Abstract
Background and purpose
Patients with posterior circulation acute ischemic stroke exhibit varied clinical presentations and functional outcomes. Whether posterior circulation acute stroke prognosis early computed tomography scores (PC-ASPECTS) predict unfavorable functional outcomes (UFO) for patients treated with different therapeutic regimens is unclear.
Methods
According to PRISMA guidelines, we performed a systematic search of electronic databases for studies assessing the functional outcomes of posterior circulation acute ischemic stroke using baseline PC-ASPECTS. The following three scales of PC-ASPECTS were retrieved: UFO prediction by using PC-ASPECTS per score decrease, UFO prediction by using binary PC-ASPECTS with a cut-off value, and the difference in PC-ASPECTS between patients with unfavorable and favorable functional outcomes. Moreover, a subgroup analysis was conducted for patients treated with intra-arterial endovascular treatment (IA-EVT) only. Sensitivity analysis with different definition of UFO and image modalities were also conducted.
Results
In total, 25 studies were included. In scale 1, PC-ASPECTS significantly predicted UFO (odds ratio [OR]: 1.66 per score decrease, 95% confidence interval [CI]: 1.32–2.07). In scale 2, binary PC-ASPECTS with a cut-off value between 6 and 9 significantly predicted UFO (OR: 3.91, 95% CI: 2.54–6.01). In scale 3, patients with UFO had lower PC-ASPECTS than those with favorable outcomes (standardized mean difference [SMD]: −0.67, 95% CI: −0.8 to −0.55). For patients treated with IA-EVT only, the scales demonstrated consistent results. Sensitivity analysis showed PC-ASPECTS significantly predicted UFO in both definitions of modified Rankin Scale ≥ 3 and ≥ 4, and magnetic resonance imaging was preferred imaging modality for PC-ASPECTS evaluation.
Conclusion
Baseline PC-ASPECTS is effective in predicting UFO for patients with posterior circulation acute ischemic stroke treated with different therapeutic regimens.
Introduction
Posterior circulation infarction accounts for one-fifth to one-fourth of all incidents of acute ischemic stroke [1,2] and has varied clinical presentations [3–5]. Acute basilar artery occlusion (BAO), the most devastating form of posterior circulation infarction, has a mortality rate of approximately 80% [6,7]. Prompt recanalization for BAO and other posterior circulation infarctions was proven to reduce morbidity and mortality [8,9]. Nevertheless, most scoring tools assessing whether stroke patients are candidates for thrombolytic therapy, such as the National Institutes of Health Stroke Scale (NIHSS; which is weighted more for anterior circulation symptoms and signs) [10] and the Alberta stroke program early computed tomography (CT) score (ASPECTS) (assessing the early ischemic changes in the middle cerebral artery territory) [11], are not universally applicable to posterior circulation infarction.
Similar to ASPECTS, posterior circulation Alberta stroke program early CT scores (PC-ASPECTS) allots 10 points to assess early ischemic changes on computed tomography angiography-source imaging (CTA-SI) or diffusion-weighted imaging (DWI) of magnetic resonance imaging (MRI) [12]. These 10 points provide semiquantitative estimates of the region of posterior circulation infarction, which include each side of the cerebellum (1 point), occipital lobe (1 point), thalamus (1 point), pons (2 point), and midbrain (2 point). Unlike anterior circulation stroke with a consensus ASPECTS of <6 as a robust predictor of unfavorable functional outcomes (UFO) and a relative contraindication of endovascular treatment [13,14], studies of posterior circulation infarction have demonstrated a discrepancy when predicting outcomes using baseline PC-ASPECTS. To address this issue, we performed a meta-analysis to determine whether baseline PC-ASPECTS effectively discriminate between unfavorable and favorable outcomes.
Materials and methods
Literature search
The first study to propose the scoring method of PC-ASPECTS was published on January 24, 2008. All relevant studies published in English were identified by searching PubMed, Embase, and Scopus from January 1, 2008, to July 31, 2020. The systematic search to identify eligible studies was conducted in accordance with PRISMA guidelines [15]. The keywords and MeSH terms within the search strategy included “stroke (MeSH),” “cerebrovascular disorders (MeSH),” “basilar artery (MeSH),” “vertebrobasilar insufficiency (MeSH),” “endovascular procedures (MeSH),” “thrombolytic therapy (MeSH),” “mechanical thrombolysis (MeSH),” “posterior circulation,” “PC-ASPECTS,” and their combination (S1 Table). Ethical approval for this study was waived by the Institutional Review Board of Far Eastern Memorial Hospital, New Taipei, Taiwan.
Study selection and quality assessment
The inclusion criteria were as follows: (1) studies reporting a series of patients with posterior circulation acute ischemic stroke and baseline PC-ASPECTS and (2) studies reporting the functional outcomes in terms of modified Rankin Scale (mRS) on day 90. The exclusion criteria were as follows: (1) abstract papers, (2) case reports, (3) review articles, (4) small studies with a sample size less than 10, (5) studies published in languages other than English, and (5) studies including pediatric populations. Independent screening of titles and abstracts was conducted by two authors (Lu WZ and Lin SF) to identify the studies that met the inclusion criteria. A final list was assembled based on their consensus (Lu WZ and Lin SF). The Newcastle–Ottawa Scale was used for quality assessment (S2 Table). Each retrieved study was critically appraised by two independent reviewers (Lu WZ and Lin SF). Disagreements between them were resolved by other two authors (Lin HA and Bai CH).
Data collection and outcomes
The study outcome was the prediction of UFO using baseline PC-ASPECTS for patients with posterior circulation acute ischemic stroke receiving any type of treatment. UFO was defined as an mRS of 3–6 or 4–6 on day 90. The association between UFO prediction and baseline PC-ASPECTS for patients was assessed using the following three scales: (1) UFO prediction by using PC-ASPECTS per score decrease, (2) UFO prediction by using binary PC-ASPECTS with a cut-off value, and (3) the difference in baseline PC-ASPECTS between posterior circulation infarction patients with UFO and those with favorable functional outcomes.
Statistical analysis
We estimated the odds ratio (OR) and standardized mean difference (SMD) and their 95% confidence interval (CI) for each cohort. Heterogeneity for each outcome was assessed using the Higgins index (I2); thereafter, the DerSimonian–Laird random effects model was applied. We defined the Higgins index value (I2) > 50% as substantial heterogeneity [16]. To evaluate heterogeneity and bias, a funnel plot was generated, followed by Begg’s test. Analyses were performed using metan package for Stata software, version 15 (StataCorp, Texas, USA). All reported P values were two-sided and were considered as statistically significant at <0.05. A step-down Bonferroni and Hochberg adjustment were used to address the problems of multiple testing.
Subgroup analyses
We conducted subgroup analyses assessed UFO prediction by using the baseline PC-ASPECTS for patients with intra-arterial endovascular treatment (IA-EVT). We also assessed UFO prediction by using baseline PC-ASPECTS in the above three scales. A random effects meta-regression test was performed to assess the heterogeneity caused by the potential modifiers of the imaging modality of CT or MRI and the definition of UFO based on an mRS of 3–6 or 4–6.
Sensitivity analyses
We performed two sensitivity analyses: (1) varied definition of UFO by mRS of 3–6 or 4–6, (2) varied imaging modalities of CT and MRI. The UFO Outcomes in three scales were analyzed as well.
Results
Search results
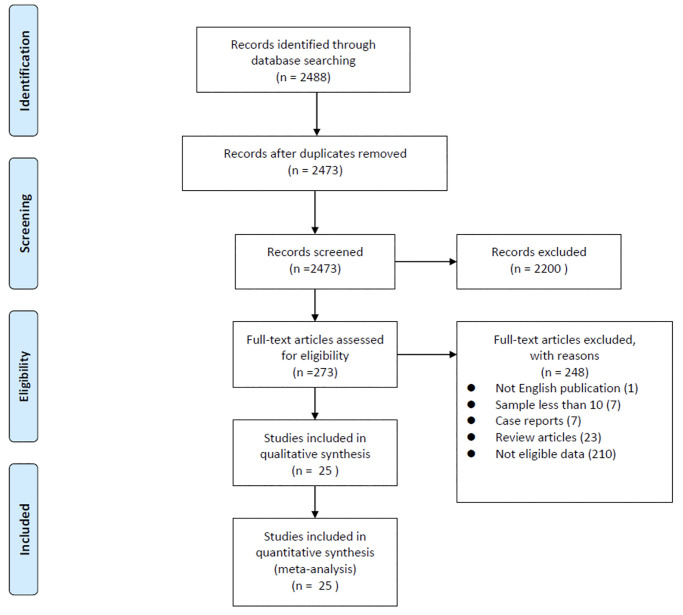
The flowchart describes the study selection process (Fig 1). During the initial search, a total of 2488 studies were identified, and only 25 studies met the inclusion and exclusion criteria. Characteristics of the included studies are summarized in Table 1. We included studies with prospective and retrospective cohort designs. In scale 1 (PC-ASPECTS per score decrease), a total of 8 studies with 609 patients were included. In scale 2 (binary PC-ASPECTS by a cut-off value), a total of 7 studies with 844 patients were enrolled. In scale 3 (SMD of PC-ASPECTS between patients with unfavorable and those with favorable functional outcomes), a total of 19 studies with 1186 patients were included in the analysis. For enrolled studies, the quality assessment was evaluated by Newcastle-Ottawa Scale. All of our included studies attained high quality with a total score of ≥ 8 (See online S2 Table).
Fig 1. PRISMA flowchart of search strategy.
Table 1. Summary of methodological characteristics of included studies pertinent to the study outcomes.
| Study | Year | Sample size (number) | PC-ASPECTS cut-off | Clinical Measures | Imaging | Patients treated with thrombolysis (number) |
|---|---|---|---|---|---|---|
| Scale 1: Unfavorable outcome prediction by PC-ASPECTS per score decrease | ||||||
| Junji Uno et al. [17] | 2020 | 50 | – | 90-day mRS of 0–2 vs 3–6 | CTP | 50 with IA-EVT |
| Xuelei Zhang et al. [18] | 2019 | 103 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 103 with IA-EVT |
| Sheng-Feng Lin et al. [19] | 2018 | 125 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 1 with IV thrombolysis only |
| Chuanhui Li et al. [20] | 2018 | 68 | – | 90-day mRS of 0–3 vs 4–6 | CTA-SI or MRI (DWI) | 68 with IA-EVT |
| Woong Yoon et al. [21] | 2015 | 50 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 14 with IV thrombolysis, 50 with IA thrombectomy |
| Isabelle Mourand et al. [22] | 2014 | 31 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 19 with IA-EVT and IV thrombolysis 12 with IA-EVT only |
| Simon Nagel et al. [23] | 2012 | 50 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 41 with recanalization therapy |
| Hideaki Tei et al. [24] | 2010 | 132 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | (No data provided) |
| Scale 2: Unfavorable outcomes prediction by binary PC-ASPECTS with a cut-off value | ||||||
| Volker Maus et al. [25] | 2019 | 104 | 0–8, 9–10 | 90-day mRS of 0–2 vs 3–6 | CTA-SI or MRI (DWI) | 104 with IA EVT 49 with IV + IA thrombolysis |
| Sheng-Feng Lin et al. [19] | 2018 | 125 | 0–7, 8–10 | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 1 with IV thrombolysis only |
| Gang Luo et al. [26] | 2018 | 69 | 0–5, 6–10 | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 69 with IA EVT |
| Woo-Jin Lee et al. [27] | 2017 | 292 | 0–6, 7–10 | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 62 with recanalization therapy |
| Woong Yoon et al. [21] | 2015 | 50 | 0–6, 7–10 | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 50 with IA EVT |
| Puetz et al. [28] (BASIC registry) | 2011 | 158 | 0–7, 8–10 | 90-day mRS of 0–2 vs 3–6 | CTA-SI | 15 with IV thrombolysis only 53 with IA EVT only 28 with IV and IA thrombolysis |
| Puetz et al. [12] (BASIC registry) | 2008 | 46 | 0–7, 8–10 | 90-day mRS of 0–3 vs 4–6 | CTA-SI | 36 with any thrombolysis 19 with IV thrombolysis 29 with IA thrombolysis |
| Scale 3: PC-ASPECTS scores between unfavorable and favorable outcomes | ||||||
| Beilei Chen et al. [29] | 2019 | 68 | – | 90-day mRS of 0–2 vs 3–6 | CT | 68 with IA-EVT |
| Xuelei Zhang et al. [18] | 2019 | 103 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 103 with IA-EVT |
| Fana Alemseged et al. [30] | 2019 | 60 | – | 90-day mRS of 0–3 vs 4–6 | CTA-SI, CTP | 28 with IV thrombolysis, 25 with IA-EVT |
| Francisco Antunes Dias et al. [31] | 2019 | 27 | – | 90-day mRS of 0–3 vs 4–6 | CTA | 27 with IA-EVT |
| Sheng-Feng Lin et al. [19] | 2018 | 125 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 1 with IV thrombolysis only |
| Alexandros Rentzos et al. [32] | 2018 | 110 | – | 90-day mRS of 0–2 vs 3–6 | CTA-SI | 110 with IA-EVT |
| Chuanhui Li et al. [20] | 2018 | 68 | – | 90-day mRS of 0–3 vs 4–6 | CTA-SI or MRI (DWI) | 68 with IA-EVT |
| Jun Young Chang et al. [33] | 2017 | 59 | – | 90-day mRS of 0–3 vs 4–6 | MRI (DWI) | 20 with IV thrombolysis 59 with IA-EVT |
| Francisco Antunes Dias et al. [34] | 2017 | 63 | – | 90-day mRS of 0–3 vs 4–6 | NCCT | 15 with IV thrombolysis 19 with IA-EVT 29 with no recanalization |
| Woo-Jin Lee et al. [35] | 2017 | 98 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 98 with no recanalization |
| Robert Fahed et al. [36] | 2017 | 34 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 34 with IA-EVT |
| Seungnam Son et al. [37] | 2016 | 35 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 35 with IA-EVT |
| Valerio Da Ros et al. [38] | 2016 | 15 | – | 90-day mRS of 0–3 vs 4–6 | CTA-SI | 15 with IA-EVT |
| Woong Yoon et al. [21] | 2015 | 50 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 14 with IV thrombolysis, 50 with IA thrombectomy |
| S. Mundiyanapurath et al. [39] | 2015 | 22 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI, SWI) | 4 with IV thrombolysis only 4 with IA EVT 14 with IV and IA thrombolysis |
| Isabelle Mourand et al. [22] | 2014 | 31 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 19 with IA-EVT and IV thrombolysis 12 with IA-EVT only |
| Simon Nagel et al. [23] | 2012 | 50 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | 41 with recanalization therapy |
| Alexander Karameshev et al. [40] | 2011 | 36 | – | 90-day mRS of 0–3 vs 4–6 | MRI (DWI) | 36 with IA-EVT |
| Hideaki Tei et al. [24] | 2010 | 132 | – | 90-day mRS of 0–2 vs 3–6 | MRI (DWI) | (No data provided) |
BASIC, The Basilar Artery International Cooperative Study; CTP, Computed tomography perfusion scan; CTA-SI, computed tomography angiography-source imaging; ECASS: European Cooperative Acute Stroke Study; EVT, endovascular therapy; mRS, modified Rankin Scale; NCCT, non-contrast computed tomography; IA, intra-arterial; IV, intravenous; MRI, magnetic resonance imaging; SWI, susceptibility-weighted imaging. IV thrombolysis defined as treatment with tissue plasminogen activator.
Outcomes: PC-ASPECTS for patients with any treatment
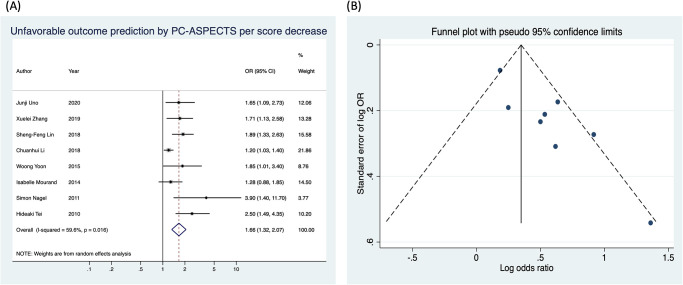
(1) OR meta-analysis for PC-ASPECTS per score decrease
This meta-analysis compared the baseline PC-ASPECTS between patients with UFO and those with favorable functional outcomes on day 90. Meta-analysis results were expressed as ORs for UFO prediction by using PC-ASPECTS per score decrease (Fig 2A). All eight studies, except one, individually revealed that the baseline PC-ASPECTS significantly predicted UFO [22]. Overall, the meta-analysis of these studies revealed a significant association between UFO prediction and PC-ASPECTS (OR: 1.66, 95% CI: 1.32–2.07 per score decrease; I2 = 59.6%, P = 0.016). The funnel plot (Fig 2B) followed by Begg’s test exhibited no significant publication bias for the eight studies (P = 0.174).
Fig 2. Unfavorable functional outcome prediction by using PC-ASPECTS per score decrease.
(A) The forest plot. (B) The funnel plot.
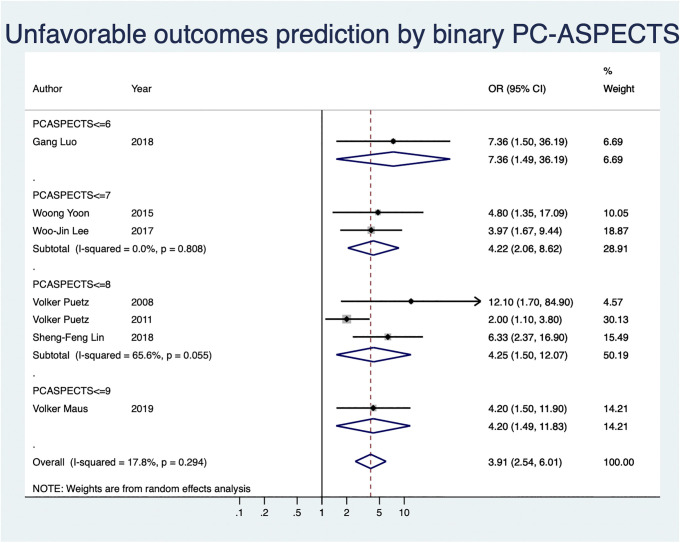
(2) OR meta-analysis for PC-ASPECTS by cut-off score
UFO prediction by using binary PC-ASPECTS with a cut-off value was analyzed for the included seven studies in this section (Fig 3). These included studies were classified into four subgroups according to their cut-off values. Of these studies, one, two, three, and one had PC-ASPECTS cut-offs of ≤6, ≤7, ≤8, and ≤9, respectively. All the studies individually revealed a significant association between UFO prediction and baseline binary PC-ASPECTS. The subgroup OR meta-analysis demonstrated a significant association between UFO prediction and binary PC-ASPECTS with cut-offs of ≤7 (OR: 4.22, 95% CI: 2.06–8.62; I2 = 0.0%, P = 0.808) and ≤8 (OR: 4.25, 95% CI: 1.5–12.07; I2 = 65.6%, P = 0.055).
Fig 3. The forest plot of unfavorable functional outcome prediction by using PC-ASPECTS with a cut-off value.
Generally, the overall OR meta-analysis consistently displayed a significant association between UFO and binary PC-ASPECTS at any cut-off value, without heterogeneity (OR: 3.91, 95% CI: 2.54–6.01; I2 = 17.8%, P = 0.294). Besides, we performed a test of significance for effect size with by using step-down Bonferroni method and Hochberg adjustment. The adjusted P values by step-down Bonferroni and Hochberg adjustment methods showed PC-ASPECTS of ≤ 7 with the smallest adjusted P value (S4 Table).
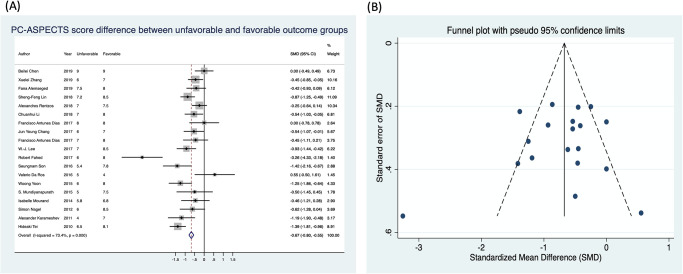
(3) SMD between unfavorable and favorable outcomes of PC-ASPECTS
The difference in PC-ASPECTS between unfavorable and favorable functional outcomes was analyzed for studies that provided PC-ASPECTS using a continuous scale (Fig 4A). In total, 19 studies were eligible in this meta-analysis. Of these, 10 studies exhibited a significant difference in score of PC-ASPECTS for patients with unfavorable and favorable outcomes, whereas 9 studies demonstrated no significant difference. Among studies revealing no significant difference, one study [38] paradoxically displayed low PC-ASPECTS in the favorable functional outcome group (SMD: 0.55, 95% CI: −0.5 to 1.61). Generally, the overall SMD meta-analysis result showed significant differences in PC-ASPECTS despite significant heterogeneity (SMD: −0.67, 95% CI: −0.8 to −0.55; I2 = 73.4%, P = 0.000). The funnel plot of 19 studies (Fig 4B) followed by Begg’s test revealed no significant publication bias (P = 0.529).
Fig 4. The standardized mean difference in PC-ASPECTS scores between patients with unfavorable and favorable outcomes.
Subgroup analyses: PC-ASPECTS for patients treated with IA-EVT
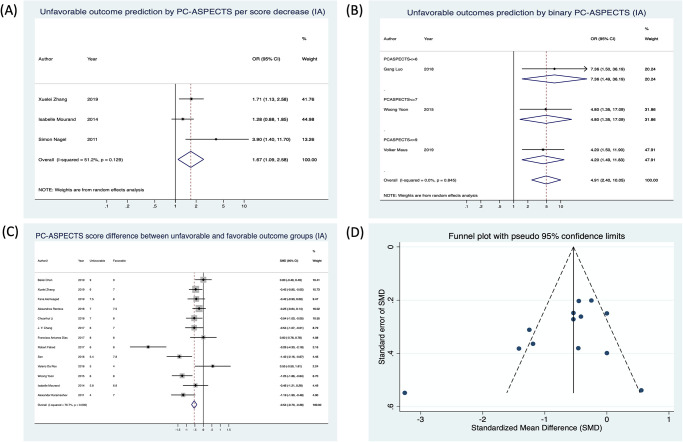
(1) OR meta-analysis for PC-ASPECTS per score
In total, three studies [18,22,23] involving patients treated with IA-EVT were included (Fig 5A). The overall results showed a significant association between UFO prediction and PC-ASPECT per score decrease for patients treated with IA-EVT, without heterogeneity (OR: 1.67, 95% CI: 1.09–2.58; I2 = 51.2%, P = 0.129).
Fig 5. Unfavorable functional outcome prediction for patients managed by intra-arterial endovascular treatment (subgroup analysis).
(A) Scale by using PC-ASPECTS per score decrease. (B) Scale by using PC-ASPECTS with a cut-off value. (C) Scale by standardized mean difference in PC-ASPECTS scores between patients with unfavorable and favorable outcomes. (D) Funnel plot of scale by standardized mean difference.
(2) OR meta-analysis for binary PC-ASPECTS by cut-off score
Three studies [21,25,26] were included for PC-ASPECTS with cut-off points at 6, 7, and 9 (Fig 5B). The overall results demonstrated a significant association between UFO and binary PC-ASPECTS, with no heterogeneity (OR: 4.91, 95% CI: 2.40–10.05; I2 = 0.0%, P = 0.845).
(3) SMD meta-analysis between unfavorable and favorable outcomes of PC-ASPECTS
In total, 13 studies were eligible in this meta-analysis (Fig 5C). Of these, six studies showed no significance in scores of PC-ASPECTS for patients with unfavorable and favorable outcomes, whereas seven studies showed no significant difference. Consistent with the analysis for patients on any treatment regimen, the overall SMD meta-analysis result for IA-EVT displayed a significant difference in PC-ASPECTS between unfavorable and favorable outcomes (SMD: −0.54, 95% CI: −0.7 to −0.38; I2 = 78.7%, P = 0.000). The funnel plot (Fig 5D) followed by Begg’s test revealed no significant publication bias (P = 0.246). In addition, a meta-regression (S3 Table) exhibited a borderline significant association between the SMD of PC-ASPECTS and the imaging modality of CT or MRI (P = 0.05), with no significant differences between different definitions of mRS (P = 0.422).
Sensitivity analyses
We conducted two sensitivity analyses: (1) with varied imaging modalities of CT or MRI, and (2) definition of UFO according to an mRS 3–6 or 4–6.
(1) Different imaging modality
OR meta-analysis for PC-ASPECTS per score decrease. Six studies with MRI (OR: 1.81, 95% CI: 1.44–2.27; I2 = 26.3%, P = 0.237) and one study with CT (OR: 1.65, 95% CI: 1.09–2.73) showed scoring of PC-ASPECTS significantly associated with UFO (S1 Fig).
OR meta-analysis for binary PC-ASPECTS by cut-off score. Four studies with MRI showed PC-ASPECTS significantly associated with UFO (OR: 5.09, 95% CI: 2.96–8.78; I2 = 0.0%, P = 0.869), whereas two studies with CT revealed no significant association between PC-APSECTS and UFO (OR: 3.84, 95% CI: 0.70–20.90; I2 = 66.2%, P = 0.085) (S2 Fig).
SMD meta-analysis between unfavorable and favorable outcomes of PC-ASPECTS. Twelve studies with MRI showed PC-ASPECTS significantly predicted UFO (SMD: −0.93, 95% CI: −1.09 to −0.77; I2 = 69.9%, P = 0.000), whereas six studies with CT demonstrated no significant association between PC-ASPECTS and UFO (SMD: −0.19, 95% CI: −0.42 to 0.03; I2 = 0.0%, P = 0.524) (S3 Fig).
(2) Different definition of unfavorable outcomes by mRS
With different definitions of UFO, PC-ASPECTS showed significantly predicted the UFO with varied definitions of mRS of 3–6 and 4–6 in three scales (S4, S5 and S6 Figs).
Discussion
This meta-analysis confirmed that baseline PC-ASPECTS effectively predict functional outcomes for patients with posterior circulation acute ischemic stroke. We analyzed its association with UFO using the following three scales: (1) PC-ASPECTS per score decrease, (2) binary PC-ASPECTS with a cut-off value, and (3) difference in PC-ASPECTS between patients with unfavorable and favorable outcomes. Each decrease in the PC-ASPECTS score was significantly associated with UFO prediction. Although the results among all cut-off value demonstrated significance, we recommended a cut-off value of 7 for PC-ASPECTS effectively discriminated between patients with unfavorable and favorable functional outcomes. Furthermore, for patients treated with IA-EVT, subgroup analyses indicated a robust association between UFO prediction and PC-ASPECTS.
Different therapeutic regimens
The included studies revealed the following varied thrombolytic therapeutic regimens for patients with posterior circulation acute ischemic stroke: IV thrombolysis, IA-EVT, combination of both, and no recanalization. Subgroup analyses for patients with IA-EVT revealed consistent results with any therapeutic regimen, and the significant heterogeneity disappeared for IA-EVT only in scale 1. This suggested that the heterogeneity in these studies might have been resulted from different intervention regimens. Despite different therapeutic regimens, the results of this meta-analysis still indicated that PC-ASPECTS have a good predicting value for identifying UFO. However, we recommend that further studies should confirm the ability of PC-ASPECTS to predict functional outcomes in subgroups treated with no recanalization or IV thrombolysis because few studies were included in our meta-analysis.
Studies with different binary PC-ASPECTS cut-offs
The included studies displayed a diverse range of cut-off values of binary PC-ASPECTS for UFO prediction (from PC-ASPECTS of ≤6 to 9). Most studies adopted cut-off points of ≤7 to 8. Despite all cut-off values displaying a significant association between UFO prediction and PC-ASPECTS, we considered that a cut-off of ≤7 would be more appropriate because of a strong effect size. The statistical test for effect size (ES) supported a cut-off point of PC-ASPECTS ≤ 7 being the best cut-off value due to the smallest raw and adjusted P value (S4 Table).
Studies with varied definitions of UFO and imaging modalities
In total, 25 studies were included in our meta-analysis. We noted a discrepancy in the definitions of UFO based on the mRS score. Of these, 17 studies defined favorable outcome as mRS scores ≤2, and the rest defined favorable outcome as mRS scores ≤3. In our analyses, we applied each study’s individual UFO definition because of a vague boundary between mRS scores 2 and 3 in clinical practice. Our sensitivity analysis suggested PC-ASPECTS was applicable in predicting UFO for studies with a varied boundary of mRS.
Besides, we noted a disparity of imaging modalities of CT and MRI were used for evaluating PC-ASPECTS. The sensitivity analysis suggested MRI should be preferred modality for employing PC-ASPECTS. The association between PC-ASPECTS and UFO with MRI showed significant in three scales, whereas with CT demonstrated significant for OR meta-analysis for PC-ASPECTS per score decrease only.
At last, the meta-regression analysis (S3 Table) for patients treated with IA-EVT supports the negligible effect on heterogeneity by UFO definition (P = 0.412). Conversely, imaging modality of CT or MRI caused a significant effect on the heterogeneity of this study (P = 0.039).
Limitation
Our study had some limitations. First, high heterogeneity was observed in most of our analyses, which may be caused by study designs, therapeutic regimens, and imaging modalities. Second, none of the included studies involving patients treated with IA-EVT were randomized trials, and data were derived from cohort studies without control groups. However, publication bias was mostly eliminated in our analyses.
Conclusion
This meta-analysis of retrospective studies revealed that low baseline PC-ASPECTS are significantly associated with UFO. PC-ASPECTS of <7 was the most reasonable cut-offs for predicting UFO. Imaging modality and recanalization regimen were responsible for the heterogeneity in our meta-analysis. Even a one-point decrease in PC-ASPECTS significantly affects the outcome.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
Lin SF conceived the idea; all authors have contributed to the design of the study; Lu WZ, Lin HA, Bai CH, and Lin SF, collected and managed the data, including quality control. Lin SF provided statistical advice on study design and analyzed the data. Lin SF supervised the conduct of the study. Lu WZ and Lin SF drafted the manuscript, and all authors contributed substantially to its revision. Lu WZ and Lin SF contributed equally. Lin SF takes responsibility for the paper as a whole.
Abbreviations
- ASPECTS
the Alberta stroke program early computed tomography computed tomography score
- BAO
Basilar artery occlusion
- CI
confidence interval
- CT
computed tomography
- CTA-SI
computed tomography angiography-source imaging
- DWI
diffusion-weighted imaging
- MRI
magnetic resonance imaging
- mRS
modified Rankin Scale
- NIHSS
National Institutes of Health Stroke Scale
- OR
odds ratio
- PC-ASPECTS
the posterior circulation Alberta stroke program early CT score
- SMD
standardized mean difference
- UFO
unfavorable functional outcomes
Data Availability
Datasets for this research are published literatures (please referred to the list of references) and the codes used for statistical analysis with Stata software, version 15 (StataCorp, Texas, USA) was available in the supplemental file.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Bogousslavsky J, Van Melle G, Regli F. The Lausanne Stroke Registry: analysis of 1,000 consecutive patients with first stroke. Stroke. 1988;19(9):1083–92. Epub 1988/09/01. 10.1161/01.str.19.9.1083 . [DOI] [PubMed] [Google Scholar]
- 2.Markus HS, van der Worp HB, Rothwell PM. Posterior circulation ischaemic stroke and transient ischaemic attack: diagnosis, investigation, and secondary prevention. Lancet Neurol. 2013;12(10):989–98. Epub 2013/09/21. 10.1016/S1474-4422(13)70211-4 . [DOI] [PubMed] [Google Scholar]
- 3.Akhtar N, Kamran SI, Deleu D, D’Souza A, Miyares F, Elsotouhy A, et al. Ischaemic posterior circulation stroke in State of Qatar. Eur J Neurol. 2009;16(9):1004–9. Epub 2009/06/23. 10.1111/j.1468-1331.2009.02709.x . [DOI] [PubMed] [Google Scholar]
- 4.Caplan LR, Wityk RJ, Glass TA, Tapia J, Pazdera L, Chang HM, et al. New England Medical Center Posterior Circulation registry. Ann Neurol. 2004;56(3):389–98. Epub 2004/09/07. 10.1002/ana.20204 . [DOI] [PubMed] [Google Scholar]
- 5.Paul NL, Simoni M, Rothwell PM, Oxford Vascular S. Transient isolated brainstem symptoms preceding posterior circulation stroke: a population-based study. Lancet Neurol. 2013;12(1):65–71. Epub 2012/12/05. 10.1016/S1474-4422(12)70299-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merwick A, Werring D. Posterior circulation ischaemic stroke. BMJ. 2014;348:g3175 Epub 2014/05/21. 10.1136/bmj.g3175 . [DOI] [PubMed] [Google Scholar]
- 7.Savitz SI, Caplan LR. Vertebrobasilar disease. N Engl J Med. 2005;352(25):2618–26. Epub 2005/06/24. 10.1056/NEJMra041544 . [DOI] [PubMed] [Google Scholar]
- 8.Maus V, Styczen H, Liman J, Maier I, Brehm A, Tsogkas I, et al. Intracranial mechanical thrombectomy of large vessel occlusions in the posterior circulation using SAVE. BMC Neurol. 2019;19(1):197 Epub 2019/08/20. 10.1186/s12883-019-1428-x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gory B, Mazighi M, Blanc R, Labreuche J, Piotin M, Turjman F, et al. Mechanical thrombectomy in basilar artery occlusion: influence of reperfusion on clinical outcome and impact of the first-line strategy (ADAPT vs stent retriever). J Neurosurg. 2018;129(6):1482–91. Epub 2018/01/13. 10.3171/2017.7.JNS171043 . [DOI] [PubMed] [Google Scholar]
- 10.National Institute of Neurological D, Stroke rt PASSG. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333(24):1581–7. Epub 1995/12/14. 10.1056/NEJM199512143332401 . [DOI] [PubMed] [Google Scholar]
- 11.Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000;355(9216):1670–4. Epub 2000/07/25. 10.1016/s0140-6736(00)02237-6 . [DOI] [PubMed] [Google Scholar]
- 12.Puetz V, Sylaja PN, Coutts SB, Hill MD, Dzialowski I, Mueller P, et al. Extent of hypoattenuation on CT angiography source images predicts functional outcome in patients with basilar artery occlusion. Stroke. 2008;39(9):2485–90. Epub 2008/07/12. 10.1161/STROKEAHA.107.511162 . [DOI] [PubMed] [Google Scholar]
- 13.Roman LS, Menon BK, Blasco J, Hernandez-Perez M, Davalos A, Majoie C, et al. Imaging features and safety and efficacy of endovascular stroke treatment: a meta-analysis of individual patient-level data. Lancet Neurol. 2018;17(10):895–904. Epub 2018/09/29. 10.1016/S1474-4422(18)30242-4 . [DOI] [PubMed] [Google Scholar]
- 14.Li W, Li S, Dai M, Wang S, Xiong Y. Comparisons of ASPECTS 5 and 6 for endovascular treatment in anterior circulation occlusive stroke. Interv Neuroradiol. 2017;23(5):516–20. Epub 2017/07/22. 10.1177/1591019917720920 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700 Epub 2009/07/23. 10.1136/bmj.b2700 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. Epub 2003/09/06. 10.1136/bmj.327.7414.557 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uno J, Kameda K, Otsuji R, Ren N, Nagaoka S, Maeda K, et al. Mechanical Thrombectomy for Basilar Artery Occlusion Compared with Anterior Circulation Stroke. World Neurosurg. 2020;134:e469–e75. Epub 2019/11/02. 10.1016/j.wneu.2019.10.097 . [DOI] [PubMed] [Google Scholar]
- 18.Zhang X, Luo G, Mo D, Ma N, Gao F, Zhang J, et al. Predictors of Good Outcome After Endovascular Treatment for Patients with Vertebrobasilar Artery Occlusion due to Intracranial Atherosclerotic Stenosis. Clin Neuroradiol. 2019;29(4):693–700. Epub 2018/12/01. 10.1007/s00062-018-0731-z . [DOI] [PubMed] [Google Scholar]
- 19.Lin SF, Chen CI, Hu HH, Bai CH. Predicting functional outcomes of posterior circulation acute ischemic stroke in first 36 h of stroke onset. J Neurol. 2018;265(4):926–32. Epub 2018/02/17. 10.1007/s00415-018-8746-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li C, Zhao W, Wu C, Shang S, Chen J, Ren M, et al. Outcome of endovascular treatment for acute basilar artery occlusion in the modern era: a single institution experience. Neuroradiology. 2018;60(6):651–9. Epub 2018/04/14. 10.1007/s00234-018-2011-7 . [DOI] [PubMed] [Google Scholar]
- 21.Yoon W, Kim SK, Heo TW, Baek BH, Lee YY, Kang HK. Predictors of Good Outcome After Stent-Retriever Thrombectomy in Acute Basilar Artery Occlusion. Stroke. 2015;46(10):2972–5. Epub 2015/09/04. 10.1161/STROKEAHA.115.010840 . [DOI] [PubMed] [Google Scholar]
- 22.Mourand I, Machi P, Milhaud D, Picot MC, Lobotesis K, Arquizan C, et al. Mechanical thrombectomy with the Solitaire device in acute basilar artery occlusion. J Neurointerv Surg. 2014;6(3):200–4. Epub 2013/05/07. 10.1136/neurintsurg-2012-010629 . [DOI] [PubMed] [Google Scholar]
- 23.Nagel S, Herweh C, Kohrmann M, Huttner HB, Poli S, Hartmann M, et al. MRI in patients with acute basilar artery occlusion—DWI lesion scoring is an independent predictor of outcome. Int J Stroke. 2012;7(4):282–8. Epub 2011/12/14. 10.1111/j.1747-4949.2011.00705.x . [DOI] [PubMed] [Google Scholar]
- 24.Tei H, Uchiyama S, Usui T, Ohara K. Posterior circulation ASPECTS on diffusion-weighted MRI can be a powerful marker for predicting functional outcome. J Neurol. 2010;257(5):767–73. Epub 2009/11/28. 10.1007/s00415-009-5406-x . [DOI] [PubMed] [Google Scholar]
- 25.Maus V, Kalkan A, Kabbasch C, Abdullayev N, Stetefeld H, Barnikol UB, et al. Mechanical Thrombectomy in Basilar Artery Occlusion: Presence of Bilateral Posterior Communicating Arteries is a Predictor of Favorable Clinical Outcome. Clin Neuroradiol. 2019;29(1):153–60. Epub 2017/12/21. 10.1007/s00062-017-0651-3 . [DOI] [PubMed] [Google Scholar]
- 26.Luo G, Mo D, Tong X, Liebeskind DS, Song L, Ma N, et al. Factors Associated with 90-Day Outcomes of Patients with Acute Posterior Circulation Stroke Treated By Mechanical Thrombectomy. World Neurosurg. 2018;109:e318–e28. Epub 2017/10/11. 10.1016/j.wneu.2017.09.171 . [DOI] [PubMed] [Google Scholar]
- 27.Lee WJ, Jung KH, Ryu YJ, Lee KJ, Lee ST, Chu K, et al. Acute Symptomatic Basilar Artery Stenosis: MR Imaging Predictors of Early Neurologic Deterioration and Long-term Outcomes. Radiology. 2016;280(1):193–201. Epub 2016/01/30. 10.1148/radiol.2016151827 . [DOI] [PubMed] [Google Scholar]
- 28.Puetz V, Khomenko A, Hill MD, Dzialowski I, Michel P, Weimar C, et al. Extent of hypoattenuation on CT angiography source images in basilar artery occlusion: prognostic value in the Basilar Artery International Cooperation Study. Stroke. 2011;42(12):3454–9. Epub 2011/10/01. 10.1161/STROKEAHA.111.622175 . [DOI] [PubMed] [Google Scholar]
- 29.Chen B, Yang L, Hang J, You S, Li J, Li X, et al. Predictive value of the THRIVE score for outcome in patients with acute basilar artery occlusion treated with thrombectomy. Brain Behav. 2019;9(10):e01418 Epub 2019/09/27. 10.1002/brb3.1418 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alemseged F, Shah DG, Bivard A, Kleinig TJ, Yassi N, Diomedi M, et al. Cerebral blood volume lesion extent predicts functional outcome in patients with vertebral and basilar artery occlusion. Int J Stroke. 2019;14(5):540–7. Epub 2017/11/22. 10.1177/1747493017744465 . [DOI] [PubMed] [Google Scholar]
- 31.Antunes Dias F, Castro-Afonso LH, Zanon Zotin MC, Alessio-Alves FF, Martins Filho R, Camilo MR, et al. Collateral Scores and Outcomes after Endovascular Treatment for Basilar Artery Occlusion. Cerebrovasc Dis. 2019;47(5–6):285–90. Epub 2019/08/23. 10.1159/000502083 . [DOI] [PubMed] [Google Scholar]
- 32.Rentzos A, Karlsson JE, Lundqvist C, Rosengren L, Hellstrom M, Wikholm G. Endovascular treatment of acute ischemic stroke in the posterior circulation. Interv Neuroradiol. 2018;24(4):405–11. Epub 2018/03/23. 10.1177/1591019918762320 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang JY, Jung S, Jung C, Bae HJ, Kwon O, Han MK. Dominant vertebral artery status and functional outcome after endovascular therapy of symptomatic basilar artery occlusion. J Neuroradiol. 2017;44(2):151–7. Epub 2017/01/31. 10.1016/j.neurad.2016.12.001 . [DOI] [PubMed] [Google Scholar]
- 34.Dias FA, Alessio-Alves FF, Castro-Afonso LH, Cougo PT, Barreira CMA, Camilo MR, et al. Clinical Outcomes of Patients with Acute Basilar Artery Occlusion in Brazil: An Observational Study. J Stroke Cerebrovasc Dis. 2017;26(10):2191–8. Epub 2017/05/30. 10.1016/j.jstrokecerebrovasdis.2017.04.043 . [DOI] [PubMed] [Google Scholar]
- 35.Lee WJ, Jung KH, Ryu YJ, Kim JM, Lee ST, Chu K, et al. Utility of digital subtraction angiography-based collateral evaluation in medically treated acute symptomatic basilar artery stenosis. Eur J Neurol. 2017;24(9):1148–55. Epub 2017/07/15. 10.1111/ene.13351 . [DOI] [PubMed] [Google Scholar]
- 36.Fahed R, Di Maria F, Rosso C, Sourour N, Degos V, Deltour S, et al. A leap forward in the endovascular management of acute basilar artery occlusion since the appearance of stent retrievers: a single-center comparative study. J Neurosurg. 2017;126(5):1578–84. Epub 2016/06/04. 10.3171/2016.2.JNS151983 . [DOI] [PubMed] [Google Scholar]
- 37.Son S, Kim YW, Oh MK, Kim SK, Park KJ, Choi NC, et al. Initial factors affecting the clinical outcome after successful recanalization via MR-based mechanical thrombectomy in patients with acute ischemic stroke due to basilar artery occlusion. J Neurointerv Surg. 2016;8(9):889–93. Epub 2015/09/16. 10.1136/neurintsurg-2015-011912 . [DOI] [PubMed] [Google Scholar]
- 38.Da Ros V, Meschini A, Gandini R, Del Giudice C, Garaci F, Stanzione P, et al. Proposal for a Vascular Computed Tomography-Based Grading System in Posterior Circulation Stroke: A Single-Center Experience. J Stroke Cerebrovasc Dis. 2016;25(2):368–77. Epub 2016/01/05. 10.1016/j.jstrokecerebrovasdis.2015.10.008 . [DOI] [PubMed] [Google Scholar]
- 39.Mundiyanapurath S, Mohlenbruch M, Ringleb PA, Bosel J, Wick W, Bendszus M, et al. Posterior Circulation Acute Stroke Prognosis Early Computed Tomography Score Using Hypointense Vessels on Susceptibility Weighted Imaging Independently Predicts Outcome in Patients with Basilar Artery Occlusion. PLoS One. 2015;10(7):e0132587 Epub 2015/07/16. 10.1371/journal.pone.0132587 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Karameshev A, Arnold M, Schroth G, Kappeler L, Stein P, Gralla J, et al. Diffusion-weighted MRI helps predict outcome in basilar artery occlusion patients treated with intra-arterial thrombolysis. Cerebrovasc Dis. 2011;32(4):393–400. Epub 2011/10/12. 10.1159/000330644 . [DOI] [PubMed] [Google Scholar]