Abstract
Objective
The study sought to examine the effects of technology-supported exercise programs on the knee pain, physical function, and quality of life of individuals with knee osteoarthritis and/or chronic knee pain by a systematic review and meta-analysis of randomized controlled trials.
Materials and Methods
We searched MEDLINE, EMBASE, CINAHL Plus, and the Cochrane Library from database inception to August 2020. A meta-analysis and subgroup analyses, stratified by technology type and program feature, were conducted.
Results
Twelve randomized controlled trials were reviewed, all of which implemented the programs for 4 weeks to 6 months. Telephone, Web, mobile app, computer, and virtual reality were used to deliver the programs. The meta-analysis showed that these programs were associated with significant improvements in knee pain (standardized mean difference [SMD] = −0.29; 95% confidence interval [CI], −0.48 to −0.10; P = .003) and quality of life (SMD = 0.25; 95% CI, 0.04 to 0.46; P = .02) but not with significant improvement in physical function (SMD = 0.22; 95% CI, 0 to 0.43; P = .053). Subgroup analyses showed that some technology types and program features were suggestive of potential benefits.
Conclusions
Using technology to deliver the exercise programs appears to offer benefits. The technology types and program features that were associated with health values have been identified, based on which suggestions are discussed for the further research and development of such programs.
Keywords: knee osteoarthritis, knee pain, exercise therapy, systematic review, meta-analysis
INTRODUCTION
Knee osteoarthritis (OA) often causes chronic knee pain1,2 and is a prevalent musculoskeletal disorder that affects many people, especially the elderly.3–9 Both knee OA and chronic knee pain are leading causes of disability that substantially decrease the quality of life and well-being of afflicted individuals.5,10,11 With a rapidly aging population, these health issues are becoming more significant.12 Thus, effective approaches are needed to facilitate treatment and care for those suffering from knee OA and/or chronic knee pain.
Exercise therapy is one of the most common and effective management strategies for these problems.13 Several care guidelines suggest exercise as a first-line treatment for knee OA and chronic knee pain.12–20 However, the conventional delivery of exercise therapy usually requires patients to participate in face-to-face exercise at clinics, which involves a time commitment, motivation, and a monetary cost, or requires patients to perform prescribed exercise in their home with limited supervision and access to resources, which can lead to poor exercise adherence and performance.21–23
In recent years, technologies have been adopted to surmount these barriers. For example, telephones are used for remote consultations between patients and physical therapists. In addition, multifeatured Web and mobile app integrated with motion- and physical activity–tracking sensors have been developed for the management of exercise progress and health conditions. Some treatment approaches use exercise games, delivered by computer, video game console, or virtual reality, to improve patients’ interactions with and engagement in exercise therapy.24,25 The support of such technologies is increasing the accessibility, affordability, and attractiveness of exercise programs to treat knee OA and chronic knee pain.
As a result of the growing interest in such technology-supported exercise programs for knee OA and/or chronic knee pain, a number of randomized controlled trials (RCTs) have been conducted to examine their effects. However, the studies reported mixed results, for which a review and meta-analysis study can be useful for obtaining more precise estimates and a better understanding of the effects of these programs. Although there is a previous review that has focused on those with knee OA, its study sample also included patients with hip OA, and thus its findings may not be specific to those with knee problems.26 In addition, the effects of programs may vary by technology type, which means that a comparison of the treatment effects of programs based on different technologies is important. Moreover, several program features have been designed to facilitate and encourage individuals to perform exercise, such as video-based exercise demonstration, sensor-based motion and physical activity tracking, and educational materials,27 but the independent effects of these features have yet to be assessed. Finally, several RCTs have been published recently28–32 and have yet to be reviewed. We therefore performed a systematic review and meta-analysis to investigate whether technology-supported exercise programs were effective interventions for a large population with knee OA and/or chronic knee pain. Our aim was to determine whether technology-supported exercise programs were associated with the improvements in the following 3 outcomes that are significant to knee OA and/or chronic knee pain: (1) knee pain, (2) physical function, and (3) quality of life.
MATERIALS AND METHODS
This study was registered with PROSPERO (CRD42020202854) and followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.33 The literature search, screening of studies, data extraction, and quality assessment were performed independently by the 2 authors (T.C. and J.C.), and disagreements were resolved by discussion to reach a consensus.
Literature search and study selection
On August 5, 2020, we searched MEDLINE via Ovid (from 1946 to present), EMBASE via Ovid (from 1974 to present), CINAHL Plus via EBSCOhost (from 1937 to present), and the Cochrane Library (no date restriction) to identify relevant studies, without language restrictions. The search used both Medical Subject Headings and free-text words related to knee OA, knee pain, exercise therapy, supporting technology, the outcomes of interest to this review, as well as the Cochrane Highly Sensitive Search Strategy to identify RCTs (see Supplementary Appendix 1 for the search details). Duplicate citations were removed using EndNote and by manual screening. We first screened the titles and abstracts, then reviewed the full texts of potentially relevant citations to determine whether they should be included in the analysis. Finally, the reference lists of the identified RCTs and relevant reviews were manually searched to identify any studies that had been missed and warranted inclusion.
Inclusion and exclusion criteria
Studies were included for review if they (1) were RCTs; (2) included adults (≥18 years of age); (3) included individuals who had a diagnosis of knee OA or had chronic knee pain for at least 1 month in the last 12 months prior to the studies; (4) examined the effects of technology-supported exercise programs on knee pain, physical function, or quality of life; (5) were written in English; and (6) were published in peer-reviewed journals. Review articles and case reports were excluded.
Data extraction
Two authors (T.C. and J.C.) used a standardized form to independently extract data on the studies’ characteristics, the details of the technology-supported exercise programs, and the statistical results. The outcomes of interest were changes in knee pain, physical function, and quality of life from baseline to the end of the implementation period of the intervention. We compared the differences in the changes between the intervention and control groups to determine the effects of technology-supported exercise programs.
Assessment of risk of bias
The methodological quality of each included RCT was assessed independently by T.C. and J.C. using the Cochrane risk-of-bias tool.34 Seven aspects were assessed, as follows: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias. Each RCT was assessed as having a low risk of bias, a high risk of bias, or an unclear risk of bias.
Data analysis
A meta-analysis was conducted to examine the main effects. We pooled data across RCTs using random effects models and calculated the standardized mean difference (SMD) for each outcome. The I2 statistic was used to measure heterogeneity, where an I2 of 0%-50% indicated low to moderate heterogeneity, an I2 of 50%-75% indicated substantial heterogeneity, and an I2 of 75%-100% indicated considerable heterogeneity.34 Egger’s regression test was used to assess the possibility of publication bias.35 In addition, subgroup analyses were conducted, stratified by (1) the types of technology used to deliver the exercise programs and (2) the program features involved in the programs that were designed to facilitate and encourage participants to perform exercise.
Assessment of quality of evidence
The quality of evidence for each outcome was assessed using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach.36 For each of the outcomes, the quality of evidence was downgraded by 1 level from high quality for each serious problem found in the domains of risk of bias, inconsistency, indirectness, imprecision, and publication bias.
RESULTS
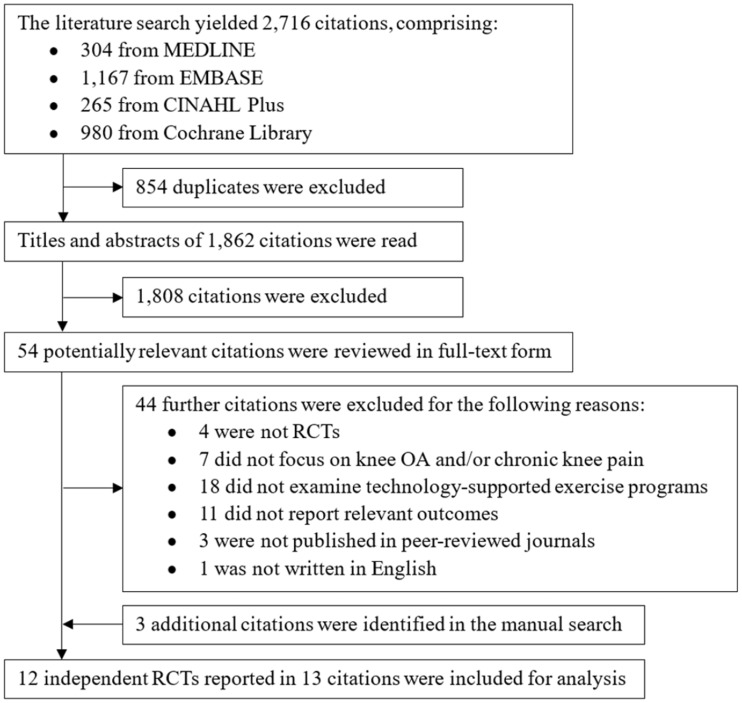
Figure 1 illustrates the literature search and selection process. Thirteen studies were identified as being eligible,28–32,37–44 but the findings reported in 2 of them41,42 were obtained from the same RCT. Therefore, the final analysis of this review comprised only 12 independent RCTs.
Figure 1.
The randomized controlled trial (RCT) selection process. OA: osteoarthritis.
Characteristics of the RCTs analyzed
The characteristics of the 12 RCTs are summarized in Table 1 (see Supplementary Appendix 2 for detailed information). All of the RCTs implemented the technology-supported exercise programs for a short period (4 weeks to 6 months). During the intervention period, the participants in the intervention group were encouraged to perform exercise at least 3 times per week, and 7 RCTs29–31,37–39,41,42 also delivered biweekly to monthly consultation with physical therapists for exercise advice. In the control groups, participants in 6 RCTs received conventional care, such as face-to-face physical therapy28,37,41,42,44 or educational materials for OA management (eg, presented in brochures and booklets),32,38 and those in the other 6 RCTs29–31,39,40,43 received minimal or no care.
Table 1.
Summary of characteristics of the 12 RCTs
| RCT characteristics | |
|---|---|
| Year of publication, n (%) | |
| Before 2010 | 1 (8.3)40 |
| 2010–2014 | 2 (16.7)41,42,44,a |
| 2015–2019 | 9 (75.0)28–32,37–39,43 |
| Region where the RCT took place, n (%) | |
| North America | 6 (50.0)28,30–32,39,43 |
| Asia | 2 (16.7)40,44 |
| Oceania | 3 (25.0)29,37,38 |
| Africa | 1 (8.3)41,42,a |
| Sample size | |
| Median (range) | 105 (34-282) |
| Age of the sample, years | |
| Mean (range) | 61.30 (46.4-75.3) |
| Knee problems examined, n (%) | |
| Knee osteoarthritis | 6 (50.0)28,37,40–44,a |
| Knee osteoarthritis and chronic knee pain | 1 (8.3)29 |
| Knee osteoarthritis or chronic knee pain | 3 (25.0)30,31,39 |
| Chronic knee pain | 2 (16.7)32,38 |
| Intervention duration, n (%) | |
| <3 months | 5 (41.7)31,39–42,44,a |
| 3-6 months | 7 (58.3)28–30,32,37,38,43 |
| Technology used to support the delivery of exercise programs, n (%) | |
| Telephone | 6 (50.0)29–31,37,39,41,42,a |
| Web | 2 (16.7)28,38 |
| Mobile app | 2 (16.7)32,43 |
| Computer | 1 (8.3)40 |
| Virtual reality | 1 (8.3)44 |
| Program features involved to facilitate and encourage exercise performance, n (%) | |
| Individualized exercise recommendation | 8 (75.0)28–31,37–39,43 |
| Video-based exercise demonstration | 4 (33.3)28,29,32,38 |
| Sensor-based motion and physical activity tracking | 7 (58.3)30–32,39,40,43,44 |
| Monitoring of exercise progression | 9 (75.0)28–32,37–39,41,42,a |
| Educational materials | 9 (75.0)28–32,37–39,43 |
| Reminder to perform exercise | 3 (25.0)28,32,38 |
Five types of technology were used to deliver exercise programs. Telephone was the most frequently used technology for remote exercise training and monitoring, with 2 RCTs37,41,42 using telephone only and the other 429–31,39 using telephone as a primary tool, complemented by the use of Web-based exercise videos or daily records of physical activity. Web and mobile app were used to deliver self-management programs, as well as for communication with physical therapists via videoconferencing. Interactive exercise games were developed with the support of computer and virtual reality. In addition, we also identified 6 program features that were used to facilitate and encourage participants to perform exercise (see Supplementary Appendix 3 for the details of the program features in each RCT).
Risk of bias assessment
The results of the risk of bias assessment are shown in Figure 2. The details of the random-sequence generation were not reported in 2 (16.7%) RCTs. It was unclear whether allocation concealment was adequate in 5 (41.7%) RCTs. A lack of or the partial blinding of participants and healthcare providers was identified in 11 (91.7%) RCTs, and it was unclear whether the outcome assessors were blinded in 8 (66.7%) RCTs. Attrition bias was detected in 1 (8.3%) RCT, as the dropout rate was > 50%. Reporting and other sources of bias were not identified in any of the 12 RCTs.
Figure 2.
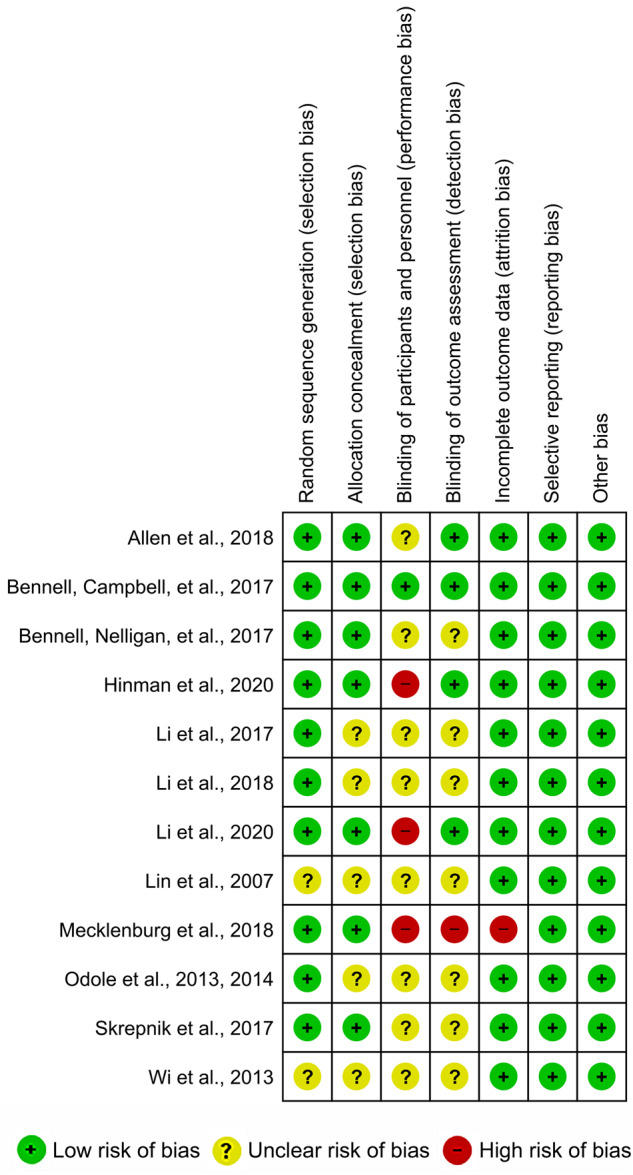
Risk of bias summary for the 12 randomized controlled trials.
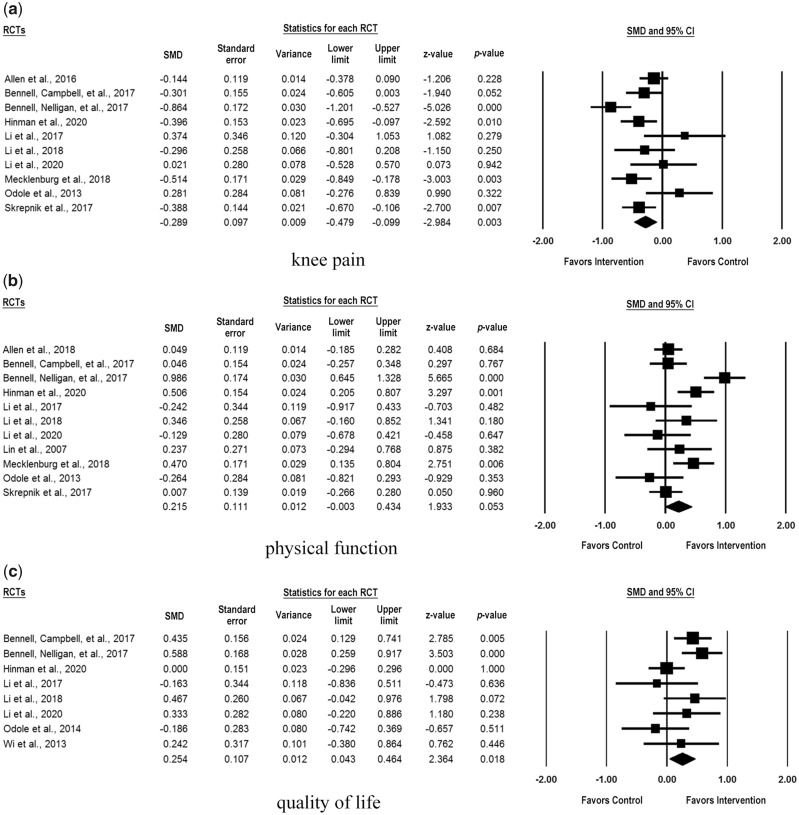
Meta-analysis of effects of technology-supported exercise programs
The meta-analysis results are presented in Table 2. Compared with the use of nontechnological or no care services in the control groups, the short-term implementation of technology-supported exercise programs was found to be associated with a significant reduction in knee pain (SMD = −0.29; 95% confidence interval [CI], −0.48 to −0.10; P = .003). Based on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale, which was most frequently reported in the 10 RCTs that examined knee pain, and a previously reported standard deviation resulted from the typical knee pain population,45,46 the observed SMD of –0.29 can be translated to a WOMAC pain change of –1.31 points on the 0-20 scale, which can be considered clinically important.47 For quality of life, a statistically significant improvement was detected (SMD = 0.25; 95% CI, 0.04 to 0.46; P = .02), and the observed SMD represented an improvement of 4.80 points on the most frequently reported 100-point Knee Injury and Osteoarthritis Outcome Score quality-of-life subscale, which is lower than the suggested minimal clinically important difference.48,49 However, we did not find evidence for a significant improvement in physical function (SMD = 0.22; 95% CI, 0 to 0.43; P = .053). No publication bias was detected, according to Egger’s regression test. The quality of evidence across all of the RCTs for quality of life was high, while that for knee pain and physical function was moderate due to substantial heterogeneity (I2 > 50%). Forest plots for the outcomes are presented in Figure 3.
Table 2.
Meta-analysis results of the effects of technology-supported exercise programs
| Outcome | Number of RCTs | Sample Size | SMD (95% CI) | P Value | I 2 (%) | Egger’s Regression Test |
Quality of Evidence (GRADE) | |
|---|---|---|---|---|---|---|---|---|
| t Value | P Value | |||||||
| Knee paina | 10 | 1335 | −0.29 (−0.48 to −0.10) | .003 | 62 | 1.20 | .26 | ⊕⊕⊕◯ Moderateb |
| Physical functionc | 11 | 1390 | 0.22 (0 to 0.43) | .053 | 73 | 0.33 | .75 | ⊕⊕⊕◯ Moderateb |
| Quality of lifec | 8 | 727 | 0.25 (0.04 to 0.46) | .02 | 45 | 0.72 | .50 | ⊕⊕⊕⊕ High |
CI: confidence interval; GRADE: Grading of Recommendations Assessment, Development and Evaluation; RCT: randomized controlled trial; SMD: standardized mean difference.
A negative difference favors the intervention group (which had technology-supported exercise programs applied), while a positive difference favors the control group.
Downgraded for substantial heterogeneity (I2 > 50%).
A positive difference favors the intervention group (which had technology-supported exercise programs applied), while a negative difference favors the control group.
Figure 3.
Forest plots for the effects of the 12 randomized controlled trials (RCTs) on (a) knee pain, (b) physical function, and (c) quality of life. CI: confidence interval; SMD: standardized mean difference.
Subgroup analysis for the outcomes by technology type
Table 3 presents the analysis of the effects of exercise programs by technology type. For knee pain, the use of web (SMD = −0.48; 95% CI, −0.90 to −0.05; P = .03) or mobile app (SMD = −0.45; 95% CI, −0.88 to −0.02; P = .04) was associated with a significant reduction in knee pain, which equated to a decrease of more than 2 points on the 20-point WOMAC pain subscale, whereas the use of telephone was not; the subgroup difference was not significant (P = .27). The use of Web to deliver the programs was associated with improved quality of life (SMD = 0.59; 95% CI, 0.11 to 1.07; P = .02), which equated to an improvement of 11.33 points on the 100-point Knee Injury and Osteoarthritis Outcome Score quality-of-life subscale, whereas the use of telephone, mobile app, or computer was not; the subgroup difference was not significant (P = .32). We did not observe any significant improvement in physical function when assessing the individual technology type, and no significant subgroup difference was detected (P = .69).
Table 3.
Effects of technology-supported exercise programs on the outcomes by technology type
| Type of Technology | Number of RCTs | SMD (95% CI) | P Value |
|---|---|---|---|
| Knee pain | |||
| Telephone | 6 | −0.12 (−0.41 to 0.17) | .42 |
| Web | 2 | −0.48 (−0.90 to −0.05) | .03 |
| Mobile app | 2 | −0.45 (−0.88 to −0.02) | .04 |
| Subgroup difference | .27 | ||
| Physical function | |||
| Telephone | 6 | 0.08 (−0.29 to 0.44) | .68 |
| Web | 2 | 0.50 (−0.08 to 1.07) | .09 |
| Mobile app | 2 | 0.23 (−0.35 to 0.81) | .43 |
| Computer | 1 | 0.24 (−0.69 to 1.16) | .62 |
| Subgroup difference | .69 | ||
| Quality of life | |||
| Telephone | 6 | 0.18 (−0.05 to 0.41) | .13 |
| Web | 1 | 0.59 (0.11 to 1.07) | .02 |
| Virtual reality | 1 | 0.24 (−0.47 to 0.96) | .51 |
| Subgroup difference | .32 | ||
CI: confidence interval; RCT: randomized controlled trial; SMD: standardized mean difference.
Subgroup analysis of the outcomes by program feature
Table 4 shows the results of subgroup analysis by program feature. We found that each of the 6 features led to the intervention groups experiencing a greater reduction in knee pain than the control groups of nontechnological or no care, although there was no evidence that the effects significantly differ between subgroups (ie, programs that involved or did not involve the feature).
Table 4.
Effects of technology-supported exercise programs on the outcomes by program feature
| Features Examined for Each Outcome | Programs That Involved the Feature |
Programs That Did Not Involve the Feature |
Subgroup Difference (P Value) | ||||
|---|---|---|---|---|---|---|---|
| Number of RCTs | SMD (95% CI) | P Value | Number of RCTs | SMD (95% CI) | P Value | ||
| Knee pain | |||||||
| Individualized exercise recommendation | 8 | −0.30 (−0.53 to −0.08) | .01 | 2 | −0.20 (−0.67 to 0.27) | .40 | .70 |
| Video-based exercise demonstration | 4 | −0.46 (−0.73 to −0.19) | .001 | 6 | −0.13 (−0.39 to 0.14) | .34 | .09 |
| Sensor-based motion and physical activity tracking | 5 | −0.32 (−0.59 to −0.05) | .02 | 5 | −0.24 (−0.54 to 0.07) | .13 | .69 |
| Monitoring of exercise progression | 9 | −0.27 (−0.49 to −0.05) | .02 | 1 | −0.39 (−0.97 to 0.20) | .19 | .71 |
| Educational materials | 9 | −0.34 (−0.52 to −0.15) | .001 | 1 | 0.28 (−0.41 to 0.97) | .42 | .09 |
| Reminder to perform exercise | 3 | −0.48 (−0.81 to −0.16) | .004 | 7 | −0.18 (−0.42 to 0.07) | .16 | .14 |
| Physical function | |||||||
| Individualized exercise recommendation | 8 | 0.22 (−0.04 to 0.49) | .10 | 3 | 0.19 (−0.27 to 0.64) | .43 | .89 |
| Video-based exercise demonstration | 4 | 0.48 (0.19 to 0.77) | .001 | 7 | 0.02 (−0.24 to 0.27) | .90 | .02 |
| Sensor-based motion and physical activity tracking | 6 | 0.14 (−0.19 to 0.46) | .40 | 5 | 0.29 (−0.04 to 0.61) | .08 | .52 |
| Monitoring of exercise progression | 9 | 0.24 (−0.01 to 0.49) | .06 | 2 | 0.10 (−0.43 to 0.63) | .71 | .64 |
| Educational materials | 9 | 0.25 (0.01 to 0.49) | .04 | 2 | −0.01 (−0.58 to 0.57) | .98 | .41 |
| Reminder to perform exercise | 3 | 0.48 (0.09 to 0.87) | .02 | 8 | 0.09 (−0.17 to 0.36) | .50 | .10 |
| Quality of life | |||||||
| Individualized exercise recommendation | 6 | 0.31 (0.08 to 0.54) | .01 | 2 | 0.01 (−0.48 to 0.50) | .97 | .29 |
| Video-based exercise demonstration | 2 | 0.29 (−0.12 to 0.69) | .16 | 6 | 0.23 (−0.06 to 0.52) | .12 | .83 |
| Sensor-based motion and physical activity tracking | 4 | 0.25 (−0.12 to 0.62) | .19 | 4 | 0.25 (−0.04 to 0.54) | .09 | .99 |
| Monitoring of exercise progression | 7 | 0.25 (0.02 to 0.49) | .04 | 1 | 0.24 (−0.52 to 1.00) | .53 | .98 |
| Educational materials | 6 | 0.31 (0.08 to 0.54) | .01 | 2 | 0.01 (−0.48 to 0.50) | .97 | .29 |
| Reminder to perform exercise | 1 | 0.59 (0.16 to 1.02) | .01 | 7 | 0.19 (−0.02 to 0.39) | .07 | .10 |
CI: confidence interval; RCT: randomized controlled trial; SMD: standardized mean difference.
We additionally found that programs that involved the feature of video-based exercise demonstration were associated with a significantly greater improvement in physical function, compared with those that did not involve this feature (subgroup difference: P = .02). Moreover, programs that involved the features of educational materials and a reminder to perform exercise led to a significant improvement in physical function, although the effects did not show heterogeneity between subgroups. For other features, we did not identify a significant improvement in physical function when programs involved each of them, and similar changes were observed between subgroups.
Furthermore, we identified that participants experienced a significant improvement in quality of life when they took part in programs that involved individualized exercise recommendation, monitoring of exercise progression, educational materials, or a reminder to perform exercise, although we did not identify the evidence that these effects significantly vary between subgroups. For programs that involved the features of video-based exercise demonstration and sensor-based motion and physical activity tracking, they did not show a significant improvement in quality of life, and similar changes were identified between subgroups.
DISCUSSION
Main findings
In this systematic review, we meta-analyzed 12 RCTs that examined the short-term effects of technology-supported exercise programs on knee pain, physical function, and quality of life among individuals with knee OA and/or chronic knee pain. We found that these programs were associated with significant and clinically important improvements in knee pain and quality of life but not with significant improvement in physical function. Positive effects were observed may be due to technological tools providing more access to healthcare resources (eg, information, knowledge, data) that raise participants’ awareness about the importance of health and exercise management,50,51 promote daily physical activity,52 increase exercise adherence,53,54 and lead to greater improvements in health-related outcomes.55
Among the 5 types of technology that were used to support the delivery of the exercise programs, Web-supported programs were suggestive of potential improvements in knee pain and quality of life, demonstrating small but significant benefits for chronic pain management.56–58 This may be due to the fact that as part of such Web-supported programs, participants receive plenty of self-management guidance, as well as professional advice from physical therapists via videoconferencing or instant messaging. Consequently, participants would be motivated to regulate their exercise behaviors in a safe, feasible, and well-accepted way.52,59,60 Similar to Web-supported programs, mobile apps also provided various exercise resources and demonstrate potential benefits for knee pain reduction. In modern society, such mobile health technology is more accessible and flexible than other modes of healthcare provision, enabling individuals to perform management of their health conditions anywhere and at any time.61–66 However, our review did not identify the evidence of heterogeneity of effects when comparing different types of technology and several technology types produced similar beneficial impacts. Healthcare providers may therefore wish to consider the specific requirements of individuals and select the most suitable technology in each instance. For example, we found that telephone was the most used technology, as it has the advantages of being easy to use and inexpensive, which is especially beneficial for people who are relatively less familiar with modern technologies (eg, older adults or individuals with low information technology literacy). In contrast, programs supported by Web and mobile app usually comprise multiple features, enabling participants to perform self-management with additional support from physical therapists. Moreover, virtual reality technology provides interactive feedback on exercise movements in a 3-dimensional environment,67–69 enabling participants to develop a clear understanding of their exercise performance. Supported by computer, virtual reality, and robotic technology, game-based exercise therapy could become a highly useful tool.70–73 However, such systems are often expensive and require a greater amount of technical assistance from healthcare professionals than other technology, and thus may not be widely accepted.74,75
Various program features were used to facilitate and encourage participants to perform exercise. Programs that involved the feature of video-based exercise demonstration appeared to have some benefits for physical function compared with those that did not. This may be attributable to the fact that exercise videos, together with audio instructions and subtitles, may help participants to develop a correct sense of gestures, speed, and range of motion for performing exercise.76 Thus, compared with text-based materials, exercise videos instructed by physical therapists will provide clearer demonstrations of movements. In addition, programs that involved some other features may also have potential benefits, although they did not show evidence of heterogeneity of effects between subgroups. For example, programs that included a reminder to perform exercise were associated with improvements in knee pain, physical function, and quality of life. This is supported by the findings that older adults may adhere poorly to prescribed home exercises due to forgetfulness or limited supervision from physical therapists, and reminders can help resolve this problem by regularly encouraging them to perform exercise and increasing participants’ adherence to exercise therapy.77–80 Another example is that programs that incorporated educational materials were also associated with improvements in all 3 outcomes, which may be related to increased knowledge and awareness of performing exercise and knee health, leading to improvements in health conditions.
Implications for research
This review has the following implications for research. First, some pilot RCTs had a small sample size (eg, 20 or fewer participants in each group); therefore, studies with larger sample sizes are required to reduce the risk of publication bias and the failure to detect significant differences.81,82 Second, just like the implementation of many other healthcare technology and protocols,65,83–85 further testing of the usability and acceptance of technology-supported exercise programs is necessary, as the success of these interventions depends primarily on them being well designed and accepted by end users.74,75,85–88
Implications for practice
A majority of the reviewed RCTs were published in 2015 or later, reflecting rapidly increasing interest in the implementation of technology-supported exercise programs.24 The use of advanced technologies, such as Web and mobile app, may overcome the barriers of limited healthcare resources, leading to these technologies supplementing or surrogating the conventional delivery of care.62,63,89,90 In addition, the feature of video-based exercise demonstration could be considered for future development of exercise programs because the programs that involved this feature led to a significantly greater improvement than did those that did not, while the potential benefits of other features should not be neglected, including reminder to perform exercise, educational materials, individualized exercise recommendation, sensor-based motion and physical activity tracking, and monitoring of exercise progression.
Thus, there are opportunities and challenges to both the development and implementation of technology-based healthcare programs for OA and/or chronic knee pain.90 One approach to improve program effects could be to provide personalized information for individuals,91 given the fact that the same exercise guidelines may not be suitable for people with different knee-related health conditions. It has also been reported that personalized reminders and feedback are more effective than their generic equivalents in healthcare programs.92–96 Another approach could be to improve the usability of a program. For example, a complex feature may be easily usable by a young adult but very difficult for an older individual to use because of aging or reduced physical function. Program developers should therefore pay more attention to all performance aspects of users, including cognitive, physical, and behavioral performance,97 and develop exercise programs that support and fit the users in the target population.88,98
Strengths and limitations
The review has the following strengths. First, with the use of a systematic and effective methodology, our review provides more supporting evidence for the effects of technology-supported exercise programs for the treatment and management of knee OA and/or chronic knee pain. Second, our review has identified technology types and program features that have demonstrated potential benefits for knee health management, based on which practical suggestions are provided. However, this review has the following limitations. First, although individuals with knee OA and chronic knee pain have overlapping clinical symptoms, they may still have potential clinical diversity, which may cause statistical heterogeneity in meta-analysis. Second, the RCTs included in the review examined the short-term effects of the exercise programs, and the long-term effects are still less clear. Third, a limited number of RCTs used computer and virtual reality to deliver exercise programs, which meant that it was difficult to identify significant changes in outcomes and examine the effects of these types of technology. Finally, participants in most RCTs were aware of the interventions that were used, and thus placebo effects could have existed.99
CONCLUSIONS
For individuals with knee OA and/or chronic knee pain, the use of technology-supported exercise programs appears to be an effective approach, at least for short-term improvements in knee pain and quality of life. Healthcare organizations may consider the use of mobile information technology or technological platforms that can facilitate the provision and accessibility of care aids and resources to deliver exercise programs. Further efforts are required to consider the specific needs of individuals and develop usable programs to better facilitate and encourage them to perform exercise. Also, the long-term effects of the exercise programs should be further examined by RCTs with large sample sizes and long implementation durations.
FUNDING
This study was supported by the Seed Fund for Basic Research of the University of Hong Kong (Project No.: 201910159250; Principal Investigator: CKO).
Supplementary Material
AUTHOR CONTRIBUTIONS
T.C. and C.O. designed the systematic review and developed the study protocol. T.C. and J.C. were responsible for literature search, study screening, data extraction, and assessment of risk of bias. T.C. performed data analysis. T.C. and C.O. contributed to the interpretation of the results and developed the manuscript.
ACKNOWLEDGMENTS
The authors would like to thank Miss Zhenzhen Xie for her assistance in data analysis and interpretation of findings.
CONFLICT OF INTEREST STATEMENT
None to declare.
REFERENCES
- 1. Hinman R, Crossley K.. Patellofemoral joint osteoarthritis: an important subgroup of knee osteoarthritis. Rheumatology 2007; 46 (7): 1057–62. [DOI] [PubMed] [Google Scholar]
- 2. Wang K, Kim HA, Felson DT, et al. Radiographic knee osteoarthritis and knee pain: cross-sectional study from five different racial/ethnic populations. Sci Rep 2018; 8 (1): 1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Felson DT, Naimark A, Anderson J, et al. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 1987; 30 (8): 914–8. [DOI] [PubMed] [Google Scholar]
- 4. Peat G, McCarney R, Croft P.. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 2001; 60 (2): 91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McAlindon TE, Cooper C, Kirwan JR, et al. Knee pain and disability in the community. Rheumatology 1992; 31 (3): 189–92. [DOI] [PubMed] [Google Scholar]
- 6. Noormohammadpour P, Mansournia MA, Koohpayehzadeh J, et al. Prevalence of chronic neck pain, low back pain, and knee pain and their related factors in community-dwelling adults in Iran. Clin J Pain 2017; 33 (2): 181–7. [DOI] [PubMed] [Google Scholar]
- 7. Dureja GP, Jain PN, Shetty N, et al. Prevalence of chronic pain, impact on daily life, and treatment practices in India. Pain Pract 2014; 14 (2): E51–62. [DOI] [PubMed] [Google Scholar]
- 8. Woo J, Leung J, Lau E.. Prevalence and correlates of musculoskeletal pain in Chinese elderly and the impact on 4-year physical function and quality of life. Public Health 2009; 123 (8): 549–56. [DOI] [PubMed] [Google Scholar]
- 9. Andersen RE, Crespo CJ, Ling SM, et al. Prevalence of significant knee pain among older Americans: results from the Third National Health and Nutrition Examination Survey. J Am Geriatr Soc 1999; 47 (12): 1435–8. [DOI] [PubMed] [Google Scholar]
- 10. Palazzo C, Nguyen C, Lefevre-Colau M-M, et al. Risk factors and burden of osteoarthritis. Ann Phys Rehabil Med 2016; 59 (3): 134–8. [DOI] [PubMed] [Google Scholar]
- 11. Messier SP, Glasser JL, Ettinger WH Jr, et al. Declines in strength and balance in older adults with chronic knee pain: a 30-month longitudinal, observational study. Arthritis Care Res 2002; 47 (2): 141–8. [DOI] [PubMed] [Google Scholar]
- 12. Hunter DJ, Bierma-Zeinstra S.. Osteoarthritis. Lancet 2019; 393 (10182): 1745–59. [DOI] [PubMed] [Google Scholar]
- 13. Cottrell E, Roddy E, Foster NE.. The attitudes, beliefs and behaviours of GPs regarding exercise for chronic knee pain: a systematic review. BMC Fam Pract 2010; 11 (1): 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Geriatrics Society Panel on Exercise and Osteoarthritis. Exercise prescription for older adults with osteoarthritis pain: consensus practice recommendations. A supplement to the AGS Clinical Practice Guidelines on the management of chronic pain in older adults. J Am Geriatr Soc 2001; 49 (6): 808–23. [DOI] [PubMed] [Google Scholar]
- 15. Altman RD, Hochberg MC, Moskowitz RW, et al. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum 2000; 43 (9): 1905–15. [DOI] [PubMed] [Google Scholar]
- 16. Felson DT, Lawrence RC, Hochberg MC, et al. Osteoarthritis: new insights. Part 2: treatment approaches. Ann Intern Med 2000; 133 (9): 726–37. [DOI] [PubMed] [Google Scholar]
- 17. Jordan K, Arden N, Doherty M, et al. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: report of a task force of the standing committee for international clinical studies including therapeutic trials (ESCISIT). Ann Rheum Dis 2003; 62 (12): 1145–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lane NE, Thompson JM.. Management of osteoarthritis in the primary-care setting: an evidence-based approach to treatment. Am J Med 1997; 103 (6): S25–30. [DOI] [PubMed] [Google Scholar]
- 19. Roddy E, Zhang W, Doherty M, et al. Evidence-based recommendations for the role of exercise in the management of osteoarthritis of the hip or knee—the MOVE consensus. Rheumatology 2005; 44 (1): 67–73. [DOI] [PubMed] [Google Scholar]
- 20. Scott DL. Guidelines for the diagnosis, investigation and management of osteoarthritis of the hip and knee: report of a joint working group of the British Society for Rheumatology and the Research Unit of the Royal College of Physicians. Clin Med (Lond) 1993; 27 (4): 391–6. [PMC free article] [PubMed] [Google Scholar]
- 21. Moore AJ, Holden MA, Foster NE, et al. Therapeutic alliance facilitates adherence to physiotherapy-led exercise and physical activity for older adults with knee pain: a longitudinal qualitative study. J Physiother 2020; 66 (1): 45–53. [DOI] [PubMed] [Google Scholar]
- 22. Joelsson M, Bernhardsson S, Larsson ME.. Patients with chronic pain may need extra support when prescribed physical activity in primary care: a qualitative study. Scand J Prim Health Care 2017; 35 (1): 64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Holden MA, Nicholls EE, Young J, et al. Role of exercise for knee pain: what do older adults in the community think? Arthritis Care Res 2012; 64 (10): 1554–64. [DOI] [PubMed] [Google Scholar]
- 24.Skjæret N, Nawaz A, Morat T, et al. Exercise and rehabilitation delivered through exergames in older adults: an integrative review of technologies, safety and efficacy. Int J Med Inform 2016; 85 (1): 1–16. [DOI] [PubMed] [Google Scholar]
- 25. Webster D, Celik O.. Systematic review of Kinect applications in elderly care and stroke rehabilitation. J Neuroeng Rehabil 2014; 11 (1): 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schäfer AGM, Zalpour C, Von Piekartz H, et al. The efficacy of electronic health-supported home exercise interventions for patients with osteoarthritis of the knee: systematic review. J Med Internet Res 2018; 20 (4): e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Naeemabadi M, Fazlali H, Najafi S, et al. Telerehabilitation for patients with knee osteoarthritis: a focused review of technologies and teleservices. JMIR Biomed Eng 2020; 5 (1): e16991. [Google Scholar]
- 28. Allen KD, Arbeeva L, Callahan LF, et al. Physical therapy vs internet-based exercise training for patients with knee osteoarthritis: results of a randomized controlled trial. Osteoarthritis Cartilage 2018; 26 (3): 383–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hinman RS, Campbell PK, Lawford BJ, et al. Does telephone-delivered exercise advice and support by physiotherapists improve pain or function in people with knee osteoarthritis? Telecare randomised controlled trial. Br J Sports Med 2020; 54 (13): 790–7. [DOI] [PubMed] [Google Scholar]
- 30. Li LC, Feehan LM, Xie H, et al. Effects of a 12-week multifaceted wearable-based program for people with knee osteoarthritis: randomized controlled trial. JMIR Mhealth Uhealth 2020; 8 (7): e19116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Li LC, Sayre EC, Xie H, et al. Efficacy of a community-based technology-enabled physical activity counseling program for people with knee osteoarthritis: proof-of-concept study. J Med Internet Res 2018; 20 (4): e159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mecklenburg G, Smittenaar P, Erhart-Hledik JC, et al. Effects of a 12-Week digital care program for chronic knee pain on pain, mobility, and surgery risk: randomized controlled trial. J Med Internet Res 2018; 20 (4): e156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151 (4): 264–9. [DOI] [PubMed] [Google Scholar]
- 34. Higgins JP, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, United Kingdom: Wiley; 2019. [Google Scholar]
- 35. Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315 (7109): 629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336 (7650): 924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bennell KL, Campbell PK, Egerton T, et al. Telephone coaching to enhance a home-based physical activity program for knee osteoarthritis: a randomized clinical trial. Arthritis Care Res 2017; 69 (1): 84–94. [DOI] [PubMed] [Google Scholar]
- 38. Bennell KL, Nelligan R, Dobson F, et al. Effectiveness of an Internet-delivered exercise and pain-coping skills training intervention for persons with chronic knee pain: a randomized trial. Ann Intern Med 2017; 166 (7): 453–62. [DOI] [PubMed] [Google Scholar]
- 39. Li LC, Sayre EC, Xie H, et al. A community-based physical activity counselling program for people with knee osteoarthritis: feasibility and preliminary efficacy of the track-OA study. JMIR Mhealth Uhealth 2017; 5 (6): e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lin DH, Lin YF, Chai HM, et al. Comparison of proprioceptive functions between computerized proprioception facilitation exercise and closed kinetic chain exercise in patients with knee osteoarthritis. Clin Rheumatol 2007; 26 (4): 520–8. [DOI] [PubMed] [Google Scholar]
- 41. Odole AC, Ojo OD.. A telephone-based physiotherapy intervention for patients with osteoarthritis of the knee. Int J Telerehab 2013; 5 (2): 11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Odole AC, Ojo OD.. Is telephysiotherapy an option for improved quality of life in patients with osteoarthritis of the knee? Int J Telemed Appl 2014; 2014: 903816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Skrepnik N, Spitzer A, Altman R, et al. Assessing the impact of a novel smartphone application compared with standard follow-up on mobility of patients with knee osteoarthritis following treatment with Hylan GF 20: a randomized controlled trial. JMIR Mhealth Uhealth 2017; 5 (5): e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wi SY, Jong Ho K, Jun Hyeok J.. Clinical feasibility of exercise game for depression treatment in older women with osteoarthritis: a pilot study. J Phys Ther Sci 2013; 25 (2): 165–7. [Google Scholar]
- 45. Parkes MJ, Maricar N, Lunt M, et al. Lateral wedge insoles as a conservative treatment for pain in patients with medial knee osteoarthritis: a meta-analysis. JAMA 2013; 310 (7): 722–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jinks C, Jordan K, Croft P.. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Pain 2002; 100 (1–2): 55–64. [DOI] [PubMed] [Google Scholar]
- 47. Angst F, Aeschlimann A, Stucki G.. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Care Res 2001; 45 (4): 384–91. [DOI] [PubMed] [Google Scholar]
- 48. Collins N, Prinsen C, Christensen R, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage 2016; 24 (8): 1317–29. [DOI] [PubMed] [Google Scholar]
- 49. Collins NJ, Misra D, Felson DT, et al. Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form, knee injury and osteoarthritis outcome score (KOOS), knee injury and osteoarthritis outcome score physical function short form (KOOS-PS), knee outcome survey activities of daily living scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res 2011; 63 (S11): S208–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Franco MR, Tong A, Howard K, et al. Older people's perspectives on participation in physical activity: a systematic review and thematic synthesis of qualitative literature. Br J Sports Med 2015; 49 (19): 1268–76. [DOI] [PubMed] [Google Scholar]
- 51. van Stralen MM, de Vries H, Mudde AN, et al. The long-term efficacy of two computer-tailored physical activity interventions for older adults: main effects and mediators. Health Psychol 2011; 30 (4): 442–52. [DOI] [PubMed] [Google Scholar]
- 52. Lai B, Young H-J, Bickel CS, et al. Current trends in exercise intervention research, technology, and behavioral change strategies for people with disabilities: a scoping review. Am J Phys Med Rehabil 2017; 96 (10): 748–61. [DOI] [PubMed] [Google Scholar]
- 53. Valenzuela T, Okubo Y, Woodbury A, et al. Adherence to technology-based exercise programs in older adults: a systematic review. J Geriatr Phys Ther 2018; 41 (1): 49–61. [DOI] [PubMed] [Google Scholar]
- 54. Husebø AML, Dyrstad SM, Søreide JA, et al. Predicting exercise adherence in cancer patients and survivors: a systematic review and meta-analysis of motivational and behavioural factors. J Clin Nurs 2013; 22 (1-2): 4–21. [DOI] [PubMed] [Google Scholar]
- 55. Hamine S, Gerth-Guyette E, Faulx D, et al. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res 2015; 17 (2): e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bender JL, Radhakrishnan A, Diorio C, et al. Can pain be managed through the internet? A systematic review of randomized controlled trials. Pain 2011; 152 (8): 1740–50. [DOI] [PubMed] [Google Scholar]
- 57. Macea DD, Gajos K, Calil YAD, et al. The efficacy of Web-based cognitive behavioral interventions for chronic pain: a systematic review and meta-analysis. J Pain 2010; 11 (10): 917–29. [DOI] [PubMed] [Google Scholar]
- 58. Ruehlman LS, Karoly P, Enders C.. A randomized controlled evaluation of an online chronic pain self management program. Pain 2012; 153 (2): 319–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Stellefson M, Chaney B, Barry AE, et al. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res 2013; 15 (2): e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tsai LLY, McNamara RJ, Moddel C, et al. Home-based telerehabilitation via real-time v1ideoconferencing improves endurance exercise capacity in patients with COPD: the randomized controlled TeleR Study. Respirology 2017; 22 (4): 699–707. [DOI] [PubMed] [Google Scholar]
- 61. Azevedo ARP, de Sousa HML, Monteiro JAF, et al. Future perspectives of smartphone applications for rheumatic diseases self-management. Rheumatol Int 2015; 35 (3): 419–31. [DOI] [PubMed] [Google Scholar]
- 62. Or CK, Liu K, So MKP, et al. Improving self-care in patients with coexisting type 2 diabetes and hypertension by technological surrogate nursing: randomized controlled trial. J Med Internet Res 2020; 22 (3): e16769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Xie Z, Liu K, Or C, et al. An examination of the socio-demographic correlates of patient adherence to self-management behaviors and the mediating roles of health attitudes and self-efficacy among patients with coexisting type 2 diabetes and hypertension. BMC Public Health 2020; 20 (1): 1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Xie Z, Nacioglu A, Or C.. Prevalence, demographic correlates, and perceived impacts of mobile health app use amongst Chinese adults: cross-sectional survey study. JMIR Mhealth Uhealth 2018; 6 (4): e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Tan J, Or C.. Themed issue on matching policies and socio-technical challenges to enhance the uptake of health information technologies. Health Policy Technol 2015; 4 (4): 297–8. [Google Scholar]
- 66. Liu K, Xie Z, Or CK.. Effectiveness of mobile app-assisted self-care interventions in improving patient outcomes in type 2 diabetes or hypertension: a systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth 2020; 8 (8): e15779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Schultheis MT, Rizzo AA.. The application of virtual reality technology in rehabilitation. Rehabil Psychol 2001; 46 (3): 296–311. [Google Scholar]
- 68. Sveistrup H, McComas J, Thornton M, et al. Experimental studies of virtual reality-delivered compared with conventional exercise programs for rehabilitation. Cyberpsychol Behav 2003; 6 (3): 245–9. [DOI] [PubMed] [Google Scholar]
- 69. Straudi S, Severini G, Charabati AS, et al. The effects of video game therapy on balance and attention in chronic ambulatory traumatic brain injury: an exploratory study. BMC Neurol 2017; 17 (1): 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Chua KSG, Kuah CWK.. Innovating with rehabilitation technology in the real world: promises, potentials, and perspectives. Am J Phys Med Rehabil 2017; 96 (10 Suppl 1): S150–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Tieri G, Morone G, Paolucci S, et al. Virtual reality in cognitive and motor rehabilitation: facts, fiction and fallacies. Expert Rev Med Devices 2018; 15 (2): 107–17. [DOI] [PubMed] [Google Scholar]
- 72. Chang WH, Kim Y-H.. Robot-assisted therapy in stroke rehabilitation. J Stroke 2013; 15 (3): 174–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Chen J, Or C.. Assessing the use of immersive virtual reality, mouse and touchscreen in pointing and dragging-and-dropping tasks among young, middle-aged and older adults. Appl Ergon 2017; 65: 437–48. [DOI] [PubMed] [Google Scholar]
- 74. Yan M, Or C.. Factors in the 4-week acceptance of a computer-based, chronic disease self-monitoring system in patients with type 2 diabetes mellitus or hypertension. Telemed J E Health 2018; 24 (2): 121–9. [DOI] [PubMed] [Google Scholar]
- 75. Yan M, Or C.. A 12-week pilot study of acceptance of a computer-based chronic disease self-monitoring system among patients with type 2 diabetes mellitus or hypertension. Health Informatics J 2019; 25 (3): 828–43. [DOI] [PubMed] [Google Scholar]
- 76. Haines TP, Russell T, Brauer SG, et al. Effectiveness of a video-based exercise programme to reduce falls and improve health-related quality of life among older adults discharged from hospital: a pilot randomized controlled trial. Clin Rehabil 2009; 23 (11): 973–85. [DOI] [PubMed] [Google Scholar]
- 77. Thomsen T, Aadahl M, Beyer N, et al. The efficacy of motivational counselling and SMS reminders on daily sitting time in patients with rheumatoid arthritis: a randomised controlled trial. Ann Rheum Dis 2017; 76 (9): 1603–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Emmerson KB, Harding KE, Taylor NF.. Home exercise programmes supported by video and automated reminders compared with standard paper-based home exercise programmes in patients with stroke: a randomized controlled trial. Clin Rehabil 2017; 31 (8): 1068–77. [DOI] [PubMed] [Google Scholar]
- 79. Fenerty SD, West C, Davis SA, et al. The effect of reminder systems on patients’ adherence to treatment. Patient Prefer Adherence 2012; 6: 127–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Clough BA, Casey LM.. Technological adjuncts to increase adherence to therapy: a review. Clin Psychol Rev 2011; 31 (5): 697–710. [DOI] [PubMed] [Google Scholar]
- 81. Macaskill P, Walter SD, Irwig L.. A comparison of methods to detect publication bias in meta-analysis. Stat Med 2001; 20 (4): 641–54. [DOI] [PubMed] [Google Scholar]
- 82. Moher D, Dulberg CS, Wells GA.. Statistical power, sample size, and their reporting in randomized controlled trials. JAMA 1994; 272 (2): 122–4. [PubMed] [Google Scholar]
- 83. Or C, Dohan M, Tan J.. Understanding critical barriers to implementing a clinical information system in a nursing home through the lens of a socio-technical perspective. J Med Syst 2014; 38 (9): 99. [DOI] [PubMed] [Google Scholar]
- 84. Or C, Wong K, Tong E, et al. Private primary care physicians' perspectives on factors affecting the adoption of electronic medical records: a qualitative pre-implementation study. Work 2014; 48 (4): 529–38. [DOI] [PubMed] [Google Scholar]
- 85. Karsh B, Holden R, Or C.. Human factors and ergonomics of health information technology implementation In: Carayon P, ed. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2nd ed.Boca Raton, FL: Taylor & Francis; 2012: 249–64. [Google Scholar]
- 86. Or CK, Karsh B-T, Severtson DJ, et al. Factors affecting home care patients' acceptance of a web-based interactive self-management technology. J Am Med Inform Assoc 2011; 18 (1): 51–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Or CK, Karsh B-T.. A systematic review of patient acceptance of consumer health information technology. J Am Med Inform Assoc 2009; 16 (4): 550–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Or C, Tao D.. Usability study of a computer-based self-management system for older adults with chronic diseases. JMIR Res Protoc 2012; 1 (2): e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Or C, Tao D.. A 3-month randomized controlled pilot trial of a patient-centered, computer-based self-monitoring system for the care of type 2 diabetes mellitus and hypertension. J Med Syst 2016; 40 (4): 81. [DOI] [PubMed] [Google Scholar]
- 90. Cheung DST, Or CK, So MKP, et al. The use of eHealth applications in Hong Kong: results of a random-digit dialing survey. J Med Syst 2019; 43 (9): 293. [DOI] [PubMed] [Google Scholar]
- 91. Choi W, Zheng H, Franklin P, et al. mHealth technologies for osteoarthritis self-management and treatment: a systematic review. Health Informatics J 2019; 25 (3): 984–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Neff R, Fry J.. Periodic prompts and reminders in health promotion and health behavior interventions: systematic review. J Med Internet Res 2009; 11 (2): e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Kreuter MW, Wray RJ.. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav 2003; 27 (1): S227–32. [DOI] [PubMed] [Google Scholar]
- 94. Lombard DN, Lombard TN, Winett RA.. Walking to meet health guidelines: the effect of prompting frequency and prompt structure. Health Psychol 1995; 14 (2): 164–70. [DOI] [PubMed] [Google Scholar]
- 95. Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA 2008; 299 (10): 1139–48. [DOI] [PubMed] [Google Scholar]
- 96. Tate DF, Jackvony EH, Wing RR.. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med 2006; 166 (15): 1620–5. [DOI] [PubMed] [Google Scholar]
- 97. Boulos MNK, Brewer AC, Karimkhani C, et al. Mobile medical and health apps: state of the art, concerns, regulatory control and certification. Online J Public Health Inform 2014; 5 (3): e229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Cheung DST, Or CKL, So MKP, et al. Usability testing of a smartphone application for delivering qigong training. J Med Syst 2018; 42 (10): 191. [DOI] [PubMed] [Google Scholar]
- 99. Fransen M, McConnell S, Harmer AR, et al. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev 2015; 49 (24): 1554–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.