Abstract
Background
The impact of the COVID-19 pandemic on mental health in people with pre-existing mental health disorders is unclear. In three psychiatry case-control cohorts, we compared the perceived mental health impact and coping and changes in depressive symptoms, anxiety, worry, and loneliness before and during the COVID-19 pandemic between people with and without lifetime depressive, anxiety, or obsessive-compulsive disorders.
Methods
Between April 1 and May 13, 2020, online questionnaires were distributed among the Netherlands Study of Depression and Anxiety, Netherlands Study of Depression in Older Persons, and Netherlands Obsessive Compulsive Disorder Association cohorts, including people with (n=1181) and without (n=336) depressive, anxiety, or obsessive-compulsive disorders. The questionnaire contained questions on perceived mental health impact, fear of COVID-19, coping, and four validated scales assessing depressive symptoms, anxiety, worry, and loneliness used in previous waves during 2006–16. Number and chronicity of disorders were based on diagnoses in previous waves. Linear regression and mixed models were done.
Findings
The number and chronicity of disorders showed a positive graded dose–response relation, with greater perceived impact on mental health, fear, and poorer coping. Although people with depressive, anxiety, or obsessive-compulsive disorders scored higher on all four symptom scales than did individuals without these mental health disorders, both before and during the COVID-19 pandemic, they did not report a greater increase in symptoms during the pandemic. In fact, people without depressive, anxiety, or obsessive-compulsive disorders showed a greater increase in symptoms during the COVID-19 pandemic, whereas individuals with the greatest burden on their mental health tended to show a slight symptom decrease.
Interpretation
People with depressive, anxiety, or obsessive-compulsive disorders are experiencing a detrimental impact on their mental health from the COVID-19 pandemic, which requires close monitoring in clinical practice. Yet, the COVID-19 pandemic does not seem to have further increased symptom severity compared with their prepandemic levels.
Funding
Dutch Research Council.
Introduction
Since the first confirmed case of COVID-19 was reported in the Netherlands on Feb 27, 2020, this disease has had a great impact on every aspect of Dutch society. Similar to many other countries worldwide, nationwide measures such as quarantine, lockdown, and physical distancing were launched in the middle of March, 2020, in response to the rising number of cases and deaths attributed to COVID-19. Although these measures might have mitigated the spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that causes COVID-19, they might also have negatively affected the economy, employment, and public health.1, 2 With worries about future uncertainty, concern has been growing about the mental health sequelae of the COVID-19 crisis.3 Most evidence on the impact of the COVID-19 pandemic on mental health is based on convenience samples, without comparable prepandemic information, thus compromising the validity of this evidence.4 So far, based on probability samples, a rise in psychological distress in April, 2020, compared with in 2018–19, has been reported among adults in the USA5 and the UK.6
Outcomes of the COVID-19 pandemic on mental health could differ between population groups. In particular, the emotional responses brought on by the pandemic and its management might be more substantial among vulnerable groups, such as people with pre-existing psychiatric conditions.7, 8 Financial instability and small social networks are common among people with mental illness; as a result of economic recession and restricted social connectivity, the COVID-19 pandemic could present an unprecedented stressor to these individuals.9 Measures such as nationwide travel restrictions and quarantine, and changes in the way health-care services are provided, could interrupt access to and provision of psychiatric care.10, 11 As a result, the risk of relapses or worsening of existing mental health conditions could rise during the COVID-19 pandemic. There is an urgent need to empirically understand to what extent the COVID-19 pandemic and related societal changes have so far affected the mental health of people with pre-existing mental health disorders.
Research in context.
Evidence before this study
We searched PubMed and Google Scholar with the terms (“mental*” OR “psychiatr*”) AND (“COVID*” OR “coronavirus”) for articles published in English between Jan 1 and Sept 30, 2020. All studies identified by our search and focusing on the mental health impact of the COVID-19 pandemic on people with mental health disorders either used a cross-sectional survey, relied on self-reported mental health, or had no prepandemic baseline data at the individual level.
Added value of this study
To the best of our knowledge, this is the first dataset based on existing psychiatry case-control cohort studies with information on the mental health of the same individuals for more than 10 years before and during the COVID-19 pandemic. The burden of depressive, anxiety, or obsessive-compulsive disorders, in terms of both number and chronicity of disorders, had a graded dose–response relation with perceived mental health impact, fear of COVID-19, and poorer coping during the COVID-19 pandemic. Although our study did not show any signs of a further increase in symptom severity in people with depressive, anxiety, or obsessive-compulsive disorders during the COVID-19 pandemic, the mental health of these individuals was and remained systematically worse than that of people without these disorders.
Implications of all the available evidence
This finding emphasises the importance of providers maintaining access to mental health-care services for people with pre-existing disorders. Since development of the COVID-19 pandemic is constantly changing, it is necessary to continue monitoring its long-term effect on mental health in people both with and without depressive, anxiety, or obsessive-compulsive disorders, along with the effect of strategies that aim to reduce the spread of COVID-19.
Evidence relating to the mental health impact of the COVID-19 pandemic among people with mental health disorders has been restricted to cross-sectional studies. In a small-scale Chinese study that used convenience sampling to recruit participants,12 more symptoms of depression and anxiety, stress, and insomnia were reported among people with psychiatric disorders than among individuals without a mental health disorder. In an Australian non-probability sample,13 psychological distress was higher among people with self-reported mood disorders than among those without. However, symptoms before the COVID-19 pandemic were not measured in these studies, leaving it unclear whether the pandemic truly led to changes in symptom levels within populations with psychiatric disorders.
We did a study using longitudinal data from three existing Dutch psychiatry case-control cohorts, including people with and without mental health disorders (depressive, anxiety, or obsessive-compulsive disorders). Data collection for the three cohorts started in the early 2000s, and the most recent information from the same individuals was collected 2–8 weeks after the national lockdown in the Netherlands. We aimed to compare between people with a different number and chronicity of mental health disorders the perceived impact of the COVID-19 pandemic on mental health and the extent to which individuals were able to positively cope with the situation, and changes in symptoms of depression, anxiety, worry, and loneliness from before to during the COVID-19 pandemic.
Methods
Participants
We recruited participants from three cohort studies: the Netherlands Study of Depression and Anxiety (NESDA),14 Netherlands Study of Depression in Older Persons (NESDO),15 and Netherlands Obsessive Compulsive Disorder Association Study (NOCDA).16 The largely similar procedures for data collection in these cohort studies allowed pooling of data for our study.
NESDA is an ongoing longitudinal study examining the development and course of depression and anxiety disorders among people aged 18–65 years with a depression or anxiety disorder (n=2329), biological siblings (n=367), and individuals without a mental health disorder (n=652).14 Between 2004 and 2007, participants were recruited from the community, primary care, and specialised mental health care in the Netherlands, and they were followed up after 2, 4, 6, and 9 years.
NESDO is a longitudinal study of depression in older people (aged 60–93 years).15 From 2007 until 2010, 378 individuals with a depressive disorder were recruited through specialised mental health-care services. People without lifetime diagnoses of depression, anxiety, dementia, or another clinically overt psychiatric disorder such as psychosis, severe addiction, or bipolar disorder (n=132) were recruited from primary care. Face-to-face assessments were done after 2 and 6 years.
NOCDA is a longitudinal study in 419 people aged 18–65 years with a lifetime diagnosis of obsessive-compulsive disorder who were recruited from mental health-care institutions.16 Baseline assessments were done between 2004 and 2009, and follow-up examinations took place after 2, 4, and 6 years.
Our study was approved by the Institutional Review Board of Vrije Universiteit Medical Center, Amsterdam, and adhered to the Declaration of Helsinki. All participants provided informed consent online.
Procedures
We obtained information about gender, age, and education (basic [elementary school], intermediate [lower vocational to general secondary education], and high [college or university]) from the regular baseline waves of the three cohorts. Age was adjusted for time elapsed since the baseline assessment. To align the three cohorts with respect to data availability, we used follow-up data obtained at 2, 4, 6, and 9 years in NESDA, baseline and 2-year and 6-year follow-up data in NESDO, and follow-up data obtained at 2, 4, and 6 years in NOCDA. Data for these previous waves were obtained between 2006 and 2016 (table 1 ).
Table 1.
Data availability in previous regular waves by cohort
| Years | Symptom assessment | Clinical diagnosis | |
|---|---|---|---|
| NESDA | |||
| 2-year follow-up | 2006–09 | QIDS, BAI, PSWQ, and DJGLS | CIDI |
| 4-year follow-up | 2008–11 | QIDS, BAI, and PSWQ | CIDI |
| 6-year follow-up | 2010–13 | QIDS, BAI, and PSWQ | CIDI |
| 9-year follow-up | 2014–16 | QIDS, BAI, and PSWQ | CIDI |
| NESDO | |||
| Baseline | 2006–10 | QIDS, BAI, and DJGLS | CIDI |
| 2-year follow-up | 2008–12 | QIDS and BAI | CIDI |
| 6-year follow-up | 2012–16 | QIDS and BAI | CIDI |
| NOCDA | |||
| 2-year follow-up | 2006–11 | BAI and DJGLS | SCID |
| 4-year follow-up | 2008–13 | BAI and DJGLS | SCID |
| 6-year follow-up | 2012–16 | BAI and DJGLS | SCID |
NESDA=Netherlands Study of Depression and Anxiety. NESDO=Netherlands Study of Depression in Older Persons. NOCDA=Netherlands Obsessive Compulsive Disorder Association Study. QIDS=16-item Quick Inventory of Depressive Symptoms. BAI=21-item Beck Anxiety Inventory. PSWQ=11-item Penn State Worry Questionnaire. DJGLS=six-item De Jong Gierveld Loneliness Scale. CIDI=Composite Interview Diagnostic Instrument. SCID=Structured Clinical Interview for DSM-IV axis I disorders.
In NESDA and NESDO, the DSM-IV-based Composite Interview Diagnostic Instrument was used to diagnose mental health disorders;17 in NOCDA, the Structured Clinical Interview for DSM-IV axis I disorders was used for diagnosis.18 Lifetime and current (within the past 6 months) presence of six disorders was assessed at all previous waves in all three cohorts: major depressive disorder, dysthymia, general anxiety disorder, panic disorder, social phobia, and agoraphobia. The diagnosis of obsessive-compulsive disorder was added in NOCDA only. We used longitudinal data to classify the overall burden of mental health disorders in two indicators: severity and chronicity. For severity across disorders, we calculated the total number of different lifetime mental health disorders an individual has been diagnosed with, because this number provides an integrative measure, and it has been consistently shown that comorbidity of mental health disorders (ie, having more disorders) is related to higher specific symptom severity and overall disability.19, 20 For chronicity, we divided the number of waves with a current diagnosis (regardless of type of disorder) by the number of waves an individual participated in and categorised into zero, less than or equal to half, and more than half of all waves with a current disorder.
Four validated symptom severity scales were used in previous waves. For depressive symptoms we used the 16-item Quick Inventory of Depressive Symptoms (QIDS);21 for anxiety symptoms the 21-item Beck Anxiety Inventory (BAI);22 for worry the 11-item Penn State Worry Questionnaire (PSWQ);23 and for loneliness the six-item De Jong Gierveld Loneliness Scale (DJGLS).24
The online questionnaire was built in Survalyzer, 3000 edition. We obtained information on living situation during the COVID-19 pandemic (living alone or not). Respondents were asked whether in the past 2 weeks they were diagnosed with COVID-19 by a doctor. We also asked whether respondents were currently in treatment for mental health disorders or felt in need of treatment. Furthermore, respondents were presented with a list of 21 statements (ie, COVID-19-specific items) about the perceived impact of the COVID-19 pandemic on their emotional state and health behaviours, how they coped with the situation, and to what extent they strictly followed the rules. Answer categories were 1 (completely disagree) to 5 (completely agree). A complete overview of the items and their coding is in appendix 2 (p 1). Four symptom severity scales used in previous regular waves, (ie, QIDS, BAI, PSWQ, and DJGLS), were also embedded in the online questionnaire.
Statistical analysis
Characteristics of the study population were compared between people with and without lifetime mental health disorders using either the χ2 test or the t test. We deemed a p value less than 0·05 statistically significant.
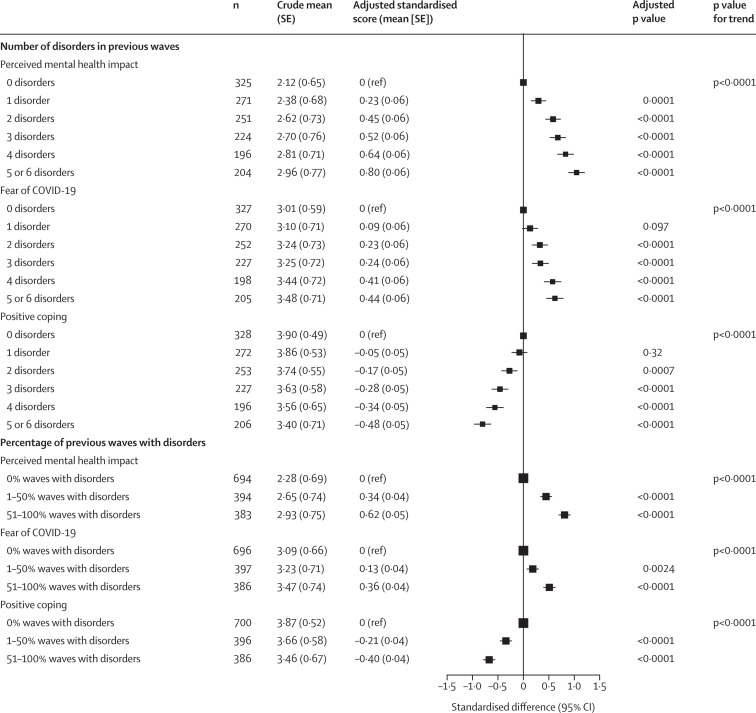
To address our first aim, which was to compare the perceived impact of the COVID-19 pandemic on mental health and the extent to which individuals were able to positively cope with the situation between people with a different number and chronicity of mental health disorders, we used exploratory factor analysis (EFA) with Principal Axis Factoring and Oblimin rotation to examine dimensionality of COVID-19-specific items. The number of dimensions was determined by evaluating Eigenvalues (>1 indicates a distinct dimension), the Scree plot, factor loadings, and conceptual plausibility. Scale scores were computed by taking the average of the items belonging to a dimension, and reliability was calculated using Cronbach's α. The EFA distinguished three dimensions in the COVID-19-specific items, which we labelled as perceived mental health impact (nine items; Cronbach's α=0·85), fear of COVID-19 (six items; α=0·73), and positive coping (five items; α=0·61). We omitted one item about the respondents’ perceived impact of the COVID-19 pandemic on their financial situation, which had factor loadings of 0·15 or less on all three dimensions. Details are reported in appendix 2 (p 1). Linear regression was used to compare COVID-19-specific dimension scale scores between people with different number and chronicity of mental health disorders.
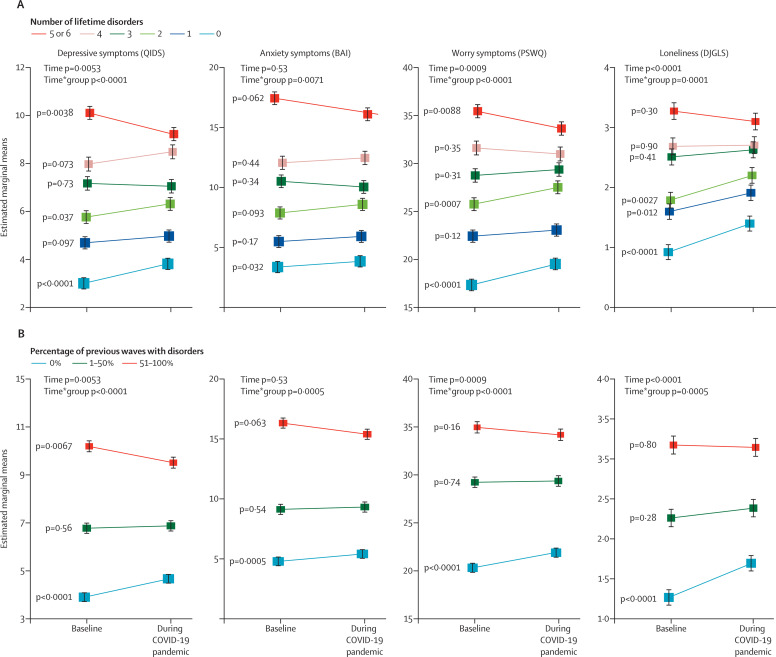
To address our second aim, which was to assess changes in symptoms of depression, anxiety, worry, and loneliness from before to during the COVID-19 pandemic, we calculated average scores of QIDS, BAI, PSWQ, and DJGLS in the preceding waves to represent baseline levels before the COVID-19 pandemic. To check the adequacy of this approach, we calculated intraclass correlations (ICCs) with people as random effects to measure the strength of interwave agreement for the four symptom severity scales (ie, QIDS, BAI, PSWQ, and the DJGLS) during pre-COVID-19 waves. ICCs were calculated for those cohorts and scales for which there were up to four waves that preceded the COVID-19 pandemic. Results indicated a generally high similarity (ICC >0·8) between values (appendix 2 p 2).25 When there was only one measurement available in the previous waves, that value was used. We used mixed models with random intercept to compare changes in QIDS, BAI, PSWQ, and the DJGLS from before to during the COVID-19 pandemic across groups. Interaction terms of time and group indicated whether changes in symptoms differed across groups. We obtained estimated marginal means to quantify changes in symptoms by the number and chronicity of mental health disorders.
In addition to reporting results using original scores of the dimension scales and symptom severity scales, we also presented results using forest plots, in which standardised scores were used that enabled easier comparison of trends among different outcomes. All models were adjusted for age, gender, education, living situation, and the date of the response.
We additionally compared effects of specific types of lifetime mental health disorders on outcomes by simultaneously entering them in the models. In linear regression, their associations with the three COVID-19-specific dimensions were largely similar regarding both direction and magnitude (appendix 2 p 3). Also, in the mixed model, changes in symptoms from before to during the COVID-19 pandemic were largely similar across disorders, except for dysthymic disorder, which showed a relative decrease in depressive symptoms and loneliness compared with those in other disorders (appendix 2 p 4). Overall, these results indicated that each disorder generally had similar effects on outcomes, which confirmed the adequacy of combining information in two indicators summarising severity and chronicity of all mental health disorders.
Several separate supplementary analyses were done. To limit the potential effect of differences in assessment timeframe after the COVID-19 outbreak, we focused on information obtained within April, 2020 (n=1427). To eliminate the potential effect of SARS-CoV-2 infection on mental health, we repeated analyses in people not diagnosed with COVID-19 (n=1500). Analyses were rerun after not considering a diagnosis of obsessive-compulsive disorder in mental health disorder status because it was selectively available. We also did stratified analyses by age 50 years, gender, and source study.
The descriptive analysis and EFA were done in SPSS version 22. The ICC function from the DescTools R package (version 0.99.28) was used to obtain ICCs. We used packages in R (version 3.6.0) for linear regression and mixed models (lme4, version 1.1–21; emmeans, version 1.4.3.01) and for figures (forestplot, version 1.9).
Role of the funding source
The funder of this study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to all data in the study and had final responsibility for the decision to submit for publication.
Results
Between April 1 and May 13, 2020, online questionnaires were sent out every 2 weeks to 2748 living participants in the three studies who gave permission to be contacted for further research activities. After excluding 110 individuals who could not be contacted, most (85%) participants were from NESDA (n=2245), with 4% from NESDO (n=108), and 11% from NOCDA (n=285). 1517 (58%) participants filled in the online questionnaire at least once. We used the first response per respondent. Compared with respondents, non-respondents were younger (p<0·0001) with a lower education level (p=0·0017), and they were more likely to have a pre-existing mental health disorder (p=0·029), but they did not differ by gender (p=0·54).
Among the 1517 respondents to the online questionnaire (mean age 56·1 [SD 13·2] years; 64% women), 1181 (78%) had a lifetime mental health disorder, either a depressive, anxiety, or obsessive-compulsive disorder (table 2 ). Compared with people without a lifetime disorder, those with lifetime mental health disorders were younger, more likely to be women, have a lower educational level, and (during the COVID-19 pandemic) were more likely to live alone and to currently be on or in need of treatment for mental health.
Table 2.
Characteristics of study population by lifetime mental health disorder
|
Overall (n=1517) |
Lifetime mental health disorder |
||||
|---|---|---|---|---|---|
| Yes (n=1181) | No (n=336) | p value | |||
| Age, years | 56·1 (13·2) | 55·7 (12·9) | 57·7 (14·4) | 0·013 | |
| Gender | .. | .. | .. | <0·0001 | |
| Women | 976 (64%) | 791 (67%) | 185 (55%) | .. | |
| Men | 541 (36%) | 390 (33%) | 151 (45%) | .. | |
| Education | .. | .. | .. | <0·0001 | |
| Basic | 48 (3%) | 42 (3%) | 6 (2%) | .. | |
| Intermediate | 827 (55%) | 671 (57%) | 156 (46%) | .. | |
| High | 642 (42%) | 468 (40%) | 174 (52%) | .. | |
| Source study | .. | .. | .. | <0·0001 | |
| NESDA | 1319 (87%) | 1016 (86%) | 303 (90%) | .. | |
| NESDO | 68 (4%) | 35 (3%) | 33 (10%) | .. | |
| NOCDA | 130 (9%) | 130 (11%) | 0 (0%) | .. | |
| Date of response to online questionnaire | .. | .. | .. | 0·76 | |
| April 1–15, 2020 | 735 (48%) | 578 (49%) | 157 (47%) | .. | |
| April 16–30, 2020 | 692 (46%) | 533 (45%) | 159 (47%) | .. | |
| May 1–15, 2020 | 90 (6%) | 70 (6%) | 20 (6%) | .. | |
| Living alone | 451 (30%) | 370 (31%) | 81 (24%) | 0·011 | |
| COVID-19 diagnosis | 17 (1%) | 15 (1%) | 2 (1%) | 0·30 | |
| Current mental health treatment | 605 (44%) | 590 (55%) | 15 (3%) | <0·0001 | |
| In need of mental health treatment | 50 (4%) | 48 (4%) | 2 (1%) | <0·0001 | |
Data are mean (SD) or n (%). Lifetime mental health disorders included depressive, anxiety, or obsessive-compulsive disorders. NESDA=Netherlands Study of Depression and Anxiety. NESDO=Netherlands Study of Depression in Older Persons. NOCDA=Netherlands Obsessive Compulsive Disorder Association Study.
The two variables for mental health disorder burden (number and chronicity of disorders) both showed a graded dose–response relation, indicating that individuals with more severe or chronic mental health disorders reported a greater impact on their mental health, more fear of COVID-19, and less positive coping with the pandemic (figure 1 ). A similar trend was noted on each of the individual item levels (appendix 2 p 5) showing that, for example, those with a higher disorder burden had more sleep problems, sad emotions, unhealthy lifestyles (eg, snacking, drinking, smoking, or inactivity), and fear of infection, and less connection and confidence with society and ability to enjoy being at home.
Figure 1.
COVID-19-specific dimensions in relation to severity and chronicity of depressive, anxiety, or obsessive-compulsive disorders
Severity is the number of lifetime disorders. Chronicity is the percentage of previous waves with current disorders. The crude mean refers to the mean score in each dimension by mental health disorder status. To create the forest plot, each COVID-19-specific dimension score was standardised. The adjusted standardised score was derived from linear regression, adjusted for age, gender, education, living situation, and date of response.
Figure 2 depicts levels of the four symptom scores (ie, QIDS, BAI, PSWQ, and DJGLS) before and during the COVID-19 pandemic, by number and chronicity of mental health disorders. Overall, both before and during the COVID-19 crisis, the four symptom scores were significantly higher in individuals with more severe and more chronic disorders. Compared with pre-COVID-19 levels, symptoms of depression (β=0·26, 95% CI 0·07 to 0·44), worry (0·66, 0·25 to 1·07), and loneliness (0·22, 0·11 to 0·33) increased during the pandemic. Overall, no significant change in symptoms of anxiety was observed (β=0·10, 95% CI –0·25 to 0·45). Judging by the significant interaction of time and group, the change in these four scales from before to during the COVID-19 pandemic differed across mental health disorder status; a dose–response gradient was observed in the change in symptom scores in relation to number and chronicity of disorders (appendix 2 p 6). Specifically, people without severe or chronic mental health disorders tended to show an increase in all four symptom scores during the COVID-19 pandemic. Average increase was rather modest: only ten (3%) participants without a history of mental health disorders scored above the threshold for moderate-to-severe depressive symptoms (QIDS scores ≥11) during the pandemic. By contrast, in individuals with the largest mental health disorder burden, no overall increase in symptom severity was seen. In fact, in a few analyses (eg, depressive symptoms and severity or chronicity indicator; worry and severity indicator), people with the most severe or chronic mental health disorders even showed an average significant decrease in symptom severity.
Figure 2.
Trajectories of symptom severity before and during the COVID-19 pandemic in relation to severity and chronicity of depressive, anxiety, or obsessive-compulsive disorders
Severity is the number of lifetime disorders (A). Chronicity is the percentage of previous waves with current disorders (B). Baseline levels refer to average scores of QIDS, BAI, PSWQ, and DeJong Q in the preceding waves before the COVID-19 pandemic. Mixed models were adjusted for age, gender, education, living situation, and date of response. Data are mean; error bars show the SE. QIDS=16-item Quick Inventory of Depressive Symptoms. BAI=21-item Beck Anxiety Inventory. PSWQ=11-item Penn State Worry Questionnaire. DJGLS=6-item De Jong Gierveld Loneliness Scale.
Our findings remained robust in all supplementary analyses. Stratified analyses by age 50 years, gender, and source study showed similar trends across strata.
Discussion
In our longitudinal study of three Dutch psychiatry case-control cohorts, we noted a graded dose–response relation between the number and chronicity of depressive, anxiety, or obsessive-compulsive disorders and perceived mental health impact of COVID-19, fear of the virus, and poorer ability to cope, during the first few weeks after the national lockdown in the Netherlands. Both before and during the COVID-19 pandemic, levels of symptoms of depression, anxiety, worry, and loneliness were systematically higher in people with multiple and chronic mental health disorders. However, we did not find evidence that there was a strong increase in symptoms during the COVID-19 pandemic in those with a higher burden of disorders. In fact, changes in scores from before to during the pandemic indicated increasing symptom levels in people without mental health disorders, whereas changes of symptom levels were minimal or even negative in individuals with the most severe and chronic mental health disorders.
By applying COVID-19-specific items (ie, 21 statements about the perceived impact of the COVID-19 outbreak on emotional state, behaviours, and coping with the situation), we were able to directly capture the mental health impact of and coping with the COVID-19 crisis among people with and without mental health disorders. As expected, the perceived mental health impact and fear of COVID-19 were more substantial among participants with lifetime mental health disorders, and these individuals struggled more to cope with the COVID-19 pandemic. However, the COVID-19-specific items have not been validated. Moreover, we administered validated scales of depressive symptoms, anxiety, worry, and loneliness. Again, participants with mental health disorders scored higher across all scales. Taken together, these findings support concerns raised at the beginning of the COVID-19 pandemic that people with psychiatric illnesses are more emotionally vulnerable during this crisis.3, 8
The current study is among the first to assess symptoms in the same individuals both before and during the COVID-19 pandemic. For people with severe or chronic mental health disorders, the COVID-19 pandemic did not seem to exacerbate their pre-existing high levels of symptoms. However, the levels of depressive symptoms, anxiety, worry, and loneliness increased more in people with no or less severe or chronic mental health disorders. Although this finding could suggest a potential increased need of mental health care among people without mental health disorders, the increase of symptoms seemed rather modest. As such, the elevated symptom levels among this population might partly represent a normal sadness and fear response to an unprecedented crisis.
Meanwhile, we noted a decrease in depressive symptoms and worry during the COVID-19 pandemic among people with the greatest mental health disorder burden, which has several possible explanations. First, with transmission mitigation strategies in place, individuals with severe mental health disorders might experience some sense of relaxation as their world and habits became more in sync with the quarantined society.2 Second, staying at home could help them build a structured and fixed daily routine, which has been expressed as a preferable setting to provide a feeling of safety.26 Third, the decrease in depressive symptoms and worry might be attributable to regression to the mean and recovering due to the naturalistic course of mental health disorders.27 However, prepandemic symptom severity levels were based on average scores across the preceding waves covering many years.
In our study, we used the first response to the online questionnaire, and more than 80% of data during the COVID-19 pandemic were collected during the first month of the national lockdown in the Netherlands. Thus, our findings represent the initial emotional reaction that could stabilise or fall after people start to adjust to the situation or to receive more information about the virus.28 Data collection is currently ongoing and will enable us to track longitudinal changes in the four symptom dimensions and the perceived mental health impact and coping during the longer pandemic trajectory and beyond the national lockdown.
Some study limitations need to be acknowledged. First, different modes of data collection were applied during the previous waves in 2006–16 (face-to-face interviews) and for the COVID-19 questionnaire (completed online). However, this difference applied to all respondents, thereby it probably does not cause differential associations by psychiatric status. Second, the response rate (58%) of the online questionnaire was rather low. Non-respondents were more likely to have a pre-existing mental health disorder, which could affect our findings by underestimating the mental health impact on individuals with mental health disorders. Third, no standardised assessment tool was applied to ascertain mental health disorders during the COVID-19 pandemic. Instead, we evaluated the severity and chronicity of mental health disorders based on previous waves of the three cohort studies. Assessment timeframes of the four symptom severity scales differed between NESDA, NESDO, and NOCDA; thus, caution is warranted when comparing trajectories of these scores. Finally, our approach of measuring severity across disorders by counting the number of disorders might not be optimal. However, we found that the association between each type of disorder and mental health outcomes was similar and that there was a graded dose–response relation between the number of disorders and symptom severity, suggesting that counting the number of disorders was a good way to distinguish meaningful psychiatric subgroups.
The strengths of our study include well characterised psychiatric status (based on several diagnostic interviews) and use of COVID-19-specific items and four validated symptom scales to assess multiple dimensions of emotional response to the COVID-19 pandemic. Our study is among the first to relate longitudinal mental health data from more than 10 years before the COVID-19 pandemic within the same individuals to symptom levels during the COVID-19 pandemic. These long-term data allowed for a valid check on the true changes in mental health symptoms due to the COVID-19 pandemic.
In summary, although the symptom severity of people with depressive, anxiety, or obsessive-compulsive disorders was systematically higher compared with individuals without mental health disorders, pre-existing illness seemed to not necessarily predispose to a greater level of emotional reactivity to the COVID-19 pandemic during the first few weeks of national lockdown in the Netherlands. Future work is warranted to track the long-term effect of the COVID-19 pandemic on mental health in people with and without mental health disorders as the pandemic developed and with implementation of transmission mitigation strategies.
This online publication has been corrected. The corrected version first appeared at thelancet.com/psychiatry on January 25, 2021
Data sharing
According to European law (General Data Protection Regulation), data containing potentially identifying or sensitive patients’ information are restricted. However, for academic researchers, data could be available on request via the NESDA (nesda@ggzingeest.nl), NESDO (d.rhebergen@ggzingeest.nl), and NOCDA (p.vanoppen@ggzingeest.nl) data access committees.
Acknowledgments
Acknowledgments
This study was funded by the Dutch Research Council (grant no 440.20.009). The infrastructure for the NESDA study is funded through the Geestkracht programme of the Netherlands Organisation for Health Research and Development (grant no 10-000-1002) and financial contributions by participating universities and mental health-care organisations (VU University Medical Center, Geestelijke gezondheidszorg (GGZ) inGeest, Leiden University Medical Center, Leiden University, GGZ Rivierduinen, University Medical Center Groningen, University of Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Rob Giel Onderzoekscentrum). The infrastructure for the NESDO study is funded through the Fonds NutsOhra (project 0701-065), Stichting tot Steun VCVGZ, NARSAD The Brain and Behaviour Research Fund (grant id 41080), and by participating universities and mental health-care organisations (VU University Medical Center, Leiden University Medical Center, University Medical Center Groningen, University Medical Center St Radboud, GGZ inGeest, GGNet, GGZ Nijmegen, GGZ Rivierduinen, Lentis, and Parnassia). The infrastructure for the NOCDA study is funded by participating universities and mental health-care organisations (Academic Department VU Medical Center, GGZ inGeest, Innova Research Centre, Mental Health Care Institute GGZ Centraal, Marina de Wolf Anxiety Research Centre, Center for Anxiety Disorders Overwaal, Dimence, GGZ Overijssel, Department of Psychiatry at Leiden University Medical Center, Vincent van Gogh Institute Mental Health Care Centre, Academic Anxiety Center, PsyQ Maastricht University, Division Mental Health and Neuroscience, and Stichting Steun).
Contributors
All authors had the idea for the study. K-YP and AALK wrote the initial analysis plan, with input from all other authors. K-YP, AALK, and EJG did the data analysis. AALK and EJG produced the figures. K-YP wrote the first draft of the report, and all other authors contributed to editing and commenting on the final version. BWJHP obtained research funding.
Declaration of interests
BWJHP reports grants from Janssen Research and Boehringer Ingelheim, outside of the submitted work. All other authors declare no competing interests.
Supplementary Materials
References
- 1.Statistics Netherlands Coronavirus crisis FAQs. Nov 16, 2020. https://www.cbs.nl/en-gb/dossier/coronavirus-crisis-cbs-figures
- 2.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pierce M, McManus S, Jessop C, et al. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7:567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Lancet Redefining vulnerability in the era of COVID-19. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30757-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020;77:891–892. doi: 10.1001/jamapsychiatry.2020.0894. [DOI] [PubMed] [Google Scholar]
- 10.Bojdani E, Rajagopalan A, Chen A, et al. COVID-19 pandemic: impact on psychiatric care in the United States. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Percudani M, Corradin M, Moreno M, Indelicato A, Vita A. Mental health services in Lombardy during COVID-19 outbreak. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hao FY, Tan WQ, Jiang L, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Rheenen TE, Meyer D, Neill E, et al. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: initial results from the COLLATE project. J Affect Disord. 2020;275:69–77. doi: 10.1016/j.jad.2020.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Penninx BW, Beekman AT, Smit JH, et al. The Netherlands Study of Depression and Anxiety (NESDA): rationale, objectives and methods. Int J Methods Psychiatr Res. 2008;17:121–140. doi: 10.1002/mpr.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Comijs HC, van Marwijk HW, van der Mast RC, et al. The Netherlands study of depression in older persons (NESDO); a prospective cohort study. BMC Res Notes. 2011;4:524–533. doi: 10.1186/1756-0500-4-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schuurmans J, van Balkom AJ, van Megen HJ, et al. The Netherlands Obsessive Compulsive Disorder Association (NOCDA) study: design and rationale of a longitudinal naturalistic study of the course of OCD and clinical characteristics of the sample at baseline. Int J Methods Psychiatr Res. 2012;21:273–285. doi: 10.1002/mpr.1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wittchen HU. Reliability and validity studies of the WHO–Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 18.First MB, Spitzer RL, Gibbon M, Williams JBW. American Psychiatric Press; New York, NY: 1996. User's guide for the Structured Clinical Interview for DSM-IV axis I disorders (SCID-I): clinician version. [Google Scholar]
- 19.Lamers F, van Oppen P, Comijs H, et al. Comorbidity patterns of anxiety and depression disorders in a large cohort study: the Netherlands Study of Depression and Anxiety (NESDA) J Clin Psychiatry. 2011;72:341–348. doi: 10.4088/JCP.10m06176blu. [DOI] [PubMed] [Google Scholar]
- 20.Hofmeijer-Sevink MK, van Oppen P, van Megen HJ, et al. Clinical relevance of comorbidity in obsessive compulsive disorder: the Netherlands OCD Association study. J Affect Disord. 2013;150:847–854. doi: 10.1016/j.jad.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 21.Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 23.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 24.De Jong Gierveld J, Van Tilburg T. A 6-item scale for overall, emotional, and social loneliness: confirmatory tests on survey data. Res Aging. 2006;28:582–598. [Google Scholar]
- 25.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pelto-Piri V, Wallsten T, Hylen U, Nikban I, Kjellin L. Feeling safe or unsafe in psychiatric inpatient care, a hospital-based qualitative interview study with inpatients in Sweden. Int J Ment Health Syst. 2019;13:23–32. doi: 10.1186/s13033-019-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Streiner DL. Regression toward the mean: its etiology, diagnosis, and treatment. Can J Psychiat. 2001;46:72–76. doi: 10.1177/070674370104600111. [DOI] [PubMed] [Google Scholar]
- 28.Bults M, Beaujean DJ, de Zwart O, et al. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: results of three consecutive online surveys. BMC Public Health. 2011;11:2–14. doi: 10.1186/1471-2458-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
According to European law (General Data Protection Regulation), data containing potentially identifying or sensitive patients’ information are restricted. However, for academic researchers, data could be available on request via the NESDA (nesda@ggzingeest.nl), NESDO (d.rhebergen@ggzingeest.nl), and NOCDA (p.vanoppen@ggzingeest.nl) data access committees.