Abstract
Objective:
To determine the association between PTSD symptoms due to prior trauma and prior trauma type with PTSD symptoms after suspected acute coronary syndrome (ACS).
Method:
A consecutive sample of patients presenting to the emergency department (ED) for suspected ACS were surveyed. Logistic regression was used to estimate the odds of elevated ACS-related PTSD symptoms [PCL-S≥33] at 1-month associated with PTSD symptoms due to prior trauma and prior trauma type at the time of suspected ACS, adjusting for demographics, comorbidities, depression, and etiology of ACS symptoms.
Results:
Of 984 patients, 81.6% reported ≥1 prior trauma type and 22.5% reported PTSD symptoms due to prior trauma at the time of suspected ACS. One month later, 18.0% had ACS-related PTSD symptoms. Patients with versus without PTSD symptoms due to prior trauma at the time of the suspected ACS had increased odds of ACS-related PTSD symptoms one month later (42.1% vs 9.9%; aOR 4.49, 95% CI:3.05–6.60; p<.001). Prior life-threatening illness was the only trauma type significantly associated with ACS-related PTSD symptoms (aOR 1.57, 95% CI:1.03–2.39; p=.04).
Conclusions:
PTSD symptoms from prior trauma and history of life-threatening medical illness at the time of suspected ACS increased risk of ACS-related PTSD symptoms one month later.
Keywords: ACS-induced PTSD, Cardiovascular disease, Posttraumatic stress disorder, Trauma, Trauma-informed care
1. Introduction
The experience of acute, life-threatening medical events, such as acute coronary syndrome (ACS), can lead to the development of posttraumatic stress disorder (PTSD).1,2,3,4,5,6,7 Approximately one in eight patients develop elevated PTSD symptoms after ACS,8 which doubles the risk of recurrent cardiovascular events and mortality.9, 10 Even patients who present to the emergency department (ED) with suspected ACS but subsequently rule out are at risk for having PTSD symptoms attributed to the suspected ACS event.11
Outside of a medical setting, prior trauma exposure is a consistent predictor of PTSD after new traumas, especially for those with pre-existing PTSD from prior trauma.12, 13, 14, 15 PTSD from medical events differs from traditional conceptualizations of PTSD, as the trauma originates from within the body (e.g., blocked coronary artery), and thus patients are often preoccupied with fears of recurrent events coming from within their bodies as opposed to memories of the past trauma.16 Prior exposure to acute, life-threatening medical illness may especially predispose individuals to PTSD symptoms after an ACS through stress sensitization from related experiences.17 In contrast, trauma from non-medical events may also predispose patients to PTSD symptoms after medical events due to a more generalized disruption of psychological and neurobiological systems responsible for recovery after trauma.
It has not yet been studied whether specific types of prior trauma exposure differentially predispose patients towards the development of ACS-induced PTSD symptoms. Accordingly, the aim of our study was to describe the prevalence of prior exposure to diverse types of trauma and associated PTSD symptoms within an adult population presenting to the ED for suspected ACS. We further sought to test the association of prior types of trauma exposure, and prior PTSD symptoms with risk for PTSD symptoms after suspected ACS.
2. Methods
2.1. Patients and Protocol
Patients were drawn from a sample of 1,741 patients enrolled between 2013 and 2016 into the Reactions to Acute Care and Hospitalization (REACH) study.18 REACH is a prospective observational cohort of consecutive patients presenting to the ED of an urban academic medical center in New York City with suspected symptoms of ACS.
Patients were eligible if given a provisional diagnosis of “probable ACS” by an ED physician. Patients with ST-segment elevations upon presentation were excluded, as they were immediately taken to the cardiac catheterization laboratory. Patients were also excluded if they were unable to provide informed consent or complete study questionnaires from cognitive or functional impairment, needed immediate psychiatric intervention, had terminal non-cardiovascular illness, or did not speak English or Spanish. All patients provided written informed consent, and the study protocol was approved by the Institutional Review Board of Columbia University Irving Medical Center.
Patients completed self-report measures of sociodemographic characteristics, prior trauma exposure, and pre-existing PTSD symptoms as baseline questionnaires administered one to three days after presentation to the ED, asked in person in the hospital setting or by telephone after discharge. All measures were available in English or professionally translated Spanish, and interviews were conducted by research coordinators who were fluent in the patients’ preferred language. Patients were contacted by telephone one month after discharge to assess PTSD symptoms related to the suspected ACS event.
2.2. Measures
Dependent Variable:
PTSD Symptoms Related to Index Suspected ACS Event
PTSD symptoms after the suspected ACS were assessed 1 month after presentation using the PCL-S, with symptoms cued to the “heart problem, emergency room visit, and hospitalization that occurred one month ago when [they] enrolled in the study”
Key Predictors:
Prior Type of Trauma Exposure
Lifetime trauma exposure was assessed using the Life Events Checklist (LEC), a 16-item inventory of potentially traumatic life events.19 Patients indicated all types of events previously experienced; if any were reported, they identified the most distressing event. Trauma types were sorted into five categories: war-related, assaultive violence, life-threatening illness, other’s death or harm, and other injury or shocking event.20,21,22
PTSD Symptoms Related to a Prior Traumatic Event
PTSD symptoms present in the month prior to ED presentation due to a prior traumatic event were measured using the PTSD Checklist-Specific Stressor (PCL-S), a 17-item survey assessing the DSM-IV symptoms of PTSD; symptoms were cued to the most distressing event prior to the index event as per responses on the LEC.23, 24, 25, 26, 27 A PCL-S score ≥33 in a general population corresponds to elevated PTSD symptoms.28, 29
Covariates:
Sociodemographic characteristics were assessed by interview at study baseline. Baseline depressive symptoms were assessed with the eight-item Patient Health Questionnaire (PHQ-8).30, 31 A PHQ-8 score ≥10 has high sensitivity and specificity for diagnosing depression.32, 33 Medical comorbidity was assessed using the Charlson Comorbidity Index.34 Patient risk for mortality from the suspected ACS event was assessed using the Global Registry of Acute Coronary Events (GRACE) score.35 Reason for the index ACS symptoms (i.e., ACS confirmed or ruled-out) was determined based on independent review of the medical chart by two board-certified physicians blinded to PTSD status.36, 37
2.4. Cohort Assembly
Of the 1,741 patients in the cohort enrolled during the time period of this substudy, 361 patients were unavailable for 1-month follow-up and 396 patients were missing all data from one or more key variables, leaving 984 patients to be included in the current analyses. Those excluded did not differ from retained patients on any outcome variables or focal predictor variables; however, there were more true ACS patients retained (34.9% v. 26.4%; p < .001).
2.5. Statistical Analysis
Demographic and clinical covariates were compared between patients with and without elevated PTSD symptoms from prior trauma at baseline t-tests, nonparametric Wilcoxon tests, and chi-square tests. Odds of a positive PTSD screen at 1 month were modeled using PROC LOGISTIC in SAS v. 9.4. Covariates for adjusted analyses were selected based on a prior review of predictors of PTSD and included age, gender, ethnicity, race, depression at ED presentation, Charlson index, GRACE score, and ACS status.38, 39 Subsequently, categories of prior trauma were added to the model. These were dummy coded such that patients could experience multiple trauma types. As a sensitivity analysis, linear regression was used to examine the association between PTSD symptoms at time of index ACS event, prior trauma type, and risk of ACS-related PTSD symptoms (continuous).
3. Results
The mean age of patients was 61 years, 47.5% identified as female, and 56.7% identified as Hispanic (Table 1). Approximately one-third (34.9%) of patients had confirmed ACS, 10.8% had a different cardiac reason for their presenting symptoms, and the remaining 54.7% had a non-cardiac reason.
Table 1:
Demographic and Medical Characteristics of Suspected Acute Coronary Syndrome (ACS) Patients With and Without Elevated PTSD Symptoms Due to Prior Trauma Exposure at Time of Suspected ACS Event (N=984)
| Characteristic | PTSD (PCL-S ≥33) due to prior trauma (N=247) | No PTSD (PCL-S <33) due to prior trauma (N=737) | P value |
|---|---|---|---|
| Age, mean (SD) | 59.00 (12.63) | 62.22 (12.68) | <.001 |
| Female, N (%) | 129 (52.23%) | 338 (45.86%) | .08 |
| Race/ethnicity, N (%) | .22 | ||
| Hispanic | 140 (56.68%) | 418 (56.72%) | |
| Non-Hispanic Black | 59 (23.89%) | 139 (18.86%) | |
| Non-Hispanic White | 37 (14.98%) | 135 (18.32%) | |
| Other | 11 (4.45%) | 45 (6.11%) | |
| Depressive symptoms (PHQ-8 ≥10), N (%) | 146 (59.11%) | 128 (17.37%) | <.001 |
| GRACE Risk Score, mean (SD) | 91.18 (29.65) | 94.99 (29.51) | .08 |
| Charlson comorbidity index, median [IQR] | 2 [0, 3] | 1 [0, 3] | .03 |
| Etiology of suspected ACS symptoms, N (%) | .29 | ||
| Non-cardiac | 139 (56.28%) | 396 (53.73%) | |
| Cardiac, non-ACS | 31 (12.55%) | 75 (10.18%) | |
| ACS confirmed | 77 (31.17%) | 266 (36.09%) |
Abbreviations: ACS, Acute Coronary Syndrome; GRACE, Global Registry of Acute Coronary Events; PCL-S, PTSD Checklist for a Specific Stressor; PHQ-8, Patient Health Questionnaire.
More than three-quarters (81.6%) of patients experienced at least one type of prior traumatic event. Among patients exposed to at least one prior type of trauma, the median number of trauma types was 3 (range 1 to 17), with the most common types including sudden accidental death (54.6%) and transportation accident (35.5%; Figure 1). Overall, patients with elevated PTSD symptoms due to prior trauma had been exposed to a greater number of types of traumatic events as compared to patients without elevated PTSD symptoms (median 4, interquartile range 2–7 versus median 2, interquartile range 1–4; p<0.001).
Figure 1:
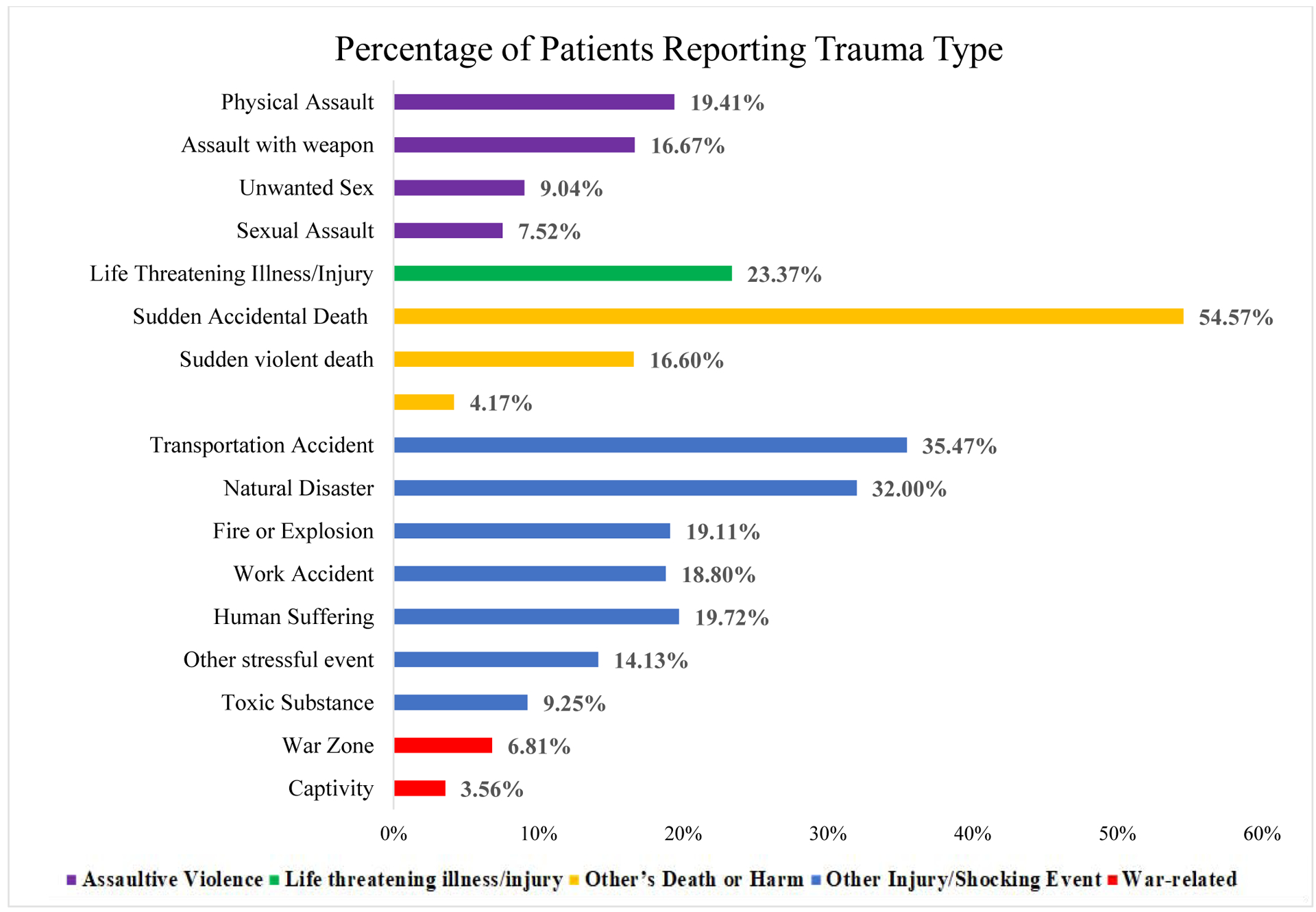
Percentage of Patients Presenting to the Emergency Department with Suspected Acute Coronary Syndrome Reporting Exposure to Each Trauma Type
Type of prior trauma exposure was evaluated using the Life Events Checklist.
Across the entire sample of patients, 25.1% had elevated PTSD symptoms from their most distressing trauma prior to the suspected ACS. Among patients with elevated PTSD symptoms from prior trauma, 42.1% had elevated PTSD symptoms attributed to their suspected ACS one month later. Among patients without prior elevated PTSD symptoms, only 9.9% had elevated PTSD symptoms after suspected ACS.
After adjustment for demographic and clinical characteristics, patients with versus without elevated PTSD symptoms from prior trauma had significantly greater odds of having PTSD from the suspected ACS event (adjusted OR 4.49, 95% CI: 3.05–6.60, p<.001; Table 2). When expanding the model to include trauma types, experiencing life-threatening illness was associated with risk of developing PTSD symptoms, over and above elevated PTSD symptoms from prior trauma (adjusted OR 1.57, 95% CI: 1.003–2.39, p=.04). Other trauma types were not significantly associated with a risk of developing PTSD symptoms (all p>0.2). In this expanded model, PTSD symptoms from prior trauma (adjusted OR 3.60, 95% CI: 2.39–5.43, p<.001) and depressive symptoms (adjusted OR 2.67, 95% CI: 1.81–3.93, p<.001) at the time of the index suspected ACS remained significant predictors of ACS-related PTSD symptoms one month later. This pattern of results replicated in sensitivity analyses examining continuous PTSD symptoms as the outcome variable.
Table 2:
Association of PTSD Symptoms due to Prior Trauma with PTSD symptoms 1-month after Suspected Acute Coronary Syndrome, with and without Adjusting for Prior Trauma Exposure (N=984)
| Characteristic | Model 1 (covariates and prior PTSD symptoms) aOR (95% CI) | p-value | Model 2 (Model 1 plus trauma types) aOR (95% CI) | p-value |
|---|---|---|---|---|
| Age | 0.99 (0.97–1.02) | .50 | 0.99 (0.97–1.02) | .54 |
| Hispanic | 1 (Ref) | 1 (Ref) | ||
| Female (versus male) | 1.0 | .37 | 1.0 | .22 |
| GRACE | 1.00 (0.99–1.01) | .99 | 1.00 (0.99–1.01) | .96 |
| Charlson index | 1.10 (0.99–1.22) | .08 | 1.09 (0.97–1.22) | .14 |
| Non-cardiac | 1 (Ref) | 1 (Ref) | ||
| PHQ-8 ≥ 10 | 2.69 (1.83–3.95) | <.001 | 2.67 (1.81–3.93) | <.001 |
| PTSD due to prior trauma (PCL-S ≥33) | 4.49 (3.05–6.60) | <.001 | 3.60 (2.39–5.43) | <.001 |
| Prior Life-Threatening Illness | 1.57 (1.03–2.39) | .04 | ||
| War-Related Trauma | 1.17 (0.66–2.07) | .59 | ||
| Assaultive Violence | 1.10 (0.81–1.82) | .35 | ||
| Other’s Death or Harm | 1.03 (0.68–1.56) | .89 | ||
| Other Injury or Shocking Event | 1.33 (0.84–2.11) | .22 |
PTSD symptoms were categorized as present if PTSD Checklist for a Specific Stressor (PCL-S) score ≥33.
Abbreviations: aOR, Adjusted Odds Ratio; ACS, Acute Coronary Syndrome; GRACE, Global Registry of Acute Coronary Events; PCL-S, PTSD Checklist for a Specific Stressor; PHQ-8, 8-Item Patient Health Questionnaire.
4. Discussion
Prior exposure to trauma was common in patients presenting to the ED with suspected ACS, with more than 80% of patients experiencing at least one type of prior trauma. Furthermore, approximately one in five patients had elevated PTSD symptoms from their most distressing prior trauma. This prevalence was within the range of PTSD estimates in the primary care setting (2–39%).40 This remains important as acute chest pain causes nearly 10% of all non-accident related presentations to the ED.41, 42
Patients with elevated PTSD symptoms from prior trauma were at markedly increased risk of having PTSD symptoms related to the suspected ACS one month later. This suggests that, consistent with PTSD that develops after non-medical traumatic events, prior trauma-related psychopathology is associated with vulnerability to ACS-induced PTSD symptoms.43 Given the high prevalence of pre-existing PTSD symptoms in patients presenting to the ED for suspected ACS and the association of PTSD at the time of suspected ACS with risk for subsequent ACS-related PTSD, a trauma-informed approach to the care of suspected ACS may be warranted. Trauma-informed care (TIC) seeks to reduce distress associated with illness through emphasis on emotional, physical, and psychological safety for trauma survivors and providers.44, 45
Small studies have shown prior trauma to be associated with the development of PTSD symptoms following myocardial infarction.46, 47 Our results expand this knowledge by showing that the only trauma type independently associated with elevated PTSD symptoms following suspected ACS was life-threatening illness. This finding differs from research showing that assaultive trauma types (e.g., combat experience) have higher conditional probabilities of PTSD than non-assaultive traumatic events.48,49 One possible explanation is that the unique traumatization experience of illness, comprised of internal somatic cues rather than external trauma cues, makes patients particularly vulnerable to traumatization by future medical events such as ACS through stress sensitization. Patients with prior trauma due to life-threatening illness may perceive themselves to be at greater risk of mortality or other adverse outcomes during the suspected ACS event. An alternative explanation, particularly if the prior life-threatening medical illness was a cardiac event, is that elevated PTSD symptoms at one month represented a continuation or exacerbation of pre-existing cardiac-related PTSD. Critically, the associations uncovered in this study emerged even when controlling for medical covariates (i.e., comorbidity, ACS type, and GRACE score).
Baseline depressive symptoms were also independently associated with elevated PTSD symptoms following suspected ACS. This finding is consistent with prior studies suggesting depression may be a risk factor for the development of PTSD, although additional research is necessary to confirm a relationship between baseline depression and subsequent PTSD given their high co-morbidity and potential shared response biases.50, 51
Study strengths included a large sample, diverse patient population, and measures of PTSD symptoms both before and after a suspected ACS. Yet, there were several limitations. The sample was enrolled from a single urban ED and excluded patients with ST-segment elevation myocardial infarction, limiting generalizability. Only a subset of patients had a confirmed ACS, though prior evidence suggests patients evaluated in the ED for suspected ACS have similar risk for developing PTSD whether or not ACS is confirmed. Additionally, PTSD symptoms were assessed using a survey instrument based on DSM-IV, while the gold standard remains psychiatric interview. ACS-related PTSD symptoms were asked with reference to the index heart problem, ED visit, or hospitalization, and thus may have been induced by traumatic aspects of their evaluation not specific to their ACS symptoms. PTSD symptoms related to prior trauma were assessed soon after presentation with a distressing suspected cardiac event; the heightened arousal associated with this suspected ACS event may have inflated PTSD symptom scores attributed to prior trauma. A substantial proportion of the enrolled sample was either unavailable follow-up or were missing data such that estimates of the prevalence of PTSD and trauma should be interpreted cautiously. Nevertheless, this is one of the largest surveys of PTSD in patients with suspected ACS events. While analyses adjusted for depressive symptoms, other mental disorders predictive of PTSD such as anxiety and conduct disorder were not included as potential confounders.68
In conclusion, among patients presenting to an ED for suspected ACS, there was a high burden of prior trauma and elevated PTSD symptoms. Patients with PTSD symptoms from prior trauma were at markedly increased risk of having PTSD symptoms one month after a suspected ACS. The specific type of prior trauma experienced was important, as only life-threatening illness was independently associated with risk for developing clinically significant ACS-induced PTSD symptoms. These findings can increase awareness about the psychological effect of prior trauma on patients who are evaluated for acute cardiac events and the importance of eliciting trauma history when assessing risk for development of adverse psychological consequences after suspected ACS.
Acknowledgments:
This project was supported by the National Heart, Lung, and Blood Institute (NHLBI; R01 HL117832, R01 HL123368). Dr. Young received additional support from NHLBI (T35HL007616-37). Dr. Chang was supported by grants from the NHLBI (R01 HL141811 and R01 HL146911). Dr. Kronish was supported by the National Institute for Aging (P30 AG064198.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
None.
References
- 1.Kutz I, Garb R, David D. Post-traumatic stress disorder following myocardial infarction. Gen Hosp Psychiatry. 1988;10(3):169–76. [DOI] [PubMed] [Google Scholar]
- 2.Edmondson D, Shaffer JA, Denton EG, Shimbo D, Clemow L. Posttraumatic stress and myocardial infarction risk perceptions in hospitalized acute coronary syndrome patients. Front Psychol. 2012;3:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gander ML, Von Känel R. Myocardial infarction and post-traumatic stress disorder: frequency, outcome, and atherosclerotic mechanisms. Eur J Cardiovasc Prev Rehabil. 2006;13(2):165–72. [DOI] [PubMed] [Google Scholar]
- 4.Spindler H, Pedersen SS. Posttraumatic stress disorder in the wake of heart disease: prevalence, risk factors, and future research directions. Psychosom Med. 2005;67(5):715–23. [DOI] [PubMed] [Google Scholar]
- 5.Tedstone JE, Tarrier N. Posttraumatic stress disorder following medical illness and treatment. Clin Psychol Rev. 2003;23(3):409–48. [DOI] [PubMed] [Google Scholar]
- 6.Edmondson D, Von Känel R. Post-traumatic stress disorder and cardiovascular disease. Lancet Psychiatry. 2017;4(4):320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sumner JA, Edmondson D. Refining our understanding of PTSD in medical settings. Gen Hosp Psychiatry. 2018;53:86–87. [DOI] [PubMed] [Google Scholar]
- 8.Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One 2012;7: 38915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kronish IM, Edmondson D, Li Y, Cohen BE. Post-traumatic stress disorder and medication adherence: results from the Mind Your Heart study. J Psychiatr Res. 2012;46(12):1595–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One. 2012;7(6):e38915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kronish IM, Edmondson D, Moise N, et al. Posttraumatic stress disorder in patients who rule out versus rule in for acute coronary syndrome. Gen Hosp Psychiatry. 2018;53:101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129(1):52–73. [DOI] [PubMed] [Google Scholar]
- 13.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68(5):748–66. [DOI] [PubMed] [Google Scholar]
- 14.Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: a prospective epidemiological study. Arch Gen Psychiatry. 2008;65(4):431–7. [DOI] [PubMed] [Google Scholar]
- 15.Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156(6):902–7. [DOI] [PubMed] [Google Scholar]
- 16.Edmondson D An Enduring Somatic Threat Model of Posttraumatic Stress Disorder Due to Acute Life-Threatening Medical Events. Soc Personal Psychol Compass. 2014;8(3):118–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Post RM, Weiss SR. Sensitization and kindling phenomena in mood, anxiety, and obsessive-compulsive disorders: the role of serotonergic mechanisms in illness progression. Biol Psychiatry. 1998;44(3):193–206. [DOI] [PubMed] [Google Scholar]
- 18.Birk J, Kronish I, Chang B, et al. The Impact of Cardiac-induced Post-traumatic Stress Disorder Symptoms on Cardiovascular Outcomes: Design and Rationale of the Prospective Observational Reactions to Acute Care and Hospitalizations (ReACH) Study. Health Psychol Bull. 2019;3:10–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004; 11:330–341. DOI: 10.1177/1073191104269954 [DOI] [PubMed] [Google Scholar]
- 20.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41(1):71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder: a study of youths in urban America. J Urban Health. 2004;81(4):530–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Breslau N, Lucia VC, Alvarado GF. Intelligence and other predisposing factors in exposure to trauma and posttraumatic stress disorder: a follow-up study at age 17 years. Arch Gen Psychiatry. 2006;63(11):1238–45. [DOI] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed Arlington: American Psychiatric Association; 2013. [Google Scholar]
- 24.Weathers F, Litz B, Herman D, Huska J, Keane T The PTSD checklist (PCL): Reliability, validity, and diagnostic utility Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX: 1993. October. [Google Scholar]
- 25.Blanchard EB, Jones-alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther. 1996;34(8):669–73. [DOI] [PubMed] [Google Scholar]
- 26.Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. J Consult Clin Psychol. 2008;76(2):272–81. [DOI] [PubMed] [Google Scholar]
- 27.Yao SN, Cottraux J, Note I, De mey-guillard C, Mollard E, Ventureyra V. [Evaluation of Post-traumatic Stress Disorder: validation of a measure, the PCLS]. Encephale. 2003;29(3 Pt 1):232–8. [PubMed] [Google Scholar]
- 28.Yeager DE, Magruder KM, Knapp RG, Nicholas JS, Frueh BC. Performance characteristics of the posttraumatic stress disorder checklist and SPAN in Veterans Affairs primary care settings. Gen Hosp Psychiatry. 2007;29(4):294–301. [DOI] [PubMed] [Google Scholar]
- 29.National Center for PTSD Using the PTSD Checklist for DSM-IV (PCL) National Center for PTSD; Washington, D.C.: U.S. Department of Veterans Affairs, 2012. [Google Scholar]
- 30.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord 2009;114:163–73. [DOI] [PubMed] [Google Scholar]
- 31.Razykov I, Ziegelstein RC, Whooley MA, Thombs BD. The PHQ-9 versus the PHQ-8--is item 9 useful for assessing suicide risk in coronary artery disease patients? Data from the Heart and Soul Study. J Psychosom Res 2012;73:163–8. [DOI] [PubMed] [Google Scholar]
- 32.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord 2009;114:163–73. [DOI] [PubMed] [Google Scholar]
- 33.Razykov I, Ziegelstein RC, Whooley MA, Thombs BD. The PHQ-9 versus the PHQ-8--is item 9 useful for assessing suicide risk in coronary artery disease patients? Data from the Heart and Soul Study. J Psychosom Res 2012;73:163–8. [DOI] [PubMed] [Google Scholar]
- 34.Charlsorn ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. [DOI] [PubMed] [Google Scholar]
- 35.Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, Van de Werf F, Avezum A, Goodman SG, Flather MD, Fox KA; Global Registry of Acute Coronary Events Investigators. Predictors [DOI] [PubMed] [Google Scholar]
- 36.Cannon CP, Battler A, Brindis RG, et al. American College of Cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. A report of the American College of Cardiology Task Force on Clinical Data Standards (Acute Coronary Syndromes Writing Committee). J Am Coll Cardiol. 2001;38(7):2114–30. [DOI] [PubMed] [Google Scholar]
- 37.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60(16):1581–98. [DOI] [PubMed] [Google Scholar]
- 38.Ozer Emily J., and Weiss Daniel S.. “Who Develops Posttraumatic Stress Disorder?” Current Directions in Psychological Science. 2004;13(4):169–172. [Google Scholar]
- 39.Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):37383. [DOI] [PubMed] [Google Scholar]
- 40.Greene T, Neria Y, Gross R. Prevalence, Detection and Correlates of PTSD in the Primary Care Setting: A Systematic Review. J Clin Psychol Med Settings. 2016;23(2):160–80. [DOI] [PubMed] [Google Scholar]
- 41.Bhuiya FA, Pitts SR, Mccaig LF. Emergency department visits for chest pain and abdominal pain: United States, 1999–2008. NCHS Data Brief. 2010;(43):1–8. [PubMed] [Google Scholar]
- 42.Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10):e56–e528. [DOI] [PubMed] [Google Scholar]
- 43.Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: a prospective epidemiological study. Arch Gen Psychiatry. 2008;65(4):431–7. [DOI] [PubMed] [Google Scholar]
- 44.Hopper EK, Bassuk EL, & Olivet J (2010). Shelter from the storm: Trauma-informed care in homelessness services settings. The Open Health Services and Policy Journal, 3, 80–100. [Google Scholar]
- 45.Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. https://store.samhsa.gov/product/SAMHSA-s-Concept-of-Trauma-and-Guidance-for-a-Trauma-Informed-Approach/SMA14-4884.html. July 2014.
- 46.Kutz I, Shabtai H, Solomon Z, Neumann M, David D. Post-traumatic stress disorder in myocardial infarction patients: prevalence study. Isr J Psychiatry Relat Sci. 1994;31(1):48–56. [PubMed] [Google Scholar]
- 47.Ayers S, Copland C, Dunmore E. A preliminary study of negative appraisals and dysfunctional coping associated with post-traumatic stress disorder symptoms following myocardial infarction. Br J Health Psychol. 2009;14(Pt 3):459–71. [DOI] [PubMed] [Google Scholar]
- 48.Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26(5):537–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Santiago PN, Ursano RJ, Gray CL, et al. A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: intentional and non-intentional traumatic events. PLoS ONE. 2013;8(4):e59236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Edmondson D, Kronish IM, Wasson LT, Giglio JF, Davidson KW, Whang W. A test of the diathesis-stress model in the emergency department: who develops PTSD after an acute coronary syndrome?. J Psychiatr Res. 2014;53:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Resnick HS, Kilpatrick DG, Best CL, Kramer TL. Vulnerability-stress factors in development of posttraumatic stress disorder. J Nerv Ment Dis. 1992;180(7):424–30. [DOI] [PubMed] [Google Scholar]
- 52.Sareen J Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Can J Psychiatry. 2014; 59(9):460–467. [DOI] [PMC free article] [PubMed] [Google Scholar]


