Abstract
Smell loss is important for coronavirus disease-2019 (COVID-19) screening and diagnosis. Particular attention should be paid to individuals with pre-COVID-19 chronic hyposmia or anosmia. We report a case of reversible taste impairment in a COVID-19 patient with chronically impaired sense of smell. This case emphasizes the importance of COVID-19-related taste assessment.
Keywords: COVID-19, chronic anosmia, hyposmia, microsmia, taste impairment
Background
Smell and taste loss emerged as distinctive and prevalent symptoms of coronavirus disease-2019 (COVID-19).1,2 Self-reporting smell and taste impairments is becoming common for COVID-19 characterization. Most of the studies rely on self-reports rather than objective assessments3 and focus on smell impairment only.4,5 Smell self-assessment apps have been developed (ie, SmellTracker) and screening tests had been suggested6,7 for identifying potentially infected persons. Recently, several studies had found that quantitative smell change is the best predictor of COVID-19 in both single and cumulative feature models and suggested COVID-19 infection probability calculators based on smell rating rather than taste.8-11
A possible reasoning for focusing on olfactory dysfunction alone is the high correlation between taste and smell loss reports by the same patient1 and in populations in general,12,13 making it obsolete to test both senses. Additionally, some researchers had speculated that taste loss is misinterpretation of flavor loss. This can be due to lack of ability to distinguish between taste receptors activation on the tongue and olfactory receptor stimulation by volatiles entering from the nasopharynx during deglutition that cause flavor sensations.14
On the other hand, commonly self-reported impairment of basic taste modalities (sweet, taste, salty, sour, and umami) by COVID-19 patients1,9 supports the notion that taste impairment in this disease can occur independently of olfactory signals and entail nonvolatile signals. In this article, we describe a case of COVID-19-positive patient with self-reported chronically impaired sense of smell (subsequently diagnosed as moderate microsmia) who reported a temporary impairment in taste during her illness.
Case Presentation
A 40-year-old COVID-19-positive patient (diagnosed via RT-PCR [reverse transcription polymerase chain reaction] swab test) reported taste loss during her illness. The patient indicated she is not a smoker nor an alcohol beverages consumer. The patient had no previously known medical histories, other than permanent use of drug treatment for thyroid function and chronic smell impairment.
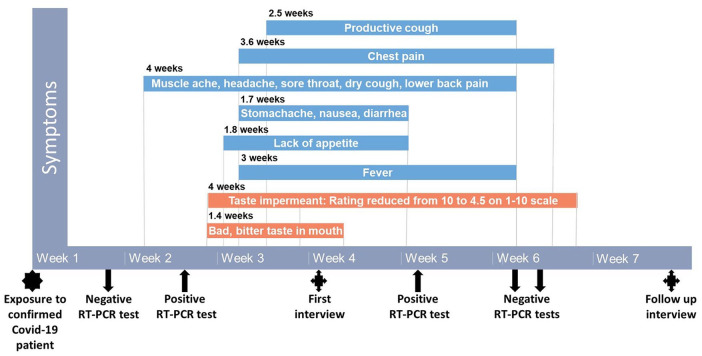
During her illness, the patient had experienced the following symptoms plotted in Figure 1: fever, dry cough, productive cough, chest pain, sore throat, muscle ache, diarrhea, nausea, lack of appetite, headache, taste impairment, and lower back pain.
Figure 1.
Symptoms Timeline.
Note. X-axis indicates timeline (weeks), with markings for exposure to confirmed COVID-19 patient and RT-PCR tests results. Y-axis indicated symptoms duration and descriptions are shown in the timeline.
When specifically inquired about her sense of smell, she stated that it did not change during her illness. When asked to rate her sense of smell on a 1 to 10 scale, she rated it as “1” (none) for before, during, and after her illness. The patient stated she first realized at the age of 25 that she had lifelong lack of ability to smell, when she was pregnant for the first time. Throughout her pregnancy, she was able to smell for the first time, leading her to realize her usual ability to smell was always impaired. Her ability to smell during her pregnancy disappeared after giving birth and this phenomenon repeated in her subsequent 5 pregnancies. Interestingly, following her recovery from COVID-19, the patient’s sense of smell was evaluated using University of Pennsylvania Smell Identification Test (UPSIT)15 and moderate microsmia was established.
The patient reported she did not have any difficulty breathing through her nose before her illness, but she had a slight impairment during the illness that completely resolved after the illness. The patient reported she had an excellent sense of taste before her illness, which was significantly decreased (evaluated by her as 10 on a 1-10 scale before her illness and 4.5 during her illness, indicating a reduction in sense of taste [hypogeusia]) during illness. Specifically, she stated that she felt a reduction in sweet, salty, sour, and bitter taste, in addition to a reduction in chemesthesis (spicy, cooling, and tingling sensations). Moreover, the patient described a sensation of bad and bitter taste in her mouth, lasting for more than a week.
Written informed consent for publication of patient’s clinical details was obtained from the patient.
Discussion and Conclusions
In this article, we present a case of a COVID-19 patient who reports chronically impaired sense of smell that did not change during the COVID-19 infection. Her self-reported sense of taste was intact prior to the disease. During the COVID-19 illness, the patient experienced reduction in her sense of taste while still unable to smell. Furthermore, she reported reduction in ability to sense spicy, cooling, or tingling sensation during her illness.
After recovery, the patient took the UPSIT test in ENT clinic and was diagnosed with moderate microsmia. Microsmia or “hyposmia” is defined as quantitatively reduced olfactory function. This objective test combined with the patient’s self-reported lack of smell before the illness suggests that the patient’s condition was chronic and that it is hyposmia rather than anosmia. Discrepancies between self-reporting and objective testing of olfactory function have been documented.16 While self-reported smell and taste impairments have already proven as powerful and sensitive tools for COVID-19 screening, it will be important to compare these with objective reading.
The realization that taste change is not limited to volatiles-induced flavors and can be impaired in COVID-19 independently of olfactory ability calls special attention to sudden onset isolated taste loss in COVID-19 infection. With estimated 5% of population chronically exhibiting functional anosmia,17 the open questions regarding the underlying mechanisms of chemosensory loss in COVID-19,18 and the immense potential of smell and taste screening for diagnosis, the importance of taste loss in COVID-19 diagnosis and screening should not be disregarded.
In accord with previous studies, we had recently found smell change to be far better predictor of COVID-19 than taste change. Nevertheless, in light of the considerable number of COVID-19 patients reporting taste impairment with no smell impairment, we suggested an alternative COVID-19 probability calculator, based on taste change rather than smell change.9 The current case underlines the significance of the taste change symptom and the need for population-targeted studies, aimed to develop better and more accurate calculators for patients with lifelong hyposmia or anosmia.
Furthermore, this case highlights the importance of anamnesis for picking up chronic taste or smell disturbances in the diagnosis of COVID-19, and the important role of taste assessment for capturing likelihood of COVID-19 within chronically hyposmic or anosmic individuals.
Acknowledgments
We thank the patient for her time and written informed consent for publication of her case history. We thank Professor Ran Nir-Paz and Professor Thomas Hummel for helpful discussions.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Israel Science Foundation Grant #1129/19 to MYN.
Ethics Approval: The study was conducted in accordance with Helsinki Committee and the required ethics approval was granted (Reference Number HMO-0236-20).
Informed Consent: Written informed consent for publication of patient’s clinical details was obtained from the patient.
ORCID iD: Noam Karni  https://orcid.org/0000-0003-2086-3500
https://orcid.org/0000-0003-2086-3500
References
- 1. Parma V, Ohla K, Veldhuizen MG, et al. More than smell—COVID-19 is associated with severe impairment of smell, taste, and chemesthesis. Chem Senses. 2020;45:609-622. doi: 10.1093/chemse/bjaa041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hopkins C, Surda P, Kumar N. Presentation of new onset anosmia during the COVID-19 pandemic. Rhinology. 2020;58:295-298. doi: 10.4193/Rhin20.116 [DOI] [PubMed] [Google Scholar]
- 3. Tong JY, Wong A, Zhu D, Fastenberg JH, Tham T. The prevalence of olfactory and gustatory dysfunction in COVID-19 patients: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2020;163:3-11. doi: 10.1177/0194599820926473 [DOI] [PubMed] [Google Scholar]
- 4. Gilani S, Roditi R, Naraghi M. COVID-19 and anosmia in Tehran, Iran. Med Hypotheses. 2020;141:109757. doi: 10.1016/j.mehy.2020.109757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Walker A, Hopkins C, Surda P. Use of Google Trends to investigate loss-of-smell-related searches during the COVID-19 outbreak. Int Forum Allergy Rhinol. 2020;10:839-847. doi: 10.1002/alr.22580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Calvo-Henriquez C, Maldonado-Alvarado B, Chiesa-Estomba C, et al. Ethyl alcohol threshold test: a fast, reliable and affordable olfactory assessment tool for COVID-19 patients. Eur Arch Otorhinolaryngol. 2020;277:2783-2792. doi: 10.1007/s00405-020-06131-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Iravani B, Arshamian A, Ravia A, et al. Relationship between odor intensity estimates and COVID-19 prevalence prediction in a Swedish population. Chem Senses. Published online May 22, 2020. doi: 10.1093/chemse/bjaa034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gerkin RC, Ohla K, Veldhuizen MG, et al. Recent smell loss is the best predictor of COVID-19: a preregistered, cross-sectional study. medRxiv. Published online July 26, 2020. doi: 10.1101/2020.07.22.20157263 [DOI] [Google Scholar]
- 9. Karni N, Klein H, Asseo K, et al. Self-rated smell ability enables highly specific predictors of COVID-19 status: a case control study in Israel. medRxiv. Published online December 28, 2020. doi: 10.1101/2020.07.30.20164327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. David P, Shoenfeld Y. The smell in COVID-19 infection: diagnostic opportunities. Isr Med Assoc J. 2020;22:401-403. [PubMed] [Google Scholar]
- 11. Yan CH, Faraji F, Prajapati DP, Ostrander BT, DeConde AS. Self-reported olfactory loss associates with outpatient clinical course in COVID-19. Int Forum Allergy Rhinol. 2020;10:821-831. doi: 10.1002/alr.22592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Asseo K, Fierro F, Slavutsky Y, Frasnelli J, Niv MY. Utility and limitations of Google searches on sensory loss as markers for new COVID-19 cases. medRxiv. Published online May 31, 2020. doi: 10.1101/2020.05.07.20093955 [DOI] [Google Scholar]
- 13. Pierron D, Pereda-Loth V, Mantel M, et al. Smell and taste changes are early indicators of the COVID-19 pandemic and political decision effectiveness. Nat Commun. 2020;11:5152. doi: 10.1038/s41467-020-18963-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Whitcroft KL, Hummel T. Olfactory dysfunction in COVID-19: diagnosis and management. JAMA. 2020;323:2512-2514 doi: 10.1001/jama.2020.8391 [DOI] [PubMed] [Google Scholar]
- 15. Doty RL, Shaman P, Dann M. Development of the University of Pennsylvania Smell Identification Test: a standardized microencapsulated test of olfactory function. Physiol Behav. 1984;32:489-502. doi: 10.1016/0031-9384(84)90269-5 [DOI] [PubMed] [Google Scholar]
- 16. Seok J, Shim YJ, Rhee CS, Kim JW. Correlation between olfactory severity ratings based on olfactory function test scores and self-reported severity rating of olfactory loss. Acta Otolaryngol. 2017;137:750-754. doi: 10.1080/00016489.2016.1277782 [DOI] [PubMed] [Google Scholar]
- 17. Hummel T, Landis BN, Hüttenbrink KB. Smell and taste disorders. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2011;10:Doc04. doi: 10.3205/cto000077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cooper KW, Brann DH, Farruggia MC, et al. COVID-19 and the chemical senses: supporting players take center stage. Neuron. 2020;107:219-233. doi: 10.1016/j.neuron.2020.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]