Abstract
Educational disparities in health and mortality are well-documented and evidence suggests that they may be widening. Yet, there is much unknown about when educational disparities begin to emerge and for whom. This paper investigates the association between educational attainment and cardiometabolic health in young adults with critical attention paid to differences across racial/ethnic and sex subgroups. We focus on cardiometabolic health in young adulthood as it is particularly relevant for understanding current population health trends. We used data from the National Longitudinal Study of Adolescent to Adult Health (Add Health) when participants were aged 12–19 years (Wave I) and aged 24–32 years (Wave IV). Using a series of logistic regression models, we first estimated the association between education and five markers of cardiometabolic health (high-risk blood pressure, high-risk waist circumference, diabetes/pre-diabetes, hyperlipidemia, and high-risk inflammation). We then examined the extent to which this association was explained by adolescent health and both adolescent and young adult socioeconomic status (SES) (including parental education, participant educational attainment, household income, and employment status). Finally, we investigated whether the association between educational attainment and cardiometabolic health differed by race/ethnicity and sex. We found evidence of an association between educational attainment and cardiometabolic health that persisted net of adolescent health, adolescent SES, and young adult SES. We also found some evidence of modest differences in this association by race/ethnicity and sex. Our findings suggest that even as early as young adulthood there are disparities in cardiometabolic health by educational attainment, which may lead to even larger disparities in late life health.
Keywords: Education, Cardiometabolic health, Young adult health, Biomarker-measured health
Highlights
-
•
Educational gradients in cardiometabolic health differ according to the cardiometabolic risk indicator investigated.
-
•
Educational disparities in cardiometabolic health persist even aafter adjustment for early life health and parental SES.
-
•
The association between education and cardiometabolic health differs in modest ways by sex and race/ethnicity.
1. Introduction
There is a large body of literature examining the association between educational attainment and adult health in the U.S. Recently, the focus of these studies has shifted to understanding the contextual dependency of the education-health relationship (Montez & Friedman, 2015). Indeed, several recent studies have demonstrated that the education-health association differs in strength and even existence by cohort, across geographic contexts, and across social groups (Hayward, Hummer, & Sasson, 2015; Masters, Link, & Phelan, 2015; Montez & Friedman, 2015; Smith, Anderson, Salinas, Horvatek, & Baker, 2015). For example, Masters et al. (2015) showed that educational attainment disparities in preventable causes of death (i.e., heart disease, etc.) in the United States were larger in younger cohorts than in older cohorts, and different by race/ethnicity and gender.
Despite a growing understanding of the nuances of the education-health relationship, critical questions remain. In the United States, in particular, educational attainment disparities in adult health and mortality rates may be as wide as they have ever been (Hummer & Hamilton, 2019). Thus, it is imperative to understand when educational disparities in U.S. adult health begin to emerge and for whom. Moreover, young adulthood seems to be a particularly salient life course period for examining this relationship (Harris, 2010; Kane, Harris, Morgan, & Guilkey, 2017; Yang, Gerken, Schorpp, Boen, & Harris, 2017).
Understanding the educational gradient in health is complex because it may differ by the structural position that individuals occupy, by the life course period examined, or by the measure of health being investigated. Some studies have focused on the differential health returns from degree attainment observed among different racial/ethnic groups. The examination of adult mortality rates, for example, suggests the educational gradient in mortality in U.S. adults is wider among Whites than Blacks or Hispanics (Zajacova & Hummer, 2009). A similar pattern was observed for metabolic syndrome in young adulthood: while Whites with a college degree had lower odds of metabolic syndrome than their less educated counterparts, the same was not true for Blacks or Hispanics (Gaydosh, Schorpp, Chen, Miller, & Harris, 2018). However, racial/ethnic differences in the relationship between education and health are not observed across all studies. For example, the study by Lawrence et al., in 2018 examining educational disparities in cardiovascular health among young adults did not find large differences in the association between education and cardiovascular health by race/ethnicity or gender (Lawrence, Hummer, Domingue, & Harris, 2018).
Investigating the relationship between education and cardiometabolic health among young adults is particularly relevant for understanding current population health trends. The high prevalence of obesity and poor cardiovascular health are perhaps the most significant health problems facing young adults as they age both because of their relevance for the current health status of young adults and as harbingers of poor health in later life. Indeed, a recent report suggests that a stalling in the decline in cardiovascular disease mortality is a primary driver of the flattening in U.S. life expectancy at age 25 since 2010 (Mehta, Abrams, & Myrskylä, 2020). Over a third of young adults in the United States are classified as obese, with an additional 8% classified as class 3 obese, or “high-risk” (Flegal, Kruszon-Moran, Carroll, Fryar, & Ogden, 2016). A substantial proportion of the young adult population is also in poor cardiovascular health, considerably worse than other high-income countries (National Research Council, & Committee on Population, 2013).
Applying the framework of fundamental cause theory (FCT), we use a nationally representative sample of U.S. adolescents that have been followed into young adulthood to examine the educational gradient in cardiometabolic risk among young adults with particular attention to racial/ethnic and sex differences. According to FCT, educational attainment structures access to both material (e.g., income, safe neighborhoods, access to medical care) and nonmaterial (e.g., social networks, prestige) resources that can be deployed flexibly to influence health. Educational attainment is therefore a fundamental cause of health in that even if one pathway linking it to health is blocked, there exists myriad other pathways by which the association is reproduced (Link & Phelan, 1996).
This study advances our understanding of the education-health relationship in four important ways. First, while much of the research on cardiometabolic health has relied on composite indices of cardiometabolic risk, we examine five indicators of cardiometabolic risk separately finding that the educational gradient is different across indicators. Second, we focus on educational attainment specifically rather than as a component of a composite indicator of socioeconomic status (SES) because educational attainment is directly policy relevant. Thus, if educational attainment is strongly associated with health, and to the extent that education has a causal effect, it can be acted upon. The same level of specificity for policy action is not possible with a composite indicator of SES. Third, we empirically test for racial/ethnic and sex differences allowing us to shed further light on the structural dependency of the education-health relationship. Finally, we focus specifically on the education-health relationship in young adults. Much, but not all, of the related work on the education-health relationship has focused on patterns later in the life course.
2. Biomarker-assessed cardiometabolic health
Biomarker-assessed cardiometabolic health offers a way to further our understanding of the education-health relationship in young adulthood. Biomarkers are useful tools for understanding underlying biological processes at work. Often, they can indicate biological dysfunction before clinical manifestation of disease occurs. For example, several studies have documented that even small changes in blood pressure in early life are related to higher risk of cardiovascular events in later life (Miura et al., 2001; Nguyen et al., 2011; Sundström, Neovius, Tynelius, & Rasmussen, 2011). To gain a fuller picture of cardiometabolic health it is useful to utilize multiple markers of cardiometabolic health rather than any single marker. Recent studies have reported that using only body mass index (BMI) to assess cardiometabolic health may misclassify the cardiometabolic profile of a considerable portion of individuals: those with ‘normal’ BMI may have a poor cardiometabolic profile while individuals classified as ‘obese’ may have a healthy cardiometabolic profile (Tomiyama, Hunger, Nguyen-Cuu, & Wells, 2016; Wildman et al., 2008). Educational attainment may also be more or less strongly associated with different dimensions of biomarker-measured health. For example, individuals from socioeconomically disadvantaged backgrounds who become more advantaged in adulthood may have lower waist circumferences and BMIs owing to access to healthier food options in adulthood than their counterparts who do not become more advantaged. However, the high effort coping required to overcome such socioeconomic hardships may result in increased rates of hypertension (James, 1994). Thus, it is imperative to examine biomarkers of multiple body systems to obtain a more holistic view of cardiometabolic health.
Additionally, previous studies incorporating multiple measure of cardiovascular risk have relied on composite indices to examine socioeconomic gradients in health. For example, Walsemann et al. used a cardiovascular risk score based on four biomarkers of cardiovascular risk to examine associations with life course SES and differences by race/ethnicity and gender (Walsemann, Goosby, & Farr, 2016). They found evidence supporting several life course models of SES and cardiovascular risk among White individuals but limited support for an association between life course SES and cardiovascular risk among Black or Hispanic individuals. One of the limitations of such an approach, however, is that each cardiovascular indicator is given equal weight in the composite score and is not investigated as an independent indicator. It may be that the ways in which SES is related to cardiovascular disease depends on the specific measure examined. Additionally, the ways in which a particular biomarker is associated with SES may vary uniquely by sex and race/ethnicity (Britton, Berry, & Hussey, 2018; Everett & Zajacova, 2015; Zamora-Kapoor, Hebert, Montañez, & Buchwald, 2020). Moreover, it is possible that one biomarker of cardiovascular risk may be more relevant for predicting future cardiovascular risk compared to another. Thus, in the current study we examined five separate indicators of cardiometabolic risk allowing for a greater specificity in the outcomes examined.
3. Education and young adult health
This work is guided primarily by fundamental cause theory (FCT) which conceptualizes educational attainment as a critical determinant of both an individual's access to resources and ability to deploy resources on behalf of one's health. However, as demonstrated by several studies, there is non-equivalence in the association between educational attainment and health across social groups (Assari, 2018; Gaydosh et al., 2018; Masters et al., 2015). In particular, the association between educational attainment and health is dependent on structural aspects of society tied to individual identity (Gee & Ford, 2011; J. A. Pearson, 2008).
A rapidly growing body of research using national cohort studies documents the unequal returns to health at equal levels of education among racial/ethnic minority groups (Assari, 2018). Recent studies have reported that higher education was not associated with reduced levels of physical inactivity or obesity among Blacks, whereas for Whites it was (Assari, Nikahd, Malekahmadi, Lankarani, & Zamanian, 2017). Additional studies of inflammatory markers, including C-Reactive Protein (CRP), found weaker longitudinal associations between educational attainment and inflammation for Blacks compared to Whites (Fuller-Rowell, Curtis, Doan, & Coe, 2015). This phenomenon has been referred to as diminished returns for the same level of education for racial minorities (Assari, 2018; Farmer & Ferraro, 2005). Among Hispanics, studies have reported higher overall life expectancy at older ages compared to Whites and Blacks, despite lower levels of education (Braveman, Cubbin, Egerter, Williams, & Pamuk, 2010; Lariscy, Hummer, & Hayward, 2015). However, recent work suggests that this pattern may not hold true for younger Hispanics (Rogers, Lawrence, Hummer, & Tilstra, 2017). While there are many factors to be considered when trying to understand this non-equivalence in the association between education and health, the most promising explanation is the burden of racism faced by racial/ethnic minority groups (Williams, Priest, & Anderson, 2016). This spans from experiences of institutional racism (e.g., residential segregation) to those of interpersonal discrimination (Williams et al., 2016). For example, the high effort coping that is required by Black men in order to navigate discrimination and achieve upward mobility can be costly to health (Fuller-Rowell, Doan, & Eccles, 2012; James, 1994). A similar phenomenon has been described among Black women, who face differential health risks both because of racial discrimination and gender subordination (Mullings, 2005).
Consistent with racial/ethnic differences in the education-health gradient, there may also be differential health returns to educational attainment by sex; however, there are mixed results as to the direction of this relationship. Some studies have found, for example, a stronger association between educational attainment and health for women relative to men (Ross, Masters, & Hummer, 2012; Ross & Mirowsky, 2010). Conversely, educational attainment is more strongly associated with men's mortality (Ross et al., 2012; Zajacova & Hummer, 2009). Understanding patterns of health by gender are inherently complicated in that both biological differences by sex as well as, and perhaps more relevant for the current study, historical systems of power, prestige, and resources that disproportionately favor men over women must be considered (Read & Gorman, 2010). Structural sexism has historically resulted in disadvantaging women in occupational achievements (including wages) and an unequal burden of caretaking in the home—all of which have downstream effects on the psychological and physiological health of women (Chen, Subramanian, Acevedo-Garcia, & Kawachi, 2005; Ross & Mirowsky, 2006; Zajacova, 2006).
Finally, accounting for other dimensions of SES and health in both adolescence and young adulthood is critical to being able to accurately understand the relationship between educational attainment and cardiometabolic health. Family socioeconomic background is an important dimension of SES that structures the association between educational attainment and health for young adults (Brown, Richardson, Hargrove, & Thomas, 2016). Early life socioeconomic disadvantage is associated with higher rates of morbidity and mortality (Galobardes, Smith, & Lynch, 2006) (Haas, 2008; Montez & Hayward, 2014) (Blackwell, Hayward, & Crimmins, 2001; Galobardes, Lynch, & Davey Smith, 2004). Experiencing a disadvantaged background in childhood may also impact adult health indirectly through constraining SES in adulthood (Kane et al., 2017). Together, these studies highlight the need to account for early life SES in understanding the relationship between educational attainment and adult health.
Additionally, health status and behaviors in adolescence are strongly related to young adult health and may be in part responsible for the association between educational attainment and adult health. A study among the Add Health cohort reported that nearly 90% of individuals who were obese in adolescence remained obese in young adulthood (Gordon-Larsen et al., 2019). Increased depressive symptoms in adolescence has also been linked with a reduced likelihood of reporting excellent health in young adulthood (Hoyt, Chase-Lansdale, McDade, & Adam, 2012). In another key study examining SES and health from adolescence to young adulthood, Bauldry et al. found that adolescent health and health behaviors, including high BMI, depressive symptoms, physical activity, smoking, and drinking, were significant mediators between early life SES and self-rated health in both adolescence and young adulthood (Bauldry, Shanahan, Boardman, Miech, & Macmillan, 2012). Adolescent health status and behaviors are thus critical to understanding the young adult educational gradient in health.
4. Current study
Given the importance of understanding cardiometabolic health among young adults, and the complexity of its relationship to educational attainment, the current study asks three critical questions and for which we develop hypotheses based on the current literature:
Q1. Is there evidence of educational disparities in biomarker-assessed cardiometabolic health among young adults in the United States?
H1: Based on FCT, we expect to find higher proportions of poor cardiometabolic health among individuals with lower educational attainment.
Q2: To what extent are educational disparities in biomarker-assessed cardiometabolic health explained by adolescent socioeconomic status (SES), adolescent health, and young adult SES?
H2: We expect that adolescent SES, adolescent health and health behaviors, and young adult SES will explain some, but not all, of the association between educational attainment and cardiometabolic health
Q3. Does the association between educational attainment and biomarker-assessed cardiometabolic health differ by race/ethnicity and sex?
H3: We hypothesize that the associations between educational attainment and cardiometabolic health will be weaker for those occupying structurally disadvantaged positions (i.e., minority racial/ethnic groups and women).
5. Methods
5.1. Data and analytic sample
We used data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative study of individuals as they transition from adolescence to adulthood. The study employs a longitudinal design to collect detailed data on the social, demographic, and health circumstances of individuals. Add Health has followed over 20,000 individuals beginning in 1994–1995, when they were in grades 7–12. Add Health began as a school-based study with an in-school student and school administrator survey. Adolescents were then sampled from schools and interviewed at Wave I. We used data from Wave I, when respondents were aged 12–19, and Wave IV, when respondents were aged 24–32. We used height, weight, waist circumference, inflammation, and cardiovascular health biomarkers collected at Wave IV as our outcome variables. Additional information on the design of Add Health has been published elsewhere (K. M. Harris et al., 2019).
Our analytic sample included individuals who participated in both Wave I and Wave IV of Add Health (n = 14,800). We excluded individuals with missing survey weights, who were pregnant or probably pregnant at Wave IV, and who did not identify as non-Hispanic Black (NHB), non-Hispanic White (NHW), or Hispanic. We excluded women who were pregnant or probably pregnant because the physiological profile of individuals during pregnancy may differ dramatically in comparison to when they are not pregnant (n = 487). We also excluded individuals who were Asian or Pacific Islander, American Indian or Native American, or other race because of relatively small sample sizes (n = 1342). With these restrictions in place, our final analytic sample size was 13,005.
5.2. Educational attainment
We used information collected during Wave IV to classify each participant's educational attainment. At Wave IV individuals were asked “What is the highest level of education that you have achieved to date?” There were thirteen response categories ranging from 8th grade or less to completed post baccalaureate profession education. Using these responses, we created a three-category variable: high school graduate or less, some college, or college graduate and above. The referent category was college graduate or above.
5.3. High-risk cardiometabolic health
We defined high-risk thresholds for five outcomes using Wave IV biomarker data. The high-risk thresholds were based on both national guidelines and previously published studies using Add Health data (ATP III Guidelines At-A-Glance, 2001; Gaydosh et al., 2018). High-risk blood pressure was defined as any one of the following: measured blood pressure greater than 130/85 mmHg, self-report of doctor-diagnosed hypertension, or the use of antihypertensive medication. High-risk waist circumference was measured as waist circumference 88 cm or greater for women and 102 cm or greater for men. Hyperlipidemia was composed of measurements for both high-density lipoprotein (HDL) cholesterol and triglycerides. Add Health released Wave IV lipid measurements in deciles. Accordingly, hyperlipidemia was defined as any one of the following: being in the top three deciles of measured triglycerides for males (top two deciles for females), being in the bottom two deciles of HDL for males (bottom three for females), self-report of doctor diagnosed hyperlipidemia, or use of antihyperlipidemic medication use. Diabetes/pre-diabetes was defined as any of the following: glycated hemoglobin A1C (HbA1c) levels of 5.7% or greater, self-reported history of diabetes, or use of any antidiabetic medication. Finally, high-risk inflammation was based on both measured high sensitivity C-Reactive Protein (CRP) levels or the use of anti-inflammatory medications. Anti-inflammatory medication use may confound classifications of cardiovascular risk based only on measured CRP. We defined categories of measured CRP based on recommendations from the American Heart Association and Centers for Disease Control and Prevention (T. A. Pearson et al., 2003): <1 mg/L was considered “Low”; 1–3 mg/L was considered “average” and >3 was considered “high.” High inflammation was defined based on a participant having a measured CRP level >3 mg/L or reported use of anti-inflammatory medication in either the past 24 h or past 4 weeks, depending on the medication.
5.4. Covariates
We examined the following covariates as potential confounders of the association between educational attainment and cardiometabolic risk: age, sex, race/ethnicity, nativity status, adolescent health, adolescent SES, and young adult SES. We also examined race/ethnicity and sex as possible moderators of the association between educational attainment and cardiometabolic risk.
We used data from Wave I to classify individual's race/ethnicity and sex. At Wave I individuals were asked “What is your race” and then separately asked “Are you of Hispanic or Latino origin?” Individuals were classified as NHB if they did not identify as Hispanic and selected Black/African American as their race. Individuals were classified as NHW if they did not identify as Hispanic and selected White as their race. Any individual that answered yes to being of Hispanic or Latino origin was classified as Hispanic. NHWs were specified as the reference category. Sex classification was based on the response to a Wave I question asking individuals to indicate their sex. Males were used as the reference category. Nativity status was based on whether the individuals reported being born in the U.S. or outside of the. U.S.
Adolescent SES was based on Wave I highest parental educational attainment, household income (<$25K, $25K—$39K, $40K-$49K, > = $50K), and family structure (two biological parents in the home, two parents [at least one non-biological] in the home, single mother, single father, or another family structure). Parental education was based on the parent survey administered at Wave I as well as response from the adolescent. Parents and adolescents were asked to report how far they, and their partner, (or their parent in the case of the adolescent) went in school. There were twelve response categories ranging from never going to school to professional training beyond a 4-year college or university. Parental education was a composite variable based on the responses from both the surveyed parent and the second parent (or parental figure). The highest level of education from either parent was used, which we then collapsed into two levels: greater than a high school education and high school graduate or below. We used high school graduation as the marker for low education given the time period when parents were likely in school.
We used six indicators of adolescent health collected at Wave I: body mass index classifications (normal, overweight, and obese based on age and sex), a depressive score that ranged from 0 to 27, smoking status (yes/no), self-rated health (range from 1 to 5, with 1 equal to poor health and 5 equal to excellent health), a sum of physical activities over the past seven days, and alcohol consumption status (yes/no).
Young adult SES was measured using Wave IV household income (<$30K, $30K—$49K, $50K-$74K, > = $75K), employment status (yes/no), health insurance status (insured (non-Medicaid), Medicaid, and uninsured), and marital status (married, cohabitating, not married/cohabitating).
We included age at Wave IV as a continuous variable in the statistical models.
5.5. Missing data
We assessed patterns of missing data in our analytic sample (n = 13,005); 34% of respondents were missing data on one or more variables. Of particular note, education attainment had 0.03% missing values. There were no missing values for race (NHW, NHB, and Hispanic), sex, or age. Two percent were missing data on parental education. Of the five outcome variables, 0.01% were missing data on blood pressure, 8% on CRP, 8% on diabetes and 13% on hyperlipidemia. There were no missing data for waist circumference.
We used multiple imputation techniques for the missing data on the variables listed above. We used a fully conditional method (FCS) for the imputation with the discriminate option to impute categorical variables. We used 50 imputations to optimize precision in our estimates. We imputed values on all covariates as well as the five health outcome variables. The imputations were carried out in SAS using the Proc MI procedure.
5.6. Statistical analyses
Descriptive statistics were used to describe the study population. Weighted proportions and mean values of key variables were calculated. To examine whether there was evidence of educational gradients in high-risk cardiometabolic health among young adults, we used logistic regression models estimating the association between educational attainment and each of five high-risk cardiometabolic outcomes (high-risk blood pressure, high-risk waist circumference, hyperlipidemia, diabetes/pre-diabetes, and high-risk inflammation). We first examined the association between educational attainment and each of the five cardiometabolic outcomes while controlling for age, race/ethnicity, sex, and nativity (model 1).
Next, to assess whether educational disparities were explained by adolescent SES, adolescent health, and young adult SES, we estimated models controlling for each set of covariates. Model 2 includes controls for age, race/ethnicity, sex, nativity, adolescent SES and adolescent health. Model 3 includes controls for age, race/ethnicity, sex, nativity, adolescent SES, adolescent health, and young adult SES.
In order to determine if educational gradients in young adult cardiometabolic health differed by race/ethnicity and sex, we first tested two-way interaction terms in the fully adjusted model (model 3). We then stratified subsequent models by race/ethnicity and sex. Given the complexity of interpreting interaction terms in logistic regression models, we estimated predicted probabilities rather than comparing coefficients across models (Long & Mustillo, 2018). We reported the predicted probabilities for each health outcome by race/ethnic and sex subgroup.
All analyses included appropriate survey weights to account for the clustered study design. A two-sided alpha of 0.05 was used to signify statistical significance. All statistical analyses were conducted using SAS 9.4 (SAS Institute, Inc., Cary, North Carolina).
6. Results
6.1. Descriptive findings
Descriptive statistics for the study sample are given in Table 1. Approximately 28% were college graduates, while 43% and 29% reported having some college or a high school education or less, respectively. A majority (86%) had a least one parent with greater than a high school education. The mean age at Wave IV was 28 years. Nearly half were women (48%) and 70% identified as NHW, 17% as NHB, and 13% as Hispanic.
Table 1.
Weighted sample characteristics of the National Longitudinal Study of Adolescent to Adult Health Waves I and IV, n = 13,005.
| Overall | High School Degree or Less | Some College | College Graduate or Higher | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) at Wave IV | 28.35 (0.12) | 28.45 (0.15) | 28.34 (0.13) | 28.27 (0.12) |
| Female | 47.91 | 39.14 | 49.58 | 53.70 |
| Race/Ethnicity | ||||
| Non-Hispanic Black | 17.22 | 21.43 | 17.57 | 12.74 |
| Hispanic | 12.87 | 16.50 | 13.72 | 8.20 |
| Non-Hispanic White | 69.90 | 62.07 | 68.71 | 79.06 |
| Nativity | ||||
| U.S.-born | 95.92 | 95.43 | 95.78 | 96.58 |
| Foreign-born | 4.08 | 4.57 | 4.22 | 3.42 |
| Adolescent SES (Wave I) | ||||
| Parental Education | ||||
| High School Degree or Less | 13.94 | 28.04 | 11.97 | 3.55 |
| Some College or More | 86.06 | 71.96 | 88.03 | 96.45 |
| Household Income | ||||
| < $25 K | 19.60 | 33.10 | 19.14 | 7.53 |
| $25K - $39,999 K | 26.65 | 31.03 | 30.69 | 16.53 |
| $40 K - $49,999 K | 11.18 | 9.59 | 12.12 | 11.30 |
| > = $50 K | 42.57 | 26.28 | 38.06 | 64.64 |
| Family Structure | ||||
| 2 biological parents | 53.84 | 41.65 | 51.27 | 69.17 |
| 2 parent home (but not 2 biological parents) | 17.09 | 19.55 | 18.53 | 12.63 |
| Single mother | 20.43 | 25.71 | 21.33 | 14.12 |
| Single father | 2.91 | 3.71 | 3.14 | 1.82 |
| Other family structure | 5.73 | 9.38 | 5.74 | 2.26 |
| Adolescent Health (Wave I) | ||||
| BMI | ||||
| Obese | 9.28 | 10.61 | 10.86 | 5.69 |
| Overweight | 19.45 | 22.17 | 20.69 | 15.05 |
| Normal | 71.27 | 67.22 | 68.45 | 79.26 |
| # Depressive Symptoms | 5.70 (0.08) | 6.62 (0.12) | 5.77 (0.09) | 4.72 (0.10) |
| Smoker (Yes/No) | 21.84 | 29.10 | 24.34 | 11.39 |
| Self-rated health | ||||
| Poor (1) | 0.57 | 0.76 | 0.60 | 0.36 |
| Fair (2) | 6.41 | 9.45 | 6.99 | 2.67 |
| Good (3) | 25.62 | 32.15 | 27.29 | 16.98 |
| Very Good (4) | 39.66 | 34.18 | 39.70 | 44.78 |
| Excellent (5) | 27.74 | 23.46 | 25.42 | 35.21 |
| Physical activities (1–15) | 7.21 (0.07) | 6.68 (0.09) | 7.15 (0.08) | 7.79 (0.09) |
| Drinker (Yes/No) | 41.78 | 40.99 | 43.12 | 40.56 |
| Young Adult SES (Wave IV) | ||||
| Educational Attainment | ||||
| High School Degree or Less | 27.57 | |||
| Some College | 43.23 | |||
| College Degree or Greater | 29.20 | |||
| Household Income | ||||
| < $30K | 24.60 | 41.17 | 22.94 | 11.40 |
| $30 K - $49,999 K | 23.30 | 24.31 | 25.95 | 18.42 |
| $50 K - $74,999 K | 23.89 | 19.59 | 25.74 | 25.22 |
| > = $75,000 K | 28.21 | 14.93 | 25.36 | 44.97 |
| Employed or in school (Yes/No) | 64.87 | 56.91 | 67.60 | 68.32 |
| Insurance Status | ||||
| Uninsured | 22.92 | 37.56 | 22.69 | 9.43 |
| Medicaid | 7.85 | 15.22 | 7.66 | 1.16 |
| Insured (non Medicaid) | 69.23 | 47.21 | 69.66 | 89.40 |
| Marital Status | ||||
| Not married/cohabitating | 37.98 | 38.28 | 36.30 | 40.19 |
| Cohabitating | 20.35 | 24.19 | 20.52 | 16.46 |
| Married | 41.67 | 37.53 | 43.18 | 43.35 |
| Wave IV Cardiometabolic Outcomes | ||||
| High-Risk Blood Pressure | 44.40 | 49.39 | 43.62 | 40.86 |
| High-Risk Waist Circumference | 49.61 | 51.95 | 53.56 | 41.56 |
| Hyperlipidemia | 48.74 | 52.64 | 50.05 | 43.13 |
| Diabetes/Pre-Diabetes | 33.13 | 39.74 | 35.38 | 23.55 |
| High Inflammation | 57.60 | 60.06 | 59.72 | 52.13 |
Note: Measurement schemes for all variables are detailed in the text.
In terms of their biomarker-measured cardiometabolic health, over half of the sample had a high-risk inflammatory load (58%) and a high-risk waist circumference (50%). Additionally, a large proportion of the sample was classified as high-risk in terms of blood pressure (44%), hyperlipidemia (49%) and diabetes/pre-diabetes (33%), respectively.
Among those with a high school education or less, 21% were NHB, 17% Hispanic, and 62% NHW compared to those with a college degree or higher, of whom 13% were NHB, 8% Hispanic, and 79% NHW. In addition, the proportion of the population with at least one parent with greater than a high school education differed across categories of educational attainment. Among those with a high school degree or less, only 72% had at least one parent with greater than a high school education. Among those with a college degree or higher, however, 96% had at least one parent with greater than a high school education.
There were also differences in the proportion of high-risk cardiometabolic outcomes by educational attainment. Those with a high school degree or less had higher proportions of individuals classified with high-risk blood pressure (49%), hyperlipidemia (53%), diabetes/pre-diabetes (40%), and high-risk inflammation (60%) compared to those with a college degree or higher for whom 41% had high-risk blood pressure, 43% had hyperlipidemia, 24% had diabetes/pre-diabetes, and 52% had high inflammation. Those with some college also had higher proportions of individuals classified in high-risk cardiometabolic outcomes compared to those with a college degree or above.
6.2. Educational disparities in cardiometabolic heath among young adults
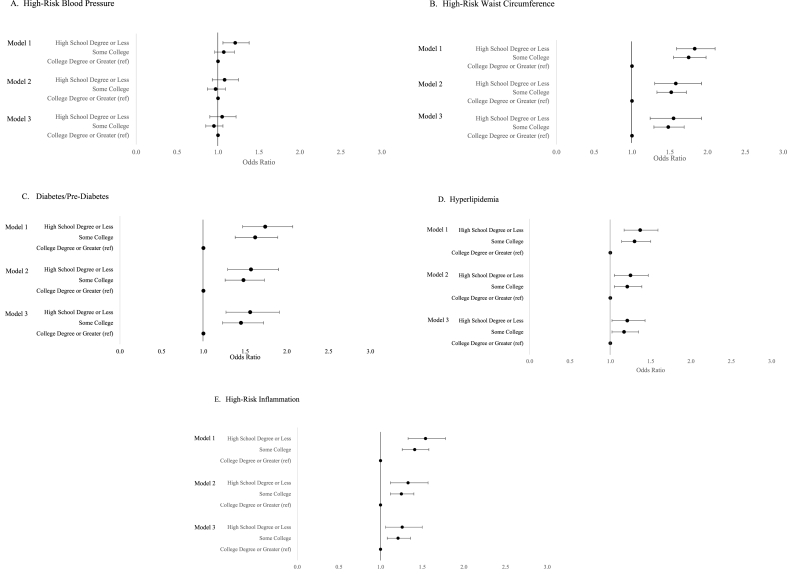
We examined associations between educational attainment and cardiometabolic health adjusting for age, sex, race/ethnicity, and nativity (Fig. 1, model 1). Among four of the five high-risk cardiometabolic outcomes examined, we observed an association between educational attainment and poor cardiometabolic health. The strongest associations in terms of magnitude were observed for high-risk waist circumference and diabetes/pre-diabetes. Those with a high school degree or less had 1.83 (95% CI: 1.59, 2.10) times the odds of a high waist circumference compared to those with a college degree or more. The association was similar for those with some college. In addition, those with a high school degree or less had 1.74 (95% CI: 1.47, 2.07) times the odds of diabetes/pre-diabetes compared to those with a college degree or more. Those with some college had 1.61 (95% CI: 1.38, 1.89) times the odds of diabetes/pre-diabetes compared to those with a college degree or more.
Fig. 1.
Regression results estimating the odds of being in a high-risk category for five cardiometabolic health indicators by levels of educational attainment in the National Longitudinal Study of Adolescent to Adult Health, n = 13,002. Model 1 controls for age, sex, race/ethnicity and nativity status. Model 2 controls for age, sex, race/ethnicity, nativity status, adolescent health, and adolescent SES indicators. Model 3 controls for age, sex, race/ethnicity, nativity status, adolescent health, adolescent SES indicators, and young adult SES indicators. Panel A corresponds to high-risk blood pressure. Panel B corresponds to high-risk waist circumference. Panel C corresponds to diabetes/pre-diabetes. Panel D corresponds to hyperlipidemia. Panel E corresponds to high-risk inflammation.
Though slightly weaker, we also saw evidence of educational disparities in hyperlipidemia and high-risk inflammation. Those with a high school degree or less had 1.37 (95% CI: 1.17, 1.59) times the odds of hyperlipidemia compared to those with a college degree or more. Those with some college had 1.31 (95% CI: 1.14, 1.50) times the odds of hyperlipidemia. Finally, those with a high school degree or less had 1.54 (95% CI: 1.33, 1.78) times the odds of high-risk inflammation compared to those with a college education or more and those with some college had 1.41 (95% CI:1.26, 1.58) times the odds of high inflammation.
Full model results are presented in Supplementary Table 1.
6.3. Educational disparities in young adult cardiometabolic health are observed net of adolescent SES, adolescent health, and young adult SES
We next examined whether there was evidence of educational disparities in young adult cardiometabolic health net of adolescent SES, adolescent health, and young adult SES. Fig. 1, model 2 shows the odds ratio for models controlling for adolescent SES and adolescent health. Fig. 1, model 3 shows the odds of a high-risk cardiometabolic outcome by educational attainment with additional controls for young adult SES. With the exception of high-risk blood pressure, a statistically significant association remained between educational attainment and poor cardiometabolic health net of SES and health factors. In particular, the association between educational attainment and both high-risk waist circumference and diabetes/pre-diabetes remained particularly strong.
6.4. Differences in the association between educational attainment and cardiometabolic health by race/ethnicity and sex
Finally, we examined whether the association between educational attainment and biomarker-measured cardiometabolic health differed by race/ethnicity and sex. We first tested two-way interaction terms in the fully adjusted model (model 3). Of the 30 interaction terms we tested, five reached the level of statistical significance (P < 0.05) with an additional three marginally significant (P < 0.10) (Table 2). Based on these results, the differences in the distribution of covariates across race/ethnic subgroups, and our a priori hypotheses regarding the structural influences of race/ethnicity and gender on health, we subsequently stratified models by race/ethnicity and sex.
Table 2.
Results of the regression analysis assessing two-way interactions between both education and race/ethnicity, and education and sex for five cardiometabolic health indicators.
| High-Risk Blood Pressure |
High-Risk Waist Circumference |
Diabetes/Pre-Diabetes |
Hyperlipidemia |
High-Risk Inflammation |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||
| Education*Race/Ethnicity Interactions | ||||||||||||||||
| High school or less*Black | 1.00 | 0.71, 1.41 | 1.00 | 0.86 | 0.59, 1.25 | 0.44 | 0.56 | 0.40, 0.78 | <.001 | 0.69 | 0.47, 1.02 | 0.07 | 0.79 | 0.57, 1.10 | 0.17 | |
| High school or less*Hispanic | 1.11 | 0.80, 1.55 | 0.54 | 0.78 | 0.46, 1.30 | 0.34 | 0.91 | 0.54, 1.54 | 0.74 | 0.96 | 0.62, 1.50 | 0.87 | 0.74 | 0.48, 1.13 | 0.17 | |
| Some college*Black | 1.03 | 0.76, 1.41 | 0.84 | 0.76 | 0.56, 1.02 | 0.07 | 0.58 | 0.44, 0.78 | <.001 | 0.63 | 0.46, 0.86 | 0.00 | 0.77 | 0.59, 1.02 | 0.07 | |
| Some college*Hispanic |
0.94 |
0.67, 1.31 |
0.71 |
0.76 |
0.51, 1.13 |
0.18 |
0.99 |
0.66, 1.50 |
0.97 |
0.92 |
0.64, 1.33 |
0.66 |
0.81 |
0.56, 1.18 |
0.27 |
|
| Education*Sex Interactions | ||||||||||||||||
| High school or less*Female | 1.05 | 0.81, 1.36 | 0.71 | 1.79 | 1.33, 2.39 | <.001 | 1.08 | 0.81, 1.43 | 0.59 | 1.36 | 1.01, 1.82 | 0.05 | 0.96 | 0.72, 1.29 | 0.81 | |
| Some college*Female | 0.93 | 0.74, 1.17 | 0.53 | 1.19 | 0.95, 1.50 | 0.13 | 0.85 | 0.63, 1.14 | 0.27 | 1.09 | 0.85, 1.39 | 0.51 | 0.82 | 0.65, 1.03 | 0.08 | |
Interaction terms were estimated in the fully adjusted model which included educational attainment, age, sex, race/ethnicity, nativity, adolescent SES characteristics, adolescent health characteristics, and young adult SES characteristics.
In stratified models, we estimated how the association between educational attainment and young adult cardiometabolic health differed across racial/ethnic and sex subgroups (Supplementary Tables 2 and 3). Using the model results shown in Supplementary Tables 2 and 3, we also derived predicted probabilities of being in a high-risk cardiometabolic category for each race/ethnic and sex subgroup on a scale from 0 to 1 and calculated separately for NHBs, Hispanics, NHWs, women, and men.
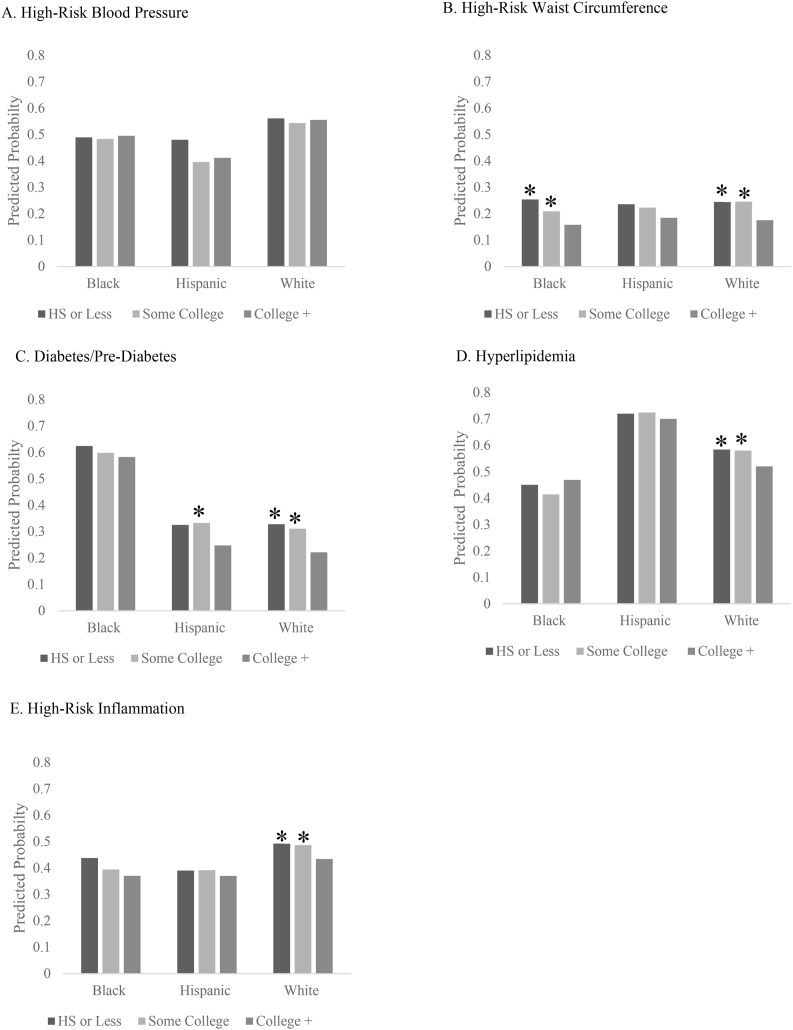
In race/ethnicity-stratified models, we found evidence that the presence and strength of the association between educational attainment and cardiometabolic health differed among NHWs, NHBs, and Hispanics and across the individual outcomes. There was no educational gradient among any racial/ethnic group for high-risk blood pressure (Fig. 2A). There was an educational gradient for high-risk waist circumference among both NHBs and NHWs. Both groups had similar predicted probabilities of high-risk waist circumference across educational categories and the association between educational attainment and high-risk waist circumference was statistically significant for both groups (Fig. 2B). Regarding diabetes/pre-diabetes, there was evidence of an educational gradient among NHWs and among Hispanics with some college education. NHBs had nearly twice the predicted probability of diabetes/pre-diabetes compared to NHWs across educational strata (Fig. 2C). Only among NHWs was there evidence of an educational gradient for both hyperlipidemia and high-risk inflammation (Fig. 2D and E) .
Fig. 2.
Predicted probability of each high-risk cardiometabolic outcome by education attainment and stratified by race/ethnicity. Asterisks indicate statistically significant differences based on the models presented in Supplementary Table 2. Panel A corresponds to high-risk blood pressure. Panel B corresponds to high-risk waist circumference. Panel C corresponds to diabetes/pre-diabetes. Panel D corresponds to hyperlipidemia. Panel E corresponds to high-risk inflammation.
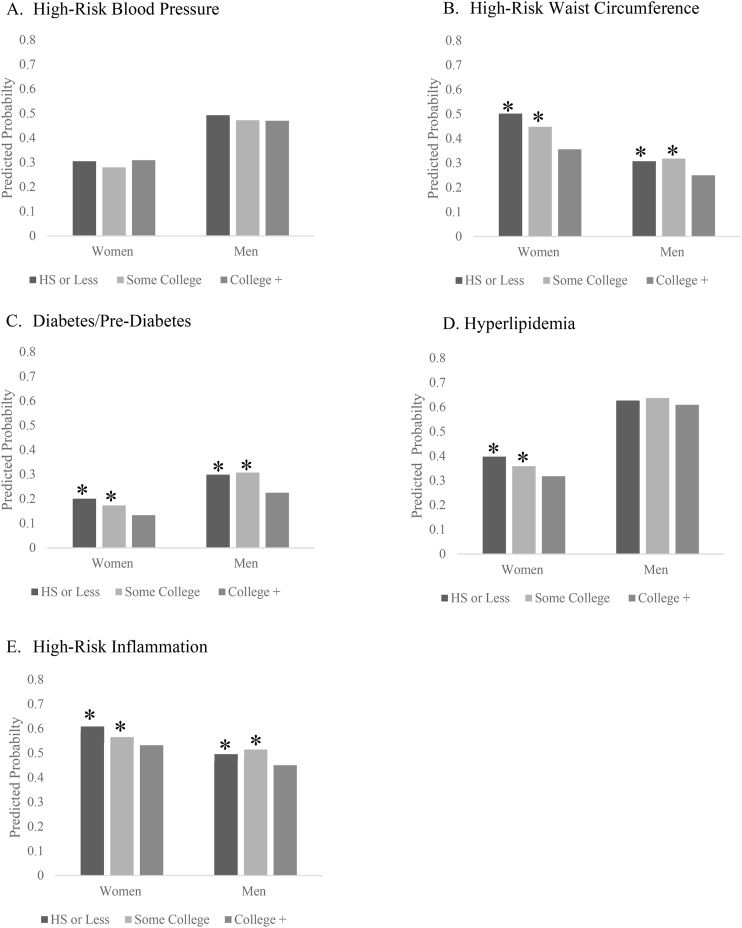
In sex-stratified models, in general we found a consistent educational gradient in cardiometabolic health among both women and men. Again, there was not a statistically significant educational gradient for either group with regards to high-risk blood pressure (Fig. 3A). For women, we observed a consistent educational gradient for high-risk waist circumference, diabetes/pre-diabetes, hyperlipidemia and high-risk inflammation though the magnitude of the association differed by outcome (Fig. 3 B-E). For men, there was evidence of an educational gradient for high-risk waist circumference, diabetes/pre-diabetes, and high-risk inflammation. It should also be noted that there were differences in the predicted probabilities of each outcome across women and men. Women had higher predicted probabilities of high-risk waist circumference and high-risk inflammation across educational strata compared to men. Men had higher predicted probabilities of diabetes/pre-diabetes and hyperlipidemia across educational strata compared to women.
Fig. 3.
Predicted probability of each high-risk cardiometabolic outcome by education attainment and stratified by sex. Asterisks indicate statistically significant differences based on the models presented in Supplementary Table 3. Panel A corresponds to high-risk blood pressure. Panel B corresponds to high-risk waist circumference. Panel C corresponds to diabetes/pre-diabetes. Panel D corresponds to hyperlipidemia. Panel E corresponds to high-risk inflammation.
7. Discussion
Educational disparities in health and mortality are well-documented and evidence suggests that they may be widening (Bosworth, 2018; Case & Deaton, 2017). Yet, there is much unknown about when educational disparities begin to emerge and for whom. Young adulthood may be a sensitive period for both the development of health and social behaviors and setting in place biological trajectories that extend into middle and late life (Harris and McDade 2018). Here, we first estimated the association between education and biomarker-assessed cardiometabolic health among young adults in the U.S. We then examined the extent to which this association was explained by adolescent health and both adolescent and young adult SES. Finally, we investigated whether the association between educational attainment and cardiometabolic health differed by race/ethnicity and sex. The results presented here contribute to our understanding of educational disparities in cardiometabolic health starting early in the adult life course. Of particular importance is how robust this association was to controls for other markers of adolescent health and adolescent and young adult SES which speaks to the critical importance of education for maintaining health, even as early as young adulthood. In addition, we found that the educational gradient differed according to the specific outcome investigated with diabetes/pre-diabetes and high-risk waist circumference showing the strongest educational gradients. We describe below the implications of the study findings, and particularly the importance of considering the heterogeneity in the education-health relationship across subgroups of the population.
In line with the education-health literature, we found educational differences in cardiometabolic health in young adulthood. These associations were consistent and strong across four of the five cardiometabolic health outcomes. This is notable given that some young adults may go on to complete additional education. We also estimated race/ethnicity- and sex-stratified models supported by statistical evidence of an interaction and our a priori hypotheses regarding the structural influence of racism and sexism. We found modest evidence suggesting that NHWs and women experienced the most robust gains in health from education across multiple indicators of risk.
Of note, we found no consistent evidence of an educational gradient in blood pressure. There was a modest association observed in Model 1 among those with less than a high school education. However, this association was null in subsequent models controlling for adolescent SES, adolescent health, and young adult SES. In sensitivity analyses, we examined whether the attenuation in the estimates was due primarily to controlling for adolescent BMI. As shown in Supplementary Table 4, the addition of adolescent BMI results in an attenuation of the educational attainment estimate. However, this does not fully account for the attenuation observed with the inclusion of additional covariates of adolescent SES and adolescent health. Additional studies investigating blood pressure in young adults are needed to further clarify the role of SES, and educational attainment specifically, in determining patterns of high-risk blood pressure.
Our findings are generally consistent with fundamental cause theory. Based on FCT, we hypothesized that there would be better cardiometabolic health among individuals with higher educational attainment and indeed we found evidence to support this. We also found evidence to support our second hypothesis that adolescent SES and health and young adult SES would explain some, but not all, of the association between educational attainment and cardiometabolic health. We investigated a broad range of control variables and, while the estimates were attenuated, there remained a significant association between educational attainment and cardiometabolic health. This is consistent with other recent studies that have reported a similarly strong association between education and health (Lawrence et al., 2018), even with extensive controls for early life socioeconomic status and health. Additional research is needed that examines education both as a life course process that generates and constrains opportunities, and as an institution that is capable of reproducing inequality (Zajacova & Lawrence, 2018).
Finally, we hypothesized there would be weaker associations between educational attainment and cardiometabolic health among those occupying structurally disadvantaged positions and found modest evidence to support this with regards to race/ethnic differences but not sex differences. Our findings were particularly poignant for NHBs and Hispanics for whom there was limited evidence of an association between educational attainment and health. This is consistent with previous studies showing weaker associations with SES and cardiometabolic risk among NHBs and Hispanics (Gaydosh et al., 2018; Walsemann et al., 2016). The differential gains hypothesis offers a helpful framework for explaining why we did not observe consistent educational gradients in health among people of color in this study. Fitting within the tenets of FCT, the ability for a particular group to leverage resources to their advantage are constrained by the structural forces at work (Assari, 2018; Assari et al., 2017). For example, structural factors such as generational poverty, segregation, racism, and discrimination may all work to reduce the health gains people of color experience from education. For instance, NHBs and Hispanics are more likely to experience discrimination at every level of socioeconomic status. It is well known that experiences of discrimination have many health consequences including higher rates of heart disease (Lewis, Williams, Tamene, & Clark, 2014), hypertension (Mezuk, Kershaw, Hudson, Lim, & Ratliff, 2011), and mortality (Barnes et al., 2008), as well as biomarker-assessed health outcomes such as higher cortisol levels (Lee et al., 2018), higher inflammation (Szanton et al., 2012), and decreased telomere length (Chae et al., 2014). Thus, for people of color operating within a structurally racist society in which they are disproportionately disadvantaged, the health gains from education may not manifest. Importantly, we do not interpret the findings of the current study to mean that education is not as important or meaningful for people of color. Rather, these findings suggest that in addition to promoting educational attainment for these groups, we must also address the underlying structures of racism that operate in tandem.
The findings with regards to women were contrary to our hypothesis. Based on FCT, as a consequence of structural sexism we expected the association between educational attainment and cardiometabolic health to be weaker among women. There are three potential reasons for the observed patterns. First, differences in the strength of the educational gradient and cardiometabolic health by sex may depend on the life stage under investigation. Young men at all SES levels engage in more risky health behaviors compared to young women which could have consequences for their cardiometabolic profiles in early adulthood, regardless of educational level (Read & Gorman, 2010). Second, the disadvantaged social standing and exposure to social stressors over the life course that women experience lead to an increasing prevalence of acute and chronic conditions as women age, including worse self-rated health, higher rates of depression, and more functional decline (Hargrove et al., 2020; Ross et al., 2012). Thus, it is plausible that our finding of a stronger educational gradient among women may not hold as the study population ages. Notably, in our sample despite a stronger educational gradient, a greater proportion of women were classified as high-risk for both waist circumference and inflammation compared to men. Finally, it may be that the pattern observed was primarily driven by NHW women. For example, Walsemann et al. (2016) reported that among NHW women SES was more strongly associated with cardiovascular risk compared to NHW men (Walsemann et al., 2016). However, there was no association between SES and cardiovascular risk for NHB women. Future studies should continue to investigate race/ethnicity and sex differences in the association between education and health, particularly as they unfold over the life course.
This work had several limitations that we hope other research will consider. First, we only estimated cross-sectional associations. Therefore, we could not firmly establish a temporal sequence nor could we investigate how these associations unfold longitudinally. Second, our assessment of educational attainment does not take into account measures of the quality of schooling, which may affect how and to what extent education influences health. Additionally, there are likely important confounders of the education-health relationship for which we were not able to control. However, given the robust relationship between education and health documented in the literature, we feel that the associations we observed would remain with the inclusion of additional confounders.
In conclusion, we documented consistent education disparities in biomarker assessed cardiometabolic health in young adulthood. We found evidence of heterogeneity in this relationship across race/ethnic subgroups. Our findings suggest that even as early as young adulthood there are disparities in health outcomes by educational attainment, which have the potential to lead to even larger disparities in late life health. Further understanding this relationship requires careful consideration of the social, economic, and political structures at work which both provide certain groups greater access to education, and the means to leverage those resources to improve health status.
Declaration of competing interest
The authors declare no conflicts of interest.
Acknowledgements
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
GN received support for this work from the National Institute of Aging grant K99AG062749 and from the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant T32 HD091058.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100752.
Author statement
Consent to submit has been received explicitly from all co-authors. Authors whose names appear on the submission have contributed sufficiently to the scientific work and therefore share collective responsibility and accountability for the results.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Assari S. Unequal gain of equal resources across racial groups. International Journal of Health Policy and Management. 2018;7(1):1. doi: 10.15171/ijhpm.2017.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari S., Nikahd A., Malekahmadi M.R., Lankarani M.M., Zamanian H. Race by gender group differences in the protective effects of socioeconomic factors against sustained health problems across five domains. Journal of racial and ethnic health disparities. 2017;4(5):884–894. doi: 10.1007/s40615-016-0291-3. [DOI] [PubMed] [Google Scholar]
- TP III Guidelines At-A-Glance. (01-3305). (2001).
- Barnes L.L., De Leon C.F.M., Lewis T.T., Bienias J.L., Wilson R.S., Evans D.A. Perceived discrimination and mortality in a population-based study of older adults. American Journal of Public Health. 2008;98(7):1241–1247. doi: 10.2105/AJPH.2007.114397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauldry S., Shanahan M.J., Boardman J.D., Miech R.A., Macmillan R. A life course model of self-rated health through adolescence and young adulthood. Social Science & Medicine. 2012;75(7):1311–1320. doi: 10.1016/j.socscimed.2012.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell D.L., Hayward M.D., Crimmins E.M. Does childhood health affect chronic morbidity in later life? Social Science & Medicine. 2001;52(8):1269–1284. doi: 10.1016/s0277-9536(00)00230-6. [DOI] [PubMed] [Google Scholar]
- Bosworth B. Increasing disparities in mortality by socioeconomic status. Annual Review of Public Health. 2018;39:237–251. doi: 10.1146/annurev-publhealth-040617-014615. [DOI] [PubMed] [Google Scholar]
- Braveman P.A., Cubbin C., Egerter S., Williams D.R., Pamuk E. Socioeconomic disparities in health in the United States: What the patterns tell us. American Journal of Public Health. 2010;100(S1):S186–S196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton L.E., Berry D.C., Hussey J.M. Comorbid hypertension and diabetes among US women of reproductive age: Prevalence and disparities. Journal of Diabetes and Its Complications. 2018;32(12):1148–1152. doi: 10.1016/j.jdiacomp.2018.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T.H., Richardson L.J., Hargrove T.W., Thomas C.S. Using multiple-hierarchy stratification and life course approaches to understand health inequalities: The intersecting consequences of race, gender, SES, and age. Journal of Health and Social Behavior. 2016;57(2):200–222. doi: 10.1177/0022146516645165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A., Deaton A. Mortality and morbidity in the 21st century. Brookings Papers on Economic Activity. 2017;(1):397–476. doi: 10.1353/eca.2017.0005. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae D.H., Nuru-Jeter A.M., Adler N.E., Brody G.H., Lin J., Blackburn E.H. Discrimination, racial bias, and telomere length in African-American men. American Journal of Preventive Medicine. 2014;46(2):103–111. doi: 10.1016/j.amepre.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y.-Y., Subramanian S., Acevedo-Garcia D., Kawachi I. Women's status and depressive symptoms: A multilevel analysis. Social Science & Medicine. 2005;60(1):49–60. doi: 10.1016/j.socscimed.2004.04.030. [DOI] [PubMed] [Google Scholar]
- Everett B., Zajacova A. Gender differences in hypertension and hypertension awareness among young adults. Biodemography and Social Biology. 2015;61(1):1–17. doi: 10.1080/19485565.2014.929488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer M.M., Ferraro K.F. Are racial disparities in health conditional on socioeconomic status? Social Science & Medicine. 2005;60(1):191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- Flegal K.M., Kruszon-Moran D., Carroll M.D., Fryar C.D., Ogden C.L. Trends in obesity among adults in the United States, 2005 to 2014. Jama. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Rowell T.E., Curtis D.S., Doan S.N., Coe C.L. Racial disparities in the health benefits of educational attainment: A study of inflammatory trajectories among African American and white adults. Psychosomatic Medicine. 2015;77(1):33–40. doi: 10.1097/PSY.0000000000000128. [DOI] [PubMed] [Google Scholar]
- Fuller-Rowell T.E., Doan S.N., Eccles J.S. Differential effects of perceived discrimination on the diurnal cortisol rhythm of African Americans and Whites. Psychoneuroendocrinology. 2012;37(1):107–118. doi: 10.1016/j.psyneuen.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B., Lynch J.W., Davey Smith G. Childhood socioeconomic circumstances and cause-specific mortality in adulthood: Systematic review and interpretation. Epidemiologic Reviews. 2004;26(1):7–21. doi: 10.1093/epirev/mxh008. [DOI] [PubMed] [Google Scholar]
- Galobardes B., Smith G.D., Lynch J.W. Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Annals of Epidemiology. 2006;16(2):91–104. doi: 10.1016/j.annepidem.2005.06.053. [DOI] [PubMed] [Google Scholar]
- Gaydosh L., Schorpp K.M., Chen E., Miller G.E., Harris K.M. College completion predicts lower depression but higher metabolic syndrome among disadvantaged minorities in young adulthood. Proceedings of the National Academy of Sciences. 2018;115(1):109–114. doi: 10.1073/pnas.1714616114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G.C., Ford C.L. Structural racism and health inequities: Old issues, new directions. Du Bois Review: Social Science Research on Race. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon-Larsen P., From the Carolina Population Center, D. o. N., University of North Carolina, School of Public Health, University of North Carolina at Chapel Hill. Adair L.S. Five-year obesity incidence in the transition period between adolescence and adulthood: The national longitudinal study of adolescent health. American Journal of Clinical Nutrition. 2019;80(3):569–575. doi: 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]
- Haas S. Trajectories of functional health: The ‘long arm’of childhood health and socioeconomic factors. Social Science & Medicine. 2008;66(4):849–861. doi: 10.1016/j.socscimed.2007.11.004. [DOI] [PubMed] [Google Scholar]
- Hargrove T.W., Halpern C.T., Gaydosh L., Hussey J.M., Whitsel E.A., Dole N. Race/ethnicity, gender, and trajectories of depressive symptoms across early-and mid-life among the Add health cohort. Journal of Racial and Ethnic Health Disparities. 2020:1–11. doi: 10.1007/s40615-019-00692-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris K.M. An integrative approach to health. Demography. 2010;47(1):1–22. doi: 10.1353/dem.0.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris K.M., Halpern C.T., Whitsel E.A., Hussey J.M., Killeya-Jones L.A., Tabor J. Cohort profile: The national longitudinal study of adolescent to adult health (Add health) International Journal of Epidemiology. 2019;48(5) doi: 10.1093/ije/dyz115. 1415–1415k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward M.D., Hummer R.A., Sasson I. Trends and group differences in the association between educational attainment and US adult mortality: Implications for understanding education's causal influence. Social Science & Medicine. 2015;127:8–18. doi: 10.1016/j.socscimed.2014.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyt L.T., Chase-Lansdale P.L., McDade T.W., Adam E.K. Positive youth, healthy adults: Does positive well-being in adolescence predict better perceived health and fewer risky health behaviors in young adulthood? Journal of Adolescent Health. 2012;50(1):66–73. doi: 10.1016/j.jadohealth.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer R.A., Hamilton E.R. Vol. 5. Univ of California Press; 2019. (Population health in America). [Google Scholar]
- James S.A. John Henryism and the health of African-Americans. Culture, Medicine and Psychiatry. 1994;18(2):163–182. doi: 10.1007/BF01379448. [DOI] [PubMed] [Google Scholar]
- Kane J.B., Harris K.M., Morgan S.P., Guilkey D.K. Pathways of health and human capital from adolescence into young adulthood. Social Forces. 2017;96(3):949–976. doi: 10.1093/sf/sox079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lariscy J.T., Hummer R.A., Hayward M.D. Hispanic older adult mortality in the United States: New estimates and an assessment of factors shaping the Hispanic paradox. Demography. 2015;52(1):1–14. doi: 10.1007/s13524-014-0357-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence E.M., Hummer R.A., Domingue B.W., Harris K.M. Wide educational disparities in young adult cardiovascular health. SSM-population health. 2018;5:249–256. doi: 10.1016/j.ssmph.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee D.B., Peckins M.K., Heinze J.E., Miller A.L., Assari S., Zimmerman M.A. Psychological pathways from racial discrimination to cortisol in African American males and females. Journal of Behavioral Medicine. 2018;41(2):208–220. doi: 10.1007/s10865-017-9887-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis T.T., Williams D.R., Tamene M., Clark C.R. Self-reported experiences of discrimination and cardiovascular disease. Current cardiovascular risk reports. 2014;8(1):365. doi: 10.1007/s12170-013-0365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B.G., Phelan J.C. Understanding sociodemographic differences in health--the role of fundamental social causes. American Journal of Public Health. 1996;86(4):471–473. doi: 10.2105/ajph.86.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long J.S., Mustillo S.A. Using predictions and marginal effects to compare groups in regression models for binary outcomes. Sociological Methods & Research. 2018 [Google Scholar]
- Masters R.K., Link B.G., Phelan J.C. Trends in education gradients of ‘preventable’mortality: A test of fundamental cause theory. Social Science & Medicine. 2015;127:19–28. doi: 10.1016/j.socscimed.2014.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta N.K., Abrams L.R., Myrskylä M. US life expectancy stalls due to cardiovascular disease, not drug deaths. Proceedings of the National Academy of Sciences. 2020;117(13):6998–7000. doi: 10.1073/pnas.1920391117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezuk B., Kershaw K.N., Hudson D., Lim K.A., Ratliff S. Job strain, workplace discrimination, and hypertension among older workers: The Health and Retirement Study. Race and Social Problems. 2011;3(1):38. doi: 10.1007/s12552-011-9041-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miura K., Daviglus M.L., Dyer A.R., Liu K., Garside D.B., Stamler J. Relationship of blood pressure to 25-year mortality due to coronary heart disease, cardiovascular diseases, and all causes in young adult men: The Chicago heart association detection project in industry. Archives of Internal Medicine. 2001;161(12):1501–1508. doi: 10.1001/archinte.161.12.1501. [DOI] [PubMed] [Google Scholar]
- Montez J.K., Friedman E.M. 2015. Educational attainment and adult health: Under what conditions is the association causal? [DOI] [PubMed] [Google Scholar]
- Montez J.K., Hayward M.D. Cumulative childhood adversity, educational attainment, and active life expectancy among US adults. Demography. 2014;51(2):413–435. doi: 10.1007/s13524-013-0261-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullings L. Resistance and resilience: The sojourner syndrome and the social context of reproduction in Central Harlem. Transforming Anthropology. 2005;13(2):79. [Google Scholar]
- National Research Council, and Committee on Population . National Academies Press; 2013. US health in international perspective: Shorter lives, poorer health. [PubMed] [Google Scholar]
- Nguyen Q.C., Tabor J.W., Entzel P.P., Lau Y., Suchindran C., Hussey J.M. Discordance in national estimates of hypertension among young adults. Epidemiology. 2011;22(4):532. doi: 10.1097/EDE.0b013e31821c79d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson J.A. Can't buy me whiteness: New lessons from the Titanic on race, ethnicity, and health. Du Bois Review: Social Science Research on Race. 2008;5(1):27–47. [Google Scholar]
- Pearson T.A., Mensah G.A., Alexander R.W., Anderson J.L., Cannon R.O., III, Criqui M.…Myers G.L. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the Centers for disease control and prevention and the American heart association. Circulation. 2003;107(3):499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- Read J.n.G., Gorman B.K. Gender and health inequality. Annual Review of Sociology. 2010;36:371–386. [Google Scholar]
- Rogers R.G., Lawrence E.M., Hummer R.A., Tilstra A.M. Racial/ethnic differences in early-life mortality in the United States. Biodemography and Social Biology. 2017;63(3):189–205. doi: 10.1080/19485565.2017.1281100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross C.E., Masters R.K., Hummer R.A. Education and the gender gaps in health and mortality. Demography. 2012;49(4):1157–1183. doi: 10.1007/s13524-012-0130-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross C.E., Mirowsky J. Sex differences in the effect of education on depression: Resource multiplication or resource substitution? Social Science & Medicine. 2006;63(5):1400–1413. doi: 10.1016/j.socscimed.2006.03.013. [DOI] [PubMed] [Google Scholar]
- Ross C.E., Mirowsky J. Gender and the health benefits of education. The Sociological Quarterly. 2010;51(1):1–19. doi: 10.1111/j.1533-8525.2009.01164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith W.C., Anderson E., Salinas D., Horvatek R., Baker D.P. A meta-analysis of education effects on chronic disease: The causal dynamics of the Population Education Transition Curve. Social Science & Medicine. 2015;127:29–40. doi: 10.1016/j.socscimed.2014.10.027. [DOI] [PubMed] [Google Scholar]
- Sundström J., Neovius M., Tynelius P., Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: Cohort study of Swedish male conscripts. BMJ. 2011;342:d643. doi: 10.1136/bmj.d643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanton S.L., Rifkind J.M., Mohanty J.G., Miller E.R., Thorpe R.J., Nagababu E. Racial discrimination is associated with a measure of red blood cell oxidative stress: A potential pathway for racial health disparities. International Journal of Behavioral Medicine. 2012;19(4):489–495. doi: 10.1007/s12529-011-9188-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomiyama A.J., Hunger J.M., Nguyen-Cuu J., Wells C. Misclassification of cardiometabolic health when using body mass index categories in NHANES 2005–2012. International Journal of Obesity. 2016;40(5):883. doi: 10.1038/ijo.2016.17. [DOI] [PubMed] [Google Scholar]
- Walsemann K.M., Goosby B.J., Farr D. Life course SES and cardiovascular risk: Heterogeneity across race/ethnicity and gender. Social Science & Medicine. 2016;152:147–155. doi: 10.1016/j.socscimed.2016.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildman R.P., Muntner P., Reynolds K., McGinn A.P., Rajpathak S., Wylie-Rosett J. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: Prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004) Archives of Internal Medicine. 2008;168(15):1617–1624. doi: 10.1001/archinte.168.15.1617. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Priest N., Anderson N.B. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychology. 2016;35(4):407. doi: 10.1037/hea0000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y.C., Gerken K., Schorpp K., Boen C., Harris K.M. 2017. Early-life socioeconomic status and adult physiological functioning: A life course examination of biosocial mechanisms. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova A. Education, gender, and mortality: Does schooling have the same effect on mortality for men and women in the US? Social Science & Medicine. 2006;63(8):2176–2190. doi: 10.1016/j.socscimed.2006.04.031. [DOI] [PubMed] [Google Scholar]
- Zajacova A., Hummer R.A. Gender differences in education effects on all-cause mortality for white and black adults in the United States. Social Science & Medicine. 2009;69(4):529–537. doi: 10.1016/j.socscimed.2009.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova A., Lawrence E.M. The relationship between education and health: Reducing disparities through a contextual approach. Annual Review of Public Health. 2018;39:273–289. doi: 10.1146/annurev-publhealth-031816-044628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamora-Kapoor A., Hebert L.E., Montañez M., Buchwald D. Risk factors in adolescence for the development of elevated blood pressure and hypertension in American Indian and Alaskan native adults. Journal of Immigrant and Minority Health. 2020:1–8. doi: 10.1007/s10903-020-01130-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.