Abstract
The significant increase in worldwide morbidity and mortality from non-communicable diseases (NCDs) indicates that the efficacy of existing strategies addressing this crisis may need improvement. Early identification of the metabolic irregularities associated with the disease process may be a key to developing early intervention strategies. Unhealthy lifestyle behaviours are well established drivers of the development of several NCDs, but the impact of such behaviours on health can vary considerably between individuals. How can it be determined if an individual’s unique set of lifestyle behaviours is producing disease? Accumulating evidence suggests that lifestyle-associated activation of oxidative and inflammatory processes is primary driver of the cell and tissue damage which underpins the development of NCDs. However, the benefit of monitoring subclinical inflammation and oxidative activity has not yet been established. After reviewing relevant studies in this context, we suggest that quantification of oxidative stress and inflammatory biomarkers during the disease-free prodromal stage of NCD development may have clinical relevance as a timely indicator of the presence of subclinical metabolic changes, in the individual, portending the development of disease. Monitoring markers of oxidative and inflammatory activity may therefore enable earlier and more efficient strategies to both prevent NCD development and/or monitor the effectiveness of treatment.
Keywords: oxidative stress, inflammation, biomarkers, non-communicable disease, lifestyle, prevention, clinical application
1. Introduction
Many benefits have arisen from recent advances in modern technology especially in the field of medical sciences, enhancing the effectiveness of numerous disease treatments with the consequent improvement in both quality of life and extension in lifespan. However, living in modern societies has proven to be a double-edged sword, with several elements of the popular Western lifestyle actually contributing to the development of age-related chronic diseases, in particular the non-communicable diseases (NCDs) such as cardiovascular diseases, diabetes, neurodegenerative dementia and cancer [1,2,3]. While the lifespan of an individual suffering from any of these diseases may be extended through the application of an efficient disease management strategy [4], the cumulative effects of unaddressed poor lifestyle choices will promote a state of chronic morbidity and make them more vulnerable to ongoing development of degenerative changes and further NCDs [5,6].
NCDs are the leading causes of morbidity and mortality worldwide. Of the global reported deaths of 56.4 million in 2015, 70%, or 39.5 million, were due to NCDs including 14 million people who died too young before the age of 70 [7]. The annual mortality from NCDs is projected to increase to 55 million throughout the world by the year 2030 [8]. This is a costly outcome in terms of both personal morbidity and financial outlay as it is estimated that NCDs alone will drain over USD 60 trillion from the global economy from 2011 to 2030 [9].
The prevention of NCDs is a global challenge assigned a high priority by the World Health Organisation (WHO, Geneva, Switzerland) [8]. NCDs generally have a long prodromal stage often taking many years to develop. As a result, the potential for developing an NCD increases as the population ages. This rise in disease morbidity linked to the ageing population poses important challenges to health care systems globally [10]. Therefore, an effective early preventive strategy is an ideal approach to slow or even halt lifestyle-linked degenerative processes. Application of such a strategy in a healthcare model that places emphasis on disease prevention, rather than just disease management, appears necessary if the burgeoning NCD problem is to be averted [8]. The benefits of implementing a successful preventive health strategy are immense as it has been estimated that around 80% of type 2 diabetes, 80% of premature heart disease and stroke, and 40% of cancers are preventable [11]. While the importance of prevention has been highlighted throughout the literature for many years, integration of a successful preventive strategy for NCDs in modern health care systems is still not apparent. Although successful in controlling many of the world’s infectious diseases, the WHO is still searching for an effective way to control runaway NCDs [8].
As mentioned, NCDs are diseases of generally slow progression with clinical symptoms only becoming apparent after considerable cellular damage has occurred in target tissues. Research now supports the argument that this damage is largely influenced by biochemical changes associated with a redox imbalance producing a state of “chronic oxidative stress” often accompanied or linked to inflammation [12,13,14]. Oxidative stress has been identified as a critical step in the initiation and the development of the pathophysiological changes associated with several NCDs [15,16]. Elevated intracellular/plasma levels of free radicals (molecules with an unpaired valence electron), such as reactive oxygen species (ROS), can cause severe damage to cellular structures including lipids, proteins and DNA molecules, disrupting their functions and leading to fundamental damage to the entire cell [16,17]. Chronic exposure to these oxidative processes creates a subclinical state of progressive cell damage which accumulates over time. This damage facilitates tissue remodelling (e.g., to vascular endothelium in CVD) and eventually results in selective system failures and the dysfunctional state known as disease [14,16,18,19]. Therefore, measurement of biochemical markers associated with oxidative stress and inflammation may be useful in identifying an individual’s early biochemical shift toward disease, especially in the initial prodromal stage. The possibility of early (preclinical) detection, afforded by use of oxidative stress/inflammatory biomarkers, may also enable a more individualised and sensitive profiling compared to conventional population-based risk assessment tools that currently rely on downstream biomarkers [20,21].
In this paper, we review the available literature evidence on the importance of lifestyle-induced oxidative stress and inflammation in the development of NCDs and suggest that early correction of redox imbalances may be useful in arresting NCD development.
2. Lifestyle Links to NCDs
Unhealthy lifestyle behaviours are widely accepted as primary initiators of the disease processes through which NCDs develop [1,3,22]. Even though genetic factors have been shown to play a role, their contribution to NCDs has been estimated to be less than 10% [23]. Therefore, modifiable lifestyle behaviours are especially relevant as they are more amenable to intervention [11,24,25]. Epidemiological studies clearly identify lifestyle as a primary risk factor for the development of NCDs [1,11,26,27]. In one large cohort study, after a 20 year follow up, it was shown that unhealthy lifestyle behaviours including physical inactivity, alcohol intake, cigarette smoking and low intake of fruits and vegetables were associated with increased mortality risk of cardiovascular disease (CVD) and cancer [1]. Furthermore, in the European Prospective Investigation into Cancer and Nutrition, after a 7-year follow up, it was shown that practicing healthy lifestyle behaviours including performing physical activity, adhering to healthy dietary principles, not smoking, and having a body mass index (BMI) lower than 30, for 7 years was associated with 78% lower risk of developing a chronic disease (93% lower risk of diabetes, 81% lower risk of myocardial infarction, 50% lower risk of stroke, and 36% lower risk of cancer) [11]. Lifestyle behaviours are strongly linked to the development of NCDs, and as also suggested by others [28,29,30] a better understanding of the possible biochemical mechanisms through which these behaviours influence the disease progression will be helpful in informing effective preventive strategies.
3. Risk Scores and Lifestyle Behaviours
It has become increasingly apparent however that the interaction between lifestyle and the body’s biochemistry is multifaceted requiring complex modelling [22,31,32,33]. Unhealthy lifestyle behaviours are well known to cause metabolic changes in plasma levels of lipids and fasting glucose [33,34]. This has led many to develop various population-based risk scores composed of these biomarkers to identify groups at risk of NCDs and also to monitor the efficacy of any preventive approach [20,35,36,37,38,39]. For example, a number of risk scores are available for the prediction of coronary heart disease such as the Framingham risk score (FRS) [20,21], World Health Organization/International Society of Hypertension (WHO/ISH) risk prediction charts [38], American College of Cardiology/American Heart Association (ACC/AHA) pooled cohort equations [36], the third Joint British Societies’ risk calculator (RiskJBS) [37], and the Systematic Coronary Risk Evaluation (SCORE) [39]. While these are validated and widely used tools for the prediction of coronary heart disease, studies suggest that they tend to underestimate an individual’s actual risk, thereby potentially delaying initiation of an appropriate intervention such as lifestyle modification [35,40,41,42,43,44,45,46,47,48].
In regard to the assessment of total cardiovascular (CVD) risk at the population level, it has been shown that WHO/ISH charts underestimate the risk of Asian populations with high total CVD risk [44]. Furthermore, the value of FRS in identifying disease risk has been reported to be less clear in patients with concomitant inflammatory diseases, such as systemic lupus erythematosus (SLE) [45] and psoriatic arthritis [46], patients with diabetes [35], breast cancer [47] and metabolic syndrome [48]. While these diseases are associated with increased risk for premature cardiovascular disease, persons with these co-morbidities are estimated to have a low risk according to the FRS calculations. In addition, based on SCORE charts, younger individuals will always be categorised in the low risk category, even when all constituent risk factor levels are very unfavourable, and no combination of risk factors will place a 40-year old individual in the high risk category [39]. Thus, other risk biomarkers not currently included in these risk score calculations appear necessary to more accurately predict actual individual risk. Current risk score calculations include numerous risk factors such as age, gender, markers of dyslipidaemia, blood pressure, body-mass index (BMI), and history of diabetes and smoking [20,35,36,37,38,39]. However, these conventional risk factors cannot account for all cases of CVD [35,40,41,42,43,44,45,46,47,48]. This is, at least partially, due to the fact that the traditional biomarkers such as total cholesterol (TC) and low density lipoprotein cholesterol (LDL-C) are not primary initiators of the disease process, but rather mediators of downstream pathology [49]. This suggests that other, currently less conventional biomarkers, that are more upstream of the primary damage process, need to be included in the risk score calculations in order to improve the risk estimation potency of a probable NCD at the individual level.
4. Oxidative Stress Is Upstream of Conventional NCD Biomarkers
There has been a growing appreciation in the literature of how non-conventional metabolic, oxidative stress and inflammatory biomarkers are more direct indicators of NCD pathologies than conventional biomarkers alone. For example, progression to type 1 diabetes has been associated with the downregulation of amino acid metabolites, sugar derivatives and fatty acids [29]. Several studies have also identified the critical role of oxidative and inflammatory processes in all phases of coronary artery disease, from foam cell formation to plaque rupture and thrombosis [50,51,52,53]. The concept originated from an in vitro observation that showed oxidised LDL-C but not native LDL-C, could increase the motility of monocytes via chemotactic activity [54]. The recruitment of monocytes/macrophages to the damage site through enhanced chemotactic activity is a critical step in the initiation and progression of the damage to the endothelial cells in the arteries. Oxidised LDL, taken up by the macrophage scavenger system, if present in excess will transform the macrophages into a non-functional foam cell which subsequently forms part of the maturing plaque in the developing atherosclerotic lesion [19]. It also triggers inflammatory processes which further exacerbate an oxidative environment [55] (Figure 1).
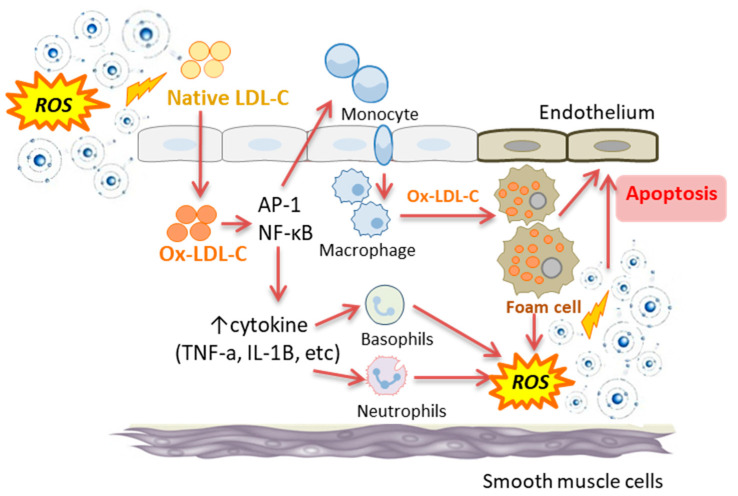
Figure 1.
The interplay between oxidative stress and inflammatory processes (i.e., NFκB and cytokine activity) in the development of endothelial cell damage and apoptosis. ROS: reactive oxygen species; Ox-LDL-C: oxidised low density lipoprotein cholesterol; AP-1: activator protein-1; NF-κB: nuclear factor-kappa B; TNF-α: tumour necrosis factor- α; IL-1β: interleukin-1β.
In this context, studies in otherwise healthy individuals have shown significant associations between oxidative stress biomarkers including F2-isoprostanes, malondialdehyde (MDA), 8- hydroxy deoxyguanosine (8-OHdG), oxidised disulphide form of cystine (CySS), and the ratio of glutathione (GSH) to its oxidised disulphide form (GSSG), and subclinical indicators of CVD development such as carotid artery intima-media thickness (CIMT) and flow-mediated vasodilation (FMD), even after controlling for the conventional CVD risk markers, such as LDL-C, and FRS [18,56].
In addition, independent and strong correlations have been reported between the lipid peroxidation biomarkers hydroxy-eicosatetraenoic acids (HETEs) and F2-isoprostanes and angiographic evidence of CVD, even after adjustment for FRS. The inclusion of these biomarkers into a multivariate prediction model that also included the FRS has been shown to significantly improve the prediction of coronary heart disease [57].
In regard to inflammatory biomarkers, the independent association between plasma levels of inflammatory biomarkers, C-reactive protein (CRP) and interleukin (IL)-6, and CVD in multivariable analyses including conventional CVD risk factors have previously been shown [58]. Importantly, it has been reported that plasma CRP levels can help to estimate the risk of initial cardiovascular events and even improve CVD risk classification in individuals with intermediate risk [59,60]. Therefore, the measurement of oxidative stress and inflammatory biomarkers as part of routine assessment appears to have clinical relevance by increasing the sensitivity of current risk scores and providing an early indication of the presence of a (subclinical) disease process.
Importantly, the part played by oxidative stress in disease development is consistent with the oxidative stress theory of ageing which posits that the accumulation of unrepaired oxidative damage at the cellular level is a primary player in the development of the aging phenotype [61]. In support of this concept, a number of recent studies from our laboratory [62,63] and others [64] have confirmed an increased level of oxidative damage biomarkers in aged tissues. Thus, the association between ageing and increased incidence of NCDs is at least partly explained by a subclinical increase in oxidative and inflammatory potential and changes in related biomarkers which underpin and/or exacerbate development of several NCDs [14]. However, what is the relationship between oxidative stress and inflammation?
5. Association between Oxidative Stress and Inflammation
Inflammation is the body’s nonspecific and immediate response by the innate immune system that is initiated in an acute phase response to environmental challenges such as pathogens and physical or chemical injuries including free radical attack [65,66]. Indeed, increased free radical generation and a state of oxidative stress and inflammation are closely interrelated. Oxidative stress can cause the damage to tissue that can trigger an inflammatory response, which in turn, can be a direct inducer of oxidative stress [53,66]. In this context, oxidative stress has been shown to cause the activation of redox-sensitive transcription factors, activator protein-1 (AP-1) and nuclear factor-kappa B (NF-κB) [67]. These factors can induce inflammatory processes and activate the innate immune system with the subsequent recruitment and the accumulation of inflammatory cells such as macrophages, leukocytes and neutrophils to the damage site [68,69]. These inflammatory cells can then produce metabolites of soluble mediators such as arachidonic acid, chemokines and pro-inflammatory cytokines such as interleukin (IL)-1β, IL-6 and tumour necrosis factor (TNF)-α [70,71]. Elevated levels of these pro-inflammatory cytokines can result in hepatic production and secretion of acute-phase proteins such as C-reactive protein (CRP) and also can further recruit inflammatory cells to the damage site [72,73]. Importantly, the generation of oxygen and/or nitrogen free radicals is a characteristic property of activated immune cells to eliminate pathogens or other stimuli. In other words, the production of free radicals is the primary damaging agents while the cytokines and acute phase proteins produced are essentially signalling molecules.
It is important to note that cytokines themselves do not cause direct cellular damage. Indeed, chronic inflammation exerts its cellular side effects largely through excessive generation of free radicals and depletion of antioxidants [14,66,74]. Hence, the accumulation of activated immune cells at the damage site accelerates the generation of free radicals and ROS which further promote the ongoing oxidative stress. Therefore, oxidative stress triggers an inflammatory response, which can in turn amplify oxidative stress [53,66] (Figure 1).
6. What Is Redox Imbalance and How Does It Relate to Oxidative Stress?
After the discovery of the oxidation of organic molecules by hydrogen peroxide in the presence of Fe++ by Fenton in 1894 [75], a series of investigations began in this area which later became known as oxidative stress. The generation of reactive oxidative species (ROS), the main players in oxidative reactions, is a normal consequence of all forms of aerobic life. In mammals, about 95% of inspired oxygen (O2) is successfully reduced to CO2 and H2O, without the formation of toxic radicals. However, the remaining 5%, proceeds through univalent reduction, producing reactive oxygen species which include superoxide (O2−) radicals, hydroxyl radical (OH−), hydrogen peroxide (H2O2) and the peroxynitrite (OONO−) radical [76]. The major sources of ROS production is mitochondrion [77], peroxisomal oxidase [78], xanthine oxidase [79], nicotinamide adenine dinucleotide phosphate (NADPH) oxidase [80] and cytochrome P450 enzymes [81]. The generation of ROS is also the major way the immune system uses to attack and kill pathogens and digest cell debris [53,66,82]. Inflammatory cells such as macrophages and neutrophils contain the NADPH oxidase system that, when activated, produces large amounts of superoxide and other damaging radical species that in the case of chronic inflammation can eventually lead to pervasive collateral cellular damage. Thus, free radical damage is the primary driver of cellular damage resulting from inflammatory activity [53,66,82,83].
Importantly, some free radical species also play a role as second messengers in controlling significant cellular functions such as the production of chemical mediators, cellular division and migration [67]. However, as free radicals with at least one unpaired electron in their atomic structure, they can be harmful at supra physiological concentrations [], and are counterbalanced by a complex antioxidant defence system comprising enzymatic (e.g., superoxide dismutase, glutathione peroxidise, glutathione reductase, and catalase) and non-enzymatic sources (e.g., dietary vitamins and phytochemicals, and glutathione) [13].
In all living cells a delicate balance exists between the generation, and the elimination of ROS by the endogenous antioxidant defence system. This is referred to commonly as the redox balance. Generally, overproduction of ROS or a defect in the ability of the endogenous antioxidant defence system to potentially detoxify these reactive substances or to repair the resulting damage, can lead to a redox imbalance [84]. Redox imbalance contributes significantly to the development of widespread cellular oxidation. This situation has been defined as oxidative stress (a state of redox imbalance), which as mentioned can eventually result in cell damage and death, with the consequent tissue alterations linked to the development of NCDs [14,16].
7. The Link between Lifestyle Behaviours, Oxidative Stress and Inflammation
As discussed above, a persuasive case is emerging for a pivotal role of oxidative damage and inflammation in the remodelling of tissue into its diseased phenotype at the biochemical and cellular levels [14,16,18,19]. Therefore, the assessment of oxidative and inflammatory biomarkers may improve disease stratification [57]. As previously mentioned, robust associations between the development of NCDs and unhealthy lifestyle behaviours have been known for some time [1,3,22]. Therefore, it is plausible that these two causal factors are interlinked. Indeed, there is a growing body of evidence showing that various lifestyle behaviours can induce a state of oxidative stress and inflammation which eventually leads to chronic NCDs [32,85,86] (Figure 2). In the following section, we provide evidence on how specific modifiable lifestyle behaviours have been linked to oxidative stress and inflammatory activity.
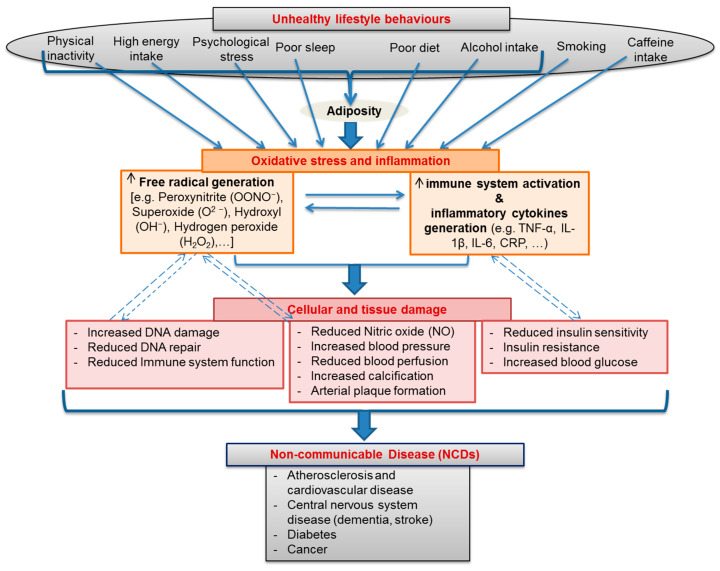
Figure 2.
A schematic showing lifestyle behaviours as major drivers behind the development of an oxidative stressed and inflammatory state which in turn play primary roles in the chronic cellular and tissue damage that leads to the final development of multiple non-communicable diseases (NCDs).
7.1. Adiposity and Total and Regional Body Fat
A positive energy balance, due to an imbalance between food (energy) intake and energy expenditure, can increase total body fat content, and visceral adipose tissue (VAT) fat mass, a key indicator of central obesity [87,88]. Total body fat and VAT have been reported to be positively associated with oxidative and inflammatory processes in several studies [89,90,91]. Indeed, ROS generation from NADPH oxidase activity has been detected in adipose tissue, and has been shown to progressively increase in aged adipose tissue [89,90]. There is also evidence that hypertrophic adipocytes can cause a state of local hypoxia due to their increased oxygen consumption [92]. Local hypoxia can increase the levels of total ROS and superoxide in particular, and decrease levels of key antioxidant enzymes, superoxide dismutase (SOD1 and SOD3) and catalase in adipocytes [90]. Furthermore, hypoxia has been shown to trigger the up-regulation of hypoxic-inducible factor (HIF) which has been linked to mitochondrial dysfunction [93] and activation of NF-κB with the subsequent production of inflammatory cytokines [94]. Another contributor to adipocyte-induced oxidative stress has been suggested to be alterations in gut microbiota that are accompanied by enhanced production of gut bacterial metabolite deoxycholic acid (DCA) [95]. DCA is known to damage DNA molecule through generation of ROS [96]. Visceral fat adipocytes can also significantly increase levels of plasma inflammatory biomarkers such as CRP [97], TNF-α [98] and IL-6 [99], either directly by releasing high amounts of these cytokines or indirectly by producing the inflammatory adipokines, leptin and resistin [91]. These inflammatory cytokines play a pivotal role in reducing insulin sensitivity and developing insulin resistant [100]. The persistent hyperglycaemia, secondary to insulin resistance, can further exacerbate the existing redox imbalance by inducing oxidative stress and contribute to beta cell destruction in type 2 diabetes [101].
7.2. Nutritional Behaviours
7.2.1. Energy Intake
In addition to the mentioned indirect effects of high energy intake in promoting a state of oxidative stress and inflammation via increasing body weight and total body fat [89,90,91], energy intake can be directly involved in producing a state of oxidative stress and inflammation [102,103,104,105,106]. Boden et al., reported that feeding healthy men with a high calorie diet (6000 kcal/day) for one week can produce a rapid onset of systemic oxidative stress detected by increased lipid peroxidation biomarker 8-iso-PGF2α and also ROS-mediated protein oxidation and carbonylation [102]. Furthermore, our own research has reported that ingestion of energy-dense phytonutrient-reduced foods including cream, ice cream or sugar can increase plasma lipid peroxidation and reduce plasma total antioxidant capacity (TAC) 2–4 h after ingestion of these foods [107]. In another study, a 25% calorie restriction for 28 days in obese subjects was reported to reduce the lipid peroxidation biomarker F2- isoprostane [106]. Furthermore, long term calorie limitation studies on healthy human subjects have shown that fasting can reduce oxidative damage to DNA and decrease plasma concentrations of thiobarbituric acid-reactive species (TBARS), carbonylated proteins, otyrosine, and m-tyrosine, all indicators of oxidative damage to lipids, proteins and amino acids, respectively [104,105]. There are also reports on the effects of short-term calorie limitation (48 h) on reducing ROS generation by leucocytes [103]. Chronic calorie restriction can attenuate the age-associated increase in inflammatory IL-6 production by peripheral mononuclear cells [108] and also reduce plasma inflammatory CRP levels [109]. Several animal and human studies have also suggested the involvement of energy intake and calorie restriction (10–50% below usual ad libitum intakes) in delaying ageing and extending lifespan [110]. As a basis for these observations, it has been suggested that calorie restriction can affect longevity-linked transcripts along the insulin-like growth factor 1 (IGF-1)/insulin/FOXO pathway [111]. However, the exact mechanism responsible for these observations is yet to be fully understood. Furthermore, it is still not clear whether these effects are due to a simple reduction in energy intake or the associated reduction in specific dietary components such as protein [112,113].
7.2.2. Protein Intake
Notwithstanding recommendations for an adequate intake of dietary proteins for the stimulation of muscle protein synthesis and/or suppression of protein breakdown [114], studies linking high intakes of proteins with ageing are emerging [115,116,117]. It has been suggested that protein restriction (40–85% of standard chow) can increase maximum lifespan by about 20% in rodents [115]. In humans, high protein intake (more than 20% of calories) has been associated with a 75% increase in overall mortality [117]. While suggested mechanisms include effects on ageing-associated molecules such as rapamycin (mTOR) [118], fibroblast growth factor 21 (FGF21), insulin [119], and insulin like growth factor 1 (IGF-1) [117], the mechanisms linking protein restriction to ageing are yet to be fully understood.
It has also been shown that protein restriction can independently reduce mitochondrial ROS generation, mitochondrial DNA oxidative damage biomarker 8-OHdG [120] and liver lipid peroxidation [121]. There are also reports that an increased protein intake can reduce the activity of the antioxidant enzyme superoxide dismutase in liver [121]. Protein intake and the metabolites of protein catabolism have also been shown to be negatively associated with the ageing-linked biomolecule, Nicotinamide adenine dinucleotide (NAD+), in a disease-free cohort [122]. Supplementation of the diet with specific amino acids (e.g., methionine) has also been shown to increase plasma lipid peroxidation biomarkers of hydroperoxides [123] and TBARS [124], and reduce tissue vitamin E levels [123].
7.2.3. Processed Meat
Several studies suggest that the source of protein can be as important as the amount of protein in the diet in ageing, development of NCDs and promoting a state of oxidative stress [117,125,126]. In this context, it has been reported that high consumption of animal proteins specifically those derived from red meat was positively associated with plasma lipid peroxidation biomarker TBARs and was negatively associated with plasma antioxidant capacity [126]. Red meat is a complex medium containing high amounts of saturated fat, trans fat and heme-iron and its effect on promoting oxidative stress may be attributed, at least in part, to the cumulative pro-oxidant properties of these components [126,127]. Furthermore, cooking meat using high-temperature methods such as frying can produce highly pro-oxidant products such as advanced glycation end products (AGE), heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs) [128,129,130,131]. Red meat is also a rich source of choline and l-carnitine, nutrients which can be metabolised to trimethylamine (TMA) by gut microbiota in colon, and then oxidised to trimethlyamine-N-oxide (TMAO) in the liver [132]. An elevated TMAO level as a result of high red meat intake has been shown to promote oxidative stress and vascular inflammation [133].
7.2.4. Polyunsaturated Fatty Acids
Polyunsaturated fatty acids (PUFAs) are fatty acids that contain more than one double bond in their structure. According to the position of their first double bond from the methyl end of the carbon chain, PUFAs can be categorised into omega-3 FAs with the first double bond at the third carbon atom (e.g., alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)), and omega-6 FAs with the first double bond at the sixth carbon atom from the methyl end of the carbon chain (e.g., linoleic acid (LA) and arachidonic acid (AA)) [134].
Both omega-3 and omega-6 PUFAs are precursors to potent lipid mediator signalling molecules, termed “eicosanoids” with critical roles in the regulation of inflammation. Omega-3 PUFAs are precursors to anti-inflammatory eicosanoids such as the 3-series prostaglandins, thromboxane A3 (TXA3), and the 5-series leukotrienes (LTs), while omega-6 PUFAs are precursors to proinflammatory eicosanoids such as the 2-series prostaglandins, and thromboxanes (TXA2), and the 4-series of leukotrienes (LTB4) [135]. Depending on their abundance in the diet, these PUFAs often compete with each other for binding to the enzymes involved in eicosanoids formation including cyclooxygenase (COX) and lipoxygenase (LOX) [136]. Therefore, a diet rich in omega-6 PUFAs and low in omega-3 PUFAs can elevate omega-6 to omega-3 ratio with a pro-inflammatory eicosanoid profile promoting an inflammatory phenotype [137]. Further anti-inflammatory properties of omega-3 PUFAs include, negative regulation of the activity of enzymes involved in inflammatory eicosanoids production such as COX-1 [138], the activation of the G-protein receptor, and reducing the activation of NF-κB [138,139]. There are also reports of involvement of omega-3 PUFAs in attenuating oxidative stress by reducing oxidative stress-induced DNA damage in vascular endothelial cells, reducing intracellular ROS and increasing the mRNA levels of antioxidant molecules, such as heme oxygenase-1, thioredoxin reductase-1, and superoxide dismutase [140]. Supplementation with n-3 fatty acids has also been shown to reduce plasma F2-isoprostanes levels [141].
In spite of some evidence regarding the antioxidant properties of omega-3 PUFAs, it should be noted that both omega-3 and omega-6 PUFAs are chemically susceptible to oxidation and are major sites of oxidative attack in vivo due to their relatively large number of double bonds and the position of these bonds within their structure [142]. Oxidative modifications to omega-3 and omega-6 PUFAs result in the formation of lipid oxidation products (LOPs), including 4-hydroxyhexenal (4-HHE), and 4-hydroxynonenal (4-HNE), respectively [143]. Furthermore, oxidation of the omega-6 linoleic acids content of LDL-C during oxidation processes produces potent pro-oxidants such as 9-hydroxy-10,12-octadecadienoic acid (9-HODE) [144].
7.2.5. Dietary Glycaemic Index
Dietary glycaemic index (GI) is a ranking of various carbohydrates according to the extent to which they raise plasma glucose levels after ingestion [145]. Consumption of foods with higher GI can contribute to either an acute or chronic elevation of plasma glucose, i.e., hyperglycaemia, which plays a significant role in developing oxidative stress and inflammation [146,147,148]. Hyperglycaemia induces oxidative stress and inflammatory processes via several well-known mechanisms, including high generation of superoxide anion by the mitochondria [149], glycation of antioxidant enzymes such as thioredoxin [150], activation of the polyol pathway, reducing plasma levels of NAD+ [151], activation of NF-κB [152], activation of protein kinase C [153], and increasing intracellular formation of the pro-oxidants such as advanced glycation end products (AGE) [154].
Several studies have shown the positive association between dietary GI assessed by a food frequency questionnaire during a 12-month period and plasma and urinary lipid peroxidation biomarkers of MDA and isoprostanes in healthy cohorts [147]. In healthy subjects after ingesting foods with different GI values, levels of the oxidative stress biomarker nitro-tyrosine and the activation of pro-inflammatory gene NF-κB were significantly higher in subjects in the high GI group compared to subjects in the low GI group [146]. Studies in diabetic subjects have also shown the effect of meals with high GI values on increasing plasma levels of MDA [151], CRP and TNF- α [155], and also raising LDL-C susceptibility to oxidation, as well as reducing total radical-trapping antioxidant parameter (TRAP) [151].
7.2.6. Fruits and Vegetables
As rich sources of various antioxidants and vitamins (e.g., vitamin C and E), and a wide range of bioactive compounds known as phytochemicals (e.g., carotenoids), fruits and vegetables have long been recognised for their antioxidant and anti-inflammatory properties [156,157,158]. In this regard, several studies have shown the effects of high intakes of fruit and vegetables on reducing levels of oxidative stress and inflammatory biomarkers such as MDA [159], 8- isoprostane F2α [160], oxidised LDL-C [161], 8OHdG [162], CRP, interleukin receptor 1 (ILR1), IL6, and TNF-α [163]. In addition, consumption of a variety of fruits and vegetables has been reported to increase plasma and tissue levels of vitamin C and E, and also carotenoids such as lutein, zeaxanthin, α-carotene, β -carotene and lycopene, leading to a significant increase in plasma total antioxidant capacity (TAC) [164,165].
As lipid-soluble phytochemicals, carotenoids can also locate within biological membranes, and consequently, play a critical role in protecting cellular membranes as well as lipoproteins against damage by peroxyl free radicals [166,167]. It has also been shown that the intake of lycopene-rich vegetable products can prevent lipid peroxidation as indicated by decreased urinary F2-isoprostane and reduced LDL-C susceptibility to oxidation [168]. Furthermore, the intake of vitamins such as C and E from dietary sources including fruits, vegetables, nuts and seeds is negatively associated with plasma levels of oxidative stress biomarkers such as 8-isoprostane F2α and 8-oxo-7,8-dihydroguanine [169].
7.2.7. Nutrient-Poor Foods
It is now widely promoted that a combination of dietary components can be more strongly associated with an inflammatory and oxidative stress profile than any single component considered individually [28]. Hence, the role of foods with complex matrices should also be taken into account in this context. Processed foods lacking nutrient density such as fast foods and sugar-sweetened soft drinks can still have a multifarious matrix rich in saturated and trans fatty acids, omega-6 PUFAs, sugar, and AGEs, which as mentioned previously, can all trigger the inflammatory response with consequent oxidative stress and cell damage [170]. In addition to increased oxidative damage regular consumption of these nutrient-poor foods can also lead to deficiencies in major micronutrients such as vitamins A, E, D, zinc and selenium which can weaken the body’s innate biochemical capability to neutralise the generated free radicals [171].
7.3. Common Social Drug Use
7.3.1. Alcohol Intake
Alcohol is mainly metabolised into acetaldehyde by alcohol dehydrogenase in the liver [172]. However, it can also be metabolised by activation of the 2E1 isoform of the cytochrome P450 (CYP2E1) oxidase system which is induced during chronic alcohol consumption [173]. This process can lead to the generation of ROS and highly reactive free radicals including hydroxyl radicals and superoxide anions [174]. Chronic alcohol intake can cause hepatic accumulation of the hydroxyethyl radical and MDA, and deplete the cellular antioxidant glutathione (GSH) levels in rats [175]. Further studies in animals have revealed that high ethanol intake can increase liver 8-oxoguanine [176], and urinary 8-iso prostaglandin-F2α [177]. Studies in humans have shown that alcohol consumption in heavy alcohol drinkers can increase plasma levels of oxidised LDL-C [178], advanced glyoxidation end products (AGE) [179] and acetaldehyde-protein adducts, all of which are potent oxidants [180]. While high intakes of alcohol are consistently linked to wide spread tissue damage, a recent study by our group observed that chronic alcohol intakes equivalent to only 1–2 standard drinks a day were associated with a reduction in levels of total NAD(H), a recognised marker of intracellular metabolic and redox status, and an increase in levels of the inflammatory cytokine IL-6 in human cerebrospinal fluid (CSF) [181].
7.3.2. Caffeine Intake
Caffeine (1,3,7-trimethylxanthine) is an alkaloid present in varying concentrations in coffee, tea, colas, energy drinks and chocolate [182,183]. While crude caffeine extract has been shown to possess limited lipophilic and hydrophilic antioxidant and cyclooxygenase-2 inhibitory activity, pure caffeine, appears to possess none of these attributes [184]. There is evidence that caffeine ingestion can increase lipid oxidation [185], enhance exercise-induced lipid peroxidation, indicated by plasma MDA and decrease plasma TAC levels in young men [186]. Furthermore, prenatal exposure to caffeinated energy drinks has been shown to induce oxidative stress and to increase lipid peroxidation in the liver, kidney and brain of newborn mice [187]. Caffeine, in either low or high concentrations has been reported to be significantly associated with a proinflammatory cytokine profile with elevated plasma levels of TNF-α, CRP [188], IL-1β [189], IL- 6, serum amyloid-A (SAA) [188], and soluble vascular cell adhesion molecule-1 (sVCAM-1) [190], and decreased serum levels of the anti-inflammatory cytokine IL-10 [189]. It has been suggested that caffeine produces these effects by inducing the expression of toll-like receptor 4 (TLR-4) and activating NF-κB pathways that increase the expression of inflammatory molecules [191,192].
7.3.3. Cigarette Smoking
As a typical example of an oxidative stress-inducing compound, cigarette smoke contains more than 4000 different chemicals including oxidants and free radicals, many of which have established harmful effects [193]. Not surprisingly, cigarette smoking not only delivers oxidants and free radicals to the body, but also induces pro-inflammatory signalling via activation of NF-κB, which can exacerbate oxidative stress [194]. Not surprisingly therefore, smoking has been shown to be associated with high plasma levels of oxidative stress biomarkers such as oxidised LDL and isoprostane, and inflammatory biomarkers such as IL-1β, IL-6, IL-8, hs-CRP and soluble adhesion molecules [195].
7.4. Physical Activity
Emerging evidence suggests that regular physical activity, especially endurance training, can elevate antioxidant and anti-inflammatory biomarkers levels in the vasculature, the skeletal muscle and the circulation by various mechanisms [196,197]. Acute exercise causes a transient increase in ROS levels, providing the required stimulus for activating the antioxidant defence system. However, during chronic exercise this situation can be compensated for by upregulating antioxidant enzymes and thus, reducing the impact of free radicals production across the day [198]. In this context, several studies in animals and humans have shown that chronic exercise can increase serum total antioxidant status (TAS) [199], and antioxidant enzymes such as glutathione peroxidase [200] and haem oxygenase-1 (HO-1) [201] and reduce the levels of serum oxidative stress biomarkers, F2-isoprostanes [202], and MDA [196]. Regular exercise has also been shown to be associated with lower levels of several proinflammatory cytokines including interferon-γ (IFN-γ), IL-1β [203], CRP [204], IL-6 [202], IL-1β and TNF-α, and higher levels of anti-inflammatory molecules such as IL-4, IL-10, and transforming growth factor-β (TGF-β) [205].
7.5. Sleep and Tissue Oxygenation
It has been hypothesised that “good sleep” represents a state in which anti-oxidant potential is increased thereby improving the removal of free radicals generated during waking hours [206,207]. Experiments support the assertion that long-lasting wakefulness and sleep deprivation are associated with elevated oxidative damage and inflammation [208,209]. Increased levels of lipid peroxidation biomarkers such as myeloperoxidase-modified LDL-C [208], reduced levels of antioxidant enzymes such as glutathione peroxidase, catalase, and superoxide dismutase [210], and elevated production of pro-inflammatory molecules including IL-1β, IL-6, IL-17 [211] and high sensitivity C-reactive protein (hs-CRP) [212] have been reported in several animal and human studies.
One of the most common sleep-related disorders that represent a key public health problem is obstructive sleep apnoea (OSA). OSA is defined by repetitive episodes of upper airway collapse during sleep resulting in nocturnal intermittent hypoxia with the consequent induction of oxidative stress [213,214]. In this context, experiments in patients with OSA have revealed excessive superoxide radical production from leukocytes [215] and reduced bioavailability of nitric oxide (NO) the main endothelial-derived vasodilator linked to oxidative stress [216]. Furthermore, increased serum concentrations of TBARs [217] and exhaled breath 8-isoprostane [216], increased urinary 8-OHdG [218], and higher plasma advanced oxidation protein products [219] have been reported. There is also evidence for decreased plasma total antioxidant status (TAS), vitamin A and E [220], and reduced plasma levels of antioxidant enzyme, superoxide dismutase [221], and paraoxonase-1 [217] in OSA. Several studies have also suggested that the intermittent hypoxia in OSA can stimulate inflammatory pathways [222]. In this context, OSA patients have shown increased plasma levels of TNF-α, and IL-8 consistent with the extent of hypoxia during sleep [223].
7.6. Psychological Factors (Stress, Anxiety and Depression)
Mild anxiety is a normal response to psychological stress. However, when such responses become extreme and persistent, it is considered pathologic and is referred to as anxiety disorder (AnxD) [224]. AnxDs are implicated in a number of psychiatric disorders, in particular depression [225]. It is well known that oxidative stress and inflammation play a major role in both initiation and progression of these diseases [226,227]. Elevated plasma levels of ROS [228,229] and oxidative stress biomarkers such as MDA [230], 8- iso-prostaglandin F2 [231], and 8-OHdG [232] are important features of AnxD and major depression. Furthermore, studies have also reported decreased plasma TAC [233], reduced activity of antioxidant enzymes such as glyoxalase 1 (GLO1) [234] and reduced plasma levels of antioxidants such as vitamin E [235], GSH [236] and coenzyme Q10 [237] in these disorders.
Anxiety and depression are also accompanied by an increased inflammatory profile as indicated by elevated serum levels of a variety of pro-inflammatory cytokines such as IL-6 [231], TNF-α [233] and CRP [238]. There is also evidence for the induction of inflammatory enzymes such as indoleamine 2,3-dioxygenase (IDO), a rate-limiting enzyme for the metabolism of tryptophan via the kynurenine pathway [239,240]. Increased catabolism of tryptophan by IDO can lead to depletion of antioxidants like tryptophan and its metabolite serotonin (5-hydroxy tryptophan), and also increased synthesis of the pro-oxidant tryptophan catabolites (TRYCATs), quinolinic acid and kynurenine [241].
A model that develops from these observations suggests that unhealthy lifestyle behaviours trigger increased oxidative activity (via several sources, including inflammation) leading to an often-chronic state of redox imbalance (oxidative stress) that gradually shifts the body’s biochemistry toward a diseased phenotype. If unhealthy lifestyle behaviours persist, the resulting biochemical adaptation will, over a period of time, drive the body to a state of disease [242,243,244] (Figure 3).
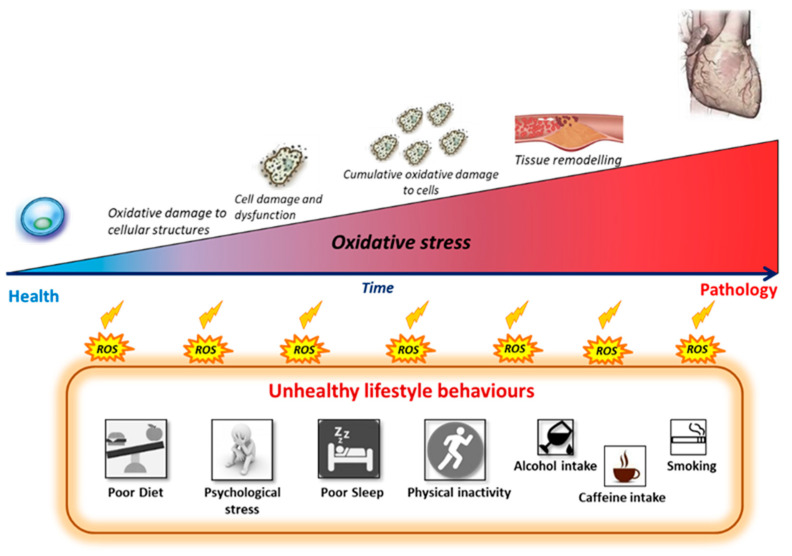
Figure 3.
Progressive oxidative damage processes induced by chronic exposure to unhealthy lifestyle behaviours. Adherence to unhealthy lifestyle behaviours can gradually shift the body’s redox balance toward a state of oxidative stress with chronic subclinical damage to cells, tissues and organs. Oxidative damage plays a major role in the onset and development of non-communicable disease such as cardiovascular disease. ROS: Reactive oxygen species.
8. Evidence that Changes in Lifestyle-Linked Oxidative Stress Is Detectable in Disease-Free Humans
As mentioned, several studies have shown significant associations between either individual lifestyle behaviours or composite lifestyle scores, and oxidative stress and inflammatory biomarkers and risk of various NCDs such as CVDs [31,32,242,245,246,247,248]. However, though oxidative stress and inflammation have been demonstrated clearly in the presence of disease, there are currently limited data showing a relationship between lifestyle behaviours, subclinical changes in oxidative stress and inflammatory biomarkers and changes in classic disease markers during the stage where no clinical symptoms of disease are present. In other words, few studies have investigated whether changes in oxidative stress and inflammatory biomarkers are observable in otherwise healthy persons in which “unfavourable” lifestyle behaviours are nonetheless present. Even though some authors have suggested the measurement of oxidative stress and inflammatory biomarkers be included in routine analysis performed in clinical laboratories [249,250,251,252,253,254], they were generally focused on disease management, and methodological aspects, rather than disease prevention. In addition, they provided no link to lifestyle behaviours as the main underlying cause of disease. Hence, additional work is required to further develop the concept and identify the potential benefits of monitoring levels of oxidative stress and inflammatory biomarkers both in terms of its value to early identification of NCD pathologies and its link to multiple lifestyle behaviours in apparently healthy individuals.
Among the few studies available in this context, results from our research group have shown that lifestyle-associated changes in oxidative stress and/or inflammatory biomarkers can indeed be detectable even in humans with no clinical symptoms of disease [255]. Thus, indicating that changes in oxidative inflammatory activity may be present during the prodromal or developmental phase of the disease process. In this study, we showed that a simple measure of redox balance, the ratio of total antioxidant capacity to hydroperoxide ratio (TAC/HPX ratio), was sensitive enough to be significantly associated with lifestyle behaviours including body fat percentage, sleep quality, sleep apnoea, depression and dietary intakes of red meat and caffeine, in healthy humans [255]. Lipid hydroperoxide (HPX) has been shown to be a reasonably stable, ubiquitous and sensitive by-product of lipid peroxidation [249,256,257]. Due to their propensity to contain double bonds, membrane-associated lipids appear to be very vulnerable to free radical insults, and thus biomarkers associated with lipid peroxidation have been shown to be more sensitive than other markers such as protein oxidation products [258]. The coupling of HPX with a measure of total antioxidant capacity (TAC), an integrated measure of all antioxidants present in plasma [259], provides an index of the degree of ongoing free radical damage, relative to available antioxidant resources, as it relates to the plasma. Thus, the TAC/HPX ratio provided an added degree of sensitivity in detecting an otherwise healthy individual’s specific changes in redox balance in response to their set of lifestyle challenges [255].
Importantly, these findings also showed that the plasma redox potential could have clinical relevance as the TAC/HPX ratio was independently associated with NCD risk and changes in classic CVD risk markers such as LDL-C, total cholesterol and fasting plasma glucose (FPG) [255]. Similar relationships had been previously reported by Brunelli et al. (2017) who showed that plasma antioxidant capacity was significantly associated with traditional cardiovascular risk factors, including total cholesterol and total cholesterol to HDL-C ratio, in a healthy population [260].
Using an otherwise healthy cohort, we also observed that the TAC/HPX ratio was associated with the Framingham risk score (FRS), an established CVD risk predictor, which was independent of the conventional CVD risk markers such as LDL-C, HDL-C and blood pressure [255]. This association is consistent with earlier reports in which FRS was associated with other serum oxidative stress-linked biomarkers such as peroxiredoxin [261], γ-glutamyltransferase (GGT) [262], bilirubin [263], glutathione redox state [56], oxidised disulphide cysteine [264], oxidised phospholipids [265], oxidised LDL [266], 9-hydroxy eicosatetraenoic acids, and F2-isoprostanes [57]. Collectively, these data suggested that changes in plasma redox balance, especially in the preclinical stage when the person is assumed to be healthy, may reflect an individual’s early biochemical shift toward disease. However, information from future longitudinal studies that include a comprehensive range of inflammatory and oxidative markers will be needed to verify this hypothesis.
As previously outlined, lifestyle behaviours are recognised as major factors influencing the subclinical risk indicators of NCDs such as CVD changes in carotid intima-media thickness (CIMT) in the general population [267,268,269]. The critical role of oxidative stress and inflammatory processes in the development of vascular abnormalities and increased CIMT has been established in several studies in clinical cohorts [18,270]. Interestingly, the results from the same healthy cohort in our lab also showed that the collage of lifestyle behaviours could link to increased risk of CIMT independent of conventional CVD risk markers. In other words, changes in an integrated measure of lifestyle behaviours were shown to be strongly associated with changes in CIMT and at the same time with plasma biomarkers of redox balance and oxidative stress [271]. As this measure of lifestyle behaviours was also associated with oxidative stress processes in our cohort with no clinical signs of disease, it can be inferred that oxidative stress may play an independent role in the initiation of subclinical abnormalities involved in the development of CVD. Therefore, relying on conventional biomarkers such as LDL-C to estimate the risk of disease without considering the redox state might not be sensitive enough to identify the actual risk of developing disease for individuals whose redox state is responding poorly to their constellation of lifestyle behaviours. These findings are consistent with results of other studies that reported independent associations between oxidative stress and CIMT in disease-free individuals [18,56].
9. Clinical Application of Monitoring Oxidative Stress and Inflammation
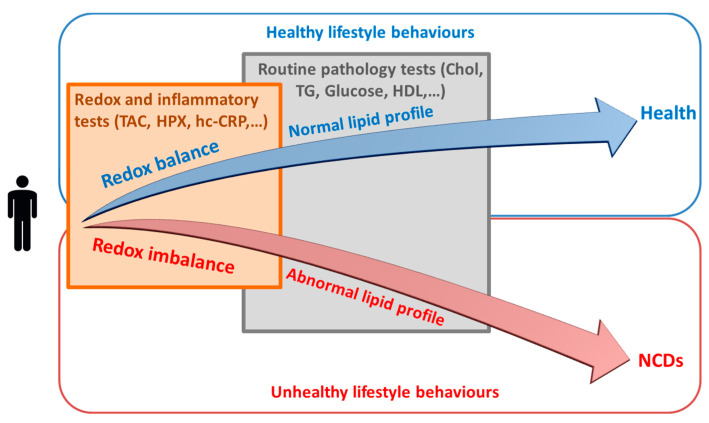
Collectively, current available evidence suggests that, oxidative stress and inflammatory pathways represents a sensitive shared molecular pathway between various lifestyle behaviours through which these behaviours may gradually drive an individual’s biochemistry/physiology toward a state of developing disease. Consistent with this hypothesis there is a developing body of evidence showing that oxidative stress-associated changes are detectable in apparently healthy individuals in association with specific lifestyle behaviours [255,271]. Thus, the measurement of biomarkers associated with oxidative stress (and inflammation), may help with predicting early shifts toward the development of NCDs and hence may enhance the ability to correctly characterise an individual’s disease trajectory. Therefore, monitoring oxidative stress and inflammatory biomarkers and/or including a measure of oxidative stress and inflammation in any risk assessment tool may provide an early and more direct assessment of the presence of damage processes that go beyond the conventional downstream risk factors currently used for predicting disease risk. An appropriate clinical application of this concept is that it may provide an early indication of whether an individual’s biochemistry is driving him/her toward health or disease (Figure 4). On-time distinction of this trajectory can enable the initiation of appropriate modifications (mainly lifestyle-related) and assist with a better health outcome in terms of prevention of chronic NCDs.
Figure 4.
Assessment of redox state (i.e., assessment of the degree to which oxidative stress is present) as a possible approach for early distinction of whether various lifestyle behaviours are driving an individual toward health or toward development of disease-related pathologies. NCDs: non-communicable diseases; TAC: total antioxidant capacity; HPX: lipid hydroperoxides; hc-CRP: high sensitivity C-reactive protein; Chol: cholesterol; TG: triglycerides; HDL: high density lipoprotein.
This may have some enhanced discriminating capacity for those at risk of disease as it will identify individuals whose biochemistry is not responding well to their collage of lifestyle choices and therefore are in the process of developing an NCD. Assessing NCD risk using (or at least including) oxidative stress and inflammatory markers is therefore increasing the focus on upstream causative metabolic processes rather than the less specific downstream risk factors such as body weight and lipid levels.
It is relevant to reiterate that a condition of oxidative stress and inflammation is not a diseased state but is rather a preclinical state representing significant cellular stress and damage [18,56,264,272]. The information and perspective presented in this paper supports the view that this state can be produced as a result of chronic exposure to various unhealthy lifestyle behaviours. The damage caused by oxidative stress and inflammation, if not detected early and prevented, can accumulate over time causing serious tissue remodelling that will eventually result in a diseased phenotype [15,16,242]. Therefore, the assessment of redox state during the early stage when no clinical symptoms of disease are manifest can assist with identifying an individual’s early biochemical shifts toward development of disease. In this way, the ongoing tissue damage due to chronic oxidative stress and inflammation can be reduced or even halted by early modification strategies such as lifestyle changes. This will prevent or limit development of irreversible organ damage and subsequent disease. Improving the course of preclinical disease in this way not only can provide improved patient outcomes but also can reverse disease progression and, therefore, reduce both the need and costs of ongoing healthcare.
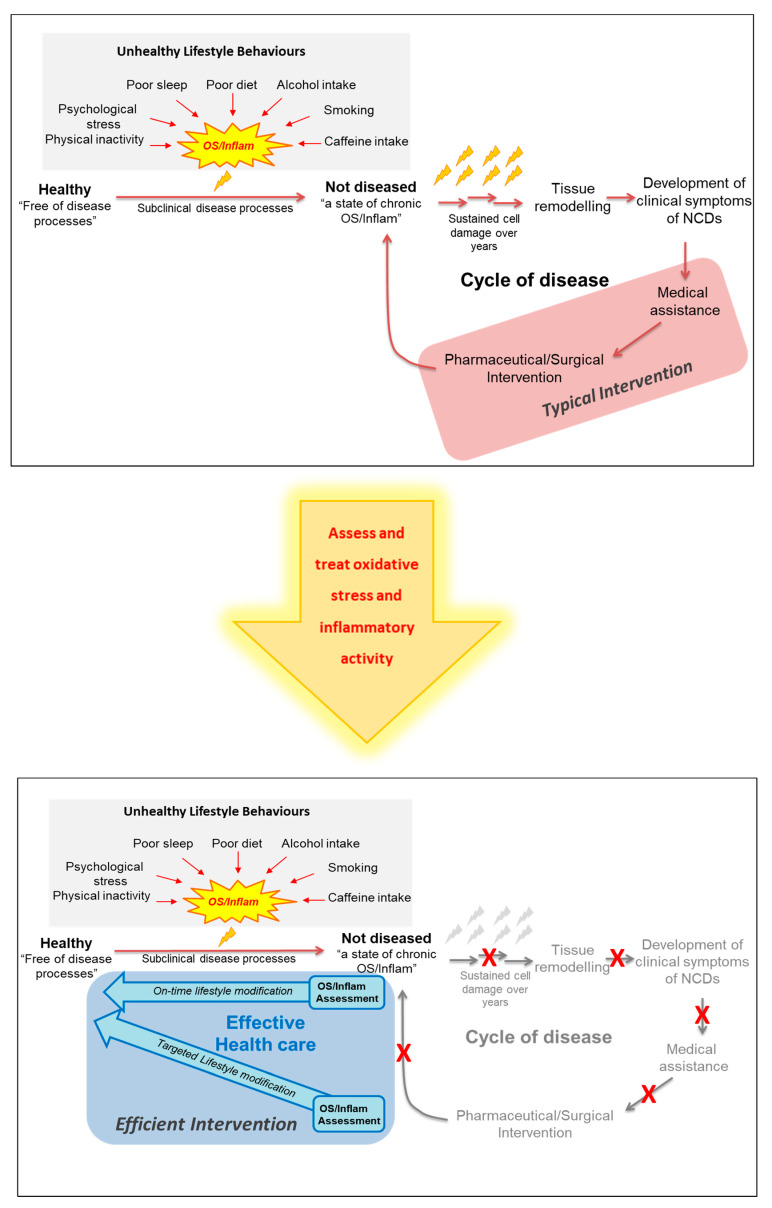
When fully developed, this approach may offer a way to bridge the gap between the preventive aims of population-based public health strategies and the therapeutic goals of patient-centred clinical practices to more favourably address individuals wellness needs (Figure 5).
Figure 5.
A suggested model for a more effective approach to treatment/prevention of the non-communicable diseases. NCDs: non-communicable disease; OS: oxidative stress; Inflam: Inflammation.
10. Monitoring Oxidative Stress and Inflammation
As mentioned, our research group previously reported that different lifestyle behaviours are associated with changes to the oxidative stress biomarkers TAC/HPX which were detectable in a human cohort with no clinical symptoms of disease [255]. In addition we showed that changes in redox balance (based on lifestyle) correlated with the TAC/HPX biomarkers and with changes in the CVD risk factor CIMT [271]. These observations are consistent with the hypothesis that OS/inflammatory markers are early indicators of developing NCDs and if monitored, can enable effective treatment strategies in the preclinical disease phase before irreparable tissue damage occurs.
Unfortunately, a clinically validated and universally accepted profile of oxidative stress (and to some extent inflammatory) biomarkers has not yet been established in the clinical context. However, a wide variety of biomarkers and analytical methods have been developed to measure oxidative stress and inflammation in the research and clinical arenas. While there are popular clinical markers of inflammation (e.g., hsCRP) clinically validated markers of oxidative stress are still not apparent. As a general recommendation, any analytical method for measuring OS and inflammation should be accurate, sensitive, specific, reproducible, and interference-free [273]. Furthermore, to promote their use in clinical settings, the methods should be based on a simple and quick protocol, and involve low cost. Considering the highly reactive nature of oxidative species and their short half-life, this is a formidable challenge and care needs to be taken to ensure the stability of the sample to avoid artefactual oxidation. Suitable analytes must be able to be stabilised in the clinical environment, present in quantifiable concentrations and measurable within the detection range of a reliable analytical method across populations, allowing the establishment of reference values. The analyte should also ideally be a specific and major product of oxidative/nitrosative damage [273,274]. To our knowledge, no individual oxidative stress biomarker meets all of these technical requirements. However, some are better than others and a select panel of currently available markers will likely provide the most clinically useful information [274]. While it is recognised that further development in this area is needed, we have listed a selected range of biomarkers used for detecting oxidative stress and inflammation that are adaptable to the clinical environment (Table 1 and Table 2) [252,275,276,277,278,279,280,281,282,283,284,285,286,287,288,289]. With careful selection of markers and consideration of the points mentioned above, erroneous interpretations can be minimised and an accurate profile of an individual’s biochemical redox health status should be obtainable and able to be applied to the (pre)clinical setting.
Table 1.
Potential biomarkers of oxidative stress (OS).
| OS Marker | Advantages | Disadvantages | Reference |
|---|---|---|---|
| IsoPros | Can be detected in various samples (serum, plasma urine) and has been shown to be elevated in the presence of a range of cardiovascular risk factors and cancer | Evidence in clinical disease still developing. Test available in specialist labs only | [275] |
| MDA | Easy to quantify in serum, plasma or urine. Studies show MDA can predict progression of coronary artery disease and carotid atherosclerosis at 3 years. | TBARS assay is non-specific (can detect aldehydes other than MDA) therefore potential for interferences. Test available in specialist labs only. | [252] |
| Hydroperoxides (HPX) | Lipid hydroperoxides are non-radical intermediates of lipid peroxidation. If frozen on collection, relatively stable in serum/plasma and can be transported. Growing body of evidence for correlation with clinical disease. Commercial test kits available | Can undergo reductive degradation if not stored properly which will decrease levels. | [276] |
| Nitrotyrosine | Human studies have demonstrated association with coronary artery disease independent of traditional risk factors | Circulating levels not equivalent to tissue levels. Current detection methods are expensive and impractical for scaling up to the clinical setting. | [277] |
| MPO | Measured in serum or plasma. Commercial assays available. Strong evidence that MPO correlates with cardiovascular disease risk | Influenced by sample storage and time to analysis. Test available in specialist labs only. | [278] |
| oxLDL | Serum or plasma levels routinely available as a clinical marker in many larger routine pathology labs. Elevated in coronary artery disease, increasing oxLDL correlates with increasing clinical severity. Also is predictive of future coronary artery disease in healthy population. Good reproducibility from frozen samples | Ox LDL has been studied mostly in relation to CVD so results not generalisable to other NCDs at this stage | [279] |
| Total antioxidant capacity (TAC) | Plasma levels considered a good measure of the activity of the low molecular weight, antioxidants, including albumin, Vitamin C, SH group containing antioxidants (glutathione), polyphenolic and carotenoid compounds and bilirubin. Has been correlated to a variety of disease states. Commercial testing kits available | The specific contribution of antioxidant enzymes such as catalase and SOD are excluded | [280] |
| Gene expression | The change in expression of various genes may reflect altered redox balance and can be measured simultaneously using microarray technology | Expensive and It is unclear if expression profiles of cells in biological samples reflect that in clinical tissues. Test only available form specialist labs | [281] |
Abbreviations: IsoPros (F2 Isoprostanes), MDA (malondialdehyde), HPX (hydroperoxide), MPO (myeloperoxiodase), oxLDL (oxidised low density lipoprotein).
Table 2.
Potential biomarkers of inflammation.
| Inflammation Linked Marker | Description/Advantage | Disadvantages | Reference |
|---|---|---|---|
| IL-6 | Early release pro-inflammatory cytokine produced in response to infections and tissue injuries | Half life of 10 min. Therefore, only elevated during active inflammatory activity. Can also have anti-inflammatory effects. Test only available in specialist labs |
[282] |
| TNF-α | Pro-inflammatory cytokine produced by macrophages and lymphocytes | Half life of 18 min. Therefore, only elevated during active inflammatory activity. Test only available in specialist labs | [282] |
| IL-1β | Pro-inflammatory cytokine and lymphocyte/monocyte activating factor | Half life of <4 h. Therefore, only elevated during active inflammatory activity. Test only available in specialist labs | [282] |
| IL-8 | Pro-inflammatory cytokine produced by polymorphonuclear (PMN) cells | Half life of ~4 h. Therefore, only elevated during active inflammation due largely to bacterial infections. Test only available in specialist labs |
[282] |
| IL-10, IL-4 | Anti-inflammatory cytokines. IL-4 produced by activated T cells, mast cells, basophils, eosinophils, and Natural killer T cells. IL-10 produced by macrophages, dendritic cells (DC),3 B cells, and various subsets of CD4+ and CD8+ T cells |
Half life of <4.5 h. Therefore, only elevated during active inflammatory activity. Test only available in specialist labs | [282] |
| Fibrinogen | Pro-inflammatory regulation. High levels well documented risk for many inflammatory conditions. Test routinely available in pathology labs | The mechanistic links between coagulation and inflammation involving fibrinogen activation and signalling are not yet fully known | [283] |
| Alb/Glob ratio | Decreased in inflammation. Sensitive indicator of inflammatory disease, in particular kidney disease. Test available in routine pathology labs | Ratio may change for reasons other than inflammation, e.g., nutritional deficiencies such as low protein intakes | [284,285] |
| Tryp/Kyn ratio | Sensitive indicator of T-helper 1 (i.e., IFN-γ) immune responses. Reduced ratio reported in a range of inflammatory associated conditions including aging, cancer, rheumatoid arthritis and CVD. Altered Kyn:Tryp ratio remains longer and fluctuates less than individual cytokines. | Test not routinely available outside of research labs | [286] |
| Neopterin | Macrophage activation product dependent on IFN-γ activation. Levels remain elevated for longer after IFN-γ levels return to normal. | Produced secondary to IFN-γ activation of macrophages. Test only available in specialist labs. | [287] |
| hs-CRP | Acute phase protein produced by liver following IL-6 activation. Widely used as a clinical marker of inflammation. Levels remain elevated longer than IL-6 and other cytokines. Test widely available in routine pathology labs. | As an acute phase protein levels rise by 2 h peak by 48 h. Half life 18 h. However, one of the 2 isoforms of CRP may have anti-inflammatory effects | [288] |
| Omega-3 Index/ratio | Primary ant-inflammatory modulators. Large body of evidence linking reduced omega-3 levels to conditions associated with chronic inflammation including rheumatoid arthritis, CAD and depression. | Indirect marker of inflammation potential. Test only available in specialist labs | [289] |
Abbreviations: IL-6 (interleukin-6), TNF-α (tumour necrosis factor alpha), IL-1β (interleukin 1-bets), IL-8 (interleukin 8), IL-10, IL-4 (interleukin 10 and interleukin 4), Alb/Glob ratio (albumin:globulin ratio), Tryp/Kyn ratio (tryptophan:kynurnein ratio), hs-CRP (high sensitivity C-Reactive protein), CVD (cardiovascular disease).
11. Conclusions
Current literature supports the view that lifestyle-induced oxidative stress and inflammation are primary drivers of metabolic imbalances that cause NCDs. Oxidative stress and inflammation produce a preclinical state of progressive tissue damage that, if continued, will result in selected system failures and accompanying disease. Effective management or prevention of the chronic subclinical tissue damage may be possible if levels of the relevant oxidative stress and inflammatory biomarkers are quantified and monitored and their link to an individual’s unique set of lifestyle behaviours are identified. The construction of such a wellness assessment profile would serve as an early alarm for the apparently healthy individual who is on a path to disease. This assessment of oxidative and inflammatory markers could also provide a baseline from which the success of any intervention can be monitored. Such a modified clinical approach has the potential to improve the effectiveness of current public health strategies to both prevent and reverse NCDs and their accompanying economic burden.
Acknowledgments
This works is funded by internal funding from the Australasian Research Institute.
Author Contributions
Conceptualisation, N.S., R.G.; writing—original draft preparation, N.S., R.G.; writing—review and editing, N.S., R.G.; funding acquisition, R.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kvaavik E., Batty G.D., Ursin G., Huxley R., Gale C.R. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: The United Kingdom Health and Lifestyle Survey. Arch. Intern. Med. 2010;170:711–718. doi: 10.1001/archinternmed.2010.76. [DOI] [PubMed] [Google Scholar]
- 2.WHO . Non Communicable Diseases Progress Monitor 2017. World Health Organization; Geneva, Switzerland: 2017. [Google Scholar]
- 3.Lim S.S., Vos T., Flaxman A.D., Danaei G., Shibuya K., Adair-Rohani H., Amann M., Anderson H.R., Andrews K.G., Aryee M., et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naghavi M., Wang H., Lozano R., Davis A., Liang X., Zhou M., Vollset S.E., Abbasoglu Ozgoren A., Abdalla S., Abd-Allah F., et al. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palotás A., Reis H.J., Bogáts G., Babik B., Racsmány M., Engvau L., Kecskeméti E., Juhász A., Vieira L.B., Teixeira A.L., et al. Coronary artery bypass surgery provokes alzheimer’s disease-like changes in the cerebrospinal fluid. J. Alzheimer’s Dis. 2010;21:1153–1164. doi: 10.3233/JAD-2010-100702. [DOI] [PubMed] [Google Scholar]
- 6.Ott A., Stolk R.P., Van Harskamp F., Pols H.A.P., Hofman A. Breteler MMB. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology. 1999;53:1937–1942. doi: 10.1212/WNL.53.9.1937. [DOI] [PubMed] [Google Scholar]
- 7.WHO . NCD Mortality and Morbidity. World Health Organization; Geneva, Switzerland: 2018. [(accessed on 8 October 2018)]. Available online: http://www.who.int/gho/ncd/mortality_morbidity/en/ [Google Scholar]
- 8.WHO . Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. World Health Organization; Geneva, Switzerland: 2013. [Google Scholar]
- 9.Bloom D.E.C.E., Jane-Llopis E., Abrahams-Gessel S., Bloom L.R., Fathima S., Feigl A.B., Gaziano T., Mowafi M., Pandya A., Prettner K., et al. The Global Economic Burden of Non-Communicable Diseases. World Economic Forum; Geneva, Switzerland: 2011. [Google Scholar]
- 10.Beard J.R., Officer A., De Carvalho I.A., Sadana R., Pot A.M., Michel J.P., Lloyd-Sherlock P., Epping-Jordan J.E., Peeters G.M.E.E., Mahanani W.R., et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet. 2016;387:2145–2154. doi: 10.1016/S0140-6736(15)00516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ford E.S., Bergmann M.M., Kröger J., Schienkiewitz A., Weikert C., Boeing H. Healthy living is the best revenge: Findings from the European prospective investigation into cancer and nutrition-potsdam study. Arch. Intern. Med. 2009;169:1355–1362. doi: 10.1001/archinternmed.2009.237. [DOI] [PubMed] [Google Scholar]
- 12.Siti H.N., Kamisah Y., Kamsiah J. The role of oxidative stress, antioxidants and vascular inflammation in cardiovascular disease (a review) Vasc. Pharmacol. 2015;71:40–56. doi: 10.1016/j.vph.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Devasagayam T.P.A., Tilak J.C., Boloor K.K., Sane K.S., Ghaskadbi S.S., Lele R.D. Free radicals and antioxidants in human health: Current status and future prospects. J. Assoc. Physicians India. 2004;52:794–804. [PubMed] [Google Scholar]
- 14.Khansari N., Shakiba Y., Mahmoudi M. Chronic inflammation and oxidative stress as a major cause of age-related diseases and cancer. Recent Pat. Inflamm. Allergy Drug Discov. 2009;3:73–80. doi: 10.2174/187221309787158371. [DOI] [PubMed] [Google Scholar]
- 15.Camps J., García-Heredia A. Introduction: Oxidation and inflammation, a molecular link between non-communicable diseases. Adv. Exp. Med. Biol. 2014;824:1–4. doi: 10.1007/978-3-319-07320-0_1. [DOI] [PubMed] [Google Scholar]
- 16.Peña-Oyarzun D., Bravo-Sagua R., Diaz-Vega A., Aleman L., Chiong M., Garcia L., Bambs C., Troncoso R., Cifuentes M., Morselli E., et al. Autophagy and oxidative stress in non-communicable diseases: A matter of the inflammatory state? Free Radic. Biol. Med. 2018;124:61–78. doi: 10.1016/j.freeradbiomed.2018.05.084. [DOI] [PubMed] [Google Scholar]
- 17.Halliwell B.G.J. Free Radicals in Biology and Disease. Volume 219. Oxford Science Pub.; Oxford, UK: 2007. pp. 21–23, 187–267. [Google Scholar]
- 18.Yoon J.H., Kim J.Y., Park J.K., Ko S.B. Oxidative damage markers are significantly associated with the carotid artery intima-media thickness after controlling for conventional risk factors of atherosclerosis in men. PLoS ONE. 2015;10:e0119731. doi: 10.1371/journal.pone.0119731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu J., Xia S., Kalionis B., Wan W., Sun T. The Role of Oxidative Stress and Inflammation in Cardiovascular Aging. BioMed Res. Int. 2014;2014:615312. doi: 10.1155/2014/615312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.D’Agostino R.B., Sr., Vasan R.S., Pencina M.J., Wolf P.A., Cobain M., Massaro J.M., Kannel W.B. General cardiovascular risk profile for use in primary care: The Framingham heart study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 21.Wilson P.W.F., D’Agostino R.B., Levy D., Belanger A.M., Silbershatz H., Kannel W.B. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.CIR.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 22.Roberts C.K., Barnard R.J. Effects of exercise and diet on chronic disease. J. Appl. Physiol. 2005;98:3–30. doi: 10.1152/japplphysiol.00852.2004. [DOI] [PubMed] [Google Scholar]
- 23.Lichtenstein P., Holm N.V., Verkasalo P.K., Iliadou A., Kaprio J., Koskenvuo M., Pukkala E., Skytthe A., Hemminki K. Environmental and heritable factors in the causation of cancer: Analyses of cohorts of twins from Sweden, Denmark, and Finland. New Engl. J. Med. 2000;343:78–85. doi: 10.1056/NEJM200007133430201. [DOI] [PubMed] [Google Scholar]
- 24.Katz D.L., Frates E.P., Bonnet J.P., Gupta S.K., Vartiainen E., Carmona R.H. Lifestyle as Medicine: The Case for a True Health Initiative. Am. J. Health Promot. 2018;32:1452–1458. doi: 10.1177/0890117117705949. [DOI] [PubMed] [Google Scholar]
- 25.Sagner M., Katz D., Egger G., Lianov L., Schulz K.H., Braman M., Behbod B., Phillips E., Dysinger W., Ornish D. Lifestyle medicine potential for reversing a world of chronic disease epidemics: From cell to community. Int. J. Clin. Pract. 2014;68:1289–1292. doi: 10.1111/ijcp.12509. [DOI] [PubMed] [Google Scholar]
- 26.King D.E., Mainous A.G., III, Geesey M.E. Turning Back the Clock: Adopting a Healthy Lifestyle in Middle Age. Am. J. Med. 2007;120:598–603. doi: 10.1016/j.amjmed.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 27.Kirkegaard H., Johnsen N.F., Christensen J., Frederiksen K., Overvad K., Tjønneland A. Association of adherence to lifestyle recommendations and risk of colorectal cancer: A prospective Danish cohort study. BMJ (Online) 2010;341:978. doi: 10.1136/bmj.c5504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsoukalas D., Sarandi E. Micronutrient deficiencies in patients with COVID-19: How metabolomics can contribute to their prevention and replenishment. BMJ Nutr. Prev. Health. 2020:1–2. doi: 10.1136/bmjnph-2020-000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lamichhane S., Kemppainen E., Trošt K., Siljander H., Hyöty H., Ilonen J., Toppari J., Veijola R., Hyötyläinen T., Knip M., et al. Circulating metabolites in progression to islet autoimmunity and type 1 diabetes. Diabetologia. 2019;62:2287–2297. doi: 10.1007/s00125-019-04980-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Margină D., Ungurianu A., Purdel C., Tsoukalas D., Sarandi E., Thanasoula M., Tekos F., Mesnage R., Kouretas D., Tsatsakis A. Chronic inflammation in the context of everyday life: Dietary changes as mitigating factors. Int. J. Environ. Res. Public Health. 2020;17:4135. doi: 10.3390/ijerph17114135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lakkur S., Bostick R.M., Roblin D., Ndirangu M., Okosun I., Annor F., Judd S., Dana Flanders W., Stevens V.L., Goodman M. Oxidative balance score and oxidative stress biomarkers in a study of Whites, African Americans, and African immigrants. Biomarkers. 2014;19:471–480. doi: 10.3109/1354750X.2014.937361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sotos-Prieto M., Bhupathiraju S.N., Falcon L.M., Gao X., Tucker K.L., Mattei J. Association between a Healthy Lifestyle Score and inflammatory markers among Puerto Rican adults. Nutr. Metab. Cardiovasc. Dis. 2016;26:178–184. doi: 10.1016/j.numecd.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang X., Devlin H.M., Smith B., Imperatore G., Thomas W., Lobelo F., Ali M.K., Norris K., Gruss S., Bardenheier B., et al. Effect of lifestyle interventions on cardiovascular risk factors among adults without impaired glucose tolerance or diabetes: A systematic review and metaanalysis. PLoS ONE. 2017;12:e0176436. doi: 10.1371/journal.pone.0176436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ramachandran A., Snehalatha C., Mary S., Mukesh B., Bhaskar A.D., Vijay V., Programme I.D.P. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1) Diabetologia. 2006;49:289–297. doi: 10.1007/s00125-005-0097-z. [DOI] [PubMed] [Google Scholar]
- 35.Anderson K.M., Odell P.M., Wilson P.W.F., Kannel W.B. Cardiovascular disease risk profiles. Am. Heart J. 1991;121:293–298. doi: 10.1016/0002-8703(91)90861-B. [DOI] [PubMed] [Google Scholar]
- 36.Goff D.C., Jr., Lloyd-Jones D.M., Bennett G., Coady S., D’Agostino R.B., Sr., Gibbons R., Greenland P., Lackland D.T., Levy D., O’Donnell C.J., et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American college of cardiology/American heart association task force on practice guidelines. J. Am. Coll. Cardiol. 2014;63:2935–2959. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deanfield J., Sattar N., Simpson I., Wood D., Bradbury K., Fox K., Boon N., Winocour P., Feher M., Doherty P., et al. Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3) Heart. 2014;100(Suppl. 2):ii1–ii67. doi: 10.1136/heartjnl-2014-305693. [DOI] [PubMed] [Google Scholar]
- 38.WHO . Prevention of Cardiovascular Disease: Guidelines for Assessment and Management of Total Cardiovascular Risk. World Health Organization; Geneva, Switzerland: 2007. [Google Scholar]
- 39.Conroy R.M., Pyörälä K., Fitzgerald A.P., Sans S., Menotti A., De Backer G., De Bacquer D., Ducimetière P., Jousilahti P., Keil U., et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 2003;24:987–1003. doi: 10.1016/S0195-668X(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 40.Bansal M., Kasliwal R.R., Trehan N. Comparative accuracy of different risk scores in assessing cardiovascular risk in Indians: A study in patients with first myocardial infarction. Indian Heart J. 2014;66:580–586. doi: 10.1016/j.ihj.2014.10.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Garg N., Muduli S.K., Kapoor A., Tewari S., Kumar S., Khanna R., Goel P.K. Comparison of different cardiovascular risk score calculators for cardiovascular risk prediction and guideline recommended statin uses. Indian Heart J. 2017;69:458–463. doi: 10.1016/j.ihj.2017.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bhopal R., Fischbacher C., Vartiainen E., Unwin N., White M., Alberti G. Predicted and observed cardiovascular disease in South Asians: Application of FINRISK, Framingham and SCORE models to Newcastle Heart Project data. J. Public Health. 2005;27:93–100. doi: 10.1093/pubmed/fdh202. [DOI] [PubMed] [Google Scholar]
- 43.Reissigová J., Zvárová J. The Framingham risk function underestimated absolute coronary heart disease risk in Czech men. Methods Inf. Med. 2007;46:43–49. [PubMed] [Google Scholar]
- 44.Otgontuya D., Oum S., Buckley B.S., Bonita R. Assessment of total cardiovascular risk using WHO/ISH risk prediction charts in three low and middle income countries in Asia. BMC Public Health. 2013;13:539. doi: 10.1186/1471-2458-13-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chung C.P., Oeser A., Avalos I., Raggi P., Stein C.M. Cardiovascular risk scores and the presence of subclinical coronary artery atherosclerosis in women with systemic lupus erythematosus. Lupus. 2006;15:562–569. doi: 10.1177/0961203306071870. [DOI] [PubMed] [Google Scholar]
- 46.Ernste F.C., Sánchez-Menéndez M., Wilton K.M., Crowson C.S., Matteson E.L., Maradit Kremers H. Cardiovascular risk profile at the onset of psoriatic arthritis: A population-based cohort study. Arthritis Care Res. 2015;67:1015–1021. doi: 10.1002/acr.22536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Law W., Johnson C., Rushton M., Dent S. The framingham risk score underestimates the risk of cardiovascular events in the HER2-positive breast cancer population. Curr. Oncol. 2017;24:e348–e353. doi: 10.3747/co.24.3684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Khanna R., Kapoor A., Kumar S., Tewari S., Garg N., Goel P.K. Metabolic syndrome & Framingham Risk Score: Observations from a coronary angiographic study in Indian patients. Indian J. Med Res. 2013;137:295–301. [PMC free article] [PubMed] [Google Scholar]
- 49.Huang H., Mai W., Liu D., Hao Y., Tao J., Dong Y. The oxidation ratio of LDL: A predictor for coronary artery disease. Dis. Markers. 2008;24:341–349. doi: 10.1155/2008/371314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chisolm G.M., Steinberg D. The oxidative modification hypothesis of atherogenesis: An overview. Free Radic. Biol. Med. 2000;28:1815–1826. doi: 10.1016/S0891-5849(00)00344-0. [DOI] [PubMed] [Google Scholar]
- 51.Steinberg D., Witztum J.L. Is the oxidative modification hypothesis relevant to human atherosclerosis? Do the antioxidant trials conducted to date refute the hypothesis? Circulation. 2002;105:2107–2111. doi: 10.1161/01.CIR.0000014762.06201.06. [DOI] [PubMed] [Google Scholar]
- 52.Navab M., Berliner J.A., Watson A.D., Hama S.Y., Territo M.C., Lusis A.J., Shih D.M., Van Lenten B.J., Frank J.S., Demer L.L., et al. The Yin and Yang of oxidation in the development of the fatty streak: A review based on the 1994 George Lyman Duff memorial lecture. Arterioscler. Thromb. Vasc. Biol. 1996;16:831–842. doi: 10.1161/01.ATV.16.7.831. [DOI] [PubMed] [Google Scholar]
- 53.Hulsmans M., Holvoet P. The vicious circle between oxidative stress and inflammation in atherosclerosis. J. Cell. Mol. Med. 2010;14:70–78. doi: 10.1111/j.1582-4934.2009.00978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Quinn M.T., Parthasarathy S., Fong L.G., Steinberg D. Oxidatively modified low density lipoproteins: A potential role in recruitment and retention of monocyte/macrophages during atherogenesis. Proc. Natl. Acad. Sci. USA. 1987;84:2995–2998. doi: 10.1073/pnas.84.9.2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schwarz A., Bonaterra G.A., Schwarzbach H., Kinscherf R. Oxidized LDL-induced JAB1 influences NF-κB independent inflammatory signaling in human macrophages during foam cell formation. J. Biomed. Sci. 2017;24:1–12. doi: 10.1186/s12929-017-0320-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ashfaq S., Abramson J.L., Jones D.P., Rhodes S.D., Weintraub W.S., Hooper W.C., Vaccarino V., Harrison D.G., Quyyumi A.A. The relationship between plasma levels of oxidized and reduced thiols and early atherosclerosis in healthy adults. J. Am. Coll. Cardiol. 2006;47:1005–1011. doi: 10.1016/j.jacc.2005.09.063. [DOI] [PubMed] [Google Scholar]
- 57.Shishehbor M.H., Zhang R., Medina H., Brennan M.L., Brennan D.M., Ellis S.G., Topol E.J., Hazen S.L. Systemic elevations of free radical oxidation products of arachidonic acid are associated with angiographic evidence of coronary artery disease. Free Radic. Biol. Med. 2006;41:1678–1683. doi: 10.1016/j.freeradbiomed.2006.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zakai N.A., Katz R., Jenny N.S., Psaty B.M., Reiner A.P., Schwartz S.M., Cushman M. Inflammation and hemostasis biomarkers and cardiovascular risk in the elderly: The Cardiovascular Health Study. J. Thromb. Haemost. 2007;5:1128–1135. doi: 10.1111/j.1538-7836.2007.02528.x. [DOI] [PubMed] [Google Scholar]
- 59.Yeboah J., McClelland R.L., Polonsky T.S., Burke G.L., Sibley C.T., O’Leary D., Carr J.J., Goff D.C., Jr. Greenland P, Herrington DM. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA J. Am. Med Assoc. 2012;308:788–795. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wilson P.W.F., Pencina M., Jacques P., Selhub J., D’Agostino R., O’Donnell C.J. C-reactive protein and reclassification of cardiovascular risk in the Framingham Heart Study. Circ. Cardiovasc. Qual. Outcomes. 2008;1:92–97. doi: 10.1161/CIRCOUTCOMES.108.831198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Harman D. Aging: A theory based on free radical and radiation chemistry. J. Gerontol. 1956;11:298–300. doi: 10.1093/geronj/11.3.298. [DOI] [PubMed] [Google Scholar]
- 62.Massudi H., Grant R., Braidy N., Guest J., Farnsworth B., Guillemin G.J. Age-associated changes in oxidative stress and NAD+ metabolism in human tissue. PLoS ONE. 2012;7:e42357. doi: 10.1371/journal.pone.0042357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Braidy N., Guillemin G.J., Mansour H., Chan-Ling T., Poljak A., Grant R. Age related changes in NAD+ metabolism oxidative stress and sirt1 activity in wistar rats. PLoS ONE. 2011;6:e19194. doi: 10.1371/journal.pone.0019194. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 64.Head E., Liu J., Hagen T.M., Muggenburg B.A., Milgram N.W., Ames B.N., Cotman C.W. Oxidative damage increases with age in a canine model of human brain aging. J. Neurochem. 2002;82:375–381. doi: 10.1046/j.1471-4159.2002.00969.x. [DOI] [PubMed] [Google Scholar]
- 65.Chen L., Deng H., Cui H., Fang J., Zuo Z., Deng J., Li Y., Wang X., Zhao L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2018;9:7204–7218. doi: 10.18632/oncotarget.23208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Closa D., Folch-Puy E. Oxygen free radicals and the systemic inflammatory response. IUBMB Life. 2004;56:185–191. doi: 10.1080/15216540410001701642. [DOI] [PubMed] [Google Scholar]
- 67.Janssen-Heininger Y.M.W., Mossman B.T., Heintz N.H., Forman H.J., Kalyanaraman B., Finkel T., Stamler J.S., Rhee S.G., van der Vliet A. Redox-based regulation of signal transduction: Principles, pitfalls, and promises. Free Radic. Biol. Med. 2008;45:1–17. doi: 10.1016/j.freeradbiomed.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xanthoulea S., Curfs D.M.J., Hofker M.H., De Winther M.P.J. Nuclear factor kappaB signaling in macrophage function and atherogenesis. Curr. Opin. Lipidol. 2005;16:536–542. doi: 10.1097/01.mol.0000180167.15820.ae. [DOI] [PubMed] [Google Scholar]
- 69.McDonald P.P., Bald A., Cassatella M.A. Activation of the NF-≃B pathway by inflammatory stimuli in human neutrophils. Blood. 1997;89:3421–3433. doi: 10.1182/blood.V89.9.3421. [DOI] [PubMed] [Google Scholar]
- 70.Duque G.A., Descoteaux A. Macrophage cytokines: Involvement in immunity and infectious diseases. Front. Immunol. 2014;5:491. doi: 10.3389/fimmu.2014.00491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Davies P., Bonney R.J., Humes J.L., Kuehl F.A. The role of macrophage secretory products in chronic inflammatory processes. J. Investig. Dermatol. 1980;74:292–296. doi: 10.1111/1523-1747.ep12543476. [DOI] [PubMed] [Google Scholar]
- 72.Eklund C.M. Chapter 5 Proinflammatory cytokines in CRP baseline regulation. Adv. Clin. Chem. 2009;48:111–136. doi: 10.1016/s0065-2423(09)48005-3. [DOI] [PubMed] [Google Scholar]
- 73.Helming L. Inflammation: Cell Recruitment versus local proliferation. Curr. Biol. 2011;21:R548–R550. doi: 10.1016/j.cub.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 74.Hold G.L., El-Omar E.M. Genetic aspects of inflammation and cancer. Biochem. J. 2008;410:225–235. doi: 10.1042/BJ20071341. [DOI] [PubMed] [Google Scholar]
- 75.Fenton H. Oxidation of tartaric acid in presence of iron. J. Chem. Sot. 1984;65:899–910. doi: 10.1039/CT8946500899. [DOI] [Google Scholar]
- 76.Cadenas E., Davies K.J.A. Mitochondrial free radical generation, oxidative stress, and aging. Free Radic. Biol. Med. 2000;29:222–230. doi: 10.1016/S0891-5849(00)00317-8. [DOI] [PubMed] [Google Scholar]
- 77.Ott M., Gogvadze V., Orrenius S., Zhivotovsky B. Mitochondria, oxidative stress and cell death. Apoptosis. 2007;12:913–922. doi: 10.1007/s10495-007-0756-2. [DOI] [PubMed] [Google Scholar]
- 78.Dansen T.B., Wirtz K.W.A. The peroxisome in oxidative stress. IUBMB Life. 2001;51:223–230. doi: 10.1080/152165401753311762. [DOI] [PubMed] [Google Scholar]
- 79.Johnson M.H., Nasresfahani M.H. Radical solutions and cultural problems: Could free oxygen radicals be responsible for the impaired development of preimplantation mammalian embryos in vitro? BioEssays. 1994;16:31–38. doi: 10.1002/bies.950160105. [DOI] [PubMed] [Google Scholar]
- 80.Cheng G., Cao Z., Xu X., Meir E.G.V., Lambeth J.D. Homologs of gp91phox: Cloning and tissue expression of Nox3, Nox4, and Nox5. Gene. 2001;269:131–140. doi: 10.1016/S0378-1119(01)00449-8. [DOI] [PubMed] [Google Scholar]
- 81.Albertolle M.E., Peter Guengerich F. The relationships between cytochromes P450 and H2O2: Production, reaction, and inhibition. J. Inorg. Biochem. 2018;186:228–234. doi: 10.1016/j.jinorgbio.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fialkow L., Wang Y., Downey G.P. Reactive oxygen and nitrogen species as signaling molecules regulating neutrophil function. Free Radic. Biol. Med. 2007;42:153–164. doi: 10.1016/j.freeradbiomed.2006.09.030. [DOI] [PubMed] [Google Scholar]
- 83.Sheppard F.R., Kelher M.R., Moore E.E., McLaughlin N.J.D., Banerjee A., Silliman C.C. Structural organization of the neutrophil NADPH oxidase: Phosphorylation and translocation during priming and activation. J. Leukoc. Biol. 2005;78:1025–1042. doi: 10.1189/jlb.0804442. [DOI] [PubMed] [Google Scholar]
- 84.Sarsour E.H., Kumar M.G., Chaudhuri L., Kalen A.L., Goswami P.C. Redox control of the cell cycle in health and disease. Antioxid. Redox Signal. 2009;11:2985–3011. doi: 10.1089/ars.2009.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Aseervatham G.S., Sivasudha T., Jeyadevi R., Arul Ananth D. Environmental factors and unhealthy lifestyle influence oxidative stress in humans--an overview. Environ. Sci. Pollut. Res. Int. 2013;20:4356–4369. doi: 10.1007/s11356-013-1748-0. [DOI] [PubMed] [Google Scholar]
- 86.Black C.N., Bot M., Scheffer P.G., Penninx B.W.J.H. Sociodemographic and Lifestyle Determinants of Plasma Oxidative Stress Markers 8-OHdG and F2-Isoprostanes and Associations with Metabolic Syndrome. Oxidative Med. Cell. Longev. 2016;2016:7530820. doi: 10.1155/2016/7530820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bowen L., Taylor A.E., Sullivan R., Ebrahim S., Kinra S., Krishna K.R., Kulkarni B., Ben-Shlomo Y., Ekelund U., Wells J.C., et al. Associations between diet, physical activity and body fat distribution: A cross sectional study in an Indian population. BMC Public Health. 2015;15:281. doi: 10.1186/s12889-015-1550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kondoh T., Takase H., Yamaguchi T.F., Ochiai R., Katashima M., Katsuragi Y., Sakane N. Association of dietary factors with abdominal subcutaneous and visceral adiposity in Japanese men. Obes. Res. Clin. Pract. 2014;8:e16–e25. doi: 10.1016/j.orcp.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 89.Furukawa S., Fujita T., Shimabukuro M., Iwaki M., Yamada Y., Nakajima Y., Nakayama O., Makishima M., Matsuda M., Shimomura I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J. Clin. Investig. 2004;114:1752–1761. doi: 10.1172/JCI21625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhang L., Ebenezer P.J., Dasuri K., Fernandez-Kim S.O., Francis J., Mariappan N., Gao Z., Ye J., Bruce-Keller A.J., Keller J.N. Aging is associated with hypoxia and oxidative stress in adipose tissue: Implications for adipose function. Am. J. Physiol. Endocrinol. Metab. 2011;301:E599–E607. doi: 10.1152/ajpendo.00059.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ouchi N., Parker J.L., Lugus J.J., Walsh K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 2011;11:85–97. doi: 10.1038/nri2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pasarica M., Sereda O.R., Redman L.M., Albarado D.C., Hymel D.T., Roan L.E., Rood J.C., Burk D.H., Smith S.R. Reduced adipose tissue oxygenation in human obesity evidence for rarefaction, macrophage chemotaxis, and inflammation without an angiogenic response. Diabetes. 2009;58:718–725. doi: 10.2337/db08-1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li Q.O.Y., Soro-Arnaiz I., Aragonés J. Age-dependent obesity and mitochondrial dysfunction. Adipocyte. 2017;6:161–166. doi: 10.1080/21623945.2017.1297346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vaupel P. The role of hypoxia-induced factors in tumor progression. Oncologist. 2004;9(Suppl. 5):10–17. doi: 10.1634/theoncologist.9-90005-10. [DOI] [PubMed] [Google Scholar]
- 95.Yoshimoto S., Loo T.M., Atarashi K., Kanda H., Sato S., Oyadomari S., Iwakura Y., Oshima K., Morita H., Hattori M., et al. Obesity-induced gut microbial metabolite promotes liver cancer through senescence secretome. Nature. 2013;499:97–101. doi: 10.1038/nature12347. [DOI] [PubMed] [Google Scholar]
- 96.Payne C.M., Weber C., Crowley-Skillicorn C., Dvorak K., Bernstein H., Bernstein C., Holubec H., Dvorakova B., Garewal H. Deoxycholate induces mitochondrial oxidative stress and activates NF-κB through multiple mechanisms in HCT-116 colon epithelial cells. Carcinogenesis. 2007;28:215–222. doi: 10.1093/carcin/bgl139. [DOI] [PubMed] [Google Scholar]
- 97.Visser M., Bouter L.M., McQuillan G.M., Wener M.H., Harris T.B. Elevated C-reactive protein levels in overweight and obese adults. J. Am. Med Assoc. 1999;282:2131–2135. doi: 10.1001/jama.282.22.2131. [DOI] [PubMed] [Google Scholar]
- 98.Hotamisligil G.S., Shargill N.S., Spiegelman B.M. Adipose expression of tumor necrosis factor-α: Direct role in obesity-linked insulin resistance. Science. 1993;259:87–91. doi: 10.1126/science.7678183. [DOI] [PubMed] [Google Scholar]
- 99.Fried S.K., Bunkin D.A., Greenberg A.S. Omental and subcutaneous adipose tissues of obese subjects release interleukin-6: Depot difference and regulation by glucocorticoid. J. Clin. Endocrinol. Metab. 1998;83:847–850. doi: 10.1210/jc.83.3.847. [DOI] [PubMed] [Google Scholar]
- 100.Tangvarasittichai S., Pongthaisong S., Tangvarasittichai O. Tumor Necrosis Factor-Α, Interleukin-6, C-Reactive Protein Levels and Insulin Resistance Associated with Type 2 Diabetes in Abdominal Obesity Women. Indian J. Clin. Biochem. 2016;31:68–74. doi: 10.1007/s12291-015-0514-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.King G.L., Loeken M.R. Hyperglycemia-induced oxidative stress in diabetic complications. Histochem. Cell Biol. 2004;122:333–338. doi: 10.1007/s00418-004-0678-9. [DOI] [PubMed] [Google Scholar]
- 102.Boden G., Homko C., Barrero C.A., Stein T.P., Chen X., Cheung P., Fecchio C., Koller S., Merali S. Excessive caloric intake acutely causes oxidative stress, GLUT4 carbonylation, and insulin resistance in healthy men. Sci. Transl. Med. 2015;7:304re7. doi: 10.1126/scitranslmed.aac4765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dandona P., Mohanty P., Hamouda W., Ghanim H., Aljada A., Garg R., Kumar V. Inhibitory effect of a two day fast on reactive oxygen species (ROS) generation by leucocytes and plasma ortho-tyrosine and meta-tyrosine concentrations. J. Clin. Endocrinol. Metab. 2001;86:2899–2902. doi: 10.1210/jcem.86.6.7745. [DOI] [PubMed] [Google Scholar]
- 104.Dandona P., Mohanty P., Ghanim H., Aljada A., Browne R., Hamouda W., Prabhala A., Afzal A., Garg R. The suppressive effect of dietary restriction and weight loss in the obese on the generation of reactive oxygen species by leukocytes, lipid peroxidation, and protein carbonylation. J. Clin. Endocrinol. Metab. 2001;86:355–362. doi: 10.1210/jcem.86.1.7150. [DOI] [PubMed] [Google Scholar]
- 105.Heilbronn L.K., De Jonge L., Frisard M.I., DeLany J.P., Larson-Meyer D.E., Rood J., Nguyen T., Martin C.K., Volaufova J., Most M.M., et al. Effect of 6-month calorie restriction on biomarkers of longevity, metabolic adaptation, and oxidative stress in overweight individuals: A randomized controlled trial. J. Am. Med. Assoc. 2006;295:1539–1548. doi: 10.1001/jama.295.13.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Buchowski M.S., Hongu N., Acra S., Wang L., Warolin J., Roberts L.J., II Effect of Modest Caloric Restriction on Oxidative Stress in Women, a Randomized Trial. PLoS ONE. 2012;7:e47079. doi: 10.1371/journal.pone.0047079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Khor A., Grant R., Tung C., Guest J., Pope B., Morris M., Bilgin A. Postprandial oxidative stress is increased after a phytonutrient-poor food but not after a kilojoule-matched phytonutrient-rich food. Nutr. Res. 2014;34:391–400. doi: 10.1016/j.nutres.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 108.Kim M.J., Aiken J.M., Havighurst T., Hollander J., Ripple M.O., Weindruch R. Adult-onset energy restriction of rhesus monkeys attenuates oxidative stress-induced cytokine expression by peripheral blood mononuclear cells. J. Nutr. 1997;127:2293–2301. doi: 10.1093/jn/127.12.2293. [DOI] [PubMed] [Google Scholar]
- 109.Fontana L., Villareal D.T., Weiss E.P., Racette S.B., Steger-May K., Klein S., Holloszy J.O. Calorie restriction or exercise: Effects on coronary heart disease risk factors. A randomized, controlled trial. Am. J. Physiol. Endocrinol. Metab. 2007;293:E197–E202. doi: 10.1152/ajpendo.00102.2007. [DOI] [PubMed] [Google Scholar]
- 110.Fontana L., Partridge L., Longo V.D. Extending healthy life span-from yeast to humans. Science. 2010;328:321–326. doi: 10.1126/science.1172539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mercken E.M., Crosby S.D., Lamming D.W., Jebailey L., Krzysik-Walker S., Villareal D.T., Capri M., Franceschi C., Zhang Y., Becker K., et al. Calorie restriction in humans inhibits the PI3K/AKT pathway and induces a younger transcription profile. Aging Cell. 2013;12:645–651. doi: 10.1111/acel.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Speakman J.R., Mitchell S.E., Mazidi M. Calories or protein? The effect of dietary restriction on lifespan in rodents is explained by calories alone. Exp. Gerontol. 2016;86:28–38. doi: 10.1016/j.exger.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 113.Fanson B.G., Weldon C.W., Pérez-Staples D., Simpson S.J., Taylor P.W. Nutrients, not caloric restriction, extend lifespan in Queensland fruit flies (Bactrocera tryoni) Aging Cell. 2009;8:514–523. doi: 10.1111/j.1474-9726.2009.00497.x. [DOI] [PubMed] [Google Scholar]
- 114.Baum J.I., Kim I.Y., Wolfe R.R. Protein consumption and the elderly: What is the optimal level of intake? Nutrients. 2016;8:359. doi: 10.3390/nu8060359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pamplona R., Barja G. Mitochondrial oxidative stress, aging and caloric restriction: The protein and methionine connection. Biochim. et Biophys. Acta Bioenerg. 2006;1757:496–508. doi: 10.1016/j.bbabio.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 116.Mair W., Piper M.D.W., Partridge L. Calories do not explain extension of life span by dietary restriction in Drosophila. PLoS Biol. 2005;3:1305–1311. doi: 10.1371/journal.pbio.0030223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Levine M.E., Suarez J.A., Brandhorst S., Balasubramanian P., Cheng C.W., Madia F., Fontana L., Mirisola M.G., Guevara-Aguirre J., Wan J., et al. Low protein intake is associated with a major reduction in IGF-1, cancer, and overall mortality in the 65 and younger but not older population. Cell Metab. 2014;19:407–417. doi: 10.1016/j.cmet.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Solon-Biet S.M., McMahon A.C., Ballard J.W.O., Ruohonen K., Wu L.E., Cogger V.C., Warren A., Huang X., Pichaud N., Melvin R.G., et al. The ratio of macronutrients, not caloric intake, dictates cardiometabolic health, aging, and longevity in ad libitum-fed mice. Cell Metab. 2014;19:418–430. doi: 10.1016/j.cmet.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Fontana L., Cummings N.E., Arriola Apelo S.I., Neuman J.C., Kasza I., Schmidt B.A., Cava E., Spelta F., Tosti V., Syed F.A., et al. Decreased Consumption of Branched-Chain Amino Acids Improves Metabolic Health. Cell Rep. 2016;16:520–530. doi: 10.1016/j.celrep.2016.05.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sanz A., Caro P., Barja G. Protein restriction without strong caloric restriction decreases mitochondrial oxygen radical production and oxidative DNA damage in rat liver. J. Bioenerg. Biomembr. 2004;36:545–552. doi: 10.1007/s10863-004-9001-7. [DOI] [PubMed] [Google Scholar]
- 121.De A.K., Chipalkatti S., Aiyar A.S. Some biochemical parameters of ageing in relation to dietary protein. Mech. Ageing Dev. 1983;21:37–48. doi: 10.1016/0047-6374(83)90014-3. [DOI] [PubMed] [Google Scholar]
- 122.Seyedsadjadi N., Berg J., Bilgin A.A., Braidy N., Salonikas C., Grant R. High protein intake is associated with low plasma NAD+ levels in a healthy human cohort. PLoS ONE. 2018;13:e0201968. doi: 10.1371/journal.pone.0201968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hidiroglou N., Gilani G.S., Long L., Zhao X., Madere R., Cockell K., Belonge B., Ratnayake W.M.N., Peace R. The influence of dietary vitamin E, fat, and methionine on blood cholesterol profile, homocysteine levels, and oxidizability of low density lipoprotein in the gerbil. J. Nutr. Biochem. 2004;15:730–740. doi: 10.1016/j.jnutbio.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 124.Mori N., Hirayama K. Long-term consumption of a methionine-supplemented diet increases iron and lipid peroxide levels in rat liver. J. Nutr. 2000;130:2349–2355. doi: 10.1093/jn/130.9.2349. [DOI] [PubMed] [Google Scholar]
- 125.Chan D.S.M., Lau R., Aune D., Vieira R., Greenwood D.C., Kampman E., Norat T. Red and processed meat and colorectal cancer incidence: Meta-analysis of prospective studies. PLoS ONE. 2011;6:e20456. doi: 10.1371/journal.pone.0020456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Romeu M., Aranda N., Giralt M., Ribot B., Nogues M.R., Arija V. Diet, iron biomarkers and oxidative stress in a representative sample of Mediterranean population. Nutr. J. 2013;12:102. doi: 10.1186/1475-2891-12-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mainous Iii A.G., Wells B., Carek P.J., Gill J.M., Geesey M.E. The mortality risk of elevated serum transferrin saturation and consumption of dietary iron. Ann. Fam. Med. 2004;2:139–144. doi: 10.1370/afm.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sinha R., Rothman N., Salmon C.P., Knize M.G., Brown D.E., Swanson C.A., Rhodes D., Rossi S., Felton J.S., Levander O.A. Heterocyclic amine content in beef cooked by different methods to varying degrees of doneness and gravy made from meat drippings. Food Chem. Toxicol. 1998;36:279–287. doi: 10.1016/S0278-6915(97)00162-2. [DOI] [PubMed] [Google Scholar]
- 129.Chen G., Scott Smith J. Determination of advanced glycation endproducts in cooked meat products. Food Chem. 2015;168:190–195. doi: 10.1016/j.foodchem.2014.06.081. [DOI] [PubMed] [Google Scholar]
- 130.Carvalho A.M., Miranda A.M., Santos F.A., Loureiro A.P.M., Fisberg R.M., Marchioni D.M. High intake of heterocyclic amines from meat is associated with oxidative stress. Br. J. Nutr. 2015;113:1301–1307. doi: 10.1017/S0007114515000628. [DOI] [PubMed] [Google Scholar]
- 131.Yamagishi S.I., Maeda S., Matsui T., Ueda S., Fukami K., Okuda S. Role of advanced glycation end products (AGEs) and oxidative stress in vascular complications in diabetes. Biochim. et Biophys. Acta Gen. Subj. 2012;1820:663–671. doi: 10.1016/j.bbagen.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 132.Wilson A., McLean C., Kim R.B. Trimethylamine-N-oxide: A link between the gut microbiome, bile acid metabolism, and atherosclerosis. Curr. Opin. Lipidol. 2016;27:148–154. doi: 10.1097/MOL.0000000000000274. [DOI] [PubMed] [Google Scholar]
- 133.Sun X., Jiao X., Ma Y., Liu Y., Zhang L., He Y., Chen Y. Trimethylamine N-oxide induces inflammation and endothelial dysfunction in human umbilical vein endothelial cells via activating ROS-TXNIP-NLRP3 inflammasome. Biochem. Biophys. Res. Commun. 2016;481:63–70. doi: 10.1016/j.bbrc.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 134.Wall R., Ross R.P., Fitzgerald G.F., Stanton C. Fatty acids from fish: The anti-inflammatory potential of long-chain omega-3 fatty acids. Nutr. Rev. 2010;68:280–289. doi: 10.1111/j.1753-4887.2010.00287.x. [DOI] [PubMed] [Google Scholar]
- 135.Patterson E., Wall R., Fitzgerald G.F., Ross R.P., Stanton C. Health implications of high dietary omega-6 polyunsaturated fatty acids. J. Nutr. Metab. 2012;2012:1–16. doi: 10.1155/2012/539426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Simopoulos A.P. Omega-3 fatty acids in inflammation and autoimmune diseases. J. Am. Coll. Nutr. 2002;21:495–505. doi: 10.1080/07315724.2002.10719248. [DOI] [PubMed] [Google Scholar]
- 137.Simopoulos A.P. An increase in the Omega-6/Omega-3 fatty acid ratio increases the risk for obesity. Nutrients. 2016;8:128. doi: 10.3390/nu8030128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Martinez-Micaelo N., González-Abuín N., Terra X., Richart C., Ardèvol A., Pinent M., Blay M. Omega-3 docosahexaenoic acid and procyanidins inhibit cyclo-oxygenase activity and attenuate NF-κB activation through a p105/p50 regulatory mechanism in macrophage inflammation. Biochem. J. 2012;441:653–663. doi: 10.1042/BJ20110967. [DOI] [PubMed] [Google Scholar]
- 139.Im D.S. Omega-3 fatty acids in anti-inflammation (pro-resolution) and GPCRs. Prog. Lipid Res. 2012;51:232–237. doi: 10.1016/j.plipres.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 140.Sakai C., Ishida M., Ohba H., Yamashita H., Uchida H., Yoshizumi M., Ishida T. Fish oil omega-3 polyunsaturated fatty acids attenuate oxidative stress-induced DNA damage in vascular endothelial cells. PLoS ONE. 2017;12:e0187934. doi: 10.1371/journal.pone.0187934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Nalsen C., Vessby B., Berglund L., Uusitupa M., Hermansen K., Riccardi G., Rivellese A., Storlien L., Erkkila A., Yla-Herttuala S., et al. Dietary (n-3) fatty acids reduce plasma F2-isoprostanes but not prostaglandin F2α in healthy humans. J. Nutr. 2006;136:1222–1228. doi: 10.1093/jn/136.5.1222. [DOI] [PubMed] [Google Scholar]
- 142.Shahidi F., Zhong Y. Lipid oxidation and improving the oxidative stability. Chem. Soc. Rev. 2010;39:4067–4079. doi: 10.1039/b922183m. [DOI] [PubMed] [Google Scholar]
- 143.Gueraud F., Atalay M., Bresgen N., Cipak A., Eckl P.M., Huc L., Jouanin I., Siems W., Uchida K. Chemistry and biochemistry of lipid peroxidation products. Free Rad. Res. 2010;44:1098–1124. doi: 10.3109/10715762.2010.498477. [DOI] [PubMed] [Google Scholar]
- 144.Jira W., Spiteller G., Carson W., Schramm A. Strong increase in hydroxy fatty acids derived from linoleic acid in human low density lipoproteins of atherosclerotic patients. Chem.Phys. Lipids. 1997;91:1–11. doi: 10.1016/S0009-3084(97)00095-9. [DOI] [PubMed] [Google Scholar]
- 145.Jenkins D.J.A., Wolever T.M.S., Taylor R.H. Glycemic index of foods: A physiological basis for carbohydrate exchange. Am. J. Clin. Nutr. 1981;34:362–366. doi: 10.1093/ajcn/34.3.362. [DOI] [PubMed] [Google Scholar]
- 146.Dickinson S., Hancock D.P., Petocz P., Ceriello A., Brand-Miller J. High-glycemic index carbohydrate increases nuclear factor-κB activation in mononuclear cells of young, lean healthy subjects1-3. Am. J. Clin. Nutr. 2008;87:1188–1193. doi: 10.1093/ajcn/87.5.1188. [DOI] [PubMed] [Google Scholar]
- 147.Hu Y., Block G., Norkus E.P., Morrow J.D., Dietrich M., Hudes M. Relations of glycemic index and glycemic load with plasma oxidative stress markers. Am. J. Clin. Nut. 2006;84:70–76. doi: 10.1093/ajcn/84.1.70. [DOI] [PubMed] [Google Scholar]
- 148.Anderson C., Milne G.L., Park Y.M.M., Sandler D.P., Nichols H.B. Dietary glycemic index and glycemic load are positively associated with oxidative stress among premenopausal women. J. Nut. 2018;148:125–130. doi: 10.1093/jn/nxx022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Du X.L., Edelstein D., Rossetti L., Fantus I.G., Goldberg H., Ziyadeh F., Wu J., Brownlee M. Hyperglycemia-induced mitochondrial superoxide overproduction activates the hexosamine pathway and induces plasminogen activator inhibitor-1 expression by increasing Sp1 glycosylation. Proc. Natl. Acad. Sci. USA. 2000;97:12222–12226. doi: 10.1073/pnas.97.22.12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Yuan Y., Jiao X., Lau W.B., Wang Y., Christopher T.A., Lopez B.L., RamachandraRao S.P., Tao L., Ma X.L. Thioredoxin glycation: A novel posttranslational modification that inhibits its antioxidant and organ protective actions. Free Radic. Biol. Med. 2010;49:332–338. doi: 10.1016/j.freeradbiomed.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ceriello A., Bortolotti N., Motz E., Pieri C., Marra M., Tonutti L., Lizzio S., Feletto F., Catone B., Taboga C. Meal-induced oxidative stress and low-density lipoprotein oxidation in diabetes: The possible role of hyperglycemia. Metab. Clin. Exp. 1999;48:1503–1508. doi: 10.1016/S0026-0495(99)90237-8. [DOI] [PubMed] [Google Scholar]
- 152.Pieper G.M., Riazul H. Activation of nuclear factor-κb in cultured endothelial cells by increased glucose concentration: Prevention by calphostin C. J. Cardiovasc. Pharmacol. 1997;30:528–532. doi: 10.1097/00005344-199710000-00019. [DOI] [PubMed] [Google Scholar]
- 153.Xia P., Kramer R.M., King G.L. Identification of the mechanism for the inhibition of Na+,K+-adenosine triphosphatase by hyperglycemia involving activation of protein kinase C and cytosolic phospholipase A2. J. Clin. Investig. 1995;96:733–740. doi: 10.1172/JCI118117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Degenhardt T.P., Thorpe S.R., Baynes J.W. Chemical modification of proteins by methylglyoxal. Cell. Mol. Biol. 1998;44:1139–1145. [PubMed] [Google Scholar]
- 155.Qi L., Van Dam R.M., Liu S., Franz M., Mantzoros C., Hu F.B. Whole-grain, bran, and cereal fiber intakes and markers of systemic inflammation in diabetic women. Diabetes Care. 2006;29:207–211. doi: 10.2337/diacare.29.02.06.dc05-1903. [DOI] [PubMed] [Google Scholar]
- 156.Esfahani A., Wong J.M.W., Truan J., Villa C.R., Mirrahimi A., Srichaikul K., Kendall C.W.C. Health Effects of Mixed Fruit and Vegetable Concentrates: A Systematic Review of the Clinical Interventions. J. Am. Coll. Nutr. 2011;30:285–294. doi: 10.1080/07315724.2011.10719971. [DOI] [PubMed] [Google Scholar]
- 157.Fiedor J., Burda K. Potential role of carotenoids as antioxidants in human health and disease. Nutrients. 2014;6:466–488. doi: 10.3390/nu6020466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Banjarnahor S.D.S., Artanti N. Antioxidant properties of flavonoids. Med J. Indones. 2014;23:239–244. doi: 10.13181/mji.v23i4.1015. [DOI] [Google Scholar]
- 159.Leeds A.R., Ferris E.A.E., Staley J., Ayesh R., Ross F. Availability of micronutrients from dried, encapsulated fruit and vegetable preparations: A study in healthy volunteers. J. Human Nutr. Diet. 2000;13:21–27. doi: 10.1046/j.1365-277x.2000.00206.x. [DOI] [Google Scholar]
- 160.Thompson H.J., Heimendinger J., Sedlacek S., Haegele A., Diker A., O’Neill C., Meinecke B., Wolfe P., Zhu Z., Jiang W. 8-Isoprostane F2α excretion is reduced in women by increased vegetable and fruit intake. Am. J. Clin. Nutr. 2005;82:768–776. doi: 10.1093/ajcn/82.4.768. [DOI] [PubMed] [Google Scholar]
- 161.Ruel G., Pomerleau S., Couture P., Lamarche B., Couillard C. Changes in plasma antioxidant capacity and oxidized low-density lipoprotein levels in men after short-term cranberry juice consumption. Metab. Clin. Exp. 2005;54:856–861. doi: 10.1016/j.metabol.2005.01.031. [DOI] [PubMed] [Google Scholar]
- 162.Thompson H.J., Heimendinger J., Gillette C., Sedlacek S.M., Haegele A., O‘Neill C., Wolfe P. In vivo investigation of changes in biomarkers of oxidative stress induced by plant food rich diets. J. Agric. Food Chem. 2005;53:6126–6132. doi: 10.1021/jf050493x. [DOI] [PubMed] [Google Scholar]
- 163.Hermsdorff H.H.M., Zulet M.A., Puchau B., Martínez J.A. Fruit and vegetable consumption and proinflammatory gene expression from peripheral blood mononuclear cells in young adults: A translational study. Nutr. Metab. 2010;7:42. doi: 10.1186/1743-7075-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Yeum K.J., Booth S.L., Sadowski J.A., Liu C., Tang G., Krinsky N.I., Russell R.M. Human plasma carotenoid response to the ingestion of controlled diets high in fruits and vegetables. Am. J. Clin. Nutr. 1996;64:594–602. doi: 10.1093/ajcn/64.4.594. [DOI] [PubMed] [Google Scholar]
- 165.Harasym J., Oledzki R. Effect of fruit and vegetable antioxidants on total antioxidant capacity of blood plasma. Nutrition. 2014;30:511–517. doi: 10.1016/j.nut.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 166.Gruszecki W.I., Strzałka K. Carotenoids as modulators of lipid membrane physical properties. Biochim. et Biophys. Acta Mol. Basis Dis. 2005;1740:108–115. doi: 10.1016/j.bbadis.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 167.Agarwal S., Rao A.V. Tomato lycopene and low density lipoprotein oxidation: A human dietary intervention study. Lipids. 1998;33:981–984. doi: 10.1007/s11745-998-0295-6. [DOI] [PubMed] [Google Scholar]
- 168.Visioli F., Riso P., Grande S., Galli C., Porrini M. Protective activity of tomato products on in vivo markers of lipid oxidation. Eur. J. Nutr. 2003;42:201–206. doi: 10.1007/s00394-003-0415-5. [DOI] [PubMed] [Google Scholar]
- 169.Asgard R., Rytter E., Basu S., Abramsson-Zetterberg L., Moller L., Vessby B. High intake of fruit and vegetables is related to low oxidative stress and inflammation in a group of patients with type 2 diabetes. Scand. J. Food Nutr. 2007;51:149–158. doi: 10.1080/17482970701737285. [DOI] [Google Scholar]
- 170.Myles I.A. Fast food fever: Reviewing the impacts of the Western diet on immunity. Nutr. J. 2014;13:61. doi: 10.1186/1475-2891-13-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.McAuliffe S., Ray S., Fallon E., Bradfield J., Eden T., Kohlmeier M. Dietary micronutrients in the wake of COVID-19: An appraisal of evidence with a focus on high-risk groups and preventative healthcare. BMJ Nutr. Prev. Health. 2020;3:93. doi: 10.1136/bmjnph-2020-000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Crabb D.W., Matsumoto M., Chang D., You M. Overview of the role of alcohol dehydrogenase and aldehyde dehydrogenase and their variants in the genesis of alcohol-related pathology. Proc. Nutr. Soc. 2004;63:49–63. doi: 10.1079/PNS2003327. [DOI] [PubMed] [Google Scholar]
- 173.Montoliu C., Sancho-Tello M., Azorin I., Burgal M., Vallés S., Renau-Piqueras J., Guerri C. Ethanol Increases Cytochrome P4502E1 and Induces Oxidative Stress in Astrocytes. J. Neurochem. 1995;65:2561–2570. doi: 10.1046/j.1471-4159.1995.65062561.x. [DOI] [PubMed] [Google Scholar]
- 174.Lu Y., Cederbaum A.I. CYP2E1 and oxidative liver injury by alcohol. Free Radic. Biol. Med. 2008;44:723–738. doi: 10.1016/j.freeradbiomed.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Roig R., Cascón E., Arola L., Bladé C., Salvadó M.J. Effects of chronic wine and alcohol intake on glutathione and malondialdehyde levels in rats. Nutr. Res. 2000;20:1547–1555. doi: 10.1016/S0271-5317(00)00239-6. [DOI] [Google Scholar]
- 176.Hirano T. Alcohol consumption and oxidative DNA damage. Int. J. Environ. Res. Public Health. 2011;8:2895–2906. doi: 10.3390/ijerph8072895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Schrieks I.C., van den Berg R., Sierksma A., Beulens J.W.J., Vaes W.H.J., Hendriks N.F.J. Effect of red wine consumption on biomarkers of oxidative stress. Alcohol Alcohol. 2013;48:153–159. doi: 10.1093/alcalc/ags086. [DOI] [PubMed] [Google Scholar]
- 178.Zima T., Fialová L., Mestek O., Janebová M., Crkovská J., Malbohan I., Štípek S., Mikulíková L., Popov P. Oxidative stress, metabolism of ethanol and alcohol-related diseases. J. Biomed. Sci. 2001;8:59–70. doi: 10.1007/BF02255972. [DOI] [PubMed] [Google Scholar]
- 179.Marta K., Tomáš Z., Petr P., Pavel Š., Martin B., Jiřina S., Květa P., Rosemarie K.E. Advanced glycation end-products in patients with chronic alcohol misuse. Alcohol Alcohol. 2004;39:316–320. doi: 10.1093/alcalc/agh058. [DOI] [PubMed] [Google Scholar]
- 180.Niemela O. Aldehyde-protein adducts in the liver as a result of ethanol-induced oxidative stress. Front. Biosci. J. Virtual Libr. 1999;4:D506–D513. doi: 10.2741/A445. [DOI] [PubMed] [Google Scholar]
- 181.Guest J., Guillemin G.J., Heng B., Grant R. Lycopene pretreatment ameliorates acute ethanol induced NAD+depletion in human astroglial cells. Oxidative Med. Cell. Longev. 2015;2015:741612. doi: 10.1155/2015/741612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Frary C.D., Johnson R.K., Wang M.Q. Food sources and intakes of caffeine in the diets of persons in the United States. J. Am. Diet. Assoc. 2005;105:110–113. doi: 10.1016/j.jada.2004.10.027. [DOI] [PubMed] [Google Scholar]
- 183.Smit H.J., Gaffan E.A., Rogers P.J. Methylxanthines are the psycho-pharmacologically active constituents of chocolate. Psychopharmacology. 2004;176:412–419. doi: 10.1007/s00213-004-1898-3. [DOI] [PubMed] [Google Scholar]
- 184.Chu Y.F., Chen Y., Brown P.H., Lyle B.J., Black R.M., Cheng I.H., Ou B., Prior R.L. Bioactivities of crude caffeine: Antioxidant activity, cyclooxygenase-2 inhibition, and enhanced glucose uptake. Food Chem. 2012;131:564–568. doi: 10.1016/j.foodchem.2011.09.024. [DOI] [Google Scholar]
- 185.Acheson K.J., Gremaud G., Meirim I., Montigon F., Krebs Y., Fay L.B., Gay L.-J., Schneiter P., Schindler C., Tappy L. Metabolic effects of caffeine in humans: Lipid oxidation or futile cycling? Am. J. Clin. Nutr. 2004;79:40–46. doi: 10.1093/ajcn/79.1.40. [DOI] [PubMed] [Google Scholar]
- 186.Zeraatpishe A., Malekirad A.A., Nik-Kherad J., Jafari A., Babadi S.Y., Tanwir F., Espanani H.R. The effects of caffeine supplements on exercise-induced oxidative damages. Asian J. Sports Med. 2015;6:e23020. doi: 10.5812/asjsm.23023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Al-Basher G.I., Aljabal H., Almeer R.S., Allam A.A., Mahmoud A.M. Perinatal exposure to energy drink induces oxidative damage in the liver, kidney and brain, and behavioral alterations in mice offspring. Biomed. Pharmacother. 2018;102:798–811. doi: 10.1016/j.biopha.2018.03.139. [DOI] [PubMed] [Google Scholar]
- 188.Zampelas A., Panagiotakos D.B., Pitsavos C., Chrysohoou C., Stefanadis C. Associations between coffee consumption and inflammatory markers in healthy persons: The ATTICA study. Am. J. Clin. Nutr. 2004;80:862–867. doi: 10.1093/ajcn/80.4.862. [DOI] [PubMed] [Google Scholar]
- 189.Chavez Valdez R., Ahlawat R., Wills-Karp M., Nathan A., Ezell T., Gauda E.B. Correlation between serum caffeine levels and changes in cytokine profile in a cohort of preterm infants. J. Pediatrics. 2011;158:57–64.e1. doi: 10.1016/j.jpeds.2010.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Correa T.A.F., Rogero M.M., Mioto B.M., Tarasoutchi D., Tuda V.L., Cesar L.A.M., Torres EAFS Paper-filtered coffee increases cholesterol and inflammation biomarkers independent of roasting degree: A clinical trial. Nutrition. 2013;29:977–981. doi: 10.1016/j.nut.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 191.Chavez-Valdez R., Ahlawat R., Wills-Karp M., Gauda E.B. Mechanisms of modulation of cytokine release by human cord blood monocytes exposed to high concentrations of caffeine. Pediatric Res. 2016;80:101–109. doi: 10.1038/pr.2016.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Karki R., Igwe O.J. Toll-Like Receptor 4–Mediated Nuclear Factor Kappa B Activation Is Essential for Sensing Exogenous Oxidants to Propagate and Maintain Oxidative/Nitrosative Cellular Stress. PLOS ONE. 2013;8:e73840. doi: 10.1371/journal.pone.0073840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Burns D.M. Cigarettes and cigarette smoking. Clin. Chest Med. 1991;12:631–642. [PubMed] [Google Scholar]
- 194.Rohrer J., Wuertz B.R.K., Ondrey F. Cigarette smoke condensate induces nuclear factor kappa-B activity and proangiogenic growth factors in aerodigestive cells. Laryngoscope. 2010;120:1609–1613. doi: 10.1002/lary.20972. [DOI] [PubMed] [Google Scholar]
- 195.Csordas A., Wick G., Laufer G., Bernhard D. An evaluation of the clinical evidence on the role of inflammation and oxidative stress in smoking-mediated cardiovascular disease. Biomark. Insights. 2008;2008:127–139. doi: 10.4137/BMI.S480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Teixeira De Lemos E., Oliveira J., Páscoa Pinheiro J., Reis F. Regular physical exercise as a strategy to improve antioxidant and anti-inflammatory status: Benefits in type 2 diabetes mellitus. Oxidative Med. Cell. Longev. 2012;2012:741545. doi: 10.1155/2012/741545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Gomez-Cabrera M.C., Domenech E., Viña J. Moderate exercise is an antioxidant: Upregulation of antioxidant genes by training. Free Radic. Biol. Med. 2008;44:126–131. doi: 10.1016/j.freeradbiomed.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 198.Finaud J., Lac G., Filaire E. Oxidative stress: Relationship with exercise and training. Sports Med. 2006;36:327–358. doi: 10.2165/00007256-200636040-00004. [DOI] [PubMed] [Google Scholar]
- 199.Caimi G., Canino B., Amodeo G., Montana M., Presti R.L. Lipid peroxidation and total antioxidant status in unprofessional athletes before and after a cardiopulmonary test. Clin. Hemorheol. Microcirc. 2009;43:235–241. doi: 10.3233/CH-2009-1215. [DOI] [PubMed] [Google Scholar]
- 200.Ferrer M.D., Sureda A., Batle J.M., Tauler P., Tur J.A., Pons A. Scuba diving enhances endogenous antioxidant defenses in lymphocytes and neutrophils. Free Radic. Res. 2007;41:274–281. doi: 10.1080/10715760601080371. [DOI] [PubMed] [Google Scholar]
- 201.Niess A.M., Passek F., Lorenz I., Schneider E.M., Dickhuth H.H., Northoff H., Fehrenbach E. Expression of the antioxidant stress protein heme oxygenase-1 (HO-1) in human leukocytes: Acute and adaptational responses to endurance exercise. Free Radic. Biol. Med. 1999;26:184–192. doi: 10.1016/S0891-5849(98)00192-0. [DOI] [PubMed] [Google Scholar]
- 202.Galassetti P.R., Nemet D., Pescatello A., Rose-Gottron C., Larson J., Cooper D.M. Exercise, caloric restriction, and systemic oxidative stress. J. Investig. Med. 2006;54:67–75. doi: 10.2310/6650.2005.05024. [DOI] [PubMed] [Google Scholar]
- 203.Martin-Cordero L., Garcia J.J., Giraldo E., De la Fuente M., Manso R., Ortega E. Influence of exercise on the circulating levels and macrophage production of IL-1β and IFNγ affected by metabolic syndrome: An obese Zucker rat experimental animal model. Eur. J. Appl.Physiol. 2009;107:535–543. doi: 10.1007/s00421-009-1140-4. [DOI] [PubMed] [Google Scholar]
- 204.Mattusch F., Dufaux B., Heine O., Mertens I., Rost R. Reduction of the plasma concentration of C-reactive protein following nine months of endurance training. Int. J. Sports Med. 2000;21:21–24. doi: 10.1055/s-2000-8852. [DOI] [PubMed] [Google Scholar]
- 205.Smith J.K., Dykes R., Douglas J.E., Krishnaswamy G., Berk S. Long-term exercise and atherogenic activity of blood mononuclear cells in persons at risk of developing ischemic heart disease. J. Am. Med. Assoc. 1999;281:1722–1727. doi: 10.1001/jama.281.18.1722. [DOI] [PubMed] [Google Scholar]
- 206.Reimund E. The free radical flux theory of sleep. Med Hypotheses. 1994;43:231–233. doi: 10.1016/0306-9877(94)90071-X. [DOI] [PubMed] [Google Scholar]
- 207.Ikeda M., Ikeda-Sagara M., Okada T., Clement P., Urade Y., Nagai T., Sugiyama T., Yoshioka T., Honda K., Inoué S. Brain oxidation is an initial process in sleep induction. Neuroscience. 2005;130:1029–1040. doi: 10.1016/j.neuroscience.2004.09.057. [DOI] [PubMed] [Google Scholar]
- 208.Boudjeltia K., Faraut B., Esposito M.J., Stenuit P., Dyzma M., van Antwerpen P., Brohée D., Vanhamme L., Moguilevsky N., Vanhaeverbeek M., et al. Temporal dissociation between myeloperoxidase (MPO)-modified LDL and MPO elevations during chronic sleep restriction and recovery in healthy young men. PLoS ONE. 2011;6:e28230. doi: 10.1371/journal.pone.0028230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Villafuerte G., Miguel-Puga A., Murillo Rodríguez E., Machado S., Manjarrez E., Arias-Carrión O. Sleep deprivation and oxidative stress in animal models: A systematic review. Oxidative Med. Cell. Longev. 2015;2015:234952. doi: 10.1155/2015/234952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Alzoubi K.H., Khabour O.F., Salah H.A., Abu Rashid B.E. The combined effect of sleep deprivation and western diet on spatial learning and memory: Role of BDNF and oxidative stress. J. Mol. Neurosci. 2013;50:124–133. doi: 10.1007/s12031-012-9881-7. [DOI] [PubMed] [Google Scholar]
- 211.van Leeuwen W.M.A., Lehto M., Karisola P., Lindholm H., Luukkonen R., Sallinen M., Härmä M., Porkka-Heiskanen T., Alenius H. Sleep restriction increases the risk of developing cardiovascular diseases by augmenting proinflammatory responses through IL-17 and CRP. PLoS ONE. 2009;4:e4589. doi: 10.1371/journal.pone.0004589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Meier-Ewert H.K., Ridker P.M., Rifai N., Regan M.M., Price N.J., Dinges D.F., Mullington J.M. Effect of sleep loss on C-Reactive protein, an inflammatory marker of cardiovascular risk. J. Am. Coll. Cardiol. 2004;43:678–683. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- 213.Eisele H.J., Markart P., Schulz R. Obstructive sleep apnea, oxidative stress, and cardiovascular disease: Evidence from human studies. Oxidative Med. Cell. Longev. 2015;2015:608438. doi: 10.1155/2015/608438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Younes M. Role of respiratory control mechanisms in the pathogenesis of obstructive sleep disorders. J. Appl. Physiol. 2008;105:1389–1405. doi: 10.1152/japplphysiol.90408.2008. [DOI] [PubMed] [Google Scholar]
- 215.Schulz R., Mahmoudi S., Hattar K., Sibelius U.L.F., Olschewski H., Mayer K., Seeger W., Grimminger F. Enhanced release of superoxide from polymorphonuclear neutrophils in obstructive sleep apnea: Impact of continuous positive airway pressure therapy. Am. J. Respir. Crit. Care Med. 2000;162:566–670. doi: 10.1164/ajrccm.162.2.9908091. [DOI] [PubMed] [Google Scholar]
- 216.Alonso-Fernández A., García-Río F., Arias M.A., Hernanz Á., De La Peña M., Piérola J., Barceló A., López-Collazo E., Agustí A. Effects of CPAP on oxidative stress and nitrate efficiency in sleep apnoea: A randomised trial. Thorax. 2009;64:581–586. doi: 10.1136/thx.2008.100537. [DOI] [PubMed] [Google Scholar]
- 217.Lavie L., Vishnevsky A., Lavie P. Evidence for lipid peroxidation in obstructive sleep apnea. Sleep. 2004;27:123–128. [PubMed] [Google Scholar]
- 218.Yamauchi M., Nakano H., Maekawa J., Okamoto J., Ohnishi Y., Suzuki T., Kimura H. Oxidative stress in obstructive sleep apnea. Chest. 2005;127:1674–1679. doi: 10.1378/chest.127.5.1674. [DOI] [PubMed] [Google Scholar]
- 219.Ozben S., Huseyinoglu N., Hanikoglu F., Guvenc T.S., Yildirim B.Z., Cort A., Ozdem S., Ozben T. Advanced oxidation protein products and ischaemia-modified albumin in obstructive sleep apnea. Eur. J. Clin. Investig. 2014;44:1045–1052. doi: 10.1111/eci.12338. [DOI] [PubMed] [Google Scholar]
- 220.Barceló A., Barbé F., de la Peña M., Vila M., Pérez G., Piérola J., Durán J., Agustí A.G.N. Antioxidant status in patients with sleep apnoea and impact of continuous positive airway pressure treatment. Eur. Respir. J. 2006;27:756–760. doi: 10.1183/09031936.06.00067605. [DOI] [PubMed] [Google Scholar]
- 221.Wysocka E., Cofta S., Cymerys M., Gozdzik J., Torlinski L., Batura-Gabryel H. The impact of the sleep apnea syndrome on oxidant-antioxidant balance in the blood of overweight and obese patients. J. Physiol. Pharmacol. 2008;59(Suppl. 6):761–769. [PubMed] [Google Scholar]
- 222.Unnikrishnan D., Jun J., Polotsky V. Inflammation in sleep apnea: An update. Rev. Endocr. Metab. Disord. 2015;16:25–34. doi: 10.1007/s11154-014-9304-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Ryan S., Taylor C.T., McNicholas W.T. Predictors of elevated nuclear factor-κB-dependent genes in obstructive sleep apnea syndrome. Am. J. Respir. Crit. Care Med. 2006;174:824–830. doi: 10.1164/rccm.200601-066OC. [DOI] [PubMed] [Google Scholar]
- 224.Gross C., Hen R. The developmental origins of anxiety. Nat. Rev. Neurosci. 2004;5:545–552. doi: 10.1038/nrn1429. [DOI] [PubMed] [Google Scholar]
- 225.Weinberger D.R. Anxiety at the frontier of molecular medicine. New Engl. J. Med. 2001;344:1247–1249. doi: 10.1056/NEJM200104193441612. [DOI] [PubMed] [Google Scholar]
- 226.Anderson G., Maes M. Oxidative/nitrosative stress and immuno-inflammatory pathways in depression: Treatment implications. Curr. Pharm. Des. 2014;20:3812–3847. doi: 10.2174/13816128113196660738. [DOI] [PubMed] [Google Scholar]
- 227.Bouayed J., Rammal H., Soulimani R. Oxidative stress and anxiety: Relationship and cellular pathways. Oxidative Med. Cell. Longev. 2009;2:63–67. doi: 10.4161/oxim.2.2.7944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Rammal H., Bouayed J., Younos C., Soulimani R. The impact of high anxiety level on the oxidative status of mouse peripheral blood lymphocytes, granulocytes and monocytes. Eur. J. Pharmacol. 2008;589:173–175. doi: 10.1016/j.ejphar.2008.06.053. [DOI] [PubMed] [Google Scholar]
- 229.Guney E., Fatih Ceylan M., Tektas A., Alisik M., Ergin M., Goker Z., Senses Dinc G., Ozturk O., Korkmaz A., Eker S., et al. Oxidative stress in children and adolescents with anxiety disorders. J. Affect. Disord. 2014;156:62–66. doi: 10.1016/j.jad.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 230.Gałecki P., Szemraj J., Bieńkiewicz M., Florkowski A., Gałecka E. Lipid peroxidation and antioxidant protection in patients during acute depressive episodes and in remission after fluoxetine treatment. Pharmacol. Rep. 2009;61:436–447. doi: 10.1016/S1734-1140(09)70084-2. [DOI] [PubMed] [Google Scholar]
- 231.Dimopoulos N., Piperi C., Psarra V., Lea R.W., Kalofoutis A. Increased plasma levels of 8-iso-PGF2α and IL-6 in an elderly population with depression. Psychiatry Res. 2008;161:59–66. doi: 10.1016/j.psychres.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 232.Maes M., Mihaylova I., Kubera M., Uytterhoeven M., Vrydags N., Bosmans E. Increased 8-hydroxy-deoxyguanosine, a marker of oxidative damage to DNA, in major depression and myalgic encephalomyelitis / chronic fatigue syndrome. Neuroendocrinol. Lett. 2009;30:715–722. [PubMed] [Google Scholar]
- 233.Arranz L., Guayerbas N., Siboni L., De la Fuente M. Effect of acupuncture treatment on the immune function impairment found in anxious women. Am. J. Chin. Med. 2007;35:35–51. doi: 10.1142/S0192415X07004606. [DOI] [PubMed] [Google Scholar]
- 234.Szego É.M., Janáky T., Szabó Z., Csorba A., Kompagne H., Müller G., Lévay G., Simor A., Juhász G., Kékesi K.A. A mouse model of anxiety molecularly characterized by altered protein networks in the brain proteome. Eur. Neuropsychopharmacol. 2010;20:96–111. doi: 10.1016/j.euroneuro.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 235.Maes M., De Vos N., Pioli R., Demedts P., Wauters A., Neels H., Christophe A. Lower serum vitamin E concentrations in major depression. Another marker of lowered antioxidant defenses in that illness. J. Affect. Disord. 2000;58:241–246. doi: 10.1016/S0165-0327(99)00121-4. [DOI] [PubMed] [Google Scholar]
- 236.Kodydková J., Vávrová L., Zeman M., Jirák R., Macášek J., Staňková B., Tvrzická E., Žák A. Antioxidative enzymes and increased oxidative stress in depressive women. Clin. Biochem. 2009;42:1368–1374. doi: 10.1016/j.clinbiochem.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 237.Maes M., Mihaylova I., Kubera M., Uytterhoeven M., Vrydags N., Bosmans E. Lower plasma Coenzyme Q10 in depression: A marker for treatment resistance and chronic fatigue in depression and a risk factor to cardiovascular disorder in that illness. Neuroendocrinol. Lett. 2009;30:462–469. [PubMed] [Google Scholar]
- 238.Vogelzangs N., Beekman A.T.F., De Jonge P., Penninx B.W.J.H. Anxiety disorders and inflammation in a large adult cohort. Transl. Psychiatry. 2013;3:e249. doi: 10.1038/tp.2013.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Wang S.J., Zhao X.H., Chen W., Bo N., Wang X.J., Chi Z.F., Wu W. Sirtuin 1 activation enhances the PGC-1á/mitochondrial antioxidant system pathway in status epilepticus. Mol. Med. Rep. 2015;11:521–526. doi: 10.3892/mmr.2014.2724. [DOI] [PubMed] [Google Scholar]
- 240.Christmas D.M., Potokar J.P., Davies S.J.C. A biological pathway linking inflammation and depression: Activation of indoleamine 2,3-dioxygenase. Neuropsychiatr. Dis. Treat. 2011;7:431–439. doi: 10.2147/NDT.S17573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Maes M., Leonard B.E., Myint A.M., Kubera M., Verkerk R. The new ‘5-HT’ hypothesis of depression: Cell-mediated immune activation induces indoleamine 2,3-dioxygenase, which leads to lower plasma tryptophan and an increased synthesis of detrimental tryptophan catabolites (TRYCATs), both of which contribute to the onset of depression. Prog. Neuro Psychopharmacol. Biol. Psychiatry. 2011;35:702–721. doi: 10.1016/j.pnpbp.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 242.Kong S.Y., Goodman M., Judd S., Bostick R.M., Flanders W.D., McClellan W. Oxidative balance score as predictor of all-cause, cancer, and noncancer mortality in a biracial US cohort. Ann. Epidemiol. 2015;25:256–262. doi: 10.1016/j.annepidem.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Geybels M.S., Verhage B.A.J., van Schooten F.J., van den Brandt P.A. Measures of combined antioxidant and pro-oxidant exposures and risk of overall and advanced stage prostate cancer. Ann. Epidemiol. 2012;22:814–820. doi: 10.1016/j.annepidem.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 244.Ilori T.O., Wang X., Huang M., Gutierrez O.M., Narayan K.M.V., Goodman M., McClellan W., Plantinga L., Ojo A.O. Oxidative Balance Score and the Risk of End-Stage Renal Disease and Cardiovascular Disease. Am. J. Nephrol. 2017;45:338–345. doi: 10.1159/000464257. [DOI] [PubMed] [Google Scholar]
- 245.Agalliu I., Kirsh V.A., Kreiger N., Soskolne C.L., Rohan T.E. Oxidative balance score and risk of prostate cancer: Results from a case-cohort study. Cancer Epidemiol. 2011;35:353–361. doi: 10.1016/j.canep.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 246.Colpani V., Baena C.P., Jaspers L., van Dijk G.M., Farajzadegan Z., Dhana K., Tielemans M.J., Voortman T., Freak-Poli R., Veloso G.G.V., et al. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: A systematic review and meta-analysis. Eur. J. Epidemiol. 2018;33:831–845. doi: 10.1007/s10654-018-0374-z. [DOI] [PubMed] [Google Scholar]
- 247.Lakkur S., Judd S., Bostick R.M., McClellan W., Flanders W.D., Stevens V.L., Goodman M. Oxidative stress, inflammation, and markers of cardiovascular health. Atherosclerosis. 2015;243:38–43. doi: 10.1016/j.atherosclerosis.2015.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Odegaard A.O., Koh W.P., Gross M.D., Yuan J.M., Pereira M.A. Combined lifestyle factors and cardiovascular disease mortality in chinese men and women: The singapore chinese health study. Circulation. 2011;124:2847–2854. doi: 10.1161/CIRCULATIONAHA.111.048843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Abuja P.M., Albertini R. Methods for monitoring oxidative stress, lipid peroxidation and oxidation resistance of lipoproteins. Clin. Chim. Acta. 2001;306:1–17. doi: 10.1016/S0009-8981(01)00393-X. [DOI] [PubMed] [Google Scholar]
- 250.Marrocco I., Altieri F., Peluso I. Measurement and Clinical Significance of Biomarkers of Oxidative Stress in Humans. Oxidative Med. Cell. Longev. 2017;2017:6501046. doi: 10.1155/2017/6501046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.D’Arena G., Vitale C., Perbellini O., Coscia M., La Rocca F., Ruggieri V., Visco C., Di Minno N.M.D., Innocenti I., Pizza V., et al. Prognostic relevance of oxidative stress measurement in chronic lymphocytic leukaemia. Eur. J. Haematol. 2017;99:306–314. doi: 10.1111/ejh.12918. [DOI] [PubMed] [Google Scholar]
- 252.Ho E., Karimi Galougahi K., Liu C.C., Bhindi R., Figtree G.A. Biological markers of oxidative stress: Applications to cardiovascular research and practice. Redox Biol. 2013;1:483–491. doi: 10.1016/j.redox.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Montuschi P., Barnes P.J., Roberts Ii L.J. Isoprostanes: Markers and mediators of oxidative stress. FASEB J. 2004;18:1791–1800. doi: 10.1096/fj.04-2330rev. [DOI] [PubMed] [Google Scholar]
- 254.Stephens J.W., Khanolkar M.P., Bain S.C. The biological relevance and measurement of plasma markers of oxidative stress in diabetes and cardiovascular disease. Atherosclerosis. 2009;202:321–329. doi: 10.1016/j.atherosclerosis.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 255.Seyedsadjadi N., Berg J., Bilgin A.A., Tung C., Grant R. Significant relationships between a simple marker of redox balance and lifestyle behaviours; Relevance to the Framingham risk score. PLoS ONE. 2017;12:e0187713. doi: 10.1371/journal.pone.0187713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Halliwell B., Chirico S., Crawford M.A., Bjerve K.S., Gey K.F. Lipid peroxidation: Its mechanism, measurement, and significance. Am. J. Clin. Nutr. 1993;57(Suppl. 5):715S–725S. doi: 10.1093/ajcn/57.5.715S. [DOI] [PubMed] [Google Scholar]
- 257.Repetto M., Semprine J., Boveris A. Lipid Peroxidation: Chemical Mechanism, Biological Implications and Analytical Determination. IntechOpen; London, UK: 2012. [Google Scholar]
- 258.Orhan H., Gurer-Orhan H., Vriese E., Vermeulen N.P.E., Meerman J.H.N. Application of lipid peroxidation and protein oxidation biomarkers for oxidative damage in mammalian cells. A Comp. Two Fluoresc. Probes. Toxicol. Vitr. 2006;20:1005–1013. doi: 10.1016/j.tiv.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 259.Ghiselli A., Serafini M., Natella F., Scaccini C. Total antioxidant capacity as a tool to assess redox status: Critical view and experimental data. Free Radic. Biol. Med. 2000;29:1106–1114. doi: 10.1016/S0891-5849(00)00394-4. [DOI] [PubMed] [Google Scholar]
- 260.Brunelli E., La Russa D., Pellegrino D. Impaired oxidative status is strongly associated with cardiovascular risk factors. Oxidative Med. Cell. Longev. 2017;2017:6480145. doi: 10.1155/2017/6480145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Abbasi A., Corpeleijn E., Postmus D., Gansevoort R.T., de Jong P.E., Gans R.O., Struck J., Schulte J., Hillege H.L., van der Harst P., et al. Peroxiredoxin 4, a novel circulating biomarker for oxidative stress and the risk of incident cardiovascular disease and all-cause mortality. J. Am. Heart Assoc. 2012;1:e002956. doi: 10.1161/JAHA.112.002956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Kim K.N., Kim K.M., Lee D.J., Joo N.S. Serum gamma-glutamyltransferase concentration correlates with Framingham risk score in Koreans. J. Korean Med. Sci. 2011;26:1305–1309. doi: 10.3346/jkms.2011.26.10.1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Kim K.M., Kim B.T., Park S.B., Cho D.Y., Je S.H., Kim K.N. Serum Total Bilirubin Concentration Is Inversely Correlated with Framingham Risk Score in Koreans. Arch. Med Res. 2012;43:288–293. doi: 10.1016/j.arcmed.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 264.Ashfaq S., Abramson J.L., Jones D.P., Rhodes S.D., Weintraub W.S., Hooper W.C., Vaccarino V., Alexander R.W., Harrison D.G., Quyyumi A.A. Endothelial function and aminothiol biomarkers of oxidative stress in healthy adults. Hypertension. 2008;52:80–85. doi: 10.1161/HYPERTENSIONAHA.107.097386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Taleb A., Witztum J.L., Tsimikas S. Oxidized phospholipids on apoB-100-containing lipoproteins: A biomarker predicting cardiovascular disease and cardiovascular events. Biomark. Med. 2011;5:673–694. doi: 10.2217/bmm.11.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Rama Krishna Reddy Y.V., Mahendra J., Gurumurthy P., Jayamathi Babu S. Identification of predictable biomarkers in conjunction to framingham risk score to predict the risk for cardiovascular disease (CVD) in non cardiac subjects. J. Clin. Diagn. Res. 2015;9:BC23–BC27. doi: 10.7860/JCDR/2015/9089.5589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Okada K., Maeda N., Tatsukawa M., Shimizu C., Sawayama Y., Hayashi J. The influence of lifestyle modification on carotid artery intima-media thickness in a suburban Japanese population. Atherosclerosis. 2004;173:329–337. doi: 10.1016/j.atherosclerosis.2003.12.025. [DOI] [PubMed] [Google Scholar]
- 268.Giannini C., Diesse L., D’Adamo E., Chiavaroli V., de Giorgis T., Di Iorio C., Chiarelli F., Mohn A. Influence of the Mediterranean diet on carotid intima-media thickness in hypercholesterolaemic children: A 12-month intervention study. Nutr. Metab. Cardiovasc. Dis. 2014;24:75–82. doi: 10.1016/j.numecd.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 269.Marshall D., Walizer E., Vernalis M. The effect of a one-year lifestyle intervention program on carotid intima media thickness. Mil. Med. 2011;176:798–804. doi: 10.7205/MILMED-D-10-00447. [DOI] [PubMed] [Google Scholar]
- 270.Yagi H., Sumino H., Yoshida K., Aoki T., Tsunekawa K., Araki O., Kimura T., Nara M., Nakajima K., Murakami M. Biological antioxidant potential negatively correlates with carotid artery intima-media thickness. Int. Heart J. 2016;57:220–225. doi: 10.1536/ihj.15-389. [DOI] [PubMed] [Google Scholar]
- 271.Seyedsadjadi N., Berg J., Bilgin A.A., Grant R. A pilot study providing evidence for a relationship between a composite lifestyle score and risk of higher carotid intima-media thickness: Is there a link to oxidative stress? Oxidative Med. Cell. Longev. 2018;2018:4504079. doi: 10.1155/2018/4504079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.de Oliveira M.C., Schoffen J.P.F. Oxidative stress action in cellular aging. Braz. Arch. Biol. Technol. 2010;53:1333–1342. doi: 10.1590/S1516-89132010000600009. [DOI] [Google Scholar]
- 273.Griendling K.K., Touyz R.M., Zweier J.L., Dikalov S., Chilian W., Chen Y.R., Harrison D.G., Bhatnagar A. Measurement of Reactive Oxygen Species, Reactive Nitrogen Species, and Redox-Dependent Signaling in the Cardiovascular System: A Scientific Statement from the American Heart Association. Circ. Res. 2016;119:e39–e75. doi: 10.1161/RES.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Dalle-Donne I., Rossi R., Colombo R., Giustarini D., Milzani A. Biomarkers of oxidative damage in human disease. Clin. Chem. 2006;52:601–623. doi: 10.1373/clinchem.2005.061408. [DOI] [PubMed] [Google Scholar]
- 275.Milne G.L., Dai Q., Roberts L.J. The isoprostanes—25 years later. Biochim. et Biophys. Acta Mol. Cell Biol. Lipids. 2015;1851:433–445. doi: 10.1016/j.bbalip.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Vassalle C., Landi P., Boni C., Zucchelli G. Oxidative stress evaluated using an automated method for hydroperoxide estimation in patients with coronary artery disease. Clin. Chem. Lab. Med. 2007;45:367–371. doi: 10.1515/CCLM.2007.073. [DOI] [PubMed] [Google Scholar]
- 277.Teixeira D., Fernandes R., Prudêncio C., Vieira M. 3-Nitrotyrosine quantification methods: Current concepts and future challenges. Biochimie. 2016;125:1–11. doi: 10.1016/j.biochi.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 278.Ndrepepa G. Myeloperoxidase—A bridge linking inflammation and oxidative stress with cardiovascular disease. Clin. Chim. Acta. 2019;493:36–51. doi: 10.1016/j.cca.2019.02.022. [DOI] [PubMed] [Google Scholar]
- 279.Najafi M., Roustazadeh A., Alipoor B. Ox-LDL Particles: Modified Components, Cellular Uptake, Biological roles and clinical assessments. Cardiovasc. Hematol. Disord. Drug Targets. 2011;11:119–128. doi: 10.2174/187152911798346990. [DOI] [PubMed] [Google Scholar]
- 280.Pellegrini N., Vitaglione P., Granato D., Fogliano V. Twenty-five years of total antioxidant capacity measurement of foods and biological fluids: Merits and limitations. J. Sci. Food Agric. 2020;100:5064–5078. doi: 10.1002/jsfa.9550. [DOI] [PubMed] [Google Scholar]
- 281.Natoli G., Ghisletti S., Barozzi I. The genomic landscapes of inflammation. Genes Dev. 2011;25:101–106. doi: 10.1101/gad.2018811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Monastero R.N., Pentyala S. Cytokines as Biomarkers and Their Respective Clinical Cutoff Levels. Int. J. Inflamm. 2017;2017:4309485. doi: 10.1155/2017/4309485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Davalos D., Akassoglou K. Fibrinogen as a key regulator of inflammation in disease. Semin. Immunopathol. 2012;34:43–62. doi: 10.1007/s00281-011-0290-8. [DOI] [PubMed] [Google Scholar]
- 284.Maeda S., Takeya Y., Oguro R., Akasaka H., Ryuno H., Kabayama M., Yokoyama S., Nagasawa M., Fujimoto T., Takeda M., et al. Serum albumin/globulin ratio is associated with cognitive function in community-dwelling older people: The Septuagenarians, Octogenarians, Nonagenarians Investigation with Centenarians study. Geriatr. Gerontol. Int. 2019;19:967–971. doi: 10.1111/ggi.13751. [DOI] [PubMed] [Google Scholar]
- 285.Suh B., Park S., Shin D.W., Yun J.M., Keam B., Yang H.K., Ahn E., Lee H., Park J.H., Cho B. Low albumin-to-globulin ratio associated with cancer incidence and mortality in generally healthy adults. Ann. Oncol. 2014;25:2260–2266. doi: 10.1093/annonc/mdu274. [DOI] [PubMed] [Google Scholar]
- 286.Wang Q., Liu D., Song P., Zou M.H. Tryptophan-kynurenine pathway is dysregulated in inflammation, and immune activation. Front. Biosci. Landmark. 2015;20:1116–1143. doi: 10.2741/4363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Gieseg S.P., Baxter-Parker G., Lindsay A. Neopterin, inflammation, and oxidative stress: What could we be missing? Antioxidants. 2018;7:80. doi: 10.3390/antiox7070080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Del Giudice M., Gangestad S.W. Rethinking IL-6 and CRP: Why they are more than inflammatory biomarkers, and why it matters. Brain Behav. Immun. 2018;70:61–75. doi: 10.1016/j.bbi.2018.02.013. [DOI] [PubMed] [Google Scholar]
- 289.Dinicolantonio J.J., O’Keefe J.H. Importance of maintaining a low omega-6/omega-3 ratio for reducing inflammation. Open Heart. 2018;5:1–4. doi: 10.1136/openhrt-2018-000946. [DOI] [PMC free article] [PubMed] [Google Scholar]