Abstract
Background
COVID-19 pandemic has necessitated mandatory e-learning in medical and nursing education. How far are developing countries like India (with wide socioeconomic and cultural diversity) geared up for this challenge remains unexplored. At this critical juncture, we aim to evaluate if online teaching methods are as feasible, acceptable, and effective as in-class teaching for medical/nursing students.
Objectives
The questionnaire captured: (1) practicability/feasibility of online classes, (2) health issues from online classes, (3) current methods for e-teaching, and (4) student attitudes and preferences.
Design
Cross-sectional survey.
Settings
Population-based study in India.
Participants
Nursing and medical undergraduate students (I-IV year).
Methodology
The online questionnaire was distributed to 200 medical and nursing colleges across India. Categorical variables were analyzed using chi-square tests. Binary logistic regression was done to analyze factors predicting health issues in students. p < 0.05 was considered significant.
Results
Overall, 1541 medical and 684 nursing students completed the survey from 156 cities. The availability of laptop (p < 0.0001), Wi-Fi (p < 0.0001), dedicated room (p < 0.0001), and computer proficiency was more in students of affluent families and those from cities (p < 0.0001). Class duration >4 h/day (p < 0.0001), each class >40 min (p < 0.009) and pre-existing health issues (p < 0.0001) predicted the occurrence headache, eyestrain, anxiety, neck/back pain, and sleep disturbance. Power-point presentation was the most widely (80%) used method of teaching. Only 30% got adequate time to interact with teachers. Only 20.4% felt e-learning can replace conventional teaching. Students preferred: 3–6 classes/day, each class <40 min, 10–20 min break between classes and interactive sessions.
Conclusion
There is a need to improve information and communication infrastructure to enhance feasibility of e-learning for nursing/medical students in India. There should be guidelines (number of classes/day, length of each class, break between classes, curriculum, etc) to improve the retention capacity in students and reduce health issues. Continuous feedback from teachers and students will be required to make e-learning effective.
Keywords: COVID-19 pandemic, Medical student, Nursing student, Online classes, Survey
1. Introduction
Coronavirus disease 2019 (COVID-19) pandemic has affected the education system across the world and brought about profound organizational changes in the traditional methods of teaching (Rose, 2020). By mid-April, there was a global shut down of schools affecting nearly 1.6 billion students in 191 countries (UNESCO, 2020). This was done to help flatten the curve of virus transmission. Many countries have resorted to online classes and assessments for their medical/nursing students. The lectures have been switched to online mode and clinical rotations canceled or modified. Exams have been temporarily suspended or are being conducted online. Medical students are graduating early in some countries to reinforce the medical teams at COVID hospitals (Lapolla and Mingoli, 2020).
India went into a nation-wide lockdown to curtail the spread of COVID-19 on 24th March 2020. The University Grants Commission (UGC) introduced mandatory e-learning for all medical and nursing students across the country as an alternative (Gazette of India, 2020). The traditional face to face, the teacher-centered educational model changed to a new face to screen, student-centered model.
Information and communication technology (ICT) has revolutionized e-learning. E-learning has the advantage of lectures being available anywhere and anytime and available for revision any number of times. However, the disadvantages include limited student feedback, need for self-motivation, dependency on internet availability and expensive digital gadgets, difficulty in psychomotor and affective skill transfer, and associated health hazards of prolonged gadget use (Cook, 2007). It has been estimated that in the rural areas of India only 14.9% of the people have access to the internet compared to 42% in urban areas (Ministry of statistics and programme implementation, 2017–2018).
The shift to online teaching methods has become a necessity rather than an option. But how far are countries geared up for this challenge is something that has not been audited. With a second wave of the pandemic striking hard and with the reinstatement of lockdowns, particularly in economically constrained nations, where there is a dearth for easy access to technology and e-learning opportunities, a newer challenge emerges i.e., a need to provide continued education and training to nursing and medical students. Some countries are wondering if e-learning will become a norm following the pandemic. At this critical juncture, it is important to evaluate if these current online teaching methods are feasible, acceptable, and as effective as in-class teaching.
We aim to provide preliminary data to the stakeholders regarding the feasibility and acceptability of e-learning. Although this study has been done in India, we assume a similar situation prevails in most countries of the world. E-learning can be a powerful teaching method provided we understand the obstacles in the path of its implementation and utilization and work towards solving them. In this study we have aimed to explore the following aspects: (1) the practicability of online education (2) the health issues arising from online classes, and (3) the current methods used for e-teaching, (4) attitudes and preferences of students.
Overall, this study is one of the first of its kind to comprehensively and systematically analyze the factors that favor and influence the acceptability of e-learning methods in nursing and medical education during this pandemic. Also, this study is on students who have received purely online classes for a prolonged duration (a situation not witnessed by the world before). Also, there have been no studies done in the past on how feasible are e-learning methods and what exactly the students expect from e-teaching.
2. Methods
This was a nationwide, self-administered, anonymous, questionnaire-based cross-sectional survey conducted between July and August 2020. Institutional ethics committee approval was obtained to conduct this research (IEC number: IEC/AIIMS/MG/2020/24).
2.1. Sample selection
A systematic random sample was generated from the list of colleges taken from the official website of the Medical Council of India and the Indian Nursing Council.
2.2. Design of the questionnaire (supplemental file 1)
The questionnaire was sent to ten subject experts for face validation. It was then pilot-tested among 100 students (both medical and nursing) and refined further in terms of flow, comprehension, and content using their feedback.
The questionnaire was organized into six sections with questions to capture the: (1) demographic details (2) feasibility of online classes (3) agenda and methods of online teaching (4) health issues (5) students' attitudes towards e-learning (6) student preferences for the duration of online classes and methods of teaching. The survey had dichotomous and multiple-choice questions. The last question was an open-ended question to allow students to mention any issue that was not covered in the questionnaire. The survey link was sent as e-mails to the principals/deans of medical/nursing colleges to be filled up by the students.
2.3. Statistical analysis
All responses were grouped into categorical variables (nominal or ordinal). The responses were parsed and the data was analyzed. Chi-square tests were used to compare categorical variables. Conditional formatting was used to sort layered responses. We used binary logistic regression to predict the association between (1) headache and eye strain/anxiety/sleep disturbance/gender/duration of online classes in a day/duration of each class and duration of breaks between the classes; (2) sleep disturbance and eye strain/headache/neck pain/back pain/anxiety/gender/duration of online classes in a day/duration of each class and duration of breaks between the classes; (3) neck pain and previous cervical spondylosis/gender/duration of online classes per day/duration of each class and duration of breaks between the classes; (4) back pain and previous chronic back pain/gender/duration of online classes per day/duration of each class and duration of breaks between classes; (5) eyestrain and pre-existing eye problems/gender/duration of online class per day/duration of each class and duration of breaks between the classes.
Two-tailed P value <0.05 was considered significant. All analysis was performed using IBM-SPSS version 23.
3. Results
3.1. Demography
The demographic details of the students who participated in this study are as shown in Table 1 .
Table 1.
Demographic details of the students.
| Medical students N (%) |
Nursing students N (%) |
Overall N (%) |
P value | ||
|---|---|---|---|---|---|
| Gender | Male | 674 (43.7) | 173 (25.3) | 847 (38.1) | <0.0001 |
| Female | 867 (56.3) | 511 (74.7) | 1378 (61.9) | ||
| Institute | Central institutions | 297 (19.3) | 50 (7.3) | 347 (15.6) | <0.0001 |
| State Government medical colleges | 415 (26.9) | 37 (5.4) | 452 (20.3) | ||
| Private medical colleges | 701 (45.5) | 455 (66.5) | 118 (52.9) | ||
| Government aided medical colleges | 118 (7.7) | 62 (9.1) | 180 (8.1) | ||
| Trust run medical college | 10 (0.6) | 80 (11.7) | 90 (4) | ||
| Residence | Village | 330 (21.4) | 408 (59.6) | 738 (33.2) | <0.0001 |
| Town | 514 (33.4) | 58 (8.5) | 572 (25.7) | ||
| City | 663 (43) | 197 (28.8) | 860 (38.7) | ||
| Hostel | 34 (2.2) | 21 (3.1) | 55 (2.5) | ||
| Primary Income | <2.5 lakh | 486 (31.5) | 488 (71.3) | 974 (43.8) | <0.0001 |
| 2.5–5 lakh | 348 (22.6) | 123 (18) | 471 (21.2) | ||
| 5–10 lakh | 372 (24.1) | 48 (7) | 420 (18.9) | ||
| >10 lakh | 335 (21.7) | 25 (3.7) | 360 (16.3) | ||
| Online platforms | Zoom | 491 (31.9) | 359 (52.5) | 850 (38.2) | <0.0001 |
| Google meet | 390 (25.3) | 85 (12.4) | 475 (27.3) | ||
| Cisco Webex meetings | 90 (5.8) | 197 (28.8) | 287 (12.9) | ||
| Microsoft teams | 264 (17.1) | 10 (1.5) | 274 (12.3) | ||
| GoToMeeting | 121 (7.9) | 1 (0.1) | 122 (5.5) | ||
| Others | 185 (12) | 32 (4.7) | 217 (9.8) | ||
| Gadgets for attending online classes | Own personal computer/laptop | 338 (21.9) | 66 (9.6) | 404 (18.2) | <0.0001 |
| Borrow gadget | 135 (8.8) | 84 (12.3) | 219 (9.8) | ||
| Phone/tablet | 1068 (69.3) | 534 (78.1) | 1602 (72) | ||
| Source of internet | Mobile data | 1133 (73.9) | 644 (94.3) | 1777 (80.2) | |
| Wi-Fi router | 401 (26.1) | 39 (5.7) | 440 (19.8) | ||
| Dedicated room for attending online classes | Yes | 804 (52.2) | 360 (52.6) | 184 (52.3) | 0.818 |
| No | 719 (46.7) | 314 (45.9) | 1033 (46.4) | ||
| Proficiency in computers | No training | 140 (9.1) | 164 (24) | 304 (13.7) | <0.0001 |
| Below average | 225 (14.6) | 129 (18.9) | 354 (15.9) | ||
| Average | 771 (50) | 341 (49.9) | 112 (50) | ||
| Above average | 302 (19.6) | 32 (4.7) | 334 (15) | ||
| Excellent | 103 (6.7) | 18 (2.6) | 121 (5.4) | ||
| Proficiency with internet | No training | 68 (4.4) | 90 (13.2) | 158 (71) | <0.0001 |
| Below average | 190 (12.3) | 135 (19.7) | 925 (19.6) | ||
| Average | 817 (53) | 392 (57.3) | 1209 (54.3) | ||
| Above average | 340 (22.1) | 37 (5.4) | 377 (16.9) | ||
| Excellent | 126 (8.2) | 30 (4.4) | 156 (7.0) | ||
We received a total of 2462 responses. But, 174 students had no online classes and 63 were not willing to participate in the study. A total of 2225 students (1541 medical and 684 nursing students) completed the survey from 156 cities.
3.2. Feasibility/practicability of online classes
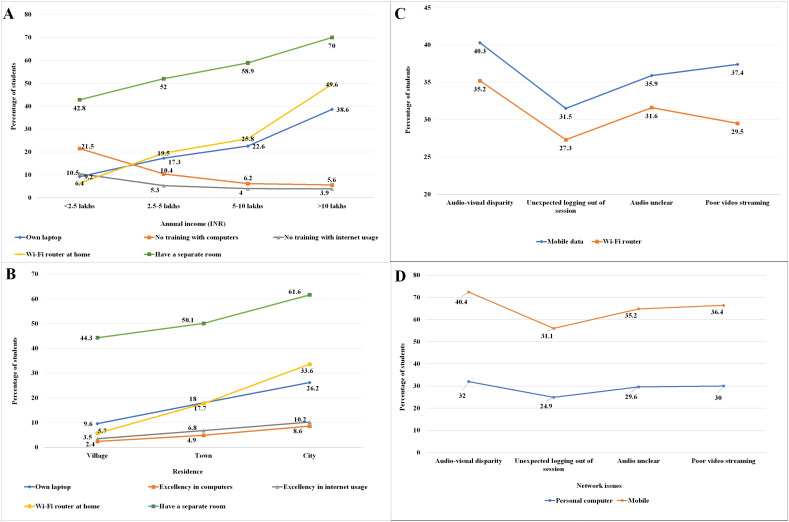
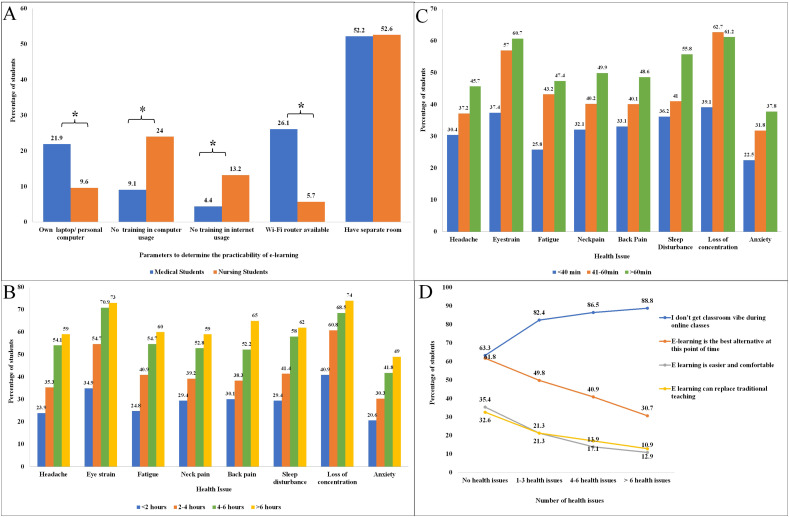
The internet facilities, device logistics, proficiency of students in computer and internet usage, and availability of dedicated space at home (where there are no environmental distractions) to attend online classes determine the feasibility/practicability of e-learning. All these variables were dependent on the annual income of the family and the geographical location of the students (Fig. 1a, b). There were also significant differences between nursing and medical students concerning these parameters (Fig. 2a).
Fig. 1.
(a–d): a) A greater proportion of students from the higher income groups had access to a Wi-Fi router and dedicated room at home to attend online classes. Also, proficiency in the usage of the internet and computers was better in the higher income groups (p < 0.0001). b) A similar pattern of responses was seen with students from cities having better availability of Wi-Fi router and dedicated room at home and better proficiency in computer and internet usage compared to those in towns and villages. c) Network issues were more frequently encountered when students used mobile data rather than Wi-Fi router for internet connection (χ2s > 3.86, df = 1, p's < 0.049) d) Network issues were less when the students used personal computer rather than mobile phones during the classes (χ2s > 9.23, df = 3, p's < 0.026).
Fig. 2.
(a–d): a) Medical students had better access to a personal computer/Wi-Fi router at home and proficiency in computer and internet usage compared to nursing students (*p < 0.001). b, c) The proportion of students reporting different health issues increased with the increase in the total duration of classes per day (p < 0.0001) and duration of each class (p < 0.0001). d) As the number of health issues that the student suffered from increased, the lesser was their tendency to favor e-learning as a modality of teaching.
3.3. Internet connectivity
Seamless internet connectivity is of paramount importance to attend classes without interruption. The majority of the students (80%) used mobile data to attend online classes and only 20% had access to Wi-Fi routers at home. Students from affluent families (χ2 = 319.94, df = 3, p < 0.0001), and those staying in cities (χ2 = 196.79, df = 3, p < 0.0001) had better access to Wi-Fi router network compared to the lower-income families and those staying in villages and towns (Fig. 1a, b).
Network-related issues were frequently reported by a significant percentage of students: audio-visual disparity (39.3%), unexpected logging out during the classes (30.6%), audio disturbances (35%), and videos not streaming properly (35.7%). These problems were less encountered among students who had their own computer (χ2s > 9.23, df = 3, p's < 0.026) and had access to Wi-Fi routers at home (χ2s > 3.86, df = 1, p's < 0.049) compared to those who used mobile phones and mobile data (Fig. 1c, d). Those students who had a separate room had fewer audio problems compared to those who did not have (25% vs 45.2%; χ2 = 93.47, df = 3, p < 0.0001). However, there was no significant difference between villages, towns, or cities concerning these network-related problems (p = 0.09). Also, these problems did not seem to depend on the proficiency of the internet (p's > 0.155)/computer (p's > 0.116) usage.
3.4. Device logistics
Only 18.2% of students had their own desktop/laptop, 9.8% of students borrowed gadgets from friends/family and the rest used their phones/tablets for attending online classes. The proportion of students who owned a laptop was more among the higher-income families (χ2 = 173.47, df = 6, p < 0.0001) and those staying in cities (χ2 = 87.74, df = 6, P < 0.0001) (Fig. 1a, b).
3.5. Proficiency of internet and computer usage
Proficiency in computer usage was better among the higher income groups (χ2 = 248.07, df = 12, p < 0.0001) and those in cities (χ2 = 208.74, df = 12, p < 0.0001) (Fig. 1a, b).
Proficiency of internet usage was better among the higher income groups (χ2 = 243.79, df = 12, p < 0.0001) and those in cities (χ2 = 168.73, df = 12, p < 0.0001) (Fig. 1a, b).
3.6. Availability of a dedicated space to attend online classes
Only half the students (52%) had the provision for separate rooms in their houses to attend online classes. Again, this was seen more often in the higher income groups (χ2 = 92.17, df = 6, p < 0.0001) and those in cities (χ2 = 798.98, df = 6, p < 0.0001) (Fig. 1a, b).
3.7. Health issues arising from online classes
Loss of concentration (58.1%) was the most common problem followed by eye strain (54%), sleep disturbance (42.8%), neck pain (40.5%), back pain (40.4%), and headache (40%) (Supplementary file 2). Medical students reported significantly more health issues compared to nursing students owing to increased screen time (χ2 = 22.49, df = 1, p < 0.0001) (Supplementary file 2).
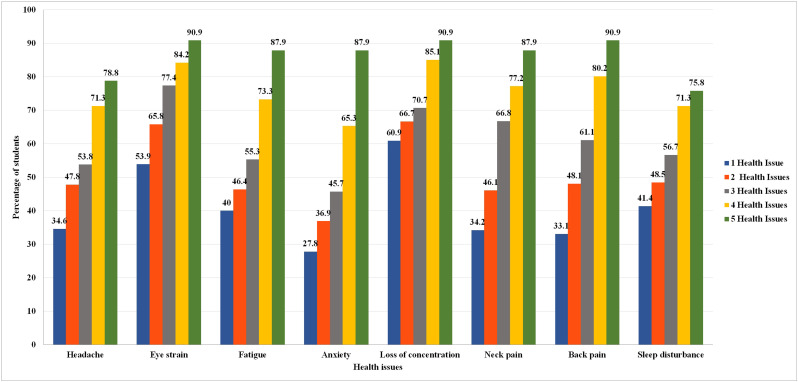
The results of binary logistic regression to analyze the predictors for headache, eye strain, sleep disturbance, neck pain, and back pain are as shown in Table 2. Longer duration of classes in a day and longer duration of each class resulted in a greater proportion of students to develop headache, eyestrain, fatigue, anxiety, loss of concentration, neck and back pain, and sleep disturbances (Fig. 2b, c). As the number of pre-existing health issues increased from 1 to 5 the proportion of students who experienced health issues also increased (Supplemental file 3).
Table 2.
Binary logistic regression model for the health issues and their significant predictors.
| Health issue | Predictors | Wald's coefficient | df | P value |
|---|---|---|---|---|
| Headache (Predictive accuracy 79.8%) |
Eye strain | 279.02 | 1 | <0.0001 |
| Anxiety | 80.84 | 1 | <0.0001 | |
| Sleep disturbance | 32.88 | 1 | <0.0001 | |
| Past history of headache | 47.93 | 1 | <0.0001 | |
| Duration of class >4 h per day | 17.59 | 1 | <0.0001 | |
| Eye strain (Predictive accuracy 64.3%) |
Pre-existing eye diseases | 89.68 | 1 | <0.0001 |
| Duration of class >4 h per day | 58.51 | 1 | <0.0001 | |
| Each class >40 min | 25.54 | 1 | <0.0001 | |
| No breaks between classes | 5.2 | 1 | 0.022 | |
| Sleep disturbance (Predictive accuracy 69.5%) |
Eye strain | 17.91 | 1 | <0.0001 |
| Anxiety | 13.53 | 1 | <0.0001 | |
| Back pain | 9.04 | 1 | 0.003 | |
| Neck pain | 5.14 | 1 | 0.023 | |
| Headache | 23.74 | 1 | <0.0001 | |
| Duration of class >4 h per day | 23.33 | 1 | <0.0001 | |
| Neck pain (Predictive accuracy 68.3%) |
Previous neck disease | 190.67 | 1 | <0.0001 |
| Duration of class >4 h per day | 34.14 | 1 | <0.0001 | |
| Each class >40 min | 6.83 | 1 | 0.009 | |
| Back pain (Predictive accuracy 66.6%) |
Duration of class >4 h per day | 47.04 | 1 | <0.0001 |
| Each class >40 min | 7.47 | 1 | 0.006 | |
| Previous back problems | 143.7 | 1 | <0.0001 |
Supplemental file 3.
Figure showing that as the number of pre-existing health issues increased from 1 to 5 the proportion of students who experienced health issues also increased.
Almost a third of the students who had headaches, neck pain, and back pain took analgesics (P < 0.0001) or home remedies. Remedies like ice packs and artificial tear drops were used by 37.5% of the students with eye strain (P < 0.0001) and 55.9% decreased the screen-time for other activities (P < 0.0001) to compensate for the increased screen time due to online classes. One-third of the students who had anxiety and loss of concentration practiced meditation/yoga (p = 0.002). Overall, 257 (11.9%) visited hospitals for their health issues due to online classes.
3.8. Methods of online teaching
3.8.1. Distribution of class time and agenda
Nearly all the students had online theory classes, 51% had online practical classes and 70.8% had online internal assessments.
The total duration of classes in a day (χ2 = 231.59, df = 3 p < 0.001) and duration of each class (χ2 = 395.51, df = 2 P < 0.001) was significantly higher in medical students compared to nursing students. Breaks between classes were infrequent in both the groups with almost 40% of the students reporting that they had no breaks between classes. Two-thirds of the students did not have adequate time to interact with teachers during online classes (Table 3 ).
Table 3.
Comparison of prevailing teaching methods in pandemic and preferred teaching methods by students.
| Parameter | Time and methods | Prevailing teaching schedule and methods |
Preferred teaching schedule and methods by students |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Medical N (%) | Nursing N (%) | Overall N (%) |
P value | Medical N (%) | Nursing N (%) | Overall N (%) |
P value | ||
| Duration of classes in a day | <2 h | 241 (15.6%) | 307 (44.9%) | 548 (24.6%) | P < 0.0001 | 370 (24.0%) | 276 (40.4%) | 646 (29.0%) | P < 0.0001 |
| 2–4 h | 831 (53.9%) | 283 (41.4%) | 1114 (50.1%) | P < 0.0001 | 1030 (66.8%) | 325 (47.5%) | 1355 (60.9%) | P < 0.0001 | |
| 4–6 h | 385 (25.0%) | 78 (11.4%) | 463 (20.8%) | P < 0.0001 | 131 (8.5%) | 80 (11.7%) | 211 (9.5%) | P < 0.0001 | |
| >6 h | 84 (5.5%) | 16 (2.3%) | 100 (4.5%) | P < 0.0001 | 10 (0.6%) | 3 (0.4%) | 13 (0.6%) | P < 0.0001 | |
| Duration of each class | <40 min | 126 (8.2%) | 288 (42.1%) | 414 (18.6%) | P < 0.0001 | 1083 (70.3%) | 428 (62.6%) | 1511 (67.9%) | P < 0.0001 |
| 41–60 min | 1148 (74.5%) | 259 (37.9%) | 1407 (63.2%) | P < 0.0001 | 400 (26.0%) | 182 (26.6%) | 582 (26.2%) | P < 0.0001 | |
| >60 min | 267 (17.3%) | 137 (20.0%) | 404 (18.2%) | P < 0.0001 | 58 (3.8%) | 74 (10.8%) | 132 (5.9%) | P < 0.0001 | |
| Breaks between classes | No Breaks | 585 (38.0%) | 264 (38.6%) | 849 (38.2%) | P < 0.0001 | 91 (5.9%) | 130 (19.0%) | 221 (9.9%) | P < 0.0001 |
| <10 mins | 356 (23.1%) | 241 (35.2%) | 597 (26.8%) | P < 0.0001 | 459 (29.8%) | 289 (42.3%) | 748 (33.6%) | P < 0.0001 | |
| 11–20 min | 170 (11.0%) | 74 (10.8%) | 244 (11.0%) | P < 0.0001 | 580 (37.6%) | 157 (23.0%) | 737 (33.1%) | P < 0.0001 | |
| 21–30 min | 153 (9.9%) | 45 (6.6%) | 198 (8.9%) | P < 0.0001 | 244 (15.8%) | 64 (9.4%) | 308 (13.8%) | P < 0.0001 | |
| >30 mins | 277 (18.0%) | 60 (8.8%) | 337 (15.1%) | P < 0.0001 | 167 (10.8%) | 44 (6.4%) | 211 (9.5%) | P < 0.0001 | |
| Teaching methods | Didactic Lecture | 366 (23.8%) | 136 (19.9%) | 502 (22.6%) | P = 0.044 | 222 (14.4%) | 302 (44.2%) | 524 (23.6%) | P < 0.0001 |
| White board with diagram/figures | 393 (25.5%) | 140 (20.5%) | 533 (24%) | P = 0.010 | 1239 (80.4%) | 449 (65.6%) | 1688 (75.9%) | P < 0.0001 | |
| Power-point presentation | 1427 (92.6%) | 344 (50.3%) | 1771 (79.6%) | P ≤ 0.0001 | 1233 (80.0%) | 538 (78.7%) | 1771 (79.6%) | P = 0.463 | |
| Case-based learning | 940 (61.0%) | 232 (33.9%) | 1172 (52.7%) | P ≤ 0.0001 | 1448 (94.0%) | 453 (66.2%) | 1901 (85.4%) | P < 0.0001 | |
| Video-based teaching | 748 (48.5%) | 294 (43.0%) | 1042 (46.8%) | P = 0.015 | 1389 (90.1%) | 573 (83.8%) | 1962 (88.2%) | P < 0.0001 | |
| Interactive session | 668 (43.3%) | 262 (38.3%) | 930 (41.8%) | P = 0.026 | 1289 (83.6%) | 522 (76.3%) | 1811 (81.4%) | P < 0.0001 | |
| Recorded lectures used in teaching | 533 (34.6%) | 220 (32.2%) | 753 (33.8%) | P = 0.265 | 931 (60.4%) | 450 (65.8%) | 1381 (62.1%) | P = 0.016 | |
| Virtual models | 357 (23.2%) | 188 (27.5%) | 545 (24.5%) | P = 0.029 | 1329 (86.2%) | 482 (70.5%) | 1811 (81.4%) | P < 0.0001 | |
| Quizzes | 598 (38.8%) | 249 (36.4%) | 847 (38.1%) | P = 0.282 | 1239 (80.4%) | 507 (74.1%) | 1746 (78.5%) | P = 0.001 | |
| Methods to enhance learning | Upload presentation in advance | 578 (37.5%) | 208 (30.4%) | 786 (35.3%) | P = 0.001 | 1212 (78.7%) | 521 (76.2%) | 1733 (77.9%) | P = 0.193 |
| Share presentation for future reading | 1012 (65.7%) | 336 (49.1%) | 1348 (60.6%) | P < 0.0001 | 1450 (71.9%) | 568 (83.0%) | 2018 (90.7%) | P < 0.0001 | |
3.8.2. Type of teaching methods employed
PowerPoint presentation was the most commonly used (80%) method [medical (92.6%), nursing students (50.3%), p < 0.0001]. Other methods employed were didactic lectures without any aids (22%), case-based learning (52.7%: medical-61%, nursing 33.9%, p < 0.0001), video-based learning (50%), interactive sessions (41%), recorded lectures (46.8%), quizzes (38.1%), virtual models in classes (24.5%) and online whiteboard teaching with diagrams (24%) (Table 3). Access to PowerPoint presentations/study materials in advance so that students can read up on the subject (flipped classroom methods) was reported by 33% and sharing of the presentation/study material after the class was reported by 40% of the students (Table 3).
3.9. Student attitudes towards e-learning
The attitudes were different between medical and nursing students (Supplemental file 4).
The majority of the students (78.9%) felt that the pandemic has affected their studies (medical students 80%, nursing75%, p < 0.0001). Overall, only 45% of the students felt that e-learning is the best alternative to continue education during the pandemic. Students who had a separate room (χ2 = 77.24, df = 4, p < 0.0001), had access to Wi-Fi internet (χ2 = 12.31, df = 2, p = 0.002), and had a good proficiency in computers (χ2 = 51.2, df = 8, p < 0.0001) and internet usage (χ2 = 44.34, df = 8, p < 0.0001) were more likely to agree to this statement than their counterparts.
Only 20.4% felt that e-learning can replace traditional classroom teaching [medical students (15%) nursing students (30%), p = 0.001]. These students had lesser health issues (χ2 = 85.313, df = 6, p < 0.0001) and less internet related issues (χ2 = 55.53, df = 8 p < 0.0001).
Half of the students disagreed that e-learning was more comfortable than classroom teaching. These students used mobile data for internet (54.2% vs 45.9%, p = 0.003), had no separate rooms(54.2% vs 42.9%, p = 0.003) and had no training in computers (56.3 vs 46.3%, p = 0.004). Similarly, almost half the students (46.9%) agreed to the fact that it was easier to take screenshots and notes during online classes.
As the number of health issues increased, the number of students who agreed to the following facts decreased: e-learning is easier and comfortable, e-learning is the best alternative during this pandemic, and e-learning can replace traditional teaching (Fig. 2d).
3.10. Preference of the students
The students preferred: 3–6 classes/day with duration of each class <40 min, at least 10–20 min break between classes, and interactive/technology-based sessions like panel discussion, quizzes, videos, and virtual models. Almost 78% of the students wanted the presentations or study materials to be uploaded in advance. Nearly all (90.7%) students wanted the presentations used in the class to be shared with them for their future reading. Almost 80% wanted the recorded lectures to be shared with them (Table 3).
4. Discussion
This study shows that students from affluent families and those living in cities had better access to e-learning facilities (internet connectivity, availability of own computer, dedicated room, and training in computer/internet usage). Power-point presentation was the most commonly used method of teaching. Only one-third of the students agreed that they had adequate time to interact with teachers during the classes. Health issues were more common in those students who had to attend classes for >4 h a day, had long classes (>40 min), and had pre-existing health issues. A significant proportion of students had to use home remedies/drugs/visit hospitals to deal with the health issues arising/exacerbated from online classes.
The COVID-19 pandemic has highlighted the digital divide in a developing nation like India. Digital divide refers to the disproportionate growth in digital technology and skills to use this technology among different socio-economic, racial, and geographical groups (Joshi et al., 2020). Over 70% of India's population lives in rural areas. However, only 14.9% have access to the internet in rural areas compared to 42% in urban areas because service providers are reluctant to invest in small towns and villages (Ministry of statistics and programme implementation, 2017–2018). In our study, we found that the availability of Wi-Fi internet connectivity was least in villages. Improving the ICT infrastructure is warranted in the long-run. Meanwhile, the following strategies can be adopted by colleges: (1) development of applications that can be accessed in the offline mode, (2) delivering classes on television/radio channels, and (3) delivering study material and weekly assignments by post/dedicated vans.
The three main domains of learning are cognitive (knowledge, comprehension, and critical thinking), psychomotor (skill development), and affective (emotional and behavioral responses) (Adams, 2015). The application of Bloom's taxonomy in e-learning can help instructors to design their classes effectively. While it is easier to deliver cognitive skills through online classes, delivering affective and psychomotor skills has become a challenge. Some methods that may be employed include the use of instructional videos, direct and indirect self-reporting, case-based learning, interviews, quizzes, small group activities, online simulations, and web-based interactive courses (Martinengo et al., 2019; Vogel and Harendza, 2016). This study shows a general lack in the use of these innovative methods for e-teaching at present. This is because the educational system was not prepared to suddenly shift to an online mode of teaching which became necessary during this pandemic. Also, doctors and nurses are more involved in the care of COVID patients and are having less time to prepare and organize themselves for online classes.
In a study (Singh et al., 2020), 50% of the students only believed that classroom teaching was better. We noted a similar trend in this study 81.1% stating that they did not get classroom vibe with online teaching and only 20% agreeing that e-learning can replace traditional teaching methods. Only 33% of the students agreed that they got adequate time to interact with the teachers. Also, 64% did not get even a 10 min gap between classes. This happens in online classes because time is lost between classes when the instructors and students have to log into a new session, sessions are not planned adequately by the instructors to finish on time, and interruptions in network connectivity can prolong the duration of classes leaving very less time for student-teacher interaction.
The attention span of the students depends on the motivation of the students, time of the day, and learning experience. Working memory processes new concepts during a lecture and integrates with existing knowledge to form long term memory (Schweppe and Rummer, 2014). New information flows-in during each lecture, and without adequate breaks, it becomes difficult for students to assimilate the new information while the previous information is still being processed. This phenomenon of interference makes learning less effective and gives rise to boredom. This can be prevented by: (1) keeping the teaching sessions short (Sheridan et al., 2017) (many institutions have adopted 2–4 h of online classes per day and breaks of 10–15 min between classes) (2) having more-interactive, learner-centered sessions (Mortensen and Nicholson, 2015) (flipped classroom model, group discussions and quizzes), (3) mixing of different methods of teaching (videos, PowerPoint slides, simulations, quiz) in a day (Hsieh et al., 2014) (4) summarizing the salient points of a lecture at the end of each class and allowing time for students to ask questions, and (5) employing micro-learning methods (Shail, 2019).
A significant percentage (37–58%) of the students reported health issues due to prolonged screen time in this study. It has been noted excessive gadget use, improper posture and ergonomics can impact the physical, mental and social well-being of computer users. In this study, 54% of the students reported eye strain, 40% reported some form of musculoskeletal problems, 42.8% reported sleep disturbance and 58.1% reported loss of concentration. Screen time (all gadgets put together) of >4 h a day has shown to increase digital eye strain (manifested as headaches, blurred vision, dry eyes, and pain in the neck and shoulders) (Sheppard and Wolffsohn, 2018). Other habits like not taking adequate breaks during screen viewing and keeping the screen at a distance of less than 36 in. (for computers) and 40 cm (for smartphones) can aggravate eye strain (Ganne et al., 2020; Long et al., 2017). Studies in computer users have shown that nearly 44% of them have some form of musculoskeletal problems (neck pain, low backache, shoulder, or wrist pain)(Borhany et al., 2018). The frequency of occurrence of these problems increases with the duration of computer usage (more than 2–5 h as per different studies) (Borhany et al., 2018; Ellahi et al., 2011). Improper ergonomics in the form of not placing the computer screen directly in front, bad sitting behavior (less frequent postural shifts, slouched or hunched back for extended periods), cold surroundings, pre-existing back problems significantly affect the neck and back pain experienced (Bontrup et al., 2019; Borhany et al., 2018; Rodrigues et al., 2017). Melatonin is a sleep facilitator in humans. Electronic gadgets emit blue light (400–490 nm) from their light-emitting diodes which can cause melatonin suppression. This affects the ability to fall asleep (Shechter et al., 2018). Extensive use of online media can impair cognitive development in youth. Studies have shown that people who engage in frequent and extensive media multi-tasking perform worse in various cognitive tasks, particularly for sustained attention due to their increased susceptibility to distraction. The habitual use of digital devices has been shown to affect the attention span negatively (Firth et al., 2019; Wilmer et al., 2017).
This is the largest survey on e-learning in medical/nursing students and included students from all over India. This survey also captures the perspective of students who are the end-users. However, the following are the limitations: being a questionnaire study it is fraught with the possibility of recall bias and the possibility of students giving desirable answers rather than the true answers. Future studies should be carried to assess the long-term health effects of e-learning and compare the efficacy of e-learning with traditional teaching methods by an objective assessment of student's post-pandemic.
4.1. Implications of the study
We found that availability of facilities like desktops/laptops, uninterrupted internet connectivity, and dedicated space to attend online classes was more among students of high-income families and those in cities. Students without access to these facilities were less likely to agree that e-learning is a good alternative to traditional classroom teaching. Hence, to make e-learning more acceptable to students, governments/academic institutions should focus on providing e-learning infrastructure such as desktops, laptops, and Wi-Fi routers at subsidized prices to the students, uninterrupted high-speed internet to students in villages and towns; improving technology awareness and fluency among teachers and students; developing easy-to-use applications on mobile phones, for both online and offline usage.
Another major finding in this study was that the duration of classes was too long and breaks between classes were inadequate. Students affirmed inadequate student-teacher interactions, reducing the acceptability of e-learning methods. It is crucial that institutions set aside guidelines for online teaching such as the number of classes per day, length of each class, break between classes, etc. Studies have shown that longer duration exposure to digital gadgets is associated with various ailments such as digital eye strain, chronic back pain, migraines, and worsening refractory errors. Hence time-to-effort optimization and inclusion of practices such as adopting creative and interactive methods of teaching (debates, quizzes, videos, case-based learning, and projects) will make e-learning effective and safe.
While COVID-19 pandemic has necessitated massive lifestyle changes including adopting online teaching/learning, continuous feedback from teachers and students will be required to make e-learning a popular and effective teaching method.
5. Conclusion
A developing country like India needs more low-cost gadgets (desktops/laptops/Wi-Fi routers), broadband internet services, and training in ICT technology to make online teaching a true success. Despite significant problems, students have embraced online classes well and have expressed a preference for the more innovative/technology-based teaching methods. Designing the classes to be of optimum duration, (each class of <40 min duration with at least 10 min gap between the classes, maximum of 2–4 h of classes a day) and incorporating the newer teaching methods are recommended to engage students without boredom and also decrease their risk of health issues.
The following are the supplementary data related to this article.
Survey questionnaire.
Variations in the health issues among medical and nursing students due to online classes.
Table showing the attitudes of the students.
CRediT authorship contribution statement
Hemant Kumar Singh and Pratyusha Ganne: Conceptualization, Methodology, formal analysis, data Curation, writing-original draft, Writing - Review & Editing, Supervision. Arvind Joshi, Raghavi N Malepati and Sahista Najeeb: Methodology, Writing - Review & Editing, Supervision. Pavithra Balakrishna, Naresh Kumar Pannerselvam, and Yashwant Kumar Singh: Writing - Review & Editing, Supervision.
All authors gave approval for the final manuscript.
Financial disclosures
None.
Declaration of competing interest
The authors report no conflicts of interests.
Acknowledgements
We would like to thank all the participants in this study.
References
- Adams N. Bloom’s taxonomy of cognitive learning objectives. J. Med. Libr. Assoc. 2015;103(3):152. doi: 10.3163/1536-5050.103.3.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontrup C., Taylor W.R., Fliesser M., Visscher R., Green T., Wippert P., Zemp R. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl. Ergon. 2019;81 doi: 10.1016/j.apergo.2019.102894. [DOI] [PubMed] [Google Scholar]
- Borhany T., Shahid E., Siddique W.A., Ali H. Musculoskeletal problems in frequent computer and internet users. J. Family Med. Prim. Care. 2018;7(2):337–339. doi: 10.4103/jfmpc.jfmpc_326_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook D.A. Web-based learning: pros, cons and controversies. Clin. Med. (Lond) 2007;7(1):37–42. doi: 10.7861/clinmedicine.7-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellahi A., Khalil M.S., Akram F. Computer users at risk: health disorders associated with prolonged computer use. J. Business Manag. Econ. 2011;2(4):171–182. [Google Scholar]
- Firth J., Torous J., Stubbs B., Firth J.A., Steiner G.Z., Smith L., Alvarez-Jimenez M., Gleeson J., Vancampfort D., Armitage C.J. The “online brain”: how the Internet may be changing our cognition. World Psychiatry. 2019;18(2):119–129. doi: 10.1002/wps.20617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganne P., Najeeb S., Chaitanya G., Sharma A., Krishnappa N.C. Digital eye strain epidemic amid COVID-19 pandemic - a cross-sectional survey. Ophthalmic Epidemiol. 2020 doi: 10.1080/09286586.2020.1862243. [DOI] [PubMed] [Google Scholar]
- Government of India, Ministry of Statistics and Programme Implementation Key indicators of household social consumption on education in India. 2017–2018. http://www.mospi.gov.in/sites/default/files/NSS75252E/KI_Education_75th_Final.pdf
- Hsieh M.L., Dawson P.H., Hofmann M.A., Titus M.L., Carlin M.T. Four pedagogical approaches in helping students learn information literacy skills. J. Acad. Librariansh. 2014;40(3–4):234–246. [Google Scholar]
- Joshi A., Malhotra B., Amadi C., Loomba M., Misra A., Sharma S., Arora A., Amatya J. Gender and the digital divide across urban slums of New Delhi, India: cross-sectional study. J. Med. Internet Res. 2020;22(6) doi: 10.2196/14714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapolla P., Mingoli A. COVID-19 changes medical education in Italy: will other countries follow? Postgrad. Med. J. 2020;96(1137):375–376. doi: 10.1136/postgradmedj-2020-137876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long J., Cheung R., Duong S., Paynter R., Asper L. Viewing distance and eyestrain symptoms with prolonged viewing of smartphones. Clin. Exp. Optom. 2017;100(2):133–137. doi: 10.1111/cxo.12453. [DOI] [PubMed] [Google Scholar]
- Martinengo L., Yeo N.J.Y., Tang Z.Q., Kasturi D., Markandran O., Kyaw B.M., Car L.T. Digital education for the management of chronic wounds in health care professionals: protocol for a systematic review by the Digital Health Education Collaboration. JMIR Res. Protoc. 2019;8(3) doi: 10.2196/12488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen C.J., Nicholson A.M. The flipped classroom stimulates greater learning and is a modern 21st century approach to teaching today’s undergraduates. J. Anim. Sci. 2015;93(7):3722–3731. doi: 10.2527/jas.2015-9087. [DOI] [PubMed] [Google Scholar]
- Rodrigues M.S., Leite R.D.V., Lelis C.M., Chaves T.C. Differences in ergonomic and workstation factors between computer office workers with and without reported musculoskeletal pain. Work. 2017;57(4):563–572. doi: 10.3233/WOR-172582. [DOI] [PubMed] [Google Scholar]
- Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323(21):2131–2132. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- Schweppe J., Rummer R. Attention, working memory, and long-term memory in multimedia learning: an integrated perspective based on process models of working memory. Educ. Psychol. Rev. 2014;26(2):285–306. [Google Scholar]
- Shail M.S. Using micro-learning on mobile applications to increase knowledge retention and work performance: a review of literature. Cureus. 2019;11(8) doi: 10.7759/cureus.5307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shechter A., Kim E.W., St-Onge M.P., Westwood A.J. Blocking nocturnal blue light for insomnia: a randomized controlled trial. J. Psychiatr. Res. 2018;96:196–202. doi: 10.1016/j.jpsychires.2017.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppard A.L., Wolffsohn J.S. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3(1) doi: 10.1136/bmjophth-2018-000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan B., Smith B., Pleggenkuhle-Miles E. Short vs. long: cognitive load, retention and changing class structures. Educ. Econ. 2017;25(5):501–512. [Google Scholar]
- Singh K., Srivastav S., Bhardwaj A., Dixit A., Misra S. Medical education during the COVID-19 pandemic: a single institution experience. Indian Pediatr. 2020;57(7):678–679. doi: 10.1007/s13312-020-1899-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Gazette of India University Grants Commission (Open and Distance Learning Programmes and Online Programmes) Regulations, 2020. 2020. https://www.ugc.ac.in/pdfnews/221580.pdf
- UNESCO COVID-19 impact on education. 2020. https://en.unesco.org/covid19/educationresponse
- Vogel D., Harendza S. Basic practical skills teaching and learning in undergraduate medical education–a review on methodological evidence. GMS J. Med. Educ. 2016;33(4) doi: 10.3205/zma001063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmer H.H., Sherman L.E., Chein J.M. Smartphones and cognition: a review of research exploring the links between mobile technology habits and cognitive functioning. Front. Psychol. 2017;8:605. doi: 10.3389/fpsyg.2017.00605. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Survey questionnaire.
Variations in the health issues among medical and nursing students due to online classes.
Table showing the attitudes of the students.