Abstract
Plastic products have played significant roles in protecting people during the COVID-19 pandemic. The widespread use of personal protective gear created a massive disruption in the supply chain and waste disposal system. Millions of discarded single-use plastics (masks, gloves, aprons, and bottles of sanitizers) have been added to the terrestrial environment and could cause a surge in plastics washing up the ocean coastlines and littering the seabed. This paper attempts to assess the environmental footprints of the global plastic wastes generated during COVID-19 and analyze the potential impacts associated with plastic pollution. The amount of plastic wastes generated worldwide since the outbreak is estimated at 1.6 million tonnes/day. We estimate that approximately 3.4 billion single-use facemasks/face shields are discarded daily as a result of COVID-19 pandemic, globally. Our comprehensive data analysis does indicate that COVID-19 will reverse the momentum of years-long global battle to reduce plastic waste pollution. As governments are looking to turbo-charge the economy by supporting businesses weather the pandemic, there is an opportunity to rebuild new industries that can innovate new reusable or non-plastic PPEs. The unanticipated occurrence of a pandemic of this scale has resulted in unmanageable levels of biomedical plastic wastes. This expert insight attempts to raise awareness for the adoption of dynamic waste management strategies targeted at reducing environmental contamination by plastics generated during the COVID-19 pandemic.
Keywords: COVID-19, Single-use plastics, Biomedical plastic waste, Plastic pollution, Effective, Waste management
COVID-19; Single-use plastics; Biomedical plastic waste; Plastic pollution; Effective; waste management
1. Introduction
A range of personal protective equipment (PPE) made from plastics have played crucial roles in protecting people during the COVID-19 pandemic. However, there is a growing concern over the unprecedented increase in single-use plastics (SUPs) including gloves, protective medical suits, masks, handsanitiser bottles, takeout plastics, food and polyethylene goods packages, and medical test kits since the coronavirus pandemic began. The management of wastes arising from SUPs is a troubling upshot of the COVID-19 pandemic which has wrecked the global healthcare systems and disrupted the economies of nations (Benson et al., 2021; Vanapalli et al., 2021; Herron et al., 2020; Silva et al., 2020). Essential municipal services such as waste collection and treatment have been threatened while there is an unprecedented rise in the amount of medical and domestic wastes generated. Data suggest that COVID-19 virus is highly contagious and could remain viable on plastic surfaces for several days (Chin et al., 2020; Doremalen et al., 2020; Nghiem et al., 2020).
Here, we present a framework for estimating the number of facemasks generated daily during COVID-19 pandemic by the global population living in the urban and semi-urban areas. We have also estimated the volume of plastic wastes generated daily, and by the end of 2020. Also, we discuss the impact of COVID-19 pandemic on the consumption and disposability of single-use plastics generated from healthcare facilities, quarantine facilities, home and hotel isolation facilities, and other sources during the management of COVID-19 patients.
1.1. Why are there so many single-use plastics as SARS-CoV-2 spreads?
Since the outbreak of SARS-CoV-2, there has been a surge in the number of discarded single-use surgical and face masks and latex gloves which are seen littering the streets and roads, medical facilities, parking lots, dumpsites, beaches, gutters, and shopping carts. Over the past few months amid the pandemic, the world has witnessed an unprecedented rise in demand for plastic products such as disposable gloves, masks, bottled water, disposable wipes, hand sanitizers, and cleaning agents (Syam, 2020; Nzediegwu and Chang, 2020). In most countries, the government issued lockdown directives, as well as social and physical distancing measures to curb the spread of COVID-19 virus. However, the COVID-19 pandemic has worsened the plastic pollution problem through consumers rejuvenescence for single-use products and materials for health and safety reasons. Shops and supermarkets have seen a widespread practice of using single-use materials to wrap vegetables and fruit because of hygiene reasons.
Moreover, given the government and healthcare providers strategy at preventing the spread of COVID-19 virus, health workers are generally advised not to reuse their personal protective equipment (PPE), implying that tonnes of plastic medical waste are generated daily. More so, most countries, World Health Organisation (WHO), US Centers for Disease Control and Prevention, European Center for Disease Prevention and Control have recommended stringent physical distancing measures, cancellation of mass gatherings, frequent handwashing, and closure of educational institutions to limit the community spread of COVID-19. Besides, almost all countries have recommended and implemented the use of facemasks to reduce the level of human-to-human transmission and protect the most vulnerable and at-risk populations (Aljazeera News, 2020; CDC, 2020a). Therefore, in line with this recommendation and stringent directives, millions of facemasks have been produced, used and discarded daily.
Largely, a lot of single-use PPE used by health workers and the public are being discarded daily. These include masks, gloves, protective aprons, face shields, safety glasses, sanitizer containers, plastics shoes and medical gowns, which are mostly made from non-woven materials including polymeric substances such as polypropylene. Also, gloves are made from several materials, including chloroethene polymers, neoprene, and vinyl. These plastic products could be categorized as macro- and mesoplastics, and can enter the environment through poor waste management or improper discharge into the marine and terrestrial ecosystems (Jeyasanta et al., 2020; Silva et al., 2020).
In general, terrestrial environments are the critical sources for marine plastic debris, which are mainly originated from the anthropogenic emissions. Over the years, our global ocean, seas, and coastal environments have been directly and indirectly riddled with billions of tons of plastic marine debris produced from human-mediated activities (Fred-Ahmadu et al., 2020a; Nghiem et al., 2020). Plastics in our oceans can come from both land-based or marine sources, and are mostly categorized into nanoplastics (particulate size range between 1 – 100 nm), microplastics (MPs) (particulate size range between 1 μm–5 mm), mesoplastics (particulate size range between 2.5 cm–5 mm), and macroplastics (particulate size range >2.5 cm) (Benson and Fred-Ahmadu, 2020; Fred-Ahmadu et al., 2020b; Jeyasanta et al., 2020). Approximately 80% of global ocean plastics arise from land-based sources while about 20% are attributed to marine sources (Li et al., 2016). Recent reports of increased anthropogenic inputs of plastic-sorbed pollutants into the marine environment have significantly resulted in elevated levels of contaminants in recent years (Benson and Fred-Ahmadu, 2020; Liu et al., 2020; Masood et al., 2016). These organic and inorganic contaminants are usually accumulated in surficial and bottom sediments Kane et al. (2020); Sarkar et al. (2019); Zhang et al. (2018).
However, there is a growing concern that discarded surgical masks, medical gowns, face shields, safety glasses, protective aprons, sanitizer containers, plastics shoes, and gloves arising from the current coronavirus pandemic could end up in our aquatic ecosystems. In March 2020, there was an avalanche of COVID-19 cases worldwide and health care facilities around the world were confronted with shortages of gloves, surgical masks, face masks and other PPE. Commonly available and recommended types of PPE include N95 and KN95 respirators and surgical masks, that are designed for maximum filtration of aerosols and infectious airborne particles, to protect the user from respiratory diseases including COVID-19, by filtering infectious airborne particles (Sampol, 2020; US FDA, 2020a).
Notably, the N95 are tightly fitted respirators while the surgical masks are loose-fitting medical masks designed in varied thickness and water percolation abilities. Both types are wearable devices that are meant to be disposed of after a single-use. According to the Centers for Disease Control and Prevention (CDC) recommendation, the respirators, surgical and face masks are labelled as “single-use” disposable medical or respiratory protective devices and should be discarded in a “plastic bag” after use and then dumped in trash (US FDA, 2020a). This recommendation is a necessary measure but could worsen the plastic waste problem as more single-use plastics are added to our environment and the global oceans, especially in situations where the PPEs are not adequately recycled (Scaraboto et al., 2020; US FDA, 2020a). The unprecedented rise in the number of disposable surgical masks and hand gloves can contribute to the plethora of plastic pollution (Boyle, 2020; Chaudhuri, 2020). This could potentially exacerbate the existing plastic pollution challenges created by over 10 million tonnes of plastic that have been estimated to threaten the health of our environments, our global oceans, and the marine organisms (Kane et al., 2020; Jambeck et al., 2015).
1.2. What are the environmental impacts of biomedical plastic wastes?
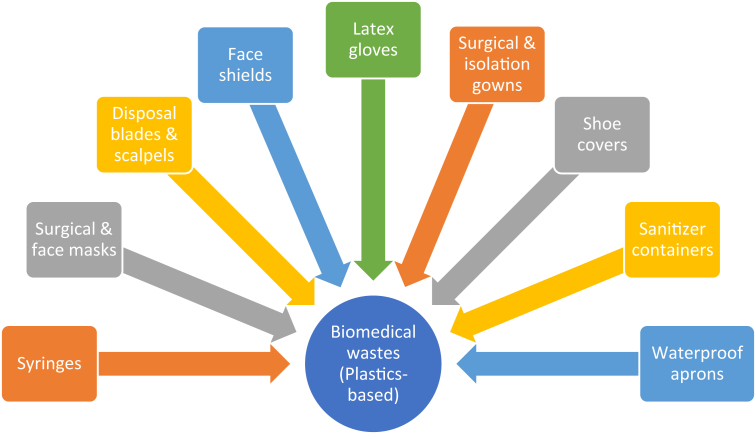
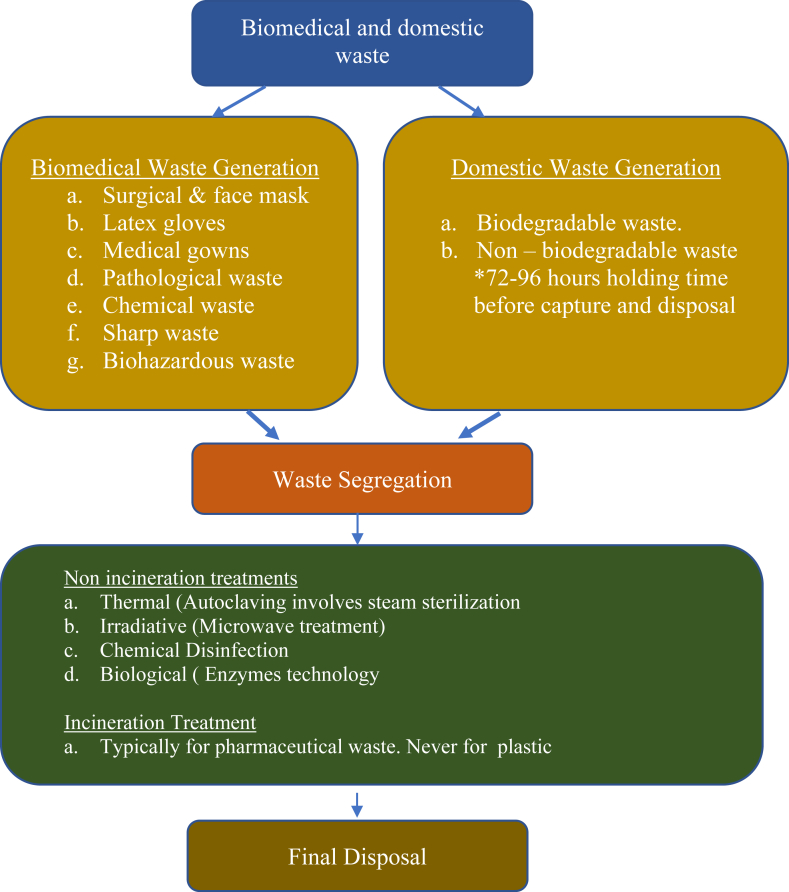
In general, land-based anthropogenic activities such as unregulated disposal of biomedical wastes have been regarded as potential sources of toxic, infectious and radioactive pollutants (WHO, 2018). Typically, healthcare wastes include cytotoxic, chemical, pathological, pharmaceutical, sharp, radioactive, and general wastes. Most of these wastes are made using plastic materials, especially for sharp and general wastes, such as syringes, and scalpels, gloves, surgical masks, surgical and isolation gowns, face shields, shoe covers, sanitizer containers, and waterproof aprons (Figure 1). The COVID-19 pandemic has created more biomedical waste in the form of waste plastics. According to the WHO, on the average, about 0.2 and 0.5 kg/day of hazardous biomedical wastes are generated by low-income and high-income countries, respectively (WHO, 2018). In China where the COVID-19 was first reported, the Emergency Management Office of the Ministry of Ecology and Environment documented a 23% increase in the amount of medical waste generated and treated (Tang, 2020). Thus, China has witnessed an accumulated 142,000 tonnes of medical wastes with the national medical waste treatment capacity increasing from 4902.8 tonnes/day before the SARS-CoV-2 outbreak to the current 6022 tonnes/day.
Figure 1.
Types of plastic based biomedical wastes originated during COVID-19 pandemic.
2. Methods
In this paper, the daily facemasks generated by each country was calculated as a product of the total population of a country and an arbitrary percent of facemask acceptance rate by the urban population (Benson et al., 2021; Nzediegwu and Chang, 2020). The daily and monthly facemask generation were computed as a product of an estimated single facemask use by an individual per day and for thirty days average, respectively. The following model equations were adopted:
| (1) |
| (2) |
where Tp = the estimated population of the country, Up = the percentage of urban population of the country, Ar = the percent face mask acceptance rate, Ac = the average daily face masks per capita. The average number of days in a month per year was estimated as 30 days.
3. Results and discussion
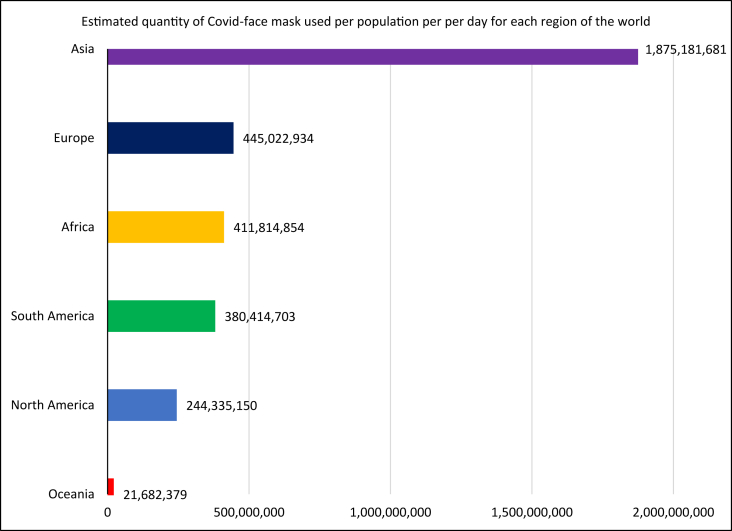
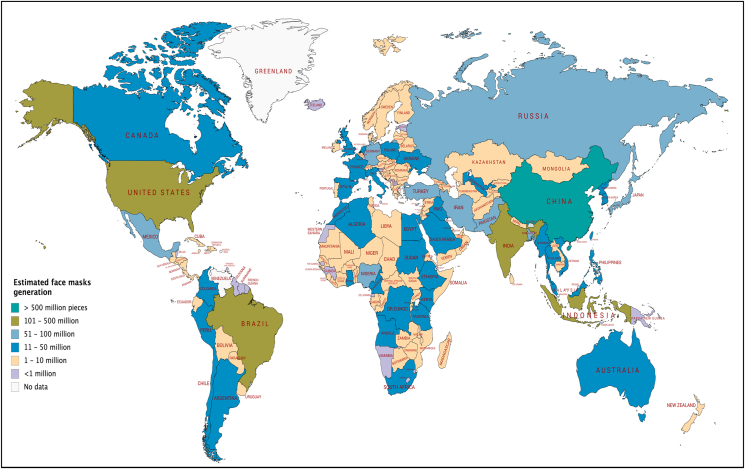
The amount of plastic wastes generated worldwide since the outbreak is estimated at 1.6 million tonnes/day (Table 1). We estimate that approximately 3.4 billion single-use facemasks or face shields are discarded daily as a result of COVID-19 pandemic. China, with the largest population, is estimated to generate nearly 702 million discarded facemasks daily, and could potentially produce approximately 108 million tonnes of plastic wastes by the end of 2020. Our estimate shows that Asia is projected to generate the highest quantity (1.8 billon) of discarded facemasks per capita per day. This is followed by Europe at 445 million, Africa at 411 million, Latin America and the Caribbean at 380 million, North America at 244 million, and Oceania at 22 million facemasks per day (Figures 2 and 3). In view of existing policies and COVID-19 protocols by many countries, the mandatory use of single-use facemasks (face shields) will potentially boost PPE wastes generation. For instance, in China (1.4 billion population), India (1.3 billion population), United States (331 million inhabitants), Brazil (212 million people), Nigeria (206 million population) and United Kingdom (67 million population), it is estimated that the daily facemasks generated if all their citizens wear and discard a facemask or face shield per day, could result in the generation of at least 702, 386, 219, 140, 75, and 45 million of contaminated masks per day. Once the masks are discarded into the environment and are not properly managed, they could be degraded into smaller sized particles which invariably tends to exacerbate the already plastic pollution problems (Fred-Ahmadu et al., 2020a, Fred-Ahmadu et al., 2020b; Patrício Silva et al., 2021; Prata et al., 2020). These discarded PPE could form the bulk of mismanaged wastes that would litter or terrestrial environments and coastal shorelines. In addition, our estimate indicates that by the end of the year 2020, about 585 million tonnes of plastic wastes would be generated by over 7.7 billion people globally, with about 82% of those plastic wastes coming from the top 35 countries listed in Table 2 (Table S1). Notably, most of them are low- and middle-income countries where facilities for effective waste management are not available. This implies that the percentage of mismanaged plastic wastes would likely increase, resulting in disposal in open landfills or uncontrolled dumpsites with a glut of plastic wastes ending up in polluting the waterways, streams, rivers and oceans.
Table 1.
Reported COVID-19 cases, deaths, and estimated total plastic waste generation by region, measured in tonnes.
| Region | Populationa | Total COVID-19 casesb | Total COVID-19 deathsb | Facemask acceptance rate by population (%)c | Average Facemask/capita/day | Estimated daily facemask disposed | Estimated plastic waste generated (Tonnes) | Estimated plastic waste generated per day (Tonnes) |
|---|---|---|---|---|---|---|---|---|
| Africa | 1,340,598,147 | 212,271 | 5,718 | 70 | 1 | 411,814,854 | 100,544,861 | 275,465 |
| Asia | 4,641,054,775 | 1,470,640 | 37,222 | 80 | 1 | 1,875,181,681 | 348,079,108 | 953,641 |
| Europe | 747,636,026 | 2,149,248 | 181,138 | 80 | 1 | 445,022,934 | 56,072,702 | 153,623 |
| South America | 653,952,454 | 1,267,858 | 54,648 | 75 | 1 | 380,414,703 | 49,046,434 | 134,373 |
| North America | 368,869,647 | 2,361,458 | 140,399 | 80 | 1 | 244,335,150 | 27,665,223 | 75,795 |
| Oceania | 42,677,813 | 8,896 | 124 | 75 | 1 | 21,682,379 | 3,200,836 | 8,769 |
| Total | 3,378,451,702 | 584,609,165 | 1,601,666 | |||||
Data retrieved from https://www.worldometers.info/population/on June 02, 2020.
Data retrieved from https://www.worldometers.info/population/on June 11, 2020.
Hypothetical data.
Figure 2.
Estimated daily single-use facemasks (face shields) discarded by each continent.
Figure 3.
Estimated global share of face masks discarded as COVID-waste generated from a given. Country. Map created with mapchart.net©.
Table 2.
Estimated daily COVID-19 facemasks and global plastic waste generation by country prior to management.
| Rank | Country | Populationa | Urban Population (%)a | Facemask acceptance rate by population (%)b | Average facemask per capita per dayb | Estimated daily facemask discarded | Total estimated plastic waste (tonnes) |
|---|---|---|---|---|---|---|---|
| 1 | China | 1,439,323,776 | 61 | 80 | 1 | 702,390,002 | 107,949,283.20 |
| 2 | India | 1,380,004,385 | 35 | 80 | 1 | 386,401,228 | 103,500,328.90 |
| 3 | United States | 331,002,651 | 83 | 80 | 1 | 219,785,760 | 24,825,198.80 |
| 4 | Brazil | 212,559,417 | 88 | 75 | 1 | 140,289,215 | 15,941,956.30 |
| 5 | Indonesia | 273,523,615 | 56 | 80 | 1 | 122,538,579 | 20,514,271.10 |
| 6 | Japan | 126,476,461 | 92 | 80 | 1 | 93,086,675 | 9,485,734.58 |
| 7 | Russia | 145,934,462 | 74 | 80 | 1 | 86,393,201 | 10,945,084.70 |
| 8 | Mexico | 128,932,753 | 84 | 75 | 1 | 81,227,634 | 9,669,956.48 |
| 9 | Nigeria | 206,139,589 | 52 | 70 | 1 | 75,034,810 | 15,460,469.20 |
| 10 | Pakistan | 220,892,340 | 35 | 80 | 1 | 61,849,855 | 16,566,925.50 |
| 11 | Bangladesh | 164,689,383 | 39 | 80 | 1 | 51,383,087 | 12,351,703.70 |
| 12 | Turkey | 84,339,067 | 76 | 80 | 1 | 51,278,153 | 6,325,430.03 |
| 13 | Iran | 83,992,949 | 76 | 80 | 1 | 51,067,713 | 6,299,471.18 |
| 14 | Germany | 83,783,942 | 76 | 80 | 1 | 50,940,637 | 6,283,795.65 |
| 15 | United Kingdom | 67,886,011 | 83 | 80 | 1 | 45,076,311 | 5,091,450.83 |
| 16 | France | 65,273,511 | 82 | 80 | 1 | 42,819,423 | 4,895,513.33 |
| 17 | Philippines | 109,581,078 | 47 | 80 | 1 | 41,202,485 | 8,218,580.85 |
| 18 | South Korea | 51,269,185 | 82 | 80 | 1 | 33,632,585 | 3,845,188.88 |
| 19 | Italy | 60,461,826 | 69 | 80 | 1 | 33,374,928 | 4,534,636.95 |
| 20 | Argentina | 45,195,774 | 93 | 75 | 1 | 31,524,052 | 3,389,683.05 |
| 21 | Egypt | 102,334,404 | 43 | 70 | 1 | 30,802,655 | 7,675,080.30 |
| 22 | Colombia | 50,882,891 | 80 | 75 | 1 | 30,529,735 | 3,816,216.83 |
| 23 | Spain | 46,754,778 | 80 | 80 | 1 | 29,923,058 | 3,506,608.35 |
| 24 | Vietnam | 97,338,579 | 38 | 80 | 1 | 29,590,928 | 7,300,393.43 |
| 25 | DR Congo | 89,561,403 | 46 | 70 | 1 | 28,838,772 | 6,717,105.23 |
| 26 | Thailand | 69,799,978 | 51 | 80 | 1 | 28,478,391 | 5,234,998.35 |
| 27 | South Africa | 59,308,690 | 67 | 70 | 1 | 27,815,775 | 4,448,151.75 |
| 28 | Canada | 37,742,154 | 81 | 80 | 1 | 24,456,916 | 2,830,661.55 |
| 29 | Ukraine | 43,733,762 | 69 | 80 | 1 | 24,141,037 | 3,280,032.15 |
| 30 | Iraq | 40,222,493 | 73 | 80 | 1 | 23,489,935 | 3,016,686.98 |
| 31 | Saudi Arabia | 34,813,871 | 84 | 80 | 1 | 23,394,921 | 2,611,040.33 |
| 32 | Algeria | 43,851,044 | 73 | 70 | 1 | 22,407,883 | 3,288,828.30 |
| 33 | Malaysia | 32,365,999 | 78 | 80 | 1 | 20,196,383 | 2,427,449.93 |
| 34 | Peru | 32,971,854 | 79 | 75 | 1 | 19,535,824 | 2472889.05 |
| 35 | Poland | 37,846,611 | 60 | 80 | 1 | 18,166,373 | 2,838,495.83 |
Data retrieved from https://www.worldometers.info/population/on June 02, 2020.
Hypothetical data.
However, the effective management of medical and domestic wastes is a major challenge, especially in developing countries. Improperly discarded plastic-based wastes and other non-biodegradable synthetic substances are capable of floating around in the environment, accumulating various toxic pollutants and pathogens on their surfaces, which could pose harmful health risks to humans and marine organisms. According to a study by the World Wide Fund for Nature (WWF), if only 1% of the surgical and face masks are improperly discarded into our terrestrial and marine environments, it could potentially lead to unprecedented liitering of our environment by as much as 100 billion masks every month. The implication is that this may result in over 405 Mt of SUPs being added to the already deplorable plastic pollution problem (Syam, 2020). However, this rapid increase in plastic wastes is happening at a time when some recycling programs in many countries are being suspended because of concerns about the virus spreading (Hagemann, 2020). Therefore, COVID-19 pandemic can worsen the global plastic waste problem.
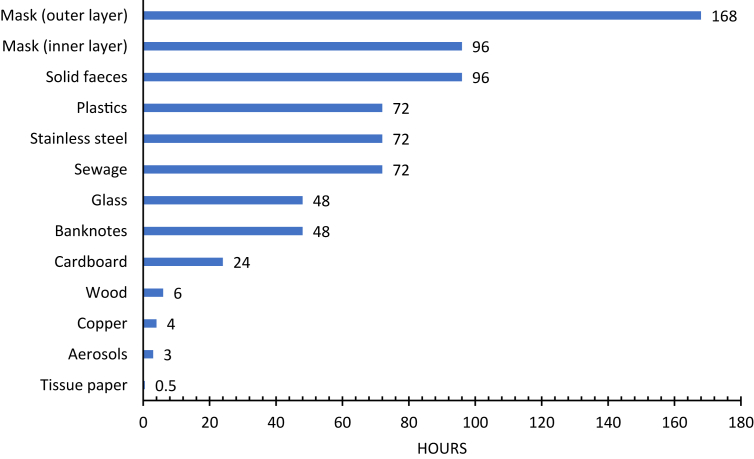
Previous studies have reported that contaminated surfaces or fomites are prime vehicles for the spread of viral diseases (Jones and Gibson, 2020; Park et al., 2015; Vasickova et al., 2010). However, recent studies have reported molecular detection of SARS-CoV-2 in sewage and wastewater samples found in the Netherlands (Lodder and de Roda Husman, 2020; Medema et al., 2020), Australia (Ahmed et al., 2020), and the USA (Wu et al., 2020). The presence of SARS-CoV-2 RNA in untreated wastewaters and sewage was detected as a result of the sorption and stability of coronavirus on surfaces of improperly discharged single-use medical wastes (Chin et al., 2020). Epidemiological data on the surface stability of SARS-CoV-2 and SARS-CoV-1 indicate that once a fomite is contaminated, the infectious viral particles remain viable on a range of surfaces for several minutes and up to several days (Figure 4). According to recent studies, SARS-CoV-2 was found to be more viable and stable for 2–3 days on plastics and stainless-steel surfaces than on cardboard, wood, banknotes and copper (Chin et al., 2020; Doremalen et al., 2020).
Figure 4.
Stability of SARS-CoV-2 on different environmental surfaces. Data sources: Doremalen et al. (2020), Chin et al. (2020).
Overall, these data underscore the standpoint that people may acquire the virus after touching contaminated and improperly discarded plastic-based biomedical wastes. This suggests that the spread and infectivity of SARS-CoV-2 through medical wastes originating from healthcare facilities, home isolation and quarantine facilities where infected patients are receiving treatment may is plausible, and could be a source of infection (Doremalen et al., 2020; Nghiem et al., 2020; Vasickova et al., 2010; Todd et al., 2009). Although the degree of SARS-CoV-2 survival for extended periods on contaminated surfaces and plastics could be a function of other environmental factors (Doremalen et al., 2020). Meanwhile, the potential ecological toxicity of SARS-CoV-2 to marine organisms is not known and would require further studies to understand its environmental risks fully. In addition, the sorption pathway and potential transmission of infectious SARS-CoV-2 virus sorbed onto macro-, meso-, and microplastics has not been documented. However, unintentional exposure could likely impact the health of marine organism and humans in the long term.
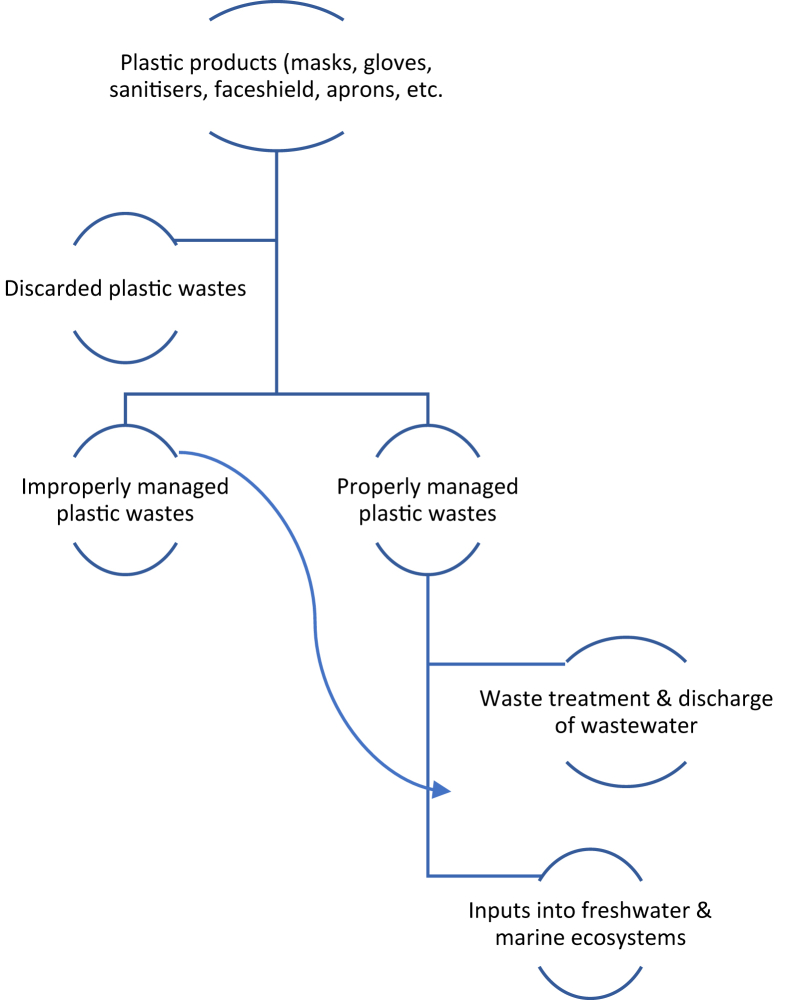
Therefore, there is a need to adequately revise existing waste collection and management procedures to foreclose the potential threat of SARS-CoV-2. Improper management of SARS-CoV-2 generated wastes including littering, disposal in uncontained landfills, and open dumping could compound the existing marine litter's pollution. It has been estimated globally that land-based waste generation is the primary source of plastics to the marine ecosystems (Jambeck et al., 2015). However, untreated terrestrially derived biomedical and domestic wastes can be redistributed into the environment, and transported to the marine systems through runoff and atmospheric deposition. According to a recent report, the fate and distribution of biomedical wastes during and post-SARS-CoV-2 outbreak would require effective waste management strategies including proper identification, collection, segregation, storage, treatment, and disposal as well as adequate awareness and training (BWS Inc, 2018; CDC, 2020b; Klemes et al., 2020; Patil et al., 2015). Figure 5 presents the components and waste treatment options that could be adopted for handling biomedical and domestic wastes in general.
Figure 5.
Components and treatment options for biomedical and domestic plastic wastes generated during SARS-CoV-2 pandemic.
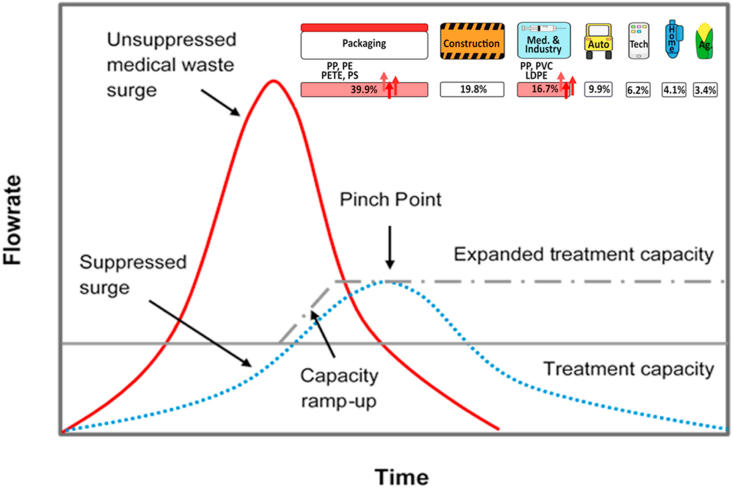
In addition, Figure 6 illustrates the demand and supply chain and identifies different sectors of COVID 19 plastic waste. Amount of waste far exceed the capacity of waste management facilities. There is a serious lack of innovation in deployment of new facilities during emergency time including mobile units to ramp up the capacity. They could also serve as potential vectors of pollutants and pathogens, contributing to a rising threat to ocean life and the terrestrial environment. A proposed chart showing the pathways for inputs of medical wastes (plastics) into freshwater and marine environment is presented in Figure 7. Unlike some other kinds of waste, it takes several years for biomedical plastic wastes to biodegrade, implying that they are capable of littering across the marine ecosystems and terrestrial environment, with far-reaching implications for human health (Geyer et al., 2017; NOAA, 2019).
Figure 6.
Supply and demand chain for medical waste during COVID 19 and relevant sectors for plastic waste generation (adapted from PlasticsEurope and Klemes et al., 2020. Brian Love and Julie Rieland, CC BY-ND).
Figure 7.
Proposed chart showing pathways for inputs of medical wastes (plastics) into freshwater and marine environments.
3.1. What can be done to reduce plastic pollution post-COVID-19 pandemic?
The overwhelming consequence of COVID-19 pandemic coupled with strategic response measures taken by governments and healthcare providers around the world have created more challenges for combating plastic pollution. There is no doubt that COVID-19 will reverse the momentum of a years-long global battle to cut down single-use plastics. If we want to keep the benefit of plastics without compromising our planet, we need to understand how to manage them. As the world focusses its attention at finding the solution to coronavirus, this review attempts to draw the attention of the world to adopt stricter waste management strategies aimed at reducing environmental contamination by coronavirus-generated plastics during this pandemic and after the lockdown period.
This can be achieved by proper disposal and strict adherence to approved hazardous medical waste management procedures for single-use medical gloves, surgical masks, surgical suits, face shields, and aprons. The development of a robust conservation strategy for proper sterilization and disinfection of surgical gowns and masks should be carried out while taking into consideration the reduction of risks such guidelines could pose to healthcare workers and the COVID-19 patients. As recommended by the US FDA, healthcare providers could implement the use of reusable surgical gowns in place of disposable single-use PPE (US FDA, 2020b). Surgical gowns are usually made of either single-use or reusable materials and worn as a barrier to microbial and fluid transmission during medical procedures (Ammirati, 2005; Song et al., 2011). In addition, extended use of PPE for multiple patients may be prioritized by healthcare providers. This would ultimately lead to a drastic reduction in the amount of plastic waste generated. In order to address the existing problem of environmental plastic pollution, used personal protective equipment should be disposed of appropriately in well-labelled clinical waste bins, followed by recycling at designated biohazard waste management facilities.
4. Conclusions
In view of the recent global efforts geared at combating the highly contagious SARS-CoV-2, the environment might have made some gains in terms of reduction in carbon footprint and improved air and surface water quality. However, there has been an unprecedented need, consumption, and release of single-use plastic products since the coronavirus outbreak. According to our estimates, enormous amount of single-use plastic wastes has been generated globally since the outbreak of COVID-19. Current worldwide estimate of daily generated single-use PPE (facemasks) is 1.6 million tonnes/day implying that approximately 3.4 billion single-use facemasks or face shields are discarded daily due to COVID-19 pandemic. Regional estimates indicate that Asia with the highest population is projected to generate the highest quantity (1.8 billon) of discarded facemasks per day, followed by Europe, Africa, Latin America and the Caribbean, North America, and Oceania at 445, 411, 380, 244, and 22 million facemasks per day, respectively. China (1.4 billion population), India (1.3 billion population), United States (331 million inhabitants), Brazil (212 million people), Nigeria (206 million population) and United Kingdom (67 million population), it is estimated that the daily facemasks generated if all their citizens wear and discard a facemask or face shield per day, could result in the generation of at least 702, 386, 219, 140, 75, and 45 million of contaminated masks per day. Given these estimates, there is a growing danger of single-use plastic and PPE which are directly attributed to COVID-19 pandemic. This is capable of exacerbating the existing plastic pollution problems and could constitute an impending threat to our collective existence and the survival of marine organisms. Not only is there a potential environmental risk of improperly discarded non-biodegradable PPE made from plastics, but there are also human health risks from minute particulate sized plastics through consumption of seafoods which is a choice source of protein for many around the world. More so, macro-, meso-, and microplastics in the environment and marine ecosystems could serve as potential vectors of pathogens. Marine organisms such as fishes, turtles, beach seabirds, sea turtles, whales, and other marine mammals might be at risk of entanglement and intentional, accidental or indirect ingestion of latex gloves which could lead to severe injuries and death.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Contributor Information
Nsikak U. Benson, Email: nbenson@covenantuniversity.edu.ng.
Thavamani Palanisami, Email: thava.palanisami@newcastle.edu.au.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
Table S1
References
- Ahmed W., Angel N., Edson J. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aljazeera News Which country have made wearing face masks compulsory. 2020. https://www.aljazeera.com/news/2020/04/countries-wearing-face-masks-compulsory-200423094510867.html
- Ammirati C.T. 25–37. Elsevier Mosby; 2005. Chapter 2: aseptic technique. (Surgery of the Skin). [Google Scholar]
- Benson N.U., Fred-Ahmadu O.H., Bassey D.E., Atayero A.A. COVID-19 pandemic and emerging plastic-based personal protective equipment waste pollution and management in Africa. J. Environ. Chem. Eng. 2021 doi: 10.1016/j.jece.2021.105222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benson N.U., Fred-Ahmadu O.H. Occurrence and distribution of microplastics-sorbed phthalic acid esters (PAEs) in coastal psammitic sediments of tropical Atlantic Ocean, Gulf of Guinea. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.139013. [DOI] [PubMed] [Google Scholar]
- Boyle l. 2020. Discarded Coronavirus Face Masks and Gloves Rising Threat to Ocean Life, Conservationists Warn.https://www.independent.co.uk/news/coronavirus-masks-gloves-oceans-pollution-waste-a9469471.html [Google Scholar]
- BWS Inc . 2018. Types of Biomedical Waste Disposal.http://www.bwaste.com/types-of-biomedical-waste-disposal/ [Google Scholar]
- CDC . 2020. Centers for Disease Control and Prevention. Use of Cloth Face Coverings to Help Slow the Spread of COVID-19.https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html [Google Scholar]
- CDC . 2020. - Centers for Disease Control and Prevention.https://www.cdc.gov/infectioncontrol/guidelines/environmental/background/medical-waste.html [Google Scholar]
- Chaudhuri S. 2020. War on Plastic Takes a Back Seat in Coronavirus Crisis.https://www-wsj-com.cdn.ampproject.org/c/s/www.wsj.com/amp/articles/war-on-plastic-takes-a-back-seat-in-coronavirus-crisis-11584624140 [Google Scholar]
- Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microb. 2020 doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doremalen N. van., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fred-Ahmadu O.H., Ayejuyo O.O., Benson N.U. Microplastics distribution and characterization in epipsammic sediments of tropical Atlantic Ocean, Nigeria. Reg. Stud. Marine Sci. 2020;38:101365. [Google Scholar]
- Fred-Ahmadu O.H., Bhagwat G., Oluyoye I., Benson N.U., Ayejuyo O.O., Palanisami T. Interaction of chemical contaminants with microplastics: principles and perspectives. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2019.135978. [DOI] [PubMed] [Google Scholar]
- Geyer R., Jambeck J.R., Law K.L. Production, use, and fate of all plastics ever made. Sci. Adv. 2017;3 doi: 10.1126/sciadv.1700782pmid:28776036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagemann H. 2020. Coronavirus Fears Prompt Suspensions of Bans on Single-Use Plastic Bags.https://www.npr.org/sections/coronavirus-live-updates/2020/04/13/832 838321/coronavirus-fears-prompt-suspensions-of-bans-on-single-use-plastic-bags [Google Scholar]
- Herron J.B.T., HayDavid A.G.C., Gilliam A.D., Brennan P.A. Personal protective equipment and Covid-19- a risk to healthcare staff? Br. J. Oral Maxillofac. Surg. 2020;58:500–502. doi: 10.1016/j.bjoms.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jambeck J.R., Geyer R., Wilcox C., Siegler T.R., Perryman M., Andrady A., Narayan R., Law K.L. Plastic waste inputs from land into the ocean. Science. 2015;347:768–771. doi: 10.1126/science.1260352. [DOI] [PubMed] [Google Scholar]
- Jeyasanta K.I., Sathish N., Patterson J., Edward J.K.P. Macro-, meso- and microplastic debris in the beaches of Tuticorin district, Southeast coast of India. Mar. Pollut. Bull. 2020;154 doi: 10.1016/j.marpolbul.2020.111055. [DOI] [PubMed] [Google Scholar]
- Jones S.L., Gibson K.E. Characterization of polyurethane foam environmental monitoring tools for the recovery and release of viruses. Food Environ. Virol. 2020;12:158–166. doi: 10.1007/s12560-020-09421-5. [DOI] [PubMed] [Google Scholar]
- Kane I.A., Clare M.A., Miramontes E., Wogelius R., Rothwell J.J., Garreau P., Pohl F. Seafloor microplastic hotspots controlled by deep-sea circulation. Science. 2020 doi: 10.1126/science.aba5899. [DOI] [PubMed] [Google Scholar]
- Klemes J.J., Fan Y.V., Tan R.R., Jiang P. Minimizing the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sustain. Energy Rev. 2020;127:109883. doi: 10.1016/j.rser.2020.109883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W.C., Tse H.F., Fok L. Plastic waste in the marine environment: a review of sources, occurrence and effects. Sci. Total Environ. 2016;566:333–349. doi: 10.1016/j.scitotenv.2016.05.084. https://www.sciencedirect.com/science/article/pii/S0048969716310154 [DOI] [PubMed] [Google Scholar]
- Liu P., Zhan X., Wu X., Li J., Wang H., Gao S. Effect of weathering on environmental behavior of microplastics: properties, sorption and potential risks. Chemosphere. 2020;242:125193. doi: 10.1016/j.chemosphere.2019.125193. [DOI] [PubMed] [Google Scholar]
- Lodder W., de Roda Husman A. SARS-CoV-2 in wastewater: potential health risk, but also data source. Lancet Gastroenterol. Hepatol. 2020;1253:30087. doi: 10.1016/S2468-1253(20)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masood N., Zakaria M.P., Halimoon N., Aris A.Z., Magam S.M., Kannan N., Mustafa S., Ali M.M., Keshavarzifard M., Vaezzadeh V., others Anthropogenic waste indicators (AWIs), particularly PAHs and LABs, in Malaysian sediments: application of aquatic environment for identifying anthropogenic pollution. Mar. Pollut. Bull. 2016;102:160–175. doi: 10.1016/j.marpolbul.2015.11.032. [DOI] [PubMed] [Google Scholar]
- Medema G., Heijnen L., Elsinga G., Italiaander R. Presence of SARS-Coronavirus-2 in sewage. medRxiv. 2020 doi: 10.1021/acs.estlett.0c00357. [DOI] [PubMed] [Google Scholar]
- Nghiem L.D., Morgan B., Donner E., Short M.D. The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case Stud. Chem. Environ. Eng. 2020;1:100006. doi: 10.1016/j.cscee.2020.100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NOAA . 2019. A Guide to Plastic in the Ocean.https://oceanservice.noaa.gov/hazards/marinedebris/plastics-in-the-ocean.html [Google Scholar]
- Nzediegwu C., Chang S.X. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour. Conserv. Recycl. 2020;161:104947. doi: 10.1016/j.resconrec.2020.104947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park G.W., Lee D., Treffiletti A., Hrsak M., Shugart J., Vinjé J. Evaluation of a new environmental sampling protocol for detection of human norovirus on inanimate surfaces. Appl. Environ. Microbiol. 2015;81(17):5987–5992. doi: 10.1128/AEM.01657-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil C.A., Chaudhary S., Sharma B.R., Manickam R. Need of biomedical waste management in rural hospitals in India. J. Pharm. Sci. Rev. Res. 2015;35(33):175–179. [Google Scholar]
- Patrício Silva A.L., Prata J.C., Walker T.R., Duarte A.C., Ouyang W., Barcelò D., Rocha-Santos T. Increased plastic pollution due to COVID-19 pandemic: challenges and recommendations. Chem. Eng. J. 2021;405:126683. doi: 10.1016/j.cej.2020.126683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata J.C., Silva A., Walker T.R., Duarte A.C., Rocha-Santos T.A.P. COVID-19 pandemic repercussions on the use and management of plastics. Environ. Sci. Technol. 2020;54(2020):1–6. doi: 10.1021/acs.est.0c02178. [DOI] [PubMed] [Google Scholar]
- Sampol C. 2020. Surgical Masks, Respirators, Barrier Masks: Which Masks Actually Protect against Coronavirus?http://emag.medicalexpo.com/which-masks-actually-protect-against-coronavirus/ [Google Scholar]
- Sarkar D.J., Sarkar S.D., Das B.K., Manna R.K., Behera B.K., Samanta S. Spatial distribution of meso and microplastics in the sediments of river Ganga at eastern India. Sci. Total Environ. 2019;694:133712. doi: 10.1016/j.scitotenv.2019.133712. [DOI] [PubMed] [Google Scholar]
- Scaraboto D., Joubert A.M., Gonzalez-Arcos C. Using lots of plastic packaging during the coronavirus crisis? You’re not alone. 2020. https://theconversation.com/using-lots-of-plastic-packaging-during-the-coronavirus-crisis-youre-not-alone-135553
- Silva A.P.L., Prata J.C., Walker T.R., Campos D., Duarte A.C., Soares A.M.V.M., Barcelò D., Rocha-Santos T. Rethinking and optimising plastic waste management under COVID-19 pandemic: policy solutions based on redesign and reduction of single-use plastics and personal protective equipment. Sci. Total Environ. 2020;742:140565. doi: 10.1016/j.scitotenv.2020.140565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song G., Cao W., Cloud R.M. Handbook of Medical Textiles. Woodhead Publishing Series in Textiles; 2011. Chapter 8: medical textiles and thermal comfort; pp. 198–218. [Google Scholar]
- Syam N. Is the pandemic triggering a spike in plastic pollution? 2020. https://newseu.cgtn.com/news/2020-05-22/Is-the-pandemic-triggering-a-spike-in-plastic-pollution--QBobeagfok/index.html
- Tang W. 21st Century Business Herald; 2020. The National "Epidemic-Related" Medical Waste Realizes that the Daily Medical Waste Treatment Market Needs to Be Standardized.http://www.21jingji.com/2020/3-12/xNMDEzODFfMTU0MjIxNQ.html [Google Scholar]
- Todd E.C., Greig J.D., Bartleson C.A., Michaels B.S. Outbreaks where food workers have been implicated in the spread of foodborne disease. Part 6. Transmission and survival of pathogens in the food processing and preparation environment. J. Food Protect. 2009;72:202–219. doi: 10.4315/0362-028x-72.1.202. [DOI] [PubMed] [Google Scholar]
- US FDA . 2020. N95 Respirators and Surgical Masks (Face Masks)https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-and-surgical-masks-face-masks [Google Scholar]
- US FDA . 2020. Surgical Mask and Gown Conservation Strategies - Letter to Health Care Providers.https://www.fda.gov/medical-devices/letters-health-care-providers/surgical-mask-and-gown-conservation-strategies-letter-health-care-providers [Google Scholar]
- Vasickova P., Pavlik I., Verani M., Carducci A. Issues concerning survival of viruses on surfaces. Food Environ. Virol. 2010;2:24–34. doi: 10.1007/s12560-010-9025-6. [DOI] [Google Scholar]
- Vanapalli K.R., Sharma H.B., Ranjan V.P., Samal B., Bhattacharya J., Dubey B.K., Goel S. Challenges and strategies for effective plastic waste management during and post COVID-19 pandemic. Sci. Total Environ. 2021;750:141514. doi: 10.1016/j.scitotenv.2020.141514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, World Health Organisation . 2018. Healthcare Waste.https://www.who.int/news-room/fact-sheets/detail/health-care-waste [Google Scholar]
- Wu F., Xiao A., Zhang J., Gu X., Lee W., Kauffman K., Hanage W., Matus M., Ghaeli N., Endo N., Duvallet C., Moniz K., Erickson T., Chai P., Thompson J., Alm E. SARS-CoV-2 titers in wastewater are higher than expected from clinically confirmed cases Authors. medRxiv. 2020 doi: 10.1128/mSystems.00614-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z.-M., Zhang H.-H., Zou Y.-W., Yang G.-P. Distribution and ecotoxicological state of phthalate esters in the sea-surface microlayer, seawater and sediment of the Bohai Sea and the Yellow Sea. Environ. Pollut. 2018;240:235–247. doi: 10.1016/j.envpol.2018.04.056. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Data Availability Statement
Data included in article/supplementary material/referenced in article.