Abstract
Antimicrobials have allowed medical advancements over several decades. However, the continuous emergence of antimicrobial resistance restricts efficacy in treating infectious diseases. In this context, the drug repositioning of already known biological active compounds to antimicrobials could represent a useful strategy. In 2002 and 2003, the SARS-CoV pandemic immobilized the Far East regions. However, the drug discovery attempts to study the virus have stopped after the crisis declined. Today’s COVID-19 pandemic could probably have been avoided if those efforts against SARS-CoV had continued. Recently, a new coronavirus variant was identified in the UK. Because of this, the search for safe and potent antimicrobials and antivirals is urgent. Apart from antiviral treatment for severe cases of COVID-19, many patients with mild disease without pneumonia or moderate disease with pneumonia have received different classes of antibiotics. Diarylureas are tyrosine kinase inhibitors well known in the art as anticancer agents, which might be useful tools for a reposition as antimicrobials. The first to come onto the market as anticancer was sorafenib, followed by some other active molecules. For this interesting class of organic compounds antimicrobial, antiviral, antithrombotic, antimalarial, and anti-inflammatory properties have been reported in the literature. These numerous properties make these compounds interesting for a new possible pandemic considering that, as well as for other viral infections also for CoVID-19, a multitarget therapeutic strategy could be favorable. This review is meant to be an overview on diarylureas, focusing on their biological activities, not dwelling on the already known antitumor activity. Quite a lot of papers present in the literature underline and highlight the importance of these molecules as versatile scaffolds for the development of new and promising antimicrobials and multitarget agents against new pandemic events.
Keywords: antimicrobials, antimalarial, antiviral, diarylurea, bis-arylurea, pandemics, COVID-19
1. Introduction
Today, bacterial resistance represents a critical problem for human health and the care of patients with numerous diseases, thus urgently calling for the immediate development and use in therapy of drugs against multi-resistant pathogens [1]. This has encouraged the research and investigation of various drug discovery approaches: one of them is drug repurposing, which is a strategy to establish new applications for approved or investigational drugs, aside from the original medical indications. Drug repurposing is becoming more appealing because it allows for overcoming the restrictions related to the expense and delay of the discovery and development of new drugs [2,3]. In the last twenty years, humans have encountered five pandemic diseases, severe acute respiratory syndrome (SARS), Avian flu, Ebola, Middle East respiratory syndrome (MERS) [4], and coronavirus disease 2019 (COVID-19) [5,6,7]. Recently, a new variant of COVID-19 was also described [8]. It has been reported that the disease prognosis of COVID-19 is largely influenced by multi-organ involvement. The multi-organ dysfunction is characterized by acute lung and liver failure, acute kidney injury, cardiovascular disease, and a wide spectrum of hematological abnormalities and neurological disorders. The most important mechanisms are related to the direct and indirect pathogenic features induced by SARS-CoV2. Moreover, organ failure may be induced by the cytokine storm, as a result of increased levels of inflammatory mediators, endothelial dysfunction, coagulation abnormalities, and the infiltration of inflammatory cells into the organs [9,10]. Medical treatment options for COVID-19 include antiviral drugs, chloroquine/hydroxychloroquine, antibiotics, beta-blockers, steroidal and nonsteroidal anti-inflammatory drugs, and some others [11,12]. In this framework, new multitarget molecules could be useful to counteract the effects of the virus at various levels and in different ways. The repositioning of anticancer diarylureas for new indications, such as antimicrobial [13], antiviral, and anti-inflammatory, could be a very interesting option for obtaining multitarget agents useful for the treatment or prevention of pandemics. Diarylureas or bis-arylureas are generally known as anticancer agents [14], for instance sorafenib, regorafenib, linifanib, tivozanib, and ripretinib, which have been recently reviewed by our research group [15]. Nevertheless, it is reported that they have also a lot of different and important biological activities [16,17]. Indeed, they are antimicrobials, particularly active in schistosomiasis and malaria [18,19,20], anti-inflammatory, antiplatelet, and antiviral agents [21,22], and allosteric modulators of the cannabinoid CB1 receptor [23], VLA-4 integrin antagonists [24], and EGFR inhibitors [25]. Taking into account the multiple factors involved in the pathogenesis of COVID-19, all the activities of diarylureas make them promising tools for the treatment of this disease. It is known that the novel coronavirus pneumonia is closely associated with inflammatory storms. Indeed, the patients with severe COVID-19 have a “cytokine storm” syndrome, given the high-levels of pro-inflammatory cytokines found in these patients [26]. Moreover, there is an increasing recognition of a prothrombotic state in COVID-19 [27] and neuropsychiatric diseases such as depression and anxiety [28]. The expression levels of angiotensin converting enzyme 2 (ACE2), acetylcholinesterase (AChE), interleukin-6 (IL-6), based on their involvement in both environmental responses and comorbid conditions, such as hypertension and type 2 diabetes mellitus, may substantially raise the respiratory syndrome coronavirus 2 (SARS-CoV-2) mortality [29]. In this review, we summarize the recent research on diarylureas with antimicrobial and antiviral activities and other properties related to pandemics. The literature data reported herein make these molecules attractive in this area.
2. Diarylureas with Antimicrobial Activity
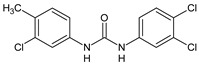
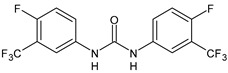
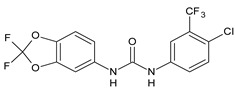
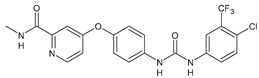
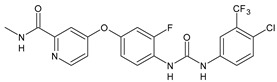
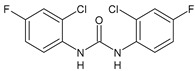
Antimicrobials are small molecules that can inhibit or kill bacteria. However, some bacteria can grow and survive despite antimicrobial pressures, a characteristic known as antimicrobial resistance. In clinical settings, resistant bacterial infections decrease the achievable treatment options and increase morbidity and mortality, compared with those caused by susceptible microbes [30]. Moreover, traditional bactericidal antibiotics kill only actively growing bacterial cells, whereas non-growing metabolically inactive cells are tolerant to and therefore “persist” in the presence of legacy antibiotics. Thus, the discovery of new antibiotics may be envisaged. Triclocarban (TCC, Table 1 and Table 2) is a diarylurea used as an antimicrobial agent in feminine care products, such as bar soaps, deodorants, detergents, and other disinfectants [31]. Besides its antimicrobial activity, TCC has been acknowledged as an endocrine disruptor, i.e., “an exogenous substance or mixture that alters function(s) of the endocrine system and consequently causes side effects in an intact organism, or its progeny, or (sub)populations” (World Health Organization 2013) resulting in hormonal effects [32]. Moreover, TCC demonstrated anti-inflammatory effects by inhibiting soluble epoxide hydrolase (sEH) in a lipopolysaccharide (LPS)-challenged murine model [33]. It has been demonstrated that TCC alter cardiac functions [34] and is associated to potential adverse birth outcomes in neonates, in particular decreased gestational age at birth [35]. The biodegradation of TCC is very slow as a result of its three chlorine atoms; thus, it can persist in the environment for years and it accumulates in aquatic habitats [36]. For these reasons, since 2016, the Food and Drug Administration (FDA) has banned its use in consumer products [37]. The mechanism of action against bacteria is still unknown. Unlike other antibacterial compounds, triclocarban does not interfere with the membrane. Therefore, it may act as an inhibitor of lipoprotein synthesis, by mimicking the natural substrate of enoyl-acyl-carrier protein reductase (ENR) enzyme. ENR is a highly conserved enzyme of lipid biosynthetic pathways in bacteria, notably gram-negative, gram-positive, and mycobacterial species [38]. Macsics et al. (2020) recently studied the TCC mechanism of action. Protein demethylmenaquinone methyltranferase (MenG) was proposed as the molecular target of TCC, which inhibits its biosynthesis finally leading to inhibition of the S. aureus menaquinone metabolism [39].
Table 1.
Diarylureas as antiparasitic agents.
| Structure | Compd | Activity | Ref |
|---|---|---|---|
| Antiparasitic agents | |||
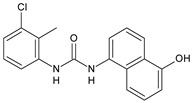
|
MMV665852 | IC50 = 4.7 µM (S. mansoni NTS) IC50 = 0.8 µM (adult S. mansoni) IC50 = 4.4 µM (juvenile S. japonicum) IC50 = 2.2 µM (adult S. japonicum) |
[47] [49] |
|
Triclocarban (TCC) | IC50 = 0.07 µM (S. mansoni NTS) IC50 = 0.4 µM (adult S. mansoni) |
[48] |
|
1 | IC50 = 1.3 µM (S. mansoni NTS) IC50 = 0.7 µM (adult S. mansoni) |
[48] |
|
2 | IC50 = 0.2 µM (adult S. mansoni) | [48] |
|
3 | IC50 = 3.6 µM (adult S. mansoni) | [48] |
|
4 | IC50 = 7.0 µM (adult S. mansoni) | [48] |
|
5 | IC50 = 2.5 µM (juvenile S. japonicum) IC50 = 1.5 µM (adult S. japonicum) |
[49] |
|
6 (Flucofuron) | IC50 = 2.8 µM (juvenile S. japonicum) IC50 = 1.5 µM (adult S. japonicum) |
[49] |
|
7 | IC50 = 0.15 µM (S. mansoni NTS) IC50 = 0.19 µM (adult S. mansoni) |
[19] |
|
Sorafenib
(BAY-43-9006) |
IC50 = 4.1 µM (S. mansoni NTS) IC50 = 1.1 µM (adult S. mansoni) |
[54] |
|
Regorafenib (BAY-73-4506) | IC50 = 6.9 µM (S. mansoni NTS) IC50 = 1.0 µM (adult S. mansoni) |
[54] |
Table 2.
Diarylureas as antibacterials and antifungals.
| Structure | Compd | Activity | Ref |
|---|---|---|---|
| Antibacterial activity | |||

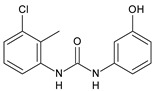
|
8 | MIC50 = 0.05 µg/mL (S. aureus ATCC 12600 and MRSA) |
[55] |
|
PK150 | MIC = 0.3 µM (S. aureus NCTC 8325) | [56] |
|
Sorafenib
(BAY-43-9006) |
MIC = 3 µM (S. aureus NCTC 8325) | [56] |
|
Regorafenib
(BAY-73-4506) |
MIC = 3 µM (S. aureus NCTC 8325) | [56] |
|
Triclocarban
(TCC) |
MIC50 = 0.5 µg/mL (S. aureus) | [55] |
|
6
(Flucofuron) |
MIC = 0.25 mg/L (S. aureus NCTC 8325; ATCC 12598 and S. epidermidis ATCC 12228; 35984) |
[58] |
|
9 | MIC = 0.5‒8.0 µg/mL (different gram-positive bacteria) |
[59] |
|
10 | Inhibition zones = 14.0 mm Gram (+) B. subtilis NCTC-10400 and Gram (‒) P. aeruginosa ATCC 10145 and E. coli ATCC 23282 |
[61] |
|
PQ401 | MIC = 4 µg/mL (different S. aureus) MBC = 4 g/mL (S. aureus VRS1 strains) |
[62] |
|
11 | Inhibition zone = 23 mm, at a concentration of 200 µg/mL (P. mirabilis ATCC 19181) |
[63] |
|
12 | Inhibition zone = 24 mm, at a concentration of 200 µg/mL (P. mirabilis ATCC 19181) |
[63] |
|
13 | MIC = 31.3 µg/mL (S. boydii ATCC 9905; E. faecalis ATCC 29212; B. cereus ATCC 10987; K. pneumoniae ATCC 10031) |
[65] |
|
14 | MIC = 31.3 µg/mL (S. boydii ATCC 9905; E. faecalis ATCC 29212; B. cereus ATCC 10987; K. pneumoniae ATCC 10031) |
[65] |
|
15 | MIC = 10 µg/mL (MRSA NRS123) |
[67] |
|
16 | MIC = 8 µg/mL (MRSA NRS123) |
[67] |
|
17 | MIC = 10 µg/mL (MRSA NRS123) |
[67] |
|
18 | MIC = 2‒4 µg/mL (various MRSA) |
[67,68] |
|
19 | MIC = 2‒4 µg/mL (various MRSA) |
[68] |
|
20 | MIC = 6.25 µg/mL (M. tuberculosis H37Rv) |
[69] |
|
21 | MIC = 3.125 µg/mL (M. tuberculosis H37Rv) |
[69] |
|
22 | MIC = 6.0 µg/mL (M. tuberculosis pathogenic strain H37Rv) MIC = 2.0 µg/mL (M. tuberculosis nonpathogenic strain mc26030) |
[70] |
|
23 | MIC = 5.2 µg/mL (M. tuberculosis pathogenic strain H37Rv) MIC = 1.0 µg/mL (M. tuberculosis nonpathogenic strain mc26030) |
[70] |
| Antifungal activity | |||
|
24 | Inhibition, at 30 μM, of the growth of P. obscurans by 80% and P. viticola and 100%, after 120 h exposure | [71] |
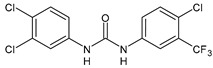
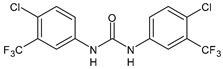
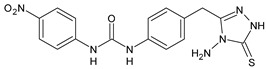
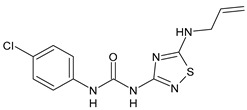
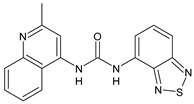
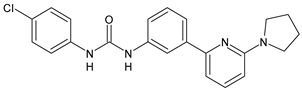
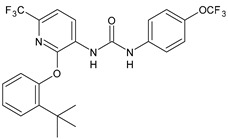
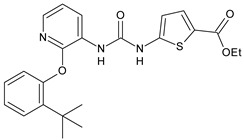
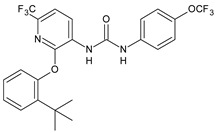
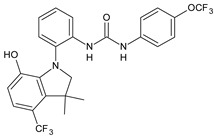
2.1. Diarylureas with Antiparasitic Activity
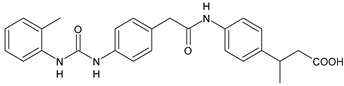
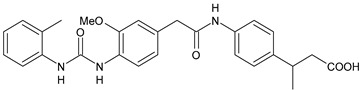
Diarylureas with antiparasitic activity are summarized in Table 1. TCC and several analogues have been studied in schistosomiasis. This disease, also called bilharzia, is one of the most dramatic parasitic diseases in tropical countries and remains a serious public health problem in the tropics and subtropics, affecting one billion people, with 250 million infected in 74 countries [40]. It is considered one of the most widespread infectious diseases among the WHO-prioritized 17 neglected tropical diseases (NTDs) [41]. Schistosomiasis is caused by the trematode worms of the genus Schistosoma (Platyhelminthes Trematoda). The clinically most relevant species are Schistosoma japonicum, S. haematobium, and S. mansoni [42]. S. japonicum is responsible for intestinal and hepatosplenic schistosomiasis in China, the Philippines, and Indonesia; S. haematobium determines urogenital schistosomiasis in Africa and in some countries of the Arabian Peninsula (it has also recently emerged on the French island of Corsica); S. mansoni causes intestinal and hepatic disease in Africa, the Arabian Peninsula, and Latin America [43]. Praziquantel (PZQ) discovered in the 1970s, is the only drug available for the treatment of schistosomiasis [44]; no schistosomiasis vaccines have been accepted for public use yet [45]. Despite many benefits of PZQ, most notably its high efficacy and excellent tolerability, the drug has important disadvantages, above all its inefficacy against juvenile schistosomes. Furthermore, the increasing administration of PZQ to millions of people annually results in high drug pressure, and thus drug-resistant parasites are likely to evolve. The Medicines for Malaria Venture (MMV) Malaria Box is a collection of over 400 compounds including families of structures identified in phenotypic screens of pharmaceutical and academic libraries against the Plasmodium falciparum malaria parasite [46]. The antischistosomal properties of some of these compounds with confirmed in vitro activity against P. falciparum were studied. Diarylurea MMV665852, a structural analog of TCC, which showed activity against P. falciparum 3D7, was also evaluated against S. mansoni in vitro on newly transformed schistosomula (NTS) and adult S. mansoni worms and showed IC50 values of 4.7 and 0.8 µM, respectively. All the compounds were then tested in vivo using the chronic S. mansoni mouse model. The compound MMV665852 showed the highest in vivo activity, given that treatment of S. mansoni infected mice with a single oral 400 mg/kg dose of MMV665852 reduced worm burden by 52.5% [47]. Then, a search for structures similar to that of MMV665852, using a Tanimoto-Rogers similarity coefficient of 0.85 as the cutoff, identified 46 compounds, 13 of which were diarylureas. All compounds were first tested in vitro on NTS and adult S. mansoni worms. MMV665852, TCC and 1 showed IC50 = 4.7, 0.07, and 1.3 µM, respectively against NTS; TCC and 1 showed IC90 of 0.3 and 2.8 µM, respectively, against NTS. TCC, compounds 1 and 2, tested at 33.3 µM, showed high in vitro activity against adult S. mansoni, showing IC50 values of 0.4, 0.7 and 0.2 µM, and IC90 of 1.4, 2.2 and 0.8 µM, respectively, after a 72-h incubation period. Interestingly, compounds 3 and 4 were found to be schistosomicidal against the adult S. mansoni 72 h post incubation, with calculated IC50 values are of 3.6 and 7.0 µM, respectively [48]. In another work, in order to enlarge the structure-activity relationships for compounds analogues of MMV665852, a series of diarylureas was studied in vitro against the juvenile S. japonicum. Compounds 5 and 6, tested at 32 μM, killed the juvenile worms within 72 h, and exhibited a higher activity than the positive control MMV665852 (IC50 = 2.5 and 2.8 μM versus 4.4 μM of MMV665852). IC50 values against the adult worms were lower than those for juvenile worms (IC50 = 1.5 and 2.2 μM versus 2.2 μM of MMV665852) [49]. However, compound 6 had been described previously in the literature, as an insecticide known to be highly toxic to fish and invertebrates, named flucofuron [50,51]. Recent studies also address it as a toxicant [52,53]. Wu et al. studied twenty diarylureas and found that compound 7 had antischistosomal activity against S. mansoni higher than that of MMV66558, by killing the NTS at a concentration of 10 µM. This compound killed both NTS and adult S. mansoni with IC50 values of 0.15 and 0.19 µM, respectively. In this paper, studies regarding the relationships existing between lipophilicity and metabolic stability were also carried out. The authors found that there were no clear relationships between lipophilicity and metabolic stability. Compound 7 had the best in vivo antischistosomal activity, with worm burden reduction value of 40% following administration of single 100 mg/kg oral doses [19]. In the last years, protein kinase inhibitors were used as starting points for drug discovery in studies on helminth growth and development. Sorafenib and its structurally related analogue regorafenib were tested in vitro against the larval and adult stage of S. mansoni and they were lethal to NTS within 24 h (IC50 = 4.1 and 1.1 µM, respectively, for sorafenib; IC50 = 6.9 and 1.0 µM, respectively for regorafenib). Sorafenib caused the death of all adults, at 33.3 μM, within 24 h [54].
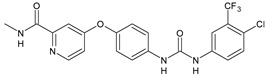
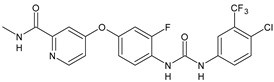
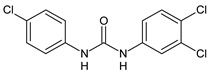
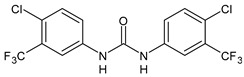
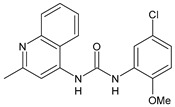
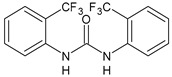
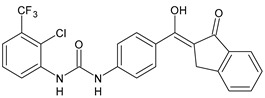
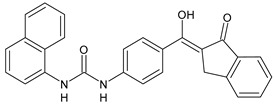
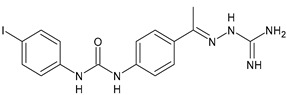
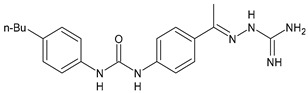
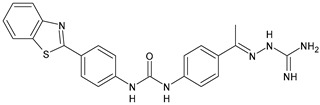
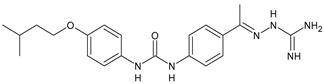
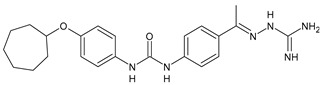
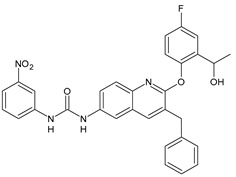
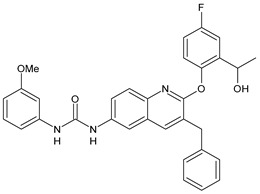
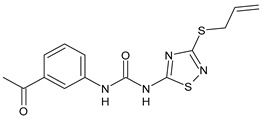
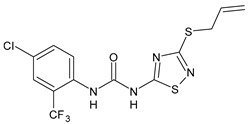
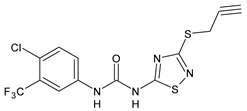
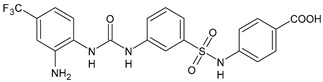
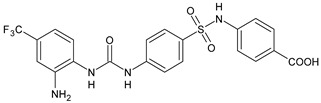
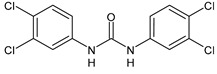
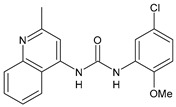
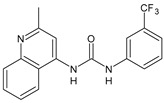
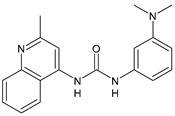
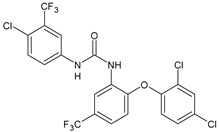
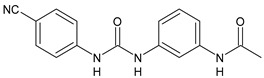
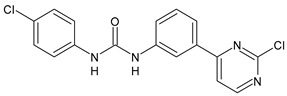
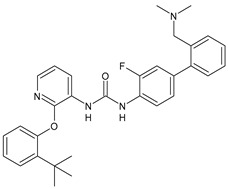
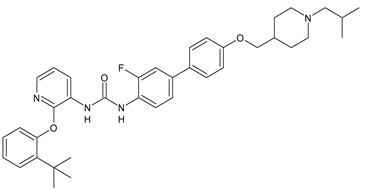
2.2. Diarylureas with Antibacterial and Antifungal Activity
In Table 2, antibacterial and antifungal diarylureas are described. The work by Pujol et al. [55] was devoted to diarylureas designed to overcome the toxicological effect of TCC due to the three chlorine atoms. One or more chlorine atoms of TCC were reduced and/or replaced by pentafluorosulfanyl groups, bioisosteres of the trifluoromethyl groups. Some of the newly synthesized compounds exhibited high potency, broad spectrum of antimicrobial activity against Gram-positive bacteria, and high selectivity index, while displaying a lower spontaneous mutation frequency than TCC. Preliminary experiments suggested a bactericidal mode of action for this family of ureas. Moreover, some of the new molecules removed preexisting S. aureus biofilms, which is important in food industry as well as in hospital settings and displayed a lower spontaneous mutation frequency in S. aureus than TCC. Compound 8 emerged as the most promising compound showing the highest potency against both S. aureus ATCC 12600 and methicillin-resistant S. aureus MRSA (MIC50 = 0.05 µg/mL versus MIC50 = 0.5 µg/mL of TCC), a broader spectrum of activity, and a higher selectivity index [55]. Le et al. (2020) has recently studied 72 compounds deriving from sorafenib as antibacterials. Compound PK150 showed anti-bacterial activity against several pathogenic strains of S. aureus at sub-micromolar concentrations. MIC value against methicillin sensitive (MSSA) S. aureus NCTC 8325 was 0.3 µM for PK150 and 3 µM for both sorafenib and regorafenib (MIC = 1 and 3 µM for vancomycin and linezolid, respectively). It exhibited a 10-fold enhanced anti-MRSA activity, lack of resistance development under laboratory conditions, killing of persisters, elimination of established biofilms, and in vivo efficacy in a mouse model. Chemical proteomic studies did not reveal a known kinase as target, but interference with menaquinone biosynthesis and dysregulation of protein secretion as putative target mechanisms [56]. Macsics et al. (2020) studied the mechanism of PK150. As TCC, it is an inhibitor of MenG biosynthesis, but unlike TCC, it is not affected by environmentally acquired TCC resistance as it causes over-activation of SpsB, the bacterial signal peptidase I enzyme from S. aureus [39]. The two anticancer agents sorafenib and regorafenib were also investigated as antibacterials and proposed for further studies in this field [57]. Chang et al. (2016) studied antibacterial and antiproliferative activity of sorafenib. The authors compared anti-Staphylococcus activity (MIC, Minimum Inhibitory Concentration) versus antiproliferative activity (IC50) of test agents against HEK-293 human embryonic kidney, K-562 human erythromyeloblastoid leukaemia, HT-29 human colon adenocarcinoma cell lines. It showed antibacterial activity against S. aureus NCTC 8325, with MIC90 (i.e., concentration that inhibits 90% of bacteria strains tested) = 4 mg/L. However, the authors concluded that it lacked selectivity, having a low selectivity ratio (IC50 for human cells/MIC for S. aureus) of 0.7–0.8, thus assessing it is not a feasible candidate for treatment of MRSA infection. Then, the authors studied other diarylureas and found that compounds 6 was highly potent against S. aureus (NCTC 8325 and ATCC 12598) and S. epidermidis (ATCC 12228 and ATCC 35984) strains, with MIC = 0.25 mg/L. It was classified as bactericidal. The selectivity ratio for this compound was higher than sorafenib, ranging between 4 and 19 [58]. In 2004, Francisco et al. [59] synthesized and studied a series of phenyl thiazolyl urea as new inhibitors of the bacterial cell-wall biosynthesis. Indeed, the peptidoglycan biosynthesis requires 10 synthetic transformations and, correspondingly, 10 specific enzymes, including MurA and MurB. Phenyl thiazolyl urea 9 demonstrated a good activity against MurA and MurB and gram-positive bacteria including MRSA, vancomycin resistant Enterococcus (VRE), and penicillin-resistant Streptococcus pneumoniae (PRSP), with MIC values ranging between 0.5 and 8.0 µg/mL. However, when tested in the presence of 4% bovine serum albumin, their MICs increased significantly [59]. The importance of compound 9 is underlined by its use as a positive control for studies on MurB [60]. Hassan et al. (2014) reported a study on diarylureas with activity against bacteria and fungi. Compound 10 possessed antimicrobial activity against the tested Gram-positive bacterium Bacillus subtilis (NCTC-10400) and Gram negative bacteria Pseudomonas aeruginosa (ATCC 10145) and Escherichia coli (ATCC 23282) showing mean values of inhibition zones (in mm) of 14.0 versus 34.0, 32.0 and 30.0 of erythromycin, respectively. The compound showed weak antifungal activity [61]. Diarylurea PQ401 is a small molecule previously described as inhibitor of the insulin like growth factor I receptor (IGF-1R) signaling and then studied in breast cancer and osteosarcoma [15]. Recently, it has been proposed as a lead candidate for repurposing as a membrane-active antimicrobial agent because it is able to kill both growing and non-growing antibiotic-tolerant MRSA by lipid bilayer disruption. When tested against a panel of antibiotic-resistant S. aureus strains (MW2, ATCC 33591, JE2, BF1‒5, BF7,8, BF10,11), including MRSA clinical isolates and a vancomycin-resistant S. aureus (VRSA; strain VRS1), it showed a MIC value of 4 µg/mL. PQ401 was demonstrated to be active against MRSA (MW2, ATCC 33591, JE2) and VRS1 strains showing a minimum bactericidal concentration (MBC) of 4 g/mL. Unlike other well-studied membrane-disrupting cationic antimicrobial low-molecular-weight antimicrobials, maximum membrane activity was shown by PQ401 in its neutral form rather than its cationic form. PQ401 also showed efficacy in both the Caenorhabditis elegans and Galleria mellonella models of MRSA infection [62]. A series of the diarylureas was synthesized and screened for antimicrobial activity against Gram positive and negative bacteria and fungi. Compounds 11 and 12 showed activity against Proteus mirabilis ATCC 19181 comparable to that of standard ciprofloxacin (zone of inhibition in 23 and 24 mm, respectively, at a concentration of 200 µg/mL compared to 30 mm of ciprofloxacin) [63]. In the work by Gezegen et al. (2017), a series of diarylureas was studied as antimicrobial and antiproliferative agents. Antimicrobial activity studies were carried out against Gram-positive and Gram-negative bacteria and yeasts, by using piperacillin/tazobactam (P/T = 8/1) and fluconazole as positive controls. The most interesting compounds were 13 and 14. They were both more active than reference against Shigella boydii ATCC 9905 and Enterococcus faecalis ATCC 29212 (MIC = 31.3 µg/mL versus 62.5 µg/mL), a clinically significant pathogen implicated in different types of infections [64], and against Bacillus cereus ATCC 10987 (MIC = 31.3 µg/mL versus 125 µg/mL), while they showed the same activity of the reference against Klebsiella pneumoniae ATCC 10031 (MIC = 31.3 µg/mL) [65]. Diarylureas 15–17, bearing an aminoguanidine group that is a common moiety in medicinal chemistry [66], were active against MRSA NRS123 showing MIC values of 10 µg/mL (for compounds 15 and 17) and 8 µg/mL (for compound 16) [67]. Compound 16 was chosen as the lead compound for further studies on a series of diarylureas bearing an alkoxy side chain in lieu of the n-butyl moiety. The substitution with an isopentyloxy or cycloheptyloxy group gave compounds 18 and 19, which showed activity in vitro against MRSA (MIC values between 2 and 4 µg/mL versus vancomycin ranging from 0.5 to 1 µg/mL). Compound 19 was chosen for further in vivo studies using a C. elegans animal model. The antibacterial activity was confirmed as 19, at 10 µg/mL, reduced the burden of MRSA USA400 by more than 50% in infected worms, which is a result better than that observed for vancomycin (at the same concentration it reduces the bacterial burden by 25%). Compound 19 also showed better pharmacokinetics, showing enhanced stability to hepatic metabolism, it was also demonstrated to be suitable for intravenous or topic administration (for treatment MRSA skin infections) [67]. In a sequent work, the investigation of action mechanism of a series diphenylureas revealed that they exert their antibacterial effect by interfering with bacterial cell wall synthesis. Interestingly, both compounds 18 and 19 are able of re-sensitizing VRSA to the effect of vancomycin. Furthermore, compound 18 can penetrate staphylococcal biofilms (S. aureus and S. epidermidis) to reduce the burden of bacteria present within the biofilm, although at high concentrations [68]. Upadhayaya et al. (2009) studied several quinoline derivatives as antimycobacterials. Tuberculosis (TB) is an old human disease and represent a major threat for mankind especially because of the emergence of resistance strain of Mycobacterium tuberculosis against antibiotics. Compounds 20 and 21 inhibited M. tuberculosis H37Rv up to 98% and 94%, respectively, at a concentration of 6.25 µg/mL. They showed MIC values of 6.25 µg/mL and 3.125 µg/mL, respectively [69]. Compounds 22 and 23 showed MIC values of 6.0 and 5.2 µg/mL, respectively, against M. tuberculosis pathogenic strain H37Rv and 2.0 and 1.0, respectively, against M. tuberculosis nonpathogenic strain mc26030. They also showed selective inhibition of mycolic acid biosynthesis. At the same time, these molecules also executed their potent immunomodulatory activity by up-regulation of the pro-inflammatory cytokines IFN-g and IL-12 and down-regulation of IL-10 [70]. Compound 24 was studied for antifungal activity, containing 1,2,4-triazole, showed good antifungal activity against Phomopsis species. These are known as Phomopsis cane and leaf spot (P. viticola) causes economic losses to the vine grape production in the USA and Europe, while P. obscurans is responsible of Phomopsis leaf blight and fruit rot of strawberry. At 30 μM, compound 24 inhibited the growth of P. obscurans and P. viticola by 80% and 100%, respectively, after 120 h exposure, showing an activity similar to that of the positive control Captan, a well-known multisite inhibitor fungicide with no systemic activity, used as a commercial protectant fungicide to prevent anthracnose diseases in fruits and ornamentals [71].
3. Diarylureas with Antiviral Activity
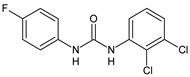
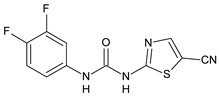
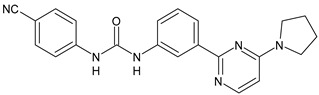
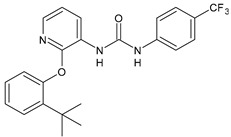
Today, viruses represent the most common cause of infections in the world; therefore, research is being conducted to identify new safe and effective antivirals [72]. Among the several virus families, the Flaviviridae one has attracted the attention of some research groups working on the diarylureas field. It includes Dengue virus (DENV), West Nile virus (WNV), and Yellow fever virus (YFV), Zika virus (ZIKV), many of which cause serious human and animal infections. Micewicz et al. (2018) described the identification of potent inhibitors of Zika virus infection, which is a mosquito-borne RNA virus, with picomolar activity in vitro. Compounds ASN 07115854, ASN 07115873, ASN 07115881, and ASN 07115927 (Table 3) were active in the low nanomolar or picomolar range (IC50 = 160.3 nM, 189.2 pM, 317.7 pM and 26.9 nM, respectively) as assessed by using a viral plaque-forming assay and the A549 human lung carcinoma cell line, described as highly permissive to Zika infection [73]. In a successive paper by the same research group, a new library of diarylureas was screened using the same assay. Several compounds in the library showed high inhibitory activity against Zika virus with IC50 values in the picomolar range. The most interesting compound was 25 which exhibited an excellent IC50 = 85.1 pM [74]. Recently, several diarylureas have been studied for the treatment of DENV. New compounds binding the flavivirus NS5 AdoMet-dependent mRNA methyltransferase (MTase) domain, a main component of DENV replication complex, were proposed using a fragment-based drug design. Compounds 26 and 27 were the most interesting compounds, as they showed high inhibitory effect in both DENV N7-MTase assay (IC50 = 91 µM and 110 µM, respectively) and in WNV 2′-O-MTase assay (IC50 = 51 µM and 71 µM, respectively) [75].
Table 3.
Diarylureas as antiviral and antimalarial agents.
| Structure | Compd | Ref | |
|---|---|---|---|
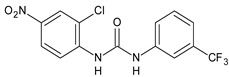
|
Antiviral agents
Inhibitors of Zika virus infection |
|||
|
ASN 07115851 | IC50 = 160.3 nM (by viral plaque assay and A549 human lung carcinoma cell line) |
[73] |

|
ASN 07115873 | IC50 = 189.2 pM (by viral plaque assay and A549 human lung carcinoma cell line) |
[73] |
|
ASN 07115881 | IC50 = 317.7 pM (by viral plaque assay and A549 human lung carcinoma cell line) |
[73] |
|
ASN 07115927 | IC50 = 26.9 nM (by viral plaque assay and A549 human lung carcinoma cell line) |
[73] |
|
25 | IC50 = 85.1 pM (by viral plaque assay and A549 human lung carcinoma cell line) |
[74] |
| DENV | |||
|
26 | IC50 = 91 µM (DENV N7-MTase assay) IC50 = 51 µM (WNV 2′-O-MTase assay) |
[75] |
|
27 | IC50 = 110 µM (DENV N7-MTase assay) IC50 = 71 µM (WNV 2′-O-MTase assay) |
[75] |
| Antimalarial agents | |||
|
MMV665852 | EC50 = 1160 nM (P. falciparum) | [47] |
|
WR268961 | IC50 = 0.03‒0.16 µg/mL (P. falciparum W2 and D6) | [76] |
|
PQ401 | EC50 = 0.053 μM (P. falciparum 3D7 and K1) |
[20] |
|
28 | EC50 = 0.32 μM (P. falciparum 3D7) |
[20] |
|
29 | EC50 = 0.031 μM (P. falciparum 3D7) EC50 = 0.11 μM (P. falciparum K1) |
[20] |
|
30 | EC50 = 0.016 μM) (P. falciparum 3D7) EC50 = 0.079 μM (P. falciparum K1) |
[20] |
|
31 | EC50 = 0.037 µM (P. falciparum 3D7) EC50 = 0.055 µM (P. falciparum Dd2) |
[77] |
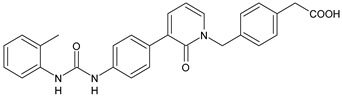
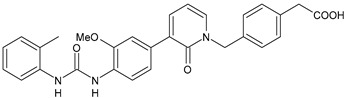
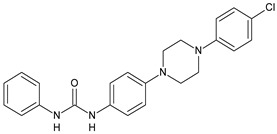
4. Diarylureas as Antimalarial Agents
Diarylurea MMV665852, the structural analog of TCC mentioned above, was also studied for antimalarial activity and showed an EC50 = 1160 nM against P. falciparum 3D7 (Table 3). Plasmepsins are aspartic proteases that malarial parasites use to digest hemoglobin during the intraerythrocytic stage. Diphenylurea derivative WR268961, obtained from the Walter Reed chemical inventory, was found to inhibit recombinant plasmepsins, which possess kinetic similarity to the native enzymes, with a Ki value between 1 and 6 µM. It inhibited the growth of P. falciparum strains W2 and D6, with IC50 ranging from 0.03 to 0.16 µg/mL and showed low toxicity to mammalian cells. Some derivatives of WR268961 in which the amidine moiety was replaced by a sulfonic acidic group, retained plasmepsin inhibitory activity but were poor inhibitors of P. falciparum growth in vitro (figures not shown) [76]. Zhang et al. 2010 studied a large library of diarylureas for antimalarial activity against chloroquine-sensitive (3D7) and chloroquine-resistant (K1) strains of P. falciparum. PQ401, showed the same potency of chloroquine (EC50 = 0.053 μM versus 0.047 μM) against the 3D7 cell line in vitro. Compounds 28 and 29 showed higher activity than the parent compound, showing EC50 values of 0.32 and 0.031 μM, respectively, against the same cell line. The most interesting compound of the series was 33 which was 3-fold more potent than chloroquine (EC50 = 0.016 μM). Compounds 29 and 30 also showed high activity against chloroquine resistant K1 strain (EC50 = 0.11 and 0.079 μM, respectively, versus 1,23 μM of chloroquine) [20]. Compound 31 demonstrated EC50 values of 0.037 µM and 0.055 µM against in vitro cultured parasite 3D7 (drug-sensitive) and Dd2 (resistant to chloroquine and pyrimethamine–sulfadoxine) P. falciparum strains, respectively. It also demonstrated in vivo efficacy in a Plasmodium berghei antimalarial mouse model, with >50% survival at day 31 post-treatment after subcutaneous administration at 256 mg/kg [77].
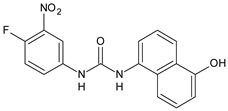
5. Diarylureas as Anti-Inflammatory Agents and Antiulcer Agents
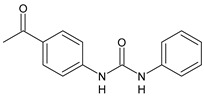
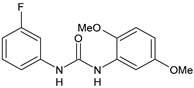
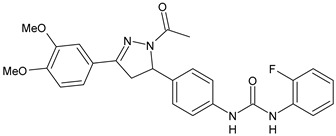
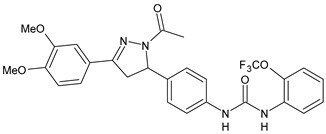
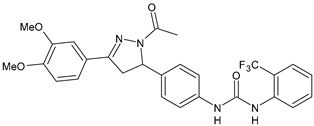
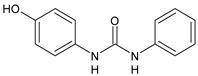
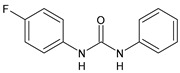
The inhibition of Δ5-desaturase by small molecules may attenuate inflammatory responses, potentially creating next-generation anti-inflammatory agents. Diarylurea CP-214339 (Table 4) acts as inhibitor of a Δ5-desaturase in rodents (IC50 = 0.13 µM), thus decreasing arachidonic acid synthesis [78,79]. Several diarylureas, in which one aryl moiety is represented by a substituted dihydropyrazole, were studied for their anti-inflammatory and antimicrobial activities. In vitro anti-inflammatory activity was tested against the pro-inflammatory cytokines (TNF-α and IL-6) by TNF-α and IL-6 inhibition assay. Compounds 32–34 exhibited anti-inflammatory activity, showing TNF-α (85%, 58% and 61%, respectively) and IL-6 (93%, 75% and 80%, respectively) inhibitory activity as compared to the standard dexamethasone but at a higher concentration (10 µM). They showed low or no antimicrobial activity [80]. Rakesh et al. (2017) studied a series of disubstituted ureas for their in vitro H+/K+ ATPase (proton pump) and anti-inflammatory activity. Diarylurea 35 behaved as an antiulcer, exhibiting higher activity against proton pump than omeprazole (IC50 = 18.4 µg/mL versus 38.2 µg/mL), while compound 36 displayed higher anti-inflammatory activity than indomethacin (IC50 = 20.3 µg/mL versus 44.8 µg/mL) [81].
Table 4.
Diarylureas with various biological activities.
| Structure | Compd | Ref | |
|---|---|---|---|
| Anti-inflammatory and antiulcer agents | |||
|
CP-214339 | IC50 = 0.13 µM (Δ5-desaturase inhibitor in rodents) |
[78,79] |
|
32 | 85% inhibition TNF-α; 93% inhibition IL-6 | [80] |
|
33 | 58% inhibition TNF-α; 75% inhibition IL-6 | [80] |
|
34 | 61% inhibition TNF-α; 80% inhibition IL-6 | [80] |
|
35 | IC50 = 18.4 µg/mL (proton pump inhibition) |
[81] |
|
36 | IC50 = 20.3 µg/mL (anti-inflammatory activity in human blood) |
[81] |
| Integrine antagonists | |||
|
37 | pKi = 7.2 (VLA-4 antagonist) |
[85] |
|
38 | pKi = 9.1 (VLA-4 antagonist) |
[85] |
|
39 | pKi = 8.7 (VLA-4 antagonist) |
[86] |
|
40 | pKi = 9.3 (VLA-4 antagonist) |
[86] |
| Allosteric Modulators of CB1 | |||
|
PSNCBAM-1 | CB1 agonist | [88] |

|
41 | CB1 agonist | [89] |
|
42 | CB1 agonist | [89] |
|
LDK1317 | CB1 agonist | [90] |
|
LDK1321 | CB1 agonist | [90] |
| Antiplatelet agents | |||
|
BPTU |
Ki = 6 nM (P2Y1 receptor) IC50 = 0.28 µM (P2Y1 receptor) |
[92] [95] |
|
43 | EC50 = 2 µM (ECAT) Ki = 17 nM (P2Y1 receptor) |
[94] |
|
44 |
Ki = 30 nM (P2Y1 receptor) |
[94] |
|
45 | IC50 = 0.21 µM (P2Y1 receptor) |
[95] |
|
46 | IC50 = 12.52 µM (P2Y1 receptor) |
[95] |
|
47 | IC50 = 7.19 µM (P2Y1 receptor) |
[95] |
|
48 |
Ki = 4.3 nM (P2Y1 receptor); IC50 = 2,5 nM (P2Y1 FLIPR) |
[96] |
|
49 |
Ki = 7.9 nM (P2Y1 receptor); IC50 = 0.12 nM (P2Y1 FLIPR); IC50 = 0.13 µM (ADP-induced PA assay) |
[97] |
|
50 |
Ki = 4.0 nM (P2Y1 receptor); IC50 = 0.22 nM (P2Y1 FLIPR); IC50 = 0.17 µM (ADP-induced PA assay) |
[98] |
|
51 |
Ki = 12.9 nM (P2Y1 receptor); IC50 = 0.22 nM (P2Y1 FLIPR); IC50 = 0.41 µM (ADP-induced PA assay) |
[98] |
| Antiepileptic | |||
|
52 | ED50 = 28.5 mg/kg (MES induced seizures) |
[99] |
| Agents for neuroinflammation | |||
|
53 |
Ki = 0.47 µM (TRPV1 capsaicin antagonism) |
[101] |
|
54 |
Ki = 0.49 µM (TRPV1 capsaicin antagonism); Ki = 1.39 μM (CB2) |
[101] |
|
55 |
Ki = 0.56 µM (TRPV1 capsaicin antagonism) |
[101] |
|
56 | Binding prediction to CXCR2 (homology model) |
[101] |
| AChE and BuChE inhibitors | |||
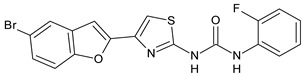
|
57 | IC50 = 3.85 µM (AChE) IC50 = 9.25 µM (BuChE) |
[102] |
6. Diarylureas as Integrine Antagonists
The inhibitors of integrin α4β1, also known as VLA-4 (Very Late Antigen-4), might serve as useful agents in the treatment of asthma, rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, Alzheimer’s disease (AD), and stroke [82]. In interstitial pneumonia (IP), integrin α4β1 expression level is known to be up regulated by inflammatory cytokines [83]. The major cause of death of COVID-19 patients is characterized by respiratory failure due to IP [84]. Compounds 37 and 38 (Table 4) were identified as potent antagonists of VLA-4 showing pKi values of 7.2 and 9.1, respectively [85]. Witherington et al. (2020) studied new diarylureas and found compounds 39 and 40 displaying excellent inhibitory potency (pKi = 8.7 and 9.3, respectively) [86].
7. Diarylureas as Allosteric Modulators of Cannabinoid Receptor 1
The activation of cannabinoid receptor 1 (CB1) is essential for the development of an effective innate immune response during bacterial infection [87]. Diarylurea PSNCBAM-1 is an allosteric modulator of CB1 and antagonized G protein coupling [88]. Starting from this lead compound, several analogues have been studied. Compounds 41 and 42 (Table 4), bearing a pyrimidine ring, were shown act as allosteric modulators of CB1 while showing an antagonism of G-protein coupling activity. They ascertained extracellular signal-regulated kinases ERK1/2 phosphorylation mediated via β-arrestin [89]. In a recent work, several restricted derivatives of PSNCBAM-1 were studied. Compounds LDK1317 and LDK1321 exhibited binding affinity (KB) and binding cooperativity factor (α) of KB = 110 nM, α = 2.3 (for LDK1317) and KB = 85 nM, α = 5.9 (for LDK1321) and had computationally predicted drug-like properties and better solubility than the parent compound [90].
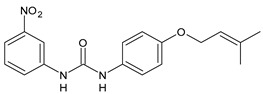
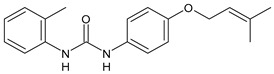
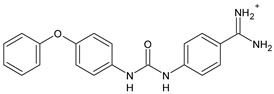
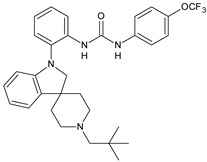
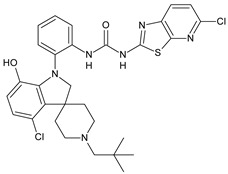
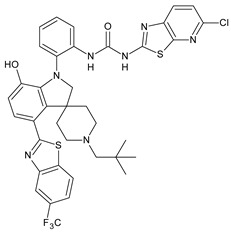
8. Diarylureas as Antiplatelet Agents
Adenosine-5′-diphosphate (ADP) plays an essential role in platelet aggregation and thrombus formation. Two G-protein coupled P2 purinergic ADP receptors, P2Y1 and P2Y12, are both required for full ADP-induced platelet aggregation. In recent years, the P2Y1 receptor has emerged as an attractive target for anti-thrombotic therapies from preclinical antithrombotic studies and haemorragic models. P2Y12 receptor antagonists are predicted to blunt platelet activation and they may exert beneficial actions on other cell types affected by COVID-19 [91]. Diarylurea BPTU showed good binding affinity with P2Y1 receptor (Ki = 6 nM) and moderate antiplatelet activity in the ADP-induced platelet aggregation assay in vitro. The pharmacokinetic profile of BPTU revealed that this compound had a moderate half-life (t1/2 = 1.43 h) and bioavailability (F = 18%) when orally dosed at 30 mg/kg in rats [92]. From the crystal structures of BPTU binding with P2Y1 receptor it emerged that BPTU bound to P2Y1 receptor on the lipid interface of the transmembrane domain, thus indicating BPTU as an allosteric modulator of P2Y1 receptor [93]. Starting from BPTU as a lead compound, several other analogues were then synthesized. Wang et al. (2013) demonstrated that compounds 43 and 44 (Table 4) showed significantly higher aqueous solubility while maintaining antiplatelet activity similar to that of BPTU. Compound 43 was efficacious and showed a dose-dependent reduction of thrombosis weight with an EC50 of 2 µM in the rabbit electrolytic-mediated carotid arterial thrombosis (ECAT) model and had a moderate prolongation of bleeding time in rats similar to that of compound BPTU. However, it showed toxicity in the rabbit [94]. A novel series of 2-(phenoxyaryl)-3-urea derivatives were designed, synthesized, and biologically evaluated for their anti-thrombotic activity and compared to BPTU. Compound 45 demonstrated a good P2Y1 receptor antagonistic potency in vitro (IC50 = 0.21 µM versus 0.28 µM of BPTU). In a study on antiplatelet aggregation, compounds 46 and 47 exhibited good antiplatelet activity (IC50 = 12.52 and 7.19 µM, respectively). The possible binding modes of compounds with P2Y1 receptor were also explored by molecular docking simulation. The docking studies demonstrated that compound 45 interacted well with Phe119 through hydrophobic interaction and modestly improved the P2Y1 receptor antagonistic activity, making it justifiable for further investigation [95]. Qiao et al. (2013) reported new conformationally constrained ortho-anilino diarylureas. Compound 48 acts as P2Y1 antagonist, showing a Ki value of 4.3 nM in the primary membrane binding assay and improved in vitro functional potency in the fluorescent imaging plate reader (FLIPR) P2Y1 assay (IC50 = 2.5 nM). It showed a strong antithrombotic effect with mild bleeding liability in the rat thrombosis and hemostasis models, showing IC50 = 4.9 µM in the ADP-induced platelet aggregation (PA) assay [96]. In a successive study, the benzothiazole-containing diarylurea 52 was demonstrated to be a potent P2Y1 antagonist and orally bioavailable with a suitable PK profile in preclinical species. It showed a good binding affinity (Ki = 7.9 nM) and improved in vitro functional potency in the FLIPR P2Y1 assay (IC50 = 0.12 nM). It also showed a strong antithrombotic effect in the ADP-induced PA assay (IC50 = 0.13 µM), better than the previously described 48 and enhanced haemorragic profile compared to P2Y12 antagonist clopidogrel in rat efficacy/bleeding models [97]. Then, other diarylureas were studied. Compound 50 was slightly stronger in binding affinity (Ki = 4.0 nM) but much stronger in FLIPR assay (IC50 = 0.22 nM) and was equiactive in the inhibition of platelet aggregation (PA IC50 = 0.17 µM). The spiropiperidinyl indoline-containing diarylurea 51, retained a good in vitro potency (Ki = 12.9 nM) and was much more active in the in vitro functional assays with FLIPR (IC50 = 0.22 nM) and PA (IC50 value of 0.41 µM). Compound 51 also showed the highest metabolic stability and lowest clearance (CL) value (thus, high i.v. exposure), small volume of distribution (Vdss) values, and modest bioavailability [98].
9. Diarylureas Acting on Central Nervous System
Several diarylureas were described in the literature for their activities on CNS. Compound 52 (Table 4) was effective as antiepileptic in both maximal electroshock (MES) and subcutaneous pentylenetetrazole (scPTZ) seizure tests, showing ED50 value of 28.5 mg/kg against MES induced seizures. Toxicological results revealed that no significant toxicity was detected after administration for 14 days (sub-acute toxicity study) in rats. It also exerted antidepressant activity in forced swim test (FST) and tail suspension test (TST) in mice [99].
10. Diarylureas for Neuroinflammation
Neuroinflammation has been connected to neurodegenerative disorders of the brain, such as AD, Parkinson’s disease (PD), and Huntington’s disease (HD). The transient receptor potential vanilloid 1 (TRPV1) plays an essential part in neuroinflammation and has been recently reviewed [100]. Feng et al. (2016) reported a study on diarylureas acting on TRPV1. Compounds 50–55 (Table 4) were the most active against TRPV1 (Ki values for capsaicin antagonism = 0.47, 0.49, 0.56 µM, respectively). Compound 57 also showed potential binding affinity (Ki = 1.39 μM) at cannabinoid receptor 2 (CB2), which is another attractive target for immunoinflammation diseases. Compound 56 was predicted to target the CXC chemokine receptor 2 (CXCR2), which is also a potential target for the treatment of chronic inflammatory diseases. However, the bioassay validation of CXCR2 with this compound was not performed [101].
11. Diarylureas as Inhibitors of AChE and BuChE
The genetic predisposition has been suggested to be involved in COVID-19 disease transmission. Genetic polymorphisms in other multiple genes, such as that codifying for the AChE, is relevant to SARS-CoV-2 pathophysiology. Several diarylureas were studied for their action on AChE for the treatment of AD. Compound 57 (Table 4) exhibited intense activity of inhibition on both AChE and butyrylcholinesterase (BuChE), with an IC50 = 3.85 and 9.25 µM, respectively; thus, it may act as a dual inhibitor. The selectivity index was 2.40 against AChE and BuChE, respectively [102].
12. Summary
This paper reviews the current status and the recent studies of biologically important diarylurea derivatives. The diarylurea moiety may be considered a privileged structure in medicinal chemistry. Besides the widely known antitumor tyrosine kinase inhibitors sorafenib and others, several diarylureas have been studied for a variety of biological activities, including antimicrobial, antiviral, anti-inflammatory and antiplatelet action. The intention of this review is to highlight the profusion of recent biological data that exists around the diarylurea class of compounds, focusing especially on their antimicrobial, antiviral and all the other activities that could be useful for the treatment or prevention of new COVID-19 pandemics, for which there is any evidence of effective treatments. Promising strategies to combat SARS-CoV-2 include the discovery of therapeutic targets, drugs and vaccines/monoclonal antibodies and, considering the emergency and urgency, approved repurposed drugs, which could be important and useful for the therapeutic management of the disease. To date the main therapies used to treat this disease are antiviral drugs, chloroquine/hydroxychloroquine and antibiotics, bronchospasmolitics, beta-blockers, steroidal and nonsteroidal anti-inflammatory drugs and so on). As most of the early-detected bacterial pneumonia can be safely and effectively treated with antibiotics, the broad-spectrum antibiotics are widely used, as well, in COVID-19 patients. Drugs such as remdesivir, chloroquine, ritonavir, tocilizumab, corticosteroids have been repurposed for the treatment of COVID-19, although their clinical effectiveness has not yet been confirmed. Unfortunately, the use of chloroquine and derivatives such as hydroxychloroquine, alone or in combination with other drugs, resulted in cardiac toxicity. Taking into account that COVID-19 is a multi-organ dysfunction, which causes comorbidities or complications and triggers an unregulated systemic inflammatory response, new molecules with multi-target and multi-properties action are need. Recently, new kinases inhibitors have been reported for their implications in modulating the inflammatory response, which is, as well, one of the major issue during the COVID-19. The different biological activities herein described for diarylureas, namely antibacterial, antiviral, anti-inflammatory and anticoagulant, may be very effective in hampering the different steps of SARS-COV-2 diffusion and progression, influencing positively the above mentioned comorbidities. Moreover, the already known anti-bacterial properties make them promising molecules for repositioning diarylureas as antimicrobial agents and interesting scaffolds for the development of multitarget COVID-19 treatments.
Acknowledgments
This work was supported by PRIN (Progetti di Rilevante Interesse Nazionale) Grant 2017M8R7N9_004 from the MIUR, Italy.
Abbreviations
| ACE2 | angiotensin converting enzyme 2 |
| AChE | acetylcholinesterase |
| AD | Alzheimer’s disease |
| ADP | adenosine-5′-diphosphate |
| CB1 | cannabinoid receptor 1 |
| CB2 | cannabinoid receptor 2 |
| CL | clearance |
| CNS | Central Nervous System |
| COVID-19 | Coronavirus disease 2019 |
| CXCR2 | CXC chemokine receptor 2 |
| DENV | dengue virus |
| ECAT | electrolytic-mediated carotid arterial thrombosis |
| ENR | enoyl-acyl-carrier protein reductase |
| FLIPR | fluorescent imaging plate reader |
| FST | forced swim test |
| HD | Huntington’s disease |
| HFF | human foreskin fibroblast |
| IGF-1R | insulin like growth factor I receptor |
| IL-6 | interleukin-6 |
| IP | interstitial pneumonia |
| K B | binding affinity |
| LPS | lipopolysaccharide |
| MenG | demethylmenaquinone methyltranferase |
| MERS | Swine flu |
| Ebola | Middle East respiratory syndrome |
| MES | maximal electroshock |
| MIC | minimum inhibitory concentration |
| MMV | Medicines for Malaria Venture |
| MRSA | methicillin-resistant S. aureus |
| MSSA | methicillin-sensitive S. aureus |
| NTDs | neglected tropical diseases |
| NTS | newly transformed schistosomula |
| PGR | plant growth regulator |
| PA | platelet aggregation |
| PD | Parkinson’s disease |
| PZQ | praziquantel |
| SARS | severe acute respiratory syndrome |
| SARS-CoV | respiratory syndrome coronavirus |
| SARS-CoV-2 | respiratory syndrome coronavirus 2 |
| scPTZ | subcutaneous pentylenetetrazole |
| sEH | soluble epoxide hydrolase |
| Sps | bacterial signal peptidase I enzyme |
| TB | tuberculosis |
| TCC | triclocarban |
| TRPV1 | transient receptor potential vanilloid 1 |
| TST | tail suspension test |
| Vdss | volume of distribution |
| VLA-4 | very late antigen-4 |
| VRSA | vancomycin-resistant S. aureus |
| WNV | West Nile virus |
| YFV | Yellow fever virus |
| ZIKV | Zika virus virus |
Author Contributions
A.C.; D.I.; M.P.; S.A.; C.F.; M.S.S. contributed to the review. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Tackling Antimicrobial Resistance. Volume 26 WHO; Geneva, Switzerland: 2020. Eurohealth (Lond) [Google Scholar]
- 2.Pushpakom S., Iorio F., Eyers P.A., Escott K.J., Hopper S., Wells A., Doig A., Guilliams T., Latimer J., McNamee C., et al. Drug repurposing: Progress, challenges and recommendations. Nat. Rev. Drug Discov. 2019;18:41–48. doi: 10.1038/nrd.2018.168. [DOI] [PubMed] [Google Scholar]
- 3.Nascimento I.J.D.S., de Aquino T.M., da Silva-Júnior E.F. Drug repurposing: A strategy for discovering inhibitors against emerging viral infections. Curr. Med. Chem. 2020 doi: 10.2174/0929867327666200812215852. [DOI] [PubMed] [Google Scholar]
- 4.Reperant L.A., Osterhaus A. Aids, Avian flu, SARS, MERS, Ebola, Zika… What next? Vaccine. 2017;35:4470–4474. doi: 10.1016/j.vaccine.2017.04.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Velavan T.P., Meyer C.G. The COVID-19 epidemic. Trop. Med. Int. Health. 2020;25:278–280. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pascarella G., Strumia A., Piliego C., Bruno F., Del Buono R., Costa F., Scarlata S., Agrò F.E. COVID-19 diagnosis and management: A comprehensive review. J. Intern. Med. 2020;288:192–206. doi: 10.1111/joim.13091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fadaka A.O., Sibuyi N.R.S., Adewale O.B., Bakare O.O., Akanbi M.O., Klein A., Madiehe A.M., Meyer M. Understanding the epidemiology, pathophysiology, diagnosis and management of SARS-CoV-2. J. Intern. Med. Res. 2020;48:0300060520949077. doi: 10.1177/0300060520949077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wise J. Covid-19: New coronavirus variant is identified in UK. BMJ. 2020;371:m4857. doi: 10.1136/bmj.m4857. [DOI] [PubMed] [Google Scholar]
- 9.Mokhtari T., Hassani F., Ghaffari N., Ebrahimi B., Yarahmadi A., Hassanzadeh G. COVID-19 and multiorgan failure: A narrative review on potential mechanisms. J. Mol. Histol. 2020;51:613–628. doi: 10.1007/s10735-020-09915-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zaim S., Chong J.H., Sankaranarayanan V., Harky A. COVID-19 and multiorgan response. Curr. Probl. Cardiol. 2020;45:100618. doi: 10.1016/j.cpcardiol.2020.100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gautret P., Lagier J.-C., Parola P., Hoang V.T., Meddeb L., Mailhe M., Doudier B., Courjon J., Giordanengo V., Vieira V.E., et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents. 2020;56:105949. doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ginsburg A.S., Klugman K.P. COVID-19 pneumonia and the appropriate use of antibiotics. Lancet Glob. Health. 2020;8:e1453–e1454. doi: 10.1016/S2214-109X(20)30444-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farha M.A., Brown E.D. Drug repurposing for antimicrobial discovery. Nat. Microbiol. 2019;4:565–577. doi: 10.1038/s41564-019-0357-1. [DOI] [PubMed] [Google Scholar]
- 14.Garuti L., Roberti M., Bottegoni G., Ferraro M. Diaryl urea: A privileged structure in anticancer agents. Curr. Med. Chem. 2016;23:1528–1548. doi: 10.2174/0929867323666160411142532. [DOI] [PubMed] [Google Scholar]
- 15.Catalano A., Iacopetta D., Sinicropi M.S., Franchini C. Diarylureas as antitumor agents. Appl. Sci. 2021;11:374. doi: 10.3390/app11010374. [DOI] [Google Scholar]
- 16.Sikka P., Sahu J.K., Mishra A.K., Hashim S.R. Role of Aryl Urea Containing Compounds in Medicinal Chemistry. Med. Chem. 2015;5:479–483. doi: 10.4172/2161-0444.1000305. [DOI] [Google Scholar]
- 17.Asif M. Short notes on diaryl ureas derivatives. J. Adv. Res. Biochem. Pharmacol. 2018;1:38–41. [Google Scholar]
- 18.Gemma S., Federico S., Brogi S., Brindisi M., Butini S., Campiani G. Annual Reports in Medicinal Chemistry. Volume 53. Elsevier; Amsterdam, The Netherland: 2019. Dealing with schistosomiasis: Current drug discovery strategies; pp. 107–138. [Google Scholar]
- 19.Wu J., Wang C., Leas D., Vargas M., White K.L., Shackleford D.M., Chen G., Sanford A.G., Hemsley R.M., Davis P.H., et al. Progress in antischistosomal N,N′-diaryl urea SAR. Bioorg. Med. Chem. Lett. 2018;28:244–248. doi: 10.1016/j.bmcl.2017.12.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang Y., Anderson M., Weisman J.L., Lu M., Choy C.J., Boyd V.A., Price J., Siga M., Clark J., Connelly M., et al. Evaluation of diarylureas for activity against Plasmodium falciparum. ACS Med. Chem. Lett. 2010;1:460–465. doi: 10.1021/ml100083c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang W., Wang Y., Lai A., Qiao J.X., Wang T.C., Hua J., Price L.A., Shen H., Chen X., Wong P., et al. Discovery of 4-aryl-7-hydroxyindoline-based P2Y1 antagonists as novel antiplatelet agents. J. Med. Chem. 2014;57:6150–6164. doi: 10.1021/jm5006226. [DOI] [PubMed] [Google Scholar]
- 22.Dighe S.N., Dua K., Chellappan D.K., Katavic P.L., Collet T.A. Recent update on anti-dengue drug discovery. Eur. J. Med. Chem. 2019;176:431–455. doi: 10.1016/j.ejmech.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen T., German N., Decker A.M., Langston T.L., Gamage T.F., Farquhar C.E., Li J.-X., Wiley J.L., Thomas B.F., Zhang Y. Novel diarylurea based allosteric modulators of the cannabinoid CB1 receptor: Evaluation of importance of 6-pyrrolidinylpyridinyl substitution. J. Med. Chem. 2017;60:7410–7424. doi: 10.1021/acs.jmedchem.7b00707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Witherington J., Blaney E.L., Bordas V., Elliott R.L., Gaiba A., Garton N., Green P.M., Naylor A., Smith D.G., Spalding D.J., et al. Pyridone derivatives as potent, orally bioavailable VLA-4 integrin antagonists. Bioorg. Med. Chem. Lett. 2006;16:5538–5541. doi: 10.1016/j.bmcl.2006.08.044. [DOI] [PubMed] [Google Scholar]
- 25.Jiang N., Bu Y., Wang Y., Nie M., Zhang D., Zhai X. Design, Synthesis and Structure–Activity Relationships of Novel Diaryl Urea Derivatives as Potential EGFR Inhibitors. Molecules. 2016;21:1572. doi: 10.3390/molecules21111572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Catalano A. COVID-19: Could Irisin Become the Handyman Myokine of the 21st Century? Coronaviruses. 2020;1:32–41. doi: 10.2174/2666796701999200617154655. [DOI] [Google Scholar]
- 27.Rapkiewicz A.V., Mai X., Carsons S.E., Pittaluga S., Kleiner D.E., Berger J.S., Thomas S., Adler N.M., Charytan D.M., Gasmi B., et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: A case series. E Clin. Med. 2020;24:100434. doi: 10.1016/j.eclinm.2020.100434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mazza M.G., Lorenzo R.D., Conte C., Poletti S., Vai B., Bollettini I., Melloni E.M.T., Furlan R., Ciceri F., Rovere-Querini P., et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phillips N., Park I.-W., Robinson J.R., Jones H.P. The perfect storm: COVID-19 health disparities in US blacks. J. Racial Ethn. Health Disparities. 2020:1–8. doi: 10.1007/s40615-020-00871-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patini R., Mangino G., Martellacci L., Quaranta G., Masucci L., Gallenzi P. The effect of different antibiotic regimens on bacterial resistance: A systematic review. Antibiotics. 2020;9:22. doi: 10.3390/antibiotics9010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Balakrishna K., Rath A., Praveenkumarreddy Y., Guruge K.S., Subedi B. A review of the occurrence of pharmaceuticals and personal care products in Indian water bodies. Ecotoxicol. Environ. Saf. 2017;137:113–120. doi: 10.1016/j.ecoenv.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 32.Bergman Å., Heindel J.J., Jobling S., Kidd K.A., Zoeller R.T. The State-of-the-Science of Endocrine Disrupting Chemicals, World Health Organization and United Nations Environment Programme Report–2012. UNEP/WHO; Geneva, Switzerland: 2013. [(accessed on 18 January 2021)]. Available online: www.who.int/ceh/publications/endocrine/en/index.html. [Google Scholar]
- 33.Liu J., Qiu H., Morisseau C., Hwang S.H., Tsai H., Ulu A., Chiamvimonvat N., Hammock B.D. Inhibition of soluble epoxide hydrolase contributes to the anti-inflammatory effect of antimicrobial triclocarban in a murine model. Toxicol. Appl. Pharmacol. 2011;255:200–206. doi: 10.1016/j.taap.2011.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xie W., Zhang W., Ren J., Li W., Zhou L., Cui Y., Chen H., Yu W., Zhuang X., Zhang Z., et al. Metabonomics indicates inhibition of fatty acid synthesis, beta-oxidation, and tricarboxylic acid cycle in triclocarban-induced cardiac metabolic alterations in male mice. J. Agric. Food Chem. 2018;66:1533–1542. doi: 10.1021/acs.jafc.7b05220. [DOI] [PubMed] [Google Scholar]
- 35.Geer L.A., Pycke B.F.G., Waxenbaum J., Sherer D.M., Abulafia O., Halden R.U. Association of birth outcomes with fetal exposure to parabens, triclosan and triclocarban in an immigrant population in Brooklyn, New York. J. Hazard. Mater. 2017;323:177–183. doi: 10.1016/j.jhazmat.2016.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang Y., Teng Y., Wang D., Han K., Wang H., Kang L. The fate of triclocarban in activated sludge and its influence on biological wastewater treatment system. J. Environ. Manag. 2020;276:111237. doi: 10.1016/j.jenvman.2020.111237. [DOI] [PubMed] [Google Scholar]
- 37.Yun H., Liang B., Kong D., Li X., Wang A. Fate, risk and removal of triclocarban: A critical review. J. Hazard. Mater. 2020;387:121944. doi: 10.1016/j.jhazmat.2019.121944. [DOI] [PubMed] [Google Scholar]
- 38.Batra S., Tusi Z., Madapa S. Medicinal chemistry of ureido derivatives as anti-infectives. Anti-Infect. Agents Med. Chem. (Former Curr. Med. Chem. Anti-Infect. Agents) 2006;5:135–160. doi: 10.2174/187152106776359048. [DOI] [Google Scholar]
- 39.Macsics R., Hackl M.W., Fetzer C., Mostert D., Bender J., Layer F., Sieber S.A. Comparative Target Analysis of Chlorinated Biphenyl Antimicrobials Highlights MenG as Molecular Target of Triclocarban. Appl. Environ. Microbiol. 2020 doi: 10.1128/AEM.00933-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McManus D.P., Dunne D.W., Sacko M., Utzinger J., Vennervald B.J., Zhou X.N. Schistosomiasis. Nat. Rev. Dis. Primers. 2018;4:13. doi: 10.1038/s41572-018-0013-8. [DOI] [PubMed] [Google Scholar]
- 41.Herricks J.R., Hotez P.J., Wanga V., Coffeng L.E., Haagsma J.A., Basanez M.G., Buckle G., Budke C.M., Carabin H., Fevre E.M., et al. The global burden of disease study 2013: What does it mean for the NTDs? PLoS Negl. Trop. Dis. 2017;11:e0005424. doi: 10.1371/journal.pntd.0005424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Campbell C.H., Jr., Binder S., King C.H., Knopp S., Rollinson D., Person B., Webster B., Allan F., Utzinger J., Ame S.M., et al. SCORE operational research on moving toward interruption of schistosomiasis transmission. Am. J. Trop. Med. Hyg. 2020;103(Suppl. 1):58–65. doi: 10.4269/ajtmh.19-0825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McManus D.P., Bergquist R., Cai P., Ranasinghe S., Tebeje B.M., You H. Schistosomiasis-from immunopathology to vaccines. Semin. Immunopathol. 2020;42:355–371. doi: 10.1007/s00281-020-00789-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mäder P., Rennar G.A., Ventura A.M.P., Grevelding C.G., Schlitzer M. Chemotherapy for fighting schistosomiasis: Past, present and future. ChemMedChem. 2018;13:2374–2389. doi: 10.1002/cmdc.201800572. [DOI] [PubMed] [Google Scholar]
- 45.McManus D.P. Recent progress in the development of liver fluke and blood fluke vaccines. Vaccines. 2020;8:553. doi: 10.3390/vaccines8030553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dang N.L., Hughes T.B., Taramelli D. Open source drug discovery with the Malaria Box compound collection for neglected diseases and beyond. PLoS Pathog. 2016;12:e1005763. doi: 10.1371/journal.ppat.1005763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ingram-Sieber K., Cowan N., Panic G., Vargas M., Mansour N.R., Bickle Q.D., Wells T.N.C., Spangenberg T., Keiser J. Orally active antischistosomal early leads identified from the open access Malaria Box. PLoS Negl. Trop. Dis. 2014;8:30. doi: 10.1371/journal.pntd.0002610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cowan N., Dätwyler P., Ernst B., Wang C., Vennerstro J.L., Spangenberg T., Keiser J. Activities of N,N’-diarylurea MMV665852 analogs against Schistosoma mansoni. Antimicrob. Agents Chemother. 2015;59:1935–1941. doi: 10.1128/AAC.04463-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yao H., Liu F., Chen J., Li Y., Cui J., Qiao C. Antischistosomal activity of N,N′-arylurea analogs against Schistosoma japonicum. Bioorg. Med. Chem. Lett. 2016;26:1386–1390. doi: 10.1016/j.bmcl.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 50.Cole S., Codling I.D., Parr W., Zabel T. Guidelines for Managing Water Quality Impacts within UK European Marine Sites. Volume 88 WRc Swindon Frankland Road Blagrove Swindon; Wiltshire, UK: 1999. UK Marine SACs Project. [Google Scholar]
- 51.Tomlin CDS . The Pesticide Manua. 10th ed. Royal Society of Chemistry; Cambridge, UK: British Crop Protection Council; London, UK: 1995. [Google Scholar]
- 52.Lee J., Hong S., Kim T., Lee C., An S.A., Kwon B.O., Lee S., Moon H.-B., Giesy J.-P., Khim J.S. Multiple bioassays and targeted and nontargeted analyses to characterize potential toxicological effects associated with sediments of masan bay: Focusing on AhR-mediated potency. Environ. Sci. Technol. 2020;54:4443–4454. doi: 10.1021/acs.est.9b07390. [DOI] [PubMed] [Google Scholar]
- 53.Chiaia-Hernández A.C., Scheringer M., Müller A., Stieger G., Wächter D., Keller A., Pintado-Herrera M.G., Lara-Martin P.A., Bucheli T.D., Hollender J. Target and suspect screening analysis reveals persistent emerging organic contaminants in soils and sediments. Sci. Total Environ. 2020;740:140181. doi: 10.1016/j.scitotenv.2020.140181. [DOI] [PubMed] [Google Scholar]
- 54.Cowan N., Keiser J. Repurposing of anticancer drugs: In vitro and in vivo activities against Schistosoma mansoni. Parasite Vect. 2015;8:417–426. doi: 10.1186/s13071-015-1023-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pujol E., Blanco-Cabra N., Julián E., Leiva R., Torrents E., Vázquez S. Pentafluorosulfanyl-containing triclocarban analogs with potent antimicrobial activity. Molecules. 2018;23:2853. doi: 10.3390/molecules23112853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Le P., Kunold E., Macsics R., Rox K., Jennings M.C., Ugur I., Reinecke M., Chaves-Moreno D., Hackl M.W., Fetzer C., et al. Repurposing human kinase inhibitors to create an antibiotic active against drug-resistant Staphylococcus aureus, persisters and biofilms. Nat. Chem. 2020;12:145–158. doi: 10.1038/s41557-019-0378-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Roberts J.L., Tavallai M., Nourbakhsh A., Fidanza A., Cruz-Luna T., Smith E., Siembida P., Plamondon P., Cycon K.A., Doern C.D., et al. GRP78/Dna K is a target for Nexavar/Stivarga/Votrient in the treatment of human malignancies, viral infections and bacterial diseases. J. Cell. Physiol. 2015;230:2552–2578. doi: 10.1002/jcp.25014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chang H.C., Huang Y.T., Chen C.S., Chen Y.W., Huang Y.T., Su J.C., Teng L.J., Shiau C.W., Chiu H.C. In vitro and in vivo activity of a novel sorafenib derivative SC5005 against MRSA. J. Antimicrob. Chemother. 2016;71:449–459. doi: 10.1093/jac/dkv367. [DOI] [PubMed] [Google Scholar]
- 59.Francisco G.D., Li Z., Albright J.D., Eudy N.H., Katz A.H., Petersen P.J., Labthavikul P., Singh G., Yang Y., Rasmussen B.A., et al. Phenyl thiazolyl urea and carbamate derivatives as new inhibitors of bacterial cell-wall biosynthesis. Bioorg. Med. Chem. Lett. 2004;14:235–238. doi: 10.1016/j.bmcl.2003.09.082. [DOI] [PubMed] [Google Scholar]
- 60.Jukič M., Hrast M., Patin D., Ogorevc E., Barreteau H., Gobec S. Virtual screening approach and biochemical evaluation on MurB. Chem. Data Collect. 2019;24:100276. doi: 10.1016/j.cdc.2019.100276. [DOI] [Google Scholar]
- 61.Hassan M.A., Sayed G.H., El-Nagar A.M., Hussien A.M. A convenient synthesis of some diarylurea and thiourea derivatives as antimicrobial compounds. Chem. Process Eng. Res. 2014;25:1–11. [Google Scholar]
- 62.Kim W., Zou G., Pan W., Fricke N., Faizi H.A., Kim S.M., Khader R., Li S., Lee K., Escorba L., et al. The neutrally charged diarylurea compound PQ401 kills antibiotic-resistant and antibiotic-tolerant Staphylococcus aureus. mBio. 2020;11:603. doi: 10.1128/mBio.01140-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sarveswari S., Vijayakumar V. A Facile Synthesis of diaylureas and their antimicrobial evaluation. Chiang Mai J. Sci. 2018;45:997–1007. [Google Scholar]
- 64.Pozzi C., Ferrari S., Cortesi D., Luciani R., Stroud R.M., Catalano A., Costi M.P., Mangani S. The structure of Enterococcus faecalis thymidylate synthase provides clues about folate bacterial metabolism. Acta Crystallogr. D Biol. Crystallogr. 2012;68:1232–1241. doi: 10.1107/S0907444912026236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gezegen H., Hepokur C., Tutar U., Ceylan M. Synthesis and Biological Evaluation of Novel 1-(4-(Hydroxy(1-oxo-1,3-dihydro-2H-inden-2-ylidene)methyl)phenyl)-3-phenylurea Derivatives. Chem. Biodivers. 2017;14:e1700223. doi: 10.1002/cbdv.201700223. [DOI] [PubMed] [Google Scholar]
- 66.Ceramella J., Mariconda A., Rosano C., Iacopetta D., Caruso A., Longo P., Sinicropi M.S., Saturnino C. α–ω Alkenyl-bis-S-guanidine thiourea dihydrobromide affects HeLa cell growth hampering tubulin polymerization. ChemMedChem. 2020 doi: 10.1002/cmdc.202000544. in press. [DOI] [PubMed] [Google Scholar]
- 67.Eissa I.H., Mohammad H., Qassem O.A., Younis W., Abdelghany T.M., Elshafeey A., Moustafa M.M.A.R., Seleem M.N., Mayhoub A.S. Diphenylurea derivatives for combating methicillin- and vancomycin-resistant Staphylococcus aureus. Eur. J. Med. Chem. 2017;130:73–85. doi: 10.1016/j.ejmech.2017.02.044. [DOI] [PubMed] [Google Scholar]
- 68.Mohammad H., Younis W., Ezzat H.G., Peters C.E., AbdelKhalek A., Cooper B., Pogliano K., Pogliano J., Mayhoub A.S., Seleem M.N. Bacteriological profiling of diphenylureas as a novel class of antibiotics against methicillin-resistant Staphylococcus aureus. PLoS ONE. 2017;12:e0182821. doi: 10.1371/journal.pone.0182821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Upadhayaya R.S., Kulkarni G.M., Vasireddy N.R., Vandavasi J.K., Dixit S.S., Sharma V. Chattapadhayaya, Design, synthesis and biological evaluation of novel triazole, urea and thiourea derivatives of quinoline against Mycobacterium tuberculosis. Bioorg. Med. Chem. 2009;17:4681–4692. doi: 10.1016/j.bmc.2009.04.069. [DOI] [PubMed] [Google Scholar]
- 70.Velappan A.B., Raja M.R.C., Datta D., Tsai Y.T., Halloum I., Wan B., Kremer L., Gramajo H., Franzblau S.G., Mahapatra S.K., et al. Attenuation of Mycobacterium species through direct and macrophage mediated pathway by unsymmetrical diaryl urea. Eur. J. Med. Chem. 2017;125:825–841. doi: 10.1016/j.ejmech.2016.09.083. [DOI] [PubMed] [Google Scholar]
- 71.Kocyigit-Kaymakcioglu B., Celen A.O., Tabanca N., Ali A., Khan S.I., Khan I.A., Wedge D.E. Synthesis and biological activity of substituted urea and thiourea derivatives containing 1,2,4-triazole moieties. Molecules. 2013;18:3562–3576. doi: 10.3390/molecules18033562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Caruso A., Ceramella J., Iacopetta D., Saturnino C., Mauro M.V., Bruno R., Aquaro S., Sinicropi M.S. Carbazole Derivatives as Antiviral Agents: An Overview. Molecules. 2019;24:1912. doi: 10.3390/molecules24101912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Micewicz E.D., Khachatoorian R., French S.W., Ruchala P. Identification of novel small-molecule inhibitors of Zika virus infection. Bioorg. Med. Chem. Lett. 2018;28:452–458. doi: 10.1016/j.bmcl.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 74.Khachatoorian R., Micewicz E.D., Micewicz A., French S.W., Ruchala P. Optimization of 1, 3-disubstituted urea-based inhibitors of Zika virus infection. Bioorg. Med. Chem. Lett. 2019;29:126626. doi: 10.1016/j.bmcl.2019.126626. [DOI] [PubMed] [Google Scholar]
- 75.Benmansour F., Trist I., Coutard B., Decroly E., Querat G., Brancale A., Barral K. Discovery of novel dengue virus NS5 methyltransferase non-nucleoside inhibitors by fragment-based drug design. Eur. J. Med. Chem. 2017;125:865–880. doi: 10.1016/j.ejmech.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 76.Jiang S., Prigge S.T., Wei L., Gao Y.E., Hudson T.H., Gerena L., Dame J.B., Kyle D.E. New class of small non peptidyl compounds blocks plasmodium falciparum development in vitro by inhibiting plasmepsins. Antimicrob. Agents Chemother. 2001;45:2577–2584. doi: 10.1128/AAC.45.9.2577-2584.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Anderson J.W., Sarantakis D., Terpinski J., Kumar T.S., Tsai H.C., Kuo M., Ager A.L., Jacobs Jr W.R., Schiehser G.A., Ekins S., et al. Novel diaryl ureas with efficacy in a mouse model of malaria. Bioorg. Med. Chem. Lett. 2013;23:1022–1025. doi: 10.1016/j.bmcl.2012.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Obukowicz M.G., Welsch D.J., Salsgiver W.J., Martin-Berger C.L., Chinn K.S., Duffin K.L., Raz A., Needlemann P. Novel, selective Δ6 or Δ5 fatty acid desaturase inhibitors as antiinflammatory agents in mice. J. Pharmacol. Exp. Ther. 1998;287:157–166. doi: 10.1007/BF02562269. [DOI] [PubMed] [Google Scholar]
- 79.Miyahisa I., Suzuki H., Mizukami A., Tanaka Y., Ono M., Hixon M.S., Matsui J. T-3364366 targets the desaturase domain of delta-5 desaturase with nanomolar potency and a multihour residence time. ACS Med. Chem. Lett. 2016;7:868–872. doi: 10.1021/acsmedchemlett.6b00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Keche A.P., Hatnapure G.D., Tale R.H., Rodge A.H., Kamble V.M. Synthesis, anti-inflammatory and antimicrobial evaluation of novel 1-acetyl-3,5-diaryl-4,5-dihydro(1H)pyrazole derivatives bearing urea, thiourea and sulfonamide moieties. Bioorg. Med. Chem. Lett. 2012;22:6611–6615. doi: 10.1016/j.bmcl.2012.08.118. [DOI] [PubMed] [Google Scholar]
- 81.Rakesh K.P., Darshini N., Vidhya S.L., Mallesha N. Synthesis and SAR studies of potent H+/K+-ATPase and anti-inflammatory activities of symmetrical and unsymmetrical urea analogues. Med. Chem. Res. 2017;26:1675–1681. doi: 10.1007/s00044-017-1878-x. [DOI] [Google Scholar]
- 82.Pietronigro E., Zenaro E., Della Bianca V., Dusi S., Terrabuio E., Iannoto G., Slanzi A., Gasemi S., Nagarajan R., Piacentino G., et al. Blockade of α4 integrins reduces leukocyte–endothelial interactions in cerebral vessels and improves memory in a mouse model of Alzheimer’s disease. Sci. Rep. 2019;9:1–15. doi: 10.1038/s41598-019-48538-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Taooka Y., Ohe M., Tada M., Sutani A., Isobe T. Up-regulated integrinα4β1 on systemic lymphocytes and serum IL-17 A in interstitial pneumonia. Clin. Respir. J. 2016;10:722–730. doi: 10.1111/crj.12277. [DOI] [PubMed] [Google Scholar]
- 84.Manfredi A., Luppi F., Cassone G., Vacchi C., Salvarani C., Sebastiani M. Pathogenesis and treatment of idiopathic and rheumatoid arthritis-related interstitial pneumonia. The possible lesson from COVID-19 pneumonia. Exp. Rev. Clin. Immunol. 2020;16:751–770. doi: 10.1080/1744666X.2020.1803064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Astles P.C., Clark D.E., Collis A.J., Cox P.J., Eastwood P.R., Harris N.V., Lai J.Y.Q., Morley A.D., Porter B. Substituted Anilines. 6,479,519. U.S. Patent. 2002 Nov 12;
- 86.Witherington J., Bordas V., Gaiba A., Green P.M., Naylor A., Parr N., Smith D.G., Takle A.K., Ward R.W. Pyridone derivatives as potent and selective VLA-4 integrin antagonists. Bioorg. Med. Chem. Lett. 2006;16:2256–2259. doi: 10.1016/j.bmcl.2006.01.025. [DOI] [PubMed] [Google Scholar]
- 87.Hernandez-Cervantes R., Mendez-Diaz M., Prospero-Garcia O., Morales-Montor J. Immunoregulatory role of cannabinoids during infectious disease. Neuroimmunomodulation. 2017;24:183–199. doi: 10.1159/000481824. [DOI] [PubMed] [Google Scholar]
- 88.Horswill J.G., Bali U., Shaaban S., Keily J.F., Jeevaratnam P., Babbs A.J., Reynet C., Wong Kai In P. PSNCBAM-1, a novel allosteric antagonist at cannabinoid CB1 receptors with hypophagic effects in rats. Br. J. Pharmacol. 2009;152:805–814. doi: 10.1038/sj.bjp.0707347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Khurana L., Fu B.-Q.Q.B., Duddupudi A.L., Liao Y.-H.H., Immadi S.S., Kendall D.A., Lu D. Pyrimidinyl biphenylureas: Identification of new lead compounds as allosteric modulators of the cannabinoid receptor CB1. J. Med. Chem. 2017;60:1089–1104. doi: 10.1021/acs.jmedchem.6b01448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dopart R., Immadi S.S., Lu D., Kendall D.A. Structural optimization of the diarylurea PSNCBAM-1, an allosteric modulator of Cannabinoid receptor 1. Curr. Ther. Res. 2020;92:100574. doi: 10.1016/j.curtheres.2019.100574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sriram K., Insel P.A. Inflammation and thrombosis in COVID-19 pathophysiology: Proteinase-activated and purinergic receptors as drivers and candidate therapeutic targets. Physiol. Rev. 2020 doi: 10.1152/physrev.00035.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chao H., Turdi H., Herpin T.F., Roberge J.Y., Liu Y., Schnur D.M., Poss M.A., Rehfuss R., Hua J., Wu Q., et al. Discovery of 2-(phenoxyaryl)-3-phenylureas as small molecule P2Y1 antagonists. J. Med. Chem. 2013;56:1704–1714. doi: 10.1021/jm301708u. [DOI] [PubMed] [Google Scholar]
- 93.Zhang D., Gao Z.-G., Zhang K., Kiselev E., Crane S., Wang J., Paoletta S., Yi C., Ma L., Zhang W., et al. Two disparate ligand-binding sites in the human P2Y1 receptor. Nature. 2015;520:317–321. doi: 10.1038/nature14287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang T.C., Qiao J.X., Clark C.G., Jua J., Price L.A., Wu Q., Chang M., Zheng J., Huang C.S., Everlof G., et al. Discovery of diarylurea P2Y1 antagonists with improved aqueous solubility. Bioorg. Med. Chem. Lett. 2013;23:3239–3243. doi: 10.1016/j.bmcl.2013.03.125. [DOI] [PubMed] [Google Scholar]
- 95.Peng J., Zhao L., Wang L., Chen H., Qiu Y., Wang J., Yang H., Liu J., Liu H. Design, synthesis, and biological evaluation of 2-(phenoxyaryl)-3-urea derivatives as novel P2Y1 receptor antagonists. Eur. J. Med. Chem. 2018;158:302–310. doi: 10.1016/j.ejmech.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 96.Qiao J.X., Wang T.C., Ruel R., Thibeault C., L’Heureux A., Schumacher W.A., Spronk S.A., Hiebert S., Bouthillier G., Lloyd J., et al. Conformationally constrained orthoanilino diaryl ureas, discovery of 1-(2-(10-neopentylspiro[indoline-3,40-piperidine]-1-yl)phenyl)-3-(4-(trifluoro-methoxy) phenyl)urea, a potent, selective, and bioavailable P2Y1 antagonist. J. Med. Chem. 2013;56:9275–9295. doi: 10.1021/jm4013906. [DOI] [PubMed] [Google Scholar]
- 97.Jeon Y.T., Yang W., Qiao J.X., Li L., Ruel R., Thibeault C., Hiebert S., Wang T.C., Wang Y., Liu Y., et al. Identification of 1-{2-[4-chloro-1′-(2,2-dimethylpropyl)-7-hydroxy-1,2-dihydrospiro[indole-3,4′-piperidine]-1-yl]phenyl}-3-{5-chloro-[1,3]thiazolo [5,4-b]pyridin-2-yl}urea, a potent, efficacious and orally bioavailable P2Y1 antagonist as an antiplatelet agent. Bioorg. Med. Chem. Lett. 2014;24:1294–1298. doi: 10.1016/j.bmcl.2014.01.066. [DOI] [PubMed] [Google Scholar]
- 98.Qiao J.X., Wang T.C., Hiebert S., Hu C.H., Schumacher W.A., Spronk S.A., Clark C.G., Han Y., Hua J., Price L.A., et al. 4-Benzothiazole-7-hydroxyindolinyl diaryl ureas are potent P2Y1 antagonists with favorable pharmacokinetics: Low clearance and small volume of distribution. ChemMedChem. 2014;9:2327–2343. doi: 10.1002/cmdc.201402141. [DOI] [PubMed] [Google Scholar]
- 99.Mishra C.B., Kumari S., Tiwari M. Design and synthesis of some new 1-phenyl-3/4-[4-(aryl/heteroaryl/alkyl-piperazine1-yl)-phenyl-ureas as potent anticonvulsant and antidepressant agents. Arch. Pharmacal Res. 2016;39:603–617. doi: 10.1007/s12272-016-0720-1. [DOI] [PubMed] [Google Scholar]
- 100.Carnevale V., Rohacs T. TRPV1: A target for rational drug design. Pharmaceuticals. 2016;9:52. doi: 10.3390/ph9030052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Feng Z., Pearce L.V., Zhang Y., Xing C., Herold B.K., Ma S., Hu Z., Turcios N.A., Yang P., Tong Q., et al. Multi-functional diarylurea small molecule inhibitors of TRPV1 with therapeutic potential for neuroinflammation. AAPS J. 2016;18:898–913. doi: 10.1208/s12248-016-9888-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kurt B.Z., Gazioglu I., Basile L., Sonmez F., Ginex T., Kucukislamoglu M., Guccione S. Potential of aryl–urea–benzofuranylthiazoles hybrids as multitasking agents in Alzheimer’s disease. Eur. J. Med. Chem. 2015;102:80–92. doi: 10.1016/j.ejmech.2015.07.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is contained within the article.


