Abstract
COVID-19 caused by SARS-CoV-2 is an ongoing global pandemic. SARS-CoV-2 affects the human respiratory tract's epithelial cells, leading to a proinflammatory cytokine storm and chronic lung inflammation. With numerous patients dying daily, a vaccine and specific antiviral drug regimens are being explored. Probiotics are live microorganisms with proven beneficial effects on human health. While probiotics as nutritional supplements are long practiced in different cuisines across various countries, the emerging scientific evidence supports the antiviral and general immune-strengthening health effects of the probiotics. Here, we present an overview of the experimental studies published in the last 10 years that provide a scientific basis for unexplored probiotics as a preventive approach to respiratory viral infections. Based on collated insights from these experimental data, we identify promising microbial strains that may serve as lead prophylactic and immune-boosting probiotics in COVID-19 management.
Keywords: COVID-19, Influenza virus, Lactobacillus, Probiotics, Respiratory viral infection, SARS-CoV-2
Abbreviations: ACE2, Angiotensin-converting enzyme 2; COVID-19, Coronavirus disease; CRP, C-reactive protein; GCSF, Granulocyte colony-stimulating factor; IFV, influenza A virus; IL, Interleukin; IFN-γ, Interferon-gamma; MERS-CoV, Middle East respiratory syndrome coronavirus; NK, Natural killer; OAS, Oligoadenylate synthetase; RVI, Respiratory virus infections; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2; TNF, Tumor Necrosis Factor; Th1/2, T-helper cells type 1 and 2; WHO, World Health Organization
1. Introduction
Coronavirus disease 2019 (COVID-19) is a severe respiratory inflammatory disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It is declared a global pandemic by the World Health Organization (WHO) [1]. Unfortunately, even after implementing various strategic and socioeconomic response plans and stringent public health measures globally, including personal hygiene, mask-wearing, social distancing, lockdowns, and quarantines, the number of infections and death are on the rise. The WHO assessment is that the disease may continue to stay with the population. It requires constant preparedness and investment in public health and other resources to manage the spread and morbidity caused by SARS-CoV-2.
SARS-CoV-2 is a new and different virus from previously known coronaviruses, namely Middle East respiratory syndrome coronavirus (MERS-CoV) and SARS-CoV [2]. Therefore, the existing antiviral or flu vaccines are not effective against it. With a constant boost from WHO, several research and development efforts are going on at the international level to develop the specific therapy and vaccine against the new virus [3]. The clinical use of Hydroxychloroquine, Lopinavir/ Ritonavir, Remdesivir, anti-inflammatory drugs, convalescent plasma, anticoagulants, Vasodilators, nonsteroidal anti-inflammatory drugs, and monoclonal antibodies is under different stages of trials, research, or approvals. Nevertheless, no treatment so far is precise to the virus [4], [5], [6], [7]. While such medicines and vaccines are not available, the virus is already mutating and manifesting in symptomatic, presymptomatic, and asymptomatic forms in affected populations. In symptomatic cases, the common COVID-19 indications include fever, tiredness, dry cough, nasal congestion, diminished sense of smell, sore throat, body pains, and gut dysbiosis [8,9].
With disease onset, the patient faces difficulty in breathing, and in due course, the disease progresses into severe respiratory tract infection and chronic inflammation [10]. Such condition may precede a presymptomatic condition that ranges from a week to a fortnight with heavy viral loads and a high risk of spreading the coronavirus to others. Similarly, the infected yet asymptomatic population serves as the carrier and transmits the virus to people without symptoms. Both presymptomatic and asymptomatic manifestations are indeed one of the primary reasons for the pandemic. At the cellular level, immunomodulatory markers such as proinflammatory cytokines, Interleukin (IL)-1β, IL-2, IL-6, IL-7, IL-12, tumor necrosis factor (TNF)-α, interferon-gamma (IFN-γ) and anti-inflammatory cytokines IL-4, IL-10, IL-11, and IL-13 control the infection. Further, natural killer (NK) cells, cytotoxic T-lymphocytes, and antibody production also play a crucial role in promoting pathogen killing [11,12].
Probiotics are nonpathogenic living microorganisms providing various health benefits to the human host. The common probiotic strains belong to the genera of Lactobacillus and Bifidobacterium. The use of probiotics in food such as fermented food is traditional knowledge and ascertained to improve nutrition and health by restoring microbial balance in the human gut [13]. Interestingly, in the last 2 decades, several studies have demonstrated the role of probiotics in managing immune responses and various disease conditions, specifically viral infections in different animal models and clinical trials. Studies suggest that dietary meals with fiber and probiotics supplementation support a stable host immune response system, preventing adverse effects of viral infections [14,15]. Various studies have reported the beneficial role of probiotic bacteria, namely, Lactobacillus plantarum [16], Bacillus subtilis [17], Lactobacillus casei [18], Lactobacillus plantarum [19], and Bifidobacterium bifidum [20] in experimental animal models of respiratory tract viral infection. Probiotic interventions led to improved animal health, easing clinical symptoms, lowering viral load in the lungs, and enhanced survival rates were observed [21].
Therefore, we first used a list of keywords (probiotics, virus, influenza virus, antiviral, respiratory tract infections, gut dysbiosis, microbial strain names, animal model, etc.) and their combinations to search PubMed, Science Direct, and Google Scholar. In this manner, we retrieved ~4500 experimental studies published on the subject between 2010 and 2020. Next, we collated and discussed the published experimental evidence of probiotics efficacy in preventing viral infections. We evaluated the insights gleaned from these studies in the SARS-CoV-2 infection scenario. Finally, we list the probiotic strains that may lead to preventive interventions and general immunity enhancers to manage COVID-19 and related viral infections.
2. Probiotics as antiviral agents
The human respiratory tract is exposed to several microorganisms. It is the primary path for the internalization of respiratory viruses. Thus, preventing the virus's adsorption onto the mucosal epithelial surfaces is crucial for reducing disease development. The human body harbors a range of mutually beneficial microorganisms. Collectively, we denote them as the human microbiota. Probiotics are also one such friendly set of microbes that positively influence human health when ingested or administered in a particular concentration. Probiotic strains of Lactobacillus and Bifidobacterium genera can trap the virus and interfere in the virus binding to the host cell receptors, which is beneficial to the host health [22,23]. Similarly, probiotics administration confers health benefits to humans against respiratory viral infections, including Respiratory syncytial virus and Influenza A virus (IFV) [15]. Here we discuss and compare (in Table 1 ) several of these experimental studies published since 2010 that have characterized probiotics as antiviral agents against different viruses using various animal models and clinical studies on human subjects.
Table 1.
List of probiotic strains and preclinical and clinical evidences of their efficacy in managing viral diseases
| Probiotic strains | Study year | Infection | Model | Outcomes | Ref. |
|---|---|---|---|---|---|
| Lactobacillus pentosus S-PT84 | 2010 | Influenza virus A/PR/8/34 (H1N1) | Female BALB/c mice | Higher survival rate and lower viral load in lungs along with increased NK cells activity along with a higher expression of IL-12 and IFN-α in the lung tissue | [59] |
| Lactobacillus rhamnosus GG and Lactobacillus gasseri TMC0356 | 2010 | Influenza virus A/PR/8/34 (H1N1) | Female BALB/c mice | Alleviate clinical symptoms and significantly lower virus load in the lungs of infected mice. | [60] |
| Lactobacillus plantarum YU | 2011 | Influenza virus A/NWS/33 (H1N1) | Male BALB/c mice | Prevented weight loss and suppressed viral proliferation due to enhanced Th1 immune response | [16] |
| Lactobacillus pentosus strain b240 | 2011 | Influenza virus A/PR/8/34 (H1N1) | Female BALB/c mice | Increased survival rate and lower virus load in the lungs along with increased production of IgA and IgG in bronchoalveolar lavage fluid and plasma | [61] |
| Bifidobacterium lactis Bb-12 | 2011 | Respiratory tract infections | Clinical trial 109 participants |
Newborn infants receiving probiotics had a lower (65%) incidence of respiratory infections as compared to 94% of infants in the control group | [44] |
| Lactobacillus rhamnosus | 2012 | Influenza virus A/NWS/33 (H1N1) | Female BALB/c mice | The increased survival rate with intranasal dosage along with increased secretory IgA production and reduced the expression levels of TNF-α and IL-6 | [24] |
|
Lactobacillus reuteri ATCC 55730 |
2012 | Inflammatory bowel diseases | Clinical trial 40 participants |
Useful in improving mucosal inflammation along with increased cytokine expression level of IL-10 and decreased levels of TNF-α, IL-1β, and IL-8 | [53] |
| Lactobacillus plantarum CNRZ1997 | 2013 | Influenza virus A/PR/8/34 (H1N1) | Female BALB/c mice | Reduced weight loss, alleviated clinical symptoms, and decreased virus load in the lungs of infected mice | [25] |
| Lactobacillus plantarum LBP-K10 | 2013 | Influenza virus H3N2 | Madin-Darby canine kidney cells | Cyclic dipeptides obtained from culture filtrate was successful in inhibiting viral infectivity and proliferation | [62] |
| Lactobacillus acidophilus L-92 | 2013 | Influenza virus A/PR/8/34 (H1N1) | Female BALB/c mice | Prevented weight loss, reduced viral load in the lungs along with an increased expression of antiviral cytokines and chemokines | [26] |
| Lactobacillus rhamnosus GG and Bifidobacterium lactis Bb-12 | 2013 | Upper respiratory tract infection | Clinical trial 231 participants |
The severity of upper respiratory infections was lower in the probiotic group along with the improved quality of life | [49] |
| Bifidobacterium infantis 35624 | 2013 | Inflammatory bowel diseases | Clinical trial 192 participants |
Significant reduction in C-reactive protein (CRP) levels and proinflammatory markers (TNF-α and IL-6) | [54] |
| Lactobacillus rhamnosus CRL1505 | 2014 | Respiratory syncytial virus and Influenza virus A/PR/8/34 (H1N1) | Male BALB/c mice | Reduced risk of lung injury and lower virus titer along with modulation of tissue factor and thrombomodulin expression in lungs of infected mice | [63] |
| Lactobacillus gasseri SBT2055 | 2014 | Influenza virus A/PR/8/34 (H1N1) | Male C57BL/6N mice | Reduced virus load and lower expression of IL-6 in the lung tissue. Increased expression of myxovirus resistance 1 (Mx1) and oligoadenylate synthetase 1A (Oas1a) resulted in viral clearance | [27] |
| Lactobacillus casei DN 114001 | 2014 | Antibiotic-associated diarrhea |
Clinical trial 258 participants |
Probiotics proved to be effective in the treatment of antibiotic-associated diarrhea in both children and adults | [43] |
| Lactobacillus rhamnosus, Lactobacillus plantarum, and Bifidobacterium longum | 2014 | Ventilator‐associated pneumonia | Clinical trials 1083 participants |
Cochrane meta-analysis review of 8 different trials reported the beneficial role of probiotic strains in reducing the risk of ventilator‐associated pneumonia | [47] |
| Lactobacillus reuteri Protectis | 2016 | Coxsackieviruses and Enterovirus 71 strain 41 | Human rhabdomyosarcoma and Caco-2 cell lines | In vitro assays confirmed significant dose-dependent antiviral activity Coxsackievirus type A and Enterovirus 71 | [30] |
| Lactobacillus rhamnosus M21 | 2016 | Influenza virus A/NWS/33 (H1N1) | Female BALB/c mice | The increased survival rate, lower viral titer in lungs of infected mice, and increased production of IFN-γ, IL-2, and IgA | [29] |
|
Lactobacillus rhamnosus HN001, Lactobacillus acidophilus DDS-1, Bifidobacterium lactis Bb-12, and Streptococcus thermophilus |
2016 | Upper respiratory tract infection | Clinical trials 6269 participants |
A meta-analysis of 23 trials reported that consumption of probiotics reduced the prevalence of respiratory tract infections along with the improved quality of life | [50] |
| Enterococcus faecalis | 2017 | Influenza virus (A/WSN/33) and Enterovirus 71 | Male C57BL/6 mice | Improved survival rate and low viral load in the bronchoalveolar lavage of infected mice | [31] |
| Lactobacillus acidophilus, Lactobacillus reuteri, and Lactobacillus salivarius | 2017 | Influenza virus A/Duck/Czech/56 (H4N6) | Madin-Darby canine kidney cells | Enhanced antiviral activity of chicken macrophages. Significantly higher expression of IL-1β, IFN-γ, and IFN-α resulted in protective responses against infection | [33] |
| Lactobacillus casei DK128 | 2017 | Influenza virus A/Philippines/2/1982 (H3N2) | Female BALB/c mice | Prevented weight loss and along with higher survival rate and lower expression of IL-6 and TNF-α inflammatory cytokines | [18] |
| Bacillus subtilis 3 | 2017 | Influenza virus A/FM/1/47 (H1N1) | BALB/c mice | Reduced viral load in lungs and increased survival rate of infected mice | |
| Lactobacillus paracasei N1115 | 2017 | Upper respiratory tract infection | Clinical trial 233 participants |
Reduced provenance of upper respiratory tract infections along with a higher percentage of CD3+ cells | [51] |
|
Lactobacillus casei strain Shirota |
2017 | Upper respiratory tract infection | Clinical trial 96 participants |
Healthy subjects reported a significantly lower (22.4%) incidence of respiratory infections than 53.2% in the control group. | [52] |
| Lactobacillus plantarum | 2018 | H1N1 and H3N2 | Female BALB/c mice | Increased survival rate and significantly lower viral proliferation in the lungs of infected mice | [19] |
| Lactobacillus paracasei, Lactobacillus casei 431, and Lactobacillus fermentum PCC | 2018 | Upper respiratory tract infection | Clinical trial 136 participants |
50% to 60% reduced prevalence of common cold and flu-like symptoms and increased levels of IFN-γ and IgA | [41] |
| Lactobacillus rhamnosus GG, Lactobacillus reuteri, and Bifidobacterium infantis 35624 | 2018 | Multiple diseases | A meta-analysis of 52 trials | Probiotics were most effective against acute respiratory tract infections, antibiotic-associated diarrhea, acute infectious diarrhea, infant colic, and necrotizing enterocolitis. | [45] |
| Bifidobacterium bifidum | 2019 | Influenza virus-A/PR/8/34 (H1N1) | Female BALB/c mice | Increased survival rate along with the induction of both humoral and cellular immune responses |
[20] |
| Lactobacillus gasseri SBT2055 | 2019 | Respiratory syncytial virus-A2 strain | Female BALB/c mice | Reduced weight loss, lower viral load in the lungs of infected mice along with the reduced expression of proinflammatory cytokines | [34] |
|
Lactobacillus rhamnosus GG, Lactobacillus casei, Bifidobacterium lactis Bb-12 |
2019 | Acute respiratory tract infections and acute otitis | A meta-analysis of 17 trials | Probiotic strains significantly reduced the prevalence of common acute infections and antibiotics utilization | [46] |
2.1. Preclinical studies in animal models
We observe that most preclinical studies have employed Lactobacillus and Bifidobacterium strains to evaluate their antiviral effect. The experimental design of most studies discussed below included administering probiotic strains, followed by infection with the virus. Here, we have discussed them in the order of year of reporting.
Using IFV in a mice model, Kawashima's group [16] evaluated the antiviral effects of L. plantarum YU strain. Administration of probiotic strain steered weight loss and virus proliferation in the lungs and bronchoalveolar lavage fluids in a dose-dependent manner. Probiotic strain activated the T-helper cells type 1 (Th1) immune response, which resulted in increased levels of IFV-specific secretory IgA and neutralizing antibody titers in bronchoalveolar lavage fluids and sera, respectively, which led to the removal of IFV from lungs and other infected sites. These results confirm that the administration of probiotics strain has a protective role against IFV infection.
Song's group [24] conducted a study to analyze the antiviral efficacy of L. rhamnosus against IFV infection. There was a significant difference in mice's survival rate after administration of live and dead L. rhamnosus bacteria via both oral and intranasal routes. Dosage of live and dead probiotic bacteria via oral route led to survival rates of 40% and 0%. In contrast, the survival rate in the intranasal route was 70% and 40%, respectively. In both cases, the survival rate was higher with the administration of live bacteria. Treatment with live bacteria increased secretory IgA production and reduced the expression levels of proinflammatory cytokines TNF-α and IL-6 in lungs of infected mice.
Further, this group's interesting experiment evaluates nine live Lactobacillus species against IFV infection. Intranasal administration of probiotic species developed protective efficacy in the mice ranging between 20% and 100%. Among the 9 species, L. fermentum-1 and L. brevis-2 showed a significantly higher protection rate of 100% and 70% against IFV infection in mice, respectively. These results confirm that Lactobacillus species, indeed, has protective efficacy against viral infection, probably by invoking immunomodulatory properties.
A similar but large-scale screening study using 158 probiotic strains concluded that the probiotic strain L plantarum CNRZ1997 is most beneficial against respiratory virus infection/ influenza virus infection in a mouse model [25]. The administration of L. plantarum CNRZ1997 led to reduced weight loss, eased clinical symptoms, and inhibited virus proliferation in lungs of infected mice. However, the action mechanism of the probiotic strain was not made clear in this study. In another study, Yamamoto's group [26] evaluated the protective effects of the probiotic strain L. acidophilus L-92 against IFV. This strain also effectively prevented weight loss and reduced viral proliferation in lungs of infected mice. Besides, NK T-cells activity was augmented, possibly due to a higher expression of antiviral cytokines and chemokines, which resulted in the prevention of viral infection in mice.
Miyazaki's group [27] performed a study to evaluate the effect of L. gasseri SBT2055 probiotic strain against IFV infection in mice. Oral dosage of probiotic bacteria prevented weight loss, significantly reduced virus load in lungs and bronchoalveolar lavage fluids along with decreased inflammatory cytokine IL-6 in the lung tissue. Besides, increased expression of antiviral genes (myxovirus resistance 1] and oligoadenylate synthetase 1A [Oas1a]) resulted in the clearance of viral infection from the lung tissues of infected mice. These results confirm that probiotic bacteria have a pivotal role in the downregulation of virus replication.
Ha's group [28] investigated 11 probiotic strains belonging to genus Bifidobacterium and Lactobacillus for their antiviral activity against Human rotavirus Wa (ATCC VR-2018) using Vero cells isolated from monkey kidney. In this in vitro experiment, the activity of each probiotic strain was determined by plaque reduction assay. Amongst the tested bacterial strains, B. longum and L. acidophilus displayed the high inhibitory activity of 38% and 31%, followed by L. reuteri with 28%, as evident from a reduced plaque formation. Further, this group also reported that the administration of 6 probiotic strains B. longum, B. lactis, L. acidophilus, L. rhamnosus, L. plantarum, and Pediococcus pentosaceus significantly reduced the duration of diarrhea in pediatric patients without adverse effects. These findings suggest that probiotics consumption can be an alternative therapy for the treatment of acute rotaviral gastroenteritis.
Park's group [29] analyzed the protective effect of probiotic strain L. rhamnosus M21 against IFV infection using mice as an animal model. The probiotic strain treatment led to an increased survival rate (~40%) compared to the control group. Pathological results confirm that probiotic strain successfully reduces chronic damage to the lung tissue of infected mice. Probiotic strain administration also resulted in significantly increased production of IFN-γ, IL-2, and secretory IgA. This study demonstrates that probiotic strain is responsible for activating immune responses and curing the mice against severe virus infection.
The in vitro assays results were employed to confirm the antiviral activity of probiotic bacteria L. reuteri Protectis and L. casei Shirota against Coxsackieviruses and Enterovirus 71 (EV71) [30]) infected Human rhabdomyosarcoma and Caco-2 cell lines. The results showed the dose-dependent protective efficacy of L. reuteri Protectis against Coxsackievirus type A (strain 6 and 16) and EV71. In another study by Shih's group [31], probiotic bacteria Enterococcus faecalis successfully reduced the pathogenicity of EV71 and IFV infections in the mice.
Bacillus genus probiotic bacteria are responsible for producing a wide variety of antimicrobial peptides [32]. Following this, Sorokulova's group [17] conducted a study to evaluate the efficacy of the probiotic strain Bacillus subtilis 3 (UCM B-5007) against the influenza virus. Probiotic strain administration resulted in the inhibition of virus replication and increased the survival rate of infected mice. Further, an oral administration of isolated P18 peptide effectively protected 80% of infected mice and significantly lowered viral load in lungs of infected mice. Also, clinical studies on peptide P18 could validate it as a potential antiviral agent.
In an exciting experiment, Kang's group [18] investigated the effect of heat-killed probiotic strain L. casei DK128 against influenza H3N2 virus. Intranasal administration of probiotic strain in BALB/c mice resulted in lower weight loss and 100% survival of the infected mice at the end of the study. They observed lower expression of IL-6 and TNF-α inflammatory cytokines and the reduced virus load in lungs of infected mice. This study suggests that heat-killed probiotic strains can be a promising prospect as an antiviral agent.
Recently, Sharif's group [33] elucidated the role of probiotic Lactobacillus species in macrophages activation against avian influenza virus infection. They administered chicken macrophage cell-line (MQ-NCSU cells) with three Lactobacillus strains (L. acidophilus, L. reuteri, and L. salivarius, respectively) individually or in different combination dosage. As observed, the combination approach induced an antiviral response in the chicken macrophages. It led to a significant reduction in the viral load validated by in vitro model (Madin-Darby canine kidney epithelial cells). Combination dosage is known to increase the expression of inflammatory cytokines (IL-1β, IFN-γ, IFN-α), interferon regulatory factor-7, and 2’, 5’-oligoadenylate synthetase (OAS) genes. These results suggest that Lactobacillus probiotic strains can effectively augment immune responses, crucial for defense mechanisms against viruses. In compliance with this study, Park's group [19] demonstrated that the probiotic strain L. plantarum is effective against influenza A virus (H1N1 and H3N2) infection. Oral administration of heat-killed bacteria led to increased survival rates and significantly reduced virus load in lungs of infected mice.
Miyazaki's group [34] evaluated the efficacy of the probiotic strain L. gasseri SBT2055 against the respiratory syncytial virus. Oral administration of the probiotic strain in mice resulted in reduced proinflammatory cytokines and significantly lowered viral load in the lungs. They also reported that SWI2/SNF2-related CREB-binding protein activator protein (SRCAP) was responsible for virus proliferation. Suppression of SRCAP scaffold protein by the probiotic strain was crucial in inhibiting the virus's binding, leading to a decreased virus load in lungs of infected mice. This recent study provides an insight into the mechanism of probiotic strain as an antiviral agent.
Ghaemi's group [20] elucidated the crucial role of probiotic bacteria B. bifidum in activating immune responses against IFV infection using mice as an animal model. Probiotic bacteria administration elicited cellular and humoral immune responses by increasing lymphocyte proliferation and IgG antibodies (IgG1 and IgG2a), respectively. Higher expression of influenza-specific cytokines IFN-γ, IL-12, and IL-4, along with increased survival rate (~80%) of mice, was also reported. This study sheds light on probiotic bacteria's essential role in activating balanced Th1/Th2 immune responses against viral infection. Apart from preventing respiratory viral infections, probiotics administration was also effective against the Hepatitis C virus, Herpes Simplex Virus type 1, Human immunodeficiency virus, Newcastle disease, and infectious bursal disease viruses [35], [36], [37], [38].
2.2. Clinical studies in human subjects
Probiotic bacteria play a fundamental role in strengthening immune responses and disease relief in the human host by modulating the balance between proinflammatory and anti-inflammatory cytokines [39,40]. Dannelly's group [41] conducted a double-blinded, placebo-controlled trial of the probiotic mixture containing L. paracasei, L. casei 431, and L. fermentum PCC on patients affected with the common cold and influenza-like respiratory infections. In this trial, among 136 subjects enrolled, 68 subjects were administered probiotic combinations, and the remaining 68 were kept on placebo daily for 12 weeks. The probiotic combination reduced the prevalence of common cold and flu-like symptoms by 50% to 60% compared to the placebo group. Subjects also had higher interferon-gamma (IFN-γ) in the serum and sIgA in the gut in the probiotic-treated group. Increased levels of IFN-γ can induce functions of macrophages and exerts different immunomodulatory actions, which may be responsible for reduced flu-like symptoms. Overall, in this study, no side effects were reported, suggesting that probiotics are safe and effective for combating upper respiratory infections. Isolauri's group [42] performed a double-blinded, placebo-controlled trial to investigate probiotics' effect in reducing the risk of acute infections in infants. In this study, infants were administered probiotic strains L. rhamnosus GG and B. lactis Bb-12 daily until they reached 12 months. Indeed, infants receiving probiotic supplementation had a significantly reduced risk (28%) of recurrent respiratory infections than the control group (55%). The similar role of probiotic bacteria strain L. casei DN 114001 in treating antibiotic-associated diarrhea in both children and adults is also seen by Dietrich's group [43]. A double-blind, placebo-controlled study to analyze the effect of probiotic strain B. animalis subsp. lactis BB-12 in reducing the risk of acute infectious diseases in newborn infants also had similar encouraging findings. Out of 109 enrolled infants, 55 were administered probiotic bacteria while 54 were on placebo twice a day up to 8 months. Only 65% of infants in the treated group developed respiratory infections than 94% of infants in the control group. Therefore, infants receiving probiotics had a lower incidence of respiratory diseases [44].
Interestingly, a meta-analysis of 52 randomized controlled trials identified probiotics effective against as many as five diseases, namely acute respiratory tract infections, antibiotic-associated diarrhea, acute infectious diarrhea, infant colic, and necrotizing enterocolitis [45]. It stated that probiotics beneficial effects are through multifactorial mechanisms, including bacterial adhesion inhibition, improved mucosal barrier function, and immune responses modulation. In another meta-analysis of 17 randomized controlled trials, Merenstein's group [46] illustrated that consumption of single or combination dosage of Lactobacillus and Bifidobacterium probiotic strains significantly reduced the prevalence of common acute infections and antibiotics use among infants and children. In a Cochrane Library systematic review, Deng's group [47] reported that probiotic strains (L. rhamnosus, L. plantarum, and B. longum) reduced the risk of ventilator‐associated pneumonia. Another Cochrane review also suggests the crucial role of probiotics in counteracting acute upper respiratory tract infections [48]. Touger-Decker's group [49] conducted a short trial of 12 weeks to evaluate the efficacy of probiotic strains (L. rhamnosus GG and B. lactis Bb-12) in improving the quality of life in patients affected by upper respiratory infections. In this study, 231 subjects were enrolled, out of which 114 subjects were administered probiotic strains, and the remaining 117 subjects received a placebo for 12 weeks. The severity of upper respiratory infections was 34% lower in the probiotic group than the placebo group. Consumption of probiotic dosage also resulted in improved quality of life of patients without any adverse effects. According to the above studies, Zhang's group [50] reported a meta-analysis of 23 randomized controlled trials involving 6269 patients. As noted, subjects supplemented with probiotic strains had a significantly lower risk of respiratory tract infections and improved quality of life than the placebo group subjects.
Recently, He's group [51] conducted a trial on middle-aged and older adults to evaluate the protective effect of yogurt supplemented with probiotic bacteria (L. paracasei N1115) against upper respiratory tract infections. In this study, 233 subjects were randomized in 2 groups to receive either yogurt supplemented with probiotic bacteria (n = 115) or the control group (n = 118) on a regular diet for 12 weeks. Only 30% of the probiotic group subjects were diagnosed with upper respiratory tract infections compared with 44% in the control group. They did not find any significant difference in the CD4+, CD8+, total protein, albumin, and pre-albumin levels between the two groups, albeit the probiotic group showed increased CD3+ cells. Ishikawa's group [52] investigated probiotics efficacy in preventing upper respiratory tract infections in healthy middle-aged office workers. In this study, 96 subjects with age group 30 to 49 years were enrolled, during winter season once daily up to 12 weeks, 49 subjects consumed L. casei strain Shirota-fermented milk and 47 subjects were in control milk group. As reported, respiratory infections were significantly lower (22.4%) in healthy subjects than the 53.2% infection rate in the control group.
Treatment with L. reuteri ATCC 55730 enhanced the mucosal expression level of IL-10 and reduced the inflammatory cytokine expression, including TNF-α, IL-1β, and IL-8 [53]. In another study, Quigley's group [54] demonstrated that administration of probiotic bacteria B. infantis 35624 resulted in immune modulation with a significant reduction in C-reactive protein levels and proinflammatory markers (TNF-α and IL-6) in patients suffering from gastrointestinal tract infections. Bibiloni's group [55] reported the efficacy of VSL#3 in the treatment of patients suffering from clinical remission of ulcerative colitis. VSL#3 is a probiotic mixture of eight strains that modulate the secretion of the anti-inflammatory cytokine, IL-10, and inhibit the secretion of IL-6, IL-8, TNF-α, and IFNγ [56], [57], [58]. Thus, probiotics consumption strengthens gut barrier integrity and improves inflammatory responses by various signaling pathways, which can play a pivotal role in curing or preventing human host diseases.
3. Clinical manifestations of SARS-CoV-2 infection
About SARS-CoV-2, the human-to-human transmission mainly occurs via respiratory droplets [2,64]. During cellular entry, SARS-CoV-2 utilizes its spike (S) glycoprotein to bind with angiotensin-converting enzyme 2 receptors present on human host epithelial cells [9]. The type 2 alveolar epithelial cells present in the human gastrointestinal tract, lungs, heart, and kidney [65]. Thus, type 2 alveolar epithelial cells act as a reservoir for virus proliferation and replication. Human lungs are having large surface areas covered with alveolar epithelial type 2 cells, which could be the reason for its higher vulnerability to COVID-19 infection as compared to other body organs. Coronavirus penetration into the lung tissue is responsible for eliciting local inflammatory responses and the disease's manifestations [65]. Disease progression leads to an imbalance in redox homeostasis and an abrupt increase in free radicals, leading to cell damage [66]. The serum of COVID-19 patients has elevated proinflammatory cytokines TNFα, IFNγ, IL-2, IL-6, IL-7, and granulocyte colony-stimulating factor (GCSF). A few other abnormal findings, such as cellular immune deficiency, renal injury, myocardial injury, hepatic injury, and increased C-reactive protein levels, were observed [67], [68], [69]. Therefore, the induction of proinflammatory “cytokine storm” is the root cause behind chronic inflammation in the human host.
During “cytokine storm,” increased circulating levels of proinflammatory cytokines and chemokines cause acute respiratory distress syndrome. In this scenario, aberrant systemic inflammatory responses are augmented in the human body, which causes damage to multiple organs, including lungs, heart, kidney, and liver, leading to organ-exhaustion and finally death [70,71]. Furthermore, COVID-19 infection is also associated with the gut microbiota's dysbiosis, leading to the abundance of pathogenic bacteria in the human host. Recent studies on COVID-19 patients from Zhejiang province (China) reported gastrointestinal tract infections such as nausea, vomiting, or diarrhea [72]. SARS-CoV-2 viral RNA is detected in the stomach, duodenum, esophagus, rectum, and fecal specimens of patients [9,73]. The abrupt production of cytokines is triggered by COVID-19 disease. Additionally, the mucosa's excessive viral load alters gut microflora, leading to loss of gut barrier integrity and chronic illness in the human host [9,39].
4. Potential preventive application of probiotics in COVID-19 management
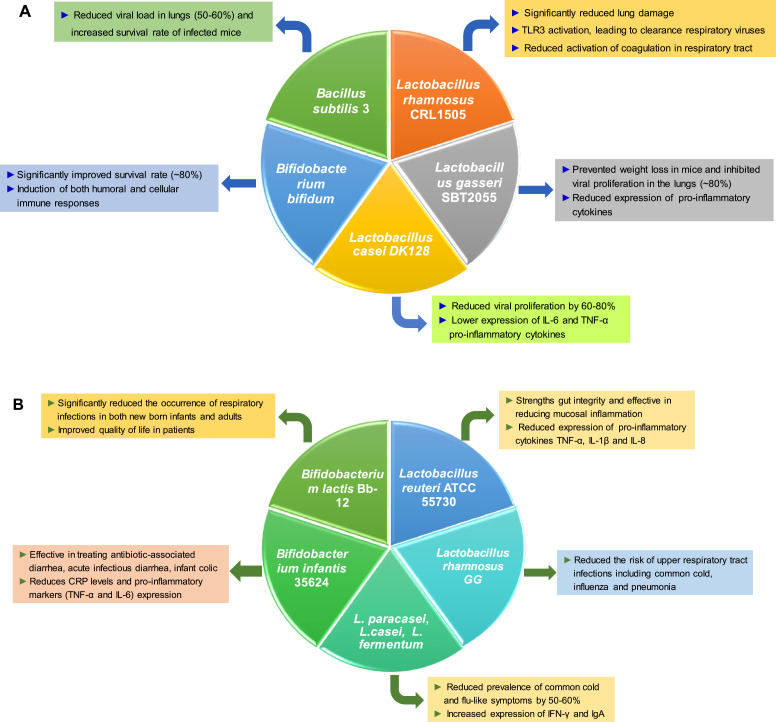
While vaccines and drug regimens to manage COVID-19 are awaited, balancing the immune responses and enhancing host immunity is paramount in this present pandemic scenario. Probiotics consumption increases immunological protection in the human host through balancing immune responses (Th1/Th2) and has a potential role in preventing or alleviating various disease pathologies [74], [75], [76]. Thus, probiotics intervention in managing viral infections like COVID-19 is plausible. As clear from Table 1, probiotic strains belonging to Lactobacillus and Bifidobacterium genera both possess general immune-enhancing and antiviral activities. Upon careful analysis of murine experimental data, survival rate, relative lowering of viral load, relative increase in proinflammatory cytokine levels/ anti-inflammatory cytokine levels, disease symptom alleviation, we identify microbial strains suitable to relieve symptoms typical of COVID 19. According to the literature, L. rhamnosus CRL1505, L. gasseri SBT2055, L. casei DK128, B. bifidum, and B. subtilis 3 appear as promising probiotics to explore further in the management of SARS-CoV-2 infection [17,34]. While L. gasseri SBT2055, L. casei DK128, and B. subtilis 3 strains exhibited the highest survival rate in the mouse model (50-80%), L. rhamnosus CRL1505, L. gasseri SBT2055, and B. bifidum strains induced the most potent anti-inflammatory response [18,[20],27,34]. Insights from clinical studies and human trials suggest that probiotic strains L. rhamnosus GG, L. casei, L. plantarum, L. casei strain Shirota, B. lactis Bb-12, and B. longum significantly reduced the prevalence of upper respiratory infections, common cold, flu-like symptoms, and antibiotic-associated diarrhea by 40% to 70% [42,46,49]. Furthermore, probiotics strains such as L. reuteri ATCC 55730, L. paracasei, L. casei 431, L. fermentum PCC, and B. infantis 35624 were pivotal in producing immunomodulatory responses during various infections [41,51,53]. The snapshot of the efficacy of probiotic strains as antiviral agents is presented in Fig. 1 . As discussed already, SARS-CoV-2 infection leads to a “cytokine storm” that deteriorates patients' lung condition. Therefore, these probiotic strains may facilitate mitigation of “cytokine storm” by balancing cellular and humoral immune responses as seen in experimental animal models. Probiotic bacteria have potential antioxidant activity that may play a crucial role in neutralizing free radical species. As reported, probiotic strains Clostridium butyricum MIYAIRI 588, L. plantarum CAI6, L. rhamnosus GG, and VSL#3 can successfully orchestrate redox homeostasis in the host cell, leading to improved total antioxidant capacity [77,78]. This crucial aspect of probiotic bacteria presents a unique opportunity to manage COVID-19 because redox homeostasis is pivotal in inhibiting disease progression. Therefore, the use of abovementioned probiotic bacteria may be explored against SARS-CoV-2, albeit detailed research with a different combination of probiotic strains and specific effect on the virus is necessary for the implementation.
Fig. 1.
Shortlist of probiotic strains based on preclinical studies on mice (A) and clinical studies in humans (B) of high relevance to COVID-19 infection management.
5. Proposed mechanism(s) of immune-modulation by probiotic bacteria during coronavirus infection
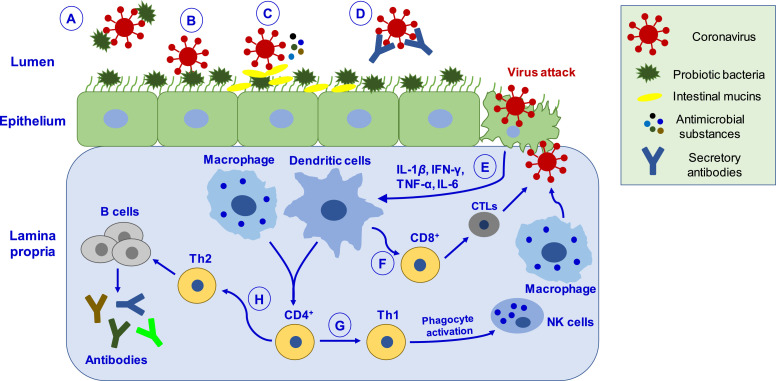
Various experimental studies have demonstrated the beneficial role of probiotic interventions in combating viral infections. The studies have also stated that probiotic bacteria act by multifactorial mechanisms to enhance antiviral immunity in the host (Fig. 2 ). Accordingly, while promising probiotic strains are listed above, it is important to understand the probable mechanism of action of probiotic strains in the cellular milieu. Probiotic bacteria can hinder the adsorption process via directly binding to the virus and inhibiting entry into epithelial cells. In coronavirus, probiotic bacteria can also bind to the mucosal epithelial surfaces, resulting in steric hindrance and blocking the attachment of viruses to angiotensin-converting enzyme 2 like host cell receptor. The colonization of probiotic bacteria plays a pivotal role in improving gut microbiota, strengthening the mucosal barrier, and managing dysbiosis and diarrhea symptoms. Bacteria release diverse substances such as bacteriocins, biosurfactants, lactic acid, hydrogen peroxide, nitric oxide, and organic acids, some or all of which may inhibit virus proliferation [79], [80], [81]. Release of intestinal mucins from mucosal cells and secretory antibodies like IgA can also effectively neutralize the coronavirus attack. Upon virus attack in epithelial cells, probiotic bacteria have a crucial role in antiviral immunity via modulation of host immunological responses, including activation of NK cells, balancing Th1/Th2-mediated immunity, production of inflammatory cytokines, and specific antibodies [82], [83], [84]. Activation of immune response leads to the differentiation of CD8+ T-lymphocytes into cytotoxic T-lymphocytes, capable of destroying virus-infected cells. Next, CD4+ T-lymphocytes cells can differentiate into Th1, which activates phagocytosis through NK cells and macrophages, promoting pathogen killing. Further, CD4+ cells differentiate into Th2 cells, which induce B-cells proliferation, resulting in the production of antibodies that may play a crucial role in combating coronavirus proliferation. Thus, probiotic bacteria may catalyze useful immune responses and improve immune homeostasis in coronavirus-infections.
Fig. 2.
Schematic depiction of putative mechanisms by which probiotics may help manage coronavirus infection. (A) Probiotic bacteria can hinder the adsorption process via directly binding to the virus and inhibiting entry into epithelial cells. (B) Binding of probiotic bacteria to the epithelial surface can cause steric hindrance and block the virus's attachment to the host cell receptor. (C) Probiotic bacteria releases antimicrobial substances (such as bacteriocins, biosurfactants, lactic acid, hydrogen peroxide, nitric oxide, organic acids) and intestinal mucins from mucosal cells, which can effectively inhibit virus proliferation. (D) Virus neutralized by secretory antibodies like IgA. (E) Upon virus attack in epithelial cells, probiotics mediate their antiviral effects by eliciting immune responses by activating macrophages and dendritic cells. (F) Activation of immune response leads to differentiating CD8+ T lymphocytes into CTLs, capable of destroying virus-infected cells. (G) CD4+ T lymphocytes cells differentiate into Th1, which activates phagocytosis through NK cells and macrophages, promoting pathogen killing. (H) CD4+ cells differentiate into Th2 cells, which induce B-cells' proliferation that produces antibodies like IgA, IgG, and IgM. CTLs, cytotoxic T-lymphocytes; Th1, T-helper cells type 1.
6. Conclusions and future perspectives
Respiratory viral infections are one of the fastest escalating global disease burdens with high mortality rates. The disease severity can range from mild upper tract airway infection to severe chronic inflammation of the mucosal layer in the respiratory tract and multiorgan failure in some patients. At this point, the SARS-CoV-2 pandemic has caused severe mortality in several countries, and yet no precise drug regimen is available to the world population. Improving/strengthening human host immunity is one of the best prophylactic approaches to reduce the severity of such viral diseases. Probiotics have numerous benefits such as balancing the composition of human gut microflora, strengthening gut barrier function, and protective immune responses. Therefore, multicentric clinical trials with a large number of COVID-19 patients should be performed, which can provide experimental data regarding the role of probiotics supplementation in disease alleviation and improvement in the quality of life in patients along with current therapy. In this context, this review provides extensive literature-backed evidence of the antiviral efficacy of several probiotic strains.
Many viral infections are associated with dysbiosis of gut microbiota leading to severe gastrointestinal tract infections. Thus, the role of probiotics-based therapy becomes pivotal in the management of viral infections. Probiotics can modulate host immune responses and counteract the “cytokine storm” produced during COVID-19 infection. However, using a probiotics-based strategy against COVID-19 infection in clinical and medicinal fields is still an open research question. How to select bacterial species (alone or in combination dosage) which may serve best against the current pandemic situation? How will human host gut microbiota respond to the new bacterial communities in order to tackle viral infections? How to select standard bacterial species for a population, since various complicated factors, such as age, lifestyle, dietary habits, and genetics, influence the human gut microbiota. Deciphering the microbiota composition of COVID-19 patients is also an essential aspect of such study as it may add new dimensions to unravel the infection mechanism and disease progression.
Acknowledgment
The authors would like to acknowledge CSIR for financial support (Project No. MLP021 and MLP040, ML041). We sincerely thank Dr. Tejinder Kaur for critical reading of the manuscript. The authors declare not conflict of interest.
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet North Am Ed. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hassan SA, Sheikh FN, Jamal S, Ezeh JK, Akhtar A. Coronavirus (covid-19): a review of clinical features, diagnosis, and treatment. Cureus. 2020;12:e7355. doi: 10.7759/cureus.7355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cevik M, Bamford C, Ho A. Covid-19 pandemic-a focused review for clinicians. Clin Microbiol Infect. 2020 doi: 10.1016/j.cmi.2020.04.023. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duan K, Liu B, Li C, Zhang H, Yu T, Qu J, Zhou M, Chen L, Meng S, Hu Y. Effectiveness of convalescent plasma therapy in severe Covid-19 patients. Proc Natl Acad Sci. 2020;117:9490–9496. doi: 10.1073/pnas.2004168117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu H. Drug treatment options for the 2019-new coronavirus (2019-ncov) Bioscience trends. 2020;14:69–71. doi: 10.5582/bst.2020.01020. [DOI] [PubMed] [Google Scholar]
- 6.Shanmugaraj B, Siriwattananon K, Wangkanont K, Phoolcharoen W. Perspectives on monoclonal antibody therapy as potential therapeutic intervention for coronavirus disease-19 (COVID-19) Asian Pac J Allergy Immunol. 2020;38:10–18. doi: 10.12932/AP-200220-0773. [DOI] [PubMed] [Google Scholar]
- 7.Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-ncov) in vitro. Cell Res. 2020;30:269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sadiq FA. Is it time for microbiome-based therapies in viral infections? Virus Res. 2020;291 doi: 10.1016/j.virusres.2020.198203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Antunes AEC, Vinderola G, Xavier-Santos D, Sivieri K. Potential contribution of beneficial microbes to face the covid-19 pandemic. Food Res Int. 2020;136 doi: 10.1016/j.foodres.2020.109577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, et al: Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis 2020:https://doi.org/ 10.1016/S1473-3099(1020)30243-30247. [DOI] [PMC free article] [PubMed]
- 11.Munoz-Carrillo JL, Contreras-Cordero JF, Gutiarrez-Coronado O, Villalobos-Gutiarrez PT, Ramos-Gracia LG, VE Hernaindez-Reyes. Cytokine profiling plays a crucial role in activating immune system to clear infectious pathogens; Immune response activation and immunomodulation. IntechOpen. 2018 doi: 10.5772/intechopen.80843. [DOI] [Google Scholar]
- 12.Cytokines in the balance. Nat Immunol. 2020;20:1557. doi: 10.1038/s41590-019-0557-0. [DOI] [PubMed] [Google Scholar]
- 13.Wieers G, Belkhir L, Enaud R, Leclercq S, Philippart de Foy J-M, et al. How probiotics affect the microbiota. Front Cell Infect Microbiol. 2020;9:454. doi: 10.3389/fcimb.2019.00454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hardy H, Harris J, Lyon E, Beal J. Probiotics, prebiotics and immunomodulation of gut mucosal defences: homeostasis and immunopathology. Nutrients. 2013;5:1869–1912. doi: 10.3390/nu5061869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al Kassaa I. Springer; 2017. New insights on antiviral probiotics: From research to applications. [Google Scholar]
- 16.Kawashima T, Hayashi K, Kosaka A, Kawashima M, Igarashi T, Tsutsui H, et al. Lactobacillus plantarum strain yu from fermented foods activates Th1 and protective immune responses. Int Immunopharmacol. 2011;11:2017–2024. doi: 10.1016/j.intimp.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 17.Starosila D, Rybalko S, Varbanetz L, Ivanskaya N, Sorokulova I. Anti-influenza activity of a Bacillus subtilis probiotic strain. Antimicrob Agents Chemother. 2017;61 doi: 10.1128/AAC.00539-17. e00539-00517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jung Y-J, Lee Y-T, Le Ngo V, Cho Y-H, Ko E-J, Hong S-M, et al. Heat-killed Lactobacillus casei confers broad protection against influenza a virus primary infection and develops heterosubtypic immunity against future secondary infection. Sci Rep. 2017;7:1–12. doi: 10.1038/s41598-017-17487-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park S, Kim JI, Bae J-Y, Yoo K, Kim H, Kim I-H, et al. Effects of heat-killed Lactobacillus plantarum against influenza viruses in mice. J Microbiol. 2018;56:145–149. doi: 10.1007/s12275-018-7411-1. [DOI] [PubMed] [Google Scholar]
- 20.Mahooti M, Abdolalipour E, Salehzadeh A, Mohebbi SR, Gorji A, Ghaemi A. Immunomodulatory and prophylactic effects of Bifidobacterium bifidum probiotic strain on influenza infection in mice. World J Microbiol Biotechnol. 2019;35:91–98. doi: 10.1007/s11274-019-2667-0. [DOI] [PubMed] [Google Scholar]
- 21.Lehtoranta L, Pitkaranta A, Korpela R. Probiotics in respiratory virus infections. Eur J Clin Microbiol Infect Dis. 2014;33:1289–1302. doi: 10.1007/s10096-014-2086-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Botic T, Dana¸ T, Weingartl H, Cencia A. A novel eukaryotic cell culture model to study antiviral activity of potential probiotic bacteria. Int J Food Microbiol. 2007;115:227–234. doi: 10.1016/j.ijfoodmicro.2006.10.044. [DOI] [PubMed] [Google Scholar]
- 23.Kanauchi O, Andoh A, AbuBakar S, Yamamoto N. Probiotics and paraprobiotics in viral infection: clinical application and effects on the innate and acquired immune systems. Curr Pharm Des. 2018;24:710–717. doi: 10.2174/1381612824666180116163411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Youn H-N, Lee D-H, Lee Y-N, Park J-K, Yuk S-S, et al. Intranasal administration of live Lactobacillus species facilitates protection against influenza virus infection in mice. Antiviral Res. 2012;93:138–143. doi: 10.1016/j.antiviral.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 25.Kechaou N, Chain F, Gratadoux J-J, Sb Blugeon, Bertho N, Chevalier C, et al. Identification of one novel candidate probiotic Lactobacillus plantarum strain active against influenza virus infection in mice by a large-scale screening. Appl Environ Microbiol. 2013;79:1491–1499. doi: 10.1128/AEM.03075-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goto H, Sagitani A, Ashida N, Kato S, Hirota T, Shinoda T, et al. Anti-influenza virus effects of both live and non-liveLactobacillus acidophilus l-92 accompanied by the activation of innate immunity. Br J Nutr. 2013;110:1810–1818. doi: 10.1017/S0007114513001104. [DOI] [PubMed] [Google Scholar]
- 27.Nakayama Y, Moriya T, Sakai F, Ikeda N, Shiozaki T, Hosoya T, et al. Oral administration of Lactobacillus gasseri SBT2055 is effective for preventing influenza in mice. Sci Rep. 2014;4:4638. doi: 10.1038/srep04638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee HA, Kim H, Lee K-W, Park K-Y. Dead nano-sized Lactobacillus plantarum inhibits azoxymethane/dextran sulfate sodium-induced colon cancer in balb/c mice. J Med Food. 2015;18:1400–1405. doi: 10.1089/jmf.2015.3577. [DOI] [PubMed] [Google Scholar]
- 29.Song JA, Kim HJ, Hong SK, Lee DH, Lee SW, Song CS, et al. Oral intake of Lactobacillus rhamnosus M21 enhances the survival rate of mice lethally infected with influenza virus. J Microbiol Immunol Infect. 2016;49:16–23. doi: 10.1016/j.jmii.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 30.Ang LYE, Too HKI, Tan EL, Chow T-KV, Shek P-CL, Tham E, et al. Antiviral activity of Lactobacillus reuteri protectis against coxsackievirus a and enterovirus 71 infection in human skeletal muscle and colon cell lines. Virol J. 2016;13:111. doi: 10.1186/s12985-016-0567-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen MF, Weng KF, Huang SY, Liu YC, Tseng SN, Ojcius DM, et al. Pretreatment with a heat-killed probiotic modulates monocyte chemoattractant protein-1 and reduces the pathogenicity of influenza and enterovirus 71 infections. Mucosal Immunol. 2017;10:215–227. doi: 10.1038/mi.2016.31. [DOI] [PubMed] [Google Scholar]
- 32.Sumi CD, Yang BW, Yeo I-C, Hahm YT. Antimicrobial peptides of the genus Bacillus: a new era for antibiotics. Can J Microbiol. 2015;61:93–103. doi: 10.1139/cjm-2014-0613. [DOI] [PubMed] [Google Scholar]
- 33.Shojadoost B, Kulkarni RR, Brisbin JT, Quinteiro-Filho W, Alkie TN, Sharif S. Interactions between Lactobacilli and chicken macrophages induce antiviral responses against avian influenza virus. Res Vet Sci. 2019;125:441–450. doi: 10.1016/j.rvsc.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 34.Eguchi K, Fujitani N, Nakagawa H, Miyazaki T. Prevention of respiratory syncytial virus infection with probiotic lactic acid bacterium Lactobacillus gasseri SBT2055. Sci Rep. 2019;9:1–11. doi: 10.1038/s41598-019-39602-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.An HM, Lee DK, Kim JR, Lee SW, Cha MK, Lee KO, et al. Antiviral activity of Bifidobacterium adolescentis SPM 0214 against herpes simplex virus type 1. Arch Pharm Res. 2012;35:1665–1671. doi: 10.1007/s12272-012-0918-9. [DOI] [PubMed] [Google Scholar]
- 36.Abdelhamid AG, El-Masry SS, El-Dougdoug NK. Probiotic Lactobacillus and Bifidobacterium strains possess safety characteristics, antiviral activities and host adherence factors revealed by genome mining. EPMA J. 2019;10:337–350. doi: 10.1007/s13167-019-00184-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patel AR, Shah NP, Prajapati JB. Immunomodulatory effects of probiotics in the treatment of human immunodeficiency virus (HIV) infection. Biomed Prevent Nutr. 2014;4:81–84. [Google Scholar]
- 38.Allam NG, Salem ML, Elbatae H, Nabieh MM. Lactobacillus acidophilus and bifidobacteria spp having antibacterial and antiviral effects on chronic hcv infection. African J Microbiol Res. 2019;13:77–90. [Google Scholar]
- 39.Infusino F, Marazzato M, Mancone M, Fedele F, Mastroianni CM, Severino P, et al. Diet supplementation, probiotics, and nutraceuticals in sars-cov-2 infection: a scoping review. Nutrients. 2020;12:1–21. doi: 10.3390/nu12061718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sundararaman A, Ray M, Ravindra PV, Halami PM. Role of probiotics to combat viral infections with emphasis on COVID-19. Appl Microbiol Biotechnol. 2020;104:8089–8104. doi: 10.1007/s00253-020-10832-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang H, Yeh C, Jin Z, Ding L, Liu BY, Zhang L, et al. Prospective study of probiotic supplementation results in immune stimulation and improvement of upper respiratory infection rate. Synth Systems Biotechnol. 2018;3:113–120. doi: 10.1016/j.synbio.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rautava S, Salminen S, Isolauri E. Specific probiotics in reducing the risk of acute infections in infancy–a randomised, double-blind, placebo-controlled study. Br J Nutr. 2009;101:1722–1726. doi: 10.1017/S0007114508116282. [DOI] [PubMed] [Google Scholar]
- 43.Dietrich CG, Kottmann T, Alavi M. Commercially available probiotic drinks containing Lactobacillus casei DN-114001 reduce antibiotic-associated diarrhea. World J Gastroenterol. 2014;20:15837–15844. doi: 10.3748/wjg.v20.i42.15837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Taipale T, Pienihakkinen K, Isolauri E, Larsen C, Brockmann E, Alanen P, et al. Bifidobacterium animalis subsp. Lactis bb-12 in reducing the risk of infections in infancy. Br J Nutr. 2011;105:409–416. doi: 10.1017/S0007114510003685. [DOI] [PubMed] [Google Scholar]
- 45.Liu Y, Tran DQ, Rhoads JM. Probiotics in disease prevention and treatment. J Clin Pharmacol. 2018;58:S164–S179. doi: 10.1002/jcph.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.King S, Tancredi D, Lenoir-Wijnkoop I, Gould K, Vann H, Connors G, et al. Does probiotic consumption reduce antibiotic utilization for common acute infections? A systematic review and meta-analysis. Eur J Public Health. 2019;29:494–499. doi: 10.1093/eurpub/cky185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bo L, Li J, Tao T, Bai Y, Ye X, Hotchkiss RS, et al. Probiotics for preventing ventilator-associated pneumonia. Cochrane Database Syst Rev. 2014;11 doi: 10.1002/14651858.CD009066.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saeterdal I, Underland V, Nilsen ES. The effect of probiotics for preventing acute upper respiratory tract infections. Glob Adv Health Med. 2012;1:124–125. doi: 10.7453/gahmj.2012.1.2.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smith TJ, Rigassio-Radler D, Denmark R, Haley T, Touger-Decker R. Effect of Lactobacillus rhamnosus LGG(r) and Bifidobacterium animalis ssp. lactis bb-12(r) on health-related quality of life in college students affected by upper respiratory infections. Br J Nutr. 2013;109:1999–2007. doi: 10.1017/S0007114512004138. [DOI] [PubMed] [Google Scholar]
- 50.Wang Y, Li X, Ge T, Xiao Y, Liao Y, Cui Y, et al. Probiotics for prevention and treatment of respiratory tract infections in children: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2016;95:e4509. doi: 10.1097/MD.0000000000004509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pu F, Guo Y, Li M, Zhu H, Wang S, Shen X, et al. Yogurt supplemented with probiotics can protect the healthy elderly from respiratory infections: a randomized controlled open-label trial. Clin Interv Aging. 2017;12:1223–1231. doi: 10.2147/CIA.S141518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shida K, Sato T, Iizuka R, Hoshi R, Watanabe O, Igarashi T, et al. Daily intake of fermented milk with Lactobacillus casei strain shirota reduces the incidence and duration of upper respiratory tract infections in healthy middle-aged office workers. Eur J Nutr. 2017;56:45–53. doi: 10.1007/s00394-015-1056-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oliva S, Di Nardo G, Ferrari F, Mallardo S, Rossi P, Patrizi G, et al. Randomised clinical trial: the effectiveness of Lactobacillus reuteri ATCC 55730 rectal enema in children with active distal ulcerative colitis. Aliment Pharmacol Ther. 2012;35:327–334. doi: 10.1111/j.1365-2036.2011.04939.x. [DOI] [PubMed] [Google Scholar]
- 54.Groeger D, O'Mahony L, Murphy EF, Bourke JF, Dinan TG, et al. Bifidobacterium infantis 35624 modulates host inflammatory processes beyond the gut. Gut Microbes. 2013;4:325–339. doi: 10.4161/gmic.25487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bibiloni R, Fedorak RN, Tannock GW, Madsen KL, Gionchetti P, Campieri M, et al. VSL#3 probiotic-mixture induces remission in patients with active ulcerative colitis. Am J Gastroenterol. 2005;100:1539–1546. doi: 10.1111/j.1572-0241.2005.41794.x. [DOI] [PubMed] [Google Scholar]
- 56.Chapman TM, Plosker GL, Figgitt DP. VSL#3 probiotic mixture: a review of its use in chronic inflammatory bowel diseases. Drugs. 2006;66:1371–1387. doi: 10.2165/00003495-200666100-00006. [DOI] [PubMed] [Google Scholar]
- 57.Isidro RA, Lopez A, Cruz ML, Gonzalez Torres MI, Chompre G, Isidro AA, et al. The probiotic VSL#3 modulates colonic macrophages, inflammation, and microflora in acute trinitrobenzene sulfonic acid colitis. J Histochem Cytochem. 2017;65:445–461. doi: 10.1369/0022155417718542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hui W, Shuhua LI, Houzhong LI, Fengxia DU, Jie G, Yanmin WU. Mechanism of probiotic VSL#3 inhibiting nf-κb and tnf-α on colitis through tlr4-nf-κb signal pathway. Iran J Public health. 2019;48:1292. [PMC free article] [PubMed] [Google Scholar]
- 59.Izumo T, Maekawa T, Ida M, Noguchi A, Kitagawa Y, Shibata H, et al. Effect of intranasal administration of Lactobacillus pentosus s-pt84 on influenza virus infection in mice. Int Immunopharmacol. 2010;10:1101–1106. doi: 10.1016/j.intimp.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 60.Kawase M, He F, Kubota A, Harata G, Hiramatsu M. Oral administration ofLactobacilli from human intestinal tract protects mice against influenza virus infection. Lett Appl Microbiol. 2010;51:6–10. doi: 10.1111/j.1472-765X.2010.02849.x. [DOI] [PubMed] [Google Scholar]
- 61.Kobayashi N, Saito T, Uematsu T, Kishi K, Toba M, Kohda N, et al. Oral administration of heat-killed Lactobacillus pentosus strain b240 augments protection against influenza virus infection in mice. Int Immunopharmacol. 2011;11:199–203. doi: 10.1016/j.intimp.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 62.Kwak M-K, Liu R, Kwon J-O, Kim M-K, Kim AH, Kang S-O. Cyclic dipeptides from lactic acid bacteria inhibit proliferation of the influenza a virus. J Microbiol. 2013;51:836–843. doi: 10.1007/s12275-013-3521-y. [DOI] [PubMed] [Google Scholar]
- 63.Zelaya H, Tsukida K, Chiba E, Marranzino G, Alvarez S, Kitazawa H, et al. Immunobiotic lactobacilli reduce viral-associated pulmonary damage through the modulation of inflammation-coagulation interactions. Int Immunopharmacol. 2014;19:161–173. doi: 10.1016/j.intimp.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 64.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. StatPearls Publishing; 2020. Features, evaluation and treatment coronavirus (COVID-19); Statpearls [internet. [PubMed] [Google Scholar]
- 65.Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from wuhan: an analysis based on decade-long structural studies of sars coronavirus. J Virol. 2020;94 doi: 10.1128/JVI.00127-20. e00127-00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Delgado-Roche L, Mesta F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch Med Res. 2020 doi: 10.1016/j.arcmed.2020.1004.1019. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet North Am Ed. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. Covid-19: consider cytokine storm syndromes and immunosuppression. Lancet North Am Ed. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020:1–3. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of covid-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The cytokine storm in covid-19: an overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor Rev. 2020 doi: 10.1016/j.cytogfr.2020.05.003. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jin X, Lian JS, Hu JH, Gao J, Zheng L, Zhang YM, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (Covid-19) with gastrointestinal symptoms. Gut. 2020;69:1002–1009. doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zuo T, Zhang F, Lui GCY, Yeoh YK, Li AYL, Ng SC. Alterations in gut microbiota of patients with covid-19 during time of hospitalization. Gastroenterology. 2020;159:944–955. doi: 10.1053/j.gastro.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kitazawa H, Villena J. Modulation of respiratory tlr3-anti-viral response by probiotic microorganisms: Lessons learned from Lactobacillus rhamnosus CRL1505. Front Immunol. 2014;5:201. doi: 10.3389/fimmu.2014.00201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Azad M, Kalam A, Sarker M, Wan D. Immunomodulatory effects of probiotics on cytokine profiles. Biomed Res Int. 2018;2018:1–10. doi: 10.1155/2018/8063647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zeng W, Shen J, Bo T, Peng L, Xu H, Nasser MI, et al. Cutting edge: probiotics and fecal microbiota transplantation in immunomodulation. J Immunol Res. 2019;2019:1–17. doi: 10.1155/2019/1603758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang Y, Wu Y, Wang Y, Xu H, Mei X, Yu D, et al. Antioxidant properties of probiotic bacteria. Nutrients. 2017;9:521. doi: 10.3390/nu9050521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mishra V, Shah C, Mokashe N, Chavan R, Yadav H, Prajapati J. Probiotics as potential antioxidants: a systematic review. J Agric Food Chem. 2015;63:3615–3626. doi: 10.1021/jf506326t. [DOI] [PubMed] [Google Scholar]
- 79.Servin AL. Antagonistic activities of Lactobacilli and Bifidobacteria against microbial pathogens. FEMS Microbiol Rev. 2004;28:405–440. doi: 10.1016/j.femsre.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 80.Choi H-J, Song J-H, Ahn Y-J, Baek S-H, Kwon D-H. Antiviral activities of cell-free supernatants of yogurts metabolites against some rna viruses. Eur Food Res Technol. 2009;228:945–950. [Google Scholar]
- 81.Pipenbaher Na, Moeller PL, DolinÅ¡ek J, Jakobsen M, Weingartl H, CenciÄ A. Nitric oxide (no) production in mammalian non-tumorigenic epithelial cells of the small intestine and macrophages induced by individual strains of Lactobacilli and Bifidobacteria. Int Dairy J. 2009;19:166–171. [Google Scholar]
- 82.Veckman V, Miettinen M, Pirhonen J, Siran J, Matikainen S, Julkunen I. Streptococcus pyogenes and Lactobacillus rhamnosus differentially induce maturation and production of th1-type cytokines and chemokines in human monocyte-derived dendritic cells. J Leukoc Biol. 2004;75:764–771. doi: 10.1189/jlb.1003461. [DOI] [PubMed] [Google Scholar]
- 83.Weiss G, Rasmussen S, Zeuthen LH, Nielsen BN, Jarmer H, Jespersen L, et al. Hanne: Lactobacillus acidophilus induces virus immune defence genes in murine dendritic cells by a toll-like receptor-2-dependent mechanism. Immunology. 2010;131:268–281. doi: 10.1111/j.1365-2567.2010.03301.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Latvala S, Miettinen M, Kekkonen R, Korpela R, Julkunen I. Potentially probiotic bacteria induce cytokine production and suppressor of cytokine signaling 3 gene expression in human monocyte-derived macrophages. Cytokine. 2009;48:100–101. [Google Scholar]