Abstract
Background and Objective
The 12-month follow-up effect of the self-efficacy-focused structured education program (SSEP) requires in-depth confirmation. This study aims to verify whether the benefits of SSEP can be maintained in 12 months.
Materials and Methods
A multicenter randomized controlled trial with 12-month follow-up conducted among 265 type 2 diabetes patients not on insulin from 4 hospitals in mainland China. The intervention group (n = 133) was administrated with SSEP, and the control group (n = 132) received the routine education. The indicators of metabolic and psychosocial aspects of the patients were assessed at baseline and 12 months.
Results
As opposed to the control group, the primary outcomes of HbA1c in the intervention group were improved obviously in the 12th month during the 12-month follow-up (−1.13%, P < 0.001). The secondary outcomes (ie, waist circumference, total cholesterol, low-density lipoprotein cholesterol, diabetes self-efficacy, diabetes self-management behaviors, diabetes knowledge and diabetes distress) were improved significantly in the intervention group as compared with the control group in the 12th month during the 12-month follow-up (−3.14 cm, P = 0.001; −0.30 mmol/L, P = 0.032; −0.25 mmol/L, P = 0.008; 0.87, P < 0.001; 10.67, P < 0.001; 3.42, P < 0.001; −4.97, P < 0.001). The non-significant difference in the secondary outcomes (ie, systolic pressure, diastolic pressure, triglycerides and high-density lipoprotein cholesterol) was identified between the two groups in the 12th month during the 12-month follow-up (P > 0.05).
Conclusion
The SSEP provided sustainable benefits in outcomes of HbA1c, waist circumference, total cholesterol, low-density lipoprotein cholesterol, diabetes knowledge, diabetes distress, diabetes self-efficacy and diabetes self-management behaviors for type 2 diabetes patients not on insulin in the 12th month during the 12-month follow-up. Thus, it will be an effective education model capable of being generalized nationwide, and it can be referenced for the nations and regions under consistent conditions.
Clinical Trial Registry
Chinese Clinical Trial Registry (ChiCTR‐IOR‐17011007).
Keywords: diabetes mellitus, type 2, self efficacy, education
Introduction
Diabetes mellitus refers to a severe global public health concern. As revealed from the International Diabetes Federation (IDF), 9.3% of adults worldwide are subjected to diabetes, of which 79.4% live in underdeveloped nations, and nearly 90% developed type 2 diabetes mellitus (T2DM).1 In addition, 12.8% of adults have been reported to suffer from diabetes mellitus in mainland China.2 Diabetes patients may develop various chronic and acute complications (eg, cardiovascular diseases, renal diseases and diabetes ketoacidosis), and it was estimated that health expenses related to diabetes were 760 billion US dollars in 2019 globally and 109 billion US dollars for China, which has imposed a significant economic burden on society.1 Thus, proper disease management covering the glycemic control and blood pressure and blood lipid control with a series of self-management behaviors (eg, sensible diet, regular exercise, self-monitoring, as well as adherence to taking medicine according to physicians’ advice) is crucial for diabetes patients.
A good diabetes education program is capable of sufficiently motivating patients to develop self-management behaviors, improve the blood sugar levels of patients and reduce the risk of chronic and acute complications.3 The structured education, for its standardized, practicable and replicable characteristics, has been recommended by the global and national guidelines to help patients manage diabetes.4–7 Diabetes education in mainland China has long been unsatisfactory, and the study on structured education for diabetes patients in the nation remains preliminary.8,9 To our best knowledge, a nurse-led structured education program developed by our research team previously, recognized as the first well-designed program for Chinese T2DM patients not on insulin therapy, has been confirmed to be feasible and acceptable.8,9 Subsequently, the structured education program was supplemented by complying with self-efficacy theory, and a six-month follow-up multicenter randomized control trial was performed, with the positive results of metabolic outcomes and psychosocial aspects,10 thereby strongly evidencing the effectiveness of the self-efficacy-focused structured education program (SSEP) among Chinese T2DM patients. However, as with some other studies on diabetes education,11–13 the short-term effect rather than the intermediate- and long-term effect of the SSEP was identified.
Moreover, as indicated from a systemic review and meta-analysis, a self-efficacy-focused education program may positively impact blood sugar level and psychosocial indicators in the short term (3–6 months) follow-up.14 However, several studies reported that the effect of diabetes education lasted only 3–6 months, and it would attenuate subsequently;15–18 for instance, a meta-analysis of 16 randomized contrail trials reported that the HbA1c improvements in the 3–6 months, 6–12 months and above 12 months reached 0.49%, 0.44% and 0.07%, respectively.16 Thus far, what the intermediate- and long-term effects of the SSEP for Chinese T2DM patients are remain unclear. Thus, this study aimed to assess the benefits of SSEP among T2DM patients not on insulin at a twelve-month follow-up.
Materials and methods
The research refers to a robust multicenter, parallel, superiority, randomized controlled trial performed in four hospitals in China. The four hospitals, with levels not above grade III-B, were chosen by convenience sampling. The study was conducted from April 2017 to December 2018, and the recruitment of participants was conducted between April to November 2017. Patients were recruited if diagnosed with T2DM, aged between 18–75 years, with their HbA1c in the past 12 weeks no less than 7.5%, as well as not on insulin in the past three months. Patients being pregnant or preparing for pregnancy, with psychological problems or cognition disorders, or developing severe diabetes complications, or participating in other researches if they reported or the nurses or the physicians registered were excluded here. The sample of the original study was calculated based on a standard deviation of HbA1c (1%) in the target population, an inter-group difference (0.4%), the two-tailed power (0.8), alpha (0.05) as well as attrition rate (20%). So, one hundred and nineteen patients were required in each group respectively after calculation.
The recruitment of participants was completed by a physician and research nurse in each hospital. The research nurse, acting as the coordinator of the research in each hospital would explain the research aim, process, risks and benefits and others to the patients after they were referred from the physician. Subsequently, the patients would be registered and included by research nurses after they agreed to be recruited by the study. The block randomization with blocks of eight was conducted at the patients’ individual level to split the patients at a ratio of 1:1 to an intervention or control group. The random allocation sequence generated with programming of SPSS 17.0 (Armonk, NY: IBM Corporation) by the researcher was sealed in opaque envelopes. The research nurse was charged with grouping. When the recruitment number of patients reached eight, each patient got a serial number, and the research nurse opened an opaque envelope to figure out the group the patients belonged to. All the research staff in the respective center received the training before research began as well as the monitoring by the central researchers every three months. The details of trial design, research sample, participants, recruitment and enrolment, randomization methods, intervention, outcome measures, quality control and others were previously reported in the other publication.10
Intervention
Intervention Group
The development of the SSEP complied with the guidelines of T2DM in China, related literature and the findings of patients’ needs assessment.8,19 In addition, SSEP followed a sound theoretical foundation.8,19 It abided by a series of educational theories, ie, the basic principles of curriculum and instructions by Tyler, the taxonomy of educational objectives, as well as the principles of adult learning.8,19 Subsequently, SSEP was further founded on self-efficacy theory based on a series of existing studies.8,10,14,20 The SSEP was composed of four structured curriculums and regular follow-ups. The program consisted of a written curriculum, and it was delivered by the trained registered nurses and physicians to ensure the quality of a range of research centers. SSEP was delivered in a group format (with 4–8 patients in the respective group), one time per week and continued in four weeks, and the one group education would begin when the number of group members reached 4–8 patients after the recruitment and grouping were completed. After the four-week modules, patients received follow-ups by face to face/telephone format every three months. The contents of follow-up covered the patients’ self-management behaviors aspects and individualized problems posed by the patients.21 Each module lasted for nearly 60–90 min, and each follow-up was basically 10–15 min. The program aimed to promote patients recruited in the learning, motivate patients to change, develop and sustain self-management behaviors by primarily stressing the enhancement of patients’ self-efficacy. Moreover, the contents of the structured curriculums and the program training were reported elsewhere.10
Control Group
The control group received the routine education reported in an existing study.10 This primarily covered the individual face-to-face diabetes education presented by physicians during each medical clinic visits, as well as the conventional class education delivered by physicians and nurses per month. In addition, the follow-up/3 months was offered by nurses via face-to-face/telephone.
Outcome Measures
The metabolic and psychosocial outcome indicators were measured at baseline, three, six- and twelve-month follow-ups when the patients received medical visits in the clinics. The indicators of the plasma lipid profile were only measured at baseline, six- and twelve-months. All the outcome measures were completed by the trained nurses in the respective research center. Metabolic outcomes covered HbA1c, weight, body mass index (BMI), waist circumference (WC), blood pressure (systolic pressure, BP; diastolic pressure, DP), as well as plasma lipid profiles (triglycerides, TG; total cholesterol, TC; high-density lipoprotein cholesterol, HDL-C; low-density lipoprotein cholesterol, LDL-C). HbA1c referred to the primary outcome, and the other indicators were the secondary outcomes in the study. The indicators in the intervention group (IG) and control group (CG) were investigated at the identical time point. HbA1c and plasma lipid profiles were drawn from the medical records in four hospitals. Weight, height, waist circumference and blood pressure were manually measured with the identical instruments.
Moreover, psychosocial outcomes included diabetes self-efficacy (DSE), diabetes self-management (DSM) behaviors, diabetes knowledge and diabetes distress, which were evaluated by employing the validated Chinese version scales or questionnaires. The DSE was assessed based on a nine-item and five point Likert-type scale of Self-efficacy for Diabetes, as translated by Wei et al.22 DSM behaviors were evaluated according to a eleven-item and eight point Likert-type scale of the Summary of Diabetes Self-Care Activities, which was validated by Wan et al.23 The diabetes knowledge was measured by employing a ten-question Diabetes Knowledge Questionnaire, which was translated by Liu et al.24 Diabetes distress was assessed by using a seventeen-item and six point Likert-type scale of Diabetes Distress, as validated by Li et al.25 The indicator measurements were further elucidated in the previous publication.10 Furthermore, the basic demographic information of participants (eg, age, gender, marital status, employment status, educational level, individual monthly income and medical insurance) and diabetes-related information (eg, T2DM duration, years of taking medicine, diabetes medication use and diabetes-related complications) were collected by employing the self-designed questionnaire at baseline. The diabetes medication use was also collected at 12-month follow-up point.
Ethical Consideration
The study was confirmed to comply with the guidelines outlined in the Declaration of Helsinki. The research was authorized and managed by the Review Board of Peking University (IRB00001052‐17031). Moreover, it was registered in China (ChiCTR‐IOR‐17011007). The study was initiated after the ethical approval and the official admission letters were gained from each research center. Furthermore, the informed consent was conducted by the research nurse, and all the participants signed the written informed consent forms after agreeing to be recruited by the study.
Data Analysis
The data analysis was conducted with SPSS 25.0 (Armonk, NY: IBM Corporation) and base on intention to treat (ITT). Descriptive statistics were adopted to present the demographic characteristics of the participants. Inferential statistics covered independent t-test and chi-square tests to determine consistency of the demographic characteristics, diabetes-related information and the comparison of diabetes medication use. Robust generalized estimation equation’s with an unstructured form were exploited to process the repeated measurement data. The variables of group and measurement time were fitted as a major effect as well as an interaction, and baseline data were adjusted in all estimating models. The missing data for the indicators of TC, TG, LDL-C and HDL-C were assumed randomly lost, and they were not substituted. The value of P, below 0.05, was considered statistically significant.
Results
Demographic Characteristics
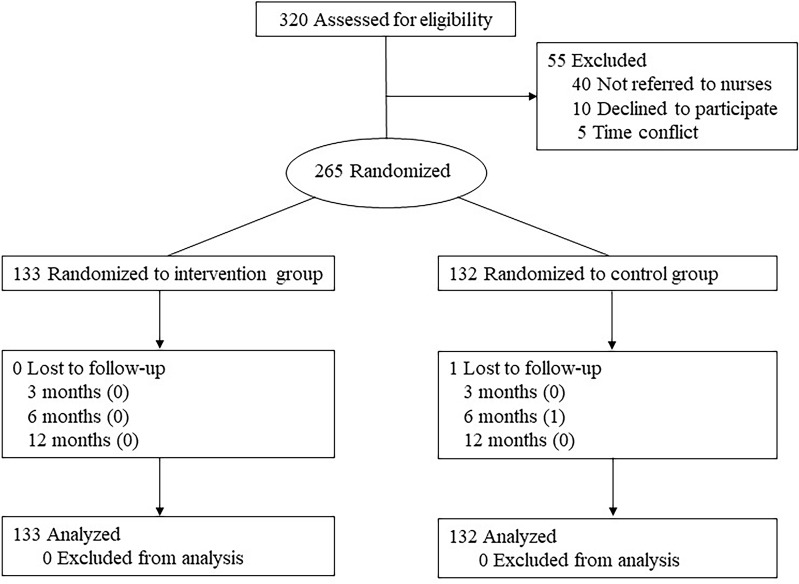
Two hundred and sixty-four of 265 patients received the 12-month follow-up. One patient was lost during the follow-up due to falling to their death and the data in the 12th month was substituted by the last follow-up time. In addition, the data of HbA1c, weight, waist circumference, blood pressure, diabetes knowledge, diabetes distress, diabetes self-efficacy and DSM behaviors were collected from 264 patients. Moreover, the data of TC, TG, HDL-C, and LDL-C in the 12-month were collected from 207, 207, 204, and 203 patients, respectively. Furthermore, this study, focusing on the 12-month follow-up time point, is a part of studies on the topic of the self-efficacy-focused structured education program. In the existing study,10,21 the demographic characteristics, and the comparisons of age, gender, marital status, education level, employment status, individual income, medical insurance, years of taking medicine, medication use and diabetes complications that was comparable between the two groups were reported. The flowchart of the participants is displayed in Figure 1.
Figure 1.
The flowchart of the participants.
Metabolic Outcomes
The Changes of the Primary Outcome of HbA1c
The interaction effect of group by time for the primary outcome of HbA1c was significant (P < 0.001). And the main effect of time, and the main effect of group were significant (P < 0.001). In comparison with the control group, HbA1c in the intervention group was ameliorated significantly (−1.13%, 95% CI: −1.42%, −0.83%, P < 0.001) with considering the baseline, measurement correlation, and the interaction effect of group by time. The variations in the primary outcome of HbA1c during the 12-month follow-up are listed in Table 1.
Table 1.
Changes in Metabolic and Psychosocial Outcomes of Patients with T2DM at 12 Months
| Variables | N (%) of Participants | Change (95% CI) | Change Between Groups(95% CI) | P value | |
|---|---|---|---|---|---|
| IG | CG | P | |||
| HbA1c, % | 1060 (100%) | − 1.59 (−1.82 to −1.37) | -0.69 (−1.01 to -0.38) | −1.13 (−1.42 to −0.83) | < 0.001 |
| Weight, kg | 1060 (100%) | −1.15 (−1.87 to −0.43) | 0.42 (−0.57 to 1.40) | −1.42 (−3.75 to 0.92) | 0.235 |
| BMI, kg/m2 | 1060 (100%) | −0.45 (−0.73 to −0.16) | 0.18 (−0.20 to 0.56) | −0.73 (−1.55 to 0.09) | 0.081 |
| WC, cm | 1060 (100%) | −1.58 (−2.61 to −0.56) | −0.16 (−1.17 to 0.85) | −3.14 (−4.91 to −1.36) | 0.001 |
| SP, mmHg | 1060 (100%) | −5.35 (−7.79 to −2.92) | −1.89 (−3.93 to 0.15) | −0.92 (−3.63 to 1.79) | 0.507 |
| DP, mmHg | 1060 (100%) | −4.37 (−6.04 to −2.70) | −3.02 (−4.35 to −1.68) | 0.30(−1.28 to1.88) | 0.710 |
| TC, mmol/L | 648 (81.5%) | −0.50 (−0.74 to −0.26) | −0.17 (−0.44 to 0.09) | −0.30 (−0.58 to −0.03) | 0.032 |
| TG, mmol/L | 647 (81.4%) | −0.43 (−0.66 to −0.20) | −0.22 (−0.49 to 0.05) | −0.09 (−0.35 to0.17) | 0.492 |
| LDL-C, mmol/L | 646 (81.3%) | −0.17 (−0.34 to 0.00) | 0.05 (−0.12 to 0.22) | −0.25 (−0.44 to −0.07) | 0.008 |
| HDL-C, mmol/L | 641 (80.6%) | −0.023 (−0.14 to 0.10) | −0.02 (−0.14 to 0.09) | −0.04 (−0.17 to 0.10) | 0.612 |
| Knowledge | 1060 (100%) | 3.87 (3.44 to 4.31) | 0.42 (−0.01 to 0.85) | 3.42 (2.91 to 3.92) | < 0.001 |
| DSE | 1060 (100%) | 1.46 (1.27 to 1.66) | 0.51 (0.29 to 0.72) | 0.87 (0.67 to 1.06) | < 0.001 |
| Diabetes distress | 1060 (100%) | −17.63 (−20.61 to −14.66) | −10.48 (−13.77 to −7.18) | −4.97 (−7.10 to −2.83) | < 0.001 |
| Behaviors | 1060 (100%) | 6.46 (3.87 to 9.05) | −2.48 (−5.08 to 0.13) | 10.67 (7.64 to 13.70) | < 0.001 |
Notes: N (%) of participants, the total number of the observations for participants during the 12 months; Change (95% CI), the change between 12 month and baseline in each group with consideration of the interaction of group by time; Change between groups (95% CI), the change between the groups at 12 months considering the interaction of groups by time.
Abbreviations: IG, intervention group; CG, control group; CI, confidence interval; BMI, body mass index; WC, waist circumference; SP, systolic pressure; DP, diastolic pressure; TC, total cholesterol; TG, triglycerides; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol, knowledge, diabetes knowledge; DSE, diabetes self-efficacy; Behaviors, diabetes self-management behaviors.
The Changes of the Other Metabolic Outcomes
The interaction effects of group by time for weight, BMI, WC, TC and TG were significant (P < 0.01), whereas these were not significant for HDL and LDL (P > 0.05). The main effects of time for weight, BMI, WC, TC and TG were significant (P < 0.01), whereas these were not significant for HDL and LDL (P > 0.05). The main effects of group for weight, BMI, TC, TG and HDL were not significant (P > 0.05), whereas these were significant for WC and LDL (P < 0.05). As opposed to the control group, the secondary outcomes of WC, TC, and LDL-C were clearly improved (−3.14 cm, 95% CI: −4.91 cm, −1.36 cm, P = 0.001); (−0.30 mmol/L, 95% CI: −0.58 mmol/L, −0.03 mmol/L, P = 0.032); (−0.25 mmol/L, 95% CI: −0.44 mmol/L, −0.07 mmol/L, P = 0.008) respectively after the baseline, measurement correlation, and the interaction effect of group by time were considered. The non-significant difference in the other secondary indicators of weight, BMI, systolic pressure, diastolic pressure, TG and HDL-C were identified between the two groups (P > 0.05). The variations of the other metabolic outcomes during the 12-month follow-up are listed in Table 1.
The Changes of the Psychosocial Outcomes
The interaction effect of group by time, the main effect of time and the major effect of group for psychosocial outcomes were significant (P < 0.001). As compared with the control group, an obvious increase in the indicator of diabetes knowledge was observed (mean (SE): 6.79 (0.26) vs 3.37 (0.29), 3.42, 95% CI: 2.91, 3.92, P < 0.001), and the indicator of diabetes distress was detected to decrease significantly in the intervention group (mean (SE): 25.58 (1.31) vs 30.55 (1.31), −4.97, 95% CI: −7.10, −2.83, P < 0.001) after considering the baseline, measurement correlation, and the interaction effect of group by time. The differences in the indicators of diabetes self-efficacy and DSM behaviors between the two groups also exhibited statistical significance (mean (SE): 4.42 (0.09) vs 3.55 (0.10), 0.87, 95% CI: 0.67, 1.06, P < 0.001); (mean (SE): 43.28 (1.66) vs 32.61 (1.75), 10.67, 95% CI: 7.64, 13.70, P < 0.001), respectively after considering the baseline, measurement correlation, and the interaction effect of group by time. Table 1 lists the variations in psychosocial outcomes during the 12-month follow-up.
Diabetes Medication Use
The glycemic control for both intervention and control groups in the 3rd, 6th and 12th months during the 12-month follow-up were achieved improvements. As compared with the regimens of antihyperglycemic drugs (AHDs) in baseline, 54 (40.60%) in the intervention group maintained the same treatment regimen; 36 (27.07%) had a decrease in the use of antihyperglycemic drugs (AHDs) or use of the less effective AHDs; 43 (32.33%) had an increase in the use of AHDs or use of the more effective AHDs after 12 months. While 65 (49.24%) in the control group had not changed the treatment regimen; 25 (18.94%) decreased the AHD’s usage, or changed to an AHD with weak effect; 42 (31.82%) increased the AHD’s usage, or changed to an AHD with strong effect. And among them, there were five patients in the intervention group and the control group in the 12th month of the 12-month follow-up who started using insulin therapy, respectively. There was no significant difference in the medication use of diabetes between the two groups (P > 0.05).
Discussion
As revealed from this study, a self-efficacy-focused structured education program (SSEP) can improve metabolic outcomes (eg, HbA1c, waist circumference, total cholesterol and low-density lipoprotein cholesterol), as well as psychosocial outcomes (eg, diabetes self-efficacy, diabetes self-management behaviors, diabetes knowledge and diabetes distress) until a 12-month follow-up. The noteworthy finding is that the improvement of HbA1c increased slightly. Besides, an unsatisfactory result is that the diabetes self-management behaviors were found to start to attenuate in the 12th month of the 12-month follow-up.
Previously, HbA1c difference at the 6-month between the intervention group and the control group was −0.740% (95% CI: −1.045%, −0.434%).10 The 12-month study increased slightly in the difference between the two groups (−1.13%, 95% CI: −1.42%, −0.83%). This was superior over the findings of the existing studies on diabetes education.15–18 As demonstrated from the result of the current study, the effect of the program on HbA1c could sustain until 12 months, and the effect on HbA1c was improved, which could be explained by three reasons. First, SSEP refers to a well-designed program with a structured format and theoretical driven principle. As suggested by a systemic review and meta-analysis, a program supported with structured curriculum and theory would achieve satisfactory results in blood sugar level.16 Besides, SSEP is patient-centered, culturally sensitive, by complying with on need assessments of patients and offering regular follow-up, which applies to T2DM patients in mainland China. Second, better DSM behaviors were associated with a lower blood sugar level. The intervention that is self-efficacy focused is capable of enhancing the self-efficacy of patients, and then further promoting patients to develop and maintain the DSM behaviors. Third, diabetes distress shows a close relation to cortisol or glycemic control,26,27 so the decrease in diabetes distress may be conducive to the patients’ glycemic control by improving the secretion of cortisol. Moreover, the diabetes medications in the 12th month of the 12-month follow-up were also analyzed, and the non-significant difference was identified between the two groups. Accordingly, the effect of medication use difference on HbA1c can be excluded. According to the UK prospective diabetes study, the improvement of HbA1c would mitigate the diabetes-related complications and premature death considerably,28 which would save considerable health expenditures.
The indicator of WC in the intervention group improved significantly in comparison with the control group. This is inconsistent with the existing studies on diabetes education.29,30 The improvement of WC might facilitate glycemic control by ameliorating insulin resistance. It was reported that WC has a close relationship with glycemic control. It was reported that compared with the T2DM patients without central obesity (< 80 cm in female and < 85 cm in the male), the insulin resistance of T2DM patients with central obesity (≥80 cm in female and ≥85 cm in the male) was more inadequate, thereby leading to high glycemic control.31 In addition, a study found that regional adipose tissue was a valid predictor of insulin resistance.32 The improvement of WC may help improve glycemic control by reducing the insulin resistance. Thus, this is probably why the indicator of HbA1c can sustain in the 12-month follow-up here. In comparison with the control group, visible improvement of TC and LDL-C was achieved in the intervention group in the 12th month, which was not observed in the 6th month. Satisfactory results in the intervention group might be attributed to the improvement of DSM behaviors, especially in the aspect of diet, and the longer term follow-up. Besides, existing studies suggested that insulin resistance and insulin dysfunction were the leading causes of dyslipidemia.33,34 The improvement of WC can alleviate insulin resistance to some extent and then facilitate the blood lipid control (eg, the TC and LDL-C). Specific to the other indicators of weight, BMI, blood pressure, TG and HDL-C, the improvements were observed in the intervention group, whereas non-significant difference was identified between the two groups.
In addition, the psychosocial outcomes of diabetes self-efficacy and DSM behaviors between the intervention group and the control group in the 12th month during the 12-month follow-up remained significant. The program was self-efficacy focused and applied a series of self-efficacy promoting strategies after finding self-efficacy as a promising point for intervention.10,20 Thus, the patients’ diabetes self-efficacy kept increasing. In accordance with self-efficacy theory,35 self-efficacy is a crucial predictor of human behaviors. As a result, DSM behaviors during the 12-month follow-up improved obviously. The results effectively evidenced the benefits of the SSEP in the indicators of diabetes self-efficacy and DSM behaviors in the 12th month during the 12-month follow-up. Furthermore, the mean score of DSM behaviors at the 12-month follow-up was slightly declining compared with the mean score at 6-month follow-up. It was therefore indicated that some other factors are affecting the persistence of DSM behaviors, so these factors should be determined and considered in the improvement of the SSEP.
In addition, the difference in the psychosocial indicator of diabetes knowledge was also significant during the 12-month follow-up between the two groups. This was consistent with a randomized controlled trial on structured education.36 The positive result in the study was largely attributed to the knowledge SSEP provided and the regular follow-up. A novel finding in the study was that diabetes distress presented a positive result, inconsistent with the result in the 6-month study.10 The positive effect in the 12th month during the 12-month follow-up was primarily attributed to the intervention of SSEP, which was self-efficacy theory-based. By complying with the self-efficacy theory,37 physiological/emotional arousal refers to one of the sources of information affecting self-efficacy. Thus, SSEP is patient-centered and incorporated with relevant contents and strategies in the program to relieve the negative emotion of the patients. Besides, patients’ negative emotion may require a longer time to eliminate, and the improvement of glycemic control may mitigate the diabetes distress of patients in reverse.
Strengths and Limitations
The trial involved a robust design that strongly evidenced the intermediate- and long-term effect of SSEP. Moreover, the well-designed nature and the effectiveness of SSEP made it likely to be generalized in other similar populations and settings. Besides, the data analysis complied with ITT and using generalized estimating equations to minimize the reporting bias. In addition, several limitations were found. The first one was that the 12-month follow-up remained insufficient to determine the long-term sustained effect of SSEP. The other was that the program has not undergone health economic assessment, so the generalization of the program was restricted to some extent.
Conclusions
The group-based self-efficacy-focused structured education program continuously impacted the metabolic outcomes (eg, HbA1c, waist circumference, total cholesterol and low-density lipoprotein cholesterol) and psychosocial outcomes (eg, diabetes self-efficacy, diabetes self-management behaviors, diabetes knowledge and diabetes distress) for T2DM patients not on insulin over 12 months. It was therefore suggested that SSEP will be an effective education model capable of being generalized nationwide. In addition, the SSEP can be referenced for managing diabetes in low- and middle-income nations and regions. Specific to subsequent studies, the long-term effect exerted by the program will be determined in depth, and the cost-effectiveness analysis of the program should be conducted. Furthermore, a further improvement of the program is worth exploring to help patients maintain DSM behaviors and HbA1c.
Acknowledgments
Many thanks to the physicians and nurses from Wuyishan Municipal Hospital in Fujian province, People’s Hospital of Leping City in Jiangxi province, Yanhua Hospital in Beijing, and Jimenli Primary Hospital in Beijing. The authors also thank the two hundred and sixty-five participants.
The authors declare that the consort checklist was used as a guide to report the study (Supplementary File 1).
Funding Statement
The study was supported by Hainan Provincial Natural Science Foundation of China (820RC631, 819QN229), Young Talents’ Science and Technology Innovation Project of Hainan Association for Science and Technology (QCXM202019), the Project of Science Research Project in Hainan University of Higher Education (Hnky2020-36), and Hainan Health Commission Health Industry Research Project (20A200286).
Data Sharing Statement
The authors don’t intend to share any data besides that which are included in the manuscript.
Disclosure
The authors declare no conflicts of interest.
References
- 1.International Diabetes Federation. IDF Atlas. 9th ed. 2019:2000. [Google Scholar]
- 2.Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ;2020:m997. doi: 10.1136/bmj.m997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chatterjee S, Davies MJ, Heller S, Speight J, Snoek FJ, Khunti K. Diabetes structured self-management education programmes: a narrative review and current innovations. Lancet Diabetes Endocrinol. 2018;6(2):130–142. doi: 10.1016/S2213-8587(17)30239-5 [DOI] [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence. Type 2 diabetes in adults: management. Guidance and guidelines. NICE; 2017. [Google Scholar]
- 5.International Diabetes Federation Guideline Development Group. Global guideline for type 2 diabetes. Diabetes Res Clin Pract. 2014;104(1):1–52. doi: 10.1016/j.diabres.2012.10.001 [DOI] [PubMed] [Google Scholar]
- 6.Beck J, Greenwood DA, Blanton L, et al. 2017 National standards for diabetes self-management education and support. DIABETES CARE. 2017;40(10):1409–1419. doi: 10.2337/dci17-0025 [DOI] [PubMed] [Google Scholar]
- 7.Chinese Diabetes Society. Guidelines for the prevention and treatment of type 2 diabetes in China (2017 edition). Chin J Diabetes Mellit. 2018;10(1):4–67. [Google Scholar]
- 8.Liu Y, Jiang X, Jiang H, Lin K, Li M, Ji L. A culturally sensitive nurse-led structured education programme in patients with type 2 diabetes. Int J Nurs Pract. 2019;25(5):e12757. doi: 10.1111/ijn.12757 [DOI] [PubMed] [Google Scholar]
- 9.Jiang X, Liu Y, Luo D, Li M. Structured education in patients with diabetes: a literature review. Chin J Nurs Educ. 2019;16(12):897–901. [Google Scholar]
- 10.Jiang XJ, Jiang H, Lu YH, et al. The effectiveness of a self-efficacy-focused structured education programme on adults with type 2 diabetes: a multicentre randomised controlled trial. J Clin Nurs. 2019;28(17–18):3299–3309. doi: 10.1111/jocn.14908 [DOI] [PubMed] [Google Scholar]
- 11.Cai C, Hu J. Effectiveness of a family-based diabetes self-management educational intervention for Chinese adults with type 2 diabetes in Wuhan, China. DIABETES EDUCATOR. 2016;42(6):697–711. doi: 10.1177/0145721716674325 [DOI] [PubMed] [Google Scholar]
- 12.Paz-Pacheco E, Sandoval MA, Ardena GJR, et al. Effectiveness of a community-based diabetes self-management education (DSME) program in a rural agricultural setting. Prim Health Care Res Dev. 2017;18(1):35–49. doi: 10.1017/S1463423616000335 [DOI] [PubMed] [Google Scholar]
- 13.Wichit N, Mnatzaganian G, Courtney M, Schulz P, Johnson M. Randomized controlled trial of a family-oriented self-management program to improve self-efficacy, glycemic control and quality of life among Thai individuals with type 2 diabetes. DIABETES RES CLIN PR. 2017;123:37–48. doi: 10.1016/j.diabres.2016.11.013 [DOI] [PubMed] [Google Scholar]
- 14.Jiang X, Wang J, Lu Y, Jiang H, Li M. Self-efficacy-focused education in persons with diabetes: a systematic review and meta-analysis. Psychol Res Behav Manag. 2019;12:67–79. doi: 10.2147/PRBM.S192571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scain SF, Friedman R, Gross JL. A structured educational program improves metabolic control in patients with type 2 diabetes: a randomized controlled trial. Diabetes Educ. 2009;35(4):603–611. doi: 10.1177/0145721709336299 [DOI] [PubMed] [Google Scholar]
- 16.Cheng L, Sit JWH, Choi KC, Chair SY, Li XM, He XL. Effectiveness of interactive self-management interventions in individuals with poorly controlled type 2 diabetes: a meta-analysis of randomized controlled trials. Worldviews Evid Based Nurs. 2017;14(1):65–73. doi: 10.1111/wvn.12191 [DOI] [PubMed] [Google Scholar]
- 17.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. DIABETES CARE. 2002;25(7):1159–1171. doi: 10.2337/diacare.25.7.1159 [DOI] [PubMed] [Google Scholar]
- 18.Reininger BM, Lee M, Hessabi M, et al. Improved diabetes control among low-income Mexican Americans through community-clinical interventions: results of an RCT. BMJ Open Diabetes Res Care. 2020;8(1):e867. doi: 10.1136/bmjdrc-2019-000867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu YL, Li MZ, Jiang H, et al. A pilot study of structured treatment and education program for type 2 diabetic patients without insulin therapy. Chin J Diabetes. 2016;24(07):638–644. [Google Scholar]
- 20.Jiang X, Jiang H, Li M, Lu Y, Liu K, Sun X. The mediating role of self-efficacy in shaping self-management behaviors among adults with type 2 diabetes. Worldviews Evid Based Nurs. 2019;16(2):151–160. doi: 10.1111/wvn.12354 [DOI] [PubMed] [Google Scholar]
- 21.Jiang XJ. The Clinical Effectiveness, Behavior Change Mechanism and Economic Evaluation of Structured Education in Patients with Type 2 Diabetes. Beijing: Peking University; 2019. [Google Scholar]
- 22.Wei J. Research on Relationship Between Diabetes Knowledge, Self-Efficacy and Self-Management Among Rural Elderly Patients. Hangzhou: Hangzhou Normal University; 2013. [Google Scholar]
- 23.Wan QQ, Shang SM, Lai XB, Pan J. Study on the reliability and validity of summary of diabetes self-care activities for type 2 diabetes patients. Chin J Pract Nurs. 2008;24(7):26–27. [Google Scholar]
- 24.Liu YL. A Structured Treatment and Education Program for Patients with Type 2 Diabetes Without Insulin Therapy: Development and Practice. Beijing: Peking University; 2016. [Google Scholar]
- 25.Li MZ. Study and Application of Depression Screening Methods in Patients with Diabetes. Beijing: Peking University; 2012. [Google Scholar]
- 26.Sang YM, Wang LJ, Mao HX, Lou XY, Zhu YJ, Zhu YH. Correlation of lower 2 h C-peptide and elevated evening cortisol with high levels of depression in type 2 diabetes mellitus. BMC PSYCHIATRY. 2020;20(1):490. doi: 10.1186/s12888-020-02901-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Asuzu CC, Walker RJ, Williams JS, Egede LE. Pathways for the relationship between diabetes distress, depression, fatalism and glycemic control in adults with type 2 diabetes. J DIABETES COMPLICAT. 2017;31(1):169–174. doi: 10.1016/j.jdiacomp.2016.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ Clin Res. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davies MJ, Heller S, Skinner TC, et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ. 2008;336(7642):491–495. doi: 10.1136/bmj.39474.922025.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khunti K, Gray LJ, Skinner T, et al. Effectiveness of a diabetes education and self management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus: three year follow-up of a cluster randomised controlled trial in primary care. BMJ. 2012;344:e2333. doi: 10.1136/bmj.e2333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou X, Ji L, Ran X, et al. Prevalence of obesity and its influence on achievement of cardiometabolic therapeutic goals in Chinese type 2 diabetes patients: an analysis of the nationwide, cross-sectional 3B study. PLoS One. 2016;11(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rattarasarn C. Physiological and pathophysiological regulation of regional adipose tissue in the development of insulin resistance and type 2 diabetes. ACTA PHYSIOL. 2006;186(2):87–101. doi: 10.1111/j.1748-1716.2005.01521.x [DOI] [PubMed] [Google Scholar]
- 33.Rosenblit PD. Common medications used by patients with type 2 diabetes mellitus: what are their effects on the lipid profile? Cardiovasc Diabetol. 2016;15:95. doi: 10.1186/s12933-016-0412-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bardini G, Rotella CM, Giannini S. Dyslipidemia and diabetes: reciprocal impact of impaired lipid metabolism and Beta-cell dysfunction on micro- and macrovascular complications. Rev Diabet Stud. 2012;9(2–3):82–93. doi: 10.1900/RDS.2012.9.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bandura A. Toward a psychology of human agency: pathways and reflections. Perspect Psychol Sci. 2018;13(2):130–136. doi: 10.1177/1745691617699280 [DOI] [PubMed] [Google Scholar]
- 36.Mohamed H, Al-Lenjawi B, Amuna P, Zotor F, Elmahdi H. Culturally sensitive patient-centred educational programme for self-management of type 2 diabetes: a randomized controlled trial. Prim Care Diabetes. 2013;7(3):199–206. doi: 10.1016/j.pcd.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 37.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]