Abstract
In Germany, large, population-based cohort studies have been implemented in order to identify risk and protective factors for maintaining health across the life span. The purpose of this systematic review is to analyse findings from three large ongoing cohorts and to identify sex-specific prevalence rates, risk and protective factors for mental health. Published studies from the Cooperative Health Research in the Region Augsburg (KORA), the Study of Health in Pomerania (SHIP) and the Gutenberg Health Study (GHS)), representing the southern, north-eastern and middle parts of Germany, were identified through searches of the databases PubMed and Web of Science. A total of 52 articles was identified from the start of each cohort until June 2019. Articles reporting prevalence rates of mental health [N = 22], explanatory factors for mental health [N = 25], or both [N = 5] were identified. Consistent across cohorts, higher prevalence rates of internalizing disorders were found for women and more externalizing disorders for men. Risk and protective factors for mental health included social factors, lifestyle, physical health, body mass index (BMI), diabetes, genetic and biological factors. In all areas, differences and similarities were found between women and men. The most evident were the sex-specific risk profiles for depression with mostly external risk factors for men and internal risk factors for women. Gender was not assessed directly, therefore we examined whether socioeconomic and family-related factors reflecting gender roles or institutionalized gender could be used as a proxy for gender. Overall, this systematic review shows differences and similarities in prevalence rates and determinants of mental health indicators between women and men. They underline the importance of focussing on sex specific approaches in mental health research and in the development of prevention measures. Current research on mental health still lacks focus on gender aspects. Therefore, an increased focus on sex and gender in mental health research is of great importance.
Keywords: systematic review, mental health, sex, gender, regional differences, Germany
Introduction
Mental disorders have become major public health concerns affecting quality of life, work productivity and life expectancy (1) of a large proportion of the general population. Representative German studies have shown that approximately one in three women and one in four or five men had a diagnosis of a mental disorder in the previous 12 months (2). For most internalizing disorders (e.g., major depression and eating disorders), women are more frequently affected (3, 4), whereas for externalizing disorders (e.g., substance abuse) men are more frequently affected.
Mental health differences between women and men have been attributed to sex and gender differences. Rooted in genetics, anatomy, and physiology (5), sex represents a biological construct. In contrast, gender comprises psychosocial variables that differentiate women and men (6) elucidating societal conditions and offering explanatory models. Gender can be differentiated according to (1) gender roles: behavioral norms attributed to women and men in a given society; (2) gender identity: how people see themselves on the dimensions of femininity-masculinity; (3) gender relations: how individuals interact with or are treated by others based on ascribed or experienced gender; and 4) institutionalized gender: distribution of power between women and men in institutions in society which shapes social norms and justifies different expectations and opportunities for women and men (5). Sex differences in mental health can be explained by sex hormones (7, 8) and dysregulations in the hypothalamic-pituitary-adrenal (HPA) axis (7, 9), especially for stress-related psychiatric disorders. Gender differences in mental health can be explained by e.g., gender-based violence (10), low self-esteem (7) and belonging to a gender minority (11). The interplay between sex and gender is an important factor in mental health. Sex and gender interact in the development of diseases (12, 13) [e.g., depressive disorders (14)] and coping strategies (15). The association between biological sex and mental health in Europe is moderated by socioeconomic and family-related factors (16), which explain about 20% of the differences in mental health between women and men. Such factors are for example employment (16, 17), education, housekeeping or looking after children and income (16, 18). The inverse association between socioeconomic position and morbidity and mortality has been termed social gradient of health (19). While multiple inequalities between women and men (e.g., gender pay gap, lower pension due to maternity leaves and part-time employment) are known, interactions between sex and socioeconomic position, which may put women at a disadvantage have been understudied (19).
Sex and gender differences vary across countries and regions (20). In a study including 48 countries, males have consistently reported higher self-esteem than females, but the strength of this effect differed between countries (21). Furthermore, sex, gender, and cultural differences for self-reported emotional intensity (arousal) were found between the Chinese and German culture (22). However, in a study on the universality of emotions across 37 countries, no differences were found between women and men (23); in all countries men reported more powerful emotions (e.g., anger), whereas women tended to report powerless emotions (e.g., fear or sadness). A study focussing on similarities and differences in three psychological domains (cognitive domain, social and personality and well-being) combined numerous meta-analyses and identified only small differences between women and men (24). These differences remained consistent across countries. Regional differences regarding material living standards and employment conditions may also affect women and men differently (20). In examining mental health, it is therefore important to consider differences between countries and regions.
In Germany, large population-based cohort studies have been implemented in order to identify risk and protective factors for health in the general population. Major ongoing cohorts have been established between 1983 and 2007. These include the Cooperative Health Research in the Region Augsburg (KORA) [formerly Monitoring of Trends and Determinants of Cardiovascular Disease (MONICA)], the Study of Health in Pomerania (SHIP) and the Gutenberg Health Study (GHS), representing different German regions, respectively, the southern, north-eastern and middle part of Germany. KORA focusses on the fields of epidemiology, health economics, and health care research (25), SHIP contains a broad range of health and quality of life indicators (26) and GHS focusses on uncovering risk factors for several conditions, such as cardiovascular and mental diseases (27). The three cohort studies followed representative samples of participants stratified by sex and age, which were drawn in comparable ways from their respective regions (28) (GHS: N = 15 010 respondents, 35–74 years; KORA: N = 18 079 respondents, 25–74 years; SHIP: N = 12 324 respondents, 20–79 years). The three German regions differ regarding socioeconomic and economic parameters: Unemployment rates are highest, discretionary incomes, and life expectancy lowest in Greifswald (SHIP). As the eastern and western states of Germany have evolved in different political and economical systems following the 2nd World War, these regions show pronounced differences regarding full-time employment rates among mothers resulting in different gender pay gaps (28).
These three cohorts also include mental health variables and are therefore particularly suitable to derive knowledge on sex, mental health and their relationships to physical health. The GESA consortium (GEnder Sensitive Analyses of mental health trajectories and implications for prevention) has recently been established to enable future conjoint analyses (28). The purpose of this systematic review is to analyse published findings from the three cohorts and to identify sex-specific prevalence rates of mental disorders and to identify risk and protective factors and regional effects.
Methods
Published studies were identified through searches of the databases PubMed and Web of Science. We included studies from initiation of each cohort until June 2019. KORA started in 1996 (25) following its precursor MONICA which had started in 1984, SHIP started in 1996 (26) and GHS started in 2007 (27). Keyword, title, authors and abstract information were used. The search terms were “KORA,” “Cooperative Health Research in the Augsburg Region,” “SHIP,” “Study of Health in Pomerania,” “GHS” or “Gutenberg Health Study” combined with “mental health,” “sex,” or “gender.” English and German publications were considered. Unpublished papers, abstracts, dissertations and book chapters were not included. The search took place from April until June 2019.
To decide whether an article fulfilled the criteria, the first rough selection was made by inspecting the title and abstract of the article. To identify relevant studies, the following inclusion criteria were used:
1) studies using KORA, SHIP or GHS data;
2) cross-sectional and longitudinal/prospective studies addressing mental health;
3) studies containing sex, respectively gender.
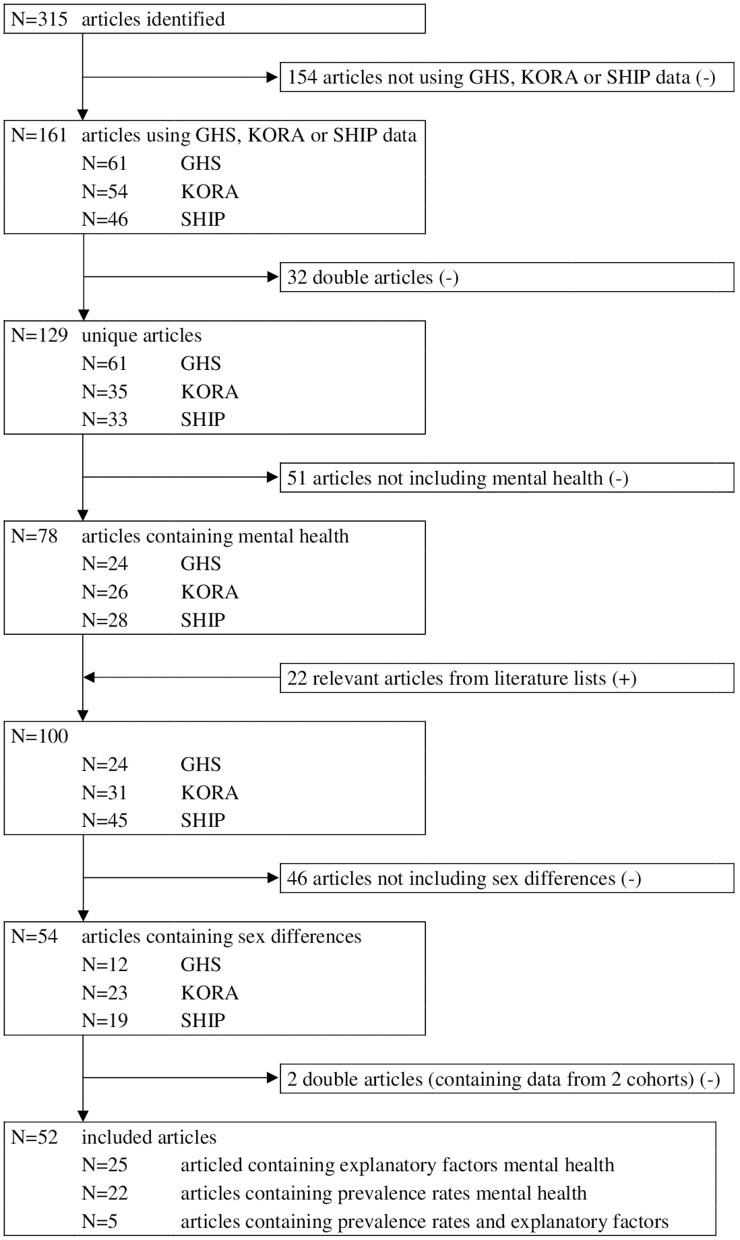
Furthermore, it was required that the articles either (1) contained descriptive statistics on mental health variables including statistical tests that probed for differences between women and men, or (2) tested factors related to mental health with separate analyses for women and men, respectively analyses with an interaction term for sex. We only selected papers that included mental health as a dependent variable. This first group of articles was used to describe prevalence rates of mental health for women and men. The second group of articles was analyzed to describe explanatory factors for mental health between women and men. Of the selected articles the literature list was meticulously examined and further relevant articles were selected. Articles including analyses with mental health as dependent variable, but only including sex as a control factor, were not taken into account. Articles containing descriptive statistics for mental health aspects, but without differences between women and men (statistically tested) were excluded. Lastly, we excluded methodological papers. The selection procedure is displayed in detail in Figure 1.
Figure 1.
Overview of identified, screened and included articles.
Mental health is a broad concept. In this article, we were guided by the definition of WHO including mental, physical and social well-being, not just the absence of mental disorders (29). Similarly, Galderisi et al. (30) interpreted mental health as a dynamic state of well-being changing through lifetime and depending on life events. Therefore, not only mental disorders, but also mental health aspects such as well-being, somatic symptoms, loneliness and resilience were taken into account in this review.
Results
Our search strategy has identified 52 articles reporting GHS, KORA or SHIP data on mental health and sex differences. We found articles reporting prevalence rates of mental health [N = 22], explanatory factors for mental health [N = 25] and articles reporting both [N = 5].
Articles assessing gender differences based on gender identity and gender relations were not found, but some articles included variables indicating gender aspects related to gender roles and institutionalized gender. Previous research indicated gender differences in power, responsibilities and in dimensions of the self (4), contributing e.g., to lower income of women, more responsibilities in childcare and more domestic work. In another previous study a gender index based on secondary data specified taking care of children, being unemployed, working few hours and lower education as indicators for feminine gender roles (31). Such socioeconomic and family-related factors were included as possible gender factors.
Prevalence of Mental Health Complaints
The articles reported a broad range of prevalence rates of mental health indicators for women and men. The articles are consistent in their findings, but most prevalence rates were only reported in one or two of the three cohorts, based on specific diagnostic instruments. The results are listed in Table 1.
Table 1.
Results prevalence rates mental health for women and men.
| References | Study | N | Mental health construct | Measurement scale, cut-off value (range) | Total | Women1 | Men1 | p-value2 |
|---|---|---|---|---|---|---|---|---|
| Grabe et al. (32) | SHIP | 3,300 | Depression | CID-S6: two items, ≥1 (0–2) | 4,310 | 807 (36.8%) | 507 (23.9%) | p < 0.05 |
| Anxiety | CID-S6: five items, ≥1 (0–5) | 4,310 | 1,223 (55.8%) | 823 (38.9%) | p < 0.05 | |||
| Somatization | CID-S6: one item, ≥1 (0–1) | 4,310 | 384 (17.5%) | 308 (14.5%) | p < 0.05 | |||
| Grabe et al. (33) | SHIP | 3,045 | Traumatic event | PTSD module of SCID7, ≥17a | 3,045 | 830 (52.8%) | 833 (56.5%) | p < 0.05 |
| PTSD3 | PTSD module of SCID7, ≥6 (0–17)7b | 1,663 | 43 (5.2%) | 24 (2.9%) | p < 0.05 | |||
| Spitzer et al. (34) | SHIP | 3,171 | PTSD3 | PTSD module of SCID7, ≥1 (0–17)7c | 3,171 | 42 (2.5%) | 20 (1.3%) | p ≤ 0.007 |
| Michal et al. (35) | GHS | 4,912 | Suicidal ideation | Item PHQ-98, ≥1 (0–3) | 4,912 | 223 (9.2%) | 151 (6%) | p < 0.001 |
| Appel et al. (36) | SHIP | 2,157 | Depressive symptoms | BDI-II9, continues (0–63) | 2,157 | 7.0 ± 7.9% | 5.7 ± 6.3 | p < 0.001 |
| MDD4 | M-CIDI10 | 2,157 | 253 (22.3%) | 117 (11.5%) | p < 0.001 | |||
| Michal et al. (37) | GHS | 4,900 | Depersonalization | CDS-211, ≥3 (0–6) | 4,900 | 20 (0.8%) | 21 (0.8%) | p = 0.96 |
| Spitzer et al. (38) | SHIP | 1,772 | Mental health problems | CID-S6, ≥1 (0–12) | 1,772 | 372 (40.9%) | 261 (30.2%) | p ≤ 0.001 |
| Wiltink et al. (39) | GHS | 5,000 | Mental distress5 | PHQ-98, ≥10 (0–27); PHQ panic module12, ≥2 (0–4); Mini-Spin13, ≥6 (0–12); GAD14-2, ≥3 (0–6) | 4,753 | 453 (19.4%) | 304 (12.6%) | p ≤ 0.001 |
| Beutel et al. (40) | GHS | 4,928 | Type D personality | DS1415, ≥10 (0–28) | 4,928 | 561 (23.1%) | 534 (21.3%) | p = 0.13 |
| Grabe et al. (41) | SHIP | 2,035 | Depressive symptoms | BDI-II9, continues outcome (0–63) | 2,035 | 7.0 ± 7.9 | 5.7 ± 6.5 | p < 0.001 |
| Grabe et al. (42) | SHIP | 1,974 | Depressive symptoms | BDI-II9, continues outcome (0–63) | 1,974 | 7.0 ± 7.8 | 5.6 ± 6.2 | p < 0.001 |
| Häfner et al. (43) | KORA | 1,369 | Sleep disturbances, no depressed mood | USI16, ≥3 (1–6); DEEX17, ≥12 women; ≥10 men (0–24) | 1,369 | 157 (22.1%) | 95 (14.4%) | p < 0.01 |
| Perna et al. (44) | KORA | 3,347 | Resilience | RS-1118, upper third | 3,347 | 536 (30.5%) | 501 (31.5%) | p = 0.173 |
| Ladwig et al. (45) | KORA | 3,000 | Full PTSD3 | PDS and IES19 | 3,000 | 32 (2.1%) | 19 (1.3%) | p < 0.001 |
| Michal et al. (46) | GHS | 4,937 | Depression | PHQ-98, ≥10 (0–27) | 4,937 | 212 (8.7%) | 145 (5.8%) | p < 0.001 |
| Michal et al. (47) | GHS | 9,751 | Severe sleep problems | Item PHQ-98, ≥2 (0–3) | 9,751 | 548 (11.4%) | 354 (7.2%) | p < 0.001 |
| Schneider et al. (48) | KORA | 12,888 | Commiting suicide | Death certificates | 12,898 | 18 (0.3%) | 30 (0.5%) | p = 0.001 |
| Zebhauser et al. (49) | KORA | 1,022 | Mild/moderate depression | Geriatric Depression Scale-1520, ≥4 (0–15) | 1,058 | 87 (17.2%) | 60 (10.9%) | p = 0.011 |
| Anxiety | GAD-714, ≥10 (0–21) | 1,005 | 53 (10.6%) | 24 (4.8%) | p = 0.005 | |||
| Low life satisfaction | Item Satisfaction With Life Scale21, ≤4 (0–10) | 1,022 | 32 (6.3%) | 24 (4.7%) | p = 0.24 | |||
| Low resilience | RS-1118, lowest two thirds | 993 | 356 (71.8%) | 333 (67%) | p = 0.10 | |||
| Zebhauser et al. (50) | KORA | 346 | Living alone and loneliness | Item living alone (dichotom); UCLA- Loneliness-Scale-1222, ≥21 (0–36) | 346 | 76 (29.6%) | 29 (32.6%) | p = 0.59 |
| Beutel et al. (51) | GHS | 14,661 | Severe loneliness | Item frequency alone, =4 (0–4) | 14,413 | 165 (2.3%) | 83 (1.2%) | p < 0.001 |
| Goltz et al. (52) | SHIP | 3,926 | Depression and obesity | PHQ-98, ≥10 (0–27); WHR23, > 0.85 females; > 1.0 males | 3,926 | 77 (3.8%) | 25 (1.3%) | p < 0.010 |
| Rose et al. (53) | GHS | 7,930 | Fatigue | PBS24, ≥50 (0–100) | 7,948 | 1,266 (35.8%) | 918 (20.9%) | p < 0.001 |
| Atasoy et al. (54) | KORA | 9,340 | Depressed mood | DEEX17, ≥12 women; ≥10 men (0–24) | 9,340 | 1,702 (37.6%) | 1,814 (37.7%) | p = 0.96 |
| Beutel et al. (55) | GHS | 12,061 | New onset of depression | PHQ-98, ≥10 (0–27) | 10,036 | 232 (5%) | 205 (3.8%) | p = 0.003 |
| König et al. (56) | SHIP | 2,265 | Lifetime MDD4 | M-CIDI10 | 2,265 | 267 (22.5%) | 119 (11%) | p < 0.001 |
| Beutel et al. (57) | GHS | 7,974 | Somatic symptom load | PHQ-1225, ≥4 (0–24) | 7,974 | 1,121 (28.8%) | 1,073 (16.1%) | p < 0.001 |
| Schlax et al. (58) | GHS | 12,484 | Depressive symptoms | PHQ-28, ≥2 (0–6) | 12,484 | 1,598 (26.4%) | 1,281 (19.9%) | p < 0.001 |
Number and percentage or mean and standard deviation.
Bold printed values significant.
Post-traumatic stress disorder.
Major depressive disorder.
Depression, panic, social anxiety or generalized anxiety.
Composite International Diagnostic Screener (CID-S): 12 yes/no questions addressing different diagnostic domains.
PTSD module of the Structured Clinical Interview for DSM-IV (SCID) measures experience of traumatic event and PTSD symptoms, including criterion A2 (experiencing high distress during/after event), criterion B (five re-experiencing symptoms), criterion C (seven avoidance symptoms), and criterion D (five arousal symptoms).
Experiencing more than one traumatic event varying from combat or war zone experience to rape or abuse and illness.
Experiencing one re-experience (0–5), three avoidance (0–7) and two hyperarousal (0–5) symptoms.
Experiencing one re-experience (0–5) [no avoidance (0–7) or hyperarousal (0–5)] symptoms.
Patient Health Questionnaire 2 or 9 (PHQ-2 or PHQ-9) screens, diagnoses, monitors and measures severity of depression with two or nine items (4-point-Likert rating scale, 0–3).
Beck Depression Inventory-II (BDI-II) measures presence and severity of depressive symptoms with 21 items (4-point-Likert rating scale, 0–3).
Munich-Composite International Diagnostic Interview (M-CIDI) assesses psychiatric disorders over the lifespan according to DSM-IV criteria.
Brief Cambridge Depersonalization Scale (CDS-2) measures frequency and duration of depersonalization symptoms with two items (4-point-Likert rating scale, 0–3).
Brief PHQ Panic Module screens panic disorders with four dichotomous items.
Mini-Social Phobia Inventory (Mini-Spin) detects social anxiety with three items (5-point-Likert rating scale, 0–4).
Generalized Anxiety Disorder 2 or 7 (GAD-2 or GAD-7) screens for anxiety disorders with 2 or 7 items (4-point-Likert rating scale, 0–3).
Type D scale (DS14) comprises two reliable subscales with seven items each for negative affectivity and social inhibition (5-point-Likert rating scale, 0–4).
Adapted version of Uppsala Sleep Inventory (USI) measures initiating and maintaining sleep with two items (3-point-Likert rating scale, 1–3).
DEpression and EXhaustion subscale (DEEX scale) measures presence and severity of depression and anxiety with eight items (4-point-Likert rating scale, 0–3). Sex-specific cut-off points were applied (≥12 for women, and ≥10 for men).
Resilience scale 11 (RS-11) with 11 items (7-point-Likert scale, 1–7); highest one third indicates resilience, lowest two thirds indicates low resilience (thirds based on data).
Post-traumatic Diagnostic Scale (PDS) and impact of event scale (IES) indicate, respectively experience of a traumatic event (criteria A, 11 events) and symptoms of PTSD (criteria B, C, and D; re-experiencing, avoidance and arousal). Exposure to one traumatic event and 1 re-experience, one avoidance and 1 hyperarousal symptom indicate full PTSD.
Geriatric Depression Scale-15 measures depression among elderly with 15 dichotomous items.
Satisfaction With Life Scale: one item measuring satisfaction with life on a 0–10 rating scale.
UCLA loneliness scale-12 measures loneliness with 12 items with a 4-point-Likert rating scale (0–3).
Waist-to-hip ratio (WHR) is calculated by dividing the waist circumference through the hip circumference and therefore can adapt divergent values.
Personal Burnout Scale (PBS) measures physical and mental exhaustion with six items with a 5-point-Likert rating scale (1–5). Data were transformed to a metric scale (1 = 0; 2 = 25; 3 = 50; 4 = 75; 5 = 100).
Patient Health Questionnaire 12 (PHQ-12) contains the somatic symptom module of the Patient Health Questionnaire-15 (PHQ-15): 12 items with a three-point-Likert rating scale (0–2).
In general, women reported more mental health problems than men (38, 39). Regardless of the measurement scale, depression or depressive symptoms were reported more often by women than by men (32, 36, 41, 42, 46, 58). This also applied to new onset of depression (55) and additionally to specific subgroups, e.g., elderly (49). Major depressive disorders were more frequently present among women compared to men (36, 56). However, when the depression and exhaustion subscale was used, no difference between women and men in reporting depressed mood was found (54). Depression combined with obesity was more often seen in women (52). Depending on operationalization, depression or depressed mood in women ranged from 8.7% (GHS) to 36.8% (SHIP) and in men from 5.8% (GHS) to 37.7% (KORA). Suicidal ideation was more often present in women (9.2% GHS) compared to men (6.0% GHS) (35). However, the risk of committing suicide was higher for men (0.5% KORA) than for women (0.3% KORA) (48). Lastly, anxiety was more often present among women (55.8% SHIP) compared to men (38.9% SHIP) (32), this also applied to elderly women (10.6% KORA) and men (4.8% KORA) (49).
Women reported more somatic complaints compared to men (32, 57). This varied from 17.5% (SHIP) to 28.8% (GHS) for women and from 14.5% (SHIP) to 16.1% (GHS) for men. Sleeping problems (47) and fatigue (53) were more often reported by women. In addition, the combination of sleep disturbances and depressed mood was more frequent among women (43). Men reported more traumatic life events than women (33), whereas women developed more often (lifetime) post-traumatic stress disorder (PTSD) after experiencing such an event (33, 34, 45). In women, PTSD ranged from 2.1% (KORA) to 5.2% (SHIP). In men, PTSD ranged from 1.3% (KORA and SHIP) to 2.9% (SHIP). Loneliness was also more frequently prevalent in women than in men (51). For women in the age groups 35–44 years and 55–64 years, living alone was strongly associated with loneliness (51). For elderly who lived alone, no difference was found for loneliness between women and men (50). Other indicators of mental health, such as presence of Type D disorder (40) and depersonalization-derealization (37) did also not differ between women and men. For elderly, no difference between women and men was found regarding resilience (44, 49) and life satisfaction (49).
Factors Associated With Mental Health
A broad range of factors was associated with mental health. We categorized the results in five categories: (1) social and gender-related factors, (2) lifestyle, (3) interplay of physical and mental health, (4) body mass index (BMI) and diabetes and (5) genetic and biological factors. An overview of the results can be found in Table 2. The main findings are described below.
Table 2.
Explanatory factors mental health for women and men from the three cohorts.
| References | Designa | N | Waveb | Main resultse |
|---|---|---|---|---|
| Grabe et al. (59) | CS | 976 | SHIP-0 (non-random) | ° Low social support associated with high mental and physical distress (f). ° Chronic diseases associated with high mental and physical distress (f, m). °S/s-genotype and s/l-genotype on serotonin transporter gene (5-HT) and unemployment related to higher mental and physical distress compared to l/l genotype (f). °S/s-genotype and s/l-genotype on the 5-HT and chronic diseases related to higher mental and physical distress compared to l/l genotype (f). |
| von Lengerke et al. (60) | CS | 947 | KORA-Survey-2000 | ° No differences between f and m in associations between different weight groups and mental health-related quality of life (HRQL). |
| Grabe et al. (61) | CS | 1,059 | SHIP-0 (subjects aged ≥ 60) | ° More years in school, respectively 12 (f) or 10 (f, m) related to better mental status for older people. ° For older people, higher income, respectively in the 3rd quintile (m) or in the 4th and 5th quintile (f, m) related to better mental status. ° Five or more children associated with worse mental status (older f, m). ° A smaller number of teeth negatively associated with mental status (older f). |
| Lucht et al. (62) | CS | 406 | SHIP-I | ° Oxytocin receptor gene (OXTR) rs53576 A/A associated with less positive affect (m). |
| Wiczinski et al. (63) | CS | 2,732 | KORA F3 | ° Normal weight more often present in younger and higher educated people (f, m). ° Not living with partner related to a higher Body Mass Index (BMI) (m). ° Statutory health insurance associated with a higher BMI (f). ° Higher BMI (direction obese) associated with lower physical HRQL (f, m). ° Interaction between social support and BMI on physical HRQL (m). ° No association between BMI and mental HRQL (f, m). |
| Grabe et al. (64) | CS | 1,638 | SHIP-LEGENDc | ° No interaction effect of emotional neglect and Corticotropin-releasing hormone receptor (CRHR1) gene on depression (f, m). ° No interaction effect of abuse and CRHR1 gene on depression (f, m). ° For male interaction effect of physical neglect and CRHR1 gene on depression. |
| Ladwig et al. (65) | CS | 3,079 | KORA F3 | ° Low net income, physical inactivity, high level of somatic complaints and pulmonary disease symptoms associated with suicidal ideation (SID) (f, m). ° Unemployment, living alone, cigarette smoking, medium level of somatic complaints, myocardial infarction associated with SID (m). |
| Ladwig et al. (66) | CS | 11,895 | MONICA S1 MONICA S2 MONICA S3 | ° High cholesterol, obesity, hypertension, low alcohol consumption and diabetes mellitus related to excessive symptom reporting (ESR) (f, m). ° No partner (f), lower educational level and higher unemployment (f, m) associated with ESR. ° Diseases (metabolic syndrome, circulatory diseases, bronchial diseases, cancer and other diseases) related to ESR (f, m). ° Regular sleep disturbances, not a good health perception and psychological symptoms related to ESR (f, m). |
| Grabe et al. (67) | CS | 4,308 | SHIP-0 | ° Confirmation of findings of the original paper of Grabe et al. (59) with an updated sample. |
| Häfner et al. (68) | CS | 1,547 | MONICA S1 MONICA S2 MONICA S3 | ° Depression associated with social isolation (f), physical inactivity (m) and lower BMI (m). ° Inflammatory marker high-sensitivity C-reactive protein (hs-CRP) not associated with depression or social isolation. °Hs-CRP levels higher for people with depression and social isolation (m). ° Inflammatory marker interleukin-6 (IL-6) associated with social isolation (m). ° IL-6 levels higher for people with depression and social isolation (m). |
| Häfner et al. (69) | CS | 1,229 | MONICA S1 MONICA S2 MONICA S3 | ° Higher C-reactive protein (CRP) levels associated with social isolation and (no) depression (m). ° Higher leptin levels associated with social isolation/integration and depression (m). ° Smoking (m) and no partner (f) associated with social isolation (regardless of having depression). ° No partner (m) and higher age (f) associated with social isolation without depression. ° Sleeping disorder, high somatic complaints and negative self-perceived health associated with depression (regardless social isolation or integration) (f, m). ° Physically inactivity related to social isolation (regardless of having depression) (f, m) and to social integration and having depression (m). |
| Schunk et al. (70) | CS | 9,579 | KORA S4 SHIP-0 | ° Type 2 diabetes related to lower score on mental HRQL (f). ° No differences in associations between no Type 2 diabetes and mental HRQL (f, m). |
| Grabe et al. (41) | CS | 2,035 | SHIP-LEGENDc | ° A three way interaction between (1) brain-derived neurotrophic factor (BDNF) Met allele, (2) biallelic/triallelic 5-HTTLPR ss-allele and (3) non/mild childhood abuse influenced depression (f). |
| Häfner et al. (43) | CS | 1,369 | MONICA S1 MONICA S2 MONICA S3 | ° No associations between leptin levels and depressed mood or sleep disturbances (f, m). ° Associations between leptin levels and an interaction between depressed mood and sleep disturbances (f). ° Higher leptin levels related to depressed mood and sleep disturbances in normal weight people (f). ° For people with obesity and elevated leptin levels no associations between higher leptin levels and depressed mood and sleep disturbances (f). |
| Lukaschek et al. (71) | CS | 3,080 | KORA S4 | ° Combat or war zone (f, m), non-sexual assaults by known assailants (f, m), experience of interpersonal conflict (m), sexual assaults by known assailant (m) and life threatening diseases (f) important factors for development of full Post-Traumatic Stress Disorder (PTSD). ° For men experience of interpersonal conflict (f, m), life threatening illness (f, m), having a serious accident (m) and sexual or non-sexual assaults by known assailants (f) important factors for development of partial PTSD. |
| Schomerus et al. (72) | CS | 395 | SHIP-0 SHIP-I SHIP-LEGENDc |
° No differences between f and m in the association between childhood abuse, personality traits and resilience and help-seeking for depression. |
| Wiltink et al. (73) | CS | 5,000 | GHS BL | ° Obesity measure waist-to-hip ratio (WHR) positively related with depression and somatic-affective symptoms (m). ° Obesity measures BMI and waist-to-height ratio (WHtR) negatively related to cognitive-affective symptoms (f). ° Obesity measure waist circumference (WC) negatively associated with cognitive-affective symptoms (m). |
| Emeny et al. (74) | CS | 985 | KORA-AGEd | ° Higher levels of insulin-like growth factor binding protein-3 (IGFBP-3) associated with higher well-being (elderly f). ° Higher insulin-like-growth factor 1 (IGF-I) levels associated with more depression (elderly f). ° No relation between IGFBP-3 and depression (elderly f, m). ° Active elderly f with the highest IGF-I and IGFBP-3 levels higher well-being than inactive elderly f with similar IGF-I levels and IGFBP-3 levels. |
| Hunger et al. (75) | CS & LS | 1,046 | KORA S4 KORA F4 |
° People of 55 years and older with prediabetes at baseline and diabetes at follow-up scored lower on mental HRQL than people with persistent prediabetes (m). ° People of 55 years and older with normal glucose tolerance (NGT) at baseline and prediabetes at follow-up scored lower on mental HRQL than people with NGT at follow-up (f). |
| Klug et al. (76) | CS | 969 | KORA-AGEd | ° For elderly people higher attachment (m) and lower loneliness (f, m) scores related to not having late life depression. |
| Laxy et al. (77) | LS | 3,080 | KORA S4 KORA F4 |
° Heavy weight gain associated with impairments in physical health (f, obese m) and improvements in mental health (f). |
| Sievers et al. (78) | CS & LS | 4,079 (CS) 3,141 (LS) | SHIP-0 SHIP-I |
° Low IGF-I levels (f) and high IGF-I levels (m) predict incidence of depressive disorders. |
| Zebhauser et al. (49) | CS | 1,022 | KORA-AGEd | ° People older than 85 years experience more loneliness than people between 64 and 84 years (f, m). ° Elderly women (>85) experience more loneliness than elderly men. ° For older people associations between a small social network and loneliness (f, m). ° Older age related physical limitations mostly not associated with loneliness (f, m). ° Inactivity related to loneliness (elderly f). ° Depression and anxiety associated with loneliness (elderly f, m). ° More life satisfaction and stronger resilience associated with not being lonely (elderly f, m). |
| Baumeister et al. (79) | LS | 4,228 (SHIP-0) 4,251 (SHIP-T) |
SHIP-0 SHIP-Trend | ° Relative increase of depressive symptoms between 1997–2001 and 2008–2012 stronger for men than for women. ° Strongest change of depressive symptoms between 1997–2001 and 2008–2012 in age group 50–64 years (f, m); smallest change in age group 20–34 years (f, m). ° No difference in prevalence of depressive symptoms between 2008–2012 and 1997–2001 (f, m). |
| Johar et al. (80) | CS | 733 | KORA-AGEd | ° Lower morning to evening cortisol ratio associated with cognitive impairment (elderly m). ° Late evening cortisol measures and cortisol awakening response (CAR) not associated with cognitive impairment (elderly f, m). |
| Schunk et al. (81) | CS | 846 | KORA S4 SHIP-0 |
° Using oral diabetic medication, insulin diabetic medication or oral and insulin diabetic medication associated with lower mental HRQL (f). |
| Lukaschek et al. (82) | CS | 3602 | KORA-AGEd | ° For elderly low income, anxiety, depression, sleeping problems, physical inactivity and multi-morbidity associated with low subjective well-being (f, m). ° Living alone associated with low subjective well-being (elderly f). |
| Rabel et al. (83) | CS & LS | 3,080 | KORA S4 KORA F4 KORA FF4 |
° Women with a higher BMI later in life less physical HRQL than men. ° Women with no or low physical activity later in life less mental HRQL than men. |
| Beutel et al. (55) | LS | 12,061 | GHS BL GHS FU 2 |
° Cancer, loneliness, social phobia and generalized anxiety risk factors for new onset of depression (f). ° Smoking and life events risk factors for new onset of depression (m). ° Social support associated with less new onset of depression (f, m). |
| Beutel et al. (57) | CS | 7,974 | GHS FU 2 | ° Lack of social support, adverse life events, depression, generalized anxiety, panic and social phobia strongest predictors for somatic symptoms (f, m). ° Loneliness predictor for somatic symptoms (f). |
CS, cross-sectional study; LS, longitudinal study.
SHIP-0 = 1997–2001, SHIP-I = 2002–2006, SHIP-LEGEND = 2007–2010, SHIP-Trend = 2008–2012, KORA S4 (1999–2001), KORA F3 = 2004–2005, KORA F4 (2006–2008), KORA FF4 (2013–2014), MONICA S1 = 1984–1985, MONICA S2 = 1989–1990, MONICA S3 = 1994–1995, GHS BL = 2007–2012, GHS FU 1 = 2009–2014, GHS FU 2 = 2012–2017.
SHIP-LEGEND is an add on study, based on the SHIP-0 cohort.
KORA-AGE includes MONICAS1, MONICAS2, MONICAS3 and KORA S4. Participants aged 65 years or older at the end of 2008 were selected.
f, female; m, male.
Social and Gender-Related Factors
The three cohorts have been drawn as local representative samples of the general population, stratified for sex, age, and urban-rural residence. In all cohorts, women had a lower income than men. Furthermore, men were more often married or living with a partner, whereas more elderly women were living alone. In addition, life expectancy differed between the regions; life expectancy was highest in the middle of Germany and lowest in the northeast of Germany. The demographic and socioeconomic differences between the cohorts influenced associations with mental health.
Social support and social isolation were often associated with mental health. Lack of social support was a strong predictor for somatic symptoms for both women and men (57). For older women and men, a smaller social network was associated with loneliness (49). For women, low social support was associated with higher mental and physical distress (59) and women without a partner reported more excessively somatic symptoms (66) and were more often socially isolated (69). The presence of social support turned out to be a protective factor against new onset of depression for both women and men (55). For men, not having a partner was associated with social isolation (69) and living alone was linked to suicidal ideation (65). Additionally, elderly women living alone reported lower subjective well-being (82). Depressed women were more likely to be socially isolated (68), and older women were also more often socially isolated, regardless of suffering from a depression (69). For women as well as men, adverse life events were strong predictors for somatic symptoms (57). For men, negative life events were a risk factor for new onset of depression (55) and associated with the development of PTSD (55). Experience of combat or war zone and non-sexual assaults by known assailants were risk factors for developing full PTSD (71) for women and men. For help seeking when suffering from depression, no differences were found between women and men (72).
With regard to gender-related factors, findings for women and men were similar. Social economic status predicted somatic symptoms for women and men (57). Low income had a negative effect on well-being (82) and was associated with suicidal ideation (65). Having five or more children was associated with a worse mental health status (61) and low educational level and unemployment were related to excessive symptom reporting (66). A difference was found in the association between unemployment and suicidal ideation, which was only present for men (65). No effects were found for social economic status on new onset of depression (55), educational level on well-being (82) and unemployment on somatic symptoms (57). Furthermore, no association between net income and status as homemaker were found (65). In general, educational attainment, income and employment did not have an effect on the increase of depressive symptoms over the last years (79).
Lifestyle
Smoking and physical inactivity are known factors to negatively influence physical and mental health. Smoking was a risk factor for new onset of depression, but only in men (55). Besides, smoking was associated with suicidal ideation (65) and with social isolation (69) for men. For physical activity, effects for women and men were found. For both women and men being physically inactive was related to social isolation and for men also to social integration and suffering from depression (69). Another study confirmed that depressed men were more likely to be physically inactive than women (68). For both women and men associations between physical inactivity and suicidal ideation were found (65). Women who were moderately active had a lower mental health-related quality of life (HRQL) score than men who were moderately active (83). For older women physical inactivity was associated with loneliness (49), whereas the association between physical inactivity and low subjective well-being was found for both elderly women and elderly men (82). Low alcohol consumption was associated with excessive symptom reporting for both women and men (66).
Interplay of Physical and Mental Health
The interplay between physical and mental health has been examined in many studies included in the current review. For both women and men chronic diseases were associated with worse mental and physical well-being (59). For women the experience of a life threatening disease was associated with the development of full and partial PTSD, for men it was only associated with partial PTSD (71). For women cancer, social phobia, generalized anxiety and loneliness were risk factors for new onset of depression (55). Sleeping disorder, somatic complaints and negative self-perceived health were associated with depression for women as well as for men (69). For elderly women and men absence of loneliness was a protective factor for depression later in life (76), for elderly men, stronger attachment was an additional a protective factor. Depression, generalized anxiety, panic and social phobia predicted somatic symptoms for women and men (57), for women somatic symptoms were also predicted by loneliness. Increased reporting of somatic symptoms was predicted by diseases in general (metabolic syndrome, circulatory diseases, bronchial diseases, cancer and other diseases) for both women and men (66) and associated with sleep disturbances, worse health perception and presence of psychological symptoms. High levels of somatic complains and pulmonary disease symptoms were associated with suicidal ideation for women and men (65), for men medium level of somatic complaints, myocardial infarction and stroke were additionally associated with suicidal ideation. For women as well as for men, depressive symptoms were associated with suicidal ideation (65).
Body Mass Index (BMI) and Diabetes
Obesity and diabetes are significant health threats in an aging population. When comparing women and men in the association between BMI and HRQL (physical and mental), women with a higher BMI reported lower physical HRQL later in life than men with a higher BMI (83). Another study found an association between high BMI and less physical HRQL for both women and men (63), but in men with strong social support, this association vanished. No association was found between BMI and mental HRQL for either women or men (63) and no differences were found between women and men (60, 83). Women with type 2 diabetes scored lower on mental HRQL compared to men with Type 2 diabetes (70), regardless of type of diabetic medication (81). Changes in the diabetes trajectory also influenced mental HRQL. Men of 55 years and older with prediabetes at baseline and diabetes at follow-up scored lower on mental HRQL than men with persistent prediabetes (75). Women with normal glucose tolerance at baseline and prediabetes at follow-up scored lower on mental HRQL compared to women who still had normal glucose tolerance at follow-up (75). For women and overweight men weight gain was associated with impaired physical health (77). For women, weight gain was associated with improvements in mental health (77). Men with lower BMI more often suffered from a depression (68) and lower BMI was associated with social isolation (69). In addition, diabetes mellitus and obesity were related to excessive somatic symptom reporting (66). Furthermore, using different indicators for obesity [e.g., waist-to-hip ratio (WHR) or BMI] led to different findings (73).
Genetic and Biological Factors
Genetic and biological factors may affect mental health status and the development of mental health disorders. For mental and physical distress, the s/s-genotype and the s/l-genotype on the serotonin transporter gene in combination with unemployment or chronic diseases was related to higher mental and physical distress for women (59, 67). Elderly women reported better well-being when higher levels of insulin-like growth factor binding protein-3 (IGFBP-3) were present. A discrepancy between women and men was found for insulin-like-growth factor 1 (IGF-I). For women, low IGF-I levels predicted the incidence of depressive disorders 5-years later, whereas for men high levels of IGF-I predicted future depression (78). In another study an association between IGF-I levels and current depression was found for elderly women, but contrary to the previous results; higher IGF-I levels were associated with more depression (74). Furthermore, for women lower cholesterol levels were associated with suffering from depression (69). Higher cholesterol levels were associated with increased symptom reporting of somatic symptoms and with hypertension for women and men (66). For men higher C-reactive protein (CRP) levels were associated with social isolation and the presence of depression (69). The inflammatory marker high-sensitivity C-reactive protein (hs-CRP) was not associated directly with either depression or social isolation, but for men with a depressed mood hs-CRP levels were higher compared to men without depressed mood and without being socially isolated (68). No associations between leptin levels and depressed mood or sleep disturbances were found for either women or men (43). However, in normal weight women, leptin levels were higher for women suffering from both depressed mood and sleep disturbances. Associations between cortisol levels and cognitive functioning depend on time of day measurement of cortisol levels (80). Associations between cortisol levels and loneliness were found in married elderly men, but not in married elderly women (84). A study focussing on the oxytocin receptor gene rs53576 A/A found an association between oxytocin receptor gene and less positive affect (strong excitement/emotion) for men (62). A three way interaction between brain-derived neurotrophic factor: Met allele, biallelic 5-HTTLPR: ss-allele and no/mild childhood abuse was found to influence depression for women (41). For men an interaction effect of physical neglect with Corticotropin-releasing hormone receptor 1 gene on depression was found (64).
Discussion
In this systematic review, we compared prevalences and determinants of mental health indicators from three large, ongoing German cohorts. The benefits of combining three different cohorts are multiple. First, the cohorts represent the general population in three regions, namely KORA in the south, SHIP in the northeast and GHS in the middle of Germany. In these three regions, the composition of populations differs with respect to socioeconomic and regional characteristics. Therefore, the articles complement each other and the conclusions based on concurrent evidence are stronger. Secondly, the stratified random sample selection in all cohorts provides representative groups for the general adult population in the respective areas of Germany. The proportions of women and men in the cohorts are equal and broad ranges of age are covered. Repeated follow-ups provide the opportunity to study participants longitudinally and determine life-span developments. A third advantage of are the overlapping psychological, medical and laboratory assessments. Lastly, the overall number of participants from the three cohorts together is more than 40 000 (28).
Mental health plays a major role in the concurrent German cohort studies and sex differences are increasingly taken into account in analyses. This is underlined by the differences of prevalence rates of mental distress between women and men. In all cohorts, women reported worse mental health than men (38, 39, 85). Particularly, depression, depressed mood or symptoms were more often present in women (32, 36, 41, 42, 46, 52, 54, 56, 58). Additionally, as reported in one or two of the three cohorts, new onset of depression (55), anxiety (32), traumatic events and PTSD (33, 34, 45), suicidal ideation (35), sleeping problems and fatigue (47, 53), somatic complaints (32, 57) and loneliness (51) were more often reported by women, whereas the risk of committing suicide was stronger in men (48). A recent paper using SHIP data confirmed that women were more often affected by depressive, anxiety, obsessive-compulsive disorder, PTSD, somatoform and eating disorders (12-month and lifetime), whereas men indicated substance use more often (86). These results indicate similarities between cohorts and thus regions in sex-specific prevalence rates of mental health. Furthermore, these findings are consistent with current literature on prevalence rates of mental health in several countries. A meta-analysis on depression including 90 studies from 30 countries reported consistently higher prevalence rates of depression in women compared to men (87). In a review on social anxiety disorder including 14 studies from different countries, women were more often suffering from anxiety and reported elevated severity compared to men (88). A systematic review on suicidal behavior and suicide in Europe and America reported that men commit suicide more frequently, whereas women have more attempts and suicidal behavior (89). Furthermore women reported more often lifetime PTSD (90), somatoform diseases (91) fatigue (92, 93) and loneliness (94, 95). The higher prevalence of loneliness is especially present in older women and consistent across several European countries (96).
With regard to risk and protective factors for mental health, differences and similarities were found between women and men. For women loneliness, social isolation and low social support were risk factors for depression or mental distress (55, 59, 68, 69, 76). This finding was consistent in the three cohorts Further, for women, cancer, social phobia, generalized anxiety (55), sleeping disorders and negative self-perceived health (69) were associated with (new onset of) depression. For men myocardial infarction and stroke were associated with suicidal ideation (65). As men experience cardiovascular events at younger age (97), their consequences may lead to a high burden in daily life which can contribute to an increase of suicidal ideation. Additionally, for men, physical inactivity was associated with depression (68, 69) and smoking with new onset of depression (55), suicidal ideation (65) and social isolation (69). With regard to biological factors, for women, lower cholesterol levels were associated with depression (69) and higher leptin levels with depressed mood (43). For men, higher interleukin-6 levels and higher hs-CRP levels were associated with depression and social isolation (68), higher leptin levels predicted depression and social isolation (69). For other mental health outcomes, no differences were found between women and men. Chronic and life threatening diseases were associated with more mental and physical distress for women as well as for men in all three cohorts (59, 66, 67). Further, for both women and men associations were found between somatic complaints and depression (69) and suicidal ideation (65), life threatening disease and partial PTSD (71) and pulmonary disease and suicidal ideation (65). Additionally, depression, generalized anxiety, panic and social phobia were predictors of somatic symptoms for both sexes (57). Lastly, no differences between sexes were found in the association of BMI with mental HRQL (60, 63, 83).
Not all mental health aspects and possible risk and protective factors were examined in all cohorts, this makes it more complicated to draw conclusions about regional similarities and differences. The most consistent and detailed findings were found for depression. In all cohorts depression, depressed mood or symptoms of depression were more often present in women compared to men (32, 36, 41, 42, 46, 52, 54, 56, 58). This gender gap is known to become manifest already in early adolescence and declines in early adulthood, remaining stable afterwards (98). When controlling for demographic and socioeconomic background this gender gap persisted (99). However, many studies question whether men actually experience less depression or if depression among men just remains frequently undetected. In a study on men's attitude regarding depression, normative expectations regarding masculinity equated suffering from depression to a weakness (100). Conforming to such traditional masculine norms is problematic for help-seeking for depression (101). This may also contribute to the higher suicide rate in men. Men are less likely to seek treatment for depression and when they seek treatment, they are less likely to be diagnosed with major depressive disorder (97). This is in part due to different symptoms of depression in women and men. When examining depressed patients, men reported more anger attacks compared to women and scored higher on irritability and overreaction (102). When testing the Gotland Scale for Male Depression (103), irritability appeared to be the best indicator of male depression (104). Studies have also strong associations between alcohol abuse, depression and suicidal behavior interacting with biological factors in men (105) and alcohol consumption as a coping strategy for depression in men (106). Thus, depression in men is often masked by atypical symptoms, such as externalizing depression symptoms. For men, external risk factors for depression were also found in this review [e.g., smoking (55) and physical inactivity (44)], whereas the risk profile for women contained more internal factors [e.g., loneliness (55) and social isolation (68)].
Since gender was not measured directly in the studies reviewed, socioeconomic and family-related factors were examined as gender-related factors. In general, women were more often housewives (41), in maternity leave (41), or unemployed (59) compared to men. On average, men had a higher income and education (41) compared to women. Differences between women and men with regard to gender indicators and mental health were found for unemployment and suicidal ideation (65, 69). For men unemployment was positively associated with suicidal ideation. Other associations between gender indicators and mental health were found for both women and men. Income was negatively associated with suicidal ideation (65), positively with mental health status (61) and for elderly positively with subjective well-being (82). Education was negatively associated with excessive symptom reporting (66) and positively with mental health status (61). Lower social economic status predicted somatic symptoms (57) and having five or more children was associated with a worse mental health status (61). Lastly, unemployment was positively associated with excessive symptom reporting (66). Unfortunately, none of the articles examined a moderation or mediation effect of gender-related factors in the relation between sex and mental health. Therefore, it is not possible to determine the contributions of sex and gender. In general interactions between sex and socioeconomic position are understudied (19). A study in Brazil testing mediating effects of socioeconomic factors in the association between sex and mental health revealed that personal income and schooling at the age of 30 mediates the association between sex and depression, anxiety and common mental disorders (107), but not family income or maternal schooling. Testing socioeconomic and family-related factors in associations between sex and mental health in longitudinal studies could contribute notably to the understanding of gender aspects in mental health.
Only very recently, the binary assessment of sex has been supplemented by the third category, diverse sex. Therefore, this paper does not discuss gender diversity, although it is known that the mental health of the German LHBTI community (lesbian, gay, bisexual, transgender and intersex individuals) should be further examined (11). Mental health of the LHBTI community has been expected to differ from the overall population [e.g., depression and suicidal behavior (108, 109)] due to the heteronormative orientation of society (110, 111)”. Increasing social acceptance could lead to more possibilities to express one's gender identity and sexual orientation which could improve the health status of sexual minorities (11). A further limitation in this study is that mental health was measured by self-report questionnaires. Since the measurements tools used are reliable and valid, it will still be a good indication of reality. Different questionnaires were used to assess the same mental health construct. In order to overcome this last limitation, the GESA project, integrating data from these three cohorts to examine mental health, harmonizes data (28). Studying interactions between socioeconomic and vocational factors with sex (e.g., full employment of women in SHIP vs. the role of housewife in KORA and GHS) will help to identify differential impact of socioeconomic inequality.
Overall, this systematic review shows the differences and similarities in prevalence rates and determinants of mental health indicators between women and men, from genetic and biological factors to indicators of the social environment. While our picture is far from complete, gender gaps regarding income, education, or living in a relationship underline the need to differentiate mental health outcomes according to sex-related determinants of mental health. Differing risk and protective factors for mental health require a sex sensitive prevention approach. However, this review shows that current research on mental health still lacks a clear focus on gender roles and identities, which have recently been included in the Gutenberg Health Study. Future research should therefore illuminate sex differences and broader sex and gender diversity (112). Therefore, an increased focus on sex and gender in mental health research is of great importance.
Author Contributions
This review was written as part of the GESA Project. All authors contributed to the development and refinement of the GESA consort. MB, EB, HB, HG, JK, K-HL, GS, and PW were grant holders. The idea for this paper came from DO and MB. DO performed the literature search, selection of paper and drafted, together with MB, the first version of the review, which was substantially revised by GS, AT, and EB. Improvements of HB, JK, K-HL, PW, and HG lead to the current version of this review.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are grateful to all study participants. Further, the authors thank the staff involved in the planning, organization and conduct of the GHS, KORA and SHIP.
Footnotes
Funding. GESA was funded by the Federal Ministry of Education and Research (BMBF; Nr.01GL1718A).
References
- 1.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. (2015) 72:334–41. 10.1001/jamapsychiatry.20142502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacobi F, Höfler M, Strehle J, Mack S, Gerschler A, Scholl L, et al. Psychische störungen in der allgemeinbevölkerung. Der Nervenarzt. (2014) 85:77–87. 10.1007/s00115-013-3961-y [DOI] [PubMed] [Google Scholar]
- 3.Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. (2011) 21:655–79. 10.1016/j.euroneuro.2011.07018 [DOI] [PubMed] [Google Scholar]
- 4.Rosenfield S, Smith D. Gender and mental health: do men and women have different amounts or types of problems? In: Scheid TL, Brown TN. editors. A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. 2nd ed Cambridge: Cambridge University Press; (2009). p. 256–67. 10.1017/CBO9780511984945017 [DOI] [Google Scholar]
- 5.Tannenbaum C, Greaves L, Graham ID. Why sex and gender matter in implementation research. BMC Med Res Methodol. (2016) 16:145. 10.1186/s12874-016-0247-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eagly AH, Wood W. Social Role Theory of Sex Differences. The Wiley Blackwell encyclopedia of gender and sexuality studies. (2016) p. 1–3. 10.1002/9781118663219wbegss1839414607 [DOI] [Google Scholar]
- 7.Kuehner C. Why is depression more common among women than among men?. Lancet Psychiatry. (2017) 4:146–58. 10.1016/S2215-0366(16)30263-2 [DOI] [PubMed] [Google Scholar]
- 8.Li SH, Graham BM. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatry. (2017) 4:73–82. 10.1016/S2215-0366(16)30358-3 [DOI] [PubMed] [Google Scholar]
- 9.Bangasser DA, Valentino RJ. Sex differences in stress-related psychiatric disorders: neurobiological perspectives. Front Neuroendocrinol. (2014) 35:303–19. 10.1016/j.yfrne.2014.03008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oram S, Khalifeh H, Howard LM. Violence against women and mental health. Lancet Psychiatry. (2017) 4:159–70. 10.1016/S2215-0366(16)30261-9 [DOI] [PubMed] [Google Scholar]
- 11.Pöge K, Dennert G, Koppe U, Güldenring A, Matthigack EB, Rommel A. The health of lesbian, gay, bisexual, transgender and intersex people. J Health Monitoring. (2020) 2020:1–27. 10.25646/6449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The EUGenMed Cardiovascular Clinical Study Group Regitz-Zagrosek V Oertelt-Prigione S Prescott E Franconi F Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J. (2016) 37:24–34. 10.1093/eurheartj/ehv598 [DOI] [PubMed] [Google Scholar]
- 13.Beutel ME., Brähler E, Tibubos AN. Gender und psychische gesundheit: bedeutung für die psychotherapeutische Praxis. In: Moeslein-Teising I, Schäfer G, Martin R. editors. Geschlechter-Spannungen. 1st ed Gießen: Psychosozial-Verlag; (2019). p. 54–65. 10.30820/9783837976229-54 [DOI] [Google Scholar]
- 14.Piccinelli M, Wilkinson G. Gender differences in depression: critical review. Br J Psychiatry. (2000) 177:486–92. 10.1192/bjp.177.6486 [DOI] [PubMed] [Google Scholar]
- 15.Möller-Leimkühler A. The gender gap in suicide and premature death or: why are men so vulnerable? Eur Arch Psychiatry Clin Neurosci. (2003) 253:1–8. 10.1007/s00406-003-0397-6 [DOI] [PubMed] [Google Scholar]
- 16.Van de Velde S, Bracke P, Levecque K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc Sci Med. (2010) 71:305–13. 10.1016/j.socscimed.2010.03035 [DOI] [PubMed] [Google Scholar]
- 17.Leupp K. Depression, work and family roles, and the gendered life course. J Health Soc Behav. (2017) 58:422–41. 10.1177/0022146517737309 [DOI] [PubMed] [Google Scholar]
- 18.Kosidou K, Dalman C, Lundberg M, Hallqvist J, Isacsson G, Magnusson C. Socioeconomic status and risk of psychological distress and depression in the stockholm public health cohort: a population-based study. J Affect Disord. (2011) 134:160–7. 10.1016/j.jad.2011.05024 [DOI] [PubMed] [Google Scholar]
- 19.O'Neil A, Russell JD, Thompson K, Martinson ML, Peters SAE. The impact of socioeconomic position (SEP) on women's health over the lifetime. Maturitas. (2020) 140:1–7. 10.1016/j.maturitas.2020.06001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pedrós Barnils N, Eurenius E, Gustafsson P. Self-rated health inequalities in the intersection of gender, social class and regional development in Spain: exploring contributions of material and psychosocial factors. Int J Equity Health. (2020) 19:1–14. 10.1186/s12939-020-01202-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bleidorn W, Arslan RC, Denissen JJ, Rentfrow PJ, Gebauer JE, Potter J, et al. Age and gender differences in self-esteem - a cross-cultural window. JPSP. (2016) 111:396. 10.1037/pspp0000078 [DOI] [PubMed] [Google Scholar]
- 22.Gong X, Wong N, Wang D. Are gender differences in emotion culturally universal? Comparison of emotional intensity between Chinese and German samples. J Cross Cult Psychol. (2018) 49:993–1005. 10.1177/0022022118768434 [DOI] [Google Scholar]
- 23.Fischer AH, Rodriguez Mosquera PM, Van Vianen AE, Manstead AS. Gender and culture differences in emotion. Emotion. (2004) 4:87 10.1037/1528-3542.4.187 [DOI] [PubMed] [Google Scholar]
- 24.Zell E, Krizan Z, Teeter SR. Evaluating gender similarities and differences using metasynthesis. AmP. (2015) 70:10–20. 10.1037/a0038208 [DOI] [PubMed] [Google Scholar]
- 25.Holle R, Happich M, Löwel H, Wichmann H-E, Group nftMKS. KORA-a research platform for population based health research. Das Gesundheitswesen. (2005) 67:19–25. 10.1055/s-2005-858235 [DOI] [PubMed] [Google Scholar]
- 26.John U, Hensel E, Lüdemann J, Piek M, Sauer S, Adam C, et al. Study of health in pomerania (SHIP): a health examination survey in an east German region: objectives and design. Sozial-und Präventivmedizin. (2001) 46:186–94. 10.1007/BF01324255 [DOI] [PubMed] [Google Scholar]
- 27.Wild PS, Zeller T, Beutel M, Blettner M, Dugi KA, Lackner KJ, et al. Die gutenberg gesundheitsstudie. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz. (2012) 55:824–30. 10.1007/s00103-012-1502-7 [DOI] [PubMed] [Google Scholar]
- 28.Burghardt J, Tibubos AN, Otten D, Brähler E, Binder H, Grabe HJ, et al. A multi-cohort consortium for GEnder-sensitive analyses of mental health trajectories and implications for prevention (GESA) in the general population in Germany. BMJ Open. (2020) 10:e034220. 10.1136/bmjopen-2019-034220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization (WHO) Promoting Mental Health: Concepts, Emerging Evidence, Practice: Summary Report. WHO; (2004). [Google Scholar]
- 30.Galderisi S, Heinz A, Kastrup M, Beezhold J, Sartorius N. Toward a new definition of mental health. World Psychiatry. (2015) 14:231–3. 10.1002/wps20231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith PM, Koehoorn M. Measuring gender when you don't have a gender measure: constructing a gender index using survey data. Int J Equity Health. (2016) 15:82. 10.1186/s12939-016-0370-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grabe HJ, Baumeister SE, John U, Freyberger HJ, Völzke H. Association of mental distress with health care utilization and costs: a 5-year observation in a general population. Soc Psychiatry Psychiatr Epidemiol. (2009) 44:835–44. 10.1007/s00127-009-0005-9 [DOI] [PubMed] [Google Scholar]
- 33.Grabe HJ, Spitzer C, Schwahn C, Marcinek A, Frahnow A, Barnow S, et al. Serotonin transporter gene (SLC6A4) promoter polymorphisms and the susceptibility to posttraumatic stress disorder in the general population. Am J Psychiatry. (2009) 166:926–33. 10.1176/appi.ajp.200908101542 [DOI] [PubMed] [Google Scholar]
- 34.Spitzer C, Barnow S, Volzke H, John U, Freyberger HJ, Grabe HJ. Trauma, posttraumatic stress disorder, and physical illness: findings from the general population. Psychosom Med. (2009) 71:1012–7. 10.1097/PSY0b013e3181bc76b5 [DOI] [PubMed] [Google Scholar]
- 35.Michal M, Wiltink J, Till Y, Wild PS, Munzel T, Blankenberg S, et al. Type-D personality and depersonalization are associated with suicidal ideation in the German general population aged 35-74: results from the gutenberg heart study. J Affect Disord. (2010) 125:227–33. 10.1016/j.jad.2010.02108 [DOI] [PubMed] [Google Scholar]
- 36.Appel K, Schwahn C, Mahler J, Schulz A, Spitzer C, Fenske K, et al. Moderation of adult depression by a polymorphism in the FKBP5 gene and childhood physical abuse in the general population. Neuropsychopharmacology. (2011) 36:1982–91. 10.1038/npp.201181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Michal M, Wiltink J, Till Y, Wild PS, Blettner M, Beutel ME. Distinctiveness and overlap of depersonalization with anxiety and depression in a community sample: results from the Gutenberg heart study. Psychiatry Res. (2011) 188:264–8. 10.1016/j.psychres.2010.11004 [DOI] [PubMed] [Google Scholar]
- 38.Spitzer C, Glaser S, Grabe HJ, Ewert R, Barnow S, Felix SB, et al. Mental health problems, obstructive lung disease and lung function: findings from the general population. J Psychosom Res. (2011) 71:174–9. 10.1016/j.jpsychores.2011.03005 [DOI] [PubMed] [Google Scholar]
- 39.Wiltink J, Beutel ME, Till Y, Ojeda FM, Wild PS, Munzel T, et al. Prevalence of distress, comorbid conditions and well being in the general population. J Affect Disord. (2011) 130:429–37. 10.1016/j.jad.2010.10041 [DOI] [PubMed] [Google Scholar]
- 40.Beutel ME, Wiltink J, Till Y, Wild PS, Munzel T, Ojeda FM, et al. Type D personality as a cardiovascular risk marker in the general population: results from the Gutenberg health study. Psychother Psychosom. (2012) 81:108–17. 10.1159/000331776 [DOI] [PubMed] [Google Scholar]
- 41.Grabe HJ, Schwahn C, Mahler J, Appel K, Schulz A, Spitzer C, et al. Genetic epistasis between the brain-derived neurotrophic factor Val66Met polymorphism and the 5-HTT promoter polymorphism moderates the susceptibility to depressive disorders after childhood abuse. Prog Neuropsychopharmacol Biol Psychiatry. (2012) 36:264–70. 10.1016/j.pnpbp.2011.09010 [DOI] [PubMed] [Google Scholar]
- 42.Grabe HJ, Schwahn C, Mahler J, Schulz A, Spitzer C, Fenske K, et al. Moderation of adult depression by the serotonin transporter promoter variant (5-HTTLPR), childhood abuse and adult traumatic events in a general population sample. Am J Med Genetics B Neuropsychiatric Genetics. (2012) 159B:298–309. 10.1002/ajmg.b32027 [DOI] [PubMed] [Google Scholar]
- 43.Häfner S, Baumert J, Emeny RT, Lacruz ME, Thorand B, Herder C, et al. Sleep disturbances and depressed mood: a harmful combination associated with increased leptin levels in women with normal weight. Biol Psychol. (2012) 89:163–9. 10.1016/j.biopsycho.2011.10005 [DOI] [PubMed] [Google Scholar]
- 44.Perna L, Mielck A, Lacruz ME, Emeny RT, Holle R, Breitfelder A, et al. Socioeconomic position, resilience, and health behaviour among elderly people. Int J Public Health. (2012) 57:341–9. 10.1007/s00038-011-0294-0 [DOI] [PubMed] [Google Scholar]
- 45.Ladwig K-H, Brockhaus AC, Baumert J, Lukaschek K, Emeny RT, Kruse J, et al. Posttraumatic stress disorder and not depression is associated with shorter leukocyte telomere length: findings from 3,000 participants in the population-based KORA F4 study. PLoS ONE. (2013) 8:e64762. 10.1371/journal.pone0064762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Michal M, Wiltink J, Kirschner Y, Wild PS, Münzel T, Ojeda FM, et al. Differential associations of depressive symptom dimensions with cardio-vascular disease in the community: results from the gutenberg health study. PLoS ONE. (2013) 8:e72014. 10.1371/journal.pone0072014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Michal M, Wiltink J, Kirschner Y, Schneider A, Wild PS, Munzel T, et al. Complaints of sleep disturbances are associated with cardiovascular disease: results from the Gutenberg health study. PLoS ONE. (2014) 9:e104324. 10.1371/journal.pone0104324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schneider B, Lukaschek K, Baumert J, Meisinger C, Erazo N, Ladwig KH. Living alone, obesity, and smoking increase risk for suicide independently of depressive mood findings from the population-based MONICA/KORA augsburg cohort study. J Affect Disord. (2014) 152–4:416–21. 10.1016/j.jad.2013.10007 [DOI] [PubMed] [Google Scholar]
- 49.Zebhauser A, Hofmann-Xu L, Baumert J, Häfner S, Lacruz M, Emeny R, et al. How much does it hurt to be lonely? Mental and physical differences between older men and women in the KORA-age study. Int J Geriatr Psychiatry. (2014) 29:245–52. 10.1002/gps3998 [DOI] [PubMed] [Google Scholar]
- 50.Zebhauser A, Baumert J, Emeny RT, Ronel J, Peters A, Ladwig KH. What prevents old people living alone from feeling lonely? Findings from the KORA-age-study. Aging Ment Health. (2015) 19:773–80. 10.1080/13607863.2014977769 [DOI] [PubMed] [Google Scholar]
- 51.Beutel ME, Klein EM, Brähler E, Reiner I, Jünger C, Michal M, et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. (2017) 17:97. 10.1186/s12888-017-1262-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goltz A, Janowitz D, Hannemann A, Nauck M, Hoffmann J, Seyfart T, et al. Association of brain-derived neurotrophic factor and vitamin D with depression and obesity: a population-based study. Neuropsychobiology. (2017) 76:171–81. 10.1159/000489864 [DOI] [PubMed] [Google Scholar]
- 53.Rose DM, Seidler A, Nubling M, Latza U, Brahler E, Klein EM, et al. Associations of fatigue to work-related stress, mental and physical health in an employed community sample. BMC Psychiatry. (2017) 17:167 10.1186/s12888-017-1237-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Atasoy S, Johar H, Fang X, Kruse J, Ladwig K. Cumulative effect of depressed mood and obesity on type II diabetes incidence: findings from the MONICA/KORA cohort study. J Psychosom Res. (2018) 115:66–70. 10.1016/j.jpsychores.2018.10007 [DOI] [PubMed] [Google Scholar]
- 55.Beutel ME, Brähler E, Wiltink J, Kerahrodi JG, Burghardt J, Michal M, et al. New onset of depression in aging women and men: contributions of social, psychological, behavioral, and somatic predictors in the community. Psychol Med. (2019) 49:1148–55. 10.1017/S0033291718001848 [DOI] [PubMed] [Google Scholar]
- 56.König J, Block A, Becker M, Fenske K, Hertel J, Van der Auwera S, et al. Assessment of subjective emotional valence and long-lasting impact of life events: development and psychometrics of the Stralsund Life Event List (SEL). BMC Psychiatry. (2018) 18:105. 10.1186/s12888-018-1649-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Beutel ME, Wiltink J, Ghaemi Kerahrodi J, Tibubos AN, Brahler E, Schulz A, et al. Somatic symptom load in men and women from middle to high age in the Gutenberg health study - association with psychosocial and somatic factors. Sci Rep. (2019) 9:4610. 10.1038/s41598-019-40709-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schlax J, Jünger C, Beutel ME, Münzel T, Pfeiffer N, Wild PS, et al. Income and education predict elevated depressive symptoms in the general population: results from the Gutenberg health study. BMC Public Health. (2019) 19:430. 10.1186/s12889-019-6730-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Grabe HJ, Lange M, Wolff B, Volzke H, Lucht M, Freyberger HJ, et al. Mental and physical distress is modulated by a polymorphism in the 5-HT transporter gene interacting with social stressors and chronic disease burden. Mol Psychiatry. (2005) 10:220–4. 10.1038/sj.mp4001555 [DOI] [PubMed] [Google Scholar]
- 60.von Lengerke T, Janssen C, John J, Group KS. Sense of coherence, health locus of control, and quality of life in obese adults: physical limitations and psychological normalcies. Int J Public Health. (2007) 52:16–26. 10.1007/s00038-006-5038-1 [DOI] [PubMed] [Google Scholar]
- 61.Grabe HJ, Schwahn C, Völzke H, Spitzer C, Freyberger HJ, John U, et al. Tooth loss and cognitive impairment. J Clin Periodontol. (2009) 36:550–7. 10.1111/j.1600-051X.2009.01426x [DOI] [PubMed] [Google Scholar]
- 62.Lucht MJ, Barnow S, Sonnenfeld C, Rosenberger A, Grabe HJ, Schroeder W, et al. Associations between the oxytocin receptor gene (OXTR) and affect, loneliness and intelligence in normal subjects. Prog Neuropsychopharmacol Biol Psychiatry. (2009) 33:860–6. 10.1016/j.pnpbp.2009.04004 [DOI] [PubMed] [Google Scholar]
- 63.Wiczinski E, Doring A, John J, von Lengerke T, Group KS. Obesity and health-related quality of life: does social support moderate existing associations? Br J Health Psychol. (2009) 14:717–34. 10.1348/135910708X401867 [DOI] [PubMed] [Google Scholar]
- 64.Grabe HJ, Schwahn C, Appel K, Mahler J, Schulz A, Spitzer C, et al. Childhood maltreatment, the corticotropin-releasing hormone receptor gene and adult depression in the general population. Am J Med Genet B Neuropsychiatr Genet. (2010) 153B:1483–93. 10.1002/ajmg.b31131 [DOI] [PubMed] [Google Scholar]
- 65.Ladwig KH, Klupsch D, Meisinger C, Baumert J, Erazo N, Schneider A, et al. Gender differences in risk assessment of death wishes and suicidal ideation in the community: results from the KORA augsburg F3 study with 3079 men and women, 35 to 84 years of age. J Nerv Ment Dis. (2010) 198:52–8. 10.1097/NMD0b013e3181c81f92 [DOI] [PubMed] [Google Scholar]
- 66.Ladwig KH., Marten-Mittag B, Lacruz ME, Henningsen P, Creed F, Investigators MK. Screening for multiple somatic complaints in a population-based survey: does excessive symptom reporting capture the concept of somatic symptom disorders? Findings from the MONICA-KORA cohort study. J Psychosom Res. (2010) 68:427–37. 10.1016/j.jpsychores.2010.01009 [DOI] [PubMed] [Google Scholar]
- 67.Grabe H, Schwahn C, Appel K, Mahler J, Schulz A, Spitzer C, et al. Update on the 2005 paper: moderation of mental and physical distress by polymorphisms in the 5-HT transporter gene by interacting with social stressors and chronic disease burden. Mol Psychiatry. (2011) 16:354. 10.1038/mp.201045 [DOI] [PubMed] [Google Scholar]
- 68.Häfner S, Emeny R, Lacruz M, Baumert J, Herder C, Koenig W, et al. Association between social isolation and inflammatory markers in depressed and non-depressed individuals: results from the MONICA/KORA study. Brain Behav Immun. (2011) 25:1701–7. 10.1016/j.bbi.2011.06017 [DOI] [PubMed] [Google Scholar]
- 69.Häfner S, Zierer A, Emeny RT, Thorand B, Herder C, Koenig W, et al. Social 737 isolation and depressed mood are associated with elevated serum leptin levels in men but not 738 in women. Psychoneuroendocrinology. (2011). 36(2):200–209. 10.1016/j.psyneuen.2010.07.009 [DOI] [PubMed] [Google Scholar]
- 70.Schunk M, Reitmeir P, Schipf S, Völzke H, Meisinger C, Thorand B, et al. Health-related quality of life in subjects with and without Type 2 diabetes: pooled analysis of five population-based surveys in Germany. Diabet Med. (2012) 29:646–53. 10.1111/j.1464-5491.2011.03465x [DOI] [PubMed] [Google Scholar]
- 71.Lukaschek K, Kruse J, Emeny RT, Lacruz ME, von Eisenhart Rothe A, Ladwig K-H. Lifetime traumatic experiences and their impact on PTSD: a general population study. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:525–32. 10.1007/s00127-012-0585-7 [DOI] [PubMed] [Google Scholar]
- 72.Schomerus G, Appel K, Meffert PJ, Luppa M, Andersen RM, Grabe HJ, et al. Personality-related factors as predictors of help-seeking for depression: a population-based study applying the behavioral model of health services use. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:1809–17. 10.1007/s00127-012-0643-1 [DOI] [PubMed] [Google Scholar]
- 73.Wiltink J, Michal M, Wild PS, Zwiener I, Blettner M, Münzel T, et al. Associations between depression and different measures of obesity (BMI, WC, WHtR, WHR). BMC Psychiatry. (2013) 13:223 10.1186/1471-244X-13-223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Emeny R, Bidlingmaier M, Lacruz M, Linkohr B, Peters A, Reincke M, et al. Mind over hormones; sex differences in associations of well-being with IGF-I, IGFBP-3 and physical activity in the KORA-age study. Exp Gerontol. (2014) 59:58–64. 10.1016/j.exger.2014.08001 [DOI] [PubMed] [Google Scholar]
- 75.Hunger M, Holle R, Meisinger C, Rathmann W, Peters A, Schunk M. Longitudinal changes in health-related quality of life in normal glucose tolerance, prediabetes and type 2 diabetes: results from the KORA S4/F4 cohort study. Qual Life Res. (2014) 23:2515–20. 10.1007/s11136-014-0689-5 [DOI] [PubMed] [Google Scholar]
- 76.Klug G, Lacruz ME, Emeny RT, Häfner S, Ladwig K-H, Huber D. Aging without depression: a cross-sectional study. Psychodynamic Psychiatry. (2014) 42:5–22. 10.1521/pdps.2014.42.15 [DOI] [PubMed] [Google Scholar]
- 77.Laxy M, Holle R, Doring A, Peters A, Hunger M. The longitudinal association between weight change and health-related quality of life: the KORA S4/F4 cohort study. Int J Public Health. (2014) 59:279–88. 10.1007/s00038-013-0506-x [DOI] [PubMed] [Google Scholar]
- 78.Sievers C, Auer MK, Klotsche J, Athanasoulia AP, Schneider HJ, Nauck M, et al. IGF-I levels and depressive disorders: results from the Study of Health in Pomerania (SHIP). Eur Neuropsychopharmacol. (2014) 24:890–6. 10.1016/j.euroneuro.2014.01008 [DOI] [PubMed] [Google Scholar]
- 79.Baumeister SE, Schomerus G, Schmidt C-O, Möckel F, van den Berg N, Hoffmann W, et al. Change in depressive symptoms and mental health-related quality of life in northeast Germany between 1997–2001 and 2008–2012. Int J Public Health. (2015) 60:33–9. 10.1007/s00038-014-0632-0 [DOI] [PubMed] [Google Scholar]
- 80.Johar H, Emeny RT, Bidlingmaier M, Lacruz ME, Reincke M, Peters A, et al. Lower morning to evening cortisol ratio is associated with cognitive impairment in men but not women: an analysis of 733 older subjects of the cross-sectional KORA-Age study. Psychoneuroendocrinology. (2015) 51:296–306. 10.1016/j.psyneuen.2014.10011 [DOI] [PubMed] [Google Scholar]
- 81.Schunk M, Reitmeir P, Schipf S, Völzke H, Meisinger C, Ladwig KH, et al. Health-related quality of life in women and men with type 2 diabetes: a comparison across treatment groups. J Diabetes Complications. (2015) 29:203–11. 10.1016/j.jdiacomp.2014.11010 [DOI] [PubMed] [Google Scholar]
- 82.Lukaschek K, Vanajan A, Johar H, Weiland N, Ladwig KH. “In the mood for ageing”: determinants of subjective well-being in older men and women of the population-based KORA-Age study. BMC Geriatr. (2017) 17:126. 10.1186/s12877-017-0513-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rabel M, Meisinger C, Peters A, Holle R, Laxy M. The longitudinal association between change in physical activity, weight, and health-related quality of life: results from the population-based KORA S4/F4/FF4 cohort study. PLoS ONE. (2017) 12:e0185205. 10.1371/journal.pone0185205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Johar H, Atasoy S, Bidlingmaier M, Henningsen P, Ladwig K-H. Married but lonely. Impact of poor marital quality on diurnal cortisol patterns in older people. Findings from the cross-sectional KORA-age study. Stress. (2020) 31:1–8. 10.1080/10253890.20201741544 [DOI] [PubMed] [Google Scholar]
- 85.Wacker ME, Hunger M, Karrasch S, Heinrich J, Peters A, Schulz H, et al. Health-related quality of life and chronic obstructive pulmonary disease in early stages – longitudinal results from the population-based KORA cohort in a working age population. BMC Pulm Med. (2014) 14:134. 10.1186/1471-2466-14-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Asselmann E, Beesdo-Baum K, Hamm A, Schmidt C, Hertel J, Grabe H, et al. Lifetime and 12-month prevalence estimates for mental disorders in northeastern Germany: findings from the Study of Health in Pomerania. Eur Arch Psychiatry Clin Neurosci. (2019) 269:341–50. 10.1007/s00406-018-0911-5 [DOI] [PubMed] [Google Scholar]
- 87.Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. (2018) 8:2861. 10.1038/s41598-018-21243-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Asher M, Asnaani A, Aderka IM. Gender differences in social anxiety disorder: a review. Clin Psychol Rev. (2017) 56:1–12. 10.1016/j.cpr.2017.05004 [DOI] [PubMed] [Google Scholar]
- 89.Cano-Montalbán I, Quevedo-Blasco R. Sociodemographic variables most associated with suicidal behaviour and suicide methods in Europe and America. A systematic review. Eur J Psychol Apll Legal Context. (2018) 10:15–25. 10.5093/ejpalc2018a2 [DOI] [Google Scholar]
- 90.Bryant RA. Post-traumatic stress disorder: a state-of-the-art review of evidence and challenges. World Psychiatry. (2019) 18:259–69. 10.1002/wps20656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Steinbrecher N, Koerber S, Frieser D, Hiller W. The prevalence of medically unexplained symptoms in primary care. Psychosomatics. (2011) 52:263–71. 10.1016/j.psym.2011.01007 [DOI] [PubMed] [Google Scholar]
- 92.Ranjith G. Epidemiology of chronic fatigue syndrome. Occup Med. (2005) 55:13–9. 10.1093/occmed/kqi012 [DOI] [PubMed] [Google Scholar]
- 93.Meng H, Hale L, Friedberg F. Prevalence and predictors of fatigue in middle-aged and older adults: evidence from the health and retirement study. J Am Geriatr Soc. (2010) 58:2033–4. 10.1111/j.1532-5415.2010.03088x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ferreira-Alves J, Magalhães P, Viola L, Simoes R. Loneliness in middle and old age: demographics, perceived health, and social satisfaction as predictors. Arch Gerontol Geriatr. (2014) 59:613–23. 10.1016/j.archger.2014.06010 [DOI] [PubMed] [Google Scholar]
- 95.Vozikaki M, Papadaki A, Linardakis M, Philalithis A. Loneliness among older European adults: results from the survey of health, aging and retirement in Europe. J Public Health. (2018) 26:613–24. 10.1007/s10389-018-0916-6 [DOI] [Google Scholar]
- 96.Hansen T, Slagsvold B. Late-life loneliness in 11 European countries: results from the generations and gender survey. Soc Indic Res. (2016) 129:445–64. 10.1007/s11205-015-1111-6 [DOI] [Google Scholar]
- 97.Mauvais-Jarvis F, Bairey Merz N, Barnes PJ, Brinton RD, Carrero J-J, DeMeo DL, et al. Sex and gender: modifiers of health, disease, and medicine. Lancet. (2020) 396:565–82. 10.1016/S0140-6736(20)31561-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Salk R, Hyde J, Abramson L. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. PsyB. (2017) 143:783–822. 10.1037/bul0000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Acciai F, Hardy M. Depression in later life: a closer look at the gender gap. Soc Sci Res. (2017) 68:163–75. 10.1016/j.ssresearch.2017.08003 [DOI] [PubMed] [Google Scholar]
- 100.Krumm S, Checchia C, Koesters M, Kilian R, Becker T. Men's views on depression: a systematic review and metasynthesis of qualitative research. Psychopathology. (2017) 50:107–24. 10.1159/000455256 [DOI] [PubMed] [Google Scholar]
- 101.Seidler ZE, Dawes AJ, Rice SM, Oliffe JL, Dhillon HM. The role of masculinity in men's help-seeking for depression: a systematic review. Clin Psychol Rev. (2016) 49:106–18. 10.1016/j.cpr.2016.09002 [DOI] [PubMed] [Google Scholar]
- 102.Winkler D, Pjrek E, Kasper S. Anger attacks in depression – evidence for a male depressive syndrome. Psychother Psychosom. (2005) 74:303–7. 10.1159/000086321 [DOI] [PubMed] [Google Scholar]
- 103.Wålinder J, Rutz W. Male depression and suicide. Int Clin Psychopharmacol. (2001) 16:S21–24. 10.1097/00004850-200103002-00004 [DOI] [PubMed] [Google Scholar]
- 104.Möller Leimkühler AM, Heller J, Paulus NC. Subjective well-being and “male depression” in male adolescents. J Affect Disord. (2007) 98:65–72. 10.1016/j.jad.2006.07007 [DOI] [PubMed] [Google Scholar]
- 105.Walther A, Rice T, Kufert Y, Ehlert U. Neuroendocrinology of a male-specific pattern for depression linked to alcohol use disorder and suicidal behavior. Front Psychiatry. (2017) 7:206. 10.3389/fpsyt.201600206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Angst J, Gamma A, Gastpar M, Lépine JP, Mendlewicz J, Tylee A. Gender differences in depression. Eur Arch Psychiatry Clin Neurosci. (2002) 252:201–9. 10.1007/s00406-002-0381-6 [DOI] [PubMed] [Google Scholar]
- 107.Loret de Mola C, Carpena MX, Gonçalves H, Quevedo LA, Pinheiro R, dos Santos Motta JV, et al. How sex differences in schooling and income contribute to sex differences in depression, anxiety and common mental disorders: the mental health sex-gap in a birth cohort from Brazil. J Affect Disord. (2020) 274:977–85. 10.1016/j.jad.2020.05033 [DOI] [PubMed] [Google Scholar]
- 108.Marshal MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J, et al. Suicidality and depression disparities between sexual minority and heterosexual youth: a meta-analytic review. J Adolesc Health. (2011) 49:115–23. 10.1016/j.jadohealth.2011.02005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Miranda-Mendizábal A, Castellví P, Parés-Badell O, Almenara J, Alonso I, Blasco MJ, et al. Sexual orientation and suicidal behaviour in adolescents and young adults: systematic review and meta-analysis. Br J Psychiatry. (2017) 211:77–87. 10.1192/bjp.bp.116196345 [DOI] [PubMed] [Google Scholar]
- 110.Robinson BA. Heteronormativity and homonormativity. In: Wong A, Wickramasinghe M, hoogland R, Naples NA. editors. The Wiley Blackwell Encyclopedia of Gender and Sexuality Studies. Chicester: John Wiley and Sons Ltd; (2016). p. 1–3. 10.1002/9781118663219wbegss013 [DOI] [Google Scholar]
- 111.Wagenknecht P. Was ist heteronormativität? zu geschichte und gehalt des begriffs. In: Hartmann J, Klesse C, Wagenknecht P, Fritzsche B, Hackmann K. editors. Heteronormativität: Empirische Studien zu Geschlecht, Sexualität und Macht. Wiesbaden: VS Verlag für Sozialwissenschaften; (2007). p. 17–34. 10.1007/978-3-531-90274-6_2 [DOI] [Google Scholar]
- 112.Nowatzki N, Grant KR. Sex is not enough: the need for gender-based analysis in health research. Health Care Women Int. (2011) 32:263–77. 10.1080/07399332.2010519838 [DOI] [PubMed] [Google Scholar]