Abstract
The World Health Organization has recently set standards emphasising the importance of emotional support during birth for improving the quality of maternal and newborn healthcare in facilities. In this study, we explore the emotional support status of women during birth in rural Bangladesh. A cross-sectional household survey of 1367 women was administered in 2018 in Brahmanbaria district. Outcomes of interest included: presence of a companion of choice; mobility; intake of fluids and food; and position of choice. Associations between outcomes of interest and background characteristics were explored through binary and multiple logistic regressions. Approximately 68% women had a companion of choice during labour or childbirth, significantly higher among women giving birth at home (75%) than in a health facility. Nearly 60% women were allowed to eat and drink during labour, also significantly higher among women giving birth at home. Seventy-per cent women were allowed to be ambulatory during labour (46% in a facility vs. 85% at home). Only 27% women were offered or allowed to give birth in the position of their choice at facility, compared to 54% giving birth at home. Among women giving birth in a facility who did not have a companion of choice, 39% reported that the health provider/health facility management did not allow this. Ensuring emotional support and thereby improving the quality of the experience of care within health facilities should be prioritised by the Bangladesh government both to improve health outcomes of women and newborns and also to promote more humanised, positive childbirth experiences.
Keywords: maternal health, newborn health, pregnant women, respectful maternity care, emotional support, child birth, quality of care, rights, male involvement
Résume
L’Organisation mondiale de la santé a récemment défini des normes soulignant l’importance du soutien psychologique pendant la naissance pour améliorer la qualité des soins de la mère et du nouveau-né dans les établissements de santé. Dans cette étude, nous nous penchons sur la situation du soutien psychologique des femmes pendant l’accouchement dans le Bangladesh rural. En 2018, une enquête transversale auprès des ménages a interrogé 1367 femmes dans le district de Brahmanbaria. Les résultats d’intérêt incluaient: la présence d’un compagnon de choix; la mobilité; la prise de liquides et d’aliments; et la position de choix. Les associations entre les résultats d’intérêt et les caractéristiques propres ont été étudiées par des régressions logistiques binaires et multiples. Environ 68% des femmes avaient eu un compagnon de leur choix pendant le travail ou la délivrance, nettement plus chez les femmes ayant accouché à la maison (75%) que dans une structure de santé. Près de 60% des femmes avaient pu manger et boire pendant le travail, un pourcentage aussi nettement supérieur chez les femmes ayant accouché chez elles. Pendant le travail, 70% des femmes avaient été autorisées à se mouvoir (46% dans un centre, contre 85% à la maison). Seules 27% des femmes accouchant dans un centre de santé se sont vu offrir de donner naissance dans la position de leur choix ou ont été autorisées à le faire, contre 54% pour celles qui étaient chez elles. Parmi les femmes ayant donné naissance dans une structure de santé et qui n’avait pas eu le compagnon de leur choix, 39% ont indiqué que c’était le prestataire de soins de santé/la direction du centre qui ne l’avait pas permis. Garantir un soutien psychologique et améliorer ainsi la qualité de l’expérience des soins dans les structures de santé devrait représenter une priorité du Gouvernement bangladeshi pour améliorer l’état de santé des femmes et des nouveau-nés, mais aussi pour promouvoir des expériences de la naissance plus humanisées et plus positives.
Resumen
La Organización Mundial de la Salud recientemente estableció estándares que hacen hincapié en la importancia de brindar apoyo emocional durante el parto para mejorar la calidad de los servicios de salud materna y de salud del recién nacido en establecimientos de salud. En este estudio exploramos el estado del apoyo emocional brindado a mujeres durante el parto en zonas rurales de Bangladesh. En el año 2018, se administró una encuesta domiciliaria transversal a 1367 mujeres en el distrito de Brahmanbaria. Entre los resultados de interés figuran: presencia de un acompañante de elección; movilidad; ingesta de líquidos y alimentos; y posición de elección. Se exploraron las asociaciones entre los resultados de interés y las carácterísticas básicas por medio de regresiones binarias y regresiones logísticas múltiples. Aproximadamente el 68% de las mujeres tenían un acompañante de elección durante el trabajo de parto o el parto; el porcentaje fue significativamente más alto entre mujeres que dieron a luz en su casa (75%) que entre las que dieron a luz en un establecimiento de salud. A casi el 60% de las mujeres se les permitió comer y beber algo durante el parto, porcentaje que también fue significativamente más alto entre las mujeres que dieron a luz en su casa. Al 70% de las mujeres se les permitió ser ambulatorias durante el trabajo de parto (46% dio a luz en un establecimiento de salud vs. 85% en su casa). Solo al 27% de las mujeres que dieron a luz en un establecimiento de salud se les ofreció o se les permitió dar a luz en la posición de su elección, comparado con el 54% que dio a luz en su casa. Entre las mujeres que dieron a luz en un establecimiento de salud que no tenían un acompañante de su elección, el 39% informó que el prestador de servicios de salud o la administración del establecimiento de salud no permitieron esto. El gobierno de Bangladesh debe dar prioridad a garantizar apoyo emocional y, por ende, mejorar la calidad de la experiencia de recibir servicios de salud en establecimientos de salud, tanto para mejorar los resultados de salud de las mujeres y recién nacidos como para promover experiencias de parto más positivas y más humanizadas.
Background
Throughout the greater part of history, childbirth typically occurred in a labouring woman’s home, with the support of her close social network. Over the course of the past two centuries, moving births primarily into health facilities equipped to manage common birth-related complications, along with ensuring the presence of skilled health service providers, has contributed to preventing innumerable deaths of women and newborns globally.1–3 However, there is also concern that this medicalisation of childbirth 4–7 may have contributed to a dehumanisation of the birthing experience, with women losing many of the benefits of the social and emotional support which they used to enjoy while giving birth in a home environment.8–11 Over the past few decades, global initiatives aiming to improve the quality of maternal and newborn health services focused predominantly on the clinical provision of care.12,13 In recent years, there has been an evolution in this regard. The quality around the experience of care has been gaining attention at the global level, both as an essential element of improving health outcomes, as well as a matter of principle to humanise the birthing experience.14–16
The World Health Organization (WHO) has recently set standards for improving the quality of maternal and newborn healthcare in facilities, which apply to the care that women and newborns receive during the intrapartum period globally.14,15 The quality of care standards position the experience of care at an equal level with the provision of clinical care within the conceptual framework they propose. In this framework, three domains are identified falling under the umbrella of the experience of care: effective communication, respect and preservation of dignity, and emotional support.15 Within the domain of emotional support, WHO recommends ensuring that every woman, along with her family, is provided emotional support during childbirth which includes the option of having a companion of choice during labour and birth, being allowed to be ambulatory during the first stages of labour, being permitted to intake fluids and food during the early stages of labour and being encouraged to give birth in the position of the woman’s choice.15
Emotional support during childbirth has been associated with both improved childbirth experiences and improved maternal and newborn health outcomes.17,18 While emotional support during birth has been increasingly emphasised in some high-income countries, it has tended to be neglected in low-resource settings, where the clinical provision of services has dominated attention around the quality of care at the time of birth. Recently, this has been shifting, as it has become recognised globally that all women have the right to benefit from a positive childbirth experience and that emotional support is necessary for realisation of this right, as well as for improving health outcomes.19,20 However, to date, there is a dearth of evidence related to women’s experiences of emotional support during childbirth in low-resource settings.
While Bangladesh has made impressive improvements in maternal and newborn health over the past several decades, the mortality burden still remains too high, with a maternal mortality ratio of 196 per 100,000 live births,21 particularly as the majority of these deaths are considered preventable.22 Use of formal services* for maternal and newborn health care remains critically low and over half (53%) of births continue to occur at home, most without the support of a trained health service provider,21 despite facility birth being a central goal of both global and national maternal health strategies.23,24
Moreover, the quality of services that women receive within the formal health system for pregnancy and childbirth care is often sub-optimal.25,26 Challenges are particularly pronounced in rural areas where it is difficult to recruit and retain trained healthcare personnel and maintain the quality of health services.27 While the status of the clinical provision services related to childbirth in the country has been well documented through national surveys and studies,25,26,28 little is known regarding the status of the experience of care, notably the emotional support the women receive during childbirth. Furthermore, there is an evidence gap with regard to the emotional support which women receive in the home setting compared to the facility setting. This is of critical importance in a context such as Bangladesh where half of births continue to occur at home.29
Expectations of emotional support may influence care-seeking behaviour and women’s decisions related to the place of birth, particularly as health facilities for women in rural communities have been found to be associated with sadness, fear and strangers, therefore dissuading them from choosing to give birth in this medicalised setting.30–32 The objective of this article is to address this key evidence gap by exploring the status of emotional support that women enjoy during birth in health facilities and at home in terms of the presence of a companion of choice at birth, mobility, intake of fluids and food during labour and position of choice during birth in rural Bangladesh. Moreover, we explore the associations between selected social, economic and demographic characteristics and the degree of emotional support that women enjoy when giving birth within these four categories.
Methods
Study design and settings
This is a cross-sectional study based on a household survey administered in 2018 in the district of Brahmanbaria. The survey was conducted as a baseline study to measure the effects of a package of health promotion interventions which was planned to be rolled out in the site. Brahmanbaria district is located in the east of Bangladesh along the border with India. Approximately three million people live in the district, which has a predominantly agriculture-based economy. We conducted the survey in three upazilas (sub-districts): namely, Bijoynagar, Kasba and Sarail, each with an approximate population of 300,000. No large scale maternal and newborn health programme was in place at the time of the survey. Supplementary Table 1 outlines the population and health systems of the selected upazilas.
Study population, sample size and sampling
Women who had given birth in the 12-month period preceding the survey and were permanent residents of the study upazilas were considered as eligible respondents. Stratified cluster sampling was used to identify potential survey respondents. The three selected upazilas were taken as the strata and the villages, with an approximate population of 1000, were considered as clusters. Using probability proportional to size (PPS) sampling, we selected 20 villages (PPS clusters) within each of the study upazilas (strata). Thereafter, all eligible women of the selected villages were invited to participate in the survey using an interviewer-administered structured questionnaire. All participants were alone during the interview and not in a position to be overheard by others. A total of 1367 women participated in the survey. The non-response rate was just under 1%. This was achieved by making at least three consecutive attempts to interview each participant, arranging interviews according to the participant’s convenience and through the employment of local interviewers. A detailed description of the sample size calculation is provided in Supplementary Table 2.
Data collection
Data were collected between the months of March and May 2018. A sketch map of the selected villages was drawn at the outset of data collection, indicating village boundaries, important landmarks and extended household locations. All households were then enumerated and listed, following which eligible women were identified within each household. All eligible respondents were approached by trained interviewers who administered the questionnaire.
The structured questionnaire included a number of questions regarding knowledge and practices of women and families around maternal and newborn health. The majority of the questions were adopted or adapted from validated tools, including Bangladesh Demographic and Health Survey (BDHS), Bangladesh Maternal Mortality Survey (BMMS), Multiple Indicator Cluster Survey (MICS) and other relevant studies.25,33,34 The data collection instruments were pre-tested in non-selected clusters of the upazilas in which the study was carried out and revised based on the pre-test findings.
Data collectors were recruited locally so that they would be familiar with the local language, culture and norms and thereby facilitate access to the communities. All interviewers received three days of training on the data collection tools followed by another three days of field practice prior to the commencement of data collection. The training was conducted by the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) study investigators and master trainers with expertise in conducting household surveys. Refresher trainings were organised fortnightly throughout the data collection period.
Field supervisors conducted periodic joint visits with the data collectors to observe the interviews and monitor the quality of data collection. On average, two joint visits were conducted per data collector per week. The field supervisor provided feedback to the data collector immediately after completing the joint visit. In addition, a random sample of 5% of households was revisited by the field supervisors. Any discrepancies were resolved with the original data. In addition, weekly review meetings were conducted with all the data collectors in each upazila to review the questionnaire and discuss key observations from joint visits, revisits and form reviews. Detailed feedback was provided on key issues and common mistakes to improve the quality of data collection.
Data analysis
Data were analysed using Stata 13.0 (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: Stata Corp LP.)
Socio-demographic characteristics, e.g. age, educational attainment of women, family size and parity were transformed into categorical variables. Due to small numbers, all other religions except “Muslim” were grouped into one category and coded as “other”. We used the standard steps of principal component analysis to generate the socio-economic indices of the households that were interviewed, based on which the wealth quintile was generated.35,36 Household-level variables such as household possessions; materials used for the construction of floor, wall, and roof; drinking water source; toilet facilities; and ownership of land and domestic animals were used to generate this index. Background characteristics were presented separately for facility births and home births.
Regarding emotional support, the following indicators were selected based on the WHO-recommended Quality of Care Framework and proposed standards related to emotional support:
companion of choice: the proportion of women who gave birth in the past 12 months who had a companion of their choice during labour and childbirth;
food and drink: the proportion of women who gave birth in the past 12 months who were allowed to have food and drink during labour;
mobility: the proportion of women who gave birth in the past 12 months who were allowed to be ambulatory during the first stage of labour;
position of choice: the proportion of women who gave birth in the past 12 months who did so in the position of their choice.
We used descriptive statistics (proportions) to report the indicators related to background characteristics and emotional support during labour and childbirth. Chi-square tests were initially used to explore whether there was any difference between facility births and home births regarding these indicators. Any significant difference was reported at p < .05.
We looked at the relationship between background characteristics and facility births and home births separately. Binary logistic regression was used to report the associations between explanatory variables (background characteristics) and outcomes of interest (emotional support). The effects of the co-variates and confounders were adjusted by multiple logistic regressions. Only the variables found significant (p < .15) in the binary logistic regression were included in the subsequent multiple logistic regression models as recommended by Bursac et al37 All odds ratios (ORs) and adjusted odds ratios (AORs) were reported with 95% confidence intervals (CI). An association (OR or AOR) was considered significant if both the lower and the upper limit of the CI were more or less than 1. The final list of variables used for each of this model is presented in Supplementary Table 3.
Findings
Table 1 presents the background characteristics of the women who had a history of childbirth in the 12 months preceding the survey. The mean age of the respondents was 25 years (SD 5.2). There was a significant difference in the age of the women between those who gave birth in a facility and those who gave birth in their homes (p = .01). Around 20% of the women had 10 or more years of formal schooling, which was higher among women who gave birth in facilities (35%) compared to those who had home births (13%). The majority of the respondents were Muslim (97%). Around three-quarters of the women belonged to families composed of five or more members, which was slightly higher among those who had homebirths (78%). Around 70% of the respondents were multiparous: 62% of women giving birth in a facility and 75% of women giving birth at home. Nearly two-thirds of women gave birth at home. Only 3% gave birth in public facilities and one-third gave birth in private health facilities. Nearly half of the respondents reported that their husbands live outside the home or abroad. A negligible proportion of the women (less than 5%) had been involved in any sort of income generating activities in the past 12 months.
Table 1. Background characteristics of study respondents.
| Background characteristics | All | Facility Birth | Home Birth | P-value |
|---|---|---|---|---|
| N = 1367 | N = 503 | N = 864 | ||
| % | % | % | ||
| Age | ||||
| ≤ 24 years | 48.4 | 52.1 | 46.3 | 0.012 |
| 25–34 years | 43.7 | 42.5 | 44.3 | |
| ≥35 years | 7.9 | 5.4 | 9.4 | |
| Education | ||||
| Secondary incomplete (0-9 years) | 79.1 | 64.8 | 87.4 | 0.000 |
| Secondary complete or higher (≥10 years) | 20.9 | 35.2 | 12.6 | |
| Religion | ||||
| Muslim | 97.4 | 96.6 | 97.8 | 0.189 |
| Other (Hindu/ Christian etc.) | 2.6 | 3.4 | 2.2 | |
| Family Size | ||||
| ≤4 | 24.8 | 29.8 | 21.9 | 0.001 |
| ≥5 | 75.2 | 70.2 | 78.1 | |
| Parity | ||||
| Nulliparous | 30.1 | 37.9 | 25.6 | 0.000 |
| Multiparous | 69.7 | 61.6 | 74.3 | |
| Type of birth attendant | ||||
| Doctor | 34.1 | 90.1 | 1.5 | 0.000 |
| Nurse, midwife, paramedic, family welfare visitors | 6.4 | 8.4 | 5.2 | |
| Community health workers | 0.5 | 0.4 | 0.58 | |
| Traditional birth attendant or other | 59.0 | 1.2 | 92.7 | |
| Place of birth | ||||
| Home | 63.2 | N/A | N/A | 0.000 |
| Public facility | 3.3 | 9.0 | N/A | |
| Private facility | 33.5 | 91.0 | N/A | |
| ANC from a health facility | ||||
| No | 36.9 | 18.9 | 47.3 | 0.000 |
| Yes | 63.1 | 81.1 | 52.7 | |
| Husband living status | ||||
| With wife | 55.4 | 51.5 | 57.8 | 0.025 |
| Lives in another place within the country or abroad | 44.6 | 48.5 | 42.2 | |
| Income generating activities | ||||
| No | 95.8 | 96.8 | 95.2 | 0.163 |
| Yes | 4.2 | 3.2 | 4.8 | |
| Wealth quintile | ||||
| Lowest | 20.0 | 10.1 | 25.8 | 0.000 |
| Second | 20.0 | 17.9 | 21.2 | |
| Middle | 20.0 | 18.7 | 20.8 | |
| Fourth | 20.0 | 22.1 | 18.8 | |
| Highest | 20.0 | 31.2 | 13.4 |
Table 2 presents the status of emotional support during childbirth among the respondents for their most recent birth. Across all categories of emotional support, the practices were much better among women giving birth at home. Around 68% of women had a companion of choice during labour or childbirth, which was significantly higher among women giving birth at home (75%) compared to women giving birth in a health facility (56%) (p = .000). Nearly 60% of women were allowed to eat and drink during labour. The practice was significantly higher among women giving birth at home (34% of women giving birth in a facility vs.74% of women giving birth at home, p = .000). Seventy-percent of women were allowed to be ambulatory during the first stages of labour, which was 46% among women giving birth in a facility and 85% among women giving birth at home (p = .000). Only 27% of the women who gave birth at a facility were offered or allowed to give birth in the position of their choice, compared to 54% of those giving birth at home (p = .000).
Table 2. Status of emotional support during labour and childbirth among women who had a recent history of childbirth.
| Emotional support | All | Facility birth | Home birth | P-values (from chi2) |
|---|---|---|---|---|
| N = 1367 | N = 503 | N = 864 | ||
| % | % | % | ||
| Had a companion of choice during labour or childbirth | 67.7 | 55.5 | 74.8 | .000 |
| Were allowed to eat and drink during labour | 59.3 | 33.6 | 74.3 | .000 |
| Were allowed to be ambulatory during the first stages of labour | 70.7 | 46.1 | 84.9 | .000 |
| Offered or allowed to give birth in the position of their choice | 43.8 | 26.6 | 53.8 | .000 |
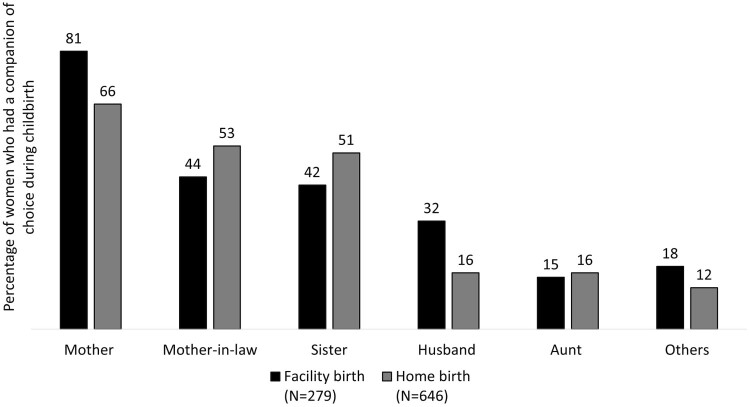
Figure 1 illustrates the types of members of women’s social networks who were present as a birth companion among women who reported having had a companion of choice during their most recent childbirth (multiple responses considered). Mothers were the most common birth companion, followed by mothers-in-law, sisters, husbands and aunts. Mothers were more common as a birth companion among women giving birth in a facility (81%), compared to women giving birth at home (66%) (p = .000). In contrast, mothers-in-law were more common as a birth companion among women giving birth at home (53%), compared to women giving birth in a facility (44%) (p = .009). Among women giving birth at home with a companion of choice, 51% reported the presence of a sister, compared to 42% of women giving birth in a facility (p = .009). The presence of the husband as a birth companion was more common among women giving birth in a facility (32%) than those giving birth at home (16%) (p = .000).
Figure 1.
Type of birth companion among women who had a companion of choice during childbirth (multiple responses considered)
Table 3 presents the association between different components of emotional support and background characteristics among women giving birth in a facility. Those who attended at least one antenatal care (ANC) contact at a health facility were more likely to have a companion of choice of during their childbirth (AOR 2.5, CI 1.6–4.0). Giving birth in a private facility or hospital was negatively associated with having a companion of choice during childbirth (AOR 0.52, CI 0.26–0.99). Similarly, non-Muslim women were less likely to have a companion of choice during childbirth (AOR 0.05, CI 0.01–0.36). Women who attended at least one ANC contact at a health facility were more likely to be offered and allowed to give birth in the position of their choice (AOR 2.6 CI 1.4–5.0). In contrast, those who had 10 or more years of formal education were less likely to be offered or allowed to give birth in the position of their choice (AOR 0.62 CI 0.4–0.9). Women who were attended during childbirth by doctors were also less likely to be permitted to eat and drink during labour (AOR 0.53, CI 0.28–0.97) or allowed to be ambulatory during the first stages of labour (AOR 0.48, CI 0.26–0.91). Women giving birth in a private facility were less likely to be permitted to eat and drink during labour (AOR 0.55, CI 0.29–1.0, p = .069) or allowed to be ambulatory during the first stages of labour (AOR 0.49, CI 0.25–.97).
Table 3. Association between different components of emotional support during childbirth and background characteristics among women giving birth in a facility (N = 503).
| Had a companion of choice during labour or childbirth | Offered or allowed to give birth in the position of their choice | Were allowed to eat and drink during labour | Were allowed to be ambulatory during the first stages of labour | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | OR (CI) | AOR (CI) | % | OR (CI) | AOR (CI) | % | OR (CI) | AOR (CI) | % | OR (CI) | AOR (CI) | |
| Age of woman | ||||||||||||
| 15–24 | 57.6 | Ref | Ref | 26.7 | Ref | Ref | 34.7 | Ref | Ref | 47.7 | Ref | Ref |
| 25–34 | 52.3 | 0.81 (0.56–1.2) |
__ | 26.6 | 0.99 (0.66–1.5) |
__ | 31.8 | 0.87 (0.60–1.3) |
__ | 44.4 | 0.87 (0.61–1.3) |
__ |
| 35+ | 59.3 | 1.1 (0.48–2.4) |
__ | 25.9 | 0.96 (0.39–2.4) |
__ | 37.0 | 1.1 (0.49–2.5) |
__ | 44.4 | 0.88 (0.40–1.9) |
__ |
| Education | ||||||||||||
| 0–9 years | 58.3 | Ref | Ref | 29.8 | Ref | Ref | 34.1 | Ref | Ref | 46.3 | Ref | Ref |
| 10 or more years | 50.3 | 0.72 (0.50–1.0) |
0.72 (0.47–1.1) |
20.9 | 0.62 (0.40–0.96) |
0.63 (0.39–1.0) |
32.8 | 0.94 (0.64–1.4) |
__ | 45.8 | 0.98 (0.68–1.4) |
__ |
| Religion | ||||||||||||
| Muslim | 57.2 | Ref | Ref | 26.9 | Ref | Ref | 33.9 | Ref | Ref | 46.5 | Ref | Ref |
| Other | 5.9 | 0.05 (0.01–0.36) |
0.05 (0.01–0.36) |
17.7 | 0.58 (0.16–2.1) |
__ | 23.5 | 0.60 (0.19–1.9) | __ | 35.3 | 0.63 (0.23–1.7) |
__ |
| Family size | ||||||||||||
| ≤4 | 59.3 | Ref | Ref | 32.7 | Ref | Ref | 31.3 | Ref | Ref | 48 | Ref | Ref |
| ≥5 | 53.8 | 0.80 (0.54–1.2) |
__ | 24.1 | 0.65 (0.43–0.99) |
0.66 (0.42–1.0) |
34.6 | 1.2 (0.77–1.7) |
__ | 45.3 | 0.90 (0.61–1.3) |
__ |
| Parity | ||||||||||||
| Nulliparous | 50.3 | Ref | Ref | 22.3 | Ref | Ref | 33.5 | Ref | Ref | 50.3 | Ref | Ref |
| Multiparous | 58.7 | 1.4 (0.98–2.0) |
1.2 (0.84–1.8) |
29.4 | 1.5 (0.97–2.2) |
1.4 (0.93–2.2) |
33.9 | 1.0 (0.69–1.5) |
__ | 43.9 | 0.77 (0.54–1.1) |
__ |
| Type of birth attendant | ||||||||||||
| Nurses/midwives/paramedics | 64.0 | Ref | Ref | 36 | Ref | Ref | 50 | Ref | Ref | 66.0 | Ref | Ref |
| Doctor | 54.5 | 0.67 (0.37–1.2) |
__ | 25.6 | 0.61 (0.33–1.1) |
0.55 (0.28–1.1) |
31.8 | 0.47 (0.26–0.84) |
0.53 (0.28–0.97) |
44.0 | 0.40 (0.22–0.75) |
0.48 (0.26–0.91) |
| Type of health facility | ||||||||||||
| Public facility | 71.1 | Ref | Ref | 31.1 | Ref | Ref | 51.1 | Ref | Ref | 66.7 | Ref | Ref |
| Private facility | 53.9 | 0.48 (0.24–0.93) |
0.52 (0.26–0.99) |
26.2 | 0.79 (0.40–1.5) |
0.55 (0.29–1.0) |
31.9 | 0.45 (0.24–0.83) |
0.55 (0.29–1.0) |
44.1 | 0.39 (0.21–0.75) |
0.49 (0.25–0.97) |
| ANC from facility | ||||||||||||
| No | 38.9 | Ref | Ref | 13.7 | Ref | Ref | 35.8 | Ref | Ref | 45.3 | Ref | Ref |
| Yes | 59.3 | 2.3 (1.4–3.6) |
2.5 (1.6–4.0) |
29.7 | 2.7 (1.4–4.9) |
2.6 (1.4–5.0) |
33.1 | 0.89 (0.56–1.4) |
__ | 46.3 | 1.0 (0.67–1.6) |
__ |
| Husband living status | ||||||||||||
| Lives with wife | 56.4 | Ref | Ref | 25.5 | Ref | Ref | 32.8 | Ref | Ref | 43.2 | Ref | Ref |
| Lives in other places within the country or abroad | 54.5 | 0.93 (0.65–1.3) |
__ | 27.9 | 1.1 (0.76–1.7) |
__ | 34.4 | 1.1 (0.74–1.6) |
__ | 49.2 | 1.3 (0.89–1.8) |
__ |
| Income generating activities | ||||||||||||
| No | 55.9 | ref | Ref | 27.3 | ref | Ref | 34.1 | Ref | Ref | 46.4 | Ref | Ref |
| Yes | 43.8 | 0.61 (0.23–1.7) |
__ | 6.3 | 0.18 (0.02–1.4) |
0.16 (0.02–1.3) |
18.8 | 0.45 (0.13–1.6) |
__ | 37.5 | 0.69 (0.25–1.9) |
__ |
| Wealth quintile | ||||||||||||
| Lowest | 70.6 | Ref | Ref | 45.1 | Ref | Ref | 51.0 | Ref | Ref | 64.7 | Ref | Ref |
| Second | 53.3 | 0.48 (0.23–0.99) |
0.50 (0.24–1.1) |
23.3 | 0.37 (0.18–0.77) |
0.37 (0.18–0.79) |
32.2 | 0.46 (0.23–0.93) |
0.47 (0.23–0.97) |
45.6 | 0.46 (0.22–0.93) |
0.47 (0.23–0.97) |
| Middle | 50 | 0.42 (0.20–0.86) |
0.48 (0.22–1.0) |
20.2 | 0.31 (0.15–0.65) |
0.35 (0.16–0.75) |
34.0 | 0.50 (0.25–0.99) |
0.54 (0.27–1.1) |
44.7 | 0.44 (0.22–0.89) |
0.48 (0.24–0.99) |
| Fourth | 52.3 | 0.46 (0.22–0.93) |
0.54 (0.25–1.1) |
24.3 | 0.39 (0.19–0.79) |
0.45 (0.22–0.94) |
29.7 | 0.41 (0.21–0.81) |
0.42 (0.21–0.84) |
47.8 | 0.50 (0.25–0.99) |
0.52 (0.26–1.0) |
| Highest | 57.3 | 0.56 (0.28–1.1) |
0.69 (0.33–1.4) |
28.0 | 0.47 (0.25–0.91) |
0.62 (0.31–1.2) |
31.2 | 0.44 (0.23–0.83) |
0.48 (0.25–0.93) |
40.1 | 0.37 (0.19–0.71) |
0.41 (0.21–0.79) |
Table 4 presents the association between different components of emotional support during childbirth and background characteristics among women giving birth at home. None of the background characteristics of the women were found to be significantly associated with having a companion of choice during childbirth after adjusting for co-variates and confounders. Women over 35 years of age were more likely to be allowed to give birth in the position of their choice (AOR 1.9, CI 1.1–3.1). In addition, the women who had 10 or more years of formal education were less likely to be offered or allowed to give birth in the position of their choice (AOR 0.62, CI 0.4–0.9). Women who were not Muslims were less likely to be allowed to have food and drink during labour (AOR 0.38, CI 0.15–0.96) or allowed to be ambulatory during the first stages of labour (AOR 0.30, CI 0.11–0.87).
Table 4. Association between different components of emotional support during childbirth and background characteristics among women giving birth at home (N = 864).
| Had a companion of choice during labour or childbirth |
Offered or allowed to give birth in the position of their choice | Were allowed to eat and drink during labour | Were allowed to be ambulatory during the first stages of labour |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | OR (CI) | AOR (CI) | % | OR (CI) | AOR (CI) | % | OR (CI) | AOR (CI) | % | OR (CI) | AOR (CI) | |
| Age of woman | ||||||||||||
| ≤ 24 years | 73.8 | Ref | Ref | 52.0 | Ref | Ref | 75.8 | Ref | Ref | 86.3 | Ref | Ref |
| 25–34 years | 75.7 | 1.1 (0.80–1.5) |
__ | 52.7 | 1.0 (0.78–1.4) |
1.0 (0.76–1.3) |
73.4 | 0.88 (0.64–1.2) |
__ | 84.1 | 0.84 (0.57–1.2) |
__ |
| ≥35 years | 75.3 | 1.1 (0.63–1.9) |
__ | 67.9 | 2.0 (1.2–3.2) |
1.9 (1.1–3.1) |
71.6 | 0.81 (0.47–1.4) |
__ | 82.7 | 0.76 (0.40–1.5) |
__ |
| Education of women | ||||||||||||
| 0–9 years | 75.8 | Ref | Ref | 55.2 | Ref | Ref | 73.8 | Ref | Ref | 83.8 | Ref | Ref |
| ≥10 years | 67.9 | 0.68 (0.44–1.0) |
0.69 (0.45–1.1) |
44.0 | 0.64 (0.43–0.96) |
0.62 (0.41–0.94) |
78.0 | 1.3 (0.78–2.0) |
__ | 92.7 | 2.4 (1.2–5.1) |
2.1 (0.94–4.5) |
| Religion | ||||||||||||
| Muslim | 75.2 | Ref | Ref | 54.0 | Ref | Ref | 74.8 | Ref | Ref | 85.3 | Ref | Ref |
| Other | 57.9 | 0.45 (0.18–1.1) |
0.48 (0.19–1.2) |
47.3 | 0.77 (0.31–1.9) |
__ | 52.6 | 0.37 (0.15–0.93) |
0.38 (0.15–0.96) |
68.4 | 0.37 (0.14–0.99) |
0.3 (0.11–0.87) |
| Family size | ||||||||||||
| ≤4 | 77.8 | Ref | Ref | 55.6 | Ref | Ref | 71.4 | Ref | Ref | 82.5 | Ref | Ref |
| ≥5 | 73.9 | 0.81 (0.55–1.2) |
__ | 53.3 | 0.91 (0.66–1.3) |
__ | 75.1 | 1.2 (0.84–1.7) |
__ | 85.6 | 1.3 (0.82–1.9) |
__ |
| Parity | ||||||||||||
| Nulliparous | 74.8 | Ref | Ref | 53.6 | Ref | Ref | 74.8 | Ref | Ref | 84.2 | Ref | Ref |
| Multiparous | 74.8 | 1.0 (0.70–1.4) |
__ | 53.9 | 1.0 (0.75–1.4) |
__ | 74.1 | 0.97 (0.68–1.4) |
__ | 85.2 | 1.1 (0.71–1.6) |
__ |
| ANC from facility | ||||||||||||
| No | 74.6 | Ref | Ref | 54.0 | Ref | Ref | 75.6 | Ref | Ref | 85.1 | Ref | Ref |
| Yes | 74.9 | 1.0 (0.75–1.4) |
__ | 53.6 | 0.98 (0.75–1.3) |
__ | 73.2 | 0.89 (0.65–1.2) |
__ | 84.8 | 0.98 (0.67–1.4) |
__ |
| Husband living status | ||||||||||||
| Lives with wife | 73.8 | Ref | Ref | 51.3 | Ref | Ref | 72.0 | Ref | Ref | 83.4 | Ref | Ref |
| Lives in other places within the country or abroad | 76.2 | 1.1 (0.83–1.6) |
__ | 57.3 | 1.3 (0.97–1.7) |
1.4 (1.0–1.8) |
76.2 | 1.2 (0.87–1.6) |
__ | 87.1 | 1.3 (0.92–2.0) |
1.1 (0.75–1.7) |
| Income generating act | ||||||||||||
| No | 74.5 | Ref | Ref | 53.8 | Ref | Ref | 74.2 | Ref | Ref | 84.7 | Ref | Ref |
| Yes | 80.5 | 1.4 (0.64–3.1) |
__ | 53.7 | 0.99 (0.53–1.9) |
__ | 75.6 | 1.1 (0.52–2.2) |
__ | 90.2 | 1.7 (0.59–4.8) |
__ |
| Wealth quintile | ||||||||||||
| Lowest | 73.5 | Ref | Ref | 53.0 | Ref | Ref | 69.1 | Ref | Ref | 79.4 | Ref | Ref |
| Second | 77.1 | 1.2 (0.77–1.9) |
__ | 59.6 | 1.3 (0.88–1.9) |
__ | 82.0 | 2.0 (1.3–3.3) |
2.0 (1.3–3.3) |
86.3 | 1.6 (0.96–2.8) |
1.6 (0.94–2.7) |
| Middle | 75 | 1.1 (0.69–1.7) |
__ | 57.2 | 1.2 (0.80–1.8) |
__ | 70.0 | 1.0 (0.68–1.6) |
1.1 (0.69–1.6) |
83.3 | 1.3 (0.78–2.2) |
1.2 (0.74–2.1) |
| Fourth | 74.7 | 1.1 (0.67–1.7) |
__ | 50.0 | 0.89 (0.59–1.3) |
__ | 76.0 | 1.4 (0.89–2.2) |
1.4 (0.91–2.3) |
89.5 | 2.2 (1.2–4.0) |
2.0 (1.0–3.6) |
| Highest | 73.3 | 0.99 (0.59–1.6) |
__ | 46.6 | 0.77 (0.49–1.2) |
__ | 76.7 | 1.5 (0.88–2.5) | 1.5 (0.89–2.5) |
89.7 | 2.3 (1.1–4.4) |
1.8 (0.89–3.7) |
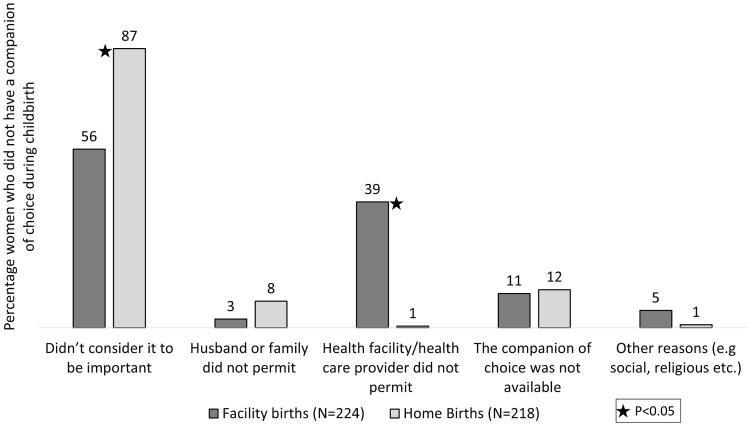
Figure 2 presents the self-reported reasons for not having a birth companion among women who did not have a companion of choice. Around 71% of women without a companion of choice reported that they did not consider having a companion of choice during childbirth to be important. This was significantly higher among women giving birth at home (87%) compared to women giving birth at a facility (56%) (p = .00). Among women giving birth in a health facility who did not have a companion of choice, 39% reported that the health care provider/health facility management did not allow them to have a birth companion. A negligible proportion of women giving birth at home without a companion of choice (less in 1%) reported this as a reason. Around 10% of women reported that their preferred companion of choice was not available at the time of childbirth with no obvious difference between women giving birth in a facility and women giving birth at home (p = .69). Less than 10% of women reported that their husbands or other family members did not allow them to have a birth companion, which also was significantly higher among women giving birth at a home than in a facility (p = .01). Less than 5% of the women reported other reasons for not having a birth companion which was significantly higher among women giving birth in a facility than at a home (p = .007).
Figure 2.
Reasons for not having a birth companion among women who did not have a companion of choice during childbirth (multiple responses considered)
Not considering companion of choice to be important during childbirth was positively associated with multi-parity (OR 3.3, CI 2.2–5.0) and having a family size of five or more members (OR 1.6, CI 1.0–2.6). In contrast, attending ANC at a health facility (OR 0.38, CI 0.24–0.61) and higher wealth status (fourth wealth quintile OR 0.43 CI 0.19–0.85; highest wealth quintile OR 0.30 CI 0.14–0.64; ref. lowest quintile) were negatively associated with not considering a companion of choice to be important.
Discussion
The results of our study indicate that the emotional support that women receive during childbirth is sub-optimal in rural Bangladesh, particularly among women giving birth in a health facility, and that women are more likely to benefit from superior emotional support when they give birth at home.
Having the support of a companion of choice is one of the most salient aspects of ensuring emotional support during childbirth. Birth companions can play a critical role in facilitating non-medical support and assistance to women during the critical period of childbirth, including by providing reassurance and praise, ensuring physical comfort, sharing information on the progression of birth, advocating for the women with medical staff, as well as arranging logistics/instrumental support.18,38,39 Birth companionship has also been identified as a core component of respectful maternity care,16,40 as some studies have found that women are less likely to experience mistreatment and abuse when they are supported by a companion of choice during labour and childbirth.41,42 Birth companionship is also associated with improved health outcomes for women and their newborns, notably, increased likelihood of vaginal birth, thereby reducing unnecessary caesarean section and assisted delivery (i.e. use of forceps or vacuum during vaginal birth), reduced overuse of pain medication, shortened duration of hospital stay and improved satisfaction with care at birth.17,18 While it is true that not all women desire to have a birth companion,43 studies have found that the majority of women prefer to have a companion of choice with them during childbirth.44,45 This is also supported by the findings of our study, as three-quarters of women had a companion of choice while giving birth at home.
Among our study participants, approximately one-third did not benefit from the support of a companion of choice at the time of birth. Women giving birth at home were significantly more likely to have the support of a companion of their choice, with three-quarters reporting having been supported by a companion of their choice, compared to just over half of women giving birth in a health facility. Factors operating at the individual, household/community and health services levels appear to have contributed to the absence of a companion of choice. Among women in our study who did not have a birth companion, the main reason cited was that they did not feel that having a companion of choice was important. This suggests that both women and health care providers should be sensitised as to the potential benefits of having a companion of choice at the time of birth and their right to this support, following which they can make an informed choice as to whether or not they would like to have a companion present with them while labouring and giving birth.
The limitations on women’s decision-making also appear to have played a role in preventing women from having the support of a companion of choice during birth. Among women giving birth at home, approximately 8% of women without a birth companion mentioned that their husband or other family members did not permit them to have a companion of choice. Among those giving birth in a facility without a birth companion, 39% mentioned that the health facility did not allow a companion of choice. This indicates that in both health facilities and homes, lack of women’s autonomy and external support for a companion of choice play an important role in preventing women from having this support even when they desire it. This is a critical consideration for programming and planning.
The high proportion of women reporting that they were not allowed to have a companion of choice when giving birth in a health facility also reflects health services-level barriers to birth companionship. Indeed, health facilities may not be logistically set up to support the presence of birth companions, e.g. birthing rooms are often small and tend to house multiple beds in order to accommodate several women at the same time. As such, not only is space for birth companions an issue, but also the maintenance of confidentiality and privacy. As such, health services providers and managers may be resistant to their presence. Some studies have found resistance from health care providers towards the inclusion of a companion of choice at birth, citing concerns around privacy and lack of trust of companions.44,46 Acceptance among health managers and health care providers could play a determining role in institutionalising the practice of having a companion of choice during childbirth and efforts should be put in place to increase their acceptance so that women and families can be the primary drivers around the decision to have a birth companion in a health facility.
Moreover, health service providers should be trained to include a companion of choice at childbirth, as this may require a different skill set and changes in attitude. Efforts should be made to assist health service providers to understand the benefits of a companion of choice at birth and build their capacity to engage with these companions appropriately and effectively.47 Health workers are often overstretched in their workload and are rarely available to provide continuous support during labour and birth, particularly in low-resource countries. In these contexts, a companion of choice from the woman’s social network can serve not only in providing the emotional support which women need during childbirth but also in reducing the workload of the health care provider.17,48 The advocacy and communication strategy for promoting birth companionship within formal health systems should also highlight this potential benefit to the health workers for wider acceptance.
Women in our study overwhelmingly favoured female family members as their birth companions, in most cases their mothers, followed by mothers-in-law and sisters. Only one-fifth of the women were supported by their husbands as a companion of choice during their most recent birthing experience. The preference towards choosing women as birth companions can be explained by the fact that in Bangladesh, pregnancy and childbirth tend to be regarded primarily as falling within the women’s sphere, thus, resulting in low involvement of husbands in maternal and newborn health.49–51 Other studies conducted on the companion of choice at birth in low-resource settings have generally found a high reliance on female members for this support, with lower support from husbands or male partners for this companionship.39,44
However, involving men in maternal and newborn health care is important and may contribute to facilitating women’s access to and utilisation of skilled health services.52,53 Indeed, WHO recommends implementing interventions to promote the involvement of men in maternal and newborn health.54 Notwithstanding, it is important to understand the preferences of women pertaining to the involvement of their husbands/male partners specifically at the time of birth. Some studies have reported ambiguity in the desire of women to have their husband/male partners present during childbirth, citing reasons such as women’s discomfort with their partners’ presence and the assumption that men cannot effectively support women during this critical moment.39,44 Programmers should be vigilant about taking into account the desires and preferences of women in designing male-involvement initiatives to promote emotional support during childbirth and avoid undermining women’s desires.
Allowing women to eat, drink and be ambulatory during the early stages of labour can contribute to women’s comfort and emotional wellbeing during labour and WHO has included these provisions in their recommendations for the augmentation of labour.12,15,55,56 In our study, there were significant differences in women benefiting from these allowances among those giving birth at home and those giving birth in a health facility. Three-quarters of women were allowed to eat and drink during labour and 85% were permitted to be ambulatory when giving birth at home, compared to 34% and 46% of those giving birth in a health facility, respectively. This suggests that health service providers need better orientation regarding the benefits of these provisions and that health facilities should be better organised in a way which allows women to benefit from these comfort mechanisms.
Moreover, WHO recommends that women be encouraged to give birth in the position of their choice.15 Approximately half of the women giving birth at home in our study reported that the birth attendant asked them which position they preferred to give birth in, and subsequently gave birth in the position of their choice. Such practices were substantially lower among women giving birth in a facility. This is consistent with another study conducted in Ethiopia which found that health service providers rarely encouraged women to give birth in the position in which they felt most comfortable.57 This may be explained by the fact that health service providers may not always be trained to support women in giving birth adopting any other positions than a supine position and may therefore not feel comfortable encouraging women to give birth in a different position. Maternal health programmes and initiatives should sensitise health care providers on the importance of encouraging women to give birth in the position in which they feel most comfortable and develop their skills and capacities to assist women to give birth in non-supine positions.
Overall, women in our study who gave birth at home were significantly more likely to benefit from the key elements of emotional support identified by WHO, i.e. the presence of a companion of choice; the ability to eat and drink and be mobile during the early stages of labour; and being permitted to and giving birth in the position of their choice. This is a particularly important finding in such a setting where over half of births take place at home.29 Births in health facilities have doubled over the past six years in the country, and facility birth is expected to rise in the near future as it has been prioritised in national strategies.24,29 However, sub-optimal emotional support that women experience during facility births can dissuade women from seeking skilled care at the time of birth,30–32 posing a barrier in the promotion of facility birth. Moreover, lack of emotional support during labour and birth can negatively affect the overall quality of maternal and newborn health services in Bangladesh.
In general, there has been a lack of prioritisation of emotional support of women during birth in existing policies, strategies and guidelines of Bangladesh. The most recent versions of Maternal Health Strategy (2017) and Neonatal Health Strategy (2009) of Bangladesh have focused more heavily on the technical and clinical provision of health services around the time of pregnancy, birth and following birth, with less emphasis on the experience of women when accessing these services. They do not provide any clear strategic guidance and a roadmap for the promotion of emotional support during labour and childbirth.24 This should be remedied at the national level in Bangladesh and the emotional support of women should be actively promoted. Considering the global evidence and findings of our study, it is high time for policymakers to prioritise birth companionship as a key intervention within health facilities to promote a positive birth experience and improved health outcomes.
Finally, it is also important to more broadly consider the context surrounding women’s choices and decisions around birth, and how these choices are made. In Bangladesh, as in many similar settings, these decisions are often made in consultation with the woman’s family and close social network. It is therefore important to consider how these negotiations occur in order to facilitate women’s decision-making for obtaining the emotional support which they desire during childbirth. We recommend further research towards these ends.
Limitations
Our study has some limitations which are important to highlight, as well as the strategies which we put in place to try to address them. First and foremost, we acknowledge that a survey is only capable of revealing certain aspects of the phenomena of interest. Future studies should critically look at the components of emotional support during childbirth and may adopt a qualitative approach to explore details regarding relevant practices and preferences. Qualitative, including ethnographic, studies are recommended in order to provide a deeper and richer understanding of the emotional and social experiences of childbirth both at home and facilities, and how these are understood, constructed and shifting in Bangladesh as the country moves further towards a biomedical model of birth.
Furthermore, as with any cross-sectional survey, we cannot draw causality for the associations that we have presented in this article. However, we have tried to adjust for the effects of potential confounders by presenting AORs with multiple regression models. We also acknowledge that ORs always give slightly inflated estimates than relative risks and the results should be interpreted with that in mind. However, we adopted a multiple logistic regression model over the log-binomial model to maintain comparability of our results across similar studies since logistic regression models are more widely used in global health literature. In addition, recall bias is a potential limitation of our study, as the pregnancy outcomes and birthing experience may have influenced women’s reporting of the emotional support. Recall error is also another potential limitation of this study, as we accepted up to 12 months of recall. However, we feel that the data collectors were well trained and had the capacity to clarify different elements of the questionnaire to respondents for their proper understanding and appropriate recall. Moreover, the recall period in our study was 12 months, which is much shorter than the 3–5 years recall period that is accepted by other surveys generating national estimates.29,58,59 Another potential limitation could be social desirability bias, which we tried to address by recruiting data collectors from local communities who are familiar with the local culture, language and norms. Moreover, we rigorously pre-tested the questionnaire to address this bias. Lastly, we were limited by the availability of data to address all the components of emotional support as outlined by WHO.15
Conclusion
The results of our study indicate that the status of emotional support during labour and childbirth is sub-optimal in rural Bangladesh and that women giving birth in their homes are more likely to benefit from emotional support. Ensuring this support and thereby improving the quality of the experience of care within health facilities should be prioritised by the government of Bangladesh both to improve health outcomes of women and newborns and also to promote a more humanised, positive childbirth experience.
Ethical approval and consent to participate
Ethical approval for this study was obtained from the Research Review Committee (RRC) and Ethical Review Committee (ERC) of the International Center for Diarrhoeal Disease Research, Bangladesh (icddr,b) (Protocol number PR-17088). Administrative approval was obtained from the health managers of the Ministry of Health and Family Welfare (MOHFW) at the national and local level prior to data collection.
Written informed consent was obtained from each participant before initiating the interview. They were informed of the scope of the study and the potential use of the data. They were also thoroughly informed of the voluntary nature of their participation, that they would receive no compensation for their participation and that they could rescind their participation at any point without any penalty. They were then given time to reflect prior to signing a written informed consent form, in the case of literate participants, or providing a thumb print and audio-recorded verbal consent for participants with limited literacy.
Confidentiality, privacy and anonymity of participants were carefully maintained throughout data collection, data management and analysis. The questionnaires are kept under lock and key, and all personal identifiers were removed from the dataset before analysis.
Supplementary Material
Acknowledgement
This study was designed by icddr,b with technical support from EdM and in consultation with Ministry of Health, Government of Bangladesh; the authors would like to acknowledge their contribution to this project. They also would like to give a special thanks to all the local health managers and participants from the three sub-districts of Brahmanbaria district and the research team, without their dedication and expertise this study could not have been accomplished.
Authors’ contribution: AER and JEP designed the study, developed the data collection tools, led the data collection process, analysed and interpreted data as the Principal Investigator and Co-Principal Investigator respectively. JEP and AER developed the first draft of the manuscript as joint first authors with equal contributions. SEA provided guidance to JEP and AER in designing the study and developing the manuscript as the senior author. SM and ABS analysed the data and reviewed the manuscript. TM and MRH were involved in the conceptualisation, data analysis and interpretation, and review of the manuscript. All authors read and approved the final draft of the manuscript.
Footnotes
By formal health services we are referring to services delivered through the government health sector, registered private for-profit services and NGO health services delivered in both health facilities and in communities. We have excluded traditional birth attendants and healers operating in communities outside of this formal health system.
Abbreviations
- AOR
adjusted odds ratio
- BDHS
Bangladesh Demographic Health Survey
- BMMS
Bangladesh Maternal Mortality Survey
- CI
confidence interval
- MICS
multiple indicator cluster surveys
- OR
odds ratio
- WHO
World Health Organization
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The datasets will be made available upon a valid request to the corresponding author (Ahmed Ehsanur Rahman, ehsanur@icddrb.org).
ORCID
Abu Bakkar Siddique http://orcid.org/0000-0002-1484-0823
Mohammad Rifat Haider http://orcid.org/0000-0002-0690-8242
References
- 1.Loudon I. Maternal mortality in the past and its relevance to developing countries today. Am J Clin Nutr. 2000;72(1):241S–246S. doi: 10.1093/ajcn/72.1.241S [DOI] [PubMed] [Google Scholar]
- 2.Van Lerberghe W, De Brouwere V.. Of blind alleys and things that have worked: history's lessons on reducing maternal mortality. Safe motherhood strategies: a review of the evidence; 2001.
- 3.Ronsmans C, Graham WJ, group LMSSs Maternal mortality: who, when, where, and why. The Lancet. 2006;368(9542):1189–1200. doi: 10.1016/S0140-6736(06)69380-X [DOI] [PubMed] [Google Scholar]
- 4.Lock M, Nguyen V-K.. An anthropology of biomedicine. Hoboken (NJ): John Wiley & Sons; 2018. [Google Scholar]
- 5.Davis-Floyd R, Pigg SL, Cosminsky S.. Introduction. Daughters of time: the shifting identities of contemporary midwives 2001. [DOI] [PubMed]
- 6.Davis-Floyd R, Cheyney M.. Birth and the big bad wolf: an evolutionary perspective. In: Selin H, Stone PK, editors. Childbirth across cultures: ideas and practices of pregnancy, childbirth and the postpartum. 5. Amherst (MA): Springer; 2009. p. 1–22. [Google Scholar]
- 7.Jordan B. Birth in four Cultures: A crosscultural investigation of childbirth in Yucatan, Holland, Sweden and the United States. Prospect Heights (IL: ): Waveland Press; 1993. [Google Scholar]
- 8.Johanson R, Newburn M, Macfarlane A.. Has the medicalisation of childbirth gone too far? Br Med J. 2002;324(7342):892–895. doi: 10.1136/bmj.324.7342.892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brubaker SJ, Dillaway HE.. Medicalization, natural childbirth and birthing experiences. Sociol Compass. 2009;3(1):31–48. doi: 10.1111/j.1751-9020.2008.00183.x [DOI] [Google Scholar]
- 10.Scott KD, Klaus PH, Klaus MH.. The obstetrical and postpartum benefits of continuous support during childbirth. J Womens Health Gend Based Med. 1999;8(10):1257–1264. doi: 10.1089/jwh.1.1999.8.1257 [DOI] [PubMed] [Google Scholar]
- 11.Van Teijlingen ER. Midwifery and the medicalization of childbirth: comparative perspectives. New York: Nova Publishers; 2004. [Google Scholar]
- 12.World Health Organization WHO recommendations for augmentation of labour. Geneva: World Health Organization; 2014. [PubMed] [Google Scholar]
- 13.World Health Organization WHO recommended interventions for improving maternal and newborn health: integrated management of pregnancy and childbirth. Geneva: World Health Organization; 2007. [Google Scholar]
- 14.World Health Organization WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- 15.World Health Organization Standards for improving quality of maternal and newborn care in health facilities. Geneva: World Health Organization; 2016. [Google Scholar]
- 16.White Ribbon Alliance Respectful maternity care charter: the universal rights of childbearing women. Washington (DC): White Ribbon Alliance; 2011. [Google Scholar]
- 17.Hodnett ED, Gates S, Hofmeyr GJ, et al. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2012;10:CD003766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bohren MA, Hofmeyr GJ, Sakala C, et al. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017;7:CD003766. doi: 10.1002/14651858.CD003766.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ndirima Z, Neuhann F, Beiersmann C.. Listening to their voices: understanding rural women’s perceptions of good delivery care at the Mibilizi district hospital in Rwanda. BMC Womens Health. 2018;18(1):38. doi: 10.1186/s12905-018-0530-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ojelade OA, Titiloye MA, Bohren MA, et al. The communication and emotional support needs to improve women's experience of childbirth care in health facilities in Southwest Nigeria: a qualitative study. Int J Gynecol Obstetr. 2017;139:27–37. doi: 10.1002/ijgo.12380 [DOI] [PubMed] [Google Scholar]
- 21.National Institute of Population Research and Training (NIPORT) International Centre for Diarrhoeal Disease Research bi, b. MEASURE evaluation. Bangladesh Maternal Mortality and Health Care Survey (BMMS) 2016: preliminary report. Dhaka, Bangladesh and Chapel Hill, NC, USA; 2017.
- 22.World Health Organization Strategies toward ending preventable maternal mortality (EPMM). 2015. Geneva: World Health Organization; 2015. [Google Scholar]
- 23.World Health Organization Global strategy for women's, children's and adolescents' health (2016-2030). Geneva: World Health Organization; 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Government of Bangladesh Bangladesh national maternal health strategy 2015-2030. Dhaka: Ministry of Health and Family Welfare (MOH&FW); 2017. p. 1–86. [Google Scholar]
- 25.National Institute of Population Research and Training (NIPORT) Associates for Community and Population Research (ACPR), ICF International. Bangladesh Health Facility Survey 2014. Dhaka, Bangladesh; 2016.
- 26.Chowdhury ME, Roy L, Biswas TK, et al. A needs assessment study for emergency obstetric and newborn care (EmONC) services in 24 districts of Bangladesh: International Centre for Diarrhoeal Disease Research, Dhaka, Bangladesh; 2014.
- 27.Ahmed SM, Hossain MA, RajaChowdhury AM, et al. The health workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable distribution. Hum Resour Health. 2011;9(1):3. doi: 10.1186/1478-4491-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wichaidit W, Alam M-U, Halder AK, et al. Availability and quality of emergency obstetric and newborn care in Bangladesh. Am J Trop Med Hyg. 2016;95(2):298–306. doi: 10.4269/ajtmh.15-0350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Institute of Population Research and Training (NIPORT) International Centre for Diarrhoeal Disease Research B, MEASURE evaluation. Bangladesh Maternal Mortality and Health Care Survey (BMMS) 2016: preliminary report. Dhaka, Bangladesh and Chapel Hill, NC, USA; 2017.
- 30.Nichter M. Global health: why cultural perceptions, social representations, and biopolitics matter. University of Arizona Press; 2008. [Google Scholar]
- 31.Adams V, Miller S, Chertow J, et al. Having a “safe delivery”: conflicting views from Tibet. Health Care Women Int. 2005;26(9):821–851. doi: 10.1080/07399330500230920 [DOI] [PubMed] [Google Scholar]
- 32.Hay MC. Dying mothers: maternal mortality in rural Indonesia. Med Anthropol. 1999;18(3):243–279. doi: 10.1080/01459740.1999.9966157 [DOI] [Google Scholar]
- 33.National Institute of Population Research and Training (NIPORT) Mitra and Associates, ICF International. Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh and Calverton, MD, USA: NIPORT, Mitra and Associates, and ICF International; 2013.
- 34.National Institute of Population Research and Training MEASURE evaluation, University of North Carolina at Chapel Hill, icddr b. Bangladesh Maternal Mortality and Health Care Survey 2010; 2012.
- 35.Vyas S, Kumaranayake L.. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21(6):459–468. doi: 10.1093/heapol/czl029 [DOI] [PubMed] [Google Scholar]
- 36.Wold S, Esbensen K, Geladi P.. Principal component analysis. Chemom Intell Lab Syst. 1987;2(1–3):37–52. doi: 10.1016/0169-7439(87)80084-9 [DOI] [Google Scholar]
- 37.Bursac Z, Gauss CH, Williams DK, et al. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17. doi: 10.1186/1751-0473-3-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Berkman LF, Glass T, Brissette I, et al. From social integration to health: Durkheim in the new millennium☆. Soc Sci Med. 2000;51(6):843–857. doi: 10.1016/S0277-9536(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 39.Kabakian-Khasholian T, Portela A.. Companion of choice at birth: factors affecting implementation. BMC Pregnancy Childbirth. 2017;17(1):265. doi: 10.1186/s12884-017-1447-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shakibazadeh E, Namadian M, Bohren MA, et al. Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. BJOG: Int J Obstetr Gynaecol. 2018;125(8):932–942. doi: 10.1111/1471-0528.15015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diamond-Smith N, Sudhinaraset M, Melo J, et al. The relationship between women's experiences of mistreatment at facilities during childbirth, types of support received and person providing the support in Lucknow, India. Midwifery. 2016;40:114–123. doi: 10.1016/j.midw.2016.06.014 [DOI] [PubMed] [Google Scholar]
- 42.Abuya T, Warren CE, Miller N, et al. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PloS One. 2015;10(4):e0123606. doi: 10.1371/journal.pone.0123606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alexander A, Mustafa A, Emil SA, et al. Social support during delivery in rural central Ghana: a mixed methods study of women's preferences for and against inclusion of a lay companion in the delivery room. J Biosoc Sci. 2014;46(5):669–685. doi: 10.1017/S0021932013000412 [DOI] [PubMed] [Google Scholar]
- 44.Afulani P, Kusi C, Kirumbi L, et al. Companionship during facility-based childbirth: results from a mixed-methods study with recently delivered women and providers in Kenya. BMC Pregnancy Childbirth. 2018;18(1):150. doi: 10.1186/s12884-018-1806-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Downe S, Finlayson K, Oladapo O, et al. What matters to women during childbirth: a systematic qualitative review. PloS One. 2018;13(4):e0194906. doi: 10.1371/journal.pone.0194906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Munabi-Babigumira S, Glenton C, Lewin S, et al. Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low-and middle-income countries: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2017;11:CD011558. doi: 10.1002/14651858.CD011558.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Safer WHODoMP, Organization WH Counselling for maternal and newborn health care: a handbook for building skills. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 48.Rosen P. Supporting women in labor: analysis of different types of caregivers. J Midwifery Women’s Health. 2004;49(1):24–31. [DOI] [PubMed] [Google Scholar]
- 49.Kululanga LI, Sundby J, Malata A, et al. Male involvement in maternity health care in Malawi. Afr J Reprod Health. 2012;16(1):145–157. [PubMed] [Google Scholar]
- 50.Carter M. Husbands and maternal health matters in rural Guatemala: wives’ reports on their spouses’ involvement in pregnancy and birth. Soc Sci Med. 2002;55(3):437–450. doi: 10.1016/S0277-9536(01)00175-7 [DOI] [PubMed] [Google Scholar]
- 51.Iliyasu Z, Abubakar IS, Galadanci HS, et al. Birth preparedness, complication readiness and fathers’ participation in maternity care in a northern Nigerian community. Afr J Reprod Health. 2010;14(1):21–32. [PubMed] [Google Scholar]
- 52.Rahman AE, Perkins J, Islam S, et al. Knowledge and involvement of husbands in maternal and newborn health in rural Bangladesh. BMC Pregnancy Childbirth. 2018;18(1):247. doi: 10.1186/s12884-018-1882-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holmes W, Davis J, Luchters S.. Engaging men in reproductive, maternal and newborn health. Melbourne: Center for international health, Burnet Institute; 2013. [Google Scholar]
- 54.World Health Organization WHO recommendations on health promotion interventions for maternal and newborn health 2015. Geneva: World Health Organization; 2015. [PubMed] [Google Scholar]
- 55.Singata M, Tranmer J, Gyte GM.. Restricting oral fluid and food intake during labour. Cochrane Database Syst Rev. 2010;1:CD003930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.O'sullivan G, Liu B, Shennan AH.. Oral intake during labor. Int Anesthesiol Clin. 2007;45(1):133–147. doi: 10.1097/AIA.0b013e31802b8dea [DOI] [PubMed] [Google Scholar]
- 57.Sheferaw ED, Bazant E, Gibson H, et al. Respectful maternity care in Ethiopian public health facilities. Reprod Health. 2017;14(1):60. doi: 10.1186/s12978-017-0323-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.MEASURE Evaluation, ICF International Guide to DHS statistics: demographic and health survey methodology. Calverton (MD): ORC Macro; 2006. [Google Scholar]
- 59.National Institute of Population Research and Training (NIPORT) Mitra and Associates, ICF International. Bangladesh Demographic and Health Survey 2014. Dhaka, Bangladesh and Calverton, MD, USA; 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets will be made available upon a valid request to the corresponding author (Ahmed Ehsanur Rahman, ehsanur@icddrb.org).