Abstract
An aerosolizing reducing technique for the extraction of impacted mandibular third molars with the use of a bibevel chisel and mallet will be presented. Every oral and maxillofacial surgeon should have this technique in their armamentarium, especially with the current global pandemic with the severe acute respiratory syndrome coronavirus 2, the cause of coronavirus disease 2019. In this era, we must all consider ways to reduce the number of aerosols produced during the extraction of third molars. Prioritizing hand instrumentation with the use of chisels and mallets will reduce aerosolization as compared with the more traditional technique of using a surgical handpiece.
As the experts in extractions of third molars, it is important that an oral and maxillofacial surgeon (OMS) is familiar and skilled in all techniques available for the removal of third molars and when to deploy them. Techniques for extraction of third molars described in literature include a chisel and mallet, rotary drills, and ultrasonic-based bone-cutting instruments.
On January 25, 2020, the World Health Organization published infection and prevention control guidelines to protect health workers, which recommended droplet and contact precautions with generalized care of the patients and airborne precautions with aerosolized generating procedures.1 The use of rotary drills and ultrasonic-based bone-cutting instruments in the extraction of third molars are aerosol-generating procedures conducted by OMSs.
Given the concern of aerosol generating techniques in dentistry and exposure of health care workers to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the authors felt now would be a prudent time to share their experience with the use of the chisel and mallet technique in the removal of third molars as a way of minimizing aerosol exposure. We also call on colleagues familiar with the use of chisels and mallets in exodontia to share their experiences in future publications.
Background
Pell and Gregory2 were the first to fully describe the extraction of impacted mandibular third molars using a mallet and chisel to split off the distal portion of the mandibular third molar in 1933. They described the benefits of this technique included smaller incisions, reduction or elimination of bone cutting, and reduction in operative time, swelling, trismus, and injury to the inferior alveolar nerve and surrounding tissues. A mallet and chisel have also been used in the lingual split technique first described by Ward in 1956.3
After the development of efficient high-speed surgical handpieces, the technique of using a chisel and mallet for extractions of mandibular third molars largely fell out of favor with most current practicing OMSs. This is evident in current publications of oral-maxillofacial surgery textbooks, including Peterson's Principles of Oral and Maxillofacial Surgery, 2nd and 3rd editions, by Miloro et al., Atlas of Oral and Maxillofacial Surgery by Kademani and Tiwana, Oral and Maxillofacial Surgery, 3rd edition, by Fonseca, and Contemporary Oral and Maxillofacial Surgery, 7th edition, by Hupp, which only demonstrate using a rotary surgical handpiece with a carbide bur for bone removal and sectioning of teeth for surgical extraction of mandibular third molars. The use of chisels is briefly mentioned in some current textbooks, but the technique is neither described nor illustrated, so it would be difficult for a surgeon to learn how to use a chisel and mallet in the removal of third molars with the contemporary literature available.
The most current published literature discussing and illustrating the chisel and mallet technique is in the 5th edition of the Oral and Maxillofacial Surgery book by W. Harry Archer that was published in 1975. In his text, Archer4 credits Pell and Gregory as the originators of the modified chisel and mallet technique. (Fig 1 ) Archer spent his career at the University of Pittsburgh where he developed new techniques and instruments.5 Author, Bernard Karian, DDS, was trained in Pittsburgh during Archer's career, where he was instructed in the removal of third molars using a chisel and mallet. There are many types of chisels and applications in exodontia. In this article, we focus on a technique to extract a mesioangular-impacted mandibular third molar, the most common type of impaction, with a chisel and mallet as an introduction to those who may not be familiar with this technique and skill.
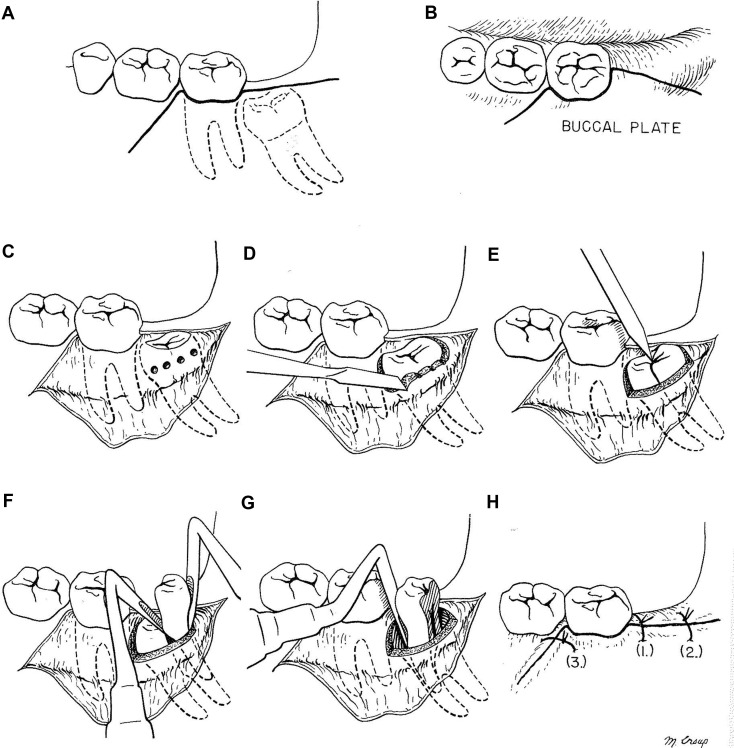
Figure 1.
Removal of class I, position C, mesioangular-impacted mandibular third molar. A, Standard flap design for extraction of mandibular third molars. B, Occlusal view of the flap design. The incision is kept on the buccal aspect to avoid the lingual nerve. C, After the flap is reflected, 4 pilot holes are drilled in the buccal cortical bone with a fissure bur. D, A sharp monobevel chisel is then used to remove buccal and distal bone around the crown of the impacted tooth. E, The crown and roots are then split with a sharp bibevel chisel. F, The distal aspect of the tooth is then removed using a No. 4 Apexo elevator placed into the split and a No. 5 Apexo elevator distally, using the buccal plate as a fulcrum to elevate the root anteriorly and superiorly. G, The mesial aspect of the tooth is then luxated with an elevator and removed. Only a small amount of bone had to be removed to deliver the impacted molar. H, Closure of the incision.
Reprinted from Oral and Maxillofacial Surgery, W. Harry Archer, Chapter 5 Impacted Teeth, page 274, (1975). This figure demonstrates the most recent illustrations of extracting impacted mandibular third molars with a chisel.4.
Surgical Technique
Patients first rinse with 1.5% hydrogen peroxide and then 0.12% chlorhexidine gluconate for 1 minute each before the start of the procedure. The CDC has stated that 0.5% hydrogen peroxide has bactericidal and virucidal activity after 1 minute,6 and a study by Kampf et al.7 in 2020 demonstrated that the coronavirus can be inactivated after 1 minute with 0.5% hydrogen peroxide. A preoperative Peridex rinse has been shown to decrease postoperative pain, infection, and alveolar osteitis8 , 9 and also decreases aerosolized infectious particles.10 The demonstrated case was performed under intravenous sedation, but can also be performed under local anesthesia.
The following will describe and demonstrate the chisel and mallet technique applied to a Pell and Gregory mesioangular class I, position B, 2rooted mandibular right third molar, #32. See Figure 2 for the panoramic image of the patient demonstrated throughout this article and in the video. (Fig 2). Go to Video 1 to see the procedure described in this article for extraction of an impacted tooth #32 with the chisel and mallet technique. (Video 1).11 The video and photographs included in this article were filmed with the proCam by Futudent.
Figure 2.
Panoramic radiograph. This is a panoramic radiograph of a 19-year-old man with a Pell and Gregory class 1, position B, mesioangular-impacted tooth #32. This is the patient demonstrated in the pictures and video mentioned in this article.
A standard full-thickness mucoperiosteal flap is performed to expose the impacted third molar. The tip of the Molt #9 elevator is then used to remove the thin alveolar bone around the coronal aspect of the impacted third molar. If the buccal bone is too thick to remove with the Molt #9 elevator, then a 4-mm stainless steel monobevel chisel and mallet are used (Figure 3, Figure 4 ). The monobevel chisel is placed at the mesiobuccal aspect of the impacted tooth with the bevel against the buccal bone aiming distally and is advanced slowly to remove the occlusal buccal bone with a mallet using light constant hammering, a motion similar to chopping onions. The chisel can be readjusted until enough of the buccal and coronal bone is removed and appropriate access is achieved. A stop cut is not used by the authors, as proper placement and positioning while using the mallet and gentle tapping prevents inappropriate fracturing of the buccal plate.
Figure 3.

Mallet. This is the Salvin Mead Mallet.
Figure 4.

Monobevel chisel. The Hartzell and Sons/Denmat SUH3 bone chisel with a 4-mm monobevel stainless steel tip is used for bone removal.
After the crown of the impacted tooth is exposed and before attempted elevation of the tooth, a 4-mm stainless steel bibevel chisel (Fig 5 ) is used to split the tooth. The tooth should not be luxated before use of a bibevel chisel because this may lead to an unsatisfactory split, mandibular fractures, and fluid splatter. The bibevel chisel is placed in the central groove at a 45° angle along the long axis of the tooth (Fig 6 ). The surgeon then uses 1 firm strike with the mallet to the bibeveled chisel to section the tooth. This 1 hit is typically enough to fracture the tooth, but sometimes, a second firm strike is required. Immediately after the initial hit, 2 smaller blows with the mallet are taken in the same location to widen the split. If there is no split after 3 blows with the mallet, this technique is abandoned, and a rotary surgical handpiece is used. If a surgical handpiece is to be used, then aerosolization will occur. An N95 or higher respiratory protection with a face shield for the surgeon and assistant are to be used if the patient is afebrile, does not have any pertinent health screening history, and the SARS-Co-2 status is not confirmed for an aerosolized procedure. If the patient has a negative PCR nasopharyngeal swab test for SARS-Co-2, in addition to the health screening history, a class III face mask with face shield is appropriate. The authors believe that the use of a chisel and mallet should be straightforward and should never be forced. This philosophy will prevent mishaps and complications.
Figure 5.

Bibevel chisel. This 4mm H & H bibevel chisel is a stainless steel chisel that is used to section teeth. It is a made to order instrument with the reference number 10-5313-04.
Figure 6.
Proper placement of the bibevel chisel for splitting of the mandibular third molar. The bibevel chisel is placed in the buccal central groove at a 45° angle to the occlusal buccal line angle along the long axis of the tooth.
Three different splits will typically occur depending on root development. The first and most common split is when the distal half of the crown is fractured. The fractured off distal coronal aspect of the tooth is first elevated out and removed with a 77R elevator and Kelly hemostats. The remaining tooth structure, including the mesial crown and the mesial and distal roots, is then elevated at the mesiobuccal aspect with the 77R elevator and delivered distally. Sometimes when elevating the mesial aspect of the tooth with both roots, the distal root fractures off and remains in place. The distal root can then be readily removed with a small hook scaler (Fig 7 ) by placing the tip of the scaler into the pulp canal and pulling coronally or by placing it in the periodontal ligament to elevate the root out of the socket (Fig 8 ). The second and most favorable fracture is a complete split through the furcation, dividing the tooth in half. The distal crown and root are elevated and removed with a 77R elevator, and then, the mesial crown and root are elevated and removed using a 77R elevator. On occasion with this scenario, the tooth is split in half, but the pieces are unable to be elevated due to thick buccal bone. At this point, the rotary surgical handpiece is used to trough the buccal bone to create space, but there is typically no need to section the tooth further. This reduces the risk of the bur passing through the tooth and perforating the lingual plate. The third type of fracture with the chisel and mallet technique is when the mesial quarter of the crown fractures off. While this does not occur often, the use of a surgical rotary handpiece is advised to complete the extraction because the mesial aspect of the crown will be locked in place below the second molar (Fig 9 ).
Figure 7.

Picture of a small hook scaler. A small hook scaler may be used to aid in the removal of fractured roots.
Figure 8.
Use of a small hook scaler for removal of a fractured root tip. This is a clinical demonstration of the placement of the small hook scaler for removal of the fractured root tip in the pulp canal.
Figure 9.
Image of split tooth #32 from the bibevel chisel. This demonstrates how the bibevel chisel split the tooth through the furcation. The distal crown fractured off and then the distal root was removed separately.
In an extraction with no debris, the authors do not see any need for irrigation which could be a potential cause of laryngospasm in the sedated patient. Figure 10 demonstrates the minimal bone removed and limited soft-tissue trauma with using the chisel and mallet technique compared with the traditional handpiece method (Fig 10).
Figure 10.
Surgical site after extraction of tooth 32. This photograph demonstrates the minimal bone removed and limited soft tissue trauma with using the chisel and mallet technique compared with the traditional handpiece method.
Discussion
“The primary objective in any form of surgery is to perform the operation successfully, skillfully, and as rapidly as possible with minimum amount of trauma to contiguous tissues.”2 The use of chisels can be gentle and swift as Pell and Gregory2 recognized in their publication by stating that the force delivered to the tooth to split it is negligible; it is a sharp but not a hard force. The chisel and mallet technique can be used with several mandibular third molar presentations, but when a surgeon is first learning the technique, we recommend starting with partial bony and mesioangular impacted teeth, as demonstrated in the article, and then advancing to other impacted teeth presentations when more comfortable.
In addition to likely preventing aerosolization because the procedure is being fully performed by hand instrumentation, there are several other advantages of the chisel and mallet technique in exodontia over the commonly used rotary handpiece. The proper use of chisels and mallets has the advantage of surgical speed and minimal trauma to the adjacent soft tissues. A rotary handpiece has a risk of causing soft-tissue lacerations to the tongue, lip, and/or cheeks and may also cause burns. The rotary handpiece can also cause damage to the adjacent teeth. A discussion was held with a national liability insurance carrier specializing in coverage of OMSs confirming that bur and handpiece injury to soft tissue and damage to adjacent teeth are common claims. It is known that a bur passing through the lingual plate of the mandible while sectioning an impacted mandibular third molar can cause injury to the lingual nerve. On occasion, the lingual plate may crack from the impact when the mallet and chisel is used to section a mandible third molar. There is little concern of lingual nerve injury when this happens because the chisel does not pass the bone and the periosteum remains intact. Another complication to consider with the use of a rotary handpiece is that the necessary irrigation has the potential to cause a laryngospasm in the sedated patient.
In the authors' experiences the complication rate using the chisel and mallet technique has not exceeded the complication rates of other practitioners that use surgical handpieces. This technique should be used when the roots are at least half developed and should not be used in a patient with osteogenesis imperfecta, an atrophic mandible, a mandibular tooth associated with a large lesion, or any other condition that would make the mandible more likely to fracture. In the combined 70 years of experience, the authors have not encountered a fractured mandible when using this technique. A surgeon familiar with the chisel and mallet technique can perform third molar extractions in the same amount of time or faster than with the use of a handpiece.
This technique is also cost effective because the cost and maintenance of a chisel and mallet is considerably less than a handpiece. The monobeveled tip chisel is $52, the bibevel tip chisel is $150, and the Salvin Mead Mallet is $147. Rotary surgical handpieces are subject to more wear and tear. The cost of repair of a surgical handpiece can range from $400 to $700 depending on the type of drill and what needs to be repaired. The handpiece is also out of service and unavailable during repairs. There are also recurrent costs associated with bur replacement, which is approximately $3 to $5 a bur.
On April 1, 2020, the American Dental Association released an algorithm to minimize the risk of SARS-CoV-2 transmission from emergency and urgent dental patients to health care personnel. In the algorithm, a procedure that did not produce any aerosols only required basic personal protective equipment including a non-N95 surgical mask, eye protection, gown, and gloves and stated that the risk of transmission was low. If there is aerosol production during a procedure, an N95 mask is then required in addition to eye protection, gown, and gloves.12 The American Dental Association also stated that hand instrumentation should be prioritized to reduce aerosol production as much as possible.13 The use of the chisel and mallet in exodontia achieves this.
In conclusion, extractions of third molars using this chisel and mallet technique are a potentially safer technique to use in regards to minimizing aerosols during the SARS-CoV-2 pandemic. Every effort should be made to reduce aerosols with all procedures as per American Dental Association guidelines. The surgeon, along with all of the other staff members, are at less risk of contracting an infection using this technique. This method is not only a safer technique for the extraction of third molars but is also time and cost effective. It is the preferred method of sectioning mandibular third molars when applicable for the authors and something all OMSs should be comfortable and familiar with as an option. This technique is also applicable in third world countries where power for instruments is not available. Once the surgeon is comfortable using a mallet and chisel to remove bone and section a mesioangular Pell and Gregory class I or II, position A or B third molar, the technique can also be used in other third molar presentations.
An extensive search of the literature shows there is no contemporary instruction of the use of chisels and mallet in exodontia. It appears to be a technique and skill that has been passed on from attending to resident in training. We encourage those with experience in the use of chisels and mallets in exodontia to publish their own experiences as these techniques are no longer taught in modern English oral and maxillofacial textbooks.
Footnotes
Conflict of Interest Disclosures: None of the authors have any relevant financial relationship(s) with a commercial interest.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.joms.2021.01.035.
Supplementary Data
Extraction of a Mandibular Third Molar with a Bi-bevel Chisel and Mallet. This video demonstrates the arousal reducing technique of extracting tooth #32 with chisels and mallets instead of using a traditional surgical handpiece.
References
- 1.World Health Organization . 2020. Infection Prevention and Control during Health Care when Novel Coronavirus (nCoV) Infection Is Suspected: Interim Guidance. [Google Scholar]
- 2.Pell G.J., Gregory G.T. Impacted Mandibular Third Molars: Classification and Modified Technique for Removal. Dent Dig. 1933;39:330. [Google Scholar]
- 3.Steel B. Lingual Split Versus Surgical Bur Technique in the Extraction of Impacted Mandibular Third Molars: A Systemic Review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:294. doi: 10.1016/j.tripleo.2011.07.028. [DOI] [PubMed] [Google Scholar]
- 4.Archer W.H. Oral and Maxillofacial Surgery (Ed 5). W.B. Saunders Company; Philadelphia, PA: 1975. Chapter 5. Impacted teeth; pp. 250–390. [Google Scholar]
- 5.About W. Harry Archer. https://www.acoms.org/page/Harry_Archer Available at:
- 6.Guideline for Disinfection and Sterilization in Healthcare Facilities. 2018. https://www.cdc.gov/infectioncontrol/guidelines/disinfection/disinfection-methods/chemical.html#Hydrogen Available at:
- 7.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of Coronavirus on Inanimate Surfaces and their Inactivation with Biocidal Agents. J Hosp Infect. 2020;104:246. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sridhar V., Wali G.G., Shyla H.N. Evaluation of the Perioperative Use of 0.2% Chlorhexidine Gluconate for the Prevention of Alveolar Osteitis After the Extraction of Impacted Mandibular Third Molars: A Clinical Study. J Maxillofac Oral Surg. 2011;10:101. doi: 10.1007/s12663-011-0206-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fenton D.A., Piecuch J.F. Perioperative Strategies for Third Molar Surgery. Atlas Oral Maxillofac Surg Clin North Am. 2012;20:225. doi: 10.1016/j.cxom.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Harrel S.K., Molinari J. Aerosols and Splatter in Dentistry: A Brief Review of the Literature and Infection Control Implications. J Am Dent Assoc. 2004;135:429. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chien A.T. Chisel and Mallet Extraction of Mandibular Right 3rd Molar (#32) 2020. https://fresnooralsurgery.com/chisel/ Available at: Accessed: 1/23/2021.
- 12.ADA Interim Guidance for Management of Emergency and Urgent Dental Care. 2020. https://www.ada.org/∼/media/CPS/Files/COVID/ADA_Int_Guidance_Mgmt_Emerg-Urg_Dental_COVID19.pdf?utm_source=adaorg&utm_medium=covid-resources-lp&utm_content=cv-pm-ebd-interim-flowchart&utm_campaign=covid-19?utm_source=adaorg&utm_medium=adanews&utm_content=c Available at:
- 13.ADA Interim Guidance for Minimizing Risk of COVID-19 Transmission. 2020. https://www.ada.org/∼/media/CPS/Files/COVID/ADA_COVID_Int_Guidance_Treat_Pts.pdf?utm_source=adaorg&utm_medium=covid-resources-lp&utm_content=cv-pm-ebd-interim-response&utm_campaign=covid-19?utm_source=adaorg&utm_medium=adanews&utm_content=cv-pm-ebd-interi Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Extraction of a Mandibular Third Molar with a Bi-bevel Chisel and Mallet. This video demonstrates the arousal reducing technique of extracting tooth #32 with chisels and mallets instead of using a traditional surgical handpiece.