Abstract
Objectives:
How race/ethnic disparities in acute stroke care contribute to disparities in outcomes is not well-understood. We examined the relationship between acute stroke care measures with mortality within the first year and 30-day hospital readmission by race/ethnicity.
Materials and Methods:
The study included fee-for-service Medicare beneficiaries age ≥65 with ischemic stroke in 2010–2013 treated at 66 hospitals in the Florida Stroke Registry. Stroke care metrics included intravenous Alteplase treatment, in-hospital antithrombotic therapy, DVT prophylaxis, discharge antithrombotic therapy, anticoagulation therapy, statin use, and smoking cessation counseling. We used mixed logistic models to assess the associations between stroke care and mortality (in-hospital, 30-day, 6-month, 1-year post-stroke) and hospital readmission by race/ethnicity, adjusting for demographics, stroke severity, and vascular risk factors.
Results:
Among 14,100 ischemic stroke patients in the full study population (73% white, 11% Black, 15% Hispanic), mortality was 3% in-hospital, 12% at 30d, 21% at 6m, 26% at 1y, and 15% had a hospital readmission within 30 days. Patients who received antithrombotics early and at discharge had lower mortality at all time points, and the protective association for early antithrombotic use was strongest among whites. Eligible patients who received statin therapy at discharge had decreased 6m and 1y mortality, but specifically among minority groups. Statin therapy was associated with lower 30-day hospital readmission.
Conclusions:
Acute stroke care measures, particularly antithrombotic use and statin therapy, were associated with reduced odds of long-term mortality. The benefits of these acute care measures were less likely among Hispanic patients. Results underscore the importance of optimizing acute stroke care for all patients.
Keywords: Race, ethnicity, disparities, rehospitalization, stroke, mortality
Introduction
Racial/ ethnic disparities are recognized across all aspects of acute stroke care and underscored as an important research priority1–3. It has long been known that ischemic stroke has a disproportionate impact on clinical outcomes and stroke related mortality across different race/ethnic groups4. The variations in stroke outcomes are thought to be multifactorial and in part related to differences in risk factor prevalence, recognition, potency and premorbid treatment of vascular related disorders in combination with age, socioeconomic status and access to care amongst different race/ethnic groups5. Others have suggested differential effects of treatment amongst different race/ethnic groups with reduced safety and efficacy of reperfusion therapies reported among Black and Hispanic populations2,3,6.
In the Florida Stroke Registry (FSR), a voluntary stroke registry designed to elucidate disparities in stroke care, we have previously reported on race/ethnic differences in the receipt of key stroke care metrics. Temporal trends in Florida between 2010–2014, however, suggested improved performance on stroke metrics for all race/ethnic groups, with an increasing percentage of patients receiving overall optimal care, and narrowing of race/ethnic differences1. For example, though Black patients were less likely to receive antithrombotics and smoking cessation counseling compared to whites in 2010, these differences were no longer apparent by 2014. Data from the FSR as well as nationally representative registry data have also demonstrated race/ethnic differences in long-term outcomes among stroke survivors7. In the FSR compared to whites, Black patients have been shown to have a lower risk of mortality at 30 days after stroke, but a higher risk of mortality at one year, as well as a higher risk of rehospitalization within 30 days8. How race/ethnic disparities in acute stroke care contribute to race/ethnic disparities in outcomes after stroke hospitalization is not well-understood. The goal of the current study was to examine the relationship between acute stroke quality of care measures and mortality within the first year as well as rehospitalization within 30 days as well as race/ethnic disparities in these relationships. This study relates stroke process of care measures captured by the Get With the Guidelines quality improvement program designed by the American Heart Association9 with long-term outcomes captured in the CMS database for Medicare recipients, while taking advantage of enhanced race/ethnicity data captured in the Florida Stroke Registry.
Materials and Methods
Study Population
The study population included Medicare fee-for-service beneficiaries age 65 and over who were discharged from a Florida Stroke -Registry hospital between 2010–2013 with a principal diagnosis of ischemic stroke (International Classification of Diseases, 9th revision, Clinical Modification [ICD-9-CM] codes 433, 434, and 436). All of the hospitals in Florida participating in the ongoing Get With the Guidelines-Stroke (GWTG-S) data collection system, the American Heart Association stroke quality care improvement program, were invited to be included in this voluntary stroke registry. At the time of this analysis, there were 66 Florida hospitals in the registry.
GWTG-S registry patients are identified from those admitted for acute stroke by trained hospital personnel using prospective clinical identification, retrospective identification using International Classification of Diseases-9 discharge codes, or a combination. Though the primary data used in the FSR are the standard GWTG-S data, it also utilizes several additional questions including self-reported ethnicity, language, and education.
The FSR was propensity matched with the Medicare claims database for long-term mortality and readmissions data. Matching was accomplished through unique combinations of identifiers, including hospital identification number, admission and discharge dates, date of birth, and sex. Details regarding the combination of data from the FSR and the Medicare claims files have been described in detail previously10. We matched 21,630 (64%) of the Medicare ischemic stroke cases to FSR cases, consistent with the matching achieved for CMS with the national GWTG registry, and the current study includes those treated in Florida only.
Medicare data was extracted from the Medicare Inpatient and Master Beneficiary Summary Files, and it is protected through a data use agreement with the Centers for Medicare and Medicaid Services (CMS). The data are privately owned by CMS and GWTG, and the authors are not authorized to make them publicly available. The study was approved by the institutional review boards of the University of Miami and Yale University.
Variables of Interest
The independent variables of interest reflected acute stroke quality of care, assessed using the following key performance metrics (1) thrombolysis administered to eligible patients who arrived at the hospital within 2 hours of symptom onset and received treatment within 3 hours of symptom onset; (2) antithrombotic therapy by the end of hospital day two; (3) deep vein thrombosis (DVT) prophylaxis by the end of hospital day two for non-ambulatory patients; (4) discharged on antithrombotic therapy; (5) appropriate anticoagulation therapy for atrial fibrillation/flutter; (6) discharged on statin medication for patients with LDL>100 or on lipid-lowering agents before admission or with unmeasured LDL in the previous 30 days; (7) counseling or medication for smoking cessation. This data was captured in the GWTG-S database for all study participants.
The primary outcomes included in-hospital, 30-day, 6-month, and 1-year all-cause mortality measured from the date of the index ischemic stroke hospital admission and 30-day all-cause readmission measured from the date of discharge and captured in the matched CMS database.
Data extracted as covariates included age, sex, race and ethnicity, NIH stroke score (NIHSS), mode of arrival, time from symptom onset to hospital arrival, health insurance status, medical history, in-hospital treatment and events (including timing of rt-PA treatment and contraindications), and discharge treatment. Race/ethnicity was self-reported and included Non-Hispanic white, Non-Hispanic Black and Hispanic categories. In Florida the sample sizes for other race/ethnic categories were too small to include in this study.
Statistical Analysis
Mixed models with a logit link function and hospital-specific random intercepts were used to assess the relationships between stroke process of care measures with in-hospital, 30-day, 6-month, and 1-year mortality and 30-day readmission. A series of two multivariable adjusted models was constructed. The first model included age, sex, race/ethnicity and NIHSS as covariates. NIHSS was included in the models using the missing indicator approach as 37% of the study population was missing this variable. A second fully adjusted model included the following covariates: demographics, NIHSS, health insurance status, mode of arrival, current smoking, hypertension, diabetes, dyslipidemia, and medical history of atrial fibrillation, coronary artery disease/prior myocardial infarction, and previous stroke/transient ischemic attack, and hospital-level factors including number of beds, years in GWTG-S and academic status. Each of the individual stroke care metrics were examined as separate independent variables, without mutual adjustment. For each performance metric examined the reference category was the population of eligible patients that did not receive that acute stroke care measure.
We examined effect modification by race/ethnicity for the associations between the stroke care metrics and mortality and readmission, adjusting for age, sex and NIHSS, and stratified analyses were performed. For these race/ethnic stratified analyses, we also ran sensitivity analyses additionally controlling for coronary artery disease/prior myocardial infarction and previous stroke/transient ischemic attack to determine if the conclusions remained consistent after adjusting for these important predictors of mortality. Analyses were conducted using SAS v9.4 (SAS Institute, Cary, NC). Statistical tests used a two-sided alpha of 0.05.
Results
There were 14,100 ischemic stroke patients treated at FSR hospitals who self-identified as Black, white or Hispanic, and had data on acute stroke care metrics and long-term outcomes included in the current study. In this study population, 73% were white, 11% Black, and 15% Hispanic. The mean age was 78.9±8.7, and 46% were male. Table 1 shows the distribution of patient characteristics and outcomes by race/ethnicity. The following percentage of patients received each of the individual stroke care metrics: (1) rt-PA administered to eligible patients who arrived at the hospital within 2 hours of symptom onset and received treatment within 3 hours of symptom onset: 89%; (2) antithrombotic therapy by the end of hospital day two: 96%; (3) DVT prophylaxis by the end of hospital day two for non-ambulatory patients: 91%; (4) discharged on antithrombotic therapy: 97%; (5) appropriate anticoagulation therapy for atrial fibrillation/flutter: 95%; (6) discharged on statin medication for patients with LDL>100 or on lipid-lowering agents before admission or with unmeasured LDL in the previous 30 days: 91%; (7) counseling or medication for smoking cessation: 96%. The mortality rate in the full study population was 3% in-hospital, 12% at 30 days, 21% at 6 months, and 26% at 1 year, and 15% had a hospital readmission within 30 days.
Table 1.
Characteristics of the study population unadjusted and stratified by race/ethnicity
| Characteristics | NH-White | NH-Black | Hispanic |
|---|---|---|---|
| N | 10341 | 1621 | 2138 |
| Age: mean (SD) | 80 (9) | 75 (9) | 79 (8) |
| Male sex: N (%) | 4722 (46) | 742 (46) | 960 (45) |
| NIHSS: mean (SD) | 7.2 (7.7) | 7.7 (7.8) | 8.1 (7.9) |
| Health insurance: N (%) | |||
| Private | 4664 (45) | 340 (21) | 254 (12) |
| Medicare | 4643 (45) | 1021 (63) | 1266 (59) |
| None | 36 (<1) | 38 (2) | 6 (1) |
| Unknown | 998 (10) | 222 (14) | 602 (28) |
| Arrival by EMS: N (%) | 6270 (61) | 886 (55) | 1230 (58) |
| Current smoker: N (%) | 939 (9) | 173 (11) | 172 (8) |
| Hypertension: N (%) | 6988 (68) | 1188 (73) | 1229 (57) |
| Diabetes: N (%) | 2434 (24) | 635 (39) | 610 (29) |
| Dyslipidemia: N (%) | 4640 (45) | 555 (34) | 685 (32) |
| Atrial fibrillation history: N (%) | 2557 (25) | 175 (11) | 375 (18) |
| CAD/MI: N (%) | 2893 (28) | 289 (18) | 474 (22) |
| Previous stroke/TIA: N (%) | 2666 (26) | 476 (29) | 468 (22) |
| rt-PA, arrive by 2 hrs and treat by 3 hrs: N (%) | 699 (89) | 59 (86) | 145 (91) |
| Early Antithrombotic Use: N (%) | 8305 (96) | 1346 (94) | 1736 (96) |
| Antithrombotics at Discharge: N (%) | 8751 (97) | 1391 (95) | 1785 (95) |
| Anticoagulation for Atrial Fibrillation: N (%) | 1855 (95) | 148 (95) | 297 (94) |
| Smoking cessation counseling: N (%) | 834 (97) | 153 (94) | 153 (96) |
| LDL 100 or ND – Statin: N (%) | 6351 (91) | 1031 (92) | 1332 (93) |
| VTE Prophylaxis: N (%) | 9051 (91) | 1424 (90) | 1867 (90) |
| In-hospital mortality: N (%) | 320 (3) | 62 (4) | 102 (5) |
| 30-day mortality: N (%) | 1193 (12) | 154 (10) | 290 (14) |
| 6-month mortality: N (%) | 2180 (21) | 317 (20) | 500 (23) |
| 1-year mortality: N (%) | 2687 (26) | 396 (24) | 599 (28) |
| 30-day readmission: N (%) | 1445 (15) | 235 (15) | 315 (16) |
The associations between the process of care measures with the five outcomes of interest in the series of multi-variable adjusted models are shown in Table 2. DVT prophylaxis, rt-PA treatment, smoking cessation counseling, and anticoagulation therapy for atrial fibrillation were not related to any of the five outcomes. Statin therapy for those with elevated LDL was associated with a lower risk of mortality at 6 months and one year, and also with a lower risk of readmissions at 30 days in the full study population. These associations were apparent even when stroke severity as measured by the NIHSS was not included as a covariate (not shown). Patients who received anti-thrombotics by the end of the second hospital day had a lower risk of mortality at all time points, as did those who were discharged on antithrombotics. However, antithrombotic treatment was unrelated to the risk of readmission within 30 days. The results remained fairly consistent in the fully adjusted models that controlled for demographics and the NIHSS, as well as medical history, smoking, health insurance, model of arrival, and hospital characteristics.
Table 2.
Acute stroke in-hospital process of care metrics in relation to post-stroke outcomes within 1 year in the FSR. These results were generated from multi-level logistic regression models to account for clustering within hospitals.
| Acute Care Metric OR (95% CI)* | In-hospital mortality (N=484 outcomes) | 30-day mortality (N=1637 outcomes) | 6-month mortality (N=2997 outcomes) | One-year mortality (N=3682 outcomes) | 30-day readmissions (N=1995 outcomes) |
|---|---|---|---|---|---|
| rt-PA, arrive by 2 hrs and treat by 3 hrs | |||||
| Model 1 | 0.66 (0.29–1.50) | 0.88 (0.44–1.73) | 0.88 (0.48–1.61) | 0.78 (0.46–1.33) | 1.04 (0.55–1.96) |
| Model 2 | 0.61 (0.26–1.44) | 0.84 (0.41–1.70) | 0.85 (0.45–1.60) | 0.76 (0.44–1.30) | 1.15 (0.60–2.22) |
| Early Antithrombotic Use | |||||
| Model 1 | 0.66 (0.42–1.03) | 0.58 (0.44–0.77) | 0.62 (0.52–0.75) | 0.65 (0.51–0.82) | 0.85(0.69–1.06) |
| Model 2 | 0.66 (0.42–1.03) | 0.59 (0.44–0.79) | 0.63 (0.51–0.77) | 0.66 (0.50–0.87) | 0.87(0.71–1.08) |
| Antithrombotics at Discharge | |||||
| Model 1 | 0.17(0.09–0.32) | 0.37 (0.24–0.58) | 0.55 (0.40–0.74) | 0.57 (0.43–0.76) | 0.97(0.75–1.25) |
| Model 2 | 0.20(0.10–0.38) | 0.39 (0.23–0.64) | 0.55 (0.40–0.76) | 0.56 (0.42–0.75) | 0.95(0.75–1.21) |
| Anticoagulation for Atrial Fibrillation | |||||
| Model 1 | 0.88 (0.19–4.13) | 0.69 (0.36–1.31) | 0.82 (0.56–1.19) | 0.79 (0.55–1.14) | 1.09 (0.66–1.81) |
| Model 2 | |||||
| Smoking Cessation Counseling | |||||
| Model 1 | 1.01 (0.43–2.42) | 1.17 (0.47–2.92) | 1.14 (0.51–2.56) | ||
| Model 2 | 1.15 (0.48–2.72) | 1.39 (0.58–3.37) | 1.29 (0.55–3.04) | ||
| LDL 100 or ND – Statin | |||||
| Model 1 | 0.54(0.28–1.05) | 0.74 (0.51–1.08) | 0.75 (0.59–0.95) | 0.68 (0.55–0.85) | 0.85 (0.73–0.98) |
| Model 2 | 0.52(0.27–1.00) | 0.75 (0.51–1.10) | 0.74 (0.58–0.95) | 0.68 (0.55–0.85) | 0.85 (0.75–0.98) |
| VTE prophylaxis | |||||
| Model 1 | 0.83 (0.59–1.16) | 1.00 (0.80–1.25) | 0.94 (0.79–1.12) | 0.90 (0.77–1.06) | .03 (0.86–1.24) |
| Model 2 | 0.81 (0.58–1.14) | 0.97 (0.78–1.22) | 0.92 (0.77–1.04) | 0.89 (0.73–1.06) | 1.02 (0.85–1.23) |
Model 1: Controlling for age, sex, race/ethnicity, and NIHSS
Model 2: Controlling for age, sex, race/ethnicity, NIHSS, health insurance status, mode of arrival, current smoker, hypertension, diabetes, dyslipidemia, and medical history of atrial fibrillation, coronary artery disease/prior myocardial infarction, and previous stroke/transient ischemic attack, and hospital-level factors including number of beds, years in GWTG-S and academic vs. not
Results are missing from models that did not converge
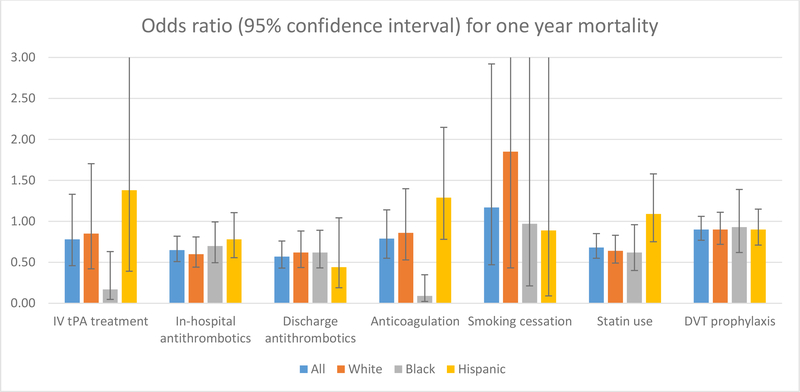
Figure 1 shows the adjusted odds ratios and confidence bounds for the associations between each of the process of care measures with one year mortality in the full study population and stratified by race/ethnicity in model 1. The associations between the process of care measures and mortality and 30-day readmissions stratified by race/ethnicity, and adjusting for age, sex, and NIHSS are shown in Table 3. Effect modification by race/ethnicity was suggested for the associations between rt-PA, early antithrombotic use, and anticoagulation for atrial fibrillation and one-year mortality (p for interaction <0.10). The protective association for rt-PA with one-year mortality was only apparent among Black patients. For early antithrombotic use, the inverse association with mortality was strongest among whites and apparent at 30 days, six months and one year, with the strongest effect estimate at 30 days. Among Black patients, a protective association for early antithrombotic use was not apparent at 30 days, but was apparent in the second half of the first year post-. The strong protective association for anticoagulation for atrial fibrillation with one-year mortality was apparent for Black patients only, and a comparison between effect estimates at 30 days, six months and one year suggest that the protective association was driven by mortality in the second half of the first year following stroke. A protective association between statin therapy and one-year mortality after stroke was statistically significant for Black participants and whites but not apparent for Hispanics. For whites, this inverse association for statin therapy was consistent at 30 days, 6 months, and one year, whereas for Black patients it was driven by mortality in the second half of the first year post-stroke and not apparent soon after stroke. Statin therapy was associated with a reduced risk of 30-day readmission only among Black patients. The associations remained consistent in sensitivity analyses that also included coronary artery disease/prior myocardial infarction and previous stroke/transient ischemic attack as covariates (not shown).
Figure 1.
Association between acute stroke in-hospital process of care metrics and mortality within 1 year, overall and stratified by race/ethnicity, and controlling for age, sex, race/ethnicity, and NIHSS.
Table 3.
Acute stroke in-hospital process of care metrics stratified by race/ethnicity in relation to mortality and 30-day readmission in the FSR. These results were generated from multi-level logistic regression models to account for clustering within hospitals.
| Acute Care Metrics | 30-day mortality OR (95% CI)* | 6-month mortality OR (95% CI)* | 30-day readmissions OR (95% CI)* |
|---|---|---|---|
| rt-PA, arrive by 2 hrs and treat by 3 hrs | |||
| White | 0.92 (0.43–1.99) | 0.92 (0.44–1.91) | 0.83 (0.45–1.55) |
| Black | 0.25 (0.05–1.20) | ||
| Hispanic | 0.93 (0.07–12.63) | 1.64 (0.19–13.95) | |
| Early Antithrombotic Use | |||
| White | 0.48 (0.34–0.67) | 0.55 (0.44–0.70) | 0.93 (0.72–1.21) |
| Black | 0.98 (0.40–2.42) | 0.70 (0.42–1.15) | 0.60 (0.34–1.05) |
| Hispanic | 0.79 (0.49–1.26) | 0.87 (0.61–1.24) | 0.97 (0.55–1.73) |
| Antithrombotics at Discharge | |||
| White | 0.38 (0.23–0.61) | 0.61 (0.40–0.91) | 1.03 (0.77–1.36) |
| Black | 0.90 (0.46–1.78) | 0.57 (0.34–0.93) | 0.87 (0.45–1.65) |
| Hispanic | 0.24 (0.10–0.59) | 0.44 (0.18–1.09) | 1.01 (0.54–1.89) |
| Anticoagulation for Atrial Fibrillation | |||
| White | 0.58 (0.29–1.18) | 0.83 (0.50–1.37) | 0.93 (0.57–1.51) |
| Black | 0.35 (0.06–2.09) | 0.45 (0.13–1.53) | 0.90 (0.08–9.57) |
| Hispanic | 1.31 (0.53–5.33) | 0.96 (0.48–1.92) | 3.40 (0.68–17.09) |
| Smoking Cessation Counseling | |||
| White | 1.77 (0.44–7.16) | 2.09 (0.68–6.42) | |
| Black | 0.67 (0.17–2.68) | 0.29 (0.03–2.44) | |
| Hispanic | 0.65 (0.04–10.30) | 0.32 (0.07–1.46) | |
| LDL 100 or ND – Statin | |||
| White | 0.60 (0.39–0.92) | 0.68 (0.51–0.90) | 0.92 (0.75–1.12) |
| Black | 2.36 (0.74–7.55) | 0.86 (0.53–1.37) | 0.65 (0.42–0.99) |
| Hispanic | 0.94 (0.58–1.52) | 1.12 (0.77–1.61) | 0.74 (0.46–1.20) |
| VTE prophylaxis | |||
| White | 0.96 (0.72–1.29) | 0.90 (0.72–1.12) | 1.01 (0.83–1.24) |
| Black | 1.18 (0.63–2.19) | 1.04 (0.68–1.59) | 0.93 (0.64–1.35) |
| Hispanic | 1.00 (0.70–1.43) | 1.07 (0.84–1.36) | 1.31 (0.84–2.04) |
Controlling for age, sex, and NIHSS (where results are missing the models did not converge)
Discussion
The results of the current study suggest that among Medicare fee-for-service beneficiaries in Florida, specific acute stroke process of care metrics were associated with reduced mortality within a year after stroke, most notably early antithrombotic use, antithrombotic use at discharge, and statin therapy. Study participants who received these acute stroke care measures were less likely to die within the first year post-stroke than the eligible study participants who did not receive these recommended measures. Race/ethnic differences were observed for the associations between some acute stroke care metrics and mortality within one year, with the associations for antithrombotic use and statin therapy strongest among whites. Previous studies using data from the Florida Stroke Registry have demonstrated race/ethnic disparities in acute stroke care as well as disparities in stroke outcomes1,8,11. The relationship between acute stroke care and post hospital outcomes is less clear and likely also depends on the quality of transitions of care to the community and post-hospital adherence to stroke medications which could differ across race-ethnic subgroups8. The current study represents a novel investigation of the association between acute stroke care and one year outcomes.
This study also provides valuable recent data on in-hospital mortality and mortality within the first year after stroke among Medicare beneficiaries, overall and stratified by race/ethnicity in a dataset designed to more accurately record self-reported race and ethnicity. In all race/ethnic groups, the first 30 days represented the period of time at highest risk of death, with absolute 30-day mortality ranging from 10% in Black patients, 12% in whites, and 14% in Hispanics, and by one year more than a quarter of all stroke patients had died (24% among Black patients, 26% among whites, and 28% among Hispanics). A previous study of Medicare beneficiaries age 65 and older showed a greater improvement from 1988 to 2013 in 30-day mortality post-stroke among Black men and women12. The fact that 26% of our study population had died within one year post-stroke is noteworthy, partly reflects the advanced age of this study population, and underscores the need for improved care during hospitalization as well as improved transition of care, rehabilitation utilization, and recommended medication and lifestyle adherence post-stroke. The 15% hospital readmission rate observed in the current study is consistent with our previous study in the FSR, which suggested that these readmissions are largely preventable10.
Black stroke patients in a nation-wide sample treated at 1181 GWTG-S hospitals in 2003–2008 were shown to be less likely to receive intravenous thrombolysis, DVT prophylaxis, smoking cessation therapy, discharge antithrombotics, anticoagulants for atrial fibrillation, lipid therapy, and more likely to die in-hospital13. However, these trends were not observed in our previously published FSR analysis, with the exception of smoking cessation therapy. We hypothesized that this may be due to temporal improvements in acute stroke care among Black patients in recent years1. Among Hispanics in the nationwide GWTG-S sample, defect-free care was similar to whites, though Hispanics were less likely to receive antithrombotics and smoking cessation during hospitalization13. The relationship between acute stroke care and improved early outcomes after stroke have been suggested14. For example, rt-PA treatment within 4.5 hours of stroke symptom onset has been associated with less disability at 3–6 months as measured by the Modified Rankin Scale, but was unrelated to overall 90-day mortality15.
In the current study, stroke patients who received early antithrombotic use and antithrombotic use at discharge had reduced mortality in-hospital, and at 30 days, six months, and one year compared to stroke patients who did not receive antithrombotics. The beneficial associations for early and discharge antithrombotic use appeared to lessen over time, between in-hospital mortality and 1-year mortality which could reflect post-hospital care differences. The data for statin therapy for those eligible suggested mortality benefits at all time points, particularly among non-Hispanics, but in the full study population the results were only significant for mortality at six months and one year likely due to improved statistical power with more outcomes accrued. For all race-ethnic groups combined, there was no significant reduction in mortality within the first year after stroke among patients wo received timely rt-PA treatment, anticoagulation therapy for atrial fibrillation, smoking cessation counseling, or VTE prophylaxis treatment compared to eligible participants who did not receive these acute stroke care measures. The high implementation of optimal metrics, including DVT prophylaxis, may explain the lack of significant association with mortality. However, among Black patients rt-PA use and anticoagulation for atrial fibrillation were protective for one year mortality. These findings support the importance of optimal stroke care performance, not only for outcomes in the hospital and at discharge, but also for one year mortality, and therefore underscore the value of quality improvement programs like GWTG and FSR, as the latter has the explicit goal of identifying and reducing disparities in stroke care.
In our previous publication on race/ethnic disparities in long-term outcomes after stroke in the FSR, we reported a higher risk of 30-day readmissions for Black patients vs whites, and a lower risk among Hispanics vs whites in Florida8. Of the process of care measures examined in the current study, only statin therapy was associated with a reduced risk of hospital readmission within 30 days, particularly among Black patients. Previous data from the FSR linked to the CMS database showed that approximately a quarter of the readmissions were attributable to acute cerebrovascular events, including 17% due to ischemic stroke or transient ischemic attack, 2% hemorrhagic stroke, and 5% cerebral artery interventions10.
A primary strength of the current study is the merging of the Florida Stroke Registry/GWTG database with the CMS database to utilize the valuable long-term mortality and readmissions data from CMS with the rich and more accurate data from Florida Stroke Registry /GWTG on stroke severity, medical history and comorbidities, vascular risk factors, and hospital-level factors. Moreover, our reliance on race and ethnicity data recorded in the FSR-enhanced GWTG-S database rather than CMS administrative records reduced misclassification16. Another strength of the current study is the ability to evaluate mortality within four points during the first year post-stroke and therefore determine if specific acute stroke care metrics are associated with mortality soon after stroke or in a delayed manner. Interestingly, among Black patients we found that the protective associations for multiple acute stroke care measures appeared to be stronger in the second half of the year post-stroke, a trend that was not as apparent among whites and Hispanics. This observation persisted in sensitivity analyses that also included prior history of coronary artery disease, myocardial infarction, stroke, and transient ischemic attack, which are important predictors of mortality that varied by race/ethnicity. Future studies are needed to elucidate how these stroke care metrics differentially impact the leading causes of mortality after stroke, and how these effects may vary by race/ethnicity.
An important limitation to note is that the stroke care captured in the current study only represents the care received during hospitalization, and we lack data on care received after hospital discharge, which is also expected to have a significant impact on long-term outcomes and mortality within the first year. The quality of transitions of care will be addressed in future studies in this population (clinicaltrials.gov NCT03452813). In addition, the study was restricted to fee-for-service Medicare beneficiaries in the FSR, and therefore our findings may not be generalizable to stroke patients who are younger or not enrolled in this Medicare program, though it has been reported that GWTG-S admissions for Medicare patients age >65 are considered representative of national samples. Greater stroke disparities however have been suggested in younger populations, with increased stroke incidence and mortality observed among Black people at younger ages and racial differences decreasing with age17–19.
In conclusion, the results of this study provide novel insight into the relationship between acute stroke care and stroke mortality and 30-day readmission, and underscore the importance of further optimizing acute stroke care for all patients as well as continued efforts to identify and eliminate disparities. Elucidating the presence, origins, and long-term effects of disparities in acute stroke care are necessary steps to eliminating them. This study contributes to a growing body of literature highlighting the need to provide evidence-based optimal care for all stroke patients and the importance of GWTG-S, the Florida Stroke Registry, and other registries that strive to improve the quality of stroke care.
Highlights.
This study relates acute stroke process of care measures with long-term outcomes.
Acute stroke care metrics were associated with reduced 1-year mortality.
Antithrombotic use early and at discharge and statin therapy were most relevant.
Associations between acute stroke care and mortality differed by race/ethnicity.
Associations for antithrombotic and statin therapy were strongest among Whites.
Acknowledgments
Funding: National Institute of Neurological Disorders and Stroke grant U54-NS081763 and National Institute on Minority Health and Health Disparities grant 1R01MD012467
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Hannah Gardener, Department of Neurology, University of Miami Miller School of Medicine, Miami, FL.
Tatjana Rundek, Department of Neurology, University of Miami Miller School of Medicine, Miami, FL.
Judith Lichtman, Department of Epidemiology, Yale School of Public Health, New Haven, CT.
Erica Leifheit, Department of Epidemiology, Yale School of Public Health, New Haven, CT.
Kefeng Wang, Department of Neurology, University of Miami Miller School of Medicine, Miami, FL.
Negar Asdaghi, Department of Neurology, University of Miami Miller School of Medicine, Miami, FL.
Jose G Romano, Department of Neurology, University of Miami Miller School of Medicine, Miami, FL.
Ralph L Sacco, Department of Neurology, University of Miami Miller School of Medicine, Miami, FL.
References
- 1.Gardener H, Leifheit EC, Lichtman JH, Wang Y, Wang K, Gutierrez CM, Ciliberti-Vargas MA, Dong C, Oluwole S, Robichaux M, et al. Racial-Ethnic Disparities in Acute Stroke Care in the Florida-Puerto Rico Collaboration to Reduce Stroke Disparities Study. J Am Heart Assoc. 2017;6:e004073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Messé SR, Khatri P, Reeves MJ, Smith EE, Saver JL, Bhatt DL, Grau-Sepulveda MV, Cox M, Peterson ED, Fonarow GC, et al. Why are acute ischemic stroke patients not receiving IV tPA? Results from a national registry. Neurology. 2016;87:1565–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rinaldo L, Rabinstein AA, Cloft H, Knudsen JM, Castilla LR, Brinjikji W. Racial and Ethnic Disparities in the Utilization of Thrombectomy for Acute Stroke. Stroke. 2019;50:2428–2432. [DOI] [PubMed] [Google Scholar]
- 4.Howard G, Anderson R, Sorlie P, Andrews V, Backlund E, Burke GL. Ethnic differences in stroke mortality between non-Hispanic whites, Hispanic whites, and blacks. The National Longitudinal Mortality Study. Stroke. 1994;25:2120–2125. [DOI] [PubMed] [Google Scholar]
- 5.Sacco RL, Boden-Albala B, Abel G, Lin IF, Elkind M, Hauser WA, Paik MC, Shea S. Race-ethnic disparities in the impact of stroke risk factors: the northern Manhattan stroke study. Stroke. 2001;32:1725–1731. [DOI] [PubMed] [Google Scholar]
- 6.Faigle R, Urrutia VC, Cooper LA, Gottesman RF. Individual and System Contributions to Race and Sex Disparities in Thrombolysis Use for Stroke Patients in the United States. Stroke. 2017;48:990–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qian F, Fonarow GC, Smith EE, Xian Y, Pan W, Hannan EL, Shaw BA, Glance LG, Peterson ED, Eapen ZJ, et al. Racial and ethnic differences in outcomes in older patients with acute ischemic stroke. Circulation Cardiovascular quality and outcomes. 2013;6:284–292. [DOI] [PubMed] [Google Scholar]
- 8.Gardener H, Leifheit EC, Lichtman JH, Wang Y, Wang K, Gutierrez CM, Ciliberti-Vargas MA, Dong C, Oluwole S, Robichaux M, et al. Racial/Ethnic Disparities in Mortality Among Medicare Beneficiaries in the FL - PR CR eSD Study. J Am Heart Assoc. 2019;8:e009649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smaha LA; American Heart Association. The American Heart Association Get With The Guidelines program. Am Heart J. 2004;148:S46–S48. [DOI] [PubMed] [Google Scholar]
- 10.Gardener H, Leifheit EC, Lichtman JH, Wang K, Wang Y, Gutierrez CM, Ciliberti-Vargas MA, Dong C, Robichaux M, Romano JG, et al. Race-Ethnic Disparities in 30-Day Readmission After Stroke Among Medicare Beneficiaries in the Florida Stroke Registry. J Stroke Cerebrovasc Dis. 2019;28:104399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oluwole SA, Wang K, Dong C, Ciliberti-Vargas MA, Gutierrez CM, Yi L, Romano JG, Perez E, Tyson BA, Ayodele M, et al. Disparities and Trends in Door-to-Needle Time: The FL-PR CReSD Study (Florida-Puerto Rico Collaboration to Reduce Stroke Disparities). Stroke. 2017;48:2192–2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yao J, Ghosh K, Perraillon MC, Cutler DM, Fang MC. Trends and racial differences in first hospitalization for stroke and 30-day mortality in the US Medicare population from 1988 to 2013. Med Care. 2019;57:262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwamm LH, Reeves MJ, Pan W, Smith EE, Frankel MR, Olson D, Zhao X, Peterson E, Fonarow GC. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010;121:1492–1501. [DOI] [PubMed] [Google Scholar]
- 14.Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Kothari RU, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006;114:168–182. [DOI] [PubMed] [Google Scholar]
- 15.Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, Brott T, Cohen G, Davis S, Donnan G, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384:1929–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eicheldinger C, Bonito A. More accurate racial and ethnic codes for Medicare administrative data. Health care financing review. 2008;29:27–42. [PMC free article] [PubMed] [Google Scholar]
- 17.Pathak EB, Sloan MA. Recent racial/ethnic disparities in stroke hospitalizations and outcomes for young adults in Florida, 2001–2006. Neuroepidemiology. 2009;32:302–311. [DOI] [PubMed] [Google Scholar]
- 18.Howard VJ, Kleindorfer DO, Judd SE, McClure LA, Safford MM, Rhodes JD, Cushman M, Moy CS, Soliman EZ, Kissela BM, Howard G. Disparities in stroke incidence contributing to disparities in stroke mortality. Annals of neurology. 2011;69:619–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morgenstern LB, Smith MA, Sanchez BN, Brown DL, Zahuranec DB, Garcia N, Kerber KA, Skolarus LE, Meurer WJ, Burke JF, Adelman EE, Baek J, Lisabeth LD. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. Annals of neurology. 2013;74:778–785. [DOI] [PMC free article] [PubMed] [Google Scholar]