Abstract
Objectives:
To assess the cognitive status of older adults in Saudi Arabia.
Methods:
This was a cross-sectional, multistage, stratified study of older individuals (≥60 years of age) attending primary healthcare centres in Riyadh, Saudi Arabia between January 2015 and April 2017. We collected data using a structured questionnaire, which incorporated questions regarding demographic and anthropometric variables, the Arabic version of Mini-Mental State Examination, the Mini-Nutritional Assessment tool, and the Modified Katz Index of Independence in activities of daily living.
Results:
Of the 1299 participants, 914 (70.4%) were male, with a mean age of 66.2 ± 5.9 years. Approximately 79.1% of the participants had intact cognitive function, 17.1 had mild cognitive impairment, and 3.8% had severe cognitive impairment. Impaired cognitive function was associated with increased age, female gender, low education, unmarried status, and unemployed (p<0.001). Reduced cognitive impairment was significantly associated with functional impairment and malnutrition (p<0.001).
Conclusion:
Cognitive impairment affected around 21% of the participants. The reduced cognitive function was associated with increased age, female gender, low education level, unmarried, low income, dependency on others, functional impairment, and malnutrition. Such information could motivate health-policy makers to introduce appropriate measures to improve older adults’ existing healthcare services in primary care, including cognitive function assessment.
Keywords: older adults, cognitive impairment, Mini-Mental State Examination
Population aging is emerging as a significant demographic trend worldwide. In 1990, persons aged 60 years or older constituted about 9.2% of the total global population. This rose to 11.7% in 2013, and is projected to reach as high as 21.1% (>2 billion) by 2050. In several developing countries, the population of individuals aged 60 years or older is increasing at a faster rate than the population as a whole.1 In Saudi Arabia, older adults (60 years of age or older) made up about 5.6% of the total population in 2017, and this percentage is expected to reach 25% by 2050. Life expectancy in the country is also expected to move from 74 to 82 years.2,3 With this rise in longevity, health workers should expect an increase in the risk of developing cognitive impairment.4 Moreover, evidence indicates the prevalence of dementia will triple worldwide over the next 2 decades.5
Significant causes of morbidity in old age include physical and mental illness due to loss of adaptability, the cumulative degenerative process, and the effects of iatrogenic disability and the social environment.6 The changes due to aging must fulfill 4 criteria: universal, progressive, intrinsic, and deleterious to the individual concerned.7 Moreover, lay care providers of elderly individuals often suffer from significant emotional, physical, and social morbidity.8,9
Even though elderly individuals are at higher risk of cognitive impairment than the rest of the population, health professionals should not consider these impairments as inevitable changes due to aging. Care providers should take prompt and aggressive action, especially in cases involving illness or injury.10-12
The assessment of an older adult’s cognitive status is instrumental in identifying early changes in physiological status, determining the ability to learn, and evaluating responses to treatment.13,14 Studies evaluating the prevalence of cognitive impairment among community-dwelling older individuals in Saudi Arabia are scarce. This study aim to assess the cognitive status of older adults attending primary healthcare centers in Riyadh, Saudi Arabia.
Methods
This cross-sectional, multistage, stratified study was part of a research project evaluating the internal environment of primary healthcare centers and assessing the health status of older people attending these centers in Riyadh, Saudi Arabia between January 2015 and April 2017.
This study included data from older adults visiting 15 primary healthcare centers (PHCCs) selected using the simple random sampling method from Riyadh, Saudi Arabia’s 5 geographical areas. the investigators estimated the sample size as follows: The mean number of elderly attending a PHCC/month (679)*15 PHCCs=10185 elderly. Approximately 15% of these elderly was selected randomly 10185*15%=1528
The authors chose 3 PHCCs from each of the following 5 areas: north, south, central, east, and west to represent the geographic sectors of the city of Riyadh. We included men and women aged ≥60 years attending the selected PHCCs for routine primary care services. Within each sector, the older adults’ sample size was determined proportional to the population attending the three selected PHCCs, and stratifying them according to gender. The older adults from each PHCC were selected consecutively. The detailed methodology has been described elsewhere.15,16
All of the participants or their caregivers provided written informed consent before the study. We assigned a number to each of the enrolled individuals that included the unique reference number of his or her primary healthcare. We maintained confidentiality throughout the investigation. The Ministry of Health ethics committee approved the study, which was supported by the National Plan for Science, Technology, and Innovation, King Abdulaziz City for Science and Technology, Saudi Arabia.
Two trained healthcare workers (one male and one female) from each primary healthcare were selected to conduct data collection under the regular supervision of one of the investigators. We assigned each of the selected healthcare workers a number (also including the centre reference number).
We collected socio-demographic data including age, marital status, educational status, and occupational status along with health data using a structured questionnaire. Cognitive status was assessed using the Mini-Mental State Examination (MMSE).17 It has been a proven effective and valid tool with high specificity and sensitivity to assess the mental status of older adults.18 The MMSE is specifically useful to assess the mental status of older adults in outpatient clinics, nursing homes, hospitals, and communities.19,20 It consists of 11 questions to measure 5 domains of cognitive function: orientation, registration, attention and calculation, recall, and language. The maximum score is 30.17 The MMSE score is used to classified elderly individuals’ cognitive impairment into the following categories: 24-30, intact cognitive function; 18-23, mild cognitive impairment; and 0-17, severe cognitive impairment. Only 5-10 minutes are required to complete the MMSE. However, the instrument relies heavily on verbal responses, reading, and writing. Therefore, patients who are illiterate, hearing impaired, or visually impaired and those with other communication disorders were excluded from the study. As the MMSE was found valid for use within Arabic-speaking populations,21 we used the Arabic version of the MMSE in this study.
We also assessed the nutritional status of the participants using the Arabic version of the Mini-Nutritional Assessment (MNA®) tool, available from the Nestlé Nutrition Institute.22 This tool has also been shown to be effective and valid with high specificity and sensitivity to determine the nutritional status of older adults.22-24 The MNA® scores range from 0-30 points. Depending on the score, the individual is classified as well-nourished (24-30 points, at risk of malnutrition (17-23.5 points), or undernourished (<17 points).25
We also used the modified Katz Index of Independence in activities of daily living (ADL) such as eating, bathing, dressing, and toileting.26 The response was recorded according to the degree of difficulty (none, a little, a lot, and unable to). We identified participants as fully functional (score: 6), with moderate functional impairment (score: 3-5), or with severe functional impairment (score: 0-2). All the instruments (MMSE, MNA, and ADL) are reliable and valid.21,27,28
Body mass index (BMI) was determined by dividing the weight in kg by the square of height in meters. We classified them as underweight (<18.5 kg/m2), normal weight(18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), or obese (≥30 kg/m2) according to the World Health Organization (WHO) international standard of BMI.25
A pilot study of 20 elderly individuals in 4 primary healthcare centers in Riyadh, Saudi Arabia was conducted to ascertain that the questions were understood, to estimate the time required to complete the questionnaire, and to explore any obstacles or constraints. Field supervisors revised the questionnaire accordingly and tested its clarity and feasibility.
Statistical analysis
Data were analyzed using Statistical Package for Social Sciences, version 22 (IBM Corp, Armonk, NY, USA) for statistical analysis. We presented age as a continuous variable (the mean ± standard deviation) in the text, while we presented all other variables as categorical variables (the frequency and percentage) in the tables.
Bivariate relationships or differences of each categorical variable with cognitive impairment were examined by the Chi-square test (χ2), while multivariate relationships between the cognitive impairment and various variables were determined by logistic regression. The binary logistic regression was applied, in which cognitive status was taking as the dependent variable and other variables as independent variables. The probability of cognitive impairment risk over the probability of no risk of cognitive impairment was presented in the form of an odds ratio. Differences were considered significant at p<0.05, at 95% confidence interval (CI).
Results
The study included 1299 older adults who completed the MMSE. The response rate was 85%. Table 1 shows the social-demographic characteristics of the participants according to cognitive status, measured using the MMSE. Of the participants, 70.4% were males. The mean age was 66.2 ± 5.9 years, with ages ranging from 60 to 93 years. The mean ages for male was 67.0 ± 6.8 years and 68.1 ± 6.5 years for female. Most participants (77.3%) were aged 60-69 years, married (89.3%), and unemployed (78.4%). The study population included 18.0% from the city’s Central, 33.4% from the Western, 16.0% from the Eastern sector, 20.4% from the Southern, and 12.1% from the Northern.
Table 1.
Socio-demographic characteristics by Mini-Mental State Examination score (N=1299).
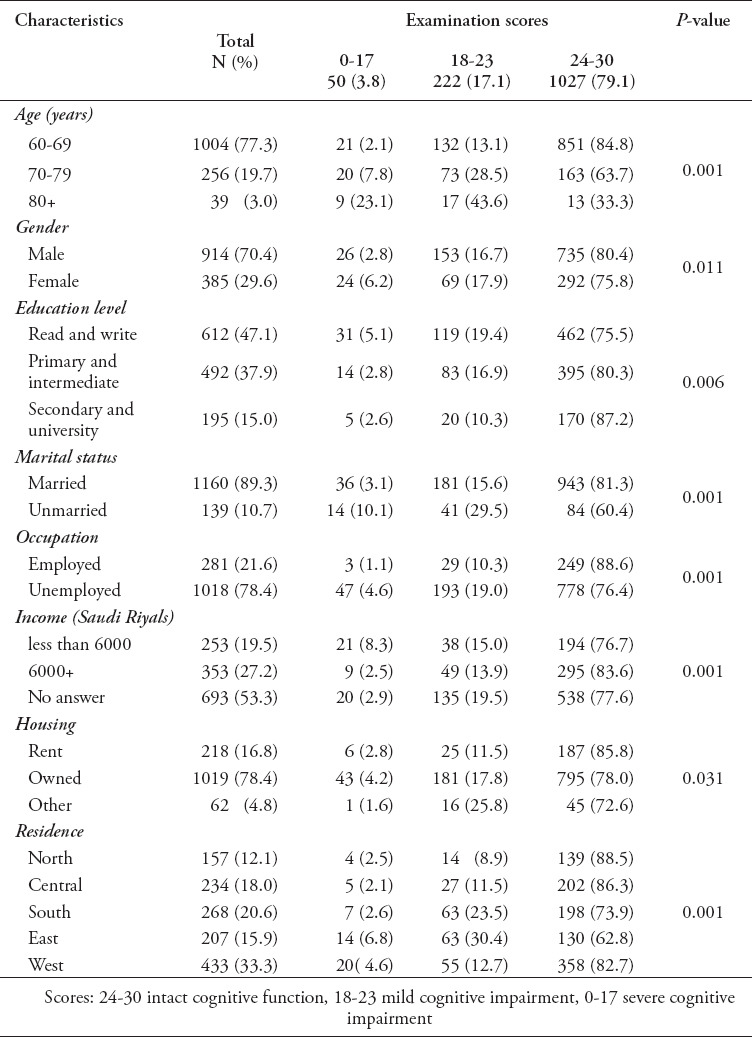
Approximately 79.1% of the participants had intact cognitive function, whereas 17.1% had mild cognitive impairment and 3.8% had severe cognitive impairment. Impaired cognitive function was associated with increased age, female gender, low education level, being unmarried, unemployed, low income, and the East and West sectors (p<0.001).
Table 2 presents the living arrangements, dependency on others, ADL, nutritional status, and BMI of the participants according to MMSE score. Only 5.6% of the participants lived alone. The majority (96.2%) were classified as fully functional based on their ADL scores, and 86.5% had a normal nutritional status. Nevertheless, 41.2% were overweight, and 39.4% were obese. Reduced cognitive impairment was significantly associated with dependency on others, functional impairment, and malnutrition (p<0.001).
Table 2.
Living arrangement, activities of daily living, and nutritional assessment by Mini-Mental State Examination score (N=1299).
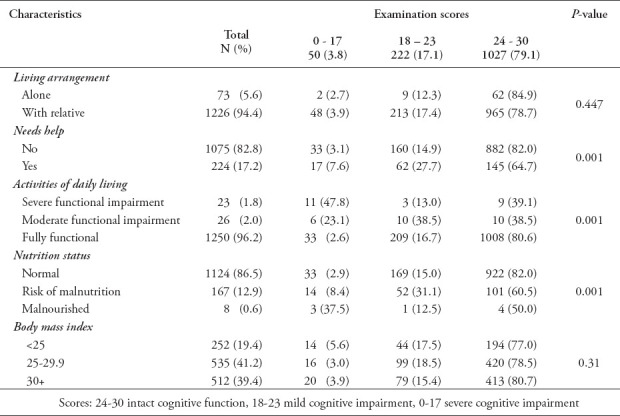
Table 3 demonstrates that the binary logistic regression for the risk of cognitive impairment MMSE versus Age, level of education, marital status, working status, income, area of residence, help requirement, ADL, and MNA maintained a marked association after adjusting for other variables. Other variables such as the participants gender, housing ownership, living arrangement, BMI failed to predict the risk of cognitive impairment.
Table 3.
Binary logistic regression: influence of the socio-demographic characteristics, activities of daily living, and nutrition status on the risk of severe or mild cognitive impairment (N=1299).
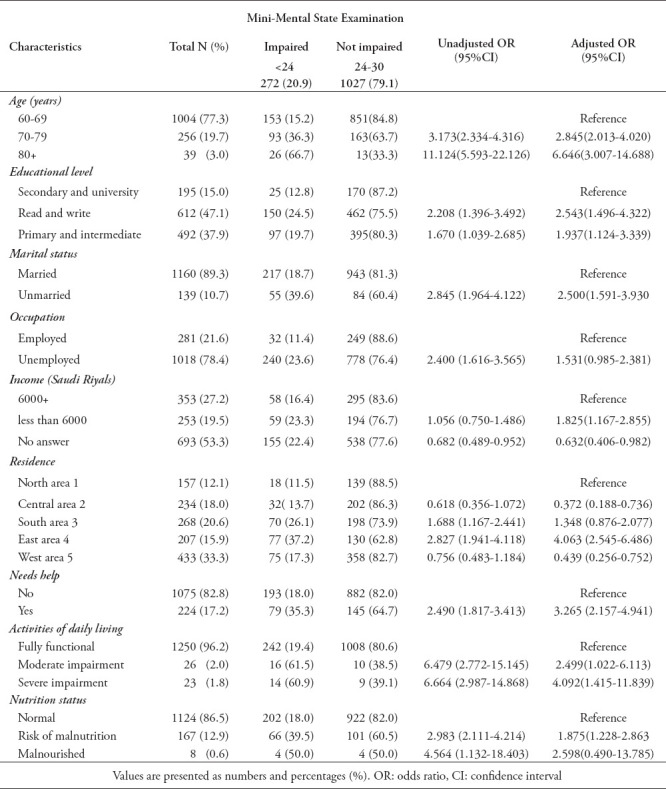
While non-modifiable risk factors such as increased in age (OR=6.646; 95% CI=3.007-14.688), modifiable risk factors such as low level of education (OR = 2.5435; 95% CI=1.496-4.322), lower performance in ADL 4.092(1.415-11.839) (OR=4.092; 95% CI=1.415-11.839) and malnutritional status MNA (OR=2.598; 95% CI=0.490-13.785)were associated with increased risk of cognitive decline.
Discussion
As the world’s population ages, the decline of cognitive function among older adults are becoming common and poses significant threats to their mental and physical wellbeing; moreover, its burden extends to family caregivers.29 Cognitive impairment affects the quality of life and increases health care costs.30 In the present study, 17.1% of the participants were affected by mild cognitive impairment and 3.8% were affected by severe cognitive impairment. These are less than the 45% (mild 38.6%) reported in a cross-sectional study of older adults in the family medicine clinics affiliated with King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia using the Montreal Cognitive Assessment test.31 Yet, our findings are consistent with the 5-7% global prevalence of dementia and the 10-20% prevalence of cognitive impairment among the elderly.32,33 The regional prevalences of dementia and mild cognitive impairment both range between 4.4% and 32%.34-36 But better than 69.8% of Morocco’s older adults were classed as having cognitive impairment. The malnutrition, gender and low education were risk factors for cognitive impairment, when moderate level of physical activity was a protective factor compared to the limited level.37
The rising rate of cognitive impairment in Saudi Arabia may be attributed to the widespread occurrence of risk factors for dementia.38,39 These risk factors include smoking (21.4%), diabetes mellitus (25.0%), hypertension (36.0%), and hypercholesterolemia (40.0%).41-43 Other possible risk factors for cognitive impairment include malnutrition and low education.30,37
Mild cognitive impairment is a transitional stage before dementia, and the annual conversion rate to dementia reaches up to 20.0%.44,45 Early detection of cognitive impairment can slow progression of the disease and offers medical, emotional, and financial benefits to affected individuals and their families.46,29 There is a need to control risk factors for cognitive impairment in Saudi Arabia because, as the aging population grows, the prevalence of dementia could increase significantly.
Our study revealed a significant association between impaired cognitive function and increased age, female gender, low education level, and low income. This finding is consistent with previous studies in which increased age, female gender, low educational level, and low income were also associated with poor cognitive performance.37,47,48 However, our findings differed from those of the Chinese longitudinal healthy longevity survey (N=13,586), which did not reveal gender differences in cognitive function across two age cohorts.49 In later life, reading was protective of cognitive function. A decreased risk of cognitive impairment for older adults at all levels of education has been correlated with regular reading practises We should encourage older adults to read as much as they can from their favorable literature such as the holy Quran, social media, and newspaper.
An unmarried status was associated with reduced cognitive function. This finding is similar to that of a previous study, which reported that being married may serve as a buffer against the negative cognitive impacts of aging.51 A sizeable number of our older adults are still living with spouse particularly men. This may contribute to their low cognitive impairment. Only 5.6% of the participants in our study lived alone. The cognitive function of those living alone and those living with relatives did not differ significantly. This finding confirmed that of a previous study in which those who lived alone did not show declines in cognitive score over 2 years, even though they reported greater feelings of emotional loneliness than those living with others.52
Interestingly, past literature supports our finding that working is protective. So policy makers may find this data in support of increasing the age of retirement. Also create an opportunities for older adults to participate in paid or voluntary work. Such effort may prevent loneliness and generate some income to them. This finding is consistent with that of a study carried out by Xue et al.53 They found the cognitive function of individuals who were not currently working to be inferior to that of their counterparts. They suggest the cognitively stimulating activities associated with employment may benefit the memory of older adults.53
The majority (96.2%) of participants in our study were able to perform ADL independently, and we found a significant association between poor cognitive function and functional impairment. This is consistent with the results of a previous study that suggest screening for independence in ADL could serve as an additional and potentially economically viable indicator to assess the risk of poor cognitive function.54,55 Health decision makers and professional should work on improving older adults ADL, since this modifiable factors may help to improve the overall cognitive function of the older adults. Also, exercise-based therapeutic strategies aiming to improve physical fitness should be implemented as recommended by previous investigators.37,56 Provided the protective effects of physical activity and physical function on the cognitive decline at later age, decision-makers should plan health promotion programs of regular physical activity, provide physical fitness facilities to improve physical and cognitive function among people across all ages. Also improve the provision of physiotherapy. These maneuver are also supported by the previous literature.37,57
Approximately 41% of the participants were overweight, and 39.4% were obese according to the WHO classification. A lower BMI was associated with a decline in cognitive function, which is similar to the findings of a previous study in the United States. The investigators found a lower BMI was associated with faster rates of cognitive decline, specifically, semantic and episodic memory.58 Although malnutrition risk is well investigated in older adult care facilities, few researches have been published to address community-dwelling older adults’ concerns.
We found a significant association between nutritional status and cognitive function. A previous study found that those with cognitive impairment were at higher risk of malnutrition, which can have significant adverse effects on quality of life, clinical outcomes, and morbidity and mortality.59 Malnutrition is one of the health problems in the elderly population, which increases the risk of poor clinical outcomes.60 These indicate that nutritional status monitoring can prevent it from leading to cognitive impairment. Thus, health professionals should assess the nutritional and cognitive status of the older adults regularly to the early dictation and timely management.
Screening, treatment, and rehabilitation should be integrated to prevent unnecessary suffering and prolonged dependency among the elderly. A previous study reported that, while a majority of older adults and primary care physicians have a positive attitude regarding regular cognitive assessments, only 16.0% of seniors receive one.29 A family physician and his or her team have a pivotal role in the assessment of an older adult’s cognitive status and in monitoring responses to treatment. The WHO recommends age-friendly primary healthcare to achieve the goal of successful aging.61 So far, in Saudi Arabia, primary health care centers provide free of charge preventive and curative services to Saudi Citizens.
Recently, aging has become a priority for primary healthcare s in Saudi Arabia, particularly in respect to continuous training programs targeting health workers in these centers provided by the Ministry of Health in the area of geriatric care. We recommend the areas of training, such as health screening, assessment, treatment, and rehabilitation, be based on evidence-based studies, practices, and resources. With this foundation, progress toward further investment in health priorities for older adults can be better assured, thereby improving these individuals’ quality of life.
Study limitations
The cross-sectional design of this study prevented us from establishing causality. Though the study was conducted in the biggest city in Saudi Arabia, our findings may not be generalizable to all areas of the country.
In conclusion, approximately 21% of the participants had cognitive impairment associated with increased age, female gender, low education level, unmarried, and a low income. Also, reduced cognitive function was associated with dependency on others, functional impairment, and malnutrition. The current study will help health-policy makers take appropriate measures to improve the existing healthcare services provided to older adults. Comprehensive geriatric assessment including cognitive function of older adults in primary healthcare would inevitably reduce these individuals’ risk of developing complications and improve their quality of life.
Acknowledgment
The study was funded by the National Plan for Science, Technology, and Innovation (MAARIFAH), King Abdulaziz City for Science and Technology, Kingdom of Saudi Arabia (Grant No. 10-MED121902). We would like to thank all of the healthcare providers involved in the research and the Ministry of Health for permitting us to conduct the study. Lastly we would like to thank Editage (www.editage.com) for the English language editing.
Footnotes
References
- 1.Sander M, Oxlund B, Jespersen A, Krasnik A, Mortensen EL, Westendorp RGJ, et al. The challenges of human population ageing. Age Ageing. 2015;44:185–187. doi: 10.1093/ageing/afu189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United Nations. World Population Ageing 2013. 2020. [Accessed October 4]. Updated 2013. Available from URL: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf .
- 3.Abusaaq HI SAMA Working Paper: Population Aging In Saudi Arabia. Saudi Arabian Monetary Agency. 2020. [Accessed October 7]. Updated 2015 February. Available from URL: https://docplayer.net/18400957-Sama-working-paper-population-aging-in-saudi-arabia-february-2015-hussain-i-abusaaq-economic-research-department-saudi-arabian-monetary-agency.html .
- 4.Batum K, Çinar N, Şahin Ş, Çakmak MA, Karşidağ S. The connection between MCI and Alzheimer disease: neurocognitive clues. Turk J Med Sci. 2015;45:1137–1140. doi: 10.3906/sag-1404-179. [DOI] [PubMed] [Google Scholar]
- 5.Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer's disease: an analysis of population-based data. Lancet Neurol. 2014;13:788–794. doi: 10.1016/S1474-4422(14)70136-X. [DOI] [PubMed] [Google Scholar]
- 6.Khoja AT, Aljawadi MH, Al-Shammari SA, Mohamed AG, Al-Manaa HA, Morlock L, et al. The health of Saudi older adults;results from the Saudi National Survey for Elderly Health (SNSEH) 2006-2015. Saudi Pharm J. 2018;26:292–300. doi: 10.1016/j.jsps.2017.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020;139:6–11. doi: 10.1016/j.maturitas.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alshammari SA, Alzahrani AA, Alabduljabbar KA, Aldaghri AA, Alhusainy YA, Khan MA, et al. The burden perceived by informal caregivers of the elderly in Saudi Arabia. J Family Community Med. 2017;24:145. doi: 10.4103/jfcm.JFCM_117_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Or R, Kartal A. Influence of caregiver burden on well-being of family member caregivers of older adults. Psychogeriatrics. 2019;19:482–490. doi: 10.1111/psyg.12421. [DOI] [PubMed] [Google Scholar]
- 10.Kelly ME. The potential of a relational training intervention to improve older adults'cognition. Behav Anal Pract. 2020;13:684–697. doi: 10.1007/s40617-020-00415-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–446. doi: 10.1016/S0140-6736(20)30367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Subramaniam H. Co-morbidities in dementia: time to focus more on assessing and managing co-morbidities. Age Ageing. 2019;48:314–315. doi: 10.1093/ageing/afz007. [DOI] [PubMed] [Google Scholar]
- 13.Garrard JW, Cox NJ, Dodds RM, Roberts HC, Sayer AA. Comprehensive geriatric assessment in primary care: a systematic review. Aging Clin Exp Res. 2020;32:197–205. doi: 10.1007/s40520-019-01183-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patnode CD, Perdue LA, Rossom RC, Rushkin MC, Redmond N, Thomas RG, et al. Screening for cognitive impairment in older adults: updated evidence report and systematic review for the US Preventive Services Task Force. Jama. 2020;323:764–85. doi: 10.1001/jama.2019.22258. [DOI] [PubMed] [Google Scholar]
- 15.Alhamadan AA, Bindawas SM, Alshammari SA, Al-Amoud MM, Al-Orf SM, Al-Muammar MN, et al. Prevalence of malnutrition and its association with activities of daily living in older adults attending primary health care centers: A multistage cross-sectional study. Progin Nutr. 2019;21:1011–1018. [Google Scholar]
- 16.Alhamdan AA, Alshammari SA, Al-Amoud MM, Hameed TA, Al-Muammar MN, Bindawas SM, et al. Evaluation of health care services provided for older adults in primary health care centers and its internal environment. A step towards age-friendly health centers. Saudi Med J. 2015;36:1091–1096. doi: 10.15537/smj.2015.9.11789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 18.Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15:116–122. doi: 10.1016/s0899-9007(98)00171-3. [DOI] [PubMed] [Google Scholar]
- 19.Schneider SM, Hebuterne X. Use of nutritional scores to predict clinical outcomes in chronic diseases. Nutr Rev. 2000;58(2 Pt 1):31–38. doi: 10.1111/j.1753-4887.2000.tb07809.x. [DOI] [PubMed] [Google Scholar]
- 20.Guigoz Y. The Mini Nutritional Assessment (MNA) review of the literature--What does it tell us? J Nutr Health Aging. 2006;10:466–485. discussion 485-487. [PubMed] [Google Scholar]
- 21.El-Hayeck R, Baddoura R, Wehbé A, Bassil N, Koussa S, Abou Khaled K, et al. An Arabic version of the mini-mental state examination for the Lebanese population: Reliability, validity, and normative data. J Alzheimers Dis. 2019;71:525–540. doi: 10.3233/JAD-181232. [DOI] [PubMed] [Google Scholar]
- 22.Guigoz Y. The Mini Nutritional Assessment (MNA®) Review of the literature-What does it tell us? J Nutr Health Aging. 2006;10:466–485. [PubMed] [Google Scholar]
- 23.Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15:116–122. doi: 10.1016/s0899-9007(98)00171-3. [DOI] [PubMed] [Google Scholar]
- 24.Schneider SM, Hebuterne X. Use of nutritional scores to predict clinical outcomes in chronic diseases. Nutr Rev. 2000;58:31–38. doi: 10.1111/j.1753-4887.2000.tb07809.x. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. Physical status: The use of and interpretation of anthropometry, Report of a WHO Expert Committee. 2020. [Accessed October 9]. Updated 1995. Available from URL: who.int/childgrowth/publications/physical_status/en/ [PubMed]
- 26.Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 27.Al-Atty A, Muhammad F, Abou Hashem RM, Abd Elaziz KM. Prevalence of malnutrition in recently hospitalized elderly in Cairo using a valid and reliable short form of Arabic version of Mini-Nutritional Assessment (MNA-SF-A) Middle East Age Ageing. 2012;83:1–5. [Google Scholar]
- 28.Nasser R, Doumit J. Validity and reliability of the Arabic version of activities of daily living (ADL) BMC. 2009;9:1. doi: 10.1186/1471-2318-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Association As. 2019 Alzheimer's disease facts and figures. Alzheimers Dement. 2019;15:321–387. [Google Scholar]
- 30.Suma S, Furuta M, Yamashita Y, Matsushita K. Aging, Mastication, and Malnutrition and Their associations with cognitive disorder: evidence from epidemiological data. Curr Oral Health Rep. 2019;6:89–99. [Google Scholar]
- 31.Alkhunizan M, Alkhenizan A, Basudan L. Prevalence of mild cognitive impairment and dementia in Saudi Arabia: A community-based study. Dement Geriatr Cogn Dis Extra. 2018;8:98–103. doi: 10.1159/000487231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9:63–75. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 33.Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. 2014;312:2551–2561. doi: 10.1001/jama.2014.13806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sweed HS, El-awam AE. Cognitive impairment among residents of elderly homes in Cairo, Egypt. MECP. 2010;84:1–6. [Google Scholar]
- 35.Afgin AE, Massarwa M, Schechtman E, Israeli-Korn SD, Strugatsky R, Abuful A, et al. High prevalence of mild cognitive impairment and Alzheimer's disease in arabic villages in northern Israel: impact of gender and education. J Alzheimers Dis. 2012;29:431–439. doi: 10.3233/JAD-2011-111667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zaitoun A, Al Ma'moun A, Sarhan M, Selim A, Mousa G. Epidemiological study of dementia after retirement. Egypt J Neurol Psychiatr Neurosurg. 2008;45:65–74. [Google Scholar]
- 37.Talhaoui A, Aboussaleh Y, Ahami A, Sbaibi R, Agoutim N. Association between malnutrition and cognitive impairment among Morocco's older adults. Open J Med Psychol. 2019;8:1–14. [Google Scholar]
- 38.Rizzi L, Rosset I, Roriz-Cruz M. Global epidemiology of dementia: Alzheimer's and vascular types. Biomed Res Int. 2014;2014:1–8. doi: 10.1155/2014/908915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sachs-Ericsson N, Blazer DG. The new DSM-5 diagnosis of mild neurocognitive disorder and its relation to research in mild cognitive impairment. Aging Ment Health. 2015;19:1–12. doi: 10.1080/13607863.2014.920303. [DOI] [PubMed] [Google Scholar]
- 40.Algabbani AM, Almubark R, Althumiri N, Alqahtani A, BinDhim N. The prevalence of cigarette smoking in Saudi Arabia in 2018. Food and Drug Regulatory Science Journal. 2018;1:1–13. [Google Scholar]
- 41.Robert AA, Al Dawish MA. The worrying trend of diabetes mellitus in Saudi Arabia: an urgent call to action. Curr Diabetes Rev. 2019;16:204–210. doi: 10.2174/1573399815666190531093735. [DOI] [PubMed] [Google Scholar]
- 42.Yusufali AM, Khatib R, Islam S, Alhabib KF, Bahonar A, Swidan HM, et al. Prevalence, awareness, treatment and control of hypertension in four Middle East countries. J Hypertens. 2017;35:1457–1464. doi: 10.1097/HJH.0000000000001326. [DOI] [PubMed] [Google Scholar]
- 43.AlQuaiz AM, Kazi A, Youssef RM, Alshehri N, Alduraywish SA. Association between standardized vitamin 25 (OH) D and dyslipidemia: a community-based study in Riyadh, Saudi Arabia. Environ Health Prev Med. 2020;25:1–9. doi: 10.1186/s12199-019-0841-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin JS, O'Connor E, Rossom RC, Perdue LA, Eckstrom E. Screening for cognitive impairment in older adults: a systematic review for the US Preventive Services Task Force. Ann Intern Med. 2013;159:601–612. doi: 10.7326/0003-4819-159-9-201311050-00730. [DOI] [PubMed] [Google Scholar]
- 45.Etgen T, Sander D, Bickel H, Förstl H. Mild cognitive impairment and dementia: the importance of modifiable risk factors. Dtsch Arztebl Int. 2011;108:743–750. doi: 10.3238/arztebl.2011.0743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mukadam N, Cooper C, Kherani N, Livingston G. A systematic review of interventions to detect dementia or cognitive impairment. International journal of geriatric psychiatry. 2015;30:32–45. doi: 10.1002/gps.4184. [DOI] [PubMed] [Google Scholar]
- 47.Huntley J, Corbett A, Wesnes K, Brooker H, Stenton R, Hampshire A, et al. Online assessment of risk factors for dementia and cognitive function in healthy adults. Int J Geriatr Psychiatry. 2018;33:e286–e293. doi: 10.1002/gps.4790. [DOI] [PubMed] [Google Scholar]
- 48.Han R, Tang Z, Ma L. Related factors of cognitive impairment in community-dwelling older adults in Beijing Longitudinal Study of Aging. Aging Clin Exp Res. 2019;31:95–100. doi: 10.1007/s40520-018-0943-8. [DOI] [PubMed] [Google Scholar]
- 49.Miyawaki CE, Liu M. Gender differences in cognitive impairment among the old and the oldest-old in China. Geriatr Gerontol Int. 2019;19:586–592. doi: 10.1111/ggi.13666. [DOI] [PubMed] [Google Scholar]
- 50.Chang Y-H, Wu I-C, Hsiung CA. Reading activity prevents long-term decline in cognitive function in older people: evidence from a 14-year longitudinal study. Int Psychogeriatr. 2002;5:1–12. doi: 10.1017/S1041610220000812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cheng GH, Chan A, Lo JC. Importance of social relationships in the association between sleep duration and cognitive function: data from community-dwelling older Singaporeans. Int Psychogeriatr. 2018;30:893–901. doi: 10.1017/S1041610217001041. [DOI] [PubMed] [Google Scholar]
- 52.Evans IEM, Llewellyn DJ, Matthews FE, Woods RT, Brayne C, Clare L, et al. Living alone and cognitive function in later life. Arch Gerontol Geriatr. 2019;81:222–233. doi: 10.1016/j.archger.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 53.Xue B, Cadar D, Fleischmann M, Stansfeld S, Carr E, Kivimaki M, et al. Effect of retirement on cognitive function: the Whitehall II cohort study. Eur J Epidemiol. 2018;33:989–1001. doi: 10.1007/s10654-017-0347-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang Y, Gu Y, Zhang Y, Liu X, Zhang Y, Wu W, et al. Effect of sociodemographic and physical activity on cognitive function in older adults: A nationwide cross-sectional survey. Int J Geriatr Psychiatry. 2019;34:243–248. doi: 10.1002/gps.4932. [DOI] [PubMed] [Google Scholar]
- 55.Roehr S, Riedel-Heller SG, Kaduszkiewicz H, Wagner M, Fuchs A, van der Leeden C, et al. Is function in instrumental activities of daily living a useful feature in predicting A lzheimer's disease dementia in subjective cognitive decline? Int J Geriatr Psychiatry. 2019;34:193–203. doi: 10.1002/gps.5010. [DOI] [PubMed] [Google Scholar]
- 56.Sampaio A, Marques-Aleixo I, Seabra A, Mota J, Marques E, Carvalho J. Physical fitness in institutionalized older adults with dementia: association with cognition, functional capacity and quality of life. Aging Clin Exp Res. 2020;32:2329–2338. doi: 10.1007/s40520-019-01445-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lim SC, Gan WY, Chan YM. The effects of socio-demographic characteristics, nutritional status, physical activity and physical function on cognitive function of community-dwelling older adults in the Klang Valley, Malaysia. Malaysian Journal of Medicine and Health Sciences. 2020;16(Suppl 6):163–169. [Google Scholar]
- 58.Arvanitakis Z, Capuano AW, Bennett DA, Barnes LL. Body Mass Index and Decline in Cognitive Function in Older Black and White Persons. J Gerontol A Biol Sci Med Sci. 2018;73:198–203. doi: 10.1093/gerona/glx152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chavarro-Carvajal D, Reyes-Ortiz C, Samper-Ternent R, Arciniegas AJ, Gutierrez CC. Nutritional assessment and factors associated to malnutrition in older adults: a cross-sectional study in Bogota, Colombia. J Aging Health. 2015;27:304–19. doi: 10.1177/0898264314549661. [DOI] [PubMed] [Google Scholar]
- 60.Yu W, Yu W, Liu X, Wan T, Chen C, Xiong L, et al. Associations of cognitive condition with nutritional status in an elderly population: an analysis based on a 7-year database in Chongqing, the Southwest of China. BMC Geriatr. 2020:1–22. [Google Scholar]
- 61.World Health Organization. Age-Friendly Primary Health Care Centres Toolkit. 2020. [Accessed October 20]. Updated 2008. Available from URL: https://www.who.int/ageing/publications/upcoming_publications/en/


