We translated, cross-culturally adapted and tested the Neck Disability Index and the Numeric Rating Scale for neck pain in a Nepalese population. A cross-sectional study with test–retest design was performed. The Nepali versions showed good measurement properties and can be for assessing neck pain and disability.
Keywords: cervical radiculopathy, construct validity, discriminative validity, measurement properties, neck disability index, neck pain disorders, Nepal, numerical rating scale, patient reported outcome measure, reliability
Abstract
Study Design.
A cross-sectional study with a test–retest design.
Objective.
To translate and culturally adapt the numerical rating scale (NRS) for neck pain intensity and the Neck Disability Index (NDI), and asses their measurement properties in a Nepalese neck pain population.
Summary of Background Data.
Neck pain is one of the most common musculoskeletal disorders in Nepal. Research on neck pain disorders has been hampered by lack of standardized patient-reported outcome measures (PROMs) in Nepali language. Therefore, we aimed at validating a Nepali version of the NDI and NRS neck pain.
Methods.
At Dhulikhel hospital in Nepal, 150 patients with neck pain and/or cervical radiculopathy completed the translated self-administered questionnaires. We had made one cultural adaption of the NDI driving item in the final Nepali version. Relative reliability was analyzed with intraclass correlation coefficient (ICC 2.1) and absolute reliability with the smallest detectable change (SDC). Internal consistency was assessed by Cronbach alpha. Construct and discriminative validity was assessed by Spearman correlation for a priori hypotheses, receiver-operating characteristics curves, and analysis of variance. Time spent and assistance needed to complete the questionnaires were used to assess feasibility.
Results.
Test–restest reliability was excellent with ICC (95% confidence intervals) of 0.87 (0.66, 0.94) for NDI and 0.97 (0.94, 0.99) for NRS neck pain. The absolute reliability was acceptable (a SDC of 1.6 for NRS and 9.3 for NDI) and a Cronbach alpha (internal consistency) of 0.70 for NDI, as well as acceptable construct validity, discriminative validity, and feasibility.
Conclusion.
The Nepali versions of the NRS neck pain and NDI can be recommended for assessing pain and disability among patients with neck pain and cervical radiculopathy, but their responsiveness to change remains to be tested.
Level of Evidence: 2
Neck pain, along with low back pain, are the leading causes of disability worldwide.1 The largest increase in disability caused by neck pain has occurred in low- and middle-income countries in Asia, Africa, and the Middle east.2 In a low-income country like Nepal the prevalence of neck pain was 12.3% in 2018.3
To assess the impact of neck pain related disability in Nepal, access to translated, culturally adapted and, validated instruments for measuring health status is mandatory. However, most of the patient-reported outcome measures (PROMs) used for musculoskeletal disorders have been developed in English speaking countries. Development of new PROMs, specific for each country is time-consuming, expensive, and impractical. Cross-cultural adaptation and validation of commonly used PROMs worldwide can facilitate research and health surveillance across geographical areas.4 Moreover, use of PROMS can aid in communication between the physicians and patients, as well as between health care providers and policy makers.4
The most frequently used neck-specific PROM is the Neck Disability Index (NDI).5–7 The NDI, originally developed by Vernon and Mior in Canada, is a self-reported questionnaire covering 10 different items of neck pain-related disability. It has demonstrated acceptable measurement properties and a moderate to strong correlation with neck pain intensity scales, but reviewers have raised concerns about its reliability, responsiveness, and dimensionality.8–10 The NDI has been translated and validated into several languages.11–24 To our knowledge, no standardized PROMs for neck pain and function have been translated and validated into Nepali. More than 29 million people living in Nepal, North-East India, Bhutan, and Myanmar, and approximately 1.9 million Nepalese people overseas use Nepali as a lingua franca.25 The aim of this study was to translate, culturally adapt and validate a Nepali version of neck pain intensity, assessed on a 0 to 10 numerical rating scale (NRS), and the NDI.
MATERIAL AND METHODS
The study was carried out in two steps. First, the PROMs were translated and cross-culturally adapted into Nepali. Secondly, the Nepali versions were tested for psychometric properties in a cross-sectional design with 2 to 3 days of follow-up for test–retest, which would be appropriate for our study design.8
PROMs
At baseline, all participants completed the Nepali version of the NDI and NRS for neck pain intensity in addition to sociodemographic information, and two concurrent outcome measures.
The questionnaire (NDI)6 consists of 10 items assessing pain intensity, headache, concentration, sleeping and activities of daily living including work, personal care, lifting, reading, driving, and recreation with six different response alternatives from 0 (highest level of function) to 5 (lowest level). The sum of the 10 items was recalculated into a percentage NDI score from 0 to 100 (no to maximum disability). A questionnaire with missing responses on more than three of 10 items was not accepted. Otherwise, item scores were imputed, by using the mean score of all completed items.7,26
Neck pain intensity was assessed on 0 to 10 NRS with the following question; “How severe was your neck pain in the last week?,” with response options ranging from 0 (“no pain”) to 10 (“worst pain that I can imagine”).
Concurrent Outcome Measures
To assess construct validity we used the five items included in the generic health-related quality-of-life measurement (EQ-5D-3L) and its adjunct, a 20 cm vertical visual analogue scale (VAS health), by which participants could assess their current general health status from 0 to 100 (worst to best imaginable).27 The Nepali version of the EQ-5D-3L tools has been validated in a previous study.28 The five items in the EQ-5D-3L cover the following dimensions: mobility, self-care, activities of daily life, pain and anxiety, and/or depression. Each item is scored on an ordinal scale with three possible levels (no, mild to moderate, and severe problems). The index score of the EQ-5D-3L was not used in this study.
Translation and Cross-cultural Adaptation
Translation and cross-cultural adaptation of the NDI and NRS for neck pain intensity were performed according to international guidelines.4 The questionnaires were translated into Nepali independently by two persons (one clinician and one philologist), whose mother tongue was Nepali. The two translated versions were synthesized into one Nepali version before it was translated back to English. The back-translations were performed by two native English-speaking translators who were blinded to the original versions of the questionnaires. An expert committee consisting of the translators, researchers, and health professionals in our research group reviewed all translations and discussed discrepancies in a formal meeting. One cultural adaption was made in item number eight of the NDI (Driving). Most Nepalese people do not drive their own car and use motorbikes or are highly reliant on public transport. Trains are not available. By western standards, transportation is time-consuming, busses are overcrowded and roads are bumpy. Therefore, the item “drive car” was replaced with “travel by vehicle” before consensus on a pre-final version was achieved. The pre-final Nepali versions were then tested in six neck pain patients to assess language and feasibility. Since none of the patients had difficulties in understanding the meaning of the items or response alternatives, no further changes were made. The final NDI version in Nepali and English and the original English NDI version6 are presented as supplemental digital content.
Sample Size in the Second Step
The study sample size was determined according to international recommendations for assessing the methodological quality of outcome measures (The COSMIN checklist), developed by Mokkink et al.29 They suggest that at least 100 patients are necessary to test internal consistency, construct and discriminative validity and ceiling/floor effects, whereas 50 patients are needed to perform a test–retest reliability analysis.
Participants
The participants were recruited consecutively from two outpatient departments (OPDs) connected to the clinics of orthopedics and physical Medicine and Rehabilitation at Dhulikhel Hospital (DH), Kathmandu University Medical School (KUMS) from March 7th to September 11, 2017. DH is located approximately 30 km east from Kathmandu, Nepal. Data collection was managed by a research assistant. Patients who were unable to understand the questions due to psychiatric, neurological problems, patients with whiplash injury, and history of recent surgery were excluded. The questionnaire was self-administered, but the research assistant helped participants with reading and/or writing problems. Informed consent was obtained from each participant. Ethical approval was obtained from the Institutional Review Committee (IRC approval number 145/16) of DH, Kathmandu University Hospital.
Eligible participants were aged 18 to 70 years with neck pain of acute (<3 weeks), subacute (3–12 weeks), and chronic (>12 weeks) onset. Based on their clinical presentation, a physician at the OPD classified the patients into two diagnostic subgroups: radiculopathy group (radiculopathy with or without neck pain, n = 28) and neck pain group (neck pain without radiculopathy, n = 122).
Statistical Analyses and Hypotheses
The SPSS version 22 (IBM Armonk, NY: IBM Corp) was used. The results are presented as mean with standard deviation (SD) or 95% confidence interval (CI) if normally distributed, or median and interquartile range (25th–75th quartile) if skewed.
Feasibility and Data Quality
Time used (minutes) to complete questionnaires was measured. Missing values and floor or ceiling effects were described as proportions who reported the lowest or highest possible score. Proportions ≥15% are considered as floor and/or ceiling effects.27
Reliability
A paired t test was used to assess the mean difference between test and retest. An intraclass correlation coefficient (ICC 2.1) was used to assess relative reliability. ICC 2.1 of ≥0.70 was considered acceptable.25,28 Absolute reliability or measurement error was assessed by the smallest detectable change (SDC). It was calculated based on the standard error of measurement (SEM), which was estimated from a 2-way random analysis of variance. A 95% CI of SDC was estimated by the formula: 1.96 × √2 × SEMagreement.26
Internal consistency of the NDI total score was assessed by calculating the Cronbach alfa coefficient. A coefficient between 0.70 and 0.95 is considered to indicate acceptable homogeneity.26,29
Construct validity was investigated with predefined hypotheses between the two PROMs (NDI and NRS for neck pain intensity) and each of the items of the EQ-5D-3L and VAS health. Hypotheses of convergent and divergent validity were formulated to address the associations between aspects of the PROMs (Table 1). It was hypothesized that there would be a high correlation (≥0.6) or moderate correlation (0.4–0.6) between measures reflecting corresponding constructs (convergent validity) and a low correlation (≤0.4) between measures reflecting noncorresponding constructs (divergent validity) (hypotheses 1–4). The hypotheses were based on results from previous studies; for example, the correlation between the NDI score and NRS were expected to be high based on correlation coefficients around 0.70 in the original paper of Vernon et al.6 Construct validity was assessed by the Spearman rank order correlation coefficients (rho). An adequate construct validity was defined as a 75% correspondence between the calculated correlation coefficient and the predefined hypothesis.29
TABLE 1.
Construct Validity for the Numerical Rating Scale for NRS and the NDI in 150 Patients With Neck Pain and/or Radiculopathy
| Apriori-defined Hypothesis | Spearman Correlation Coefficient | Hypothesis Confirmed (Yes/No) |
| A high correlation was expected between NRS and total score of the NDI. | 0.79 | Yes |
| A high correlation was expected between NRS and the pain item from the EQ-5D ∗. | 0.83 | Yes |
| NRS was expected to be highly correlated to the personal care item in the EQ-5D. | 0.63 | Yes |
| NRS was expected to be highly correlated to the ADL item in the EQ-5D. | 0.70 | Yes |
| A moderate correlation was expected between NRS and the anxiety/depression item of the EQ-5D. | 0.66 | No |
| NRS was expected to be moderately correlated to the walking item in the EQ-5D | 0.58 | Yes |
| NRS were expected to be moderately correlated to health status by VAS† health. | −0.71 | No |
| We expected high correlation between the NDI and the personal care item from EQ-5D. | 0.67 | Yes |
| We expected high correlation between the NDI and the ADL item from EQ-5D. | 0.68 | Yes |
| We expected high correlation between the NDI and the pain item from the EQ-5D. | 0.78 | Yes |
| We expected high correlation between the NDI and the NRS. | 0.79 | Yes |
| We expected moderate correlation between the NDI and the walking item in the EQ-5D. | 0.60 | No |
| A moderate correlation was expected between the NDI and the anxiety/depression item of the EQ-5D. | 0.69 | No |
| NDI score was expected to be moderately correlated to health status by VAS health. | −0.74 | No |
NDI indicates Neck Disability Index; NRS, Numerical Rating Scale; VAS, visual analogue scale.
EuroQol- 5D 3L questionnaire, ADL indicates activities of daily living.
Visual analogue scale.
Discriminative validity was assessed by analysis of variance (ANOVA), comparing the mean PROM scores in the radiculopathy and neck pain only groups, expecting higher scores in the radiculopathy compared to the neck pain group. ANOVA was also used to assess whether the NRS and NDI could discriminate between different levels of health status. Low, moderate, and high levels of health status were calculated based on the 25th, 25 to 75th, and 75th percentiles of the 0 to 100 VAS health scale.
Discriminative validity was also assessed by using receiver-operating characteristics (ROC) analysis.26,29 We computed the area under the ROC curve (AUC), which reflects the accuracy of the measurement to differentiate between patients with cervical radiculopathy and those with neck pain only. The AUC may range from 0.50 (no discriminative ability) to 1.0 (perfect discriminative ability).26
RESULTS
Of a total of 150 patients, 50 participated in the test–retest evaluations. Baseline characteristics of the study population including the test–retest subgroup are presented in Table 2. Among patients with radiculopathy there were more females, and they were older and had higher pain and NDI scores compared to patients with neck pain only. The patients with neck pain only had higher educational level and less illiteracy than the patients with radiculopathy.
TABLE 2.
Characteristics of the Study Population (n = 150)
| Subgroups | Radiculopathy (n = 28) | Neck Pain Only (n = 122) |
| Age, mean (SD)a | 46.7 (13.2) | 36.2 (13.4) |
| Female sex, n (%) | 20 (71.4) | 69 (56.6) |
| Duration of neck pain | ||
| Acute (<3 wk) | 5 (17.9) | 45 (36.9) |
| Subacute (3–12 wk) | 7 (25.0) | 36 (29.5) |
| Chronic (>12 wk | 16 (57.1) | 41 (33.6) |
| NDI score, mean (SD) | 56.4 (19.2) | 37.6 (19.5) |
| NRS, mean (SD) | 6.4 (1.3) | 4.9 (1.7) |
| VAS Health state, mean (SD) | 56.0 (17.8) | 67.5 (17.4) |
| Bachelor or master education, n (%) | 5 (17.9) | 44 (36.1) |
| Illiterate, n (%) | 18 (64.3) | 38 (31.1) |
| Daily working hours, mean (SD) | 6.2 (2.9) | 6.6 (3.0) |
| Low monthly income < 10,000 NRs, n (%) | 20 (71.4) | 75 (61.5) |
| Smoker, n (%) | 5 (17.9) | 26 (22.0) |
| Occupation, n (%) | ||
| White collars | 7 (25.0) | 67 (54.9) |
| Blue collars | 21 (75.0) | 55 (41.5) |
| Ethnicity, n (%) | ||
| Brahmin | 5 (17.9) | 28 (23.0) |
| Chheri | 7 (25.0) | 23 (18.9) |
| Newar | 7 (25.0) | 43 (35.2) |
| Tamang | 4 (14.3) | 7 (5.7) |
| Magar | 1 (3.6) | 1 (0.8) |
| Dalit | 0 | 5 (4.1) |
| Others | 4 (14.3) | 15 (12.3) |
NDI indicates Neck Disability Index; NRS, Numerical R; SD, standard deviation; VAS, Visual analogue scale.
Feasibility, Data Quality, and Internal Consistency of the Measurements
Mean time used to complete the questionnaires was 7.7 (SD 2.1) minutes, and 67 (45%) of the patients needed assistance. Data on NDI completeness and internal consistency are presented in Table 3. All questionnaires were accepted. None had missing responses on more than two of 10 items. Of the individual items, two had a relatively high frequency of missing responses which were imputed: item 4 (reading, 36.7%) and 6 (concentration, 40.7%). No floor or ceiling effects were found.
TABLE 3.
Data quality and Internal Consistency of the NDI, n = 150.
| NDI ∗ | Missing, n (%) | Mean (SD) | Lowestn (%) | Highestn (%) | Cronbach Alpha/Item-Total Correlation |
| NDI total score (0–100) | 0 | 41.09 (20.72) | 0 | 0 | 0.70 |
| 1. Pain intensity | 0 | 2.60 (0.84) | 1 (0.7) | 1 (0.7) | 0.68 |
| 2. Personal care | 0 | 1.36 (0.97) | 28 (18.7) | 0 | 0.67 |
| 3. Lifting | 0 | 1.56 (1.18) | 28 (18.7) | 1 (0.7) | 0.66 |
| 4. Reading | 55 (36.7)† | 4.03 (3.86) | 19 (20.0) | 1 (0.7) | 0.67 |
| 5. Headache | 1 (0.7) | 1.96 (1.35) | 14 (9.3) | 4 (2.7) | 0.70 |
| 6. Concentration | 61 (40.7) | 4.33 (3.94) | 20 (22.5) | 0 | 0.67 |
| 7. Work | 0 | 1.45 (1.14) | 27 (18.0) | 3 (2.0) | 0.67 |
| 8. Driving | 0 | 1.27 (1.13) | 40 (26.7) | 0 | 0.67 |
| 9. Sleeping | 0 | 1.07 (1.11) | 57 (38.0) | 0 | 0.67 |
| 10. recreation | 0 | 0.91 (0.93) | 52 (34.7) | 1 (0.7) | 0.69 |
NDI indicates Neck Disability Index.
Items are scored on a 0–5point scale (5 represents more disability).
Non respondents were illiterate.
Test–Retest Reliability
There was no statistically significant difference between the total sample and the test–retest sample in the NRS pain intensity and NDI scores. Both NRS and NDI showed excellent test–retest reliability with ICC (95% CI) of 0.87 (0.66, 0.94) and 0.97 (0.94, 0.99), respectively. The absolute reliability was acceptable with a SDC of 1.6 for NRS and 9.3 for NDI (Table 4).
TABLE 4.
Internal Consistency and Reliability of the NRS for Neck Pain Intensity and the NDI. Retest Was 2 to 3 Days After the First Test (n = 50).
| Test (n = 50) | Retest (n = 50) | Chron-bach Alpha | ICC | Mean diff (SD) | SEM | SDC | |
| NRS (0–10), mean (SD) | 4.96 (1.91) | 4.44 (1.70) | — | 0.87 (0.66, 0.94) | 0.52 (0.79) | 0.56 | 1.55 |
| NDI score (0–100), mean (SD) | 36.8 (21.8) | 34.5 (21.0) | 0.99 | 0.97 (0.94, 0.99) | 2.28 (4.75) | 3.37 | 9.31 |
ICC indicates intra class correlation coefficient; NDI, Neck Disability Index; NRS, Numerical Rating Scale; SEM, standard error of measurement; SD, standard deviation; SDC, smallest detectable change.
Construct Validity
Table 1 displays the a priori defined hypotheses between the NDI and NRS for neck pain intensity and each of the items of the EQ-5D-3L and VAS health. Five of seven hypotheses (71%) for the NRS were confirmed (Table 1), whereas only four of seven hypotheses (57%) were confirmed for the NDI.
Discriminative Validity
The mean difference in NRS and NDI scores between the patients with cervical radiculopathy and those with neck pain only (Figure 1) was statistically significant (P < 0.001).
Figure 1.
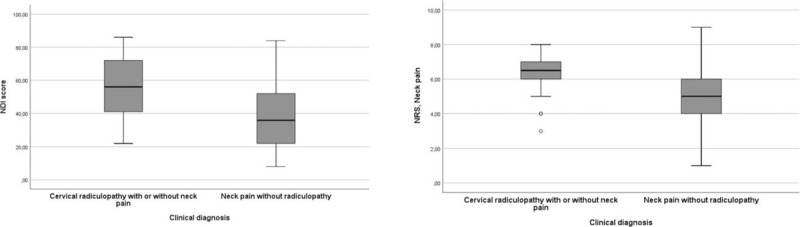
Discriminative ability of the NDI (left column) and the NRS for neck pain (right column). Mean scores differences were statistically significant P < 0.001 (analysis of variance) between subgroups with cervical radiculopathy and neck pain only (n = 150). NDI indicates Neck Disability Index; NRS, Numerical Rating Scale.
ROC analyses showed that the two instruments were moderately able to discriminate between the patients with radiculopathy and those with neck pain only. The AUC was 0.75 (0.66–0.85) for NDI and 0.75 (0.65–0.84) for NRS (Figure 2).
Figure 2.
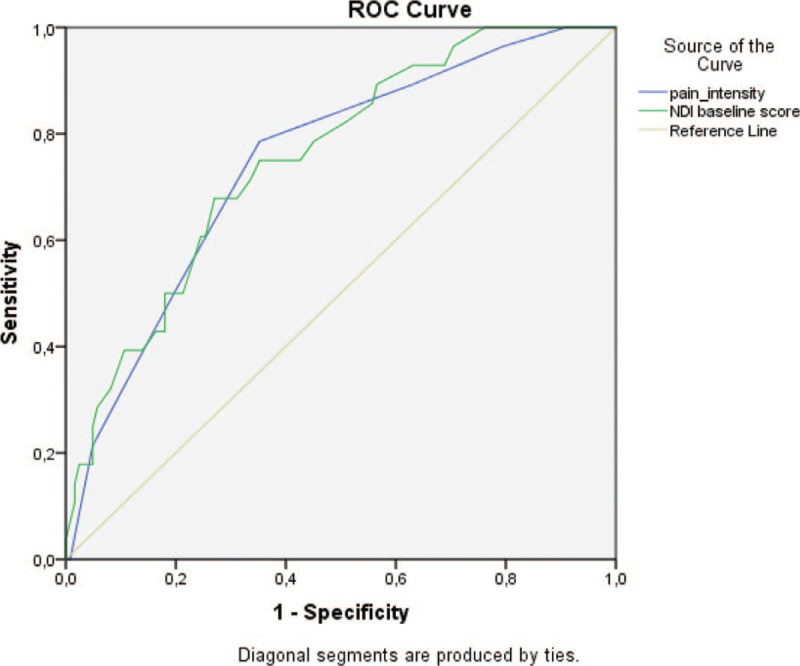
Discriminative ability (ROC) of the numerical rating scale (NRS) for neck pain and the NDI to distinguish between subgroups with cervical radiculopathy and neck pain only (n = 150). NDI indicates Neck Disability Index; ROC, receiver-operating characteristics.
Finally, ANOVA analyses showed that both NRS and NDI could discriminate between low, moderate and high severity of VAS health status (Table 5).
TABLE 5.
Mean (95% CI) of the NRS for Neck Pain and the NDI According to Patient-reported Health Status (Visual Analogue Scale [0–100]), Graded as Low (<25 Percentile), Moderate (50–75 Percentile), And high (>75 Percentile) Severity
| N | Mean | 95% CI | |
| NRS neck pain | |||
| High severity | 49 | 6.1 | 5.7–6.5 |
| Moderate severity | 53 | 4.9 | 4.5–5.3 |
| Low severity | 48 | 4.5 | 4.0–5.5 |
| NDI score | |||
| High severity | 49 | 53.2 | 47.3–59.1 |
| Moderate severity | 53 | 42.0 | 36.7–47.3 |
| Low severity | 48 | 27.8 | 23.8–31.7 |
CI indicates confidence interval; NDI, Neck Disability Index; NRS, Numerical Rating Scale.
DISCUSSION
In this study we have translated and cross-culturally adapted two core PROMs into Nepali for use among patients with neck pain. The Nepali versions of the NRS and NDI were feasible, had acceptable reliability and measurement error, as well as discriminative validity. Less than 75% of hypotheses about the construct validity of the NRS and the NDI were confirmed. This can indicate that the construct validity of the Nepalese questionnaires is lower as compared to other versions.29
To maintain the validity of an instrument across different countries and cultures, the items must not only be well translated linguistically, but also adapted culturally.4,8 In this study, a modification in the translation was performed for cultural reasons. Since few people in Nepal have their own car, we changed item eight in the NDI from “Driving car” to “Travel by vehicle.” Similar problems with the content validity of that item has been described by other authors.14,15,17,22,24 We made this cultural adaption because transportation is a major issue of concern in daily living for most people in Nepal. An alternative approach could be to follow the lead suggested by Costa and Marshman in 2015, that is, sub-fixing the travelling/driving question by “if applicable.” They found that this strategy used on the item eight regarding sex life in the in the standard Oswestry Disability Index (ODI), did not lead to any reduction in ODI participation.30
The feasibility of the final versions of the NDI and NRS of the NDI and NRS was acceptable, but in the reading and concentration items (4 and 6), most probably due to the high proportion of illiteracy, and many patients (45%) needed assistance to complete the questionnaires. Since no patients had more than two missing item values the final NDI version, a complete case analysis could be achieved by imputation.7,30,31
The NDI has been translated into many languages and its internal psychometric properties have been established in many cultural groups with neck pain.11–24 Furthermore, it has been used in >50 surgical clinical trials, trials of injection therapies, and randomized controlled trials of numerous conservative therapies.10,31,32 The psychometric properties of the NDI in the present study are generally in line with most previous studies.8–24 Internal consistency was acceptable (0.70), but lower than in other reports,9 reporting a Cronbach alpha between 0.7414 and 0.92.17 Previous test–retest NDI ICC estimates range from 0.8518 to 0.9822, compared to 0.97 in the present study. We used a short test–retest time interval (2–3 days). This is in accordance with current recommendations (0–3 days).8 However, our results might still be vulnerable for recall bias. We estimated a relatively high SDC (9.3 points),8 but lower than what was found in a Thai neck pain population (16.1 points)18 and closer to what Cleland et al33 reported from a population with cervical radiculopathy (10.2 points).
In contrast to some previous studies both the NRS and NDI we found no ceiling effects. They discriminated well between patients with radiculopathy and neck pain only.
Strengths and Limitations
There are several limitations to this study. Some problems with the psychometric properties of the NDI, especially feasibility, were directly related to socioeconomic factors, typical for low-income countries: Due to the high proportion of illiteracy many patients had to be interviewed. Even though the research assistant was instructed to ask questions in a standardized way without discussing the response alternatives, the interview setting may have influenced the answers. However, a recent meta-analysis showed that administrating questionnaires by self-completion or assisted completion produced equivalent scores.34 We did not assess responsiveness to change (longitudinal discriminative validity). The responsiveness of NDI and NRS will be tested in subsequent studies on patients treated for neck disorders.
The main strength of this study is that we included patients with both radiculopathy and neck pain, which has been warranted.8 The study design and methods were also in accordance with international recommendations for assessing measurement properties.26,29
CONCLUSION
The Nepali version of pain intensity NRS and NDI can be recommended as reliable and valid measures of disability due to neck pain and cervical radiculopathy. Their responsiveness to change remains to be assessed in future studies.
Key Points
No validated Nepali version of the NDI and the NRS for neck pain exists.
We translated, cross-culturally adapted and tested these two patient-reported outcome measures in a Nepalese population with neck pain and cervical radiculopathy. A cross-sectional study with a test–retest design was performed.
The Nepalese versions of the pain intensity NRS and NDI can be recommended as reliable and valid measures to assess pain and disability in neck pain patients.
Supplementary Material
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
No funds were received in support of this work.
No relevant financial activities outside the submitted work.
Supplemental digital content is available for this article.
References
- 1.Vos T, Allen C, Arora M, et al. Global Burden of Disease, Injury Incidence, Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388:1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoy DG, Smith E, Cross M, et al. Reflecting on the global burden of musculoskeletal conditions: lessons learnt from the global burden of disease 2010 study and the next steps forward. Ann Rheum Dis 2015; 74:4–7. [DOI] [PubMed] [Google Scholar]
- 3.Mahto P, Bhupal Gautam B. Prevalence of work-related musculoskeletal disorders in agricultural farmers of Bhaktapur District, Nepal. Int J Occup Saf Health 2018; 8:3–7. [Google Scholar]
- 4.Beaton DE, Bombardier C, Guillemin F, et al. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 2000; 25:3186–3191. [DOI] [PubMed] [Google Scholar]
- 5.Riddle DL, Stratford PW. Use of generic versus region-specific functional status measures on patients with cervical spine disorders. Phys Ther 1998; 78:951–963. [DOI] [PubMed] [Google Scholar]
- 6.Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther 1991; 14:409–415. [PubMed] [Google Scholar]
- 7.Vernon HT. The neck disability index: state of the art. 1991–2008. J Manipulative Physiol Ther 2008; 31:491–502. [DOI] [PubMed] [Google Scholar]
- 8.MacDermid J, Walton DM, Avery S, et al. Measurement properties of the neck disability index: a systematic review. J Orthop Sports Phys Ther 2009; 39:400–417. [DOI] [PubMed] [Google Scholar]
- 9.Pellicciari L, Bonetti F, Di Foggia D, et al. Patient-reported outcome measures for non-specific neck pain validated in the Italian-language: a systematic review. Arch Physiother 2016; 6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schellingerhout JM, Verhagen AP, Heymans MW, et al. Measurement properties of disease-specific questionnaires in patients with neck pain: a systematic review. Qual Life Res 2012; 21:659–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vos CJ, Verhagen AP, Koes BW. Reliability and responsiveness of the Dutch version of the Neck Disability Index in patients with acute neck pain in general practice. Eur Spine J 2006; 15:1729–1736. [DOI] [PubMed] [Google Scholar]
- 12.Wu S, Ma C, Mai M, et al. Translation and Validation Study of Chinese Versions of the Neck Disability Index and the Neck Pain and Disability Scale. Spine (Phila Pa 1976) 2010; 35:1575–1579. [DOI] [PubMed] [Google Scholar]
- 13.En MC, Clair DA, Edmondston JS. Validity of the Neck Disability Index and Neck Pain and Disability Scale for measuring disability associated with chronic, non-traumatic neck pain. Man Ther 2009; 14:433–438. [DOI] [PubMed] [Google Scholar]
- 14.Cook C, Richardson JK, Braga L, et al. Cross-cultural adaptation and validation of the Brazilian and Portuguese version of the Neck Disability Index and the neck pain and disability scale. Spine (Phila Pa 1976) 2006; 31:1621–1627. [DOI] [PubMed] [Google Scholar]
- 15.Salo P, Ylinen J, Kautiainen H, et al. Reliability and Validity of the Finnish Version of the Neck Disability Index and the Modified Neck Pain and Disability Scale. Spine (Phila Pa 1976) 2010; 35:552–556. [DOI] [PubMed] [Google Scholar]
- 16.Mousavi SJ, Parnianpour M, Montazeri A, et al. Translation and validation study of the Iranian versions of the Neck Disability Index and the Neck Pain and Disability Scale. Spine (Phila Pa 1976) 2007; 32:E825–E831. [DOI] [PubMed] [Google Scholar]
- 17.Lee H, Nicholson LL, Adams RD, et al. Development and psychometric testing of Korean language versions of 4 neck pain and disability questionnaire. Spine (Phila Pa 1976) 2006; 31:1841–1845. [DOI] [PubMed] [Google Scholar]
- 18.Uthaikhup S, Paungmali A, Pirunsan U. Validation of Thai versions of the Neck Disability Index and Neck Pain and Disability Scale in patients with neck pain. Spine (Phila Pa 1976) 2011; 36:E1415–E1421. [DOI] [PubMed] [Google Scholar]
- 19.Trouli MN, Vernon HT, Kakavelakis KN, et al. Translation of the Neck Disability Index and validation of the Greek version in a sample of neck pain patients. BMC Musculoskelet Disord 2008; 9:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aslan E, Karaduman A, Yakut Y, et al. The cultural adaptation, reliability and validity of neck disability index in patients with neck pain: a Turkish version study. Spine (Phila Pa 1976) 2008; 33:362–365. [DOI] [PubMed] [Google Scholar]
- 21.Monticone M, Baiardi P, Nido N, et al. Development of the Italian version of the Neck Pain and Disability Scale, NPDS-I: cross-cultural adaptation, reliability, and validity. Spine (Phila Pa 1976) 2008; 33:429–434. [DOI] [PubMed] [Google Scholar]
- 22.Kovacs FM, Bagó J, Royuela A, et al. Psychometric characteristics of the Spanish version of instruments to measure neck pain disability. BMC Musculoskelet Disord 2008; 9:42–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jovicic MD, Konstantinovic LM, Grgurevic AD, et al. Validation of the Neck Disability Index in Serbian patients with cervical radiculopathy. J Manipulative Physiol Ther 2018; 41:496–502. [DOI] [PubMed] [Google Scholar]
- 24.Wlodyka-Demaille S, Poiraudeau S, Catanzariti JF, et al. French translation and validation of 3 functional disability scales for neck pain. Arch Phys Med Rehabil 2002; 83:376–382. [DOI] [PubMed] [Google Scholar]
- 25.Path R. Population monograph of Nepal, vol. II (Social demography). [Central Bureau of Statistics, Nepal web site] 2014. Available at: https://nepal.unfpa.org/sites/default/files/pubpdf/Popu lationMonographVolume2.pdf. Accessed October 15, 2019. [Google Scholar]
- 26.Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60:34–42. [DOI] [PubMed] [Google Scholar]
- 27.EuroQoL Group. EuroQoL—a new facility for the measurement of health-related quality of life. Health Policy 1990; 16:199–208. [DOI] [PubMed] [Google Scholar]
- 28.Bhattarai P, Niessen L, Shrestha N, et al. Health related quality of life of adults in Nepal with respiratory symptoms using WHOQOL and EQ-5D. Thesis Samir Kumar, K C. [University of Groningen] 2009: [S.n.]. 146 p. [Google Scholar]
- 29.Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res 2010; 19:539–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Costa M, Marshman LA. Sex life and the Oswestry Disability Index. Spine J 2015; 15:1225–1232. [DOI] [PubMed] [Google Scholar]
- 31.Vernon H. The Neck Disability Index: state-of-the-art. J Manipulative Physiol Ther 2008; 31:491–502. [DOI] [PubMed] [Google Scholar]
- 32.Pietrobon R, Coeytaux RR, Carey TS, et al. Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine (Phila Pa 1976) 2002; 27:515–522. [DOI] [PubMed] [Google Scholar]
- 33.Cleland JA, Fritz JM, Whitman JM, et al. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976) 2006; 31:598–602. [DOI] [PubMed] [Google Scholar]
- 34.Rutherford C, Costa D, Mercieca-Bebber R, et al. Mode of administration does not cause bias in patient-reported outcome results: a meta-analysis. Qual Life Res 2016; 25:559–574. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


