Abstract
Background
Self-care practice among people with diabetes is not well-implemented in Ethiopia. So far, in Ethiopia, several observational studies have been done on self-care practice and its determinants in people with diabetes. However, a comprehensive review that would have a lot of strong evidence for designing intervention is lacking. So, this review with a meta-analysis was conducted to bridge this gap.
Methods
A systematic review of an observational study is conducted following the PRISMA checklist. Three reviewers have been searched and extracted from the World Health Organization’s Hinari portal (SCOPUS, African Index Medicus, and African Journals Online databases), PubMed, Google Scholar and EMBASE. Articles’ quality was assessed using the Newcastle-Ottawa Scale by two independent reviewers, and only studies with low and moderate risk were included in the final analysis. The review presented the pooled proportion of non-adherence to self-care practice in people with diabetes and the odds ratios of risk factors hindering to self-care practice after checking for heterogeneity and publication bias. The review has been registered in PROSPERO with protocol number CRD 42020149478.
Results
We included 21 primary studies (with 7,134 participants) in this meta-analysis. The pooled proportion of non-adherence to self-care in the diabetes population was 49.91 (95% CI: 44.73–55.08, I2 = 89.8%). Male (Pooled Odds Ratio (POR): 1.84 95%CI; 1.04–2.64, I2 = 15.0%), having private glucometer (POR: 2.71; 95%CI: 1.46–3.95, I2 = 0.0%), short-term Diabetes Mellitus (DM) duration (POR: 3.69; 95%CI: 1.86–5.52, I2 = 0.0%), DM complication (POR: 2.22; 95%CI: 1.48–2.95, I2 = 0.0%), treatment satisfaction (POR: 1.8; 95% CI: 1.15–2.44, I2 = 0.0%), received diabetes self-management education (POR: 2.71; 95% CI: 1.46–3.95, I2 = 0.0%) and poor self-efficacy (POR: 3.09; 95% CI: 1.70–4.48, I2 = 0.0%) were statistically significant factors of non-adherence to self-care practice.
Conclusions
The overall pooled proportion of non-adherence to self-care among adult diabetes in Ethiopia was high. Further works would be needed to improve self-care practice in the diabetes population. So, factors that were identified might help to revise the plan set by the country, and further research might be required to health facility fidelity and each domain of self-care practice according to diabetes self-management guideline.
Background
Diabetes Mellitus (DM) is one of the major public health problems worldwide. DM is one of the four priorities on non-communicable diseases increasing by epidemic proportions [1–5]. The number of people living with diabetes will reach 693 million cases in the world by the end of 2045. Of this, 16 to 41 million cases will be in Africa [6,7]. Now a day, DM is recognized as an important cause of premature death and lifelong disability [8,9]. People with diabetes have an increased risk of developing serious life-threatening health problems, increasing medical care costs, and compromise the quality of life [4,6,7,10].
Diabetes brings a global economic burden that will increase from the United State $1.3 trillion in 2015 to $2.1 trillion in the target scenarios by 2030. This translates to an increase in costs as a share of global gross domestic product [11,12]. Health systems in Sub-Saharan Africa countries are unable to cope with the current burden of DM. The unique challenges to combat DM in these regions are lack of [1] fund for non-communicable disease-specific to the diabetes population [2], availability of enough guidelines specific to the diabetes population [3], availability of adequate medications, and [4] service access differences in the urban and the rural person with diabetes and [5] inequity between the public and the private sector of healthcare. Because of such obstacles, diabetes has a greater impact on morbidity and mortality in sub-Saharan Africa as compared to other regions in the world [8,9,11,13–15].
Individuals with DM develop lifelong self-care skills and are committed to making behavioral changes to prevent or delay complications [16,17]. Self-care is the practice of activities that an individual initiates and performs on his or her own behalf to keep up with a healthy life. It is also a way of life, not just a task [18,19]. Adherence to self-care is the extent to which a person’s behavior in which following a recommended diet, foot care practice, self-monitoring of plasma glucose, and/or executing lifestyle changes corresponds with agreed recommendations from a healthcare provider [17,20].
The main reason for non-adhered to self-care practice was health care providers, and diabetes educators did not check perceived client barriers to self-care practice and make recommendations with these in mind. Many health care providers are not discussing self-care practice with diabetic people [21–24]. Through multiple barriers to accepting self-care practice, low health literacy, socioeconomic burden, and social support, factors influence self-care non-adherence in a person with diabetes. In Ethiopia, diabetes self-management programs, including diabetes education, are not accessible where the care is [25,26].
Realizing the multi-faceted nature of the problem, the health care providers and the patient shall build a trusting relationship, a systematic, multi-pronged, and integrated approach is required for promoting self-care practice adherence. Non-adherence to self-care practice in diabetes has been found to vary from region to region in Ethiopia [27–31]. Even though the pooled proportion (49%) of good diabetes self-care behavior among people with diabetes is documented in Ethiopia [32], the overall non-adherence and common factors that hinder self-care practice are not documented in the country. Thus, this study aimed to assess the pooled proportion of non-adherence to self-care and associated factors among the adult diabetes population in Ethiopia.
Materials and methods
Protocol design and registration
A systematic review of an observational study is conducted following the meta-analysis of observational studies in an epidemiology statement. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocol (PRISMA—P) [33,34] and Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guideline [35] were used for the development of this study protocol, the conduct and design, and reporting these results (S 1). To minimize duplication of the same reviews, provide transparency, and reduce reporting bias of the current review, the protocol was registered with the International Registration of Systematic Reviews (PROSPERO) with PROSPERO registration number CRD 42020149478 (S 2).
Eligibility criteria
The studies (all published and unpublished) were that used observational epidemiological designs (cross-sectional), intended to assessed non-adherence to self-care practice and associated factors among people with diabetes aged 15 and above, and articles that were published in the English language. Studies were conducted in a case series, unclear definition of self-care practice (like unclear measurement of questionnaires in the outcome variables, and did not report specific outcomes for self-care adherence/non-adherence quantitatively) were excluded in the final analysis.
Data sources and searching strategy
A search strategy has been developed using fundamental concepts in the research question: “self-care adherence”, “self-care practice”, “therapy adherence”, “treatment adherence”, “medication intake adherence”, “medication compliance”, “patient compliance”, “diabetes mellitus”, “diabetes”, “patients”, “clients”, and “factors”, “determinants”, “influences”, “risk factors”, “predictors” and “Ethiopia”. For each key concept, appropriate free-text words and Medical Subject Heding (MeSH) were used and combined using boolean operators such as “AND’ and “OR.” This enabled the retrieval of relevant articles that might have used different synonyms for the same word. Notably, to fit the advanced PubMed database, the search was strategy applied (S 3).
A pretest of the search strategy by three authors was performed in PubMed, and the actual electronic search was done between 25 February and March 5, 2020. Three reviewers implemented the electronic search in the following electronic databases: PubMed, Embase, GOOGLE SCHOLAR, CINAHL, MEDLINE, and Hinari electronic databases for articles published on 17 April 2012 to 10 September 2019. Hinari is the World Health Organization (WHO) database portal for low and middle income countries and includes Web of Science, SCOPUS, African Index Medicus (AIM), Cumulative Index to Nursing and Allied Health Literature (CINAHL), WHO’s Institutional Repository for Information Sharing (IRIS), and African Journals Online databases. In addition, articles were also searched through a review of the grey literature available on institutional repositories (Addis Ababa University). Besides, find articles by reviewing the reference lists of already identified researches.
Study selection
All the citation identified by our search strategy, which was potentially eligible for inclusion, was exported to EndNote software version X7, Thomson Reuters, New York, NY, and the duplicate were removed. Title and abstracts of the remaining citation were screened by three independent reviewers (TWA, EA, and GD) and ineligible studies were further excluded. The full texts of selected articles were retrieved and read thoroughly to ascertain their suitability before data extraction. Articles that fulfilled the earlier criteria used as sources of data for analysis.
Data extraction
The abstract and full-text review and data abstraction were done by two independent reviewers (HG and MT) using a standardized data abstraction form, developed according to the sequence of variables required from primary studies on MS-Excel sheet. The disagreement between the two reviewers was resolved by a third independent reviewer (GD or AE). Before analysis, a transformation of the Adjusted odds ratios and proportion.
The New castle Ottawa Scale criteria was selected for quality assessment of selected studies before analysis [36]. Two independent reviewers (HG and MT) critically appraised each article using the NOS. Discrepancies between reviewers resolved by discussion and by including a third reviewer (MB). The average of two independent reviewer’s quality scores used to decide whether the articles included or not. Articles with methodological flaws or incomplete reporting of results in the full-text excluded from the analysis. The data extraction formant included primary author, publication year, region, outcome measuring tool, study design, response rate, sample size, and proportion.
Outcome measurement
The primary outcome of this review the pooled proportion of non-adherence to the self-care practice of people with diabetes in Ethiopia. The proportion measured as the number of adult diabetes with non-adherence to self-care practice in the studies divided by the total number of diabetes people in a study multiplied by 100. For the analysis of the secondary outcomes (factors), we extracted data on factors that were related to non-adherence to self-care practice in the literature. Such as social support, having own glucometer at home, duration of diabetes, diabetes-related complication, diabetes knowledge, received diabetes self-management education, and socio-demographic related factors. In examining factors associated with non-adherence to self-care practice, data used from the primary studies of the Adjusted Odd Ratios (AOR) to find the association between the independent variables and having non-adherence to self-care practice.
Quality assessment
The risk of bias of included studies is assessed using the 10-item rating scale developed by Hoy et al. for prevalence studies [37]. The assessment tool has a representative sample size, method of data collection, reliability and validity of study tools, case definition, and prevalence periods of the studies. Researchers categorized each study as having a low risk of bias (“yes” answers to domain questions) or a high risk of bias (“no” answers to domain questions). Each study assigned a score of 1 (Yes) or 0 (No) for each domain, and these domain scores were summed to give an overall study quality score. Scores of 8–10 were considered as having a “low risk of bias”, 6–7 a “moderate risk”, and 0–5 a “high risk” (S 4). For the least risk of bias classification, discrepancies between the reviewers resolved via consensus.
Statistical analysis
Testing for heterogeneity
Heterogeneity between the result of the primary studies was assessed using Cochran’s Q test and quantified with the I2 statistics. A p-value of less than 0.1 was considered to suggest statically significant heterogeneity, considering a category a small number of studies and their heterogeneity in design [38]. Heterogeneity had taken low, moderate, and high categories when the I2 values were below 25%, between 25% and 75%, and above 75%, respectively [39,40]. Thus, the random effect model was used to pool the proportion of non-adherence to self-care practice since the studies were found heterogeneous. The random effect model accounts for heterogeneity among study results beyond the variation associated with chance, unlike the fixed-effect model [41]. To investigate the source of heterogeneity, the random-effects meta-regression was conducted by taking primary study characteristics such as study year, region, and study setting (hospitals). The meta-regression analysis was weighted to account for the residual between-study heterogeneity (i.e., heterogeneity not explained by the covariates in the regression) [42]. Subgroup analyses by region and type of study setup (hospitals) were carried out because of significant heterogeneity between studies (i.e., I2 = 89.8%, p < 0.05).
Publication bias assessment
Publication bias was assessed by visual inspection of funnel plots based on the shape of the graph (subjective assessment). The symmetrical graph was interpreted to suggest an absence of publication bias, whereas an asymmetrical one indicates the presence of publication bias. On the other hand, qualitatively (objective ealuation), Egger’s weighted regression tests was used to assess publication bias with a p-value less than 0.1 considered as indicative of a statistically significant publication bias [43].
Sensitivity analysis
Lastly, a sensitivity analysis was done to estimate whether the pooled effect size was affected by single studies. A leave-one-out sensitivity analysis was performed to confirm whether there were studies that potentially biased the direction of the pooled estimate.
Result
Study selection
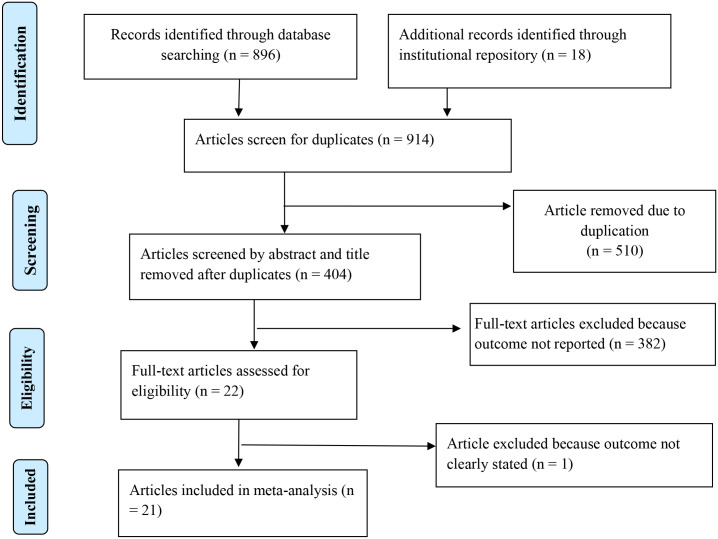
The database search and desk review yielded a total of 914 articles. Of these, 896 articles were retrieved from PubMed, Google Scholar, EMBASE, and the World Health Organization’s Hinari portal (which includes the SCOPUS, African Index Medicus, and African Journals Online databases). The remaining 18 observational studies were found from institutional repositories (Addis Ababa, Gondar, and Bahir Dar Universities). After reviewing the titles and abstracts, we excluded 510 articles due to duplication. In screening, we excluded 382 articles because their outcomes were not in line with the desired eligibility criteria. The full-text of the remaining 22 articles were accessed for eligibility and quality. Additionally, an article was excluded because its outcomes variable was not clearly stated [44] (S 5). The remaining 21 studies were included in the analysis (Fig 1).
Fig 1. PRISMA statement presentation for a meta-analysis of a pooled proportion of non-adherence to self-care practice among DM in Ethiopia, 2011–2019.
Study characteristics
Overall, a total of 21 observational studies were selected in this systematic review and meta-analysis. This consisted of 7,134 participants (aged 15–86 years). The number of participants in each study ranged from 222 to 595. The mean age ranged from 38 to 55.03 years and the duration of the disease from 1.74 to 12 years. All studies were cross-sectional design to estimate self-care adherence. The most retrieved studies (n = 5) were from Oromia region [45–49], followed by Addis Ababa (n = 4) [50–53], and Amhara region (n = 3) [31,54,55], Eastern Ethiopia (Dire Dawa and Harari) [27,56,57], and Tigray region [29,58,59] were represented by three studies, whereas Southern Nations Nationalities and People’s Region (SNNPR) represented by two studies [60,61], and Benishangul Gumez region was represented by one study [62]. Except for two studies [51,52], all the studies reported in peer-reviewed journals are reported in peer-reviewed journals. All of the studies used a summary of diabetes self-care activities to investigate the non-adherence to self-care practice and reported high response rates (> 95%) (Table 1).
Table 1. Descriptive summary of 21 studies included in the meta-analysis of the proportion of non-adherence to self-care practice in Ethiopia from 2011–2019.
| Authors name | Study year | Source types | Region | Types of hospital | Age of subjects | RR (%) | SS | Total outcome | Prevalence (%) | Quality score (NOS) |
|---|---|---|---|---|---|---|---|---|---|---|
| Abate TW. et al | 2017 | Journal | Amhara | Referral | ≥18 | 99.5 | 416 | 298 | 71.6 | 8 |
| Addisu Y. et al | 2013 | Journal | SNNPR | Referral | ≥18 | 100 | 310 | 72 | 23.2 | 6 |
| AlemayhuT.et al | 2018 | Journal | Dire Dawa | General | ≥18 | 98.6 | 506 | 223 | 44.1 | 8 |
| Amente T. et al | 2013 | Journal | Oromia | Referral | ≥15 | 98 | 254 | 114 | 45 | 7 |
| AschalewAY.et al | 2017 | Journal | Amhara | Referral | ≥18 | 100 | 403 | 209 | 51.86 | 6 |
| Ayele K. et al | 2011 | Journal | Harai | Referral | ≥18 | 100 | 222 | 135 | 60.8 | 7 |
| Ayele BH.et al | 2017 | Journal | Harar and Dire Dawa | General | ≥18 | 97.8 | 320 | 198 | 61.9 | 8 |
| Berhan T. et al | 2015 | IR | A.A | General | ≥18 | 100 | 595 | 284 | 47.7 | 8 |
| Berhe KK.et al | 2012 | Journal | A.A | Referral | 30–85 | 99.1 | 320 | 142 | 44.4 | 7 |
| Berhe KK. et at | 2013 | Journal | Tigray | Referral | ≥18 | 96.8 | 300 | 147 | 49 | 7 |
| Chali SW. et al | 2018 | Journal | Benishangul Gumuz | General | ≥18 | 96 | 383 | 175 | 45.7 | 8 |
| Dedefo MG.et al | 2016 | Journal | Oromia | Referral | ≥15 | 100 | 252 | 99 | 39.3 | 6 |
| FEYISSA L.et at | 2014 | IR | A.A | Referral | ≥18 | 98.8 | 324 | 157 | 48.5 | 7 |
| Gurmu Y.et al | 2017 | Journal | Oromia | General | ≥18 | 100 | 257 | 117 | 45.5 | 8 |
| Kassahun T.et al | 2014 | Journal | Oromia | Referral | ≥18 | 95 | 309 | 152 | 49.1 | 8 |
| Mamo M. et al | 2011 | Journal | A. A | Referral | ≥18 | 97.8 | 646 | 256 | 39.7 | 8 |
| Mariye T. et al | 2017 | Journal | Tigray | General | ≥18 | 100 | 284 | 178 | 62.7 | 7 |
| Niguse H. et al | 2017 | Journal | Tigray | Referral | ≥18 | 100 | 338 | 252 | 74.5 | 7 |
| Sorato MM.et al | 2015 | Journal | SNNPR | General | ≥15 | 100 | 194 | 114 | 58.8 | 5 |
| Tadesse E. et al | 2014 | Journal | Oromia | Referral | ≥30 | 100 | 116 | 59 | 50.9 | 6 |
| Tiruneh SA.et al | 2018 | Journal | Amhara | General | ≥18 | 95 | 385 | 142 | 36.9 | 8 |
SS: Sample size; RR: Response Rate; IR: Institutional repository; A.A: Addis Ababa, NOS: New-castle Ottaw Scale.
Quality appraisal
The quality score of the included study ranged from 5 to 8 with a mean score of 7.14 (SD = 0.91). Out of 21 studies, 16 (76.19%) studies received a low risk of bias, and 5 (23.81%) studies received a moderate risk of bias. The authors also find types of bias: 10 studies [63–72] had a high risk of case definition, 8 studies [65,68,71,73–77] had a high risk of sampling and representation [64,68,69,73,74,76,78,79] bias, and 5 studies [66,67,69,71,73] had a high risk of random selection bias (S4).
Meta-analysis
Pooled estimates of non-adherence to self-care
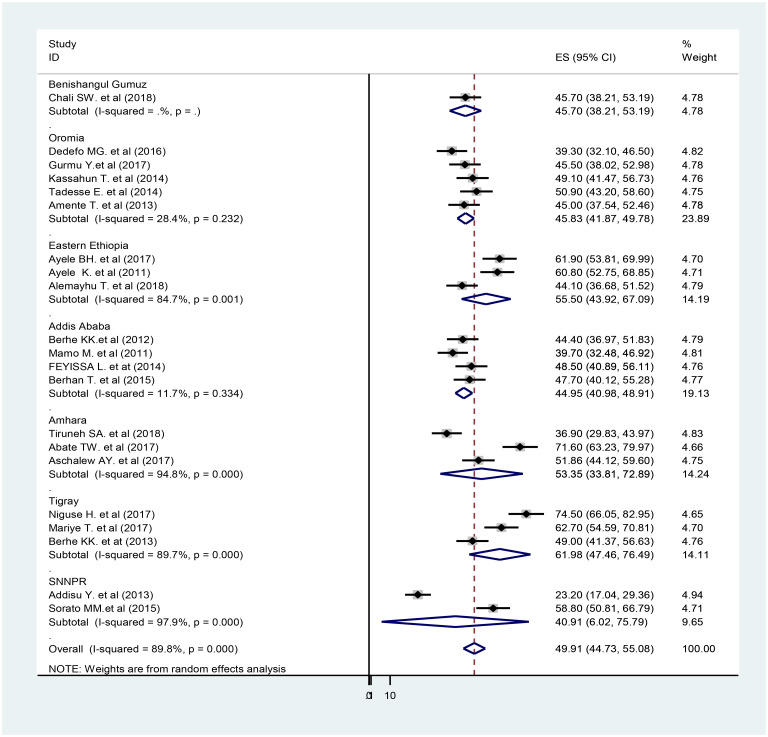
The analysis of twenty-one observational studies was ranked as low and moderate-quality. The pooled proportion of non-adherence to self-care practice in people with diabetes was 49.91% (95%CI: 40.12–55.25, I2 = 89.8). The highest (71.60%) [55] and the lowest (23.20%) [60] non-adherence of self-care practice reported in the Amhara region and in the SNNPR respectively. High heterogeneity was observed among the included studies (Q test P<0.001) and I2 (I2 = 89.8%) (Fig 2). Due to the heterogeneity of included studies, further sub-group analysis was done by using the following study characteristics: regional location and study setting (hospital). The random-effect model was applied for reporting the pooled proportion of non-adherence to the self-care practice of the sub-group analysis.
Fig 2. A subgroup analysis of the forest plot showing the pooled proportion of non-adherence to self-care practice among DM in Ethiopia, 2011–2019.
Subgroup analysis
On subgroup analysis by region, the highest pooled proportion of non-adherence self-care was found in the Tigray region (Pooled Proportion (PP) = 61.98%; 95% CI: 47.46–76.49) and the lowest in the SNNPR (PP = 40.91%; 95% CI: 6.02–75.79). The pooled proportion of non-adherence to elf-care among DM in the Amhara region was 53.35% (95% CI: 33.81, 72.89), and 44.95% (95% CI: 40.98, 48.91) in Addis Ababa. The pooled proportion of non-adherence to self-care practice in a referral hospital is 49.5% (42.20, 57.18) (Table 2).
Table 2. Sub-group analysis of non-adherence to self-care practice based on hospital and region in Ethiopia from 2011 to 2019.
| Variables | Characteristics | Estimated proportion of non-adherence to self-care practice | I2 p value |
|---|---|---|---|
| Region | Benishangul Gumuz | Single study | Single study |
| Oromia region | 45.83 (41.81, 49.78) | 28.4%, p = 0.232 | |
| Eastern Ethiopia* | 55.50 (43.92, 67.09) | 84.7%, p < 0.001 | |
| Addis Ababa | 44.95 (40.98, 48.91) | 11.7%, p = 0.334 | |
| Amhara | 53.35 (33.81, 72.89) | 98.8%, p <0.001 | |
| Tigray | 61.98 (47.48, 76.49) | 89.7%, p <0.001 | |
| SNNPR | 40.91 (6.02, 75.79) | 97.9%, p <0.001 | |
| Hospitals | General | 50.28 (43.74, 55.81) | 82.9%, p <0.001 |
| Referral | 49.69 (42.20, 57.18) | 92.20%, p <0.001 |
SNNPR = Southern Nations Nationalities and Peoples’ Region,
* = Harai and Dire Dawa.
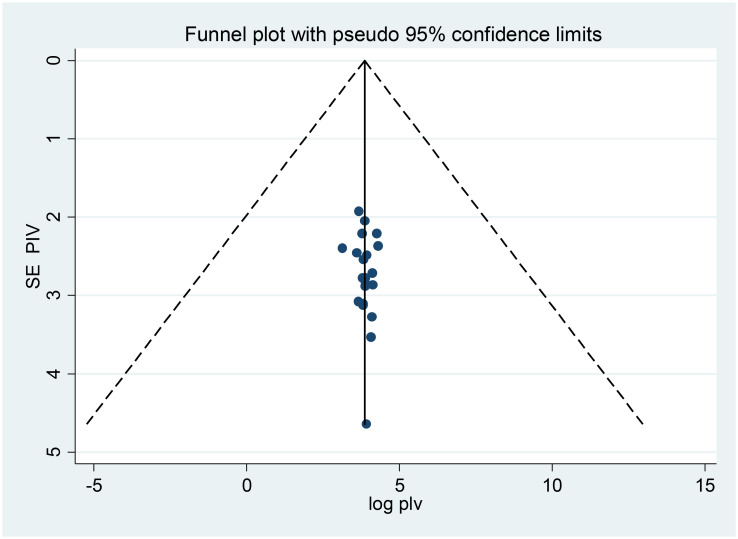
Publication bias
Both funnels plots of precision asymmetry and the Egger’s test of the intercept showed that there is no publication bias in the primary studies. Visual examination of the funnel plot showed a symmetric distribution of studies. Additionally, Egger’s test of the intercept was 0.0786 (95% CI: -0.18, 0.34) p > 0.05 (0.54), as judged by Egger’s test, there was no evidence of publication bias being presented at 5% significance level (Fig 3).
Fig 3. Meta funnels presentations of the proportion of non-adherence to self-care practice among diabetes in Ethiopia, 2011–2019, whereby SE PIV (standard error of proportion) plotted on the Y-axis and log PIV (logarithm of proportion) on the X-axis.
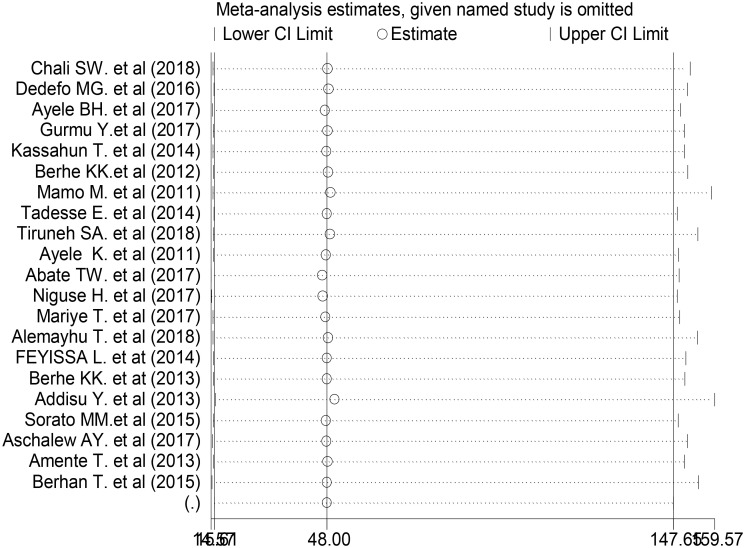
Meta-regression and sensitivity analysis
The sub-group analysis showed that heterogeneity across the studies was widespread. To name the source of heterogeneity, we conducted a meta-regression and sensitivity analysis. During the meta-regression analysis, we conducted using the following study covariance: publication years, sample size, and region. However, the results showed that none of these variables were a statistically significant source of heterogeneity (Table 3). We also performed a sensitivity analysis to find the influence of each study on the overall effect size. No single primary study affected the overall pooled proportion of non-adherence to self-care practice among people with diabetes in Ethiopia (Fig 4).
Table 3. Meta-regression output to explore heterogeneity of the pooled proportion of non-adherence to diabetes self-care practice among the diabetes population in Ethiopia from 2011 to 2019.
| Variables | Coefficients | P-value | 95% CI |
|---|---|---|---|
| Study Year | 0.67 | 0.983 | -63.62, 64.95 |
| Sample size | 0.01 | 0.987 | -1.16, 1.15 |
| Region | |||
| Benishangul Gumuze | Single study | ||
| Addis Ababa | -0.65 | 0.961 | -28.52, 27.22 |
| Amhara | 9.71 | 0.57 | -20.97, 36.58 |
| Eastern Ethiopia (Harai and Dire Dawa) | 9.79 | 0.479 | -19.04, 38.61 |
| Oromia | 0.19 | 0.989 | -27.22, 27.59 |
| SNNPR | -5.14 | 0.725 | -35.76, 25.51 |
| Tigray | 16.45 | 0.241 | -12.37, 45.27 |
Fig 4. One-leave-out sensitivity analysis for studies conducted on proportion of non-adherence to self-care practice among people with DM in Ethiopia, 2011–2019.
Determinants of non-adherence to self-care practice
Extracted adjusted odds ratios from primary studies were organized into four themes (socio-demographic, clinical, get access to glucometere and DM education, and psychosocial) and pooled to identify the predominant risk factors for non-adherence to self-care practice among diagnosed diabetes population in Ethiopia.
Socio-demographics factors
In the primary studies, a significant association was observed between socio-demographic variables and non-adherence to self-care. Such as, participants who had a family history of DM (AOR: 0.5; 95% CI: 0.30,0.90) [47], being widowed (AOR: 4.05; 95% CI: 1.41, 11.5) [55], self-employed (AOR: 5.94; 95%CI: 1.97, 17.94) [29], being single (AOR: 5.39; 95% CI: 1.75, 16.75) [75], and being divorced (AOR: 0.2; 95% CI: 0.05, 0.89) [80] had higher odds of non-adherence to self-care practice.
Twelve primary studies [27,31,46–48,52,53,55–57,59,81] assessed the association between educational level and non-adherence to self-care practice. Three primary studies [45,52,53] found that male people with DM were more likely to non-adherence to self-care practice than female people with DM (AOR: 1.84, 95% CI: 1.04, 2.64). Three [48,53,61], four [27,31,45,58] and five [31,52,57,58,61] primary studies were reported age, residency, and income were associated with non-adherence to self-care practice respectively.
The pooled effect of male participants (Pooled Odds Ratio (POR): 1.84; 95%CI: 1.04–3.92; I2 = 51.2%), and participants with low level of literacy (POR: 2.89; 95%CI: 1.52–4.25; I2 = 0.0%) were significantly affect on non-adherence to self-care practice in people with diabetes. However, no significant association between age (POR: 1.49; 95% CI: -0.95–3.92, I2 = 51.2%), residency (POR: 0.48; 95% CI: -0.26-.21, I2 = 0.0%) and income (AOR: 0.85; 95% CI: 0.15, 1.54, I2 = 69.5%), and non-adherence to self-care practice were observed (Table 4).
Table 4. The relationship between non-adherence to diabetes self-care practice and the pooled effect of factors eligible for meta-analysis among diabetes population in Ethiopia from 2011–2019.
| Factors | Non-Adherence to Self-Care Practice | ||
|---|---|---|---|
| AOR (95% CI) | I2 (%) | P-value (n) | |
| Socio-demographic factors | |||
| Age | 1.49 (-0.94, 3.92) | 51.2 | 0.129 |
| Sex | 1.84 (1.04, 2.64) | 15.0 | 0.803* |
| Residency | 0.48 (-0.26, 1.21) | 0.0 | 0.499 |
| Educational status | 2.89 (1.52, 4.25) | 72.3 | <0.001* |
| Income | 0.85 (0.15, 1.54) | 69.5 | <0.011 |
| Accessibility | |||
| Access to DSME | 2.76 (1.97, 3.55) | 0.0 | <0.001* |
| Access to glucometer at home | 2.71 (1.46, 3.95) | 0.0 | 0.926* |
| Knowledge toward DM | 1.48 (0.79, 2.17) | 77.3 | <0.001 |
| Clinical related factors | |||
| DM duration | 3.69 (1.86, 5.52) | 0.0 | 0.631* |
| DM complication | 2.22 (1.48, 2.95) | 0.0 | 0.891* |
| Satisfaction for medical care | 1.8 (1.55, 2.44) | 0.0 | 0.604* |
| Treatment modality | 1.19 (-0.19, 2.57) | 90.4 | <0.001 |
| Psychosocial related factors | |||
| Socials support | 1.31 (0.72, 1.89) | 86.5 | <0.001 |
| Self-efficacy | 3.09 (1.70, 4.48) | 0.0 | 0.845 |
*Significanty associated; DSME: Diabetes Self-Management Education.
Access to DM education and glucometer
The pooled effect of five primary studies [29,50,54,57] on diabetes self-management education revealed the association with non-adherence to self-care practice. People with DM who did not access diabetes self-management education had higher odds of non-adherence to self-care practice (POR: 2.76; 95% CI: 1.7–3.55, I2 = 0.0%). Four [29,54,57,62] primary studies were examined the association between access to private glucometer and non-adherence to self-care practice. After pooling four primary studies, participants who had no private glucometer at home had higher odds of non-adherence to self-care practice (POR: 2.71; 95% CI: 1.46–3.95, I2 = 0.0%). Eight primary studies [29,48,51,54,56,57,62] reported a relationship between knowledge towards diabetes and non-adherence to self-care practice. However, the pooled result showed no significant relationship between knowledge towards diabetes and non-adherence to self-care practice (POR: 1.48; 95% CI: 0.79–2.17, I2 = 77.3) (Table 4).
Clinical factors
Studies investigated the association between clinical variables and non-adherence to self-care practice. These clinical factors are co-morbidity (AOR: 1.68; 1.07–2.56) [51], medication burden (AOR: 2.87; 1.43–5.76) [55], uncontrolled plasma glucose level (AOR: 1.68; 1.02–2.79) [27], the level of medication adherence (AOR: 0.4; 95%CI: 0.30–0.80), and alcohol consumption (AOR: 4.6; 95%CI: 1.30–15.7) [47]. The pooled effect of four [45,46,48,52] primary studies found that people who lived a shorter time with DM were more than three times more likely to have non-adherence to self-care practice than people who lived a long time with DM (POR: 3.69; 95% CI: 1.86–5.52, I2 = 0.0%).
The pooled result of four [27,31,52,53] observational studies found that people who had one or more DM complication were more likely to non-adherence to self-care practice than those who did not have a DM complication (AOR: 2.22; 95% CI: 1.48–2.95, I2 = 0.0%). The pooled effect of two primary studies found that people who did not satisfy with medical care were more likely non-adherence to self-care practice than people who had medical care satisfied (POR: 1.8; 95% CI: 1.15–2.44, I2 = 0.0%). Treatment modality did not affect non-adherence to self-care practice across two different observational studies [51,53] (POR: 1.19; 95% CI: -0.19–2.57, I2 = 90.4%) (Table 4).
Psycho-social factors
Eight observational studies [29,31,50,55–57,81,82] were investigated on the association between psychosocial variables and non-adherence to self-care practice. People who had moderate perceived barriers towards self-care practice were 70% more likely non-adherence to self-care practice than people who had less perceived barriers towards self-care practice (AOR: 0.3; 95% CI: 0.12–0.64) [57]. People with DM who did not perceive the severity of diabetes and its complications were twelve times more non-adhere to self-care practice than highly perceived ones (AOR: 12.3; 95% CI: 1.19–13.25) [57]. People with DM who had an unfavorable attitude toward perceived benefit (AOR: 5.94; 1.87–17.94) and perceived barrier (AOR: 0.47; 0.27–0.39) were most likely to non-adherence to self-care practice than favorable attitude toward the perceived benefit and perceived barrier [29] respectively.
Seven primary studies [50,55,56,81–84] investigated the relationship between social support and non-adherence to self-care practice. Pooled results showed that social support did not affect non-adherence to self-care practice (POR: 1.31; 95% CI: 0.72–1.89, I2 = 86.5%). Two observational studies [62,82] examined the association between self-efficacy of self-care practice and non-adherence to self-care practice. After pooling the two studies’ result, people with diabetes who had poor self-efficacy towards self-care practice were more likely to self-care non-adherence than those who had good self-efficacy (POR: 3.09; 95% CI: 1.70–4.48, I2 = 0.0%) (Table 4).
Discussion
To the best of our review, this is the first systemic review and meta-analysis study that conducted to show the pooled proportion of non-adherence and factors associated with non-adherence to self-care practice in Ethiopian adults with diabetes.
This study identified that many people with diabetes (49.91%) in Ethiopia fail to adhere to self-care practices as recommended or agreed between people with diabetes and healthcare providers. This is supported by a systemic review in sub-Saharan Africa (49%), which is of poor quality of life and a serious threat to the health of people, and the health system capacity [85].
This is because chronic care health systems in sub-Saharan Africa have significantly developed in the last decade, the capacity for managing diabetes remains in its infancy, including in Ethiopia [86]. In addition to this, the international community is certainly aware of sub-Saharan Africa problems caused by malnutrition and HIV and other infectious diseases, awareness of the increasing burden of chronic non-communicable diseases including diabetes is still low. This turns into a vital part of self-care behaviors, health beliefs, attitudes toward diabetes, and self-efficacy underutilized in developing countries, including Ethiopia [87,88].
This finding was higher than a study in Bangladesh (28.2%) (28.2%) [89] and much lower than the study reported in Australia (85.5%) [90], Oman (73%) [91], and Iran (65.15%) [92]. Health care facility access, prevent the incidence and prevalence of type 2 diabetes, prevention, and control of diabetes have proven successful at identifying high-risk people, particularly in rural and remote-access areas, and screen and increase awareness of people about diabetes on special days, and places. These could be the reasons for the difference. Another issue related to the healthcare system is a tremendous mismatch between supply and demand in Ethiopia. This is because of the unavailability of the system for the continuity of DM care. For instance, inadequate knowledge and skills of health workers, frequent stock-outs of DM supplies, and people with diabetes inability to pay for DM related medical service [93].
In Oman, diabetes care focuses on community resources, well-designed health system organization of diabetes health care, self-management support, delivery system design, decision support, and clinical information systems. The execution of these types of the system by healthcare authorities in Oman is a key element in the success of diabetes care [94]. Whereas in Iran, the healthcare system is the referral feedback loop from academic specialized centers back to the lowest levels of healthcare facility helped support the continuum of care for people with pre-diabetes and diabetes that is a primary level (diabetes unit) to secondary level (diabetes center) to tertiary level (specialized care) and vice-versa [95].
When to see the Australian diabetes care, the Australian National Diabetes Strategy 2016–2020 sets different goals to prevent and control diabetes. Some of these are preventing people from developing type 2 diabetes, promoting awareness and earlier detection of type 1 and type 2 diabetes, reducing the occurrence of diabetes-related complications and improving quality of life among people with diabetes, and strengthen prevention and care through research, evidence, and well-organized database [96]. Diabetes care in Bangladesh was seeking pharmaceutical therapy and dependence on health professional care rather than self-management. That is why diabetes significantly increases healthcare use and expenditure and is likely to impose a huge economic burden on the healthcare systems in Bangladesh [97,98].
Non-adherence to recognized standards of care is the principal cause of the development of complications of diabetes and associated people, societies, and economic costs [99]. Non-adherence to diabetes self-care could lead to short-term complications and uncontrolled diabetes [100] which results in avoidable suffering for people with diabetes and excess cost to the healthcare systems too [101,102]. Uncontrolled diabetes increases susceptibility to infection and worsens outcomes for some of the world’s major infectious diseases including tuberculosis and Melioidosis [103].
This study indicated that socio-demographic related characters (age, sex, family history, and income), overall health beliefs, clinically related characters (treatment modality, complications, and satisfaction with medical care), self-efficacy, social support, and diabetes self-management education about diabetes were factors consistently reported in the literature associated with diabetes self-care practice.
Sex is one of the potential factors for non-adherence to self-care practice. Males with diabetes were non-adhered to self-care practice more than women. This supported by a qualitative study in Pakistan [104], Mexico [105], and Indonesia [106]. This is due to women being more adaptable to diabetes conditions, disclosing their diabetes more readily, and being a lot more ready to integrate management into their daily lives. They also used socially interactive resources such as internet access and education classes, because men relied more on self-directed learning, more reluctant to tell friends and family about their diabetes due to the stigma attached to the disease, and were less observant of self-management practices in social settings [107].
In this study, the educational level is a potential reason. Those people with diabetes who have low levels of literacy had more likely to self-care non-adherence behaviors. A previous systemic review with a meta-analysis study done in China suggested that participants with a higher educational level were linked to better diabetes self-care practice [108]. Being higher education levels could lead to having better judgment and decision-making ability for adhering to self-care behaviors [92].
Diabetes Self-Management Education (DSME) associated with self-care practice. In line with earlier studies [85,92,109,110], people with diabetes who had no access to diabetes self-management education were associated with non-adherence to self-care practice. Not access to diabetes self-management education associated with inadequate diabetes self-care practice [111]. Diabetes self-management education plays an important role in self-care for all people with diabetes and is necessary to improve patient outcomes [112]. It has also facilitated the knowledge, skill, and ability necessary for diabetes self-care practices. This is having a positive impact on people with diabetes access, use, and outcomes [113].
National standards for DSME and support recommended that all people with diabetes should take part in diabetes self-management education to ease the knowledge, skills, and ability necessary for diabetes self-care and in diabetes self-management support to help with implementing and sustaining skills and behaviors needed for ongoing self-management [114]. Given the impact of DSME in developing countries, it has positive effects on knowledge, glycemic control, and behavioral outcomes on short-term follow-up. DSME on people with diabetes’ self-care practice can reduce complications like arterial stiffness, improve quality of life, and improve their self-care behaviors [115,116].
We found that the proportion of non-adherence to self-care practice is more pronounced among people with diabetes who did not have glucometer access at their home. This estimation is precise as a confidence interval ranged from 1.70 (almost double effect on the odds of non-adherence to self-care practice) to 3.55 (almost four times the effect). This supported by a systemic review was done in Sub-Saharan Africa [85] and a qualitative study done in Ghana [117]. This may have a serious financial implication (the high cost of blood glucose meter and reagent strips) and supplies (no access to blood glucometer) [118].
Self-monitoring of blood glucose is an important practice for people with diabetes. Self-monitoring of blood glucose systems has the potential to play an important role in the management of diabetes and in the reduction of risks of serious clinical complications. Therefore, effective balanced costs of blood glucose meter and reagent strips are required to support and potentially cost-saving for people with diabetes. It is also promoted easy access to glucometer and reagents which are offered free of charge to people with diabetes to increase self-care adherence [118–120].
People with diabetes living for with shorter time with diabetes are almost quadrupled prone to non-adherence to self-care practice than people with diabetes living for a long time. The experience of living with diabetes can take significant sounds on the well-being of people in terms of the success of survival skills with the disease living a long duration. Individuals with diabetes who have lived a long time with diabetes realize, master the basic skills and information, acquire in-depth and advanced diabetes knowledge throughout their lifetime, both formally through programs of continuing education and informally through experience and sharing of information with other people with diabetes. Individuals with positive coping strategies such as confrontation tend to more proactive in learning to manage their disease.
In contrast, newly diagnosed and/or short-live with diabetes is challenged to master the basic skills and information and take time to acquire in-depth and advanced diabetes knowledge. The new diagnosis of people with diabetes may have negative coping strategies such as avoidance or acceptance-resignation. They may not be willing to follow management recommendations. Therefore, diabetes educators should focus on helping newly diagnosed people with diabetes to develop positive coping strategies to adhere to self-care practices [108,121].
We found that participants who had one or more DM complications were more often non-adherence to self-care practice than those who did not have DM complications. This finding is not in line with the previous study done in China [108]. This difference is due to the difference between health service access (multi-discipline approach in China’s health service use modern and traditional approach), different study populations (type 2), and different sociocultural characteristics of participants.
We found that participants who did not satisfied with their medical care was more likely non-adherence to self-care practice than their counterparts. In line with earlier studies, dissatisfaction with medical care restricted self-care activities in developing countries including Ethiopia [122]. This is due to the barrier of medical care satisfaction is a part of the provider’s perspective (belief by providers that recommended self-care practice cannot cure/help clients, no confidence in their own ability to alert client behaviors and inadequate training in standard diabetes car), client factors (attitude, belief, knowledge about diabetes, frustration due to dynamic and chronic nature of diabetes, financial resources and co-morbidity) and clinical environment (health facility readiness, management systems for service and unequal distribution of health providers between different health facilities) [117,123–125].
Therefore, interventions to improve adherence to diabetes self-care should focus on helping people with diabetes develop a favorable attitude and how to overcome behavioral control barriers. In addition to this, improving access to standard diabetic care, basic technologies, and competence of health workers can improve the care process leading to better outcomes.
People with diabetes who had poor self-efficacy towards self-care practice were to have non-adherence to self-care practice than those who had good self-efficacy. This was supported by the previous study [108], there was a consistently strong association between poor self-efficacy level and non-adherence to self-care practice in people with diabetes. This implies that the highest resistance to diabetes self-care practice, the less confidence the people with diabetes are in their ability to adhere to self-care practice recommendations. Therefore, the clinical implication is that self-efficacy in people with diabetes the first step in the development of people’s tailored adherence to self-care practice.
Strength and limitations
This systematic review and meta-analysis have several strengths. It is the first study that pooled the results of several studies in the country giving stronger evidence of different factors that restrict self-care practice among people with diabetes. It was able to include a relatively large number of people with diabetes (N = 7,134), which is much more than sample sizes of each study. Also tried to find many factors that hinder the recommended self-care practice in people with diabetes.
Despite its strengths, the study also has a few limitations. Even though most of the studies had good quality, all of the primary studies were cross-sectional, which is limited in this study. In addition, although extensive and diverse search strategies were used to find all possible available literature, some grey literature, such as conference proceedings, was still difficult to find. Furthermore, the study was not able to conduct a subgroup analysis based on the different domains of self-care practice which would have given important information to find a potential target to improve self-care practice.
Implication
This study has many implications for clinical practice and future research. Firstly, the health care provider (especially physicians and nurses) can develop effective strategies to improve certain diabetes self-care practice behaviors that people with DM exhibit, such as non-adherence to self-care practice. Secondly, identifying and understanding factors that restrict diabetes self-care practice is the first step in developing evidence-based interventions to promote short and long-term health outcomes and quality of life. Future research should focus on developing and testing a conceptual model that can use to enhance diabetes self-care practice in a national context. Finally, to give a long-term reduction in diabetes-related co-morbidity and mortality, researches should assess ways to extend and sustain diabetes self-care practice among this population.
Conclusions
This meta-analysis revealed that a high proportion of people with diabetes failed to adhere to self-care practices. Socio-demographic related characters (age, sex, family history, income level, and residency), overall health beliefs, clinically related characters (treatment modality, complications, satisfaction with medical care and knowledge towards diabetes disease), self-efficacy, social support, and diabetes self-management education was hinder factors consistently reported in the literature with diabetes self-care practice.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(PDF)
(PDF)
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
No specific funding for this work.
References
- 1.Organization WH. World Health Statistics 2018: monitoring health for the SDGs sustainable development goals. Geneva: World Health Organization, 2018. [Google Scholar]
- 2.Organization WH. World health statistics 2018: Monitoring health for the SDGs (sustainable development goals). Geneva: World Health Organization; 2018. [Google Scholar]
- 3.ADA Diabetes JC. Standards of medical care in diabetes—2019 abridged for primary care providers. 2019;37(1):11–34. 10.2337/cd18-0105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Organization WWH. Global report on diabetes. 2016.
- 5.Gouda HN, Charlson F, Sorsdahl K, Ahmadzada S, Ferrari AJ, Erskine H, et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990–2017: results from the Global Burden of Disease Study 2017. 2019;7(10):e1375–e87. [DOI] [PubMed] [Google Scholar]
- 6.Cho N, Shaw J, Karuranga S, Huang Y, da Rocha Fernandes J, Ohlrogge A, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. 2018;138:271–81. [DOI] [PubMed] [Google Scholar]
- 7.Federation ID. IDF Diabetes Atlas 8th Edition (2017). 2017.
- 8.Pastakia SD, Pekny CR, Manyara SM, Fischer L JD, metabolic syndrome, targets o, therapy. Diabetes in sub-Saharan Africa–from policy to practice to progress: targeting the existing gaps for future care for diabetes. 2017;10:247 10.2147/DMSO.S126314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunachie S, Chamnan P JToTRSoTM, Hygiene. The double burden of diabetes and global infection in low and middle-income countries. 2018;113(2):56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herman WH. The global burden of diabetes: an overview Diabetes mellitus in developing countries and underserved communities: Springer; 2017. p. 1–5. [Google Scholar]
- 11.Bommer C, Sagalova V, Heesemann E, Manne-Goehler J, Atun R, Bärnighausen T, et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. 2018;41(5):963–70. [DOI] [PubMed] [Google Scholar]
- 12.Atun R, Davies J, Gale E, Barnighausen T, Beran D, Kengne AJ, Tssbtepodis SA, et al. Diabetes in sub-Saharan Africa: from clinical care to health policy. Lancet Diabetes Endocrinol. 2017; 5 (8): 622–67. 10.1016/S2213-8587(17)30181-X [DOI] [PubMed] [Google Scholar]
- 13.Moucheraud C, Lenz C, Latkovic M, Wirtz V JJBgh. The costs of diabetes treatment in low-and middle-income countries: a systematic review. 2019;4(1):e001258 10.1136/bmjgh-2018-001258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirigia JM, Sambo HB, Sambo LG, Barry SP JBih, rights h. Economic burden of diabetes mellitus in the WHO African region. 2009;9(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ovbiagele BJ Jotns. Tackling the growing diabetes burden in Sub-Saharan Africa: a framework for enhancing outcomes in stroke patients. 2015;348(1–2):136–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Organization WH. Adherence to long-term therapies: evidence for action. 2003.
- 17.Chaudri NA. Adherence to Long-term Therapies Evidence for Action. King Faisal Specialist Hospital & Research Centre; 2004.
- 18.Hartweg D. Dorothea Orem: Self-care deficit theory: Sage publications; 1991. [Google Scholar]
- 19.Smith MC, Parker ME. Nursing theories and nursing practice: FA Davis; 2015. [Google Scholar]
- 20.Bosworth H. Improving patient treatment adherence: A clinician’s guide: Springer; 2010. [Google Scholar]
- 21.Glasgow RE, Strycker LA. Preventive care practices for diabetes management in two primary care samples. American journal of preventive medicine. 2000;19(1):9–14. 10.1016/s0749-3797(00)00157-4 [DOI] [PubMed] [Google Scholar]
- 22.Austin M. Importance of self-care behaviors in diabetes management: business briefing. US Endocrine Review 2005. 2005:16–21. [Google Scholar]
- 23.Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes research and clinical practice. 2011;93(1):1–9. 10.1016/j.diabres.2011.02.002 [DOI] [PubMed] [Google Scholar]
- 24.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. Journal of diabetes & Metabolic disorders. 2013;12(1):14 10.1186/2251-6581-12-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feleke Y, Enquselassie F. An assessment of the health care system for diabetes in Addis Ababa, Ethiopia. Ethiopian journal of health development. 2005;19(3):203–10. [Google Scholar]
- 26.Alemu S, Watkins V, Dodds W, Turowska J, Watkins P. Access to diabetes treatment in northern Ethiopia. Diabetic medicine. 1998;15(9):791–4. [DOI] [PubMed] [Google Scholar]
- 27.Ayele BH, Mengesha MM, Tesfa T. Predictors of self-care activities of outpatient diabetic residents in Harar and Dire Dawa: A hospital-based cross-sectional study. SAGE Open Med. 2019;7:2050312119865646 10.1177/2050312119865646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abate TW, Tareke M, Tirfie M. Self-care practices and associated factors among diabetes patients attending the outpatient department in Bahir Dar, Northwest Ethiopia. BMC Res Notes. 2018;11(1):800 10.1186/s13104-018-3874-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mariye T, Tasew H, Teklay G, Gerensea H, Daba W. Magnitude of diabetes self-care practice and associated factors among type two adult diabetic patients following at public Hospitals in central zone, Tigray Region, Ethiopia, 2017. BMC Res Notes. 2018;11(1):380 10.1186/s13104-018-3489-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sorato MM, Tesfahun C, Lamessa DJ JDM. Levels and predictors of adherence to self-care behaviour among adult type 2 diabetics at Arba Minch general hospital, Southern Ethiopia. 2016;7(6):11. [Google Scholar]
- 31.Aschalew AY, Yitayal M, Minyihun A, Bisetegn TA. Self-care practice and associated factors among patients with diabetes mellitus on follow up at University of Gondar Referral Hospital, Gondar, Northwest Ethiopia. BMC Res Notes. 2019;12(1):591 10.1186/s13104-019-4630-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ketema DB, Leshargie CT, Kibret GD, Assemie MA, Alamneh AA, Kassa GM, et al. Level of self-care practice among diabetic patients in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):1–12. 10.1186/s12889-020-8425-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG JAoim. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. 2009;151(4):264–9. [DOI] [PubMed] [Google Scholar]
- 34.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj. 2015;349 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 35.Rajasekhar A, Lottenberg R, Lottenberg L, Liu H, Ang D. Pulmonary embolism prophylaxis with inferior vena cava filters in trauma patients: a systematic review using the meta-analysis of observational studies in epidemiology (MOOSE) guidelines. Journal of thrombosis and thrombolysis. 2011;32(1):40–6. 10.1007/s11239-010-0544-7 [DOI] [PubMed] [Google Scholar]
- 36.Stang A JEjoe. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. 2010;25(9):603–5. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 37.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. Journal of clinical epidemiology. 2012;65(9):934–9. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 38.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142 10.1002/14651858.ED000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychological methods. 2006;11(2):193 10.1037/1082-989X.11.2.193 [DOI] [PubMed] [Google Scholar]
- 41.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed‐effect and random‐effects models for meta‐analysis. Research synthesis methods. 2010;1(2):97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 42.Thompson SG, Higgins JP. How should meta‐regression analyses be undertaken and interpreted? Statistics in medicine. 2002;21(11):1559–73. 10.1002/sim.1187 [DOI] [PubMed] [Google Scholar]
- 43.G R-G. Detecting publication bias in random effects meta-analysis: An empirical comparison of statistical methods. 2006.
- 44.Bonger Z, Shiferaw S, Tariku EZ. Adherence to diabetic self-care practices and its associated factors among patients with type 2 diabetes in Addis Ababa, Ethiopia. Patient Prefer Adherence. 2018;12:963–70. 10.2147/PPA.S156043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dedefo MG, Ejeta BM, Wakjira GB, Mekonen GF, Labata BG. Self-care practices regarding diabetes among diabetic patients in West Ethiopia. BMC Res Notes. 2019;12(1):212 10.1186/s13104-019-4258-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gurmu Y, Gela D, Aga F. Factors associated with self-care practice among adult diabetes patients in West Shoa Zone, Oromia Regional State, Ethiopia. BMC Health Serv Res. 2018;18(1):732 10.1186/s12913-018-3448-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kassahun T, Gesesew H, Mwanri L, Eshetie T. Diabetes related knowledge, self-care behaviours and adherence to medications among diabetic patients in Southwest Ethiopia: a cross-sectional survey. BMC Endocr Disord. 2016;16(1):28 10.1186/s12902-016-0114-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Amente T, Belachew T, Hailu E, Berhanu N JWJMMS. Self care practice and its predictors among adults with diabetes mellitus on follow up at Nekemte hospital diabetic clinic, West Ethiopia. 2014;2(3):1–16. [Google Scholar]
- 49.Tadesse E, Adem AM, Gelaw BK, Ahmed M, Se MF JGJoMR. Assessment of knowledge, attitude and practices regarding life style modification among type 2Diabetic mellitus patients attending Adama hospital Medical college, Oromia region, Ethiopia. 2015. [Google Scholar]
- 50.Mamo M, Demissie MJ JDCM. Self care practice and its associated factors among diabetic patients in addisababa public hospitals, cross sectional study. 2016;1(1):2–5. [Google Scholar]
- 51.Hagströmer M, Troiano RP, Sjöström M, Berrigan D. Levels and patterns of objectively assessed physical activity—a comparison between Sweden and the United States. American journal of epidemiology. 2010;171(10):1055–64. 10.1093/aje/kwq069 [DOI] [PubMed] [Google Scholar]
- 52.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obesity reviews. 2012;13(8):659–80. 10.1111/j.1467-789X.2011.00982.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Berhe KK, Kahsay BA G JGJMS. Adherence to diabetes self-management practices among Type II diabetic patients in Ethiopia: A Cross Sectional Study. 2013;3(6):211–21. [Google Scholar]
- 54.Tiruneh SA, Ayele AA, Emiru YK, Tegegn HG, Ayele BA, Engidaw MT, et al. Factors influencing diabetes self-care practice among type 2 diabetes patients attending diabetic care follow up at an Ethiopian General Hospital, 2018. J Diabetes Metab Disord. 2019;18(1):199–206. 10.1007/s40200-019-00408-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abate TW, Tareke M, Tirfie M JBrn. Self-care practices and associated factors among diabetes patients attending the outpatient department in Bahir Dar, Northwest Ethiopia. 2018;11(1):800 10.1186/s13104-018-3874-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alemayhu T, Geda B, Mihret AG. Self-Care Practices and Associated Factors among Adult Diabetic Patients in Public Hospitals of Dire Dawa Administration, Eastern Ethiopia: Haramaya University; 2018. [DOI] [PMC free article] [PubMed]
- 57.Ayele K, Tesfa B, Abebe L, Tilahun T, Girma E JPo. Self care behavior among patients with diabetes in Harari, Eastern Ethiopia: the health belief model perspective. 2012;7(4):e35515 10.1371/journal.pone.0035515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Niguse H, Belay G, Fisseha G, Desale T, Gebremedhn G. Self-care related knowledge, attitude, practice and associated factors among patients with diabetes in Ayder Comprehensive Specialized Hospital, North Ethiopia. BMC Res Notes. 2019;12(1):34 10.1186/s13104-019-4072-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Berhe KK, Gebru HB, Kahsay HB, Kahsay AA JGJoMR. Assessment of Self Care Management and its Associated Factors among Type 2 Diabetes Patients in Mekelle Hospital and Ayder Referral Hospitals, Mekelle City, Tigray, Northern Ethiopia, 2012/13. 2017. [Google Scholar]
- 60.Addisu Y, Eshete A, Hailu EJ JMS. Assessment of diabetic patient perception on diabetic disease and self-care practice in Dilla University Referral Hospital, South Ethiopia. 2014;3(166):2167–0943.1000166. [Google Scholar]
- 61.Sorato M M, C T. Levels and Predictors of Adherence to Self-care Behaviour among Adult Type 2 Diabetics at Arba Minch General Hospital, Southern Ethiopia. Journal of Diabetes & Metabolism. 2016;7(6). [Google Scholar]
- 62.Chali SW, Salih MH, Abate AT. Self-care practice and associated factors among Diabetes Mellitus patients on follow up in Benishangul Gumuz Regional State Public Hospitals, Western Ethiopia: a cross-sectional study. BMC Res Notes. 2018;11(1):833 10.1186/s13104-018-3939-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chali SW, Salih MH, Abate AT. Self-care practice and associated factors among Diabetes Mellitus patients on follow up in Benishangul Gumuz Regional State Public Hospitals, Western Ethiopia: a cross-sectional study. BMC research notes. 2018;11(1):833 10.1186/s13104-018-3939-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ayele BH, Mengesha MM, Tesfa T. Predictors of self-care activities of outpatient diabetic residents in Harar and Dire Dawa: A hospital-based cross-sectional study. SAGE open medicine. 2019;7:2050312119865646 10.1177/2050312119865646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Berhe KK, Kahsay AB, Gebru HB. Adherence to diabetes Self-management practices among type II diabetic patients in Ethiopia; a cross sectional study. Green J Med Sci. 2013;3(6):211–21. [Google Scholar]
- 66.Mamo M, Demissie M. Self Care Practice and Its Associated Factors Among Diabetic Patients In Addis Ababa Public Hospitals, Cross Sectional Study. Journal of Diabetes and Cholesterol Metabolism. 2016;1(1):101. [Google Scholar]
- 67.Kassahun T, Gesesew H, Mwanri L, Eshetie T. Diabetes related knowledge, self-care behaviours and adherence to medications among diabetic patients in Southwest Ethiopia: a cross-sectional survey. BMC Endocrine Disorders. 2016;16(1):28 10.1186/s12902-016-0114-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tadesse E, Adem AM, Gelaw BK, Ahmed M, Se MF. Assessment of knowledge, attitude and practices regarding life style modification among type 2Diabetic mellitus patients attending Adama hospital Medical college, Oromia region, Ethiopia. Global Journal of Medical Research. 2014;14(7):14. [Google Scholar]
- 69.Mariye T, Tasew H, Teklay G, Gerensea H, Daba W. Magnitude of diabetes self-care practice and associated factors among type two adult diabetic patients following at public Hospitals in central zone, Tigray Region, Ethiopia, 2017. BMC research notes. 2018;11(1):380 10.1186/s13104-018-3489-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Getie Mihret A, Alemayhu T, Geda B. Self-Care Practices and Associated Factors among Adult Diabetic Patients in Public Hospitals of Dire Dawa Administration, Eastern Ethiopia [MSc thesis]: Haramaya University; 2018. [DOI] [PMC free article] [PubMed]
- 71.Berhe KK, Gebru HB, Kahsay HB, Kahsay AA. Assessment of Self Care Management and its Associated Factors among Type 2 Diabetes Patients in Mekelle Hospital and Ayder Referral Hospitals, Mekelle City, Tigray, Northern Ethiopia, 2012/13. Global Journal of Medical Research. 2017. [Google Scholar]
- 72.Amente T, Belachew T, Hailu E, Berhanu N. Self care practice and its predictors among adults with diabetes mellitus on follow up at Nekemte hospital diabetic clinic, West Ethiopia. World J Med Med Sci. 2014;2(3):1–16. [Google Scholar]
- 73.Gurmu Y, Gela D, Aga F. Factors associated with self-care practice among adult diabetes patients in West Shoa Zone, Oromia Regional State, Ethiopia. BMC health services research. 2018;18(1):732 10.1186/s12913-018-3448-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ayele K, Bisrat Tesfa LA, Tilahun T, Girma E. Self care behavior among patients with diabetes in Harari, Eastern Ethiopia: the health belief model perspective. PloS one. 2012;7(4). 10.1371/journal.pone.0035515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lemessa F. Assessment of Self-care Practices and Associated Factors among Type 2 Diabetic Patients at Tikur Anbessa Specialized Hospital Addis Ababa, Ethiopia [MSc Thesis]: Addis Ababa University; 2014.
- 76.Addisu Y, Eshete A, Hailu E. Assessment of diabetic patient perception on diabetic disease and self-care practice in Dilla University Referral Hospital, South Ethiopia. J Metabolic Synd. 2014;3(166):2167–0943.1000166. [Google Scholar]
- 77.Sorato MM, Tesfahun C, Lamessa D. Levels and predictors of adherence to self-care behaviour among adult type 2 diabetics at Arba Minch general hospital, Southern Ethiopia. J Diabetes Metab. 2016;7(6):11. [Google Scholar]
- 78.Mamo M, Demissie M. Self Care Practice and Its Associated Factors Among Diabetic Patients In Addisababa Public Hospitals, Cross Sectional Study. Diabetes Cholest metabol 1: 101. Diabetes Cholest Metabol. 2016;1(1):2–5. [Google Scholar]
- 79.Niguse H, Belay G, Fisseha G, Desale T, Gebremedhn G. Self-care related knowledge, attitude, practice and associated factors among patients with diabetes in Ayder Comprehensive Specialized Hospital, North Ethiopia. BMC research notes. 2019;12(1):34 10.1186/s13104-019-4072-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tassew B. Assessment of Diabetes Self-Care Practice and its Associated Factors among Patient on Follow up At Public and Private Primary Level Health Care in Addis Ababa, Ethiopia [Thesis]: Addis Ababa; 2015.
- 81.Chali SW, Salih MH, Abate AT JBrn. Self-care practice and associated factors among Diabetes Mellitus patients on follow up in Benishangul Gumuz Regional State Public Hospitals, Western Ethiopia: a cross-sectional study. 2018;11(1):833 10.1186/s13104-018-3939-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gurmu Y, Gela D, Aga FJ Bhsr. Factors associated with self-care practice among adult diabetes patients in West Shoa Zone, Oromia Regional State, Ethiopia. 2018;18(1):732 10.1186/s12913-018-3448-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Aschalew AY, Yitayal M, Minyihun A, Bisetegn TA JBrn. Self-care practice and associated factors among patients with diabetes mellitus on follow up at University of Gondar Referral Hospital, Gondar, Northwest Ethiopia. 2019;12(1):1–6. 10.1186/s13104-019-4630-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tiruneh SA A A, Emiru YK, Tegegn HG, Ayele BA, Engidaw MT, Gebremariam AD. Factors influencing diabetes self-care practice among type 2 diabetes patients attending diabetic care follow up at an Ethiopian General Hospital,2018 J Diabetes Metab Disord. 2019;18(1):199–206. 10.1007/s40200-019-00408-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Stephani V, Opoku D, Beran D. Self-management of diabetes in Sub-Saharan Africa: a systematic review. BMC public health. 2018;18(1):1148 10.1186/s12889-018-6050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nuche-Berenguer B, Kupfer LE. Readiness of sub-Saharan Africa healthcare systems for the new pandemic, diabetes: a systematic review. Journal of diabetes research. 2018;2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Levitt NS. Diabetes in Africa: epidemiology, management and healthcare challenges. Heart. 2008;94(11):1376–82. 10.1136/hrt.2008.147306 [DOI] [PubMed] [Google Scholar]
- 88.Motala AA, Omar MA, Pirie FJ. Epidemiology of diabetes in Africa The epidemiology of diabetes mellitus (2nd edn) Chichester: Wiley; 2008:133–46. [Google Scholar]
- 89.Saleh F, Mumu SJ, Ara F, Hafez MA, Ali L. Non-adherence to self-care practices & medication and health related quality of life among patients with type 2 diabetes: a cross-sectional study. BMC public health. 2014;14:431 10.1186/1471-2458-14-431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Al-Amer R, Ramjan L, Glew P, Randall S, Salamonson Y. Self-efficacy, depression, and self-care activities in adult Jordanians with type 2 diabetes: the role of illness perception. Issues in mental health nursing. 2016;37(10):744–55. 10.1080/01612840.2016.1208692 [DOI] [PubMed] [Google Scholar]
- 91.D’Souza MS, Karkada SN, Venkatesaperumal R, Natarajan J. Self-care behaviours and glycemic control among adults with type 2 diabetes. GSTF J Nurs Health Care. 2015;2(1). [Google Scholar]
- 92.RobatSarpooshi D, Mahdizadeh M, Siuki HA, Haddadi M, Robatsarpooshi H, Peyman N. The Relationship Between Health Literacy Level and Self-Care Behaviors in Patients with Diabetes. Patient Related Outcome Measures. 2020;11:129–35. 10.2147/PROM.S243678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Workneh MH, Bjune GA, Yimer SA. Assessment of health system challenges and opportunities for possible integration of diabetes mellitus and tuberculosis services in South-Eastern Amhara Region, Ethiopia: a qualitative study. BMC health services research. 2016;16(1):1–11. 10.1186/s12913-016-1378-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Alyaarubi S. Diabetes care in Oman: obstacles and solutions. Sultan Qaboos university medical journal. 2011;11(3):343 [PMC free article] [PubMed] [Google Scholar]
- 95.Noshad S, Afarideh M, Heidari B, Mechanick JI, Esteghamati A. Diabetes care in Iran: where we stand and where we are headed. Annals of global health. 2015;81(6):839–50. 10.1016/j.aogh.2015.10.003 [DOI] [PubMed] [Google Scholar]
- 96.Health AGDo. Australian National Diabetes Strategy 2016‐2020. Commonwealth of Australia Canberra; 2015.
- 97.Islam SMS, Lechner A, Ferrari U, Laxy M, Seissler J, Brown J, et al. Healthcare use and expenditure for diabetes in Bangladesh. BMJ global health. 2017;2(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Islam SS. Healthcare Use and Expenditure for Diabetes In Bangladesh: A Matched-Case-Control Study. Value in Health. 2015;18(7):A619. [Google Scholar]
- 99.Sabaté E, Sabaté E. Adherence to long-term therapies: evidence for action: World Health Organization; 2003. 211 p.
- 100.Ahern MM, Hendryx M. Avoidable hospitalizations for diabetes: comorbidity risks. Disease Management. 2007;10(6):347–55. 10.1089/dis.2007.106709 [DOI] [PubMed] [Google Scholar]
- 101.Rubens M, Saxena A, Ramamoorthy V, Khera R, Hong J, Veledar E, et al. Trends in diabetes-related preventable hospitalizations in the US, 2005–2014. Diabetes Care. 2018;41(5):e72–e3. 10.2337/dc17-1942 [DOI] [PubMed] [Google Scholar]
- 102.Kirigia JM, Sambo HB, Sambo LG, Barry SP. Economic burden of diabetes mellitus in the WHO African region. BMC international health and human rights. 2009;9(1):6 10.1186/1472-698X-9-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dunachie S, Chamnan P. The double burden of diabetes and global infection in low and middle-income countries. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2019;113(2):56–64. 10.1093/trstmh/try124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ansari RM, Hosseinzadeh H, Harris M, Zwar N. Self-management experiences among middle-aged population of rural area of Pakistan with type 2 diabetes: a qualitative analysis. Clinical Epidemiology and Global Health. 2019;7(2):177–83. [Google Scholar]
- 105.Whittemore R, Vilar-Compte M, De La Cerda S, Marron D, Conover R, Delvy R, et al. Challenges to diabetes self-management for adults with type 2 diabetes in low-resource settings in Mexico City: a qualitative descriptive study. International journal for equity in health. 2019;18(1):133 10.1186/s12939-019-1035-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rahayu E, Kamaluddin R, Hapsari ED. Determinants of Diabetes Self Care in Patients With Type 2 Diabetes Mellitus in Banyumas Regency. Jurnal Keperawatan Soedirman. 2018;13(2):71–6. [Google Scholar]
- 107.Rustveld LO, Pavlik VN, Jibaja-Weiss ML, Kline KN, Gossey JT, Volk RJ. Adherence to diabetes self-care behaviors in English-and Spanish-speaking Hispanic men. Patient preference and adherence. 2009;3:123 10.2147/ppa.s5383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Luo X, Liu T, Yuan X, Ge S, Yang J, Li C, et al. Factors influencing self-management in Chinese adults with type 2 diabetes: a systematic review and meta-analysis. International journal of environmental research and public health. 2015;12(9):11304–27. 10.3390/ijerph120911304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Nagelkerk J, Reick K, Meengs L. Perceived barriers and effective strategies to diabetes self‐management. Journal of advanced nursing. 2006;54(2):151–8. 10.1111/j.1365-2648.2006.03799.x [DOI] [PubMed] [Google Scholar]
- 110.Fransen MP, von Wagner C, Essink-Bot M-L. Diabetes self-management in patients with low health literacy: ordering findings from literature in a health literacy framework. Patient education and counseling. 2012;88(1):44–53. 10.1016/j.pec.2011.11.015 [DOI] [PubMed] [Google Scholar]
- 111.Rafferty AP, Winterbauer NL, Luo H, Bell RA, Little NRG. Diabetes Self-Care and Clinical Care Among Adults With Low Health Literacy. Journal of public health management and practice: JPHMP. 2019. [DOI] [PubMed] [Google Scholar]
- 112.Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes care. 2008;31(Supplement 1):S97–S104. 10.2337/dc08-S097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National standards for diabetes self-management education and support. The Diabetes Educator. 2018;44(1):35–50. 10.1177/0145721718754797 [DOI] [PubMed] [Google Scholar]
- 114.Association AD. Lifestyle management: standards of medical care in diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S38–S50. [DOI] [PubMed] [Google Scholar]
- 115.Dube L, Van den Broucke S, Housiaux M, Dhoore W, Rendall-Mkosi K. Type 2 diabetes self-management education programs in high and low mortality developing countries: a systematic review. The Diabetes Educator. 2015;41(1):69–85. 10.1177/0145721714558305 [DOI] [PubMed] [Google Scholar]
- 116.Cicero AF F F, Tocci G, Ventura F, Presta V, Grandi E, et al. Awareness of major cardiovascular risk factors and its relationship with markers of vascular aging: Data from the Brisighella Heart Study. Nutrition, Metabolism and Cardiovascular Diseases. 2020. 10.1016/j.numecd.2020.03.005 [DOI] [PubMed] [Google Scholar]
- 117.Mogre V, Johnson NA, Tzelepis F, Paul C. Barriers to diabetes self-care: qualitative study of patients’ and health care providers’ perspective. Journal of clinical nursig. 2019;28 (11–12). [DOI] [PubMed] [Google Scholar]
- 118.Clarke S, Foster J. A history of blood glucose meters and their role in self-monitoring of diabetes mellitus. British journal of biomedical science. 2012;69(2):83–93. [PubMed] [Google Scholar]
- 119.Harris MI, Cowie CC, Howie LJ. Self-monitoring of blood glucose by adults with diabetes in the United States population. Diabetes care. 1993;16(8):1116–23. 10.2337/diacare.16.8.1116 [DOI] [PubMed] [Google Scholar]
- 120.Nyomba B, Berard L, Murphy L. Facilitating access to glucometer reagents increases blood glucose self‐monitoring frequency and improves glycaemic control: a prospective study in insulin‐treated diabetic patients. Diabetic Medicine. 2004;21(2):129–35. 10.1046/j.1464-5491.2003.01070.x [DOI] [PubMed] [Google Scholar]
- 121.Smeltzer SC, Bare BG, Hinkle JL, Cheever KH. Textbook of Medical-Surgical Nursing 12th ed. 2364 p.
- 122.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. Journal of diabetes and Metabolic disorders. 2013;12(1):14 10.1186/2251-6581-12-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Birabwa Catherine, Bwambale Mulekya F., Waiswa P Mayega RW. Quality and barriers of outpatient diabetes care in rural health facilities in Uganda—a mixed methods study. BMC Health Services Research. 2019;19(706):10 10.1186/s12913-019-4535-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Adu MD, Malabu UH, Aduli E. O. Malau-Aduli BSM-A. Enablers and barriers to effective diabetes self-management: A multi-national investigation. PLOS ONE. 2019;14(6s). 10.1371/journal.pone.0217771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nam S, Chesla C, Stotts NA, Kroon L, Sanson SL. Barriers to diabetes management: patient and provider factors. Diabetes research and clinical practice. 2011. July;93(1):1–9. 10.1016/j.diabres.2011.02.002 [DOI] [PubMed] [Google Scholar]