Summary
In cancer epidemiology using population-based data, regression models for the excess mortality hazard is a useful method to estimate cancer survival and to describe the association between prognosis factors and excess mortality. This method requires expected mortality rates from general population life tables: each cancer patient is assigned an expected (background) mortality rate obtained from the life tables, typically at least according to their age and sex, from the population they belong to. However, those life tables may be insufficiently stratified, as some characteristics such as deprivation, ethnicity, and comorbidities, are not available in the life tables for a number of countries. This may affect the background mortality rate allocated to each patient, and it has been shown that not including relevant information for assigning an expected mortality rate to each patient induces a bias in the estimation of the regression parameters of the excess hazard model. We propose two parametric corrections in excess hazard regression models, including a single-parameter or a random effect (frailty), to account for possible mismatches in the life table and thus misspecification of the background mortality rate. In an extensive simulation study, the good statistical performance of the proposed approach is demonstrated, and we illustrate their use on real population-based data of lung cancer patients. We present conditions and limitations of these methods and provide some recommendations for their use in practice.
Keywords: Excess mortality hazard, Exponentiated Weibull distribution, General hazard structure, Life tables, Net survival
1. Net survival and excess mortality hazard model
Survival analysis after the diagnosis of cancer is an active research area in cancer epidemiology and a primary interest of many countries. The three typical frameworks adopted to model cancer survival data are: (i) the overall survival setting (where overall or all-cause mortality is studied), (ii) the cause-specific setting (where the cause of death is known), and (iii) the relative survival setting. The overall survival setting is not the optimal choice for cancer epidemiology when the main interest is on comparing two or more populations (e.g. two countries, two periods in the same country, two groups with different deprivation levels within the same country and at the same period, and etc.), since it is affected by other causes of mortality, which may differ for the populations of interest. In practice, the cause of death is typically unavailable or, in the absence of a standardized protocol, not reliable. Thus, the cause-specific setting may not be a reasonable choice either. The relative survival setting (Pohar-Perme and others, 2016) represents a useful alternative, where the mortality hazard associated to other causes is approximated by the general population hazard  , which is typically obtained from life tables based on the available sociodemographic characteristics
, which is typically obtained from life tables based on the available sociodemographic characteristics  (e.g. sex, region, and deprivation level) in addition to age and year. The general population hazard is also referred to as the “expected hazard” and the “background mortality rate.” While defined in a hypothetical world, where patients could only die from the cancer under study, net survival (the main object of interest in the relative survival setting) represents a useful way of reporting and comparing the probability of survival of cancer patients since this quantity is not affected by differences in expected mortality (due to other causes) between populations. The basic idea behind net survival consists of decomposing the hazard function associated to an individual,
(e.g. sex, region, and deprivation level) in addition to age and year. The general population hazard is also referred to as the “expected hazard” and the “background mortality rate.” While defined in a hypothetical world, where patients could only die from the cancer under study, net survival (the main object of interest in the relative survival setting) represents a useful way of reporting and comparing the probability of survival of cancer patients since this quantity is not affected by differences in expected mortality (due to other causes) between populations. The basic idea behind net survival consists of decomposing the hazard function associated to an individual,  , as the sum of the hazard associated to the disease of interest (e.g. a specific cancer),
, as the sum of the hazard associated to the disease of interest (e.g. a specific cancer),  , and the hazard associated to other causes in the population of interest,
, and the hazard associated to other causes in the population of interest,  . The hazard associated to other causes is approximated with the general population hazard
. The hazard associated to other causes is approximated with the general population hazard  , assuming that the contribution in the general population hazard of a specific cancer type is small compared to all other causes of death. This is:
, assuming that the contribution in the general population hazard of a specific cancer type is small compared to all other causes of death. This is:
 |
(1.1) |
where  and
and  are vectors of covariates, and
are vectors of covariates, and  typically corresponds to a subset of covariates of
typically corresponds to a subset of covariates of  . The variables “
. The variables “ ” and “
” and “ ” represent the age at diagnosis and the year of diagnosis, respectively, thus
” represent the age at diagnosis and the year of diagnosis, respectively, thus  and
and  represent the age and the year at time
represent the age and the year at time  after diagnosis. This model is also known as excess hazard model (Esteve and others, 1990). The net survival is defined as the survival function associated to the excess hazard function
after diagnosis. This model is also known as excess hazard model (Esteve and others, 1990). The net survival is defined as the survival function associated to the excess hazard function  . Estimation of the net survival function has been largely studied from parametric, semiparametric, and non-parametric perspectives (see Remontet and others, 2007; Pohar Perme and others, 2009; Perme and others, 2012; Rubio and others, 2018).
. Estimation of the net survival function has been largely studied from parametric, semiparametric, and non-parametric perspectives (see Remontet and others, 2007; Pohar Perme and others, 2009; Perme and others, 2012; Rubio and others, 2018).
In practice, a limitation of quantities derived in the relative survival setting (Perme and others, 2012), such as the excess hazard, is that patients need to be matched to groups of the general population sharing the available characteristics  in order to obtain the background mortality rates
in order to obtain the background mortality rates  from the life tables. The number of available characteristics
from the life tables. The number of available characteristics  varies for different countries, and there exist certain characteristics that are not available at the population level that may affect the background mortality rates such as deprivation, ethnicity, drug use (tobacco, alcohol, and etc.), comorbidities, among others. For instance, it has been shown that deprivation levels are associated with life expectancy in some populations (Woods and others, 2005). Thus, if life tables are obtained without a proper stratification of deprivation levels, this will imply that two individuals with different deprivation levels (e.g. most affluent vs. most deprived), but sharing other sociodemographic characteristics, will be assigned the same background mortality. We will refer to the case when the life table is not sufficiently stratified as a “mismatch in the life table.” This mismatch may also apply to other characteristics (e.g. smoking status), thus potentially impacting the comparison ability of the net survival measure (Pavlič and Pohar-Perme, 2018). Moreover, Dickman and others (1998) and Grafféo and others (2012) showed that not including relevant information for matching the mortality rates of patients induces a bias in the estimation of the parameters in net survival models (even for other variables than those included in the life tables). Concerns about the implications of this kind of mismatches in the life tables have recently been discussed in Pavlič and Pohar-Perme (2018) and Bower and others (2018). Thus, it is desirable to produce models that can capture possible mismatching information in the background mortality rates associated to each patient, and that allow the assessment of the impact of this mismatch. In this work, we study an existing model for correcting the background mortality using a single correction parameter (Cheuvart and Ryan, 1991), and extend it to a general hazard structure for excess hazard regression models (Rubio and others, 2018). We also propose a correction model using a random effect (instead of a single parameter). For each of these models, we study the properties of maximum likelihood estimation of the corresponding parameters. We assess the performance of this inferential procedure in an extensive simulation study. We apply and compare these methods using a lung cancer data example. We conclude with some practical advice and summarize the conditions and limitations of these methods, as well as potential directions for further research.
varies for different countries, and there exist certain characteristics that are not available at the population level that may affect the background mortality rates such as deprivation, ethnicity, drug use (tobacco, alcohol, and etc.), comorbidities, among others. For instance, it has been shown that deprivation levels are associated with life expectancy in some populations (Woods and others, 2005). Thus, if life tables are obtained without a proper stratification of deprivation levels, this will imply that two individuals with different deprivation levels (e.g. most affluent vs. most deprived), but sharing other sociodemographic characteristics, will be assigned the same background mortality. We will refer to the case when the life table is not sufficiently stratified as a “mismatch in the life table.” This mismatch may also apply to other characteristics (e.g. smoking status), thus potentially impacting the comparison ability of the net survival measure (Pavlič and Pohar-Perme, 2018). Moreover, Dickman and others (1998) and Grafféo and others (2012) showed that not including relevant information for matching the mortality rates of patients induces a bias in the estimation of the parameters in net survival models (even for other variables than those included in the life tables). Concerns about the implications of this kind of mismatches in the life tables have recently been discussed in Pavlič and Pohar-Perme (2018) and Bower and others (2018). Thus, it is desirable to produce models that can capture possible mismatching information in the background mortality rates associated to each patient, and that allow the assessment of the impact of this mismatch. In this work, we study an existing model for correcting the background mortality using a single correction parameter (Cheuvart and Ryan, 1991), and extend it to a general hazard structure for excess hazard regression models (Rubio and others, 2018). We also propose a correction model using a random effect (instead of a single parameter). For each of these models, we study the properties of maximum likelihood estimation of the corresponding parameters. We assess the performance of this inferential procedure in an extensive simulation study. We apply and compare these methods using a lung cancer data example. We conclude with some practical advice and summarize the conditions and limitations of these methods, as well as potential directions for further research.
2. Corrections of the background mortality in excess hazard regression
In this section, we present two parametric corrections that can account for mismatches in the life table. The first one corresponds to the single parameter correction proposed by Cheuvart and Ryan (1991). The second one corresponds to our proposal, which assumes that the correction to the background mortality is random and can be modeled with a parametric distribution. Next, we present a brief summary of these methods, as well as some of their properties and limitations.
2.1. Single parameter correction: Cheuvart and Ryan’s approach
In the context of clinical trials, Cheuvart and Ryan (1991) proposed an extension of model (1.1) in which they allowed for a constant correction on the population hazard: the overall hazard after  years of follow-up for a patient who entered the trial at age
years of follow-up for a patient who entered the trial at age  in year
in year  and with covariates
and with covariates  was assumed to be
was assumed to be
 |
(2.2) |
where  is an unknown parameter differentiating the competing mortality of eligible patients from that of the general population. Cheuvart and Ryan (1991) employ the proportional excess hazard model
is an unknown parameter differentiating the competing mortality of eligible patients from that of the general population. Cheuvart and Ryan (1991) employ the proportional excess hazard model  , where
, where  is the baseline excess hazard with parameter
is the baseline excess hazard with parameter  ,
,  is a vector of regression parameters, including the effects of treatment and other prognostic factors. In the context of clinical trials, the correction parameter can be reasonably assumed to be the same for all individuals since the population entering the trials is selected based on their characteristics (usually patients without comorbid conditions, and etc.).
is a vector of regression parameters, including the effects of treatment and other prognostic factors. In the context of clinical trials, the correction parameter can be reasonably assumed to be the same for all individuals since the population entering the trials is selected based on their characteristics (usually patients without comorbid conditions, and etc.).
Model (2.2) can be rewritten in terms of the cumulative hazard and the survival functions as follows:
 |
(2.3) |
 |
(2.4) |
where  and
and  are the cumulative hazard functions obtained from
are the cumulative hazard functions obtained from  and
and  , respectively.
, respectively.
In principle, model (2.2) can also be used to account for mismatched life tables, as the correction is made on the population hazard. The basic assumption behind this model is that the true competing mortality is proportional to the mortality of the population obtained from the life tables, and the correction is the same for all individuals. Expression (2.3) also indicates that the information used for estimating the additional correction parameter  comes from the differences in the cumulative hazard
comes from the differences in the cumulative hazard  , which are not used in the estimation of the classical model (1.1).
, which are not used in the estimation of the classical model (1.1).
2.2. Frailty correction for the population hazard
One limitation of model (2.2) is that the correction  , made on the population hazard, is assumed to be constant across all the individuals. This assumption may not be realistic in population studies, where the diversity of unavailable sociodemographic characteristics used to obtain the life tables may induce a non-constant mismatch. Thus, instead of assuming that
, made on the population hazard, is assumed to be constant across all the individuals. This assumption may not be realistic in population studies, where the diversity of unavailable sociodemographic characteristics used to obtain the life tables may induce a non-constant mismatch. Thus, instead of assuming that  is constant in model (2.2), we assume that
is constant in model (2.2), we assume that  is a positive continuous random variable. This implies that the correction factor
is a positive continuous random variable. This implies that the correction factor  is allowed to vary across the different individuals. More specifically, consider the conditional hazard model
is allowed to vary across the different individuals. More specifically, consider the conditional hazard model
 |
(2.5) |
where  is an arbitrary absolutely continuous cumulative distribution function with support on
is an arbitrary absolutely continuous cumulative distribution function with support on  . The conditional overall survival function is given by
. The conditional overall survival function is given by
 |
Then, after integrating out the frailty  with respect to the distribution
with respect to the distribution  (see Appendix of the supplementary material available at Biostatistics online), the individual marginal overall survival function can be written as
(see Appendix of the supplementary material available at Biostatistics online), the individual marginal overall survival function can be written as
 |
(2.6) |
where  denotes the Laplace transform of
denotes the Laplace transform of  evaluated at time
evaluated at time  . Next, we consider a specific choice for the distribution
. Next, we consider a specific choice for the distribution  : a Gamma distribution. This choice allows for obtaining a closed-form expression of the marginal survival function, in addition to its appealing flexibility and interpretability of parameters.
: a Gamma distribution. This choice allows for obtaining a closed-form expression of the marginal survival function, in addition to its appealing flexibility and interpretability of parameters.
Gamma frailty
Consider the conditional hazard model (2.5) and suppose that  , where
, where  denotes a Gamma distribution with mean parameter
denotes a Gamma distribution with mean parameter  , scale parameter
, scale parameter  , and probability density function
, and probability density function  . Then, it follows that
. Then, it follows that
- The marginal individual survival function is given by
(2.7) - The marginal individual hazard function is given by
(2.8)
Expression (2.8) provides a nice interpretation of our approach since the observed hazard can be seen as a model with a correction function  , which is identifiable and provides a functional form that involves the mean correction, the scale or spread of the correction, and the differences on the population cumulative hazards. Another property of the correction function is that
, which is identifiable and provides a functional form that involves the mean correction, the scale or spread of the correction, and the differences on the population cumulative hazards. Another property of the correction function is that  , which indicates that the correction model (2.2) is a limit case. This property, however, does not imply that the correction parameter in (2.2) represents the mean correction when
, which indicates that the correction model (2.2) is a limit case. This property, however, does not imply that the correction parameter in (2.2) represents the mean correction when  , as shown in our simulations. We can also observe that if two patients have the same sociodemographic characteristics (or virtually the same) but different survival times, then the corresponding value of the weight
, as shown in our simulations. We can also observe that if two patients have the same sociodemographic characteristics (or virtually the same) but different survival times, then the corresponding value of the weight  will differ since the corresponding differences in the cumulative hazards
will differ since the corresponding differences in the cumulative hazards  will be different. This, intuitively, suggests that the more extreme the survival time
will be different. This, intuitively, suggests that the more extreme the survival time  of a patient is (either too small or too large), compared to other patients with the same sociodemographic characteristics, the more likely this patient has been assigned the incorrect mortality rate from the life table. This approach implicitly assumes that the excess hazard model
of a patient is (either too small or too large), compared to other patients with the same sociodemographic characteristics, the more likely this patient has been assigned the incorrect mortality rate from the life table. This approach implicitly assumes that the excess hazard model  is correctly specified and includes all important prognosis factors (see Section 6). It also indicates that the information about the parameters of the frailty distribution is provided by the variability in the observed survival times of similar individuals regarding their sociodemographic characteristics and tumor prognosis factors. This suggests the need for a certain amount of observations for groups of patients with similar characteristics.
is correctly specified and includes all important prognosis factors (see Section 6). It also indicates that the information about the parameters of the frailty distribution is provided by the variability in the observed survival times of similar individuals regarding their sociodemographic characteristics and tumor prognosis factors. This suggests the need for a certain amount of observations for groups of patients with similar characteristics.
2.3. Hazard structure and baseline hazard
For models (1.1), (2.2), and (2.8), we adopt the general excess hazard model (GH) proposed in Rubio and others (2018):
 |
(2.9) |
where  is the baseline hazard. This hazard structure contains, as particular cases, the proportional hazards (PH) model when
is the baseline hazard. This hazard structure contains, as particular cases, the proportional hazards (PH) model when  , the accelerated hazards (AH) model when
, the accelerated hazards (AH) model when  , the accelerated failure time (AFT) model when
, the accelerated failure time (AFT) model when  , as well as combinations of these for
, as well as combinations of these for  . Thus, this structure covers the most popular hazard structures used in the literature, allowing also to capture time-dependent effects through
. Thus, this structure covers the most popular hazard structures used in the literature, allowing also to capture time-dependent effects through  (i.e. effects which are not assumed to be constant over the whole follow-up period, such as the effects estimated in PH models). For an extensive discussion on the properties of this GH structure, we refer the reader to Rubio and others (2018).
(i.e. effects which are not assumed to be constant over the whole follow-up period, such as the effects estimated in PH models). For an extensive discussion on the properties of this GH structure, we refer the reader to Rubio and others (2018).
The baseline hazard in (2.9) will be modeled using the Exponentiated Weibull (EW) distribution. The EW distribution contains three positive parameters  (shape, scale, and power), and the corresponding hazard function can capture some basic shapes: increasing, decreasing, unimodal (up-then-down), bathtub (down-then-up), and constant. The EW density and cumulative distribution functions with shape, scale, and power parameters
(shape, scale, and power), and the corresponding hazard function can capture some basic shapes: increasing, decreasing, unimodal (up-then-down), bathtub (down-then-up), and constant. The EW density and cumulative distribution functions with shape, scale, and power parameters  are given, respectively, by:
are given, respectively, by:
 |
Thus, the combination of the GH structure with the choice of the EW baseline hazards can capture a variety of hazard structures, time-dependent effects (through the parameters in  ), and baseline hazard shapes, while allowing for a parsimonious implementation of all the proposed models (Rubio and others, 2018).
), and baseline hazard shapes, while allowing for a parsimonious implementation of all the proposed models (Rubio and others, 2018).
3. Inference
3.1. The classical model
Let  ,
,  , be the sample of times to event from a population of cancer patients, with covariates
, be the sample of times to event from a population of cancer patients, with covariates  , and vital status indicators
, and vital status indicators  (
( -death,
-death,  -censored).
-censored).
For the classical model (1.1), we will rely on the maximum likelihood estimation method, which has been shown to have good inferential properties with the hazard structure detailed in (2.9) (Rubio and others, 2018). With this model, the likelihood is defined as:
M1. Classical model (1.1):
 |
where  represent the parameters of the excess hazard model. In our case,
represent the parameters of the excess hazard model. In our case,  . Notice that here for model (1.1), we omit the expected survival from the likelihood, as this quantity does not depend on parameters.
. Notice that here for model (1.1), we omit the expected survival from the likelihood, as this quantity does not depend on parameters.
3.2. The models with correction of the background mortality
For the models of interest, (2.2) and (2.8), we will estimate the parameters using the maximum likelihood method. The corresponding likelihood functions are presented below for the single-parameter correction model (2.2) and the frailty correction model (2.8)
M2. Single-parameter correction model (2.2):
 |
where  .
.
M3. Frailty correction model (2.8):
 |
where  .
.
These likelihood functions can be maximized using standard optimization routines from the R software (e.g. “nlminb” or “optim”). In order to select between models M1–M3, we use the Akaike Information Criterion (AIC), as these models are estimated using the maximum likelihood method.
3.3. Choice of initial points for the optimization process
For the optimization process, we consider a two-step algorithm. In the first step, we initialize the search at the initial values:  , where
, where  ,
,  ,
,  ,
,  , and then move from these initial values using one cycle of a coordinate descend algorithm (CDA), coupled with the R command “nlminb” on each step of the CDA (see Wright, 2015 for more details on the CDA). The CDA is an algorithm which successively maximizes an objective function along coordinate directions. In our case, we first obtain a new value of the first parameter,
, and then move from these initial values using one cycle of a coordinate descend algorithm (CDA), coupled with the R command “nlminb” on each step of the CDA (see Wright, 2015 for more details on the CDA). The CDA is an algorithm which successively maximizes an objective function along coordinate directions. In our case, we first obtain a new value of the first parameter,  , after maximizing the objective function with respect to
, after maximizing the objective function with respect to  , while setting the other parameter values at their initial values. Then, we maximize again the objective function, obtained by setting this time the initial values to
, while setting the other parameter values at their initial values. Then, we maximize again the objective function, obtained by setting this time the initial values to  to get
to get  . We repeat the same process for all other parameters to finally get a vector
. We repeat the same process for all other parameters to finally get a vector  . In the second step, we utilize the values obtained with the CDA as new initial values in a general purpose optimization algorithm (e.g. “nlminb” or “optim” from the R software), in order to obtain the MLE
. In the second step, we utilize the values obtained with the CDA as new initial values in a general purpose optimization algorithm (e.g. “nlminb” or “optim” from the R software), in order to obtain the MLE  .
.
For model M2, we use the initial values  , with
, with  , while for model M3, we employ the initial values
, while for model M3, we employ the initial values  , with
, with  and
and  . In practice, we recommend running the optimization process at several initial points in order to ensure that the global maximum of the likelihood is reached.
. In practice, we recommend running the optimization process at several initial points in order to ensure that the global maximum of the likelihood is reached.
4. Simulation studies
In this section, we present a simulation study where we assess the impact of mismatches in the population hazard on the estimation of the excess hazard, as well as the performance of the proposed correction models (M2–M3). The true values of the parameters are chosen in order to produce scenarios that resemble cancer population studies concerning an aggressive type of cancer (relatively low 5-year net survival, see Appendix Table 1 of the supplementary material available at Biostatistics online), such as lung cancer, similar to the simulations presented in Rubio and others (2018). An additional extensive simulation scenario resembling a less aggressive type of cancer (such as colon cancer, see Appendix Table 2 of the supplementary material available at Biostatistics online) is presented in the Appendix (Simulation design II) of the supplementary material available at Biostatistics online.
4.1. Data generation
Briefly, in the Simulation Design I of the supplementary material available at Biostatistics online, we simulated  data sets of size
data sets of size  , assuming the additive hazard decomposition given in (1.1). The variable “age” was simulated as a continuous variable using a mixture of uniform distributions with
, assuming the additive hazard decomposition given in (1.1). The variable “age” was simulated as a continuous variable using a mixture of uniform distributions with  probability on
probability on  ,
,  probability on
probability on  , and
, and  probability on
probability on  years old. The binary variables “sex” and “W” were both simulated from a binomial distribution with probability
years old. The binary variables “sex” and “W” were both simulated from a binomial distribution with probability  (the binary variable “W” could be viewed as “treatment” or “comorbidity” or “stage” (early and late)). In all scenarios, we simulated the “other-causes” time to event using the UK life tables based on “age” and “sex” (assuming that all patients were diagnosed on the same year). The time to event from the excess hazard (cancer death time) was generated using the inverse transform method, assuming effects of the three variables “age,” “sex,” and “W” and an EW distribution. We assumed either (i) only administrative censoring at
(the binary variable “W” could be viewed as “treatment” or “comorbidity” or “stage” (early and late)). In all scenarios, we simulated the “other-causes” time to event using the UK life tables based on “age” and “sex” (assuming that all patients were diagnosed on the same year). The time to event from the excess hazard (cancer death time) was generated using the inverse transform method, assuming effects of the three variables “age,” “sex,” and “W” and an EW distribution. We assumed either (i) only administrative censoring at  years, which induced approximately
years, which induced approximately  censoring in all cases, or (ii) an additional independent random censoring (drop-out) using an exponential distribution with rate parameter
censoring in all cases, or (ii) an additional independent random censoring (drop-out) using an exponential distribution with rate parameter  , inducing approximately
, inducing approximately  censoring in these cases. Given the GH structure (2.9) adopted for the simulation, all variables affect the time scale (i.e. time-dependent effects) as well as the hazard scale (i.e. changing the level of the hazard). We refer the reader to Rubio and others (2018) for a more detailed discussion on the interpretation of the GH structure.
censoring in these cases. Given the GH structure (2.9) adopted for the simulation, all variables affect the time scale (i.e. time-dependent effects) as well as the hazard scale (i.e. changing the level of the hazard). We refer the reader to Rubio and others (2018) for a more detailed discussion on the interpretation of the GH structure.
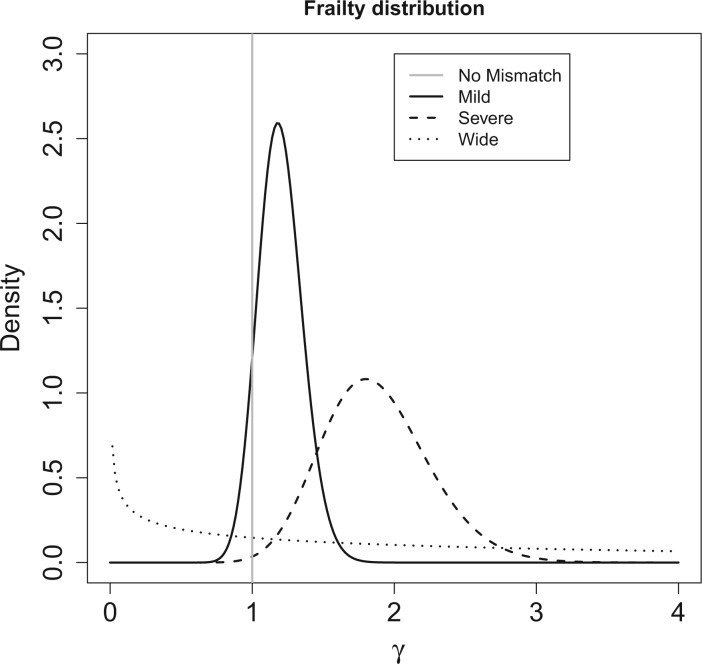
We consider four scenarios that represent mismatches in the life tables: (i) No mismatch, where the data are generated from model (1.1); (ii) Moderate mismatch, where the data are generated from the hazard model (2.5) with  ; (iii) Severe mismatch, where the data are generated from the hazard model (2.5) with
; (iii) Severe mismatch, where the data are generated from the hazard model (2.5) with  ; and (iv) Wide mismatch, where the data are generated from the hazard model (2.5) with
; and (iv) Wide mismatch, where the data are generated from the hazard model (2.5) with  (see Figure 1). In all of these scenarios, we fit models M1–M3. We also consider selecting between models M1–M3 using AIC, in order to identify the model favored by the data. The estimates of the parameters of the excess hazard model selected using AIC are reported, and this model is referred to as model M4. For model M4, we report the estimated correction parameter
(see Figure 1). In all of these scenarios, we fit models M1–M3. We also consider selecting between models M1–M3 using AIC, in order to identify the model favored by the data. The estimates of the parameters of the excess hazard model selected using AIC are reported, and this model is referred to as model M4. For model M4, we report the estimated correction parameter  associated to the selected model. This is,
associated to the selected model. This is,  if AIC selects model M1,
if AIC selects model M1,  if AIC selects model M2, and
if AIC selects model M2, and  if AIC selects model M3. We report coverage of the asymptotic normal confidence intervals in all the scenarios.
if AIC selects model M3. We report coverage of the asymptotic normal confidence intervals in all the scenarios.
Fig. 1.
Frailty distributions used in the simulation.
4.2. Simulation results
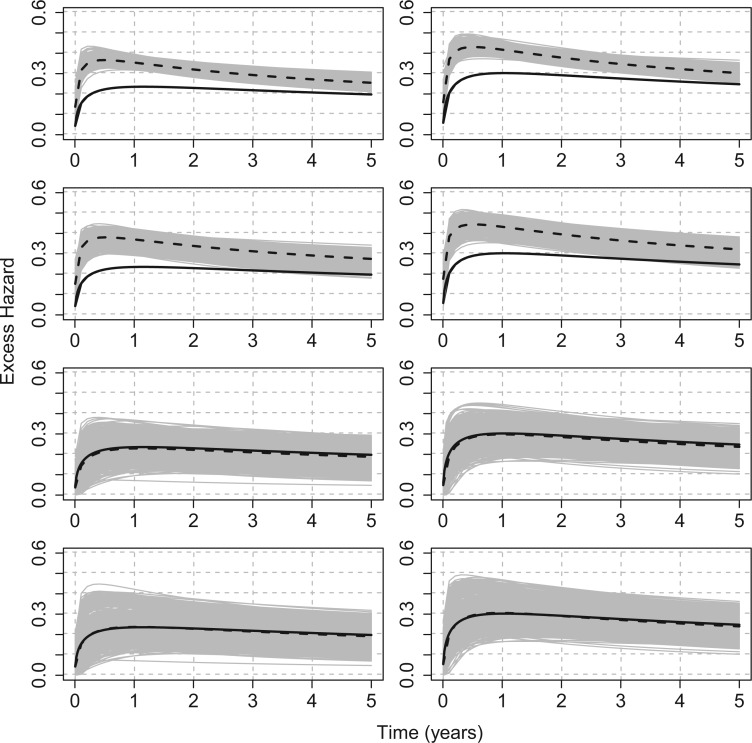
For illustration, Table 1 and Figure 2 show the results for the scenario with  , 30% of censoring and a Wide mismatch (iv). The results of the remaining scenarios are shown in the Appendix of the supplementary material available at Biostatistics online, as well as the results with sample size of
, 30% of censoring and a Wide mismatch (iv). The results of the remaining scenarios are shown in the Appendix of the supplementary material available at Biostatistics online, as well as the results with sample size of  and the simulation design II with a higher net survival. As expected, we observe that when there is Severe and Wide mismatch (iii)–(iv), the model without correction (M1) will lead to biased parameters estimates, as well as poor coverage (Table 1, Figure 2; Appendix Tables 5, 8, and 9 and Appendix Figures 4, 7, and 8 of the supplementary material available at Biostatistics online). This is reflected in the MLEs of the model parameters as well as on the fitted excess hazards. The bias of the parameter estimates and the poor coverages of M1 are more pronounced in the simulation design II with high net survival (Appendix Tables 12, 13, 16, and 17 and Appendix Figures 11, 12, 15, and 16 of the supplementary material available at Biostatistics online). In scenarios (i) and (ii) with No or Moderate mismatch, the fitted correction models M2 and M3 are centered around the true generating model, although they exhibit (as expected) a slightly larger variability compared to model M1 (Appendix Tables 3, 4, 6, 7, 10, 11, 14, and 15, and Appendix Figures 2, 3, 5, 6, 9, 10, 13, and 14 of the supplementary material available at Biostatistics online). In scenario (iii) with Severe mismatch, the fitted correction models M2 and M3 properly correct the mismatch as these models are centered around the true generating model, with the cost of higher variability. The parameters estimated with model M1 are biased with a very low coverage (Appendix Tables 5, 8, 12, and 16 and Appendix Figures 4, 7, 11, and 15 of the supplementary material available at Biostatistics online). In scenario (iv) with Wide mismatch, the fitted models M1 and M2 are biased and far from the true generating model. On the other hand, model M3 can capture this mismatch and reduce the bias properly (Table 1, Figure 2, Appendix Tables 9, 13, and 17 and Appendix Figures 8, 12, and 16 of the supplementary material available at Biostatistics online). The models selected with AIC (M4) are also centered around the true generating model in all scenarios. In cases with no mismatch or moderate mismatch, we observe that the bias on the estimates is small, the coverage is close to
and the simulation design II with a higher net survival. As expected, we observe that when there is Severe and Wide mismatch (iii)–(iv), the model without correction (M1) will lead to biased parameters estimates, as well as poor coverage (Table 1, Figure 2; Appendix Tables 5, 8, and 9 and Appendix Figures 4, 7, and 8 of the supplementary material available at Biostatistics online). This is reflected in the MLEs of the model parameters as well as on the fitted excess hazards. The bias of the parameter estimates and the poor coverages of M1 are more pronounced in the simulation design II with high net survival (Appendix Tables 12, 13, 16, and 17 and Appendix Figures 11, 12, 15, and 16 of the supplementary material available at Biostatistics online). In scenarios (i) and (ii) with No or Moderate mismatch, the fitted correction models M2 and M3 are centered around the true generating model, although they exhibit (as expected) a slightly larger variability compared to model M1 (Appendix Tables 3, 4, 6, 7, 10, 11, 14, and 15, and Appendix Figures 2, 3, 5, 6, 9, 10, 13, and 14 of the supplementary material available at Biostatistics online). In scenario (iii) with Severe mismatch, the fitted correction models M2 and M3 properly correct the mismatch as these models are centered around the true generating model, with the cost of higher variability. The parameters estimated with model M1 are biased with a very low coverage (Appendix Tables 5, 8, 12, and 16 and Appendix Figures 4, 7, 11, and 15 of the supplementary material available at Biostatistics online). In scenario (iv) with Wide mismatch, the fitted models M1 and M2 are biased and far from the true generating model. On the other hand, model M3 can capture this mismatch and reduce the bias properly (Table 1, Figure 2, Appendix Tables 9, 13, and 17 and Appendix Figures 8, 12, and 16 of the supplementary material available at Biostatistics online). The models selected with AIC (M4) are also centered around the true generating model in all scenarios. In cases with no mismatch or moderate mismatch, we observe that the bias on the estimates is small, the coverage is close to  , and all models tend to be relatively close to the true generating model. In those cases, the AIC tends to favor model M1. Table 18 in the Appendix of the supplementary material available at Biostatistics online shows the proportion of selected models using AIC. Overall, we can see that M3 is favored in scenario (iv) with Wide mismatch. In the scenario (iii) with Severe mismatch, the proportion of selected models depends on the contribution of the excess hazard compared to the population hazard. In general, selecting the models using AIC or another model selection tool is advised in order to identify the need for correcting the population hazard. The simulation study results obtained with
, and all models tend to be relatively close to the true generating model. In those cases, the AIC tends to favor model M1. Table 18 in the Appendix of the supplementary material available at Biostatistics online shows the proportion of selected models using AIC. Overall, we can see that M3 is favored in scenario (iv) with Wide mismatch. In the scenario (iii) with Severe mismatch, the proportion of selected models depends on the contribution of the excess hazard compared to the population hazard. In general, selecting the models using AIC or another model selection tool is advised in order to identify the need for correcting the population hazard. The simulation study results obtained with  per sample were very similar to the ones obtained with
per sample were very similar to the ones obtained with  .
.
Table 1.
Simulation results for the scenario GH with  ,
,  ,
,  ,
,  , and wide mismatch
, and wide mismatch  . Mean of the MLEs (MMLE), median of the MLEs (mMLE), empirical standard deviation (ESD), mean (estimated) standard error, root-mean-square error (RMSE), and coverage proportions (Coverage)
. Mean of the MLEs (MMLE), median of the MLEs (mMLE), empirical standard deviation (ESD), mean (estimated) standard error, root-mean-square error (RMSE), and coverage proportions (Coverage)
Design I: 
| |||||||
|---|---|---|---|---|---|---|---|
| Model | Parameter | MMLE | mMLE | ESD | Mean Std error | RMSE | Coverage |
| M1 |
 (1.75) (1.75) |
1.212 | 1.214 | 0.228 | 0.218 | 0.584 | 0.464 |
 (0.6) (0.6) |
0.592 | 0.593 | 0.046 | 0.045 | 0.047 | 0.934 | |
 (2.5) (2.5) |
2.365 | 2.315 | 0.328 | 0.308 | 0.355 | 0.887 | |
 (0.1) (0.1) |
0.119 | 0.118 | 0.012 | 0.012 | 0.023 | 0.700 | |
 (0.1) (0.1) |
0.409 | 0.405 | 0.214 | 0.220 | 0.376 | 0.711 | |
 (0.1) (0.1) |
−0.034 | −0.030 | 0.233 | 0.221 | 0.268 | 0.902 | |
 (0.05) (0.05) |
0.065 | 0.065 | 0.002 | 0.002 | 0.015 | 0.000 | |
 (0.2) (0.2) |
0.296 | 0.296 | 0.047 | 0.045 | 0.107 | 0.449 | |
 (0.25) (0.25) |
0.161 | 0.159 | 0.047 | 0.046 | 0.101 | 0.484 | |
| M2 |
 (1.75) (1.75) |
1.284 | 1.308 | 0.232 | 0.243 | 0.520 | 0.741 |
 (0.6) (0.6) |
0.625 | 0.635 | 0.060 | 0.065 | 0.065 | 0.845 | |
 (2.5) (2.5) |
2.199 | 2.106 | 0.412 | 0.402 | 0.510 | 0.689 | |
 (0.1) (0.1) |
0.119 | 0.118 | 0.012 | 0.013 | 0.023 | 0.715 | |
 (0.1) (0.1) |
0.411 | 0.406 | 0.215 | 0.223 | 0.378 | 0.717 | |
 (0.1) (0.1) |
−0.011 | −0.001 | 0.225 | 0.225 | 0.251 | 0.928 | |
 (0.05) (0.05) |
0.066 | 0.067 | 0.003 | 0.003 | 0.017 | 0.004 | |
 (0.2) (0.2) |
0.308 | 0.309 | 0.046 | 0.047 | 0.117 | 0.352 | |
 (0.25) (0.25) |
0.155 | 0.152 | 0.044 | 0.045 | 0.105 | 0.412 | |
 (6.5) (6.5) |
0.453 | 0.001 | 0.652 | 0.549 | 6.082 | 0.846 | |
| M3 |
 (1.75) (1.75) |
1.406 | 1.323 | 0.745 | 0.721 | 0.820 | 0.978 |
 (0.6) (0.6) |
0.543 | 0.546 | 0.127 | 0.122 | 0.139 | 0.966 | |
 (2.5) (2.5) |
4.082 | 2.992 | 7.019 | 3.070 | 7.192 | 0.970 | |
 (0.1) (0.1) |
0.099 | 0.099 | 0.028 | 0.024 | 0.028 | 0.913 | |
 (0.1) (0.1) |
0.121 | 0.134 | 0.340 | 0.339 | 0.340 | 0.959 | |
 (0.1) (0.1) |
0.089 | 0.103 | 0.354 | 0.326 | 0.354 | 0.950 | |
 (0.05) (0.05) |
0.048 | 0.049 | 0.009 | 0.009 | 0.010 | 0.948 | |
 (0.2) (0.2) |
0.187 | 0.198 | 0.089 | 0.089 | 0.090 | 0.954 | |
 (0.25) (0.25) |
0.262 | 0.251 | 0.087 | 0.085 | 0.087 | 0.949 | |
 (10) (10) |
13.060 | 9.072 | 12.247 | 10.379 | 12.618 | 0.847 | |
 (6.5) (6.5) |
7.010 | 7.134 | 1.839 | 1.727 | 1.908 | 0.853 | |
| M4 |
 (1.75) (1.75) |
1.367 | 1.274 | 0.733 | 0.686 | 0.826 | 0.920 |
 (0.6) (0.6) |
0.540 | 0.546 | 0.122 | 0.117 | 0.136 | 0.968 | |
 (2.5) (2.5) |
3.992 | 2.978 | 6.479 | 2.694 | 6.645 | 0.960 | |
 (0.1) (0.1) |
0.100 | 0.100 | 0.028 | 0.023 | 0.028 | 0.895 | |
 (0.1) (0.1) |
0.139 | 0.151 | 0.341 | 0.328 | 0.343 | 0.938 | |
 (0.1) (0.1) |
0.082 | 0.092 | 0.350 | 0.317 | 0.350 | 0.945 | |
 (0.05) (0.05) |
0.049 | 0.049 | 0.010 | 0.008 | 0.010 | 0.859 | |
 (0.2) (0.2) |
0.194 | 0.203 | 0.092 | 0.086 | 0.093 | 0.904 | |
 (0.25) (0.25) |
0.257 | 0.248 | 0.089 | 0.082 | 0.089 | 0.907 | |
 (6.5) (6.5) |
6.709 | 7.137 | 2.470 | – | 2.477 | – | |
Fig. 2.
Scenario with wide mismatch:  . Models M1–M4 from top to bottom. Mean of the fitted excess hazards (dashed lines), compared to the true generating excess hazard (continuous lines), and 1000 sample-specific fitted excess hazards (grey lines) for
. Models M1–M4 from top to bottom. Mean of the fitted excess hazards (dashed lines), compared to the true generating excess hazard (continuous lines), and 1000 sample-specific fitted excess hazards (grey lines) for  and
and  censoring. Panels from left to right correspond to two sets of values for the covariates (age, sex, comorbidity) =
censoring. Panels from left to right correspond to two sets of values for the covariates (age, sex, comorbidity) =  , respectively. Design I:
, respectively. Design I: 
5. Application: lung cancer data
We now analyze a dataset obtained from population-based national cancer registry of Non-Small Cell Lung Cancer (NSCLC) patients diagnosed in 2012 in England. For deriving information on stage at diagnosis and presence of comorbidities at the time of diagnosis, we linked these data to administrative data (Hospital Episode Statistics [HES] and the Lung Cancer Audit data [LUCADA]) and then applied specific algorithms (Benitez-Majano and others, 2016; Maringe and others, 2017). We used a 6-year period up to 6 months before diagnosis to retrieve information on comorbidity. We checked for the presence of cardiovascular comorbidity (at least one of: myocardial infarction, congestive heart failure, peripheral vascular disease, and cerebrovascular disease) and chronic obstructive pulmonary disease (COPD). We measured deprivation using the Income Domain from the 2010 England Indices of Multiple Deprivation, defined at the Lower Super Output Area level (mean population  ). The Income Domain measures the proportion of the population in an area experiencing deprivation related to low income, and ranges from
). The Income Domain measures the proportion of the population in an area experiencing deprivation related to low income, and ranges from  to
to  in our data (https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010). Follow-up was assessed on the 31st of December 2015, at which time patients alive were censored (so the maximum follow-up was 4 years). We restricted our analysis to men with no missing data. We observed
in our data (https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010). Follow-up was assessed on the 31st of December 2015, at which time patients alive were censored (so the maximum follow-up was 4 years). We restricted our analysis to men with no missing data. We observed  patients with complete cases among which
patients with complete cases among which  died before the 31st of December 2015, and 17 patients were lost to follow-up (censored before the 31st of December 2015). The median follow-up among patients censored was
died before the 31st of December 2015, and 17 patients were lost to follow-up (censored before the 31st of December 2015). The median follow-up among patients censored was  years, mainly because of administrative censoring. The
years, mainly because of administrative censoring. The  ,
,  and
and  quantiles of the patients’ age at diagnosis was
quantiles of the patients’ age at diagnosis was  ,
,  ,
,  while the mean was
while the mean was  . Among the patients,
. Among the patients,  were diagnosed at Stage I,
were diagnosed at Stage I,  at Stage II,
at Stage II,  at Stage III, and
at Stage III, and  at Stage IV. Finally,
at Stage IV. Finally,  patients were classified with a cardiovascular comorbidity and
patients were classified with a cardiovascular comorbidity and  with a chronic obstructive pulmonary disease.
with a chronic obstructive pulmonary disease.
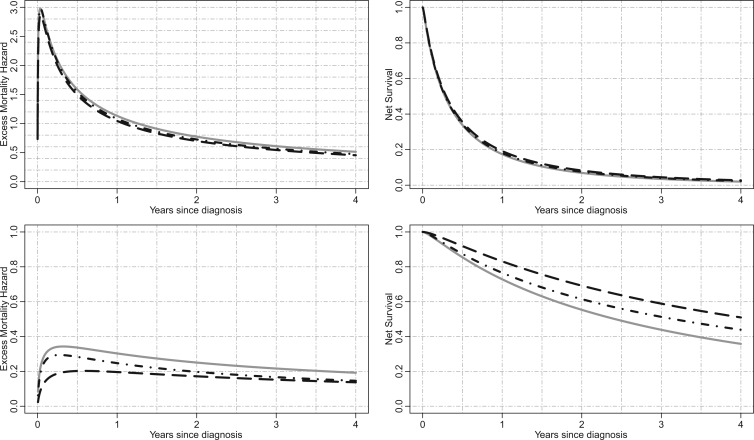
We applied models M1–M3 to estimate the excess mortality hazard using deprivation-specific life tables (detailed by sex, age, year, and Government Office Region in addition to the deprivation quintile). Consequently, we are implicitly assuming that the variables age, sex, deprivation, tumor stage, and comorbidity accurately explain the excess hazard in NSCLC patients. The regression parameter estimates for the excess hazard models M1–M3, as well as the correction parameters (for models M2–M3), are reported in Table 2. For illustrating the results, the excess mortality hazard and the corresponding Net Survival for two pre-defined subgroups of patients are depicted in Figure 3.
Table 2.
Regression parameter estimates (standard errors) using models M1–M3, with their corresponding AIC on the men lung cancer dataset. Note: The time- dependent effects are indicated with -t. For model M2,  is estimated, while
is estimated, while  is estimated for model M3. Age, age at diagnosis (centered at 70, and divided by 10), Dep, Income Deprivation Score (centered at 0.1, and divided by 10); CV, CardioVascular comorbidity; COPD, chronic obstructive pulmonary disease; AIC, Akaike information criteria (best model indicated in bold font)
is estimated for model M3. Age, age at diagnosis (centered at 70, and divided by 10), Dep, Income Deprivation Score (centered at 0.1, and divided by 10); CV, CardioVascular comorbidity; COPD, chronic obstructive pulmonary disease; AIC, Akaike information criteria (best model indicated in bold font)
| M1 | M2 | M3 | |
|---|---|---|---|

|
— | — | 9.83 (3.03) |

|
— | 2.7 (0.21) | 6.54 (0.91) |

|
0.05 (0.01) | 0.03 (0.01) | 0.03 (0.01) |

|
0.38 (0.01) | 0.35 (0.01) | 0.34 (0.01) |

|
4.64 (0.34) | 5.64 (0.48) | 5.92 (0.58) |
| Age-t | 0.29 (0.04) | 0.29 (0.04) | 0.16 (0.05) |
| Dep-t | 0.11 (0.04) | 0.12 (0.04) | 0.09 (0.04) |
| Stage 1-t | −2.66 (0.25) | −2.17 (0.32) | −5.4 (1.4) |
| Stage 2-t | −2.2 (0.2) |
 2 (0.22) 2 (0.22) |
−2.69 (0.35) |
| Stage 3-t | −1.66 (0.11) | −1.57 (0.11) | −1.75 (0.13) |
| CV-t | 0.31 (0.11) | 0.31 (0.11) | 0.42 (0.11) |
| COPD-t | 0.13 (0.11) | 0.08 (0.12) | 0.37 (0.14) |
| Age | 0.27 (0.01) | 0.23 (0.02) | 0.16 (0.02) |
| Dep | 0.06 (0.01) | 0.06 (0.01) | 0.04 (0.01) |
| Stage 1 | −2.84 (0.06) | −3.13 (0.1) | −3.53 (0.36) |
| Stage 2 | −2.16 (0.06) | −2.32 (0.07) | −2.65 (0.1) |
| Stage 3 | −1.23 (0.03) | −1.27 (0.04) | −1.36 (0.04) |
| CV | 0.24 (0.04) | 0.26 (0.04) | 0.3 (0.04) |
| COPD | 0.19 (0.04) | 0.17 (0.04) | 0.25 (0.05) |
| AIC | 20 304.69 | 20 241.27 | 20 213.41 |
Fig. 3.
Illustration for lung cancer patients: Excess mortality hazard (left panels) and the corresponding net survival (right panels) for men aged 70 years at diagnosis, with Income Deprivation score equals to 0.1 (i.e. least deprived), without Cardiovascular comorbidity nor COPD, and with stage IV cancer at diagnosis (upper panels) or stage II cancer at diagnosis (lower panels). M1=solid grey lines, M2=dot-dashed black lines, M3=long-dashed black lines.
In Table 2, between the three models (M1, M2, and M3), the AIC favors model M3 (i.e. the frailty correction model). Differences on  estimates (regression coefficients) between M1 and M3 are substantial. For example, the protective effect of Stage I cancer (compared to being diagnosed with a Stage IV cancer) is even higher when accounting for mismatched life tables. This interpretation follows by noticing that the two parameters associated with Stage I are negative (see Rubio and others, 2018 for details on those hazard-structure models and their interpretation). The impact of the presence of a comorbidity is higher in M3 compared to M1 and M2. Thus, correcting the population life table for unobserved predicting variables of background mortality seems to be quite relevant in this example. An unobserved variable which certainly affects the population mortality hazard here is smoking status. We observe that the frailty distribution, used for correcting the population mortality in M3, cumulates
estimates (regression coefficients) between M1 and M3 are substantial. For example, the protective effect of Stage I cancer (compared to being diagnosed with a Stage IV cancer) is even higher when accounting for mismatched life tables. This interpretation follows by noticing that the two parameters associated with Stage I are negative (see Rubio and others, 2018 for details on those hazard-structure models and their interpretation). The impact of the presence of a comorbidity is higher in M3 compared to M1 and M2. Thus, correcting the population life table for unobserved predicting variables of background mortality seems to be quite relevant in this example. An unobserved variable which certainly affects the population mortality hazard here is smoking status. We observe that the frailty distribution, used for correcting the population mortality in M3, cumulates  of the probability mass below
of the probability mass below  , and
, and  above
above  . That is, the value
. That is, the value  represents the
represents the  quantile of the fitted Gamma frailty distribution with scale parameter
quantile of the fitted Gamma frailty distribution with scale parameter  and mean
and mean  . These values are in fact related to the proportion of smokers (roughly
. These values are in fact related to the proportion of smokers (roughly  , which would, in principle, require a correction higher than 1) for England lung cancer patients (Ellis and others, 2014), which provides an intuitive interpretation of the frailty distribution parameters. This interpretation, of course, has to be taken only at an intuitive level since the correction induced with the frailty model M3 is not interpretable in terms of a single missing characteristic, but it represents a combination of missing characteristics such as drug use (most likely tobacco in this case), the presence of comorbidities among other lifestyle related diseases and its impact on the general population mortality, and etcetera.
, which would, in principle, require a correction higher than 1) for England lung cancer patients (Ellis and others, 2014), which provides an intuitive interpretation of the frailty distribution parameters. This interpretation, of course, has to be taken only at an intuitive level since the correction induced with the frailty model M3 is not interpretable in terms of a single missing characteristic, but it represents a combination of missing characteristics such as drug use (most likely tobacco in this case), the presence of comorbidities among other lifestyle related diseases and its impact on the general population mortality, and etcetera.
In order to evaluate the effect of not having deprivation-specific life tables, we have also fitted excess hazard models using life tables without the deprivation variable (i.e. national life tables). The results obtained with the deprivation-specific life tables and those obtained with the national life tables (excluding deprivation) are very similar (see Section 5, Table 19, in the Appendix of the supplementary material available at Biostatistics online), which is due to the high lethality of lung cancer (inducing negligible differences of population mortality between deprivation groups). Figure 1 in the Appendix of the supplementary material available at Biostatistics online shows the net survival curves obtained for the whole population with models M1–M3 as well as the non-parametric Pohar-Perme estimator (Perme and others, 2012). We observe that model M1 and the Pohar-Perme estimator are virtually the same, which indicates that M1 can properly capture time-dependent effects (Rubio and others, 2018), an assumption made for the correction models. Model M2 produces a net survival curve which is consistently above that obtained with M1. The net survival curve obtained with M3 is above all others, which is explained by the fact that most of the probability mass ( ) of the frailty correction is above
) of the frailty correction is above  . We compared estimates of the excess mortality hazard and the corresponding net survival for two subgroups of patients (Figure 3). For stage IV patients, the differences between each model is almost not visible (upper panels), while the difference between models M1–M3 could be more clearly seen in stage II patients subgroup (lower panels).
. We compared estimates of the excess mortality hazard and the corresponding net survival for two subgroups of patients (Figure 3). For stage IV patients, the differences between each model is almost not visible (upper panels), while the difference between models M1–M3 could be more clearly seen in stage II patients subgroup (lower panels).
6. Discussion
6.1. Summary of findings
Using the general hazard structure in Rubio and others (2018), we have proposed excess hazard regression models that can account for mismatches in the life tables induced by the unavailability of information on relevant population characteristics. The correction models based on a frailty distribution account for non-specific mismatches in the life table, in the sense that the correction is not associated to the lack of known specific variables for constructing the life tables, but to the effect of potentially several unavailable characteristics, which is allowed to be different for each patient. This is the main difference with Cheuvart’s model (2.2), which we used here for comparison purpose even though this model was mainly developed in the context of a randomized clinical trial when a selection bias of the patient population is expected. Thus, Cheuvart’s model assumes the same constant correction parameter for all patients, which is the main difference with our proposed frailty correction models used in population-based cancer registry data. We have shown that the proposed frailty correction models are able to properly identify and correct these mismatches in several simulation scenarios, provided that the sample size is large enough ( or more). Not accounting for mismatched life tables in the relative survival setting may lead to inappropriate net survival comparisons between populations. The need for relatively large samples in order to identify mismatches in the life tables is unsurprising, as there may be several reasons why general population life tables are not fit for our cancer patient population (drug use, lifestyle related diseases, deprivation, ethnicity, and etc.), and only a large enough sample would guarantee that the data contain enough information to adjust for the unavailability of those variables. Intuitively, the information about these correction parameters is provided by the sample of differences of the population cumulative hazards
or more). Not accounting for mismatched life tables in the relative survival setting may lead to inappropriate net survival comparisons between populations. The need for relatively large samples in order to identify mismatches in the life tables is unsurprising, as there may be several reasons why general population life tables are not fit for our cancer patient population (drug use, lifestyle related diseases, deprivation, ethnicity, and etc.), and only a large enough sample would guarantee that the data contain enough information to adjust for the unavailability of those variables. Intuitively, the information about these correction parameters is provided by the sample of differences of the population cumulative hazards  . The implicit assumptions behind the proposed correction model M3 (2.8) are:
. The implicit assumptions behind the proposed correction model M3 (2.8) are:
(i) The set of covariates
 includes the relevant cancer-specific variables. Thus, all missing information (if any) is produced from a mismatch of the population mortality rate.
includes the relevant cancer-specific variables. Thus, all missing information (if any) is produced from a mismatch of the population mortality rate.(ii) The model
 is properly specified. This is, the fitted excess hazard model is flexible enough to approximate the excess hazard.
is properly specified. This is, the fitted excess hazard model is flexible enough to approximate the excess hazard.
Assumption (i) reflects the fact that the model was constructed to only capture mismatches in the life tables, since the correction parameter only affects the population mortality hazard. For instance, in our lung cancer data example, we assume that the excess hazard is accurately explained by age, sex, deprivation, tumor stage, and comorbidity. However, a potential risk factor that is not included there is the smoking status, which is not available at the population level in England. This risk factor might affect both the background mortality hazard (because of diseases or complications associated with smoking) and the cancer-related mortality hazard, in the case that patients continue smoking after the diagnosis of cancer. Indeed, smoking is a driver of lung cancer incidence, but its impact on cancer-related mortality hazard may not be that clear because comorbidity conditions already accounts (at least partially) to smoking-related complications. Thus, the main interest of including smoking status in the predictor variables of the cancer-related mortality hazard would be for patients who continue smoking after the diagnosis of cancer, and it would certainly be interesting to explore the effect of including this variable in the model once it becomes available. Assumption (ii) is important since model misspecification can also affect the correction made on the population hazard. If a covariate which appears in  and
and  is wrongly modeled in
is wrongly modeled in  (e.g. not accounting for time-dependent effects), this may also affect the correction. In principle, this is not an onerous condition since one would usually aim at properly modeling the excess hazard, which is typically the main function of interest. Moreover, recent developments in the use of splines and parametric models (Royston and Parmar, 2002; Giorgi and others, 2003; Nelson and others, 2007; Remontet and others, 2007; Remontet and others, 2018; Charvat and others, 2016; Rubio and others, 2018) allow for a tractable inclusion of non-linear and time-dependent effects in excess hazard models. We also assume that there is enough heterogeneity about the unobserved variables of interest. For instance, if we want to assess the impact of mismatched life tables in terms of deprivation, we assume that the sample contains large enough numbers of individuals with different deprivation levels. The amount of data required to accurately estimate the parameters of the correction models has been explored through a simulation study. Certainly, we would not recommend trying to correct for mismatches in the life tables in samples containing substantially fewer than
(e.g. not accounting for time-dependent effects), this may also affect the correction. In principle, this is not an onerous condition since one would usually aim at properly modeling the excess hazard, which is typically the main function of interest. Moreover, recent developments in the use of splines and parametric models (Royston and Parmar, 2002; Giorgi and others, 2003; Nelson and others, 2007; Remontet and others, 2007; Remontet and others, 2018; Charvat and others, 2016; Rubio and others, 2018) allow for a tractable inclusion of non-linear and time-dependent effects in excess hazard models. We also assume that there is enough heterogeneity about the unobserved variables of interest. For instance, if we want to assess the impact of mismatched life tables in terms of deprivation, we assume that the sample contains large enough numbers of individuals with different deprivation levels. The amount of data required to accurately estimate the parameters of the correction models has been explored through a simulation study. Certainly, we would not recommend trying to correct for mismatches in the life tables in samples containing substantially fewer than  observations, or with high censoring rates (e.g. higher than
observations, or with high censoring rates (e.g. higher than  ). Overall, we have found that model M3 is a good option for accounting for mismatches in the life tables, provided a large enough sample. Its use however is not automatic and should be analyzed on a case by case basis. Comparing the results between corrected (M3) and uncorrected (M1) models, as well as the non-parametric Pohar-Perme estimator, is advisable in practice, in addition to the use of expert knowledge from clinicians or epidemiologists in order to understand and explain the source of the mismatches.
). Overall, we have found that model M3 is a good option for accounting for mismatches in the life tables, provided a large enough sample. Its use however is not automatic and should be analyzed on a case by case basis. Comparing the results between corrected (M3) and uncorrected (M1) models, as well as the non-parametric Pohar-Perme estimator, is advisable in practice, in addition to the use of expert knowledge from clinicians or epidemiologists in order to understand and explain the source of the mismatches.
6.2. Other models in the literature: shared and correlated frailty models
Zahl (1997) describes two extensions of long-term excess hazards models, where the main goal is to account for an increased risk of dying of other diseases in patients with certain cancers. The first extension consists of a shared frailty model in which a random effect (frailty) is multiplied by the population hazard and the excess hazard as follows:
 |
(6.10) |
where  , and
, and  is a distribution with positive support, typically chosen to be a Gamma distribution with unknown shape and scale parameters. Perhaps unsurprisingly, the induced model is non-identifiable unless the random effect has unit mean. Given that the Gamma distribution is asymmetric, the assumption of unit mean implies that
is a distribution with positive support, typically chosen to be a Gamma distribution with unknown shape and scale parameters. Perhaps unsurprisingly, the induced model is non-identifiable unless the random effect has unit mean. Given that the Gamma distribution is asymmetric, the assumption of unit mean implies that  , which may not be a reasonable assumption in some scenarios since this implies that there is a higher probability of requiring a shrinking correction to the population hazard (
, which may not be a reasonable assumption in some scenarios since this implies that there is a higher probability of requiring a shrinking correction to the population hazard ( ) than an increasing one (
) than an increasing one ( ). For a general framework of frailty hazard models we refer the reader to Aalen and others (2008).
). For a general framework of frailty hazard models we refer the reader to Aalen and others (2008).
Zahl (1997) proposed a correlated frailty model, by using frailties on both the population hazard and the excess hazard:
 |
(6.11) |
where  , and
, and  is a bivariate distribution with support on the positive quadrant. Intuitively, it is difficult (if at all feasible) to obtain information about the factors affecting the population hazard and the excess hazard (which is typically a flexible parametric model), and the dependencies between them, simultaneously. In fact, Zahl (1997) found that the maximum likelihood estimators of the parameters of model (6.11) do not exist, suggestive of identifiability issues of this model. Zahl (1997) proposed a number of restrictions of the parameter space (to a compact set) in order to alleviate these estimation issues. However, even after those restrictions, the MLE was on the boundary of the restricted parameter space, which suggests remaining lack of identifiability.
is a bivariate distribution with support on the positive quadrant. Intuitively, it is difficult (if at all feasible) to obtain information about the factors affecting the population hazard and the excess hazard (which is typically a flexible parametric model), and the dependencies between them, simultaneously. In fact, Zahl (1997) found that the maximum likelihood estimators of the parameters of model (6.11) do not exist, suggestive of identifiability issues of this model. Zahl (1997) proposed a number of restrictions of the parameter space (to a compact set) in order to alleviate these estimation issues. However, even after those restrictions, the MLE was on the boundary of the restricted parameter space, which suggests remaining lack of identifiability.
6.3. Further research
From the results of our simulation study, we have observed a larger variability in the estimators of additional parameters corresponding to the correction of the background mortality hazard. In order to reduce this variability, penalized maximum likelihood estimation methods could be used to shrink the correction parameter (i.e. for M2 or for M3) towards the value  . This will be explored in future research.
. This will be explored in future research.
From the simulation study, the coverage proportions of the additional parameter correcting the life table were lower than the nominal value. Using a robust estimator of the variance for this additional parameter may be an option to reach a better coverage, as may be calculating profile likelihood intervals.
Another extension of model (2.2) consists of modeling the correction parameters  and
and  in terms of a set of covariates, say
in terms of a set of covariates, say  . A related approach has recently been studied in Touraine and others (2019). Possible limitations include the inferential challenges in estimating
. A related approach has recently been studied in Touraine and others (2019). Possible limitations include the inferential challenges in estimating  (the dimension of
(the dimension of  ) when the sample size is not large enough. In addition, the assumption of proportional population hazards is often too restrictive in the cancer survival field. In practice, one natural question is whether the Gamma frailty distribution is flexible enough to model the random correction. Using maximum likelihood estimation implies that the estimators of the parameters of the frailty distribution will converge to the values that minimize the distance (in fact, the Kullback–Leibler divergence) to the true generating model. Section 6, Appendix Tables 20–21 and Appendix Figures 17 and 18 of the supplementary material available at Biostatistics online, shows a simulated example where the random correction is simulated from a lognormal distribution (instead of Gamma). This example indicates that model M3 has a good performance even if the random corrections are not generated from a Gamma distribution, but as long as the Gamma distribution can approximate the shape of the true generating distribution. A possible extension consists of using a more flexible frailty distribution with a tractable Laplace transform, in order to obtain tractable expressions for the hazard and cumulative hazard functions. An attractive option is the power variance function (PVF) family of distributions (Aalen and others, 2008), which contains three parameters instead of two. This, of course, complicates the estimation process.
) when the sample size is not large enough. In addition, the assumption of proportional population hazards is often too restrictive in the cancer survival field. In practice, one natural question is whether the Gamma frailty distribution is flexible enough to model the random correction. Using maximum likelihood estimation implies that the estimators of the parameters of the frailty distribution will converge to the values that minimize the distance (in fact, the Kullback–Leibler divergence) to the true generating model. Section 6, Appendix Tables 20–21 and Appendix Figures 17 and 18 of the supplementary material available at Biostatistics online, shows a simulated example where the random correction is simulated from a lognormal distribution (instead of Gamma). This example indicates that model M3 has a good performance even if the random corrections are not generated from a Gamma distribution, but as long as the Gamma distribution can approximate the shape of the true generating distribution. A possible extension consists of using a more flexible frailty distribution with a tractable Laplace transform, in order to obtain tractable expressions for the hazard and cumulative hazard functions. An attractive option is the power variance function (PVF) family of distributions (Aalen and others, 2008), which contains three parameters instead of two. This, of course, complicates the estimation process.
Software
Software in the form of R code, together with a sample input data set and complete documentation is available under request, and an R Markdown document entitled “Simulation design I: Excess hazard models for insufficiently stratified life tables” is available on the website http://www.rpubs.com/FJRubio/FGH and the GitHub repository https://github.com/FJRubio67/ExcessHazardModels.
Supplementary Material
Acknowledgments
The authors thank two referees, an Associate Editor, and the Editor for helpful comments. We obtained the ethical and statutory approvals required for this research (PIAG 1-05(c)/2007; ECC 1-05(a)/2010); ethical approval updated 6 April 2017 (REC 13/LO/0610). We attest that we have obtained appropriate permissions and paid any required fees for use of copyright protected materials.
Conflict of Interest: None declared.
Funding
This research was supported by Cancer Research UK grant number C7923/A18525. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of Cancer Research UK.
References
- Aalen, O., Borgan, O. and Gjessing, H. (2008). Survival and Event History Analysis: A Process Point of View. New York: Springer. [Google Scholar]
- Benitez-Majano, S., Fowler, H., Maringe, C., Di Girolamo, C. and Rachet, B. (2016). Deriving stage at diagnosis from multiple population-based sources: colorectal and lung cancer in England. British Journal of Cancer 115, 391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower, H., Andersson, T. M. L., Crowther, M. J., Dickman, P. W., Lambe, M. and Lambert, P. C. (2018). Adjusting expected mortality rates using information from a control population: an example using socioeconomic status. American Journal of Epidemiology 187, 828–836. [DOI] [PubMed] [Google Scholar]
- Charvat, H., Remontet, L., Bossard, N., Roche, L., Dejardin, O., Rachet, B., Launoy, G. and Belot, A. (2016). A multilevel excess hazard model to estimate net survival on hierarchical data allowing for non-linear and non-proportional effects of covariates. Statistics in Medicine 35, 3066–3084. [DOI] [PubMed] [Google Scholar]
- Cheuvart, B. and Ryan, L. (1991). Adjusting for age-related competing mortality in long-term cancer clinical trials. Statistics in Medicine 10, 65–77. [DOI] [PubMed] [Google Scholar]
- Dickman, P. W., Auvinen, A., Voutilainen, E. T. and Hakulinen, T. (1998). Measuring social class differences in cancer patient survival: is it necessary to control for social class differences in general population mortality? A Finnish population-based study. Journal of Epidemiology and Community Health 52, 727–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis, L., Coleman, M. P. and Rachet, B. (2014). The impact of life tables adjusted for smoking on the socio-economic difference in net survival for laryngeal and lung cancer. British Journal of Cancer 111, 195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteve, J., Benhamou, E., Croasdale, M. and Raymond, L. (1990). Relative survival and the estimation of net survival: elements for further discussion. Statistics in Medicine 9, 529–538. [DOI] [PubMed] [Google Scholar]
- Giorgi, R., Abrahamowicz, M., Quantin, C., Bolard, P., Estève, J., Gouvernet, J. and Faivre, J. (2003). A relative survival regression model using B-spline functions to model non-proportional hazards. Statistics in Medicine 22, 2767–2784. [DOI] [PubMed] [Google Scholar]
- Grafféo, N., Jooste, V. and Giorgi, R. (2012). The impact of additional life-table variables on excess mortality estimates. Statistics in Medicine 31, 4219–4230. [DOI] [PubMed] [Google Scholar]
- Maringe, C., Fowler, H., Rachet, B. and Luque-Fernandez, M. A. (2017). Reproducibility, reliability and validity of population-based administrative health data for the assessment of cancer non-related comorbidities. PLoS One 12, e0172814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, C. P., Lambert, P. C., Squire, I. B. and Jones, D.R. (2007). Flexible parametric models for relative survival with application in coronary heart disease. Statistics in Medicine 26, 5486–5498. [DOI] [PubMed] [Google Scholar]
- Pavlič, K. and Pohar-Perme, M. (2018). Using pseudo-observations for estimation in relative survival. Biostatistics. 10.1093/biostatistics/kxy008. [DOI] [PubMed]
- Perme, M. P., Stare, J. and Estève, J. (2012). On estimation in relative survival. Biometrics 68, 113–120. [DOI] [PubMed] [Google Scholar]
- Pohar-Perme, M., Estève, J. and Rachet, B. (2016). Analysing population-based cancer survival–settling the controversies. BMC Cancer 16, 933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pohar Perme, M., Henderson, R. and Stare, J. (2009). An approach to estimation in relative survival regression. Biostatistics 10, 136–146. [DOI] [PubMed] [Google Scholar]
- Remontet, L., Bossard, N., Belot, A. and Esteve, J. (2007). An overall strategy based on regression models to estimate relative survival and model the effects of prognostic factors in cancer survival studies. Statistics in Medicine 26, 2214–2228. [DOI] [PubMed] [Google Scholar]
- Remontet, L., Uhry, Z., Bossard, N., Iwaz, J., Belot, A., Danieli, C., Charvat, H. and Roche, L. (2018). Flexible and structured survival model for a simultaneous estimation of non-linear and non-proportional effects and complex interactions between continuous variables: performance of this multidimensional penalized spline approach in net survival trend analysis. Statistical Methods in Medical Research. 10.1177/0962280218779408. [DOI] [PubMed]
- Royston, P. and Parmar, M. K. B. (2002). Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Statistics in Medicine 21, 2175–2197. [DOI] [PubMed] [Google Scholar]
- Rubio, F. J., Remontet, L., Jewell, N. P. and Belot, A. (2018). On a general structure for hazard-based regression models: an application to population-based cancer research. Statistical Methods in Medical Research. 10.1177/0962280218782293. [DOI] [PubMed]
- Touraine, C., Grafféo, N., Giorgi, R. and the CENSUR working survival group. (2019). More accurate cancer-related excess mortality through correcting background mortality for extra variables. Statistical Methods in Medical Research. 10.1177/0962280218823234. [DOI] [PubMed]
- Woods, L. M., Rachet, B., Riga, M., Stone, N., Shah, A. and Coleman, M. P. (2005). Geographical variation in life expectancy at birth in England and Wales is largely explained by deprivation. Journal of Epidemiology and Community Health 59, 115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, S. J. (2015). Coordinate descent algorithms. Mathematical Programming 151, 3–34. [Google Scholar]
- Zahl, P. H. (1997). Frailty modelling for the excess hazard. Statistics in Medicine 16, 1573–1585. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.