Abstract
Purpose: Department of Defense policy prohibits, with limited exceptions, transgender individuals from serving in their affirmed gender in the U.S. Military, citing potential impact on unit cohesion and military readiness. To date, however, little is known about the sociodemographic profile and health of transgender military personnel.
Methods: U.S. Military personnel who self-identified as transgender completed anonymous online measures of demographics and military service. Participants also completed measures of health, mood, eating pathology, and risk behaviors.
Results: One hundred ninety-five service members (mean age: 28.9±7.2 years, 48.7% transmale, 70.3% non-Hispanic White, 7.83±5.9 years in service) completed the survey. The majority of respondents first identified as transgender before military accession. Most had disclosed their gender identity to their command and providers, and had undertaken steps toward gender affirmation. The sample as a whole reported above average physical health, with mood symptoms within normal ranges and few reported risk behaviors. Analyses of covariance indicated that transmales reported significantly better mental health and psychosocial functioning compared with transfemales.
Conclusion: In light of current policy that precludes, with limited exceptions, transgender individuals from serving in the U.S. Military in their affirmed gender, the current study provides an initial sociodemographic profile of this understudied population and indicates that transgender service members report above average physical health and few risk behaviors. Preliminary analyses indicated that transfemales in the military may be at higher risk for mental health concerns, compared with transmales. Additional research is needed to elucidate risk and protective factors among transgender service members.
Keywords: active duty, gender dysphoria, military, transgender
Implications and Contribution
The current study provides descriptive and psychosocial information about transgender active duty service members in the U.S. Military. In light of Department of Defense policy that prohibits, except under limited circumstances, transgender individuals with a diagnosis or history of gender dysphoria from serving in the military in their affirmed gender, these data may be useful in better understanding this understudied population.
Introduction
In 2019, the Department of Defense issued a policy stipulating that, with limited exceptions, transgender individuals are ineligible for accession and retention in the U.S. Military unless they serve in their biological sex.1 It is estimated, however, that up to 8000 transgender individuals currently serve on active duty in the U.S. military2,3; although the actual number may be greater4,5 due to insufficient study of this population and potential fear of disclosure of one's gender identity, which may reduce willingness to seek gender-affirming care or self-identify as transgender in surveys. Notably, transgender persons appear twice as likely as members of the general population to serve in the military; 20% of respondents from the National Transgender Discrimination Survey had served in the military, compared to 10% of the general population.6
Despite the possible overrepresentation of transgender individuals in the U.S. Military, there is a paucity of data about the demographic characteristics, military service, and psychosocial functioning of these individuals. To our knowledge, only two studies7,8 have been conducted that specifically examined transgender active duty service members. Given the potential vulnerabilities of both active duty service members9–12 and transgender individuals13–18 to mental health concerns, such as depression, anxiety, stress, substance use, and eating disorders, the risks facing transgender service members may be multi-fold. Additional information about transgender service members is necessary, as the policy pertaining to these individuals continues to evolve. The present study, therefore, aimed to elucidate the sociodemographic profile, psychosocial functioning, health, and military service of active duty service members who self-identify as transgender. As few studies have conducted subgroup analyses by affirmed gender among samples of transgender persons, we also aimed to compare affirmed men and affirmed women on relevant psychosocial factors.
Materials and Methods
Participants and procedures
Participants were active duty service members (≥18 years) who self-identified as transgender. The study was advertised through flyers around military installations in the Washington Metropolitan Area and electronic advertisements disseminated via relevant social media pages. Participants completed all questionnaires anonymously through an online data gathering website (SurveyMonkey) between July and December, 2017. More information on recruitment and data collection may be found elsewhere.19 Written informed consent was waived and no personal identifying information was collected. This study received approval from the authors' Institutional Review Board.
Measures
Demographic data were collected using a 26-item questionnaire designed for the present study that assessed standard demographic characteristics and military service, along with height and weight (from which body mass index [BMI, kg/m2] was determined). Gender identity was assessed using the two-question method20 wherein individuals were asked: “What sex were you assigned at birth, on your original birth certificate?” from which individuals could select male, female, or intersex. Intersex refers broadly to individuals born with sex characteristics or anatomy (e.g., chromosomes, gonads, genitals) that do not fit the traditional definitions of male or female.21 Participants were then asked “What is your current gender identity (check all that apply)”; individuals could select: male, female, intersex, transmale/trans man, transfemale/trans woman, genderqueer/gender nonconforming, and/or other. Individuals were determined to be transgender by the research team if their current gender identity differed from their birth-assigned sex.
The Short-Form 36 Health Survey (SF-36)22 is a widely used self-report measure of emotional and physical health and functioning, comprising two summary scales: Physical Component Summary (PCS) and Mental Health Component Summary (MCS). Scales are calculated using established SF-36 scoring algorithms.23 Final component scores range from 0 to 100, with higher scores indicating better health and functioning.23
The Depression, Anxiety, and Stress Scale (DASS-21)24,25 is a 21-item self-report measure assessing symptoms of depression, anxiety, and stress. The three subscales (Depression, Anxiety, Stress) demonstrated good reliability in the present sample (α's=0.83–0.95). Higher scores indicate greater symptomatology. In accordance with prior convention,26,27 scores were also dichotomized to indicate “normal” vs. “positive” screen for moderate and severe symptomatology.
Given that social norms and positive expectancies around alcohol and drug use may differ among sexual and gender minorities,28,29 a 9-item Risk Behaviors Questionnaire developed for the present study was administered to assess recent and lifetime alcohol, tobacco, and drug use.
As service members and gender minorities both appear to be at increased risk for body dissatisfaction and eating pathology,30–33 the Eating Disorder Examination Questionnaire (EDE-Q),34 a 28-item instrument that assesses diagnostic criteria for eating disorders and related symptomatology in the past 28 days, was administered. The EDE-Q captures the frequency of “binge-eating episodes” defined by the DSM-535 as the consumption of an unambiguously large amount of food accompanied by the subjective experience of loss of control while eating. The episodes are assessed with the following queries: In the past 28 days, how many times have you eaten what other people would regard as an unusually large amount of food (given the circumstances)? On how many of these times did you have a sense of having lost control over your eating (at the time that you were eating)?. Participants also indicate the frequency of compensatory behaviors in the past 28 days (e.g., How many times have you made yourself sick [vomit] as a means of controlling your shape or weight?). The EDE-Q generates four subscales: dietary restraint, eating concern, weight concern, and shape concern, in addition to a global eating pathology score, all of which range from 1 to 6. Higher scores indicated more severe pathology. The EDE-Q subscales demonstrated good reliability in the current sample (α's=0.83–0.89).
Data analytic plan
All analyses were conducted using SPSS for Windows version 25 (SPSS, Inc., Chicago, IL). Descriptive statistics (percentages, central tendencies) were calculated for demographic, military, and psychosocial characteristics. Multiple analyses of covariance were conducted to assess for gender differences (transmale vs. transfemale) adjusting for age, race (White vs. NonWhite), and service rank (Enlisted vs. Officer). For analyses utilizing the EDE-Q, BMI was also included as a covariate. For analyses comparing groups based on affirmed gender, participants identifying as intersex (n=1) or gender nonbinary/other (n=12) were excluded due to the small sample size of these groups. These individuals were retained for all other analyses.
Results
Participant characteristics
Two hundred twenty-nine individuals consented to the survey; of those, 85% (n=195) provided information pertaining to birth-assigned sex and current gender identity. For the purposes of this study, only data from these 195 individuals will be presented. Average age of participants was 28.9±7.2 years. The racial distribution of the sample was 70.3% White, 13.3% Multiracial, 6.2% Black, and 2.6% Asian; 9.2% of the sample was Hispanic.
Of those who currently had a partner or spouse (74%), the majority (77%) were in relationships with cisgender women (individuals assigned female at birth who identify as female) and 16% were in relationships with transgender individuals (See Table 1 for additional demographic information).
Table 1.
Demographic and Psychosocial Characteristics
| Measure | Total sample (n=195) |
|
|---|---|---|
| M±SD | N | |
| Age (years) | 28.8±7.2 | 177 |
| Years in service | 7.9±5.9 | 195 |
| Body mass index (kg/m2) |
25.5±3.8 |
190 |
| |
Valid % |
N |
| Transmale |
48.7 |
95 |
| Transfemale |
44.6 |
87 |
| Other gender identity |
6.7 |
13 |
| Race | ||
| White |
70.3 |
137 |
| Multiracial |
13.3 |
26 |
| Black |
6.2 |
12 |
| Asian |
2.6 |
5 |
| Other/missing |
7.7 |
15 |
| Hispanic ethnicity |
9.2 |
18 |
| Service | ||
| Army |
44.1 |
86 |
| Air Force |
28.2 |
55 |
| Navy |
13.3 |
26 |
| Marine Corps |
6.7 |
13 |
| Coast Guard |
1.5 |
3 |
| Reserves |
6.2 |
12 |
| Rank | ||
| Enlisted |
86.6 |
168 |
| Officer |
13.4 |
26 |
| Marital status | ||
| Unmarried |
59.6 |
115 |
| Married |
40.4 |
78 |
| One or more child |
27.7 |
54 |
| Highest degree | ||
| Some college or less |
70.3 |
137 |
| Bachelor's degree or more |
29.7 |
58 |
| Transition status |
|
|
| No transition/living as birth sex |
16.4 |
32 |
| Any transition | 83.6 | 163 |
Gender identity
Nearly half (48.7%) of participants identified as transmale, 44.6% identified as transfemale, 6.2% identified as nonbinary, genderqueer, or “other,” and 0.5% (n=1) identified as intersex. Half of the sample first self-identified as transgender before the age of 11, 15% during adolescence, and 29.5% between 18 and 29 years. Less than 4% of the sample was older than 30 at the time they first self-identified as transgender.
Gender affirmation
The majority of respondents (n=163) reported undergoing at least some measure of gender affirmation (e.g., gender affirming surgery, hormone therapy, legal name/sex change, and/or dressing in accordance with chosen gender). The majority of the sample (79%) reported dressing in accordance with their affirmed gender. Seventy percent have undergone or are undergoing gender-affirming hormone therapy (Testosterone: 35%, Estrogen: 25%, Progestin: 5%, Anti-Androgens: 21%, “Other” [e.g., Finasteride for hair loss, gonadotropin-releasing hormone agonist]: 2%). Thirty-one percent have undergone gender-affirming surgery (chest reconstruction or breast augmentation [27%] and/or gonadectomy and/or genital reconstruction [10%]). Forty-eight percent have legally changed their names and 43% have changed their gender marker on legal documents. Sixteen percent (n=32) reported that they have not undertaken any measures of transition and are living as their birth-assigned sex.
Nearly all participants (99.5%) indicated that at least one person is aware of their gender identity. The majority reported that their mother (74%), father (65%), and/or significant others (64%) are aware. The majority also indicated that their primary care physician (79%), chain of command (74%), and/or supervisor (69%) know of their gender identity. Sixty-three percent reported that “almost everyone” in their lives is aware of their gender identity.
Military service
Most (86.6%) respondents were enlisted (vs. officers). Forty-four percent of respondents were serving on active duty in the Army, 28% Air Force, 13% Navy, 6.7% Marine Corps, and 1.5% Coast Guard. Six percent were in the Reserves (any service). On average, participants had served ∼8 years (7.8±5.9) in the military; nearly a third (29%) had served 10 years or more. Sixty-eight percent reported at least one deployment with 40% having deployed to a combat zone (e.g., Afghanistan, Iraq).
Mood symptoms
Mean scores for depression (10.2±10.9), anxiety (6.6±7.3), and stress (12.2±8.9) subscales of the DASS-21 indicated minimal levels of symptomatology (Table 2). Using recommended cutoff scores,27 34.1% of respondents screened positive for moderate to severe depression, 28.3% for moderate to severe anxiety, and 21.7% for moderate to severe stress.
Table 2.
Subgroup Analyses for Psychological Variables by Gender Identity
| Measure | Rangea | Transmales (n=95) |
Transfemales (n=87) |
|
||
|---|---|---|---|---|---|---|
| M±SD | N | M±SD | N | F | ||
| Depression | 0–40 | 7.8±10.2 | 71 | 12.7±10.9 | 57 | 6.8* |
| Anxiety | 0–40 | 5.5±7.0 | 71 | 7.4±7.6 | 57 | 2.0 |
| Stress | 0–40 | 10.6±9.4 | 71 | 13.3±7.9 | 57 | 3.1 |
| Eating disorder examination | ||||||
| Restraint | 0–6.0 | 1.2±1.5 | 53 | 2.8±1.8 | 48 | 21.7*** |
| Eating concern | 0–5.8 | 0.24±0.60 | 52 | 1.1±1.4 | 46 | 15.1*** |
| Shape concern | 0–5.5 | 1.6±1.5 | 52 | 2.7±1.7 | 46 | 11.7** |
| Weight concern | 0–5.4 | 0.91±1.2 | 52 | 2.0±1.7 | 46 | 13.1*** |
| Global eating Pathology | 0–6.0 | 0.97±1.0 | 53 | 2.2±1.5 | 48 | 23.3*** |
| Physical health | 0–100 | 55.1±7.4 | 79 | 56.1±9.2 | 69 | 0.58 |
| Mental health | 0–100 | 48.5±12.2 | 79 | 39.0±14.1 | 69 | 19.2*** |
Statistical test conducted: one-way analysis of variance.
Higher scores indicate greater pathology, except for SF-36 scales (Physical Health and Mental Health), wherein higher scores indicate better health.
p<0.05, **p<0.01, ***p<0.001.
SF-36, Short-Form 36 Health Survey.
Health indices and behaviors
Participants' mean PCS score was 55.5±8.3 and mean MCS score was 43.4±14.1 (wherein 100 indicates perfect health). The mean BMI of the sample was 25.5 (indicating the presence of overweight); over half (56%) of the sample had overweight (BMI ≥25) and 11% had obesity (BMI ≥30).
Utilizing a cutoff of ≥4 as a marker of clinical significance on the EDE-Q,36 15% of respondents scored in the clinically significant range on the Restraint subscale, 3% on the Eating Concern subscale, 16% on the Shape Concern subscale, 7% on the Weight Concern subscale, and 9% on the Global score. Over one quarter (25.8%) reported a binge-eating episode (consuming an objectively large amount of food while experiencing a subjective feeling of loss of control) in the past month, and over one-third (34%) reported engaging in compulsive exercise as a means of controlling their shape/weight. Few (n=4) reported purging or laxative misuse.
Twenty-nine percent of respondents reported ever smoking; 22% of the sample were current smokers (defined as smoking ≥100 cigarettes in their lifetime and currently smoking at least once/week), and 7% were current daily smokers. Among those who had ever smoked, the mean age of initiation was 17.5±4.0 years. The majority (70.4%) of participants reported drinking alcoholic beverages no more than three times per month. Twenty-eight percent of respondents reported drinking alcoholic beverages between one and six times per week. The majority (80%) of respondents consume between one and four drinks per drinking occasion, with 7% consuming five or more drinks per drinking occasion. The majority (81.5%) denied any lifetime drug use. Among those who reported any lifetime drug use (n=25), the most common substances were: marijuana (100%), prescription narcotics (32%), prescription sedatives (32%), psychedelics (28%), cocaine (24%), and ecstasy (24%).
Subgroup analyses by gender identity
Those identifying as transfemale were significantly more likely to be non-Hispanic White (86% vs. 68%; Pearson's χ2=9.2, p=0.03) and were significantly more likely to have children (56% vs. 17%; Pearson's χ2=23.89, p<0.001) when compared with transmales. Transfemales were less likely to have undertaken steps toward affirmation than transmales (76% vs. 92%; Pearson's χ2=8.37, p<0.004). Transfemales were also older (30.06±7.30 years vs. 27.06±5.91 years; p=0.004), had served longer in the military (9.70±6.75 years vs. 5.97±3.93 years; p<0.001), and had significantly lower BMI (24.88±3.97 vs. 26.16±3.52, p=0.02) compared with transmales.
Adjusting for age, race (White vs. NonWhite), and rank (Enlisted vs. Officer), transfemales had significantly better physical health [SF-PCS: 56.11 vs. 55.07; F (1, 120)=5.40, p=0.022], whereas transmales had significantly better mental health [SF-MCS: 48.49 vs. 39.01; F (1, 120)=11.88, p=0.001] and fewer depressive symptoms [DASS Depression: 7.77 vs. 12.67; F(1, 103)=4.92, p=0.029]. Compared with transmales, transfemales were over two and a half times more likely to report moderate to severe depression (odds ratio: 2.57, 95% confidence interval 1.06–6.23). Adjusting for age, race, service rank, and BMI, transfemales had significantly greater dietary restraint, eating, shape, and weight concerns, and global eating pathology (p's≤0.004) (Table 2 and Fig. 1). There were no significant gender differences for anxiety, stress, smoking status, or any other risk behavior or demographic variable (p's>0.05).
FIG. 1.
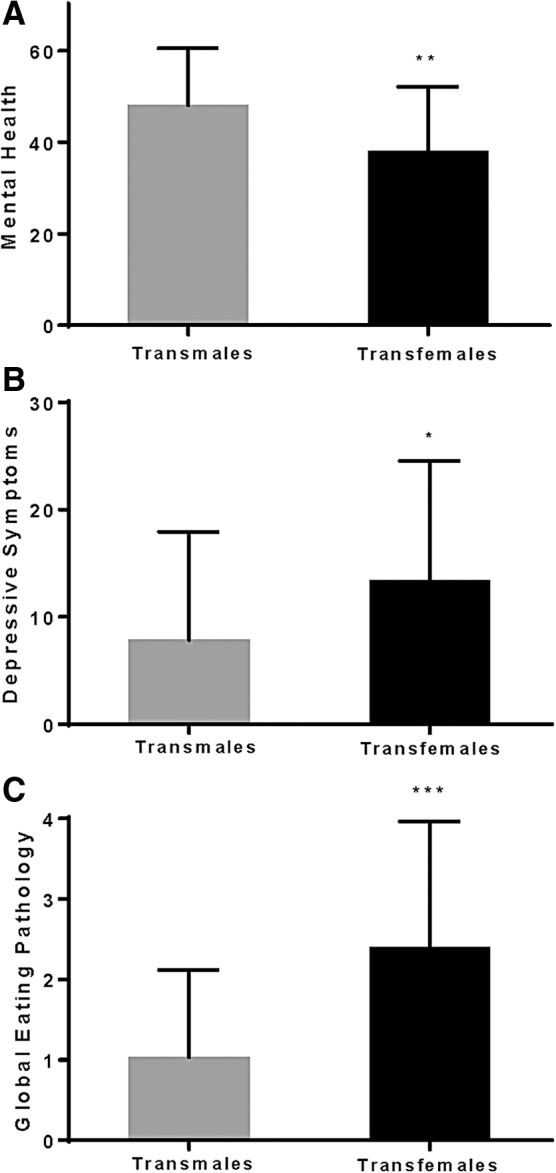
Significant differences in (A) mental health, (B) depressive symptoms, and (C) global eating pathology by gender identity (p's ≤0.029), after adjusting for covariates.
Discussion
This study is among the first to provide a sociodemographic and psychosocial profile of transgender active duty personnel in the U.S. Military. Findings indicated that participants, on average, had spent nearly 8 years in the military, and that the majority had deployed at least once, including to combat zones. The majority of the sample first identified as transgender before joining the military, and most reported that they are currently living as their affirmed gender. To that end, most reported use of gender-affirming hormone therapy and wearing clothing consistent with their affirmed gender to achieve transition, whereas a significant minority reported gender-affirming surgery. Nearly all respondents reported that at least one person is aware of their gender identity, and most reported that multiple individuals, including fellow service members, are aware. In addition, most reported that their chains of command, military supervisors, and primary care physicians are aware of their gender identity.
The sample as a whole was largely healthy, with unadjusted physical health scores (as assessed by the SF-36) comparable to those observed in a sample of over 75,000 active duty military service members.37 Scores on the mental health component of the SF-36, however, were 10 points lower than this same reference group,37 and both transmales and transfemales in the current sample scored lower than their respective cisgender counterparts.37 The decrement in emotional well-being may be partially attributable to the chronic stress associated with gender minority status and stigma.19,38–40
The prevalence of depression in the current sample was considerably higher than that reported in a meta-analysis of major depression among active duty service members (34% in the current sample compared to 13.1% of previously deployed service members observed in the meta-analysis).41 Participants' mean depression scores were lower, however, than a sample of older (mean age 57 years) military veterans.42
The current sample largely denied the use of prescription and illicit drugs and few reported problematic drinking behaviors. A greater proportion of the sample currently smoked cigarettes when compared with the general population (22% vs. 15.5%43), though rates were considerably lower than those observed among military veterans of a similar age (37%).44
Over half of the sample had overweight, which is comparable to larger studies of active duty service members.45 Overall, the present sample endorsed disordered eating pathology that was greater than nonclinical community samples of young men,46 roughly equivalent to samples of young adult women,47,48 but less severe than clinical eating disorder-treatment-seeking samples.49 Norms on the EDE-Q for military samples have not yet been established; therefore, it is unknown whether transgender service members are at increased risk for eating pathology compared to the broader population of military personnel. As both service members50–57and gender minorities30,58–60 may independently be at high-risk for eating disorders, it is possible that transgender service members' vulnerability may be compounded by membership in two high-risk groups.
Extant studies of transgender service members typically do not include subgroup analyses by affirmed gender;3,8 the current study, in contrast, included exploratory analyses to examine differences by gender identity. The physical health of transfemales exceeded that of transmales in the current study. Further, the physical health score of transmales in the current sample approximated the physical health score of a large age-matched sample of cisgender male military personnel (55.1 and 54.2, respectively), while the physical health score for transfemales in the current study exceeded that observed in an age-matched sample of cisgender female military personnel (56.1 and 53.5, respectively).
Findings from the current study indicated that transfemales had significantly greater mental health, depressive and eating disorder symptoms compared with transmales, even after adjusting for relevant covariates. These data corroborate previous studies of both active duty61 and veteran62–64 populations indicating that cisgender females report greater symptoms of mood and eating disorders than cisgender males. Transfemales in the current sample had higher rates of clinically significant anxiety on the DASS compared with a cisgender sample of female veterans (27.6% vs. 24.1%). In contrast, transmales in the current study had lower rates of clinically significant anxiety on the DASS compared with their cisgender male veteran counterparts (20.0% vs. 23.1%).65 Prior studies have also found higher rates of post traumatic stress disorder (PTSD) among male service members when compared with women; however, PTSD symptoms were not assessed in the current study, therefore we are unable to determine whether these gender differences manifest among transgender service members. Though direct comparisons with previously published data should be interpreted cautiously, these preliminary comparisons suggest that the psychosocial risk profile of transgender service members may most closely resemble that of their affirmed gender. Specifically, with regard to mental health characteristics, transfemales in the current sample seem to more closely match cisgender females from prior studies, while transmales seem to most closely match cisgender males.
Of note, far more transfemales were living as their birth-assigned sex when compared with transmales. This may be due to cultural norms that encourage a broader spectrum of gender presentations among those born female while penalizing those born male for gender expressions that deviate from societal expectations. Further, the traditionally male culture and emphasis on hypermasculinity within the military66–68 may contribute to feelings of alienation and subsequent negative affect among transfemales. The finding that transmales, who were significantly more likely to have taken steps toward gender affirmation, presented with better mental health may provide further evidence supporting the effectiveness of gender-affirming treatments in ameliorating distress and improving quality of life.69,70
Further gender disparities were observed among indices of eating- and weight-related pathology. More specifically, similar to the gender differences observed in cisgender samples that largely indicate that females are disproportionately affected by eating disorders,71 transfemales in the current sample reported significantly greater eating- and weight-related concerns when compared with transmales. These disparities are in contrast to a prior study finding no gender differences in eating pathology in a sample of transgender adolescents.72 However, these differences are consistent with prior research demonstrating that sexual and gender minority natal males may be at greater risk for body dissatisfaction and eating pathology compared with sexual and gender minority natal females.31,73–76 The pursuit of a conventionally feminine shape may contribute to the increased eating- and weight-related pathology observed among transfemales in the current study. In contrast, body ideals for transmales may be more lenient or encouraging of a larger body size.77 Overall, findings indicate that transgender military members closely match or exceed physical health scores observed in a large, age-matched cisgender military sample. Furthermore, we observed differences in psychosocial risk profiles, indicating that transfemales were more likely than transmales to experience mental health symptomatology, including eating and weight concerns.
The present study is limited by its reliance on self-reported, cross-sectional survey data, which precludes causal interpretations. The lack of a cisgender military or transgender civilian control group also precludes direct comparisons and the ability to isolate the unique effects of gender identity on health and functioning among service members. Previous research using similar psychological assessments enables preliminary comparisons with norms from military and civilian samples; however, given differences in methodologies, demographics, and cohorts, comparisons with previously published research should be interpreted conservatively.
Finally, all data were collected after notification in July 2017 of a possible policy change impacting transgender military personnel.1 Therefore, it is possible that specific factors unique to the data collection time period exist that further limit generalizability. Despite these limitations, this study provides novel sociodemographic and psychosocial information about an understudied and highly vulnerable group.
This study is an important first step in better understanding the sociodemographic and health profile of transgender active duty service members. However, more research is needed. Specifically, future research should include matched cisgender controls to elucidate possible health disparities based on gender identity, while controlling for military-specific factors. In addition, analyses should be undertaken in adequately powered studies to ascertain differences based on other sociodemographic factors, such as race, ethnicity, extent of affirmation, and the effects of intersectionality on outcomes. In addition, prospective research is needed to understand the health trajectories of transgender individuals over the course of their military careers, the potential impact of current Department of Defense policy on health and functioning, and to elucidate protective factors, such as social support, that might affect outcomes.
Acknowledgements
The authors wish to thank the study participants for their contributions to the current research and their military service.
Abbreviations Used
- BMI
Body Mass Index
- DASS-21
Depression, Anxiety, and Stress Scale
- EDE-Q
Eating Disorder Examination Questionnaire
- SF-36
Short-Form 36 Health Survey
- MCS
Mental Health Component Summary
- PCS
Physical Component Summary
- PTSD
Post-Traumatic Stress Disorder
Disclaimer
The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of USU, the U.S. Air Force, U.S. Army, U.S. Navy, U.S. Military at large, or U.S. Department of Defense.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This study was funded by an American Psychological Foundation Visionary Grant (awarded to N.A.S.). Funding sources had no involvement in the study design, data collection and analysis, preparation of the article, or decision to submit the article for publication.
Cite this article as: Schvey NA, Klein DA, Pearlman AT, Riggs DS (2020) A descriptive study of transgender active duty service members in the U.S. Military, Transgender Health 5:3, 149–157, DOI: 10.1089/trgh.2019.0044.
References
- 1. Directive-type Memorandum (DTM)-19-004—Military Service by Transgender Persons and Persons with Gender Dysphoria [press release]. 2019 [Google Scholar]
- 2. Schaefer AG, Iyengar R, Kadiyala S, et al. Assessing the Implications of Allowing Transgender Personnel to Serve Openly. Santa Monica, CA: Rand Corporation, 2016 [Google Scholar]
- 3. Meadows SO, Engel CC, Collins RL, et al. 2015 Department of Defense Health Related Behaviors Survey (HRBS). Santa Monica, CA: Rand Corporation, 2018 [PMC free article] [PubMed] [Google Scholar]
- 4. Belkin A. Caring for our transgender troops—the negligible cost of transition-related care. N Engl J Med. 2015;373:1089–1092 [DOI] [PubMed] [Google Scholar]
- 5. 2016 Workplace and Gender Relations Survey of Active Duty Members. In: OPA Report No. 2016–050. ((OPA) OoPA, ed). Alexandria, VA: Office of People Analytics, 2017 [Google Scholar]
- 6. Harrison-Quintana J, Herman JL. Still serving in silence: transgender service members and veterans in the National Transgender Discrimination Survey. LGBTQ Policy J. 2013;3:1–13 [Google Scholar]
- 7. Parco JE, Levy DA, Spears SR. Transgender military personnel in the post-DADT repeal era: a phenomenological study. Armed Forces Soc. 2015;41:221–242 [Google Scholar]
- 8. Hill BJ, Bouris A, Barnett JT, Walker D. Fit to serve? Exploring mental and physical health and well-being among transgender active-duty service members and veterans in the U.S. Military. Transgend Health. 2016;1:4–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hoge CW, Toboni HE, Messer SC, et al. The occupational burden of mental disorders in the US military: psychiatric hospitalizations, involuntary separations, and disability. Am J Psychiatry. 2005;162:585–591 [DOI] [PubMed] [Google Scholar]
- 10. Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22 [DOI] [PubMed] [Google Scholar]
- 11. Hoge CW, Lesikar SE, Guevara R, et al. Mental disorders among U.S. military personnel in the 1990s: association with high levels of health care utilization and early military attrition. Am J Psychiatry. 2002;159:1576–1583 [DOI] [PubMed] [Google Scholar]
- 12. Jordan BK, Schlenger WE, Hough R, et al. Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Arch Gen Psychiatry. 1991;48:207–215 [DOI] [PubMed] [Google Scholar]
- 13. Blosnich JR, Gordon AJ, Fine MJ. Associations of sexual and gender minority status with health indicators, health risk factors, and social stressors in a national sample of young adults with military experience. Ann Epidemiol. 2015;25:661–667 [DOI] [PubMed] [Google Scholar]
- 14. Matarazzo BB, Barnes SM, Pease JL, et al. Suicide risk among lesbian, gay, bisexual, and transgender military personnel and veterans: what does the literature tell Us? Suicide Life Threat Behav. 2014;44:200–217 [DOI] [PubMed] [Google Scholar]
- 15. Bockting WO, Miner MH, Swinburne Romine RE, et al. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013;103:943–951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Budge SL, Adelson JL, Howard KA. Anxiety and depression in transgender individuals: the roles of transition status, loss, social support, and coping. J Consult Clin Psychol. 2013;81:545. [DOI] [PubMed] [Google Scholar]
- 17. Grant JM, Mottet LA, Tanis J, et al. National Transgender Discrimination Survey Report on Health and Health Care. National Center for Transgender Equality and National Gay and Lesbian Task Force Washington, DC, 2010, pp. 1–23 [Google Scholar]
- 18. Lombardi EL, Wilchins RA, Priesing D, Malouf D. Gender violence: transgender experiences with violence and discrimination. J Homosex. 2002;42:89–101 [DOI] [PubMed] [Google Scholar]
- 19. Schvey N, Klein DA, Pearlman A, et al. Stigma, health, and psychosocial functioning among transgender active duty service members in the U.S. Military. Stigma Health. 2020;5:188–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tate CC, Ledbetter JN, Youssef CP. A two-question method for assessing gender categories in the social and medical sciences. J Sex Res. 2013;50:767–776 [DOI] [PubMed] [Google Scholar]
- 21. Kraus C. Classifying intersex in DSM-5: critical reflections on gender dysphoria. Arch Sex Behav. 2015;44:1147–1163 [DOI] [PubMed] [Google Scholar]
- 22. Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483 [PubMed] [Google Scholar]
- 23. Ware J, Ma K, Keller SD. SF-36 Physical and Mental Health Summary Scales: a User's Manual. Boston, MA: The Health Institute,1994 [Google Scholar]
- 24. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–343 [DOI] [PubMed] [Google Scholar]
- 25. Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–239 [DOI] [PubMed] [Google Scholar]
- 26. McGraw L, Pickering MA, Ohlson C, Hammermeister J. The influence of mental skills on motivation and psychosocial characteristics. Mil Med. 2012;177:77–84 [DOI] [PubMed] [Google Scholar]
- 27. Lovibond S, Lovibond P. Manual for the Depression Anxiety & Stress Scales, 2nd ed. Sydney: Psychology Foundation, 1995 [Google Scholar]
- 28. Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135:707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hatzenbuehler ML, Corbin WR, Fromme K. Trajectories and determinants of alcohol use among LGB young adults and their heterosexual peers: results from a prospective study. Dev Psychol. 2008;44:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Watson RJ, Veale JF, Saewyc EM. Disordered eating behaviors among transgender youth: probability profiles from risk and protective factors. Int J Eat Disord. 2017;50:515–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Katz-Wise SL, Scherer EA, Calzo JP, et al. Sexual minority stressors, internalizing symptoms, and unhealthy eating behaviors in sexual minority youth. Ann Behav Med. 2015;49:839–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mason TB, Lewis RJ. Minority stress and binge eating among lesbian and bisexual women. J Homosex. 2015;62:971–992 [DOI] [PubMed] [Google Scholar]
- 33. Bartlett BA, Mitchell KS. Eating disorders in military and veteran men and women: a systematic review. Int J Eat Disord. 2015;48:1057–1069 [DOI] [PubMed] [Google Scholar]
- 34. Fairburn C, Beglin S. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16:363–370 [PubMed] [Google Scholar]
- 35. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Arlington: American Psychiatric Publications, 2013 [Google Scholar]
- 36. Carter JC, Stewart DA, Fairburn CG. Eating disorder examination questionnaire: norms for young adolescent girls. Behav Res Ther. 2001;39:625–632 [DOI] [PubMed] [Google Scholar]
- 37. Smith TC, Zamorski M, Smith B, et al. The physical and mental health of a large military cohort: baseline functional health status of the Millennium Cohort. BMC Public Health. 2007;7:340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. 1995:38–56 [PubMed] [Google Scholar]
- 39. Meyer IH, Frost DM. Minority stress and the health of sexual minorities. In: Handbook of Psychology and Sexual Orientation. (Patterson CJ, D'Augelli AR; eds). New York: Oxford University Press, 2013, pp. 252–266 [Google Scholar]
- 40. Frost DM, Lehavot K, Meyer IH. Minority stress and physical health among sexual minority individuals. J Behav Med. 2015;38:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gadermann AM, Engel CC, Naifeh JA, et al. Prevalence of DSM-IV major depression among US military personnel: meta-analysis and simulation. Mil Med. 2012;177(suppl_8):47–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Owens GP, Steger MF, Whitesell AA, Herrera CJ. Posttraumatic stress disorder, guilt, depression, and meaning in life among military veterans. J Trauma Stress Disord. 2009;22:654–657 [DOI] [PubMed] [Google Scholar]
- 43. Jamal A, Phillips E, Gentzke AS, et al. Current cigarette smoking among adults—United States, 2016. Morb Mortal Wkly Rep. 2018;67:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Brown DW. Smoking prevalence among US veterans. J Gen Intern Med. 2010;25:147–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Eilerman PA, Herzog CM, Luce BK, et al. A comparison of obesity prevalence: military health system and United States populations, 2009–2012. Mil Med. 2014;179:462–470 [DOI] [PubMed] [Google Scholar]
- 46. Lavender JM, De Young KP, Anderson DA. Eating Disorder Examination Questionnaire (EDE-Q): norms for undergraduate men. Eat Behav. 2010;11:119–121 [DOI] [PubMed] [Google Scholar]
- 47. Welch E, Birgegård A, Parling T, Ghaderi A. Eating disorder examination questionnaire and clinical impairment assessment questionnaire: general population and clinical norms for young adult women in Sweden. Behav Res Ther. 2011;49:85–91 [DOI] [PubMed] [Google Scholar]
- 48. Mond JM, Hay PJ, Rodgers B, Owen C. Eating Disorder Examination Questionnaire (EDE-Q): norms for young adult women. Behav Res Ther. 2006;44:53–62 [DOI] [PubMed] [Google Scholar]
- 49. Aardoom JJ, Dingemans AE, Slof Op't Landt M, Van Furth EF. Norms and discriminative validity of the Eating Disorder Examination Questionnaire (EDE-Q). Eating Behav. 2012;13:305–309 [DOI] [PubMed] [Google Scholar]
- 50. Forman-Hoffman VL, Mengeling M, Booth BM, et al. Eating disorders, post-traumatic stress, and sexual trauma in women veterans. Mil Med. 2012;177:1161–1168 [DOI] [PubMed] [Google Scholar]
- 51. Jacobson IG, Smith TC, Smith B, et al. Disordered eating and weight changes after deployment: longitudinal assessment of a large US military cohort. Am J Epidemiol. 2009;169:415–427 [DOI] [PubMed] [Google Scholar]
- 52. Antczak A, Brininger T. Diagnosed eating disorders in the U.S. Military: a nine year review. Eat Disord. 2008;16:363–377 [DOI] [PubMed] [Google Scholar]
- 53. Warner C, Matuszak T, Rachal J, et al. Disordered eating in entry-level military personnel. Mil Med. 2007;172:147–151 [DOI] [PubMed] [Google Scholar]
- 54. Carlton J, Manos G, Van Slyke J. Anxiety and abnormal eating behaviors associated with cyclical readiness testing in a naval hospital active duty population. Mil Med. 2005;170:663–667 [DOI] [PubMed] [Google Scholar]
- 55. McNulty P. Prevalence and contributing factors of eating disorder behaviors in active duty service women in the Army, Navy, Air Force, and Marines. Mil Med. 2001;166:53–58 [PubMed] [Google Scholar]
- 56. Lauder TD, Williams MV, Campbell CS, et al. Abnormal eating behaviors in military women. Med Sci Sports Exerc. 1999;31:1265–1271 [DOI] [PubMed] [Google Scholar]
- 57. McNulty P. Prevalence and contributing factors of eating disorder behaviors in active duty Navy men. Mil Med. 1997;162:753–758 [PubMed] [Google Scholar]
- 58. Guss CE, Williams DN, Reisner SL, et al. Disordered weight management behaviors and non-prescription steroid use in Massachusetts transgender youth. J Adolesc Health. 2016;58:S102–S103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Diemer EW, Grant JD, Munn-Chernoff MA, et al. Gender identity, sexual orientation, and eating-related pathology in a national sample of college students. J Adolesc Health. 2015;57:144–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ålgars M, Santtila P, Sandnabba NK. Conflicted gender identity, body dissatisfaction, and disordered eating in adult men and women. Sex Roles. 2010;63:118–125 [Google Scholar]
- 61. Luxton DD, Skopp NA, Maguen S. Gender differences in depression and PTSD symptoms following combat exposure. Depress Anxiety. 2010;27:1027–1033 [DOI] [PubMed] [Google Scholar]
- 62. Maguen S, Cohen B, Ren L, et al. Gender differences in military sexual trauma and mental health diagnoses among Iraq and Afghanistan veterans with posttraumatic stress disorder. Womens Health Issues. 2012;22:e61–e66 [DOI] [PubMed] [Google Scholar]
- 63. Haskell SG, Gordon KS, Mattocks K, et al. Gender differences in rates of depression, PTSD, pain, obesity, and military sexual trauma among Connecticut War Veterans of Iraq and Afghanistan. J Womens Health (Larchmt). 2010;19:267–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Maguen S, Ren L, Bosch JO, et al. Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care. Am J Public Health. 2010;100:2450–2456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Street AE, Gradus JL, Giasson HL, et al. Gender differences among veterans deployed in support of the wars in Afghanistan and Iraq. J Gen Intern Med. 2013;28:556–562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Brown GR. Transsexuals in the military: flight into hypermasculinity. Arch Sex Behav. 1988;17:527–537 [DOI] [PubMed] [Google Scholar]
- 67. Rosen LN, Bliese PD, Wright KA, Gifford RK. Gender composition and group cohesion in US army units: a comparision across five studies. Armed Forces Soc. 1999;25:365–386 [Google Scholar]
- 68. Rosen LN, Knudson KH, Fancher P. Cohesion and the culture of hypermasculinity in US Army units. Armed Forces Soc. 2003;29:325–351 [Google Scholar]
- 69. Nguyen HB, Chavez AM, Lipner E, et al. Gender-affirming hormone use in transgender individuals: impact on behavioral health and cognition. Curr Psychiatry Rep. 2018;20:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Bränström R, Pachankis JE. Reduction in mental health treatment utilization among transgender individuals after gender-affirming surgeries: a total population study. Am J Psychiatry. 2019. DOI: 10.1176/appi.ajp.2019.19010080 [DOI] [PubMed] [Google Scholar]
- 71. Hoek HW. Distribution of eating disorders. In: Eating Disorders and Obesity: A Comprehensive Handbook. (Fairburn CG, Brownell KD; eds). New York: Guilford Press, vol. 2. 2002, pp. 233–237 [Google Scholar]
- 72. Avila JT, Golden NH, Aye T. Eating disorder screening in transgender youth. J Adolesc Health. 2019;65:815–817 [DOI] [PubMed] [Google Scholar]
- 73. Calzo JP, Sonneville KR, Haines J, et al. The development of associations among body mass index, body dissatisfaction, and weight and shape concern in adolescent boys and girls. J Adolesc Health. 2012;51:517–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Austin SB, Nelson LA, Birkett MA, et al. Eating disorder symptoms and obesity at the intersections of gender, ethnicity, and sexual orientation in US high school students. Am J Public Health. 2013;103:e16–e22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Grammer A, Byrne M, Pearlman A, et al. Overweight and obesity in sexual and gender minority adolescents: a systematic review. Obes Rev. 2019;20:1350–1366 [DOI] [PubMed] [Google Scholar]
- 76. Calzo JP, Blashill AJ, Brown TA, Argenal RL. Eating disorders and disordered weight and shape control behaviors in sexual minority populations. Curr Psychiatry Rep. 2017;19:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. McClain Z, Peebles R. Body image and eating disorders among lesbian, gay, bisexual, and transgender youth. Pediatr Clin. 2016;63:1079–1090 [DOI] [PMC free article] [PubMed] [Google Scholar]


