Abstract
Objective: To investigate beliefs and attitudes of the public toward attention deficit hyperactivity disorder (ADHD) in children and adults. Method: In a representative population survey in Germany (N = 1,008) using computer-assisted telephone interviews, we asked participants about causal beliefs, illness recognition, treatment recommendations, and beliefs about ADHD, presenting an unlabelled vignette of a child or an adult with ADHD. Results: The most frequently endorsed causal beliefs for the depicted child with ADHD were “TV or Internet,” “lack of parental affection,” and “broken home.” In comparison with the child vignette, biological causal beliefs were endorsed more often after the adult vignette. In the child vignette, 66% advised against a treatment with stimulant medication. About 90% of respondents had heard of ADHD. Of those, 20% said they believed ADHD to be not a real disease. Conclusion: Beliefs of the German public partly contradict evidence and should be considered in therapeutical and public contexts.
Keywords: ADHD, population survey, attitudes, knowledge, causal beliefs, treatment recommendations, stigma
Introduction
With a worldwide-pooled prevalence of 5.3% among children (Polanczyk, de Lima, Horta, Biederman, & Rohde, 2007) and 2.5% among adults (Simon, Czobor, Bálint, Mészáros, & Bitter, 2009), attention deficit hyperactivity disorder (ADHD) is a mental illness of high epidemiological, clinical, and cultural importance. In recent years, controversial discussions about diagnostic labels (Asherson et al., 2010; Moncrieff & Timimi, 2010), etiology (Batstra, te Meerman, Conners, & Frances, 2017; Dehue et al., 2017; Hoogman et al., 2017), and pharmacotherapy (Boesen et al., 2017; Gerlach, Banaschewski, Coghill, Rohde, & Romanos, 2017; Häßler, 2019; Kölch, 2019; Romanos, Coghill et al., 2016; Romanos, Reif, & Banaschewski, 2016; Storebø et al., 2015) have dominated a large part of academic debates surrounding this disorder. Thus, the authors of a recent mega-analysis of subcortical structures and intracranial volumes using magnetic resonance imaging (MRI) brain scans, covered widely in the media, concluded that
patients with ADHD have altered brains; therefore, ADHD is a disorder of the brain. This message is clear for clinicians to convey to parents and patients, which can help to reduce the stigma of ADHD and improve understanding of the disorder. (Hoogman et al., 2017, p. 311)
It remains important to stress that this assertion was found to be incorrect for the general population with respect to other mental disorders such as schizophrenia or depression, where biological illness concepts were generally associated with more rather than less stigma (Angermeyer, Holzinger, Carta, & Schomerus, 2011; Kvaale, Gottdiener, & Haslam, 2013; Schomerus, Matschinger, & Angermeyer, 2014; Speerforck, Schomerus, Pruess, & Angermeyer, 2014). Also, issues with methodological limitations and the heterogenic etiology of ADHD were raised in reply to that mega-analysis (Batstra et al., 2017; Dehue et al., 2017). Furthermore, evidence for treatments with stimulants such as methylphenidate was subject to intensive academic debate: Whereas a Cochrane Review on methylphenidate for children and adolescents concluded that “the low quality of the underpinning evidence means that we cannot be certain of the magnitude of the effects” (Storebø et al., 2015), other researchers repeatedly criticized this main conclusion (e.g., Gerlach et al., 2017; Romanos, Coghill et al., 2016; Romanos, Reif, & Banaschewski, 2016). Another review on methylphenidate for adults even was withdrawn from the Cochrane Library after substantial criticism of its methods and flawed conclusions (Boesen et al., 2017).
In the face of such polarizing academic arguments, questions arise regarding the general population: Does the public take note of such debates, and what are the beliefs underlying them in the general population? After all, public beliefs about people with mental illness are particularly important, as they not only shape the thoughts and actions of patients but also influence the advice of caregivers and friends (Angermeyer, Matschinger, & Riedel-Heller, 1999). The decision to seek professional help for a mental health problem is closely related to prevalent public attitudes and beliefs (Angermeyer, Matschinger, & Schomerus, 2017; Angermeyer & Schomerus, 2017).
Against this background, the present study uses data from the first population-based survey on public beliefs about ADHD in children and adults in an European country to address the following questions:
Does the German public recognize typical symptoms of ADHD, and is ADHD considered to be a real disorder?
What are the suspected causes of ADHD?
How many people recommend seeking professional help for a person with the core symptoms of ADHD? And if so, what is expected from professionals?
What causal beliefs are associated with a higher approval of professional help or an identification as mental illness or real disease?
Do disorder-related beliefs differ regarding the age of the person depicted with ADHD?
Method
Participants
A representative population survey of German-speaking adults (>18 years) was conducted in Germany between March and May 2017. Fieldwork was done by USUMA (Berlin), a company specialized in market and social research. Altogether, 1,008 persons completed the interview, reflecting a response rate of 20.1%. Reasons for nonresponse were the following: partial interviews (n = 21), refusal or termination of interview by the survey respondent (n = 1,859), no contact with eligible household and answering machine (n = 1,154), and other difficulties with communication due to problems with language or understanding (n = 432). Ethical considerations prohibited the collection of any detailed information on nonrespondents. The sample contained slightly more women, more elderly, and more educated persons in comparison with the German general population (Supplementary Table 1).
Interview and Case Vignettes
After training the interviewers and conducting a field pretest to evaluate the comprehensibility and internal consistency of the interview, a computer-assisted telephone interview (CATI) was conducted using real-time monitoring by trained supervisors. The interview started with the playing of a previously recorded unlabeled case vignette of a child (n = 505) or an adult (n = 503) with all core symptoms of ADHD according to Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013). During and after hearing the vignette, we controlled the attentiveness of respondents by asking about their problems with understanding. The two vignette conditions differed only with regard to age (12 years/35 years) and contextual factors (e.g., school/work). The gender of the person described in the vignette (Anne/Robert) varied at random. The wording of the vignettes had undergone validation by five blinded experts with experience in general or child/adolescence psychiatry and is included in the appendix.
Measures
Illness recognition and questions about ADHD
At the beginning of the interview, we asked respondents (a) how they would label the depicted problem as an open question, (b) to estimate changes in the prevalence of the depicted problem during the last 20 years, and (c) whether they identify the problem as a mental illness. At the very end of the interview, we disclosed ADHD as the diagnosis and asked about familiarity with it and whether respondents perceived it as a real disorder.
Causal beliefs
We elicited beliefs about possible causes of the problem described in the vignette with a list of 18 possible causes, each of which was rated on a 5-point Likert-type scale anchored with 1 = “certainly a cause” and 5 = “certainly not a cause.” Answers to these items were entered into an exploratory principal component factor analysis with varimax rotation, yielding four main factors: “family and childhood,” “current stress,” “biogenetic,” and “environment and diet.” We used a z-transformed score for each factor (mean = 0, standard deviation = 1) and reversed the rotated factor scores, with higher scores indicating higher agreement with the appropriate causes.
Help-seeking and treatment recommendations
We asked respondents what intervention they would recommend in the depicted situation. If they advised seeking professional help immediately or after several months, participants were presented with a list of six help-seeking and six treatment recommendations that were used in earlier studies (Riedel-Heller, Matschinger, & Angermeyer, 2005) and were asked to what extent they would recommend each treatment modality for the person described in the vignette. The strength of each recommendation was rated on a 5-point Likert-type scale, with 1 = “recommend urgently” and 5 = “strongly advise against.” For our analyses, we reversed the item scores, with higher scores indicating higher approval to the recommendation. To investigate first-choice help-seeking and treatment options, we asked respondents which of their previously preferred options they are recommending most strongly.
Statistical Analysis
To allow statements to be representative of the German-speaking general population, all results were calculated as weighted percentages accounting for household size, study design, and the German general population. To illustrate the prevalence of public beliefs, respondents who endorsed the two points on either side of the midpoint of the 5-point scales (values 1 + 2 and 4 + 5) were grouped together into the categories “a cause” and “not a cause” (causal beliefs), and “recommend” and “advise against” (help-seeking and treatment recommendations). Differences in responses were tested for statistical significance using Fisher’s exact test regarding the vignette condition.
To analyze associations between causal beliefs and help-seeking or treatment recommendations and illness conceptualizations, we calculated weighted simple (dichotomous ordinal-scaled variables) and ordered (nondichotomous ordinal-scaled variables) logistic regression models with help-seeking or treatment recommendations, identification as mental illness, or perception of ADHD as outcome and causal belief factor variables as exposure. The models were controlled for age, gender, and education (categorial). To deal with missing observations (19.0% of participants with at least one missing in a causal belief item), we used multiple imputation by chained equations (Royston, 2005; van Buuren, Boshuizen, & Knook, 1999) to perform identical regression models with the same weighting as before as a sensitivity analysis. Imputations were calculated 20 times for all participants who had less than 22.2% (from ≤4 to 18) missing within all causal belief items. After imputation, 1.7% of participants remained with >22.2% missings. Only associations that remained statistically significant within the sensitivity analysis are reported.
The statistical analyses were carried out using Stata 13.1 MP (StataCorp, 2013).
More detailed information on the “Method” section is available in the online supplement.
Results
Illness Recognition and Questions About ADHD
Twenty-nine percent and 28% of the German general population spontaneously described the case vignette of a 12-year-old child as ADHD or hyperactivity (disorder), respectively; this was significantly higher than descriptions of the adult case vignette (Table 1). In all, 44% (child vignette) or 55% (adult vignette) categorized the depicted symptoms as mental illness, and 74% (child vignette) or 83% (adult vignette) believed that the number of people with such problems has risen. Although more than 90% of the general population had heard of “attention deficit hyperactivity disorder” or “ADHD,” about three quarters of those believed ADHD to be a real disease, whereas 20% did not.
Table 1.
Illness Recognition and Beliefs About ADHD.
| Answers/“agree” (%)a |
|||
|---|---|---|---|
| ADHD child (n = 503) | ADHD adult (n = 505) | F testb (df 1, 1007) | |
| How would you describe the condition of Robert/Anne? (spontaneous answers) | |||
| ADHD | 29 | 20 | F = 6.46, p = .011 |
| Attention deficit/disorder | 15 | 13 | F = 0.83, p = .363 |
| Hyperactivity (disorder) | 28 | 21 | F = 4.00, p = .046 |
| Would you say Anne/Robert has a mental illness? | |||
| Yes | 44 | 55 | F = 6.29, p = .012 |
| No | 47 | 39 | F = 2.74, p = .098 |
| Don’t know | 9 | 6 | F = 2.99, p = .084 |
| Do you think that during the last 20 years the number of people who have problems like Robert/Anne has | |||
| Increased. | 74 | 83 | F = 6.17, p = .013 |
| Decreased. | 1 | 1 | F = 0.35, p = .557 |
| Not changed. | 17 | 10 | F = 4.01, p = .045 |
| Don’t know | 9 | 6 | F = 1.34, p = .247 |
| Have you ever heard of “attention deficit hyperactivity disorder” or “ADHD”? | |||
| Yes | 91 | 92 | F = 0.19, p = .665 |
| Do you think that “attention deficit hyperactivity disorder” or “ADHD” is a real disorder | |||
| Yes | 75 | 77 | F = 0.04, p = .533 |
| No | 20 | 20 | F = 0.00, p = .977 |
| Not specifiedd | 5 | 2 | F = 2.50, p = .114 |
Note. Illness recognition and questions about ADHD and weighted response frequencies of the German-speaking general population sorted by vignette. Due to rounding, percentages do not necessarily add up to 100%.
Values are weighted percentages including missing observations.
F statistics after weighted logistic regression analysis with vignette condition (exposure) and the related response category as outcome testing the hypothesis that estimates differ between vignette conditions.
The given weighted percentages were calculated among those who stated to have ever heard of ADHD before.
Stated here due to a relevant prevalence.
Causal Beliefs
The four most frequently endorsed causal beliefs after hearing the child vignette were “too much TV or Internet,” a “lack of parental affection,” a “broken home,” and “problems with parents or friends” (Table 2). After presentation of the adult vignette, a “stressful life event,” “pressure to perform,” “problems with partner or family,” and “chemical imbalance in the brain” were endorsed most frequently. “Environmental pollution” was endorsed least frequently in both vignettes. In comparison with an adult person depicted with ADHD, biological causal beliefs such as “chemical imbalance in the brain,” “brain disease,” or “drug abuse” were endorsed less frequently after the child vignette. Otherwise, causal beliefs from the family-social context such as “too much TV or Internet,” “lack of parental affection,” or “poor parenting” were selected more frequently after the child vignette. Biogenetic causes were more frequently rejected after the description of a child with ADHD in comparison with an adult with the same symptoms.
Table 2.
Causal Beliefs.
| “A cause” (%)a
Rankb |
“Not a cause” (%)a
Rankb |
|||||
|---|---|---|---|---|---|---|
| ADHD child (n = 503) | ADHD adult (n = 505) | F testc (df 1, 1007) | ADHD child (n = 503) | ADHD adult (n = 505) | F testc (df 1, 1007) | |
| Too much TV or Internet | 58 (1.) |
44 (8.) |
F = 10.09, p = .002 |
18 (12.) |
30 (7.) |
F = 9.21, p = .003 |
| Lack of parental affection | 58 (1.) |
48 (5.) |
F = 5.93, p = .015 |
15 (16.) |
20 (12.) |
F = 2.36, p = .125 |
| Broken home | 55 (3.) |
48 (5.) |
F = 2.61, p = .107 |
20 (11.) |
20 (12.) |
F = .00, p = .975 |
| Problems with parents or friends / partner or family | 54 (4.) |
49 (2.) |
Differing items | 15 (16.) |
17 (17.) |
Differing items |
| Pressure to perform | 52 (5.) |
49 (2.) |
F = 0.58, p = .446 |
18 (12.) |
23 (11.) |
F = 1.38, p = .241 |
| School / Work-related stress | 49 (6.) |
44 (8.) |
Differing items | 18 (12.) |
27 (9.) |
Differing items |
| Stressful life event | 48 (7.) |
56 (1.) |
F = 2.84, p = .093 |
15 (16.) |
19 (15.) |
F = 0.85, p = .356 |
| Unconscious conflict | 47 (8.) |
45 (7.) |
F = 0.25, p = .621 |
16 (15.) |
19 (15.) |
F = 0.42, p = .518 |
| Insufficient self-control | 41 (9.) |
42 (10.) |
F = 0.03, p = .852 |
23 (9.) |
28 (8.) |
F = 1.81, p = .178 |
| Chemical imbalance of the brain | 39 (10.) |
49 (2.) |
F = 5.14, p = .023 |
23 (9.) |
11 (18.) |
F = 13.59, p < .001 |
| Heredity | 35 (11.) |
41 (11.) |
F = 1.65, p = .200 |
39 (5.) |
27 (9.) |
F = 8.96, p = .003 |
| Childhood sexual abuse | 33 (12.) |
35 (14.) |
F = 0.28, p = .598 |
28 (8.) |
33 (5.) |
F = 1.60, p = .206 |
| Poor parenting | 33 (12.) |
20 (17.) |
F = 11.53, p < .001 |
36 (6.) |
49 (2.) |
F = 9.95, p = .0017 |
| Brain disease | 31 (14.) |
41 (11.) |
F = 5.68, p = .017 |
32 (7.) |
20 (12.) |
F = 10.54, p = .001 |
| Poor diet | 27 (15.) |
24 (16.) |
F = 0.74, p = .390 |
42 (3.) |
48 (3.) |
F = 1.90, p = .168 |
| Vitamin deficiency | 22 (16.) |
25 (15.) |
F = 0.75, p = .387 |
41 (4.) |
43 (4.) |
F = 0.28, p = .598 |
| Drug abuse | 21 (17.) |
36 (13.) |
F = 14.84, p < .001 |
56 (2.) |
32 (6.) |
F = 31.85, p < .001 |
| Environmental pollution | 13 (18.) |
11 (18.) |
F = 0.74, p = .389 |
66 (1.) |
66 (1.) |
F = 0.02, p = .887 |
Note. Queried causal beliefs and weighted percentages of answers among the German-speaking general population. The causal beliefs are ordered by their frequency as “a cause” in relation to the child vignette.
Values are weighted percentages including missing observations. Respondents who endorsed the two points on either side of the midpoint of the 5-point scales (values 1 + 2 and 4 + 5) were grouped together into the categories “a cause” and “not a cause.”
Relative rank of the causal belief in relation to the weighted percentages of other causal beliefs with regard to vignette condition and answer category.
F statistics after weighted logistic regression analysis with vignette condition (exposure) and the related response category as outcome testing the hypothesis that estimates differ between vignette conditions.
Help-seeking and treatment recommendations
Seventy-one percent (child vignette) or 75% (adult vignette) of the general population recommended seeking professional help (Table 3). Of the respondents who initially endorsed the options “do nothing and wait” or “try to do something with the help of family or close friends,” more than three quarters recommended seeking professional help when the condition would not change over several months. At the latest after several months, in total 94% (child vignette) or 95% (adult vignette) of the German general population recommended seeing a professional for the depicted core symptoms of ADHD.
Table 3.
Professional Help-Seeking and Treatment Recommendations.
| What to do? | “Agree” (%)a |
|||||
|---|---|---|---|---|---|---|
| ADHD child | ADHD adult | F testb (df 1, 1007/263) | ||||
|
What to do in such a situation?
(child; n = 503)/(adult; n = 505) | ||||||
| Nothing and wait. | 2 | 1 | F = 0.91, p = .341 | |||
| Try to do something with the help of family or close friends. | 27 | 24 | F = 0.57, p = .449 | |||
| Seek professional help. | 71 | 75 | F = 0.91, p = .340 | |||
| What to do when the condition of Robert/Anne would not change over several months?c (child; n = 149)/(adult; n = 115) | ||||||
| Nothing and wait. | 2 | 2 | F = 0.05, p = .827 | |||
| Try to do something with the help of family or close friends. | 20 | 15 | F = 0.61, p = .436 | |||
| Seek professional help. | 78 | 82 | F = 0.28, p = .599 | |||
| Professional help in total, at least after several months.d (child; n = 503)/(adult; n = 505) | 94 | 95 | F = 0.81, p = .368 | |||
| Help-seeking and treatment recommendations | ||||||
| “Recommend” (%)e |
“Advise against” (%)e |
|||||
| ADHD child (n = 503) | ADHD adult (n = 505) | F testb (df 1, 1007) | ADHD child (n = 503) | ADHD adult (n = 505) | F testb (df 1, 1007) | |
| Help-seeking | ||||||
| Psychotherapist | 68 | 71 | F = 0.60, p = .438 | 6 | 6 | F = 0.00, p = .994 |
| Educational psychologist/Take a cure | 68 | 42 | Differing items | 7 | 24 | Differing items |
| Psychiatrist | 55 | 67 | F = 6.93, p = .009 | 18 | 12 | F = 3.56, p = .0594 |
| General practitioner | 53 | 56 | F = 0.43, p = .512 | 20 | 23 | F = 0.52, p = .470 |
| Psychiatric hospital | 14 | 24 | F = 8.65, p = .003 | 58 | 47 | F = 6.52, p = .011 |
| Pharmacy | 5 | 3 | F = 0.79, p = .373 | 80 | 83 | F = 0.60, p = .437 |
| Treatment | ||||||
| Concentration and memory training | 76 | 79 | F = 0.65, p = .419 | 3 | 4 | F = 1.06, p = .304 |
| Psychotherapy | 64 | 63 | F = 0.03, p = .859 | 12 | 11 | F = 0.01, p = .931 |
| Autogenic training | 63 | 66 | F = 0.46, p = .498 | 6 | 7 | F = 0.11, p = .741 |
| Homeopathic remedies | 30 | 27 | F = 0.65, p = .420 | 35 | 34 | F = 0.04, p = .842 |
| Stimulants like Ritalin® | 6 | 5 | F = 0.00, p = .965 | 66 | 68 | F = 0.15, p = .702 |
| Sedatives like Valium® or Faustan® | 2 | 4 | F = 2.71, p = .100 | 87 | 80 | F = 4.22, p = .040 |
Note. Endorsed further procedure as well as professional help-seeking and treatment recommendations and weighted frequencies of response categories. The recommendations are ordered by the frequency of recommendations in relation to the child vignette.
Values are weighted percentages including missing observations.
F statistics after weighted logistic regression analysis with vignette condition (exposure) and the related response category as outcome testing the hypothesis that estimates differ between vignette conditions.
Only participants were asked who initially did not advise to seek professional help.
Weighted percentages of respondents recommending professional help at least after several months.
Values are weighted percentages including missing observations. Respondents who endorsed the two points on either side of the midpoint of the 5-point scales (values 1 + 2 and 4 + 5) were grouped together into the categories “recommend” and “advise against.”
Help-seeking
After presentation of the child vignette, the two help-seeking recommendations that were endorsed the most were to consult a psychotherapist or an educational psychologist (Table 3). As a first choice, 30% recommended consulting a psychotherapist, 29% recommended consulting an educational psychologist, and 24% suggested seeing a psychiatrist (Supplementary Figure 1). For an adult with ADHD, consultation with a psychotherapist or a psychiatrist was recommended most frequently. When respondents were forced to choose, 30% recommended seeing a psychotherapist and 29% decided to recommend a general practitioner first. In comparison with recommendations for a child, the consultation of a psychiatrist or a psychiatric hospital was endorsed more frequently for an adult with ADHD.
Treatment
For children and adults with ADHD, concentration and memory training, psychotherapy, and autogenic training were recommended most frequently (Table 3). The use of stimulants was recommended as rarely as the use of sedatives. As the large majority of the German general population disapproved of stimulants, 50% (child vignette) and 53% (adult vignette) strongly advised against the use of stimulants (5 on the 5-point Likert-type scale). When respondents had to choose, psychotherapy (37%/40%) or concentration and memory training (36%/32%) were most frequently mentioned as first-line treatments (Supplementary Figure 1).
Associations of causal beliefs with recommendations, identification as mental illness, and perception of ADHD
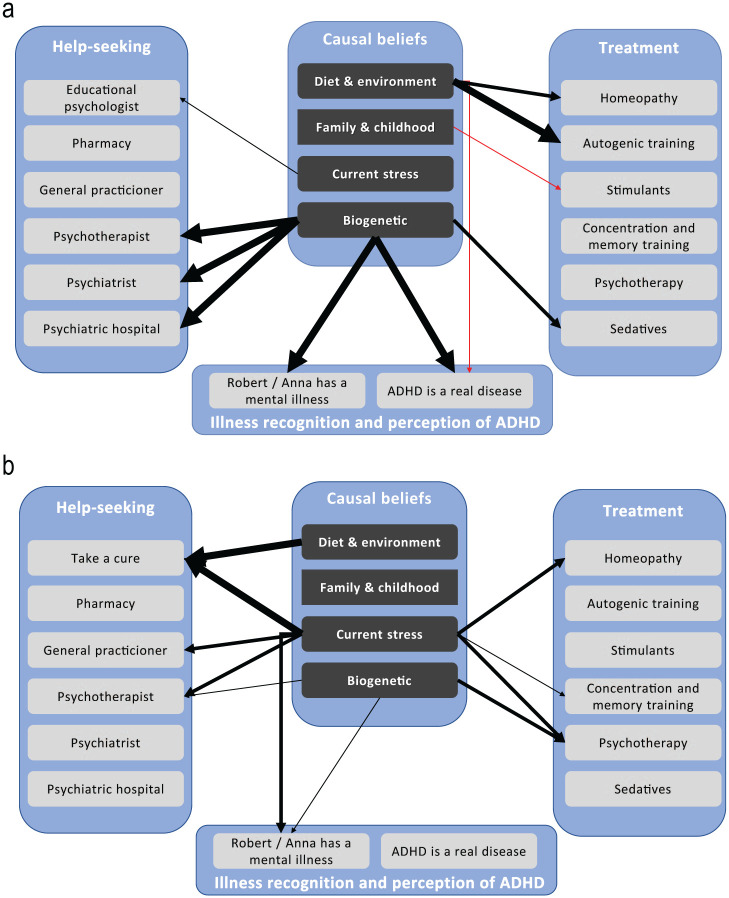
After hearing the child vignette, the factor score comprising causal beliefs around “diet and environment” was predominately associated with a higher approval of homeopathic remedies, autogenic training, and a lower likelihood of a perception as a real disorder, whereas the factor score “family and childhood” was only associated with less approval of a drug therapy with stimulants (Figure 1).
Figure 1.
Associations of causal beliefs with professional recommendations and illness perception after depicting a child (A) or an adult. (B) with ADHD.
Note. Statistically significant odds ratios (0.65; 0.77; 1.39 – 2.41) from weighted ordered (help-seeking / treatment) and simple (illness perception) logistic regression models with factor scores from exploratory principal-component factor analysis of all causal beliefs as exposure are shown, controlled for age, gender and education. Only statistically significant results based on a significant regression model that were reproduced in sensitivity analysis with imputed data are illustrated as arrows of different thickness: 1 point ≙ p<0.05; 4 points ≙ p≤0.01; 8 points ≙ p≤0.001; red arrow ≙ negative association. For every outcome, an independent model was calculated: N= 369 – 403 observations without imputation; 420 – 472 observations after imputation. For details see supplementary table 2.
Although “current stress” in relation to the child vignette was only associated with a higher level of endorsement of an educational psychologist, we found multiple associations with a higher approval of professional help-seeking and treatment as well as with a higher likelihood of classifying the depicted symptoms as a mental illness for an adult with ADHD.
Following the depiction of a child with ADHD, the factor score “Biogenetic” was strongly associated with a higher endorsement for seeing a psychiatrist, a psychotherapist, or being admitted to a psychiatric hospital. Furthermore, it was associated not only with a higher likelihood of conceptualizing the symptoms as mental illness or identifying ADHD as a real disorder but also with a higher recommendation for sedative medication.
Supplementary Table 2 comprises a detailed summary of the regression analysis.
Discussion
The present study indicates that about half of the German-speaking general population identifies the core symptoms of ADHD depicted in the vignettes as mental illness, and that one fifth of those who had heard of ADHD do not believe ADHD to be a real disease. It also shows that the causes for ADHD in children are mostly felt to arise from family-social contexts, while biological causal beliefs are more frequent in relation to the adult phenotype of ADHD. About two thirds of the public advise against the use of stimulants, whereas homeopathic remedies are 4 times more likely to be recommended. Predominantly biogenetic causal beliefs are associated with a higher approval of professional help and the conceptualization of the problem in the child vignette as a mental illness.
To sum up, a large gap exists between evidence-based guidelines and public opinion. The fact that more respondents spontaneously identified the child vignette as having ADHD or hyperactivity (disorder) in comparison with the adult vignette might be linked to a low level of awareness of adult ADHD (Asherson et al., 2012). Interestingly, however, more people recognized the depicted symptoms as mental illness after hearing of the adult vignette, which might point to a higher tolerance in children with respect to unusual behavior. The overall percentage of how many people identified the depicted symptoms as mental illness after hearing the child vignette is comparable with data from the U.S. general population (United States, 46%; Germany, 44%; Pescosolido et al., 2008). Also, a similar percentage believed ADHD to be a real disease (United States, 78%; Germany, 75%; McLeod, Fettes, Jensen, Pescosolido, & Martin, 2007). In contrast to an estimate of 64% in the U.S. general population, in this study more than 90% of respondents stated that they had heard of ADHD (McLeod et al., 2007), although it should be taken into account when comparing these studies that the U.S. survey was conducted in 2002. The predominant perception that the number of people with problems as depicted in the vignettes has increased may reflect the increased rates of ADHD diagnoses (Bachmann, Philipsen, & Hoffmann, 2017), a perception that the disorder is overdiagnosed (Merten, Cwik, Margraf, & Schneider, 2017; Partridge, Lucke, & Hall, 2014), or a wider resonance of the disorder in the media. Also, a change of behavioral norms in society, which possibly leads to higher conspicuousness and burden of symptoms, would be in accordance with the perception of an increase in ADHD-associated symptoms (Conrad & Bergey, 2014). In contrast to this perception, a meta-regression analysis of epidemiological data found no evidence for an increase in the prevalence of ADHD over the last 30 years (Polanczyk, Willcutt, Salum, Kieling, & Rohde, 2014).
In considering causal beliefs of the public, it is important to note that to current understanding, ADHD is a multifactorial disorder with a heterogeneous etiology encompassing genetic predisposition as well as early environmental risk factors and remains a disorder with only a few clear causal risk factors (Banaschewski et al., 2017; Thapar & Cooper, 2016). Even considering growing evidence regarding the causal relationship of early severe institutional deprivation (Kennedy et al., 2016), the strong emphasis on family-social causes we found in relation to the child vignette is not scientifically substantiated (Banaschewski et al., 2017; Thapar & Cooper, 2016). By contrast, biological causes were endorsed considerably less frequently after hearing the child vignette compared with the adult description. At the same time, particularly after depiction of a child with ADHD, these were associated with a higher approval of professional assistance and the identification as mental illness. This is consistent with associations regarding other mental illnesses (Speerforck, Schomerus, Matschinger, & Angermeyer, 2017) and with the finding that a high percentage of the U.S. population with knowledge about medication and biological causes believe ADHD to be a real disorder (McLeod et al., 2007). Conclusions like a future emphasis on biological causal explanations for ADHD should not be drawn carelessly, as possible relations with stigmatizing attitudes or emotions require a better understanding (Angermeyer et al., 2011; Mueller, Fuermaier, Koerts, & Tucha, 2012; Schomerus et al., 2014; Speerforck et al., 2014). Especially, since a higher agreement with the contraindicated treatment with sedatives was associated with biogenetic causal beliefs as well. Interestingly, the rarely endorsed causal beliefs around “environment and diet” were the only ones associated with a higher approval of homeopathic remedies, autogenic training, and a reduced likelihood of conceptualizing ADHD as a real disorder. These findings might be rooted in lifestyle phenomena. In relation to an adult depicted with ADHD, the associations with causal beliefs were overall more complex, with causal beliefs around current stress being more important.
The high preference for nonpharmaceutical treatments for ADHD corroborates findings from a large meta-analysis of public attitudes toward psychiatry and psychiatric treatment (Angermeyer, van der Auwera, Carta, & Schomerus, 2017). What is psychiatry supposed to learn from a finding such as this? On one hand, the strong rejection of a treatment with stimulants contradicts current treatment guidelines (National Institute for Health and Care Excellence [NICE], 2008; Association of the Scientific Medical Societies in Germany [AWMF], 2017) as well as the important role of stimulants in treating the core symptoms of ADHD (Banaschewski et al., 2017). This is especially noteworthy, as the updated version of the German guideline on diagnosis and management of ADHD (likewise NICE, 2008) recommends consideration of a drug treatment for a moderate severity of the disorder, considering the concrete circumstances, preferences, and resources of the patient and related caregivers (AWMF, 2017). On the other hand, these are partly the “preferences of the patient and related caregivers” that are reflected in this study. One could also think of this attitude of the German public toward stimulant medication as advocating psychiatric care that not only includes psychoeducation but also provides sufficient resources for providing effective non-pharmaceutical treatment options on an individual, social, and structural level (Thapar & Cooper, 2016). Although the low frequency of recommendations for stimulants might be due to a generally low level of familiarity with the term “stimulants” or “Ritalin®,” the attitude toward this treatment option was not characterized by indifference but by strong rejection by the majority of respondents. Other studies confirmed a widespread public skepticism toward treating ADHD with stimulants: As in the United States, the majority of respondents recommended a combination of psychotherapy and drug treatment, and only 5% recommended a drug therapy alone (McLeod et al., 2007). Population studies from Australia reported a significantly lower acceptance of drug therapy for ADHD in comparison with the treatment of major depression (Partridge, Lucke, & Hall, 2012; Partridge et al., 2014), and a population survey from Brazil found that more than 50% of respondents were not only skeptical about the use of stimulants but thought that they cause addiction (Gomes, Palmini, Barbirato, Rohde, & Mattos, 2007). However, in any case, the strong rejection of drug therapy for ADHD seems especially important to the psychiatrists and psychotherapists involved. When counseling patients and their caregivers, a particularly high demand for psychoeducation and a complex process of shared decision making may be expected. Further qualitative and quantitative evidence is required to improve our understanding of the associations between drug therapy and stigmatizing beliefs (e.g., personality changes) among patients, caregivers, and the general public (Mueller et al., 2012; Speerforck et al., 2017).
Limitations
This is the first population-based survey from a European country on public beliefs about ADHD in children and adults, using quality assured interviewing, unlabelled case vignettes to avoid possible bias due to the use of medical vocabulary, and allowing direct comparison between ADHD in adults and children. Despite its strengths, the present study should be interpreted in light of the following limitations. First, in investigating the identification of typical symptoms of ADHD as mental illness, we used unlabelled case vignettes depicting core symptoms of ADHD, while reactions to labeled vignettes or persons with the described mental illness or only some symptoms might differ. Second, despite weighting for representativity, participants of higher age and education were overrepresented, and our study design carries a risk for selection and agreement bias as well as social desirability. Third, our study has been conducted in Germany and results are likely to differ in other sociocultural contexts. Fourth, we investigated prevalent beliefs among the German public using a cross-sectional study design and established quantitative methods in population-based attitude research. No conclusions about other causal beliefs or recommendations for professional help among the German public can be made. Finally, we used regression analysis with low explanatory power on cross-sectional data without an experimental design to elucidate possibly important associations of causal beliefs. Therefore, no statements regarding causality can be made, and there are probably other factors associated with help-seeking and treatment recommendations that were not examined in our study.
Conclusion
A marked disparity exists between evidence-based guidelines for diagnosis and management of ADHD and public opinion. This gap should be considered by professionals when counseling patients and caregivers or by the media when covering health-related issues about ADHD. The sensitive promotion of a multifactorial disease model, the consideration of multilevel preferences, and a thorough and balanced psychoeducation should form the cornerstone of therapeutic intervention, particularly in a disorder such as ADHD.
Supplemental Material
Supplemental material, Supplement for Attention Deficit Hyperactivity Disorder in Children and Adults: A Population Survey on Public Beliefs by Sven Speerforck, Johannes Hertel, Susanne Stolzenburg, Hans J. Grabe, Mauro G. Carta, Matthias C. Angermeyer and Georg Schomerus in Journal of Attention Disorders
Prioritisation of help-seeking and treatment recommendations. Weighted percentages of respondents that recommended the related professional (above) or treatment (below) the most after hearing the child (left) or adult (right) vignette. The recommendations for an educational psychologist or for a cure were asked vignette specific and are therefore highlighted separately.
Acknowledgments
The authors thank all participants for their participation in the study and their extra effort. Furthermore, we want to thank USUMA and all the participating interviewers for the skilled and thorough support in conducting this study. The authors thank Dr. Nicholas Meyer, Kings College London, for valuable comments on the manuscript.
Author Biographies
Sven Speerforck is working as an academic psychiatrist interested in attitude research at the University Medicine Greifswald and currently funded by the Gerhard Domagk postdoctoral scholarship awarded by the University Medicine Greifswald.
Johannes Hertel is a psychologist and biomathematician currently working in various interdisciplinary epidemiological research projects and specialized in statistical analysis.
Susanne Stolzenburg is a clinical psychologist working in the field of attitude research and untreated mental illness.
Hans J. Grabe is a psychiatrist and holds the chair of the Department of Psychiatry of the University Medicine Greifswald.
Mauro G. Carta holds the chair of Quality of Care—Applied Medical Technologies and is the head of the Liaison Psychiatry Unit at the University of Cagliari.
Matthias C. Angermeyer holds the chair emeritus of the Department of Psychiatry at Leipzig University and is among the most cited experts on population-based attitude research on mental health.
Georg Schomerus holds the chair of the Department of Psychiatry at Leipzig University and is an international expert on population-based attitude research and stigma.
Appendix
Child Vignette, Male
Since about a year, 12-year-old Robert often makes careless mistakes in schoolwork, has difficulty remaining focused during class, does not follow through on instructions, and fails to finish his schoolwork. In school as at home, Robert often does not seem to listen when spoken to directly and is often easily distracted by extraneous stimuli. He often loses things like keys or mobile telephones and is forgetful in daily activities like doing chores or running errands. Robert often fidgets with or taps hands or feet. He often leaves his place in the classroom or when sitting at the dining table. Unable to be still for an extended time, he is often “on the go” and acting as if “driven by a motor,” which is experienced by others as difficult to keep up with. Robert often talks excessively and blurts out an answer before a question has been completed. He often butts into conversations, games, or other activities and starts using other people’s things without asking or receiving permission. Several of these behaviors were already present prior to age 12. These behaviors interfere with Robert’s functioning in school and negatively affect relationships with adults and peers.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr. Sven Speerforck was funded by the Gerhard Domagk postdoctoral scholarship awarded by the University Medicine Greifswald. The study was supported by funds from the Institute for Social Psychiatry Mecklenburg-Vorpommern e.V.
Compliance With Ethical Standards: The study protocol was approved by the ethics committee of Greifswald University (BB 072/17). Our data will be made available to interested colleagues upon request
ORCID iD: Sven Speerforck  https://orcid.org/0000-0002-9281-8461
https://orcid.org/0000-0002-9281-8461
Supplemental Material: Supplemental material for this article is available online.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Angermeyer M. C., Holzinger A., Carta M. G., Schomerus G. (2011). Biogenetic explanations and public acceptance of mental illness: Systematic review of population studies. The British Journal of Psychiatry: The Journal of Mental Science, 199, 367-372. doi: 10.1192/bjp.bp.110.085563 [DOI] [PubMed] [Google Scholar]
- Angermeyer M. C., Matschinger H., Riedel-Heller S. G. (1999). Whom to ask for help in case of a mental disorder? Preferences of the lay public. Social Psychiatry & Psychiatric Epidemiology, 34, 202-210. doi: 10.1007/s001270050134 [DOI] [PubMed] [Google Scholar]
- Angermeyer M. C., Matschinger H., Schomerus G. (2017). 50 Jahre psychiatrische Einstellungsforschung in Deutschland. [50th Anniversary of Psychiatric Attitude Research in Germany.] Psychiatrische Praxis, 44, 377-392. doi: 10.1055/s-0043-105723 [DOI] [PubMed] [Google Scholar]
- Angermeyer M. C., Schomerus G. (2017). State of the art of population-based attitude research on mental health: A systematic review. Epidemiology and Psychiatric Sciences, 26, 252-264. doi: 10.1017/S2045796016000627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angermeyer M. C., van der Auwera S., Carta M. G., Schomerus G. (2017). Public attitudes towards psychiatry and psychiatric treatment at the beginning of the 21st century: A systematic review and meta-analysis of population surveys. World Psychiatry, 16, 50-61. doi: 10.1002/wps.20383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asherson P., Adamou M., Bolea B., Muller U., Morua S. D., Pitts M., Young S. (2010). Is ADHD a valid diagnosis in adults? Yes. British Medical Journal, 340, Article c549. doi: 10.1136/bmj.c549 [DOI] [PubMed] [Google Scholar]
- Asherson P., Akehurst R., Kooij J. J. S., Huss M., Beusterien K., Sasané R., . . . Hodgkins P. (2012). Under diagnosis of adult ADHD: Cultural influences and societal burden. Journal of Attention Disorders, 16(5 Suppl.), 20S-38S. doi: 10.1177/1087054711435360 [DOI] [PubMed] [Google Scholar]
- Association of the Scientific Medical Societies in Germany [Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V.] (2017). ADHD in children, adolescents and adults. [ADHS bei Kindern, Jugendlichen und Erwachsenen.] Retrieved from https://www.awmf.org/leitlinien/detail/ll/028-045.html
- Bachmann C. J., Philipsen A., Hoffmann F. (2017). ADHD in Germany: Trends in diagnosis and pharmacotherapy: A country-wide analysis of health insurance data on attention-deficit/hyperactivity disorder (ADHD) in children, adolescents and adults from 2009-2014. Deutsches Ärzteblatt International, 114, 141-148. doi: 10.3238/arztebl.2017.0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banaschewski T., Becker K., Dopfner M., Holtmann M., Rosler M., Romanos M. (2017). Attention-deficit/hyperactivity disorder. Deutsches Arzteblatt International, 114, 149-159. doi: 10.3238/arztebl.2017.0149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batstra L., te Meerman S., Conners K., Frances A. (2017). Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults. The Lancet Psychiatry, 4, 439. doi: 10.1016/S2215-0366(17)30107-4 [DOI] [PubMed] [Google Scholar]
- Boesen K., Saiz L. C., Erviti J., Storebø O. J., Gluud C., Gøtzsche P. C., Jørgensen K. J. (2017). The Cochrane Collaboration withdraws a review on methylphenidate for adults with attention deficit hyperactivity disorder. Evidence-Based Medicine, 22, 143-147. doi: 10.1136/ebmed-2017-110716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad P., Bergey M. R. (2014). The impending globalization of ADHD: Notes on the expansion and growth of a medicalized disorder. Social Science & Medicine, 122, 31-43. doi: 10.1016/j.socscimed.2014.10.019 [DOI] [PubMed] [Google Scholar]
- Dehue T., Bijl D., Winter M., de Scheepers F., Vanheule S., van Os J., . . . Verhoeff B. (2017). Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults. The Lancet Psychiatry, 4, 438-439. doi: 10.1016/S2215-0366(17)30158-X [DOI] [PubMed] [Google Scholar]
- Gerlach M., Banaschewski T., Coghill D., Rohde L. A., Romanos M. (2017). What are the benefits of methylphenidate as a treatment for children and adolescents with attention-deficit/hyperactivity disorder? Attention Deficit and Hyperactivity Disorders, 9, 1-3. doi: 10.1007/s12402-017-0220-2 [DOI] [PubMed] [Google Scholar]
- Gomes M., Palmini A., Barbirato F., Rohde L. A., Mattos P. (2007). Knowledge about attention-deficit hyperactivity disorder in Brazil. Jornal Brasileiro de Psiquiatria, 56, 94-101. doi: 10.1590/S0047-20852007000200004 [DOI] [Google Scholar]
- Häßler F. (2019). The use of stimulants for therapy of ADHD is harmful for growth and bone density—Pro. Psychiatrische Praxis, 46, 9-10. doi: 10.1055/a-0759-9374 [DOI] [Google Scholar]
- Hoogman M., Bralten J., Hibar D. P., Mennes M., Zwiers M. P., Schweren L. S. J., . . . Franke B. (2017). Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: A cross-sectional mega-analysis. The Lancet Psychiatry, 4, 310-319. doi: 10.1016/S2215-0366(17)30049-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy M., Kreppner J., Knights N., Kumsta R., Maughan B., Golm D., . . . Sonuga-Barke E. J. S. (2016). Early severe institutional deprivation is associated with a persistent variant of adult attention-deficit/hyperactivity disorder: Clinical presentation, developmental continuities and life circumstances in the English and Romanian Adoptees study. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 57, 1113-1125. doi: 10.1111/jcpp.12576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kölch M. (2019). The use of stimulants for therapy of ADHD is harmful for growth and bone density—Contra. Psychiatrische Praxis, 46, 10-11. doi: 10.1055/a-0759-9659 [DOI] [Google Scholar]
- Kvaale E. P., Gottdiener W. H., Haslam N. (2013). Biogenetic explanations and stigma: A meta-analytic review of associations among laypeople. Social Science & Medicine, 96, 95-103. doi: 10.1016/j.socscimed.2013.07.017 [DOI] [PubMed] [Google Scholar]
- McLeod J. D., Fettes D. L., Jensen P. S., Pescosolido B. A., Martin J. K. (2007). Public knowledge, beliefs, and treatment preferences concerning attention-deficit hyperactivity disorder. Psychiatric Services, 58, 626-631. doi: 10.1176/appi.ps.58.5.626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merten E. C., Cwik J. C., Margraf J., Schneider S. (2017). Overdiagnosis of mental disorders in children and adolescents (in developed countries). Child and Adolescent Psychiatry and Mental Health, 11, Article 5. doi: 10.1186/s13034-016-0140-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moncrieff J., Timimi S. (2010). Is ADHD a valid diagnosis in adults? No. British Medical Journal, 340, Article c547. doi: 10.1136/bmj.c547 [DOI] [PubMed] [Google Scholar]
- Mueller A. K., Fuermaier B. M., Koerts J., Tucha L. (2012). Stigma in attention deficit hyperactivity disorder. Attention Deficit and Hyperactivity Disorders, 4, 101-114. doi: 10.1007/s12402-012-0085-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. (2008). Attention deficit hyperactivity disorder: Diagnosis and management. Retrieved from https://www.nice.org.uk/guidance/cg72 [PubMed]
- Partridge B., Lucke J., Hall W. (2012). Public attitudes towards the acceptability of using drugs to treat depression and ADHD. Australian & New Zealand Journal of Psychiatry, 46, 958-965. doi: 10.1177/0004867412450755 [DOI] [PubMed] [Google Scholar]
- Partridge B., Lucke J., Hall W. (2014). Over-diagnosed and over-treated: A survey of Australian public attitudes towards the acceptability of drug treatment for depression and ADHD. BMC Psychiatry, 14(1), Article 74. doi: 10.1186/1471-244X-14-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescosolido B. A., Jensen P. S., Martin J. K., Perry B. L., Olafsdottir S., Fettes D. (2008). Public knowledge and assessment of child mental health problems: Findings from the National Stigma Study-Children. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 339-349. doi: 10.1097/CHI.0b013e318160e3a0 [DOI] [PubMed] [Google Scholar]
- Polanczyk G. V., de Lima M. S., Horta B. L., Biederman J., Rohde L. A. (2007). The worldwide prevalence of ADHD: A systematic review and metaregression analysis. The American Journal of Psychiatry, 164, 942-948. doi: 10.1176/ajp.2007.164.6.942 [DOI] [PubMed] [Google Scholar]
- Polanczyk G. V., Willcutt E. G., Salum G. A., Kieling C., Rohde L. A. (2014). ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. International Journal of Epidemiology, 43, 434-442. doi: 10.1093/ije/dyt261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedel-Heller S. G., Matschinger H., Angermeyer M. C. (2005). Mental disorders—Who and what might help? Social Psychiatry & Psychiatric Epidemiology, 40, 167-174. doi: 10.1007/s00127-005-0863-8 [DOI] [PubMed] [Google Scholar]
- Romanos M., Coghill D., Gerlach M., Becker K., Holtmann M., Döpfner M., Banaschewski T. (2016). Check and Double Check—The Cochrane review by Storebo et al. (2015) is indeed flawed. Zeitschrift fur Kinder- und Jugendpsychiatrie und Psychotherapie, 44, 336-337. doi: 10.1024/1422-4917/a000473 [DOI] [PubMed] [Google Scholar]
- Romanos M., Reif A., Banaschewski T. (2016). Methylphenidate for attention-deficit/hyperactivity disorder. Journal of the American Medical Association, 316, 994-995. doi: 10.1001/jama.2016.10279 [DOI] [PubMed] [Google Scholar]
- Royston P. (2005). Multiple imputation of missing values: Update of ice. Stata Journal, 5, 527-536. [Google Scholar]
- Schomerus G., Matschinger H., Angermeyer M. C. (2014). Causal beliefs of the public and social acceptance of persons with mental illness: A comparative analysis of schizophrenia, depression and alcohol dependence. Psychological Medicine, 44, 303-314. doi: 10.1017/S003329171300072X [DOI] [PubMed] [Google Scholar]
- Simon V., Czobor P., Bálint S., Mészáros A., Bitter I. (2009). Prevalence and correlates of adult attention-deficit hyperactivity disorder: Meta-analysis. The British Journal of Psychiatry: The Journal of Mental Science, 194, 204-211. doi: 10.1192/bjp.bp.107.048827 [DOI] [PubMed] [Google Scholar]
- Speerforck S., Schomerus G., Matschinger H., Angermeyer M. C. (2017). Treatment recommendations for schizophrenia, major depression and alcohol dependence and stigmatizing attitudes of the public: Results from a German population survey. European Archives of Psychiatry and Clinical Neuroscience, 267, 341-350. doi: 10.1007/s00406-016-0755-9 [DOI] [PubMed] [Google Scholar]
- Speerforck S., Schomerus G., Pruess S., Angermeyer M. C. (2014). Different biogenetic causal explanations and attitudes towards persons with major depression, schizophrenia and alcohol dependence: Is the concept of a chemical imbalance beneficial? Journal of Affective Disorders, 168, 224-228. doi: 10.1016/j.jad.2014.06.013 [DOI] [PubMed] [Google Scholar]
- StataCorp L. P. (2013). Stata Statistical Software: Release 13. College Station, TX: StataCorp LP. [Google Scholar]
- Storebø O. J., Ramstad E., Krogh H. B., Nilausen T. D., Skoog M., Holmskov M., . . . Gluud C. (2015). Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD). The Cochrane Database of Systematic Reviews, 11, CD009885. doi: 10.1002/14651858.CD009885.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A., Cooper M. (2016). Attention deficit hyperactivity disorder. The Lancet, 387, 1240-1250. doi: 10.1016/S0140-6736(15)00238-X [DOI] [PubMed] [Google Scholar]
- van Buuren S., Boshuizen H. C., Knook D. L. (1999). Multiple imputation of missing blood pressure covariates in survival analysis. Statistics in Medicine, 18, 681-694. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplement for Attention Deficit Hyperactivity Disorder in Children and Adults: A Population Survey on Public Beliefs by Sven Speerforck, Johannes Hertel, Susanne Stolzenburg, Hans J. Grabe, Mauro G. Carta, Matthias C. Angermeyer and Georg Schomerus in Journal of Attention Disorders
Prioritisation of help-seeking and treatment recommendations. Weighted percentages of respondents that recommended the related professional (above) or treatment (below) the most after hearing the child (left) or adult (right) vignette. The recommendations for an educational psychologist or for a cure were asked vignette specific and are therefore highlighted separately.