Abstract
Background: Environmental health is a growing area of knowledge, continually increasing and updating the body of evidence linking the environment to human health. Aim: This study summarizes the epidemiological evidence on environmental risk factors from meta-analyses through an umbrella review. Methods: An umbrella review was conducted on meta-analyses of cohort, case-control, case-crossover, and time-series studies that evaluated the associations between environmental risk factors and health outcomes defined as incidence, prevalence, and mortality. The specific search strategy was designed in PubMed using free text and Medical Subject Headings (MeSH) terms related to risk factors, environment, health outcomes, observational studies, and meta-analysis. The search was limited to English, Spanish, and French published articles and studies on humans. The search was conducted on September 20, 2020. Risk factors were defined as any attribute, characteristic, or exposure of an individual that increases the likelihood of developing a disease or death. The environment was defined as the external elements and conditions that surround, influence, and affect a human organism or population’s life and development. The environment definition included the physical environment such as nature, built environment, or pollution, but not the social environment. We excluded occupational exposures, microorganisms, water, sanitation and hygiene (WASH), behavioral risk factors, and no-natural disasters. Results: This umbrella review found 197 associations among 69 environmental exposures and 83 diseases and death causes reported in 103 publications. The environmental factors found in this review were air pollution, environmental tobacco smoke, heavy metals, chemicals, ambient temperature, noise, radiation, and urban residential surroundings. Among these, we identified 65 environmental exposures defined as risk factors and 4 environmental protective factors. In terms of study design, 57 included cohort and/or case-control studies, and 46 included time-series and/or case-crossover studies. In terms of the study population, 21 included children, and the rest included adult population and both sexes. In this review, the largest body of evidence was found in air pollution (91 associations among 14 air pollution definitions and 34 diseases and mortality diagnoses), followed by environmental tobacco smoke with 24 associations. Chemicals (including pesticides) were the third larger group of environmental exposures found among the meta-analyses included, with 19 associations. Conclusion: Environmental exposures are an important health determinant. This review provides an overview of an evolving research area and should be used as a complementary tool to understand the connections between the environment and human health. The evidence presented by this review should help to design public health interventions and the implementation of health in all policies approach aiming to improve populational health.
Keywords: environmental risk factors, umbrella review, meta-analyses, systematic review, epidemiological studies
1. Introduction
In 2012, the World Health Organization (WHO) estimated that 12.6 million global deaths, representing 23% (95% CI: 13–34%) of all deaths, were attributable to the environment [1]. Air pollution and second-hand smoke are responsible for 52 million lower-respiratory diseases each year, representing 35% of the global cases [1]. Non-communicable diseases are also related to air pollution, chemicals, and second-hand smoke, which are responsible for 119 million cardiovascular diseases each year, 49 million cancers, and 32 million chronic respiratory diseases [1]. Environmental risks to health include pollution, radiation, noise, land use patterns, or climate change [2].
Environmental health is a growing area of knowledge, continually increasing and updating the body of evidence linking the environment to human health. The Global Burden of Disease project considers 26 environmental and occupational risk factors in their estimations [3]. Such risk factors are those that have enough evidence to be translated with available global exposure data to quantify their impact across the globe. However, these are far from representing the totality of evidence related to environmental exposures and human health.
Global populations are also facing population growth and aging, increasing groups vulnerable to environmental risk factors. Around 10% of the global gross domestic product is spent on healthcare [2], but little is allocated to primary prevention and public health. Be able to identify environmental risk factors is crucial in the decision-making process aiming to protect public health. The investment in measures and policies aiming to reduce environmental risks could help alleviate the health burden that health care systems around the globe are facing.
This study aims to provide an overview of the most recent evidence linking environmental risk factors and health outcomes. Applying an umbrella review approach, this study presents a synthesis of the epidemiological evidence from meta-analyses. The umbrella review systematically identifies and selects the available scientific publications in a research area. The review focuses on meta-analyses from cohort, case-control, case-crossover, and time-series observational studies, relating short and long-term environmental exposures to morbidity and mortality. The review summarizes the statistically significant associations reported in the latest published meta-analysis with the largest available number of individual studies and populations.
2. Methodology
This study is a systematic collection and assessment of multiple systematic reviews with meta-analyses performed on a specific research topic, also known as an umbrella review. The methods of the umbrella review are standardized. In this work, we follow state-of-the-art approaches, as in previously published umbrella reviews on risk factors for health outcomes [4]. The study protocol was developed in accordance with the reporting guidance in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement and registered in the International Prospective Register of Systematic Reviews (PROSPERO—CRD42020196152).
2.1. Literature Search
A search strategy was designed to identify studies published in Medline via PubMed. The search strategy identified systematic reviews of observational studies with a meta-analysis that evaluated the associations between environmental risk factors and health outcomes defined as incidence, prevalence, and mortality. We further hand-searched reference lists of the retrieved eligible publications to identify additional relevant studies. The specific search strategy included free text and Medical Subject Headings (MeSH) terms related to risk factors, environment, health outcome, observational studies, and meta-analysis. The search was limited to English, Spanish, and French published articles and studies on humans. The last search was conducted on 20 September 2020. The results of the searches were cross-checked to eliminate duplicates.
Search Strategy
(“Risk Factors” [Mesh]) OR risk factor OR Environmental risk factors)
AND
(Environment * OR “Environment”[Mesh] OR Environmental pollution OR “Environmental Pollution”[Mesh] OR Environmental exposures OR “Environmental Exposure”[Mesh] OR Environment Design OR “Environment Design”[Mesh] OR Built Environment OR “Built Environment”[Mesh] OR Environmental Medicine OR “Environmental Medicine”[Mesh] OR Decontamination OR “Decontamination”[Mesh])
AND
(Health OR “Health”[Mesh] OR Health Outcome OR Population Health OR “Population Health”[Mesh] OR Pathological Conditions OR “Pathological Conditions, Signs and Symptoms”[Mesh] OR Pathologic Processes OR “Pathologic Processes”[Mesh] OR Disease OR “Disease”[Mesh] OR Syndrome OR “Syndrome”[Mesh] OR Morbidity OR “Morbidity”[Mesh] OR Incidence OR “Incidence”[Mesh] OR Prevalence OR “Prevalence”[Mesh] OR Mortality OR “Mortality”[Mesh] OR Death OR “Death”[Mesh] OR Cause of Death OR “Cause of Death”[Mesh] OR Life Expectancy OR “Life Expectancy”[Mesh])
AND
(Longitudinal Studies OR “Longitudinal Studies”[Mesh] OR Observational Study OR “Observational Study” [Publication Type] OR Cohort Studies OR “Cohort Studies”[Mesh] OR Case-Control Studies OR “Case-Control Studies”[Mesh] OR Time Series OR “Interrupted Time Series Analysis”[Mesh])
AND
(Meta-Analysis OR “Meta-Analysis” [Publication Type])
NOT
(“Social Environment” [MeSH Terms] OR Social Environment)
2.2. Selection Criteria
We included meta-analyses of cohort, case-control, case-crossover, and time-series studies examining associations between health outcomes and potential environmental risk factors. Health outcomes were defined as disease incidence, prevalence, cause-specific mortality, and all-cause mortality. Risk factors were defined as any attribute, characteristic, or exposure of an individual that increases the likelihood of developing a disease or death. The environment was defined as the external elements and conditions that surround, influence, and affect a human organism or population’s life and development. The environment definition included the physical environment such as nature, built environment, or pollution, but not the social environment. We excluded occupational exposures, microorganisms, water, sanitation and hygiene (WASH), behavioral risk factors, and no-natural disasters. We only included meta-analyses that reported statistically significant pooled effect estimates and confidence intervals (CI) from observational studies. When two or more meta-analyses existed for an association, we included the most recent meta-analysis with the largest number of studies and populations. We chose eligible articles by consecutively examining the titles, abstracts, and the full-text. Two investigators (DRR and EMZ) independently and blindly screened the titles and abstracts to determine the articles’ inclusion. Eligibility criteria were applied to the full-text articles during the final selection. We manually searched the references of the relevant articles and attempted to identify and include eligible studies. Disagreements were resolved via discussion between reviewers.
2.3. Data Extraction and Analysis
Data extracted from each meta-analysis included the first author, publication year, environmental risk factor, exposure unit or exposure comparator, exposure temporality, study design, population, health outcome, number of studies included, summary meta-analytic estimates (i.e., odds ratio or relative risk) and corresponding 95% CI, random effect p-value, and heterogeneity measure. A narrative synthesis of the included meta-analyses was carried out by environmental risk factors, health outcomes, and population.
To assess the strength of epidemiologic evidence, we considered the estimate’s precision and the results’ consistency. We noted which associations met the following criteria: (1) precision of the estimate (i.e., p < 0.001, a threshold associated with significantly fewer false-positive results), and (2) consistency of results (I2 < 50%). The strength of the epidemiologic evidence was rated as high (when both criteria were satisfied), moderate (if 1 consistency of results was not satisfied), or low (if both consistencies of results were not satisfied.
3. Results
3.1. Literature Review
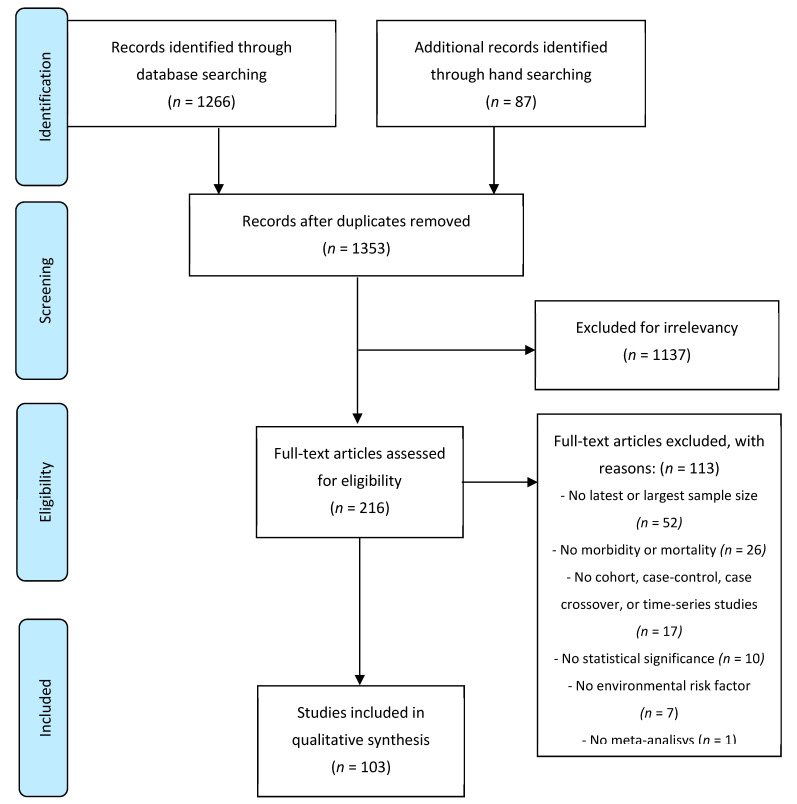
We identified 1266 publications in PubMed and 87 publications through a hand search (Figure 1). We excluded 1137 (89%) publications after screening the titles and abstracts for duplications or for not meeting our inclusion criteria. After, we reviewed the full texts of the remaining 216 (11%) publications. From these publications, 1 publication was excluded because it did not report a meta-analysis, 7 because they did not include an environmental risk factor, 10 due to the lack of statistical significance in the pooled meta-estimates, 17 because the meta-analysis did not include cohort, case-control, case-crossover, and time-series studies or combined cross-sectional studies with cohort or case-control studies, 26 because they did not report morbidity (incidence or prevalence) or related mortality estimates, and finally, 52 others because the studies they did not provide the latest available evidence and/or the largest sample size.
Figure 1.
Flow diagram of the study selection.
In total, 103 publications associating environmental risk factors and health outcomes through were included in this umbrella review. These studies include a total of 69 environmental risk factors that were grouped in air pollutants (14 risk factors), environmental tobacco smoke (6 risk factors), chemicals and heavy metals (25 risk factors), physical exposures (14 risk factors), and surrounding residential exposures (10 risk factors). On average, the meta-analysis included 37 studies ranging from 2 to 652. In terms of study design, 57 included cohort and/or case-control studies, and 46 included time-series and/or case-crossover studies. In terms of the study population, 1 included the elderly, 1 included only men, 13 included only women, 21 included children, and the rest included adult population and both sexes. From all the meta-analyses included, 9 were published before 2013, 13 were published in 2014, 7 in 2015, 11 in 2016, 13 in 2017, 14 in 2018, 24 in 2019, and 12 in 2020. In total, the studies reported 72 different long- and short-term diseases or mortality diagnoses.
3.2. Air Pollution
We identified 14 air pollutants related to 34 diseases and mortality diagnoses. The air pollutant with the most extensive list of health impacts (29 diagnoses) was the particulate matter with less than 2.5 micrometers of diameter (PM2.5), followed by particulate matter with less than 10 micrometers of diameter (PM10) (17), nitrogen dioxide (NO2) (17), ozone (O3) (7), household air pollution (5), sulfur dioxide (SO2) (4), carbon monoxide (CO) (4), solid fuel use (4), nitrogen oxides (2), desert dust (2), biomass burning (2), black carbon (1), and indoor air pollution from solid fuel (1). Air pollution was reported to affect all age groups and both sexes.
Long-term impacts of particulate matter (PM2.5 and PM10) were reported for 35 diagnoses and causes of death (Table 1, Table 2 and Table 3). Adults exposed to PM2.5 or PM10 reported an increased risk of chronic kidney disease [5], type 2 diabetes [6], lung cancer mortality [7,8], and cancer mortality [7]. Adults exposed to PM2.5 also reported an increased risk of Alzheimer’s disease [9], all-cause mortality [10], cardiovascular mortality [11], chronic obstructive pulmonary disease (COPD) [8], colorectal cancer mortality [7], dementia [9], depression [12], ischemic heart disease (IHD) mortality [8], liver cancer mortality [7], natural mortality [11], respiratory mortality [11], stroke [13], stroke mortality [8] and Parkinson’s disease [14]. Adults exposed to PM10 reported an increased incidence of coronary events [15] and chronic bronchitis [16]. Pregnant women exposed to PM2.5 reported an association with offspring diagnosis of autistic syndrome disorder [17], small for gestational age [18], and those exposed to PM10 reported an association with low birth weight [18] and preterm birth [18]. For children, exposure to PM2.5 was associated with asthma [19], acute respiratory infections [8], and autistic spectrum disorder [20]. Moreover, children’s exposure to PM10 was also associated with an increased risk of asthma [19] and autistic spectrum disorder [20].
Table 1.
Particulate matter less than 2.5 micrometers of diameter (PM2.5) and long-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PM2.5 | per 1 mcg/m3 | Long-term | Cohort | Adults, both sexes | Alzheimer’s disease | 3 | [9] | 2019 | 86 | 0 | HR | 4.82 | 2.28 | 7.36 | Moderate |
| per 10 mcg/m3 | All-cause mortality | 13 | [10]. | 2013 | 65 | 0.001 | RR | 1.06 | 1.04 | 1.08 | Moderate | ||||
| Cardiovascular mortality | 17 | [11] | 2014 | 98 | NR | RR | 1.19 | 1.09 | 1.31 | Low | |||||
| Chronic kidney disease | 4 | [5] | 2020 | 82 | 0.001 | RR | 1.10 | 1.00 | 1.21 | Low | |||||
| Chronic Obstructive Pulmonary Disease | 4 | [8] | 2014 | NR | NR | IRF | F | F | F | Low | |||||
| Dementia | 4 | [9] | 2019 | 97 | 0 | HR | 3.26 | 1.20 | 5.31 | Moderate | |||||
| Depression | 5 | [12] | 2019 | 0 | 0.97 | OR | 1.10 | 1.02 | 1.19 | Moderate | |||||
| Ischemic heart disease mortality | 16 | [8] | 2014 | NR | NR | IRF | F | F | F | Low | |||||
| Lung cancer mortality | 49 | [8] | 2014 | NR | NR | IRF | F | F | F | Low | |||||
| Liver cancer mortality | 2 | [7] | 2018 | 67 | NR | RR | 1.29 | 1.06 | 1.58 | Low | |||||
| Colorectal cancer mortality | 2 | [7] | 2018 | 97 | NR | RR | 1.08 | 1.00 | 1.17 | Low | |||||
| Cancer mortality | 19 | [7] | 2018 | 97 | <0.001 | RR | 1.17 | 1.11 | 1.24 | Moderate | |||||
| Natural mortality | 11 | [11] | 2014 | 87 | NR | RR | 1.05 | 1.01 | 1.01 | Low | |||||
| Respiratory mortality | 8 | [11] | 2014 | 61 | NR | RR | 1.05 | 1.01 | 1.09 | Low | |||||
| Stroke | 16 | [13] | 2019 | 77 | 0 | HR | 1.11 | 1.05 | 1.17 | Moderate | |||||
| Stroke mortality | 16 | [8] | 2014 | NR | NR | IRF | F | F | F | Low | |||||
| Type 2 diabetes | 10 | [6] | 2020 | 55 | 0.012 | RR | 1.11 | 1.03 | 1.19 | Low | |||||
| Parkinson’s disease | 8 | [14] | 2019 | 86 | <0.001 | RR | 1.06 | 0.99 | 1.14 | Moderate |
LCI: lower confidence intervals; UCI: upper confidence intervals; NR: No reported; HR: hazard rations; RR: relative risk; IRF: integrated response function; F: function; OR: odds ratio.
Table 2.
Particulate matter less than 2.5 micrometers of diameter (PM2.5), long-term, and short-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PM2.5 | per 10 mcg/m3 | Long-term | Cohort | Children | Asthma | 10 | [36] | 2017 | 28 | 0.18 | OR | 1.03 | 1.01 | 1.05 | Moderate |
| Autism spectrum disorder | 3 | [20] | 2016 | 0 | 0.54 | OR | 2.32 | 2.15 | 2.51 | Moderate | |||||
| Children (<5 years) | Acute low respiratory infections | 28 | [8] | 2014 | NR | NR | IRF | F | F | F | Low | ||||
| Pregnant women | Small for gestational age | 5 | [18] | 2019 | 51 | NR | OR | 1.01 | 1.00 | 1.03 | Low | ||||
| Autistic syndrome disorder | 9 | [17] | 2020 | 91 | <0.001 | RR | 1.06 | 1.01 | 1.11 | Moderate | |||||
| per 10 mcg/m3 | Short-term | Case-crossover | Adults, both sexes | Out-of-hospital cardiac arrest | 12 | [21] | 2017 | 70 | NR | RR | 1.04 | 1.01 | 1.07 | Low | |
| Time-series | Adults, both sexes | Cardiac arrhythmia | 17 | [22] | 2016 | 78 | NR | RR | 1.15 | 1.01 | 1.03 | Low | |||
| Daily cardiovascular mortality | 652 | [23] | 2019 | NR | NR | RR | 1.36 | 1.30 | 1.43 | Low | |||||
| Daily mortality | 652 | [23] | 2019 | NR | NR | RR | 1.68 | 1.59 | 1.77 | Low | |||||
| Daily respiratory mortality | 652 | [23] | 2019 | NR | NR | RR | 1.47 | 1.35 | 1.58 | Low | |||||
| Children (<18 years) | Pneumonia | 11 | [24] | 2017 | 38 | 0.08 | RR | 1.02 | 1.01 | 1.03 | Moderate |
LCI: lower confidence intervals; UCI: upper confidence intervals; NR: No reported; HR: hazard rations; RR: relative risk; IRF: integrated response function; F: function; OR: odds ratio.
Table 3.
Particulate matter less than 10 micrometers of diameter (PM10), desert dust, black carbon, long-term and short-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PM10 | per 2 mcg/m3 | Long-term | Cohort | Adults, both sexes | Chronic kidney disease | 4 | [5] | 2020 | 81 | 0.001 | RR | 1.16 | 1.05 | 1.29 | Low |
| per 10 mcg/m3 | Type 2 diabetes | 6 | [6] | 2020 | 68 | 0.004 | RR | 1.12 | 1.01 | 1.23 | Moderate | ||||
| Incidence of coronary events | 11 | [15] | 2014 | 0 | 0.81 | HR | 1.12 | 1.01 | 1.25 | Moderate | |||||
| Lung cancer mortality | 9 | [7] | 2018 | 93 | NR | RR | 1.07 | 1.03 | 1.11 | Low | |||||
| Cancer mortality | 12 | [7] | 2018 | 91 | <0.001 | RR | 1.09 | 1.04 | 1.14 | Moderate | |||||
| Incidence of chronic bronchitis | 3 | [16] | 2015 | NR | NR | RR | 1.11 | 1.04 | 1.18 | Low | |||||
| Children | Asthma | 12 | [36] | 2017 | 29 | 0.16 | OR | 1.05 | 1.02 | 1.08 | Moderate | ||||
| Pregnant women | Low birth weight | 11 | [18] | 2019 | 73 | NR | OR | 1.06 | 1.02 | 1.09 | Low | ||||
| Preterm birth | 8 | [18] | 2019 | 81 | NR | OR | 1.05 | 1.02 | 1.07 | Low | |||||
| Case-control | Children | Autism spectrum disorder | 6 | [20] | 2016 | 2 | 0.41 | OR | 1.07 | 1.06 | 1.08 | Moderate | |||
| Short-term | Case-crossover | Adults, both sexes | Out-of-hospital cardiac arrest | 9 | [21] | 2017 | 78 | NR | RR | 1.02 | 1.01 | 1.04 | Low | ||
| Time-series | Adults, both sexes | Cardiac arrhythmia | 12 | [22] | 2016 | 79 | NR | RR | 1.01 | 1 | 1.02 | Low | |||
| Daily cardiovascular mortality | 652 | [23] | 2019 | NR | NR | RR | 1.55 | 1.45 | 1.66 | Low | |||||
| Daily mortality | 652 | [23] | 2019 | NR | NR | RR | 1.44 | 1.39 | 1.5 | Low | |||||
| Daily respiratory mortality | 652 | [23] | 2019 | NR | NR | RR | 1.74 | 1.53 | 1.95 | Low | |||||
| per 20 mcg/m3 | Suicide | 7 | [12] | 2019 | 42 | 0.15 | RR | 1.02 | 1 | 1.03 | Moderate | ||||
| Children (<18 years) |
Pneumonia | 10 | [24] | 2017 | 66 | 0 | RR | 1.02 | 1.01 | 1.02 | Moderate | ||||
| Desert dust | per 10 mcg/m3 | Short-term | Time-series | Adults, both sexes | Cardiovascular mortality | 11 | [25] | 2016 | 0 | 0.77 | IR | 1.01 | 1 | 1.02 | Moderate |
| Mortality | 11 | [25] | 2016 | 0 | 0.75 | IR | 1.01 | 1 | 1.01 | Moderate | |||||
| Black carbon | per 0.5 × 10−5 M−1 | Long-term | Cohort | Children | Asthma | 8 | [36] | 2017 | 0 | 0.87 | OR | 1.08 | 1.03 | 1.14 | Moderate |
LCI: lower confidence intervals; UCI: upper confidence intervals; NR: No reported; HR: hazard rations; RR: relative risk; IRF: integrated response function; F: function; OR: odds ratio.
Particulate matter that includes PM2.5 and PM10 reported six diagnoses and causes of death related to short-term exposures (Table 2). In adults, short-term exposure to PM2.5 and PM10 were associated with out-of-hospital cardiac arrest [21], cardiac arrhythmia [22], daily cardiovascular, respiratory, and natural mortality [23]. In addition, for PM10, suicide was also reported as a short-term impact [12]. In children, short-term exposure to PM2.5 or PM10 was associated with pneumonia [24].
Desert dust, an important natural source of particulate matter, was also associated with health impacts (Table 3). This review identified one meta-analysis of adult exposure to desert dust, reporting an increased risk of cardiovascular mortality and natural mortality [25]. Another component of particulate matter is black carbon, which originates from fossil fuel and biomass combustion. We identified one meta-analysis on black carbon in children reporting an increased risk of asthma [19].
Nitrogen oxides (NOx and NO2) were associated with 18 different diagnoses and causes of death (Table 4). Pregnant women’s exposure to NOx was associated with low birth weight [18] and preterm birth [18]. For the same group, exposure to NO2 reported an increased risk of low birth weight [18] and small for gestational age [18]. For adults, long-term exposure to NO2 was associated with an increased risk of all-cause mortality [11], autistic syndrome disorder [17], cancer mortality [7], cardiovascular mortality [11], chronic kidney disease [5], cancer mortality [7], respiratory mortality [11], and type 2 diabetes [26]. Furthermore, for adults, short-term exposure to NO2 was associated with an increased risk of out-of-hospital cardiac arrest [21], cardiac arrhythmia [22], conjunctivitis [27], depression [28], and natural mortality [16]. Lastly, children’s long-term exposure to NO2 was associated with an increased risk of asthma [19], and short-term exposure with an increased risk of pneumonia [24].
Table 4.
Nitrogen oxides (NOx), nitrogen dioxide (NO2), long-term and short-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NO2 | per 4 mcg/m3 | Long-term | Cohort | Adults, both sexes | Autistic syndrome disorder | 7 | [17] | 2020 | 58 | 0.007 | RR | 1.02 | 1.01 | 1.04 | Low |
| per 10 mcg/m3 | Cancer mortality | 16 | [7] | 2018 | 95 | 0.003 | RR | 1.06 | 1.02 | 1.10 | Low | ||||
| Cardiovascular mortality | 18 | [11] | 2014 | 98 | NR | RR | 1.13 | 1.08 | 1.18 | Low | |||||
| Chronic kidney disease | 3 | [5] | 2020 | 0 | 0.47 | RR | 1.11 | 1.09 | 1.14 | Moderate | |||||
| All-cause mortality | 12 | [11] | 2014 | 89 | NR | RR | 1.04 | 1.01 | 1.06 | Low | |||||
| Respiratory mortality | 9 | [11] | 2014 | 0 | NR | RR | 1.02 | 1.02 | 1.03 | Moderate | |||||
| Type 2 diabetes | 6 | [26] | 2018 | 46 | <0.001 | RR | 1.11 | 1.07 | 1.16 | High | |||||
| Cancer mortality | 16 | [7] | 2018 | 95 | 0.003 | RR | 1.06 | 1.02 | 1.10 | Moderate | |||||
| Children | Asthma | 20 | [36] | 2017 | 65 | <0.001 | OR | 1.05 | 1.02 | 1.07 | Moderate | ||||
| Pregnant women | Low birth weight | 11 | [18] | 2019 | 32 | NR | OR | 1.02 | 1.00 | 1.04 | Moderate | ||||
| Small for gestational age | 5 | [18] | 2019 | 87 | NR | OR | 1.02 | 1.01 | 1.03 | Low | |||||
| per 10 mcg/m3 | Short-term | Time-series | Adults | Natural mortality | 30 | [16] | 2015 | NR | NR | RR | 1.002 | 1.002 | 1.004 | Low | |
| per 10 ppb | Case-crossover | Adults, both sexes | Out-of-hospital cardiac arrest | 11 | [21] | 2017 | 66 | NR | RR | 1.02 | 1.00 | 1.03 | Low | ||
| Time-series | Adults, both sexes | Cardiac arrhythmia | 13 | [22] | 2016 | 93 | NR | RR | 1.04 | 1.01 | 1.05 | Low | |||
| Conjunctivitis | 12 | [27] | 2019 | NR | NR | RR | 1.02 | 1.01 | 1.04 | Low | |||||
| per 20 ppb | Depression | 7 | [28] | 2020 | 65 | 0.008 | RE | 1.02 | 1.00 | 1.04 | Low | ||||
| Children (<18 years) |
Pneumonia | 10 | [24] | 2017 | 71 | 0 | RR | 1.01 | 1.00 | 1.02 | Moderate | ||||
| NOx | per 20 ppb | Long-term | Cohort | Pregnant women | Low birth weight | 3 | [18] | 2019 | 58 | NR | OR | 1.03 | 1.01 | 1.05 | Low |
| Preterm birth | 5 | [18] | 2019 | 88 | NR | OR | 1.02 | 1.01 | 1.03 | Low |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio.
Ozone (O3) was found as a risk factor for seven diagnoses and causes of death (Table 5). Long-term exposure to O3 was reported to increase IHD mortality [29] and Parkinson’s disease [14] in adults and for pregnant women with preterm birth [18]. Short-term exposure to ozone was associated as a risk factor for pneumonia in children [24] and in adults with out-of-hospital cardiac arrest [21], all-cause mortality [16], and cardiovascular and respiratory mortality [16].
Table 5.
Ozone (O3), Sulfur Dioxide (SO2), and Carbon Monoxide (CO), long-term and short-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| O3 | per 5 ppb | Long-term | Cohort | Adults, both sexes | Ischemic heart disease mortality | 4 | [29] | 2016 | 67 | 0.02 | RR | 1.02 | 1 | 1.04 | Low |
| per 10 mcg/m3 | Pregnant women | Preterm birth | 3 | [18] | 2019 | 0 | NR | OR | 1.04 | 1 | 1.07 | Moderate | |||
| per 10 ppb | Cohort and Case-Control | Adults, both sexes | Parkinson’s disease | 5 | [14] | 2019 | 0 | 0.69 | RR | 1.01 | 1 | 1.02 | Moderate | ||
| Short-term | Case-crossover | Adults, both sexes | Out-of-hospital cardiac arrest | 11 | [21] | 2017 | 53 | NR | RR | 1.02 | 1.01 | 1.02 | Low | ||
| per 20 ppb | Time-series | Children (<18 years) |
Pneumonia | 12 | [24] | 2017 | 75 | 0 | RR | 1.02 | 1.01 | 1.03 | Moderate | ||
| per 10 mcg/m3 | Adults | All-cause mortality | 32 | [16] | 2015 | NR | NR | RR | 1.003 | 1.001 | 1.004 | Low | |||
| Cardiovascular and respiratory mortality | 32 | [16] | 2015 | NR | NR | RR | 1.005 | 1.001 | 1.009 | Low | |||||
| SO2 | per 5 ppb | 1st pregnancy trimester | Cohort | Pregnant women | Gestational diabetes mellitus | 5 | [30] | 2020 | 93 | 0 | OR | 1.39 | 1.01 | 1.77 | Moderate |
| per 10 mcg/m3 | Long-term | Cohort | Pregnant women | Low birth weight | 5 | [18] | 2019 | 98 | NR | OR | 1.21 | 1.08 | 1.35 | Low | |
| per 10 ppb | Short-term | Time-series | Adults, both sexes | Cardiac arrhythmia | 10 | [22] | 2016 | 77 | NR | RR | 1.02 | 1 | 1.04 | Low | |
| Children (<18 years) |
Pneumonia | 8 | [24] | 2017 | 48 | 0.04 | RR | 1.03 | 1 | 1.05 | Moderate | ||||
| CO | per 1 mcg/m3 | Long-term | Cohort | Pregnant women | Preterm birth | 7 | [18] | 2019 | 89 | NR | OR | 1.06 | 1.04 | 1.08 | Low |
| per 1 ppm | Short-term | Case-crossover | Adults, both sexes | Out-of-hospital cardiac arrest | 11 | [21] | 2017 | 44 | NR | RR | 1.06 | 1 | 1.14 | Moderate | |
| Time-series | Adults, both sexes | Cardiac arrhythmia | 12 | [22] | 2016 | 90 | NR | RR | 1.04 | 1.02 | 1.06 | Low | |||
| per 1000 ppb | Children (<18 years) |
Pneumonia | 7 | [24] | 2017 | 68 | 0.004 | RR | 1.01 | 1 | 1.02 | Low |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio.
Sulfur dioxide (SO2) is a prevalent pollutant and was found as a risk factor for four diagnoses (Table 5). SO2 is a gas primarily emitted from fossil fuel combustion at power plants and other industrial facilities as well as from fuel combustion in mobile sources like locomotives or ships. In their first trimester, pregnant women exposed to SO2 reported an increased risk of gestational diabetes mellitus [30]. Pregnant women exposed during any trimester also reported an increased risk of low birth weight [18]. Short-term exposures to SO2 were associated with pneumonia in children [24] and cardiac arrhythmia in adults [22].
Carbon monoxide (CO) is a gas produced by fuel combustion in motorizing vehicles, small engines, stoves, and fireplaces, among others (Table 5). We identified four health impacts associate with CO exposure. In short term exposures, CO was reported as a risk factor for pneumonia in children [24], and cardiac arrhythmia [22], and out-of-hospital cardiac arrest in adults [21]. CO exposure during pregnancy was also reported as a risk factor for preterm birth [18].
Household air pollution represents indoor air pollution from multiple sources (e.g., cooking and heating) (Table 6). Under this review, we identified five types of cancers related to household air pollution exposure. Specifically, one meta-analysis reported an increased risk for cervical, laryngeal, nasopharyngeal, oral, and pharyngeal cancers [31]. Indoor air pollution from solid fuels was also found as a risk factor for hypertension [32]. Solid fuel use by pregnant women was associated with low birth weight, stillbirth, preterm birth, and intrauterine growth retardation in another meta-analysis [33]. Finally, biomass burning was associated with an increased risk of esophageal squamous cell carcinoma [34] and COPD [35].
Table 6.
Household Air Pollution, indoor air pollution from solid fuel, biomass burning, and long-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Household air pollution | Exposed vs. not exposed | Long-term | Case-controls | Adults, both sexes | Cervical cancer | 4 | [31] | 2015 | NR | 0.45 | OR | 6.46 | 3.12 | 13.36 | Low |
| Laryngeal cancer | 5 | [31] | 2015 | NR | 0.49 | OR | 2.35 | 1.72 | 3.21 | Low | |||||
| Nasopharyngeal cancer | 6 | [31] | 2015 | NR | 0.06 | OR | 1.8 | 1.42 | 2.29 | Low | |||||
| Oral cancer | 4 | [31] | 2015 | NR | 0.93 | OR | 2.44 | 1.87 | 3.19 | Low | |||||
| Pharyngeal cancer | 4 | [31] | 2015 | NR | 0.99 | OR | 3.56 | 2.22 | 5.7 | Low | |||||
| Indoor air pollution from solid fuel | Exposed vs. not exposed | Long-term | Cohort | Adults, both sexes | Hypertension | 11 | [32] | 2020 | 90 | 0 | OR | 1.52 | 1.26 | 1.85 | Moderate |
| Solid fuel use | Exposed vs. not exposed | Long-term | Cohort | Pregnant women | Low birth weight | 12 | [33] | 2014 | 28 | 0.07 | OR | 1.35 | 1.23 | 1.48 | Moderate |
| Stillbirth | 5 | [33] | 2014 | 0 | 0.44 | OR | 1.29 | 1.18 | 1.41 | Moderate | |||||
| Preterm birth | 3 | [33] | 2014 | 0 | 0.39 | OR | 1.30 | 1.06 | 1.59 | Moderate | |||||
| Intrauterine growth retardation | 2 | [33] | 2014 | 0 | 0.89 | OR | 1.23 | 1.01 | 1.49 | Moderate | |||||
| Biomass burning | Exposed vs. not exposed | Long-term | Case-controls | Adults, both sexes | Esophageal squamous cell carcinoma | 16 | [34] | 2019 | 79 | NR | OR | 3.02 | 2.22 | 4.11 | Low |
| Cohort and Case-Control | Adults, both sexes | Chronic Obstructive Pulmonary Disease | 8 | [35] | 2017 | 93 | <0.001 | OR | 2.21 | 1.3 | 3.76 | Moderate |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; OR: odds ratio.
3.3. Environmental Tobacco Smoke
Environmental tobacco smoke is an involuntary exposure to tobacco smoke, also known as passive smoke or secondhand smoke. Environmental tobacco smoke is generated by tobacco products’ combustion and is a complex mixture of over 4000 compounds. These include more than 40 known or suspected human carcinogens, such as 4-aminobiphenyl, 2-naphthylamine, benzene, nickel, and various polycyclic aromatic hydrocarbons (PAHs) and N-nitrosamines. Furthermore present are several irritants, such as ammonia, nitrogen oxides, sulfur dioxide, and aldehydes, and cardiovascular toxicants, such as carbon monoxide, nicotine, and some PAHs [37,38].
This review identified 23 diseases and causes of death related to environmental tobacco smoke, parental, and prenatal smoke (Table 7). Specifically, environmental tobacco smoke was reported to be associated in adults with stroke [39], lung cancer in women [40], and in pregnant women with low birth weight [37] and small for gestational age [37]. Passive smoking was associated in adults with an increased risk of breast cancer [41], cardiovascular disease [42], cervical cancer [43], lung cancer, lung adenocarcinoma, large cell lung cancer, small cell lung cancer, squamous cell carcinoma [44], all-cause mortality [42], and type 2 diabetes [45]. In pregnant women, passive smoking was associated with neural tube defects [46]. In children, passive smoking was associated as a risk factor for asthma [47] and otitis media [48]. Prenatal smoke was found to be associated with schizophrenia [49], offspring depression [50], and attention-deficit/hyperactivity disorder [51]. Parental smoke with childhood obesity [52], maternal smoke with neuroblastoma [53], and paternal smoke with acute myeloid leukemia [54] and acute lymphoblastic leukemia [55].
Table 7.
Environmental Tobacco Smoke and long-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Environmental tobacco smoke | Exposed vs. not exposed | Long-term | Cohort | Adults, both sexes | Stroke | 23 | [39] | 2017 | NR | NR | RR | 1.15 | 1.06 | 1.24 | Low |
| Cohort and Case-Control | Women | Lung cancer | 41 | [40] | 2018 | NR | <0.05 | RR | 1.33 | 1.17 | 1.51 | Low | |||
| Pregnant women | Low birth weight | 10 | [37] | 2008 | 54 | 0.009 | OR | 1.32 | 1.07 | 1.63 | Moderate | ||||
| Small for gestational age | 9 | [37] | 2008 | 0 | 0.004 | OR | 1.21 | 1.06 | 1.37 | Moderate | |||||
| Parental smoking | Exposed vs. not exposed | Long-term | Cohort | Children | Childhood obesity | 6 | [52] | 2014 | 0 | NR | RR | 1.33 | 1.23 | 1.44 | Moderate |
| Paternal smoking | Exposed vs. not exposed | Long-term | Case-controls | Children | Acute myeloid leukemia | 17 | [54] | 2019 | 0.5 | 0.003 | OR | 1.15 | 1.038 | 1.275 | Moderate |
| Exposed vs. not exposed | Long-term | Case-controls | Children | Acute lymphoblastic leukemia | 10 | [55] | 2012 | 28 | 0.18 | OR | 1.15 | 1.06 | 1.24 | Moderate | |
| Maternal smoking | Exposed vs. not exposed | Long-term | Case-controls | Children | Neuroblastoma | 14 | [53] | 2019 | 17 | NR | OR | 1.1 | 1.0 | 1.3 | Moderate |
| Passive smoking | Exposed vs. not exposed | Long-term | Case-controls | Adults, both sexes | Lung adenocarcinoma | 18 | [44] | 2014 | NR | 0.26 | OR | 1.35 | 1.23 | 1.48 | Low |
| Lung cancer | 18 | [44] | 2014 | NR | 0.01 | OR | 1.34 | 1.24 | 1.45 | Low | |||||
| Lung large cell cancer | 18 | [44] | 2014 | NR | 0.68 | OR | 1.36 | 1.04 | 1.79 | Low | |||||
| Lung small cell cancer | 18 | [44] | 2014 | NR | 0.98 | OR | 1.63 | 1.31 | 2.04 | Low | |||||
| Lung squamous cell carcinoma | 18 | [44] | 2014 | NR | 0.06 | OR | 1.36 | 1.17 | 1.58 | Low | |||||
| Pregnant women | Neural tube defects | 11 | [46] | 2018 | 50 | 0.02 | OR | 1.90 | 1.56 | 2.31 | Low | ||||
| Cohort | Adults, both sexes | Cardiovascular disease | 38 | [42] | 2015 | 66 | 0 | RR | 1.23 | 1.16 | 1.31 | Moderate | |||
| All-cause mortality | 11 | [42] | 2015 | 69 | 0 | RR | 1.18 | 1.10 | 1.27 | Moderate | |||||
| Type 2 diabetes | 7 | [26] | 2018 | 31 | <0.001 | RR | 1.22 | 1.10 | 1.35 | High | |||||
| Cohort and Case-Control | Women | Breast cancer | 51 | [41] | 2014 | 75 | <0.001 | OR | 1.62 | 1.39 | 1.85 | Moderate | |||
| Cervical cancer | 14 | [43] | 2018 | 64 | 0 | OR | 1.70 | 1.40 | 2.07 | Moderate | |||||
| Cohort | Children | Asthma | 41 | [47] | 2020 | 86 | <0.01 | OR | 1.21 | 1.15 | 1.26 | Low | |||
| Otitis Media | 9 | [48] | 2014 | 80 | 0.04 | OR | 1.39 | 1.02 | 1.89 | Low | |||||
| Prenatal smoke | Exposed vs. not exposed | Long-term | Cohort | Pregnant women | Schizophrenia | 7 | [49] | 2020 | 71 | NR | OR | 1.29 | 1.10 | 1.51 | Low |
| Offspring depression | 4 | [50] | 2017 | 54 | 0.084 | OR | 1.20 | 1.08 | 1.34 | Low | |||||
| Cohort and Case-Control | Attention-deficit/hyperactivity disorder | 20 | [51] | 2017 | 79 | 0.000 | OR | 1.60 | 1.45 | 1.76 | Moderate |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio.
3.4. Chemicals, Pesticides, and Heavy Metals
This review identified two health outcomes associated with childhood exposure to 1,3-butadiene (Table 8). 1,3-Butadiene is a synthetic gas used primarily as a monomer to manufacture many different polymers and copolymers and as a chemical intermediate in industrial chemical production. Motor vehicle exhaust is also a source of 1,3-butadiene. One meta-analysis found that long-term exposure to 1,3-Butadiene during childhood increased the risk of acute lymphoblastic leukemia and all leukemias [56]. Another group of chemicals found to be associated with health impacts were the hydrocarbons (Table 8). Hydrocarbons are present in a broad range of products, including petroleum and other fuels, solvents, paints, glues, and cleaning products [57]. A meta-analysis of 14 studies showed that long-term exposure to hydrocarbons was associated with Parkinson’s disease [58]. Organic solvents and other solvents were also found to be associated with neurological and rheumatological diseases (Table 8). Specifically, long-term exposure to organic solvents was associated with multiple sclerosis [59] and Parkinson’s disease [58]. Long-term exposure to solvents was also found to be associated with an increased risk of systemic sclerosis [60]. Organic solvents are used in many industries. They are used in paints, varnishes, lacquers, adhesives, glues, and degreasing and cleaning agents, and the production of dyes, polymers, plastics, textiles, printing inks, agricultural products, and pharmaceuticals.
Table 8.
Chemicals and long-term health impacts.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1,3-Butadiene | High exposed vs. low exposed | Long-term | Case-controls | Children | Acute lymphoblastic leukemia | 2 | [56] | 2019 | 0 | 0 | RR | 1.31 | 1.11 | 1.54 | High |
| All leukemia | 2 | [56] | 2019 | 28 | 0.025 | RR | 1.45 | 1.08 | 1.95 | Moderate | |||||
| Bisphenol A | High exposed vs. low exposed | Long-term | Cohort | Adults, both sexes | Diabetes | 3 | [64] | 2015 | 0 | 0.55 | OR | 1.47 | 1.21 | 1.80 | Moderate |
| Obesity | 3 | [64] | 2015 | 0 | 0.44 | OR | 1.67 | 1.41 | 1.98 | Moderate | |||||
| Dioxins | High exposed vs. low exposed | Long-term | Cohort | Women | Endometriosis | 10 | [62] | 2019 | 72 | <0.01 | OR | 1.65 | 1.14 | 2.39 | Low |
| Hydrocarbon exposure | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Parkinson’s disease | 14 | [58] | 2016 | 28 | NR | OR | 1.36 | 1.13 | 1.63 | Moderate |
| Mono (2-ethyl-5-hydroxyhexyl) phthalate |
High exposed vs. low exposed | Long-term | Cohort and Case-Control | Women | Endometriosis | 6 | [65] | 2019 | 44 | 0.11 | OR | 1.24 | 1.00 | 1.54 | Moderate |
| Organic solvents | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Multiple sclerosis | 15 | [59] | 2015 | 77 | 0.06 | RR | 1.54 | 1.03 | 2.29 | Low |
| Parkinson’s disease | 18 | [58] | 2016 | 43 | NR | OR | 1.22 | 1.01 | 1.47 | Moderate | |||||
| Polychlorinated biphenyls (PCBs) | High exposed vs. low exposed | Long-term | Cohort | Women | Endometriosis | 9 | [62] | 2019 | 78 | <0.01 | OR | 1.70 | 1.20 | 2.39 | Low |
| High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | Non-Hodgkin Lymphoma | 7 | [61] | 2012 | NR | NR | OR | 1.43 | 1.31 | 1.55 | Low | |
| Polychlorinated biphenyls 153 | per log2 ng/L | Long-term | Cohort | Children | Bronchitis | 7 | [63] | 2014 | NR | 0.89 | RR | 1.06 | 1.01 | 1.12 | Low |
| Solvents | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Systemic sclerosis | 11 | [60] | 2018 | 55 | <0.001 | OR | 2.41 | 1.73 | 3.37 | Moderate |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio.
In adults, long-term exposure to polychlorinated biphenyls (PCBs) were found to be associated with non-Hodgkin lymphoma [61], in women with endometriosis [62], and in children (<18 months of age), PCB 153 was found to be associated win increase risk of bronchitis [63] (Table 8). Polychlorinated biphenyls are a large group of human-made organic chemicals that, due to their properties like non-flammability, chemical stability, high boiling point, and electrical insulating capacity, are widely used industrial and commercial applications. Bisphenol A (BPA), a chemical used primarily in the production of polycarbonate plastics and epoxy resins, for example, in food and drink packaging, was found to be a risk factor for diabetes [64] and obesity in adults [64] (Table 8). Women’s exposure to mono-(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP) has been found as a risk factor for endometriosis [65] (Table 8). MEHHP is a metabolite of phthalate acid esters (PAEs). MEHHP is often found in the blood and tissues of the general population. Studies have shown that women are more likely to be exposed to PAEs through products such as perfume, cosmetics, and personal care products. The review found evidence of dioxins as a risk factor for endometriosis [62] (Table 8). Dioxins are a group of chemically-related compounds that are persistent environmental pollutants (POPs). Dioxins are unwanted by-products of a wide range of manufacturing processes, including smelting, chlorine bleaching of paper pulp, manufacturing some herbicides and pesticides, and incinerators.
Pesticide exposure also was found by multiple meta-analyses as a risk factor for several diseases in adults and children (Table 9 and Table 10). In adults, pesticides, in general, were found to be associated with Alzheimer’s disease [66], amyotrophic lateral sclerosis [67], brain tumors [68], myelodysplastic syndromes [69], and Parkinson’s disease [70]. Organochlorine pesticides were associated with endometriosis [62]. Paraquat, a dichloride pesticide, was also found to be related to Parkinson’s disease [71]. Non-Hodgkin lymphoma was also associated with multiple types of pesticides, like organophosphate [72], organochlorine [73], chlordane [73], diazinon [72], hexachlorobenzene [73], hexachlorocyclohexane [73], and dichlorodiphenyldichloroethylene(DDE) pesticides [73]. Finally, children (<18 months of age) reported a higher risk of bronchitis when exposed to DDE [63], and children’s residential exposure to pesticides was reported as a risk factor for acute lymphoblastic leukemia, acute myeloid leukemia, and childhood leukemia [74].
Table 9.
Pesticides and health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pesticides | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Alzheimer’s disease | 7 | [66] | 2016 | 0 | 0.885 | OR | 1.34 | 1.08 | 1.67 | Moderate |
| High exposed vs. low exposed | Cohort and Case-Control | Adults, both sexes | Amyotrophic lateral sclerosis | 7 | [67] | 2016 | 41 | 0.16 | RR | 1.20 | 1.02 | 1.41 | Moderate | ||
| High exposed vs. low exposed | Case-controls | Children | Brian tumors | 18 | [68] | 2017 | 0 | NR | OR | 1.26 | 1.13 | 1.14 | Moderate | ||
| Exposed vs. not exposed | Case-controls | Adults, both sexes | Myelodysplastic Syndromes | 11 | [69] | 2014 | 80 | 0 | OR | 1.95 | 1.23 | 3.09 | Moderate | ||
| 10 years of exposure vs. no exposure | Cohort | Adults, both sexes | Parkinson’s disease | 10 | [70] | 2018 | 50 | 0.032 | OR | 1.11 | 1.05 | 1.18 | Low | ||
| Residential pesticide exposure | High exposed vs. low exposed | Long-term | Case-controls | Children | Acute lymphoblastic leukemia | 8 | [74] | 2019 | NR | NR | OR | 1.42 | 1.13 | 1.80 | Low |
| Acute myeloid leukemia | 5 | [74] | 2019 | NR | NR | OR | 1.90 | 1.35 | 2.67 | Low | |||||
| Childhood leukemia | 15 | [74] | 2019 | 73 | NR | OR | 1.57 | 1.27 | 1.95 | Low |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio.
Table 10.
Pesticides and health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure temporality | Study Design | Population | Health outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chlordane | High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | non-Hodgkin lymphoma | 8 | [73] | 2016 | 17 | 0.29 | OR | 1.93 | 1.51 | 2.48 | Moderate |
| Diazinon | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | non-Hodgkin lymphoma | 7 | [72] | 2017 | 0 | 0.668 | OR | 1.39 | 1.11 | 1.73 | Moderate |
| Dichlorodiphenyldichloroethylene (DDE) | High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | non-Hodgkin lymphoma | 11 | [73] | 2016 | 0 | 0.94 | OR | 1.38 | 1.14 | 1.66 | Moderate |
| per log2 ng/L | Long-term | Cohort | Children | Bronchitis | 7 | [63] | 2014 | NR | 0.38 | RR | 1.05 | 1.00 | 1.11 | Low | |
| Hexachlorobenzene | High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | non-Hodgkin lymphoma | 7 | [73] | 2016 | 0 | 0.64 | OR | 1.54 | 1.20 | 1.99 | Moderate |
| Hexachlorocyclohexane | High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | non-Hodgkin lymphoma | 6 | [73] | 2016 | 34 | 0.17 | OR | 1.42 | 1.08 | 1.87 | Moderate |
| Organochlorine pesticides | High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | non-Hodgkin lymphoma | 13 | [73] | 2016 | 12 | 0.253 | OR | 1.40 | 1.27 | 1.56 | Moderate |
| Cohort | Women | Endometriosis | 5 | [62] | 2019 | 65 | 0.02 | OR | 1.97 | 1.25 | 3.13 | Low | |||
| Organophosphate pesticides | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | non-Hodgkin lymphoma | 10 | [72] | 2017 | 41 | 0.032 | OR | 1.22 | 1.04 | 1.43 | Moderate |
| Paraquat | Exposed vs. not exposed | Long-term | Case-controls | Adults, both sexes | Parkinson’s disease | 14 | [71] | 2019 | 31 | 0.126 | OR | 1.70 | 1.28 | 2.25 | Moderate |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; OR: odds ratio.
In terms of mineral and heavy metals, aluminum, asbestos, cadmium, chromium, arsenic, lead, and silica, were also associated with multiples health outcomes (Table 11). Aluminum was associated with dementia in adults [45]. Non-occupational asbestos was associated with mesothelioma [75]. Cadmium exposure was associated with cancer, especially lung cancer [76]. Chromium exposure was associated with schizophrenia [77]. Inorganic arsenic was associated with type 2 diabetes [78]. Lead exposure to amyotrophic lateral sclerosis [79] and mild mental retardation [80]. Silica exposure with systemic sclerosis [60].
Table 11.
Heavy metals, minerals and long-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALUMINUM | Exposed vs. not exposed | Long-term | Cohort | Adults, both sexes | Dementia | 8 | [45] | 2017 | 6.2 | <0.001 | OR | 1.72 | 1.33 | 2.21 | High |
| Asbestos (non-occupational) | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Mesothelioma | 27 | [75] | 2018 | 99 | NR | RR | 5.33 | 2.53 | 11.23 | Low |
| Cadmium | High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | Cancer | 3 | [76] | 2015 | 0 | 0.84 | RR | 1.22 | 1.13 | 1.31 | Moderate |
| Lung Cancer | 3 | [76] | 2015 | 0 | 0.41 | RR | 1.68 | 1.47 | 1.92 | Moderate | |||||
| Chromium | High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | Schizophrenia | 7 | [77] | 2019 | >50 | <0.01 | SMD | 0.32 | 0.01 | 0.63 | Moderate |
| Inorganic arsenic | High exposed vs. low exposed | Long-term | Cohort | Adults, both sexes | Type 2 diabetes | 3 | [78] | 2014 | 39 | 0.18 | RR | 1.39 | 1.06 | 1.81 | Moderate |
| Lead | High exposed vs. low exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Amyotrophic lateral sclerosis | 3 | [79] | 2020 | 51 | 0.01 | RR | 1.46 | 1.16 | 1.83 | Low |
| Blood levels in mg/L | Long term | Cohort | Children | Mild mental retardation | 7 | [80] | 2005 | NR | NR | OR | F | F | F | Low | |
| Silica exposure | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Systemic sclerosis | 16 | [60] | 2018 | 96 | 0.002 | OR | 2.96 | 1.65 | 5.29 | Low |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio; SMD: standard median difference; F: function.
3.5. Physical Exposures
Physical exposures refer to environmental factors such as temperature, noise, or radiation. Our review identified 21 meta-analyses covering 14 physical environmental exposures and 27 different diseases or causes of death among children, women, adults, and elderly populations. Ambient temperature and extreme weather were the most common physical environmental risk factor studied among the meta-analysis found in this review (Table 12). Changes in ambient temperature (increases or decreases) were related to short-term health impacts. Particularly in adults, increases in the ambient temperature above the 93rd percentile were found to be a risk factor of suicide [81], those expose to temperatures above 90th percentile or below 10th percentile to diabetes mortality [82], and those under orthopedic procedure during warmer weather periods of the year had an increased risk of postoperative infection [83]. Comparing high versus low temperatures, high temperature increases the risk of low birth weight and stillbirth among pregnant women [84]. Furthermore, changes in diurnal temperature by increases of 10 degrees Celsius were related to increased mortality [85]. Furthermore, heatwaves, defined as a high temperature lasting for several days, were associated with cardiovascular and respiratory mortality in adults [86] and preterm birth [84]. For the elderly populations, heat changes by 1 Celsius degree increment above a threshold were related to acute renal failure, cardiovascular disease mortality, cerebrovascular mortality, diabetes, ischemic heart disease mortality, respiratory disease, and respiratory mortality [87]. In terms of cold temperatures, reductions of 1 Celsius degree during winter times were related to an increased risk of cardiovascular mortality, cerebrovascular mortality, intracerebral hemorrhage, pneumonia, and respiratory mortality [87]. Cold waves were also associated with cardiovascular mortality [88]. For children, reductions of 1 degree Celsius during cold weather were related to an increased risk of asthma(<12 years old) [89].
Table 12.
Ambient temperature and short-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ambient temperature | Maximum suicide temperature 93rd percentile vs. minimum suicide temperature | Short-term | Time-series | Adults, both sexes | Suicide | 341 | [81] | 2019 | 3.3 | NR | RR | 1.33 | 1.30 | 1.36 | Moderate |
| Orthopedic procedures during warmer periods of the year | Short-term | Time-series | Adults, both sexes | Post-operative infection | 12 | [83] | 2019 | 65 | 0.001 | OR | 1.16 | 1.04 | 1.30 | Moderate | |
| High versus low temperatures | Short-term | Time-series | Pregnant women | Low birth weight | 9 | [84] | 2020 | NR | NR | OR | 1.07 | 1.05 | 1.16 | Low | |
| Stillbirth | 2 | [84] | 2020 | 27.8 | NR | OR | 3.39 | 2.33 | 4.96 | Moderate | |||||
| Cold | per 1 Celsius degree decrease | Short-term | Time-series | Children <12 years | Asthma | 13 | [89] | 2017 | NR | NR | OR | 1.07 | 1.01 | 1.12 | Low |
| Elderly | Cardiovascular disease mortality | 9 | [87] | 2016 | 98 | <0.0001 | RR | 1.01 | 1.00 | 1.00 | Moderate | ||||
| Cerebrovascular mortality | 3 | [87] | 2016 | 60 | 0.001 | RR | 1.01 | 1.00 | 1.01 | Low | |||||
| Intracerebral hemorrhage | 2 | [87] | 2016 | 0 | 0.39 | RR | 1.01 | 1.01 | 1.02 | Moderate | |||||
| Pneumonia | 5 | [87] | 2016 | 94 | <0.0001 | RR | 1.06 | 1.01 | 1.12 | Moderate | |||||
| Respiratory disease mortality | 8 | [87] | 2016 | 90 | <0.0001 | RR | 1.02 | 1.00 | 1.00 | Moderate | |||||
| 10th and 1st percentile vs. 25th percentile of temperature | Short-term | Time-series | Adults, both sexes | Diabetes mortality | 9 | [82] | 2016 | NR | NR | RR | 1.11 | 1.03 | 1.19 | Low | |
| Cold wave | Exposed vs. not exposed | Short-term | Time-series | Adults, both sexes | Cardiovascular mortality | 31 | [88] | 2020 | 84.3 | <0.001 | OR | 1.54 | 1.21 | 1.97 | Moderate |
| Diurnal temperature range | per 10 Celsius degrees | Short-term | Time-series | Adults, both sexes | Mortality | 308 | [98] | 2018 | NR | NR | RR | 1.03 | 1.02 | 1.03 | Low |
| Heat | 90th and the 99th percentile vs. 75th percentile of temperature | Short-term | Time-series | Adults, both sexes | Diabetes mortality | 9 | [82] | 2016 | NR | NR | RR | 1.20 | 1.12 | 1.3 | Low |
| per 1 Celsius degree increase | Short-term | Time-series | Elderly | Acute renal failure | 2 | [87] | 2016 | 16 | 0.27 | RR | 1.01 | 1.01 | 1.02 | Moderate | |
| Cardiovascular disease mortality | 15 | [87] | 2016 | 99 | <0.0001 | RR | 1.03 | 1.03 | 1.04 | Moderate | |||||
| Cerebrovascular mortality | 3 | [87] | 2016 | 72 | 0.03 | RR | 1.01 | 1.00 | 1.02 | Low | |||||
| Diabetes | 3 | [87] | 2016 | 25 | 0.26 | RR | 1.01 | 1.00 | 1.01 | Moderate | |||||
| Ischemic heart disease mortality | 3 | [87] | 2016 | 81 | 0.004 | RR | 1.01 | 1.00 | 1.03 | Low | |||||
| Respiratory disease | 11 | [87] | 2016 | 82 | <0.0001 | RR | 1.02 | 1.01 | 1.04 | Moderate | |||||
| Respiratory disease mortality | 9 | [87] | 2016 | 92 | <0.0001 | RR | 1.00 | 1.00 | 1.00 | Moderate | |||||
| Heatwave | Exposed vs. not exposed | Short-term | Time-series | Adults, both sexes | Cardiovascular mortality | 36 | [86] | 2019 | 99 | <0.01 | RE | 1.15 | 1.09 | 1.21 | Low |
| Respiratory mortality | 27 | [86] | 2019 | 97 | <0.01 | RE | 1.18 | 1.09 | 1.28 | Low | |||||
| Pregnant women | Preterm birth | 6 | [84] | 2020 | 44.7 | 0.11 | OR | 1.16 | 1.10 | 1.23 | Moderate |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio.
Natural and artificial light exposure was also associated with positive and negative health impacts (Table 13). Outdoor light exposure was found as a protective factor for myopia in children [90]. The main explanation for this effect is the impact of sunlight on eyeball size, neurotransmitters released in the retina, and vitamin D synthesis. In contrast, artificial light exposure at night was associated as a risk factor for women’s breast cancer [91]. The main explanation for the increased risk of breast cancer is the impact of artificial light on reducing sleep duration and melatonin release. Melatonin is suggested as a carcinogenesis inhibitor; thus, low melatonin concentrations could contribute to breast cancer development. Ultraviolet radiation was found to be a protective factor for positive Epstein–Barr Virus Hodgkin lymphoma in adults [92], and recreational sun exposure was associated with non-Hodgkin lymphoma [93].
Table 13.
Light, noise, radon, electromagnetic fields, and long-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Artificial light exposure at night | High exposed vs. low exposed | Long-term | Case-controls | Women | Breast cancer | 6 | [91] | 2014 | 1.9 | 0.4 | RR | 1.17 | 1.11 | 1.24 | Moderate |
| Outdoor light exposure | High exposed vs. low exposed | Long-term | Cohort | Children | Myopia | 4 | [90] | 2019 | 91 | 0.02 | OR | 0.57 | 0.35 | 0.92 | Low |
| Ultraviolet radiation | High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | Epstein–Barr Virus positive Hodgkin lymphoma |
4 | [92] | 2013 | NR | 0.10 | OR | 0.59 | 0.36 | 0.96 | Low |
| Recreational sun exposure | High exposed vs. low exposed | Long-term | Case-controls | Adults, both sexes | Non-Hodgkin lymphoma | 4 | [93] | 2008 | NR | 0.001 | OR | 0.76 | 0.63 | 0.91 | Moderate |
| Extremely low-frequency electromagnetic fields | High exposed vs. low exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Amyotrophic lateral sclerosis | 5 | [67] | 2016 | 58 | 0.34 | RR | 1.30 | 1.10 | 1.60 | Low |
| High vs. low current wiring configuration codes | Long-term | Cohort and Case-Control | Children | Childhood leukemia | 6 | [99] | 1999 | NR | NR | OR | 1.46 | 1.05 | 2.04 | Low | |
| Indoor radon | Exposed vs. not exposed | Long-term | Case-controls | Adults, both sexes | Lung cancer | 31 | [100] | 2019 | NR | NR | OR | 1.14 | 1.08 | 1.21 | Low |
| High exposed vs. low exposed | Long-term | Case-controls | Children | Leukemia | 7 | [101] | 2012 | 9 | 0.36 | OR | 1.37 | 1.02 | 1.82 | Moderate | |
| Noise | High exposed vs. low exposed | Long-term | Cohort | Adults, both sexes | Diabetes | 5 | [94] | 2018 | 31 | 0.18 | HR | 1.04 | 1.02 | 1.07 | Moderate |
| per 5 dB | Hypertension | 5 | [95] | 2017 | 51 | 0.086 | RR | 1.20 | 1.09 | 1.31 | Low | ||||
| Road traffic noise | per 5 dB | Long-term | Cohort | Adults, both sexes | Diabetes | 3 | [94] | 2018 | 33 | 0.222 | HR | 1.07 | 1.02 | 1.12 | Moderate |
| per 10 dB (Lden) | Ischemic heart disease | 7 | [97] | 2018 | NR | NR | RR | 1.08 | 1.01 | 1.15 | Low | ||||
| Men | Hypertension | 2 | [96] | 2018 | 0 | <0.001 | RR | 1.62 | 1.02 | 1.09 | High |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio; HR: hazard ratio.
The noise was another environmental risk factor that was found to be associated with non-communicable diseases (Table 13). In particular, noise exposure from any source was found to be a risk factor for diabetes [94], and each increment of 5 decibels of ambient noise was associated with an increased risk of hypertension [95]. In addition, road traffic noise increments were associated with diabetes [94], hypertension in men [96], and ischemic heart disease [97].
Radon, a radioactive natural, was found in a recent meta-analysis as a risk factor for lung cancer [100] at indoor radon exposure levels above 100 Bq/m3 (Table 13). In another meta-analysis, indoor radon exposure was also associated as a risk factor for childhood leukemia [101]. Finally, long-term exposures to extremely low-frequency electromagnetic fields were also found associated as a risk factor for amyotrophic lateral sclerosis [67] and childhood leukemia [99] (Table 13). Extremely low-frequency (ELF) magnetic fields are alternating fields generated by the distribution and supply of electricity.
3.6. Residential Surroundings
In this category, we summarized the environmental exposures related to residential surroundings, such as greenness, proximity to roadways and petrochemical complexes, or the degree of urbanization. We also located other residential exposures, such as the presence of pets that are suggested as a protective factor for non-communicable diseases. We identified two meta-analyses associating residential greenness as a protective factor for adults and newborns health (Table 14). Specifically, we found evidence that greenness in a 300 m buffer around homes was associated with a reduced risk for mortality in adults [102] and a reduced risk of low birth weight [103]. In addition, residential greenness in a 500 m buffer from homes was also associated with a reduced risk of newborns being small for their gestational age [103]. Living near major roadways or being exposed to traffic around homes was found as a risk factor for type 2 diabetes in adults [104] and leukemia in children [105] (Table 14). Living near petrochemical industrial complexes was also found to produce multiple types of leukemias (Table 14). Specifically, living in an 8 km radius from a petrochemical complex was found to be a risk factor for acute myeloid leukemia, chronic lymphocytic leukemia, and all leukemias [106].
Table 14.
Greenness, major roads, petrochemical, and long-term health outcomes.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Petrochemical industrial complexes | Residence >8 km distance from petrochemical industrial complexes | Long-term | Cohort and Case-Control | Adults, both sexes | Acute myeloid leukemia | 7 | [106] | 2020 | 50 | 0.01 | RR | 1.61 | 1.12 | 2.31 | Low |
| Chronic lymphocytic leukemia | 7 | [106] | 2020 | 92 | 0.048 | RR | 1.85 | 1.01 | 6.42 | Low | |||||
| Leukemia | 13 | [106] | 2020 | 73 | 0.001 | RR | 1.36 | 1.14 | 1.62 | Low | |||||
| Proximity to major roadways | Exposed vs. not exposed | Long-term | Cohort | Adults, both sexes | Type 2 diabetes | 6 | [104] | 2017 | 36 | 0.025 | RR | 1.13 | 1.02 | 1.27 | Moderate |
| Residential traffic exposure | High exposed vs. low exposed | Long-term | Case-controls | Children | Childhood leukemia | 7 | [105] | 2014 | 57 | 0.02 | OR | 1.39 | 1.03 | 1.88 | Low |
| Residential greenness | per 0.1 NDVI within 300 m buffer from residence | Long-term | Cohort | Adults, both sexes | All-cause mortality | 9 | [102] | 2019 | 95 | <0.001 | HR | 0.96 | 0.94 | 0.97 | Low |
| Low birth weight | 10 | [103] | 2020 | 41 | <0.001 | RR | 0.98 | 0.97 | 0.99 | High | |||||
| per 0.1 NDVI within 500 m buffer from residence | Small for gestational age | 13 | [103] | 2020 | 59 | 0.037 | RR | 0.99 | 0.98 | 1.00 | Low |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio; HR: hazard ratio.
The degree of urbanization was also related to several health impacts (Table 15). Specifically, living in a highly urbanized area was found to be associated with schizophrenia [107]. Urban exposure during childhood has been associated with an increased risk of Crohn’s disease and inflammatory bowel disease [108]. Live in a modern house was (compared to traditional house) was found to be a protective factor for clinical malaria [109]. In contrast, living in rural areas has been suggested as a risk factor from Parkinson’s disease [58]. Finally, having pets at home has been suggested to be a protective factor for non-communicable diseases in children and adults (Table 15). Specifically, being exposed to pets in the first year of life was found to reduce the risk of acute lymphoblastic leukemia [110]. For adults, being exposed to a pet was suggested to reduce Crohn’s disease and ulcerative colitis [108].
Table 15.
Urbanization, pets, and long-term health impacts.
| Environmental Risk Factor | Exposure Unit or Comparator | Exposure Temporality | Study Design | Population | Health Outcome | Studies Included | Reference | Year | I2 (%) | p-Value | Risk Estimate | Effect Size | LCI | UCI | Strength of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rural living | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Parkinson’s disease | 31 | [58] | 2016 | 78 | NR | OR | 1.32 | 1.18 | 1.48 | Low |
| Urban exposure during childhood | Rural exposure during childhood | Long-term | Case-controls | Adults, both sexes | Crohn’s disease | 12 | [108] | 2019 | 71 | 0 | OR | 1.45 | 1.14 | 1.85 | Moderate |
| Cohort and Case-Control | Adults, both sexes | Inflammatory bowel disease | 4 | [108] | 2019 | 71 | 0 | OR | 1.35 | 1.15 | 1.58 | Moderate | |||
| Urbanicity | Highest vs. lowest category | Long-term | Cohort | Adults, both sexes | Schizophrenia | 8 | [107] | 2018 | 99 | 0 | OR | 2.39 | 1.62 | 3.51 | Moderate |
| Modern housing | Exposed vs. not exposed | Long-term | Cohort | Adults, both sexes | Clinical malaria | 3 | [109] | 2015 | 67 | 0.05 | OR | 0.55 | 0.36 | 0.84 | Low |
| Pet in the first year of life | Exposed vs. not exposed | Long-term | Case-controls | Children | Acute lymphoblastic leukemia | 12 | [110] | 2018 | 39 | 0.08 | OR | 0.91 | 0.82 | 1.00 | Low |
| Pet | Exposed vs. not exposed | Long-term | Cohort and Case-Control | Adults, both sexes | Crohn’s disease | 14 | [108] | 2019 | 67 | 0 | OR | 0.77 | 0.59 | 0.94 | Moderate |
LCI: lower confidence intervals; UCI: upper confidence intervals NR: No reported; RR: relative risk; OR: odds ratio; HR: hazard ratio.
4. Discussion
This umbrella review found 193 associations among 68 environmental exposures and 83 diseases and death causes reported in 101 meta-analyses. The environmental factors found in this review were air pollution, environmental tobacco smoke, heavy metals, chemicals, ambient temperature, noise, radiation, and urban residential surroundings. Among these, we identified 64 environmental exposures defined as risk factors and 4 environmental protective factors. This review offers a comprehensive overview of the latest available evidence on environmental exposures and health outcomes. This, to our knowledge, is the first umbrella review on environmental risk factors and health. We included the most recent meta-analyses that summarize the largest number of individual studies and populations in each research area. We also selected only those meta-estimates that reported statistically significant associations between environmental exposures and health outcomes. In contrast with previous reviews in the area, which only focused on a single exposure or a single health outcome, we provided a general overview of multiples exposures and multiples health outcomes. Furthermore, we focused on observational studies with short and long-term environmental exposures.
Most of the meta-analyses found were focused on adults (80), 57 included cohorts or case-control studies, and 44 included case-crossover or time series analysis and form all meta-analyses included 79 were published in the last five years. In this review, the largest body of evidence was found in air pollution (91 associations among 14 air pollution definitions and 34 diseases and mortality diagnoses). That could be a reflection of two main factors: a) the relevance of air pollution as the most important environmental risk factor worldwide being one of the top 10 global health risk factors accounting for 4.8 million deaths globally in 2017 [3]; and combined with b) the available research funding, interest, and knowledge to integrate air pollution as an exposure factor in epidemiological studies compared to other pollutants. In terms of air pollution, in this review, particulate matter (PM2.5 and PM10) was the leading pollutant group that reported the largest number of associations (45). Environmental tobacco smoke was the second-largest exposure included in meta-analyses, with 24 associations among 6 exposure definitions. Chemicals (including pesticides) were the third larger group of environmental exposures found among the meta-analyses included, with 19 associations. Four environmental exposures were found to be protective for different health outcomes. These protective factors were residential greenness, modern housing, pet exposure, UV radiation, and recreational sun exposure. Despite the evidence on protective environmental factors, the largest body of evidence found in this review was on environmental risk factors (64 exposure definitions). Most of the meta-analyses included in this review reported observational studies from multiple geographical locations and multiple nations. Although some meta-analyses on specific geographical regions or countries were found during the screening step, we only selected those that included the largest number of observational studies. In all cases, this led to select those meta-analyses that do not restrict by geographical location.
In terms of the strength of evidence, we only found six associations that were assessed with “high” strength of evidence (defined as those associations that reported precision of the estimate (p < 0.001) and consistency of results (I2 < 50%)). The associations with “high” strength of evidence were NO2 and Type 2 diabetes; passive smoking and Type 2 diabetes; 1,3 Butadiene and acute lymphoblastic leukemia; aluminum and dementia; road traffic noise and hypertension; and residential greenness and low birth weight. In all the cases, but 1,3 Butadiene (case-control in children), the associations were reported in cohort studies from adult populations. Based on our definition of the strength of evidence, we consider that those six associations will be the only ones that we do not expect to change in direction (i.e., risk vs. protective factor) or magnitude of the association even if new studies on these topics are published.
This study encountered several limitations that should be considered. As with any systematic review, publication bias was the main limitation. To mitigate this, we focused our research on PubMed publications, where we searched for free text and medical subheadings (MESH) terms. A hand search complemented this effort. One important limitation of this review is the inclusion of a single literature database (Medline via PubMed). We acknowledge that this review will probably only capture the literature published primarily in health journals. Other data sources (i.e., Web of Science) could capture other sectoral journals (i.e., environment). Due to the limited resources and the large scope of this review, we decided to concentrate our resources on “PubMed” because it was considered the primary data source on health evidence. Another limitation we found was the quality of the included studies as most of the examined meta-analyses had a large heterogeneity. This review aimed to include studies focusing on the “environment” defined as the external elements and conditions which surround, influence, and affect the life and development of a human organism or population. While this review considers physical environments such as nature, the built environment, and pollution, it does not consider social environments. This review does not include occupational exposures; water, sanitation, and hygiene (WASH) exposures; behavioral risk factors (e.g., physical activity or diet); or exposure to microorganisms and no-natural disasters. This review selected only those meta-analysis that includes disease prevalence, incidence, and causes of death. The current epidemiological evidence provides a large body of studies (e.g., on biomarkers, metabolic and cardiovascular risk factors, symptoms, sings, hospitalizations, and emergency room visits, among others) that were beyond the scope of this review. We favored health evidence on defined diseases and causes of death that could be more easily translated into public health interventions and practices, although we acknowledge that preclinical and symptomatic health indicators could affect the largest portion of the population. In addition, there are several environmental exposures that were not included in this umbrella review based on the inclusion criteria. For example, large single observational studies were not included in the scope of this review. Furthermore, in the case that several observational studies on the similar exposure and outcome where published this study would be not able to include those type of evidence if those where not combined in a meta-analysis. For those reasons this umbrella review should be considered as a complementary tool to understand the universe of evidence available on environmental health.
Although this umbrella review found several publications and associations among environmental exposures and health outcomes, we also identified several evidence gaps. Most of the studies focus on identifying environmental risk factors, and only a few studies have been focusing on identifying environmental protective factors. Furthermore, few studies have focused on vulnerable and disadvantaged populations (children, elders, social disadvantaged, ethnic minorities, etc.). Furthermore, most studies do not provide a clear definition of the health outcomes using the international classification of diseases (ICD), nor a comparable exposure definition when the same pollutant is used. In terms of the meta-analysis, we exclude several studies from this review because, in the analyses, cross-sectional studies were mixed with other observational studies (i.e., cohorts). Additionally, several studies did not report heterogeneity values (i.e., I2) or do not provide dose-response functions essential for population risk assessment, health impact assessments and policy translation. We have summarized a list of recommendations for future research in environmental health studies based on these gaps, and we have listed those recommendations in Table 16.
Table 16.
Recommendations on observational studies and meta-analyses in environmental health.
| Recommendations |
|---|
| Observational studies:< - Increase studies on protective environmental risk factors |
| - Increase studies on vulnerable and disadvantaged populations |
| - Provide international classification of diseases (ICD) codes as part of the definitions for health outcomes |
| - Use comparable exposure definitions for environmental risk factors - Support longitudinal study designs |
| Meta-analyses - Avoid combining cross-sectional studies with cohort or case-control studies in the meta-estimates |
| - Provide heterogeneity values (i.e., I2) |
| - Provide dose-response functions to support populational risk assessment, quantitative health impact assessments, and policy translation |
5. Conclusions
Environmental exposures are an important health determinant. This umbrella review identified 68 environmental exposures that were associated to 83 health outcomes. This review provides an overview of an evolving area of research and should be used as a complementary tool to understand the connections between the environment and human health. This review also found the need of research prioritization using longitudinal approaches with harmonized exposure and outcome definitions, including vulnerable and susceptible populations in environmental health. The evidence presented by this review should help to design public health interventions and the implementation of a health in all policies approach aiming to improve populational health.
Author Contributions
W.A.A., C.H.H. and D.R.-R. conceived, designed, and coordinated assessment. D.R.-R. and E.M.-Z. analyzed the data and drafted the first manuscript. W.A.A., C.H.H., S.M.A., R.A., and M.A. participated in drafting the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The present work was funded under the 2020 Reimbursable Advisory Services Program on Health, Nutrition and Population, between the World Bank and the Ministry of Finance, Saudi Arabia.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
There are no competing financial interests.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Prüss-Ustün A., Neira M. Preventing Disease through Healthy Environments: A Global Assessment of the Environmental Burden of Disease. Volume 259 World Health Organization; Geneva, Switzerland: 2016. [Google Scholar]
- 2.Prüss-Ustün A. Environmental risks and non-communicable diseases. BMJ. 2019;365:17–19. doi: 10.1136/bmj.l265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stanaway J.D., Afshin A., Gakidou E., Lim S.S., Abate D., Abate K.H., Abbafati C., Abbasi N., Abbastabar H., Abd-Allah F., et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ioannidis J.P.A. Integration of evidence from multiple meta-analyses: A primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ. 2009;181:488–493. doi: 10.1503/cmaj.081086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu M.Y., Lo W.C., Chao C.-T., Wu M.S., Chiang C.K. Association between air pollutants and development of chronic kidney disease: A systematic review and meta-analysis. Sci. Total Environ. 2020;706 doi: 10.1016/j.scitotenv.2019.135522. [DOI] [PubMed] [Google Scholar]
- 6.Yang M., Cheng H., Shen C., Liu J., Zhang H., Cao J., Ding R. Effects of long-term exposure to air pollution on the incidence of type 2 diabetes mellitus: A meta-analysis of cohort studies. Environ. Sci. Pollut. Researc. 2020;27:798–811. doi: 10.1007/s11356-019-06824-1. [DOI] [PubMed] [Google Scholar]
- 7.Kim H.-B.B., Shim J.-Y.Y., Park B., Lee Y.-J.J. Long-Term Exposure to Air Pollutants and Cancer Mortality: A Meta-Analysis of Cohort Studies. Int. J. Environ. Res. Public Health. 2018;15:2608. doi: 10.3390/ijerph15112608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burnett R.T., Arden Pope C., Ezzati M., Olives C., Lim S.S., Mehta S., Shin H.H., Singh G., Hubbell B., Brauer M., et al. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ. Health Perspect. 2014;122:397–403. doi: 10.1289/ehp.1307049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsai T.L., Lin Y.T., Hwang B.F., Nakayama S.F., Tsai C.H., Sun X.L., Ma C., Jung C.R. Fine particulate matter is a potential determinant of Alzheimer’s disease: A systemic review and meta-analysis. Environ. Res. 2019;177:108638. doi: 10.1016/j.envres.2019.108638. [DOI] [PubMed] [Google Scholar]
- 10.Hoek G., Krishnan R.M., Beelen R., Peters A., Ostro B., Brunekreef B., Kaufman J.D. Long-term air pollution exposure and cardio- respiratory mortality: A review. Environ. Health. 2013;12:43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faustini A., Rapp R., Forastiere F. Nitrogen dioxide and mortality: Review and meta-analysis of long-term studies. Eur. Respir. J. 2014;44:744–753. doi: 10.1183/09031936.00114713. [DOI] [PubMed] [Google Scholar]
- 12.Braithwaite I., Zhang S., Kirkbride J.B., Osborn D.P.J., Hayes J.F. Air pollution (Particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: A systematic review and meta-analysis. Environ. Health Perspect. 2019;127:126002. doi: 10.1289/EHP4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yuan S., Wang J., Jiang Q., He Z., Huang Y., Li Z., Cai L., Cao S. Long-term exposure to PM2.5 and stroke: A systematic review and meta-analysis of cohort studies. Environ. Res. 2019;177:108587. doi: 10.1016/j.envres.2019.108587. [DOI] [PubMed] [Google Scholar]
- 14.Kasdagli M.I., Katsouyanni K., Dimakopoulou K., Samoli E. Air pollution and Parkinson’s disease: A systematic review and meta-analysis up to 2018. Int. J. Hyg. Environ. Health. 2019;222:402–409. doi: 10.1016/j.ijheh.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Cesaroni G., Stafoggia M., Galassi C., Hilding A., Hoffmann B., Houthuijs D., Ostenson C., Overvad K., Pedersen N.L. Long term exposure to ambient air pollution and incidence of acute coronary events: Prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ. 2014;7412:1–16. doi: 10.1136/bmj.f7412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Héroux M., Anderson H., Atkinson R., Brunekreef B., Cohen A., Forastiere F., Hurley F., Katsouyanni K., Krewski D., Krzyzanowski M., et al. Quantifying the health impacts of ambient air pollutants: Recommendations of a WHO/Europe project. Int. J. Public Health. 2015;60:619–627. doi: 10.1007/s00038-015-0690-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chun H.K., Leung C., Wen S.W., McDonald J., Shin H.H. Maternal exposure to air pollution and risk of autism in children: A systematic review and meta-analysis. Environ. Pollut. 2020;256 doi: 10.1016/j.envpol.2019.113307. [DOI] [PubMed] [Google Scholar]
- 18.Guo L.-Q., Chen Y., Mi B.-B., Dang S.-N., Zhao D.-D., Liu R., Wang H.-L., Yan H. Ambient air pollution and adverse birth outcomes: A systematic review and meta-analysis. J. Zhejiang Univ. Sci. B (Biomed. Biotechnol.) 2019;20:238–252. doi: 10.1631/jzus.B1800122. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.Khreis H., Ramani T., De Hoogh K., Mueller N. Traffic-related air pollution and the local burden of childhood asthma in Bradford, UK. Int. J. Transp. Sci. Technol. 2018;8:116–128. doi: 10.1016/j.ijtst.2018.07.003. [DOI] [Google Scholar]
- 20.Lam J., Sutton P., Kalkbrenner A., Windham G., Halladay A., Koustas E., Lawler C., Davidson L., Daniels N., Newschaffer C., et al. A systematic review and meta-analysis of multiple airborne pollutants and autism spectrum disorder. PLoS ONE. 2016;11:e0161851. doi: 10.1371/journal.pone.0161851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao R., Chen S., Wang W., Huang J., Wang K., Liu L., Wei S. The impact of short-term exposure to air pollutants on the onset of out-of-hospital cardiac arrest: A systematic review and meta-analysis. Int. J. Cardiol. 2017;226:110–117. doi: 10.1016/j.ijcard.2016.10.053. [DOI] [PubMed] [Google Scholar]
- 22.Song X., Liu Y., Hu Y., Zhao X., Tian J., Ding G., Wang S. Short-Term Exposure to Air Pollution and Cardiac Arrhythmia: A Meta-Analysis and Systematic Review. Int. J. Environ. Res. Public Health. 2016;13:642. doi: 10.3390/ijerph13070642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu C., Chen R., Sera F., Vicedo-Cabrera A.M., Guo Y., Tong S., Coelho M.S.Z.S., Saldiva P.H.N., Lavigne E., Matus P., et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N. Engl. J. Med. 2019;381:705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nhung N.T.T., Amini H., Schindler C., Kutlar Joss M., Dien T.M., Probst-Hensch N., Perez L., Künzli N. Short-term association between ambient air pollution and pneumonia in children: A systematic review and meta-analysis of time-series and case-crossover studies. Environ. Pollut. 2017;230:1000–1008. doi: 10.1016/j.envpol.2017.07.063. [DOI] [PubMed] [Google Scholar]
- 25.Stafoggia M., Zauli-Sajani S., Pey J., Samoli E., Alessandrini E., Basagaña X., Cernigliaro A., Chiusolo M., Demaria M., Díaz J., et al. Desert Dust Outbreaks in Southern Europe: Contribution to Daily PM 10 Concentrations and Short-Term Associations with Mortality and Hospital Admissions. Environ. Health Perspect. 2016;124:413–419. doi: 10.1289/ehp.1409164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bellou V., Belbasis L., Tzoulaki I., Evangelou E. Risk factors for type 2 diabetes mellitus: An exposure-wide umbrella review of meta-analyses. PLoS ONE. 2018 doi: 10.1371/journal.pone.0194127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen R., Yang J., Zhang C., Li B., Bergmann S., Zeng F., Wang H., Wang B. Global Associations of Air Pollution and Conjunctivitis Diseases: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health. 2019;16:3652. doi: 10.3390/ijerph16193652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fan S.J., Heinrich J., Bloom M.S., Zhao T.Y., Shi T.X., Feng W.R., Sun Y., Shen J.C., Yang Z.C., Yang B.Y., et al. Ambient air pollution and depression: A systematic review with meta-analysis up to 2019. Sci. Total Environ. 2020;701:134721. doi: 10.1016/j.scitotenv.2019.134721. [DOI] [PubMed] [Google Scholar]
- 29.Atkinson R.W., Butland B.K., Dimitroulopoulou C., Heal M.R., Stedman J.R., Carslaw N., Jarvis D., Heaviside C., Vardoulakis S., Walton H., et al. Long-term exposure to ambient ozone and mortality: A quantitative systematic review and meta-analysis of evidence from cohort studies. BMJ Open. 2016;6:e009493. doi: 10.1136/bmjopen-2015-009493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang H., Wang Q., He S., Wu K., Ren M., Dong H., Di J., Yu Z., Huang C. Ambient air pollution and gestational diabetes mellitus: A review of evidence from biological mechanisms to population epidemiology. Sci. Total Environ. 2020;719:137349. doi: 10.1016/j.scitotenv.2020.137349. [DOI] [PubMed] [Google Scholar]
- 31.Josyula S., Lin J., Xue X., Rothman N., Lan Q., Rohan T.E., Dean H., Iii H. Household air pollution and cancers other than lung: A meta-analysis. Env. Health. 2015 doi: 10.1186/s12940-015-0001-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li L., Yang A., He X., Liu J., Ma Y., Niu J., Luo B. Indoor air pollution from solid fuels and hypertension: A systematic review and meta-analysis. Environ. Pollut. 2020;259:613–621. doi: 10.1016/j.envpol.2020.113914. [DOI] [PubMed] [Google Scholar]
- 33.Amegah A.K., Quansah R., Jaakkola J.J.K. Household air pollution from solid fuel use and risk of adverse pregnancy outcomes: A systematic review and meta-analysis of the empirical evidence. PLoS ONE. 2014;9:e113920. doi: 10.1371/journal.pone.0113920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Okello S., Akello S.J., Dwomoh E., Byaruhanga E., Opio C.K., Zhang R., Corey K.E., Muyindike W.R., Ocama P., Christiani D.D. Biomass fuel as a risk factor for esophageal squamous cell carcinoma: A systematic review and meta-analysis. Environ. Health. 2019;18 doi: 10.1186/s12940-019-0496-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang Y., Mao J., Ye Z., Li J., Zhao H., Liu Y. Risk factors of chronic obstructive pulmonary disease among adults in Chinese mainland: A systematic review and meta-analysis. Respir. Med. 2017;131:158–165. doi: 10.1016/j.rmed.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 36.Khreis H., Kelly C., Tate J., Parslow R., Lucas K., Nieuwenhuijsen M. Exposure to traffic-related air pollution and risk of development of childhood asthma: A systematic review and meta-analysis. Environ. Int. 2017;100:1–31. doi: 10.1016/j.envint.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 37.Leonardi-Bee J., Smyth A., Britton J., Coleman T. Environmental tobacco smoke and fetal health: Systematic review and meta-analysis. Arch. Dis. Child. Fetal Neonatal Ed. 2008;93:F351–F361. doi: 10.1136/adc.2007.133553. [DOI] [PubMed] [Google Scholar]
- 38.Chen Y., Liu Q., Li W., Deng X., Yang B., Huang X. Association of prenatal and childhood environment smoking exposure with puberty timing: A systematic review and meta-analysis. Environ. Health Prev. Med. 2018;23 doi: 10.1186/s12199-018-0722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee P.N., Thornton A.J., Forey B.A., Hamling J.S. Environmental Tobacco Smoke Exposure and Risk of Stroke in Never Smokers: An Updated Review with Meta-Analysis. J. Stroke Cerebrovasc. Dis. 2017;26:204–216. doi: 10.1016/j.jstrokecerebrovasdis.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 40.Ni X., Xu N., Wang Q. Meta-Analysis and Systematic Review in Environmental Tobacco Smoke Risk of Female Lung Cancer by Research Type. Int. J. Environ. Res. Public Health. 2018;15:1348. doi: 10.3390/ijerph15071348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen C., Huang Y.-B., Liu X.-O., Gao Y., Dai H.-J., Song F.-J., Li W.-Q., Wang J., Yan Y., Wang P.-S., et al. Active and passive smoking with breast cancer risk for Chinese females: A systematic review and meta-analysis. Chin. J. Cancer. 2014;33:306–316. doi: 10.5732/cjc.013.10248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lv X., Sun J., Bi Y., Xu M., Lu J., Zhao L., Xu Y. Risk of all-cause mortality and cardiovascular disease associated with secondhand smoke exposure: A systematic review and meta-analysis. Int. J. Cardiol. 2015;199:106–115. doi: 10.1016/j.ijcard.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 43.Su B., Qin W., Xue F., Wei X., Guan Q., Jiang W., Wang S., Xu M., Yu S. The relation of passive smoking with cervical cancer A systematic review and meta-analysis. Medicine. 2018 doi: 10.1097/MD.0000000000013061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim C.H., Lee A.Y.C., Hung R.J., McNallan S.R., Cote M.L., Lim W.-Y., Chang S.-C., Kim J.H., Ugolini D., Chen Y., et al. Exposure to secondhand tobacco smoke and lung cancer by histological type: A pooled analysis of the International Lung Cancer Consortium (ILCCO) Int. J. Cancer. 2014;135:1918–1930. doi: 10.1038/jid.2014.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bellou V., Belbasis L., Tzoulaki I., Middleton L.T., Ioannidis J.P.A., Evangelou E. Systematic evaluation of the associations between environmental risk factors and dementia: An umbrella review of systematic reviews and meta-analyses. Alzheimer’s Dement. 2017;13:406–418. doi: 10.1016/j.jalz.2016.07.152. [DOI] [PubMed] [Google Scholar]
- 46.Meng X., Sun Y., Duan W., Jia C. Meta-analysis of the association of maternal smoking and passive smoking during pregnancy with neural tube defects. Int. J. Gynecol. Obstet. 2018;140:18–25. doi: 10.1002/ijgo.12334. [DOI] [PubMed] [Google Scholar]
- 47.He Z., Wu H., Zhang S., Lin Y., Li R., Xie L., Li Z., Sun W., Huang X., Zhang C.J.P., et al. The association between secondhand smoke and childhood asthma: A systematic review and meta-analysis. Pediatr. Pulmonol. 2020;55:2518–2531. doi: 10.1002/ppul.24961. [DOI] [PubMed] [Google Scholar]
- 48.Zhang Y., Xu M., Zhang J., Zeng L., Wang Y., Zheng Q.Y. Risk factors for chronic and recurrent otitis media-A meta-analysis. PLoS ONE. 2014;9 doi: 10.1371/journal.pone.0086397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murray R., Asher L., Leonardi-Bee J., Hunter A. The Effects of Tobacco Smoking, and Prenatal Tobacco Smoke Exposure, on Risk of Schizophrenia: A Systematic Review and Meta-Analysis. Nicotine Tob. Res. 2020;22:3–10. doi: 10.1093/ntr/nty160. [DOI] [PubMed] [Google Scholar]
- 50.Taylor A.E., Carslake D., De Mola C.L., Rydell M., Nilsen T.I.L.L., Bjørngaard J.H., Horta B.L., Pearson R., Rai D., Galanti M.R., et al. Maternal Smoking in Pregnancy and Offspring Depression: A cross cohort and negative control study. Sci. Rep. 2017;7:1–8. doi: 10.1038/s41598-017-11836-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Huang L., Wang Y., Zhang L., Zheng Z., Zhu T., Qu Y., Mu D. Maternal Smoking and Attention- Deficit / Hyperactivity Disorder in Offspring: A Meta-analysis. Pediatrics. 2018;141:e20172465. doi: 10.1542/peds.2017-2465. [DOI] [PubMed] [Google Scholar]
- 52.Riedel C., Schö K., Yang S., Koshy G., Chen Y.-C., Gopinath B., Ziebarth S., Diger Von Kries R. Parental smoking and childhood obesity: Higher effect estimates for maternal smoking in pregnancy compared with paternal smoking-a meta-analysis. Int. J. Epidemiol. 2014:1593–1606. doi: 10.1093/ije/dyu150. [DOI] [PubMed] [Google Scholar]
- 53.Rios P., Bailey H.D., Poulalhon C., Valteau-Couanet D., Schleiermacher G., Bergeron C., Petit A., Defachelles A.S., Marion G., Sirvent N., et al. Parental smoking, maternal alcohol consumption during pregnancy and the risk of neuroblastoma in children. A pooled analysis of the ESCALE and ESTELLE French studies. Int. J. Cancer. 2019;145:2907–2916. doi: 10.1002/ijc.32161. [DOI] [PubMed] [Google Scholar]
- 54.Chunxia D., Meifang W., Jianhua Z., Ruijuan Z., Xiue L., Zhuanzhen Z., Linhua Y., Gutti R.K. Tobacco smoke exposure and the risk of childhood acute lymphoblastic leukemia and acute myeloid leukemia: A meta-Analysis. Medicine. 2019;98 doi: 10.1097/MD.0000000000016454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Milne E., Greenop K.R., Scott R.J., Bailey H.D., Attia J., Dalla-Pozza L., De Klerk N.H., Armstrong B.K. Parental prenatal smoking and risk of childhood acute lymphoblastic leukemia. Am. J. Epidemiol. 2012;175:43–53. doi: 10.1093/aje/kwr275. [DOI] [PubMed] [Google Scholar]
- 56.Filippini T., Hatch E.E., Rothman K.J., Heck J.E., Park A.S., Crippa A., Orsini N., Vinceti M. Association between Outdoor Air Pollution and Childhood Leukemia: A Systematic Review and Dose–Response Meta-Analysis. Environ. Health Perspect. 2019;127:046002. doi: 10.1289/EHP4381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Palin O., Herd C., Morrison K.E., Jagielski A.C., Wheatley K., Thomas G.N., Clarke C.E. Systematic review and meta-analysis of hydrocarbon exposure and the risk of Parkinson’s disease. Park. Relat. Disord. 2015;21:243–248. doi: 10.1016/j.parkreldis.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 58.Bellou V., Belbasis L., Tzoulaki I., Evangelou E., Ioannidis J.P.A. Environmental risk factors and Parkinson’s disease: An umbrella review of meta-analyses. Park. Relat. Disord. 2016;23:1–9. doi: 10.1016/j.parkreldis.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 59.Belbasis L., Bellou V., Evangelou E., Ioannidis J.P.A.A., Tzoulaki I. Environmental risk factors and multiple sclerosis: An umbrella review of systematic reviews and meta-analyses. Lancet Neurol. 2015;14:263–273. doi: 10.1016/S1474-4422(14)70267-4. [DOI] [PubMed] [Google Scholar]
- 60.Belbasis L., Dosis V., Evangelou E. Elucidating the environmental risk factors for rheumatic diseases: An umbrella review of meta-analyses. Int. J. Rheum. Dis. 2018;21:1514–1524. doi: 10.1111/1756-185X.13356. [DOI] [PubMed] [Google Scholar]
- 61.Freeman M.D., Kohles S.S. Plasma levels of polychlorinated biphenyls, non-hodgkin lymphoma, and causation. J. Environ. Public Health. 2012;2012 doi: 10.1155/2012/258981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cano-Sancho G., Ploteau S., Matta K., Adoamnei E., Louis G.B., Mendiola J., Darai E., Squifflet J., Le Bizec B., Antignac J.P. Human epidemiological evidence about the associations between exposure to organochlorine chemicals and endometriosis: Systematic review and meta-analysis. Environ. Int. 2019;123:209–223. doi: 10.1016/j.envint.2018.11.065. [DOI] [PubMed] [Google Scholar]
- 63.Gascon M., Sunyer J., Casas M., Martínez D., Ballester F., Basterrechea M., Bonde J.P., Chatzi L., Chevrier C., Eggesbø M., et al. Prenatal exposure to DDE and PCB 153 and respiratory health in early childhood: A meta-analysis. Epidemiology. 2014;25:544–553. doi: 10.1097/EDE.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 64.Rancière F., Lyons J.G., Loh V.H., Botton J., Galloway T., Wang T., Shaw J.E., Magliano D.J., Loh V.H.Y., Botton J., et al. Bisphenol A and the risk of cardiometabolic disorders: A systematic review with meta-analysis of the epidemiological evidence. Environ. Health. 2015;14:46. doi: 10.1186/s12940-015-0036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cai W., Yang J., Liu Y., Bi Y., Wang H. Association between Phthalate Metabolites and Risk of Endometriosis: A Meta-Analysis. Int. J. Environ. Res. Public Health. 2019;16:3678. doi: 10.3390/ijerph16193678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yan D., Zhang Y., Liu L., Yan H. Pesticide exposure and risk of Alzheimer’s disease: A systematic review and meta-analysis. Sci. Rep. 2016;6:1–9. doi: 10.1038/srep32222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Belbasis L., Bellou V., Evangelou E. Environmental Risk Factors and Amyotrophic Lateral Sclerosis: An Umbrella Review and Critical Assessment of Current Evidence from Systematic Reviews and Meta-Analyses of Observational Studies. Neuroepidemiology. 2016;46:96–105. doi: 10.1159/000443146. [DOI] [PubMed] [Google Scholar]
- 68.Van Maele-Fabry G., Gamet-Payrastre L., Lison D. Residential exposure to pesticides as risk factor for childhood and young adult brain tumors: A systematic review and meta-analysis. Environ. Int. 2017;106:69–90. doi: 10.1016/j.envint.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 69.Jin J., Yu M., Hu C., Ye L., Xie L. Pesticide Exposure as a Risk Factor for Myelodysplastic Syndromes: A Meta-Analysis Based on 1,942 Cases and 5,359 Controls. PLoS ONE. 2014;9 doi: 10.1371/journal.pone.0110850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yan D., Zhang Y., Liu L., Shi N., Yan H. Pesticide exposure and risk of Parkinson’s disease: Dose-response meta-analysis of observational studies. Regul. Toxicol. Pharmacol. 2018;96:57–63. doi: 10.1016/j.yrtph.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 71.Tangamornsuksan W., Lohitnavy O., Sruamsiri R., Chaiyakunapruk N., Norman Scholfield C., Reisfeld B., Lohitnavy M. Paraquat exposure and Parkinson’s disease: A systematic review and meta-analysis. Arch. Environ. Occup. Health. 2019;74:225–238. doi: 10.1080/19338244.2018.1492894. [DOI] [PubMed] [Google Scholar]
- 72.Hu L., Luo D., Zhou T., Tao Y., Feng J., Mei S. The association between non-Hodgkin lymphoma and organophosphate pesticides exposure: A meta-analysis. Environ. Pollut. 2017;231:319–328. doi: 10.1016/j.envpol.2017.08.028. [DOI] [PubMed] [Google Scholar]
- 73.Luo D., Zhou T., Tao Y., Feng Y., Shen X., Mei S. Exposure to organochlorine pesticides and non-Hodgkin lymphoma: A meta-analysis of observational studies. Sci. Rep. 2016;6 doi: 10.1038/srep25768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Van Maele-Fabry G., Gamet-Payrastre L., Lison D. Household exposure to pesticides and risk of leukemia in children and adolescents: Updated systematic review and meta-analysis. Int. J. Hyg. Environ. Health. 2019;222:49–67. doi: 10.1016/j.ijheh.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 75.Xu R., Barg F.K., Emmett E.A., Wiebe D.J., Hwang W.-T. Association between mesothelioma and non-occupational asbestos exposure: Systematic review and meta-analysis. Environ. Health. 2018;17 doi: 10.1186/s12940-018-0431-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nawrot T.S., Martens D.S., Hara A., Plusquin M., Vangronsveld J., Roels H.A., Staessen J.A. Association of total cancer and lung cancer with environmental exposure to cadmium: The meta-analytical evidence. Cancer Causes Control. 2015;26:1281–1288. doi: 10.1007/s10552-015-0621-5. [DOI] [PubMed] [Google Scholar]
- 77.Ma J., Yan L., Guo T., Yang S., Guo C., Liu Y., Xie Q., Wang J. Association of typical toxic heavy metals with schizophrenia. Int. J. Environ. Res. Public Health. 2019;16:4200. doi: 10.3390/ijerph16214200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang W., Xie Z., Lin Y., Zhang D. Association of inorganic arsenic exposure with type 2 diabetes mellitus: A meta-analysis. J. Epidemiol. Community Health. 2014;68:176–184. doi: 10.1136/jech-2013-203114. [DOI] [PubMed] [Google Scholar]
- 79.Meng E., Mao Y., Yao Q., Han X., Li X., Zhang K., Jin W. Population-based study of environmental/occupational lead exposure and amyotrophic lateral sclerosis: A systematic review and meta-analysis. Neurol. Sci. 2020;41:35–41. doi: 10.1007/s10072-019-04067-z. [DOI] [PubMed] [Google Scholar]
- 80.Lanphear B.P., Hornung R., Khoury J., Yolton K., Baghurst P., Bellinger D.C., Canfield R.L., Dietrich K.N., Bornschein R., Greene T., et al. Low-Level Environmental Lead Exposure and Children’s Intellectual Function: An International Pooled Analysis. Environ. Health Perspect. 2005;113:894–899. doi: 10.1289/ehp.7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kim Y., Kim H., Gasparrini A., Armstrong B., Honda Y., Chung Y., Ng C.F.S., Tobias A., Íñiguez C., Lavigne E., et al. Suicide and Ambient Temperature: A Multi-Country Multi-City Study. Environ. Health Perspect. 2019;127:117007. doi: 10.1289/EHP4898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yang J., Yin P., Zhou M., Ou C.Q., Li M., Liu Y., Gao J., Chen B., Liu J., Bai L., et al. The effect of ambient temperature on diabetes mortality in China: A multi-city time series study. Sci. Total Environ. 2016;543:75–82. doi: 10.1016/j.scitotenv.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 83.Vickers M.L., Pelecanos A., Tran M., Eriksson L., Assoum M., Harris P.N., Jaiprakash A., Parkinson B., Dulhunty J., Crawford R.W. Association between higher ambient temperature and orthopaedic infection rates: A systematic review and meta-analysis. ANZ J. Surg. 2019;89:1028–1034. doi: 10.1111/ans.15089. [DOI] [PubMed] [Google Scholar]
- 84.Chersich M.F., Pham M.D., Areal A., Haghighi M.M., Manyuchi A., Swift C.P., Wernecke B., Robinson M., Hetem R., Boeckmann M., et al. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: Systematic review and meta-analysis. BMJ. 2020;371:1–13. doi: 10.1136/bmj.m3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lee W., Bell M.L., Gasparrini A., Armstrong B.G., Sera F., Hwang S., Lavigne E., Zanobetti A., Coelho M.d.S.Z.S., Saldiva P.H.N., et al. Mortality burden of diurnal temperature range and its temporal changes: A multi-country study. Environ. Int. 2018;110:123–130. doi: 10.1016/j.envint.2017.10.018. [DOI] [PubMed] [Google Scholar]
- 86.Cheng J., Xu Z., Bambrick H., Prescott V., Wang N., Zhang Y., Su H., Tong S., Hu W. Cardiorespiratory effects of heatwaves: A systematic review and meta-analysis of global epidemiological evidence. Environ. Res. 2019;177:108610. doi: 10.1016/j.envres.2019.108610. [DOI] [PubMed] [Google Scholar]
- 87.Bunker A., Wildenhain J., Vandenbergh A., Henschke N., Rocklöv J., Hajat S., Sauerborn R. Effects of Air Temperature on Climate-Sensitive Mortality and Morbidity Outcomes in the Elderly; a Systematic Review and Meta-analysis of Epidemiological Evidence. EBioMedicine. 2016;6:258–268. doi: 10.1016/j.ebiom.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chen J., Zhou M., Yang J., Yin P., Wang B., Ou C.Q., Liu Q. The modifying effects of heat and cold wave characteristics on cardiovascular mortality in 31 major Chinese cities. Environ. Res. Lett. 2020;15 doi: 10.1088/1748-9326/abaea0. [DOI] [Google Scholar]
- 89.Cong X., Xu X., Zhang Y., Wang Q., Xu L., Huo X. Temperature drop and the risk of asthma: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. 2017;24:22535–22546. doi: 10.1007/s11356-017-9914-4. [DOI] [PubMed] [Google Scholar]
- 90.Ho C.-L., Wu W.-F., Liou Y.M. Dose-Response Relationship of Outdoor Exposure and Myopia Indicators: A Systematic Review and Meta-Analysis of Various Research Methods. Int. J. Environ. Res. Public Health. 2019;16:2595. doi: 10.3390/ijerph16142595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yang W.S., Deng Q., Fan W.Y., Wang W.Y., Wang X. Light exposure at night, sleep duration, melatonin, and breast cancer: A dose-response analysis of observational studies. Eur. J. Cancer Prev. 2014;23:269–276. doi: 10.1097/CEJ.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 92.Monnereau A., Glaser S.L., Schupp C.W., Smedby K.E., De Sanjosé S., Kane E., Melbye M., Forétova L., Maynadié M., Staines A., et al. Exposure to UV radiation and risk of Hodgkin lymphoma: A pooled analysis. Blood. 2013;122:3492–3499. doi: 10.1182/blood-2013-04-497586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kricker A., Armstrong B.K., Hughes A.M., Goumas C., Smedby K.E., Zheng T., Spinelli J.J., De Sanjose S., Hartge P., Melbye M., et al. Personal sun exposure and risk of non Hodgkin lymphoma: A pooled analysis from the Interlymph Consortium. Int. J. Cancer. 2008;122:144–154. doi: 10.1002/ijc.23003. [DOI] [PubMed] [Google Scholar]
- 94.Zare Sakhvidi M.J., Zare Sakhvidi F., Mehrparvar A.H., Foraster M., Dadvand P. Association between noise exposure and diabetes: A systematic review and meta-analysis. Environ. Res. 2018;166:647–657. doi: 10.1016/j.envres.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 95.Fu W., Wang C., Zou L., Liu Q., Gan Y., Yan S., Song F., Wang Z., Lu Z., Cao S. Association between exposure to noise and risk of hypertension: A meta-analysis of observational epidemiological studies. J. Hypertens. 2017;35:2358–2366. doi: 10.1097/HJH.0000000000001504. [DOI] [PubMed] [Google Scholar]
- 96.Dzhambov A.M., Dimitrova D.D. Residential road traffic noise as a risk factor for hypertension in adults: Systematic review and meta-analysis of analytic studies published in the period 2011–2017. Environ. Pollut. 2018;240:306–318. doi: 10.1016/j.envpol.2018.04.122. [DOI] [PubMed] [Google Scholar]
- 97.Van Kempen E., Casas M., Pershagen G., Foraster M. WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Cardiovascular and Metabolic Effects: A Summary. Int. J. Environ. Res. Public Health. 2018;15:379. doi: 10.3390/ijerph15020379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lee W., Kim Y., Honda Y., Kim H. Association between diurnal temperature range and mortality modified by temperature in Japan, 1972–2015: Investigation of spatial and temporal patterns for 12 cause-specific deaths. Environ. Int. 2018;119:379–387. doi: 10.1016/j.envint.2018.06.020. [DOI] [PubMed] [Google Scholar]
- 99.Angelillo I.F., Villari P. Residential exposure to electromagnetic fields and childhood leukaemia: A meta-analysis. Bull. World Health Organ. 1999;77:906–915. [PMC free article] [PubMed] [Google Scholar]
- 100.Malinovsky G., Yarmoshenko I., Vasilyev A. Meta-analysis of case-control studies on the relationship between lung cancer and indoor radon exposure. Radiat. Environ. Biophys. 2019;58:39–47. doi: 10.1007/s00411-018-0770-5. [DOI] [PubMed] [Google Scholar]
- 101.Tong J., Qin L., Cao Y., Li J., Zhang J., Nie J., An Y. Environmental radon exposure and childhood leukemia. J. Toxicol. Environ. Health Part B Crit. Rev. 2012;15:332–347. doi: 10.1080/10937404.2012.689555. [DOI] [PubMed] [Google Scholar]
- 102.Rojas-Rueda D., Nieuwenhuijsen M.J., Gascon M., Perez-Leon D., Mudu P., Rojas-Rueda D., Nieuwenhuijsen M.J., Gascon M., Perez-Leon D., Mudu P. Green spaces and mortality: A systematic review and meta-analysis of cohort studies. Lancet Planet. Health. 2019;3:e469–e477. doi: 10.1016/S2542-5196(19)30215-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhan Y., Liu J., Lu Z., Yue H., Zhang J., Jiang Y. Influence of residential greenness on adverse pregnancy outcomes: A systematic review and dose-response meta-analysis. Sci. Total Environ. 2020;718:37420. doi: 10.1016/j.scitotenv.2020.137420. [DOI] [PubMed] [Google Scholar]
- 104.Zhao Z., Lin F., Wang B., Cao Y., Hou X., Wang Y. Residential Proximity to Major Roadways and Risk of Type 2 Diabetes Mellitus: A Meta-Analysis. Int. J. Environ. Res. Public Health. 2017;14:3. doi: 10.3390/ijerph14010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Boothe V.L., Boehmer T.K., Wendel A.M., Yip F.Y. Residential traffic exposure and childhood leukemia: A systematic review and meta-analysis. Am. J. Prev. Med. 2014;46:413–422. doi: 10.1016/j.amepre.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lin C.K., Hsu Y.T., Brown K.D., Pokharel B., Wei Y., Chen S.T. Residential exposure to petrochemical industrial complexes and the risk of leukemia: A systematic review and exposure-response meta-analysis. Environ. Pollut. 2020;258 doi: 10.1016/j.envpol.2019.113476. [DOI] [PubMed] [Google Scholar]
- 107.Belbasis L., Köhler C.A., Stefanis N., Stubbs B., van Os J., Vieta E., Seeman M.V., Arango C., Carvalho A.F., Evangelou E. Risk factors and peripheral biomarkers for schizophrenia spectrum disorders: An umbrella review of meta-analyses. Acta Psychiatr. Scand. 2018;137:88–97. doi: 10.1111/acps.12847. [DOI] [PubMed] [Google Scholar]
- 108.Piovani D., Danese S., Peyrin-biroulet L., Nikolopoulos G.K., Lytras T., Bonovas S. Environmental Risk Factors for Inflammatory Bowel Diseases: An Umbrella Review of Meta-analyses. Gastroenterology. 2019;157:647–659. doi: 10.1053/j.gastro.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 109.Tusting L.S., Ippolito M.M., Willey B.A., Kleinschmidt I., Dorsey G., Gosling R.D., Lindsay S.W. The evidence for improving housing to reduce malaria: A systematic review and meta-analysis. Malar. J. 2015;14 doi: 10.1186/s12936-015-0724-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Orsi L., Magnani C., Petridou E.T., Dockerty J.D., Metayer C., Milne E., Bailey H.D., Dessypris N., Kang A.Y., Wesseling C., et al. Living on a farm, contact with farm animals and pets, and childhood acute lymphoblastic leukemia: Pooled and meta-analyses from the Childhood Leukemia International Consortium. Cancer Med. 2018;7:2665–2681. doi: 10.1002/cam4.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.