Summary
The COVID-19 outbreak has already become a global pandemic and containing this rapid worldwide transmission is of great challenge. The impacts of temperature and humidity on the COVID-19 transmission rate are still under discussion. Here, we elucidated these relationships by utilizing two unique scenarios, repeated measurement and natural experiment, using the COVID-19 cases reported from January 23 – February 21, 2020, in China. The modeling results revealed that higher temperature was most strongly associated with decreased COVID-19 transmission at a lag time of 8 days. Relative humidity (RH) appeared to have only a slight effect. These findings were verified by assessing SARS-CoV-2 infectivity under the relevant conditions of temperature (4°C–37°C) and RH (> 40%). We concluded that temperature increase made an important, but not determined, contribution to restrain the COVID-19 outbreak in China. It suggests that the emphasis of other effective controlling polices should be strictly implemented to restrain COVID-19 transmission in cold seasons.
Graphical Abstract
Public Summary
-
•
Temperature increase was associated with restrained transmission of COVID-19 on the Chinese Mainland
-
•
The above association was estimated to be strongest when the lag time from SARS-CoV-2 infection to the official confirmation report was 8 days
-
•
In geographical regions without central heating, temperature increase had a stronger effect on restraining COVID-19 transmission
-
•
Cellular infectivity experiment results indicated that higher temperature decreased the half-life of SARS-CoV-2
-
•
We provided integrated information to confirm the independent inhibiting effect of temperature on COVID-19 transmission
Introduction
Global transmission of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is occurring on an unprecedented scale. The spread of confirmed cases has been sufficiently substantial that the event has already been declared a pandemic event. Controlling this rapid worldwide transmission is an imminent challenge. SARS-CoV-2 has gene sequences identical to those of SARS-CoV with more than 79.6% similarity.1 In addition, its environmental stability is similar to that of the two other β-coronaviruses of SARS-CoV and MERS-CoV. For example, the half-lives of SARS-CoV-2 in aerosols and on surfaces of various materials are generally comparable with those of SARS-CoV.2 Low temperature and low humidity favor the survival of both SARS-CoV and MERS-CoV.3,4 Sajadi et al.5 depicted a pattern of significantly high community transmission in countries coincidentally located in similar latitudes in the Northern Hemisphere (e.g., China, Iran, France, Italy, and the USA), which is linked with certain ranges of temperature (3°C–17°C) and absolute humidity (4–9 g/m3).6 Until now, the implication of COVID-19 transmission in view of fluctuating temperature and humidity is somewhat uncertain, but pertinent scientific questions need to be answered, not only for scientists but also, and more importantly, for the public and policymakers.
An experimental study indicated that the SARS-CoV-2 virus has multi-factorial immune responses similar to those of the avian H7N9 disease.7 It is well established that the transmission trend of influenza viruses (e.g., H1N1 and H7N9) depends greatly on the season.8 However, until now, very little solid information has been available about the effects of temperature and humidity on the transmission rate of SARS-CoV-2, and this is also true for the previous SARS-CoV and MERS-CoV coronaviruses. We are aware of several studies on the association of temperature or humidity with the modulation of COVID-19 transmission in peer-reviewed journals or preprint websites of MedRxiv, BioRxiv, and SSRN. Most of them showed that increase in temperature or humidity may reduce transmission rates of COVID-19 on both regional and global scales.9, 10, 11, 12, 13, 14 Some other studies may have found the opposite phenomenon. For example, it has been reported that there was no dependence of the rate of spread of the COVID-19 pandemic on temperature.15 Oliveiros et al.16 pointed out that the transmission rate correlates positively with relative humidity. However, the latter claim is not consistent with the overall distribution characteristics of COVID-19,6,17 nor previous environmental stability test results on SARS-CoV and MERS-CoV.3,4 Soon after the Wuhan lockdown on January 23, 2020, localized COVID-19 cases, with minimal chances of intrusion from other areas, were examined by Luo et al.18; however, some other important potential confounders, especially those pertaining to heterogeneities among cities in China or around the world (e.g., availability of medical treatment in various cities, population mobility), incubation period, and meteorological differences between indoor and outdoor environments, were not well controlled. The same limitations also exist in the other aforementioned studies.6,9, 10, 11, 12, 13, 14, 15, 16, 17,19 Provisioning of concrete evidence is therefore imperative. Based on current knowledge of the transmission characteristics of SARS-CoV-2, we proposed a hypothesis that both temperature and relative humidity can modulate the spread of COVID-19. To evaluate the causal effects of temperature and humidity on COVID-19 transmission, it is crucial to select an appropriate scenario in which important confounders can be controlled, and validate the relevant results with certain intervention evidence.
Results and Discussion
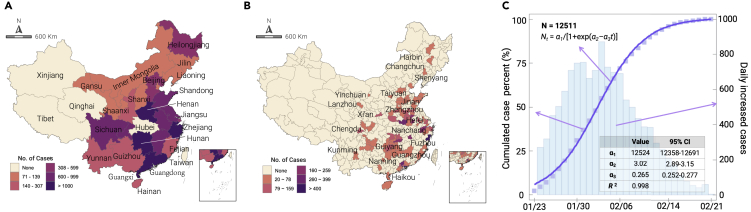
We explored the relationships between the COVID-19 transmission rate and the relevant meteorological factors using the following four steps. First, we developed the relationship between daily cumulative increase of COVID-19 cases and time. After excluding cluster infection events (such as a cluster infection occurring in a prison) (Table S1), we found a tangible increase in the daily cumulative cases following a three-parameter logistic model for all geographic units under consideration for the selected 27 provinces and 99 cities (Table S2), the geographical information of which is provided in Figures 1A and 1B. For the 27 provinces, the increasing trends of cumulative COVID-19 cases with time were fitted by Equation (1) with high R2 > 0.97 (see Figure S1). Here, we only show the increasing trend of the total COVID-19 cases from the 27 provinces, which could be fitted well with R2 = 0.998 (see Figure 1C).
Figure 1.
Cummulated Confirmed Cases of COVID-19 and Its Geographic Distribution
The geographic distribution of the total confirmed COVID-19 cases in the 27 provinces (A) and 99 cities (B) included from January 23 to February 21, 2020; only the large typical cities were marked for readers' convenience. (C) The increasing trend of total COVID-19 cases from the 27 provinces. Cumulated confirmed case percent during that period is shown as scatters and fitting curve, corresponding to the left Y-axis. Daily increased cases are shown as vertical bars, corresponding to the right Y-axis. Total confirmed cases (N) of the 27 provinces as of February 21 was 12,511. The parameters of the fitted curve are shown in the table inserted in (C).
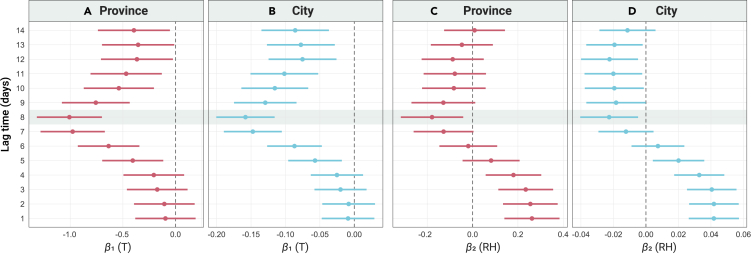
Second, we explored the associations of environmental temperature and relative humidity with transmission rate. The mean (minimum–maximum) ambient temperature and relative humidity in selected regions were 3.85°C (−27.17°C–24.47°C) and 79.66% (27.25%–100%) during the relevant period. The linear mixed model results showed that the transmission rate had an apparent association with temperature or relative humidity, which varied with the lag time (denoted LT), with a U-shaped relationship (Figure 2). At either the province or city level (Figures 2A and 2B), an overall broadly negative association was recorded between outdoor temperature and transmission rate when LT ≥ 5 days, and the above association (i.e., the absolute value of regression coefficients of β1) was observed to be strongest when LT = 8 days, as highlighted by the gray rectangle. For relative humidity at the city level, a negative association with transmission rate was found when LT ≥ 8 days. At the province level, however, a statistically significant association between these was observed only when LT = 8 days (Figure 2C), which was not consistent with the results at the city level (Figure 2D). The sensitive analyses results (Figures S5 and S6) indicated that the above associations were overall consistent when mobility index was excluded from the model, or the event-based information was not corrected according to Table S1. We also confirmed the sensitivity of β1 to the confounders of wind speed, precipitation, population mobility indexes, and population density (Figure S7). It seemed that the precipitation and mobility indexes had obvious effects on β1, while the population density and wind speed had negligible effects. However, the overall results were consistent under the condition of excluding any of them. We further analyzed the interactive effects between temperature and relative humidity on the transmission rate of COVID-19 (see Table S3). No such effects were observed between them at either the province or city level, nor were effects observed with or without public central heating. It seemed that relative humidity did not have any modifying effects with temperature on the transmission rate. Therefore, the effect of relative humidity on the transmission rate is not analyzed in the following.
Figure 2.
Ambient Temperature & Relative Humidity and COVID-19 Transmission
Associations of ambient temperature (A, province level; B, city level) and relative humidity (C, province level; D, city level) with the transmission rate of COVID-19. Transmission rate was defined as the increased rate of cumulated confirmed cases per day in a logistic growth model: Equation (1). The regression coefficients (β1 and β2) were obtained using a linear mixed-effect model as follows: R[t, s]= β1Tt+ β2RHt+ β3WSt + β4PRt+ β5MIIt+ β6MOIt+ β7PDt + γ(L). This formula incorporated seven fixed terms (β1-7) to model the effects of temperature (T), relative humility (RH), wind speed (WS), precipitation (PR), population mobility indexes of moving-in (MII) and moving-out (MOI), population density (PD), and a random intercept (γ) to control for the location (L)-specific effects. Data are shown with an estimated value with 95% confidence interval.
Shi et al.20 reported that a lag period of meteorological conditions on COVID-19 transmission may exist among the population, which included the entire time from case infection with SARS-CoV-2 to the day when the infection confirmation information was reported on the official website. Using the distributions of incubation time21 and report interval,22 the estimated LT value was 10.0 (interquantile range: 6.3–14.8) days (Figure S8). For incubation time, another study reported a median incubation period, from as many as 1,099 confirmed cases, of 3 days,23 which was about 2 days less than the median incubation time of 5.1 days used in our study.21 In addition, the report interval was estimated based on national data, i.e., including Hubei Province, China,22 which should be larger than those of other provinces because Hubei Province had limited medical resources during the period of rapid increase after January 23, 2020. Thus, the practical LT value of the other regions, except for Hubei Province, in China should have been smaller than the 10-day interval estimated from these data. Our modeling results revealed that the most probable LT value was 7 or 8 days, which was reasonable when considering the time estimate based on published studies.
With regard to temperature, we found that there seemed to be a strong inhibitory effect on the transmission rate of COVID-19, which is consistent with the results of studies published in peer-reviewed or posted on preprint websites.6,9, 10, 11, 12, 13, 14,16, 17, 18, 19,24 Regarding relative humidity, a significant protective effect on COVID-19 transmission at the province level was found only when LT = 8 days, whereas a significant inhibiting effect at the city level was observed when LT = 8–13 days. Therefore, the effect of relative humidity does not appear to be stable like that of temperature, but it may account for a trivial inhibitory effect on the spread of COVID-19 based on our current data analysis. Moreover, the above-mentioned studies did not consider the lag period of environmental factors on the transmission rate. The lag time is the crucial parameter to link the meteorological conditions to the spreading rate of COVID-19 because there is a latent period between SARS-COV-2 infection and syndrome onset.
When LT = 8, we did not find any interactive effect between temperature and humidity on transmission rate. It had been proposed that the optimal temperature and relative humidity for COVID-19 transmission may be less than 5°C–11°C and 47%–79%, respectively.17 In our study, more than half of the areas screened during the study period had a high relative humidity of more than 80% (Figures S2 and S3). Our study indicated that there was very slight inhibitory effect of relative humidity on transmission rate. Further studies need to be conducted to assess the effect of the coming monsoon in some Asian regions. In the sensitivity analyses, we found the confounders of precipitation and population mobility, but not population density or wind speed, had a significant effect on the value of β1, which was not consistent with the study of Islam et al.24 One possible explanation is that the virus shed by COVID-19 cases can be removed by rain. In addition, outdoor activities should decrease during rainy weather, resulting in a diminished chance of population infection by contacts.
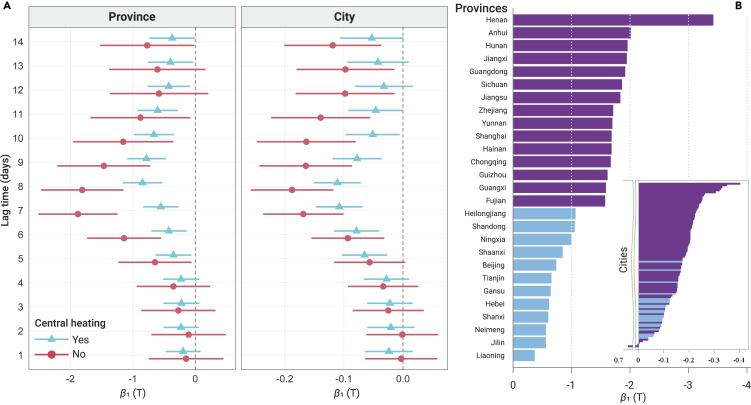
Third, we also chose a natural experiment scenario to verify the effect of temperature. It has been reported that the population of China overall spends 83% of time indoors.25 Therefore, the outdoor temperature cannot represent the real ambient environmental living conditions for those with public central heating. If an effect of a meteorological variable on transmission rate existed, the maintenance of different household temperatures could strengthen or weaken the association, which can be verified by adding an interaction term of temperature or relative humidity with public central heating status. Here, a significant modification effect of public central heating status on the association between temperature and transmission rate (p < 0.05) was observed when LT = 5–10 days (Figure 3A). For areas without public central heating, the decrease of transmission rate seemed larger than for areas with public central heating at both the province and city levels. The most obvious coefficient (β1) was also found when LT = 7 or 8 days. These associations were consistent overall without adjusting the mobility indexes (Figure S9). Here, two views can be promulgated. The first is that the outdoor temperature is less likely to be consistent with the actual living conditions of the population residing in northern China, which might have caused a relatively low transmission rate depending on the outdoor temperature in northern China compared with that in southern China. The second view highlights the nature of the heating facilities, which is public central heating and shared among populations confined within geographic units, with limited mobility, thus creating a condition that may trigger further changes in transmission rate. Nevertheless, this natural experiment scenario, which was not documented in previously reported studies, is highly relevant to validation of our findings related to temperature effects. This suggests a decisive role of temperature control as an efficient phenomenon in the regulation of COVID-19 transmission rate in residential environments over large areas. We subsequently compared the variance of β1 among the relevant provinces and cities (Figure 3B), and the detailed data are provided in Table S4. Overall, higher magnitudes of change of transmission rate with temperature were found in the provinces or cities in southern China (e.g., the top five provinces were Henan, Anhui, Hunan, Jiangxi, and Guangdong) than in those in northern China (e.g., the last five were Liaoning, Jilin, Inner Mongolia, Shanxi, and Hebei). The nonlinear relationship between ambient temperature and COVID-19 transmission is shown in Figure S10 when LT = 8 days. It seemed that their relationship was close to being linear, but a temperature threshold was not found. When assuming that Tref was the 1-week average temperature around the date of LT earlier than January 23, 2020, the dependence of the reduction in COVID-19 cases with LT (ΔNM) was estimated taking into consideration of the geographic variance of the effect of temperature on the transmission rate. During the relevant period, we estimated that there were about 4,066 persons who were not affected by SARS-CoV-2 due to the temperature increase when LT = 8 days. The detailed results of ΔNM of other lag times are shown in Table S5. In this natural experiment scenario, the distribution of central heating is not randomly distributed in China, i.e., only some northern provinces with very low temperature during the winter season have municipally supplied central heating, while the southern provinces do not. This allows us to conduct the stratification analysis by using the public central heating status.
Figure 3.
Modification Effect of the Central Heating Status
Modification effect of the central heating status on the association of ambient temperature with the transmission rate of COVID-19 (A) and geographic variances of the effects of temperature on the transmission rate when LT = 8 days (B). Transmission rate was defined as the increased rate of cumulated confirmed cases per day in a logistic growth model: Equation (1). The regression coefficient (β1) was obtained using a linear mixed-effect model as follows: R[t, s]= β1Tt+ β2RHt+ β3WSt + β4PRt+ β5MIIt+ β6MOIt+ β7PDt + γ(L). This formula incorporated seven fixed terms (β1-7) to model the effects of temperature (T), relative humility (RH), wind speed (WS), precipitation (PR), population mobility indexes of moving-in (MII) and moving-out (MOI), population density (PD), and a random intercept (γ) to control for the location (L)-specific effects. For (A), the data are shown with an estimated value with a 95% confidence interval. For (B), the geographic areas with central heating are indicated in blue and those without in purple.
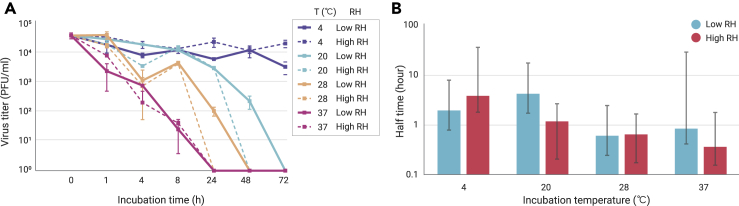
Fourth, we utilized virus persistence experiments to test the effects of temperature and relative humidity on SARS-CoV-2 infectivity. The residual viral infectivity was titrated at different time points (Figure 4A). We found that the titer decrease mainly occurred in the first 4 h after the first-order decay trend, of which the half times were calculated (Figure 4B). The detailed viral titer at each time point is given in Table S6. There was a decreasing trend of half-time with incubation temperature (ANOVA test p < 0.05), especially under high humidity conditions. Pairwise comparison results also indicated that significant differences were observed at 20°C versus 28°C under low relative humidity conditions, 4°C versus 37°C and 20°C versus 37°C under high relative humidity condition (Tukey adjusted p < 0.05), respectively. At 4°C, SARS-CoV-2 maintained a high residual titer, even up to 72 h, with ∼4 Log10PFU/mL. The reduction was more dramatic when the temperature exceeded 28°C and almost no live virus could be observed after 24 h incubation (Figure 4A). Under both low and high relative humidity conditions, the trends of residual titers (Log10PFU/mL) of SARS-CoV-2 were similar. For the half times during the first 4 h, we only observed a significant difference between high and low relative humidity at 20°C (Tukey’s adjusted p < 0.05).
Figure 4.
Environmental Persistence of SARS-CoV-2
The viability of SARS-CoV-2 under various temperature conditions (4°C, 20°C, 28°C, and 37°C) and relative humidity (RH) (low [L]: 40%–60%; high [H] > 99%) with time (0, 1, 4, 8, 24, and 48 h) on the surface of gauze cloth (A) and their half time of decay (B). The initial titer of the working virus solution was approximately 4.56 Log10(PFU)/mL. (A) The experiments were conducted in replicates and the mean values and standard error of virus titer are shown. (B) The half-time was calculated according to the first 4-h virus viability and the 95% confidence interval was added as the error bar. The differences between the two groups were compared by Tukey's honestly significant difference pairwise comparison test.
The laboratory experimental study provides a more ideal scenario by controlling other confounders. While the modeling study, conducted based on the daily confirmed cases and meteorological data, reflects an uncontrolled but real-life situation. Although it is difficult to harmonize the related findings from these two approaches, they both can contribute to explain the effects of temperature and humidity on the transmission rate of SARS-CoV-2.26 Previous studies showed that the infectivity of SARS-CoV significantly decreased with increase in temperature from 28°C to 38°C and decreased more rapidly from 35°C to 38°C.3 MERS-CoV was shown to be more stable at low temperature/low humidity conditions. Our results, implying that the coronavirus is more stable at lower temperatures, especially at 4°C, were consistent with previous results. However, relative humidity plays different roles with regard to these viruses. A strong inhibitory effect of humidity on infectivity of SARS-CoV was found mainly when the temperature was >28°C.3 MERS-CoV was more stable at low humidity conditions, but no relative humidity effect on stability was observed for SARS-CoV-2. However, in a previous study, only three experimental conditions of temperature and relative humidity (i.e., 20°C and 40%, 30°C and 30%, and 30°C and 80%) were chosen, and these could not facilitate analysis of any independent effect of temperature or relative humidity.4 Our study included relatively more exposure conditions of temperature by referring to the ambient environments in the study regions during the study period. To our surprise, SARS-CoV-2 could maintain high infectivity at 4°C even after 72 h (3 days). However, the residual infectivity decreased dramatically when the temperature exceeded 20°C. Another study investigated the stability of SARS-CoV-2 on cloth at room temperature (22°C) and a relative humidity (∼65%) with the initial titer (4.84 Log10TCID50/mL), which was comparable with one of the conditions in our study where the room temperature was 20°C and relative humidity was around 40%–60% with an initial titer of 4.56 Log10PFU/mL. Overall, the decay rate in our study was relatively lower than that on cloth,27 but it cannot be well explained using the current data. The choice of the materials may cause different results between studies, which needs confirmation in further studies. Compared with temperature, relative humidity seemed to have a weak effect on the stability of SARS-CoV-2. In a previous infectivity study, it was reported that the viability of SARS-CoV-2 significantly decreased with increase of relative humidity from 20% to 60%, but not from 60% to 80%.28 Our study further showed the dependence of SARS-CoV-2 infectivity on relative humidity from 40%–60% to 100%. Among the included cities, the relative humidity mostly ranged from 60% to 95%. This can partly explain our modeling findings to a certain extent. However, one must be aware that social distancing between susceptible persons is important in addition to the change of virus stability. Our study provided very comprehensive experimental results pertaining to the stability of SARS-CoV-2 under ambient conditions of temperature and relative humidity.
Some previous studies have indicated nonlinear associations between respiratory infections (e.g., influenza) and the year-round temperature range.29 However, because the COVID-19 epidemic was mostly well controlled in most regions of the Chinese Mainland, we cannot conduct a comparison study between the winter and summer seasons to provide more solid evidence. Our study only focused on our hypotheses at the limited range of meteorological conditions, which makes it difficult to extrapolate our results to more broad temperature ranges. The results obtained through our model were based on only a portion of the regions on Mainland China. Extrapolation of our results into areas with different geographical conditions should be done with care. Even within China, a stronger effect of temperature on COVID-19 transmission rate was observed in the southern regions. We did not take family-cluster infections into account, which might bias our results. We also did not consider the asymptomatic COVID-19 infection cases32 due to limited data. Further studies are still needed to investigate the relationship between asymptomatic infection and transmission of COVID-19. Our virus persistence experiments only utilized gauze with suspended virus in working solution to investigate the relationship between SARS-CoV-2 infectivity and environmental temperature and humidity, which can only represent the real environment to a certain extent and the related results should be extrapolated with care. Nevertheless, the findings presented here have some advantages due to their demonstration of the effects of temperature and humidity on the transmission of COVID-19 in practical living scenarios in combination with the results of environmental stability for SARS-CoV-2. First, prevention and control policies in China can be executed simultaneously and forcefully in the province of concern. After January 23, 2020, there were only sporadic imported cases from Hubei Province in other cities. From the sensitivity analysis, we found that the model results were consistent with or without modification of imported and cluster infection cases. Second, the effects of temperature and humidity were investigated using a quasi-repeated measurement study followed by a linear mixed-effect model to control, to some extent, the differences among various regions in medical availability and executive force following the prevention and control plan issued by the National Health Commission (NHC) in China. Third, we adopted a natural experiment by using the public central heating status, which could significantly distinguish the intervention effect of temperature and humidity in the living environment. Fourth, the LT values, due to their lag effect on the transmission rate, were reasonably estimated at 7 or 8 days. It is crucial for us to estimate the relatively accurate effect of temperature on transmission rate. Finally, to the best of our knowledge, this is the first investigation to examine the effects of temperature and relative humidity on SARS-CoV-2 using a cellular experiment. Overall, the cellular infectivity results provided considerable supportive evidence for our modeling results.
Conclusions
Based on the results from the modeling and environmental stability analysis of SARS-CoV-2, we finally highlighted an emerging trend that increase in ambient temperature, irrespective of relative humidity, had a strong influence on restraining the transmission rate of COVID-19 in China. For the cold seasons, the emphasis on social distancing should be strictly implemented to restrain COVID-19 transmission. Still, we need other efficient prevention and control measures to entirely halt COVID-19 transmission.
Materials and Method
Information of Confirmed COVID-19 Cases
Numbers of daily confirmed cases for all of the Chinese cities or provinces of concern, during the period of January 23 to February 21, 2020, were collected from official reports on the website of the National Health Commission (NHC) or Provincial Health Commission (PHC) of China. Confirmed cases were defined as suspected cases with a positive test result for viral nucleic acid. In some cases, the Chinese NHC or PHC might have reported the “wrong” number of confirmed cases (but they made correction reports the following day); in such a situation, we would calculate “negative increase case number.” Another situation existed when aggregation infection events occurred, the striking increase of which was obviously caused by close contact and confirmed by a rapid concentrated virus nucleic acid test. We denoted both situations as “abnormal data” (a detailed description is given in Table S1). A sensitivity analysis was conducted to compare the key findings with and without correction of the abnormal data. The data of daily increased COVID-19 cases, with and without corrections, are provided in Data S1. In addition, there were no imported cases from abroad.
Mobility Data, Population Density, Temperature, and Relative Humidity
A human mobility index from the Baidu Company was used to indicate individual movement among the provinces or cities of concern in our simulation study (see: http://qianxi.baidu.com/). The data were collected using the application program interface from the platform, and the information is given in Data S2. Population density was calculated by using 2017 census data in China at the county level. The daily averages of temperature and relative humidity were collected from the National Centers for Environmental Prediction (NCEP) reanalyzed climate database provided by the NOAA/OAR/ESRL PSD, Boulder, Colorado, USA. The data can be accessed freely from their website: https://www.esrl.noaa.gov/psd/. The product was based on a state-of-the-art data assimilation approach, which combined in situ observations with climate forecast results. We obtained the meteorological data in the two pixels that covered the city areas, and aggregated them into one daily time series for each variable. Their spatial resolution was 2.5° × 2.5°. The original data were obtained using the R package “RNCEP.” The information included geographic distributions of average temperature and relative humidity (Figure S2), as well as the daily changes in temperature and relative humidity (Figure S3), at both the province and city levels. The information is included in Data S3.
Study Area and Duration
Since January 23, 2020, travel restrictions had been implemented for Wuhan. Intervention in the COVID-19 transmission rate of Hubei Province was exceptional because of the strong control policies; complex local situations also played a part. We therefore excluded regions of Hubei Province from this study. In total, 29 provinces or regions in Mainland China, as well as their 461 cities, were originally included in our model. For the geographic units of concern, we further excluded units with cumulative confirmed COVID-19 cases <20, and the fitting coefficient of determination (R2) was ≤0.97. For example, the two provinces of Tibet and Qinghai were excluded due to their small numbers of COVID-19 cases. The fitting results are displayed in detail in Figure S1. During the second (announced on January 23, 2020) and fifth (announced on February 22, 2020) versions of the COVID-19 prevention and control plan from the Chinese NHC, the outbreak of COVID-19 in China had two main stages: a phase with rapid increase and a stationary phase. Moreover, during this period there seemed to be no obvious trend of warming, which may slightly bias our analyses results (See Figure S3). Therefore, we chose the period from January 23 to February 21, 2020, for data analysis. During this time, all of the provinces simultaneously implemented the NHC prevention and control plan with high executive force, as monitored by the central government inspection team.
Model Design
We first derived the daily infection transmission rate of COVID-19 for each geographic unit using a logistic growth model. The daily count of COVID-19 cases in each region (N[t, s]) was assumed to increase with time (t), following a nonlinear curve, pre-determined by three parameters. The model can be specified as follows:
| N[t, s] = α1/[1 + exp(α2 – α3t)], | (Equation 1) |
where α1, α2, and α3 are tuning parameters and can be estimated by finding the minimum of the residual sum of squares of the model. Therefore, the daily transmission rate (R[t, s]) of COVID-19 at time t in region s is the first derivative of Equation (1), which can be calculated as follows:
| R[t, s] = α1/[1 + exp(α2 – α3t)]2 × exp(α2 – α3t) × α3. | (Equation 2) |
Given differences in social distances, control policies, and many other aspects for each geographic unit, we fitted a logistic growth model and calculated a time series of daily transmission rate of [R1, R2, …, RD] for the duration of concern of D days in each region. The cumulative number of daily increased COVID-19 cases is equal to ΣNt (noted as N). We then explored the relationship between the daily transmission rate and the independent variables of concern using a linear mixed-effect model, specified as follows:
| R[t, s]= β1Tt+ β2RHt+ β3WSt + β4PRt+ β5MIIt+ β6MOIt+ β7PDt + γ(L). | (Equation 3) |
The model incorporated seven fixed terms with coefficients of β1–7 to model the effects of the four meteorological factors of temperature (T), relative humidity (RH), wind speed (WS), and precipitation (PR), the two population mobility indexes (moving-in index [MII] and moving-out index [MOI]), and the population density (PD), as well as a random intercept to control for location (L)-specific effects (e.g., size of susceptible population, social distancing, medical resources, COVID-19 control policies), which were unavailable. Population migration between cities could also affect the daily transmission rates. Particularly, during the period surrounding the Chinese New Year (“Spring Festival”) on January 25, 2020, between-city migration increased dramatically. Therefore, we incorporated the population mobility index of moving in or moving out (i.e., MII and MOI) as covariates in the model.
Effects of Temperature and Relative Humidity on the Stability of SARS-CoV-2
To illustrate the relationship between COVID-19 transmission and meteorological factors, we further utilized a virus persistence experiment. SARS-CoV-2 was isolated from the bronchoalveolar lavage fluid of a patient1 and passaged in a monkey kidney cell line (Vero-E6) for eight generations. The titer of the SARS-CoV-2 working solution was ∼5 × 105 plaque-forming units (PFU)/mL, as determined by plaque assay on the Vero-E6 cells incubated in the culture medium (DMEM with 2% FBS). Ninety-six cotton gauzes were prepared for the exposure experiment and placed in culture dishes, which were placed in incubators without light. A volume of 50 μL of SARS-CoV-2 working solution in DMEM culture medium with 2% FBS was spotted in droplets on the cotton gauze, dried for 30 min in a biological safety cabinet, and then incubated under specific temperature conditions (4°C, 20°C, 28°C, and 37°C) and relative humidity (low and high). In this stage, there was an immediate reduction in infectivity of the virus during drying in culture medium. After 30 min drying, they were incubated for about 1, 4, 8, 24, 48, and 72 h, respectively. At each exposure time point, the cotton gauzes were collected and soaked in 400 μL DMEM for 10 min, and the infectivity of the lixivium was then determined by plaque assay. For the high humidity groups, papers soaked with ultrapure water were placed in a zip-lock bag with the culture dish and cotton gauze inside. However, we could not measure the relative humidity directly. To mimic this environment, the wet paper tower was placed in a sealed box of an appropriate size, and the relative humidity was measured to be higher than 99% within 1 h measured using a psychrometer (Deli, model 9026, Ningbo City, China). Therefore, the relative humidity in the sealed bags with the wet paper towel was expected to be higher than 99%. The experiment was conducted in an animal biosafety level-III lab, where the indoor relative humidity was kept consistently at 40%–60%; this was measured using the same psychrometer and adopted as the low relative humidity in our study. The relative humidity in the bags without the wet paper towel was expected to be the same as the indoor relative humidity in the room. All experiments were conducted in replicates.
Data Analysis
The logistic growth model was executed using SAS software (SAS University Edition). The nonlinear (NLIN) regression procedure was used where the Gauss-Newton algorithm was utilized to search for the parameters that produced the smallest residual sum of squares. At the same time, the transmission rate was subsequently calculated based on Equation (2). Calculation of the linear mixed-effect model and mapping of the geographic distribution of the data of concern were carried out using the R package of “lme4” using R software (version 3.6.1). Cities were dynamically included if they were simultaneously accompanied by information on temperature, humidity, wind speed, precipitation, mobility, and population density at the lag times of concern with an assumed range of 1–14 days. Considering that the absolute humidity is highly positively correlated with the temperature (r = 0.938, p < 0.001) (see Figure S4A), it is not appropriate to adopt them together in our linear model due to the multicollinearity. Theoretically, the absolute humidity is significantly influenced by the environmental temperature. Likewise, temperature has been proved to be an independent factor that affects virus stability, thus we chose only the temperature, rather than the absolute humidity, as the main independent variable. The relative humidity is also statistically correlated with temperature (see Figure S4B), but has a very weak correlation (r = 0.27, p < 0.001), resulting in a negligible effect on the linear regression model. In considering that we had integrated information of temperature, absolute humidity, and atmospheric pressure, we therefore adopted this in our mixed model analysis. To validate the robustness of our model results, we further conducted sensitivity analyses by excluding the mobility index, or without correction by the event-based information. We also further confirmed the sensitivity of β1 to the confounders of wind speed, precipitation, population mobility indexes, and population density.
For data interpretation, we adopted the “lag time” (LT) to evaluate the environmental lag period of temperature or relative humidity, i.e., the period from the case infection of SARS-CoV-2 to the day when infection confirmation information was reported on the NHC website. This time period included the two main intervals of the time between the person being infected by SARS-CoV-2 and the onset of symptoms (i.e., the incubation time) and the time between the onset of symptoms and the report after infection confirmation on the NHC website (i.e., the report interval). These two intervals both followed gamma distributions, and their parameters were both provided in previous studies.21,22 The value distribution of LT was obtained by summing incubation time and report interval, which was carried out using SAS software. Subsequently, the LT value was used to compare our modeling results.
To further examine the association between temperature and relative humidity on COVID-19 transmission rate, we explored whether the linkage was modified by maintained household temperature. After January 23, 2020, most residents were encouraged to minimize their outdoor activities, and household heating considerably affected the indoor environment. In China, almost all household heating is municipally supplied at the city level, denoted as “public central heating,” and this is determined by geographical latitude in China. The Ministry of Housing and Urban-Rural Development of the People's Republic of China requires that the critical outdoor temperature for municipal heating is 5°C.30 On the other hand, the China District Heating Association requires that the municipally supplied indoor heating temperature should not be lower than 18°C.31 Therefore, in cities with public central heating, the indoor-versus-outdoor differences in temperature and relative humidity were obviously larger than those in cities without public central heating. If an effect of a weather variable on COVID-19 transmission existed, different household temperature control could strengthen or weaken the association. To check the above hypothesis, we incorporated the public central heating status of each city as an effect modifier and modeled its interactions with both temperature and relative humidity.
To investigate the nonlinear relationship of ambient temperature on COVID-19 transmission at the longest possible lag time, a generalized additive mixed model with random intercept was utilized using the R package of “mgcv.”
We constructed a scenario by assuming that the average of the relevant meteorological factors among the relevant geographic areas remains unchanged during the study period after the date of the earlier lag time before the January 23, 2020, around which the average meteorological condition was set as the reference (Mref). The daily change of Rt (ΔRt) can be obtained by the product of βM (Mt – Mref), where βM is the regression coefficient of the relevant meteorological factor from Equation (3). Thus, the accumulated number of COVID-19 cases (ΔNM) associated with the change of the individual relevant meteorological factor during the D days is equal to ΣβM (Mt – Mref).
For the results of the virus persistence experiments, we calculated the half times by assuming that they followed first-order decay. An ANOVA test was used to compare the mean difference of half times among different temperature and humidity treatments. Tukey's honestly significant difference pairwise comparison was also performed to compare the differences among all possible combination of treatments, and Tukey’s adjusted p value was used to indicate the false-positive statistical results. The key analysis code is provided in the Supplemental Code file.
Acknowledgments
We would like to express our gratitude for discussions with the researchers from the environmental exposure and human health working group of the China Cohort Consortium (http://chinacohort.bjmu.edu.cn/), as well as special thanks to Dr. Ping Zhong and Dr. Wentao Wang for their instructive guidance. This work was supported by the National Key Research and Development Program, P.R. China (Grant No. 2020YFC0846300 and 2020YFC0846200) and the National Natural Science Foundation of China (Grant No. 41771527; 41922057).
Author Contributions
B.W., M.R., B.J., J.C., T.X., G.S., and X.Y. conceived the study. B.J., J.C., and T.X. curated the data. M.R., B.J., J.C., and T.X. performed the analysis. B.W., T.X., M.R., and K.L. wrote the first draft of the manuscript. R.P., Z.C., X.C., F.D., and W.G. finished the virus stability experiment. R.P., C.L., Z.C., X.C., F.D., X.J., L.Z., R.Y., Z.D., K.L., L.Z., Y.Z., G.Z., and W.G. reviewed and edited the manuscript. B.W. and Z.L. managed the program.
Declaration of Interests
All authors declare no competing interests.
Published Online: December 15, 2020
Footnotes
Supplemental Information can be found online at https://doi.org/10.1016/j.xinn.2020.100071.
Contributor Information
Wuxiang Guan, Email: guanwx@wh.iov.cn.
Bin Wang, Email: binwangpku@foxmail.com.
Supplemental Information
Data S1. The data of daily increases in COVID-19 cases with and without corrections from the NHC website report.
Data S2. Human mobility index used to indicate of the individual movement among the relevant provinces or cities in our study. Sourced from the Baidu (see http://qianxi.baidu.com/).
Data S3. The temperature and relative humidity during the study period.
References
- 1.Zhou P., Yang X.L., Wang X.G., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Doremalen N., Bushmaker T., Morris D.H., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan K.H., Peiris J.S., Lam S.Y., et al. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011;2011:734690. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Doremalen N., Bushmaker T., Munster V.J. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Euro Surveill. 2013;18 doi: 10.2807/1560-7917.es2013.18.38.20590. [DOI] [PubMed] [Google Scholar]
- 5.Sajadi M.M., Habibzadeh P., Vintzileos A., et al. Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19) JAMA Netw. Open. 2020;3:e2011834. doi: 10.1001/jamanetworkopen.2020.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bukhari Q., Jameel Y. Will coronavirus pandemic diminish by summer? SSRN. 2020 doi: 10.2139/ssrn.3556998. [preprint] [DOI] [Google Scholar]
- 7.Thevarajan I., Nguyen T.H.O., Koutsakos M., et al. Breadth of concomitant immune responses prior to patient recovery: a case report of non-severe COVID-19. Nat. Med. 2020 doi: 10.1038/s41591-020-0819-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paules C., Subbarao K. Influenza. Lancet. 2017;390:697–708. doi: 10.1016/S0140-6736(17)30129-0. [DOI] [PubMed] [Google Scholar]
- 9.Ma Y., Zhao Y., Liu J., et al. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu L., Liu X., Huang H., et al. Meteorological impact on the COVID-19 pandemic: a study across eight severely affected regions in South America. Sci. Total Environ. 2020;744:140881. doi: 10.1016/j.scitotenv.2020.140881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Y., Jing W., Liu J., et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729:139051. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Demongeot J., Flet-Berliac Y., Seligmann H. Temperature decreases spread parameters of the new Covid-19 case dynamics. Biology (Basel) 2020;9 doi: 10.3390/biology9050094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qi H., Xiao S., Shi R., et al. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728:138778. doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi P., Dong Y., Yan H., et al. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020;728:138890. doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yao Y., Pan J., Liu Z., et al. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020;55 doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oliveiros B., Caramelo L., Ferreira N.C., et al. Role of temperature and humidity in the modulation of the doubling time of COVID-19 cases. medRxiv. 2020 doi: 10.1101/2020.03.05.20031872. [preprint] [DOI] [Google Scholar]
- 17.Sajadi M.M., Habibzadeh P., Vintzileos A., et al. Temperature and latitude analysis to predict potential spread and seasonality for COVID-19. SSRN. 2020 doi: 10.2139/ssrn.3550308. [preprint] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luo W., Majumder M.S., Liu D., et al. The role of absolute humidity on transmission rates of the COVID-19 outbreak. medRxiv. 2020 doi: 10.1101/2020.02.12.20022467. [preprint] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang M., Jiang A., Gong L., et al. Temperature significantly change COVID-19 transmission in 429 cities. medRxiv. 2020 doi: 10.1101/2020.02.22.20025791. [preprint] [DOI] [Google Scholar]
- 20.Shi P., Dong Y., Yan H., et al. The impact of temperature and absolute humidity on the coronavirus disease 2019 (COVID-19) outbreak—evidence from China. medRxiv. 2020 doi: 10.1101/2020.03.22.20038919. [preprint] [DOI] [Google Scholar]
- 21.Lauer S.A., Grantz K.H., Bi Q., et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li R., Pei S., Chen B., et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science. 2020;368:489–493. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Islam N., Shabnam S., Erzurumluoglu A.M. Temperature, humidity, and wind speed are associated with lower Covid-19 incidence. medRxiv. 2020 doi: 10.1101/2020.03.27.20045658. [preprint] [DOI] [Google Scholar]
- 25.Wang B., Wang Z., Zhao X., et al. Investigation on indoor and outdoor time of Chinese adults. J. Environ. Health. 2014;31:945–948. [in Chinese] [Google Scholar]
- 26.National Academies of Sciences, E. The National Academies Press; 2020. Medicine, Rapid Expert Consultation on SARS-CoV-2 Survival in Relation to Temperature and Humidity and Potential for Seasonality for the COVID-19 Pandemic (April 7, 2020) p. 8. [Google Scholar]
- 27.Chin A.W.H., Chu J.T.S., Perera M.R.A., et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. 2020;1:e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Biryukov J., Boydston J.A., Dunning R.A., et al. Increasing temperature and relative humidity accelerates inactivation of SARS-CoV-2 on surfaces. mSphere. 2020;5 doi: 10.1128/mSphere.00441-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dai Q., Ma W., Huang H., et al. The effect of ambient temperature on the activity of influenza and influenza like illness in Jiangsu Province, China. Sci. Total Environ. 2018;645:684–691. doi: 10.1016/j.scitotenv.2018.07.065. [DOI] [PubMed] [Google Scholar]
- 30.MOHURD, Design Code for Heating Ventilation and Air Conditioning of Civil Buildings. 2012,
- 31.CDHA Urban Heating service. 2020. http://www.china-heating.org.cn/hangyebz/471710200.html
- 32.Jia Xiaoqian, Chen Junxi, Li Liangjing, et al. Modeling the Prevalence of Asymptomatic COVID-19 Infections in the Chinese Mainland. The Innovation. 2020;1:100026. doi: 10.1016/j.xinn.2020.100026. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. The data of daily increases in COVID-19 cases with and without corrections from the NHC website report.
Data S2. Human mobility index used to indicate of the individual movement among the relevant provinces or cities in our study. Sourced from the Baidu (see http://qianxi.baidu.com/).
Data S3. The temperature and relative humidity during the study period.