Abstract
Carbapenem-resistant gram-negative bacteria are an increasingly significant clinical threat globally. This risk may be underestimated in Kenya as only four carbapenemase genes in three bacterial species have been described. The study aimed to understand the antibiotic resistance profiles, genes, sequence types, and distribution of carbapenem-resistant gram-negative bacteria from patients in six hospitals across five Kenyan counties by bacterial culture, antibiotic susceptibility testing, and whole-genome sequence analysis. Forty-eight, non-duplicate, carbapenem non-susceptible, clinical isolates were identified across the five counties (predominantly in Nairobi and Kisii): twenty-seven Acinetobacter baumannii, fourteen Pseudomonas aeruginosa, three Escherichia coli, two Enterobacter cloacae, and two Klebsiella pneumoniae. All isolates were non-susceptible to β-lactam drugs with variable susceptibility to tigecycline (66%), minocycline (52.9%), tetracycline (29.4%), and levofloxacin (22.9%). Thirteen P. aeruginosa isolates were resistant to all antibiotics tested. Eleven carbapenemase genes were identified: blaNDM-1, blaOXA-23, -58, -66, -69, and -91 in A. baumannii (STs 1, 2, 164 and a novel ST1475), blaNDM-1 in E. cloacae (STs 25,182), blaNDM-1, blaVIM-1and -6, blaOXA-50 in P. aeruginosa (STs 316, 357, 654, and1203), blaOXA-181, blaNDM-1 in K. pneumoniae (STs 147 and 219), and blaNDM-5 in E. coli (ST164). Five A. baumannii isolates had two carbapenemases, blaNDM-1, and either blaOXA-23 (4) or blaOXA-58 (1). AmpC genes were detected in A. baumannii (blaADC-25), E. cloacae (blaDHA-1 and blaACT-6, 16), and K. pneumoniae (blaCMY). Significant multiple-drug resistant genes were the pan-aminoglycoside resistance16srRNA methyltransferase armA, rmtB, rmtC, and rmtF genes. This study is the first to report blaOXA-420, -58, -181, VIM-6, and blaNDM-5 in Kenyan isolates. High-risk STs of A. baumannii (ST1475, ST2), E. cloacae ST182, K. pneumoniae ST147, P. aeruginosa (ST357, 654), and E. coli ST167, ST648 were identified which present considerable therapeutic danger. The study recommends urgent carbapenem use regulation and containment of high-risk carbapenem-resistant bacteria.
Introduction
Multidrug resistance among clinically significant gram-negative bacteria (GNB) (Escherichia coli, Klebsiella pneumoniae, Enterobacter spp. Pseudomonas aeruginosa, and Acinetobacter baumannii) has led to increased morbidity and an estimated 40% mortality in developing countries [1, 2]. These adverse outcomes are due to treatment options being limited to expensive, often unavailable, last-line drugs such as tigecycline. Carbapenems are an important β-lactam drug class used to treat serious multidrug-resistant bacterial infections. Therefore, the global increase in carbapenem resistance (CR) has been recognized as a severe health threat [3].
CR is mediated primarily by the expression of chromosomally-encoded or plasmid-encoded carbapenemases that fall into three classes: Class A (e.g., K. pneumoniae carbapenemases (KPC), Class B (e.g., New Delhi Metallo-β-lactamase (NDM), the Verona integrin-encoded Metallo-β-lactamase (VIM), and Imipenemase (IMP), and Class D (e.g.OXA-48 and -181) [4]. Secondary mechanisms for CR are the constitutive over-production of AmpC and changes in permeability due to loss or down-regulation of porins [5].
The global spread of CR is due to the carriage of CR genes on mobile genetic elements (plasmids, transposons, and integrons). These elements also harbor genes that confer resistance against multiple antibiotic classes [6, 7]. With the increased use of carbapenems, the prediction is that GNB will evolve to accumulate multiple CR genes and mechanisms of resistance [8]. This further increases the likelihood and clinical threat of the emergence of extensively drug-resistant (XDR) GNB. Growing global diversity and distribution of CR genes, which have been described extensively [9–12], and the identification of high-risk XDR strain types (STs) associated with outbreaks, further anchors this prediction. These high-risk clones include the international clone I-III [13] of A. baumannii, ST235, ST357, and ST664 of P. aeruginosa, ST258, and ST307 of K. pneumoniae [14, 15] and ST78 of Enterobacter cloacae [16].
Carbapenem resistance is a growing problem in Africa, with a reported prevalence ranging from <1% to 60% among GNB [17–19]. Recent studies in Tanzania and Uganda have shown that this prevalence could be as high as 22.4–35% with the circulation of CR genes blaVIM, blaOXA-48, blaIMP, blaKPC, and blaNDM-1 predominantly among K. pneumonia and P. aeruginosa [20, 21]. In Kenya, only the carbapenemase genes blaNDM-1 in K. pneumoniae, P. aeruginosa and A. baumannii, blaOXA-23 in A. baumannii [22–24], blaSPM in K. pneumoniae [25], and blaVIM-2 in P. aeruginosa [26] have been identified. These are from hospitals in three Kenyan counties: Nairobi, Kiambu, and Kilifi. With increasing carbapenem use in Kenya because of the high levels of ESBL-producing Enterobacteriaceae [27–29], a concomitant rise in CR is expected that warrants close monitoring.
This study aimed to address the limited data available on the diversity and distribution of carbapenemase and other antibiotic resistance genes and strain types of clinically relevant C-NS GNB. The focus was on five bacterial species: E. coli, K. pneumoniae, A. baumannii, P. aeruginosa, and Enterobacter spp. from clinical isolates in hospitals from five Kenyan counties. The research demonstrated a greater variety and distribution of carbapenemase genes in Kenya than previously recognized. It further identified the therapeutic risks associated with CR infections and identified high-risk, multidrug-resistant strains. These findings underscore the importance of targeted surveillance and control of C-NS GNB.
Materials and methods
Ethics and approvals
This study was approved by the Kenya Medical Research Institute (KEMRI) Scientific and Ethics Review Unit (#2767), the Walter Reed Army Institute of Research (WRAIR) Institutional Review Board (#2089), and the U.S. Army Medical Research and Materiel Command, Office of Research Protection, Human Research Protections Office (USAMRMC ORP HRPO) (Log#A-18129). The investigators adhered to the policies for the protection of human subjects as prescribed in AR 70–25. Study participants provided written consent to participate in the study.
Isolate culture and antimicrobial susceptibility testing
A. baumannii, P. aeruginosa, Enterobacter spp., K. pneumoniae, and E. coli isolates were obtained from patients with skin and soft tissue infections (SSTI) and urinary tract infections (UTI). These patients were enrolled in an antimicrobial resistance surveillance study conducted between 2015 to 2018 in six hospitals in 5 Kenyan counties: Nairobi, Kisumu, Kisii, Kilifi, and Kericho. The Nairobi and Kisii county hospitals are full-service teaching and referral hospitals with large inpatient capacities. In contrast, the other four hospitals are county or sub-county level hospitals that offer primary outpatient care, surgical, laboratory, maternity, and inpatient services.
Demographic and clinical information was collected from each study subject. The isolates were identified, and antimicrobial susceptibility testing performed on the VITEK 2® automated platform (bioMérieux, Marcy l’Etoile, France) using the GN-ID and XN05 AST cards. Only one isolate was tested on a Microscan (Beckman Coulter, Indianapolis, USA). The antibiotics reported in this study are ceftriaxone, cefepime, ticarcillin-clavulanic acid, piperacillin, meropenem, levofloxacin, tetracycline, tigecycline, and minocycline. Minimum inhibitory concentration (MIC) data for each organism were interpreted according to the Clinical and Laboratory Standards Institute guidelines (2015) and the VITEK 2® Advanced Expert System (AES). All non-duplicate carbapenem non-susceptible (C-NS) isolates, both intermediate and resistant to meropenem, detected from 2015 to 2018 were selected for further analysis.
Genomic characterization and strain typing
Whole-genome sequencing was performed on C-NS isolates to detect the antibiotic resistance genes. DNA was extracted using the DNeasy UltraClean Microbial Kit (Qiagen, Germantown, MD, USA), and libraries constructed using the KAPA HyperPlus Library preparation kit (Roche Diagnostics, Indianapolis, Indiana, USA). These libraries were quantified using the KAPA Library Quantification Kit–Illumina/Bio-Rad iCycler™ (Roche Diagnostics, Indianapolis, Indiana, USA) and sequenced with a MiSeq Reagent Kit v3 (600 cycles) on an Illumina MiSeq desktop sequencer (Illumina Inc., San Diego, CA, USA). Species identification and contamination detection were performed from sequencing reads using Kraken2 [30]. The reads were trimmed for adapter content and quality, followed by de novo assembly using Newbler v2.7. Antimicrobial resistance genes were annotated using ResFinder v3.2 [31], and MLST assignment performed using parsed nucleotide BLAST results against the relevant schema hosted by PubMLST [32]. Whole-genome sequences are deposited in GenBank® BioProject IDs PRJNA636771 and PRJNA555206. For isolates with no assigned sequence types (STs), genome assemblies were submitted to PubMLST for strain assignment using the BIGSdb software [33].
Data management and analysis
Patient data (clinical and demographic) and the antimicrobial susceptibility (AS) data for each isolate extracted from the automated platforms were compiled in a Microsoft Access database. These compiled data were transferred to Microsoft Excel for descriptive statistical analysis with frequency distributions and the results summarized in tables.
Results
Demographic and clinical characteristics of subjects
C-NS isolates were identified from forty-eight subjects in all the five study counties. Demographic and clinical information was available for all but one subject, KPA1. The majority of the C-NS isolates were from subjects in the larger referral hospitals in Nairobi (29, 60.4%) and Kisii counties (11, 22.9%). Approximately 69% of the isolates were from male subjects, 87% were inpatient, and 64% were healthcare-associated infections (HAI) per the CDC/NHSN Surveillance Definition of Healthcare-Associated Infection [34]. Approximately 64% (30/47) of isolates were from SSTI, including ear infections, injury wounds, cellulitis, abscesses, burns, bedsores, cancer lesions, amputation sites, and surgical site infections. The remaining 36% (17/47) of the isolates were from inpatient subjects with UTIs, of which 70.5% (12/17) were catheter-associated (Table 1).
Table 1. Characteristics of subjects from whom C-NS isolates were obtained.
| Isolate ID | County | Sex | Patient type | Infection type | Infection site | Infection acquisition |
|---|---|---|---|---|---|---|
| Acinetobacter baumannii | ||||||
| KAB1 | Nairobi | F | Inpatient | SSTI | Leg | CAI |
| KAB2 | Nairobi | M | Inpatient | UTI | Catheter | CAI |
| KAB3 | Nairobi | M | Inpatient | UTI | Catheter | HAI |
| KAB4 | Nairobi | M | Inpatient | UTI | Catheter | HAI |
| KAB5 | Nairobi | M | Inpatient | SSTI | Catheter | HAI |
| KAB6 | Nairobi | M | Inpatient | SSTI | Leg | unclear |
| KAB7 | Nairobi | M | Inpatient | SSTI | Leg | HAI |
| KAB8 | Kisumu | F | Outpatient | UTI | Catheter | HAI |
| KAB9 | Nairobi | M | Inpatient | UTI | na | HAI |
| KAB10 | Nairobi | F | Inpatient | SSTI | Leg | HAI |
| KAB11 | Nairobi | F | Outpatient | SSTI | Foot | HAI |
| KAB12 | Kericho | F | Inpatient | SSTI | Leg | CAI |
| KAB13 | Kisii | F | Inpatient | SSTI | Leg | HAI |
| KAB14 | Kisii | M | Inpatient | SSTI | Leg | CAI |
| KAB15 | Kisumu | F | Inpatient | UTI | Catheter | HAI |
| KAB16 | Kisumu | F | Inpatient | SSTI | Trunk | HAI |
| KAB17 | Kisii | F | Inpatient | SSTI | Breast | CAI |
| KAB18 | Kisii | M | Inpatient | SSTI | Thigh | HAI |
| KAB19 | Kisii | M | Inpatient | SSTI | Scrotum | CAI |
| KAB20 | Kisii | F | Inpatient | SSTI | Buttocks | CAI |
| KAB21 | Kisii | F | Inpatient | SSTI | Breast | CAI |
| KAB22 | Kisii | M | Outpatient | SSTI | Leg | CAI |
| KAB23 | Kisii | M | Inpatient | SSTI | Foot | CAI |
| KAB24 | Kisii | F | Inpatient | SSTI | Abdomen | HAI |
| KAB25 | Kericho | M | Inpatient | SSTI | Thigh | CAI |
| KAB26 | Kericho | M | Inpatient | SSTI | Thigh | CAI |
| KAB27 | Kisumu | M | Inpatient | SSTI | Penis | CAI |
| Enterobacter cloacae | ||||||
| KEB1 | Nairobi | M | Inpatient | UTI | Catheter | HAI |
| KEB2 | Nairobi | M | Inpatient | SSTI | Arm | HAI |
| Escherichia coli | ||||||
| KEC1 | Kisii | F | Inpatient | SSTI | Back | CAI |
| KEC2 | Nairobi | M | Inpatient | UTI | na | HAI |
| KEC3 | Nairobi | F | Inpatient | SSTI | na | HAI |
| Klebsiella pneumoniae | ||||||
| KKPI | Nairobi | M | Outpatient | SSTI | Leg | CAI |
| KKP2 | Kilifi | M | Outpatient | SSTI | Leg | CAI |
| Pseudomonas aeruginosa | ||||||
| KPA1 | Nairobi | na | na | na | na | na |
| KPA2 | Nairobi | M | Inpatient | UTI | Catheter | HAI |
| KPA3 | Nairobi | M | Inpatient | UTI | Clean-catch | CAI |
| KPA4 | Nairobi | M | Inpatient | UTI | Catheter | HAI |
| KPA5 | Nairobi | M | Inpatient | UTI | na | HAI |
| KPA6 | Nairobi | M | Inpatient | UTI | Catheter | HAI |
| KPA7 | Nairobi | M | Inpatient | SSTI | Leg wound | HAI |
| KPA8 | Nairobi | M | Inpatient | SSTI | na | HAI |
| KPA9 | Nairobi | M | Inpatient | SSTI | na | HAI |
| KPA10 | Nairobi | M | Inpatient | UTI | Catheter | HAI |
| KPA11 | Nairobi | M | Inpatient | SSTI | Buttocks | HAI |
| KPA12 | Nairobi | M | Inpatient | UTI | na | HAI |
| KPA13 | Nairobi | M | Inpatient | UTI | na | HAI |
| KPA14 | Nairobi | M | Outpatient | UTI | Catheter | CAI |
SSTI, skin and soft tissue; UTI, urinary tract infections; CAI, community-acquired infection; HAI, healthcare-associated infection; M, male; F, female; na, information not available.
Identity and antimicrobial susceptibility patterns of carbapenem-non-susceptible isolates
The forty-eight isolates selected based on their non-susceptibility to meropenem (Table 2) were: twenty-seven A. baumannii, fourteen P. aeruginosa, three E. coli, two E. cloacae, and two K. pneumoniae (Tables 1 and 2). All isolates were resistant to meropenem except for three A. baumannii isolates (KAB14, 15, 16). These had intermediate resistance (MIC = 8), or AES interpreted intermediate resistance (MIC = 4). All the isolates were resistant to penicillin, penicillin/β-lactamase inhibitor combination, and cephalosporin drugs tested. The only exception was a single isolate (KPA3) that was susceptible to cefepime. The isolates were most susceptible to tigecycline (66%), followed by minocycline (52.9%), tetracycline (29.4%), and levofloxacin (22.9%). All fourteen P. aeruginosa isolates, two A. baumannii (KAB4, KAB6) and one K. pneumoniae (KKP1) isolates were resistant to all antibiotics tested. Eight A. baumannii isolates (KAB1-3, 7, 9–11, 13, 25–27), three E. coli (KEC1, 2, 3), and one E. cloacae (KEB1) were resistant to all but tigecycline.
Table 2. Antimicrobial susceptibility profiles of the C-NS bacterial isolates.
| Isolate ID | Antibiotic susceptibility test MICs in μg/mL (Interpretation) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| MEM | CRO | PIP | TIM | FEP | LVX | TET | MIN | TGC | |
| Acinetobacter baumannii (n = 27) | |||||||||
| KAB1 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | 4 (S) | 1 (S) |
| KAB2 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | 4 (S) | 1 (S) |
| KAB3 | > = 16 (R) | > = 64 (R) | > = 128 (R) | nd | > = 64 (R) | > = 8 (R) | > = 16 (R) | 4 (S) | 1 (S) |
| KAB4 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | > = 16 (R) | > = 8 (R) |
| KAB5 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | 4 (S) | 2 (S) |
| KAB6 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | > = 16 (R) | 4 (I) |
| KAB7 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | 8 (I) | 2 (S) |
| KAB8 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | 0.5 (S) | > = 16 (R) | < = 1 (S) | 2 (S) |
| KAB9 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | 8 (I) | 2 (S) |
| KAB10 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | 8 (I) | 2 (S) |
| KAB11 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | 8 (I) | 2 (S) |
| KAB12 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | 2 (S) | 2 (S) |
| KAB13 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | 4 (R) | > = 16 (R) | > = 16 (R) | 2 (S) |
| KAB14 | 8 (I) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | 4 (R) | > = 16 (R) | < = 1 (S) | < = 0.5 (S) |
| KAB15 | 4 (I*) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | 4 (R) | 2 (S) | < = 1 (S) | < = 0.5 (S) |
| KAB16 | 8 (I) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | 4 (R) | 4 (S) | < = 1 (S) | < = 0.5 (S) |
| KAB17 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | < = 0.12 (S) | 4 (S) | < = 1 (S) | 1 (S) |
| KAB18 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | < = 0.12 (S) | 4 (S) | < = 1 (S) | 1 (S) |
| KAB19 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | 0.25 (S) | 8(I) | 2 (S) | 4 (I) |
| KAB20 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | < = 0.12 (S) | 4 (S) | < = 1 (S) | < = 0.5 (S) |
| KAB21 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | < = 0.12 (S) | 4 (S) | < = 1 (S) | < = 0.5 (S) |
| KAB22 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | < = 0.12 (S) | 4 (S) | 2 (S) | 1 (S) |
| KAB23 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | < = 0.12 (S) | 4 (S) | < = 1 (S) | 1 (S) |
| KAB24 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | < = 0.12 (S) | 4 (S) | 2 (S) | < = 0.5 (S) |
| KAB25 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | 4 (R) | > = 16 (R) | > = 16 (R) | 1 (S) |
| KAB26 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | 4 (R) | > = 16 (R) | > = 16 (R) | 2 (S) |
| KAB27 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | 4 (R) | 8 (I) | > = 16 (R) | 2 (S) |
| Enterobacter cloacae (n = 2) | |||||||||
| KEB1 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | > = 16 (R) | 2 (S) |
| KEB2 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | 32 (R) | 0.25 (S) | 4 (S) | > = 16 (R) | 2 (S) |
| Escherichia coli (n = 3) | |||||||||
| KEC1 | 8 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | > = 16 (R) | < = 0.5 (S) |
| KEC2 | 8 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | > = 16 (R) | < = 0.5 (S) |
| KEC3 | 8 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | > = 16 (R) | < = 0.5 (S) |
| Klebsiella pneumoniae(n = 2) | |||||||||
| KKPI | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | > = 16 (R) | > = 16 (R) | > = 8 (R) |
| KKP2 | > = 16 (R) | > = 64 (R) | > = 128 (R) | > = 128 (R) | 16 (R) | 1 (S) | > = 16 (R) | 4 (S) | < = 0.5 (S) |
| Pseudomonas aeruginosa(n = 14) | |||||||||
| KPA1 | > = 8 (R)# | nd | >64 (R) # | nd | >8 (R) # | > = 4 (R) # | nd | nd | nd |
| KPA2 | > = 16 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA3 | > = 16 (R) | nd | 64 (R) | > = 128 (R) | 8 (S) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA4 | > = 16 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA5 | > = 16 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA6 | > = 16 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA7 | > = 16 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA8 | > = 16 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA9 | > = 16 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA10 | > = 8 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA11 | > = 8 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA12 | > = 16 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA13 | > = 16 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| KPA14 | > = 8 (R) | nd | > = 128 (R) | > = 128 (R) | > = 64 (R) | > = 8 (R) | nd | nd | > = 8 (R) |
| No. tested | 48 | 34 | 48 | 46 | 48 | 48 | 34 | 34 | 47 |
| No. susceptible (S) | 0 | 0 | 0 | 0 | 1 | 11 | 10 | 18 | 31 |
| % S | 0.0 | 0.0 | 0.0 | 0 | 2.1 | 22.9 | 29.4 | 52.9 | 66.0 |
MIC values that indicate non-susceptibility to the antibiotic are shaded grey.
The %S is the number of susceptible isolates as a percentage of all isolates tested for each antibiotic.
MIC, minimum inhibitory concentration; CRO, ceftriaxone; FEP, cefepime; TIM, ticarcillin-clavulanic acid; PIP, piperacillin; MEM, meropenem; LVX, levofloxacin; TET, tetracycline; TGC, tigecycline; MIN, minocycline; nd, antibiotics not tested.
*Non-susceptibility inferred by the VITEK 2® AES system.
# AST performed on a Microscan platform.
Carbapenemase genes detected across bacterial species
Eleven different carbapenemases from the class B Metallo-β-lactamases (blaNDM-1, blaNDM-5, blaVIM-2, and blaVIM-6) and the Class D oxacillinases (blaOXA-23, blaOXA-50, blaOXA-58, blaOXA-181, blaOXA-66, blaOXA-69, blaOXA-91) were detected in the 48 isolates (Tables 3 and 4).
Table 3. The diversity of carbapenemase genes identified among the bacterial species.
| Carbapenemase Ambler Class | B: Metallo- β lactamases | Class D: Oxacillinases | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bacterial species | NDM-1 | NDM-5 | VIM-1 | VIM-6 | OXA-23 | OXA-58 | OXA-66 | OXA-69 | OXA-91 | OXA-181 | OXA-50 |
| A. baumannii | 7 | 23 | 1 | 11 | 13 | 2 | |||||
| E. cloacae | 2 | ||||||||||
| P. aeruginosa | 11 | 1 | 2 | 1 | |||||||
| K. pneumoniae | 1 | 1 | |||||||||
| E. coli | 3 | ||||||||||
| No of occurrences | 21 | 3 | 1 | 2 | 23 | 1 | 11 | 13 | 2 | 1 | 1 |
| (n = 79) (%) | (26.6) | (3.8) | (1.3) | (2.5) | (29.1) | (1.3) | (13.9) | (16.5) | (2.5) | (1.3) | (1.3) |
NDM, New Delhi Metallo-β-lactamase; OXA, oxacillinase; VIM, Verona integron-encoded Metallo-β-lactamase.
Table 4. Distribution of drug resistance genes among the C-NS species and strain types.
| Isolate IDs | Species (No. of isolates) | ST | Carbapenemases | Penicillinases and β-lactamases * | Aminoglycoside resistance genes # | Efflux genes | Other significant antibiotic resistance genes |
|---|---|---|---|---|---|---|---|
| KAB18-20 | AB (3) | 1 | OXA-23, 69 | ADC-25 | sul2 | ||
| KAB17,21–24 | AB (5) | 1 | OXA-23, 69 | ADC-25 | ant(2’’)-Ia | sul2 | |
| KAB25, 26,27 | AB (3) | 1 | NDM-1, OXA-23, 69 | ADC-191 | aac(3)-I, aadA1, adeC aph(3’)-Ia, aph(3’’)-Ib, aph(3’)-Via, aph(6)-Id ant(3’’)-Iia | amvA | ble, dfrA1, sat2, sul1/2, tetB |
| KAB16 | AB (1) | 1 | NDM-1, OXA-69 | ADC-25, CARB-16 | aadA1, aph(3’)-Ia, aph(3’)-VI | mphE, msrE, sul2, dfrA1 | |
| KAB1-5,7,9, 10 | AB (8) | 2 | OXA-23, OXA-66 | ADC-25, TEM-1D | armA, aph(3’’)-Ib, aph(3’)-Ia, aph(6)-Id | mphE, msrE, tetB, sul2 | |
| KAB6,11 | AB (2) | 2 | OXA-23, OXA-66 | ADC-25, TEM-1D | armA aph(3’’)-Ib, aph(3’)-Ia, aph(6)-Id | mphE, msrE, tetB | |
| KAB12 | AB (1) | 2 | OXA-23, OXA-66 | ADC-25, TEM-1D | aac(3)-Ia, aadA1,aph(3’)-Ia | mphE, msrE, sul1/2 | |
| KAB13 | AB (1) | 1475 | NDM-1, OXA-23, 69 | ADC-25 | aac(3)-Ia, aadA1, aph(3’’)-Ib, aph(3’)-Ia, aph(3’)-Via, aph(6)-Id | dfrA1, sul1/2, tetB | |
| KAB8 | AB (1) | 374 | NDM-1 | ADC-26, OXA-259, CARB-16 | aadA1, ant(2’’)-Ia, ant(3’’)-Iia, aph(3’)-Ia | amvA | ble, dfrA1, mphE, msrE, sat2, sul2, tet39 |
| KAB14 | AB (1) | 164 | NDM-1, OXA-58, 91 | CARB-16 | aac(3)-Iid, ant(2’’)-Ia, aph(3’’)-Ib, aph(3’)-Ia, aph(3’)-Via, aph(6)-Id | floR, mphE, msrE, tet39, sul2 | |
| KAB15 | AB (1) | 164 | OXA-420, 91 | CARB-16 | ant(2’’)-Ia, aph(3’’)-Ib, aph(3’)-Ia, aph(6)-Id | dfrA20, sul2 | |
| KEB1 | ECL (1) | 182 | NDM-1 | ACT-16, DHA-1 TEM-1B, OXA-1 | rmtC, aac(6’)-Ib-cr, aph(3’’)-Ib, aph(3’)-Ia, aph(6)-Id | oqxA/B, mdfA | arr-3, catA2/B3, dfrA14, fosA, mphA, qnrB4, sul1/2, tetA/D |
| KEB2 | ECL (1) | 25 | NDM-1 | DHA-1 ACT-6 | oqxA/B, mdfA | ||
| KEC1 | EC (1) | 167 | NDM-5 | CTX-M-15, OXA-1, TEM-1B | rmtB, aac(6’)-Ib-cr, aadA2 | mdfA | catB3, dfrA12, mphA, sul1, tetA |
| KEC2 | EC (1) | 167 | NDM-5 | CTX-M-15, EC, OXA-1 | aac(6’)-Ib-cr5, aadA5 | acrF, mdtM, emrD | ble, dfrA17, mphA, sul1, tetA |
| KEC3 | EC (1) | 648 | NDM-5 | CTX-M-15, EC, OXA-1, TEM-1 | aac(3)-Iia, aac(6’)-Ib-cr5, aac(3)-Iia, aac(6’)-Ib-cr5, aadA5 | acrF, mdtM, emrD | ble, catA1, dfrA17, mphA, sul1, tetB |
| KKPI | KP (1) | 147 | OXA-181 | CTX-M-15, SHV-67, TEM-1B | rmtF, aac(6’)-Ib3, aph(3’’)-Ib, aph(6)-Id | mdfA, oqxA/B | arr-2, dfrA14, fosA, mphA, sul2 |
| KKP2 | KP (1) | 219 | NDM-1 | CMY, CTX-M-15, SHV-1 | rmtC aac(6’)-Ib3, aadA2, aph(3’)-Ia, aph(3’’)-Ib, aph(6)-Id | oqxA10/B5, kdeA, emrD | ble, dfrA12, floR, fosA, mphA, qnrS1, sul1/2, tetA |
| KPA2-5 | PA (4) | 357 | NDM-1, OXA-50 | OXA-10, PAO,VEB-1 | aph(3’)-Iib, aadA1, ant(2’’)-Ia, aac(6’)-Il, aph(3’)-VI | catB7, fosA, sul1, cmlA1, dfrB2, arr-3, tetA | |
| KPA9-13 | PA (5) | 357 | NDM-1 | OXA-10, OXA-846, PDC-11, VEB-9 | aac(6’)-Il, aadA1, aac(6’)-Il, ant(2’’)-Ia, aph(3’)-Iib, aph(3’)-VI | mexA/E/X | arr-3, ble, catB7, cmlA5, dfrB2, fosA, sul1, tetA |
| KPA14 | PA (1) | 357 | NDM-1 | OXA-396, PDC-3 | ant(4’)-Iib, aph(3’’)-Ib, aph(3’)-Iib, aph(6)-Id | mexE | catB7, fosA, sul1 |
| KPA6 | PA (1) | 654 | NDM-1 | OXA-396, PAO | aph(3’’)-Ib, aph(6)-Id, ant(4’)-Iib, aph(3’)-Iib | catB7, fosA, sul1 | |
| KPA1 | PA (1) | 316 | VIM-1 | OXA-10, OXA-395, PAO | aph(3’’)-Ib, aph(6)-Id, aph(3’)-Iib, aac(6’)-Ib3 | catB7, fosA, sul1, tetG, floR | |
| KPA7 | PA (1) | 1203 | VIM-6 | OXA-10, OXA-395, PAO | aph(3’)-Iib, aadA1, ant(2’’)-Ia, aac(6’)-Ib3 | catB7, fosA, sul1, qnrVC1, dfrA5, dfrB5, ereA | |
| KPA8 | PA (1) | 1203 | VIM-6 | OXA-10, OXA-395, PAO | aph(3’)-Iib, aadA1, ant(2’’)-Ia, aac(6’)-Ib3 | catB7, fosA, sul1, qnrVC1, dfrA5/B5, ereA |
PA, P. aeruginosa; KP, K. pneumoniae; EC, E. coli; ECL, E. cloacae; AB, A. baumannii. Antibiotic resistance gene families: AmpC: CMY, ADC-25, ACT-16, DHA-1, ESBL: CTX-M, SHV, TEM. Antibiotic resistance gene targets: Bleomycin-ble; Rifampicin-arr-2, arr-3; Chloramphenicols-catA1, catA2,catB3, catB7, cmlA5, cmlA1, floR; Fosfomycin-fosA;Tetracylines- tetA, B, D, G, and 39; Sulfonamides—sul1and 2; Erythromycin—ereA; Trimethoprim—dfrA1, A5, A12, A14, A17, A20, B2, and B5; Quinolones—qnrVC1, S1, and B4; Macrolides—msrE, mphA, and E; Streptothricin—sat2.
*AmpC genes are highlighted in bold.
#The16srRNA methyltransferases are highlighted in bold.
The oxacillinases were the most abundant carbapenemases (23/79, 29.1%) detected mostly in A. baumannii isolates. Among the A. baumannii isolates, the predominant genes were blaOXA-23, 66, and 69, with only a few isolates bearing blaOXA-58 and blaOXA-91. The blaOXA-181 and blaOXA-50 genes were detected in K. pneumonia and P. aeruginosa isolates, respectively. Among the Metallo- β–lactamases, blaNDM1 (21/79, 26.6%) was detected in A. baumannii, E. cloacae, P. aeruginosa, and K. pneumoniae species. blaVIM-1 and blaVIM-6 genes were detected in three P. aeruginosa isolates and blaNDM-5 genes in three E. coli isolates. The greatest diversity of carbapenemases was found among A. baumannii (blaNDM-1, blaOXA-23, 58, 66, 69, 91,) and P. aeruginosa (blaVIM-1, 6, blaNDM-1, blaOXA-50) (Table 3). Although most isolates had a single carbapenemase gene, five A. baumannii isolates (blaOXA-23/ blaNDM-1 (KAB13, 25, 26, 27) and blaNDM1/blaOXA-58 (KAB 14) and four P. aeruginosa isolates (KPA2-5) (blaNDM-1, blaOXA-50) (Table 4) bore both a Class B and D carbapenemase gene. Genes for AmpC were detected among 17/27 A. baumannii (blaADC-25), E. cloacae (blaDHA-1 and blaACT-16), and K. pneumoniae (blaCMY) isolates (Table 4).
Detection of other antimicrobial resistance genes among C-NS isolates
Given the phenotypic evidence of multidrug resistance in the C-NS isolates, it was unsurprising to find resistance genes against all significant antibiotic classes. Aminoglycoside resistance genes (aph, aac, aad, ade, acr, and ant gene families) were detected among all but one E. cloacae and three A. baumannii isolates. Apart from these genes specific to different aminoglycosides, the potent acquired 16srRNA methyltransferase genes (armA, rmtA, rmtC, and rmtF), which confer pan-aminoglycoside resistance, were detected among A. baumannii, E. cloacae, K. pneumoniae, and E. coli (Table 4). These genes render this drug class virtually ineffective in the treatment of C-NS infections. Sulfonamide resistance genes (sul1/2) were detected in all isolates but one E. cloacae and two A. baumannii isolates. Various macrolide (mphE, msrE, mphA, ereA), trimethoprim (dfrA and B), chloramphenicol (catA and B, floR, cm1) and tetracycline genes (tetA, B, D, G, 39) were detected across all species (Table 4). Less frequently identified were resistance genes for quinolone, rifampin, and fosfomycin, as described in Table 4. Genes for efflux pumps that contribute to multidrug resistance (amvA, oqxA/B, mdfA, mexA, E, and X, kdeA, acrF, emrD) were also detected, particularly among E. cloacae, P. aeruginosa, E. coli, and K. pneumoniae isolates.
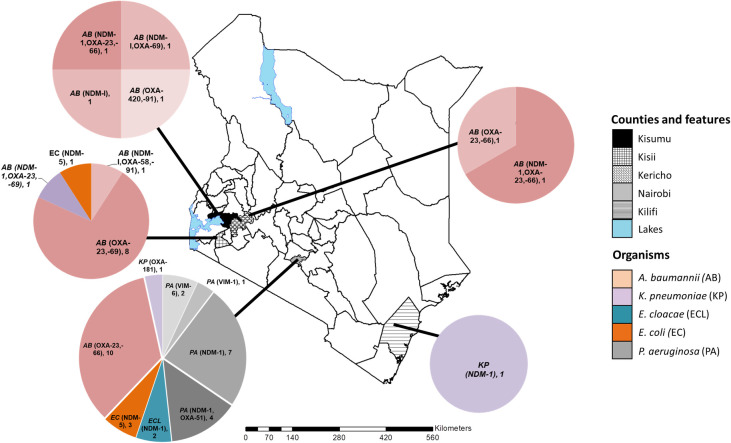
Sequence types and geographical distribution of the C-NS isolates
Carbapenemases were identified in all the study counties. However, the geographical distribution of the CR genes, bacterial species, and strain types were variable (Fig 1). Among the C-NS bacterial species, A. baumannii was the most broadly distributed across the counties, while E. cloacae and P. aeruginosa were only detected in Nairobi. Kisii and Nairobi counties had the most types of carbapenemases. The bacterial strain types and their characteristics varied between counties as described for each species in the following section.
Fig 1. The geographical distribution of the carbapenem non-susceptible gram-negative bacteria and carbapenemase genes in five Kenyan counties.
The map of Kenya with the study counties highlighted. The pie charts indicate the distribution of bacterial species, carbapenemase genes identified and the number of each isolate type detected. This custom map was generated in-house using the ArcGIS software Version 10.3.1 (Environmental Systems Research Institute, Red-lands, CA, USA).
Acinetobacter baumannii
The C-NS A. baumannii isolates belonged to four STs: 1, 2, 164, and a novel type. The isolate with a novel ST possessed a new single variant allele of the rplB gene (rplB 213) and was assigned to ST1475. In this study, all twelve ST1 A. baumannii isolates were detected in counties in western Kenya. They are predominantly associated with community-acquired infections (CAI) and were the least drug-resistant of the A. baumannii STs (Fig 1 and Table 1).
The ST1 isolates were mostly susceptible to fluoroquinolones, tetracyclines, tigecycline, and minocycline. A majority of ST1 isolates had the blaOXA-23 and blaOXA-69 carbapenemase and the blaADC-25 genes. The exception was one isolate (KAB16), which had the blaNDM-1 carbapenemase, blaCARB-16, and genes not found in the other ST1 isolates conferring resistance to macrolides, aminoglycosides, and fluoroquinolones. In contrast, the eleven ST2 isolates were multidrug-resistant, predominantly hospital-associated (8/11), and originated from the same hospital in Nairobi (10/11). These ST2 isolates expressed the blaOXA-23 and blaOXA-66 carbapenemase, the AmpC gene blaADC-25, and the 16s rRNA methyltransferase armA (Table 2), among other resistance genes.
The ST164 A. baumannii isolates (KAB 14, 15) differed in antibiotic resistance profiles and gene composition. The community-acquired KAB14 from Kisii had the blaNDM1 and blaOXA-58 carbapenemases and more resistance genes than KAB15 from Kisumu. This healthcare-associated KAB15 had fewer resistance genes and the blaOXA-420 carbapenemase gene. The ST374 isolate (KAB8) from an HAI in Kisumu was multidrug-resistant and unique because it lacked the oxacillinases. The ST1475 isolate (KAB13) associated with blaNDM1 and blaOXA-23 was isolated from an HA-SSTI infection in Kisii. The isolate was susceptible to only the last line drug tigecycline representing a localized high-risk MDR strain.
Enterobacter cloacae
The two E. cloacae isolates, both isolated from Nairobi, belonged to ST182 and ST25. They expressed the blaNDM1 carbapenemase, blaDHA-1, blaACT-6, mdfA, oqxA, oqxB genes, and were associated with HAIs. ST25 (KEB2) was the least resistant isolate, susceptible to levofloxacin and tigecycline. ST182 (KEB1) was resistant to all drugs tested except tigecycline. It had many drug resistance genes, including the potent 16S methyltransferase rmtC contributing to the highly drug-resistant phenotype.
Escherichia coli
All three E. coli isolates harbored blaNDM-5. However, the isolates from Nairobi (KEC1, 2) were ST167, while the Kisii isolate (KEC3) was ST648. All the E. coli isolates were only susceptible to tigecycline among the tested antibiotics, although ST648 had more antibiotic-resistant genes than the ST167 isolates implying a greater resistance level.
Klebsiella pneumoniae
ST219 and ST147 K. pneumoniae isolates were identified in Kilifi and Nairobi hospitals (Fig 1), respectively. The ST147 isolate from a CAI expressed a blaOXA-181 carbapenemase and was resistant to all drugs tested. On the other hand, K. pneumoniae ST219 had the blaNDM-1, blaCMY, and the 16S methyltransferase rmtC genes. It was susceptible to levofloxacin, minocycline, and tigecycline.
Pseudomonas aeruginosa
Thirteen of the fourteen P. aeruginosa isolates were resistant to all antibiotics tested. Four ST types, 357, 654, 316, and 1203 –were identified among C-NS P. aeruginosa isolates from Nairobi. All ST357 isolates and the single ST654 isolate (KPA6) had the blaNDM1 carbapenemase. The single P. aeruginosa ST316 isolate, for which there was limited demographic information available, expressed blaVIM-2. Of the two isolates identified as ST1203 (KPA 7, 8), both had the blaVIM-6 gene and genes not identified in any of the other STs of P. aeruginosa in this study: qnrVC1, dfrA5, dfrB5, ereA genes.
Discussion
This study aimed to identify the diversity and distribution of carbapenemase genes among GNB bacteria from an ongoing surveillance study in six hospitals across Kenya. The analysis detected eleven different carbapenemases among five clinically significant bacteria species. Five of the eleven CR genes detected were previously undescribed in Kenya: blaOXA-420, 58,181, blaNDM-5, and blaVIM-6. Notably, blaVIM-6 has not been reported before in Africa since it was first observed in Singapore in 2004 [35] and subsequently spread across Asia [36]. Neither has blaNDM-5 been reported in East Africa. Other carbapenemase genes identified are naturally occurring or widespread in their species, such as the class D oxacillinases blaOXA-23 and blaOXA-66 and 69 in A. baumannii [37]. One ST374 isolate (KAB8) was unique because it lacked these intrinsic oxacillinases.
Previous studies on carbapenemases in Kenya have focused mostly on Enterobacteriaceae [18]. Our findings show that A. baumannii was the most abundant and widely distributed of the C-NS bacteria carrying approximately 72% of the CR genes detected. It was followed by P. aeruginosa, with approximately 19%. The two species had the most carbapenemase gene diversity. As A. baumannii and P. aeruginosa are significant causes of HAI, their carriage of CR genes could contribute to hard-to-treat hospital outbreaks across broad geographical settings in Kenya—a challenge the World Health Organization (WHO) recognizes [38]. A substantial number of infections were among inpatients with SSTI and catheter-associated UTIs. These indicators stood out as potential risk factors for the acquisition of C-NS infections. Surprisingly, a third of the infections caused by C-NS bacteria were CAI, consistent with the trend witnessed in other parts of the world [39] deviating from the previously strong association of C-NS infections with HAIs. To avoid missing community circulation of C-NS bacteria, CAI should be included in surveillance efforts.
This study also detected various AmpC genes (blaADC-25, blaCMY, blaDHA-1, and blaACT-16), which have not previously been reported to coexist with carbapenemase genes in Kenya, and ESBL genes (blaCTX-M, SHV, and TEM). Hyper-production of these genes combined with mutations in porin genes or efflux pumps that reduce the influx or increase the efflux can contribute to the carbapenemase resistant phenotype [40]. It is necessary to include all these contributing factors in CR surveillance because, even in the absence of carbapenemases genes, they can cause carbapenem treatment failure.
Multiple antibiotic resistance genes (some of which were not phenotypically tested in this study) and efflux pumps (whose substrates can include antibiotics of multiple classes) coexisted in the C-NS bacteria. These data indicate the breadth of drug resistance and the therapeutic challenge posed by C-NS bacteria. Aminoglycosides are reported to be the third most prescribed drug class after cephalosporins and penicillins in a Kenyan referral hospital [41]. They are often used in combination with other antibiotic classes to treat severe infections. The high rate of aminoglycoside resistance, reflective of this prescription pattern, and the presence of the pan-aminoglycoside resistance genes among all isolates render this drug class ineffective against most C-NS infections. The 16srRNA methyltransferase genes have been previously associated with CR genes, particularly blaNDM-1 and blaOXA [42, 43], similar to the findings in this study where 16srRNA methyltransferase was detected alongside blaOXA-23/66, blaNDM-1, blaOXA-181, and blaNDM-5 genes.
The multidrug-resistant phenotypes in most C-NS isolates suggest an inevitable rise in untreatable GNB infections unless urgent measures are taken to curb these infections. This risk is evident in multiple MDR A. baumannii ST2 isolates identified in one hospital, indicating localized, clonal spread within the hospital. This pattern suggests a prolonged outbreak, as previously reported in a Nairobi Hospital [44]. Carbapenem, considered a last-resort antibiotic, is used to treat MDR infections and is the most commonly prescribed antibiotic in a study in a hospital in Nairobi [45]. As higher-level drugs are often unavailable or too expensive in Kenya, C-NS infections pose a serious challenge. This study shows that the most effective drugs against C-NS infections are tigecycline and minocycline. However, the innate resistance of P. aeruginosa and two A. baumannii isolates resistant to both drugs further limit the therapeutic options.
Few studies in Kenya have identified the strain types of C-NS bacteria. This study has set the baseline for tracking and detecting C-NS STs in Kenya by identifying the C-NS bacteria’s strain types. For example, the identification of A. baumannii STs (1, 2, 164, and a novel ST1475 type) was different from the OXA-23 producing strains identified in a study in a referral hospital in Kenya (ST110, 92, and 109) [44] indicating the broad strain diversity in the C-NS A. baumannii population in Kenya. A. baumannii ST1 and ST2 are global clonal strains associated with multidrug resistance [46]. ST164 is a rare strain type recently reported in Sudan, Brazil, and Turkey [47]. The ST164 A. baumannii bearing blaOXA-58 and blaOXA-420 carbapenemases are typically plasmid-mediated and geographically limited to Europe [48], Tunisia [49], and Nepal [50]. These ST164 isolates that carry potentially plasmid-mediated CR genes could be efficient disseminators of CR and MDR among the community and hospital settings in which they were found in Kenya. The A. baumannii ST1475 was previously un-typed, representing a novel strain first identified in Kenya. Carbapenem-resistant P. aeruginosa (CRPA) isolates carrying blaVIM-2 have been identified in an un-typed Kenya isolate [26] and ST244 and ST640 isolates in Tanzania and throughout Africa, often occurring in outbreaks [51–56]. Other CRPA ST316 isolates have been identified in China expressing the IMP-9 gene [57], but the isolate in this study represents a new case of a blaVIM-2 ST316 CRPA.
This study observed that different strain types had different drug resistance profiles making it easier to identify the most important strains for close monitoring. Based on the resistance profiles of the CR strains, the study identified high-risk MDR strains of A. baumannii (ST1475, ST2), E. cloacae (ST182), K. pneumoniae (ST147), P. aeruginosa (ST357, 654), and E. coli (ST167, ST648). A. baumannii ST1475 is a recognized international high-risk clone associated with multidrug resistance and hyper-virulence (44). P. aeruginosa ST654 isolates have been identified in Europe [58, 59], Singapore [60], Tunisia [61], and South America [62] associated with KPC, VIM, and IMP carbapenemases. Apart from this study, an extensively drug-resistant ST654 blaNDM1-producing P. aeruginosa isolate has only been reported in Canada [63]. NDM-5 was first detected in 2011 in an E. coli ST648 strain from India described as a highly virulent and MDR strain [64]. Since then, NDM-5 has been identified globally in different E. coli and K. pneumoniae STs indicating the rapid horizontal transfer of the gene across species. E. coli ST167 is a globally disseminated clone in human and animal populations associated with both multiple resistance and hyper-virulence genes. NDM-5 harboring strains have been described in Europe [65, 66] and China from humans [67]and poultry [68]. The potential zoonotic spread of these blaNDM-5 E. coli ST167 and ST648 strains in the Kenyan community poses a considerable risk to animal and human populations. The high-risk blaNDM-1 MDR E. cloacae ST182 isolate has been associated with outbreaks in several countries related to transmissible plasmid-borne blaNDM-1 [65, 69, 70]. These high-risk strains warrant close monitoring in Kenya as they could act as disseminators of carbapenemases.
An example of the potential or spread of carbapenemase genes is the increasing detection of blaNDM-1, previously identified in K. pneumoniae, A. baumannii, and P. aeruginosa from Nairobi and Kilifi [22–24, 71, 72]. This distribution is mirrored by this study’s findings of blaNDM-1 K. pneumoniae and P. aeruginosa in the two counties. However, what was different is that blaNDM-1 was also detected in E. cloacae isolates (Nairobi) and in A. baumannii (Nairobi, Kisii, and Kericho), an indication of a broader distribution of the CR gene. There have been few reports to date of P. aeruginosa expressing blaNDM-1 in sub-Saharan Africa and only one in Kenya [71]. It was surprising that five of the eight P. aeruginosa isolates in this study had blaNDM-1 as P. aeruginosa is most often associated with the Metallo-β lactamases VIM and IMP [73]. But NDM-1 expressing strains, typically associated with ST235, are increasing worldwide since they were first reported in 2011 [74] in Europe [75], India [76], Northern Africa [77] and North America [63] and may also become widespread in Kenya.
The study outcomes suggest that differences in CR’s type and scale among bacterial species exist between hospitals and counties. The greatest number and diversity of C-NS isolates were observed in the two referral hospitals in Kisii and Nairobi. Referral hospitals have factors that contribute to a greater risk of MDR infections, such as more hospital-acquired infections, extended hospitalization stays, invasive devices, and more frequent use of third-and fourth-line drugs [45]. These factors could explain why more carbapenemase genes were detected in Nairobi and Kisii hospitals than in the other lower-level hospitals with less than four carbapenem genes.
The study had some limitations. Only forty eight isolates representing all the available carbapenemase isolates detected over the study period were studied. Additional C-NS GNB isolates will be explored in the future within this ongoing surveillance program to improve the understanding of the geospatial distribution, emergence, spread, and evolution of CR in Kenya. The susceptibility testing was performed on a limited panel of antibiotics on the VITEK2 platform, and the AST results were not confirmed using an independent method. However, the detection of carbapenemase and other antibiotic resistance genes by WGS confirmed the observed resistance phenotypes. The primary concern with CR is the possibility of transmissible versus chromosomal carbapenemases. In this study, detailed analysis to detect the genomic location of the CR genes (chromosomal or plasmid) was not performed as it exceeded its scope, whose main goal was to describe the presence and distribution of carbapenemase genes. These analyses will be the focus of future studies to evaluate the dissemination risks within and between bacterial species.
Conclusions
In conclusion, while CR and the presence of carbapenemase genes have been recognized in Kenya, this study expands our understanding in several ways outlined below.
First, the study has described the diversity of CR genes among clinically significant gram-negative bacteria, including for the first time in E. coli and Enterobacter spp. Second, the research has shown the wide geographical spread of CR across Kenya, including three counties (Kisumu, Kisii, and Kericho) not previously studied. Third, the study provides the first report of carbapenemases OXA-420, 58,181, and VIM-6 and the simultaneous carriage of both carbapenemase genes and AmpC genes in Kenyan isolates. Fourth, CR is identified as a more significant challenge in larger referral hospitals where risk factors such as numbers of inpatient and critical care populations and greater use of third- and fourth-line antibiotics exist. Fifth, the study has made clear that across all hospitals, C-NS A. baumannii warrants attention as its significance in the CR landscape was not previously appreciated. Sixth, the notion that CR is only a nosocomial challenge is dispelled by the C-NS GNB detected in both community and healthcare-associated isolates. Finally, the study has identified STs of globally disseminated high-risk and multidrug-resistant isolates that should be specifically targeted for close monitoring. These isolates are reservoirs and possible transmitters of multiple-drug resistance.
These data highlight the importance of CR surveillance to adequately measure the scale of the problem and identify high-risk strains and emerging resistance genes to track the spread of resistance. Based on this data, measures such as improving infection control and implementing antibiotic stewardship should be implemented with the urgency required to reduce the spread of resistance, limit the morbidity and mortality associated with carbapenem resistance, and to preserve this critical drug class in Kenya.
Acknowledgments
We acknowledge the contributions of Erick Odoyo and Amanda Roth for manuscript review, Martin Georges, Daniel Matano, Fred Tiria for sample processing, bacterial culture, and antimicrobial susceptibility testing, Peter Sifuna for generating the figures, and LTC Dr. Angela Nderi for site support and coordination.
We acknowledge the staff at the Walter Reed Army Institute of Research–Multidrug-Resistant Organism Repository and Surveillance Network (WRAIR/MRSN) for whole-genome sequencing and analysis support, bioinformatics analyses, visualization, interpretation, and reporting.
We appreciate the contribution of the study staff, study participants, and the participating hospitals in the AMR Surveillance Project. This work has been reviewed and published with the permission of the Director KEMRI and the Walter Reed Army Institute of Research.
Data Availability
Whole-genome sequences are deposited in GenBank® BioProject IDs PRJNA636771 and PRJNA555206.
Funding Statement
This work was funded by the Armed Forces Health Surveillance Division, Global Emerging Infections Surveillance (GEIS) Branch (PROMIS ID 20160270153 FY17-19 Awarded to LM). The study funders had no role in study design, data collection, analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Antimicrobial Resistance: Global Report on Surveillance. World Health Organization; 2014. [Google Scholar]
- 2.Founou RC, Founou LL, Essack SY. Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS One. 2017;12: e0189621 10.1371/journal.pone.0189621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Organization WH, Others. Global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics [Internet]. Geneva: WHO; 2017. [Google Scholar]
- 4.Bush K, Jacoby GA. Updated functional classification of beta-lactamases. Antimicrob Agents Chemother. 2010;54: 969–976. 10.1128/AAC.01009-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martínez-Martínez L, Pascual A, Hernández-Allés S, Alvarez-Díaz D, Suárez AI, Tran J, et al. Roles of beta-lactamases and porins in activities of carbapenems and cephalosporins against Klebsiella pneumoniae. Antimicrob Agents Chemother. 1999;43: 1669–1673. 10.1128/AAC.43.7.1669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chavda KD, Chen L, Fouts DE, Sutton G, Brinkac L, Jenkins SG, et al. Comprehensive Genome Analysis of Carbapenemase-Producing Enterobacter spp.: New Insights into Phylogeny, Population Structure, and Resistance Mechanisms. MBio. 2016;7 10.1128/mBio.02093-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carattoli A. Plasmids and the spread of resistance. Int J Med Microbiol. 2013;303: 298–304. 10.1016/j.ijmm.2013.02.001 [DOI] [PubMed] [Google Scholar]
- 8.Meletis G. Carbapenem resistance: overview of the problem and future perspectives. Ther Adv Infect Dis 3: 15–21. 2016. 10.1177/2049936115621709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nordmann P, Poirel L. The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin Microbiol Infect. 2014;20: 821–830. 10.1111/1469-0691.12719 [DOI] [PubMed] [Google Scholar]
- 10.van Duin D, Doi Y. The global epidemiology of carbapenemase-producing Enterobacteriaceae. Virulence. 2017;8: 460–469. 10.1080/21505594.2016.1222343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Djahmi N, Dunyach-Remy C, Pantel A, Dekhil M, Sotto A, Lavigne J-P. Epidemiology of carbapenemase-producing Enterobacteriaceae and Acinetobacter baumannii in Mediterranean countries. Biomed Res Int. 2014;2014: 305784 10.1155/2014/305784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brolund A, Lagerqvist N, Byfors S, Struelens MJ, Monnet DL, Albiger B, et al. Worsening epidemiological situation of carbapenemase-producing Enterobacteriaceae in Europe, assessment by national experts from 37 countries, July 2018. Euro Surveill. 2019;24 10.2807/1560-7917.ES.2019.24.9.1900123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karah N, Sundsfjord A, Towner K, Samuelsen Ø. Insights into the global molecular epidemiology of carbapenem non-susceptible clones of Acinetobacter baumannii. Drug Resist Updat. 2012;15: 237–247. 10.1016/j.drup.2012.06.001 [DOI] [PubMed] [Google Scholar]
- 14.Pitout JDD, Nordmann P, Poirel L. Carbapenemase-Producing Klebsiella pneumoniae, a Key Pathogen Set for Global Nosocomial Dominance. Antimicrob Agents Chemother. 2015;59: 5873–5884. 10.1128/AAC.01019-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haller S, Kramer R, Becker K, Bohnert JA, Eckmanns T, Hans JB, et al. Extensively drug-resistant Klebsiella pneumoniae ST307 outbreak, north-eastern Germany, June to October 2019. Euro Surveill. 2019;24 10.2807/1560-7917.ES.2019.24.50.1900734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Annavajhala MK, Gomez-Simmonds A, Uhlemann A-C. Multidrug-Resistant Enterobacter cloacae Complex Emerging as a Global, Diversifying Threat. Front Microbiol. 2019;10: 44 10.3389/fmicb.2019.00044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manenzhe RI, Zar HJ, Nicol MP, Kaba M. The spread of carbapenemase-producing bacteria in Africa: a systematic review. J Antimicrob Chemother. 2015;70: 23–40. 10.1093/jac/dku356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitgang EA, Hartley DM, Malchione MD, Koch M, Goodman JL. Review and mapping of carbapenem-resistant Enterobacteriaceae in Africa: Using diverse data to inform surveillance gaps. Int J Antimicrob Agents. 2018;52: 372–384. 10.1016/j.ijantimicag.2018.05.019 [DOI] [PubMed] [Google Scholar]
- 19.Ssekatawa K, Byarugaba DK, Wampande E, Ejobi F. A systematic review: the current status of carbapenem resistance in East Africa. BMC Res Notes. 2018;11: 629 10.1186/s13104-018-3738-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okoche D, Asiimwe BB, Katabazi FA, Kato L, Najjuka CF. Prevalence and Characterization of Carbapenem-Resistant Enterobacteriaceae Isolated from Mulago National Referral Hospital, Uganda. PLoS One. 2015;10: e0135745 10.1371/journal.pone.0135745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mushi MF, Mshana SE, Imirzalioglu C, Bwanga F. Carbapenemase genes among multidrug resistant gram negative clinical isolates from a tertiary hospital in Mwanza, Tanzania. Biomed Res Int. 2014;2014: 303104 10.1155/2014/303104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poirel L, Revathi G, Bernabeu S, Nordmann P. Detection of NDM-1-producing Klebsiella pneumoniae in Kenya. Antimicrob Agents Chemother. 2011;55: 934–936. 10.1128/AAC.01247-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Henson SP, Boinett CJ, Ellington MJ, Kagia N, Mwarumba S, Nyongesa S, et al. Molecular epidemiology of Klebsiella pneumoniae invasive infections over a decade at Kilifi County Hospital in Kenya. Int J Med Microbiol. 2017;307: 422–429. 10.1016/j.ijmm.2017.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Revathi G, Siu LK, Lu P-L, Huang L-Y. First report of NDM-1-producing Acinetobacter baumannii in East Africa. Int J Infect Dis. 2013;17: e1255–8. 10.1016/j.ijid.2013.07.016 [DOI] [PubMed] [Google Scholar]
- 25.Maina D, Revathi G, Whitelaw AC. Molecular characterization of multidrug-resistant Klebsiella pneumoniae and Escherichia coli harbouring extended spectrum beta-lactamases and carbapenemases genes at a tertiary hospital, Kenya. Microbiologia Medica. 2017;32: 132. [Google Scholar]
- 26.Pitout JDD, Revathi G, Chow BL, Kabera B, Kariuki S, Nordmann P, et al. Metallo-beta-lactamase-producing Pseudomonas aeruginosa isolated from a large tertiary centre in Kenya. Clin Microbiol Infect. 2008;14: 755–759. 10.1111/j.1469-0691.2008.02030.x [DOI] [PubMed] [Google Scholar]
- 27.Storberg V. ESBL-producing Enterobacteriaceae in Africa—a non-systematic literature review of research published 2008–2012. Infect Ecol Epidemiol. 2014;4 10.3402/iee.v4.20342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kiiru J, Kariuki S, Goddeeris BM, Butaye P. Analysis of β-lactamase phenotypes and carriage of selected β-lactamase genes among Escherichia coli strains obtained from Kenyan patients during an 18-year period. BMC Microbiol. 2012;12: 155 10.1186/1471-2180-12-155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saisi H, Makobe C, Kangongo M, Kariuki S. Prevalence of CTXM, SHV, TEM AND OXA Genes among Extended-Spectrum Beta-Lactamase Producing Klebsiella pneumoniae from Mukuru Slum, Kenya. Acta Inform Med. 2019;09: 853–862. [Google Scholar]
- 30.Wood DE, Salzberg SL. Kraken: ultrafast metagenomic sequence classification using exact alignments. Genome Biol. 2014;15: R46 10.1186/gb-2014-15-3-r46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zankari E, Hasman H, Cosentino S, Vestergaard M, Rasmussen S, Lund O, et al. Identification of acquired antimicrobial resistance genes. J Antimicrob Chemother. 2012;67: 2640–2644. 10.1093/jac/dks261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jolley KA, Bray JE, Maiden MCJ. Open-access bacterial population genomics: BIGSdb software, the PubMLST.org website and their applications. Wellcome Open Res. 2018;3: 124 10.12688/wellcomeopenres.14826.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maiden MC, Bygraves JA, Feil E, Morelli G, Russell JE, Urwin R, et al. Multilocus sequence typing: a portable approach to the identification of clones within populations of pathogenic microorganisms. Proc Natl Acad Sci U S A. 1998;95: 3140–3145. 10.1073/pnas.95.6.3140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Healthcare Safety Network (NHSN) Patient Safety Component Manual. [cited 23 Aug 2019]. Available: https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf
- 35.Koh TH, Wang GCY, Sng L-H. IMP-1 and a novel metallo-beta-lactamase, VIM-6, in fluorescent pseudomonads isolated in Singapore. Antimicrob Agents Chemother. 2004;48: 2334–2336. 10.1128/AAC.48.6.2334-2336.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Castanheira M, Bell JM, Turnidge JD, Mendes RE, Jones RN. Dissemination and genetic context analysis of bla(VIM-6) among Pseudomonas aeruginosa isolates in Asian-Pacific Nations. Clin Microbiol Infect. 2010;16: 186–189. 10.1111/j.1469-0691.2009.02903.x [DOI] [PubMed] [Google Scholar]
- 37.Evans BA, Amyes SGB. OXA β-lactamases. Clin Microbiol Rev. 2014;27: 241–263. 10.1128/CMR.00117-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guidelines for the Prevention and Control of Carbapenem-Resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in Health Care Facilities Geneva: World Health Organization; 2018. [PubMed] [Google Scholar]
- 39.van Duin D, Paterson DL. Multidrug-Resistant Bacteria in the Community. Infectious Disease Clinics of North America. 2016. pp. 377–390. 10.1016/j.idc.2016.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jacoby GA. AmpC beta-lactamases. Clin Microbiol Rev. 2009;22: 161–82 10.1128/CMR.00036-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Momanyi L, Opanga S, Nyamu D, Oluka M, Kurdi A, Godman B. Antibiotic Prescribing Patterns at a Leading Referral Hospital in Kenya: A Point Prevalence Survey. Am J Pharmacogenomics. 2019;8: 149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Karah N, Haldorsen B, Hermansen NO, Tveten Y, Ragnhildstveit E, Skutlaberg DH, et al. Emergence of OXA-carbapenemase- and 16S rRNA methylase-producing international clones of Acinetobacter baumannii in Norway. Journal of Medical Microbiology. 2011. pp. 515–521. 10.1099/jmm.0.028340-0 [DOI] [PubMed] [Google Scholar]
- 43.Berçot B, Poirel L, Nordmann P. Updated multiplex polymerase chain reaction for detection of 16S rRNA methylases: high prevalence among NDM-1 producers. Diagn Microbiol Infect Dis. 2011;71: 442–445. 10.1016/j.diagmicrobio.2011.08.016 [DOI] [PubMed] [Google Scholar]
- 44.Huber CA, Sartor AL, McOdimba F, Shah R, Shivachi P, Sidjabat HE, et al. Outbreaks of multidrug-resistant Acinetobacter baumannii strains in a Kenyan teaching hospital. J Glob Antimicrob Resist. 2014;2: 190–193. 10.1016/j.jgar.2014.03.007 [DOI] [PubMed] [Google Scholar]
- 45.Mariita KM, Chirima HA, Maina CK. Broad spectrum antibiotic use among in-patients at a hospital in Nairobi, Kenya. International Journal of Basic & Clinical Pharmacology. 2018. p. 1 10.18203/2319-2003.ijbcp20185154 [DOI] [Google Scholar]
- 46.Diancourt L, Passet V, Nemec A, Dijkshoorn L, Brisse S. The population structure of Acinetobacter baumannii: expanding multiresistant clones from an ancestral susceptible genetic pool. PLoS One. 2010;5: e10034 10.1371/journal.pone.0010034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Acinetobacter baumannii MLST Home Page. [cited 14 Apr 2020]. Available: https://pubmlst.org/abaumannii/
- 48.Karah N, Giske CG, Sundsfjord A, Samuelsen Ø. A diversity of OXA-carbapenemases and class 1 integrons among carbapenem-resistant Acinetobacter baumannii clinical isolates from Sweden belonging to different international clonal lineages. Microb Drug Resist. 2011;17: 545–549. 10.1089/mdr.2011.0089 [DOI] [PubMed] [Google Scholar]
- 49.Mathlouthi N, Ben Lamine Y, Somai R, Bouhalila-Besbes S, Bakour S, Rolain J-M, et al. Incidence of OXA-23 and OXA-58 Carbapenemases Coexpressed in Clinical Isolates of Acinetobacter baumannii in Tunisia. Microb Drug Resist. 2018;24: 136–141. 10.1089/mdr.2016.0306 [DOI] [PubMed] [Google Scholar]
- 50.Shrestha S, Tada T, Miyoshi-Akiyama T. Molecular epidemiology of multidrug-resistant Acinetobacter baumannii isolates in a university hospital in Nepal reveals the emergence of a novel epidemic clonal …. International journal of. 2015. Available: https://www.sciencedirect.com/science/article/pii/S0924857915002824 [DOI] [PubMed] [Google Scholar]
- 51.Moyo S, Haldorsen B, Aboud S. Identification of VIM-2-producing Pseudomonas aeruginosa from Tanzania is associated with sequence types 244 and 640 and the location of blaVIM-2 in a TniC …. Antimicrob Agents Chemother. 2015. Available: https://aac.asm.org/content/59/1/682.short [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mansour W, Poirel L, Bettaieb D, Bouallegue O, Boujaafar N, Nordmann P. Metallo-β-lactamase–producing Pseudomonas aeruginosa isolates in Tunisia. Diagn Microbiol Infect Dis. 2009;64: 458–461. 10.1016/j.diagmicrobio.2009.04.003 [DOI] [PubMed] [Google Scholar]
- 53.Hammami S, Gautier V, Ghozzi R, Da Costa A, Ben-Redjeb S, Arlet G. Diversity in VIM-2-encoding class 1 integrons and occasional blaSHV2a carriage in isolates of a persistent, multidrug-resistant Pseudomonas aeruginosa clone from Tunis. Clin Microbiol Infect. 2010;16: 189–193. 10.1111/j.1469-0691.2009.03023.x [DOI] [PubMed] [Google Scholar]
- 54.Jacobson RK, Minenza N, Nicol M, Bamford C. VIM-2 metallo-β-lactamase-producing Pseudomonas aeruginosa causing an outbreak in South Africa. J Antimicrob Chemother. 2012;67: 1797–1798. 10.1093/jac/dks100 [DOI] [PubMed] [Google Scholar]
- 55.Jeannot K, Guessennd N, Fournier D, Müller E, Gbonon V, Plésiat P. Outbreak of metallo-β-lactamase VIM-2-positive strains of Pseudomonas aeruginosa in the Ivory Coast. J Antimicrob Chemother. 2013;68: 2952–2954. 10.1093/jac/dkt296 [DOI] [PubMed] [Google Scholar]
- 56.Touati M, Diene SM, Dekhil M, Djahoudi A, Racherache A, Rolain J-M. Dissemination of a class I integron carrying VIM-2 carbapenemase in Pseudomonas aeruginosa clinical isolates from a hospital intensive care unit in Annaba, Algeria. Antimicrob Agents Chemother. 2013;57: 2426–2427. 10.1128/AAC.00032-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yin S, Chen P, You B, Zhang Y, Jiang B, Huang G, et al. Molecular Typing and Carbapenem Resistance Mechanisms of Pseudomonas aeruginosa Isolated From a Chinese Burn Center From 2011 to 2016. Front Microbiol. 2018;9: 1135 10.3389/fmicb.2018.01135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pobiega M, Maciąg J, Chmielarczyk A, Romaniszyn D, Pomorska-Wesolowska M, Ziolkowski G, et al. Molecular characterization of carbapenem-resistant Pseudomonas aeruginosa strains isolated from patients with urinary tract infections in Southern Poland. Diagn Microbiol Infect Dis. 2015;83: 295–297. 10.1016/j.diagmicrobio.2015.07.022 [DOI] [PubMed] [Google Scholar]
- 59.Golle A, Janezic S, Rupnik M. Low overlap between carbapenem resistant Pseudomonas aeruginosa genotypes isolated from hospitalized patients and wastewater treatment plants. PLoS One. 2017;12: e0186736 10.1371/journal.pone.0186736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Koh TH, Khoo CT, Tan TT, Mohamed Amir Bin, Ang LP, Lau LJ, et al. Multilocus Sequence Types of Carbapenem-Resistant Pseudomonas aeruginosa in Singapore Carrying Metallo-β-Lactamase Genes, Including the Novel blaIMP-26 Gene. J Clin Microbiol. 2010;48: 2563–2564. 10.1128/JCM.01905-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Samuelsen Ø, Toleman MA, Sundsfjord A. Molecular epidemiology of metallo-β-lactamase-producing Pseudomonas aeruginosa isolates from Norway and Sweden shows import of international clones and local clonal expansion. Antimicrob Agents Chemother. 2010;54: 346–352 10.1128/AAC.00824-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pasteran F, Faccone D, Gomez S, De Bunder S, Spinelli F, Rapoport M, et al. Detection of an international multiresistant clone belonging to sequence type 654 involved in the dissemination of KPC-producing Pseudomonas aeruginosa in Argentina. J Antimicrob Chemother. 2012;67: 1291–1293. 10.1093/jac/dks032 [DOI] [PubMed] [Google Scholar]
- 63.Mataseje LF, Peirano G, Church DL, Conly J, Mulvey M, Pitout JD. Colistin-Nonsusceptible Pseudomonas aeruginosa Sequence Type 654 with blaNDM-1 Arrives in North America. Antimicrob Agents Chemother. 2016;60: 1794–1800. 10.1128/AAC.02591-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Schaufler K, Semmler T, Wieler LH, Trott DJ, Pitout J, Peirano G, et al. Genomic and Functional Analysis of Emerging Virulent and Multidrug-Resistant Escherichia coli Lineage Sequence Type 648. Antimicrob Agents Chemother. 2019;63 10.1128/AAC.00243-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Giufrè M, Errico G, Accogli M, Monaco M, Villa L, Distasi MA, et al. Emergence of NDM-5-producing Escherichia coli sequence type 167 clone in Italy. Int J Antimicrob Agents. 2018;52: 76–81. 10.1016/j.ijantimicag.2018.02.020 [DOI] [PubMed] [Google Scholar]
- 66.Grönthal T, Österblad M, Eklund M, Jalava J, Nykäsenoja S, Pekkanen K, et al. Sharing more than friendship–transmission of NDM-5 ST167 and CTX-M-9 ST69 Escherichia coli between dogs and humans in a family, Finland, 2015. Eurosurveillance. 2018. 10.2807/1560-7917.es.2018.23.27.1700497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Huang Y, Yu X, Xie M, Wang X, Liao K, Xue W, et al. Widespread Dissemination of Carbapenem-Resistant Escherichia coli Sequence Type 167 Strains Harboring blaNDM-5 in Clinical Settings in China. Antimicrob Agents Chemother. 2016;60: 4364–4368. 10.1128/AAC.00859-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tang B, Chang J, Cao L, Luo Q, Xu H, Lyu W, et al. Characterization of an NDM-5 carbapenemase-producing Escherichia coli ST156 isolate from a poultry farm in Zhejiang, China. BMC Microbiology. 2019. 10.1186/s12866-019-1454-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Torres-González P, Bobadilla-Del Valle M, Tovar-Calderón E, Leal-Vega F, Hernández-Cruz A, Martínez-Gamboa A, et al. Outbreak caused by Enterobacteriaceae harboring NDM-1 metallo-β-lactamase carried in an IncFII plasmid in a tertiary care hospital in Mexico City. Antimicrob Agents Chemother. 2015;59: 7080–7083. 10.1128/AAC.00055-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Du N, Liu S, Niu M, Duan Y, Zhang S, Yao J, et al. Transmission and characterization of bla NDM-1 in Enterobacter cloacae at a teaching hospital in Yunnan, China. Ann Clin Microbiol Antimicrob. 2017;16: 58 10.1186/s12941-017-0232-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mukaya KJS, Maina J, Museve B, Nyerere AK, Kiiru J. Antimicrobial Resistance Profile and Genetic Profiling of Pseudomonas aeruginosa Strains Obtained from Different Inpatient Wards at Kenyatta National Hospital. IOSR Journal of Pharmacy and Biological Sciences (IOSR-JPBS). 2018;13 Available: http://www.academia.edu/download/57137294/A1304030109.pdf [Google Scholar]
- 72.Khan A, Hanson B, Dinh A, Wanger A, Ostrosky-Zeichner L, Miller W, et al. 705. Four Superbugs Isolated From a Single Patient in the United States: E. coli (EC) and K. pneumoniae (KP) Harboring NDM-5, P. aeruginosa (PA) Harboring NDM-1 and Candida auris. Open Forum Infectious Diseases. 2018. pp. S254–S254. 10.1093/ofid/ofy210.712 [DOI] [Google Scholar]
- 73.Cornaglia G, Giamarellou H, Rossolini GM. Metallo-β-lactamases: a last frontier for β-lactams? Lancet Infect Dis. 2011;11: 381–393. 10.1016/S1473-3099(11)70056-1 [DOI] [PubMed] [Google Scholar]
- 74.Jovcic B, Lepsanovic Z, Suljagic V, Rackov G, Begovic J, Topisirovic L, et al. Emergence of NDM-1 metallo-β-lactamase in Pseudomonas aeruginosa clinical isolates from Serbia. Antimicrob Agents Chemother. 2011;55: 3929–3931. 10.1128/AAC.00226-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Carattoli A, Fortini D, Galetti R, Garcia-Fernandez A, Nardi G, Orazi D, et al. Isolation of NDM-1-producing Pseudomonas aeruginosa sequence type ST235 from a stem cell transplant patient in Italy, May 2013. Euro Surveill. 2013;18 10.2807/1560-7917.es2013.18.46.20633 [DOI] [PubMed] [Google Scholar]
- 76.Khajuria A, Praharaj AK, Kumar M, Grover N. Emergence of NDM—1 in the Clinical Isolates of Pseudomonas aeruginosa in India. J Clin Diagn Res. 2013;7: 1328–1331. 10.7860/JCDR/2013/5509.3137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zafer MM, Al-Agamy MH, El-Mahallawy HA, Amin MA, Ashour MSE-D. Antimicrobial resistance pattern and their beta-lactamase encoding genes among Pseudomonas aeruginosa strains isolated from cancer patients. Biomed Res Int. 2014;2014: 101635 10.1155/2014/101635 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Whole-genome sequences are deposited in GenBank® BioProject IDs PRJNA636771 and PRJNA555206.