role in the observed benefits of Tai Chi on gait and postural control. Given the exploratory nature of these analyses, larger and longer-duration randomized trials in both healthy and health challenged adult populations are needed to evaluate the effect of Tai Chi on co-contraction and its benefit on gait and postural control.
Supporting information
(DOC)
(DOC)
(DOCX)
Acknowledgments
We thank Jacquelyn Walsh, Matthew Lough, Danielle Berkowitz and Mary Quilty for research assistance.
Abbreviations
- TC
Tai Chi
- EMG
Electromyography
- CCI
Co-contraction index
- ST
single-task
- DT
dual-task
- CV
coefficient of variation
- BMI
Body Mass Index
- SE
standard error
- CI
confidence interval
Data Availability
All relevant data are available on Physionet at: https://physionet.org/content/taichidb/1.0.1/ DOI: https://doi.org/10.13026/51h0-rs07.
Funding Statement
This work was supported by grant R21 AT005501-01A1 and K24 AT009282 from the National Center for Complementary and Integrative Health (NCCIH: https://nccih.nih.gov/), National Institutes of Health (NIH: http://www.nih.gov/) awarded to PW. Dr. LL was supported by grant R03-AG025037 from the National Institute on Aging (NIA: http://www.nia.nih.gov/) and the Irving and Edyth S. Usen and Family Chair in Geriatric Medicine at Hebrew SeniorLife. Dr. YM was supported by grant NCCIH T32AT000051 from the National Institutes of Health. Dr. CP was supported by a grant (NSC 102-2911-I-008-001) from Ministry of Science and Technology of Taiwan (https://www.most.gov.tw/en/public). Dr. BM was supported by grant 5 KL2 RR025757-04 from the Harvard Catalyst (http://catalyst.harvard.edu/) and grant 1K01 AG044543-01A1 from the National Institute on Aging (NIA: http://www.nia.nih.gov/). Dr. PR was supported by grant K01 HL128791 from the National Center for Complementary and Integrative Health (NCCIH: https://nccih.nih.gov/), National Institutes of Health (NIH: http://www.nih.gov/). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCCIH, NHLBI, NCRR, or the NIH. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Krasovsky T, Levin MF. Review: toward a better understanding of coordination in healthy and poststroke gait. Neurorehabilitation and neural repair. 2010;24(3):213–24. Epub 2009/10/14. 10.1177/1545968309348509 . [DOI] [PubMed] [Google Scholar]
- 2.Hallal CZ, Marques NR, Spinoso DH, Vieira ER, Gonçalves M. Electromyographic patterns of lower limb muscles during apprehensive gait in younger and older female adults. Journal of Electromyography and Kinesiology. 2013;23:1145–9. 10.1016/j.jelekin.2013.06.006 . [DOI] [PubMed] [Google Scholar]
- 3.Callisaya ML, Blizzard L, Schmidt MD, McGinley JL, Srikanth VK. Ageing and gait variability—a population-based study of older people. Age and ageing. 2010;39(2):191–7. 10.1093/ageing/afp250 [DOI] [PubMed] [Google Scholar]
- 4.Busse ME, Wiles CM, Van Deursen RWM. Co-activation: Its association with weakness and specific neurological pathology. Journal of NeuroEngineering and Rehabilitation. 2006;3:1–8. 10.1186/1743-0003-3-1 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hallal CZ, Marques NR, Vieira ER, Brunt D, Spinoso DH, Castro A, et al. Lower limb muscle coactivation levels in healthy younger and older adults during functional dual-task gait. Motriz Revista de Educacao Fisica. 2013;19:620–6. 10.1590/S1980-65742013000300013 .26378330 [DOI] [Google Scholar]
- 6.Hortobágyi T, Solnik S, Gruber A, Rider P, Steinweg K, Helseth J, et al. Interaction between age and gait velocity in the amplitude and timing of antagonist muscle coactivation. Gait and Posture. 2009;29:558–64. 10.1016/j.gaitpost.2008.12.007 . [DOI] [PubMed] [Google Scholar]
- 7.Ho CY, Bendrups AP. Ankle reflex stiffness during unperceived perturbation of standing in elderly subjects. The journals of gerontology Series A, Biological sciences and medical sciences. 2002;57:B344–B50. 10.1093/gerona/57.9.b344 . [DOI] [PubMed] [Google Scholar]
- 8.Peterson DS, Martin PE. Effects of age and walking speed on coactivation and cost of walking in healthy adults. Gait and Posture. 2010;31:355–9. 10.1016/j.gaitpost.2009.12.005 . [DOI] [PubMed] [Google Scholar]
- 9.Mian OS, Thom JM, Ardigò LP, Narici MV, Minetti AE. Metabolic cost, mechanical work, and efficiency during walking in young and older men. Acta Physiologica. 2006;186:127–39. 10.1111/j.1748-1716.2006.01522.x . [DOI] [PubMed] [Google Scholar]
- 10.Benjuya N, Melzer I, Kaplanski J. Aging-Induced Shifts From a Reliance on Sensory Input to Muscle Cocontraction During Balanced Standing. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2004;59:M166–M71. 10.1093/gerona/59.2.m166 . [DOI] [PubMed] [Google Scholar]
- 11.Nagai K, Yamada M, Uemura K, Yamada Y, Ichihashi N, Tsuboyama T. Differences in muscle coactivation during postural control between healthy older and young adults. Archives of Gerontology and Geriatrics. 2011;53(3):338–43. 10.1016/j.archger.2011.01.003 [DOI] [PubMed] [Google Scholar]
- 12.Nagai K, Yamada M, Tanaka B, Uemura K, Mori S, Aoyama T, et al. Effects of balance training on muscle coactivation during postural control in older adults: a randomized controlled trial. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2012;67(8):882–9. [DOI] [PubMed] [Google Scholar]
- 13.Freyler K, Weltin E, Gollhofer A, Ritzmann R. Improved postural control in response to a 4-week balance training with partially unloaded bodyweight. Gait & Posture. 2014;40(2):291–6. 10.1016/j.gaitpost.2014.04.186 [DOI] [PubMed] [Google Scholar]
- 14.Wayne PM, Manor B, Novak V, Costa MD, Hausdorff JM, Goldberger AL, et al. A systems biology approach to studying Tai Chi, physiological complexity and healthy aging: design and rationale of a pragmatic randomized controlled trial. Contemporary clinical trials. 2013;34:21–34. 10.1016/j.cct.2012.09.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolf SL, Barnhart HX, Ellison GL, Coogler CE. The Effect of Tai Chi Quan and Computerized Balance Training on Postural Stability in Older Subjects. Physical Therapy. 1997;77:371–81. 10.1093/ptj/77.4.371 . [DOI] [PubMed] [Google Scholar]
- 16.Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. 2012;(9). 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harmer PA, Li F. Tai Chi and falls prevention in older people. Tai Chi Chuan. 52: Karger Publishers; 2008. p. 124–34. [DOI] [PubMed] [Google Scholar]
- 18.Liu H, Frank A. Tai chi as a balance improvement exercise for older adults: A systematic review. Journal of Geriatric Physical Therapy. 2010;33:103–9. 10.1097/JPT.0b013e3181eda1c4 . [DOI] [PubMed] [Google Scholar]
- 19.Yan JH. Tai Chi practice improves senior citizens’ balance and arm movement control. Journal of Aging and Physical Activity. 1998;6(3):271–84. [Google Scholar]
- 20.Judge JO, Whipple RH, Wolfson LI. Effects of resistive and balance exercises on isokinetic strength in older persons. Journal of the American Geriatrics Society. 1994;42(9):937–46. 10.1111/j.1532-5415.1994.tb06584.x [DOI] [PubMed] [Google Scholar]
- 21.Wang C, Collet J, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions. ACC Current …. 2004;164:493–501. 10.1001/archinte.164.5.493 [DOI] [PubMed] [Google Scholar]
- 22.Wu G, Zhao F, Zhou X, Wei L. Improvement of isokinetic knee extensor strength and reduction of postural sway in the elderly from long-term Tai Chi exercise. Archives of Physical Medicine and Rehabilitation. 2002;83:1364–9. 10.1053/apmr.2002.34596 . [DOI] [PubMed] [Google Scholar]
- 23.Judge JO, Lindsey C, Underwood M, Winsemius D. Balance improvements in older women: effects of exercise training. Physical Therapy. 1993;73(4):254–62. 10.1093/ptj/73.4.254 [DOI] [PubMed] [Google Scholar]
- 24.Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Galver J, et al. Tai chi and postural stability in patients with Parkinson's disease. New England Journal of Medicine. 2012;366(6):511–9. 10.1056/NEJMoa1107911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wayne PM, Hausdorff JM, Lough M, Gow BJ, Lipsitz L, Novak V, et al. Tai Chi Training may Reduce Dual Task Gait Variability, a Potential Mediator of Fall Risk, in Healthy Older Adults: Cross-Sectional and Randomized Trial Studies. Frontiers in Human Neuroscience. 2015;9:1–10. 10.3389/fnhum.2015.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vergara-Diaz G, Osypiuk K, Hausdorff JM, Bonato P, Gow BJ, Miranda JG, et al. Tai Chi for Reducing Dual-task Gait Variability, a Potential Mediator of Fall Risk in Parkinson’s Disease: A Pilot Randomized Controlled Trial. Global Advances In Health and Medicine. 2018;7:2164956118775385 10.1177/2164956118775385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forrest W. Anticipatory postural adjustment and T'ai Chi Ch'uan. Biomedical sciences instrumentation. 1997;33:65–70. [PubMed] [Google Scholar]
- 28.Gatts SK, Woollacott MH. Neural mechanisms underlying balance improvement with short term Tai Chi training. Aging Clinical and Experimental Research. 2006;18:7–19. 10.1007/BF03324635 . [DOI] [PubMed] [Google Scholar]
- 29.Lo J, Lo O-Y, Olson EA, Habtemariam D, Iloputaife I, Gagnon MM, et al. Functional implications of muscle co-contraction during gait in advanced age. Gait & Posture. 2017;53:110–4. 10.1016/j.gaitpost.2017.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wayne PM, Gow BJ, Costa MD, Peng CK, Lipsitz LA, Hausdorff JM, et al. Complexity-based measures inform effects of tai chi training on standing postural control: Cross-sectional and randomized trial studies. PLoS ONE. 2014;9:2005 10.1371/journal.pone.0114731 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walsh JN, Manor B, Hausdorff J, Novak V, Lipsitz L, Gow B, et al. Impact of short- and long-term Tai Chi mind-body exercise training on cognitive function in healthy adults: Results from a hybrid observational study and randomized trial. Global Advances In Health and Medicine. 2015;4:38–48. 10.7453/gahmj.2015.058 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gow BJ, Hausdorff JM, Manor B, Lipsitz LA, Macklin EA, Bonato P, et al. Can Tai Chi training impact fractal stride time dynamics, an index of gait health, in older adults? Cross-sectional and randomized trial studies. PLoS ONE. 2017;12:1–17. 10.1371/journal.pone.0186212 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fischer M, Fugate-Woods N, Wayne PM. Use of pragmatic community-based interventions to enhance recruitment and adherence in a randomized trial of Tai Chi for osteopenic women: Insights from a qualitative sub-study. Menopause (New York, NY). 2014;21(11):1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arbuthnott K, Frank J. Trail making test, part B as a measure of executive control: validation using a set-switching paradigm. Journal of clinical and experimental neuropsychology. 2000;22(4):518–28. 10.1076/1380-3395(200008)22:4;1-0;FT518 [DOI] [PubMed] [Google Scholar]
- 35.Salthouse TA. Relations between cognitive abilities and measures of executive functioning. Neuropsychology. 2005;19(4):532 10.1037/0894-4105.19.4.532 [DOI] [PubMed] [Google Scholar]
- 36.Zeger SL, Liang K-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986:121–30. [PubMed] [Google Scholar]
- 37.Li JX, Xu DQ, Hong Y. Changes in muscle strength, endurance, and reaction of the lower extremities with Tai Chi intervention. Journal of biomechanics. 2009;42(8):967–71. 10.1016/j.jbiomech.2009.03.001 [DOI] [PubMed] [Google Scholar]
- 38.Xu D-Q, Li J-X, Hong Y. Effect of regular Tai Chi and jogging exercise on neuromuscular reaction in older people. Age and Ageing. 2005;34(5):439–44. 10.1093/ageing/afi114 [DOI] [PubMed] [Google Scholar]
- 39.Fong S-M, Ng GY. The effects on sensorimotor performance and balance with Tai Chi training. Archives of physical medicine and rehabilitation. 2006;87(1):82–7. 10.1016/j.apmr.2005.09.017 [DOI] [PubMed] [Google Scholar]
- 40.Sun W, Zhang C, Song Q, Li W, Cong Y, Chang S, et al. Effect of 1-year regular tai chi on neuromuscular reaction in elderly women: a randomized controlled study. Research in Sports Medicine. 2016;24(2):145–56. 10.1080/15438627.2015.1126280 [DOI] [PubMed] [Google Scholar]
- 41.Wu G. Age-related differences in Tai Chi gait kinematics and leg muscle electromyography: a pilot study. Archives of physical medicine and rehabilitation. 2008;89(2):351–7. 10.1016/j.apmr.2007.08.147 [DOI] [PubMed] [Google Scholar]
- 42.Wu G, Liu W, Hitt J, Millon D. Spatial, temporal and muscle action patterns of Tai Chi gait. Journal of Electromyography and Kinesiology. 2004;14:343–54. 10.1016/j.jelekin.2003.09.002 [DOI] [PubMed] [Google Scholar]
- 43.Tseng SC, Liu W, Finley M, McQuade K. Muscle activation profiles about the knee during Tai-Chi stepping movement compared to the normal gait step. Journal of Electromyography and Kinesiology. 2007;17:372–80. 10.1016/j.jelekin.2005.12.005 . [DOI] [PubMed] [Google Scholar]
- 44.Wang S-J, Xu D-Q, Li J-X. Effects of regular Tai Chi practice and jogging on neuromuscular reaction during lateral postural control in older people. Research in Sports Medicine. 2017;25(1):111–7. 10.1080/15438627.2016.1258649 [DOI] [PubMed] [Google Scholar]
- 45.Montero‐Odasso M, Verghese J, Beauchet O, Hausdorff JM. Gait and cognition: a complementary approach to understanding brain function and the risk of falling. Journal of the American Geriatrics Society. 2012;60(11):2127–36. 10.1111/j.1532-5415.2012.04209.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Springer S, Giladi N, Peretz C, Yogev G, Simon ES, Hausdorff JM. Dual‐tasking effects on gait variability: The role of aging, falls, and executive function. Movement disorders: official journal of the Movement Disorder Society. 2006;21(7):950–7. [DOI] [PubMed] [Google Scholar]
- 47.Sunderaraman P, Maidan I, Kozlovski T, Apa Z, Mirelman A, Hausdorff JM, et al. Differential associations between distinct components of cognitive function and mobility: implications for understanding aging, turning and dual-task walking. Frontiers in aging neuroscience. 2019;11:166 10.3389/fnagi.2019.00166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wayne PM, Hausdorff JM, Lough M, Gow BJ, Lipsitz L, Novak V, et al. Tai Chi Training may Reduce Dual Task Gait Variability, a Potential Mediator of Fall Risk, in Healthy Older Adults: Cross-Sectional and Randomized Trial Studies. Front Hum Neurosci. 2015;9:332 10.3389/fnhum.2015.00332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tsang WW, Hui-Chan CW, Fu SN. Effects of Tai Chi on pre-landing muscle response latency during stepping down while performing a concurrent mental task in older adults. Eur J Appl Physiol. 2012;112(7):2663–9. Epub 2011/11/23. 10.1007/s00421-011-2243-2 . [DOI] [PubMed] [Google Scholar]
- 50.Montero-Odasso M, Verghese J, Beauchet O, Hausdorff JM. Gait and cognition: a complementary approach to understanding brain function and the risk of falling. Journal of the American Geriatrics Society. 2012;60(11):2127–36. 10.1111/j.1532-5415.2012.04209.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mirelman A, Gurevich T, Giladi N, Bar‐Shira A, Orr‐Urtreger A, Hausdorff JM. Gait alterations in healthy carriers of the LRRK2 G2019S mutation. Annals of neurology. 2011;69(1):193–7. 10.1002/ana.22165 [DOI] [PubMed] [Google Scholar]
- 52.Mirelman A, Herman T, Brozgol M, Dorfman M, Sprecher E, Schweiger A, et al. Executive function and falls in older adults: new findings from a five-year prospective study link fall risk to cognition. PloS one. 2012;7(6):e40297 10.1371/journal.pone.0040297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wayne PM, Walsh JN, Taylor‐Piliae RE, Wells RE, Papp KV, Donovan NJ, et al. Effect of Tai Chi on cognitive performance in older adults: Systematic review and meta‐Analysis. Journal of the American Geriatrics Society. 2014;62(1):25–39. 10.1111/jgs.12611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wu M-T, Tang P-F, Goh JO, Chou T-L, Chang Y-K, Hsu Y-C, et al. Task-Switching Performance Improvements After Tai Chi Chuan Training Are Associated With Greater Prefrontal Activation in Older Adults. Frontiers in aging neuroscience. 2018;10:280 10.3389/fnagi.2018.00280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jor'dan AJ, Manor B, Hausdorff JM, Lipsitz LA, Habtemariam D, Novak V, et al. Long-term Tai Chi Training Is Associated With Better Dual-task Postural Control and Cognition in Aging Adults. Advances in mind-body medicine. 2018;32(3):4–11. [PMC free article] [PubMed] [Google Scholar]
- 56.Ghandali E, Moghadam ST, Hadian MR, Olyaei G, Jalaie S, Sajjadi E. The effect of Tai Chi exercises on postural stability and control in older patients with knee osteoarthritis. Journal of bodywork and movement therapies. 2017;21(3):594–8. 10.1016/j.jbmt.2016.09.001 [DOI] [PubMed] [Google Scholar]
- 57.Lee KY, Hui-Chan CW, Tsang WW. The effects of practicing sitting Tai Chi on balance control and eye-hand coordination in the older adults: a randomized controlled trial. Disability and rehabilitation. 2015;37(9):790–4. 10.3109/09638288.2014.942003 [DOI] [PubMed] [Google Scholar]
- 58.Wong AM, Chou S-W, Huang S-C, Lan C, Chen H-C, Hong W-H, et al. Does different exercise have the same effect of health promotion for the elderly? Comparison of training-specific effect of Tai Chi and swimming on motor control. Archives of gerontology and geriatrics. 2011;53(2):e133–e7. 10.1016/j.archger.2010.07.009 [DOI] [PubMed] [Google Scholar]
- 59.Wei G, Xu T, Fan F, Dong H, Jiang L, Li H. Can Taichi reshape the brain. A brain morph. 2013. 10.1371/journal.pone.0061038 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
(DOCX)
Data Availability Statement
All relevant data are available on Physionet at: https://physionet.org/content/taichidb/1.0.1/ DOI: https://doi.org/10.13026/51h0-rs07.