Abstract
Tracheobronchial foreign body aspiration (TB-FBA) with subsequent airway obstruction typically occurs in children younger than 4 years. TB-FBA results in significant morbidity and mortality in children requiring urgent recognition and prompt management. Some cases remain more indolent and cause unusual respiratory insults ranging from chronic respiratory symptoms such as persistent cough, wheezing, and recurrent pneumonia to life-threatening airway obstruction. This case report presents a rare case of TB-FBA in an 8-year-old girl with a prolonged history of cough and dyspnea for 15 months despite many medical treatments and a rigid bronchoscopy examination performed by a board-certified pediatric surgeon. The patient was referred to Namazi Hospital's Pediatric Interventional Pulmonology Division where fiberoptic bronchoscopic exploration was conducted to remove a foreign body (a 6-cm wheat cluster) from the right lower lobe bronchus. This case report demonstrates the importance of clinical history in the diagnosis of aspirated foreign bodies despite unusual age and normal radiological findings.
Keywords: chronic cough, tracheobronchial foreign body aspiration, case report
Background
Tracheobronchial foreign body aspiration (TB-FBA) is one of the medical challenges threatening children's lives. Its highest incidence is in children aged under 4 years.1 Outside this age range, we are faced with neurological dysfunction, trauma, alcohol abuse, and psychological disorders.2 For the first time in 1897, Gustav Killian removed a pig bone from a German farmer's tract through bronchoscopy. Over the years, rigid bronchoscopy performed using the same method has been the most sensitive and specific way to diagnose and treat TB-FBA.3
Foreign bodies observed in chest X-ray imaging include various objects (from visible to invisible objects) based on the radiodensity of foreign bodies. In 37% of cases, translucent foreign bodies may not be detected in plain chest X-ray.4 As a result, typical history of choking, severe acute-onset cough, wheezing, and cyanosis and no history of a specific disease will be helpful for diagnosis.5 Otherwise, lack of such clear history and radiological findings will make the diagnosis complicated, and this would be a challenge. So, clinical diagnosis needs a high degree of suspicion. In this report, an 8-year-old girl with this challenge was referred.
Case Presentation
An 8-year-old girl with a history of 6 months of chronic cough was referred to Namazi Hospital (southern of Iran) for the first time. The patient showed an unclear history of bluish discoloration. Her parents complained of their child's cough without any previous history of asthma, seasonal sensitivity, infections, or respiratory problems. The patient's vital signs were stable, and she had no fever. The lung examination was normal. There was no abnormal finding in her laboratory results except for an unremarkable increase in erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) at 28 mm/hour and 7 mg/L, respectively. In addition, plain chest imaging was clear. She was managed under the impression of viral pneumonia and reactive airway disease. After a few days of hospitalization, the patient's cough recovered, and she was eventually discharged.
Approximately a month later, she was admitted for the second time because of severe wet cough and low-grade fever. Chest examination revealed normal respiratory movements in amplitude and frequency. Upon auscultation, mild unilateral wheezing and decreased breath sounds were detected at the lower third of the right hemithorax with normal percussion. The remaining examinations were normal. Laboratory results include a white blood cell count (WBC) of 10,200/μL (32.2 × 109/L; 67% neutrophils and 30% monocytes), and ESR and CRP were slightly increased at 34 mm/hour and 11 mg/L, respectively. Her posteroanterior chest X-ray showed radiopacity located at the level of the right lower lobe with a cardiac silhouette.
The patient was suspected of TB-FBA and was consulted by the paediatric surgery division. She underwent rigid bronchoscopy performed by a board-certified pediatric surgeon in the operating room. Except for some mucosal plugging, no particular finding was seen, and the medical team failed to diagnose the problem. Again, the patient was discharged from the hospital, and her chronic cough lasted for approximately eight months, although she was on antiasthma drugs including salbutamol (one to two puffs at the time of presenting cough spells) and fluticasone (125 mcg metered-dose inhaler, one puff twice per day) but without any improvement.
Finally, she was referred to our service for her unresolved symptoms and, even after doing more workups, for tuberculosis infection. Her vital signs were normal. In the physical examination, localized wheezing was heard in the lower zone of her right lung. Her WBC count was 18,200/μL (32.2 × 109/L; 80% neutrophils and 18% monocytes), and ESR and CRP increased to 50 mm/hour and 35 mg/L, respectively. In her plain chest imaging, a consolidation was seen again in the lower lobe of the right lung. Intravenous antibiotics were prescribed under the impression of pneumonia versus retained TB-FBA.
Considering the patient's history, physical examination, image findings, and TB-FBA suspicion as one of the differential diagnoses, fiberoptic bronchoscopy was performed to further investigate.
The patient was anesthetized in a spontaneous breathing setting. Propofol and lidocaine solution were given using the spray and go technique. Using a pediatric flexible bronchoscope (with a 4.3-mm diameter size including a 2-mm working channel [Olympus, Japan]), an unusual object was found embedded in a thick exudative mucosal plug in the lower lobe of the bronchus of the right lung. Surprisingly, a 6-cm wheat cluster was seen in the B7 zone of the respiratory tract after suctioning and was successfully removed using alligator forceps (Figure 1). After that, bronchoalveolar lavage was performed, and the area was rechecked to make sure there was nothing left (Figure 2).
Figure 1.
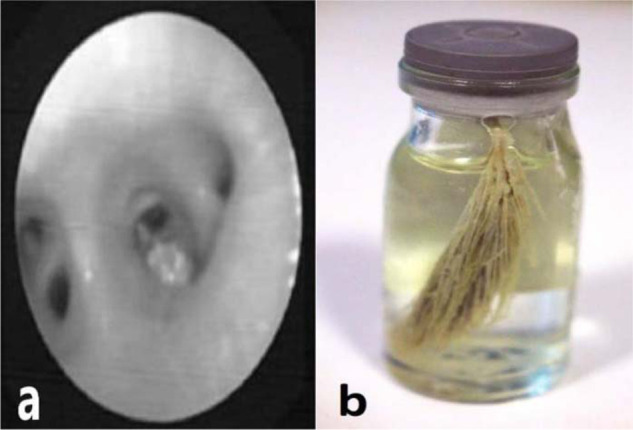
(a) A foreign body found in the B7 zone of the respiratory tract in flexible bronchoscopic view. (b) A 6-cm wheat cluster was removed.
Figure 2.
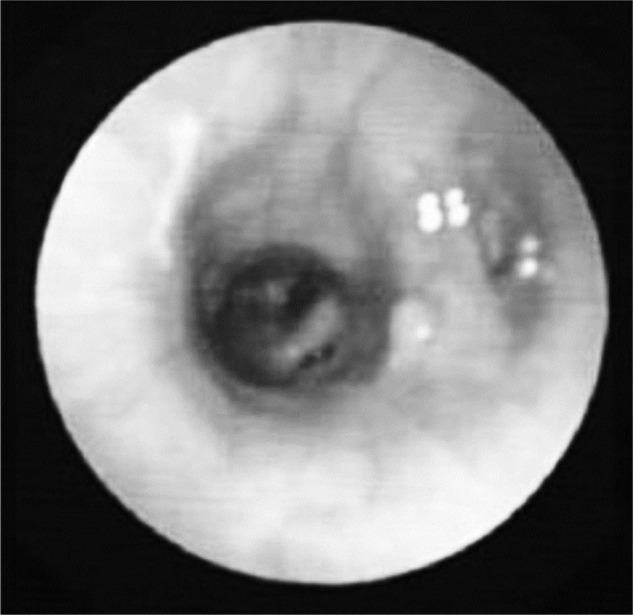
The right lower lobe bronchus (B7 zone) following the immediate removal of the wheat cluster.
The patient weighing 24.7 kg was prescribed with 50 mg/kg ceftriaxone every 12 hours for 5 days to manage her long-term symptoms, increased laboratory results, and bronchoscopy findings. She was also given clindamycin 30 mg/kg every 8 hours for five days. After removing the foreign body, the child's condition improved dramatically, and her chronic symptoms including her cough significantly reduced. Eventually, clinical and paraclinical findings were normalized within a one-month follow-up.
Discussion
TB-FBA is particularly common in toddlers and young children. The most common aspirated FBs are organic materials including peanut, seeds, and nuts.6 Diagnosis of TB-FBA in children is still challenging, and all cases of TB-FBA should be treated as a medical emergency. If FBA in children and adults is not found at the right time, it can be lethal.1 The complication rate of FBA in children ranged from 14.6% to 27.8%, and complications included recurrent pneumonia, chronic respiratory symptoms (such as cough spells, cyanotic spells, and continuous wheezing), pneumothorax, pneumomediastinum, abscess formation, and plural effusion.7
The abovementioned special case presented an 8-year-old girl who was not in the usual age range for TB-FBA, had tolerated a large wheat cluster in her respiratory tract for 8 months, and had only complained of chronic cough. However, since the patient was afraid that the previous invasive procedures would be performed again, she refrained from disclosing her history of chokes and cyanosis.
With the recent improvement of flexible instruments, flexible bronchoscopy is rapidly gaining use in airway TB-FBA extraction and is now considered by some authors as the first line in airway FB extraction. Various bronchoscopic instruments such as different types of forceps, baskets, and balloons are used to treat TB-FBA. Cryoprobes also opened the way for managing TB-FBA, especially with a friable texture, even in infants.8
Since many foreign bodies are lodged in the central airways, rigid bronchoscopy has become the gold standard in the diagnosis and extraction of airway FB. It is unusual for foreign bodies to be missed on rigid bronchoscopy as the foreign body may be embedded in granulation tissue or covered by mucus or pus secretions.9 In this study, rigid bronchoscopy was unsuccessful since the foreign body was located in the B7 zone of the lower lobe of the right lung and detected within exudates. The removal of more distal foreign bodies can present a significant challenge, and they can be reached and extracted using a flexible bronchoscope or a combination of both methods.10 Recently, FB removal by flexible bronchoscopy under fluoroscopy guidance was used as a potentially safe procedure.11
Foreign bodies commonly enter the right-main bronchus because of its greater diameter and vertical anatomy. The anatomy of the right bronchus is also a well-known contributing variable to many respiratory conditions such as right-main stem intubation and aspiration pneumonia. Further research suggests that in children younger than 15 years, foreign bodies lodge within the left lung because of the symmetric tracheal takeoff angle found in some children before the development of an aortic indentation on the trachea and left bronchus. This may suggest that the difference in the occurrence of FB aspiration in the left and right bronchial trees is less pronounced because children have immature airways. Therefore, the differences between the left and right bronchial trees may not be significant.12,13 Although there is no correlation between the location of foreign bodies and age, sex, bronchoscopy time, and hospitalization length, the right lower lobe is the most common site of recurrent pneumonia following TB-FBA.14 Because of the size and flexibility of this foreign body type and the lack of complete pathway obstruction, clinical and radiological findings in the chest X-ray appeared with delay. In addition, since the history of choking and cyanosis was unclear and the initial rigid bronchoscopy did not report any problems, the diagnosis was postponed. Microvariables such as local inflammation, edema, cellular infiltration, ulceration, and granulation tissue formation, which may contribute to airway obstruction, make bronchoscopic identification more difficult and explain why the surgical team was unable to identify the FB on their first pass. Several other articles also reported TB-FBA with radiolucent foreign bodies such as flowers, plants, and plastic whistles; since the respiratory tract was not completely blocked, no specific symptom was observed.15 Another similar case was a 12-year-old girl, who suffered from one-year episodic breathlessness and was impressed of asthma. Finally, after a bronchoscopic examination, a plastic pen cap, as a radiolucent foreign body, was extracted from her lung.16 Considering the age, chronic coughing, atypical history, and previous unsuccessful procedures, our patient was exclusive. Delayed diagnosis of a retained TB-FBA may lead to a bronchial reaction with granulation tissue formation, recurrent pneumonia, atelectasis, lung abscess, pneumomediastinum, pneumothorax, bronchopleural or bronchovascular fistulization, and asphyxia.17–19
Conclusion
In diagnosing TB-FBA, the main emphasis is on getting a clear and reliable history and a strong doctor's suspicion of occurrence, especially when many radiolucent foreign bodies are presented with normal imaging. It should be remembered that having a normal physical examination, plain chest X-ray imaging, and even rigid bronchoscopy does not mean that there is no foreign body in the lungs.
Ethical approval and consent to participate
Ethical approval relevant to our case report was not necessary. Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Consent for publication
A copy of the written consent provided by the patient for the publication of the necessary data, images, and/or videos is available for review by the Editor-in-Chief of this journal.
Availability of data and materials
All data and materials are available in our clinic and laboratory.
Conflict of interest
The authors declare that they have no competing interests.
Funding
The authors declare that they have not received any funding for this work.
References
- 1. Grassi R, Faggian A, Somma F, De Cecco CN, Laghi A, Caseiro-Alves F. Application of imaging guidelines in patients with foreign body ingestion or inhalation: literature review. Semin Ultrasound CT MR. 2015;36(1):48–56. [DOI] [PubMed]
- 2. Lewis C, Hsu HK, Hoover E. Aspiration of foreign bodies in adults with personality disorders: impact on diagnosis and recurrence. J Natl Med Assoc. 2011;103(7):620–622. [DOI] [PubMed]
- 3. Hitter A, Hullo E, Durand C, Righini CA. Diagnostic value of various investigations in children with suspected foreign body aspiration: review. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128(5):248–252. [DOI] [PubMed]
- 4. van Schuppen J, van Rijn R. Foreign body aspiration in children: evidence-based emergency imaging. In: Evidence-Based Emergency Imaging 1st ed. Cham: Springer; 2018. p. 605–614.
- 5. Samarei R. Survey of foreign body aspiration in airways and lungs. Glob J Health Sci. 2014;6(7):130–135. [DOI] [PMC free article] [PubMed]
- 6. Aslan N, Yıldızdas¸ D, Özden Ö, Yöntem, A, Horoz, ÖÖ, Kılıç, S. Evaluation of foreign body aspiration cases in our pediatric intensive care unit: Single-center experience. Turk Pediatri Arsivi. 2019;54(1):44–48. [DOI] [PMC free article] [PubMed]
- 7. Yang YH, Zhang XG, Zhang JL, Zhang YB, Kou CP. Risk factors for preoperative respiratory complications in children with tracheobronchial foreign bodies. Int J Med Res. 2016; 44(2):338–345. [DOI] [PMC free article] [PubMed]
- 8. Moslehi MA. Approach to foreign body aspiration in an infant using a cryoprobe. Respir Case Rep. 2020;9(1):4–7.
- 9. Eyekpegha OJ, Onakpoya UU, Obiajunwa PO, Famurewa OC, Ogunrombi AB. Missed distal tracheal foreign body in consecutive bronchoscopies in a 6-year-old boy. Niger J Surg. 2017;23(1):67–70. [DOI] [PMC free article] [PubMed]
- 10. Goussard P, Mfingwana L, Morrison J. Removal of distal airway foreign body with the help of fluoroscopy in a child. Pediatr Pulmonol. 2020;55(3):E5–E7. [DOI] [PubMed]
- 11. Mahmud T, Shafiq A, Hafeez A, Saqib M, Farooq S. Sewing machine needle retrieval from distal airways using flexible bronchoscope under fluoroscopy. Respir Med Case Rep. 2016;19:132–134. [DOI] [PMC free article] [PubMed]
- 12. Laya BF, Restrepo R, Lee EY. Practical imaging evaluation of foreign bodies in children. Radiol Clin N Am. 2017;55(4):845–867. [DOI] [PubMed]
- 13. Yang C, Hua R, Xu K, Hua X, Ma P, Zheng JN, et al. The role of 3D computed tomography (CT) imaging in the diagnosis of foreign body aspiration in children. Eur Rev Med Pharmacol Sci. 2015;19(2):265–273. [PubMed]
- 14. Xu Y, Feng RL, Jiang L, Ren HB, Li Q. Correlative factors for the location of tracheobronchial foreign bodies in infants and children. J Thorac Dis. 2018;10(2):1037–1042. [DOI] [PMC free article] [PubMed]
- 15. Can D, Yilmaz O, Asilsoy S, Gulle S, Yuksel H. Aspiration of foreign bodies that allow air passage through. Open J Pediatr. 2011;1(4):90–93.
- 16. Daines CL, Wood RE, Boesch RP. Foreign body aspiration: an important etiology of respiratory symptoms in children. J Allergy Clin Immunol. 2008;121(5):1297–1298. [DOI] [PubMed]
- 17. Moslehi MA. A rare case of massive foreign body aspiration mimic asthma. Respir Med Case Rep. 2019;28:100963. [DOI] [PMC free article] [PubMed]
- 18. Newby MD, Thomas D, Mullett CJ, Vijay C, Carr MM. Foreign body aspiration presenting as pneumothorax in a child. Cureus. 2020;12(5):e8161. [DOI] [PMC free article] [PubMed]
- 19. Bourrous M, Lahmini W, Nouri H, Haimeur N. Subcutaneous emphysema and pneumomediastinum in child with asthma revealing occult foreign body aspiration: a case report. J Med Case Rep. 2019;13(1):14. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data and materials are available in our clinic and laboratory.


