Abstract
Objectives:
Congenital syphilis (CS) is the result of antepartum transmission from mother to fetus of the spirochete Treponema pallidum. Although preventable through timely screening and treatment, the incidence of CS in the United States (US) is increasing. This review describes the epidemiological trends in CS in the US from 1980 to 2019 and characteristics of mothers of infants with CS.
Methods:
We performed a narrative review of epidemiological studies of CS following PRISMA guidelines for reporting of observational studies in epidemiology. Quality and bias of included studies were assessed using the Newcastle-Ottawa scale. Studies which described the demographics and characteristics of pregnant women with syphilis or who delivered an infant with CS in the US were identified from PubMed and Embase.
Results:
We identified a total of 2,771 studies, of which 309 were selected for further review and 27 were included in the final analysis. Substance use during pregnancy was a risk factor for CS in 16 studies. Maternal cocaine use was described in 11 of the 16 studies, 10 of which were published between the years 1980 and 1999. No prenatal care was a risk factor for CS in 17 studies. Evidence of inadequate syphilis testing (i.e. no maternal screen, first screen after the first trimester, or no repeat screen in third trimester) or treatment (i.e. no treatment, treatment <30 days prior to delivery, or nonpenicillin treatment) was significantly associated with CS in 13 studies. Finally, higher rates of CS were reported among African-American women in 11 studies.
Conclusion:
Infection with and antepartum transmission of syphilis disproportionately affect certain subgroups of women. Women who report substance use during pregnancy are more likely to give birth to an infant with CS. No prenatal care and evidence of inadequate syphilis testing and treatment during pregnancy are also significantly associated with giving birth to an infant with CS. Finally, cases of CS disproportionately affect African-American women. Addressing the CS epidemic will require identification and targeted allocation of resources to communities at elevated risk for syphilis, removal of barriers to prenatal care, and ensuring timely treatment and adequate partner notification of identified cases.
Summary
Substance use, no or inadequate prenatal care and African-American ethnicity place women at greater risk for maternal syphilis and delivering an infant with congenital syphilis in the United States.
INTRODUCTION
Syphilis is a sexually transmitted infection that is caused by the spirochete, Treponema pallidum. The primary stage of syphilis is defined by a single, painless genital ulcer, called a chancre, at the site of inoculation. If untreated, syphilis can evolve to a secondary stage characterized by a polymorphic rash, lymphadenopathy, and other systemic manifestations. The secondary stage is followed by a variable asymptomatic latent period divided into early (<1 year) and late (>1 year) stages, until it progresses to the tertiary stage marked by cardiovascular and neurologic sequelae.(1) Syphilis can also be transmitted from mother to fetus antepartum, which can result in spontaneous abortion, still birth, and hydrops fetalis, or congenital syphilis (CS) in live-born infants. Early manifestations of CS (i.e. onset before 2 years of age) include mucocutaneous lesions and hepatosplenomegaly, while late manifestations (i.e. onset after 2 years of age) include Hutchinson teeth, saddle nose, saber shins and sensorineural deafness.(1)
The accepted therapy for syphilis in pregnancy is a penicillin regimen appropriate for the stage of syphilis the woman presents in. For primary, secondary and early latent syphilis, a single dose of 2.4 million units of benzathine penicillin G intramuscularly is recommended. Late latent and tertiary syphilis are treated with 3 weekly doses of 2.4 million units.
Despite the widespread availability of penicillin and serologic tests for syphilis, the period from 1983–1991 saw an increase in the incidence of CS in all regions of the United Sates (US). During the same period, an increase in the number of women using cocaine during pregnancy was observed, and an association between cocaine use and CS was described.(2) Following a steady decline since 1991, CS in the US has increased by 185% from 2013–2018, from 362 cases to 1,306.(3) Geographically, the West and South US carry the heaviest burden of CS, with the majority of cases concentrated in California, Texas, Louisiana, Arizona and Nevada. Commonalities in demographic data across four recent studies suggest that no prenatal care, substance use during pregnancy, African-American ethnicity, public health insurance, education less than high school and a history of incarceration may be associated with the increased incidence of maternal syphilis and antepartum transmission.(4–6)
The objective of this narrative review was to summarize knowledge on the structural and individual factors contributing to CS both historically and currently. By developing a better understanding of risk factors for maternal syphilis infection and CS transmission, public health interventions can be tailored and targeted to populations at greatest risk.
METHODS
Literature Search
We performed a narrative review of epidemiological studies following PRISMA guidelines for search of the literature. PubMed and Embase were searched from January 1, 1980, to December 31, 2019. We developed our search strategy in collaboration with a librarian. We used the following Mesh terms to search PubMed and Embase, respectively:
((“Syphilis, Congenital”[Mesh] AND (“1980/01/01”[PDat] : “2019/12/31”[PDat]) AND Humans[Mesh] AND English[lang])) OR (((Congenital syphilis[Text Word]) OR Hutchinson teeth[Text Word]) AND (“1980/01/01”[PDat] : “2019/12/31”[PDat]) AND Humans[Mesh] AND English[lang])
(‘congenital syphilis’/exp OR ’congenital syphilis: ab, ti’ OR ’hutchinson teeth: ab, ti’) AND [1980–2019]/py AND [humans]/lim AND [english]/lim
In addition to these searches, bibliographies of existing reviews and primary studies were scanned. Searches were limited to articles published in English and in the US.
Study Selection
The initial search of PubMed and EMBASE identified 2,761 citations. An additional 10 articles were included after reviewing relevant bibliographies. After removing duplicates, 2,676 citations underwent a crude title and abstract screen (Carolyn Smullin). The full text of 309 articles were screened for eligibility using the following inclusion criteria: (1) research conducted in the United States and in English (US); (2) included characteristics of pregnant women with positive serologic tests for syphilis; (3) include characteristics of pregnant women who delivered an infant with CS (CS). We included quantitative and qualitative studies in our review. While qualitative studies may not provide the same evidence for identification of risk factors as quantitative do, our goal for this review was to describe risk factors across studies and explore differences in those risk factors over time. We therefore determined it not necessary to remove cross-sectional studies or studies without a comparison group and included qualitative studies for greater data collection. While the initial literature search was not restricted by geography, we later chose to include only studies conducted in the US after recognizing that our aim was to inform clinical practice guidelines in the US. After excluding articles based on failure to meet inclusion criteria, 27 articles were identified, the full texts of which were read by two reviewers (CS, Shivani Mehta).(Figure 1)
Figure 1.
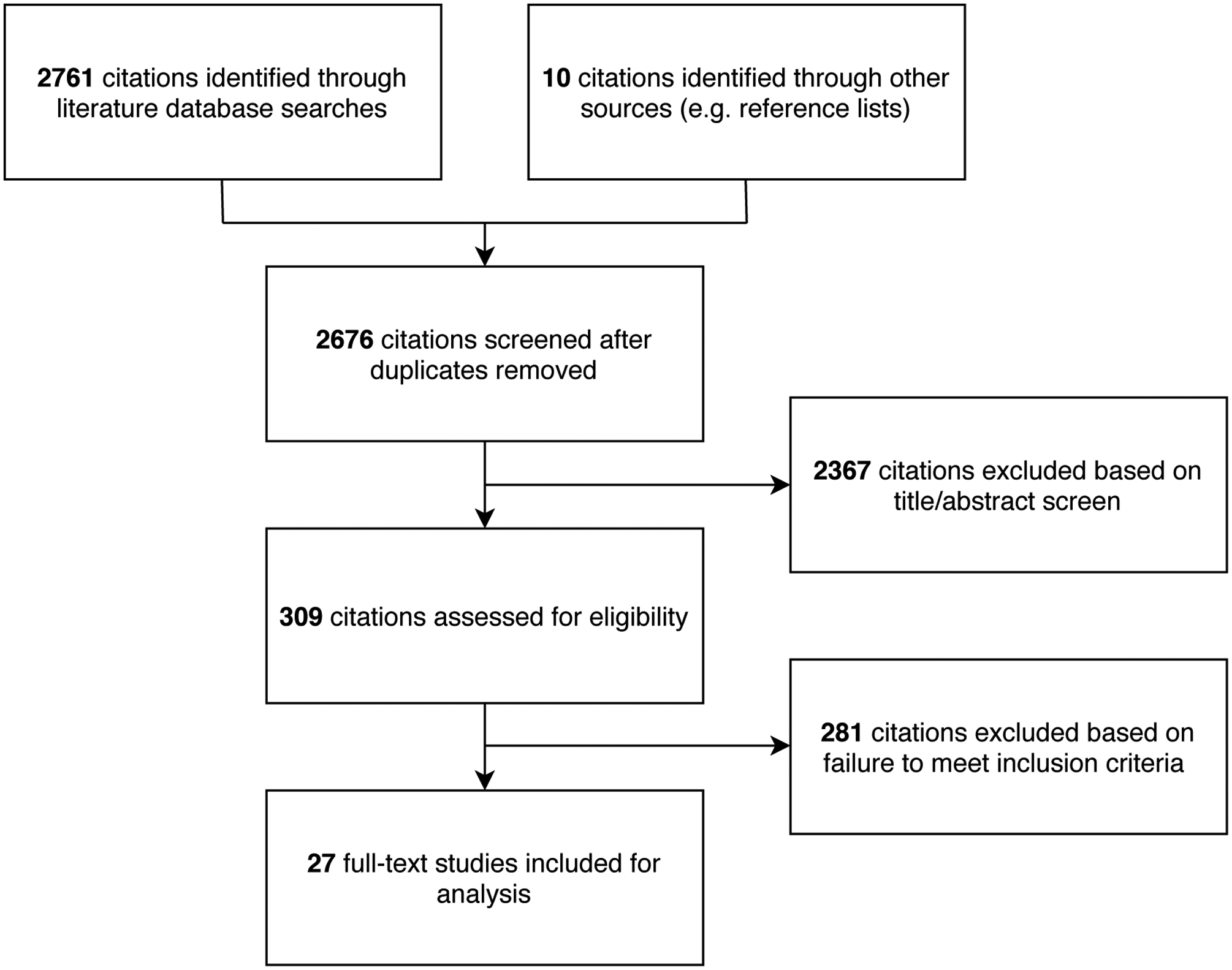
Article Screening and Selection Process
Data Extraction and Quality Assessment
The Newcastle-Ottawa scale was used to assess quality of each of the observational studies included in this review. Each study was judged on eight items assessing the selection of study groups, comparability of study groups, and ascertainment of the outcome, and rated as good, fair, or poor.(Supplemental Table 1) A good-quality study met all quality criteria. A fair-quality study failed to meet at least 1 criterion but had no known issue that would invalidate its results. Studies were rated as poor quality if they had major risk of bias. In order to maximize data for this review, no studies were excluded on the basis of poor quality. Following MOOSE guidelines for the evaluation and reporting of observational studies in epidemiology, we extracted the following data from each study: year, design, location, sample size, and effect estimates (e.g. odds ratios, rate ratios, risk ratios, or risk differences).
RESULTS
Study Design and Participant Demographics
Fourteen studies were published between the years 1980–1999; thirteen were published between the years 2001–2019. The majority of the studies were case control (number of studies (n)=16), followed by cross sectional (n=7) and cohort (n=4). Settings included New York (n=10), California (n=4), Texas (n=3), Michigan (n=3), Arizona (n=2), Georgia (n=2), Florida (n=1) and South Carolina (n=1). One study included data from across the US. Studies were conducted in urban and rural settings.
Among the 14 studies published between 1980–1999, an association was reported between CS and substance use during pregnancy in 12 studies, no prenatal care in 10 studies, inadequate syphilis testing and treatment in 7 studies, and African-American ethnicity in 7 studies. Of the 13 studies published between 2001–2019, an association was reported between CS and no prenatal care in 7 studies, inadequate syphilis testing and treatment in 6 studies, substance use during pregnancy in 4 studies, and African-American ethnicity in 4 studies. Other characteristics found to be associated with CS included single marital status (n=5), young maternal age (<30 years old) (n=4), low socioeconomic status (mean income <40,000) (n=2), education less than high school (n=2), having public insurance (n=2), being uninsured (n=1), and history of incarceration (n=1).(Table 1)
Table 1.
Summary of Study Characteristics Included in the Narrative Review
| Author | Year | Location | Study Design | Sample Size | Characteristics of mothers who gave birth to an infant with CS | Quality |
|---|---|---|---|---|---|---|
| Mascola L | 1984 | Texas | Cohort | 50 CS infants | African-American (RR 3.5, 95% CI 1.7–7.2) | Good |
| Minkoff HL | 1990 | New York | Case control | 1,206 parturient women | Cocaine use associated with maternal syphilis (OR 9.3l, 95% CI 5.2–16.5) | Good |
| Nanda D | 1990 | New York | Cross-sectional | 81 CS infants | 37% of women had no prenatal care 55% of women had inadequate therapy 40% of women reported substance use 88% of women who used substances reported cocaine use |
Good |
| Greenberg MS | 1991 | New York | Case control | 882 mother-infant pairs | Prenatal care (aOR 0.9, 95% CI 0.88–0.93) Maternal cocaine use (aOR 3.9, 95% CI 2.8–5.3) Maternal alcohol use (aOR 2.1, 95% 1.2–3.4) Single marital status (aOR 2.2, 95% 1.7–2.8) Education less than high school (aOR 1.3, 95% 1.1–1.7) |
Good |
| Desenclos JC | 1992 | Florida | Case control | 492 mother-infant pairs | African American (OR 15.6, 95% CI 4.8–50.4) Maternal substance use (OR 17.4, 95% CI 2.1–141.3) Lack of prenatal care (OR 6.3, 95% CI 2.0–16.7) Younger maternal age (OR 0.90, 95% CI 0.83–0.98) Single marital status (OR 4.6, 95% CI 1.4–14.9) Education less than high school (OR 3.3, 95% 0.8–13.4) |
Good |
| Rawstron SA | 1993 | New York | Case control | 403 pregnant women with syphilis | Protective effect of prenatal care (p<0.001) Protective effect of maternal therapy (p<0.001) High RPR titer (p<0.001) |
Good |
| Reyes MP | 1993 | Michigan | Cross-sectional | 148 mother-CS infant pairs | 95% African American 33% maternal cocaine use |
Fair |
| Webber MP | 1993 | New York | Cohort | 2,229 CS infants | Rates of CS increased the greatest for African American infants and rates were greatest in the highest cocaine exposure quartiles. | Good |
| Webber MP | 1993 | New York | Case control | 223 mother-infant pairs | Lack of prenatal care (aOR 11.0, 95% Cl 1.3–93 1) Maternal cocaine use (aOR 4.9, 95% Cl 1.8–13.0) African American (aOR 2.08, 95% CI 0.80–5.4) |
Good |
| McFarlin BL | 1994 | Michigan | Case control | 253 pregnant women with syphilis | High VDRL titer at diagnosis (p<0.001) | Good |
| Coles FB | 1995 | New York | Cross-sectional | 322 CS infants | 95% of women were of a racial minority (e.g. African American, Hispanic) 46% of women had no prenatal care 38% of women reported substance use 78% of women were < 30 years old 80% of women reported single marital status |
Good |
| Sison CG | 1997 | Michigan | Case control | 1012 infants | Positive meconium drug screen (OR 3.0, 95% CI 1.6–5.7) Positive cocaine screen (OR 3.7, 95% CI 1.9–7.0) |
Good |
| Mobley JA | 1998 | South Carolina | Case control | 673 CS and non-CS infants | African American (aOR 4.5, 95% CI 1.3–15.5) Maternal cocaine use (OR 9.3, 95% CI 2.6–33.1) No prenatal care (aOR 2.7, 95% CI 1.3–5.5) |
Good |
| Southwick KL | 1999 | Texas | Cohort | 91 pregnant women with syphilis | No prenatal care (RR 1.9, 95% CI 1.4–2.8) No syphilis test (RR 2.2, 95% CI 1.5–3.3) Syphilis test in 2nd or 3rd trimester (RR 1.4; 95% CI 0.9–2.2) Maternal cocaine use (RR 1.5, 95% CI 1.1–2.1) |
Good |
| Warner L | 2001 | Georgia | Case control | 157 CS infants | Racial minority (e.g. African American, Hispanic) (OR 5.6, 95% CI 2.5–12.7) Single marital status (OR 3.4, 95% CI 1.9–5.8) Maternal tobacco use (OR 5.8, 95% CI 4.2–7.9) Maternal alcohol use (OR 5.2, 95% CI 3.6–7.3) No prenatal care (OR 4.6, 95% CI 3.3–6.4) |
Good |
| Sheffield JS | 2002 | Texas | Case control | 43 pregnant women with syphilis | High VDRL titers (p=0.005) Treatment < 30 days prior to delivery (p<0.001) |
Good |
| Ogunyemi D | 2004 | California | Case control | 400 mother-infant pairs | Maternal cocaine use (OR 9.29, 95% CI 2.14–40.28) | Good |
| Taylor MM | 2008 | Arizona | Cross-sectional | 131 CS infants | 34% of women had no prenatal care 25% of women received treatment < 30 days prior to delivery 31% of women reported substance use |
Good |
| Kirckaldy RD | 2011 | Arizona | Case control | 242 pregnant women with syphilis | No prenatal care (p<0.001) Test in 1st or 2nd trimester (p<0.001) |
Good |
| Sia VM | 2011 | New York | Cross-sectional | 21 CS infants | 86% poor prenatal care | Fair |
| Patel S | 2012 | New York | Cross-sectional | 195 CS infants | 63% of women had one or more missed opportunities for prevention (late, inappropriate [nonpenicillin], or no therapy) | Good |
| Ghazaryan L | 2014 | New York | Case control | 85 CS infants | Lack of prenatal care (p=0.0338) | Good |
| Kachikis A | 2016 | Georgia | Cross-sectional | 101 CS infants | 61% of women were African American 72.3% of women had one or more missed opportunities for prevention (late, inappropriate [nonpenicillin], or no therapy) 21.8% of women had no prenatal care |
Good |
| Biswas HH | 2018 | California | Case control | 427 mother-infant pairs | No prenatal care (p<0.001) Protective effect of receipt of any prenatal care (p<0.001) First prenatal visit in third trimester (p<0.001) Inadequate testing (none, <40 days before delivery) (p<0.001) Inadequate treatment (no treatment, treatment <30 days prior to delivery, inappropriate for stage of syphilis) (p<0.001) |
Good |
| Veesenmeyer AF | 2018 | California | Cohort | African American vs. Caucasian (RR 5.97; 95% CI 4.36–8.17) Private insurance vs. public insurance (RR 0.29, 95% CI 0.19–0.43) Higher income (>45,000) vs. lower income household (< 25,000) (RR 0.87, 95% CI 0.80–0.94) |
Good | |
| Plotzker R | 2019 | California | Case control | 616 pregnant women with syphilis | Maternal methamphetamine use (p<0.001) | Good |
| Umapathi KK | 2019 | Nationwide | Case control | 5912 CS infants | African American vs. Caucasian (aOR 6.51, 95% CI 5.55–7.64) Private insurance vs. public insurance (aOR 0.24, 95% CI 0.21–0.29) Higher income (>45,000) vs. lower income household (< 25,000) (aOR 0.36, 95% CI 0.29–0.46) |
Good |
Maternal Risk Factors and Preventable Factors
Maternal substance use
The use of illicit substances during pregnancy was found to be a risk factor for CS in 16 of the 27 studies, 12 of which were published between 1980–1999 (7–18) and 4 between 2001–2019.(19–22) Of the remaining 11 studies, 4 failed to find an association between substance use during pregnancy and CS (4, 23–25) and 7 studies did not examine substance use.(5, 6, 26–30) Among the 16 studies which found substance use during pregnancy to be a risk factor for CS, 11 studies examined and found an association specifically with cocaine use, 10 of which were published between the years 1980–1999 (7–9, 11–14, 16–18) and 1 between 2001–2019 (20); one study examined and found an association specifically with methamphetamine use, which was conducted in California in 2019 (22); and 4 studies examined and found an association with non-disclosed substance use.(10, 15, 19, 21) Among the 4 studies which found no association between substance use during pregnancy and CS, one examined and found no association specifically with cocaine use (23) and one examined and found no association specifically with methamphetamine use.(4)
A confounding effect of drug use on utilization of prenatal care services and risk of CS was documented in 3 studies. Minkoff et al. reported that parturient women with syphilis and negative cocaine screens had higher rates of prenatal care compared to women with positive cocaine screens.(7) Similarly, a study from 1990 measuring the frequency of CS and association with maternal cocaine use found that more than 40% of CS case mothers reported drug use during pregnancy (88% of whom used cocaine) and that among the patients who used drugs, 76% received no prenatal care.(8) Finally, Plotzker et al. found that use of methamphetamines during pregnancy was associated with a decreased number of prenatal care visits, syphilis screenings, initiation of syphilis treatment and reduced CS prevention ratio.(22)
Prenatal care
Prenatal care was an important factor in informing whether a women was treated for syphilis during pregnancy and whether she delivered an infant with CS. Of the 27 studies, 17 found an association between no prenatal care and CS, 10 of which were published between 1980–1999 (7–11, 13, 15, 17, 18, 26) and 7 between 2001–2019.(4, 5, 19, 21, 25, 27, 29) Evidence of inadequate syphilis testing (i.e. no maternal screen, first screen after the first trimester, or no repeat screen in third trimester) or treatment (i.e. no treatment, treatment <30 days prior to delivery, or nonpenicillin treatment) in pregnancy was associated with CS in 13 studies, 7 of which were published between 1980–1999 (7, 8, 11, 12, 18, 23, 26) and 6 between 2001–2019.(4, 5, 21, 24, 25, 28) Importantly, most of these studies utilized the Council of State and Territorial Epidemiologists (CSTE) case definition for CS, which includes both probable and confirmed cases of CS. Probable cases of CS include infants born to mothers whose syphilis was untreated or inadequately treated; therefore, by definition women with no or late prenatal care will deliver an infant who meets the CSTE case definition for CS regardless of actual symptoms. The association between no or inadequate prenatal care and CS is therefore complicated. Screening and treatment of syphilis in pregnancy was protective against CS in 3 studies.(4, 11, 25) The following issues surrounding prenatal care were significantly associated with CS: no prenatal care (n=17); presenting late to prenatal care (i.e. first prenatal care visit after the first trimester) (n=3); inadequate syphilis testing during pregnancy (i.e. no test, first test after the first trimester, or no repeat test in third trimester) (n=4); and inadequate syphilis treatment during pregnancy (i.e. no treatment, treatment <30 days prior to delivery, or treatment with a nonpenicillin agent) (n=8). These findings suggest that lack of prenatal care significantly increases women’s risk of delivering an infant with CS, and furthermore, that even if women receive prenatal care, the care may be inadequate and therefore not protective against CS. These studies were equally distributed across 1980–2019, suggesting a longitudinal role of no or inadequate prenatal as a risk factor for CS.
African-American ethnicity
Cases of CS disproportionately affected infants born to African-American women and/or women of minority ethnicity (e.g. African-American, Hispanic) in 11 studies, 7 of which were published between the years 1980–1999 (10, 12–15, 17, 26) and 4 between 2001–2019.(5, 6, 19, 30) Mascola et al. found that among pregnant women receiving prenatal care, the rate of CS was 3 times higher for African-American women as for US-born Hispanic women, and that lack of prenatal care increased the risk for delivering an infant with CS to 30 times among African-American women.(26) On the other hand, 2 studies, published in 2011 and 2018, found no significant difference in the proportion of women by ethnicity who delivered infants with CS.(4, 25)
DISCUSSION
In this review, we summarize structural and individual factors associated with increased risk for CS among pregnant women in the US. We used data from 27 studies conducted across the US between the years 1980 and 2019. We found that infection with and antepartum transmission of syphilis disproportionately affect certain subgroups of women. Key maternal determinants of delivering an infant with CS included substance use during pregnancy, no prenatal care or late initiation of prenatal care, inadequate testing or treatment of syphilis during pregnancy, and being of African American ethnicity. Developing a better understanding of risk factors for maternal syphilis infection and CS transmission will be necessary in order to improve public health interventions in CS.
Women who reported substance use during pregnancy were found to be at increased risk for CS. Use of cocaine was specifically described as a risk factor for CS in 11 studies, 10 of which were published between 1980–1999 and one between 2001–2019. Despite a steady increase in rates of methamphetamine use by pregnant women since 2000, only one paper published during this time found methamphetamine use during pregnancy to be a risk factor for CS. Several thoughts have been offered on the association between substance use in pregnancy and CS. Substance use may increase the frequency of sexual activity due to exchange of sex for drugs, or may lead to increased unprotected (e.g., condom-less) sexual activity. Substance use may also lead to reduced use of prenatal care services out of longstanding medical mistrust. For example, the 1989 “Interagency Policy on Cocaine Abuse in Pregnancy”, which resulted from collaborations between the Medical University of South Carolina and local police and prosecutors and permitted nonconsensual drug testing of pregnant women, resulted in disproportionate arrest of poor and Black women on the charges of child neglect and distribution of drugs to a minor.(31) These measures, informed by national drug policy and longstanding racial stereotypes against women who use drugs during pregnancy, deter women from seeking prenatal care, causing missed opportunities for testing and treatment of maternal syphilis and prevention of CS. Limited data on substance use in pregnancy lessens our understanding of its potential role in CS and the need to consider more aggressive surveillance and intervention in less traditional settings.
Significantly higher rates of CS were found among parturient women who reported no prenatal care, delays in initiating prenatal care or inadequate prenatal care. A review of CS cases reported to the CDC in 2014 showed that 21.8% of mothers had no prenatal care, and among mothers of infants with CS who had one or more prenatal visits, 30% received inadequate treatment and 43% received no treatment for syphilis during the course of their pregnancy.(32) Low utilization of and engagement with prenatal care services can be explained by multiple factors, including burdens of poverty (e.g. cost of co-pays, discontinuities in health care coverage), competing priorities secondary to poverty (e.g. employment status, food insecurity), unmet social needs (e.g. housing, transportation, child care, mental health and substance use treatment), and undocumented status and fear of being denied legal permanent resident status on Public Charge grounds, which make prenatal care less of a priority. Missed opportunities for prevention can occur when providers fail to adequately screen and treat pregnant women with syphilis. Inadequate clinical guidance on the diagnosis and management of syphilis during pregnancy can leave prenatal care providers feeling unsure in their approach. Cuts to public health funding has undermined clinics’ and pharmacies’ ability to carry the appropriate treatment for syphilis, creating barriers to adequate treatment. A major price differential in the standard treatment for syphilis, Bicillin®, for clinics that do not qualify for 340B drug pricing (~$0.37/box vs $3,869.63/box manufacturer’s suggested retail price), disutility for other conditions, and reimbursement issues with Medi-Caid and Medi-Cal all present barriers to adequately treating pregnant women with syphilis.
Cases of CS disproportionately affect infants born to African-American women in the US. In 2018, 40.4% of reported CS cases occurred among Blacks, 32.6% occurred among Hispanics, and 22.7% occurred among Whites.(3) Higher rates of CS cases among Black infants parallels the higher rates of primary and secondary syphilis cases among Black persons. In 2018, 34.7% of reported primary and secondary syphilis cases occurred among Blacks, with a rate 4.7 times that seen among Whites. Missed opportunities for prevention of CS differ by race and ethnicity. As described in a 2020 Morbidity and Mortality Weekly Report (MMWR), the most commonly missed opportunity for prevention among Black and Hispanic mothers of infants with CS in the US South was lack of adequate maternal treatment, while lack of timely prenatal care was more common among white mothers. However, this racial/ethnic difference was not observed in the US West, where the most common missed opportunity for prevention among mothers of infants with CS – regardless of race/ethnicity – was lack of timely prenatal care.(33) Black and African-American women may be less likely to seek, utilize or engage in prenatal care due to disadvantages stemming from social, economic and political factors. More frequent contacts with the health care system increase the likelihood of both detecting and treating maternal syphilis infections early in pregnancy and reinfections after adequate treatment, and is therefore a critical component to managing syphilis in pregnancy. Efforts to reduce underlying racial disparities in health care may help to ameliorate racial differences in CS prevalence.
Finally, young maternal age, single marital status, low household income, uninsured or having public health insurance, and low educational achievement were found to be associated with increased risk for CS. Prior history of incarceration, which may interfere with recommended care during pregnancy, was common among parturient women with syphilis but not a risk factor for delivering an infant with CS. Systematic identification and treatment of the highest-risk women infected with syphilis can have the greatest impact on CS control.
There are potential limitations to this review. First, the results of this review may lack external validity. Results of publications from the 1980’s and 1990’s may no longer be relevant to our understanding of the present CS epidemic. However, monitoring variation in epidemiological trends over time enables us to identify longitudinal risk factors which can be targeted for intervention. Finally, due to our inclusion criteria, our review failed to include findings from qualitative studies which, while not representative or population-based, provide rich understanding of the very important contextual pieces.
Our review provides important insight into the CS epidemic. Despite the highest number of CS cases in recent years being in California, and the highest CS incidence rates being in Los Angeles county, very few studies on the topic have come from California, and zero from Los Angeles. Additional research is needed to better characterize the demographic and behavioral characteristics that place pregnant women at risk of delivering an infant with CS, to understand barriers to early antenatal care as well as what enables women to obtain care, and to identify obstacles to appropriate screening and timely treatment of syphilis.(Table 2) The primary prevention of CS requires new approaches. Previous studies have shown success in reducing rates of maternal and congenital syphilis through alternative screening methods and multi-disciplinary engagements.(Table 3) These studies support the conclusion that an effective CS prevention program will require strengthening of public health infrastructure and collaboration between health departments, prenatal care providers and other local organizations in order to engage women in prenatal care, perform proper community surveillance and contact tracing, and ensure timely access to adequate and appropriate prenatal care.
Table 2.
Key Research Priorities in the CS Epidemic
| Category | Example |
|---|---|
| Structural Factors | Identify systems with which at-risk women interface with (e.g. detention centers, drug rehabilitation programs, food banks). |
| Characterize how recent changes to Medicaid funding, coverage, and eligibility criteria influence rates of CS. | |
| Identify barriers to the implementation of syphilis screening and treatment guidelines in healthcare settings, including delays in test results, access to benzathine penicillin, costs, and administrative barriers. | |
| Individual Factors | Analyze the demographic and behavioral characteristics of mothers with infants with CS |
| Perform ethnographic assessments to understand and determine problems that occur along the pathway to prevention of CS. | |
| Assess women’s knowledge and awareness of sexual and reproductive health information. | |
| Assess women’s awareness of the importance of prenatal care. | |
| Identify barriers preventing women from engaging in prenatal care. | |
| Assess provider knowledge of the epidemiological profile of syphilis and CS, mother-to-child-transmission of syphilis. | |
| Assess provider knowledge and use of serological tests for identifying syphilis. | |
| Assess provider knowledge of correct treatment of an infected women and sexual partners. | |
| Assess provider knowledge of correct treatment of an infected women and sexual partners. |
Table 3.
Interventions Effective in Improving Syphilis Screening in Pregnancy and Reducing Incidence of CS in the US
| Author | Study | Location | Date | Study population | Description of Intervention | Results |
|---|---|---|---|---|---|---|
| Swain GR | Reducing the incidence of congenital syphilis in Milwaukee: a public/private partnership | Wisconsin | 1992–1996 | Pregnant women; physicians | -Asked public health nursing staff and Women, Infants and Children (WIC) providers to request 3 tests for syphilis from a pregnant woman’s provider. -Encouraged agencies which ran pregnancy tests for high-risk women to run a syphilis serology in parallel. -Targeted hospitals with the highest numbers of CS and provided education on epidemiology and screening guidelines for CS to medical staff. -Engaged the help of HMOs to encourage physicians to screen for syphilis according to guidelines. |
Calculated a 47% reduction in the risk of a pregnant woman with syphilis giving birth to an infant with CS (RR=0.53, 95% CI 0.33–0.84, P-0.0025) |
| Matthias J | Effectiveness of Prenatal Screening and Treatment to Prevent Congenital Syphilis | Louisiana, Florida | 2013–2014 | Pregnant women | Retrospectively analyzed the effect of third trimester screening (defined as 28 weeks GA to 30 days before delivery) on reducing rates of CS. | Identified 30 potential CS cases prevented due to third trimester screening and treatment. |
| Blank S | New Approaches to Syphilis Control | New York | 1996 | Female correctional inmates | Introduced on-site, rapid nontreponemal syphilis testing to the usual admission medical evaluation at a women’s correctional health clinic and evaluated its effectiveness in preventing CS. | Identified 17 of 55 pregnant women with positive syphilis tests. Prospective follow up for birth outcomes revealed 8 live births, of which only one which required CS treatment. |
| Silberstein GS | Effectiveness and Cost-Benefit of Enhancements to a Syphilis Screening and Treatment Program | New York | 2000 | Male and female correctional inmates | Implemented a rapid syphilis-screening program and estimated the number of cases of CS prevented using a model developed by the CDC. | Prevented 6.42 total case-equivalents of congenital syphilis. |
CONCLUSION
Congenital syphilis is a preventable disease. The most effective method of CS prevention includes regular prenatal care visits where appropriate screening, diagnosis and treatment of maternal syphilis can occur. This review is a reminder that the elimination of CS is a public health priority. Addressing the CS epidemic will require identification and targeted allocation of resources to communities at elevated risk for syphilis, removal of barriers to prenatal care, and ensuring timely treatment and adequate partner notification of identified cases.
Supplementary Material
Funding
JDK received funding from 1R01AI139265.
Footnotes
Competing interests None to declare.
References
- 1.Singh A, Romanowski B. Syphilis: Review with Emphasis on Clinical, Epidemiologic, and Some Biologic Features. Clin Microbiol Rev. 1999;12(2):187–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control (CDC). Syphilis and congenital syphilis--United States, 1985–1988. MMWR Morb Mortal Wkly Rep. 1988;37(32):486–489. [PubMed] [Google Scholar]
- 3.Centers for Disease Control (CDC). Sexually Transmitted Disease Surveillance 2018. Atlanta, GA: Department of Health and Human Services; 2019;https://www.cdc.gov/nchhstp/newsroom/2019/2018-STD-surveillance-report.html. [Google Scholar]
- 4.Biswas HH, Chew Ng RA, Murray EL, et al. Characteristics Associated With Delivery of an Infant With Congenital Syphilis and Missed Opportunities for Prevention-California, 2012 to 2014. Sex Transm Dis. 2018;45(7):435–441. [DOI] [PubMed] [Google Scholar]
- 5.Kachikis A, Schiff MA, Chapple-McGruder T, et al. Characteristics of and factors contributing to congenital syphilis cases in Georgia: 2000–2009. In: IDSOG Abstracts Am J Obstet Gynecol. 2016:835. [Google Scholar]
- 6.Umapathi KK, Thavamani A, Chotikanatis K. Incidence Trends, Risk Factors, Mortality and Healthcare Utilization in Congenital Syphilis-related Hospitalizations in the United States: A Nationwide Population Analysis. Pediatr Infect Dis J. 2019;38(11):1126–1130. [DOI] [PubMed] [Google Scholar]
- 7.Minkoff HL, McCalla S, Delke I, et al. The relationship of cocaine use to syphilis and human immunodeficiency virus infections among inner city parturient women. Am J Obstet Gynecol. 1990;163(2):521–526. [DOI] [PubMed] [Google Scholar]
- 8.Nanda D, Feldman J, Delke I, et al. Syphilis among parturients at an inner city hospital: association with cocaine use and implications for congenital syphilis rates. NY Med. 1990;90(10):488–490. [PubMed] [Google Scholar]
- 9.Greenberg MS, Singh T, Htoo M, et al. The association between congenital syphilis and cocaine/crack use in New York City: a case-control study. Am J Public Health. 1991;81(10):1316–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Desenclos JC, Scaggs M, Wroten JE. Characteristics of mothers of live infants with congenital syphilis in Florida, 1987–1989. Am J Epidemiol. 1992;136(6):657–661. [DOI] [PubMed] [Google Scholar]
- 11.Rawstron SA, Jenkins S, Blanchard S, et al. Maternal and congenital syphilis in Brooklyn, NY: epidemiology, transmission, and diagnosis. Am J Dis Child. 1993;147(7):727–731. [DOI] [PubMed] [Google Scholar]
- 12.Reyes MP, Hunt N, Ostrea EM, et al. Maternal/congenital syphilis in a large tertiary-care urban hospital. Clin Infect Dis. 1993;17(6):1041–1046. [DOI] [PubMed] [Google Scholar]
- 13.Webber MP, Lambert G, Bateman DA, et al. Maternal Risk Factors for Congenital Syphilis: A Case-Control Study. Am J Epidemiol. 1993;137(3):415–422. [DOI] [PubMed] [Google Scholar]
- 14.Webber MP, Hauser WA. Secular trends in New York City hospital discharge diagnoses of congenital syphilis and cocaine dependence, 1982–88. Public Health Rep. 1993;108(3):279–284. [PMC free article] [PubMed] [Google Scholar]
- 15.Coles FB, Hipp SS, Silberstein GS, et al. Congenital syphilis surveillance in upstate New York, 1989–1992: implications for prevention and clinical management. J Infect Dis. 1995;171(3):732–735. [DOI] [PubMed] [Google Scholar]
- 16.Sison CG, Ostrea EMJ, Reyes MP, et al. The resurgence of congenital syphilis: a cocaine-related problem. J Pediatr. 1997;130(2):289–292. [DOI] [PubMed] [Google Scholar]
- 17.Mobley JA, McKeown RE, Jackson KL, et al. Risk factors for congenital syphilis in infants of women with syphilis in South Carolina. Am J Public Health. 1998;88(4):597–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Southwick KL, Guidry HM, Weldon MM, et al. An epidemic of congenital syphilis in Jefferson County, Texas, 1994–1995: inadequate prenatal syphilis testing after an outbreak in adults. Am J Public Health. 1999;89(4):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Warner L, Rochat RW, Fichtner RR, et al. Missed opportunities for congenital syphilis prevention in an urban southeastern hospital. Sex Transm Dis. 2001;28(2):92–98. [DOI] [PubMed] [Google Scholar]
- 20.Ogunyemi D, Hernández-Loera GE. The impact of antenatal cocaine use on maternal characteristics and neonatal outcomes. J Matern Fetal Neonatal Med. 2004;15(4):253–259. [DOI] [PubMed] [Google Scholar]
- 21.Taylor MM, Mickey T, Browne K, et al. Opportunities for the prevention of congenital syphilis in Maricopa County, Arizona. Sex Transm Dis. 2008;35(4):341–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Plotzker R, Olson Burghardt N, Bauer H. Prenatal care entry among pregnant women with syphilis who use methamphetamines: a key to congenital syphilis prevention. Sex Trans Dis. 2019;95(Suppl 1):A81.2–A82. [Google Scholar]
- 23.McFarlin BL, Bottoms SF, Dock BS, et al. Epidemic syphilis: maternal factors associated with congenital infection. Am J Obstet Gynecol. 1994;170(2):535–540. [DOI] [PubMed] [Google Scholar]
- 24.Sheffield JS, Sánchez PJ, Morris G, et al. Congenital syphilis after maternal treatment for syphilis during pregnancy. Am J Obstet Gynecol. 2002;186(3):569–573. [DOI] [PubMed] [Google Scholar]
- 25.Kirkcaldy RD, Su JR, Taylor MM, et al. Epidemiology of syphilis among Hispanic women and associations with congenital syphilis, Maricopa county, Arizona. Sex Transm Dis. 2011;38(7):598–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mascola L, Pelosi R, Blount JH, et al. Congenital syphilis. Why is it still occurring? JAMA. 1984;252(13):1719–1722. [DOI] [PubMed] [Google Scholar]
- 27.Sia VM, Romero C, Sia DC, et al. Epidemiology of congenital syphilis in a South Bronx population: a follow-up study. J Perinat Med. 2011;39(1):71–75. [DOI] [PubMed] [Google Scholar]
- 28.Patel SJ, Klinger EJ, OʼToole D, et al. Missed opportunities for preventing congenital syphilis infection in New York City. Obstet Gynecol. 2012;120(4):882–888. [DOI] [PubMed] [Google Scholar]
- 29.Ghazaryan L, Muse A, Lee A, et al. Ten-Year Epidemiologic Review of Congenital Syphilis in New York State, Excluding New York City, 2003–2012. Presented at: STD Prevention Conference 2014;Atlanta https://www.cdc.gov/stdconference/2014/posters.htm [Google Scholar]
- 30.Veesenmeyer A, Boyajian J. Risk Factors for Congenital Infection in the United States: Analysis of the Kids’ Inpatient Database (KID). Open Forum Infect Dis. 2018;5(1):S221–222. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


