The increased research on bat coronaviruses after severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) allowed the very rapid identification of SARS-CoV-2. This is an excellent example of the importance of knowing viruses harbored by wildlife in general, and bats in particular, for global preparedness against emerging viral pathogens.
KEYWORDS: Viral metagenomics, bat rotavirus, rotavirus genetic diversity, SA11, zoonosis
ABSTRACT
Bats host many viruses pathogenic to humans, and increasing evidence suggests that rotavirus A (RVA) also belongs to this list. Rotaviruses cause diarrheal disease in many mammals and birds, and their segmented genomes allow them to reassort and increase their genetic diversity. Eighteen out of 2,142 bat fecal samples (0.8%) collected from Europe, Central America, and Africa were PCR-positive for RVA, and 11 of those were fully characterized using viral metagenomics. Upon contrasting their genomes with publicly available data, at least 7 distinct bat RVA genotype constellations (GCs) were identified, which included evidence of reassortments and 6 novel genotypes. Some of these constellations are spread across the world, whereas others appear to be geographically restricted. Our analyses also suggest that several unusual human and equine RVA strains might be of bat RVA origin, based on their phylogenetic clustering, despite various levels of nucleotide sequence identities between them. Although SA11 is one of the most widely used reference strains for RVA research and forms the backbone of a reverse genetics system, its origin remained enigmatic. Remarkably, the majority of the genotypes of SA11-like strains were shared with Gabonese bat RVAs, suggesting a potential common origin. Overall, our findings suggest an underexplored genetic diversity of RVAs in bats, which is likely only the tip of the iceberg. Increasing contact between humans and bat wildlife will further increase the zoonosis risk, which warrants closer attention to these viruses.
INTRODUCTION
Rotaviruses are the leading cause of diarrheal disease in the young of mammals and birds. In humans, rotaviruses are responsible for 122,000 to 216,000 deaths in under-5-year-old infants on a yearly basis, mainly in developing countries (1). The Rotavirus genus belongs to the family Reoviridae and contains 9 species designated A to I (RVA to RVI). The rotavirus genome consists of 11 dsRNA segments encoding 6 structural viral proteins (VP1-6) and 6 nonstructural proteins (NSP1-6) (2).
The RVA outer capsid antigens, VP4 and VP7, are used for a dual classification system defining P-genotype (VP4 is protease sensitive) and G-genotype (VP7 is glycosylated), respectively (2). However, as gene reassortment is a common phenomenon after coinfection for viruses with segmented genomes, a more comprehensive classification approach became necessary to better account for the genome evolution and genetic diversity of RVAs. In 2008, a nucleotide sequence-based, complete genome classification system was developed for RVA, defining genotypes for each of the 11 gene segments. These genotypes allowed extending the dual classification to a full “genotype constellation” classification (3, 4). The gene assignments are reported as Gx-P[x]-Ix-Rx-Cx-Mx-Ax-Nx-Tx-Ex-Hx, where “x” denotes the particular genotype. The Rotavirus Classification Working Group (RCWG) was formed in order to assign new genotypes to rotavirus genes that could not be assigned to an established genotype (5).
Accumulating whole-genome sequencing data demonstrated that there are typical genotype constellations (GCs) present in most animal species. Two of them, Wa-like and DS-1-like, are responsible for most of the human disease and designated I1-R1-C1-M1-A1-N1-T1-E1-H1 and I2-R2-C2-M2-A2-N2-T2-E2-H2, respectively, for the non-G/P genotypes (3). Furthermore, various animal species are known to have specific GCs such as I2-R2-C2-M2-A3/A11/A13-N2-T6-E2-H3 for cattle and other even-toed ungulates (6), I1/I5-R1-M1-A1/A8-N1-T1/T7-E1-H1 for swine (3, 7), I2/I6-R2-C2-M3-A10-N2-T3-E2/E12-H7 for horses (8), and I3-R3-C3-M3-A3/A9-N2-T3-E3-H3/H6 for cats and dogs (9). Partially shared genotype patterns between established GCs, such as Wa-like human RVA strains and porcine RVAs, as well as DS-1-like human RVA strains and bovine RVAs, suggest a common origin and important zoonotic transfer events in the past (3).
Bats belong to the Chiroptera order, which is the second largest order of mammals (10). They harbor a high diversity of viruses, among which are zoonotic viruses such as lyssavirus, Hendra and Nipah viruses, filovirus, and several coronaviruses (11–17). Given their great population densities, migration ability, and proximity to human habitats, bats are often screened for emerging and reemerging viral pathogens (18, 19). Such screenings have resulted in the sporadic identification of rotavirus strains in bats in the last decade. There are reports of RVH in South Korean bats (20) and Cameroonian bats (21), and a novel rotavirus species (tentatively named RVJ) was identified from Schreiber's bats in Serbia (22); however, RVA is the most commonly detected species and there are currently more than 20 bat RVA strains identified. In 2010, Esona and colleagues reported the first partially sequenced RVA strain (RVA/Bat-wt/KEN/KE4852/07/2007/G25P[6]) in a Kenyan Eidolon helvum (straw-colored fruit bat), and the majority of retrieved gene segments were only distantly related to known mammalian RVA strains (23). During the subsequent decade, sporadic and scattered reports have been published about RVA strains in bats collected from serum, gut, and fecal samples in insectivorous and fruit bats. Several of these reports came from Chinese studies (24–27), but bat RVAs were also detected and (partially) characterized from France (28), Brazil (29), Zambia (30, 31), Cameroon (32), Kenya (33), and Saudi Arabia (34). These studies investigated samples from a variety of bat families, such as Rhinolophidae (24, 30), Hipposideridae (25, 26), Vespertilionidae (26, 28), Molossidae, Phyllostomidae (29), Emballonuridae (26, 33), Pteropodidae (23, 31–34), and Rhinopomatidae (34). From some of these novel bat RVA strains, a few gene segments were sequenced, whereas other strains were sequenced completely, often resulting in one or multiple novel genotypes (23, 26, 29, 31, 32).
Even though RVAs are generally considered to have a relatively restricted host range, a number of unusual strains have been described in the literature, suggestive of interspecies transmissions involving bat RVA strains. One example is the RVA/Horse-wt/ARG/E3198/2008/G3P[3] strain that was isolated from a diarrheic foal in Argentina in 2008 (35). Although its GC was distantly related to feline/canine-like RVA strains at that time, two more recent publications showed a closer relationship with Chinese bat RVA strains in several gene segments (24, 25). A second example was the unusual human G3P[3] RVA strain RVA/Human-wt/JPN/12638/2014/G3P[3], isolated from a 4-year-old child with severe gastroenteric symptoms in Japan. Three of its eleven gene segments were closely related to a South African bat RVA strain, suggesting a reassortment involving a bat RVA strain (36). A third example are two unique G20 human RVA strains, RVA/Human-wt/ECU/Ecu534/2006/G20P[28] (37) and RVA/Human-wt/SUR/2014735512/2013/G20P[28] (38). The recent identification of the G20 genotype in a Brazilian bat RVA strain (RVA/Bat-wt/BRA/3081/2013/G20P[x]) also suggests a potential bat reservoir for these human strains (29).
All in all, slowly emerging data on bat RVA strains start to show that some unusual human and animal RVA strains might actually have been derived from bats. Therefore, the global surveillance of novel and reassorted RVA bat strains has to continue in order to better understand the genetic diversity of bat RVA strains, as well as to maintain both public and animal health. Here, we report identification of 11 bat RVA strains from Bulgaria, Gabon, Ghana, and Costa Rica, suggesting evidence of multiple reassortment and host switching events from bats to bats and to other mammals.
RESULTS AND DISCUSSION
Bats are known hosts of various human pathogens, including viruses such as rabies virus, henipaviruses, Marburg virus, SARS-CoV and MERS-CoV (11–17). In addition, there have been sporadic reports on several other RNA viruses in bats, such as paramyxoviruses, picornaviruses, orthoreoviruses, and astroviruses (39–42). Bat rotaviruses have also been sporadically reported during the last decade and it is rotavirus A (RVA) that has been the most frequently reported rotavirus species. This is not very surprising, given that RVA has been detected in a wide range of mammals and birds (43–45). Furthermore, there are plenty of examples in the literature of this enteric pathogen being capable of interspecies transmission, sometimes in combination with reassortments, between various mammalian species, including humans (46). On some occasions, such animal-derived gene segments (e.g., VP7 genotypes from cattle [G8] and pigs [G9 and presumably G12]) or complete GCs (AU-1 like strains from cats) have become established in the human population. This established circulation either happened in a limited geographical region (AU-1 like or G8) or worldwide, such as the epidemiologically important human-pathogenic G9 and G12 RVAs (47, 48).
In order to further investigate the potential of bat RVA strains to spill over between bats or toward other mammalian species, we investigated RVA strains from over 2,000 bats, spanning five countries on three continents. The bat fecal samples that were collected from Bulgaria, Romania, Germany, Gabon, Ghana, and Costa Rica were screened for RVA using a nested reverse transcriptase PCR (RT-PCR) targeting a short piece of the highly conserved polymerase gene (VP1, Table S1 in the supplemental material). This screening yielded 18 positive samples out of the 2,142 screened samples (0.8%) (Table S2). The RVA detection rate per species ranged from 0 to 1.1%, except for Macronycteris gigas (previously Hipposideros gigas) (14.9%). The reason for this higher detection rate is unknown, but could be due to: (i) better matching oligonucleotides used for the detection, (ii) an ongoing RVA outbreak in the sampled caves, or (iii) higher circulation of enteropathogens in M. gigas. RVA-positive samples were collected from five bat families: Pteropodidae, Rhinolophidae, Hipposideridae, Phyllostomidae, and Vespertilionidae, which originated from all sampling sites except Romania.
RT-PCR oligonucleotides for the initial rotavirus screening against VP1. Download Table S1, DOCX file, 0.01 MB (13.4KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Taxonomical annotation, sampling time and location, and RVA PCR detection information of the bat samples. Download Table S2, DOCX file, 0.02 MB (23.7KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Eleven near-complete bat RVA genomes, including six novel genotypes.
From 16 of the RVA-positive samples, a sufficient amount of sample was available for complete viral genome sequencing using the NetoVIR protocol (Table S3). A total of 118.9 million paired-end (PE) reads (2 × 150 base pairs) and an average of 7 million PE reads/sample were generated by Illumina sequencing (Table 1). Four samples from Gabon and one sample from Germany did not yield any RVA contigs longer than 500 bp and were therefore not investigated further. From 11 samples, near-complete RVA genomes could be retrieved. These RVA samples belonged to 5 out of the 46 tested bat species (10.8%) and 4 out of the 10 (40%) tested families, as shown in the bat phylogenetic tree (Table S2, Fig. S1). The percentage of reads mapping to RVA in each sample ranged from 0 to 90% (Table 1).
TABLE 1.
Meta-data and NGS summary of the sequenced RVA-positive samples
| Sample ID | Location | Country | Year | Bat species | Bat diet | Raw reads | Trimmed reads | No. of RVA readsa | RVA read percentageb |
|---|---|---|---|---|---|---|---|---|---|
| BB89-15 | Elenas Cave | Bulgaria | 2008 | Rhinolophus blasii | Insect | 13,508,743 | 3,850,458 | 56,536 | 1.5% |
| BR89-60 | Roman Horse Cave | Bulgaria | 2008 | Rhinolophus euryale | Insect | 11,812,353 | 3,224,700 | 2,278 | 0.1% |
| SW78-39 | Wahlstorf, SH | Germany | 2008 | Myotis daubentonii | Insect | 5,720,709 | 5,411,241 | 0 | 0.0% |
| GKS-660 | Zadie | Gabon | 2009 | Hipposideros caffer | Insect | 7,356,697 | 5,404,115 | 4 | 0.0% |
| GKS-897 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 6,994,665 | 3,938,299 | 30,929 | 0.8% |
| GKS-912 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 4,018,151 | 2,968,694 | 1,236,102 | 41.6% |
| GKS-926 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 6,346,691 | 4,955,591 | 4,479,073 | 90.4% |
| GKS-929 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 993,739 | 718,192 | 315,056 | 43.9% |
| GKS-934 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 7,341,726 | 5,454,901 | 35,259 | 0.7% |
| GKS-941 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 5,923,863 | 3,741,568 | 442,380 | 11.8% |
| GKS-942 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 8,363,558 | 6,453,805 | 0 | 0.0% |
| GKS-953 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 4,361,523 | 3,358,374 | 22 | 0.0% |
| GKS-954 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 7,358,552 | 5,683,659 | 201,335 | 3.5% |
| GKS-955 | Faucon | Gabon | 2009 | Macronycteris gigas | Insect | 5,704,559 | 3,820,529 | 23 | 0.0% |
| K212 | Kumasi | Ghana | 2009 | Eidolon helvum | Fruit | 8,367,278 | 5,189,608 | 17,206 | 0.3% |
| KCR10-93 | Orosi | Costa Rica | 2010 | Carollia perspicillata | Insect | 7,731,234 | 2,235,422 | 12,179 | 0.5% |
| Average | 6,994,003 | 4,150,572 | 426,774 | 12.2% | |||||
| Total | 118,929,778 | 67,370,384 | 6,828,382 |
Number of unique trimmed reads mapping to RVA genomic segments in the corresponding sample.
Proportion of RVA reads to all the reads in the corresponding sample.
RVA-positive bat samples detected by targeted RT-PCR and having undergone viral metagenomics. Download Table S3, DOCX file, 0.01 MB (14.6KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
RVA-positive bat families and species. Download FIG S1, DOCX file, 0.1 MB (97.8KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
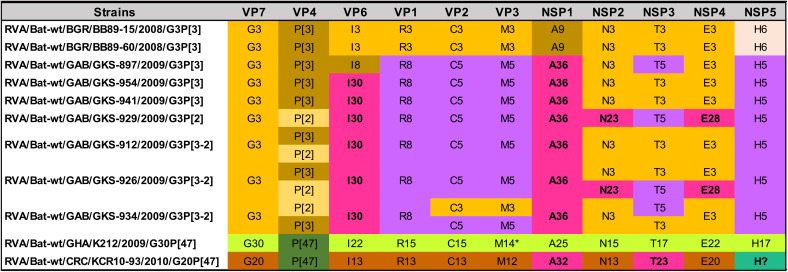
The GCs of the 11 bat RVA strains are shown in Table 2. The genotype assignments, including novel VP6 (I30), NSP1 (A36), NSP2 (N23), and NSP4 (E28) genotypes for some of the Gabonese strains and NSP1 (A32) and NSP3 (T23) genotypes for the strain from Costa Rica were made according to the guidelines determined by the RCWG (4). Although the NSP5 gene segment of RVA/Bat-wt/CRC/KCR10-93/2010/G20P[47] most likely also represents a novel genotype, we were not able to retrieve the complete open reading frame (ORF) (despite several attempts using RT-PCR and Sanger sequencing), which is required for the assignment of a novel genotype (5). Particular GCs were identified in different geographic locations (Table 2). Gabonese strains were similar to each other, with certain genotypes shared with the Bulgarian strains (G3, P[3], C3, M3, N3, T3, and E3). However, they do not cluster phylogenetically closely together (see above), indicating nonrecent reassortment events. KCR10-93 also possessed a unique GC, except for the VP4 genotype P[47], which was shared with the Ghanaian strain. Interestingly, these two VP4 genes were very closely related (see above), suggesting a recent reassortment event. Gabonese GKS-912, GKS-926, and GKS-934 appeared to have a coinfection, as multiple genotypes were identified in these samples for VP2, VP3, VP4, NSP2, NSP3, and NSP4. For GKS-934, two near-complete VP7 gene segments were identified, both belonging to the G3 genotype and yet having substantial nucleotide-level dissimilarity (19%, see below). This was also the case for K212, possessing two distinct M14 genotypes with 12% nucleotide sequence distance.
TABLE 2.
Color-coded GCs of the bat RVA strains identified in this studya
In some samples, two different variants of the same gene segments were identified, suggesting coinfections. K212 possessed two distinct VP3 gene segments belonging to the same M14 genotype (indicated with an asterisk). The NSP5 gene of KCR10-93 could not be assigned to any of the established genotypes, as the complete ORF could not be determined, and therefore “H?” is used to indicate the genotype.
At least seven distinct bat RVA genotype constellations.
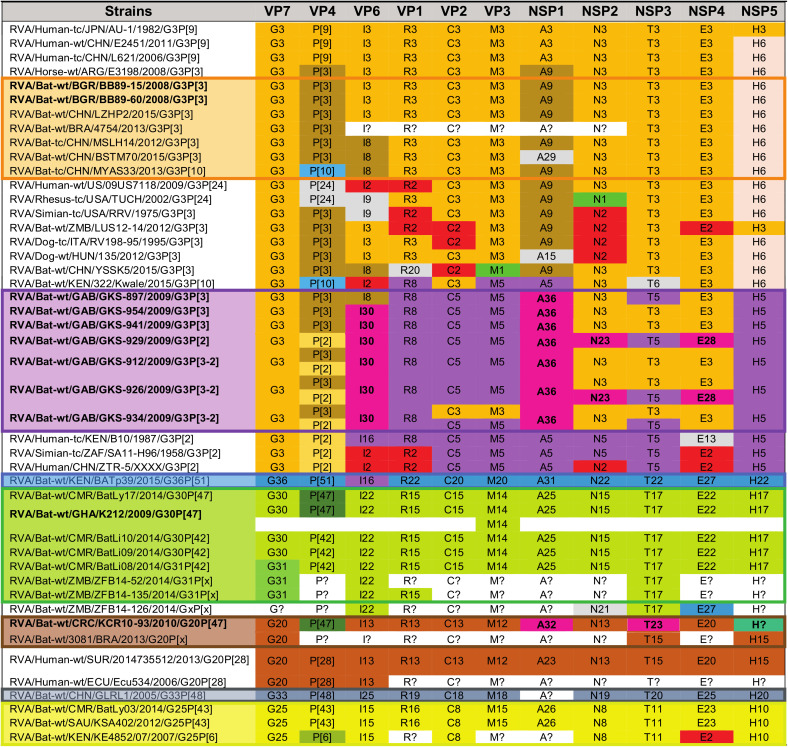
Despite that most animal species, including humans, have a limited number of typical RVA GCs, the RVAs harbored by bats show a great genetic diversity. Combining our data with previously published bat RVA genomes showed there are at least 7 distinct bat RVA GCs circulating in the bat population (Table 3), ranging from completely unique to partially overlapping with each other. The Bulgarian RVA/Bat-wt/BGR/BB89-15/2008/G3P[3] and RVA/Bat-wt/BGR/BR89-60/2008/G3P[3] strains were identical or very similar to MSLH14-like RVA strains from China and a partially sequenced strain from Brazil (orange GC in Table 3). Even though at least three of the samples from Gabon possessed more than one RVA strain, they possessed at least three distinct but related GCs (purple GC in Table 3) not previously identified in bats. The RVA/Bat-wt/GHA/K212/2009/G30P[47] strain (green GC in Table 3) was identical or very similar to several previously identified Cameroonian bat RVA strains (32), as well as some partially sequenced bat RVA strains from Zambia (31). RVA/Bat-wt/CRC/KCR10-93/2010/G20P[47] had a distinct GC (brown GC in Table 3), including at least two previously undescribed genotypes, and shared the G20 genotype with RVA/Bat-wt/BRA/3081/2013/G20P[x]. Of interest was the P[47] genotype, which was shared with two African strains from the green GC. The yellow GC in Table 3 was composed of two strains with identical genotypes, RVA/Bat-wt/CMR/BatLy03/2014/G25P[43] and RVA/Bat-wt/SAU/KSA402/2012/G25P[43], detected in Cameroon and Saudi Arabia, respectively, as well as the partially sequenced strain RVA/Bat-wt/KEN/KE4852/2007/G25P[6] from Kenya. Two GCs (blue and dark gray in Table 3) were only represented by a single bat strain from Kenya (RVA/Bat-wt/KEN/BATp39/2015/G36P[51]) and China (RVA/Bat-wt/CHN/GLRL1/2005/G33P[48]), respectively (Table 3).
TABLE 3.
Color-coded GCs for the bat RVA strains identified in this study, previously published bat RVA strains, as well as a selection of RVA strains from other host species potentially related to batsa
The “[letter code]?” notation is used to denote nonsequenced segments or unassigned genotypes. The genotypes colored in light gray are less relevant due to a lack of (in)direct genomic relationship with the bat RVAs identified in the current study. The strain names are color-matched with the corresponding GCs (orange, purple, blue, green, brown, dark gray, and yellow).
Reassortments among bat RVA strains.
Though the GCs are somewhat conserved, there are ample examples for the occurrence of reassortments. In the orange GC, there are some unusual genotypes such as P[10] for VP4, R20 for VP1, and A29 for NSP1 (Table S4a and S4b), which are most likely the results of reassortment events with currently unknown RVA strains (25, 26). Reassortment also takes place between different bat RVA GCs, albeit to a limited extent. For example, RVA/Bat-wt/GAB/GKS-897/2009/G3P[3] is the only strain from the purple GC with the I8 VP6 genotype, which is shared with several strains from the orange GC (RVA/Bat-tc/CHN/MSLH14/2012/G3P[3], RVA/Bat-wt/CHN/BSTM70/2015/G3P[3], RVA/Bat-tc/CHN/MYAS33/2013/G3P[10], and RVA/Bat-wt/CHN/YSSK5/2015/G3P[3]), suggesting a reassortment event. A second example is the shared P[47] VP4 genotype between RVA/Bat-wt/GHA/K212/2009/G30P[47] and RVA/Bat-wt/CMR/BatLy17/2014/G30P[47] (green GC) and RVA/Bat-wt/CRC/KCR10-93/2010/G20P[47] (brown GC) (Table 2). Interestingly, these last three strains were 97 to 100% identical to each other on the nucleotide level for VP4, suggesting a recent reassortment event. Finally, there are also a few bat RVA strains with unusual genotype compositions that do not clearly fall into the seven described GCs. RVA strains RVA/Bat-wt/ZMB/LUS12-14/2012/G3P[3] and RVA/Bat-wt/CHN/YSSK5/2015/G3P[3] possess several genotypes typical for the orange GC, in addition to several other genotypes of unknown origin (Table S4b). Finally, RVA/Bat-wt/KEN/322/Kwale/2015/G3P[10] possesses both genotypes typical to the orange and purple GCs, in addition to some atypical bat RVA genotypes.
Examples of reassortments and unusual genotype constellations among bat RVA strains and distinct RVA genotype constellations in the same bat species. Download Table S4, DOCX file, 0.02 MB (19.6KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
RVA interspecies transmission in bats and potential host range restriction.
As demonstrated by the orange GC, RVAs belonging to certain bat families might undergo multiple host switching events. The Bulgarian RVA strains were isolated from rhinolophid bats, whereas the Chinese MSLH14-like strains were found in bats from the Rhinolophidae, Hipposideridae, and Emballonuridae families (Table S4a).
In addition to RVAs potentially being able to infect multiple bat families, individual bat families could also harbor more than one GC, as is shown in Table S4c. Pteropodid bats harbor completely unique GCs (green and yellow), suggesting that the associated RVA strains have a high epidemiologic fitness in these populations. This further indicates that the Pteropodidae, which includes the straw-colored fruit bats, has been a substantial virus reservoir for a long time already, as also shown for Marburg virus, Hendra and Nipah viruses (12–14).
Wide geographic dispersal of bat RVA GCs.
The global distribution of the bat RVA GCs revealed several patterns regarding RVA circulation in bats, as shown in Fig. 1. Bat RVAs belonging to the brown, purple, blue, and dark gray GCs have so far only been identified in Costa Rica (and perhaps Brazil), Gabon, Kenya, and China, respectively. On the other hand, the green and yellow GCs were confirmed to be further dispersed, from Cameroon to Saudi Arabia (G25P[43]), and from Ghana and Cameroon to Zambia, respectively, as was previously suggested by Sasaki et al. (31). However, highly similar RVA strains belonging to the orange MSLH14-like GCs span at least three different continents and subcontinents, e.g., Asia, Europe, and possibly Central America. Furthermore, it was also shown that RVA strains with distinct GCs could cocirculate in the same region, as is the case in Cameroon (green, yellow, and purple GCs) and China (orange and dark gray GCs) (Fig. 1).
FIG 1.
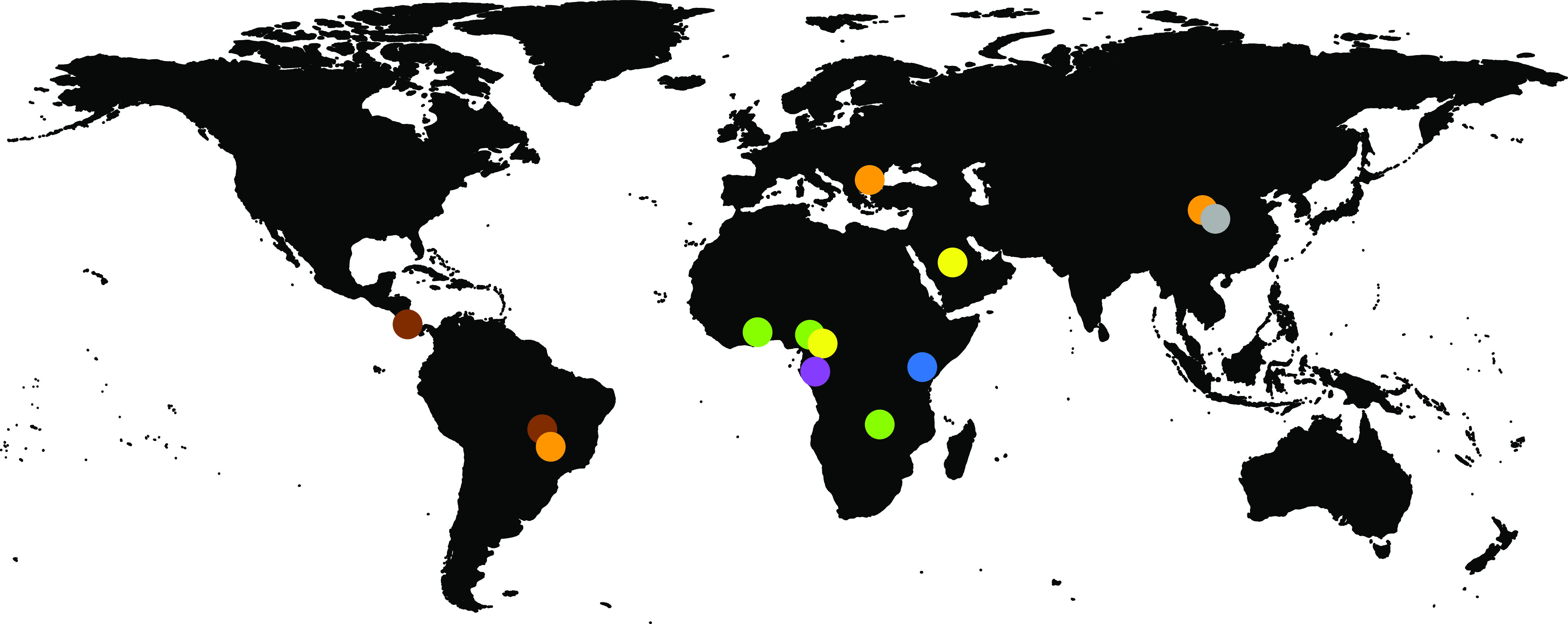
Geographic distribution of the currently known bat RVA GCs. The colored dots on the map represent the circulating genotypes at the specified locations according to the GCs shown in Table 3.
With powered flight, migratory bats can travel long distances between summer and winter roosts, for foraging, and for searching for a mate (49). Among long-distance migratory bats, E. helvum can cover a range of 270 to 2,500 km (50), and vespertilionid “tree bats” and the subtropical/tropical molossid bats can fly over 1,000 km (51, 52). Global distribution and intercontinental bat virus transfers are also typical of other bat viruses (53). In addition to migration across vast distances, the fact that some distinct GCs seem to have overlapping geographical ranges (such as in China and West Africa in Fig. 1) suggest a fitness advantage for these particular genotypes occurring together. However, there is also ample evidence of gene reassortment events among established GCs (e.g., P[47] in the green and brown GCs, or I8 in the purple and orange GCs), or with RVA strains of currently unknown origin (e.g., A29, A15, or E27).
It is clear that more bats should be sampled in order to have a comprehensive understanding of the driving and restricting forces of bat RVA genetic diversity, or the lack thereof. The detection of P[47] reassortment between Ghanaian and Costa Rican bat RVAs, which are located more than 9,000 km apart, cannot only be explained by the flight ability of bats, but rather the lack of sampling between these two locations. We hypothesize that with the increasing bat RVA sequencing efforts, the geographical and host range of most GCs (such as the blue, dark gray, yellow, and brown) will be significantly expanded.
Potential of interspecies transmissions of bat RVA to mammalian hosts.
We further investigated whether there is potential for unusual RVA strains detected in other mammals (including humans) to be a result of an interspecies transmission from bat strains identified in the current and other studies (Table 3).
(a) Likely transmission of bat RVA strains to a horse. In 2013, Miño and colleagues reported an unusual Argentinian equine G3P[3] RVA strain, RVA/Horse-wt/ARG/E3198/2008/G3P[3]. Based on the GC, it was speculated to have a common ancestor with both feline/canine RVA strains as well as the unusual rhesus RVA strain RRV. However, the nucleotide identities were below 90% for most of the genome segments, suggesting that the original host may not be identified yet (35). When more bat RVA genomes became available in subsequent years, Xia and colleagues, and later also Biao He and colleagues, suggested that E3198 might be of bat origin, based on the GCs and nucleotide similarities (25, 26). The close genetic relationship between E3198 and the Bulgarian strains presented here, across all 11 gene segments, might further suggest a bat origin of this unusual equine RVA strain (nucleotide similarities 87 to 97%) (Fig. 2, Fig. 3, Fig. 4, Fig. S2a).
FIG 2.
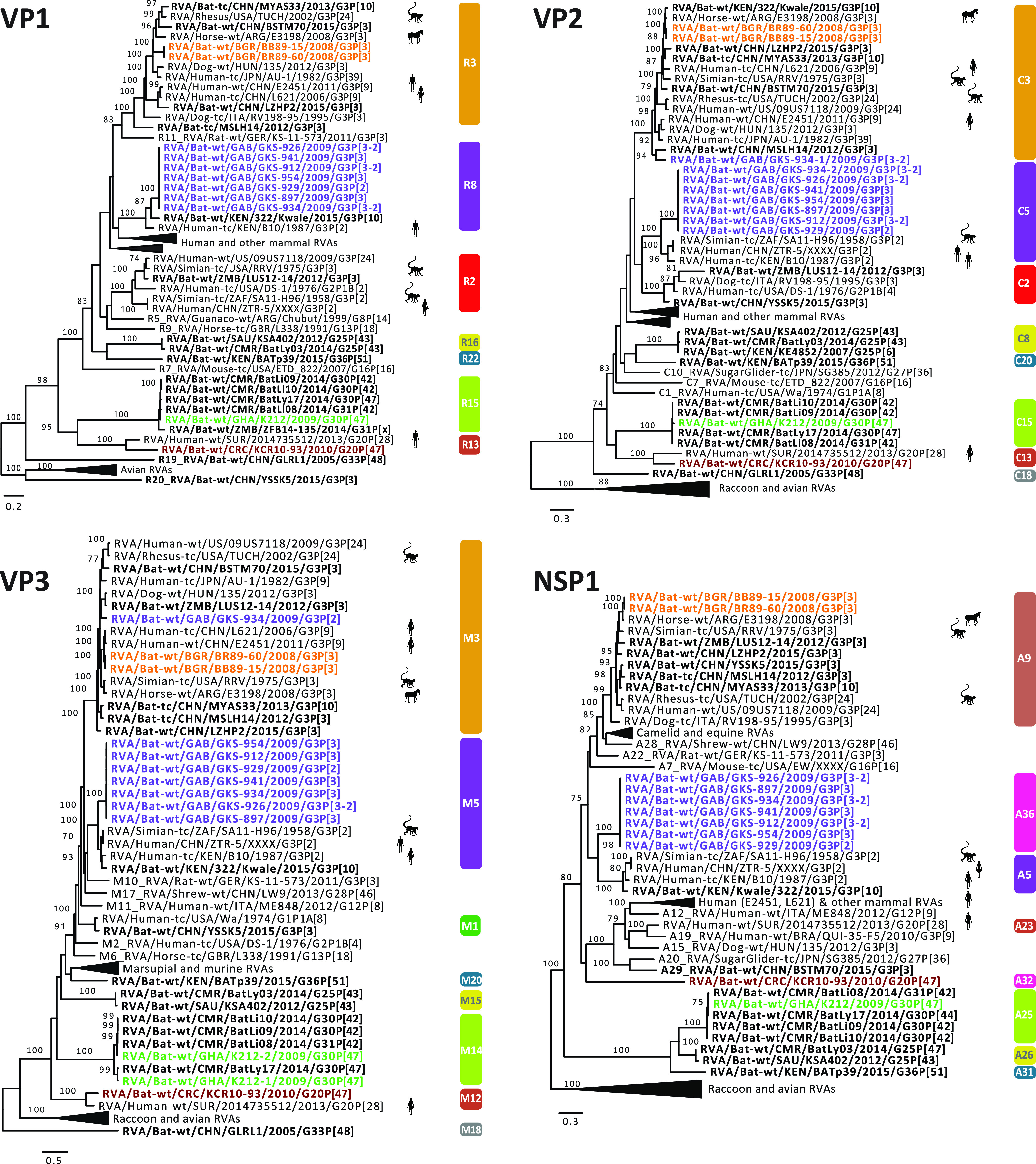
Maximum likelihood trees of the VP1, VP2, VP3, and NSP1 genes of the identified bat RVA strains with known human, bat, and other mammal RVAs. Only bootstrap values above 70 are shown. The genotypes are listed on the right side of the trees. The bat RVA strains identified in this study are shown in bold and colored to their GC, while previously reported bat RVA strains are shown in bold in black. Non-bat RVA strains related to the bat RVA strains identified in this study are marked with silhouettes indicating their host.
FIG 3.
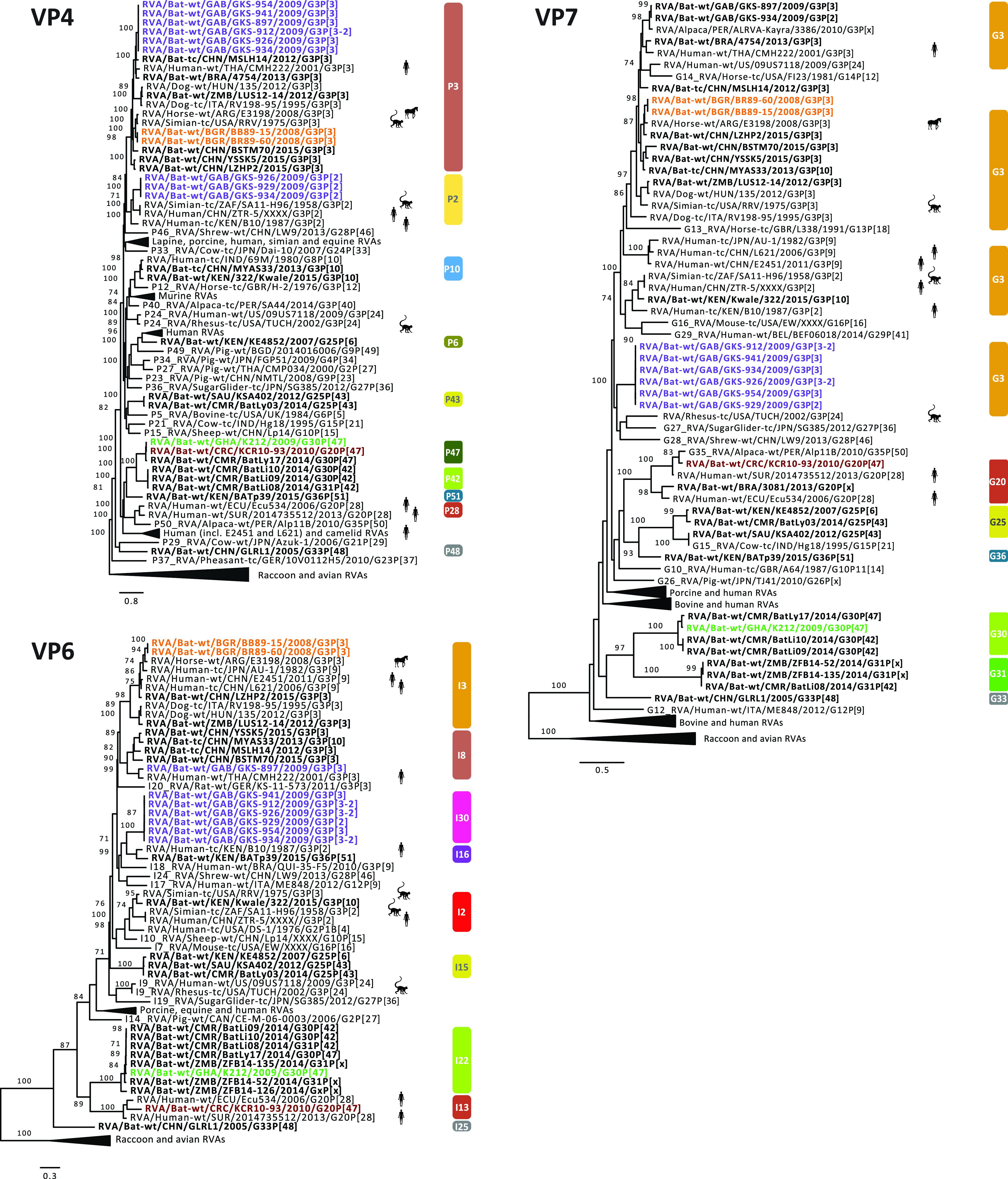
Maximum likelihood trees of the VP4, VP6, and VP7 genes of the identified bat RVA strains with known human, bat, and other mammal RVAs. Only bootstrap values above 70 are shown. The genotypes are listed on the right side of the trees. The bat RVA strains identified in this study are shown in bold and colored to their GC, while previously reported bat RVA strains are shown in bold in black. Non-bat RVA strains related to the bat RVA strains identified in this study are marked with silhouettes indicating their host.
FIG 4.
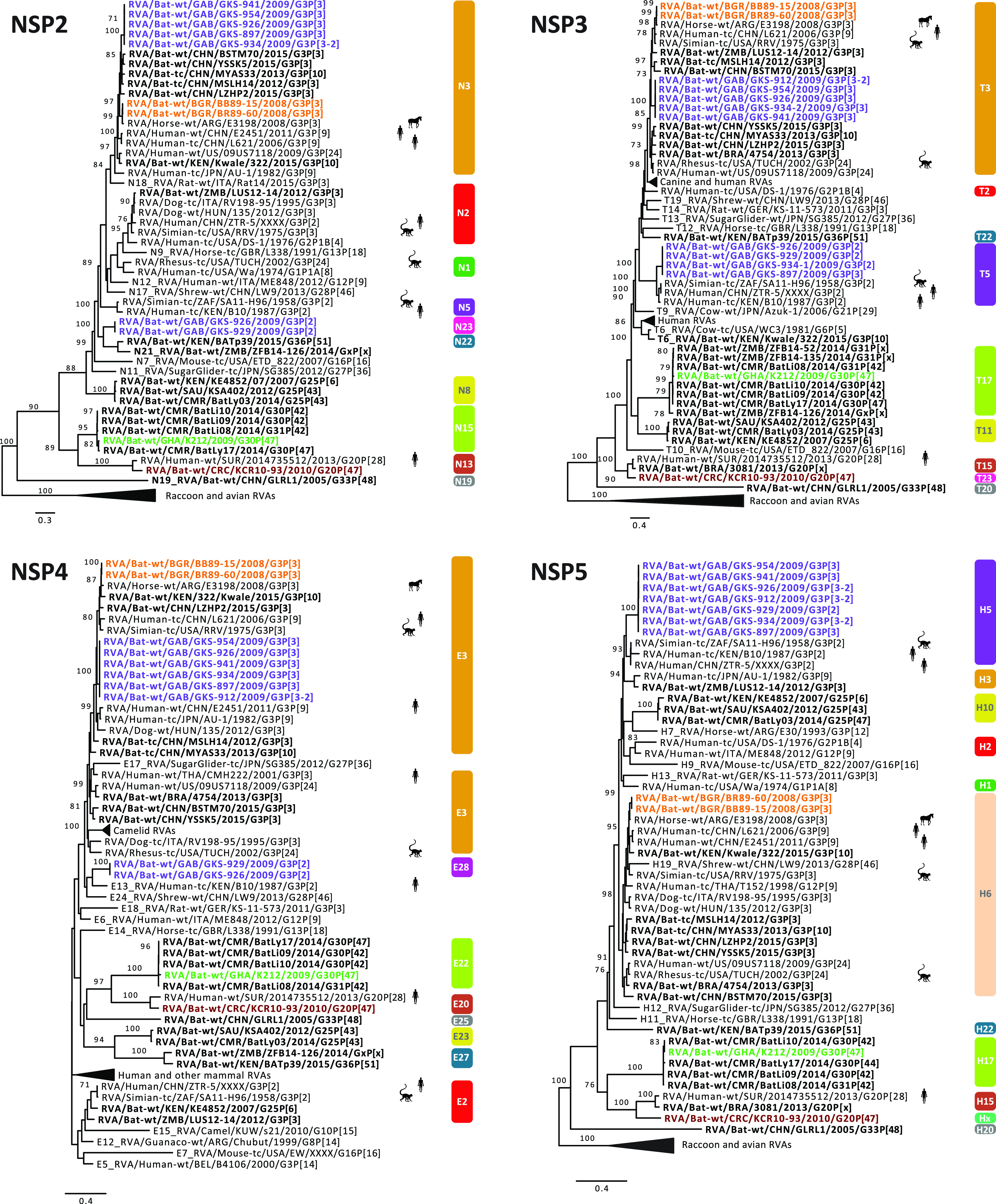
Maximum likelihood trees of the NSP2, NSP3, NSP4, and NSP5 genes of the identified bat RVA strains with known human, bat and other mammal RVAs. Only bootstrap values above 70 are shown. The genotypes are listed on the right side of the trees. The bat RVA strains identified in this study are shown in bold and colored to their GC, while previously reported bat RVA strains are shown in bold in black. Non-bat RVA strains related to the bat RVA strains identified in this study are marked with silhouettes indicating their host.
Heatmap of pairwise nucleotide identities (NI) of the unusual RVA strains RVA/Horse-wt/ARG/E3198/2008/G3P[3] (a), RVA/Simian-tc/ZAF/SA11-H96/1958/G3P[2] (b), RVA/Human-tc/KEN/B10/1987/G3P[2] (c), and RVA/Human-wt/SUR/2014735512/2013/G20P[28] (d). The gray color indicates the nucleotide identities that are below 0.6 or have lack of sequence information for the compared strain. Download FIG S2, DOCX file, 0.3 MB (293.6KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
(b) Unexpected high similarities between bat and simian RVA strains. RVA strain RVA/Simian-tc/ZAF/SA11-H96/1958/G3P[2] was isolated from an overtly healthy vervet monkey and has subsequently been used extensively as a laboratory strain in RVA growth, virulence, genome replication, and, in recent years, also reverse genetics research (54–56). However, its origin remained obscure, as related strains were never identified in vervet monkeys or other nonhuman primates. In 2011, Ghosh and colleagues identified an unusual RVA strain, RVA/Human-tc/KEN/B10/1987/G3P[2], from a child in Kenya, which shared 8 of 11 genotypes with SA11-H96. They speculated about a simian or other animal origin of this strain (57). Around the same time, a second human RVA strain, RVA/Human/CHN/ZTR-5/XXXX/G3P[2], nearly identical to SA11-H96 (Figure S2b), was deposited in GenBank as a potential vaccine candidate. However, the controversy about the origin of these SA11-like strains (SA11-H96, B10, and ZTR-5) remained. To our surprise, the purple GC described in this paper, containing only the bat RVA strains from Gabon, showed up to seven genotypes in common with these SA11-like strains (Table 3), with various degrees of nucleotide similarities (Fig. S2b and c). According to phylogenetic analyses, the bat RVAs from Gabon and Kenya clustered with B10 for the VP1, VP6, and NSP4 gene segments, and with all 3 strains (B10, SA11-H96, and ZTR-5) for VP2-4, NSP1, NSP3, and NSP5 (Fig. 2, Fig. 3, Fig. 4).
Not only for SA11-H96, but also for RVA/Simian-tc/USA/RRV/1975/G3P[3] and RVA/Rhesus-tc/USA/TUCH/2002/G3P[24], some close relationships with bat RVA strains were noted. The VP1, VP3, VP4, VP6, VP7, and NSP1-5 genes of RRV clustered closely with one or multiple bat and bat-related RVA strains (Fig. 2, Fig. 3, Fig. 4). For TUCH, the VP1, NSP1, and NSP5 gene segments also clustered close to bat RVA strains (Fig. 2, Fig. 3, Fig. 4).
The finding that the purple SA11-like GC was found in multiple bats in Gabon but only on a single occasion in vervet monkeys and in two unrelated human cases suggests bats as the prime suspect for being the major hosts of these viruses; this makes the monkey and humans strains putative examples of interspecies transmissions. It should, however, be noted that the phylogenetic clustering between these bat, simian, and human strains is still rather variable, and the nucleotide similarities are not as high as between bat RVA strains and RVA/Horse-wt/ARG/E3198/2008/G3P[3] (Figure S2a, Fig. 2, Fig. 3, Fig. 4), suggesting that more RVAs from yet-unsampled animal species will likely cluster in between. However, two other bat strains are of further interest: (i) the bat RVA strain RVA/Bat/KEN/322/Kwale/2015/G3P[10] (only available as a GenBank entry at this point) seems to have a mixed GC possessing characteristics of both the orange and purple GCs (Table 3), where the purple genotypes R8, M5, and A5 of 322/Kwale are of special interest as they are much more closely related to the SA11-like strains than the Gabon bat RVA strains (Fig. 2); and (ii) the bat RVA strain RVA/Bat-wt/KEN/BATp39/2015/G36P[51] (only available in GenBank) possesses a single purple genotype I16, and again this is more closely related to the SA11-like strain B10 compared to the Gabon RVA strains. Taken together, we speculate that with further RVA screenings in bat populations, more bat RVA strains that are closely related to the vervet monkey RVA strain SA11-H96 and human SA11-like RVA strains may be detected.
(c) Evidence of bat RVA strains transmitted to humans? The G3 genotype is usually associated with P[8] genotype in humans RVAs, and combinations such as G3P[3] and G3P[9] are only sporadically found in the human population (58). Nonetheless, in the 2000 to 2001 season, the VP4, VP7, VP6, and NSP4 genes were sequenced from a rare human strain RVA/Human-wt/THA/CMH222/2001/G3P[3], detected in a 2-year-old, severely diarrheic patient in Thailand (41). This strain was reported to have a VP7 gene closely related to RVA/Simian-tc/USA/RRV/1975/G3P[3] and a VP4 gene that was caprine-like. Subsequently, Xia and colleagues speculated that this strain is distinct from typical human RVA GCs and very likely shared a common ancestor with Asian bat RVAs (33). Our study provides further evidence for the bat origin of CMH222, as the VP6 I8 genotype of CMH222 is closely related to RVA/Bat-wt/GAB/GKS-897/2009/G3P[3] (Fig. 3).
Later, Wang and colleagues contributed to the list of unusual Southeast Asian human RVA strains possessing the G3P[9] genotypes; both the RVA/Human-tc/CHN/L621/2006/G3P[9] and RVA/Human-wt/CHN/E2451/2011/G3P[9] strains were isolated from a symptomatic adult and a symptomatic child, respectively (59). Complete genome analyses revealed a high genetic relatedness to strains of feline/canine origin for almost all 11 genes. L621 and E2451 also clustered near the aforementioned unusual RVA/Horse-wt/ARG/E3198/2008/G3P[3] for the VP3, VP6, NSP2, and NSP5 genes, and L621 also clustered with the E3198 NSP3 gene. Here, we observed that these atypical Asian human strains were also closely related to the Bulgarian bat RVA strains for VP3, VP6, NSP2, NSP4, and NSP5 and to Gabonese bat strains for NSP2, NSP3, and NSP4 of the orange GC (Fig. 2, Fig. 3, Fig. 4). These findings further substantiate, as well as complicate, the identification of the likely bat host from which the L621 and E2451 strains likely jumped to humans.
Following these potential zoonosis reports, Esona and colleagues also revealed remarkable findings in Latin America in 2018, where only limited bat RVA information is present to date (38). A human strain, RVA/Human-wt/SUR/2014735512/2013/G20P[28], was isolated in Suriname, and possessed a rare G20 genotype, which was also detected in an Ecuadorian human RVA strain (Ecu534) in 2006. Remarkably, 2014735512 showed high similarities with bat strain RVA/Bat-wt/BRA/3081/2013/G20P[x] for the VP7, NSP3, and NSP5 genes (Figure S2d) and it was speculated to be of bat origin, as these genotypes have not been detected in any other animal species so far. RVA/Bat-wt/CRC/KCR10-93/2010/G20P[47] showed nucleotide similarities for 9 out of 11 gene segments ranging from 82% to 92% with 2014735512, and they also phylogenetically clustered together, albeit not very closely (Fig. 2, Fig. 3, Fig. 4). Even though more evidence is needed, this finding might indicate a bat RVA origin for this rare human RVA strain.
Conclusions. Despite the limited number of bat species that have been screened for rotaviruses, a surprisingly large genetic diversity of RVA strains is presented in this study, including six novel genotypes. With increasing screening efforts, it is doubtless that this diversity will expand both genetically and geographically. We also presented multiple examples of close genetic relatedness of several mammalian and bat rotaviruses. The indicated zoonoses have—to the best of our knowledge—always been restricted to sporadic cases so far and have never resulted in major outbreaks in humans. However, it is believed that the rotavirus genotype constellations currently circulating in humans also have a common ancestor with animal rotaviruses, highlighting that interspecies transmissions allowed establishment in the human population and that this could happen again (3).
Another notable finding is that several gene segments of bat RVA strains and the simian SA11 RVA strain (the latter being used in global rotavirus research for decades) have a common origin. Furthermore, the SA11 strain has been recently used as the backbone of a RVA reverse genetics system, and is therefore likely to be used even more in the future. It would be intriguing to test whether or not SA11 grows well in bat cell lines, or in in vivo infection experiments.
MATERIALS AND METHODS
Sample collection.
Fecal samples were collected from 2,142 bats from 10 bat families, representing 46 bat species (Table S2 in the supplemental material). Sample collection took place in Ghana, Gabon, Bulgaria, Romania, Germany, and Costa Rica during 2008 to 2010 as part of investigations of other viruses in bats, such as coronavirus, astrovirus, and picornavirus, as described previously (53, 60–63). Bat species were determined by trained field biologists. For European and Costa Rican studies, bats were caught with mist nets, put into cotton bags, and fecal pellets are collected. Ghanaian fecal droppings were collected with plastic foil from the trees in which E. helvum bats were roosting. The pellets were kept in RNAlater RNA stabilization solution (Qiagen, Hilden, Germany). Gabonese bats were also captured with mist nets just before twilight and were individually euthanized. Bat feces were collected with the corresponding permissions of the host countries in all of the studies.
RT-PCR rotavirus screening and viral metagenomics.
Viral RNA was isolated from the fecal specimens as described previously (62). To screen the RVA presence in bats, conserved RVA-specific primer pairs targeting the VP1 gene were used (277-nucleotide-long PCR product) in a hemi-nested and single round reverse transcription PCR (RT-PCR) assay (Table S1). Among the 18 positive specimens (Tables S2 and S3), 16 fecal samples for which sufficient material remained were shipped to the Laboratory of Clinical and Epidemiological Virology, Leuven, Belgium on dry ice, for further complete genome analyses (Table 1).
The NetoVIR protocol was used for viral enrichment of the fecal suspensions, as described previously (64). Briefly, the fecal samples were suspended in Dulbecco’s phosphate-buffered saline (DPBS) and homogenized with a MINILYS homogenizer (Bertin Technologies) for 20 s at 3,000 rpm. The homogenates were centrifuged for 3 min at 17,000 × g and filtered with 0.8-μm PES filters (Sartorius). Filtrates were treated with benzonase (Novagen) and micrococcal nuclease (New England BioLabs) at 37°C for 2 h to remove the free-floating nucleic acids. Subsequently, samples were extracted using the QIAamp Viral RNA minikit (Qiagen) according to the manufacturer's instructions, without addition of carrier RNA to the lysis buffer. Reverse transcription and second strand synthesis were performed by an adjusted version of the whole-transcriptome amplification (WTA2) protocol (Sigma-Aldrich), as described previously (32). A sequencing library was constructed with the Nextera XT library preparation kit (Illumina). The size of the library was checked with Bioanalyzer (Agilent Technologies) with a high sensitivity DNA chip and the 2 nM pooled libraries were sequenced on an Illumina NextSeq 500 platform (2 × 150 bp paired ends).
Data analysis.
Low-quality reads, ambiguous bases, and primer and adapter sequences were removed from the paired-end reads with Trimmomatic v0.36 with default parameters (65). Trimmed reads were de novo assembled with metaSPAdes from SPAdes software v3.11.1 using 21, 33, 55, and 77 k-mer lengths (66). The obtained contigs were annotated with DIAMOND v0.9.10 against a nonredundant protein database (67). The contigs annotated as “Rotavirus” were further investigated using the nucleotide BLAST against a nucleotide reference database to identify the gene segments (68). The incomplete contigs were completed in silico by mapping the trimmed reads of corresponding samples against the reference sequence determined by the highest BLASTn nucleotide similarity with the lowest E value using BWA software v0.5.9 (69) and SAMtools v1.6 (70). Open reading frames were determined by the web-based NCBI ORF Finder tool (71) (www.ncbi.nlm.nih.gov/orffinder).
Assignment of GCs and phylogenetic analyses.
The genotypes were assigned using the RotaC tool (http://rotac.regatools.be). The sequences whose genotypes could not be determined were sent to the RCWG for assignment of novel genotypes.
Reference strains were downloaded from GenBank in order to represent all the relevant genotypes per gene segment. Codon-based, nucleotide-level multiple sequence alignments were done using MUSCLE (72) with default parameters in MEGA software v7.0.26 (73). Pairwise nucleotide distances were calculated using the number of identical residues in relation to the length of the alignment with the bio3d package in R (74). Alignments were trimmed with trimAL v1.2 with automated1 parameter (75). The optimized number of bootstrap replicates (100 to 1,000) was determined by the autoMRE option, and maximum-likelihood trees were reconstructed with RaxML-NG (76). The GTR+G+I nucleotide substitution model was used for trees of all segments, except for NSP4 and NSP5, as they did not converge after 1,000 bootstraps under the GTR+G+I model (TIM3+I+G and HKY+I+G, respectively). FigTree v1.4.3 from the BEAST package was used for phylogenetic tree visualization and manipulation (77). The GCs were illustrated on a world map using the maps package in R software (78).
Data availability.
The data have been deposited with links to BioProject accession number PRJNA562472 in the NCBI BioProject database (https://www.ncbi.nlm.nih.gov/bioproject/). The data are also deposited to GenBank under the following accession numbers: MN433617 to MN433627 (BB89-15), MN539284 to MN539294 (BR89-60), MN528116 to MN528126 (GKS-897), MN477236 to MN477246 (GKS-912), MN528101 to MN528115 (GKS-926), MN528075 to MN528085 (GKS-929), MN528086 to MN528100 (GKS-934), MN551587 to MN551597 (GKS-941), MN477225 to MN477235 (GKS-954), MN551598 to MN551608 (KCR10-93), and MN567261 to MN567272 (K212). Reference strains that were used to construct the multiple sequence alignments are listed in Table S5.
Genbank accession numbers of the reference RVA strains used in the study. Download Table S5, DOCX file, 0.04 MB (37.7KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Ethical statement.
Bat capture and sampling were conducted with the following permissions: the Wildlife and Hunting Department of the Gabonese Ministry of Water and Forestry (N°003/MEFE-PA/SG/DGEF/DCF and N°0021/MEFE-PA/SG/DGEF/DCF); under clearance 314/5327.74.1.6 from the State Office of Energy and Agriculture, the Environment and Rural Areas Schleswig-Holstein (LANU); and clearances 133/24.03.2008 and 192/26.03.2009 from the Bulgarian Ministry of Environment and Water. For the Ghanaian bats, ethics approval was obtained from the Committee for Human Research, Publications and Ethics of Komfo Anokye Teaching Hospital and School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi. Research samples were exported under a state agreement between the Republic of Ghana and the Federal Republic of Germany, represented by the City of Hamburg. Additional export permission was obtained from the Veterinary Services of the Ghana Ministry of Food and Agriculture.
ACKNOWLEDGMENTS
This project has received funding from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie agreement no. 721367 granted to J.F.D., J.M., and M.V.R. EU Horizon 2020 projects EVAg (grant agreement number 653316) and COMPARE (agreement number 643476) granted to C.D., and the Russian Science Foundation grant 19-15-00055 to A.N.L. also provided funding to the current study. H.U.E. had a personal scholarship from the BONFOR intramural program at the University of Bonn. German Federal Ministry of Education and Research (BMBF) (project code 01KIO16D), Deutsche Forschungsgemeinschaft (DFG DR 772-3/1), Deutsche Forschungsgemeinschaft within the Africa Infectious Diseases program gave grants to C.D. and Y.A.S. (DR 772/3-1) and to S.O. (KA1241/18-1) that were also among the funding contributions. A personal scholarship granted to A.R. from the German Academic Exchange Service (DAAD) supported field work in Costa Rica. D.J. was supported by the Fonds Wetenschappelijk Onderzoek (Research foundation Flanders) (1S78019N). L.B. was supported by the Fonds Wetenschappelijk Onderzoek (1S61618N). K.C.Y. was funded by the Interfaculty Council for Development Cooperation (IRO) from the KU Leuven. The computing power in this work was provided by the VSC (Flemish Supercomputer Centre), financed by the FWO and the Flemish government, department EWI.
C.D., J.F.D., J.M., and M.V.R. designed the research; V.M.C., H.U.E., A.N.L., A.R., G.D.M., T.B., F.G.-R., A.S.-H., S.Y., A.S., S.O., Y.A.S., P.V., M.B., and E.M.L. were involved in sample collection; V.M.C., H.U.E., A.N.L., and C.S. performed the research; C.S., D.J., L.B., W.D., H.U.E., V.M.C., and K.C.Y. contributed to data analysis; J.F.D., C.D., C.S., and J.M. drafted the paper; the final version was approved by all coauthors.
Footnotes
Citation Simsek C, Corman VM, Everling HU, Lukashev AN, Rasche A, Maganga GD, Binger T, Jansen D, Beller L, Deboutte W, Gloza-Rausch F, Seebens-Hoyer A, Yordanov S, Sylverken A, Oppong S, Sarkodie YA, Vallo P, Leroy EM, Bourgarel M, Yinda KC, Van Ranst M, Drosten C, Drexler JF, Matthijnssens J. 2021. At least seven distinct rotavirus genotype constellations in bats with evidence of reassortment and zoonotic transmissions. mBio 12:e02755-20. https://doi.org/10.1128/mBio.02755-20.
REFERENCES
- 1.Clark A, Black R, Tate J, Roose A, Kotloff K, Lam D, Blackwelder W, Parashar U, Lanata C, Kang G, Troeger C, Platts-Mills J, Mokdad A, Sanderson C, Lamberti L, Levine M, Santosham M, Steele D. 2017. Estimating global, regional and national rotavirus deaths in children aged <5 years: current approaches, new analyses and proposed improvements. PLoS One 12:e0183392. doi: 10.1371/journal.pone.0183392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Estes MK, Kapikian AZ. 2007. Rotaviruses, p 1917–1974. In Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, Roizman B, Straus SE (ed), Fields virology. Kluwer Health/Lippincott, Williams and Wilkins, Philadelphia, PA. [Google Scholar]
- 3.Matthijnssens J, Ciarlet M, Heiman E, Arijs I, Delbeke T, McDonald SM, Palombo EA, Iturriza-Gómara M, Maes P, Patton JT, Rahman M, Van Ranst M. 2008. Full genome-based classification of rotaviruses reveals a common origin between human Wa-like and porcine rotavirus strains and human DS-1-like and bovine rotavirus strains. J Virol 82:3204–3219. doi: 10.1128/JVI.02257-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matthijnssens J, Ciarlet M, McDonald SM, Attoui H, Bányai K, Brister JR, Buesa J, Esona MD, Estes MK, Gentsch JR, Iturriza-Gómara M, Johne R, Kirkwood CD, Martella V, Mertens PPC, Nakagomi O, Parreño V, Rahman M, Ruggeri FM, Saif LJ, Santos N, Steyer A, Taniguchi K, Patton JT, Desselberger U, Van Ranst M. 2011. Uniformity of rotavirus strain nomenclature proposed by the Rotavirus Classification Working Group (RCWG). Arch Virol 156:1397–1413. doi: 10.1007/s00705-011-1006-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matthijnssens J, Ciarlet M, Rahman M, Attoui H, Bányai K, Estes MK, Gentsch JR, Iturriza-Gómara M, Kirkwood CD, Martella V, Mertens PPC, Nakagomi O, Patton JT, Ruggeri FM, Saif LJ, Santos N, Steyer A, Taniguchi K, Desselberger U, Van Ranst M. 2008. Recommendations for the classification of group A rotaviruses using all 11 genomic RNA segments. Arch Virol 153:1621–1629. doi: 10.1007/s00705-008-0155-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matthijnssens J, Potgieter CA, Ciarlet M, Parreño V, Martella V, Bányai K, Garaicoechea L, Palombo EA, Novo L, Zeller M, Arista S, Gerna G, Rahman M, Van Ranst M. 2009. Are human P[14] rotavirus strains the result of interspecies transmissions from sheep or other ungulates that belong to the mammalian order Artiodactyla? J Virol 83:2917–2929. doi: 10.1128/JVI.02246-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim H-H, Matthijnssens J, Kim H-J, Kwon H-J, Park J-G, Son K-Y, Ryu E-H, Kim D-S, Lee WS, Kang M-I, Yang D-K, Hyun B-H, Park S-I, Park S-J, Cho K-O. 2012. Full-length genomic analysis of porcine G9P[23] and G9P[7] rotavirus strains isolated from pigs with diarrhea in South Korea. Infect Genet Evol 12:1427–1435. doi: 10.1016/j.meegid.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 8.Matthijnssens J, Miño S, Papp H, Potgieter C, Novo L, Heylen E, Zeller M, Garaicoechea L, Badaracco A, Lengyel G, Kisfali P, Cullinane A, Collins PJ, Ciarlet M, O'Shea H, Parreño V, Bányai K, Barrandeguy M, Van Ranst M. 2012. Complete molecular genome analyses of equine rotavirus A strains from different continents reveal several novel genotypes and a largely conserved genotype constellation. J Gen Virol 93:866–875. doi: 10.1099/vir.0.039255-0. [DOI] [PubMed] [Google Scholar]
- 9.Matthijnssens J, De Grazia S, Piessens J, Heylen E, Zeller M, Giammanco GM, Bányai K, Buonavoglia C, Ciarlet M, Martella V, Van Ranst M. 2011. Multiple reassortment and interspecies transmission events contribute to the diversity of feline, canine and feline/canine-like human group A rotavirus strains. Infect Genet Evol 11:1396–1406. doi: 10.1016/j.meegid.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 10.Schmid R, Wilson DE, Reeder DM. 1993. Mammal species of the world: a taxonomic and geographic reference. Taxon 42:512. doi: 10.2307/1223169. [DOI] [Google Scholar]
- 11.Badrane H, Tordo N. 2001. Host switching in lyssavirus history from the Chiroptera to the Carnivora orders. J Virol 75:8096–8104. doi: 10.1128/jvi.75.17.8096-8104.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chua KB, Lek Koh C, Hooi PS, Wee KF, Khong JH, Chua BH, Chan YP, Lim ME, Lam SK. 2002. Isolation of Nipah virus from Malaysian Island flying-foxes. Microbes Infect 4:145–151. doi: 10.1016/S1286-4579(01)01522-2. [DOI] [PubMed] [Google Scholar]
- 13.Halpin K, Young PL, Field HE, Mackenzie JS. 2000. Isolation of Hendra virus from pteropid bats: a natural reservoir of Hendra virus. J Gen Virol 81:1927–1932. doi: 10.1099/0022-1317-81-8-1927. [DOI] [PubMed] [Google Scholar]
- 14.Towner JS, Amman BR, Sealy TK, Carroll SAR, Comer JA, Kemp A, Swanepoel R, Paddock CD, Balinandi S, Khristova ML, Formenty PBH, Albarino CG, Miller DM, Reed ZD, Kayiwa JT, Mills JN, Cannon DL, Greer PW, Byaruhanga E, Farnon EC, Atimnedi P, Okware S, Katongole-Mbidde E, Downing R, Tappero JW, Zaki SR, Ksiazek TG, Nichol ST, Rollin PE. 2009. Isolation of genetically diverse Marburg viruses from Egyptian fruit bats. PLoS Pathog 5:e1000536. doi: 10.1371/journal.ppat.1000536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li W, Shi Z, Yu M, Ren W, Smith C, Epstein JH, Wang H, Crameri G, Hu Z, Zhang H, Zhang J, McEachern J, Field H, Daszak P, Eaton BT, Zhang S, Wang L-F. 2005. Bats are natural reservoirs of SARS-like coronaviruses. Science 310:676–679. doi: 10.1126/science.1118391. [DOI] [PubMed] [Google Scholar]
- 16.Wang Q, Qi J, Yuan Y, Xuan Y, Han P, Wan Y, Ji W, Li Y, Wu Y, Wang J, Iwamoto A, Woo PCY, Yuen K-Y, Yan J, Lu G, Gao GF. 2014. Bat origins of MERS-CoV supported by bat coronavirus HKU4 usage of human receptor CD26. Cell Host Microbe 16:328–337. doi: 10.1016/j.chom.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W, Si H-R, Zhu Y, Li B, Huang C-L, Chen H-D, Chen J, Luo Y, Guo H, Jiang R-D, Liu M-Q, Chen Y, Shen X-R, Wang X, Zheng X-S, Zhao K, Chen Q-J, Deng F, Liu L-L, Yan B, Zhan F-X, Wang Y-Y, Xiao G-F, Shi Z-L. 2020. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calisher CH, Childs JE, Field HE, Holmes KV, Schountz T. 2006. Bats: important reservoir hosts of emerging viruses. Clin Microbiol Rev 19:531–545. doi: 10.1128/CMR.00017-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olival KJ, Hosseini PR, Zambrana-Torrelio C, Ross N, Bogich TL, Daszak P. 2017. Host and viral traits predict zoonotic spillover from mammals. Nature 546:646–650. doi: 10.1038/nature22975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim HK, Yoon S-W, Kim D-J, Koo B-S, Noh JY, Kim JH, Choi YG, Na W, Chang K-T, Song D, Jeong DG. 2016. Detection of severe acute respiratory syndrome-like, Middle East respiratory syndrome-like bat coronaviruses and group H rotavirus in faeces of Korean bats. Transbound Emerg Dis 63:365–372. doi: 10.1111/tbed.12515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yinda CK, Ghogomu SM, Conceição-Neto N, Beller L, Deboutte W, Vanhulle E, Maes P, Van Ranst M, Matthijnssens J. 2018. Cameroonian fruit bats harbor divergent viruses, including rotavirus H, bastroviruses, and picobirnaviruses using an alternative genetic code. Virus Evol 4:vey008. doi: 10.1093/ve/vey008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bányai K, Kemenesi G, Budinski I, Földes F, Zana B, Marton S, Varga-Kugler R, Oldal M, Kurucz K, Jakab F. 2017. Candidate new rotavirus species in Schreiber’s bats, Serbia. Infect Genet Evol 48:19–26. doi: 10.1016/j.meegid.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Esona MD, Mijatovic-Rustempasic S, Conrardy C, Tong S, Kuzmin IV, Agwanda B, Breiman RF, Banyai K, Niezgoda M, Rupprecht CE, Gentsch JR, Bowen MD. 2010. Reassortant group A rotavirus from straw-colored fruit bat (Eidolon helvum). Emerg Infect Dis 16:1844–1852. doi: 10.3201/eid1612.101089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.He B, Yang F, Yang W, Zhang Y, Feng Y, Zhou J, Xie J, Feng Y, Bao X, Guo H, Li Y, Xia L, Li N, Matthijnssens J, Zhang H, Tu C. 2013. Characterization of a novel G3P[3] rotavirus isolated from a lesser horseshoe bat: a distant relative of feline/canine rotaviruses. J Virol 87:12357–12366. doi: 10.1128/JVI.02013-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xia L, Fan Q, He B, Xu L, Zhang F, Hu T, Wang Y, Li N, Qiu W, Zheng Y, Matthijnssens J, Tu C. 2014. The complete genome sequence of a G3P[10] Chinese bat rotavirus suggests multiple bat rotavirus inter-host species transmission events. Infect Genet Evol 28:1–4. doi: 10.1016/j.meegid.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 26.He B, Huang X, Zhang F, Tan W, Matthijnssens J, Qin S, Xu L, Zhao Z, Yang L, Wang Q, Hu T, Bao X, Wu J, Tu C. 2017. Group A rotaviruses in Chinese bats: genetic composition, serology, and evidence for bat-to-human transmission and reassortment. J Virol 91:e02493-16. doi: 10.1128/JVI.02493-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zheng X, Qiu M, Guan W, Li J, Chen S, Cheng M, Huo S, Chen Z, Wu Y, Jiang L, Chen Q. 2018. Viral metagenomics of six bat species in close contact with humans in southern China. Arch Virol 163:73–88. doi: 10.1007/s00705-017-3570-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dacheux L, Cervantes-Gonzalez M, Guigon G, Thiberge J-M, Vandenbogaert M, Maufrais C, Caro V, Bourhy H. 2014. A preliminary study of viral metagenomics of French bat species in contact with humans: identification of new mammalian viruses. PLoS One 9:e87194. doi: 10.1371/journal.pone.0087194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Asano KM, Gregori F, Hora AS, Scheffer KC, Fahl WO, Iamamoto K, Mori E, Silva FDF, Taniwaki SA, Brandão PE. 2016. Group A rotavirus in Brazilian bats: description of novel T15 and H15 genotypes. Arch Virol 161:3225–3230. doi: 10.1007/s00705-016-3010-9. [DOI] [PubMed] [Google Scholar]
- 30.Sasaki M, Orba Y, Sasaki S, Gonzalez G, Ishii A, Hang'ombe BM, Mweene AS, Ito K, Sawa H. 2016. Multi-reassortant G3P[3] group A rotavirus in a horseshoe bat in Zambia. J Gen Virol 97:2488–2493. doi: 10.1099/jgv.0.000591. [DOI] [PubMed] [Google Scholar]
- 31.Sasaki M, Kajihara M, Changula K, Mori-Kajihara A, Ogawa H, Hang'ombe BM, Mweene AS, Simuunza M, Yoshida R, Carr M, Orba Y, Takada A, Sawa H. 2018. Identification of group A rotaviruses from Zambian fruit bats provides evidence for long-distance dispersal events in Africa. Infect Genet Evol 63:104–109. doi: 10.1016/j.meegid.2018.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yinda CK, Zeller M, Conceição-Neto N, Maes P, Deboutte W, Beller L, Heylen E, Ghogomu SM, Van Ranst M, Matthijnssens J. 2016. Novel highly divergent reassortant bat rotaviruses in Cameroon, without evidence of zoonosis. Sci Rep 6:34209. doi: 10.1038/srep34209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Waruhiu C, Ommeh S, Obanda V, Agwanda B, Gakuya F, Ge X-Y, Yang X-L, Wu L-J, Zohaib A, Hu B, Shi Z-L. 2017. Molecular detection of viruses in Kenyan bats and discovery of novel astroviruses, caliciviruses and rotaviruses. Virol Sin 32:101–114. doi: 10.1007/s12250-016-3930-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mishra N, Fagbo SF, Alagaili AN, Nitido A, Williams SH, Ng J, Lee B, Durosinlorun A, Garcia JA, Jain K, Kapoor V, Epstein JH, Briese T, Memish ZA, Olival KJ, Lipkin WI. 2019. A viral metagenomic survey identifies known and novel mammalian viruses in bats from Saudi Arabia. PLoS One 14:e0214227. doi: 10.1371/journal.pone.0214227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miño S, Matthijnssens J, Badaracco A, Garaicoechea L, Zeller M, Heylen E, Van Ranst M, Barrandeguy M, Parreño V. 2013. Equine G3P[3] rotavirus strain E3198 related to simian RRV and feline/canine-like rotaviruses based on complete genome analyses. Vet Microbiol 161:239–246. doi: 10.1016/j.vetmic.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 36.Okitsu S, Hikita T, Thongprachum A, Khamrin P, Takanashi S, Hayakawa S, Maneekarn N, Ushijima H. 2018. Detection and molecular characterization of two rare G8P[14] and G3P[3] rotavirus strains collected from children with acute gastroenteritis in Japan. Infect Genet Evol 62:95–108. doi: 10.1016/j.meegid.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 37.Solberg OD, Hasing ME, Trueba G, Eisenberg JNS. 2009. Characterization of novel VP7, VP4, and VP6 genotypes of a previously untypeable group A rotavirus. Virology 385:58–67. doi: 10.1016/j.virol.2008.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Esona MD, Roy S, Rungsrisuriyachai K, Gautam R, Hermelijn S, Rey-Benito G, Bowen MD. 2018. Molecular characterization of a human G20P[28] rotavirus a strain with multiple genes related to bat rotaviruses. Infect Genet Evol 57:166–170. doi: 10.1016/j.meegid.2017.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Drexler JF, Corman VM, Müller MA, Maganga GD, Vallo P, Binger T, Gloza-Rausch F, Cottontail VM, Rasche A, Yordanov S, Seebens A, Knörnschild M, Oppong S, Sarkodie YA, Pongombo C, Lukashev AN, Schmidt-Chanasit J, Stöcker A, Carneiro AJB, Erbar S, Maisner A, Fronhoffs F, Buettner R, Kalko EKV, Kruppa T, Franke CR, Kallies R, Yandoko ERN, Herrler G, Reusken C, Hassanin A, Krüger DH, Matthee S, Ulrich RG, Leroy EM, Drosten C. 2012. Bats host major mammalian paramyxoviruses. Nat Commun 3:796. doi: 10.1038/ncomms1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lau SKP, Woo PCY, Lai KKY, Huang Y, Yip CCY, Shek C-T, Lee P, Lam CSF, Chan K-H, Yuen K-Y. 2011. Complete genome analysis of three novel picornaviruses from diverse bat species. J Virol 85:8819–8828. doi: 10.1128/JVI.02364-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pritchard LI, Chua KB, Cummins D, Hyatt A, Crameri G, Eaton BT, Wang L-F. 2006. Pulau virus; a new member of the Nelson Bay orthoreovirus species isolated from fruit bats in Malaysia. Arch Virol 151:229–239. doi: 10.1007/s00705-005-0644-4. [DOI] [PubMed] [Google Scholar]
- 42.Chu DKW, Poon LLM, Guan Y, Peiris JSM. 2008. Novel astroviruses in insectivorous bats. J Virol 82:9107–9114. doi: 10.1128/JVI.00857-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Holland RE 1990. Some infectious causes of diarrhea in young farm animals. Clin Microbiol Rev 3:345–375. doi: 10.1128/cmr.3.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guy JS 1998. Virus infections of the gastrointestinal tract of poultry. Poult Sci 77:1166–1175. doi: 10.1093/ps/77.8.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dhama K, Chauhan RS, Mahendran M, Malik SVS. 2009. Rotavirus diarrhea in bovines and other domestic animals. Vet Res Commun 33:1–23. doi: 10.1007/s11259-008-9070-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cook N, Bridger J, Kendall K, Gomara MI, El-Attar L, Gray J. 2004. The zoonotic potential of rotavirus. J Infect 48:289–302. doi: 10.1016/j.jinf.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 47.Rahman M, Matthijnssens J, Goegebuer T, De Leener K, Vanderwegen L, van der Donck I, Van Hoovels L, De Vos S, Azim T, Van Ranst M. 2005. Predominance of rotavirus G9 genotype in children hospitalized for rotavirus gastroenteritis in Belgium during 1999–2003. J Clin Virol 33:1–6. doi: 10.1016/j.jcv.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 48.Rahman M, Matthijnssens J, Yang X, Delbeke T, Arijs I, Taniguchi K, Iturriza-Gómara M, Iftekharuddin N, Azim T, Van Ranst M. 2007. Evolutionary history and global spread of the emerging G12 human rotaviruses. J Virol 81:2382–2390. doi: 10.1128/JVI.01622-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Voigt CC, Frick WF, Holderied MW, Holland R, Kerth G, Mello MAR, Plowright RK, Swartz S, Yovel Y. 2017. Principles and patterns of bat movements: from aerodynamics to ecology. Q Rev Biol 92:267–287. doi: 10.1086/693847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richter HV, Cumming GS. 2008. First application of satellite telemetry to track African straw-coloured fruit bat migration. J Zoology 275:172–176. doi: 10.1111/j.1469-7998.2008.00425.x. [DOI] [Google Scholar]
- 51.Cryan PM, Stricker CA, Wunder MB. 2014. Continental-scale, seasonal movements of a heterothermic migratory tree bat. Ecol Appl 24:602–616. doi: 10.1890/13-0752.1. [DOI] [PubMed] [Google Scholar]
- 52.Fleming TH, Eby P. 2005. Ecology of bat migration, p 159–166. In Kunz TH, Fenton B (ed), Bat ecology. University of Chicago Press, Chicago, IL. [Google Scholar]
- 53.Lukashev AN, Corman VM, Schacht D, Gloza-Rausch F, Seebens-Hoyer A, Gmyl AP, Drosten C, Drexler JF. 2017. Close genetic relatedness of picornaviruses from European and Asian bats. J Gen Virol 98:955–961. doi: 10.1099/jgv.0.000760. [DOI] [PubMed] [Google Scholar]
- 54.Malherbe H, Harwin R. 1963. The cytopathic effects of vervet monkey viruses. S Afr Med J 37:407–411. [PubMed] [Google Scholar]
- 55.Small C, Barro M, Brown TL, Patton JT. 2007. Genome heterogeneity of SA11 rotavirus due to reassortment with “O” agent. Virology 359:415–424. doi: 10.1016/j.virol.2006.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Komoto S, Sasaki J, Taniguchi K. 2006. Reverse genetics system for introduction of site-specific mutations into the double-stranded RNA genome of infectious rotavirus. Proc Natl Acad Sci U S A 103:4646–4651. doi: 10.1073/pnas.0509385103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ghosh S, Gatheru Z, Nyangao J, Adachi N, Urushibara N, Kobayashi N. 2011. Full genomic analysis of a simian SA11-like G3P[2] rotavirus strain isolated from an asymptomatic infant: identification of novel VP1, VP6 and NSP4 genotypes. Infect Genet Evol 11:57–63. doi: 10.1016/j.meegid.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 58.Dóró R, László B, Martella V, Leshem E, Gentsch J, Parashar U, Bányai K. 2014. Review of global rotavirus strain prevalence data from six years post vaccine licensure surveillance: is there evidence of strain selection from vaccine pressure? Infect Genet Evol 28:446–461. doi: 10.1016/j.meegid.2014.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang Y-H, Pang B-B, Zhou X, Ghosh S, Tang W-F, Peng J-S, Hu Q, Zhou D-J, Kobayashi N. 2013. Complex evolutionary patterns of two rare human G3P[9] rotavirus strains possessing a feline/canine-like H6 genotype on an AU-1-like genotype constellation. Infect Genet Evol 16:103–112. doi: 10.1016/j.meegid.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 60.Corman VM, Rasche A, Diallo TD, Cottontail VM, Stöcker A, Souza B. F d C D, Corrêa JI, Carneiro AJB, Franke CR, Nagy M, Metz M, Knörnschild M, Kalko EKV, Ghanem SJ, Morales KDS, Salsamendi E, Spínola M, Herrler G, Voigt CC, Tschapka M, Drosten C, Drexler JF. 2013. Highly diversified coronaviruses in neotropical bats. J Gen Virol 94:1984–1994. doi: 10.1099/vir.0.054841-0. [DOI] [PubMed] [Google Scholar]
- 61.Pfefferle S, Oppong S, Drexler JF, Gloza-Rausch F, Ipsen A, Seebens A, Müller MA, Annan A, Vallo P, Adu-Sarkodie Y, Kruppa TF, Drosten C. 2009. Distant relatives of severe acute respiratory syndrome coronavirus and close relatives of human coronavirus 229E in bats. Emerg Infect Dis 15:1377–1384. doi: 10.3201/eid1509.090224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Drexler JF, Gloza-Rausch F, Glende J, Corman VM, Muth D, Goettsche M, Seebens A, Niedrig M, Pfefferle S, Yordanov S, Zhelyazkov L, Hermanns U, Vallo P, Lukashev A, Müller MA, Deng H, Herrler G, Drosten C. 2010. Genomic characterization of severe acute respiratory syndrome-related coronavirus in European bats and classification of coronaviruses based on partial RNA-dependent RNA polymerase gene sequences. J Virol 84:11336–11349. doi: 10.1128/JVI.00650-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rougeron V, Suquet E, Maganga GD, Jiolle D, Mombo IM, Bourgarel M, Motsch P, Arnathau C, Durand P, Drexler F, Drosten C, Renaud F, Prugnolle F, Leroy EM. 2016. Characterization and phylogenetic analysis of new bat astroviruses detected in Gabon, Central Africa. Acta Virol 60:386–392. doi: 10.4149/av_2016_04_386. [DOI] [PubMed] [Google Scholar]
- 64.Conceição-Neto N, Zeller M, Lefrère H, De Bruyn P, Beller L, Deboutte W, Yinda CK, Lavigne R, Maes P, Ranst M, Van Heylen E, Matthijnssens J. 2015. Modular approach to customise sample preparation procedures for viral metagenomics: a reproducible protocol for virome analysis. Sci Rep 5:16532. doi: 10.1038/srep16532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bolger AM, Lohse M, Usadel B. 2014. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nurk S, Meleshko D, Korobeynikov A, Pevzner PA. 2017. MetaSPAdes: a new versatile metagenomic assembler. Genome Res 27:824–834. doi: 10.1101/gr.213959.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Buchfink B, Xie C, Huson DH. 2015. Fast and sensitive protein alignment using DIAMOND. Nat Methods 12:59–60. doi: 10.1038/nmeth.3176. [DOI] [PubMed] [Google Scholar]
- 68.Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. 1990. Basic local alignment search tool. J Mol Biol 215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 69.Li H, Durbin R. 2010. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics 26:589–595. doi: 10.1093/bioinformatics/btp698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, Marth G, Abecasis G, Durbin R, 1000 Genome Project Data Processing Subgroup . 2009. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25:2078–2079. doi: 10.1093/bioinformatics/btp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wheeler DL, Church DM, Federhen S, Lash AE, Madden TL, Pontius JU, Schuler GD, Schriml LM, Sequeira E, Tatusova TA, Wagner L. 2003. Database resources of the National Center for Biotechnology. Nucleic Acids Res 31:28–33. doi: 10.1093/nar/gkg033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Edgar RC 2004. MUSCLE: multiple sequence alignment with high accuracy and high throughput. Nucleic Acids Res 32:1792–1797. doi: 10.1093/nar/gkh340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kumar S, Stecher G, Tamura K. 2016. MEGA7: Molecular Evolutionary Genetics Analysis version 7.0 for bigger datasets. Mol Biol Evol 33:1870–1874. doi: 10.1093/molbev/msw054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Grant BJ, Rodrigues APC, ElSawy KM, McCammon JA, Caves LSD. 2006. Bio3d: an R package for the comparative analysis of protein structures. Bioinformatics 22:2695–2696. doi: 10.1093/bioinformatics/btl461. [DOI] [PubMed] [Google Scholar]
- 75.Capella-Gutierrez S, Silla-Martinez JM, Gabaldon T. 2009. trimAl: a tool for automated alignment trimming in large-scale phylogenetic analyses. Bioinformatics 25:1972–1973. doi: 10.1093/bioinformatics/btp348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kozlov AM, Darriba D, Flouri T, Morel B, Stamatakis A. 2019. RAxML-NG: a fast, scalable and user-friendly tool for maximum likelihood phylogenetic inference. Bioinformatics 35:4453–4455. doi: 10.1093/bioinformatics/btz305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rambaut A FigTree, a graphical viewer of phylogenetic trees. http://tree.bio.ed.ac.uk/software/figtree. [Google Scholar]
- 78.Becker RA, Wilks AR, Deckmyn A, Brownrigg R, Minka TP. 2018. Maps: draw geographical maps. https://CRAN.R-project.org/package=maps. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
RT-PCR oligonucleotides for the initial rotavirus screening against VP1. Download Table S1, DOCX file, 0.01 MB (13.4KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Taxonomical annotation, sampling time and location, and RVA PCR detection information of the bat samples. Download Table S2, DOCX file, 0.02 MB (23.7KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
RVA-positive bat samples detected by targeted RT-PCR and having undergone viral metagenomics. Download Table S3, DOCX file, 0.01 MB (14.6KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
RVA-positive bat families and species. Download FIG S1, DOCX file, 0.1 MB (97.8KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Examples of reassortments and unusual genotype constellations among bat RVA strains and distinct RVA genotype constellations in the same bat species. Download Table S4, DOCX file, 0.02 MB (19.6KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Heatmap of pairwise nucleotide identities (NI) of the unusual RVA strains RVA/Horse-wt/ARG/E3198/2008/G3P[3] (a), RVA/Simian-tc/ZAF/SA11-H96/1958/G3P[2] (b), RVA/Human-tc/KEN/B10/1987/G3P[2] (c), and RVA/Human-wt/SUR/2014735512/2013/G20P[28] (d). The gray color indicates the nucleotide identities that are below 0.6 or have lack of sequence information for the compared strain. Download FIG S2, DOCX file, 0.3 MB (293.6KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Genbank accession numbers of the reference RVA strains used in the study. Download Table S5, DOCX file, 0.04 MB (37.7KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Data Availability Statement
The data have been deposited with links to BioProject accession number PRJNA562472 in the NCBI BioProject database (https://www.ncbi.nlm.nih.gov/bioproject/). The data are also deposited to GenBank under the following accession numbers: MN433617 to MN433627 (BB89-15), MN539284 to MN539294 (BR89-60), MN528116 to MN528126 (GKS-897), MN477236 to MN477246 (GKS-912), MN528101 to MN528115 (GKS-926), MN528075 to MN528085 (GKS-929), MN528086 to MN528100 (GKS-934), MN551587 to MN551597 (GKS-941), MN477225 to MN477235 (GKS-954), MN551598 to MN551608 (KCR10-93), and MN567261 to MN567272 (K212). Reference strains that were used to construct the multiple sequence alignments are listed in Table S5.
Genbank accession numbers of the reference RVA strains used in the study. Download Table S5, DOCX file, 0.04 MB (37.7KB, docx) .
Copyright © 2021 Simsek et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.