Abstract
Approximately 19% of all cancer-related deaths are due to lung cancer, which is the leading cause of mortality worldwide. Small cell lung cancer (SCLC) affects approximately 15% of patients diagnosed with lung cancer. SCLC is characterized by aggressiveness; the majority of SCLC patients present with metastatic disease, and less than 5% of patients are alive at 5 years. The gold standard of SCLC treatment is platinum and etoposide-based chemotherapy; however, its effects are short. In recent years, treatment for SCLC has changed; new drugs have been approved, and new biomarkers are needed for treatment selection. Liquid biopsy is a non-invasive, rapid, repeated and alternative tool to the traditional tumor biopsy that could allow the most personalized medicine into the management of SCLC patients. Circulating tumor cells (CTCs) and cell-free DNA (cfDNA) are the most commonly used liquid biopsy biomarkers. Some studies have reported the prognostic factors of CTCs and cfDNA in SCLC patients, independent of the stage. In this review, we summarize the recent SCLC studies of CTCs, cfDNA and other liquid biopsy biomarkers, and we discuss the future utility of liquid biopsy in the clinical management of SCLC.
Keywords: lung cancer, SCLC, liquid biopsy, cfDNA, CTC
1. Introduction
Small cell lung cancer (SCLC) accounts for approximately 15% of all lung cancers diagnosed worldwide and up to 25% of lung cancer deaths [1]. The majority of patients with SCLC present with metastatic disease, and the prognosis is poor, with less than 5% of patients alive at 5 years. SCLC diagnosis is performed by morphological assessment of a tissue biopsy or cytology sample. Radiological staging with the conventional TNM criteria is recommended, but according to the Veterans Administration of Lung Study Group staging, SCLC is classified into two stages: limited disease (LD-SCLC), when it is confined to a hemithorax, where curative treatment with radiochemotherapy is feasible; or extensive disease (ED-SCLC), defined as the presence of metastatic disease outside the hemithorax at first diagnosis [2].
Liquid biopsy, principally circulating tumor cells (CTCs) and cell-free DNA (cfDNA), has the potential to improve the management of SCLC at different levels: screening, minimal residual disease detection, monitoring systemic treatment initiation and response and determining the development of resistance. These techniques generate promising data to better understand SCLC biology and guide patient treatment [3]. This review will focus on the current and future clinical utility of liquid biopsies, which represent a key factor in improving outcomes for patients with SCLC.
2. Clinical Management of SCLC
2.1. Small Cell Lung Cancer Treatment Landscape
Systemic treatment of SCLC patients is based on the combination of platinum and etoposide-based chemotherapy, and recently, the use of immunotherapy has also been incorporated in patients with metastatic disease [4,5,6,7]. The goal of LD-SCLC therapy is to cure. Surgery is an option to treat patients who are diagnosed with tumors smaller than 3 cm in size and without hilar lymph node metastasis [7]. However, in most patients, the standard treatment is the combination of platinum plus etoposide chemotherapy administered concurrently with radiotherapy. Unfortunately, the prognosis of these patients is poor; specifically, the median overall survival (OS) of patients with LD-SCLC ranges from 23 to 30 months, with an estimated 2-year survival rate ranging from 47 to 56% [4,5]. Radiation therapy is also an important part in the treatment of every stage of SCLC, in curative as well as in palliative therapy, and it is changing in recent years [8]. For this reason, its role remains somewhat controversial [9,10]. There is consensus that thoracic radiation should be considered in patients with residual disease after chemotherapy, with a range of doses being appropriate. Moreover, it must also be considered after chemo-immunotherapy in patients with residual disease [9].
Regarding their response to first-line treatments, SCLC patients are classified as chemorefractory or chemosensitive, and this trait is a key factor in guiding the choice of second-line therapy. Chemorefractory disease is defined as the occurrence of progression during first-line therapy or within 90 days of its completion. If the time to progression after chemotherapy is greater than 90 days, the disease is defined as chemosensitive. This classification is a prognostic factor for early recurrence and reduced response to subsequent cytotoxic therapies; however, it might not be relevant to the clinical development of novel therapies [11].
Unfortunately, the majority of SCLC patients progress on treatment, and the choice of the second-line treatment is topotecan or cyclophosphamide, doxorubicin and vincristine (CAV), with poor results [12]. However, recently, new drugs have been approved in this setting. For instance, lurbinectedin has been approved by the US Food and Drug Administration (FDA) for salvage treatment of SCLC that has relapsed from platinum compound-based, first-line chemotherapy [13]. Currently, the efficacy of the lurbinectedin plus doxorubicin combination is being investigated in the randomized phase 3 trial ATLANTIS (NCT02566993) [14]. However, this study appears not to meet the pre-specified criteria of significance for the primary endpoint of OS in the intent-to-treat (ITT) population, comparing lurbinectedin in combination with doxorubicin to the control arm (https://pharmamar.com/wp-content/uploads/2020/12/PR_PhM_and_Jazz_anounce_results_ATLANTIS_DEF.pdf, last accessed on 21 December 2020). Nivolumab and pembrolizumab have also been approved by the FDA for refractory SCLC based on the results of the CheckMate-032 (NCT01928394) and Keynote-158 (NCT02628067) clinical trials, respectively [15,16]. However, in the Checkmate-331 trial (NCT02481830), nivolumab failed to demonstrate an improvement in OS versus standard treatment in patients with relapsed or refractory SCLC treated with a platinum-based line of chemotherapy [17].
On the other hand, first-line treatment in patients with ED-SCLC is undergoing great changes, especially in the field of immunotherapy. For example, blocking the programmed death 1 receptor (PD-1) or its ligand (PD-L1) pathway has been shown to improve the prognosis of patients with ED-SCLC [18,19]. The Impower 133 (NCT02763579) and CASPIAN phase III trials (NCT03043872) demonstrated that adding atezolizumab or durvalumab to platinum plus etoposide chemotherapy improves OS and progression-free survival (PFS) compared to chemotherapy alone [20,21]. More recently, the KEYNOTE-604 (NCT03066778) study reported that combining pembrolizumab with platinum and etoposide improves PFS but does not significantly improve OS in patients with ED-SCLC [22].
2.2. New Therapies
In another type of tumor, non-small cell lung adenocarcinoma, growing knowledge of its molecular characteristics, especially driver mutations, has been accompanied by the development of targeted drugs that have significantly improved survival. By contrast, the identification of new therapeutic targets in SCLC has been challenging, partly because driver mutations are primarily loss of function (genes RB1 and TP53) or currently difficult to target [23,24].
Recent advances have made it possible to deepen the molecular knowledge of SCLC, which has allowed us to distinguish between four different subtypes characterized by distinct gene expression profiles. These subtypes are the neuroendocrine subtypes SCLC-A (ASCL1-positive) and SCLC-N (NEUROD1-positive) and the non-neuroendocrine subtypes SCLC-P (POU2F3-positive) and SCLC-Y (YAP1-positive) [25]. Previous work has demonstrated activity of CDK4/6 inhibitors in RB1 wild-type SCLC cell lines [26,27]. Based on these results, a clinical trial is testing abemaciclib, a CDK4/6 inhibitor, as a single agent in ED-SCLC patients with wild-type RB1, with platinum refractory disease (ClinicalTrials.gov Identifier NCT04010357).
Moreover, genomic analyses have determined that SCLC tumors present extensive copy number alterations (CNAs) and high mutation rates, although SCLCs are not characterized by homologous recombination (HR) deficiency or mutations in BRCA1/2 [28,29]. The development of new drugs for SCLC patients should be based on a better understanding of the nature of these subtypes, characterizing their differences, similarities and what determines their growth, patient survival rates and tendency to metastasize. In this sense, poly [ADP ribose] polymerase (PARP), delta-like canonical Notch ligand 3 (DLL3) in SCLC-A subtypes and Aurora kinase in SCLC-A constitute promising drug targets [30,31].
Veliparib is an oral PARP inhibitor that potentiated standard chemotherapy against SCLC in preclinical studies. The addition of veliparib to front-line cisplatin and etoposide chemotherapy has shown a potential benefit in PFS in ED-SCLC [32]. In relapsed or refractory SCLC patients, veliparib plus temozolomide failed to find improvement in PFS compared to placebo plus temozolomide [33]. However, in patients with high SLFN11 expression, veliparib significantly prolonged PFS and OS; thus, SLFN11 has been postulated as a new drug target [33,34]. Although it has not yet found an application in daily clinical practice, the usefulness of SLFN11 expression is being explored to select patients who may benefit from adding veliparib to maintenance treatment with atezolizumab in stage IV SCLC patients (ClinicalTrials.gov Identifier NCT04334941).
Rovalpituzumab tesirine (Rova-T) is an antibody–drug conjugate designed to specifically target delta-like ligand 3 (DLL3). Initially, in a human phase I trial, Rova-T showed a promising signal of activity [35]. Unfortunately, Rova-T has not been superior to second-line treatment in two randomized trials, and its development is compromised in this setting. Alisertib is an investigational, oral, selective inhibitor of Aurora kinase A. In patients with refractory or recurrent SCLC, alisertib has been shown to be active both in monotherapy and in combination with paclitaxel [36,37].
All of these therapeutic approaches have opened new horizons and hopes for improving SCLC outcomes. However, more research is still required to reach a better understanding of the molecular mechanisms that can be used to find new predictive biomarkers to apply the most convenient therapeutic strategy for each patient, and the field of liquid biopsy would be crucial for this objective.
3. Liquid Biopsy as a Clinical Tool in SCLC
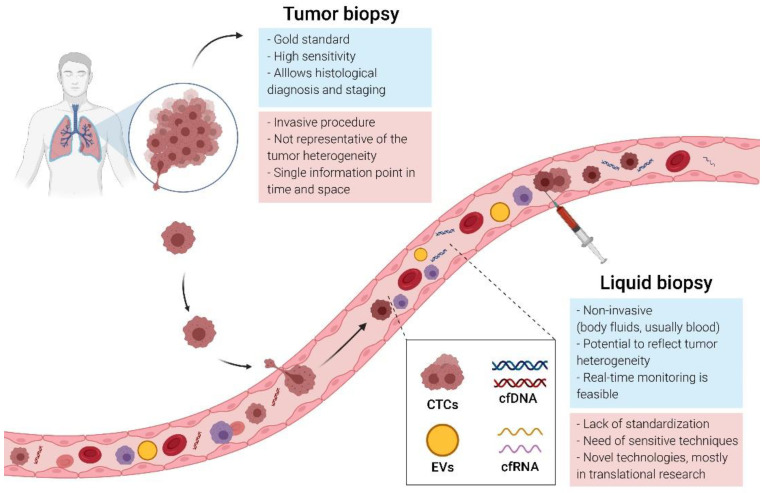
Tumor molecular profiling is essential for optimizing treatment in clinical practice, and tissue biopsy or cytology samples remain the gold standard. However, a tissue biopsy requires invasive procedures and is not always possible or repeatable (Figure 1). In lung cancer, fine-needle aspirates or biopsy samples are often of poor quality or quantity, and up to 25% of biopsies fail to obtain enough tissue for assessment [38], justifying the need to explore new diagnostic tools. In SCLC, due to their intratumoral and intertumoral heterogeneity, tumor samples obtained from a single biopsy may not capture the complete genomic profile of tumors, considering that the biopsy is a partial photograph of the tumor at a specific time. Additionally, the genomic landscape of SCLC can change during the course of therapy, and the follow-up of this dynamic process with repeated sampling is essential, which is difficult to address based on solid samples. Liquid biopsy has emerged as a rapid and noninvasive alternative to obtain a more complete image of the disease and to monitor its evolution over time and as a consequence of treatment pressure [39,40]. Indeed, recently, the possibility of early detection of cancer using liquid biopsy has been reported in diverse tumor types [41,42], although in SCLC, this application has been infrequently explored.
Figure 1.
Tissue versus liquid biopsy: comparison of the advantages and limitations.
Overall, liquid biopsy is used to refer to analytes from various biological fluids, such as blood or other accessible fluids: ascites, pleural effusions, saliva or urine. The term primarily refers to circulating tumor cells (CTCs), cell-free DNA (cfDNA), circulating cell-free RNA (cfRNA) and circulating extracellular vehicles (EVs), among others [43] (Figure 1). Clinical applications of these circulating biomarkers include the early detection of cancer, tumor recurrence, therapy monitoring, detection of drug resistance and predictive response [38,44]. Although the application of liquid biopsy is infrequent in SCLC, promising advances have been achieved in recent years. In this review, we summarize the current state of knowledge on CTCs and cfDNA assays in SCLC. We also highlight potential future research directions in liquid biopsy-based approaches.
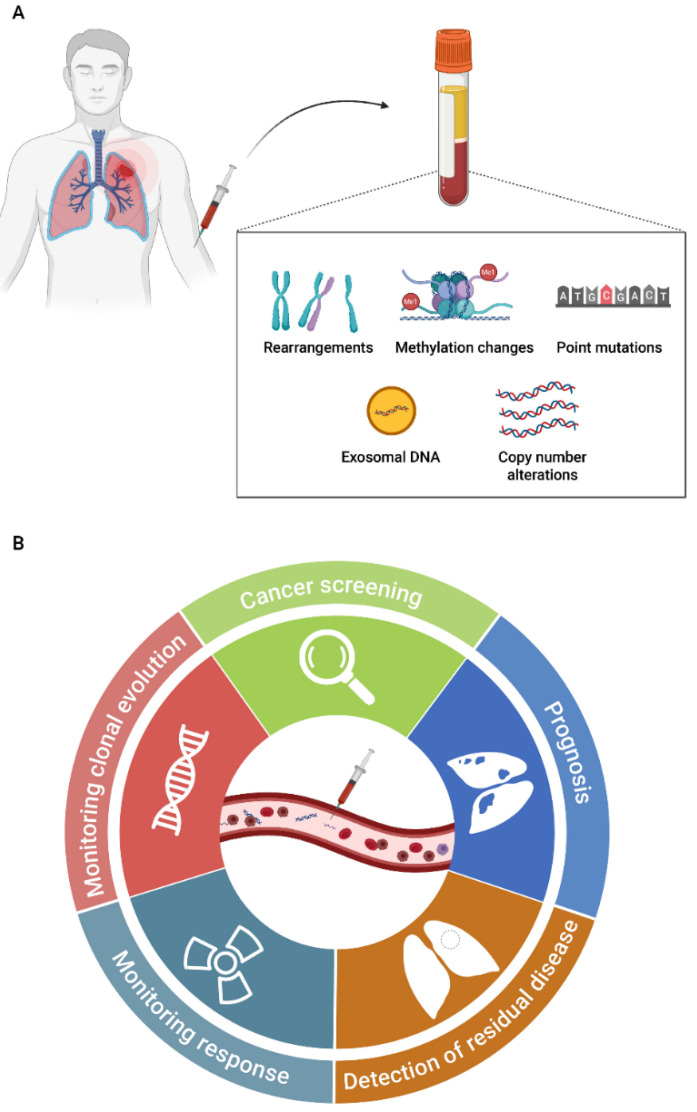
3.1. Cell-Free DNA
Cell-free DNA (cfDNA) was first reported in healthy and diseased individuals by Mandel and Métais in 1948 [45]. Later, Leon et al. described cfDNA for the first time in the field of oncology, reporting cfDNA levels higher in cancer patients than in healthy individuals [46]. cfDNA comprises extracellular DNA molecules (double-stranded DNA and mitochondrial DNA) released into the blood and other fluids through different mechanisms, including apoptosis, necrosis, senescence and active secretions [47,48] (Figure 2A). The short half-life of cfDNA varies from several minutes to 1–2 h, enabling real-time monitoring of molecular biomarkers for response or relapse and serving as a perfect biomarker to monitor cancer evolution [47].
Figure 2.
Potential clinical applications of ctDNA in small cell lung cancer (SCLC) patients. (A) Range of alterations in cell-free DNA; (B) applications of ctDNA analysis during the course of the disease management.
During the last decade, a type of cfDNA, the tumor-derived fraction of cfDNA, or circulating tumor DNA (ctDNA), specifically present in cancer patients, has received much attention in the field of oncology (Figure 2A). The circulating tumor DNA concentration varies from 0.01% to 1% of total cfDNA in early-stage disease to over 40–90% for late-stage disease [49,50]. It tends to be more fragmented than cfDNA, with sizes ranging from 90 to 150 base pairs. Circulating tumor DNA has value in early cancer detection and can be used to determine the tissue of origin and prognosis; to monitor response and assess potential resistance to the treatments; and to detect minimal residual disease [51] (Figure 2B). Of note, a desired cfDNA assay should: (1) quantify ctDNA in order to monitor the presence and extend the disease and (2) identify ctDNA alterations that can help to make therapeutic decisions. In fact, ctDNA detection technologies could lead to personalization of therapy based on the identification of somatic alterations present in tumors and their changes during therapy administration, which have been associated with clinical outcomes in several cancer types [52,53,54,55,56].
3.1.1. Circulating Tumor DNA Detection Technologies
The low concentration of ctDNA into total cfDNA involves a challenge for detecting genetic alterations (point mutations, CNAs or small indels), particularly at the early stages of tumor development. Two principal approaches have been developed to solve this challenge. First, the detection of single or a low number of point mutations using highly sensitive and specific techniques has a rather fast and cost-effective rate [57]. These techniques include assays based on qPCR, such as the Cobas EGFR mutations Test v2, which was approved in 2016 by the FDA and the European Medicines Agency (EMA) in NSCLC patients [58], and the Idylla platform. Additionally, assays based on digital PCR (BEAMing and droplet digital PCR (ddPCR)) can detect specific known mutations, showing high concordance with results obtained in tumor tissue [59,60,61], with high sensitivity (0.001–0.005%) [62]. However, in these approaches, previous information about the tumor type and the common mutations is needed. The second type of approach is focused on a genome-wide analysis of CNAs or point mutations through next-generation sequencing (NGS) strategies. This genome-wide characterization allows a more complete and patient-specific genotyping to assess tumor heterogeneity and to follow the clonal evolution across the treatment. The principal limitations of NGS-based strategies are the high cfDNA input requirement and general low sensitivity (5–10%) [51,57]. Fortunately, the technologies are improving very fast, and there are options of comprehensive targeted NGS panels able to detect genetic alterations present in lower frequencies <1% [63]. More recently, a third strategy based on the combined analysis of DNA methylation and fragmentation with targeted or wide-genome sequencing to improve ctDNA detection in early tumor stages has been described [64,65]. It has been well reported that smoking history, environment and age affect DNA methylation status [66,67]. Therefore, methylation analyses of cfDNA in cancer, and specially in SCLC patients, where the rate of smokers is high, should be performed with caution.
3.1.2. Cell-Free DNA Studies in SCLC
Due to the rapid growth and highly metastatic capacity of SCLC tumors, as well as the high levels of cfDNA in SCLC patients, cfDNA analyses should allow for better characterization of the tumor. However, few studies have analyzed the role of cfDNA in SCLC (Table 1). TP53 and RB1 alterations play an essential role in SCLC tumorigenesis [28] and are also present at relapse, representing valuable targets to monitor ctDNA levels. Thus, Fernandez-Cuesta et al. studied the possibility of detecting TP53 mutations in SCLC patients using cfDNA samples [49]. Their results show the potential to detect TP53 mutations in cfDNA of 49% of patients (with different tumor stages) and, more importantly, in the 35.7% of early-stage patients, demonstrating the potential of cfDNA as a promising tool for the early detection of SCLC patients with TP53 mutations. However, they also found the presence of TP53 mutations in healthy controls (11.1%). In fact, the appearance of germline mutations due to clonal hematopoiesis constitutes an aspect to take into account for the development of ctDNA screening tests. This finding has led to the recommendation to include the blood cell fraction in NGS studies, although the percentage of variants associated with the phenomenon of clonal hematopoiesis is normally low [68]. Based on an NGS strategy, Almodovar et al. analyzed serial plasma samples of 11 LD-SCLC and 16 ED-SCLC patients using a custom panel of the most frequently mutated genes in SCLC tumors, including TP53 and RB1 [69]. Somatic variations were found in 85% of the patients, with TP53 and RB1 being the most common altered genes, in line with previous studies [70]. The results of this study also showed that ctDNA monitoring could identify disease recurrence prior to disease progression detected on imaging or in cases with ambiguous imaging findings. Moreover, increased cfDNA levels in SCLC patients were associated with worse OS [69]. To determine the subclonal architecture of SCLC and its molecular evolution during treatment, Nong et al. analyzed cfDNA samples from 22 SCLC patients before treatment onset and at different points within therapy using a panel that covers 430 genes altered in cancer [71]. They detected mutations in all patients at baseline, the most common being TP53 mutations, observed in 91% (20/22) of patients, together with RB1 mutations, observed in 64% (14/22) of patients. Moreover, in eight patients, both plasma and tissue samples were analyzed, showing a concordance of 94% for mutations, indicating that cfDNA sequencing is a sensitive tool to detect somatic mutations in SCLC patients. Despite this high concordance, in one patient, none of the 26 mutations detected in tumor tissue were detected in cfDNA, while two of the discordant cases became positive after increasing the sequencing depth. Importantly, a subset of mutations was exclusively detected in cfDNA in some patients. In addition, high cfDNA levels were associated with significantly worse PFS and OS. Overall, this study demonstrated a similar subclonal architecture between tissue and cfDNA, supporting the use of cfDNA for the detection of somatic mutations and studying the molecular heterogeneity of SCLC [71].
Table 1.
Summary of cfDNA studies in SCLC.
| Study | Cohort (LD-SCLC/ED-SCLC) | Method | Main Results |
|---|---|---|---|
| Morgensztern D et al., 2016 [70] | 134 patients | NGS (Guardant360) | 132/134 (92.3%) of patients had at least one mutation. The most common mutations were found in TP53 (70%) and RB1 (32%). |
| Fernandez-Cuesta L et al., 2016 [49] | 51 (42/9) patients and 225 healthy controls | NGS (Custom panel) | 25/51 (49%) patients had mutations in TP53. 25/225 (11.1%) controls had mutations in TP53. |
| Ou S.H.I et al., 2017 [74] | 1 NSCLC patients transform to SCLC | NGS (FoundationACT) | An NSCLC with an ALK fusion transforms the histology into SCLC. |
| Almodovar K et al., 2018 [69] | 27 (11/16) patients | NGS (Custom panel of 14 genes) | 23/27 (85%) patients had disease-associated mutations. The most common altered genes were TP53 (70%) and RB1 (52%). Changes in cfDNA levels correlated with response to therapy and relapse. |
| Nong J et al., 2018 [71] | 22 (11/11) patients | NGS (Custom panel of 430 genes) | All patients had at least one mutation. Mutations were mostly found in TP53 (91%) and RB1 (64%). 94% of mutations detected in tumor DNA were also detected in the paired ctDNA sample. High cfDNA levels in SCLC patients were associated with significantly worse PFS and OS. |
| Du M et al., 2018 [72] | 24 (11/13) patients | WGS for CNA and NGS (xGen Pan-Cancer Panel) | 16/24 (66.7%) of patients had CNAs. All patients had any mutation. TP53 and RB1 mutations were found in 4/17 patients (23.5%). A higher mutation risk index was strongly associated with poor PFS and OS. |
| Devarakonda S et al., 2019 [75] | 564 patients | NGS (Guardant360) | 94% of patients had at least one mutation or amplification. The most common mutations were found in TP53 (72.5%) and RB1 (18%). A higher percentage of alterations in APC and AR were observed in samples obtained at relapse. |
| Mohan S et al., 2020 [73] | 69 (39/30) patients and 32 healthy controls | WGS for CNA and NGS (Custom panel of 110 genes) |
58/62 (94%) of patients had at least one mutation. Most of the mutations were found in TP53 (79%) and RB1 (34%). 0/23 (0%) controls had genetic alterations. The presence of CNAs was associated with OS, being a potential prognostic factor and monitoring tool in SCLC patients. |
| Iams W.T et al., 2020 [76] | 23 LD-SCLC patients | NGS (Custom panel of 14 genes) | Detection of ctDNA in patients with LS-SCLC after curative intent therapy predicts disease relapse and death. |
Abbreviations: SCLC: small cell lung cancer; NGS: next-generation sequencing; NSCLC: non-small cell lung cancer; WGS: whole-genome sequencing; CNA: copy number alteration; cfDNA: cell-free DNA; ctDNA: circulating tumor DNA; PFS: progression-free survival; OS: overall survival LD-SCLC: limited disease SCLC.
Similarly, Du et al. demonstrated the feasibility of using cfDNA for genomic profiling and prognostication in a cohort of 24 SCLC patients (11 LD-SCLC and 13 ED-SCLC) [72]. They reported the presence of CNAs in 66.7% of patients and the presence of point mutations in all patients. The most common genetic alterations occurred in KMT2D and NCOR1, while the presence of SETBP1, PBRM1, ATM and ATXR mutations was associated with patient survival. A higher mutation risk index was strongly related to poor PFS and OS. A subsequent study demonstrated that a simple cfDNA-based genome-wide copy number approach was an effective tool for monitoring patients during treatment and that targeted cfDNA sequencing identifies potential therapeutic targets in more than 50% of SCLC patients [73]. CNAs were observed in 84% of patients, with a gain in copy number for SOX2, MYC, NFIB and CD274 and losses for CNTN3, FHIT, RASSF1, RB1 and KIF2A, showing significant differences between LD-SCLC and ED-SCLC.
Devarakonda et al. analyzed cfDNA from a larger cohort of SCLC patients using NGS at diagnosis and when the disease relapsed [75]. The results reported that 552 of a total of 609 (94%) patients had at least one point mutation or amplification (531/609). The most commonly altered genes were TP53 (72.5%) and RB1 (18%). Moreover, the authors observed a higher percentage of alterations in APC and AR in samples obtained at relapse. Recently, it has been hypothesized that the detection of ctDNA in patients with LS-SCLC after definitive therapy would predict disease relapse and death, after showing that residual ctDNA can be detected prior to radiographic relapse [76]. Overall, all of these studies demonstrate that cfDNA analyses constitute a powerful tool for SCLC diagnosis, therapy selection and monitoring that can be a key element to improve this tumor management in the close future.
3.2. Circulating Tumor Cells
CTCs are tumor cells originating from the primary or metastatic sites that are able to enter the circulation and disseminate to distant sites. Peripheral blood offers the possibility to analyze the presence of this circulating tumor population for cancer diagnosis and disease monitoring. The importance of CTCs for diagnostic and prognostic purposes has been well reported in different cancer types, such as metastatic breast [77,78], prostate [79], NSCLC [80] and colorectal cancer [81]. Of note, in SCLC, several studies have reported higher CTC levels in comparison to other cancer types [82], supporting the interest of this circulating population as an accessible tumor biopsy (Table 2).
Table 2.
Summary of studies that analyzed circulating tumor cells (CTCs) in SCLC.
| Study | Cohort (LD-SCLC/ED-SCLC) | Platform | Main Results |
|---|---|---|---|
| Hou J.M et al., 2009 [109] | 50 (20/30) | CellSearch with CD56 in the 4th channel | CTCs were detected in 86% of patients at baseline. Increased CTC counts at baseline and after 22 days of treatment were associated with worse OS. |
| Hiltermann T.J.N et al., 2012 [99] | 59 (21/38) | CellSearch | CTCs were detected in 73% of patients at baseline. At baseline, the presence of <2 CTCs was associated with OS. Lower number of CTCs in LD-SCLC (median = 6) compared with ED-SCLC (median = 63). CTCs levels decreased after one cycle of chemotherapy. No changes were found after 4 cycles of treatment. |
| Hou J.M et al., 2012 [100] | 97 (31/66) | CellSearch | CTCs were detected in 85% of patients at baseline. OS was poorer for patients with ≥50CTCs/7.5 mL at baseline. |
| Naito T et al., 2012 [108] | 51 (27/24) | CellSearch | ≥2 CTCs were detected in 68.6% of patients at baseline. Lower number of CTCs in LD (median = 1) compared with ED-SCLC (median = 9.5). Patients with ≥8 CTCs had worse survival than those with <8 CTCs. |
| Igawa S et al., 2014 [113] | 30 (8/22) | TelomeScan | CTCs were detected in 96% of patients at baseline. ≥2 CTCs at baseline was associated with OS. |
| Normanno N et al., 2014 [104] | 60 ED | CellSearch | CTCs were detected in 90% of patients at baseline. Reduction in CTC number >89% was associated with lower risk of death. |
| Huang C.H et al., 2014 [106] | 26 ED | CellSearch | Non-significant association was reported between CTCs at baseline and PFS, or OS, but trended towards significance. |
| Cheng Y et al., 2016 [105] | 86 ED | CellSearch | CTCs were detected in 87.6% of patients at baseline. ≥10 CTCs levels were associated with OS. ≥10 CTCs after the second chemotherapy cycle was associated with PFS and OS. |
| Chudziak J et al., 2016 [96] | 12 (2/10) | Parsortix vs. CellSearch | CTCs were detected in 100% of patients at baseline using Parsortix and in 83.33% of patients using CellSearch. Parsortix system is a valuable tool for CTC enrichment that enables CTC analysis independently on surface epitopes. |
| Carter L et al., 2017 [11] | 13 | CellSearch and DEPArray | CTCs were detected in 100% of patients at baseline. Single-cell analyses of CTCs allowed classifying patients with chemosensitive disease and chemorefractory disease. |
| Messaritakis I et al., 2017 [101] | 62 (22/40) | CellSearch | CTCs were detected in 62.1% of patients at baseline. Increased CTC count at baseline was associated with worse PFS and OS. Increased CTC count after one cycle of treatment was associated with poorer OS. |
| Messaritakis I et al., 2018 [102] | 108 (37/71) | CellSearch | CTCs were detected in 60.2% of patients at baseline. Increased CTC count at baseline and at progressive disease was associated with worse PFS and OS, respectively. |
| Salgia R et al., 2017 [107] | 42 ED-SCLC in clinical trial | CellSearch + CXCR4 expression | CTCs were detected in 83.3% of patients at baseline. ≥6 CTCs/7.5 mL blood at baseline and post-treatment (cycle 2, day 1) was predictive of worse PFS and OS. |
| Aggarwal C et al., 2017 [103] | 50 (20/30) | CellSearch | CTCs were detected in 94% of patients at baseline. Lower number of CTCs in LD-SCLC (median = 1.5) compared with ED-SCLC (median = 71). Patients with <5 CTCs were associated with longer PFS. Patients with <50 CTCs were associated with longer OS and PFS. |
| Su Z et al., 2019 [116] | 48 (8/40) | CellSearch | CTCs were detected in 100% of patients at baseline. The CNAs analyses predict the response to first line of chemotherapy. |
| Obermayr E et al., 2019 [112] | 48 (4/31/13 unknown) | Parsortix | CTCs were detected in 31.4% of patients at baseline. CTCs in SCLC patients can be assessed using epithelial and neuroendocrine cell lineage markers at the molecular level. |
| Mohan S et al., 2020 [73] | 48 (28/20) | CellSearch | CTCs were detected in 77.1% of patients at baseline 77.1% (24 of the 28 with ED-SCLC and 13 of the 20 with LD-SCLC). The mean and median CTC numbers per 7.5 mL of blood were 523 and 5, respectively (range 0–15,352). |
| Wang P et al., 2020 [114] | 138 | Fluorescence in situ hybridization | CTCs could be a predictive and prognostic factor for SCLC. Authors reported a nomogram model using CTCs and a clinical parameter to predict the median survival time of SCLC patients. |
Abbreviations: SCLC: small cell lung cancer; CTC: circulating tumor cell; LD-SCLC: limited disease SCLC; ED-SCLC: extensive disease SCLC.; OS: overall survival; CNAs: copy number alterations; PFS: progression-free survival.
The proportion of CTCs in the bloodstream is very low, approximately 1 CTC per 106–107 leukocytes [83]. CTCs are released from the primary tumor into the blood and have a very short half-life (1–2.4 h) [84]. The majority of these cells are rapidly cleared; however, some of them evade recognition by immune cells, survive into the bloodstream and can reach distant locations to generate metastasis [85,86,87]. These cells are characterized by a hybrid phenotype in terms of epithelial and mesenchymal markers that favor their survival in circulation [86,87,88,89].
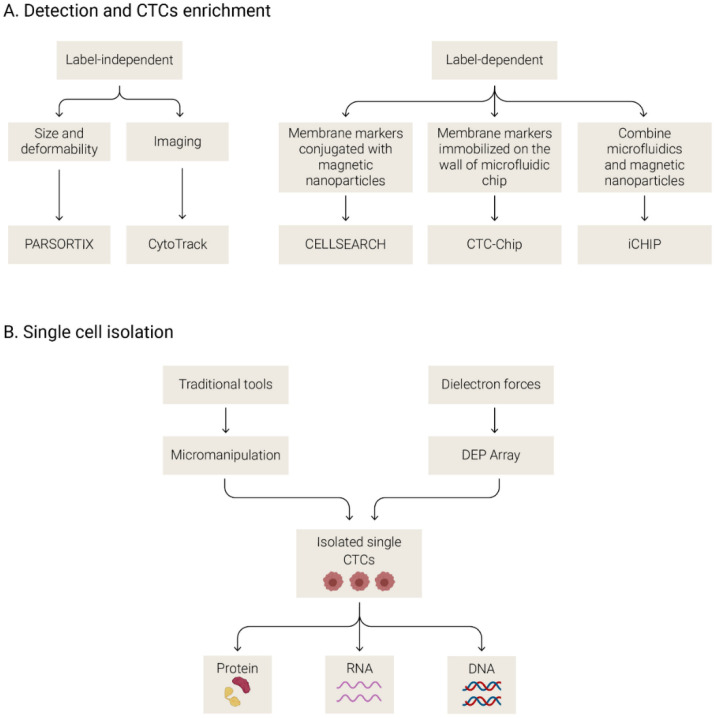
3.2.1. Methods to Isolate and Analyze CTCs
The low proportion of CTCs in the bloodstream together with the molecular heterogeneity that characterizes these cells is the principal challenge for CTC isolation and detection. Several CTC detection platforms have been developed in the past decade. Each technology isolates CTCs and focuses on differential features between CTCs and blood cells, such as protein expression, morphology, volume and biophysical properties, presenting different advantages and limitations.
These technologies can be categorized based on the method of isolation as label-dependent (affinity-based) or label-independent [90] (Figure 3A). The label-dependent methods are the most commonly used approaches and are based on the expression of cell surface markers (such as EpCAM). These methods use antibodies against membrane markers conjugated with magnetic nanoparticles or immobilized on the walls of microfluidic chips. They are also called immune-based detection methods, and the most commonly used is the CellSearch system (Menarini, Silicon Biosystem, Bologna, Italy). The CellSearch system employs anti-EpCAM-coated ferrofluid nanoparticles for the selection of EpCAM-positive CTCs. Then, after an immunostaining step, CTCs are discriminated from leukocytes based on the positive expression of cytokeratins and the absence of CD45 staining (leukocyte marker) together with morphologic criteria. This system has been used for many years as the reference technology because it is a unique system with FDA approval for clinical use in metastatic breast, prostate and colorectal cancer [81,91,92]. However, this approach has the limitation of only isolating CTCs based on EpCAM expression, ignoring other low epithelial CTCs [93]. On the other hand, label-independent approaches allow the isolation of CTCs with a low epithelial phenotype because these platforms discriminate CTCs from other cells based on physical characteristics such as size, density, deformability and electrical properties [90]. For example, there are size-based separation methods [94] (filter-based detection, microfluidic chips, centrifugal forces or inertial focusing) and direct imaging and biophysical property-based methods [90,95]. Other methods combine antigen-based capture with the advantages of microfluidics methods, such as CTC-iChip for increasing the isolation efficacy [90]. Due to the similar size of leukocytes and CTCs in SCLC patients, label-independent approaches based on the cell size are less efficient than in other tumors [96]. This carryover of leukocytes is seen in all CTC enrichment platforms, and when the objective is the enumeration of CTCs, a posterior step of labeling CTCs with specific antibodies is needed. Furthermore, after the detection of CTCs, some platforms allow the isolation of pure CTCs at the single-cell or cluster level by the use of micromanipulation or via dielectron force manipulation (DEPArray system), among other strategies [97] (Figure 3B). Analyses of individual CTCs/clusters at the DNA, RNA or protein level provide valuable information about the molecular heterogeneity of these cells and a more precise characterization of the disease [98].
Figure 3.
Different strategies for circulating tumor cells enrichment and detection (A) and single cell isolation (B).
3.2.2. Circulating Tumor Cells in SCLC
The most commonly used platform to isolate CTCs in SCLC studies has been the CellSearch platform (Table 2), reporting a detection rate of 60.2–94% of SCLC patients with at least 1 CTC per 7.5 mL of blood before treatment [99,100,101,102,103,104,105,106,107]. Naito et al. detected ≥2 CTCs/7.5 mL in 68% of SCLC patients before treatment [108]. This percentage of positivity is clearly higher than in other tumors. Furthermore, high CTC numbers have been associated with the clinical stage and presence of liver metastases, representing a prognostic factor for survival [100,109]. In fact, numerous studies have reported differences in the number of CTCs detected between patients with LD-SCLC and ED-SCLC. Hilterman et al. reported that the levels of CTCs detected in LD-SCLC patients (median = 6 CTCs/7.5 mL of blood) were lower than those in patients with ED-SCLC (median = 63) [99]. Similar results were reported by Aggarwal et al., with a median of 1.5 CTCs/7.5 mL of blood in LD-SCLC patients and a median of 71 CTCs in ED-SCLC patients [103].
In line with these results, several studies have reported the association of CTC levels with patient outcomes. Hilterman et al. showed that the presence of ≥2 CTCs/7.5 mL of blood was the strongest prognostic factor to predict OS in a cohort of 59 patients with SCLC [99]. A meta-analysis also supported the prognostic value of CTCs in a study analyzing a total of 440 patients diagnosed with SCLC [110]. The study concluded that the presence of ≥2 CTCs/7.5 mL of blood was significantly associated with poorer OS and PFS, although the CTC isolation methods varied across the studies included in the meta-analysis. Despite these data, the prognostic and pharmacodynamic importance of CTCs has not reached a consensus regarding the optimal cut-off for clinical prognostication. Hou et al. reported that the persistence of more than 50 CTCs after one chemotherapy cycle is strongly associated with prognosis, showing clinical utility to guide treatment decisions even in clinical trials that test novel agents [100]. Due to the molecular heterogeneity of CTCs, studies using label-independent platforms have also reported correlating the presence of CTCs with prognosis [96,111,112,113,114]. Recently, Obermayr et al. showed that CTCs isolated by the microfluidic platform Parsortix can be assessed using epithelial and neuroendocrine cell lineage markers at the molecular level, showing the potential utility of label-independent platforms to detect CTCs during epithelial-to-mesenchymal transition (EMT) [112]. Moreover, RNA analyses of isolated CTCs showed that the expression of a Notch pathway delta-like 3 ligand (DDL3), the actionable target of rovalpituzumab tesirine (Rova-T), is associated with PFS and OS in SCLC patients. However, the number of CTC-positive samples using the Parsortix system was smaller than that reported using the CellSearch system in other studies [115]. In contrast, Chudziak et al. reported a good rate of detection in their cohort (n = 12/12 SCLC patients with at least 1 CTC) using the Parsortix system [96].
On the other hand, single-cell sequencing of CTCs can provide relevant information about the mutational atlas of SCLC. It has been reported that CNAs analyses of single CTCs showed the potential to distinguish SCLC from lung adenocarcinoma [117]. Another study that analyzed CTCs at the single-cell level in a cohort of 31 SCLC patients generated a CNA-based classification to distinguish chemosensitive from chemorefractory disease [11]. More recently, a single-CTC-based CNA score was developed to predict the response to first-line chemotherapy, which provided insight into biomarker development and constituted a convenient approach for clinical disease differentiation [116]. In addition to molecular characterization, CTC isolation in SCLC has allowed the generation of xenograft models and short-term ex vivo cultures for phenotypic and transcriptomic characterization and preclinical drug screening. Thus, circulating tumor cells-derived explants (CDXs) hold promise as additional tools to gain mechanistic insights into treatment sensitivity and resistance [118].
3.3. Extracellular Vesicles
The last of the three important circulating biomarkers are circulating extracellular vesicles (EVs), representing a promising option in the oncology field. EVs are a heterogeneous population of cell-derived membranous structures that include exosomes (ranging from 30 to 100 nm), microvesicles (ranging from 50 to 5000 nm) and apoptotic bodies (typically 500–4000 nm) that are released by the cells through various mechanisms [119,120]. They are implicated in cancer progression, favoring the interaction between tumoral and stromal cells, promoting cell proliferation, invasion and distant colonization [121,122,123]. Of note, EVs can be isolated from several body fluids, and patients with cancer normally show higher levels than healthy people [123]. In addition to their increase in circulation as a consequence of the disease, the characterization of their membrane components and their molecular cargo (proteins, mRNAs and ncRNAs, and single- or double-stranded DNA) constitutes a valuable source of biomarkers [119].
3.3.1. Methods to Isolate and to Characterize EVs
Several methods have been reported in order to obtain a better knowledge of EVs and to understand their molecular biology and possible therapeutic value. First, EV isolation can be mainly addressed by ultracentrifugation, immunoaffinity or precipitation strategies, although standardization of methodologies remains a challenge [124]. Ultracentrifugation is the most common isolation method; however, a high amount of start samples are needed and a low yield or insufficient purity of obtained EVs has been reported [125]. For small volumes and specially for exosomes, immunoaffinity capture is often used, obtaining a high-quality yield. Nevertheless, the method is based on the interactions with a membrane antigen; therefore, only EVs positives for a specific antigen are isolated. Specific EVs markers are still the object of investigations. In the last year, several commercial kits based on precipitation of EVs using an agglutinating agent have been developed [125], but again a lack of standardization remains a challenge.
Next, several methods to characterize EVs and to confirm their correct isolation are employed. EVs imaging plays an important role; however, due to the small size of EVs, they often require labeling prior to their subsequent visualization. Electron microscopy, transmission electron microscopy and optical microscopy have been employed to image the different EVs [126]. The Western blot technique is also employed in order to confirm the correct EVs isolation, but is not valid for EVs quantification and a specific EVs housekeeping protein remains unclear [125].
3.3.2. EVs in SCLC
In SCLC, some studies have described the potential of EVs as a clinical tool. For example, Sandfeld-Paulsen et al. found that the CD151 marker was significantly upregulated in the plasma of SCLC after the application of an extracellular vesicle array to phenotype exosomes [127]. Exosomal circulating miR-141 was also upregulated in plasma and serum samples from 122 SCLC patients compared to a control group, and this increase was associated with advanced stages. In addition, the activity of this exosomal miRNA was implicated in angiogenesis, which supported its candidature as a potential novel target for SCLC patients [128]. Another study characterized the miRNA cargo of serum-derived exosomes isolated from 9 SCLC and 11 NSCLC patients and 10 healthy controls. This strategy identified a total of 17 miRNAs differentially expressed in cancer patients. Some of these miRNAs were found to be altered in exosomal samples obtained at baseline and after chemotherapy treatment, evidencing the potential of exosomal miRNAs for developing noninvasive tumor characterization in lung cancer patients [129].
3.4. Other Liquid Biopsy Biomarkers
There are other biomarkers in the field of liquid biopsy that are in an emerging state. The expansion of the range of analytes examined might help to obtain more complete information and add value to data obtained from CTCs and cfDNA assessment. MicroRNAs (miRNAs) are small RNA molecules (19–24 nucleotides) that constitute an evolutionary highly conserved class of non-coding RNAs. They play a significant role in the regulation of gene expression, and their discovery has provided new directions for the study of human cancer pathogenesis [130]. Different authors have reported that miRNAs could be useful as tissue biomarkers for classifying lung neuroendocrine neoplasms (NENs) [131,132,133,134,135]. MicroRNAs are also promising tissue biomarkers for examining chemoresistance and can be used as a new therapeutic approach in SCLC [136]. However, circulating miRNAs have been comparatively less studied as blood-based biomarkers in SCLC. Using a 24-miRNA signature previously described for lung cancer in blood [137], metastatic adenocarcinoma and SCLC was predicted with a high accuracy [138]. In the same line, Lu et al. reported two plasma microRNA panels with a considerable clinical value in the diagnosis of lung cancer, being able to perform a relevant role in determining optimal treatment strategies based on discrimination between SCLC and NSCLC [139]. Recently, Li et al. evaluated the expression of candidate circulating miRNAs in SCLC patients to identify potential noninvasive biomarkers [140]. The study revealed that plasma miR-92b and miR-375 might be used as biomarkers of chemotherapy resistance and prognostic factors for SCLC. The presence of circulating miRNAs in plasma and/or serum is highly stable, being detected at low concentrations with great efficiency, so it has huge potential to be utilized as a biomarker in cancer screening and monitoring [141], SCLC in this case. However, there is currently a need for retrospective and prospective larger studies.
The neutrophil-to-lymphocyte ratio (NRL), red cell distribution width (RDW) and platelet-to-lymphocyte ratio (PRL) have been studied as prognostic factors in SCLC patients [142,143]. The NLR is defined as the neutrophil count in blood divided by the lymphocyte count in blood and is a marker for the general immune response to distinct stress stimuli. A correlation between the outcomes of SCLC patients and the NLR has been reported and proposed as a potential biomarker in ES-SCLC patients under different therapies [143] or all stages of SCLC patients under anti-PD-1/PD-L1 therapy [142]. Indeed, elevated RDW and PLR are poor prognostic factors in ES-SCLC patients and LS-SCLC, respectively [143]. However, a recent study did not find an association between these biomarkers and patients receiving anti-PD-1/PD-L1 therapy. Several serum biomarkers have been also reported in SCLC, such as neuron-specific enolase (NSE), lactate dehydrogenase (LDH), serum pro-gastrin-releasing peptide (ProGRP) and carcinoembryonic antigen (CEA) [144].
4. Conclusions and Future Perspectives
Liquid biopsy is being incorporated as a useful procedure in many fields, especially in oncology, due to its minimal invasiveness and its great capacity to monitor the disease. The search for new biomarkers will help clinicians manage patients in a personalized way, with the aim of turning the management of cancer into an oncology of precision [145]. The recent development of new technologies has propelled liquid biopsy as a promising diagnostic tool. In recent years, several integrated biological strategies have been used to identify noninvasive markers to predict response and identify new biomarkers in SCLC patients. However, multiple challenges remain before liquid biopsies can be widely used for cancer management, such as the need for standardization of pre-analytical samples and standardized platforms [146].
Recent improvements in cfDNA analysis have made possible the development of cfDNA assays with high sensitivity and specificity, such as WGS, NGS and ddPCR. In SCLC patients, cfDNA-based assays will become increasingly important because they allow minimization of the need for a tumor tissue biopsy. Several studies have found that the levels of cfDNA or CNA are associated with patient outcomes, and good concordance between cfDNA and tissue was reported [71]. In contrast, it is important to remark that the standardized method to isolate and analyze cfDNA is still a challenge. Plasma cfDNA is a complex mixture of DNA from many sources, including germline, fetal, infectious and malignant origins [147], but mutations can also be found on cfDNA of hematopoietic origin, with the risk of considering these mutations as tumor-derived. The incorporation of strict quality controls and/or bioinformatic filtering is critical to ensure that they are specific to the tumor of interest. Therefore, the sequencing of matched PBMCs together with cfDNA would be important for the correct implementation of NGS analyses using plasma samples [72,148].
Analysis of ctDNA could also be potentially integrated in early cancer detection protocols. Lung screening trials showed that lung cancer screening by low-dose computed tomography (LDCT) reduced lung cancer mortality. However, it is necessary to improve the sensitivity and specificity of LDCT and avoid performing invasive tests on patients who do not need them. The combination of imaging and liquid biopsy techniques may be useful in this context. Thus, in the BioMILD assay, it proved the additional value of blood miRNA analysis at the time of LDCT in a large series of volunteers, with the aim of targeting the next LDCT intervals based on an individual risk profile [149].
On the other hand, CTCs are cells with tumor-specific information and can also enable cancer diagnosis and treatment evaluation. In SCLC, the number of CTCs is higher than in other cancer types, including LD-SCLC patients, and this high number of CTCs has been associated with a poor response to different treatments [150]. The high number of CTCs detected in SCLC patients appears to be due to high tumor growth and early disseminative capacity [111]. The CellSearch system has been shown to be the most robust platform to isolate CTCs in SCLC patients, but this platform is only based on the expression of epithelial markers in CTCs; thus, high mesenchymal CTCs can be underestimated using this system. New markers to detect these mesenchymal CTCs would be of great value, together with the validation of new label-independent platforms, which are a promising option to detect the presence of clinical biomarkers, such as PD-L1 or c-MET [151,152]. Another advantage of label-independent platforms is the possibility of performing molecular analyses with isolated CTCs and developing novel therapeutic targets, such as DDL3, the actionable target of Rova-T [112]. Additionally, thanks to methods that allow the preservation and capture of intact CTCs, single-cell analyses or cluster analyses are possible. Single- or cluster-cell characterization of CTCs will allow more precise characterization of the entire cancer in each patient. RNA and DNA analyses are possible and could show the intertumoral and intratumoral heterogeneity in each patient [153]. CDXs models derived from CTCs will also allow for improved knowledge of the mechanisms of tumor development [154]. In contrast, a robust and standardized platform to capture CTCs and rigorous validation remain a challenge.
Author Contributions
Conceptualization, P.M.-M. and R.D.-P.; investigation, P.M.-M., J.G.-G. and L.L.-M.; writing—original draft preparation, P.M.-M., J.G.-G., L.L.-M. and R.D.-P.; writing—review and editing, L.M.-R., R.L.-L. and R.D.-P.; visualization, P.M.-M., A.C.-G. and R.D.-P.; supervision, R.D.-P.; funding acquisition, R.L.-L., L.M.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This study was financed by all the donors who participated in the Liquid Biopsy Crowdfunding campaign in 2017.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
Jorge García-González reports personal fees from AstraZeneca, Boehringer-Ingelheim, Novartis, Pierre Fabre, Rovi and Sanofi; and personal fees and non-financial support from Bristol-Myers Squibb, Lilly, MSD and Roche, outside the submitted work. Luis León-Mateos reports personal fees from AstraZeneca, Boehringer-Ingelheim, Novartis, Jansen, Astellas and Sanofi; and personal fees and non-financial support from Bristol-Myers Squibb, Lilly, MSD and Roche, outside the submitted work. Rafael López-López reports grants and personal fees from Roche, Merck, AstraZeneca, Bayer, Pharmamar and Leo; and personal fees and non-financial support from Bristol-Myers Squibb and Novartis, outside of the submitted work.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Govindan R., Page N., Morgensztern D., Read W., Tierney R., Vlahiotis A., Spitznagel E.L., Piccirillo J. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: Analysis of the surveillance, epidemiologic, and end results database. J. Clin. Oncol. 2006;24:4539–4544. doi: 10.1200/JCO.2005.04.4859. [DOI] [PubMed] [Google Scholar]
- 2.Micke P., Faldum A., Metz T., Beeh K.M., Bittinger F., Hengstler J.G., Buhl R. Staging small cell lung cancer: Veterans Administration Lung Study Group versus International Association for the Study of Lung Cancer-What limits limited disease? Lung Cancer. 2002;37:271–276. doi: 10.1016/S0169-5002(02)00072-7. [DOI] [PubMed] [Google Scholar]
- 3.Blackhall F., Frese K.K., Simpson K., Kilgour E., Brady G., Dive C. Will liquid biopsies improve outcomes for patients with small-cell lung cancer? Lancet Oncol. 2018;19:e470–e481. doi: 10.1016/S1470-2045(18)30455-8. [DOI] [PubMed] [Google Scholar]
- 4.Turrisi A.T., Kim K., Blum R., Sause W.T., Livingston R.B., Komaki R., Wagner H., Aisner S., Johnson D.H. Twice-daily compared with once-daily thoracic radiotherapy in limited small-cell lung cancer treated concurrently with cisplatin and etoposide. N. Engl. J. Med. 1999;340:265–271. doi: 10.1056/NEJM199901283400403. [DOI] [PubMed] [Google Scholar]
- 5.Faivre-Finn C., Snee M., Ashcroft L., Appel W., Barlesi F., Bhatnagar A., Bezjak A., Cardenal F., Fournel P., Harden S., et al. Concurrent once-daily versus twice-daily chemoradiotherapy in patients with limited-stage small-cell lung cancer (CONVERT): An open-label, phase 3, randomised, superiority trial. Lancet Oncol. 2017;18:1116–1125. doi: 10.1016/S1470-2045(17)30318-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rossi A., Di Maio M., Chiodini P., Rudd R.M., Okamoto H., Skarlos D.V., Früh M., Qian W., Tamura T., Samantas E., et al. Carboplatin- or cisplatin-based chemotherapy in first-line treatment of small-cell lung cancer: The COCIS meta-analysis of individual patient data. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2012;30:1692–1698. doi: 10.1200/JCO.2011.40.4905. [DOI] [PubMed] [Google Scholar]
- 7.Dómine M., Moran T., Isla D., Martí J.L., Sullivan I., Provencio M., Olmedo M.E., Ponce S., Blasco A., Cobo M. SEOM clinical guidelines for the treatment of small-cell lung cancer (SCLC) (2019) Clin. Transl. Oncol. 2020;22:245–255. doi: 10.1007/s12094-020-02295-w. [DOI] [PubMed] [Google Scholar]
- 8.Glatzer M., Schmid S., Radovic M., Früh M., Putora P.M. The role of radiation therapy in the management of small cell lung cancer. Breathe. 2017;13:e87–e94. doi: 10.1183/20734735.009617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins K.A., Simone C.B., Amini A., Chetty I.J., Donington J., Edelman M.J., Chun S.G., Kestin L.L., Movsas B., Rodrigues G.B., et al. American Radium Society Appropriate Use Criteria on Radiation Therapy for Extensive-Stage SCLC. J. Thorac. Oncol. 2020;16:54–65. doi: 10.1016/j.jtho.2020.09.013. [DOI] [PubMed] [Google Scholar]
- 10.Chun S.G., Simone C.B., Amini A., Chetty I.J., Donington J., Edelman M.J., Higgins K.A., Kestin L.L., Movsas B., Rodrigues G.B., et al. American Radium Society Appropriate Use Criteria: Radiation Therapy for Limited-Stage SCLC 2020. J. Thorac. Oncol. 2020;16:66–75. doi: 10.1016/j.jtho.2020.10.020. [DOI] [PubMed] [Google Scholar]
- 11.Carter L., Rothwell D.G., Mesquita B., Smowton C., Leong H.S., Fernandez-Gutierrez F., Li Y., Burt D.J., Antonello J., Morrow C.J., et al. Molecular analysis of circulating tumor cells identifies distinct copy-number profiles in patients with chemosensitive and chemorefractory small-cell lung cancer. Nat. Med. 2017;23:114–119. doi: 10.1038/nm.4239. [DOI] [PubMed] [Google Scholar]
- 12.Früh M., Panje C.M., Reck M., Blackhall F., Califano R., Cappuzzo F., Besse B., Novello S., Garrido P., Felip E., et al. Choice of second-line systemic therapy in stage IV small cell lung cancer (SCLC)–A decision-making analysis amongst European lung cancer experts. Lung Cancer. 2020;146:6–11. doi: 10.1016/j.lungcan.2020.03.024. [DOI] [PubMed] [Google Scholar]
- 13.Trigo J., Subbiah V., Besse B., Moreno V., López R., Sala M.A., Peters S., Ponce S., Fernández C., Alfaro V., et al. Lurbinectedin as second-line treatment for patients with small-cell lung cancer: A single-arm, open-label, phase 2 basket trial. Lancet. Oncol. 2020;21:645–654. doi: 10.1016/S1470-2045(20)30068-1. [DOI] [PubMed] [Google Scholar]
- 14.Farago A.F., Drapkin B.J., Lopez-Vilarino de Ramos J.A., Galmarini C.M., Núñez R., Kahatt C., Paz-Ares L. ATLANTIS: A Phase III study of lurbinectedin/doxorubicin versus topotecan or cyclophosphamide/doxorubicin/vincristine in patients with small-cell lung cancer who have failed one prior platinum-containing line. Future Oncol. (Lond. Engl.) 2019;15:231–239. doi: 10.2217/fon-2018-0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Antonia S.J., López-Martin J.A., Bendell J., Ott P.A., Taylor M., Eder J.P., Jäger D., Pietanza M.C., Le D.T., de Braud F., et al. Nivolumab alone and nivolumab plus ipilimumab in recurrent small-cell lung cancer (CheckMate 032): A multicentre, open-label, phase 1/2 trial. Lancet Oncol. 2016;17:883–895. doi: 10.1016/S1470-2045(16)30098-5. [DOI] [PubMed] [Google Scholar]
- 16.Chung H.C., Lopez-Martin J.A., Kao S.C.-H., Miller W.H., Ros W., Gao B., Marabelle A., Gottfried M., Zer A., Delord J.-P., et al. Phase 2 study of pembrolizumab in advanced small-cell lung cancer (SCLC): KEYNOTE-158. J. Clin. Oncol. 2018;36:8506. doi: 10.1200/JCO.2018.36.15_suppl.8506. [DOI] [Google Scholar]
- 17.Reck M., Vicente D., Ciuleanu T., Gettinger S., Peters S., Horn L., Audigier-Valette C., Pardo N., Juan-Vidal O., Cheng Y., et al. Efficacy and safety of nivolumab (nivo) monotherapy versus chemotherapy (chemo) in recurrent small cell lung cancer (SCLC): Results from CheckMate 331. Ann. Oncol. 2018;29:x43. doi: 10.1093/annonc/mdy511.004. [DOI] [Google Scholar]
- 18.Esposito G., Palumbo G., Carillio G., Manzo A., Montanino A., Sforza V., Costanzo R., Sandomenico C., La Manna C., Martucci N., et al. Immunotherapy in Small Cell Lung Cancer. Cancers. 2020;12:2522. doi: 10.3390/cancers12092522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Facchinetti F., Di Maio M., Tiseo M. Adding PD-1/PD-L1 inhibitors to chemotherapy for the first-line treatment of extensive stage small cell lung cancer (Sclc): A meta-analysis of randomized trials. Cancers. 2020;12:1245. doi: 10.3390/cancers12092645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Horn L., Mansfield A.S., Szczęsna A., Havel L., Krzakowski M., Hochmair M.J., Huemer F., Losonczy G., Johnson M.L., Nishio M., et al. First-Line Atezolizumab plus Chemotherapy in Extensive-Stage Small-Cell Lung Cancer. N. Engl. J. Med. 2018;379:2220–2229. doi: 10.1056/NEJMoa1809064. [DOI] [PubMed] [Google Scholar]
- 21.Paz-Ares L., Dvorkin M., Chen Y., Reinmuth N., Hotta K., Trukhin D., Statsenko G., Hochmair M.J., Özgüroğlu M., Ji J.H., et al. Durvalumab plus platinum–etoposide versus platinum–etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): A randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394:1929–1939. doi: 10.1016/S0140-6736(19)32222-6. [DOI] [PubMed] [Google Scholar]
- 22.Rudin C.M., Awad M.M., Navarro A., Gottfried M., Peters S., Csőszi T., Cheema P.K., Rodriguez-Abreu D., Wollner M., Yang J.C.H., et al. Pembrolizumab or Placebo Plus Etoposide and Platinum as First-Line Therapy for Extensive-Stage Small-Cell Lung Cancer: Randomized, Double-Blind, Phase III KEYNOTE-604 Study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2020;38:2369–2379. doi: 10.1200/JCO.20.00793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hirsch F.R., Scagliotti G.V., Mulshine J.L., Kwon R., Curran W.J.J., Wu Y.-L., Paz-Ares L. Lung cancer: Current therapies and new targeted treatments. Lancet (Lond. Engl.) 2017;389:299–311. doi: 10.1016/S0140-6736(16)30958-8. [DOI] [PubMed] [Google Scholar]
- 24.Camidge D.R., Doebele R.C., Kerr K.M. Comparing and contrasting predictive biomarkers for immunotherapy and targeted therapy of NSCLC. Nat. Rev. Clin. Oncol. 2019;16:341–355. doi: 10.1038/s41571-019-0173-9. [DOI] [PubMed] [Google Scholar]
- 25.Rudin C.M., Poirier J.T., Byers L.A., Dive C., Dowlati A., George J., Heymach J.V., Johnson J.E., Lehman J.M., MacPherson D., et al. Molecular subtypes of small cell lung cancer: A synthesis of human and mouse model data. Nat. Rev. Cancer. 2019;19:289–297. doi: 10.1038/s41568-019-0133-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sonkin D., Vural S., Thomas A., Teicher B.A. Neuroendocrine negative SCLC is mostly RB1 WT and may be sensitive to CDK4/6 inhibition. bioRxiv. 2019 doi: 10.1101/516351. [DOI] [Google Scholar]
- 27.McColl K., Wildey G., Sakre N., Lipka M.B., Behtaj M., Kresak A., Chen Y., Yang M., Velcheti V., Fu P., et al. Reciprocal expression of INSM1 and YAP1 defines subgroups in small cell lung cancer. Oncotarget. 2017;8:73745–73756. doi: 10.18632/oncotarget.20572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.George J., Lim J.S., Jang S.J., Cun Y., Ozretić L., Kong G., Leenders F., Lu X., Fernández-Cuesta L., Bosco G., et al. Comprehensive genomic profiles of small cell lung cancer. Nature. 2015;524:47–53. doi: 10.1038/nature14664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Allison Stewart C., Tong P., Cardnell R.J., Sen T., Li L., Gay C.M., Masrorpour F., Fan Y., Bara R.O., Feng Y., et al. Dynamic variations in epithelial-to-mesenchymal transition (EMT), ATM, and SLFN11 govern response to PARP inhibitors and cisplatin in small cell lung cancer. Oncotarget. 2017;8:28575–28587. doi: 10.18632/oncotarget.15338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schulze A.B., Evers G., Kerkhoff A., Mohr M., Schliemann C., Berdel W.E., Schmidt L.H. Future options of molecular-targeted therapy in small cell lung cancer. Cancers. 2019;11:690. doi: 10.3390/cancers11050690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Den Borg R., Leonetti A., Tiseo M., Giovannetti E., Peters G.J. Novel targeted strategies to overcome resistance in small-cell lung cancer: Focus on PARP inhibitors and rovalpituzumab tesirine. Expert Rev. Anticancer Ther. 2019;19:461–471. doi: 10.1080/14737140.2019.1624530. [DOI] [PubMed] [Google Scholar]
- 32.Owonikoko T.K., Dahlberg S.E., Sica G.L., Wagner L.I., Wade J.L., Srkalovic G., Lash B.W., Leach J.W., Leal T.B., Aggarwal C., et al. Randomized phase II trial of cisplatin and etoposide in combination with veliparib or placebo for extensive-stage small-cell lung cancer: ECOG-ACRIN 2511 study. J. Clin. Oncol. 2019;37:222–229. doi: 10.1200/JCO.18.00264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pietanza M.C., Waqar S.N., Krug L.M., Dowlati A., Hann C.L., Chiappori A., Owonikoko T.K., Woo K.M., Cardnell R.J., Fujimoto J., et al. Randomized, double-blind, phase II study of temozolomide in combination with either veliparib or placebo in patients with relapsed-sensitive or refractory small-cell lung cancer. J. Clin. Oncol. 2018;36:2386–2394. doi: 10.1200/JCO.2018.77.7672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sidaway P. SLFN11: A new synthetic lethal target? Nat. Rev. Clin. Oncol. 2018;15:533. doi: 10.1038/s41571-018-0064-5. [DOI] [PubMed] [Google Scholar]
- 35.Rudin C.M., Pietanza M.C., Bauer T.M., Ready N., Morgensztern D., Glisson B.S., Byers L.A., Johnson M.L., Burris H.A., Robert F., et al. Rovalpituzumab tesirine, a DLL3-targeted antibody-drug conjugate, in recurrent small-cell lung cancer: A first-in-human, first-in-class, open-label, phase 1 study. Lancet Oncol. 2017;18:42–51. doi: 10.1016/S1470-2045(16)30565-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Melichar B., Adenis A., Lockhart A.C., Bennouna J., Dees E.C., Kayaleh O., Obermannova R., DeMichele A., Zatloukal P., Zhang B., et al. Safety and activity of alisertib, an investigational aurora kinase A inhibitor, in patients with breast cancer, small-cell lung cancer, non-small-cell lung cancer, head and neck squamous-cell carcinoma, and gastro-oesophageal adenocarcinoma: A five-arm p. Lancet. Oncol. 2015;16:395–405. doi: 10.1016/S1470-2045(15)70051-3. [DOI] [PubMed] [Google Scholar]
- 37.Owonikoko T.K., Niu H., Nackaerts K., Csoszi T., Ostoros G., Mark Z., Baik C., Joy A.A., Chouaid C., Jaime J.C., et al. Randomized Phase II Study of Paclitaxel plus Alisertib versus Paclitaxel plus Placebo as Second-Line Therapy for SCLC: Primary and Correlative Biomarker Analyses. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer. 2020;15:274–287. doi: 10.1016/j.jtho.2019.10.013. [DOI] [PubMed] [Google Scholar]
- 38.Siravegna G., Mussolin B., Venesio T., Marsoni S., Seoane J., Dive C., Papadopoulos N., Kopetz S., Corcoran R.B., Siu L.L., et al. How liquid biopsies can change clinical practice in oncology. Ann. Oncol. 2019;30:1580–1590. doi: 10.1093/annonc/mdz227. [DOI] [PubMed] [Google Scholar]
- 39.Russano M., Napolitano A., Ribelli G., Iuliani M., Simonetti S., Citarella F., Pantano F., Dell’Aquila E., Anesi C., Silvestris N., et al. Liquid biopsy and tumor heterogeneity in metastatic solid tumors: The potentiality of blood samples. J. Exp. Clin. Cancer Res. 2020;39:120. doi: 10.1186/s13046-020-01615-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tellez-Gabriel M., Heymann M.F., Heymann D. Circulating tumor cells as a tool for assessing tumor heterogeneity. Theranostics. 2019;9:4580–4594. doi: 10.7150/thno.34337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cohen J.D., Javed A.A., Thoburn C., Wong F., Tie J., Gibbs P., Schmidt C.M., Yip-Schneider M.T., Allen P.J., Schattner M., et al. Combined circulating tumor DNA and protein biomarker-based liquid biopsy for the earlier detection of pancreatic cancers. Proc. Natl. Acad. Sci. USA. 2017;114:10202–10207. doi: 10.1073/pnas.1704961114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cohen J.D., Li L., Wang Y., Thoburn C., Afsari B., Danilova L., Douville C., Javed A.A., Wong F., Mattox A., et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science (N. Y.) 2018;359:926–930. doi: 10.1126/science.aar3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heitzer E., Haque I.S., Roberts C.E.S., Speicher M.R. Current and future perspectives of liquid biopsies in genomics-driven oncology. Nat. Rev. Genet. 2019;20:71–88. doi: 10.1038/s41576-018-0071-5. [DOI] [PubMed] [Google Scholar]
- 44.Heidrich I., Ačkar L., Mossahebi Mohammadi P., Pantel K. Liquid biopsies: Potential and challenges. Int. J. Cancer. 2020:1–18. doi: 10.1002/ijc.33217. [DOI] [PubMed] [Google Scholar]
- 45.Mandel P., Metais P. Les acides nucléiques du plasma sanguin chez l’homme. Comptes Rendus Des. Seances Soc. Biol. Ses. Fil. 1948;142:241–243. [PubMed] [Google Scholar]
- 46.Leon S.A., Shapiro B., Sklaroff D.M., Yaros M.J. Free DNA in the serum of cancer patients and the effect of therapy. Cancer Res. 1977;37:646–650. [PubMed] [Google Scholar]
- 47.Kustanovich A., Schwartz R., Peretz T., Grinshpun A. Life and death of circulating cell-free DNA. Cancer Biol. Ther. 2019;20:1057–1067. doi: 10.1080/15384047.2019.1598759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aucamp J., Bronkhorst A.J., Badenhorst C.P.S., Pretorius P.J. The diverse origins of circulating cell-free DNA in the human body: A critical re-evaluation of the literature. Biol. Rev. 2018;93:1649–1683. doi: 10.1111/brv.12413. [DOI] [PubMed] [Google Scholar]
- 49.Fernandez-Cuesta L., Perdomo S., Avogbe P.H., Leblay N., Delhomme T.M., Gaborieau V., Abedi-Ardekani B., Chanudet E., Olivier M., Zaridze D., et al. Identification of Circulating Tumor DNA for the Early Detection of Small-cell Lung Cancer. EBioMedicine. 2016;10:117–123. doi: 10.1016/j.ebiom.2016.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Corcoran R.B., Chabner B.A. Application of cell-free DNA analysis to cancer treatment. N. Engl. J. Med. 2018;379:1754–1765. doi: 10.1056/NEJMra1706174. [DOI] [PubMed] [Google Scholar]
- 51.Keller L., Belloum Y., Wikman H., Pantel K. Clinical relevance of blood-based ctDNA analysis: Mutation detection and beyond. Br. J. Cancer. 2020 doi: 10.1038/s41416-020-01047-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shao X., He Y., Ji M., Chen X., Qi J., Shi W., Hao T., Ju S. Quantitative analysis of cell-free DNA in ovarian cancer. Oncol. Lett. 2015;10:3478–3482. doi: 10.3892/ol.2015.3771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sozzi G., Conte D., Mariani L., Lo Vullo S., Roz L., Lombardo C., Pierotti M.A., Tavecchio L. Analysis of circulating tumor DNA in plasma at diagnosis and during follow-up of lung cancer patients. Cancer Res. 2001;61:4675–4678. [PubMed] [Google Scholar]
- 54.Kim K., Shin D.G., Park M.K., Baik S.H., Kim T.H., Kim S., Lee S. Circulating cell-free DNA as a promising biomarker in patients with gastric cancer: Diagnostic validity and significant reduction of cfDNA after surgical resection. Ann. Surg. Treat. Res. 2014;86:136–142. doi: 10.4174/astr.2014.86.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Czeiger D., Shaked G., Eini H., Vered I., Belochitski O., Avriel A., Ariad S., Douvdevani A. Measurement of circulating cell-free DNA levels by a new simple fluorescent test in patients with primary colorectal cancer. Am. J. Clin. Pathol. 2011;135:264–270. doi: 10.1309/AJCP4RK2IHVKTTZV. [DOI] [PubMed] [Google Scholar]
- 56.Olsson E., Winter C., George A., Chen Y., Howlin J., Tang M.-H.E., Dahlgren M., Schulz R., Grabau D., van Westen D., et al. Serial monitoring of circulating tumor DNA in patients with primary breast cancer for detection of occult metastatic disease. Embo Mol. Med. 2015;7:1034–1047. doi: 10.15252/emmm.201404913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Elazezy M., Joosse S.A. Techniques of using circulating tumor DNA as a liquid biopsy component in cancer management. Comput. Struct. Biotechnol. J. 2018;16:370–378. doi: 10.1016/j.csbj.2018.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kwapisz D. The first liquid biopsy test approved. Is it a new era of mutation testing for non-small cell lung cancer? Ann. Transl. Med. 2017;5:46. doi: 10.21037/atm.2017.01.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thress K.S., Brant R., Carr T.H., Dearden S., Jenkins S., Brown H., Hammett T., Cantarini M., Barrett J.C. EGFR mutation detection in ctDNA from NSCLC patient plasma: A cross-platform comparison of leading technologies to support the clinical development of AZD9291. Lung Cancer (Amst. Neth.) 2015;90:509–515. doi: 10.1016/j.lungcan.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 60.Bando H., Kagawa Y., Kato T., Akagi K., Denda T., Nishina T., Komatsu Y., Oki E., Kudo T., Kumamoto H., et al. A multicentre, prospective study of plasma circulating tumour DNA test for detecting RAS mutation in patients with metastatic colorectal cancer. Br. J. Cancer. 2019;120:982–986. doi: 10.1038/s41416-019-0457-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.García-Foncillas J., Tabernero J., Élez E., Aranda E., Benavides M., Camps C., Jantus-Lewintre E., López R., Muinelo-Romay L., Montagut C., et al. Prospective multicenter real-world RAS mutation comparison between OncoBEAM-based liquid biopsy and tissue analysis in metastatic colorectal cancer. Br. J. Cancer. 2018;119:1464–1470. doi: 10.1038/s41416-018-0293-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ou C.-Y., Vu T., Grunwald J.T., Toledano M., Zimak J., Toosky M., Shen B., Zell J.A., Gratton E., Abram T.J., et al. An ultrasensitive test for profiling circulating tumor DNA using integrated comprehensive droplet digital detection. Lab A Chip. 2019;19:993–1005. doi: 10.1039/C8LC01399C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen M., Zhao H. Next-generation sequencing in liquid biopsy: Cancer screening and early detection. Hum. Genom. 2019;13:34. doi: 10.1186/s40246-019-0220-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Snyder M.W., Kircher M., Hill A.J., Daza R.M., Shendure J. Cell-free DNA Comprises an In Vivo Nucleosome Footprint that Informs Its Tissues-Of-Origin. Cell. 2016;164:57–68. doi: 10.1016/j.cell.2015.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu L., Toung J.M., Jassowicz A.F., Vijayaraghavan R., Kang H., Zhang R., Kruglyak K.M., Huang H.J., Hinoue T., Shen H., et al. Targeted methylation sequencing of plasma cell-free DNA for cancer detection and classification. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2018;29:1445–1453. doi: 10.1093/annonc/mdy119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Joehanes R., Just A.C., Marioni R.E., Pilling L.C., Reynolds L.M., Mandaviya P.R., Guan W., Xu T., Elks C.E., Aslibekyan S., et al. Epigenetic Signatures of Cigarette Smoking. Circ. Cardiovasc. Genet. 2016;9:436–447. doi: 10.1161/CIRCGENETICS.116.001506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dor Y., Cedar H. Principles of DNA methylation and their implications for biology and medicine. Lancet. 2018;392:777–786. doi: 10.1016/S0140-6736(18)31268-6. [DOI] [PubMed] [Google Scholar]
- 68.Chan H.T., Nagayama S., Chin Y.M., Otaki M., Hayashi R., Kiyotani K., Fukunaga Y., Ueno M., Nakamura Y., Low S.K. Clinical significance of clonal hematopoiesis in the interpretation of blood liquid biopsy. Mol. Oncol. 2020;14:1719–1730. doi: 10.1002/1878-0261.12727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Almodovar K., Iams W.T., Meador C.B., Zhao Z., York S., Horn L., Yan Y., Hernandez J., Chen H., Shyr Y., et al. Longitudinal cell-free DNA analysis in patients with small cell lung cancer reveals dynamic insights into treatment efficacy and disease relapse. J. Thorac. Oncol. 2018;13:112–123. doi: 10.1016/j.jtho.2017.09.1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Morgensztern D., Devarakonda S.H., Masood A., Waqar S.N., Carmack A.C., Banks K.C., Lanman R.B., Govindan R. Circulating cell-free tumor DNA (cfDNA) testing in small cell lung cancer. J. Clin. Oncol. 2016;34:e23077. doi: 10.1200/JCO.2016.34.15_suppl.e23077. [DOI] [Google Scholar]
- 71.Nong J., Gong Y., Guan Y., Yi X., Yi Y., Chang L., Yang L., Lv J., Guo Z., Jia H., et al. Circulating tumor DNA analysis depicts subclonal architecture and genomic evolution of small cell lung cancer. Nat. Commun. 2018;9:1–8. doi: 10.1038/s41467-018-05327-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Du M., Thompson J., Fisher H., Zhang P., Huang C.C., Wang L. Genomic alterations of plasma cell-free DNAs in small cell lung cancer and their clinical relevance. Lung Cancer. 2018;120:113–121. doi: 10.1016/j.lungcan.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 73.Mohan S., Foy V., Ayub M., Leong H.S., Schofield P., Sahoo S., Descamps T., Kilerci B., Smith N.K., Carter M., et al. Profiling of Circulating Free DNA Using Targeted and Genome-wide Sequencing in Patients with SCLC. J. Thorac. Oncol. 2020;15:216–230. doi: 10.1016/j.jtho.2019.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ou S.H.I., Lee T.K., Young L., Fernandez-Rocha M.Y., Pavlick D., Schrock A.B., Zhu V.W., Milliken J., Ali S.M., Gitlitz B.J. Dual occurrence of ALK G1202R solvent front mutation and small cell lung cancer transformation as resistance mechanisms to second generation ALK inhibitors without prior exposure to crizotinib. Pitfall of solely relying on liquid re-biopsy? Lung Cancer. 2017;106:110–114. doi: 10.1016/j.lungcan.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 75.Devarakonda S., Sankararaman S., Herzog B.H., Gold K.A., Owonikoko T.K., Li B.T., Poirier J.T., Rudin C.M., Govindan R., Morgensztern D. Circulating Tumor DNA Profiling in Small Cell Lung Cancer Identifies Potentially Targetable Alterations. Clin.Cancer Res. 2019;25:6119–6126. doi: 10.1158/1078-0432.CCR-19-0879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Iams W.T., Kopparapu P.R., Yan Y., Muterspaugh A., Zhao Z., Chen H., Cann C., York S., Horn L., Ancell K., et al. Blood-Based Surveillance Monitoring of Circulating Tumor DNA From Patients With SCLC Detects Disease Relapse and Predicts Death in Patients With Limited-Stage Disease. JTO Clin. Res. Rep. 2020;1:100024. doi: 10.1016/j.jtocrr.2020.100024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bidard F.-C., Peeters D.J., Fehm T., Nolé F., Gisbert-Criado R., Mavroudis D., Grisanti S., Generali D., Garcia-Saenz J.A., Stebbing J., et al. Clinical validity of circulating tumour cells in patients with metastatic breast cancer: A pooled analysis of individual patient data. Lancet. Oncol. 2014;15:406–414. doi: 10.1016/S1470-2045(14)70069-5. [DOI] [PubMed] [Google Scholar]
- 78.Bao-Caamano A., Rodriguez-Casanova A., Diaz-Lagares A. Epigenetics of Circulating Tumor Cells in Breast Cancer. Adv. Exp. Med. Biol. 2020;1220:117–134. doi: 10.1007/978-3-030-35805-1_8. [DOI] [PubMed] [Google Scholar]
- 79.Pantel K., Hille C., Scher H.I. Circulating Tumor Cells in Prostate Cancer: From Discovery to Clinical Utility. Clin. Chem. 2019;65:87–99. doi: 10.1373/clinchem.2018.287102. [DOI] [PubMed] [Google Scholar]
- 80.Lindsay C.R., Blackhall F.H., Carmel A., Fernandez-Gutierrez F., Gazzaniga P., Groen H.J.M., Hiltermann T.J.N., Krebs M.G., Loges S., López-López R., et al. EPAC-lung: Pooled analysis of circulating tumour cells in advanced non-small cell lung cancer. Eur. J. Cancer. 2019;117:60–68. doi: 10.1016/j.ejca.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 81.Cohen S.J., Punt C.J.A., Iannotti N., Saidman B.H., Sabbath K.D., Gabrail N.Y., Picus J., Morse M., Mitchell E., Miller M.C., et al. Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2008;26:3213–3221. doi: 10.1200/JCO.2007.15.8923. [DOI] [PubMed] [Google Scholar]
- 82.Hamilton G., Rath B. Mesenchymal-epithelial transition and circulating tumor cells in small cell lung cancer. Adv. Exp. Med. Biol. 2017;994:229–245. doi: 10.1007/978-3-319-55947-6_12. [DOI] [PubMed] [Google Scholar]
- 83.Allan A.L., Vantyghem S.A., Tuck A.B., Chambers A.F., Chin-Yee I.H., Keeney M. Detection and quantification of circulating tumor cells in mouse models of human breast cancer using immunomagnetic enrichment and multiparameter flow cytometry. Cytometry. Part A J. Int. Soc. Anal. Cytol. 2005;65:4–14. doi: 10.1002/cyto.a.20132. [DOI] [PubMed] [Google Scholar]
- 84.Alix-Panabières C., Pantel K. Clinical applications of circulating tumor cells and circulating tumor DNA as liquid biopsy. Cancer Discov. 2016;6:479–491. doi: 10.1158/2159-8290.CD-15-1483. [DOI] [PubMed] [Google Scholar]
- 85.Baccelli I., Schneeweiss A., Riethdorf S., Stenzinger A., Schillert A., Vogel V., Klein C., Saini M., Bäuerle T., Wallwiener M., et al. Identification of a population of blood circulating tumor cells from breast cancer patients that initiates metastasis in a xenograft assay. Nat. Biotechnol. 2013;31:539–544. doi: 10.1038/nbt.2576. [DOI] [PubMed] [Google Scholar]
- 86.Pantel K., Speicher M.R. The biology of circulating tumor cells. Oncogene. 2016;35:1216–1224. doi: 10.1038/onc.2015.192. [DOI] [PubMed] [Google Scholar]
- 87.Genna A., Vanwynsberghe A.M., Villard A.V., Pottier C., Ancel J., Polette M., Gilles C. EMT-Associated Heterogeneity in Circulating Tumor Cells: Sticky Friends on the Road to Metastasis. Cancers. 2020;12:1632. doi: 10.3390/cancers12061632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mariscal J., Alonso-Nocelo M., Muinelo-Romay L., Barbazan J., Vieito M., Abalo A., Gomez-Tato A., Maria de Los Angeles C., Garcia-Caballero T., Rodriguez C., et al. Molecular Profiling of Circulating Tumour Cells Identifies Notch1 as a Principal Regulator in Advanced Non-Small Cell Lung Cancer. Sci. Rep. 2016;6:37820. doi: 10.1038/srep37820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Abreu M., Cabezas-Sainz P., Alonso-Alconada L., Ferreirós A., Mondelo-Macía P., Lago-Lestón R.M., Abalo A., Díaz E., Palacios-Zambrano S., Rojo-Sebastian A., et al. Circulating Tumor Cells Characterization Revealed TIMP1 as a Potential Therapeutic Target in Ovarian Cancer. Cells. 2020;9:1218. doi: 10.3390/cells9051218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Habli Z., Alchamaa W., Saab R., Kadara H., Khraiche M.L. Circulating tumor cell detection technologies and clinical utility: Challenges and opportunities. Cancers. 2020;12:1930. doi: 10.3390/cancers12071930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hayes D.F., Cristofanilli M., Budd G.T., Ellis M.J., Stopeck A., Miller M.C., Matera J., Allard W.J., Doyle G.V., Terstappen L.W.W.M. Circulating tumor cells at each follow-up time point during therapy of metastatic breast cancer patients predict progression-free and overall survival. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2006;12:4218–4224. doi: 10.1158/1078-0432.CCR-05-2821. [DOI] [PubMed] [Google Scholar]
- 92.de Bono J.S., Scher H.I., Montgomery R.B., Parker C., Miller M.C., Tissing H., Doyle G.V., Terstappen L.W.W.M., Pienta K.J., Raghavan D. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2008;14:6302–6309. doi: 10.1158/1078-0432.CCR-08-0872. [DOI] [PubMed] [Google Scholar]
- 93.Swennenhuis J.F., van Dalum G., Zeune L.L., Terstappen L.W.M.M. Improving the CellSearch® system. Expert Rev. Mol. Diagn. 2016;16:1291–1305. doi: 10.1080/14737159.2016.1255144. [DOI] [PubMed] [Google Scholar]
- 94.Hao S.-J., Wan Y., Xia Y.-Q., Zou X., Zheng S.-Y. Size-based separation methods of circulating tumor cells. Adv. Drug Deliv. Rev. 2018;125:3–20. doi: 10.1016/j.addr.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 95.Ogle L.F., Orr J.G., Willoughby C.E., Hutton C., McPherson S., Plummer R., Boddy A.V., Curtin N.J., Jamieson D., Reeves H.L. Imagestream detection and characterisation of circulating tumour cells-A liquid biopsy for hepatocellular carcinoma? J. Hepatol. 2016;65:305–313. doi: 10.1016/j.jhep.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 96.Chudziak J., Burt D.J., Mohan S., Rothwell D.G., Mesquita B., Antonello J., Dalby S., Ayub M., Priest L., Carter L., et al. Clinical evaluation of a novel microfluidic device for epitope-independent enrichment of circulating tumour cells in patients with small cell lung cancer. Analyst. 2016;141:669–678. doi: 10.1039/C5AN02156A. [DOI] [PubMed] [Google Scholar]
- 97.Valihrach L., Androvic P., Kubista M. Platforms for Single-Cell Collection and Analysis. Int. J. Mol. Sci. 2018;19:807. doi: 10.3390/ijms19030807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lawson D.A., Kessenbrock K., Davis R.T., Pervolarakis N., Werb Z. Tumour heterogeneity and metastasis at single-cell resolution. Nat. Cell Biol. 2018;20:1349–1360. doi: 10.1038/s41556-018-0236-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hiltermann T.J.N., Pore M.M., Van den Berg A., Timens W., Boezen H.M., Liesker J.J.W., Schouwink J.H., Wijnands W.J.A., Kerner G.S.M.A., Kruyt F.A.E., et al. Circulating tumor cells in small-cell lung cancer: A predictive and prognostic factor. Ann. Oncol. 2012;23:2937–2942. doi: 10.1093/annonc/mds138. [DOI] [PubMed] [Google Scholar]
- 100.Hou J.M., Krebs M.G., Lancashire L., Sloane R., Backen A., Swain R.K., Priest L.J.C., Greystoke A., Zhou C., Morris K., et al. Clinical significance and molecular characteristics of circulating tumor cells and circulating tumor microemboli in patients with small-cell lung cancer. J. Clin. Oncol. 2012;30:525–532. doi: 10.1200/JCO.2010.33.3716. [DOI] [PubMed] [Google Scholar]
- 101.Messaritakis I., Politaki E., Kotsakis A., Dermitzaki E.-K., Koinis F., Lagoudaki E., Koutsopoulos A., Kallergi G., Souglakos J., Georgoulias V. Phenotypic characterization of circulating tumor cells in the peripheral blood of patients with small cell lung cancer. PLoS ONE. 2017;12:e0181211. doi: 10.1371/journal.pone.0181211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Messaritakis I., Nikolaou M., Politaki E., Koinis F., Lagoudaki E., Koutsopoulos A., Georgoulia N., Georgoulias V., Kotsakis A. Bcl-2 expression in circulating tumor cells (CTCs) of patients with small cell lung cancer (SCLC) receiving front-line treatment. Lung Cancer (Amst. Neth.) 2018;124:270–278. doi: 10.1016/j.lungcan.2018.08.021. [DOI] [PubMed] [Google Scholar]
- 103.Aggarwal C., Wang X., Ranganathan A., Torigian D., Troxel A., Evans T., Cohen R.B., Vaidya B., Rao C., Connelly M., et al. Circulating tumor cells as a predictive biomarker in patients with small cell lung cancer undergoing chemotherapy. Lung Cancer (Amst. Neth.) 2017;112:118–125. doi: 10.1016/j.lungcan.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 104.Normanno N., Rossi A., Morabito A., Signoriello S., Bevilacqua S., Di Maio M., Costanzo R., De Luca A., Montanino A., Gridelli C., et al. Prognostic value of circulating tumor cells’ reduction in patients with extensive small-cell lung cancer. Lung Cancer (Amst. Neth.) 2014;85:314–319. doi: 10.1016/j.lungcan.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 105.Cheng Y., Liu X.Q., Fan Y., Liu Y.P., Liu Y., Liu Y., Ma L.X., Liu X.H., Li H., Bao H.Z., et al. Circulating tumor cell counts/change for outcome prediction in patients with extensive-stage small-cell lung cancer. Future Oncol. 2016;12:789–799. doi: 10.2217/fon.15.346. [DOI] [PubMed] [Google Scholar]
- 106.Huang C.H., Wick J.A., Sittampalam G.S., Nirmalanandhan V.S., Ganti A.K., Neupane P.C., Williamson S.K., Godwin A.K., Schmitt S., Smart N.J., et al. A multicenter pilot study examining the role of circulating tumor cells as a blood-based tumor marker in patients with extensive small-cell lung cancer. Front. Oncol. 2014;4:271. doi: 10.3389/fonc.2014.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Salgia R., Weaver R.W., McCleod M., Stille J.R., Yan S.B., Roberson S., Polzer J., Flynt A., Raddad E., Peek V.L., et al. Prognostic and predictive value of circulating tumor cells and CXCR4 expression as biomarkers for a CXCR4 peptide antagonist in combination with carboplatin-etoposide in small cell lung cancer: Exploratory analysis of a phase II study. Investig. New Drugs. 2017;35:334–344. doi: 10.1007/s10637-017-0446-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Naito T., Tanaka F., Ono A., Yoneda K., Takahashi T., Murakami H., Nakamura Y., Tsuya A., Kenmotsu H., Shukuya T., et al. Prognostic impact of circulating tumor cells in patients with small cell lung cancer. J. Thorac. Oncol. 2012;7:512–519. doi: 10.1097/JTO.0b013e31823f125d. [DOI] [PubMed] [Google Scholar]
- 109.Hou J.M., Greystoke A., Lancashire L., Cummings J., Ward T., Board R., Amir E., Hughes S., Krebs M., Hughes A., et al. Evaluation of circulating tumor cells and serological cell death biomarkers in small cell lung cancer patients undergoing chemotherapy. Am. J. Pathol. 2009;175:808–816. doi: 10.2353/ajpath.2009.090078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang J., Wang H.-T., Li B.-G. Prognostic significance of circulating tumor cells in small--cell lung cancer patients: A meta-analysis. Asian Pac. J. Cancer Prev. APJCP. 2014;15:8429–8433. doi: 10.7314/APJCP.2014.15.19.8429. [DOI] [PubMed] [Google Scholar]
- 111.Hodgkinson C.L., Morrow C.J., Li Y., Metcalf R.L., Rothwell D.G., Trapani F., Polanski R., Burt D.J., Simpson K.L., Morris K., et al. Tumorigenicity and genetic profiling of circulating tumor cells in small-cell lung cancer. Nat. Med. 2014;20:897–903. doi: 10.1038/nm.3600. [DOI] [PubMed] [Google Scholar]
- 112.Obermayr E., Agreiter C., Schuster E., Fabikan H., Weinlinger C., Baluchova K., Hamilton G., Hochmair M., Zeillinger R. Molecular Characterization of Circulating Tumor Cells Enriched by A Microfluidic Platform in Patients with Small-Cell Lung Cancer. Cells. 2019;8:880. doi: 10.3390/cells8080880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Igawa S., Gohda K., Fukui T., Ryuge S., Otani S., Masago A., Sato J., Murakami K., Maki S., Katono K., et al. Circulating tumor cells as a prognostic factor in patients with small cell lung cancer. Oncol. Lett. 2014;7:1469–1473. doi: 10.3892/ol.2014.1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wang P.-P., Liu S.-H., Chen C.-T., Lv L., Li D., Liu Q.-Y., Liu G.-L., Wu Y. Circulating tumor cells as a new predictive and prognostic factor in patients with small cell lung cancer. J. Cancer. 2020;11:2113–2122. doi: 10.7150/jca.35308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Foy V., Fernandez-Gutierrez F., Faivre-Finn C., Dive C., Blackhall F. The clinical utility of circulating tumour cells in patients with small cell lung cancer. Transl. Lung Cancer Res. 2017;6:409–417. doi: 10.21037/tlcr.2017.07.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Su Z., Wang Z., Ni X., Duan J., Gao Y., Zhuo M., Li R., Zhao J., Ma Q., Bai H., et al. Inferring the Evolution and Progression of Small-Cell Lung Cancer by Single-Cell Sequencing of Circulating Tumor Cells. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2019;25:5049–5060. doi: 10.1158/1078-0432.CCR-18-3571. [DOI] [PubMed] [Google Scholar]
- 117.Ni X., Zhuo M., Su Z., Duan J., Gao Y., Wang Z., Zong C., Bai H., Chapman A.R., Zhao J., et al. Reproducible copy number variation patterns among single circulating tumor cells of lung cancer patients. Proc. Natl. Acad. Sci. USA. 2013;110:21083–21088. doi: 10.1073/pnas.1320659110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lallo A., Gulati S., Schenk M.W., Khandelwal G., Berglund U.W., Pateras I.S., Chester C.P.E., Pham T.M., Kalderen C., Frese K.K., et al. Ex vivo culture of cells derived from circulating tumour cell xenograft to support small cell lung cancer research and experimental therapeutics. Br. J. Pharmacol. 2019;176:436–450. doi: 10.1111/bph.14542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.van Niel G., D’Angelo G., Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat. Rev. Mol. Cell Biol. 2018;19:213–228. doi: 10.1038/nrm.2017.125. [DOI] [PubMed] [Google Scholar]
- 120.Akers J.C., Gonda D., Kim R., Carter B.S., Chen C.C. Biogenesis of extracellular vesicles (EV): Exosomes, microvesicles, retrovirus-like vesicles, and apoptotic bodies. J. Neuro-Oncol. 2013;113:1–11. doi: 10.1007/s11060-013-1084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lafitte M., Lecointre C., Roche S. Roles of exosomes in metastatic colorectal cancer. Am. J. Physiology. Cell Physiol. 2019;317:C869–C880. doi: 10.1152/ajpcell.00218.2019. [DOI] [PubMed] [Google Scholar]
- 122.Becker A., Thakur B.K., Weiss J.M., Kim H.S., Peinado H., Lyden D. Extracellular Vesicles in Cancer: Cell-to-Cell Mediators of Metastasis. Cancer Cell. 2016;30:836–848. doi: 10.1016/j.ccell.2016.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Peinado H., Alečković M., Lavotshkin S., Matei I., Costa-Silva B., Moreno-Bueno G., Hergueta-Redondo M., Williams C., García-Santos G., Ghajar C., et al. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat. Med. 2012;18:883–891. doi: 10.1038/nm.2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Shao H., Im H., Castro C.M., Breakefield X., Weissleder R., Lee H. New Technologies for Analysis of Extracellular Vesicles. Chem. Rev. 2018;118:1917–1950. doi: 10.1021/acs.chemrev.7b00534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lucchetti D., Fattorossi A., Sgambato A. Extracellular Vesicles in Oncology: Progress and Pitfalls in the Methods of Isolation and Analysis. Biotechnol. J. 2019;14:1700716. doi: 10.1002/biot.201700716. [DOI] [PubMed] [Google Scholar]
- 126.Chuo S.T.-Y., Chien J.C.-Y., Lai C.P.-K. Imaging extracellular vesicles: Current and emerging methods. J. Biomed. Sci. 2018;25:91. doi: 10.1186/s12929-018-0494-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sandfeld-Paulsen B., Jakobsen K.R., Bæk R., Folkersen B.H., Rasmussen T.R., Meldgaard P., Varming K., Jørgensen M.M., Sorensen B.S. Exosomal Proteins as Diagnostic Biomarkers in Lung Cancer. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer. 2016;11:1701–1710. doi: 10.1016/j.jtho.2016.05.034. [DOI] [PubMed] [Google Scholar]
- 128.Mao S., Lu Z., Zheng S., Zhang H., Zhang G., Wang F., Huang J., Lei Y., Wang X., Liu C., et al. Exosomal miR-141 promotes tumor angiogenesis via KLF12 in small cell lung cancer. J. Exp. Clin. Cancer Res. Cr. 2020;39:193. doi: 10.1186/s13046-020-01680-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Poroyko V., Mirzapoiazova T., Nam A., Mambetsariev I., Mambetsariev B., Wu X., Husain A., Vokes E.E., Wheeler D.L., Salgia R. Exosomal miRNAs species in the blood of small cell and non-small cell lung cancer patients. Oncotarget. 2018;9:19793–19806. doi: 10.18632/oncotarget.24857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Carthew R.W., Sontheimer E.J. Origins and Mechanisms of miRNAs and siRNAs. Cell. 2009;136:642–655. doi: 10.1016/j.cell.2009.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gilad S., Lithwick-Yanai G., Barshack I., Benjamin S., Krivitsky I., Edmonston T.B., Bibbo M., Thurm C., Horowitz L., Huang Y., et al. Classification of the Four Main Types of Lung Cancer Using a MicroRNA-Based Diagnostic Assay. J. Mol. Diagn. 2012;14:510–517. doi: 10.1016/j.jmoldx.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 132.Mairinger F.D., Ting S., Werner R., Walter R.F.H., Hager T., Vollbrecht C., Christoph D., Worm K., Mairinger T., Sheu-Grabellus S.-Y., et al. Different micro-RNA expression profiles distinguish subtypes of neuroendocrine tumors of the lung: Results of a profiling study. Mod. Pathol. 2014;27:1632–1640. doi: 10.1038/modpathol.2014.74. [DOI] [PubMed] [Google Scholar]
- 133.Rapa I., Votta A., Felice B., Righi L., Giorcelli J., Scarpa A., Speel E.-J.M., Scagliotti G.V., Papotti M., Volante M. Identification of MicroRNAs Differentially Expressed in Lung Carcinoid Subtypes and Progression. Neuroendocrinology. 2015;101:246–255. doi: 10.1159/000381454. [DOI] [PubMed] [Google Scholar]
- 134.Demes M., Aszyk C., Bartsch H., Schirren J., Fisseler-Eckhoff A. Differential miRNA-Expression as an Adjunctive Diagnostic Tool in Neuroendocrine Tumors of the Lung. Cancers. 2016;8:38. doi: 10.3390/cancers8040038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wong J.J.M., Ginter P.S., Tyryshkin K., Yang X., Nanayakkara J., Zhou Z., Tuschl T., Chen Y.-T., Renwick N. Classifying Lung Neuroendocrine Neoplasms through MicroRNA Sequence Data Mining. Cancers. 2020;12:2653. doi: 10.3390/cancers12092653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mizuno K., Mataki H., Arai T., Okato A., Kamikawaji K., Kumamoto T., Hiraki T., Hatanaka K., Inoue H., Seki N. The microRNA expression signature of small cell lung cancer: Tumor suppressors of miR-27a-5p and miR-34b-3p and their targeted oncogenes. J. Hum. Genet. 2017;62:671–678. doi: 10.1038/jhg.2017.27. [DOI] [PubMed] [Google Scholar]
- 137.Keller A., Leidinger P., Borries A., Wendschlag A., Wucherpfennig F., Scheffler M., Huwer H., Lenhof H.-P., Meese E. miRNAs in lung cancer-Studying complex fingerprints in patient’s blood cells by microarray experiments. BMC Cancer. 2009;9:353. doi: 10.1186/1471-2407-9-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Leidinger P., Backes C., Blatt M., Keller A., Huwer H., Lepper P., Bals R., Meese E. The blood-borne miRNA signature of lung cancer patients is independent of histology but influenced by metastases. Mol. Cancer. 2014;13:202. doi: 10.1186/1476-4598-13-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Lu S., Kong H., Hou Y., Ge D., Huang W., Ou J., Yang D., Zhang L., Wu G., Song Y., et al. Two plasma microRNA panels for diagnosis and subtype discrimination of lung cancer. Lung Cancer. 2018;123:44–51. doi: 10.1016/j.lungcan.2018.06.027. [DOI] [PubMed] [Google Scholar]
- 140.Li M., Shan W., Hong B., Zou J., Li H., Han D., Zhang Y., Li L., Li D., Lin W. Circulating miR-92b and miR-375 for monitoring the chemoresistance and prognosis of small cell lung cancer. Sci. Rep. 2020;10:12705. doi: 10.1038/s41598-020-69615-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mitchell P.S., Parkin R.K., Kroh E.M., Fritz B.R., Wyman S.K., Pogosova-Agadjanyan E.L., Peterson A., Noteboom J., O’Briant K.C., Allen A., et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl. Acad. Sci. USA. 2008;105:10513–10518. doi: 10.1073/pnas.0804549105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Xiong Q., Huang Z., Xin L., Qin B., Zhao X., Zhang J., Shi W., Yang B., Zhang G., Hu Y. Post-treatment neutrophil-to-lymphocyte ratio (NLR) predicts response to anti-PD-1/PD-L1 antibody in SCLC patients at early phase. Cancer Immunol. Immunother. 2020 doi: 10.1007/s00262-020-02706-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Xie D., Marks R., Zhang M., Jiang G., Jatoi A., Garces Y.I., Mansfield A., Molina J., Yang P. Nomograms Predict Overall Survival for Patients with Small-Cell Lung Cancer Incorporating Pretreatment Peripheral Blood Markers. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer. 2015;10:1213–1220. doi: 10.1097/JTO.0000000000000585. [DOI] [PubMed] [Google Scholar]
- 144.Pezzuto F., Fortarezza F., Lunardi F., Calabrese F. Are there any theranostic biomarkers in small cell lung carcinoma? J. Thorac. Dis. 2019;11:S102–S112. doi: 10.21037/jtd.2018.12.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Muinelo-Romay L., García-González J., León-Mateos L. Lung Cancer and Liquid Biopsy: Realities and Challenges in Routine Clinical Practice. Arch. Bronconeumol. 2019;55:289–290. doi: 10.1016/j.arbres.2018.11.011. [DOI] [PubMed] [Google Scholar]
- 146.Rossi G., Ignatiadis M. Promises and pitfalls of using liquid biopsy for precision medicine. Cancer Res. 2019;79:2798–2804. doi: 10.1158/0008-5472.CAN-18-3402. [DOI] [PubMed] [Google Scholar]
- 147.Wan J.C.M., Massie C., Garcia-Corbacho J., Mouliere F., Brenton J.D., Caldas C., Pacey S., Baird R., Rosenfeld N. Liquid biopsies come of age: Towards implementation of circulating tumour DNA. Nat. Rev. Cancer. 2017;17:223–238. doi: 10.1038/nrc.2017.7. [DOI] [PubMed] [Google Scholar]
- 148.Chaudhuri A.A., Lovejoy A.F., Chabon J.J., Newman A., Stehr H., Merriott D.J., Carter J.N., Azad T.D., Padda S., Gensheimer M.F., et al. Circulating Tumor DNA Analysis during Radiation Therapy for Localized Lung Cancer Predicts Treatment Outcome. Int. J. Radiat. Oncol. Biol. Phys. 2017;99:S1–S2. doi: 10.1016/j.ijrobp.2017.06.021. [DOI] [Google Scholar]
- 149.Pastorino U., Boeri M., Sestini S., Sabia F., Silva M., Suatoni P., Verri C., Cantarutti A., Sverzellati N., Corrao G., et al. Blood MicroRNA and LDCT Reduce Unnecessary LDCT Repeats in Lung Cancer Screening: Results of Prospective BioMILD Trial. J. Thorac. Oncol. 2019;14:S5–S6. doi: 10.1016/j.jtho.2019.08.057. [DOI] [Google Scholar]
- 150.Tay R.Y., Fernández-Gutiérrez F., Foy V., Burns K., Pierce J., Morris K., Priest L., Tugwood J., Ashcroft L., Lindsay C.R., et al. Prognostic value of circulating tumour cells in limited-stage small-cell lung cancer: Analysis of the concurrent once-daily versus twice-daily radiotherapy (CONVERT) randomised controlled trial. Ann. Oncol. 2019;30:1114–1120. doi: 10.1093/annonc/mdz122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Janning M., Kobus F., Babayan A., Wikman H., Velthaus J.L., Bergmann S., Schatz S., Falk M., Berger L.A., Böttcher L.M., et al. Determination of PD-L1 expression in circulating tumor cells of NSCLC patients and correlation with response to PD-1/PD-L1 inhibitors. Cancers. 2019;11:835. doi: 10.3390/cancers11060835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Mondelo-Macía P., Rodríguez-López C., Valiña L., Aguín S., León-Mateos L., García-González J., Abalo A., Rapado-González O., Suárez-Cunqueiro M., Díaz-Lagares A., et al. Detection of MET Alterations Using Cell Free DNA and Circulating Tumor Cells from Cancer Patients. Cells. 2020;9:522. doi: 10.3390/cells9020522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Cortés-Hernández L.E., Eslami-S Z., Pantel K., Alix-Panabières C. Molecular and Functional Characterization of Circulating Tumor Cells: From Discovery to Clinical Application. Clin. Chem. 2019;66:97–104. doi: 10.1373/clinchem.2019.303586. [DOI] [PubMed] [Google Scholar]
- 154.Tellez-Gabriel M., Cochonneau D., Cadé M., Jubellin C., Heymann M.-F., Heymann D. Circulating Tumor Cell-Derived Pre-Clinical Models for Personalized Medicine. Cancers. 2018;11:19. doi: 10.3390/cancers11010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.