Abstract
Purpose of Review
In current review, we evaluate the current literature examining the role of disgust in eating disorders (EDs), and provide a theoretical model designed to inform the study and treatment of disgust-based symptoms in EDs.
Recent Findings
Findings from this review suggest that aberrant disgust-conditioning processes represent promising but understudied mechanisms that may contribute to the risk and maintenance of core eating disorder (ED) psychopathology. In addition, preliminary evidence supports the use of interventions designed to target aversive disgust cues and disrupt maladaptive disgust-based conditioning that may maintain eating pathology. However, experimental studies designed to elucidate the role of disgust and aversive learning processes remain limited.
Summary
Disgust is a promising risk and maintenance factor in EDs. Future systematic investigation is needed to examine disgust-based processes at a mechanistic level in order to better understand the links between disgust, avoidance behaviors, and EDs. Further investigation of the mechanistic role of disgust in EDs is warranted.
Keywords: Anxiety, Aversive threat conditioning, Disgust, Eating disorders, Extinction
Introduction
Eating disorders (EDs), including anorexia nervosa (AN), bulimia nervosa (BN), avoidant/restrictive food intake disorder (ARFID), and binge eating disorder (BED), are characterized by elevated rates of mortality [1], medical complications [2], and decreased quality of life [3]. The processes underlying ED symptoms remain poorly understood and data indicates that current first-line treatments result in remission for only 60% of patients [4, 5]. Given the need for effective interventions, it is critical that research and clinical efforts aim to better identify and characterize key factors underlying core ED psychopathology.
A growing body of work suggests that alterations in aversive learning processes (i.e., fear and disgust conditioning) represent candidate risk and maintenance processes for avoidance-based ED symptoms (e.g., food avoidance, caloric restriction, compensatory behaviors) [6–10]. Observations that EDs, anxiety disorders, and anxiety-related disorders often co-occur [11, 12] prompted interest in these learning processes, which traditionally have been implicated in anxiety disorders [13–15]. EDs and anxiety disorders also share chief clinical features (e.g., elevations in anxiety and avoidance behaviors) [16] and secondary clinical characteristics (e.g., intolerance of uncertainty, threat-cue attentional biases) [17–20]. Accordingly, drawing from research in anxiety [13, 15], researchers have begun to explore the relevance of conditioning processes to EDs. The majority of this work has focused on acute-threat (fear) and future-threat (anxiety) relevant paradigms and constructs [7–10]. However, emerging evidence suggests that disgust, another threat-related emotion, may contribute to pervasive and persistent aversive conditioning processes and avoidance behaviors [14, 21, 22].
Research implicates a distinct role for disgust in understanding and treating anxiety-related disorders [14], and initial data suggests that this may also be the case in EDs [23••, 25••, 26••]. Using fear-based research as a guide, directly exploring the role of disgust in EDs offers one possibility for improving existing theoretical frameworks and increasing treatment effectiveness. In this paper, we review the current literature on the role of disgust and aversive threat-related learning in EDs, and discuss future directions for this domain. Specifically, we (a) outline the main theoretical models of EDs that implicate disgust, (b) review existing experimental and applied work exploring aversive threat-based learning, and (c) present a theoretical model designed to inform clinical efforts and future research directions to clarify the role of disgust in EDs. See Table 1 for definitions and theoretical frameworks central to this review.
Table 1.
Key terms and definitions relevant to the study of aversive conditioning processes in eating disorders
| Key term/construct | Definition |
|---|---|
| Pavlovian (classical) conditioning | A learning procedure wherein informative pairings between a neutral cue (conditioned stimulus; CS+) and a cue that elicits an innate biobehavioral response (unconditioned stimulus; US) result in the formation of an association between the CS+ and the US (CS-US), and subsequently, a conditioned response (CR) to the CS+ when presented independently. Abnormalities in classical conditioning processes are implicated in the development of anxiety disorders [15]. |
| Evaluative conditioning | A form of Pavlovian conditioning in which the affective value (like or dislike) of a stimulus (CS+) changes after it is repeatedly paired with a US that evokes like or dislike, which may occur in the absence of US expectancy [30••]. Evaluative conditioning has been particularly implicated in conditioned disgust [25••]. |
| Instrumental (operant) conditioning | A learning procedure wherein an organism learns associations between a given biobehavioral response and its positive or negative consequences. Within instrumental conditioning (also commonly referred to as “operant conditioning”), responses followed by desirable consequences are more likely to be repeated, and those followed by aversive consequences are more likely to decrease. Instrumental conditioning has been implicated in generation of behavior that functions to avoid or escape aversive outcomes [31]. |
| Acquisition | Acquisition of a conditioned response occurs when the CS+ is repeatedly presented with the US, such that the association between CS+ and US is strengthened over time. |
| Generalization | A phenomenon wherein physiological, cognitive, and behavioral responses to a conditioned threat cue (conditioned stimulus; CS+) that has been paired with an aversive event (unconditioned stimulus, US) extend, or generalize, to stimuli that have never been paired with the US but that resemble the CS+ (e.g., a safe stimulus that is similar in color to a CS+ may evoke US-expectancy, physiological arousal, and behavioral avoidance). |
| Extinction | Extinction of a conditioned response occurs when the CS+ and CS- are both repeatedly presented without the US, such that discrimination between the CS+ and CS-decreases over time. |
| Avoidance response | A behavioral response wherein an organism performs or omits a behavior in order to avoid an impending threatening event. |
| Escape response | A specific behavioral response wherein an organism performs or omits a behavior in order to cancel or interrupt an ongoing threatening event. |
Disgust Conditioning and Avoidance in EDs: a Brief Review of the Literature
Over the past decade, researchers have proposed a central role of aberrant threat-based learning and avoidance behaviors in ED models, with a particular focus on the contribution of fear- and anxiety-specific conditioning processes [7–10, 16, 27, 28]. However, the field has only recently considered the role of disgust in eating pathology [23••, 25••, 26••, 29, 30••]. In the following section, we discuss several novel models and emerging evidence that implicate altered disgust and aversive conditioning processes in the onset and maintenance of ED psychopathology.
Disgust-Based Models of ED Psychopathology
Current etiological models implicate fear and anxiety as key affective factors that contribute to core ED symptoms. For instance, neurobiological models suggest trait anxiety serves as a predisposing factor for ED behaviors, such as chronic restriction, which lead to neurobiological changes that further increase anxiety around food, maintaining food avoidance [27]. Other models suggest that disorder-specific fears (e.g., fear of food, weight gain) present key factors that, via fear conditioning, maintain restrictive eating behaviors in AN [8–20, 27, 28].
Hildebrandt and colleagues’ [29] model of AN was the first to specifically implicate disgust. Given the persistence of food avoidance in AN, the authors posit that disgust conditioning, which appears particularly resistant to extinction [21, 31–35], may play a role through increased interoceptive processing of aversive eating cues [24]. In this model, anxiogenic stimuli related to food or body image increase attentional biases toward threat, which interact with learned associations between food and weight gain to heighten threat appraisal and emotional response (fear, worry, disgust), leading to food avoidance [29]. Therefore, altered disgust conditioning to various ED-related stimuli including food (e.g., forbidden foods, novel foods), aversive interoceptive cues (e.g., bloating, fullness), and shape and weight (e.g., seeing reflection or pictures of oneself) is posited to increase engagement in dietary restriction and other behaviors that function to reduce or avoid disorder-specific disgust in AN. Emerging evidence of altered interoceptive processes in AN [36, 37] and findings supporting the efficacy of targeting theoretically aversive cues via interoceptive exposure for AN [38, 39•] and ARFID [40•] provides initial support for this disgust-based model of restrictive eating pathology.
More recent theoretical work has argued that disgust sensitivity and conditioning may influence the onset and maintenance of selective eating and food avoidance in ARFID, a restrictive ED not characterized by concerns about weight or shape, to help inform more targeted treatment approaches [30••]. Menzel and colleagues [30••] suggest that while avoidance can be motivated by both disgust and fear, these emotions are characterized by distinct cognitive appraisals, physiological responses, and behaviors. Accordingly, research in adults supports that anxiety and disgust provide differential contributions to ARFID classification and picky eating severity [23••]. Critically, a latent disgust factor was more related to the severity of picky eating and ARFID classification than an anxiety factor, and disgust mediated the relationship between anxiety and ARFID classification [23••]. Thus, the association between anxiety and food avoidance in ARFID may be largely driven by disgust, highlighting a critical need for future research in this domain [30••].
Transdiagnostic models of body image disturbances in EDs also implicate disgust as a key emotional state directed toward one’s own body [41•]. Accordingly, body image aversion is posited to motivate individuals to engage in behaviors that reduce or avoid feelings of body dissatisfaction or disgust [42]. Within exposure-based treatment frameworks, body checking and other ED behaviors are hypothesized to function to avoid experiencing disgust or appearing disgusting to one’s self or others [6] and may be effectively targeted using mirror exposure [43].
No formal theories exist that specify the role of disgust in binge-type disorders, including BN or BED. However, early efforts to develop exposure and response prevention protocols for purging behaviors (P-ERP) focused on compensatory behaviors believed to reduce food-specific or eating-induced anxiety [6]. P-ERP was based on the premise that individuals with BN demonstrate difficulties tolerating affective and interoceptive distress experienced following a binge-eating episode, and engage in conditioned behavioral responses that function to reduce distress associated with perceived acute and future threats (e.g., vomiting in response to consuming an aversive food item, purging to reduce anxiety about potential weight gain) [44, 45]. Although not explored in early P-ERP studies, this approach may increase tolerance of aversive interoceptive cues following a binge-eating episode (e.g., fullness, bloating, nausea). Recent work in adults with BED suggests that binge-eating behaviors function to reduce negative affect states [46, 47], and thus may provide initial evidence for the role of instrumental conditioning in the maintenance of symptoms (e.g., reinforcement of associations between binge-eating episodes and mood improvement). However, the exact roles of specific aversive emotion states have yet to be clarified in relation to binge-eating and subsequent compensatory behaviors.
Evidence of Altered Threat Conditioning in EDs
The proposed centrality of disgust to EDs warrants consideration of associative learning or conditioning—a basic process implicated in avoidance behavior in humans and animals [48]—in the etiology and maintenance of EDs. To date, research on associative learning in EDs is limited. However, extensive research from the anxiety-related disorder fields provides foundational knowledge of transdiagnostic conditioning processes that may inform research in EDs. For instance, the validity of Pavlovian conditioning (wherein pairing a neutral cue [conditioned stimulus; CS+] with a cue that elicits an innate biobehavioral response [unconditioned stimulus; US] results in the formation of an association between the CS+ and the US) and instrumental conditioning (wherein an organism learns associations between a chosen biobehavioral response and its consequences) in explaining heightened anxious arousal and behavioral avoidance in anxiety disorders is well documented [15, 49–51]. Lab-based conditioning studies have demonstrated that enhanced acquisition, overgeneralization, and slowed extinction of conditioned fear are characteristic of anxiety disorders [13, 15, 52]. The validity of conditioning models of anxiety disorders is further strengthened by the efficacy of exposure therapy, which targets altered threat-conditioning processes believed to contribute to these disorders [53, 54].
Conditioning models of EDs center on the supposition that eating is susceptible to Pavlovian and instrumental conditioning [9, 10, 29, 55, 56]. Basic conditioning processes have long been considered key drivers of eating behavior, with food and bodily cues serving as conditioned stimuli (CS+) and nutritive, sensory, and affective consequences of eating serving as unconditioned stimuli (US), which inform meal size and frequency [55, 56]. Recently, calls for experimental testing of fear-conditioning models in EDs have proposed enhanced acquisition and slowed extinction of food-threat associations [10], as well as aberrant habit formation around consuming and/or avoiding foods [57]. Behavioral accounts of threat-conditioning ED models suggest that conditioning abnormalities introduce or heighten approach-avoidance conflict around eating behavior, with enjoyment and survival relevance of foods conflicting with anxiogenic expectancies of undesirable weight gain or other aversive outcomes. For instance, one study [58] demonstrated heightened approach-avoidance conflict, resulting in heightened motivational ambivalence, toward food cues in BED compared to controls. In addition, a recent review of lab-based approach-avoidance tasks [59] indicated diminished approach toward food stimuli in AN compared to controls. However, given the lack of research examining the precise role of disgust in EDs, additional research is warranted.
Emerging Evidence for Disgust and Aversive Conditioning in EDs
In contrast to the focus on anxiety and fear conditioning in EDs [7–10], the same attention has not been given to the role of disgust-conditioning processes in the onset and maintenance of ED pathology. Understanding the role of disgust has particular relevance for developing effective ED treatments. For instance, recent research in anxiety disorders suggests that conditioned disgust is particularly resistant to extinction [21, 22, 60] and can persist following habituation of an associated fear response [33]. Even after extensive extinction trials, conditioned disgust responses are only slightly attenuated, signaling that disgust either requires a higher “dose” of extinction or that a qualitatively different process is involved in disgust learning. Ultimately, the “stickiness” of conditioned disgust is concerning, as disgust is frequently elevated and disgust-based avoidance is common among individuals with anxiety-related psychopathologies [31, 61]. Because many ED symptoms can be conceptualized as avoidance behaviors [16], determining the exact manner in which Pavlovian and instrumental disgust-conditioning processes motivate and maintain ED behaviors represents an important research endeavor for enhancing treatment.
Little data exists on the role of disgust conditioning in EDs. Several cross-sectional studies in non-clinical populations support associations between disgust and various aspects of ED pathology, including body image avoidance [62], caloric restriction [25••, 63], and global ED symptoms [64–66]. Disgust is also a better predictor of pathological food avoidance (i.e., ARFID) than of general picky eating [23••]. To date, only two experimental studies have examined disgust conditioning within EDs. In a clinical analogue sample, conditioned disgust to neutral food items was stronger among female participants scoring high on measured ED risk compared to low-risk participants [25••]. Furthermore, self-reported disgust to the CS+ was associated with consumption of comparatively fewer calories 24 h following the study [25••]. Recent evidence also indicates that individuals with AN have more difficulty unlearning disgust associations (evidenced by self-reported disgust and facial electromyography) compared to healthy controls [24]. Altogether, prior findings provide preliminary evidence that aberrant disgust conditioning plays a role in EDs. However, additional work is needed to extend this knowledge in ways that could inform treatment development and optimization.
A Framework for Examining the Role of Disgust in EDs
Despite growing empirical support for the role of disgust in EDs, systematic research clarifying associations between disgust, aversive learning processes, and EDs is still needed. In particular, we believe efforts to elucidate the mechanistic role of disgust-based aversive learning processes represent a fruitful direction for research, given similar work in other areas of psychiatry (e.g., anxiety disorders, obsessive-compulsive disorder [OCD]) [14, 21, 31–33]. To encourage such research, we present a framework designed to inform future efforts to (1) identify key factors that may predispose an individual to developing or maintaining disgust-based ED behaviors, and (2) characterize key disgust-conditioning processes that may contribute to the development or maintenance of avoidance-based ED symptoms (see Fig. 1).
Fig. 1.
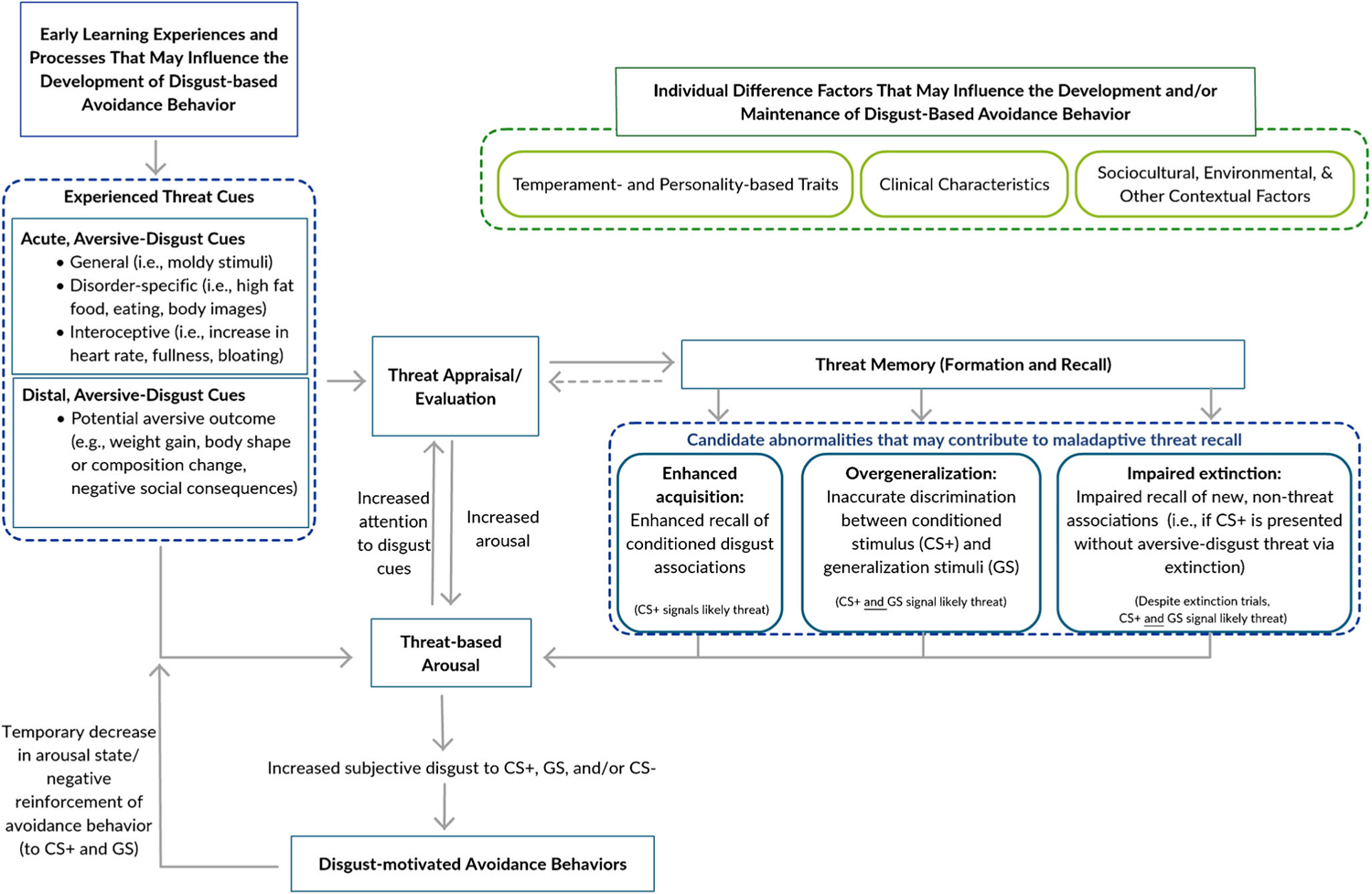
Disgust-based framework for the development and maintenance of maladaptive avoidance behavior in eating disorders
In our framework, we posit that several factors may predispose an individual to developing maladaptive disgust-based avoidance behaviors after an initial aversive learning experience. Adverse childhood events and trauma in particular are associated with elevated threat sensitivity, attention bias toward potential threat cues, and reactivity to perceived threats in adolescence and adulthood [67, 68]. Early trauma may therefore predispose an individual to developing and maintaining a range of maladaptive behaviors in response to aversive threat experiences. Food-specific traumas that result in a violent vomiting episode or gagging while eating may be particularly salient, as these physiological responses are innately paired with disgust. Such early experiences may provide potent, initial, aversive learning experiences that are not easily extinguished or overridden. Early conditioning—particularly evaluative conditioning (e.g., observing someone express disgust toward specific stimuli)—may also increase risk for developing disgust-based associations that maintain avoidance behavior. Furthermore, repeated disgust responses to disorder-relevant threat cues (e.g., body images, specific foods or food characteristics, pre/postprandial physical sensations) may decrease likelihood for extinguishing disgust-based avoidance reactions.
Figure 1 outlines mechanisms that may contribute to the development and maintenance of maladaptive avoidance behaviors, but presently remain poorly understood in EDs. First, we propose that Pavlovian conditioning (see Table 1 for detailed definition) plays a key role in the development and maintenance of EDs, as anecdotal evidence suggests that wide range of disorder-relevant stimuli are often appraised as inherently aversive threats (e.g., food, body stimuli, current or impending sensations such as bloating, fullness). If appraised as aversive, exposure to these stimuli may result in subsequent physiological arousal and increased disgust. Ultimately, experienced disgust may enhance the likelihood for attending to disgust threat cues, and subsequent encoding and recall of Pavlovian stimulus-disgust associations.
In addition, we highlight the role of instrumental conditioning, through which associations between disgust cues (e.g., food, body, internal sensation stimuli) and ED symptoms that function as avoidance behaviors [16] are learned and strengthened. For example, when presented with aversive high-fat food items, individuals with EDs may engage in caloric restriction in an effort to avoid or reduce the experience of disgust. Alternatively, purging behaviors following a meal or in response to postprandial bloating/fullness sensations may function to reduce or avoid the experience of disgust associated with food intake. In both cases, the ED behavior is negatively reinforced and the association between ED behavior engagement and disgust reduction is strengthened, increasing the likelihood for future engagement in these avoidance or escape behaviors when disgust stimuli are presented or perceived. The tendency of conditioned Pavlovian disgust to prompt instrumental avoidance (i.e., Pavlovian-instrumental covariation) is also relevant, as those for whom the experience of disgust strongly motivates avoidance may be at greater risk for developing ED behaviors.
Central to our framework for studying disgust in EDs, we posit that three key candidate abnormalities in disgust-conditioning processes, applicable to both Pavlovian and instrumental conditioning, contribute to avoidance-based ED behaviors following the pairing of a food stimulus or behavior with some aversive outcome. First, individuals with EDs may more readily acquire conditioned disgust responses to food stimuli, as supported by recent evidence suggesting heightened acquisition of conditioned disgust to food stimuli in individuals with restrictive EDs [25••] and heightened anterior insula involvement during food-disgust conditioning [69]. Anecdotal evidence suggests individuals with EDs may exploit this process by intentionally upregulating disgust as a means of pursuing weight loss goals, further heightening aversive arousal toward food cues (e.g., pouring water over food to increase aversion; mentally conceptualizing food as “disgusting”). EDs might also be characterized by impaired discrimination between conditioned disgust-food-cues and “safe” or stimuli with similarities to past conditioned disgust-food-cues, leading to overgeneralization of conditioned fear and disgust toward novel food cues (e.g., disgust in response to and avoidance of an entire category of food), as has been found in other anxiety disorders [70–73]. Although not yet studied in EDs, this proposal is bolstered by initial experimental evidence of maladaptive avoidance prompted by generalization of conditioned disgust [70]. Finally, those with EDs appear to demonstrate slowed extinction of conditioned disgust responses toward foods [24, 25••], which may contribute to sustained aversion toward former threat cues that are now safe.
A breakdown in any or all of these disgust-conditioning processes suggests that alterations in threat memory function, including enhanced encoding and recall of threat memory (e.g., disgust acquisition), impaired ability to recall and discriminate between threat stimuli and non-threat stimuli (e.g., overgeneralization), and impaired recall of new safety learning (e.g., slow extinction of previously conditioned disgust) may contribute to problematic aversion commonly observed in EDs. Whether driven by enhanced acquisition, overgeneralization, or slowed extinction, altered disgust conditioning may increase the likelihood for engaging in more frequent instrumental avoidance behavior in EDs. Growing evidence suggests that the extent of Pavlovian-instrumental covariation for generalized conditioned fear scales with anxiety-related traits [74]. Similarly, in the case that acquisition, generalization, or extinction lead to increased Pavlovian disgust in EDs, this heightened disgust might also be more likely to prompt instrumental avoidance of disgust-eliciting stimuli, such that Pavlovian-instrumental covariance itself contributes to ED maintenance. Thus, in the case that breakdowns in Pavlovian processes lead to increased disgust conditioning in EDs, the resulting persistent avoidance of disgust-eliciting stimuli in itself may contribute to symptom resistance and ED maintenance. Such avoidance would preclude adaptive safety learning, prompting a self-perpetuating cycle of maladaptive avoidance [75] and excessive conditioned disgust responding to food cues.
Other Factors that May Influence Disgust Conditioning in EDs
When clarifying the role of disgust in EDs, future investigations must also consider individual difference factors, including temperament and personality-based characteristics, and broader environmental or sociocultural contextual factors that could further influence the development and maintenance of disgust-related avoidance behaviors in EDs (Fig. 1). For instance, various temperament- and personality-based characteristics associated with anxiety and avoidance-based psychopathologies may also influence risk for developing and maintaining disgust-based ED symptoms. In particular, elevated intolerance of uncertainty [17, 19], threat overestimation [76], threat-related attentional bias [18, 20], cognitive rigidity [77, 78], affect regulation difficulties [79, 80], and anxiety [16, 81] increase the risk for acquisition and maintenance of maladaptive avoidance behavior. EDs are characterized by a somewhat similar profile of heightened threat sensitivity [26••, 82–88], altered interoceptive sensitivity [89–95], and sensory sensitivity [96, 97]. Individuals for whom heightened threat and visceral (e.g., interoceptive) sensitivities co-occur with the typically anxiety-related traits of heightened attention toward disgust cues and over-estimation of threat might be particularly prone to acquiring aversive disgust associations. Similarly, factors such as intolerance of uncertainty (e.g., ambiguous risk of disgust/aversive threat), tendency to attend to aversive threat cues, difficulties shifting attention from threat cues or related thought patterns (e.g., worry, rumination about potential threat), and difficulty regulating aversive emotion states may predispose an individual toward more readily acquiring and difficulties extinguishing problematic disgust-based psychopathology.
Social norms and disgust-based attitudes may also influence the development and maintenance of food- and body-related disgust-driven behaviors. For instance, exposure to and internalization of anti-fat attitudes or weight stigma may predispose the development of disgust reactions to larger bodies via evaluative conditioning (e.g., observing others’ disgust reactions to larger bodies) or specific foods (e.g., hearing a diet commercial associate low-calorie foods with “clean eating”). Given the pervasiveness of “diet culture” and wide-spread endorsement of weight stigma within Western societies [98, 99], it is likely that these social norms and attitudes provide a powerful context in which disgust-based associations between food or body cues and ED behaviors might persist. Future research must clarify the impact that these broader sociocultural factors might have on the development and maintenance of disgust-based ED psychopathology.
The Clinical Utility of Targeting Disgust and Other Clinical Considerations
Our disgust-based framework is intended to provide a starting point for future investigators to explore key processes that may contribute to ED risk and represent crucial treatment targets. Testing and refining the framework proposed here will therefore represent vital steps toward developing novel interventions and optimizing existing exposure-based treatment approaches that target aversive learning processes in EDs [38, 39•, 40•, 100–104]. We propose that, as observed in anxiety disorders and OCD [14], disgust is central to the etiology and maintenance of EDs for a substantial subgroup of ED patients, and that these individuals would glean substantial benefit from interventions targeting disgust. With this in mind, clinicians can consider specifically assessing disgust, including enhanced acquisition, overgeneralization, and/or slowed extinction of conditioned disgust toward disorder-relevant stimuli, in initial case conceptualizations with ED patients. If assessments do reveal a key role of disgust for a given patient, the optimal treatment protocols might involve (1) identification of cues that specifically elicit disgust, (2) tracking of disgust ratings over the course of exposures, in addition to traditional anxiety and distress ratings, and (3) intervention approaches devoted to “deepening” exposure [105] and more sessions than is typical for fear-based interventions, in line with evidence that disgust is resistant to extinction relative to fear [21, 22]. Without disgust-specific adjustments, patients might display illusory gains in treatment if fear declines but disgust is not addressed, increasing the likelihood of relapse; or might be incorrectly classified as resistant to exposure treatment if disgust ratings are assessed and show slow or absent declines. Moreover, if abnormalities in the acquisition, generalization, and extinction of conditioned disgust are identified, this may indicate a need to increase behavioral intervention efforts to deepen extinction through exposure therapy [105, 106] or explore the potential for noninvasive neuromodulation approaches that offer the possibility to biologically enhance new extinction learning when paired with exposure protocols [107, 108].
Efforts to identify traits associated with disgust and aversive learning processes will also provide complementary insight regarding which individuals may be at greatest risk for developing aversion- and avoidance-based ED symptoms. Prior research suggests elevated trait anxiety, anxiety sensitivity, and intolerance of uncertainty influence Pavlovian-instrumental covariation [74, 101, 109–111]. As these traits are common in EDs, clinicians may use this information to identify individuals at greatest risk for developing “sticky” patterns of avoidance behaviors and, subsequently, select and/or adapt treatment plans for these particular patients. For instance, noting that disgust appears more resistant to extinction than other threat emotions [21, 22, 24, 31–33], treatment plans for individuals with elevated disgust-based symptoms may indicate a need to adapt exposure interventions or utilize novel methods (e.g., counter conditioning, adjunctive neuromodulation) that might strengthen treatment effectiveness. Alternatively, if future research reveals exposure treatments ineffective for reducing disgust-based ED symptoms, this may indicate a need to focus on harm reduction and increase functionality and quality of life without directly challenging disgust-based avoidance in EDs.
Future Directions and Controversies
We hope that future research will focus on directly testing proposed relations in the models, particularly those that have yet to be supported by empirical data in ED samples. In undertaking this work, there are several important methodological and conceptual considerations worth noting, outlined below.
Assessment of Anxiety Versus Fear Versus Disgust
Disgust seems to display unique neurophysiological properties which differentiate it from anxiety and fear. Unlike anxiety and fear, disgust is associated with increased parasympathetic nervous system response, as evidenced by robust findings of heart rate deceleration in response to disgust stimuli versus fear stimuli [31, 112, 113]. While disgust shares similar neural correlates with fear (e.g., elevated amygdala activation associated with threat reactivity), some findings indicate that disgust is particularly linked with elevated activation of the anterior insula [114, 115]. This finding may indicate that disgust is comprised of unique interoceptive qualities given the insular cortex involvement in interoceptive processing [116]. Data also suggest specificity with respect to facial expression and cognitive appraisal for disgust and fear. Disgust is strongly linked to activity in the levator labii (facial muscles between the upper lip and outside edge of the nose) [112, 113], and to gustatory sensations and actions, including nausea and food rejection [112]. Finally, disgust is linked to cognitive appraisals of contamination and contagion as opposed to other sources of acute danger that evoke a fear response [112, 113, 117]. However, while it is important to note the differences between fear and disgust and the unique patterns of learning and extinction associated with each, there remains significant overlap in neural substrates and behavioral presentations of fear and disgust [31]. It may be that both fear- and disgust-related associations may operate simultaneously (e.g., feeling scared and disgusted by the potential for significant weight gain). While some work has established unique characteristics of these affective states [31, 112, 113, 117], the clinical or practical relevance of these differences remains understudied.
Diagnostic Differences and Similarities
Our framework attempts to take a transdiagnostic approach to exploring disgust across ED groups; however, most existing work has focused on restrictive EDs (e.g., ARFID, AN). No research to date has explored potential differences in these processes across diagnostic groups. For instance, while ARFID is characterized by food avoidance in a similar manner to other EDs, individuals with ARFID do not endorse the shape and weight concerns that are commonplace for individuals with AN or BN. It is possible that these symptom-specific differences may simply represent differences in the objects/cues that are conditioned (i.e., body fat versus the food itself). Alternatively, it is possible that differences in specific symptom presentations are a result of or influence mechanistic processes implicated in our model (i.e., conditioning, extinction). While prior work has focused on restrictive EDs, similar disgust-conditioning processes may also contribute to the development and maintenance of binge-type EDs, as research suggests that binge-eating episodes are reinforced via reductions in shame, guilt, and disgust [46, 47]. While this is consistent with the role of instrumental conditioning proposed within our framework, additional research is needed to explore the possibility that individuals who engage in binge-eating behaviors may have multiple, competing associations with “binge” food characteristics—some of which may be rewarding (e.g., pleasant taste) and some of which may be aversive (e.g., associated with disgust or self-disgust due to secondary conditioning associating the food with aversive outcomes such as weight gain). This may introduce a complex approach-avoidance conflict, in which consuming a given food could be associated with both rewarding (e.g., food is tasty, associated with social events/connection) and aversive qualities (e.g., food is comprised of fat or other disgust-linked characteristics, may lead to aversive interoceptive sensations, may confer social shame), thus eliciting both approach and avoidance tendencies, simultaneously. For instance, it is possible that binge-eating pathology reflects some dysfunction when navigating eating situations defined by approach-avoidance conflict, with approach tendencies overriding avoidance tendencies in a way that results in binge-eating behaviors. In addition, it may be that when under conditions involving marked negative affect (e.g., disgust, self-disgust), the rewarding biological properties of “binge” foods (e.g., high percentage of fat, sucrose) may become more salient, whereas secondary aversive conditioning (e.g., association between a food and weight gain or later social stigma) is more salient during periods when one’s baseline affective states are more neutral or positive. To our knowledge, approach-avoidance conflict relating to binge-eating pathology has been infrequently studied [58]; this may represent a promising conceptual framework for the interplay of approach tendencies with aversion or disgust before and during binge-eating episodes. Of course, these hypotheses are speculative, and indicate a great need for future research elucidating the role of disgust in binge-eating pathology. Altogether, potential diagnosis-specific differences in disgust-behavior associations represent important considerations for future research.
Clinical Relevance of In-Lab Paradigms
When moving forward with experimental, analogue research exploring aversive conditioning in EDs, researchers must reflect on the clinical relevance of in-lab paradigms and balance rigor and experimental control with external validity in paradigm selection. Work in anxiety disorders has revealed the importance of selecting appropriate cues in experimental paradigms [47], and ongoing work on learning and memory high-lights challenges of translating basic work conducted in animal models to human experiences [118–120]. If the proposed associations in our framework exist, they do so amidst an intricate web of other risk and maintenance processes across levels of analysis (social; psychological; biological); for that reason, we propose that when clinically relevant, researchers incorporate this complexity into their research design and methodological tools.
The Role of Culture
Researchers investigating the role of food- and eating-related disgust in EDs must account for cultural differences in food choices, as cross-cultural research indicates that the perception of food characteristics and subsequent decision to consume certain foods varies based on cultural background and prior exposure [121, 122]. Indeed, individuals may be more likely to perceive a novel food to be potentially disgusting and demonstrate greater refusal to consume it [122]. Investigators must consider the degree to which food avoidance contributes to ED psychopathology, or whether it is merely a reflection of cultural specificity.
Conclusions
The relevance of aversion-based learning processes to EDs remains poorly understood. Existing theoretical models and emerging research suggest that aberrant disgust conditioning and extinction processes may contribute to the risk and maintenance of EDs. Recent findings suggest that exposure-based interventions designed to target aberrant threat-based conditioning and extinction processes yield promising results for individuals with restrictive EDs, including ARFID and AN. However, while these findings are promising, additional research focused on the exact mechanisms through which aversion-based avoidance behaviors (e.g., caloric restriction, food avoidance, or rejection) develop and are maintained across EDs is still needed. To encourage the development of additional research in this area, we propose a model for identifying and understanding disgust-based mechanisms that may promote and maintain problematic avoidance behaviors characteristic of EDs. By highlighting theoretical mechanisms and potential moderators, we hope that this framework will inform the development of effective, targeted treatments for individuals with EDs.
Funding
This research was supported by the National Institute of Mental Health of the National Institutes of Health under award numbers T32MH082761 and K23MH123910. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
This article is part of the Topical Collection on Eating Disorders
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7): 724–31. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2006;19(4):438–43. [DOI] [PubMed] [Google Scholar]
- 3.Winkler LA, Christiansen E, Lichtenstein MB, Hansen NB, Bilenberg N, Støving RK. Quality of life in eating disorders: a meta-analysis. Psychiatry Res. 2014;219(1):1–9. [DOI] [PubMed] [Google Scholar]
- 4.Culbert KM, Racine SE, Klump KL. Research review: what we have learned about the causes of eating disorders-a synthesis of sociocultural, psychological, and biological research. J Child Psychol Psychiatry. 2015;56(11):1141–64. [DOI] [PubMed] [Google Scholar]
- 5.Hay P. A systematic review of evidence for psychological treatments in eating disorders: 2005–2012. Int J Eat Disord. 2013;46(5):462–9. [DOI] [PubMed] [Google Scholar]
- 6.Butler RM, Heimberg RG. Exposure therapy for eating disorders: a systematic review. Clin Psychol Rev. 2020. 10.1016/j.cpr.2020.101851. [DOI] [PubMed] [Google Scholar]
- 7.Cardi V, Leppanen J, Mataix-Cols D, Campbell IC, Treasure J. A case series to investigate food-related fear learning and extinction using in vivo food exposure in anorexia nervosa: a clinical application of the inhibitory learning framework. Eur Eat Disord Rev. 2019;27(2):173–81. [DOI] [PubMed] [Google Scholar]
- 8.Guarda AS, Schreyer CC, Boersma GJ, Tamashiro KL, Moran TH. Anorexia nervosa as a motivated behavior: relevance of anxiety, stress, fear and learning. Physiol Behav. 2015;152:466–72. [DOI] [PubMed] [Google Scholar]
- 9.Murray SB, Strober M, Craske MG, Griffiths S, Levinson CA, Strigo IA. Fear as a translational mechanism in the psychopathology of anorexia nervosa. Neurosci Biobehav Rev. 2018;95:383–95. [DOI] [PubMed] [Google Scholar]
- 10.Strober M. Pathologic fear conditioning and anorexia nervosa: on the search for novel paradigms. Int J Eat Disord. 2004;35(4):504–8. [DOI] [PubMed] [Google Scholar]
- 11.Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev. 2007;15(4): 253–74. [DOI] [PubMed] [Google Scholar]
- 12.Swinbourne J, Hunt C, Abbott M, Russell J, St Clare T, Touyz S. The comorbidity between eating disorders and anxiety disorders: prevalence in an eating disorder sample and anxiety disorder sample. Aust N Z J Psychiatry. 2012;46(2):118–31. [DOI] [PubMed] [Google Scholar]
- 13.Duits P, Cath DC, Lissek S, Hox JJ, Hamm AO, Engelhard IM, et al. Updated meta-analysis of classical fear conditioning in the anxiety disorders. Depress Anxiety. 2015;32(4):239–53. [DOI] [PubMed] [Google Scholar]
- 14.Knowles KA, Jessup SC, Olatunji BO. Disgust in anxiety and obsessive-compulsive disorders: recent findings and future directions. Curr Psychiatry Rep. 2018;20(9):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pittig A, Treanor M, LeBeau RT, Craske MG. The role of associative fear and avoidance learning in anxiety disorders: gaps and directions for future research. Neurosci Biobehav Rev. 2018;88: 117–40. [DOI] [PubMed] [Google Scholar]
- 16.Pallister E, Waller G. Anxiety in the eating disorders: understanding the overlap. Clin Psychol Rev. 2008;28(3):366–86. [DOI] [PubMed] [Google Scholar]
- 17.Brown M, Robinson L, Campione GC, Wuensch K, Hildebrandt T, Micali N. Intolerance of uncertainty in eating disorders: a systematic review and meta-analysis. Eur Eat Disord Rev. 2017;25(5):329–43. [DOI] [PubMed] [Google Scholar]
- 18.Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, Van Ijzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. 2007;133(1):1–24. [DOI] [PubMed] [Google Scholar]
- 19.Carleton RN, Mulvogue MK, Thibodeau MA, McCabe RE, Antony MM, Asmundson GJ. Increasingly certain about uncertainty: intolerance of uncertainty across anxiety and depression. J Anxiety Disord. 2012;26(3):468–79. [DOI] [PubMed] [Google Scholar]
- 20.Smith KE, Mason TB, Lavender JM. Rumination and eating disorder psychopathology: a meta-analysis. Clin Psychol Rev. 2018;61:9–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olatunji BO, Forsyth JP, Cherian A. Evaluative differential conditioning of disgust: a sticky form of relational learning that is resistant to extinction. J Anxiety Disord. 2007;21(6):820–34. 10.1016/j.janxdis.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Engelhard IM, Leer A, Lange E, Olatunji BO. Shaking that icky feeling: effects of extinction and counterconditioning on disgust-related evaluative learning. Behav Ther. 2014;45(5):708–19. 10.1016/j.beth.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 23.••.Harris AA, Romer AL, Hanna EK, et al. The central role of disgust in disorders of food avoidance. Int J Eat Disord. 2019;52(5):543–53. 10.1002/eat.23047 [DOI] [PMC free article] [PubMed] [Google Scholar]; This exploratory, cross-sectional study examined the associations between disgust, anxiety, sensory sensitivity, and picky eating in a large sample of adults (N = 1644); evidence indicates that disgust is more strongly related to severity of ARFID and maladaptive picky eating than anxiety, and that disgust may drive the link between anxiety and food aversion.
- 24.Hildebrandt T, Grotzinger A, Reddan M, Greif R, Levy I, Goodman W, et al. Testing the disgust conditioning theory of food-avoidance in adolescents with recent onset anorexia nervosa. Behav Res Ther. 2015;71:131–8. [DOI] [PubMed] [Google Scholar]
- 25.••.Olatunji BO. Linking Pavlovian disgust conditioning and eating disorder symptoms: an analogue study. Behav Ther. 2020;51(1): 178–89 [DOI] [PubMed] [Google Scholar]; Findings from this clinical analogue study indicate that individuals with elevated eating disorder symptom severity demonstrate enhanced food disgust during a food-disgust conditioning paradigm, and that rate of disgust acquisition was negatively associated with caloric consumption over the 24-h period following disgust conditioning, as compared to individuals with low eating disorder symptoms.
- 26.••.Bell K, Coulthard H, Wildbur D. Self-disgust within eating disordered groups: associations with anxiety, disgust sensitivity and sensory processing. Eur Eat Disord Rev. 2017;25(5):373–80 [DOI] [PubMed] [Google Scholar]; This cross-sectional online survey study assessed self-reported anxiety, disgust sensitivity, disgust propensity, self-disgust, and sensory processing variables among women with eating disorder diagnoses (n = 270 AN, 104 BN) or no eating disorder diagnosis (n = 217); findings suggest that self-disgust is elevated in individuals with eating disorders and is positively associated with altered sensory traits (e.g., sensory sensitivity, sensory avoidance, low responsiveness to sensory cues).
- 27.Kaye WH, Fudge JL, Paulus M. New insights into symptoms and neurocircuit function of anorexia nervosa. Nat Rev Neurosci. 2009;10(8):573–84. [DOI] [PubMed] [Google Scholar]
- 28.Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the application of exposure and response prevention to the treatment of anorexia nervosa. Int J Eat Disord. 2011;44(2):134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hildebrandt T, Bacow T, Markella M, Loeb KL. Anxiety in anorexia nervosa and its management using family-based treatment. Eur Eat Disord Rev. 2012;20(1):e1–e16. [DOI] [PubMed] [Google Scholar]
- 30.••.Menzel JE, Reilly EE, Luo TJ, Kaye WH. Conceptualizing the role of disgust in avoidant/restrictive food intake disorder: implications for the etiology and treatment of selective eating. Int J Eat Disord. 2019;52(4):462–5 [DOI] [PubMed] [Google Scholar]; This manuscript reviews current findings supporting the role of disgust as a central factor for pathological selective eating patterns characteristic of avoidant/restrictive feeding and eating disorder (ARFID), and introduces future clinical and research directions that may inform our understanding of selective eating and food avoidance in ARFID.
- 31.Cisler JM, Olatunji BO, Lohr JM. Disgust, fear, and the anxiety disorders: a critical review. Clin Psychol Rev. 2009;29(1):34–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mason EC, Richardson R. Looking beyond fear: the extinction of other emotions implicated in anxiety disorders. J Anxiety Disord. 2010;24(1):63–70. [DOI] [PubMed] [Google Scholar]
- 33.Olatunji BO, Smits JA, Connolly K, Willems J, Lohr JM. Examination of the decline in fear and disgust during exposure to threat-relevant stimuli in blood-injection-injury phobia. J Anxiety Disord. 2007;21(3):445–55. [DOI] [PubMed] [Google Scholar]
- 34.Olatunji BO, Wolitzky-Taylor KB, Willems J, Lohr JM, Armstrong T. Differential habituation of fear and disgust during repeated exposure to threat-relevant stimuli in contamination-based OCD: an analogue study. J Anxiety Disord. 2009;23(1): 118–23. [DOI] [PubMed] [Google Scholar]
- 35.Smits JA, Telch MJ, Randall PK. An examination ofthe decline in fear and disgust during exposure-based treatment. Behav Res Ther. 2002;40(11):1243–53. [DOI] [PubMed] [Google Scholar]
- 36.Wierenga CE, Bischoff-Grethe A, Berner LA, Simmons AN, Bailer U, Paulus MP, et al. Increased anticipatory brain response to pleasant touch in women remitted from bulimia nervosa. Transl Psychiatry. 2020;10(1):236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khalsa SS, Hassanpour MS, Strober M, Craske MG, Arevian AC, Feusner JD. Interoceptive anxiety and body representation in anorexia nervosa. Front Psychiatry. 2018;9:444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boswell JF, Anderson LM, Oswald JM, Reilly EE, Gorrell S, Anderson DA. A preliminary naturalistic clinical case series study of the feasibility and impact of interoceptive exposure for eating disorders. Behav Res Ther. 2019;117:54–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.•.Plasencia M, Sysko R, Fink K, Hildebrandt T. Applying the disgust conditioning model of food avoidance: a case study of acceptance-based interoceptive exposure. Int J Eat Disord. 2019;52(4):473–7 [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper presents findings from a single case study supporting the initial efficacy of adjunctive interoceptive exposure, a treatment that targets interoceptive aversive disgust cues, in an adolescent with anorexia nervosa.
- 40.•.Brown M, Hildebrandt T. Parent-facilitated behavioral treatment for avoidant/restrictive food intake disorder: a case report. Cogn Behav Pract. 2020;27:231–51 [Google Scholar]; This paper presents findings from a single case report examining a novel behavioral intervention that utilizes a counter-conditioning approach to target anxiety- and disgust-based food avoidance behaviors in youth with avoidant/restrictive food intake disorder.
- 41.•.Stasik-O’Brien SM, Schmidt J. The role of disgust in body image disturbance: incremental predictive power of self-disgust. Body Image. 2018;27:128–37 [DOI] [PubMed] [Google Scholar]; Findings from this study suggest that self-disgust may be a particularly important predictor of body image disturbances, above and beyond global negative affect, anxiety sensitivity, disgust propensity, and disgust sensitivity.
- 42.Shafran R, Fairburn CG, Robinson P, Lask B. Body checking and its avoidance in eating disorders. Int J Eat Disord. 2004;35(1):93–101. [DOI] [PubMed] [Google Scholar]
- 43.Griffen TC, Naumann E, Hildebrandt T. Mirror exposure therapy for body image disturbances and eating disorders: a review. Clin Psychol Rev. 2018;65:163–74. [DOI] [PubMed] [Google Scholar]
- 44.Johnson WG, Schlundt DG, Jarrell MP. Exposure with response prevention, training in energy balance, and problem solving therapy for bulimia nervosa. Int J Eat Disord. 1988;5(1):35–45. [Google Scholar]
- 45.Rosen JC, Litenberg H. The anxiety model of bulimia nervosa and treatment with exposure plus response prevention In: The psychobiology of bulimia nervosa. Berlin: Springer; 1988. p. 146–51. [Google Scholar]
- 46.Berg KC, Crosby RD, Cao L, Peterson CB, Engel SG, Mitchell JE, et al. Facets of negative affect prior to and following binge-only, purge-only, and binge/purge events in women with bulimia nervosa. J Abnorm Psychol. 2013;122(1):111–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schaefer LM, Smith KE, Anderson LM, Cao L, Crosby RD, Engel SG, et al. The role of affect in the maintenance of binge-eating disorder: evidence from an ecological momentary assessment study. J Abnorm Psychol. 2020;129(4):387–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Krypotos AM, Effting M, Kindt M, Beckers T. Avoidance learning: a review of theoretical models and recent developments. Front Behav Neurosci. 2015;9:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arnaudova I, Kindt M, Fanselow M, Beckers T. Pathways towards the proliferation of avoidance in anxiety and implications for treatment. Behav Res Ther. 2017;96:3–13. [DOI] [PubMed] [Google Scholar]
- 50.Scheveneels S, Boddez Y, Vervliet B, Hermans D. The validity of laboratory-based treatment research: bridging the gap between fear extinction and exposure treatment. Behav Res Ther. 2016;86:87–94. [DOI] [PubMed] [Google Scholar]
- 51.Vervliet B, Raes F. Criteria of validity in experimental psychopathology: application to models of anxiety and depression. Psychol Med. 2013;43(11):2241–4. [DOI] [PubMed] [Google Scholar]
- 52.Lissek S, Powers AS, McClure EB, et al. Classical fear conditioning in the anxiety disorders: a meta-analysis. Behav Res Ther. 2005;43(11):1391–424. [DOI] [PubMed] [Google Scholar]
- 53.Foa EB, McLean CP. The efficacy of exposure therapy for anxiety-related disorders and its underlying mechanisms: the case of OCD and PTSD. Annu Rev Clin Psychol. 2016;12:1–28. [DOI] [PubMed] [Google Scholar]
- 54.Ougrin D. Efficacy of exposure versus cognitive therapy in anxiety disorders: systematic review and meta-analysis. BMC Psychiatry. 2011;11:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Booth DA. Culturally corralled into food abuse: the eating disorders as physiologically reinforced excessive appetites In: Pirke KM, Vandereycken W, Ploog D, editors. The psychobiology of bulimia nervosa: Springer; 1988;18–32. [Google Scholar]
- 56.Jansen A. A learning model of binge eating: cue reactivity and cue exposure. Behav Res Ther. 1998;36(3):257–72. [DOI] [PubMed] [Google Scholar]
- 57.Steinglass J, Walsh BT. Habit learning and anorexia nervosa: a cognitive neuroscience hypothesis. Int J Eat Disord. 2006;39(4): 267–75. [DOI] [PubMed] [Google Scholar]
- 58.Leehr EJ, Schag K, Brinkmann A, Ehlis AC, Fallgatter AJ, Zipfel S, et al. Alleged approach-avoidance conflict for food stimuli in binge eating disorder. PLoS One. 2016;11(4):e0152271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fricke K, Vogel S. How interindividual differences shape approach-avoidance behavior: relating self-report and diagnostic measures of interindividual differences to behavioral measurements of approach and avoidance. Neurosci Biobehav Rev. 2020;111:30–56. [DOI] [PubMed] [Google Scholar]
- 60.Armstrong T, Olatunji BO. Pavlovian disgust conditioning as a model for contamination-based OCD: evidence from an analogue study. Behav Res Ther. 2017;93:78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Olatunji BO, McKay D. Disgust and its disorders: theory, assessment, and treatment implications. Washington, DC: American Psychological Association; 2009;9–292. [Google Scholar]
- 62.Spreckelsen PV, Glashouwer KA, Bennik EC, Wessel I, de Jong PJ. Negative body image: relationships with heightened disgust propensity, disgust sensitivity, and self-directed disgust. PLoS One. 2018;13(6):e0198532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Houben K, Havermans RC. A delicious fly in the soup. The relationship between disgust, obesity, and restraint. Appetite. 2012;58(3):827–30. [DOI] [PubMed] [Google Scholar]
- 64.Anderson LM, Reilly EE, Thomas JJ, Eddy KT, Franko DL, Hormes JM, et al. Associations among fear, disgust, and eating pathology in undergraduate men and women. Appetite. 2018;125: 445–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Harvey T, Troop NA, Treasure JL, Murphy T. Fear, disgust, and abnormal eating attitudes: a preliminary study. Int J Eat Disord. 2002;32(2):213–8. [DOI] [PubMed] [Google Scholar]
- 66.Troop N, Baker A. Food, body, and soul: the role of disgust in eating disorders In: Olatunji BO, McKay D, editors. Disgust and its disorders: theory, assessment, and treatment implications. Washington, DC: American Psychological Association; 2009. p. 229–51. [Google Scholar]
- 67.McLaughlin KA, Lambert HK. Child trauma exposure and psychopathology: mechanisms of risk and resilience. Curr Opin Psychol. 2017;14:29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McLaughlin KA, DeCross SN, Jovanovic T, Tottenham N. Mechanisms linking childhood adversity with psychopathology: learning as an intervention target. Behav Res Ther. 2019;118: 101–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hildebrandt T (2019) Disgust conditioning as a model for food avoidance among adolescents with low-weight eating disorders. Paper presented at: Association for Behavioral and Cognitive Therapies 53rd Annual Convention; Atlanta, GA. [Google Scholar]
- 70.Berg H, Cooper SE, Ross JP, Lissek S (2019) Generalization of conditioned disgust: individual differences and temporal dynamics. Paper presented at: Association for Behavioral and Cognitive Therapies 53rd Annual Convention; Atlanta, GA. [Google Scholar]
- 71.Kaczkurkin AN, Burton PC, Chazin SM, Manbeck AB, Espensen-Sturges T, Cooper SE, et al. Neural substrates of overgeneralized conditioned fear in PTSD. Am J Psychiatry. 2017;174(2):125–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lissek S, Rabin S, Heller RE, Lukenbaugh D, Geraci M, Pine DS, et al. Overgeneralization of conditioned fear as a pathogenic marker of panic disorder [published correction appears in Am J Psychiatry. 2010 Jan;167(1):106]. Am J Psychiatry. 2010;167(1):47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lissek S, Kaczkurkin AN, Rabin S, Geraci M, Pine DS, Grillon C. Generalized anxiety disorder is associated with overgeneralization of classically conditioned fear. Biol Psychiatry. 2014;75(11):909–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hunt C, Cooper SE, Hartnell MP, Lissek S. Anxiety sensitivity and intolerance of uncertainty facilitate associations between generalized Pavlovian fear and maladaptive avoidance decisions. J Abnorm Psychol. 2019;128(4):315–26. [DOI] [PubMed] [Google Scholar]
- 75.Pittig A, Wong AHK, Glück VM, Boschet JM. Avoidance and its bi-directional relationship with conditioned fear: mechanisms, moderators, and clinical implications. Behav Res Ther. 2020;126:103550. [DOI] [PubMed] [Google Scholar]
- 76.Abramowitz JS, Blakey SM. Overestimation of threat In: Abramowitz JS, Blakey SM, editors. Clinical handbook of fear and anxiety: maintenance processes and treatment mechanisms: American Psychological Association; 2020. p. 7–25. [Google Scholar]
- 77.Ottaviani C, Watson DR, Meeten F, Makovac E, Garfinkel SN, Critchley HD. Neurobiological substrates of cognitive rigidity and autonomic inflexibility in generalized anxiety disorder. Biol Psychol. 2016;119:31–41. [DOI] [PubMed] [Google Scholar]
- 78.Roberts ME, Tchanturia K, Stahl D, Southgate L, Treasure J. A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychol Med. 2007;37(8):1075–84. [DOI] [PubMed] [Google Scholar]
- 79.Prefit AB, Cândea DM, Szentagotai-Tătar A. Emotion regulation across eating pathology: a meta-analysis. Appetite. 2019;143: 104438. [DOI] [PubMed] [Google Scholar]
- 80.Sloan E, Hall K, Moulding R, Bryce S, Mildred H, Staiger PK. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: a systematic review. Clin Psychol Rev. 2017;57:141–63. [DOI] [PubMed] [Google Scholar]
- 81.Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry. 2004;161(12):2215–21. [DOI] [PubMed] [Google Scholar]
- 82.Aharoni R, Hertz MM. Disgust sensitivity and anorexia nervosa. Eur Eat Disord Rev. 2012;20(2):106–10. [DOI] [PubMed] [Google Scholar]
- 83.Anestis MD, Holm-Denoma JM, Gordon KH, Schmidt NB, Joiner TE. The role of anxiety sensitivity in eating pathology. Cogn Ther Res. 2014;32(3):370–85. [Google Scholar]
- 84.Davey GC, Buckland G, Tantow B, Dallos R. Disgust and eating disorders. Eur Eat Disord Rev. 1998;6(3):201–11. [Google Scholar]
- 85.Harrison A, O’Brien N, Lopez C, Treasure J. Sensitivity to reward and punishment in eating disorders. Psychiatry Res. 2010;177(1–2):1–11. [DOI] [PubMed] [Google Scholar]
- 86.Jappe LM, Frank GK, Shott ME, et al. Heightened sensitivity to reward and punishment in anorexia nervosa. Int J Eat Disord. 2011;44(4):317–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Monteleone AM, Cardi V, Volpe U, Fico G, Ruzzi V, Pellegrino F, et al. Attachment and motivational systems: relevance of sensitivity to punishment for eating disorder psychopathology. Psychiatry Res. 2018;260:353–9. [DOI] [PubMed] [Google Scholar]
- 88.Troop NA, Treasure JL, Serpell L. A further exploration of disgust in eating disorders. Eur Eat Disord Rev. 2002;10(3):218–26. [Google Scholar]
- 89.Klabunde M, Acheson DT, Boutelle KN, Matthews SC, Kaye WH. Interoceptive sensitivity deficits in women recovered from bulimia nervosa. Eat Behav. 2013;14(4):488–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jenkinson PM, Taylor L, Laws KR. Self-reported interoceptive deficits in eating disorders: a meta-analysis of studies using the eating disorder inventory. J Psychosom Res. 2018;110:38–45. [DOI] [PubMed] [Google Scholar]
- 91.Brown TA, Berner LA, Jones MD, Reilly EE, Cusack A, Anderson LK, et al. Psychometric evaluation and norms for the Multidimensional Assessment of Interoceptive Awareness (MAIA) in a clinical eating disorders sample. Eur Eat Disord Rev. 2017;25(5):411–6. [DOI] [PubMed] [Google Scholar]
- 92.Khalsa SS, Craske MG, Li W, Vangala S, Strober M, Feusner JD. Altered interoceptive awareness in anorexia nervosa: effects of meal anticipation, consumption and bodily arousal. Int J Eat Disord. 2015;48(7):889–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Berner LA, Simmons AN, Wierenga CE, Bischoff-Grethe A, Paulus MP, Bailer UF, et al. Altered interoceptive activation before, during, and after aversive breathing load in women remitted from anorexia nervosa. Psychol Med. 2018;48(1):142–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.••.Zucker NL, Bulik CM. On bells, saliva, and abdominal pain or discomfort: Early aversive visceral conditioning and vulnerability for anorexia nervosa. Int J Eat Disord. 2020;53(4):508–12 [DOI] [PMC free article] [PubMed] [Google Scholar]; This article briefly reviews emerging evidence for conceptualizing aversive visceral conditioning, early gastrointestinal pain or discomfort, and altered interoceptive processes as key vulnerability factors for later onset and maintenance of anorexia nervosa.
- 95.Berner LA, Simmons AN, Wierenga CE, Bischoff-Grethe A, Paulus MP, Bailer UF, et al. Altered anticipation and processing of aversive interoceptive experience among women remitted from bulimia nervosa. Neuropsychopharmacology. 2019;44(7):1265–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kambanis PE, Kuhnle MC, Wons OB, Jo JH, Keshishian AC, Hauser K, et al. Prevalence and correlates of psychiatric comorbidities in children and adolescents with full and subthreshold avoidant/restrictive food intake disorder. Int J Eat Disord. 2020;53(2):256–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zucker NL, Merwin RM, Bulik CM, Moskovich A, Wildes JE, Groh J. Subjective experience of sensation in anorexia nervosa. Behav Res Ther. 2013;51(6):256–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vartanian LR, Herman CP, Polivy J. Consumption stereotypes and impression management: how you are what you eat. Appetite. 2007;48(3):265–77. [DOI] [PubMed] [Google Scholar]
- 99.Puhl RM, Moss-Racusin CA, Schwartz MB, Brownell KD. Weight stigmatization and bias reduction: perspectives of overweight and obese adults. Health Educ Res. 2008;23(2):347–58. [DOI] [PubMed] [Google Scholar]
- 100.Boswell JF, Anderson LM, Anderson DA. Integration of interoceptive exposure in eating disorder treatment. Clin Psychol Sci Pract. 2015;22(2):194–210. [Google Scholar]
- 101.McIntosh VV, Carter FA, Bulik CM, Frampton CM, Joyce PR. Five-year outcome of cognitive behavioral therapy and exposure with response prevention for bulimia nervosa. Psychol Med. 2011;41(5):1061–71. [DOI] [PubMed] [Google Scholar]
- 102.Steinglass J, Albano AM, Simpson HB, Carpenter K, Schebendach J, Attia E. Fear of food as a treatment target: exposure and response prevention for anorexia nervosa in an open series. Int J Eat Disord. 2012;45(4):615–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Schmidt U, Marks I. Cue exposure to food plus response prevention of binges for bulimia: a pilot study. Int J Eat Disord. 1988;7(5):663–72. [Google Scholar]
- 104.Hildebrandt T. Mirror exposure therapy for body image disturbances and eating disorders: a review. Clin Psychol Rev. 2018;65:163–74. [DOI] [PubMed] [Google Scholar]
- 105.Craske MG, Treanor M, Conway CC, Zbozinek T, Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behav Res Ther. 2014;58:10–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bosman RC, Borg C, de Jong PJ. Optimising extinction of conditioned disgust. PLoS One. 2016;11(2):e0148626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.van’t Wout M, Faucher C, Garnaat S, Philip N, Burwell R. Learning not to avoid: effects of transcranial direct current stimulation on reversal learning In: Neuropsychopharmacology, vol. 44, no. Suppl 1. London: Nature Publishing Group; 2019. p. 87–8. [Google Scholar]
- 108.van’t Wout-Frank M, Shea MT, Larson VC, Greenberg BD, Philip NS. Combined transcranial direct current stimulation with virtual reality exposure for posttraumatic stress disorder: feasibility and pilot results. Brain Stimul. 2019;12(1):41–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Krypotos AM, Engelhard IM. Pavlovian-to-instrumental transfer in subclinical obsessive-compulsive disorder. J Exp Psychopathol. 2020;11(3):2043808720925244. [Google Scholar]
- 110.van Meurs B, Wiggert N, Wicker I, Lissek S. Maladaptive behavioral consequences of conditioned fear-generalization: a pronounced, yet sparsely studied, feature of anxiety pathology. Behav Res Ther. 2014;57:29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Flores A, López FJ, Vervliet B, Cobos PL. Intolerance of uncertainty as a vulnerability factor for excessive and inflexible avoidance behavior. Behav Res Ther. 2018;104:34–43. [DOI] [PubMed] [Google Scholar]
- 112.Olatunji BO, Sawchuk CN. Disgust: characteristic features, social manifestations, and clinical implications. J Soc Clin Psychol. 2005;24(7):932–62. [Google Scholar]
- 113.Whitton AE, Henry JD, Grisham JR. Cognitive and psychophysiological correlates of disgust in obsessive-compulsive disorder. Br J Clin Psychol. 2015;54(1):16–33. [DOI] [PubMed] [Google Scholar]
- 114.Klucken T, Schweckendiek J, Koppe G, Merz CJ, Kagerer S, Walter B, et al. Neural correlates of disgust-and fear-conditioned responses. Neuroscience. 2012;201:209–18. [DOI] [PubMed] [Google Scholar]
- 115.Schweckendiek J, Klucken T, Merz CJ, Kagerer S, Walter B, Vaitl D, et al. Learning to like disgust: neuronal correlates of counterconditioning. Front Hum Neurosci. 2013;7:346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kerr KL, Moseman SE, Avery JA, Bodurka J, Zucker NL, Simmons WK. Altered insula activity during visceral interoception in weight-restored patients with anorexia nervosa. Neuropsychopharmacology. 2016;41 (2):521–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Woody SR, Teachman BA. Intersection of disgust and fear: normative and pathological views. Clin Psychol Sci Pract. 2000;7(3): 291–311. [Google Scholar]
- 118.Lissek S, Pine DS, Grillon C. The strong situation: a potential impediment to studying the psychobiology and pharmacology of anxiety disorders. Biol Psychol. 2006;72(3):265–70. [DOI] [PubMed] [Google Scholar]
- 119.Elsey JW, Kindt M. Breaking boundaries: optimizing reconsolidation-based interventions for strong and old memories. Learn Mem. 2017;24(9):472–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fullana MA, Dunsmoor JE, Schruers KRJ, Savage HS, Bach DR, Harrison BJ. Human fear conditioning: from neuroscience to the clinic. Behav Res Ther. 2020;124:103528. [DOI] [PubMed] [Google Scholar]
- 121.Rozin P. Food and eating In: Kitayama S, Cohen D, editors. Handbook of cultural psychology. New York: The Guilford Press; 2010. p. 391–416. [Google Scholar]
- 122.Martins Y, Pliner P. Human food choices: an examination of the factors underlying acceptance/rejection of novel and familiar animal and nonanimal foods. Appetite. 2005;45(3):214–24. [DOI] [PubMed] [Google Scholar]


