Abstract
The socio-economic implications of COVID-19 are devastating. Considerable morbidity is attributed to ‘long-COVID’ – an increasingly recognized complication of infection. Its diverse symptoms are reminiscent of vitamin B12 deficiency, a condition in which methylation status is compromised.
We suggest why SARS-CoV-2 infection likely leads to increased methyl-group requirements and other disturbances of one-carbon metabolism. We propose these might explain the varied symptoms of long-COVID. Our suggested mechanism might also apply to similar conditions such as myalgic encephalomyelitis/chronic fatigue syndrome.
The hypothesis is evaluable by detailed determination of vitamin B12 and folate status, including serum formate as well as homocysteine and methylmalonic acid, and correlation with viral and host RNA methylation and symptomatology. If confirmed, methyl-group support should prove beneficial in such individuals.
Keywords: Coronavirus, COVID-19, Vitamin B12, Folic acid, N6-methyladenosine (m6A), Serine, Formate
Background
A novel form of coronavirus, “severe acute respiratory syndrome coronavirus 2” (SARS-CoV-2) was reported in Wuhan in 2019 [1]. The COVID-19 outbreak caused by SARS-CoV-2 was declared a pandemic in March 2020.
Long Covid
“Long Covid” is a recognized yet unexplained complication of COVID-19 [2]. Symptoms are diverse and can last for months following resolution of initial infection [3]. They include fatigue, ‘brain fog’, myalgia, headache, dizziness, breathlessness, palpitations, anosmia and gastrointestinal problems [3], [4], [5].
There is a remarkable overlap with symptoms described by patients with pernicious anaemia (PA), especially those who suffered significant delay between presentation and diagnosis [6] (See Table 1 ). PA is an autoimmune disease caused by deficient synthesis of gastric intrinsic factor and subsequent malabsorption of vitamin B12. Moreover, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is also a B12-responsive syndrome [7]. It is often initiated by infection and probably elicits autoimmunity at some stage [8]. Clinical experience of these syndromes led us to consider whether a ‘common denominator’ exists between vitamin B12 status and SARS-CoV-2 infection and its aftermath ‘Long-Covid’.
Table 1.
Comparative frequency of symptoms reported by patients with PA (n = 889) [6] and 6 months post-hospitalisation with COVID 19 (n = 165) [5].
| Neurological Symptoms | Pernicious Anaemia | “Long COVID” |
|---|---|---|
| Fatigue | 87% | 34% |
| Memory complaints | 78% | 31% |
| Sleep Disturbance | 87% | 26% |
| Numbness/tingling | 66% | 18% |
| Myalgia | Not documented | 30% |
| Confusion | 62% | 13% |
| Dizziness | 59% | 12% |
| Headaches | 52% | 10% |
| Depression | 45% | 26% |
| Gait disturbance | 34% | 11% |
| Hyposmia | 26% | 16% |
| Urinary dysfunction/UTI | 21% | 14% |
One-carbon metabolism
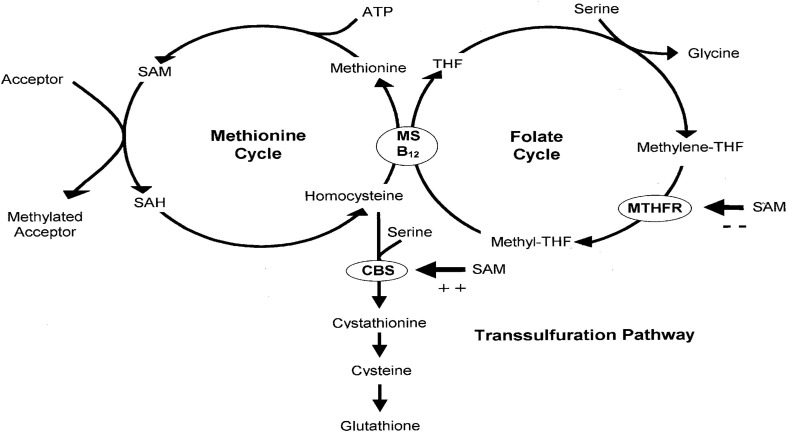
Our hypothesis concerns SARS-CoV-2-induced changes in the host’s one-carbon metabolism and methyl-group availability. Of central importance is the B12-dependent methionine synthase (MS) reaction (See Fig. 1 ).
Fig. 1.
One-carbon metabolism.
Briefly, adenosylation of methionine by the enzyme methionine adenosyltransferase generates S-adenosylmethionine (SAM) - a universal methyl-donor supplying methyl groups for a multitude of intracellular processes [9]. SAM is converted to S-adenosylhomocysteine (SAH) following transfer of its methyl-group by SAM-dependent methyltransferases, and thence to homocysteine by SAH hydrolase. The ‘methionine cycle’ is completed by conversion of homocysteine back to methionine by MS (Fig. 1).
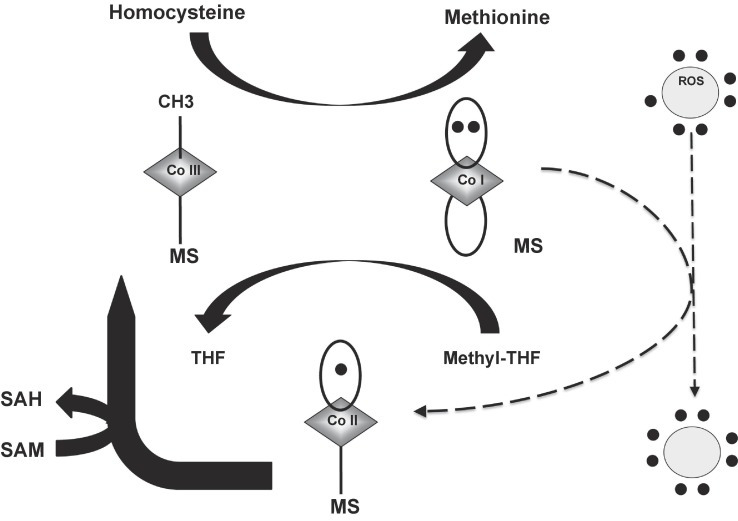
Fig. 2 magnifies the MS reaction: MS-bound methyl-B12 transfers its methyl group to homocysteine to generate methionine and a transient free cob(I)alamin intermediate. MS-bound methyl-B12 is regenerated when cob(I)alamin accepts a methyl group from methyl-tetrahydrofolate (methyl-THF), generating free tetrahydrofolate (THF) in the process.
Fig. 2.
In the primary turnover cycle of the MS reaction, homocysteine reacts with the methyl (CH3) group of MS-bound methylcobalamin to produce methionine and an unstable intermediate form of vitamin B12, cob(I)alamin (upper bold arrow). This highly reactive species then reacts with methyl-tetrahydrofolate (methyl-THF) to generate free THF and regenerate MS-bound methylcobalamin (lower bold arrow). Cobalamin therefore shuttles between methylcobalamin and cob(I)alamin states. Cob(I) alamin is occasionally de-activated by reactive oxygen species (ROS) and oxidised to cob(II)alamin (dashed arrows). The return of cob(II)alamin to the primary turnover cycle requires a re-activation step in which SAM provides the methyl group (lateral bold arrows). De-activation and re-activation usually occur every few thousand cycles. We suggest this process is significantly augmented with SARS-CoV-2 infection.
N6-methyladenosine (m6A)
Widespread mRNA methylation occurs at the N6 position of adenosine (N6-methyladenosine), abbreviated as m6A. Such post-transcriptional methylation of adenosine was first described in the 1970′s and is now considered a natural epigenetic phenomenon [10], [11]. It is critical for various physiological and pathological processes including transcription, translation and decay of mRNA [12], [13]. It is probably applicable to all RNA viral infections and even several DNA viruses [14], [15].
Three types of protein determine the prevalence and distribution of m6A. Methyl groups are added by methyltransferases (writers) but removed by demethylases (erasers). M6A modification of mRNA exerts its function by interaction with m6A binding proteins (readers). A myriad of m6A readers exist, suggesting that m6A has evolved to permit widespread regulatory control of gene expression.
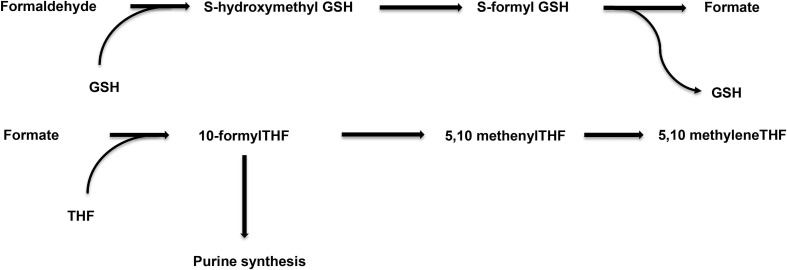
In mammalian cells, m6A-related methyltransferases predominantly comprise a complex of methyltransferase-like protein 3 (METTL3) and 14 (METTL14) [16], [17]. The main demethylase is fat mass and obesity-associated protein (FTO) [18]. Importantly, FTO sequentially oxidises m6A to adenosine via N6-hydroxymethyladenosine and N6-formyladenosine intermediates, releasing the one-carbon unit as formaldehyde and formate [19]. In the cytosol formaldehyde is metabolized to formate in a glutathione (GSH) dependent process via hydroxymethyl-GSH and formyl-GSH (Fig. 3 ).
Fig. 3.
GSH-dependent metabolism of formaldehyde, and the intracellular fate of formate.
Formate has several intracellular fates - direct export as CO2 or formate itself, substrate provision for purine synthesis, or regeneration of a methyl-group via synthesis of methionine and SAM. Cellular recycling is dependent on free THF, and additionally B12 in the case of SAM synthesis (Fig. 1, Fig. 3).
The reversibility of mRNA methylation by demethylases suggests it is a dynamic process affording additional regulatory control beyond that determined simply by the primary sequence or secondary structure of mRNA [20].
Although m6A is the most prevalent mRNA methyl-modification, methyl groups are also required for 5-methylcytidine, N4-acetylcytidine and 2′O-methylation of the ribose moiety of all four ribonucleosides [11].
SARS-CoV-2 genome
The genome of SARS-CoV-2 is roughly 30 kB long. It possesses genes that code for structural proteins, namely spike, envelope, membrane and nucleocapsid [21]. At the 5′ end of the genome is a gene known as orf1ab that encodes for polyprotein bearing all the non-structural proteins (nsp) [22]. The polyprotein arising from orf1ab may undergo proteolytic processing to give rise to 16 proteins namely nsp’s 1–16 [23]. For example, the nsp12 protein houses the RNA-dependent RNA polymerases (RdRp) that are responsible for duplication of the genome, N7-methyltransferase activities are present in the nsp14 protein, and the nsp16 protein has SAM dependent O-methyltransferase activity [22].
The hypothesis
We suggest there are several implications of SARS-CoV-2 infection regarding both the supply of, and demand for, SAM.
-
1.
COVID-19 is associated with a ‘cytokine storm’ and significant oxidative stress [24]. This has important implications for the MS reaction.
Cob(I)alamin is vulnerable to oxidation by free radicals. MS inactivation occurs when free radicals oxidise cob(I)alamin to a cob(II)alamin species. Re-activation requires methyl group donation by SAM [25] (Fig. 2). The net effect is SAM depletion (and an increase in homocysteine levels) as a consequence of oxidative stress [26]. De-activation and re-activation usually occur every few thousand cycles. We suggest this process is augmented with SARS-CoV-2 infection. Indeed, it is likely also applicable to other conditions associated with a cytokine storm, such as influenza.
-
2.
Viral replication places significant demands on methyl-groups, and one-carbon availability in general.
SARS-CoV-2 nsp’s 14 and 16 have methyltransferase function and play key roles in the m7G cap and 2′-O-methylation modification (see below). However, most RNA viruses that replicate in the cytoplasm do not encode any enzymes with m6A methyltransferase activity and therefore hijack the host m6A machinery to modify the RNA.
A recent study on SARS-Cov-2 infected Vero-E6 cells (from monkey kidney) concluded that the host m6A machinery interacts with viral key proteins to facilitate the replication of SARS-CoV-2. Firstly, the hijacked METTL3 functions as a methyltransferase, adding the m6A modification to viral RNA. Secondly, METTL3 interacts with viral RdRp, which boosts the expression of METTL3 (through an unknown mechanism). In summary, the host m6A modification complex interacts with viral proteins to modulate SARS-CoV-2 replication [27].
Generally speaking, m6A modification of host mRNAs can either enhance viral infections or promote host resistance. For example, m6A modification is documented in another member of the coronavirus family - porcine epidemic diarrhoea virus (PEDV) [13]. PEDV infection triggers an increase in the m6A ratio in host RNA, suggesting that hosts may try to restrict viral replication by m6A modification [13]. We suggest this defensive response might be compromised in individuals with low pre-morbid methyl reserves, resulting in a lower m6A/A ratio in patients with long-COVID.
SAM is also required for methyl groups for viral RNA capping [28]. Coronaviruses replicate in the cytoplasm and cannot access the host’s nuclear capping machinery; they have evolved their own capping and methylation apparatus – nsp’s 14 and 16 [28], [29]. In the case of SARS-CoV-2, SAM provides the two methyl-groups required for m7G cap formation [30].
As mentioned in the ‘background information’, the virus nsp12 protein houses the RdRp activity responsible for replication of the viral genome. The nsp12 protein is thus a target to find molecules which can inhibit RdRp activity and thus reduce viral titers and limit disease severity. A computational model of SARS-CoV-2 nsp12 was used to carry out in silico screening to identify such potential inhibitors [31]. Interestingly, methylcobalamin proved to be the best matching molecule, i.e., the best overlap was found between the binding sites of the natural substrates of nsp12 and methylcobalamin. Methylcobalamin (methylated vitamin B12) may thus be a potential inhibitor of nsp12 and prevent RNA synthesis necessary for viral genome replication. This is, of course, supportive to our hypothesis but requires in vivo confirmation.
-
3.
SARS-Cov-2 disrupts co-ordination between remethylation and transsulfuration through SAM
SAM is an inhibitor of 5,10-methyleneTHF reductase (MTHFR) but an activator of cystathionine beta synthase (CBS) (Fig. 1). This affords a mechanism by which re-methylation and transsulfuration are co-ordinated [32], [33] (Fig. 1). However, disruption of co-ordination by SARS-CoV-2-induced increased methylation demands will lead to falling intracellular SAM concentration, reduced CBS activity and diversion of homocysteine away from synthesis of reduced GSH – a key intracellular antioxidant. Thus, MTHFR activity and methylation via folate/B12 and MS will be given priority before transsulfuration and GSH synthesis in the scenario of SARS-Cov-2 replication.
In summary, we suggest that SARS-CoV-2 significantly stresses the host’s one-carbon metabolism. It simultaneously increases demand but impairs supply of methyl-groups.
Biochemical implications of clinical importance
There are several biochemical implications of our hypothesis for the host. These include serine depletion, elevated homocysteine and GSH depletion. It is possible each makes a distinct contribution to the various symptoms of long-COVID. An individual’s ‘baseline’ metabolic and dietary status might predict their influence on specific symptoms. With this in mind, each predicted biochemical consequence, and its associated clinical sequelae, is considered separately below.
Serine
The increased demand for singe-carbon units following SARS-CoV-2 infection should be reflected in declining serine levels, the ultimate supplier of one-carbon units for 5-methylTHF (Fig. 1).
The kidney plays an important role in serine metabolism. It removes glycine from the circulation and converts it to serine, which is then released into the renal vein. The kidney produces about 4 g of serine per day, approximately equivalent to a typical Western diet [34]. Renal serine production falls in patients with chronic renal disease and is reflected in a decreased plasma serine concentration [35]. Patients with underlying kidney problems, and renal transplant patients, are vulnerable to developing COVID-19, and there is involvement of kidney function in this viral infection [36].
Given the role of L-serine in myelin synthesis others suggest that some patients with peripheral neuropathy have mild serine deficiency [37], [38]. Serine depletion might contribute to the “pins and needles” (paraesthesia) often described by patients with long-COVID. This is also a common, yet unexplained, symptom of PA.
Additional metabolic demands for serine also occur as a consequence of a SARS-CoV-2-induced T-cell response. Reducing serum serine and glycine levels through dietary intervention dramatically reduces pathogen-driven T-cell expansion, indicating a key requirement for these amino acids in this response [39].
Homocysteine
Our hypothesis implies an elevated homocysteine concentration in patients with long-COVID. As a ‘post-viral fatigue syndrome’, long-COVID also resembles ME/CFS, a suspected consequence of various viral infections [8], [40]. ME/CFS has no definitive laboratory hallmarks but evolution of its diagnosis over decades has increased its recognition as a serious and crippling disorder. A metabolomic study of ME/CFS suggests it is a hypometabolic syndrome [41]. Although blood homocysteine levels are not consistently elevated, patients with ME/CFS have very markedly raised homocysteine in cerebrospinal fluid (CSF), with no overlap compared with control subjects [42]. Moreover, CSF homocysteine levels significantly correlate with objective ratings of ‘fatigue’ [42].
Elevated homocysteine in blood is common in patients with cognitive impairment and dementia, including Alzheimer's Disease (AD) [43]; the association fulfils Bradford-Hill’s criteria suggesting causality [44]. Lowering homocysteine with high dose B vitamins effectively slows cognitive decline and brain atrophy [45], and such treatment is currently the most promising intervention for AD prevention [46]. We suggest that elevated homocysteine contributes to the ‘brain-fog’ described by long-COVID patients. There is also some evidence for cognitive deficit in post COVID-19 patients relative to controls [47].
Thromboembolism is an important part of the pathogenesis of SARS-CoV-2 infection [48]. Although not related to long-COVID itself, an increased tendency for hypercoagulability and thromboembolism is predicted by our hypothesised elevation of serum homocysteine [49].
Glutathione
As discussed previously, GSH is required for cytosolic formaldehyde metabolism (Fig. 3). It is also required for intracellular processing of B12 [50]. However, reduced metabolic flux through the transsulfuration pathway due to effects of falling SAM levels on CBS activity predicts a decline in GSH (and change in GSH/GSSG ratio) in patients with long-COVID.
Besides being efficient antioxidants, GSH and/or its precursor N-acetylcysteine have useful antiviral activity toward a wide range of viruses, such as influenza, dengue, herpes simplex, rotavirus, and PEDV [51].
A recent Russian case report described four females with confirmed COVID-19, two with mild disease and a normal GSH/GSSG ratio. The others, with a more severe form of COVID-19, had a low GSH/GSSG ratio, “clearly indicating GSH deficiency and oxidative stress”. One remained severely ill at time of publication, GSH treatment being reportedly unavailable [52]. In a case report from USA, two patients with shortness of breath due to COVID-19 pneumonia were treated with GSH and showed a dramatic and rapid response within hours [53].
Suggestions for research
Determination should be made of the predicted metabolic effects in patients with long-COVID. These include measurement of serum serine and evaluation of markers of ‘oxidative stress,’ including the GSH/GSSG ratio. Our hypothesis also predicts changes in indices of vitamin B12 and folate status. Regarding B12, its reliable evaluation is the subject of debate, but its key indicators are determination of total serum B12, holo-transcobalamin (holoTC), and the two metabolic markers methylmalonic acid and homocysteine [54]. The latter is also elevated in folate deficiency; determination of plasma formate may help to distinguish the two [55], [56].
There may also be evidence of inactive B12 ‘analogues’ in these patients, which may represent endogenous inactive oxidation products [57], [58].
If available, one could also consider determination of the SAM/SAH ratio which should be demonstrably altered in these patients [59].
Implications for treatment
If confirmed, treatment should address restoration of methyl-group supply, reasonably tailored to an individual’s specific requirements. Replacement of vitamin B12 and folate in combination with glutathione or a precursor, and possibly serine, would likely form the mainstay of therapy. Interestingly, a recent study of ten European countries showed that suboptimal B12 consumption correlates with increased COVID-19 incidence and mortality [60].
Attention should also be given to general diet, including daily methionine intake. Avoidance of other nutrient deficiencies and effective nutrition policies may help strengthen population resilience to COVID-19 itself [61], [62]. For example, 17 patients hospitalized for COVID-19 who received daily vitamin D (1,000 IU) magnesium (150 mg) and vitamin B12 (500mcg) had a significantly improved clinical course compared to 26 non-supplemented patients [63].
There are precedents for this approach. One study suggested ME/CFS is a hypometabolic syndrome that could “..theoretically be supported by interventions directed at folate, B12, glycine, and serine pools, and B6 metabolism” [41], and there are reports of good responses to treatment with high-dose B12 – subcutaneous and frequent injections - and folic acid in such patients [7].
It is also necessary to address chronic ‘oxidative stress’ in long-COVID patients. N-acetylcysteine is a precursor to glutathione and has the additional benefit of lowering homocysteine levels [64].
Conclusion
We suggest that SARS-CoV-2 induces an increased demand for methyl-groups whilst simultaneously impairing their supply due to viral-induced oxidative stress.
The biochemical implications of our hypothesis might explain the diverse symptoms experienced by patients with long-COVID and, if confirmed, suggests possible approaches to treatment.
It would be ironic if the socio-economic devastation of COVID-19, by intensifying world-wide research in a viral pandemic, leads to valuable insights into other conditions such as ME/CFS, as well as providing additional clues to the aetiology of memory disorders and dementia, including Alzheimer’s disease.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Ciotti M., Angeletti S., Minieri M., Giovannetti M., Benvenuto D., Pascarella S., et al. COVID-19 outbreak: an overview. Chemotherapy. 2020;64(5-6):215–223. doi: 10.1159/000507423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baig A.M. Chronic COVID syndrome: need for an appropriate medical terminology for Long-COVID and COVID Long-Haulers. J Med Virol. 2020 doi: 10.1002/jmv.26624. [DOI] [PubMed] [Google Scholar]
- 3.Morley J.E. Editorial: COVID-19 – the long road to recovery. J Nutr Health Aging. 2020;24(9):917–919. doi: 10.1007/s12603-020-1497-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marshall M. The lasting misery of coronavirus long-haulers. Nature. 2020;585(7825):339–341. doi: 10.1038/d41586-020-02598-6. [DOI] [PubMed] [Google Scholar]
- 5.Pilotto A., Cristillo V., Piccinelli S.C., Zoppi N., Bonzi G., Sattin D., et al. COVID-19 severity impacts on long-term neurological manifestation after hospitalisation. medRxiv. 2021 2020.12.27.20248903. [Google Scholar]
- 6.Hooper M., Hudson P., Porter F., McCaddon A. Patient journeys: diagnosis and treatment of pernicious anaemia. Br J Nurs. 2014;23(7):376–381. doi: 10.12968/bjon.2014.23.7.376. [DOI] [PubMed] [Google Scholar]
- 7.Regland B., Forsmark S., Halaouate L., Matousek M., Peilot B., Zachrisson O., et al. Response to vitamin B12 and folic acid in myalgic encephalomyelitis and fibromyalgia. PLoS ONE. 2015;10(4):e0124648. doi: 10.1371/journal.pone.0124648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blomberg J., Gottfries C.G., Elfaitouri A., Rizwan M., Rosen A. Infection elicited autoimmunity and myalgic encephalomyelitis/chronic fatigue syndrome: an explanatory model. Front Immunol. 2018;9:229. doi: 10.3389/fimmu.2018.00229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Selhub J. Folate, vitamin B12 and vitamin B6 and one carbon metabolism. J Nutr Health Aging. 2002;6(1):39–42. [PubMed] [Google Scholar]
- 10.Desrosiers R., Friderici K., Rottman F. Identification of methylated nucleosides in messenger RNA from Novikoff hepatoma cells. Proc Natl Acad Sci USA. 1974;71(10):3971–3975. doi: 10.1073/pnas.71.10.3971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsai K., Cullen B.R. Epigenetic and epitranscriptomic regulation of viral replication. Nat Rev Microbiol. 2020;18(10):559–570. doi: 10.1038/s41579-020-0382-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao B.S., Roundtree I.A., He C. Post-transcriptional gene regulation by mRNA modifications. Nat Rev Mol Cell Biol. 2017;18(1):31–42. doi: 10.1038/nrm.2016.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen J., Jin L.i., Wang Z., Wang L., Chen Q., Cui Y., et al. N6-methyladenosine regulates PEDV replication and host gene expression. Virology. 2020;548:59–72. doi: 10.1016/j.virol.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams G.D., Gokhale N.S., Horner S.M. Regulation of Viral Infection by the RNA Modification N6-Methyladenosine. Annu Rev Virol. 2019;6(1):235–253. doi: 10.1146/annurev-virology-092818-015559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manners O., Baquero-Perez B., Whitehouse A. m(6)A: Widespread regulatory control in virus replication. Biochim Biophys Acta, Gene Regul Mech. 2019;1862(3):370–381. doi: 10.1016/j.bbagrm.2018.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bokar J.A., Rath-Shambaugh M.E., Ludwiczak R., Narayan P., Rottman F. Characterization and partial purification of mRNA N6-adenosine methyltransferase from HeLa cell nuclei. Internal mRNA methylation requires a multisubunit complex. J Biol Chem. 1994;269(26):17697–17704. [PubMed] [Google Scholar]
- 17.Liu J., Yue Y., Han D., Wang X., Fu Y.e., Zhang L., et al. A METTL3-METTL14 complex mediates mammalian nuclear RNA N6-adenosine methylation. Nat Chem Biol. 2014;10(2):93–95. doi: 10.1038/nchembio.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jia G., Fu Y.e., Zhao X.u., Dai Q., Zheng G., Yang Y., et al. N6-methyladenosine in nuclear RNA is a major substrate of the obesity-associated FTO. Nat Chem Biol. 2011;7(12):885–887. doi: 10.1038/nchembio.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fu Y.e., Jia G., Pang X., Wang R.N., Wang X., Li C.J., et al. FTO-mediated formation of N6-hydroxymethyladenosine and N6-formyladenosine in mammalian RNA. Nat Commun. 2013;4(1) doi: 10.1038/ncomms2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roundtree I.A., Evans M.E., Pan T., He C. Dynamic RNA modifications in gene expression regulation. Cell. 2017;169(7):1187–1200. doi: 10.1016/j.cell.2017.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shang W., Yang Y., Rao Y., Rao X. The outbreak of SARS-CoV-2 pneumonia calls for viral vaccines. npj Vaccines. 2020;5:18. doi: 10.1038/s41541-020-0170-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu F., Zhao S.u., Yu B., Chen Y.-M., Wang W., Song Z.-G., et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Graham R.L., Sparks J.S., Eckerle L.D., Sims A.C., Denison M.R. SARS coronavirus replicase proteins in pathogenesis. Virus Res. 2008;133(1):88–100. doi: 10.1016/j.virusres.2007.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Delgado-Roche L., Mesta F. Oxidative Stress as Key Player in Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) Infection. Arch Med Res. 2020;51(5):384–387. doi: 10.1016/j.arcmed.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Banerjee R.V., Matthews R.G. Cobalamin-dependent methionine synthase. FASEB J. 1990;4(5):1450–1459. doi: 10.1096/fasebj.4.5.2407589. [DOI] [PubMed] [Google Scholar]
- 26.McCaddon A., Regland B., Hudson P., Davies G. Functional vitamin B(12) deficiency and Alzheimer disease. Neurology. 2002;58(9):1395–1399. doi: 10.1212/wnl.58.9.1395. [DOI] [PubMed] [Google Scholar]
- 27.Zhang X., Hao H., Ma L., Zhang Y., Hu X., Chen Z., et al. Methyltransferase-like 3 modulates severe acute respiratory syndrome coronavirus-2 RNA N6-methyladenosine modification and replication. bioRxiv. 2020 doi: 10.1128/mBio.01067-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maranon D.G., Anderson J.R., Maranon A.G., Wilusz J. The interface between coronaviruses and host cell RNA biology: novel potential insights for future therapeutic intervention. Wiley Interdiscip Rev RNA. 2020;11(5) doi: 10.1002/wrna.1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Y.u., Guo D. Molecular mechanisms of coronavirus RNA capping and methylation. Virol Sin. 2016;31(1):3–11. doi: 10.1007/s12250-016-3726-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Romano M., Ruggiero A., Squeglia F., Maga G., Berisio R. A structural view of SARS-CoV-2 RNA replication machinery RNA synthesis, proofreading and final capping. Cells. 2020;9(5):1267. doi: 10.3390/cells9051267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Narayanan N., Nair D.T. Vitamin B12 may inhibit RNA-dependent-RNA polymerase activity of nsp12 from the SARS-CoV-2 virus. IUBMB Life. 2020;72(10):2112–2120. doi: 10.1002/iub.2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Selhub J., Miller J.W. The pathogenesis of homocysteinemia: interruption of the coordinate regulation by S-adenosylmethionine of the remethylation and transsulfuration of homocysteine. Am J Clin Nutr. 1992;55(1):131–138. doi: 10.1093/ajcn/55.1.131. [DOI] [PubMed] [Google Scholar]
- 33.Jhee K.H., Kruger W.D. The role of cystathionine beta-synthase in homocysteine metabolism. AntioxidRedoxSignal. 2005;7(5–6):813–822. doi: 10.1089/ars.2005.7.813. [DOI] [PubMed] [Google Scholar]
- 34.Brosnan J.T. The 1986 Borden award lecture. The role of the kidney in amino acid metabolism and nutrition. Can J Physiol Pharmacol. 1987;65(12):2355–2362. doi: 10.1139/y87-373. [DOI] [PubMed] [Google Scholar]
- 35.Tizianello A., De Ferrari G., Garibotto G., Gurreri G., Robaudo C. Renal metabolism of amino acids and ammonia in subjects with normal renal function and in patients with chronic renal insufficiency. J Clin Invest. 1980;65(5):1162–1173. doi: 10.1172/JCI109771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adapa S., Chenna A., Balla M., Merugu G.P., Koduri N.M., Daggubati S.R., et al. COVID-19 pandemic causing acute kidney injury and impact on patients with chronic kidney disease and renal transplantation. J Clin Med Res. 2020;12(6):352–361. doi: 10.14740/jocmr4200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Koning T.J. Amino acid synthesis deficiencies. J Inherit Metab Dis. 2017;40(4):609–620. doi: 10.1007/s10545-017-0063-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gantner M.L., Eade K., Wallace M., Handzlik M.K., Fallon R., Trombley J., et al. Serine and lipid metabolism in macular disease and peripheral neuropathy. N Engl J Med. 2019;381(15):1422–1433. doi: 10.1056/NEJMoa1815111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ma E.H., Bantug G., Griss T., Condotta S., Johnson R.M., Samborska B., et al. Serine is an essential metabolite for effector T cell expansion. Cell Metab. 2017;25(2):345–357. doi: 10.1016/j.cmet.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 40.Cortes Rivera M., Mastronardi C., Silva-Aldana C., Arcos-Burgos M., Lidbury B. Myalgic encephalomyelitis/chronic fatigue syndrome: a comprehensive review. Diagnostics (Basel) 2019;9(3):91. doi: 10.3390/diagnostics9030091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Naviaux R.K., Naviaux J.C., Li K., Bright A.T., Alaynick W.A., Wang L., et al. Metabolic features of chronic fatigue syndrome. Proc Natl Acad Sci USA. 2016;113(37):E5472–E5480. doi: 10.1073/pnas.1607571113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Regland B., Andersson M., Abrahamsson L., Bagby J., Dyrehag L.E., Gottfries C.G. Increased concentrations of homocysteine in the cerebrospinal fluid in patients with fibromyalgia and chronic fatigue syndrome. Scand J Rheumatol. 1997;26(4):301–307. doi: 10.3109/03009749709105320. [DOI] [PubMed] [Google Scholar]
- 43.McCaddon A. Vitamin B12 in neurology and ageing; clinical and genetic aspects. Biochimie. 2013;95(5):1066–1076. doi: 10.1016/j.biochi.2012.11.017. [DOI] [PubMed] [Google Scholar]
- 44.McCaddon A., Miller J.W. Assessing the association between homocysteine and cognition: reflections on Bradford Hill, meta-analyses, and causality. Nutr Rev. 2015;73(10):723–735. doi: 10.1093/nutrit/nuv022. [DOI] [PubMed] [Google Scholar]
- 45.Smith A.D., Refsum H., Bottiglieri T., Fenech M., Hooshmand B., McCaddon A., et al. Homocysteine and dementia: an international consensus statement. J Alzheimers Dis. 2018;62(2):561–570. doi: 10.3233/JAD-171042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yu J.T., Xu W., Tan C.C., Andrieu S. Evidence-based prevention of Alzheimer's disease: systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials. J Neurol Neurosurg Psychiatry. 2020;91:1201–1209. doi: 10.1136/jnnp-2019-321913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hampshire A., Trender W., Chamberlain S.R., Jolly A., Grant J.E., Patrick F., et al. Cognitive deficits in people who have recovered from COVID-19 relative to controls: An N=84,285 online study. medRxiv. 2020 doi: 10.1016/j.eclinm.2021.101044. 2020.10.20.20215863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pillai P., Joseph J.P., Fadzillah N.H.M., Mahmod M. COVID-19 and major organ thromboembolism: manifestations in neurovascular and cardiovascular systems. J Stroke Cerebrovasc Dis. 2021;30(1):105427. doi: 10.1016/j.jstrokecerebrovasdis.2020.105427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Spence J.D. Homocysteine lowering for stroke prevention: unravelling the complexity of the evidence. Int J Stroke. 2016;11(7):744–747. doi: 10.1177/1747493016662038. [DOI] [PubMed] [Google Scholar]
- 50.Kim J., Hannibal L., Gherasim C., Jacobsen D.W., Banerjee R. A human B12 trafficking protein uses glutathione transferase activity for processing alkylcobalamins. J Biol Chem. 2009 doi: 10.1074/jbc.M109.057877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Khanfar A., Al Q.B. Could glutathione depletion be the Trojan horse of COVID-19 mortality? Eur Rev Med Pharmacol Sci. 2020;24(23):12500–12509. doi: 10.26355/eurrev_202012_24046. [DOI] [PubMed] [Google Scholar]
- 52.Polonikov A. Endogenous deficiency of glutathione as the most likely cause of serious manifestations and death in COVID-19 patients. ACS Infect Dis. 2020;6(7):1558–1562. doi: 10.1021/acsinfecdis.0c00288. [DOI] [PubMed] [Google Scholar]
- 53.Horowitz R.I., Freeman P.R., Bruzzese J. Efficacy of glutathione therapy in relieving dyspnea associated with COVID-19 pneumonia: a report of 2 cases. Respir Med Case Rep. 2020;30 doi: 10.1016/j.rmcr.2020.101063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Green R., Allen L.H., Bjørke-Monsen A.-L., Brito A., Guéant J.-L., Miller J.W., et al. Vitamin B12 deficiency. Nat Rev Dis Primers. 2017;3(1) doi: 10.1038/nrdp.2017.40. [DOI] [PubMed] [Google Scholar]
- 55.Lamarre S.G., Morrow G., Macmillan L., Brosnan M.E., Brosnan J.T. Formate: an essential metabolite, a biomarker, or more? Clinical chemistry and laboratory medicine. CCLM/FESCC. 2013;51(3):571–578. doi: 10.1515/cclm-2012-0552. [DOI] [PubMed] [Google Scholar]
- 56.Lamarre S.G., Molloy A.M., Reinke S.N., Sykes B.D., Brosnan M.E., Brosnan J.T. Formate can differentiate between hyperhomocysteinemia due to impaired remethylation and impaired transsulfuration. Am J Physiol Endocrinol Metab. 2012;302(1):E61–E67. doi: 10.1152/ajpendo.00345.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kondo H., Osborne M.L., Kolhouse J.F., Binder M.J., Podell E.R., Utley C.S., et al. Nitrous oxide has multiple deleterious effects on cobalamin metabolism and causes decreases in activities of both mammalian cobalamin-dependent enzymes in rats. J Clin Invest. 1981;67(5):1270–1283. doi: 10.1172/JCI110155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hardlei T.F., Obeid R., Herrmann W., Nexo E., Szecsi P.B. Cobalamin analogues in humans: a study on maternal and cord blood. PLoS ONE. 2013;8(4):e61194. doi: 10.1371/journal.pone.0061194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bottiglieri T. Isocratic high performance liquid chromatographic analysis of S-adenosylmethionine and S-adenosylhomocysteine in animal tissues: the effect of exposure to nitrous oxide. Biomed Chromatogr. 1990;4(6):239–241. doi: 10.1002/bmc.1130040606. [DOI] [PubMed] [Google Scholar]
- 60.Galmés S., Serra F., Palou A. Current state of evidence: influence of nutritional and nutrigenetic factors on immunity in the COVID-19 pandemic framework. Nutrients. 2020;12(9):2738. doi: 10.3390/nu12092738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Im J.H., Je Y.S., Baek J., Chung M.-H., Kwon H.Y., Lee J.-S. Nutritional status of patients with COVID-19. Int J Infect Dis. 2020;100:390–393. doi: 10.1016/j.ijid.2020.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Richardson D.P., Lovegrove J.A. Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective. Br J Nutr. 2021;125(6):678–684. doi: 10.1017/S000711452000330X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tan C.W., Ho L.P., Kalimuddin S., Cherng B.P.Z., Teh Y.E., Thien S.Y., et al. Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B12 in combination on progression to severe outcomes in older patients with coronavirus (COVID-19) Nutrition. 2020;79-80:111017. doi: 10.1016/j.nut.2020.111017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Roes E.M., Raijmakers M.T., Peters W.H., Steegers E.A. Effects of oral N-acetylcysteine on plasma homocysteine and whole blood glutathione levels in healthy, non-pregnant women. Clin Chem Lab Med. 2002;40(5):496–498. doi: 10.1515/CCLM.2002.086. [DOI] [PubMed] [Google Scholar]