Abstract
Objective:
This study tests the effectiveness of parent-teen psychotherapy for adolescent ADHD (Supporting Teens’ Autonomy Daily; STAND) versus Usual Care (UC) in four community clinics.
Method:
A randomized clinical trial was conducted with double randomization of adolescents and therapists to STAND vs. UC. Participants were 278 culturally-diverse adolescents diagnosed with DSM-5 ADHD at baseline and 82 community therapists. Seven primary outcomes were assessed at baseline (BL), post-treatment (PT; M=5.11 months post-BL, SD=2.26), and follow-up (FU; M=9.81 months post-BL, SD=2.50): inattention (IN; parent/teacher-rated), academics (parent-rated/official records), family functioning (parent/adolescent-rated), and disciplinary records. Treatment engagement indicated consumer fit (e.g., number or sessions received, percentage of sessions attended by parent, satisfaction). The impact of treatment on concurrent medication use was also examined. Service delivery features were examined as moderators of outcome.
Results:
Intent to treat (N=278) analyses indicated no significant group × time effects. STAND only led to superior outcomes when therapists were licensed (22% of sample) vs. unlicensed (parent-rated IN: p<.001, d=1.08; parent-rated academic impairment: p=.010, d=1.17). Compared to UC, STAND was associated with greater parent participation (p<.001, d=.88) and higher scores on certain indices of parent satisfaction. STAND also was associated with superior medication engagement over time compared to UC (OR=7.18).
Conclusion:
Evidence-based psychosocial treatment for adolescent ADHD did not outperform UC on outcome trajectories despite improving some indices of treatment engagement. STAND requires additional adaptation for community contexts.
Clinical trial registration information:
STAND Community Trial (STAND); clinicaltrials.gov; NCT02694939.
Keywords: ADHD, community-based treatment, psychotherapy, adolescence
Introduction
Practice parameters recommend medication as first-line treatment for adolescent Attention-deficit/hyperactivity disorder (ADHD) with psychosocial treatment encouraged as needed1,2. Despite the efficacy of both approaches, adolescents with ADHD access far fewer services than children in their communities3–5. Medication is the cornerstone childhood ADHD treatment; however, adolescents often discontinue ADHD medication perceiving adverse effects, stigma, and ineffectiveness6–7. Adolescents with ADHD appear willing to engage in psychosocial treatments8–9. However, evidence-based practices (EBPs) are costlier and more burdensome to implement than medication and usual care psychological services10,11; as a result, they are offered in few community clinics12. To bridge this gap, research should adapt and refine adolescent ADHD EBPs to fit the constraints of community contexts, evaluating their implementation and effectiveness. In this trial, we utilize a Hybrid Type 1 implementation-effectiveness design13 to evaluate an EBP for adolescent ADHD (Supporting Teen’s Autonomy Daily; STAND)14–16 compared to usual care at four community clinics. Implementation outcomes are previously reported.17
STAND
STAND is a ten-session manualized EBP that targets ADHD symptoms and related impairments (i.e., family conflict, organization skills, homework problems) and is delivered individually to parent-teen dyads18. Like other EBPs for adolescent ADHD, STAND directly teaches skills (e.g., organization and time management, communication) and engages adults in autonomy-supportive roles—not merely supervisors of behavior modification18,19. Because patient barriers often prompt premature disengagement from adolescent ADHD treatment20, STAND includes engagement-focused components: (1) parent-teen collaboration, (2) Motivational Interviewing (MI)21, (3) modular treatment22, and (4) strength-based, autonomy-supportive activities. STAND is divided into engagement, skills, and planning sessions. Population-relevant process issues are addressed through MI (i.e., motivation deficits, inconsistent family routines, intrusive parenting, regulating electronics, skepticism about behavioral techniques)23.
Three randomized clinical trials (RCTs) of STAND demonstrate efficacy in university settings14–16. In a pilot RCT (N=36), STAND was delivered with high fidelity (i.e., 93%-100% content fidelity across sessions) and was highly acceptable to families. Compared to treatment as usual, large effects were present for ADHD and ODD symptoms (d=.82 to 1.42), academic indices (d=1.30 to 5.15), and parent-teen conflict (d=.65) from baseline to post-treatment14. A larger RCT (N=128) demonstrated full or partial maintenance of similar effects at six-month follow-up (d=.63 to 1.01) and detected effects on parental outcomes including parenting stress (d=.60) and use of behavioral strategies (d=.49 to 1.07)15. A third RCT (N=123) compared STAND to standard group behavioral parent training and teen organization skills training and found superior effects for STAND when parents possessed elevated ADHD (d=.50) or depression symptoms (d=.64) or dyads displayed high parent-teen conflict (d=.51)16.
Community-Based STAND Implementation Outcomes
Recently, we reported implementation outcomes for this trial17. Adolescents with ADHD (N=278) were randomly assigned to receive psychosocial treatment from agency therapists who also were randomized either to delivery usual care psychotherapy or receive training and supervision in STAND. Approximately 96% of therapists assigned to STAND completed the three-day training and, on average, attended 87% of scheduled weekly supervision sessions. Although therapists rated STAND as highly acceptable, relevant, and lower burden than UC practices (d=.40-.86), fidelity was poorer than in university-based trials14–16. Average community-based fidelity ranged from 85% in skills sessions to 24% in planning sessions17. Therapists delivered STAND at a slower pace and lower intensity than the manual intended. However, they also demonstrated significantly higher MI integrity scores compared to UC therapists (d=.21 to .79) and delivered STAND with high fidelity in office-based and early sessions. Thus, implementation of STAND in community contexts was promising but requires refinement to improve aspects of fidelity.
Aim 1: Effect of Community-Based STAND on Symptoms and Impairment
The current study’s primary aim is to test whether STAND improves patient outcome trajectories (i.e., ADHD symptoms, academic, family, and behavioral functioning) compared to UC. Due to previously documented fidelity disruptions22, we hypothesize that effectiveness will decrease when STAND is delivered in community contexts (versus past university trials) but will exceed UC. Although standard EBPs for youth psychiatric disorders often do not outperform UC,24–25 STAND includes elements that promote engagement and effectiveness in community settings21–22,26. STAND also outperforms standard behavior therapy when families are clinically complex, which is characteristic of community contexts27–28. Thus, even a diluted dose of STAND may outperform UC.
Aim 2: Therapeutic Engagement
We also examined whether STAND increases therapeutic engagement (i.e., improved retention in services, parent participation, stakeholder satisfaction), including concurrent medication utilization. Because of its engagement-focused approach, we hypothesized that community-delivered STAND would be associated with higher retention in services, greater parent participation, and higher levels of stakeholder satisfaction across targeted domains of treatment. We also hypothesized that engagement in concurrent medication treatment would be enhanced by STAND because STAND targets facilitators of adherence (i.e., oppositional behavior, consistency of daily routine, teen motivation to succeed).29
Aim 3: Service-Delivery Features that Moderate of Effectiveness
If STAND demonstrates reduced effectiveness compared to university trials, identification of service delivery features (i.e., therapist characteristics, treatment setting, whether treatment is combined with medication) that moderate effectiveness can guide refinement of STAND’s community implementation strategy. For example, if clinician years of experience influences outcomes, future implementation efforts might focus on skill development. If indices of therapist autonomy (e.g., achievement of clinical licensure) predict effectiveness, therapist empowerment or motivational strategies might increase engagement in STAND delivery30. Given this study’s culturally diverse context, we also hypothesized that therapist-patient ethnicity match might enhance treatment outcomes—signaling a need to pair adolescents with therapist of similar cultural backgrounds31.
Childhood EBPs for ADHD demonstrate reduced patient engagement when delivered subsequent to ADHD medication32. If the same finding stands in adolescence, STAND might be maximally effective when implemented with unmedicated teens. However, if ADHD medication use is associated with stronger treatment response, combined treatment might be optimal for adolescents in community settings. Additionally, if patient engagement indices are significant treatment moderators, implementation efforts might enhance STAND’s engagement strategies. Finally, if therapy is more effective in office-based (vs. home-based) sessions, future efforts might address barriers to effective home-based care.
Method
All procedures were approved by the Florida International University Institutional Review Board. All parents, therapists, and adolescents signed consent/assent documents prior to participating.
Participants
Adolescents.
Adolescents (N=278; ages 11–17) were incoming patients at four community agencies in a large pan-Latinx and pan-Caribbean U.S. city (see Figure 1). They were required to meet full DSM-5 ADHD criteria (see Supplement 1, available online). Autism spectrum disorder and intellectual disability (IQ<70) were exclusionary. Adolescents were randomly assigned to STAND or UC using a stratified randomization procedure within agency. Randomization occurred after agency and study intake and before initiation of treatment at the agency (see Supplement 1, available online). Table 1 presents sample demographic characteristics. There were no significant group differences on any variable.
Figure 1.
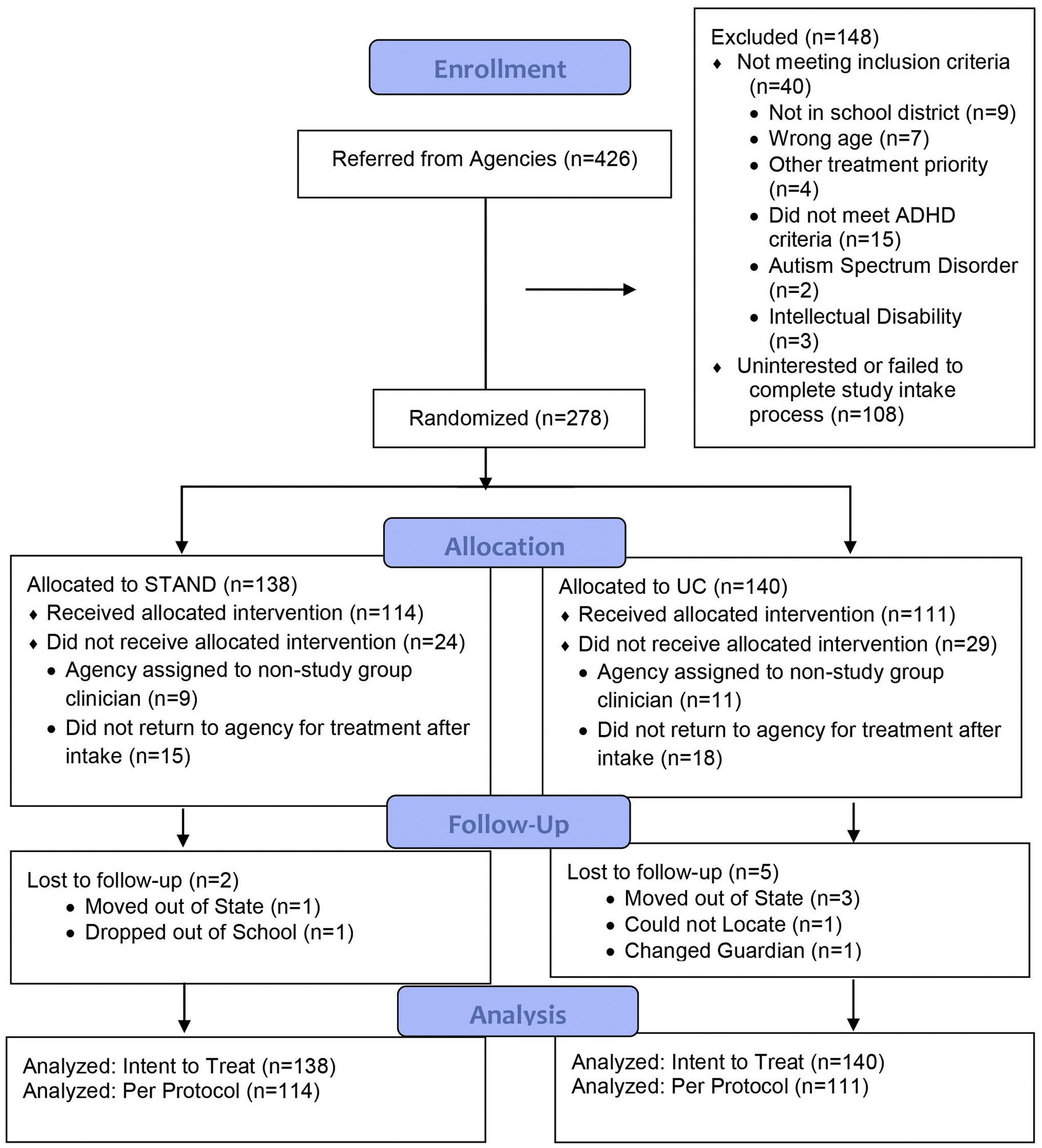
CONSORT Flow Diagram: Adolescent Participants
Table 1.
Baseline Characteristics of Adolescent Sample
| STAND (N = 138) | UC (N = 140) | |
|---|---|---|
| Diagnostic Variables | ||
| WASI estimated Full-Scale IQ M(SD) | 94.15(14.07) | 96.81(13.20) |
| ADHD Presentation | ||
| ADHD-Predominantly Inattentive (%) | 50.0 | 54.3 |
| ADHD-Combined (%) | 50.0 | 45.7 |
| ODD/CD | 50.7 | 47.1 |
| Current ADHD Medication (%) | 31.2 | 23.6 |
| Demographic Variables | ||
| Age M(SD) | 13.97(1.51) | 14.08(1.50) |
| Male Patients (%) | 70.3 | 70.7 |
| Race/Ethnicity (%) | ||
| White Non-Hispanic | 5.1 | 3.6 |
| Black Non-Hispanic | 16.7 | 10.0 |
| Hispanic Any Race | 77.5 | 85.7 |
| Other | 0.7 | 0.7 |
| Single Parent (%) | 35.5 | 36.4 |
| Limited Parent English Proficiency (%) | 36.2 | 46.4 |
| Billing Source (%) | ||
| Medicaid | 57.0 | 55.0 |
| State/County Subsidy | 12.2 | 14.4 |
| Sliding Scale | 29.8 | 28.8 |
| Pro Bono | 0.0 | 1.8 |
| Private Insurance | 0.9 | 0.0 |
| Parent Education Level | ||
| High School Grad or less (%) | 23.9 | 27.3 |
| Part College or Specialized Training (%) | 30.4 | 30.2 |
| College or University Graduate (%) | 33.3 | 33.1 |
| Graduate Professional Training (%) | 12.3 | 9.4 |
Note. ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; M = mean; ODD = oppositional defiant disorder; STAND = Supporting Teens Autonomy Daily; UC = usual care; WASI = Wechsler Abbreviated Scale of Intelligence.
Therapists.
Therapists (N=82) were mental health professionals employed at four agencies. Therapists self-identified as 19.8% non-Hispanic White (n=16), 14.8% Black or African-American (n=12), 64.2% Hispanic (n=53), and 1.2% Other (n=1). 86.6% were female therapists (n=71), with 61.0% (n=50) offering treatment in both Spanish and English. 22.0% of therapists (n=18) were licensed and 86.6% (n=71) held a master’s degree [7.3% held a doctorate (n=6) and 6.1% were bachelor’s level interns (n=5)]. On average, clinicians reported 5.24 years delivering therapy (SD=5.00). STAND (n=44) and UC therapists (n=38) did not differ on any of the background variables noted above.
Procedures
Recruitment and Intake.
At agency intake, agency staff provided study information to parents of 6th-12th grade students with attention, organization, motivation, or behavior problems. Parents signed a permission to contact form and study staff administered an eligibility screen by phone that queried ADHD symptoms, impairment, exclusionary criteria, and treatment priority25. If another presenting problem (e.g., anxiety, substance use) took priority over ADHD, the teen was not eligible. Students with at least four inattention (IN) or hyperactivity/impulsivity (H/I) symptoms according to the screen attended a full diagnostic assessment to evaluate inclusion criteria. The study intake included an IQ screener (Wechsler Abbreviated Scale of Intelligence-2nd Edition)33 and parent-administered Diagnostic Interview Schedule for Children (DISC)34.
Therapist Recruitment.
Detailed information about therapist recruitment can be found in Supplement 1, available online. All therapists were randomly assigned to STAND or UC at baseline.
Intervention Content.
STAND is a manualized engagement-focused psychosocial treatment for adolescent ADHD. STAND consists of 10 weekly 60-minute sessions attended by the adolescent and parent16. Skill instruction is blended with MI and guided parent-teen behavioral contracting17. Treatment targets family, behavioral, and academic impairment. Treatment is modular to promote flexibility and treatment tailoring. In the engagement phase, MI increases awareness of personal values and goals, identifies strengths, and recognizes ways to achieve personal goals and act consistently with values. The skills phase teaches parent-teen communication, parent behavioral strategies, and organization, time management and planning skills applied to homework, school, and chores. Planning sessions teach families to integrate skills into a daily routine, transfer new habits to school settings, and build a final parent-teen contract. MI in the final session promotes maintenance of change.
Therapist Procedures.
Therapy was delivered across three years. Duration of treatment varied naturalistically to avoid builtin between-group dose differences. Participating therapists treated an average of 2.74 study participants (range: 0 to 14). Study interventions were provided by agency employees using typical billing procedures. Therapists randomized to STAND were offered a three-day training and 30-minutes of weekly supervision while treating study participants. Every 12 months, a four-hour booster training was provided. STAND therapists were provided with a treatment manual and a family workbook for each participant. Therapists in both groups were instructed to utilize usual care procedures for termination, allowing STAND therapists to continue treatment after completing STAND manualized content. UC therapists were instructed to treat study participants using usual procedures in the agency and the treatments they believed would be most effective for the youth. They received weekly supervision for study participants from agency supervisors according to typical agency practices. UC therapists were offered STAND training at study conclusion.
Treatment Differentiation.
Therapists in both groups were asked to provide sample audio-recorded sessions for each participant (available for 70.2% of treated sample). Fidelity data for STAND are reported in detail elsewhere17. Coding of 78 available UC audio tapes using STAND fidelity checklists indicated high treatment differentiation (53.8% of items were not present on any UC recordings). Seven items were present on greater than 5% of recordings and typically represented non-specific therapy activities: discussion of presenting problems (43.8%), cognitive behavioral strategies for emotion regulation (8.2%), reviewing therapy homework (8.2%), reviewing progress on goals (5.5%), instruction in daily planner utilization (9.6%), instruction in time management skills (6.8%), and recognizing positive client changes (5.5%).
Data Collection.
Participants were permitted to utilize naturalistic stimulant medication during the study; all medications were monitored and controlled for in analyses. Because therapy duration was allowed to vary naturalistically, PT assessments were scheduled for 16 weeks after the participant’s first session at the agency, which provided ample time for families to complete the 10 session STAND protocol with assumed cancellations. On average, PT assessments occurred 5.11 months after BL (SD=2.26). FU assessments were attempted at approximately 12 weeks after PT. On average, FU assessments occurred approximately 4.70 months after PT (SD=2.50). Retention was 99.3% (n=276) at PT and 97.5% (n=271) at FU (data provided by at least one informant). Academic records and teacher ratings were obtained directly from schools. Electronic health records were accessed directly. Parent ratings were available in Spanish or English. Teachers and therapists received $20 and families received $100 for each assessment.
Primary Outcome Measures
ADHD Symptoms.
Parent and teacher reports of IN and HI symptom severity were measured on the Conners 3 Parent Short Form Rating Scale (C3RS)35 and parent and teacher DSM-5 ADHD checklist36. Respondents rated symptoms on both scales as 0 (not at all) to 3 (very much). Symptom severity scale scores was the mean level (0–3) of subscale items. For the C3RS, scale scores were converted into T-scores based on age and gender for IN (five items) and HI (six items). The DSM-5 checklist contains nine items per subscale that correspond with DSM-5 items. Psychometric properties of both measures are very good, with empirical support for an internally consistent subscales36–37. In this sample, ADHD subscale alphas ranged from .86-.92.
Academic Impairment.
Two indices of academic impairment were Grade Point Average (GPA) and parent report of academic organization, time management, and planning (OTP) problems. Report cards were obtained directly from the school district. GPA for each academic quarter was calculated by converting class grades (e.g., English, Math) to a 5-point scale (i.e., 4.0=A to 0.0=F). At each assessment, GPA was calculated for the immediately preceding academic quarter. The 24-item parent Adolescent Academic Problems Checklist (AAPC) measures observable secondary-school specific OTP problems and is validated in samples of adolescents with ADHD38. The AAPC possesses two distinct factors and a total score, with strong internal reliability and concurrent validity38. In this study, total score was used (alpha=.91).
Family Impairment.
For family impairment, the parent and adolescent versions of the Conflict Behavior Questionnaire-20 (CBQ-20) assessed parent-teen conflict39. Informants rated statements about the parent-teen relationship on a five-point scale from 1-strongly agree to 5-strongly disagree. In this study, alpha ranged from .92 to .93.
Disciplinary Incidents.
The school district provided records of student disciplinary incidents. Counts of all disciplinary incidents (e.g., detention, in-school suspension) were calculated for the academic quarter immediately preceding each assessment.
Measures of Treatment Engagement
Psychosocial Treatment Engagement.
Electronic health records at each agency were accessed for all participants for a 12-month period beginning with the baseline assessment. Information was collected about the dates and durations of all therapy sessions (including STAND sessions), who attended, who provided therapy, dates of cancellations, and the location that treatment was provided. Parent treatment participation was calculated by dividing the total number of sessions the parent attended by the total of number of sessions the youth received.
Stakeholder Satisfaction.
At PT, parents and adolescents completed 20-item treatment utility scales designed to measure stakeholder satisfaction (i.e., perceptions of how ADHD treatment was helpful)16. Parents and adolescents indicated level of agreement with statements on a 5-point scale (1=strongly disagree to 5=strongly agree). As in previous trials, items were analyzed individually to identify stakeholder perspectives of specific treatment features that differentiated STAND from active control16. In the current trial, alpha for the parent and youth scales were excellent (alpha=.95-.97).
Medication Utilization.
ADHD medication use (stimulant or non-stimulant) was naturalistic. At each assessment, parents and teens completed a medication interview used extensively in past trials of adolescent ADHD treatment40. Respondents indicated current medications received, doses, administration schedules, settings taken, changes made since the last assessment, reasons for changes, and information about frequency of medication visits. Data were screened for discordant parent-teen reports, which were resolved by discussion. Based on these combined reports, current medication utilization was coded for each time point.
Measurement of Moderators
Service Delivery Moderators.
Receipt of combined treatment, number of sessions received, therapist ethnicity match, therapist years of experience, therapist licensure, percentage of office-based sessions, and percentage of sessions attended by a parent were moderators. Medication status was derived from the medication interview; number of sessions received over twelve months, percentage office-based sessions, and percentage of sessions attended by parent were collected from the electronic health record. Therapists provided information about their ethnicity, years of experience, and licensure status at BL.
Analytic Plan
Initially planned sample size was 300 with 15% attrition (i.e., N=255); however, at the end of the three-year planned recruitment period, power analyses were conducted for the sample size to date (N=278) with true, rather than estimated, design effects. The originally estimated design effects due to clustering between were between 1.3 and 1.6; however, true design effects were between 1.1 and 1.3, based on Intraclass Correlation (ICC) values at BL and PT for primary outcomes. Based on these new estimates of design effect, 202 participants achieved 80% power for expected effects (d=.3 to .4). The variable with the most missing data possessed 239 participants at FU (14% attrition). All participants possessed complete baseline data.. ICC and design effects for adolescent-level outcomes revealed that all design effects were < 2. As a result, we elected not to include clustering in the analysis based on the recommendation of Muthen and Satorra41. A false-discovery rate correction was applied within outcome domain for all analyses42.
Primary Outcomes
Linear mixed models (LMMs) with random intercepts were conducted in SPSS 25. We first conducted intent to treat analyses including all randomized participants (N=278). Separate Linear Mixed Models were conducted for each outcome. In LMMs, dummy codes were specified for group (UC=0, STAND=1). To model agency-specific effects, we included three dummy codes with agency 1 (largest) serving as the reference group. We tested various time curves and found linear time to possess the best fit. Time was coded as a continuous, subject-specific measure reflecting months since BL (BL time=0). Data were assumed missing at random (MAR)43. A full information robust Maximum Likelihood estimator was employed. For each outcome, the following specifications were evaluated. The linear effects of time and group × time were the effects of interest to test aim 1 hypotheses.
We then conducted per protocol (PP) analyses that included only participants who initiated treatment (n=225). This supplemental analysis isolates the upper limit on true effects of STAND in community settings, given that ITT effects may be deflated by randomized participants who never engaged in services after agency intake44. Compared to those who initiated treatment, those who did not (n=53) did not differ on demographic or clinical variables listed in Table 1.
Treatment Engagement
Linear regression tested group differences on cross-sectional continuous outcomes and logistic regression tested group differences on cross-sectional categorical outcomes. A generalized estimating equation using a binomial probability distribution, logit link function, and maximum likelihood estimator was used to test group differences on categorical longitudinal outcomes (medication use). Cohen’s d effect size was calculated for continuous outcomes and relative risk odds ratios were calculated for categorical outcomes.
Service Delivery Moderators
Per protocol LMMs tested service delivery moderators (non-initiators had no values for these variables). For moderator analyses, the list of outcomes was trimmed to include one variable from each of the four domains. Three-way interactions of moderator × group × time indicated whether the group’s effect on outcome over time varied by the moderator level. False discovery rate corrections were applied within domain.
Results
Primary Outcomes: Intent to Treat (ITT) Analyses
Results (see Table 2) indicated no group × time difference on any outcome. The full sample demonstrated significant improvements over time on all IN, HI, and academic impairment measures.
Table 2.
Intent to Treat (ITT) Analyses: Results From Linear Mixed Models
| ITT STAND (N=138) | ITT UC (N=140) | ITT Time | ITT Group × Time | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BL M (SD) | PT M (SD) | FU M (SD) | d | BL M (SD) | PT M (SD) | FU M (SD) | d | b (SE) | p | 95% CI | b (SE) | p | da | 95% CI | |
| Inattention | |||||||||||||||
| Parent C3RS | 75.51(13.32) | 69.54(13.54) | 66.54(14.67) | .52 | 73.74(12.66) | 69.02(13.15) | 64.68(13.84) | .72 | −.92(.11) | <.001 | −1.15 to −.70 | .21(. 16) | .171 | −.16 | −.09 to .52 |
| Parent DSM | 1.92(.69) | 1.69(.70) | 1.44(.65) | .70 | 2.00(.66) | 1.70(.67) | 1.42(.74) | .89 | −.06(.01) | <.001 | .00 to .03 | .01(.01) | .162 | −.16 | .00 to .03 |
| Teacher DSM | 1.84(.66) | 1.66(.76) | 1.49(.83) | .53 | 1.63(.65) | 1.48(.80) | 1.33(.80) | .47 | −.03(.01) | <.001 | −.05 to −.02 | .00(.01) | .634 | .07 | −.03 to .02 |
| H/I | |||||||||||||||
| Parent C3RS | 65.37(17.19) | 62.44(15.82) | 59.74(16.71) | .33 | 63.02(16.71) | 60.99(14.75) | 59.12(15.33) | .23 | −.40(.11) | <.001 | −.61 to −.19 | .18(.15) | .236 | .10 | −.46 to .11 |
| Parent DSM | 1.02(.79) | .86(.71) | .71(.69) | .39 | 1.06(.78) | .94(.73) | .83(.78) | .30 | −.02(.00) | <.001 | −.03 to −.01 | .01(.01) | .272 | .09 | −.02 to .01 |
| Teacher DSM | .99(.87) | .78(.70) | .56(.70) | .50 | .90(.81) | .69(.73) | .50(.72) | .50 | −.04(.01) | <.001 | −.06 to −.03 | .00(.01) | .801 | −.03 | −.02 to .02 |
| Academic Impairment | |||||||||||||||
| School | 1.60(.84) | 1.71(.80) | 1.80(.91) | .24 | 1.83(.75) | 1.93(.82) | 2.02(.78) | .26 | .02(.01) | .002 | .01 to .03 | .00(.01) | .904 | −.01 | −.02 to .02 |
| Parent | 1.53(.56) | 1.36(.53) | 1.21(.53) | .57 | 1.52(.50) | 1.34(.53) | 1.16(.55) | .72 | −.04(.00) | <.001 | −.05 to −.03 | .00(.01) | .466 | −.08 | −.01 to .02 |
| Family Impairment | |||||||||||||||
| Parent | 2.95(.78) | 2.85(.80) | 2.75(.84) | .26 | 2.85(.78) | 2.82(.81) | 2.79(.82) | .08 | −.01(.01) | .286 | −.02 to .01 | .01(.01) | .082 | .18 | −.03 to .00 |
| Adolescent | 2.42(.69) | 2.46(.78) | 2.50(.76) | −.10 | 2.32(.75) | 2.31(.67) | 2.31(.74) | .01 | .00(.01) | .869 | −.01 to .01 | .01(.01) | .258 | −.11 | −.01 to .02 |
| Disciplinary Incidents | 6.21(15.62) | 4.89(9.90) | 3.66(8.04) | .16 | 3.03(5.03) | 2.78(6.40) | 2.55(4.53) | −.10 | −.05(.08) | .549 | −.21 to .11 | .21(.11) | .063 | .20 | −.43 to .01 |
Note. Means are marginal estimates controlling for agency. Cohen’s d within groups is difference between baseline (BL) and follow-up (FU) divided by baseline pooled standard deviation. Boldface type indicates significant p values. alpha=05. C3RS = Conners 3 Rating Scale; H/I = Hyperactivity/Impulsivity; PT = post-treatment.
difference between group change scores divided by baseline pooled standard deviation.
Primary Outcomes: Per Protocol Analyses
The full sample demonstrated significant improvement over time on all IN, HI, and academic impairment measures (see Table S1, available online). Group × time effects were significant for parent-rated DSM-5 IN, such that UC showed greater decreases in IN from BL to FU than STAND (b=.02, SE=.01, p=.009, d=.37, 95% CI: .01 to .04). Results indicate that null findings in ITT analyses were not solely accounted for by participants who did not initiate treatment.
Treatment Engagement
There were no group differences in treatment initiation after agency intake (STAND=82.6%, UC=79.3%; b=−.22, SE=.31, p=.481, OR=.81) or number of sessions that initiating participants received over 12 months [STAND M=13.99, SD=13.80, UC M=17.38, SD=15.26; F(1,223)=3.43, p=.065, d=−.23]. Among initiating participants, parents of STAND participants attended a greater percentage of sessions than UC parents [STAND M=74.2%, SD=32.0%, UC M=45.7%, SD=32.8%; F(1, 223)=43.72, p<.001, d=.88]. There were no group differences in cancellations (p=.296).
After applying false discovery rate corrections (see Table S2, available online), parents who received STAND had greater satisfaction than UC parents in 3 of 20 domains: (1) receiving new parenting techniques as a result of treatment (p<.001, d=.53), (2) gaining greater awareness of how their habits influence the adolescent’s behavior (p=.001, d=.47), and (3) learning valuable lessons from practicing skills at home (p=.006, d=.39). There were no group differences in adolescent satisfaction (see Table S3, available online).
For medication utilization, both the linear (b=.20, SE=.05, p=.002, 95% CI: .08 to .33) and quadratic (b=−.02, SE=.01, p=.001, 95% CI: −.03 to −.01) group × time effects were significant. Results (see Figure 3) indicated that participants in STAND were significantly more likely to utilize medication over time compared to UC. At BL, the odds of using medication in the STAND group were 1.43 times the odds of using medication in the UC group; this effect grew to 3.99 at PT and 10.27 at FU. Compared to the BL odds ratio, the FU between-group odds ratio is 7.18 times larger. Between BL and PT, 13.0% of STAND participants (n=18) either started medication for the first time (n=8) or resumed (n=10) a pre-BL prescription (UC=5.0%; n=7 new prescriptions, n=0 resumptions) and 26.1% of STAND group (n=36) sustained an ongoing prescription (UC=17.9%; n=25). Between PT and FU, an additional 3.8% of STAND participants (n=5) started (n=1) or resumed (n=4) a prescription (UC=6.7%; n=4 new prescriptions; n=5 resumptions) and 30.3% (n=42) sustained an ongoing prescription (UC=7.8%; n=11).
Figure 3.
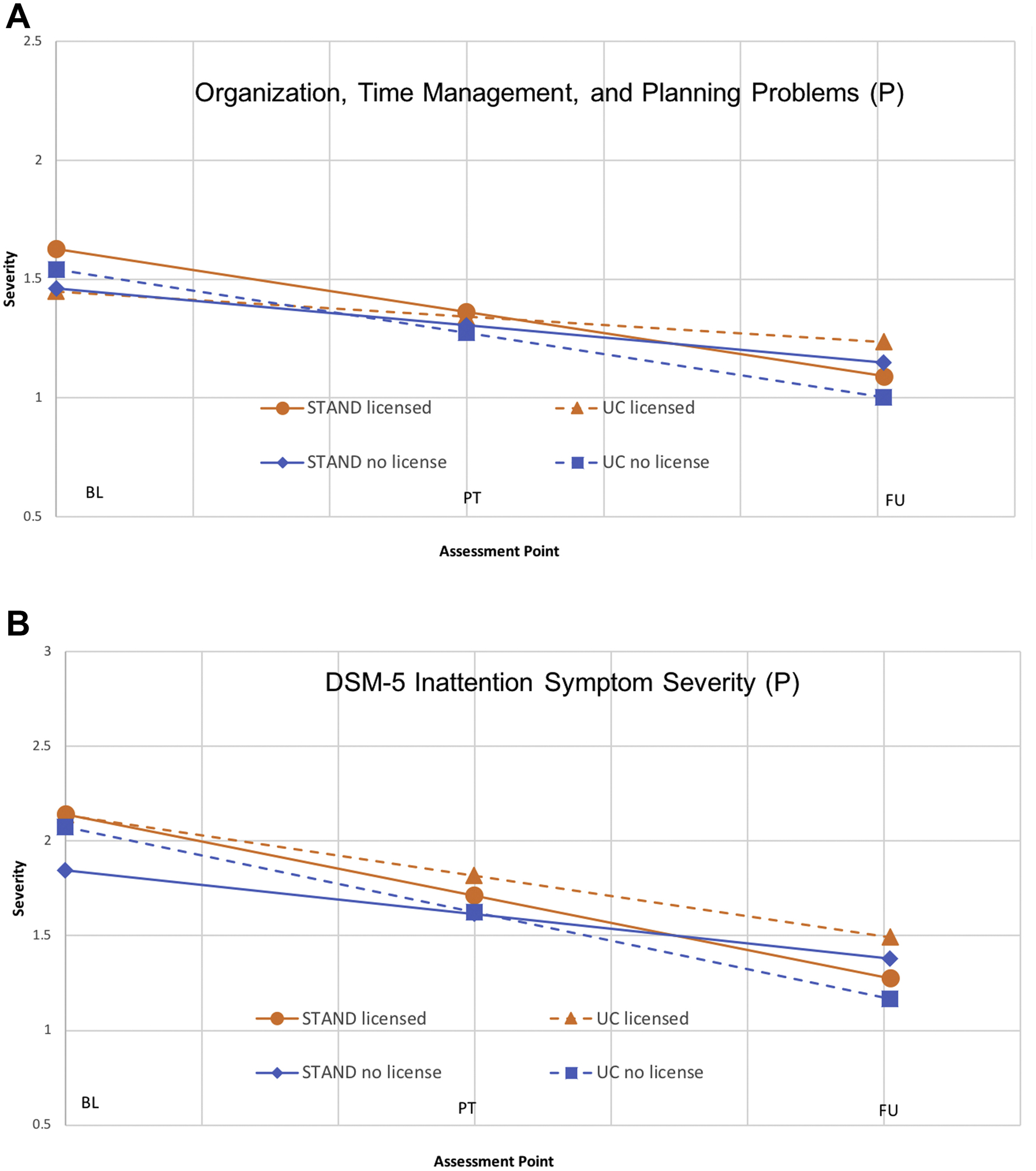
The Effect of Licensure Status and Group on Effectiveness in Community Clinics
Note. Post-treatment (PT) and follow-up (FU) represent mean functioning for each group at the mean number of months since baseline (BL) that PT and FU assessments occurred. STAND = Supporting Teens’ Autonomy Daily; UC = Usual Care.
Service Delivery Moderators
See Table S4, available online. Significant three-way interactions (see Figure 3) indicated that STAND (vs. UC) led to greater reductions in parent-rated IN over time (b=.04, SE=.01, p<.001, 95% CI: .02 to .06) and parent-rated academic problems over time (b=.02, SE=.01, p=.017. 95% CI: .00 to .03) when the therapist was licensed. The standardized difference scores for these three-way interactions (time × group × licensure) was d=1.08 for IN and d=1.13 for academic problems, indicating large differences in the impact of group over time for therapists who are licensed vs. unlicensed. Group × Time × Moderator and Time × Moderator effects were non-significant for medication status, number of sessions received, billing source, therapist ethnicity match, therapist years of experience, percentage of office-based sessions, and percentage of sessions attended by a parent.
Discussion
Study findings were as follows. First, there were no significant group × time effects in ITT analyses and PP demonstrated a significant group × time on one of eleven outcomes (indicating that UC outperformed STAND on parent-rated DSM-5 IN; d=.37). Thus, overall, community-based STAND did not outperform UC on any primary outcome. Second, significant improvements in ADHD symptom severity and academic impairment were demonstrated for both STAND (d=.33 to .70) and UC (d=.23 to 89); however, these within-group effect sizes were notably lower than those reported for similar indices in university trials of STAND (d=.71–1.93)15,16. Despite reduced effectiveness in the community setting, STAND outperformed UC on some indices of treatment engagement (i.e., parent participation in session, parent satisfaction indices, concurrent medication engagement). In addition, STAND outperformed UC on primary outcomes when therapists were licensed (22% of therapists), but not when they were unlicensed (78% of therapists).
Regarding clinical outcomes, both groups demonstrated average parent-rated IN symptoms within the C3RS35 “Very Elevated” range at BL and “Elevated” range by FU. Parent-rated C3RS HI symptom averages were in the “Elevated” range at BL and “High Average” range at FU. Parent and teacher ratings of DSM-5 ADHD symptom were of similar magnitudes. Given the chronicity of ADHD, full remission of symptoms after discontinuation of ADHD treatment is not expected.45 However, unlike in past trials of STAND, symptoms remained in the clinical (rather than subclinical) range15,16. Similarly, average school grades in this trial improved from a D to a C- average, which indicates continued impairment following treatment for both groups. No improvements in family impairment of disciplinary incidents were present.
Among adolescents who attended at least one therapy session, retention in agency services was strong in both groups. Compared to UC, STAND parents showed greater participation in treatment (d=.88) and higher levels of satisfaction with the impact of treatment on their parenting (d=.39-.53). STAND also outperformed UC on concurrent medication engagement, including both sustainment of ongoing medication, resuming stopped medication, and initiating new medication. This finding is not surprising because several STAND elements are known to improve medication utilization in other populations (i.e., psychoeducation, MI, goal-setting, increasing self-awareness, and parent-teen behavioral contracting)46. However, despite these promising effects, treatment engagement in the STAND group was lower than in university trials15–16 did not lead to superior outcomes than UC at approximately 10 months post-treatment (see Table 2).
STAND was more effective when delivered by licensed (versus unlicensed) therapists, suggesting that therapist engagement may be an important target. In this trial, therapist licensure was unrelated competence or fidelity17; however, literature review suggests that licensed therapists demonstrate higher levels of autonomy and self-efficacy than unlicensed therapists30. Perhaps therapist engagement and empowerment efforts may improve STAND implementation beyond basic fidelity metrics. Because the majority of community therapists are unlicensed, these initiatives may have a meaningful effect on outcomes47. Future work should identify strategies to increase therapist engagement within the constraints of community clinics.
There were no significant moderation or prediction effects for patient attendance, concurrent medication use, therapist ethnicity match, therapist years of experience, or setting of treatment, indicating that these factors did not influence treatment effectiveness (see Table S1, available online). The null attendance finding is common48–49 when youth characteristics that dampen treatment outcomes (i.e., adolescent symptom severity) also increase motivation to engage in treatment. Our results also fail to replicate Pelham and colleagues’ finding that receiving medication prior to psychosocial treatment reduces treatment response in younger children32. Similar to university trials, community-based STAND was equally effective when delivered as monotherapy or adjunctive to medication—despite improved medication use in the STAND group14. Future analyses are planned to examine the extent to which STAND’s effectiveness was impacted by reduced implementation outcomes (i.e., therapist knowledge and competence, fidelity and MI integrity, parent use of behavioral strategies during treatment, pace of delivery). These analyses will further guide a refined community-based implementation strategy.
Therapist participation in the study was voluntary; thus, we may have oversampled therapists with openness to new interventions. Given the nature of the treatment, it was not possible to mask therapists and participants to study group, though they were masked to study hypotheses (teachers and coders were masked). Therapist to client ratio was low in this trial (i.e., 1:2.74) due to high turnover in community contexts and fine-grained patient-therapist matching that required consideration of agency, parent language, therapist catchment area, and insurance type. As a result, we did not cluster within therapist in analyses (though we covaried for agency). We did not assess the number of potential participants (therapist or adolescent) who were present at agencies but elected not to enroll in the trial. We did not assess psychological service utilization outside of the agencies. It is not clear which therapies were administered in UC; future work is needed to develop measures that can detect common UC practices for adolescent ADHD.
In sum, STAND implemented by community practitioners demonstrated overall effectiveness that was no different than UC, despite improving some aspects of therapeutic engagement. Only licensed community therapists delivered STAND in a manner that outperformed standard services. Additional work with this sample will pursue a revised implementation strategy by: (1) investigating relationships between implementation outcomes and patient outcomes and (2) querying stakeholder perspectives (e.g., therapists, supervisors, agency leadership, parents, adolescents) about barriers and facilitators to community-based STAND implementation. Future iterations of community-based treatment for adolescent ADHD will address key barriers directed during the course of this trial.
Supplementary Material
Figure 2.
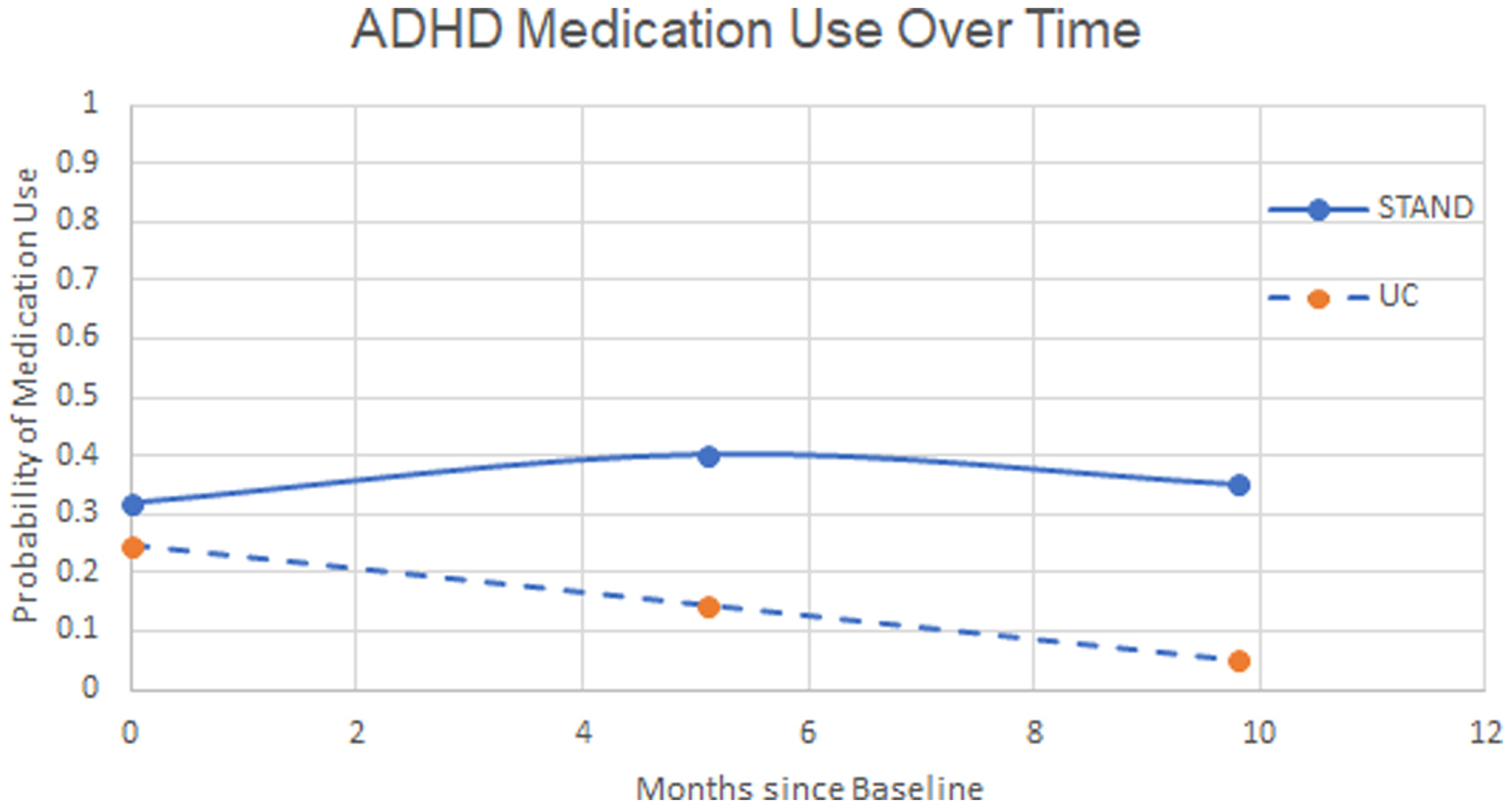
Attention-Deficit/Hyperactivity Disorder (ADHD) Medication Use over Time
Note. Figure represents marginal probabilities derived from the generalized estimating equation.
Acknowledgments
This trial was funded by the National Institute of Mental Health (R01 MH106587).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure:
Dr. Sibley has received royalties from Guilford Press for the treatment manual described in this paper. She has received royalties from Vimeo, Inc. for STAND training videos and has provided consultation to Takeda Pharmaceuticals. Drs. Graziano, Coxe, Bickman and Mr. Martin have reported no biomedical financial interests or potential conflicts of interest.
References
- 1.Wolraich ML, Hagan JF, Allan C, et al. Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. Pediatrics. 2019;144(4):e20192528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pliszka S, AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(7):894–921. [DOI] [PubMed] [Google Scholar]
- 3.DuPaul GJ, Chronis-Tuscano A, Danielson ML, e al. Predictors of receipt of school services in a national sample of youth with ADHD. Journal of attention disorders. 2019;23(11):1303–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bussing R, Zima BT, Mason DM, et al. Receiving treatment for attention-deficit hyperactivity disorder: do the perspectives of adolescents matter?. Journal of Adolescent Health. 2011;49(1):7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Danielson ML, Bitsko RH, Ghandour RM, et al. Prevalence of parent-reported ADHD diagnosis and associated treatment among US children and adolescents, 2016. Journal of Clinical Child & Adolescent Psychology. 2018;47(2):199–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brinkman WB, Simon JO, Epstein JN. Reasons why children and adolescents with attention-deficit/hyperactivity disorder stop and restart taking medicine. Academic pediatrics. 2018;18(3):273–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Molina BS, Hinshaw SP, Swanson JM, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(5):484–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan E, Fogler JM, Hammerness PG. Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. Jama. 2016;315(18):1997–2008. [DOI] [PubMed] [Google Scholar]
- 9.Sibley MH, Kuriyan AB, Evans SW, Waxmonsky JG, Smith BH. Pharmacological and psychosocial treatments for adolescents with ADHD: An updated systematic review of the literature. Clinical psychology review. 2014;34(3):218–32. [DOI] [PubMed] [Google Scholar]
- 10.Jensen PS, Garcia JA, Glied S, et al. Cost-effectiveness of ADHD treatments: findings from the multimodal treatment study of children with ADHD. American Journal of Psychiatry. 2005;162(9):1628–36. [DOI] [PubMed] [Google Scholar]
- 11.Roundfield KD, Lang JM. Costs to community mental health agencies to sustain an evidence-based practice. Psychiatric services. 2017. Sep 1;68(9):876–82. [DOI] [PubMed] [Google Scholar]
- 12.Epstein JN, Kelleher KJ, Baum R, et al. , Variability in ADHD care in community-based pediatrics. Pediatrics. 2014;134(6):1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sibley MH, Pelham WE, Derefinko KJ, Kuriyan AB, Sanchez F, Graziano PA. A pilot trial of Supporting Teens’ Academic Needs Daily (STAND): A parent-adolescent collaborative intervention for ADHD. Journal of Psychopathology and Behavioral Assessment. 2013;35(4):436–49. [Google Scholar]
- 15.Sibley MH, Graziano PA, Kuriyan AB, et al. Parent–teen behavior therapy+ motivational interviewing for adolescents with ADHD. Journal of consulting and clinical psychology. 2016;84(8):699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sibley MH, Rodriguez L, Coxe S, Page T, Espinal K. Parent–Teen Group versus Dyadic Treatment for Adolescent ADHD: What Works for Whom?. Journal of Clinical Child & Adolescent Psychology. 2019. April 18:1–7. [DOI] [PubMed] [Google Scholar]
- 17.Sibley MH, Graziano PA, Bickman L, Coxe SJ, Martin P, Rodriguez LM, Fallah N, Ortiz M. Implementing Parent-Teen Motivational Interviewing+ Behavior Therapy for ADHD in Community Mental Health. Prevention Science. 2020; 26:1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sibley MH. Parent-teen therapy for executive function deficits and ADHD: Building skills and motivation. Guilford Publications; 2016. [Google Scholar]
- 19.Sprich SE, Safren SA, Finkelstein D, et al. A randomized controlled trial of cognitive behavioral therapy for ADHD in medication-treated adolescents. Journal of Child Psychology and Psychiatry. 2016;57(11):1218–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barkley RA, Edwards G, Laneri M, et al. The efficacy of problem-solving communication training alone, behavior management training alone, and their combination for parent–adolescent conflict in teenagers with ADHD and ODD. Journal of consulting and clinical psychology. 2001;69(6):926. [PubMed] [Google Scholar]
- 21.Miller WR, Rollnick S. Motivational interviewing: Helping people change. Guilford press; 2013. [Google Scholar]
- 22.Chorpita BF, Daleiden EL, Park AL, et al. Child STEPs in California: A cluster randomized effectiveness trial comparing modular treatment with community implemented treatment for youth with anxiety, depression, conduct problems, or traumatic stress. Journal of consulting and clinical psychology. 2017;85(1):13. [DOI] [PubMed] [Google Scholar]
- 23.Sibley MH, LaCount PA. Enhancing engagement and motivation with adolescents and parents. In Allen Hawes, and Essau (Eds.) Family-Based Intervention for Child and Adolescent Mental Health: A Core Competencies Approach. Cambridge University Press; 2021. [Google Scholar]
- 24.Southam-Gerow MA, Weisz JR, Chu BC, et al. Does cognitive behavioral therapy for youth anxiety outperform usual care in community clinics? An initial effectiveness test. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):1043–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weisz JR, Southam-Gerow MA, Gordis EB, et al. Cognitive–behavioral therapy versus usual clinical care for youth depression: An initial test of transportability to community clinics and clinicians. Journal of Consulting and Clinical Psychology. 2009;77(3):383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith JD, Stormshak EA, Kavanagh K. Results of a pragmatic effectiveness–implementation hybrid trial of the Family Check-Up in community mental health agencies. Administration and Policy in Mental Health and Mental Health Services Research. 2015;42(3):265–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garland AF, Haine-Schlagel R, Brookman-Frazee L, et al. Improving community-based mental health care for children: Translating knowledge into action. Administration and Policy in Mental Health and Mental Health Services Research. 2013. January 1;40(1):6–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoagwood K, Kolko DJ. Introduction to the special section on practice contexts: A glimpse into the nether world of public mental health services for children and families. Administration and Policy in Mental Health and Mental Health Services Research. 2009;36(1):35–36. [DOI] [PubMed] [Google Scholar]
- 29.Gau SS, Shen HY, Chou MC, et al. Determinants of adherence to methylphenidate and the impact of poor adherence on maternal and family measures. Journal of Child & Adolescent Psychopharmacology. 2006;16(3):286–97. [DOI] [PubMed] [Google Scholar]
- 30.Daniels LG. The relationship between counselor licensure and aspects of empowerment. Journal of Mental Health Counseling. 2002. July 1;24(3):213–24. [Google Scholar]
- 31.Halliday-Boykins CA, Schoenwald SK, Letourneau EJ. Caregiver-therapist ethnic similarity predicts youth outcomes from an empirically based treatment. Journal of Consulting and Clinical Psychology. 2005. October;73(5):808. [DOI] [PubMed] [Google Scholar]
- 32.Pelham WE Jr, Fabiano GA, Waxmonsky JG, et al. Treatment sequencing for childhood ADHD: A multiple-randomization study of adaptive medication and behavioral interventions. Journ Clin Child & Adol Psycholo. 2016;45(4):396–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wechsler D WASI-II: Wechsler abbreviated scale of intelligence. PsychCorp; 2011. [Google Scholar]
- 34.Shaffer D, Fisher P, Dulcan MK, et al. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA study. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(7):865–77. [DOI] [PubMed] [Google Scholar]
- 35.Conners CK. Conners third edition (Conners 3). Los Angeles, CA: Western Psychological Services. 2008. [Google Scholar]
- 36.Sibley MH, Kuriyan AB. DSM-5 changes enhance parent identification of symptoms in adolescents with ADHD. Psychiatry research. 2016;242:180–5. [DOI] [PubMed] [Google Scholar]
- 37.Sibley MH, Yeguez CE. The impact of DSM-5 A-criteria changes on parent ratings of ADHD in adolescents. Journal of attention disorders. 2018;22(1):83–91. [DOI] [PubMed] [Google Scholar]
- 38.Sibley MH, Altszuler AR, Morrow AS, et al. Mapping the academic problem behaviors of adolescents with ADHD. School Psychology Quarterly. 2014;29(4):422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Robin AL, Foster SL. Negotiating parent-adolescent conflict: A behavioral-family systems approach. Guilford Press; 2002. [Google Scholar]
- 40.Kuriyan AB, Pelham WE Jr, Molina BS, et al. Concordance between parent and physician medication histories for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Child and Adol Psychopharm. 2014;24(5):269–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muthen BO, Satorra A. Complex sample data in structural equation modeling. Sociological methodology. 1995; 267–316. [Google Scholar]
- 42.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal statistical society: series B (Methodological). 1995;57(1):289–300. [Google Scholar]
- 43.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological methods. 2002;7(2):147. [PubMed] [Google Scholar]
- 44.Hernán MA, Hernández-Díaz S Beyond the intention-to-treat in comparative effectiveness research. Clinical Trials. 2012; 9(1): 48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jensen PS, Arnold LE, Swanson JM, Vitiello B, Abikoff HB, Greenhill LL et al. 3-year follow-up of the NIMH MTA study. Journal of the American Academy of Child & Adolescent Psychiatry, 2007; 46(8): 989–1002. [DOI] [PubMed] [Google Scholar]
- 46.Rapoff MA. Adherence to pediatric medical regimens. Springer Science & Business Media; 2009. October 3. [Google Scholar]
- 47.Schoenwald SK, Chapman JE, Kelleher K, et al. Research Network on Youth Mental Health. A survey of the infrastructure for children’s mental health services: Implications for the implementation of empirically supported treatments (ESTs). Administration and Policy in Mental Health and Mental Health Services Research. 2008;35(1–2):84–97. [DOI] [PubMed] [Google Scholar]
- 48.Langberg JM, Evans SW, Schultz BK, Becker SP, Altaye M, Girio-Herrera E. Trajectories and predictors of response to the Challenging Horizons Program for adolescents with ADHD. Behavior Therapy. 2016;47(3):339–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nix RL, Bierman KL, McMahon RJ. How attendance and quality of participation affect treatment response to parent management training. Journal of consulting and clinical psychology. 2009;77(3):429. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


