Abstract
Context:
Older adults with advanced cancer face uncertainty related to their disease and treatment.
Objective:
To evaluate the associations of uncertainty with psychological health and quality of life (QoL) in older adults with advanced cancer.
Methods:
Secondary cross-sectional analysis of baseline data from a national clustered geriatric assessment trial. Patients ≥70 years with advanced cancer considering a new line of chemotherapy were recruited. We measured uncertainty using the modified 9-item Mishel Uncertainty in Illness Scale. Dependent variables included anxiety (Generalized Anxiety Disorder-7), depression (Generalized Depression Scale-15), distress (Distress Thermometer), QoL ([Functional Assessment of Cancer Therapy-General (FACT-G)], and emotional well-being (FACT-G subscale). We used multivariate linear regression analyses to evaluate the association of uncertainty with each dependent variable. We conducted a Partial Least Squares (PLS) analysis with a Variable Importance in Projection (VIP) plot to assess the contribution of individual variables to the model. Variables with a VIP <0.8 were considered less influential.
Results:
We included 527 patients (median age: 76 years, range 70-96). In multivariate analyses, higher levels of uncertainty were significantly associated with greater anxiety (β=0.11, SE=0.04), depression (β=0.09, SE=0.02), and distress (β=0.12, SE=0.02), and lower QoL (β=−1.08, SE=0.11) and emotional well-being (β=−0.29, SE=0.03); the effect sizes were considered small. Uncertainty items related to disease and treatment were most strongly associated with psychological health and QoL scores (all VIP > 0.8).
Conclusions:
Uncertainty among older patients with advanced cancer is associated with worse psychological health and QoL. Tailored uncertainty management strategies are warranted.
Keywords: Uncertainty, psychological health, quality of life, older adults, oncologists
Introduction
Patients with advanced cancer face uncertainties such as whether their disease may progress or recur, or how long they may live. Uncertainty is the cognitive state created when a person cannot adequately structure an event due to insufficient cues. It occurs when the individual is unable to assign definite value to objects or events and/or to accurately predict outcomes.(1) In cancer care, uncertainty may arise from the unknown probability of treatment success, the complexity of information, lack of or poor communication with healthcare personnel, complex processes related to healthcare, or psychosocial and existential consequences of cancer.(2) In older adults, who actually constitute the largest proportion of new patients with cancer,(3) these issues might be amplified by aging-related concerns, such as the impact of treatment on independent living and cognition.
Uncertainty can negatively affect physical, psychological, and existential outcomes.(4,5) In the general population of patients with cancer, greater uncertainty is associated with increased fatigue, insomnia,(6) emotional distress,(4) anxiety, depression,(7) and lower quality of life (QoL).(8) Uncertainty can also influence psychosocial adjustment to the diagnosis of cancer.(9) Older adults may not seek health information on their own and may have little social support to provide them with such information, both of which may contribute to uncertainty.(10)
In this secondary analysis, we described uncertainty among older adults with advanced cancer and its association with psychological health and QoL. We hypothesized that higher uncertainty was associated with worse psychological health and QoL in this population.
Materials and Methods
Study Design
We performed a cross-sectional analysis of baseline data from a national cluster-randomized trial that evaluated the effect of geriatric assessment (GA) information and GA-driven recommendations on patient satisfaction and communication with oncologists regarding age-related concerns [University of Rochester Cancer Center (URCC) 13070; ClinicalTrials.gov identifier: NCT02107443].(11) This trial was carried out within the URCC National Cancer Institute Community Oncology Research Program (NCORP) and enrolled patients from 31 community oncology practice sites between October 2014 and April 2017. The study was approved by the Research Subjects Review Board at URCC and institutional review boards at all enrolled practice sites. All patients provided informed consent at enrollment.
Participants and Measures
The primary study included patients aged ≥70 years, with a stage III or IV solid tumor or lymphoma deemed to be incurable, considering or receiving any line of cancer treatment, and with at least one impaired GA domain (i.e. vulnerable older patients with age-related conditions). After informed consent was provided, demographics and GA were obtained. Assessed GA domains included functional status, physical performance, comorbidity, medications, nutrition, cognition, psychological health, and social support. (12-14) Some GA assessments were completed by the patients and others were administered by clinical research associates (Supplemental Table 1). Patients completed additional measures via self-administered questionnaires at baseline, as described below.
Independent variable - Uncertainty
Uncertainty was evaluated using the Mishel’s Uncertainty in Illness Scale (MUIS).(15,16) The original measure consists of 32 questions measuring several aspects of uncertainty (ambiguity, complexity, inconsistency, and unpredictability).(17) MUIS has been validated in patients with cancer.(15,16) For this study, we selected 9 items deemed relevant for patients with advanced cancer based on investigator consensus. Each item is presented in a Likert scale of 1 to 5, with total scores ranging from 9 to 45 and higher scores indicating greater uncertainty. Cronbach’s alpha was 0.72 for the modified 9-item MUIS scale. If participants had <100% of missing data for the uncertainty measure, we imputed missing data by averaging the items. Patients with complete missing of MUIS items were excluded.
Dependent variables - Psychological health and QoL
All measures were assessed using validated instruments: 1) Anxiety [Generalized Anxiety Disorder −7 (GAD-7) scale], 2) Depression [Geriatric Depression Scale-15 (GDS-15)], 3) Distress (Distress Thermometer), 4) QoL [Functional Assessment of Cancer Therapy-General (FACT-G) questionnaire overall score], and 5) Emotional well-being (subscale of the FACT-G; this was reported separately and in addition to FACT-G as we were interested in examining psychological health of patients). GAD-7 consists of 7 questions scored in a scale from 0 (hardly ever) to 3 (nearly every day), with a score of 0-21 and a higher score indicating worse anxiety symptoms.(18) GDS-15 consists of 15 yes/no questions, scored 0 or 1, with higher scores indicating worse depressive symptoms.(19) The Distress Thermometer consists of an 11-point Likert scale (range 0-10), with a higher score indicating higher distress.(20) FACT-G is comprised of 27 questions scored on a 0-4 Likert scale, with a range of 0-108 and higher scores indicating better QoL. Emotional well-being is one of the FACT-G subscales, scored in the same fashion as FACT-G, with a range of 0-24 and higher scores indicating better emotional well-being.(21) Based on prior studies, minimal clinically important differences (MCID) were 3 points, 4-5 points, 2 points, 4-7 points and 1-2 points respectively for GAD-7, GDS-15, Distress Thermometer, FACT-G, and emotional well-being.(22-25)
Covariates
Covariates were identified a priori based on investigator consensus and prior literature.(15,26,27) These included patient demographics, cancer type, and number of impaired GA domains. Patient sociodemographic factors included age, gender, marital status, race, education, and annual household income.
Statistical analyses
Demographics and summary scores for uncertainty, depression, distress, QoL, and emotional well-being were reported using descriptive analyses. We conducted bivariate and multivariate linear regression analyses to evaluate the associations of uncertainty with anxiety, depression, distress, QoL, and emotional well-being. Each dependent variable was evaluated in a separate model, adjusting for covariates. The effect of practice oncology site clusters was tested by likelihood ratio tests linear mixed models with practice site included as random effects and not statistically significant (all p>0.10); therefore, results from the original multivariate models are presented. To account for the potential problem of multiple comparisons, two-sided p values of <0.01 were considered statistically significant.(28)
To provide understanding on which individual MUIS items contributed the most to our dependent variables, we conducted an exploratory Partial Least Squares (PLS) analysis using the 9 MUIS items as independent variables, and psychological health and QoL measures as dependent variables. PLS provides the Variable Importance for Projection (VIP) statistic, which summarizes the contribution of an individual variable to the PLS model. Variables with a VIP <0.8 were deemed less influential in the model.(29) All analyses were performed using the SAS software package (version 9.4; SAS Institute, Cary, NC), and Stata 15.0 (StataCorp LLC, College Station, TX).
Results
The primary study included 541 patients; we excluded 14 patients with 100% missing data on the uncertainty measure, resulting in a final sample of 527 patients. Fifty-five patients (10.4%) had <50% missing uncertainty data. The mean age of patients was 76.6 years (SD 5.2 years, range 70–96); 51.2% were male, 51.8% completed at least some college education, and 50.6% of patients had an annual household income of >$50,000. Around half of the patients had a gastrointestinal or lung primary tumor. The mean number of impaired GA domains was 4.4 (SD 1.5). Other characteristics are shown in Table 1.
Table 1.
Patient characteristics
| Characteristics (N=527) | N (%) or mean (SD) | |
|---|---|---|
| Age, mean (SD) | 76.6 (5.2) | |
| Gender, N (%) | Female | 257 (48.7) |
| Male | 270 (51.2) | |
| Marital status, N (%) | Married | 339 (64.4) |
| Not married | 187 (35.5) | |
| Race, N (%) | White Non-Hispanic | 471 (89.3) |
| Other | 56 (10.6) | |
| Education, N (%) | Less than complete high school | 63 (11.9) |
| Complete high school | 191 (36.2) | |
| Some college or above | 273 (51.8) | |
| Annual household income, N (%) | ≤$50,000 | 259 (49.3) |
| >$50,000 or Decline to answer | 266 (50.6) | |
| Cancer type, N (%) | Gastrointestinal | 136 (25.8) |
| Lung | 135 (25.6) | |
| Other | 255 (48.4) | |
| Number of impaired GA domains, mean (SD) | 4.4 (1.5) | |
| Uncertainty, modified 9-item MUIS, mean (SD) | 19.7 (4.8) | |
| Anxiety, GAD-7 , mean (SD) | 2.9 (4.0) | |
| Depression, GDS-15, mean (SD) | 3.1 (2.7) | |
| Distress thermometer, mean (SD) | 2.9 (2.7) | |
| Quality of Life, FACT-G, mean (SD) | 80.7 (14.7) | |
| Emotional well-being, mean (SD) | 18.9 (4.0) |
Abbreviations: SD, standard deviation; GA, geriatric assessment, MUIS, Mishel’s Uncertainty in Illness Scale; GAD-7, Generalized Anxiety Disorder −7; GDS-15, Geriatric Depression Scale-15; FACT-G, Functional Assessment of Cancer Therapy-General
Uncertainty
The mean score for the modified 9-item MUIS was 19.7 (SD 4.8, range 9-33). The distribution of each item is shown in Table 2. The majority of patients agreed or strongly agreed with statements regarding communication with providers: “The doctors and nurses use everyday language so I can understand what they are saying” (93.1%) and “I understand everything explained to me” (74.8%). Half of the patients (50.4%) agreed or strongly agreed with the statement “The treatment I am receiving (or may receive) has a known probability of success.” Most patients (73.0%) agreed or strongly agreed with the statement “The seriousness of my prognosis has been determined.”
Table 2.
Distribution of Modified 9-Item Mishel Uncertainty in Illness (data shown prior to imputation)
| Mishel Uncertainty in Illness (MUIS) Item |
Strongly Agree |
Agree | Undecided | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| 1) I have a lot of questions without answers.a,b | 4.2% | 13.4% | 20.2% | 35.9% | 26.3% |
| 2) The purpose of the treatment options is clear to me.c | 39.1% | 45.5% | 10.5% | 3.2% | 1.7% |
| 3) The explanations I've heard about what to expect for the course of my illness seem hazy to me.a,d | 4.8% | 18.8% | 20.2% | 32.9% | 23.3% |
| 4) I understand everything explained to me. | 26.4% | 48.4% | 16.3% | 7.0% | 1.9% |
| 5) The effectiveness of treatment is undetermined.a,b | 13.0% | 36.6% | 26.5% | 16.4% | 7.4% |
| 6) The treatment I am receiving (or may receive) has a known probability of success.b,d | 13.0% | 37.4% | 33.2% | 5.5% | 2.9% |
| 7) I can depend on the nurses to be there when I need them.e | 46.6% | 43.2% | 7.3% | 1.5% | 1.4% |
| 8) The seriousness of my prognosis has been determined.f | 26.6% | 46.4% | 20.7% | 3.8% | 2.5% |
| 9) The doctors and nurses use everyday language so I can understand what they are saying.c | 45.7% | 47.4% | 5.0% | 0.8% | 1.1% |
Item was reversely scored
3 missing responses
2 missing responses
42 patients (8.0%) selected “not applicable”
8 missing response
5 missing response
Psychological health and QoL
The average scores were 2.9 (SD 4.0, range 0-21) for GAD-7, 3.1 (SD 2.7, range 0-13) for GDS-15, 2.9 (SD 2.7, range 0-10) for distress, 80.7 (SD 14.7, range 30-108) for FACT-G, and 18.9 (SD 4.0, range 3-24) for emotional well-being respectively. The correlation coefficients among the dependent variables are shown in Table 3.
Table 3.
Correlation between psychological and quality of life measures
| Measures | Correlation coefficient (p) | ||||
|---|---|---|---|---|---|
| FACT-G | EWB | GAD7 | GDS | DT | |
| FACT-G total (FACT-G) | 1 | 0.72 (<0.001) | −0.44 (<0.001) | −0.59 (<0.001) | −0.47 (<0.001) |
| Emotional well-being subscale of FACT-G (EWB) | 0.72 (<0.001) | 1 | −0.49 (<0.001) | −0.45 (<0.001) | −0.51 (<0.001) |
| Anxiety (GAD7) | −0.44 (<0.001) | −0.49 (<0.001) | 1 | 0.43 (<0.001) | 0.56 (<0.001) |
| Depression (GDS) | −0.59 (<0.001) | −0.45 (<0.001) | 0.43 (<0.001) | 1 | 0.44 (<0.001) |
| Distress thermometer (DT) | −0.47 (<0.001) | −0.51 (<0.001) | 0.56 (<0.001) | 0.44 (<0.001) | 1 |
Multivariate analyses
In multivariate analyses, greater uncertainty was statistically significantly associated with higher levels of anxiety (β=0.10, SE=0.04, p=0.006), depression (β=0.10, SE=0.03, p<0.001), and distress (β=0.11, SE=0.02, p<0.001), as well as worse QoL (β=−1.10, SE=0.11, p<0.001) and emotional well-being (β=−0.29, SE=0.03, p<0.001) (Table 4). In other words, a 1-point increase in the 9-item uncertainty scale was associated with a 0.10 point increase in GAD-7, a 0.10 point increase in GDS, a 0.11 point increase in the Distress Thermometer, a 1.10 point decrease in total FACT-G and 0.29 point decrease in the emotional well-being subscale. The effect sizes were considered small.
Table 4.
Multivariate analyses evaluating the associations of uncertainty with psychological health and quality of life
| Dependent variable | Covariates | B coefficient,a standard error (SE) |
95% CI | p value |
|---|---|---|---|---|
| Anxiety, GAD-7 scoreb | Uncertainty, modified 9-item MUIS | 0.10 (0.04) | 0.03 to 0.17 | 0.006 |
| Age | −0.08 (0.03) | −0.14 to −0.01 | 0.018 | |
| Number of impaired GA domains | 0.69 (0.14) | 0.42 to 0.95 | <0.001 | |
| Depression, GDS-15 scoreb | Uncertainty, modified 9-item MUIS | 0.10 (0.02) | 0.05 to 0.14 | <0.001 |
| Age | −0.05 (0.02) | −0.09 to −0.01 | 0.019 | |
| Number of impaired GA domains | 0.66 (0.09) | 0.49 to 0.83 | <0.001 | |
| Distress thermometer scoreb | Uncertainty, modified 9-item MUIS | 0.11 (0.02) | 0.06 to 0.16 | <0.001 |
| Age | −0.06 (0.02) | −0.11 to −0.02 | 0.005 | |
| Number of impaired GA domains | 0.43 (0.09) | 0.25 to 0.61 | <0.001 | |
| Quality of Life, FACT-G scorec | Uncertainty, modified 9-item MUIS | −1.10 (0.11) | −1.33 to −0.88 | <0.001 |
| Age | 0.28 (0.10) | 0.07 to 0.48 | 0.009 | |
| Number of impaired GA domains | −3.90 (0.43) | −4.74 to −3.05 | <0.001 | |
| Emotional well-being subscorec | Uncertainty, modified 9-item MUIS | −0.29 (0.03) | −0.36 to −0.22 | <0.001 |
| Age | 0.07 (0.03) | 0.01 to 0.13 | 0.031 | |
| Race (non-white vs. white) | 1.16 (0.52) | 0.14 to 2.18 | 0.027 | |
| Number of impaired GA domains | −0.52 (0.13) | −0.77 to −0.27 | <0.001 |
Changes in dependent variable scores for every 1 point increment in modified 9-item MUIS, based on separate multivariate linear regression models, adjusting for age, gender, race, education, marital status, income, tumor type, and number of impaired geriatric assessment domains
Higher score indicates a worse outcome
Lower score indicates a worse outcome
Regarding covariates, older age was associated with lower levels of distress as well as better QoL scores. In contrast, a higher number of impaired GA domains was associated with higher levels of anxiety, depression, and distress as well as worse QoL and emotional well-being (Table 4).
Partial Least Squares (PLS) analysis
The VIP resulting from PLS (Figure 1) showed that uncertainty items related to patient-provider communication and those related to treatment options and effectiveness were more influential in the association with psychological health and QoL (all VIP > 0.8). Uncertainty related to trust in nursing personnel (MUIS7) or severity of prognosis (MUIS8) were less influential for determining patient outcomes.
Figure 1.
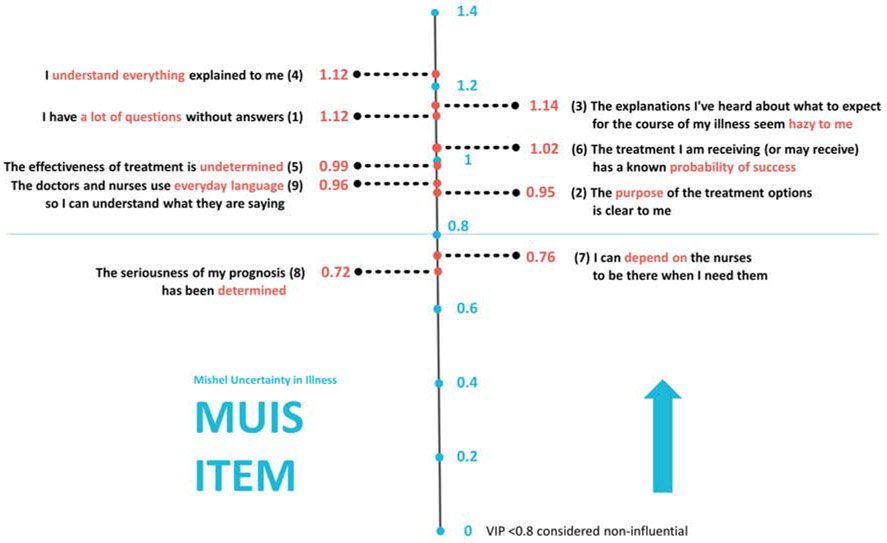
Modified 9-item MUIS Variable Importance for Projection (VIP) plot
Discussion
In this secondary analysis, we describe uncertainty in a population of vulnerable older adults with advanced cancer. Consistent with our hypotheses, we found that higher levels of uncertainty were associated with poorer psychological health and QoL. Uncertainty items related to patient-provider communication and those related to treatment options and effectiveness were most influential in these associations.
There are no clear validated cut-offs to define levels of uncertainty. The original MUIS scale (32-item) was initially described in multiple cohorts of patients, including those with cancer, with mean scores ranging from 59.8 to 103.7 on a 160-point scale.(17) In a study of older patients with cancer undergoing surgery, a 25-item MUIS scale (125-point scale) was used and mean score was 59.6.(30) In our sample, a 9-item MUIS scale (45-point scale) was used and mean score was 19.7, which was relatively similar to the aforementioned studies.
Cognitive, emotional, and behavioral responses to uncertainty can be both negative (e.g., anxiety, distress, avoidance) and positive (e.g., feelings of hope, information seeking). The balance between these responses is called “uncertainty tolerance”, which is an individual characteristic mediated by personal and stimulus-dependent factors, such as education level or the complexity of the disease process.(31) In our study, we examined negative responses to uncertainty in vulnerable older adults with cancer, and found that uncertainty was associated with worse psychological health and QoL scores. However, effect sizes for these relationships were considered small based on previously reported MCID for the respective measures. (22-25) Findings from our study were consistent with previous reports in populations unselected by age. In a cross-sectional study of 30 patients with cancer (median age: 66 years), a higher level of uncertainty was associated with a higher level of anxiety.(32) In another cross-sectional study of 49 patients with lung cancer (mean age: 64 years), a higher level of uncertainty in the form of ambiguity was associated with increased perception of stress and poorer emotional well-being.(15) Furthermore, intolerance of uncertainty was associated with increased perception of stress, more depressive symptoms, and worse emotional well-being.(15) Uncertainty regarding prognosis is also prevalent in hospitalized patients with advanced cancer and can lead to distress and lower QoL.(4) For those with higher uncertainty-related distress, palliative care consultation may be beneficial.(4)
Management of uncertainty in older adults is under studied. Mishel and colleagues performed a randomized trial evaluating an uncertainty management intervention based on cognitive-behavioral strategies in older survivors of breast cancer.(33) At 10 months, the intervention improved cognitive reframing, cancer knowledge, patient-healthcare provider communication, and coping skills. Uncertainty remained low 20 months after the intervention. In another study, patients with early prostate cancer (mean age: 62) were randomized to an uncertainty management decision-making intervention consisting of provision of information about the disease, communication strategies, and telephone calls performed between the diagnosis of prostate cancer and the first appointment with their physician.(34) Compared to usual care, patients receiving the intervention had improved cancer knowledge, problem-solving skills, and participation in decision-making, with less decisional regret. Importantly, there was no difference in mood or QoL.
Results from our exploratory PLS analysis showed that uncertainty items related to patient-provider communication and those related to treatment options and effectiveness were more influential in the association with psychological health and QoL. This treatment-related uncertainty may be addressed by improving communication. On the other hand, prognosis-related uncertainty was less influential in our model. Physicians may try to reduce uncertainty by providing extensive information but some patients may prefer to remain uncertain about a poor prognosis (35). Most of the patients in our study agreed that the seriousness of their prognosis had been determined. However, we have previously shown that 60% of these patients have different beliefs about their cancer curability compared to their oncologist (36). These patients could have a positive appraisal of prognosis-related uncertainty leading to hope. Attempting to reduce uncertainty by increasing prognostic understanding without addressing their psychological state may instead increase anxiety and lead to worse QoL.
Uncertainty may also arise from irreducible sources, such as existential concerns. Physicians also need to identify other potential causes of uncertainty, such as the potential impact of cancer in daily life and personal relationships. The GA can address some of these areas. Therefore, it is important that physicians first ascertain how much patients wish to know about their disease and prognosis, their preferred role in decision-making, and then assess if they would benefit from any intervention.(37,38) In patients with distress due to information-related uncertainty, improving communication may be an adequate strategy, whereas in those with distress due to irreducible uncertainty, a cognitive reframing of uncertainty might be more useful, so that patients are able to cope with it. (39)
Our study has several strengths. We recruited a large number of patients from community oncology practices where most vulnerable patients are treated. We used several validated instruments to assess psychological health and QoL. There are some limitations to our study. First, we did not inquire about the meaning of uncertainty to the patients. Second, our study sample was mostly non-Hispanic white and relatively well-educated, and therefore our findings may not be generalizable to patients of other ethnicities and races or lower education levels. Third, we adapted the original MUIS into a modified 9-item scale with items selected by the perspectives of the study team in an effort to reduce missing data, which limits comparison to other studies. Data was also imputed in about 10% of patients. In addition, the original MUIS and Mishel’s uncertainty model did not assess aspects such as personal relationships or existential concerns.(40) Fourth, we did not collect information on the length of relationships between patients and oncologists, which may potentially affect uncertainty levels. Finally, we cannot infer causation due to the cross-sectional nature of our study.
Significant gaps remain in knowledge about uncertainty in older adults with advanced cancer. Sources of uncertainty in older adults are not well studied. It is also unknown if all patients benefit from addressing uncertainty. Individual tolerance to uncertainty may differ, and influence the cognitive appraisal and response to an uncertainty-triggering situation, such as the diagnosis of cancer. (31) Future efforts to study uncertainty in older adults should aim to identify sources of uncertainty and the effects of uncertainty on psychological health and QoL in a prospective fashion, as well as other outcomes such as prognostic understanding, treatment decision-making, and treatment adherence.
In conclusion, in a vulnerable population of older patients with advanced cancer, higher uncertainty was associated with poorer psychological health and QoL. Uncertainty management strategies tailored to the needs of older adults with advanced cancer are warranted.
Supplementary Material
Key message: This article describes the association of uncertainty with anxiety, depression, distress, and quality of life in an understudied population of older adults with advanced cancer. Our results indicate that a higher level of uncertainty is associated with worse psychological health and quality of life.
Acknowledgement:
We would like to thank Ms. Shuhan Yang for creation of the figure.
Funding
This work was funded through a Patient-Centered Outcomes Research Institute (PCORI) Program contract (4634; Mohile), K99CA237744 (Loh), UG1CA189961, R01CA177592 (Mohile), and R01CA168387 (Duberstein) from the National Cancer Institute, K24AG056589 from the National Institute of Aging (Mohile), Wilmot Research Fellowship (Loh), and UICC Technical Fellowship (Verduzco-Aguirre). This work was made possible by the generous donors to the Wilmot Cancer Institute (WCI) geriatric oncology philanthropy fund. All statements in this report, including its findings and conclusions, are solely those of the authors, do not necessarily represent the official views of the funding agencies, and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors, or Methodology Committee.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors have no conflicts of interest to disclose.
References
- 1.Mishel MH. The measurement of uncertainty in illness. Nurs Res 1981;30:258–263. [PubMed] [Google Scholar]
- 2.Han PKJ, Babrow A, Hillen MA, et al. Uncertainty in health care: Towards a more systematic program of research. Patient Educ Couns 2019;102:1756–1766. DOI: 10.1016/j.pec.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 3.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. DOI: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 4.Gramling R, Stanek S, Han PKJ, et al. Distress Due to Prognostic Uncertainty in Palliative Care: Frequency, Distribution, and Outcomes among Hospitalized Patients with Advanced Cancer. J Palliat Med 2018;21:315–321. DOI: 10.1089/jpm.2017.0285. [DOI] [PubMed] [Google Scholar]
- 5.Parker PA, Alba F, Fellman B, et al. Illness uncertainty and quality of life of patients with small renal tumors undergoing watchful waiting: a 2-year prospective study. Eur Urol 2013;63:1122–1127. DOI: 10.1016/j.eururo.2013.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall DL, Mishel MH, Germino BB. Living with cancer-related uncertainty: associations with fatigue, insomnia, and affect in younger breast cancer survivors. Support Care Cancer 2014;22:2489–2495. DOI: 10.1007/s00520-014-2243-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richardson A, Wagland R, Foster R, et al. Uncertainty and anxiety in the cancer of unknown primary patient journey: a multiperspective qualitative study. BMJ Support Palliat Care 2015;5:366–372. DOI: 10.1136/bmjspcare-2013-000482. [DOI] [PubMed] [Google Scholar]
- 8.Wallace M Uncertainty and quality of life of older men who undergo watchful waiting for prostate cancer. Oncol Nurs Forum 2003;30:303–309. DOI: 10.1188/03.ONF.291-300. [DOI] [PubMed] [Google Scholar]
- 9.Mishel MH, Hostetter T, King B, et al. Predictors of psychosocial adjustment in patients newly diagnosed with gynecological cancer. Cancer Nurs 1984;7:291–299. [PubMed] [Google Scholar]
- 10.Zhang Y Uncertainty in Illness: Theory Review, Application, and Extension. Oncol Nurs Forum 2017;44:645–649. DOI: 10.1188/17.ONF.645-649. [DOI] [PubMed] [Google Scholar]
- 11.Mohile SG, Epstein RM, Hurria A, et al. Communication With Older Patients With Cancer Using Geriatric Assessment: A Cluster-Randomized Clinical Trial From the National Cancer Institute Community Oncology Research Program. JAMA oncology 2019:1–9. DOI: 10.1001/jamaoncol.2019.4728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohile SG, Dale W, Somerfield MR, et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy: ASCO Guideline for Geriatric Oncology. J Clin Oncol 2018:Jco2018788687. DOI: 10.1200/jco.2018.78.8687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pergolotti M, Deal AM, Williams GR, et al. Activities, function, and health-related quality of life (HRQOL) of older adults with cancer. J Geriatr Oncol 2017;8:249–254. DOI: 10.1016/j.jgo.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Decoster L, Quinten C, Kenis C, et al. Health related quality of life in older patients with solid tumors and prognostic factors for decline. J Geriatr Oncol 2019;10:895–903. DOI: 10.1016/j.jgo.2019.03.018. [DOI] [PubMed] [Google Scholar]
- 15.Kurita K, Garon EB, Stanton AL, et al. Uncertainty and psychological adjustment in patients with lung cancer. Psychooncology 2013;22:1396–1401. DOI: 10.1002/pon.3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clayton MF, Mishel MH, Belyea M. Testing a model of symptoms, communication, uncertainty, and well-being, in older breast cancer survivors. Res Nurs Health 2006;29:18–39. DOI: 10.1002/nur.20108. [DOI] [PubMed] [Google Scholar]
- 17.Mishel M Uncertainty in Illness Scales Manual. Chapel Hill, NC: University of North Carolina, 1997. [Google Scholar]
- 18.Wild B, Eckl A, Herzog W, et al. Assessing generalized anxiety disorder in elderly people using the GAD-7 and GAD-2 scales: results of a validation study. Am J Geriatr Psychiatry 2014;22:1029–1038. DOI: 10.1016/j.jagp.2013.01.076. [DOI] [PubMed] [Google Scholar]
- 19.Burke WJ, Roccaforte WH, Wengel SP. The short form of the Geriatric Depression Scale: a comparison with the 30-item form. J Geriatr Psychiatry Neurol 1991;4:173–178. [DOI] [PubMed] [Google Scholar]
- 20.Hurria A, Li D, Hansen K, et al. Distress in older patients with cancer. J Clin Oncol 2009;27:4346–4351. DOI: 10.1200/jco.2008.19.9463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Overcash J, Extermann M, Parr J, et al. Validity and reliability of the FACT-G scale for use in the older person with cancer. Am J Clin Oncol 2001;24:591–596. [DOI] [PubMed] [Google Scholar]
- 22.Toussaint A, Hüsing P, Gumz A, et al. Sensitivity to change and minimal clinically important difference of the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7). J Affect Disord 2020;265:395–401. DOI: 10.1016/j.jad.2020.01.032 [DOI] [PubMed] [Google Scholar]
- 23.Quinten C, Kenis C, Decoster L, et al. Determining clinically important differences in health-related quality of life in older patients with cancer undergoing chemotherapy or surgery. Qual Life Res 2019;28:663–676. DOI: 10.1007/s11136-018-2062-6 [DOI] [PubMed] [Google Scholar]
- 24.Hobbelink-van den Bos K Reliability of the distress thermometer as a measuring instrument for geriatric (70+) oncology patients. Physiotherapy 2016;102:E275–E276. DOI: 10.1016/j.physio.2016.10.349 [DOI] [Google Scholar]
- 25.King MT, Cella D, Osoba D, et al. Meta-analysis provides evidence-based interpretation guidelines for the clinical significance of mean differences for the FACT-G, a cancer-specific quality of life questionnaire. Patient Relat Outcome Meas 2010;1:119–26. DOI: 10.2147/PROM.S10621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kehoe LA, Xu H, Duberstein P, et al. Quality of Life of Caregivers of Older Patients with Advanced Cancer. J Am Geriatr Soc 2019;67:969–977. DOI: 10.1111/jgs.15862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parker PA, Davis JW, Latini DM, et al. Relationship between illness uncertainty, anxiety, fear of progression and quality of life in men with favourable-risk prostate cancer undergoing active surveillance. BJU Int 2016;117:469–477. DOI: 10.1111/bju.13099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wright SP. Adjusted P-Values for Simultaneous Inference. Biometrics 1992;48:1005–1013. DOI: 10.2307/2532694 [DOI] [Google Scholar]
- 29.Sawatsky M, Clyde M, Meek F. Partial Least Squares Regression in the Social Sciences. The Quantitative Methods for Psychology 2015;11:52–62. DOI: 10.20982/tqmp.11.2.p052. [DOI] [Google Scholar]
- 30.Lien Chin-Yen Lin Hung-Ru, Kuo Ing-Tiau, et al. Perceived uncertainty, social support and psychological adjustment in older patients with cancer being treated with surgery. J Clin Nurs 2009;18:2311–9. DOI: 10.1111/j.1365-2702.2008.02549.x. [DOI] [PubMed] [Google Scholar]
- 31.Strout TD, Hillen M, Gutheil C, et al. Tolerance of uncertainty: A systematic review of health and healthcare-related outcomes. Patient Educ Couns 2018;101:1518–1537. DOI: 10.1016/j.pec.2018.03.030. [DOI] [PubMed] [Google Scholar]
- 32.Vera N, McMillan SM. The relationship between uncertainty in illness and anxiety in patients with cancer. M s, University of South Florida, 2009. [Google Scholar]
- 33.Mishel MH, Germino BB, Gil KM, et al. Benefits from an uncertainty management intervention for African-American and Caucasian older long-term breast cancer survivors. Psychooncology 2005;14:962–978. DOI: 10.1002/pon.909. [DOI] [PubMed] [Google Scholar]
- 34.Mishel MH, Germino BB, Lin L, et al. Managing uncertainty about treatment decision making in early stage prostate cancer: a randomized clinical trial. Patient Educ Couns 2009;77:349–359. DOI: 10.1016/j.pec.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 35.Borneman T, Irish T, Sidhu R, et al. Death awareness, feelings of uncertainty, and hope in advanced lung cancer patients: can they coexist? International journal of palliative nursing 2014;20:271–277. DOI: 10.12968/ijpn.2014.20.6.271. [DOI] [PubMed] [Google Scholar]
- 36.Loh KP, Mohile SG, Lund JL, et al. Beliefs About Advanced Cancer Curability in Older Patients, Their Caregivers, and Oncologists. Oncologist 2019;24:e292–e302. DOI: 10.1634/theoncologist.2018-0890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Curtis JR, Engelberg R, Young JP, et al. An approach to understanding the interaction of hope and desire for explicit prognostic information among individuals with severe chronic obstructive pulmonary disease or advanced cancer. J Palliat Med 2008;11:610–620. DOI: 10.1089/jpm.2007.0209. [DOI] [PubMed] [Google Scholar]
- 38.Moth EB, Kiely BE, Martin A, et al. Older adults' preferred and perceived roles in decision-making about palliative chemotherapy, decision priorities and information preferences. J Geriatr Oncol 2019. DOI: 10.1016/j.jgo.2019.07.026. [DOI] [PubMed] [Google Scholar]
- 39.Hillen MA, Gutheil CM, Strout TD, et al. Tolerance of uncertainty: Conceptual analysis, integrative model, and implications for healthcare. Soc Sci Med 2017;180:62–75. DOI: 10.1016/j.socscimed.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 40.Han PK, Klein WM, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Making 2011;31:828–838. DOI: 10.1177/0272989X10393976. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


