Abstract
The Saudi Initiative for Asthma 2021 (SINA-2021) is the fifth version of asthma guidelines for the diagnosis and management of asthma for adults and children, which is developed by the SINA group, a subsidiary of the Saudi Thoracic Society. The main objective of the SINA is to have guidelines that are up to date, simple to understand, and easy to use by healthcare workers dealing with asthma patients. To facilitate achieving the goals of asthma management, the SINA panel approach is mainly based on the assessment of symptom control and risk for both adults and children. The approach to asthma management is aligned for age groups: adults, adolescents, children aged 5–12 years, and children aged less than 5 years. SINA guidelines have focused more on personalized approaches reflecting better understanding of disease heterogeneity with the integration of recommendations related to biologic agents, evidence-based updates on treatment, and the role of immunotherapy in management. Medication appendix has also been updated with the addition of recent evidence, new indications for existing medication, and new medications. The guidelines are constructed based on the available evidence, local literature, and the current situation at national and regional levels. There is also an emphasis on patient–doctor partnership in the management that also includes a self-management plan.
Keywords: Asthma, asthma control test, guidelines, Saudi Arabia
Section 1: Introduction
Asthma is a chronic heterogeneous disease usually characterized by chronic airflow limitation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness, and cough that vary over time and in intensity, together with variable expiratory airflow limitation.[1] Asthma is one of the most common chronic diseases in Saudi Arabia, with an increasing prevalence in the past decades.[2] It has a significant impact on patients, their families, and the community as a whole in terms of lost work and school days, poor quality of life, frequent emergency department (ED) visits, hospitalizations, and deaths.[3,4,5] As part of its long-term commitment to promote best practice in the field of respiratory diseases, the Saudi Thoracic Society (STS) launched the Saudi Initiative for Asthma (SINA) group in 2008. The SINA panel is a group of Saudi experts with well-respected academic backgrounds and experience in the field of asthma. Sections related to asthma in children represent the views of a panel from the Saudi Pediatric Pulmonology Association, another subsidiary of the STS.
The SINA panel aims to have updated guidelines, which are simple to understand and easy to use. It also aims toward enhancing the multidisciplinary care of asthma patients with special attention to nonasthma specialists, including primary care and general practice physicians and other healthcare workers.[6,7,8,9] The updated 2021 version of SINA guidelines received a comprehensive update with an emphasis on personalized approaches reflecting a better understanding of disease heterogeneity with an integration of recommendations related to new medications, approved biologic agents, evidence-based updates on treatment, especially on mild asthma, and the role of immunotherapy in management. A special attention is made to managing asthma during the time of emerging acute respiratory infections, such as the recent coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The SINA panel stratified the guidelines based on the following age groups: adults: age above 18 years; adolescents: age of 13–18 years; and children who were stratified into two groups: age of 5–12 years and age below 5 years.[10]
Methods
The SINA guidelines document was initially based on the Global Initiative for Asthma (GINA) strategies with reference to related major international guidelines.[10] The SINA is supplemented by the available local literature and the current setting in Saudi Arabia. Consensus among the SINA panel was followed whenever there was lack of evidence.[11] The following criteria are used to grade the evidence:
Evidence Category A: Randomized controlled trials with rich body of data
Evidence Category B: Randomized controlled trials with limited body of data
Evidence Category C: Nonrandomized trials and observational studies
Evidence Category D: SINA panel consensus judgment. This category is only used in cases where the provision of some guidance was deemed valuable, but the clinical literature addressing the subject was insufficient to justify the placement in one of the other categories.
For this update, the similar approach to previous updates has been employed, whereby each section has been internally reviewed at least twice by the SINA panel members. The SINA panel conducted frequent round-table and virtual discussions. A panel of international experts reviewed the guidelines and their recommendations were thoughtfully considered.
Epidemiology
Asthma is one of the most common chronic illnesses in Saudi Arabia, and local reports suggest that the prevalence of asthma is increasing.[3,12,13] Inadequate knowledge, unfamiliarity with new drugs, and lack of awareness of the importance of disease control are common among primary care physicians who care for asthma patients in Saudi Arabia.[14,15] In addition to these key factors, there are other attributes to the magnitude of disease burden such as socioeconomic status, number of siblings, knowledge of caregivers, and income.[16,17,18,19] Consequently, many asthma patients are uncontrolled and continue to be under-diagnosed, under-treated, and at risk of acute attacks, resulting in missed work or school, increased use of expensive acute healthcare services, and reduced quality of life.[12,20] This was also observed among pregnant women with asthma as one study from Saudi Arabia showed that almost half of pregnant women had the intention to stop asthma medications during pregnancy.[21]
A meta-analysis on the prevalence of asthma in different regions in Saudi Arabia showed a rise in the prevalence from 1990 to 2000, with stabilization in the prevalence of asthma since 2000.[3] The pooled weighted prevalence rate of asthma was 14.3%, lifetime wheeze was 16.5%, and rhinitis was 21.4%. The prevalence of asthma varied in different regions without any disparity in prevalence in the rural and urban areas of Saudi Arabia.[3] The overall prevalence of asthma in children from Saudi Arabia has been reported to range from 8% to 25%, based on studies conducted over the past three decades. The increasing prevalence of asthma in the past three decades may be attributed to rapid lifestyle changes related to the modernization of Saudi society, changes in dietary habits, and exposure to environmental factors, such as indoor allergens, dust, sandstorms, and tobacco. In addition, this high prevalence of asthma could be attributed to an increase in asthma awareness in the general population and among healthcare workers, allowing more individuals to be diagnosed. Other explanations have attributed the increased prevalence to the hygiene hypothesis, which proposes that there is a lack of sufficient microbial exposure early in life due to pharmacological manipulations and vaccines.[22,23]
Most of the studies investigating the prevalence of asthma in various countries have focused on children aged below 15 years or adults aged above 18 years. A study conducted by the STS investigated the prevalence of asthma and its associated symptoms in 16–18-year-old adolescents attending high schools in Riyadh.[24] This study utilized the International Study of Asthma and Allergies in Children (ISAAC) questionnaire tool. Out of 3073 students, the prevalence of lifetime wheeze, wheeze during the past 12 months, and physician-diagnosed asthma was 25.3%, 18.5%, and 19.6%, respectively. The prevalence of exercise-induced wheezing and night coughing in the previous 12 months was 20.2% and 25.7%, respectively. The prevalence of rhinitis symptoms in students with lifetime wheeze, physician-diagnosed asthma, and exercise-induced wheeze was 61.1%, 59.9%, and 57.4%, respectively. Rhinitis symptoms were significantly associated with lifetime wheeze, physician-diagnosed asthma, and exercise-induced wheeze. By utilizing the ISAAC questionnaire method, another study conducted among 5188 primary schoolchildren in Madinah showed that the prevalence of asthma was 23.6%, while 41.7% had symptoms suggestive of at least one allergic disorder.[25] A national Saudi household survey conducted in 2013 estimated the self-reported clinical diagnosis of asthma to be 4.05%.[26] Another survey using the European Community Respiratory Health Survey questionnaire, conducted in Riyadh among a total of 2405 Saudi nationals aged 20–44 years, showed that the prevalence of wheezing in the last 12 months was 18.2% and physician-diagnosed asthma reported was 11.3%. There were no significant differences between asthmatic and nonasthmatic patients, with respect to living area, level of education, and vaping history.[2]
Among a group of university students in Najran, a report revealed that the overall prevalence of physician-diagnosed allergic diseases was 27% for asthma, 13.1% for atopic dermatitis, and 5% for allergic rhinitis.[27] The prevalence of physician-diagnosed asthma among school students in Jazan, Najran, Taif, and Madinah was 10%, 27%, 13%, and 23%, respectively.[28] A cross-sectional study conducted in adult patients with asthma who attended primary care clinics at three major hospitals in Riyadh reported that 58.9% of men and 77.0% of women had uncontrolled asthma. Factors associated with uncontrolled asthma were stress, smoking, obesity, and low socioeconomic status.[29] In the Epidemiological Study on the Management of Asthma in Asthmatic Middle East Adult population, 1009 patients from Saudi Arabia were analyzed and found that 30.1% have controlled asthma. Controlled asthma was more prevalent among male patients and those with high educational level, while age, body mass index, and adherence to treatment were found to have no effect on asthma control.[30]
Data regarding the relationship between asthma and SARS-CoV-2 are limited, and most of the current knowledge was derived from studies addressing the outcomes of multiple medical conditions, including asthma on patients with COVID-19. The most frequent trigger factor of asthma exacerbation is airway infections, particularly viral infection. However, interestingly, SARS-CoV-2 infection does not increase the risk of asthma exacerbations or mortality. Several studies including several thousand patients from different countries found that the comorbidity rates of COVID-19 with asthma were significantly low. In a review of 1265 consecutive patients, the prevalence of asthma was found to be 12.6%. When compared with nonasthmatics, COVID-19 did not lead to a significant impact on length of stay, hospital readmission, intubation, tracheostomy tube placement, or mortality.[31] Older adults with underlying chronic medical conditions such as hypertension, diabetes, cardiovascular diseases, obesity, chronic obstructive pulmonary disease (COPD), but not asthma are at a higher risk of severe COVID-19 and death.[32,33,34,35] In spite of this, the SINA panel emphasizes that physicians should not underestimate COVID-19 in asthma patients. Asthma medications should continue the same and the physicians should follow the usual step approach management of asthma. It is worth to notice that the knowledge regarding COVID-19 is rapidly growing, and by the time of publishing these guidelines, maybe new data will be published in regard to the interaction between asthma and SARS-CoV-2, we highly encourage the reader to keep updated to the most recent data.
Section 2: Pathophysiology of Asthma
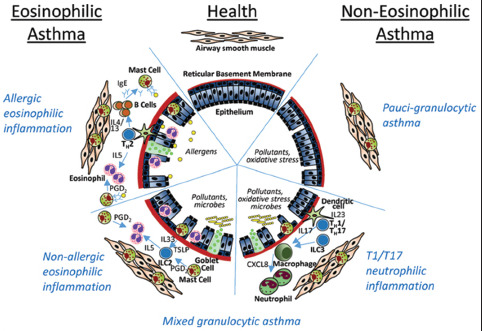
Asthma is a chronic inflammatory airway disease that results in narrow airway lumen. The airway narrowing is caused by increased mucus secretion as well as bronchial wall thickening due to edema, smooth muscle hypertrophy, and subepithelial fibrosis. The pathophysiological mechanisms that underlie these changes are diverse and heterogeneous [Box 2.1]. They are driven by a variety of cell types including immune cells; mainly T-helper cells (Th2, Th17, Th1), B-cells, mast cells, eosinophils, dendritic cells, and neutrophils; as well as structural bronchial cells such as epithelial cells, myofibroblasts, and smooth muscle cells.[36] These mechanisms can be broadly classified into four categories (endotypes). Other classifications exist, but this classification is more pertinent to severe asthma and therefore has special implications on biological therapy.
Box 2.1.
Immunopathology of asthma
Type 2-high (eosinophilic) asthma
This is the most common type and includes 40%–70% of asthma patients. It is defined by sputum eosinophilia of ≥2% of leukocytes in a sample. Patients frequently have blood eosinophilia of ≥150/μL and FeNO ≥20 ppb. This eosinophils' cutoff is way below the lower normal peripheral eosinophil count. This is because patients with severe asthma are already on high-dose inhaled corticosteroids (ICSs) or maintenance systemic oral corticosteroid (OCS). Eosinophils secrete mediators such as major basic protein and eosinophil cationic protein that can cause bronchial epithelial damage and subepithelial fibrosis. Those patients usually respond well to ICSs, especially if they have mild or moderate disease. It is further subdivided into two types:
Early-onset allergic eosinophilic airway inflammation (extrinsic asthma) type usually starts in childhood and can be triggered by allergen exposure. Allergens are taken up by dendritic cells and presented to naïve T-cells that develop into Th2 cells characterized by the secretion of type 2 cytokines: interleukin (IL)-4, 5, and 13. IL-4 and 13 are necessary for specific B-cell activation and switching into immunoglobulin (Ig) E-producing cells. IgE binds to its high affinity receptor on mast cells. Subsequent cross-linking of IgE molecules by the allergen will lead to mast cell degranulation and release of mediators, such as histamine and tryptase as well as type 2 cytokines. In addition, IL-13 causes smooth muscle and goblet cell hyperplasia. On the other hand, IL-5 is essential for eosinophil maturation and survival and contributes with certain other chemokines to their recruitment to the bronchial airways.[37,38] Symptoms could also be triggered by similar triggers of the nonallergic type (see below)
Late-onset nonallergic eosinophilic airway inflammation (intrinsic asthma) type usually starts during adulthood. Patients typically have no allergies but usually more severe airway limitation and airway hyperresponsiveness (AHR). It is triggered by microbes (bacteria and viruses), pollutants, and irritants. Bronchial epithelial cells will subsequently release IL-25, IL-33, and thymic stromal lymphopoietin (TSLP) that will stimulate innate lymphoid cells type 2 to release IL-5 and IL-13.[39]
Type 2-low (noneosinophilic) asthma
This can further be subdivided into two types:
Neutrophilic inflammation is variably defined as neutrophils of ≥40%–60% of leukocytes in an induced sputum sample. It is less clearly characterized and involves release of Th1- and Th17-related cytokines and IL-8, GM-CSF that attracts neutrophils to the airways. It is triggered by infections, irritants, and tobacco smoke and may be a manifestation of the use of steroids in patients with eosinophilic inflammation. Those patients are mostly adults and do not respond to ICSs as well[40]
Paucigranulocytic inflammation is not as much inflammation. The airway limitation is supposedly driven by other mechanisms. It is the least common and patients usually have milder disease.[41]
Mixed type 2-high and type 2-low (granulocytic) asthma
This type has features of both eosinophilic and neutrophilic inflammation including their cytokine profile. It is less common than the two previous main types and tends to be more severe and more difficult to treat.[42]
Airway hyperresponsiveness
AHR is a major feature of all asthma endotypes. Its mechanisms and mediators are poorly understood. It worsens during and immediately after asthma attacks. It is usually worse in patients with severe asthma. However, it does not correlate well with markers of inflammation. Smooth muscle hypertrophy and neurohumoral factors may play a role in determining AHR.[43]
Airway remodeling
This is a major feature of asthma that starts early in the disease process and causes incomplete reversibility by bronchodilators. It is characterized by bronchial epithelial damage, thickening of the basement membrane, and muscle hypertrophy.[44,45] It is influenced by the ongoing airway inflammation and recurrent bronchoconstriction.[46]
Pathophysiology of acute asthma
The pathophysiology of acute asthma is less clear due to limited information. This is because of the difficulty in studying disease pathology and obtaining samples during exacerbations. The pathological manifestations generally depend on the trigger. At least 80% of cases of moderate-to-severe acute asthma are triggered by viruses, most commonly rhinovirus but also respiratory syncytial and influenza viruses.[47] Viral infections can cause significant epithelial damage and symptoms tend to be more severe and last longer. On the other hand, allergen- or irritant-triggered attacks tend to be milder and resolve more quickly. Recurrent attacks may lead to progressive decline in lung function and increasing baseline asthma severity.[48,49,50]
Section 3: Diagnosis of Asthma in Adults and Adolescents
The diagnosis of asthma is based on clinical assessment by a detailed history and physical examination supported by spirometry with reversibility testing.
History
The symptoms of asthma are wheezing, cough, shortness of breath, and chest tightness, but they are not specific for asthma and can be seen with other pulmonary diseases. However, the combination of these symptoms increases the probability of asthma. The pattern of symptoms is usually variable over time, and the patient may be entirely asymptomatic between attacks.[51,52] Symptoms are usually worse at night, particularly in children, and can be provoked by exercise or other triggering factors such as viral infections and/or smoke. Asthma diagnosis can be supported by taking detailed history including patient's occupation, family history of asthma, other allergic disorders, and smoking and vaping. [Box 3.1] lists the relevant questions that are commonly considered when taking a history where the diagnosis of asthma is under consideration. Asthma control may be worsened by coexisting symptomatic gastroesophageal reflux disease (GERD), rhinosinusitis, obesity, sleep disorders, or the use of some medications such as beta-blockers and nonsteroidal anti-inflammatory drugs (NSAIDs) including aspirin (ASA).[53,54] Asthma and rhinosinusitis commonly coexist.[55,56]
Box 3.1.
Relevant questions in the diagnosis of asthma
| Does the patient or his/her family have a history of asthma or other atopic conditions, such as eczema or allergic rhinitis? |
| Does the patient have recurrent attacks of wheezing? |
| Does the patient have a troublesome cough at night? |
| Does the patient wheeze or cough after exercise? |
| Does the patient experience wheezing, chest tightness, or cough after exposure to pollens, dust, feathered or furry animals, exercise, viral infection, or environmental smoke (cigarettes, burning incense “Bukhoor,” or wood)? |
| Does the patient experience worsening of symptoms after taking aspirin/nonsteroidal anti-inflammatory medication or use of B-blockers? |
| Does the patient’s cold “go to the chest” or take more than 10 days to clear up? |
| Are symptoms improved by appropriate asthma treatment? |
| Are there any features suggestive of occupational asthma? |
Physical examination
The physical examination of the chest may be normal in stable and controlled asthma, but the presence of bilateral expiratory widespread, high-pitched, variable musical wheezing is a characteristic feature of asthma. This may be accompanied by shortness of breath or diminished oxygen saturation. Examination of the upper airways is important to look for evidence of allergic rhinitis, such as nasal mucosal swelling, nasal polyps, and postnasal dripping. Other allergic manifestations, such as atopic dermatitis, also support the diagnosis of allergic asthma.[51,57] The presence of a localized wheeze, crackles, stridor, clubbing, or heart murmurs should suggest alternative diagnoses.[58,59] Therefore, a careful consideration of any alternative diagnoses before commencing asthma treatment by a physician should be made.
Investigations
Spirometry is necessary to confirm airflow obstruction and demonstrates a significant reversibility by performing a spirometry. The degree of significant reversibility is defined as an improvement in FEV1 ≥12% and ≥200 mL from the prebronchodilator value.[60] It may also help to identify other alternative diagnoses such as upper airway obstruction. However, normal spirometry or failure to show reversibility does not rule out the diagnosis of asthma as it can be normal with the patient still being symptomatic.[61,62] Serial peak expiratory flow (PEF) rate measurements may be helpful in the diagnosis of asthma by showing the characteristic increased variability and for follow-up after starting treatment. Bronchoprovocation testing is another tool to rule out asthma with atypical presentation and normal spirometry, but it is not routinely required. A diagnostic therapeutic trial with an ICS and a bronchodilator combination may be useful in confirming a diagnosis when it shows a favorable response.[62]
Chest X-ray (CXR) is not routinely recommended unless the diagnosis is in doubt, when symptoms are not typical or suggest alternative diagnoses. Peripheral eosinophilia and elevated IgE level are supportive of the diagnosis but are not routinely recommended unless dealing with moderate-to-severe asthma. Exhaled nitric oxide is an alternative method for detecting airway inflammation in eosinophilic asthma, but it is not widely available and can be suppressed with the use of ICSs in smokers.[63] Skin prick testing and radioallergosorbent test (RAST) may be helpful in identifying allergens to which the patient has been sensitized and in developing a strategy for avoiding allergen exposure.[64]
Section 4: Clinical Assessment in Adults and Adolescents
Principles of asthma assessment
The principles of optimal asthma management is recommended to initially consist of an assessment of asthma control.[65] Before commencing a patient on treatment, the SINA panel recommends ensuring the following:
Assessment of asthma control
Assessment of risk factors for poor asthma control and fixed airway obstruction
Performance of pulmonary function testing with spirometry and/or PEF to assess for airflow limitations and postbronchodilator reversibility
Documentation of current treatment and any issues related to adherence, inhaler technique, or side effects
Utilization of a written asthma action plan
Assessment of comorbidities such as rhinosinusitis, GERD, obesity, obstructive sleep apnea, anxiety, and exercise-induced laryngeal obstruction[66]
Close monitoring for patients with severe asthma and history of asthma attacks.
Assessment of asthma symptoms control
In adults and adolescents, asthma control is based on assessing asthma symptoms, use of reliever medications, and impact on daily activities. Asthma control reflects the adequacy of management by describing the clinical status of a patient as controlled, partly controlled, or uncontrolled over the past 4 weeks. The control status may vary markedly over time and is recommended to entail frequent assessment of current asthma status, asthma burden, and medical management.[67] Focusing on asthma control may improve patient perceptions and expectations that improve symptoms reporting and subsequently treatment decisions by clinicians.[68] Poor asthma control is associated with increased burden of the disease, asthma attacks, and mortality.[69] Therefore, symptoms control assessment should be carried out during any clinical evaluation. The SINA panel recommends the utilization of either the GINA assessment of asthma symptoms' control or the asthma control test (ACT).
Global Initiative for Asthma assessment of asthma symptoms' control
It is a short questionnaire utilized to assess asthma control over the past 4 weeks [Box 4.1].[1,70] It consists of four items: (1) daytime symptoms more than twice a week, (2) any night waking due to asthma, (3) reliever needed for symptoms more than twice a week, and (4) any activity limitation due to asthma.[1] Control status is classified as follows:
Box 4.1.
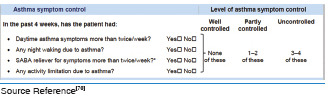
Global Initiative for Asthma assessment of asthma control in adults and adolescents
Controlled: None of the items is present
Partly controlled: 1–2 items are present
Uncontrolled: 3–4 items are present.
Asthma control test
The ACT is a commonly used tool to assess asthma control which is correlated with the GINA asthma symptoms assessment.[71,72] It is a short, validated, self-administered questionnaire to assess asthma control in the past 4 weeks [Box 4.2].[73,74] It consists of five items including limitation of activity, shortness of breath, frequency of night symptoms, use of rescue medication, and rating of overall control of the disease over the past 4 weeks.[74] The score of ACT is the sum of the five questions where each is scored from 1 (worst) to 5 (best), leading to a maximum best score of 25. The SINA panel recommends the utilization of ACT to initiate asthma treatment in adults and adjust it at follow-up.[75,76,77] The clinically important a significant change in ACT score is considered to be ≥3 units.[78] The level of asthma control is categorized into:
Box 4.2.
Asthma control test74
Controlled: An ACT score of ≥20
Partly controlled: An ACT score of 16–19
Uncontrolled: An ACT score of <16
Assessment of risk factors for future asthma attacks
The future risk of adverse outcomes should be assessed. This is achieved by assessing future risk of attacks, fixed airflow obstruction, and adverse effect of medications.[1] The SINA panel recommends the assessment of risk factors for poor asthma outcomes, especially in patients experiencing attacks by assessing risk factors for:
Independent risk factors for acute severe asthma attacks in the past 12 months or prior history of admission to an intensive care unit (ICU), especially if intubated[79,80]
Other modifiable risk factors are recommended to be addressed, such as high usage of relievers, frequent use of OCS, low forced expiratory volume in the 1st s (FEV1), pregnancy, inadequate ICS, smoking and vaping, comorbidities, major psychological disorders, reduced socioeconomic status, and presence of comorbidities
Risk factors for fixed airway obstruction including inadequate ICS treatment, exposure to tobacco smoke or other noxious substances, low initial FEV1, or sputum/blood eosinophilia.[81]
Asthma severity assessment in clinical practice
There is a trend in clinical practice to retrospectively assess asthma severity based on the step of treatment required to control symptoms and attacks.[10,81,82,83] Before classifying asthma severity, it is essential to ensure that control is achieved and maintained while using the minimal level of medications over a few months.[1] Since asthma severity level could change over years or months, asthma level of severity can be classified as follows:
Mild asthma: Controlled asthma at step 1 or 2
Moderate asthma: Controlled asthma at step 3
Severe asthma: Asthma that requires treatment step 4 or 5.
Assessment when control is not achieved
If asthma control is not achieved at any step during therapy, the SINA panel recommends assessing the following:
Appropriateness of prescribed medications and doses
Patient's adherence and correct technique in using devices
Selection of the appropriate device and appropriate spacer with pressurized metered-dose inhaler (pMDI) device
Obstacles in taking prescribed medications (e.g., cost, time, and patients' concerns on lack of perceived need)
Environmental exposure to allergens at home
Assessment of comorbidities such as rhinosinusitis, GERD, obesity, obstructive sleep apnea, and anxiety
Future risk of attacks and fixed airflow obstruction.
Section 5: Nonpharmacological Management
The long-term goal of asthma therapy is to achieve and maintain asthma control by utilizing pharmacological and nonpharmacological measures [Box 5.1]. The appropriate implementation of nonpharmacological measures also aims to use the least possible doses of asthma medications to minimize their side effects.
Box 5.1.
Long-term goals of asthma management
| Control asthma symptoms (cough, wheezing, and shortness of breath) |
| Infrequent and minimal use (≤2 days a week) of the reliever therapy |
| Maintain (near) normal pulmonary function |
| Maintain normal level of exercise and physical activity |
| Prevent asthma attacks and minimize the need for emergency department visits or hospitalizations |
| Optimize asthma control with the lowest possible dose of medications |
| Improve quality of life and reduce the risk of adverse outcomes |
| Reduce mortality |
Developing a partnership with the patient
The development of a partnership between patients and healthcare professionals leads to the enhancement of knowledge, skills, and attitude toward a better understanding of asthma and its management. Based on agreed goals of management, a written self-management action plan should be offered to all patients. A wide variety of plans are available. This is expected to reflect positively on patient adherence, which is a major issue in the management. Factors leading to nonadherence may be related to poor inhaler technique, a regimen with multiple drugs or devices, concern regarding side effects from the drugs, and cost of medications.[84,85,86,87] Other factors include lack of knowledge about asthma, lack of partnership in its management, inappropriate expectations, underestimation of asthma symptoms, use of unconventional therapy, and cultural issues.[30,88]
Asthma education
The goal of asthma education is to provide patients with adequate training to enhance their knowledge and skills to be able to adjust treatment, according to guided self-management plan.[89,90,91,92] To enhance the level of knowledge and skills among asthma patients, it is recommended to include knowledge about asthma and skills related to prescribed inhaler devices, as there may be misperceptions about the use of inhalers and the safety of ICSs [Box 5.2].[93,94,95,96] Asthma education should be conducted by a well-trained healthcare worker, who has good communication skills and is able to create an interactive dialog in a friendly environment. With the availability of appropriate information, patients are expected to continue on the management plan and be reassured about the control of their asthma.[97] It is essential to get feedback from the patient to maintain a bidirectional rapport. Reproducible evidence has shown that a well-structured asthma education program improves the quality of life, reduces cost, and decreases the utilization of healthcare resources.[98,99,100] Asthma should be structured based on available resources.
Box 5.2.
Outcomes of asthma education program
| Creation of patient-healthcare worker partnership |
| Understanding of clinical presentation of asthma and methods of diagnosis |
| Ability to differentiate between “reliever” and “controller” medications and their appropriate indications |
| Recognition of potential side effects of medications and the appropriate action to minimize them |
| The ability to use inhaler devices correctly |
| Identification of symptoms and signs that suggest worsening of asthma control and the appropriate action to be taken |
| Understanding the approach for monitoring asthma control |
| Recognition of the situations that need urgent medical attention |
| Ability to use a written self-management plan |
Identify and reduce exposure to risk factors
Measures to prevent or reduce exposures to risk factors should be implemented wherever possible. There are different triggers leading to acute asthma attacks, which may include allergens, viral infections, pollutants, drugs, and occupational agents. These factors can be classified as indoor or outdoor allergens and occupational sensitizers.
Indoor allergens and air pollutants
There is a wide spectrum of indoor allergens that include dust mites, animals (mainly cats), cockroaches, and fungi (e.g., Alternaria and Aspergillus). Single-allergen interventions are likely to fail. However, multifaceted, tailored, and intensive interventions may help in improving asthma control. There are still several gaps in the literature in this area. It may take a few months for the allergen level to become significantly lower from the implementation of the related control measures.[101] The most important indoor air pollutant is related to tobacco exposure. Measures to avoid tobacco exposure are expected to lead to better asthma control and avoidance of long-term lung function impairment.
Outdoor allergens and dust
Outdoor allergens such as pollens and molds are impossible to avoid completely; however, exposure may be reduced by closing windows and doors and using air conditioning. It is recommended to avoid strenuous outdoor physical activities in cold weather, low humidity, or high air pollution. In a single-center study in Saudi Arabia, sandstorms were shown to worsen asthma symptoms but not hospital admission in children with asthma. It is advisable to avoid going out in the storm, especially for those with uncontrolled asthma.[102]
Occupational exposures
Whenever an occupational sensitizer is identified, it is advisable to keep the affected person away from that environment. The earlier the removal of this sensitizer takes place, the higher the chance of complete recovery from occupational asthma (See Asthma in Special Situation).
Food and drugs
Food and food additives are uncommon triggers of asthma. Avoidance is not generally recommended until it is documented by a specialist. However, certain drugs that could worsen asthma symptoms should be avoided (e.g., beta-blockers), whenever possible.
Vaccination
Annual influenza vaccination is strongly recommended for individuals with asthma, especially those with severe asthma.[103,104,105] It usually becomes available early on the fall season. Pneumococcal vaccination is also recommended as per the local guidelines.[106]
Section 6: Pharmacological Management in Adults and Adolescents
The SINA panel recommends asthma treatment to be based on the following phases:
Initiation of treatment
Adjustment of treatment
Maintenance of treatment.
At each phase, the patient is recommended to have a clinical assessment that includes symptoms assessment by ACT, a physiological measurement with PEF or spirometry, review of current medications and patients' adherence and inhaler technique, a risk for attacks, and the response to treatment. Based on the clinical and physiological assessment, the patient is placed on the appropriate treatment step. Medication Appendix contains more information about medications used in asthma treatment. The SINA panel recommends the following strategies for asthma treatment:
A controller medication is recommended for all steps. ICS is considered the most effective controller and the cornerstone of asthma treatment (Evidence A).[107,108] Uncontrolled patients may require the addition of other controllers
-
Reliever medications must be available to patients at all steps. Increasing the use of reliever treatment should be considered as an early sign of worsening of asthma control (Evidence A).[109] The available relievers are as follows:
- A short-acting bronchodilator (SABA), such as salbutamol, is recommended to be taken as needed to relieve symptoms. Using SABA alone was found to increase the risk of asthma attacks and asthma-related death; therefore, asthma patients are not recommended to use it without being on a controller treatment; alternatively, ICS is recommended to be used whenever SABA is needed in Step 1[110,111]
Formoterol/ICS combination could be used as a reliever therapy on “as-needed basis” as per physician prescription. Formoterol is a long-acting bronchodilator (LABA) with fast-acting bronchodilator effect (Evidence A).[112,113,114] For Steps 3–5, it is only recommended when the combination of formoterol/ICS is prescribed as maintenance therapy. The maximum recommended dose of formoterol component is 72 mcg. Exceeding this level for 2–3 days may be a warning sign of deterioration of asthma control.[113,114,115]
Regular assessment of adequate doses of treatment, proper technique, and adherence
Regular assessment of independent risk factors for acute asthma attacks in the past 12 months or prior history of admission to an ICU, especially if intubated.[79,116] Other modifiable risk factors are recommended to be addressed, such as low initial FEV1, pregnancy, inadequate ICS, smoking and vaping, comorbidities, and major psychological conditions
-
Regular assessment of risk factors for fixed airway obstruction that includes inadequate ICS treatment, exposure to tobacco smoke or other noxious substances, low initial FEV1, or sputum/blood eosinophilia[117]
- Management of comorbidities with special attention to concomitant rhinosinusitis. As this condition affects asthma control, its treatment is expected to improve asthma outcome (Evidence A).[118,119,120] Treatment includes nasal saline washes, nasal steroids, leukotriene receptor antagonists (LTRAs), and antihistamines. Concomitant rhinosinusitis is recommended to be treated appropriately as well.
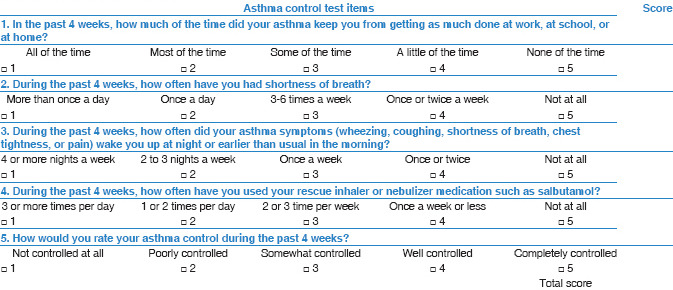
Initiation of treatment
Patients with asthma often underestimate the presence of symptoms and tend to assume that their asthma is controlled even when this is not the case. Therefore, the consensus among the SINA panel is to simplify the approach and supplement the initiation of asthma therapy by utilizing an objective measurement with the ACT questionnaire [Box 4.2].[77] The following initial steps are recommended for treatment-naïve patients based on the ACT score [Box 6.1]:
Box 6.1.
Initiation of asthma treatment for adults and adolescents
-
ACT score ≥20 (controlled status)
- Maintenance daily low-dose ICS is recommended in special situations:
- For patients with symptoms more than twice a week and risk factors for acute attack (severe attacks in the past 12 months or prior history of admission to an ICU, especially if intubated) or evidence of fixed airway obstruction (Evidence B).[117,120,123] Early introduction of ICS leads to greater improvement of FEV1 and lower the future doses of ICS.[123]
-
ACT score 16–19 (partially controlled status)
- Low-dose ICS for patients with an ACT score of 16–19 (Evidence A).[77] Alternative options may be considered as described in the Adjustment Section below, which includes starting formoterol/ICS combination on as-needed basis or LTRA.
-
ACT score <16 (uncontrolled status)
- A combination of regular low-dose ICS and LABA as maintenance treatment for patients with an ACT score of <16.(Evidence B)[77]
- For patients who have poorly uncontrolled asthma at presentation, initiation of asthma treatment with a combination of medium-dose ICS and LABA as a maintenance treatment such as those with aforementioned risk factors (Evidence D)
- For patients with early signs of attack at presentation, it is recommended to prescribe medium-dose ICS and LABA and consider a short course of oral steroids.[124]
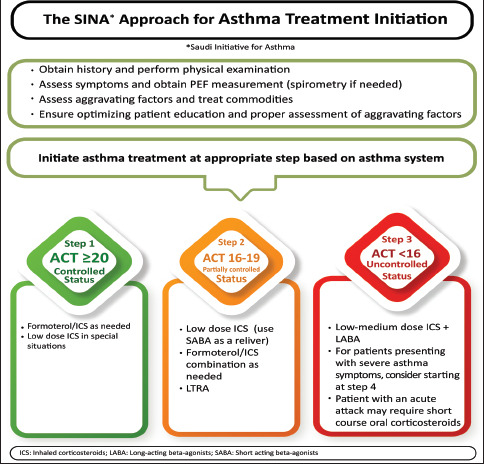
Adjustment of treatment
After initiation of asthma treatment, it is recommended to assess the patient at 1–3 months' intervals (Evidence D).[125] The SINA panel recommends the utilization of stepwise approach of therapy to achieve asthma control. The stepwise approach consists of five steps as shown in [Box 6.2]. The SINA panel recommends that the stepwise approach is not meant to be compartmental; it is rather a continuum of care based on patient engagement and close monitoring of the disease (Evidence D).[126] In clinical practice, asthma severity can be retrospectively assessed based on the step of treatment required to control symptoms:[10,81,82,83]
Box 6.2.
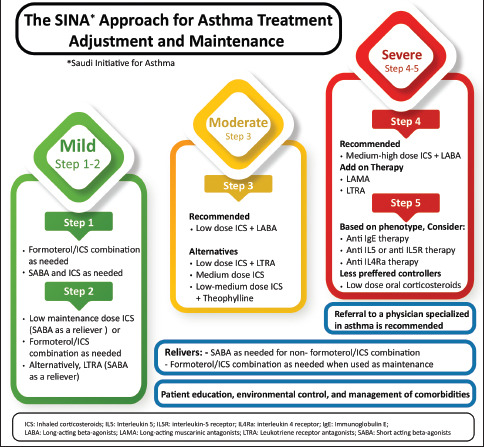
Outpatient asthma treatment for adults and adolescents
Mild asthma: controlled asthma at step 1 or 2
Moderate asthma: controlled asthma at step 3
Severe asthma: Requires asthma management at step 4 or 5.
Reliever medications must be made available to patients at all steps. Increasing the use of reliever treatment is usually an early sign of asthma worsening (Evidence A).[109,127] Approximately one in five patients with mild asthma may develop at least one attack of severe asthma in 12 months.[114,128,129] The available relievers are detailed above. The following paragraphs describe the asthma treatment at each step.
Treatment at step 1
Recommended option: Anti-inflammatory reliever therapy in the form of ICS/formoterol on as-needed basis (Evidence A).[114,115,121] Symptoms are usually mild and infrequent (usually < twice a month) with an ACT score of ≥20 and no risk factors for asthma attacks
Alternative option: Use SABA together with low-dose ICS both on as-needed basis (Evidence B)[110,111,122]
Patients with seasonal asthma who are symptomatic during the season are recommended to be treated with low-dose ICS before the beginning of the season (Evidence D).
Treatment at step 2
-
Recommended options
- Combination of ICS/formoterol on “as-needed basis” (Evidence A).[113,114] When compared to regular maintenance with low-dose ICS alone, it was found to be inferior with respect to controlling symptoms and noninferior with respect to the rate of severe asthma attacks and time to first attack. The combination of budesonide/formoterol on “as-needed basis” achieved such outcome with substantially lower ICS dose equivalent to 17%–25% of the maintenance dose of ICS.
-
Alternative options
- LTRA (Montelukast) especially for those patients who are reluctant to use ICS or continue to have side effects, despite preventive measures (Evidence A).[131] LTRA is less effective than low-dose ICS in achieving asthma control and in reducing the risk of attacks.
Maintenance of low-dose ICS could be recommended for patients who are controlled at the time of assessment (an ACT score of ≥20) but have risk factors for asthma attacks or fixed airway obstruction (Evidence B).[107,126,132,133]
Treatment at step 3
Combined low-dose ICS with LABA was found to improve asthma control for patient whose asthma is not controlled at step 2 and reduce asthma attacks (Evidence A).[134,135] The patient is recommended to continue on reliever treatment on “as-needed basis” (Evidence A). ICS with LABA are available (refer Medication Appendix) as follows:
ICS combined with formoterol can be used as maintenance and reliever without adding SABA
ICSs in the form of beclomethasone dipropionate, budesonide, or fluticasone propionate are available in combination with salmeterol. These are normally prescribed twice daily with SABA as a reliever
Once-a-day combination of ICS and LABA (fluticasone furoate with vilanterol) is also available. SABA should be utilized as a reliever.
Inhaled LABA alone is not available in the Saudi market since it should never be used alone in asthma management.[136] Asthma patients taking inhaled LABA without inhaled ICS are at an increased risk of asthma attacks, hospitalizations, and death.[137]
-
Recommended options
- If a formoterol/ICS combination is prescribed, it is recommended to be used as maintenance with 1–2 inhalations twice daily. Extra doses up to 12 inhalations per day can be used as the reliever therapy from the same device (Evidence A).[110,111,112,122] Those patients who require such high doses for 2–3 days should seek medical advice to step up maintenance therapy, and they may require the use of a short course of oral prednisolone (Evidence A)[112]
- If salmeterol/ICS combination is selected, an escalation of the regular daily doses to maximum dosing achieves asthma control in a majority of patients on uncontrolled at Steps 2 and 3 (Evidence A).[138] Salmeterol has a slow onset of action; therefore, it should only be used as a maintenance treatment with SABA as a reliever
- The once-a-day combination of ICS/LABA in the form of fluticasone furoate/vilanterol (Relvar) can be prescribed at a daily inhalation dose of 100/25 mcg for adults and children above 12 years (Evidence A).[139,140] As vilanterol has an onset of action within 15 min and a long half-life, it can only be used as a maintenance treatment while continuing SABA as a reliever.
-
Alternative options
- Tiotropium is a long-acting anticholinergic (antimuscarinic) agent (LAMA) approved for the treatment of COPD.[146,147,148] Evidence has shown that when tiotropium is added to an ICS, it improves symptoms, reduces risk of attack, and improves the lung function in patients with inadequately controlled asthma. Its effect appears to be at least equivalent to LABA (Evidence A).[149,150,151] This evidence supports that tiotropium can be combined with ICS whenever LABA cannot be used.[152]
Consultation with an asthma specialist is recommended whenever there is a difficulty in achieving control at step 3 (Evidence D).
Treatment at step 4
Consultation with an asthma specialist is recommended for patients who require this step of therapy (Evidence D).[153]
-
Recommended options
-
Additional options
If control is not achieved with the recommended options, the following can be considered:
- Once-a-day combination of fluticasone furoate (100 mcg), umeclidinium (62.5 mcg), and vilanterol (25 mcg) (Trelegy Ellipta®) is an option for adults. Adding umeclidinium to the combination of ICS/LABA was found to be effective treatment option with a favorable risk–benefit profile as it led to improved symptoms and FEV1 but did not result in significant reduction in moderate and/or severe exacerbations.[155] Higher dose of fluticasone furoate (200 mcg) primarily reduced the rate of exacerbations, particularly in patients with raised biomarkers of type 2 airway inflammation
-
Other considerations
- High-dose ICS/LABA may be considered in some patients who are uncontrolled on medium-dose ICS/LABA.[142,163] However, it is recommended to step down whenever possible to avoid potential side effects.[141,164] An additional controller is recommended to be introduced before considering the high-dose ICS
- If a patient is still uncontrolled at step 4, biologic therapy is recommended to be considered as described in step 5.
Treatment at step 5
Early consideration of biological therapy may save the patient from frequent or chronic use of OCSs and reduce asthma attacks. This therapy is recommended to be considered based on appropriate indications and availability. When choosing a biological agent, several factors should be considered including the frequency of administration, cost, side effect profile, age at onset of asthma, and presence of comorbid conditions, such as nasal polyps, previous response, and physician experience with the treatment. Consultation with an asthma specialist is strongly recommended for patients requiring treatment at step 5 (Evidence D). The following biological agents are available for step 5:
Anti-IgE therapy (Omalizumab) is recommended for those patients uncontrolled on maximum treatment at step 4, who have allergic asthma as determined by a positive skin test or RAST study and IgE level within the appropriate therapeutic range (for more information refer Medication Appendix, Medications Section) (Evidence A). A history of documented atopy might be used as a marker of allergic asthma if RAST test and skin test are unavailable (Evidence D).[142,144,154] During the course of therapy, anti-IgE led to more reduction of asthma attacks in a category of asthma patients who showed >50% reduction in blood eosinophils.[165,166] The dose is determined by the IgE level and weight. If this treatment does not control asthma after 16 weeks of therapy, it should be stopped[167,168,169]
-
Anti-IL-5 therapy can be considered for uncontrolled eosinophilic asthma or ≥2 attacks in the past 12 months requiring systemic corticosteroids at step 4 (for more information refer to Medication Appendix).[170] There are no data to determine the duration before deciding on treatment ineffectiveness. However, until this evidence is available, the treatment may be continued for up to 6 months before the decision of stopping/switching treatment (Evidence D).[171] The available options are as follows:
- Mepolizumab, an anti-IL-5 therapy, that is indicated when blood eosinophils count is ≥150 cells/μL at treatment initiation or ≥300 cells/μL at any time in the prior 12 months. The recommended dose is 100 mg subcutaneously every 4 weeks
- Benralizumab, an anti-IL-5 receptor therapy, that is indicated when blood eosinophils count at initiation of treatment is ≥300 cells/μL or ≥150 cells/μL for patients with prolonged OCS.[172] The recommended dose is 30 mg subcutaneously every 4 weeks for the first 3 months and then every 8 weeks thereafter.
Dupilumab is an anti-interleukin 4 receptor α (anti-IL4Rα) antibody indicated in severe eosinophilic asthma with blood eosinophils ≥150/μl or FeNO >25.[173] It is also indicated for oral steroid-dependent severe asthma, regardless of blood eosinophils count, although patients with eosinophil count >300/μL had significantly more benefit. It is approved for patients ≥12 years of age. For eosinophilic asthma phenotype, the dose is 400 mg SC once and then 200 mg every 2 weeks.[174] For the oral steroid-dependent asthma or those with comorbid conditions responsive to dupilumab such as moderate-to-severe atopic dermatitis or chronic rhinosinusitis with nasal polyposis, the dose is 600 mg once and then 300 mg every 2 weeks (refer to more information in the Medications Index). It is recommended not to start dupilumab in patients with blood eosinophil count >1500/μL
To date, there is no available evidence to favor either anti-IgE therapy versus anti-IL-5 agents or anti-IL4Rα for patients with evidence of both atopy and high blood eosinophils counts.
If the patient does not have any of the biological therapy phenotypes, or biologic therapy is not available or not adequately controlling the disease, the alternative approach is to use the lowest possible dose of long-term OCSs (Evidence D).[175] Other alternatives are mentioned in the Severe Asthma Section, such as thermoplasty and long-term macrolides.
For patients who require long-term systemic corticosteroids, the following are recommended to be considered:
Use the lowest possible dose to maintain control
Closely monitor the development of corticosteroid-related side effects
When asthma control is achieved, attempts to reduce the dose of systemic corticosteroids, preferably to every other day frequency, are recommended. Maintaining high-dose of ICS therapy may help reduce the dose of systemic corticosteroid
Upward adjustment of the corticosteroid dose at the time of stress (e.g., infection, asthma attacks, surgery) is essential
Concurrent treatments with calcium supplements, Vitamin D, and bone-sparing medications (e.g., bisphosphonates) in patients who have risk factors for osteoporosis or low bone mineral density are strongly recommended (Evidence C).
Maintaining asthma control
Regular follow-up by a healthcare worker is essential. Depending on the level of asthma control, it is recommended to have a follow-up at 1–3 months' intervals after treatment initiation (Evidence D).[97,176] Follow-up is recommended to include monitoring and reviewing the patient's written asthma action plan, medication adherence and inhaler technique, patient's behaviors, comorbidities, and possible side effects of the medications. Once asthma is controlled and the control is maintained for at least 3 months, a step down in pharmacologic therapy is recommended at the minimum level that can maintain the good control and minimize the side effects (Evidence D). The following are the general recommendations:
Reduction in therapy is recommended to be gradual and closely monitored based on clinical judgment of the individual patient's response to therapy and ACT score (Evidence D)
If the patient is on ICS as monotherapy, the dose of ICS may be reduced gradually every 3–6 months to the lowest dose possible that is required to maintain control (Evidence B)[90,177,178] and then changed to a single daily dose (Evidence A).[179] It is recommended to be clearly explained to the patient that asthma control may deteriorate if treatment is abruptly discontinued[180]
If the patient is on combination of ICS/LABA at step 3 or 4, abrupt discontinuation of LABA is not recommended as it may lead to deterioration of the control. Therefore, initial gradual reduction of ICS to the lowest possible ICS dose before discontinuation of LABA is recommended[181]
If the patient is on a combination of ICS and LABA, LTRA, or other controllers, then start by tapering ICS to the lowest possible dose (Evidence B).[182,183] If control is achieved, LTRA may be discontinued first (Evidence D)[182]
For significant side effects, consider a change in therapy, reduction in the dose, or frequency of ICS (if possible), advise vigorous mouth washing after inhalation, use of spacer (concomitant with MDI devices), and/or use of appropriate local antifungal therapy for severe oral thrush[184]
Patients should be informed that asthma control may deteriorate if treatment is completely discontinued.[180]
Referral to an asthma specialist
Situations that require referral to an asthma specialist for consultation or comanagement include:
Uncertainty regarding the diagnosis
Difficulty achieving or maintaining asthma control
Immunotherapy or biologic therapy is being considered
Difficulty to achieve asthma control at step 3 or higher
Acute asthma attack requiring hospitalization
Request of a patient for second opinion or further advice.
Allergen immunotherapy
Allergen immunotherapy (AIT) is a treatment modality to desensitize patients to specific allergens. It is considered for those with stable asthma and evidence of clinically relevant allergic sensitization at which the immunotherapy can be directed, especially if they have coexisting allergic rhinitis. Patients with poorly controlled asthma should not be started on immunotherapy.[185,186] Although there are insufficient data on the impact of AIT on asthma attacks and quality of life scores, it has specifically been shown to:
Improve asthma symptoms and stepping down asthma treatment (Evidence A)[187]
Improve airway hyperresponsiveness (Evidence B)[188]
Decrease the progression of allergic rhinitis to asthma (Evidence B)[189]
Decrease the chance of development of new sensitizations (Evidence B).[185]
AIT is likely to be cost-effective when appropriately used.[186] There are currently two types of AIT in clinical practice; subcutaneous immunotherapy (SCIT) and sublingual immunotherapy (SLIT). Most studies that compared SCIT to SLIT showed a better clinical efficacy of SCIT. However, SLIT has a better safety profile than SCIT as SCIT may rarely cause anaphylaxis.[187] Patients at risk are mainly those with asthma, especially if uncontrolled. High level of caution should be taken in patients using beta-blockers due to the risk of more serious anaphylaxis that is resistant to treatment with epinephrine.[185] Data are limited in pediatrics, but AIT has been used safely in children over 5 years of age and was shown to reduce long-term asthma medication use and improve FEV1.[190] Although beneficial effects may be observed a few months from starting AIT, treatment with AIT needs patient's commitment for at least 3 years to have sustained desensitization after stopping the treatment. Furthermore, AIT can be continued, but not initiated, during pregnancy. Most studied allergen-specific immunotherapies are dust mites, Alternaria, grass pollens, ragweed, and cat. Anti-IgE therapy could improve tolerability to AIT in patients with moderate-to-severe asthma.[191] If the patient is considered a candidate for AIT, referral to an allergist is recommended to explore this option further.
Severe asthma
There are several terms used in practice for uncontrolled asthma where each point to an aspect of the diseases such as chronic severe asthma, steroid-dependent asthma, and refractory asthma are some of these terminologies.[192,193] However, it is important to distinguish between severe asthma and uncontrolled asthma. Severe asthma is defined as the “uncontrolled asthma at SINA step 4 despite adequate adherence and after addressing all comorbidities.”[83] Severe asthma probably accounts for 5%–10% of adult asthma, but the health cost is disproportionally high.[194] Morbidity and mortality are also higher compared to regular asthma patients because of increased side effects of treatment and more frequent attacks and/or hospitalizations.[195,196] Before a diagnosis of severe asthma is considered, patients must undergo a systematic assessment where the diagnosis of asthma is confirmed, and comorbidities are identified and treated.[197] Patients whose poor asthma control is related to other factors, such as poor adherence, inhaler use technique, or the presence of other diseases, are to be termed “difficult-to-treat asthma.”[1] There are common comorbidities that need to be assessed in severe asthma such as allergic rhinoconjunctivitis, rhinosinusitis/nasal polyps (in 50%), COPD, vocal cord dysfunction (in 32%–50%), anxiety/depression (in 4%–17%), obstructive sleep apnea (in 31%), GERD (in 17%–74%), bronchiectasis (in 25%–40%), and allergic bronchopulmonary aspergillosis (in 1%–2%).[198] The following are recommended for the assessment of patients with severe asthma:[199,200,201,202,203,204]
Patient is adherent to all medications with a good inhalation technique
Other possible misdiagnoses where the problem is not bronchial asthma to start with but other diseases that mimic asthma symptoms, e.g., bronchiectasis, endobronchial tumors, vocal cord dysfunction, allergic bronchopulmonary aspergillosis (ABPA), or eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome)[202,205]
Comorbidities that can worsen bronchial asthma and make it difficult to manage (e.g., chronic rhinosinusitis, GERD, sleep apnea syndrome, ABPA, obesity, and congestive heart failure [CHF])[206]
Medications overuse or side effects
Any psychosocial contributing factors
Other confounding factors, e.g., presence of allergens at home or work, active or passive smoking and vaping, or psychosocial problems.[202]
As it may be difficult to achieve full control in many patients with severe asthma, the aim of treatment in this situation is to reach the best possible control.[207] After dealing with all comorbidities and other confounding factors that could have made asthma difficult to control, maximum therapy is recommended at step 5, which may include combination therapy of high-dose ICS/LABA, LTRA, or LAMA and addition of one of the available biological therapies as appropriate.[171,208,209]
A significant percentage of patients with severe asthma do not respond adequately to high-dose ICS and other controller therapy; thus, they need frequent or continuous oral steroid therapy to achieve a reasonable response.[210] Such control may be lost when oral steroid is discontinued. Patients may differ in the degree of their responsiveness to oral steroids.[211] Some patients may fail to improve their FEV1 by more than 15% following treatment with oral prednisolone for 2 weeks, a condition called “corticosteroid-resistant asthma.”[212,213] If oral steroids are necessary, then it is recommended to use the lowest possible dose and to shorten the duration as much as possible.[214] In this situation, osteoporosis prophylaxis is recommended.
For patients with severe asthma that do not qualify or respond to biologic therapy, other modalities of treatment of severe asthma are recommended for consideration which includes:
Macrolides: Due to their role in reducing neutrophilic airway inflammation, they were shown to have a role in the management of severe asthma. A study has assessed the benefit of azithromycin at a dose of 250–500 mg 3 days/week as add-on therapy for 48 weeks for patient with persistent symptomatic asthma.[215] Azithromycin significantly reduced the experience of at “least one asthma attack” from 61% to 44%. It has significantly improved asthma-related quality of life measures, and responses in eosinophilic asthma were greater than in those without eosinophils
Bronchial thermoplasty (BT): Utilizing radiofrequency energy to alter the smooth muscles of the airways and possibly bronchial wall innervation, BT has been shown to reduce the risk of asthma attacks in clinical trial setting.[216] In well-selected patients with moderate-to-severe asthma, it may improve various aspects of asthma, including FEV1, quality of life, asthma control, attacks, and use of rescue medications.[217,218,219] Until solid evidence is available, it is recommended to perform it in the setting of clinical trials and approval of an independent institutional review board.[83] Contraindications to BT include moderate and severe bronchiectasis, very high sputum production, and fixed airflow obstruction with FEV1 levels below 50% as predicted.
Section 7: Management of Acute Asthma in Adults and Adolescents
Acute asthma attack is a challenging clinical scenario that requires a systemic approach to rapidly diagnose, evaluate, and initiate therapy. The most specific marker associated with increased asthma mortality is a history of repeated hospital admissions, particularly if the patient required intensive care treatment or ventilatory assistance.[220,221] Patients admitted with severe asthma attack in Saudi Arabia were found to be younger and predominantly males and used less ICS/LABA combination.[2,222]
This section includes assessment of the patients presented with acute asthma, initial management, and follow-up after hospital discharge. Detailed information about medications used in acute asthma can be found in Medication Appendix. [Box 7.1] shows the summary of the key recommendations of acute asthma management.
Box 7.1.
Key recommendations of acute asthma management
| Assess the severity of the attack based on the degree of dyspnea, pulse rate, respiratory rate, peak expiratory flow rate, and oxygen saturation |
| Start treatment immediately by repeated administration of salbutamol, controlled oxygen concentration and systemic steroid |
| Review response to treatment after 1 h of continuous therapy |
| Consider other therapy (ipratropium bromide and magnesium sulfate) in severe attacks |
| DO NOT request routine CXR or blood gases routinely unless indicated |
| DO NOT prescribe routine antibiotics or sedatives |
| Evaluate the need of hospital admission based on response to therapy, history of previous admission, and the ability to manage at home |
CXR: Chest X-ray
Clinical assessment of acute asthma
The initial clinical assessment should rapidly determine whether the patient's presenting symptoms are related to an acute asthma attack or not [Box 7.2]. Although most acute asthma attacks develop over a period of days, patients with brittle asthma may present with a much more dramatic deterioration.[223,224] It is important to realize that most patients who die from an acute asthma attack had chronically uncontrolled asthma, had received suboptimal treatment with ICS, and had inadequate monitoring of their asthma.[225] Management of acute asthma is the extreme spectrum of uncontrolled asthma and represents the failure to reach adequate asthma control. Poor prognostic features of acute asthma include previous history of near-fatal asthma or hospital admission in the last year, heavy usage of SABA, patients who are not on regular ICS, a history of psychiatric or psychosocial illness, and poor adherence to asthma medications and lack of asthma action plan.[226,227]
Box 7.2.
Levels of severity of acute asthma in adults
| Level | Characteristics |
|---|---|
| Moderate asthma attacks | Increasing symptoms PEF >50%-75% best or predicted reading No features of acute severe asthma |
| Acute severe asthma | Any one of the following PEF 30%-50% best or predicted reading Respiratory rate ≥25/min Heart rate ≥120/min Inability to complete sentences in one breath |
| Life-threatening asthma | Any one of the following in a patient with severe asthma SpO2<92% (PaO2<60 mmHg) on high-flow FiO2 PEF <30% best or predicted Bradycardia Dysrhythmia Cyanosis Hypotension Normal or high PaCO2 Exhaustion Confusion Silent chest Coma Weak respiratory effort |
| Near-fatal asthma | Raised PaCO2 and/or requiring mechanical ventilation |
| Brittle asthma | Type 1: Wide PEF variability (>40% diurnal variation for >50% of the time over a period of >3-6 months) despite intense therapy Type 2: Sudden severe attacks on a background of apparently well-controlled asthma |
PEF: Peak expiratory flow
On presentation, the patient should be carefully assessed to determine the severity of the attacks [Box 7.3] and the type of treatment required [Box 7.4].[228,229] PEF and pulse oximetry measurements are complementary to history-taking and physical examination. The likely cause for death in acute asthma is probably related to asphyxia, due to severe airflow obstruction and hypoxemia. This is supported by the pathologic evidence of extensive airway obstruction, mucous plugging, and dynamic hyperinflation found at autopsy in patients who died of acute severe asthma.[230]
Box 7.3.
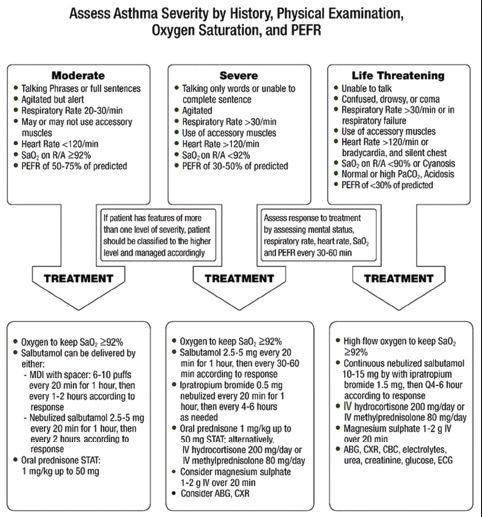
Initial management of acute asthma for adults and adolescents
Box 7.4.
Adjustment of acute asthma treatment for adults and adolescents
The SINA panel recommends the following steps for the management of acute asthma:
To assess severity of the attack
To initiate treatment to rapidly control the attack
To evaluate continuously the response to treatment.
The levels of acute asthma severity and the initial management are summarized in Box 7.3 and Box 7.4, respectively. It is recommended to adjust treatment intensity based on the severity of the attack, and the following are the general guidelines for the treatment of acute asthma.
Oxygen: Controlled concentration of oxygen is recommended to maintain saturation between 92% and 95%. There is evidence that high concentration of oxygen may be harmful[231,232]
-
SABA: Salbutamol is the bronchodilator of choice in acute asthma.[233,234] It could be delivered by either:
- pMDI with spacer: 4–10 puffs every 20 min for 1 h and then adjusting the dose based on the patient's response (Evidence A), or
- Nebulizer: salbutamol 2.5–5 mg every 20 min for 1 h and then adjusting the dose based on the patient's response (driven by oxygen if patient is hypoxic) (Evidence A).
Because the nebulizers increase the risk of disseminating viruses to other patients and to healthcare professionals, in the time of viral pandemic (such as COVID-19), the pMDI via a spacer is the preferred treatment during severe attacks. The routine use of intravenous (IV) β2 agonist is not supported by the current evidence but may be used in life-threatening asthma when inhaled therapy could not be tolerated by the patient.
Steroid therapy: If the patient can tolerate orally, oral prednisolone 1 mg/kg/day (to the maximum of 50 mg daily) should be started as soon as possible. Alternatively, IV hydrocortisone 200–400 mg or methylprednisolone 80 mg in divided doses should be administered.[235] Adding high-dose ICS to systemic corticosteroid in acute asthma is controversial; however, keeping it may ensure continuation of therapy after discharge[236]
Ipratropium bromide is recommended to be added to salbutamol in moderate–severe acute asthma. The initial dose is 4–8 puffs every 20 min by pMDI with a spacer or 0.5 mg every 20 min or by a nebulizer for three doses (Evidence B).[237] This therapy has been shown to improve treatment effectiveness by reducing the rate of hospital admission and improving lung function when it is added to SABA in severe acute asthma[237]
Magnesium sulfate is not recommended routinely in acute asthma. However, in severe cases with inadequate response to the initial therapy, a single dose of IV magnesium sulfate of 1–2 g over 20 min is recommended to be considered as it has been shown to reduce hospital admission, especially in those patients who present with a very low lung function (FEV1 <30% of the predicted) (Evidence A)[238]
IV aminophylline use in acute asthma is associated with severe, and potentially fatal, side effects; hence, its use in acute asthma is prohibited[236]
Antibiotics and sedatives: Unless there is a strong evidence of pneumonia, the routine use of antibiotics in acute asthma is not recommended. Similarly, the use of anxiolytic and hypnotic drugs should be strictly avoided in acute asthma, as their usage has been associated with respiratory failure and death.[236]
Management of life-threatening/near-fatal asthma
Patients in this category can progress rapidly to respiratory failure and death. Hence, an aggressive management approach and continuous monitoring are mandatory. Aside from the routine initial therapy, the following steps are recommended in the management of life-threatening or near-fatal asthma:
Consult ICU service and ensure that the intubation setting is readily available
Administer adequate oxygen concentration to keep saturation ≥92%[227]
Deliver continuous nebulized salbutamol (10–15 mg) with ipratropium bromide dose of 1.5 mg over 1 h (Evidence A).[236,239,240] Continuous treatment was found to be safe and well tolerated and led to better improvement in pulmonary functions and reduction in hospitalization when compared to intermittent delivery (Evidence A).[236,239,240] Oxygen-driven nebulizers are recommended to be used to avoid the risk of oxygen desaturation while using air-driven compressors (Evidence A).[236,239,240] Strict infection-control measure should be taken to prevent the dissemination of viral infection to the healthcare professionals or other patients during the nebulization sessions, especially of time of viral infections pandemics (such as COVID-19). Once the patient showed adequate response to continuous nebulization, shift to intermittent delivery is recommended[241]
Systemic steroid is recommended to be initiated as soon as possible
Consider a single dose of IV magnesium sulfate
Other adjunct therapy (e.g., intramuscular epinephrine, IV β2 agonist, and helium oxygen therapy) may be considered in selected cases, but the evidence supporting their use is less robust
Noninvasive ventilation (NIV): The data of the use of NIV are less robust in acute asthma compared to COPD attack.[239,240] If used, the patient should be monitored closely for signs of fatigue or respiratory failure. NIV should be avoided in agitated patients and in those who are in impending respiratory failure
Extracorporeal membrane oxygenation (ECMO) may be considered in cases of acute respiratory failure secondary to near-fatal or life-threatening asthma. Few case series suggested that early introduction of ECMO in those patients may lead to dramatic improvement in gas exchange and lung mechanics and avoid the serious complications of mechanical ventilation[242]
Frequent clinical evaluation and serial CXR, electrolytes, glucose, 12-lead electrocardiogram, and Arterial blood gases (ABGs) are recommended in this patients' population.
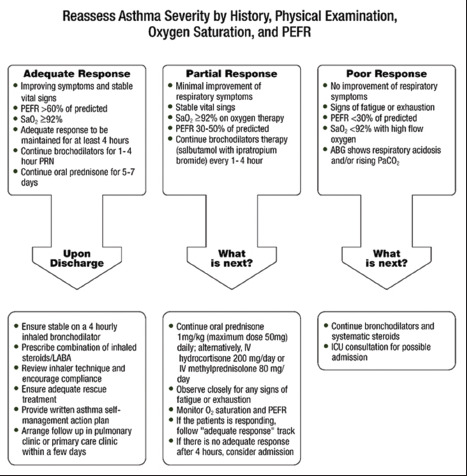
Follow-up after initial treatment and discharge planning
Close evaluation of the treatment response is essential. This includes patient's mental and physical status, respiratory rate, heart rate, blood pressure, oxygen saturation, and PEF. Response to treatment is defined as adequate, partial, or poor. Assessment of the treatment response, subsequent action, and discharge planning are illustrated in [Box 7.4].
Criteria for intensive care unit referral
ICU referral is recommended for patients who are:
Presenting, or progressing to, severe acute or life-threatening asthma
-
Failing to respond to initial therapy, as defined by:
- Requiring ventilatory support
- Deteriorating lung function (FEV1/PEF)
- Persisting or worsening hypoxia
- Hypercapnia (either initially or subsequently)
- ABG analysis showing respiratory acidosis
- Exhaustion, shallow respiration, or drowsiness.
Section 8: Asthma in Special Situations
Gastroesophageal reflux disease
GERD is more prevalent in patients with asthma, compared to the general population.[243,244] The mechanisms by which GERD worsens asthma include vagal-mediated reflex and also reflux secondary to microaspiration of gastric contents into the upper and lower airways.[245] All patients with asthma should be questioned about the symptoms of GERD. If present, a trial of anti-GERD measures, including a proton pump inhibitor and lifestyle modifications, is recommended for 6–8 weeks. However, if symptoms are not resolved, further investigation is warranted. Benefit of proton pump inhibitors is limited to patients with symptomatic GERD and night-time respiratory symptoms. On the contrary, patients with uncontrolled asthma and asymptomatic GERD are not likely to benefit from empiric GERD therapy.[246]
Rhinitis/sinusitis and nasal polyp
Most asthma patients have coexisting rhinitis and/or sinusitis, and around 40% of patients with rhinitis do have asthma.[247] Asking patients about rhinitis symptoms and examination of the upper airways is recommended to be part of the routine management of asthma. Treatment with intranasal corticosteroids has been associated with a decrease in asthma hospitalization and ED.[193,248,249]
Obesity and asthma
Asthma is more common in obese than nonobese patients.[250] Obese asthma patients have more symptoms, more frequent and severe exacerbations, reduced response to asthma medications, and poor quality of life. This could be in part related to reduced lung volumes, lack of fitness, and associated sleep apnea and GERD. However, recent work has shown that the obesity is associated with peripheral airways dysfunction, increased small airways resistance, and increased low frequency reactance area, leading to increase lung stiffness.[251]
Treatment of obese asthma patients follows the same step approach for nonobese asthmatic; however, weight reduction, exercise, and diet control are essential part of their management.[252] For morbidly obese patient with asthma, it is recommended to discuss the risks and benefits of bariatric surgery when other measures are failed.[253,254]
Cough-variant asthma
Patients with cough-variant asthma may have chronic cough as their main symptoms, especially at night.[255,256] Other diagnoses to be considered are drug-induced cough caused by angiotensin-converting enzyme inhibitors, GERD, chronic upper airway cough syndrome manifesting as postnasal drip, eosinophilic bronchitis, and chronic sinusitis. Once the diagnosis is established, treatment is recommended with ICS.[257,258] This condition may be confused with eosinophilic bronchitis which is characterized by cough and sputum eosinophilia with normal spirometry and AHR.[259,260]
Exercise-induced bronchoconstriction
Exercise-induced bronchoconstriction (EIB) is common in inadequately controlled asthma patients. However, asthma-like symptoms can sometimes be triggered only by physical activities. Normally, bronchodilation occurs during exercise and lasts for a few minutes.[261,262] In patients with EIB, the initial bronchodilation is followed by bronchoconstriction that generally peaks within 10–15 min after completing the exercise and resolves within 60 min. EIB can be prevented by using SABA or ICS/formoterol a few minutes before exercise.[263,264] A warm-up period before exercise may also reduce EIB symptoms. If this approach does not control the symptoms, the patient is recommended to have maintenance therapy with ICS.[145,263] Regular use of LTRA may also help in this condition, especially in children.[145,261,263]
Aspirin-exacerbated respiratory disease
ASA-exacerbated respiratory disease (AERD) is a special phenotype characterized by a triad of asthma, chronic rhinosinusitis with nasal polyposis, and respiratory reactions to ASA.[265] About 7% of adult asthma patients and 15% in those with severe asthma suffer from attacks in response to ASA or NSAIDs that inhibit cyclooxygenase-1 (COX-1).[266] Majority of patients experience first symptoms during their third or fourth decade of life. Once ASA or NSAID hypersensitivity develops, it persists for life. Characteristically, within minutes to 2 h following ingestion of ASA, an acute severe asthma attack develops. It is usually accompanied by rhinorrhea, nasal obstruction, conjunctival irritation, and scarlet flush of the head and neck.[267] A typical history of upper and lower respiratory reaction to ASA or NSAIDs is very suggestive for the diagnosis, which is confirmed by ASA challenge.[268] A normal sinus CT almost excludes AERD. Patients known to have ASA-induced asthma should avoid all ASA-containing products and NSAIDs. Where an NSAID is indicated, COX-2 inhibitors or alternative analgesics such as paracetamol are recommended.[269] Prophylactic low-dose ASA should also be avoided. However, referral to an allergy specialist for ASA desensitization is recommended in patients for whom ASA is required as antiplatelet therapy, patients with difficult to manage polyposis, or patients with severe asthma.[270] Montelukast may help in the treatment of this type of asthma in some patients.[271]
Pregnancy
A study conducted in a tertiary care hospital in Saudi Arabia showed that almost half of the pregnant women had the desire to stop asthma medications during pregnancy as they believed that asthma medications would harm them and their babies more than asthma itself.[21] As such, a great effort should be directed toward the education of asthma in pregnancy to correct this misbelief. The course of asthma during pregnancy is unpredictable; however, one-third of pregnant asthmatics may have a worsening of their asthma control.[272,273] Maintaining adequate control of asthma during pregnancy is essential for the health and well-being of both the mother and her baby, and the occurrence of poor asthma control during the first trimester of pregnancy significantly increases the risk of a congenital malformation.[274] Identifying and avoiding triggers are recommended as the first step of therapy for asthma during pregnancy, and treatment is recommended to take the same stepwise approach as in the nonpregnant patient. Salbutamol is the preferred SABA due to its excellent safety profile. ICSs are the preferred treatment for long-term control.[275] All asthma medications, including ICS, theophylline, antihistamines, β2-agonists, and LTRA, are generally safe and have not shown to increase the risk of fetal abnormalities.[276,277] However, prolonged use of systemic steroids may be associated with pregnancy-related complications, especially in the first trimester.[273]
Pregnant women are recommended to receive the same drug treatment for acute asthma as nonpregnant patients (Evidence B), including systemic steroids if indicated (Evidence C).[278,279,280] Fetal monitoring is recommended in severe asthma attack. If anesthesia is required during labor, regional anesthesia is recommended whenever possible (Evidence C).[281] The use of prostaglandin F2α may be associated with severe bronchospasm and should be avoided if possible.[282] If asthma is well controlled during pregnancy, acute asthma is rare during labor. Pregnant asthma patients should be encouraged to breastfeed after delivery and to continue their usual asthma medications during lactation.[283,284]
Occupational asthma
All patients with asthma should be asked about their occupational history and exposures for possible related occupation-related allergens. A simple screening test is to ask the patient if their symptoms improve when they are away from work.[285] Once identified, early detection and elimination of occupational sensitizers and removal of patients from further exposure are essential aspects of the management. Referral to an asthma for assessment and advice is recommended for patients with suspected or confirmed occupational asthma because of the legal implications of the diagnosis.[286,287]
Asthma-chronic obstructive pulmonary disease overlap
Distinguishing asthma from COPD may be difficult in patients who show features of both diseases, hence the name asthma-COPD overlap (ACO).[288] ACO is a unique complex descriptive entity sharing features of both COPD and asthma. At this stage, there is no formal definition of ACO as there are inadequate data to describe its features, characteristics, and its optimal therapeutic intervention.[282] ACO has been estimated to account for approximately 15%–25% of the obstructive airway diseases in adults and may carry worse outcomes compared with asthma or COPD alone.[282] Patients with ACO have the combined risk factors of smoking and atopy. They are generally younger and have more frequent exacerbation, worse quality of life, a more rapid decline in lung function, greater healthcare utilization, and higher mortality compared to patients with COPD alone.[289,290,291] Spirometry is required to confirm the diagnosis of chronic airflow limitation and document persistent airflow limitation, variability, and reversibility.
If the initial assessment suggests the diagnosis of asthma or ACO, or there is uncertainty about the diagnosis of COPD, it is prudent to treat as asthma by starting ICS (with or without LABA) and to avoid using LABA and/or LAMA as the only therapeutic option. For ACO patients, we recommend considering smoking cessation, pulmonary rehabilitation, vaccinations, and treatment of comorbidities as additive therapeutic strategies.
Section 9: Management of Asthma in Children
Asthma represents one of the most common chronic illnesses of childhood with significant economic impact.[292] It is also a leading cause for childhood morbidity as measured by school absences, ED visits, and hospitalizations.[293] From the prospective of both patient and society, the cost of not treating asthma is higher than the cost of asthma treatment.[294,295] The sections related to asthma in children aims toward enhancing the multidisciplinary care of asthma patients with special attention to nonasthma specialists, including primary care and general practice physicians and other healthcare workers.[296]
Asthma diagnosis in children
Clinical considerations
Accurate diagnosis of asthma in children is crucial to prevent inappropriate management and reducing morbidity and mortality due to under- or over-diagnosis.[297,298] Therefore, asthma diagnosis in children should be based on a careful clinical assessment that includes recurrent or chronic symptoms related to airway obstruction such as wheezing, coughing, night symptoms, activity limitation, and shortness of breath. These symptoms typically result from airway hyperreactivity (AH) or various stimuli that would be reversible either spontaneously or after receiving an asthma therapy. The diagnosis can be further supported by the presence of atopy, early sensitization, and a family history of atopy. Whenever possible, spirometry is recommended for children to be performed to show reversibility of airway obstruction after bronchodilator therapy.[292] Spirometry can generally be performed in children aged 5–12 years. It is preferably planned when the initial diagnosis is made and after 3–6 months of controller therapy initiation with subsequent follow-up assessment. [Box 9.1] presents a summary of signs and symptoms, suggestive of the diagnosis of asthma in children.
Box 9.1.
Diagnosis of asthma in children
| Symptoms and signs | Remarks |
|---|---|
| History of multiple attacks of SOB or wheezing in a season | More than 3 attacks/season, recurrent, and worse during sleep with triggers such as physical activity, laughing, crying, or exposure to tobacco smoke or air pollution |
| Coughing | More than 2 weeks, not related to URTI, recurrent, and worse during sleep with triggers such as activity, laughing, crying, or exposure to tobacco smoke or air pollution |
| Reduced activity | Not able to run, play, or laugh at the same intensity as other children and tires earlier during walks (wants to be carried) |
| Wheezing | Equal at both sides of the chest, during expiratory phase, especially on forced expiration |
| Atopy | Eczema, environmental/food sensitization |
| Family history | Atopy (allergic rhinitis, atopic dermatitis, food allergy) and asthma in the first-degree relative |
| Breath sounds | Prolonged expiratory phase |
| Therapeutic trial | Trial of short-acting bronchodilator or corticosteroid therapy |
| Spirometry | Typically, in children >6 years with bronchodilator response assessment |
| Chest X-ray | May be considered in infants to rule out congenital causes |
| Tests for hypersensitivity | Both skin testing or/and allergen-specific IgE blood testing |
URTI: Upper respiratory tract infection, IgE: Immunoglobulin E
Asthma mimics should be suspected when any of the following is present: failure to thrive, onset of symptoms during infancy, vomiting associated with respiratory symptoms, continuous wheezing, failure to respond to asthma controller medication, clubbing or focal auscultation signs, and symptoms that are not associated with typical triggers.[299]
Clinical suspicion of asthma mimics is an acceptable indication for CXR in a child suspected of having asthma; however, a routine CXR is not recommended to be part of the initial routine work-up of asthma in children.[300,301]
Wheeze in preschool children
Wheezing and shortness of breath in preschool children are among the most common presenting symptoms in pediatric practice. Approximately one-third of children have at least one episode of wheeze before their third birthday.[302,303] In preschool children, asthma diagnosis and management differ from that of older children and adolescent in many ways. Early childhood wheezing can evolve to different asthma phenotypes that can have variable response to standard therapy.[304] In addition to the diagnosis of asthma, wheezing in preschool children can be due to unique differential diagnoses such as congenital defects, infections especially viral bronchiolitis, bronchopulmonary dysplasia, and cystic fibrosis. In this age group, asthma diagnosis represents a challenging clinical judgment due to the lack of objective assessment such as pulmonary function test or biomarkers. The use of “reactive airway disease,” as a diagnosis, is discouraged as it can restrain full clinical assessment and proper management of asthmatic children in this age group.[305,306,307]
Wheezing phenotypes in children
Wheezing phenotype in young children can be classified either symptom-based or age-based [Box 9.2].[303]
Box 9.2.
Wheezing phenotypes in young children
| Phenotype | Presentation | Characteristics |
|---|---|---|
| Symptom-based | Episodic | Wheezing occurs during specific time periods Often associated with URTIs Absent between these episodes |
| Multi-trigger | Episodic wheeze Can occur between episodes, during sleep, and can be triggered by crying, laughing etc. |
|
| Age-based | Early transient | Wheezing starts before the age of 3 years with resolution by the age of 6 years |
| Persistent | Wheezing starts before the age of 3 years and continues after the age of 6 years | |
| Late-onset | Wheezing begun between 3 and 6 years of age |
URTI: Upper respiratory tract infection
Based on several longitudinal studies, wheezing has been categorized epidemiologically into transient and persistent wheeze phenotypes. It is also categorized based on symptoms into episodic/viral induced and multi-trigger wheeze phenotypes.[303,308] Different responses to treatment and variable outcomes have been attributed to phenotype heterogeneity, overlap, and instability over time. Major factors that may predict persistent symptoms are allergic disease, reduced lung function, viral respiratory infection, and bacterial colonization in infancy. Asthma wheeze phenotype in children has been classified as:[303,309]
Early transient wheezing before the age of 3 years with resolution by the age of 6 years
Persistent wheezing that starts before the age of 3 years and continues after the age of 6 years
Late-onset wheezing between 3 and 6 years of age.
The allocation of children into these categories still remains a subject of debate, as their clinical usefulness is still under investigation.[310]
Prediction of asthma in preschool children
For early identification of the risk for persistent asthma among preschool children, the SINA expert panel recommends the utilization of the modified asthma predictive index (modified-API). This tool is a clinical scoring instrument that can be used to predict whether a child with intermittent wheezing before the age of 3 years will develop persistent asthma pattern during school-aged years [Box 9.3].[311,312] For children with a history of ≥4 wheezing attacks (at least one is diagnosed by physician) and either one major or two minor criteria at 3 years of age, there will be 4–10-fold increase in the risk of having asthma later in their childhood. On other side, children with negative modified-API will have 95% chance of outgrowing their asthma later on life.[313]
Box 9.3.
Modified asthma predictive index
| History of ≥4 wheezing episodes with at least one physician diagnosed and either | ||
|---|---|---|
| ≥1 of the major criteria | OR | ≥2 of the minor criteria |
| Parental history of asthma | Eosinophilia (≥4%) | |
| Skin test positive to aeroallergens | Wheezing unrelated to colds | |
| Eczema (physician-diagnosed atopic dermatitis) | Allergic sensitization to milk, egg, or peanuts | |
Strategies of asthma management in children
The long-term goals of asthma management in children are not different from those of adults [Box 5.1].[314] Asthma management requires effective partnership between patients/caregivers and their healthcare providers.[315] Once established and strengthened, this relationship will positively impact asthma control.
Assessment of asthmatic patient
Asthma management requires careful evaluation of asthmatic patients at the individual level. Assessment of future risk of adverse outcomes and assessment of symptom control represent a key element in the strategy of asthma management in children.
Assessing future risk of adverse outcomes
This is achieved by assessing future risk of attacks, fixed airflow obstruction, and adverse effect of medications [Box 9.4].
Box 9.4.
Assessment of future risk of adverse outcomes of asthma in children*
| Risk factors | Assessment |
|---|---|
| Asthma attacks within the next few months | Uncontrolled asthma symptoms One or more severe asthma attacks in the previous year The start of the child’s usual “flare-up” season (especially if autumn/fall) Exposures: Tobacco smoke; indoor or outdoor air pollution; indoor allergens, especially in combination with viral infection Major psychological or socioeconomic problems for child or family Poor adherence manifested as underuse of ICS and/or over-use of SABAs |
| Fixed airflow limitation | Severe asthma with several hospitalizations History of bronchiolitis |
| Medication side effects | Systemic: Frequent courses of oral corticosteroids or high-dose ICS; neuropsychiatric adverse reactions after the initiation of LTRA Local: Moderate/high-dose or potent ICS; incorrect inhaler technique; failure to protect skin or eyes when using ICS by nebulizer or spacer with face mask |
ICS: Inhaled corticosteroid, LTRA: Leukotriene receptor antagonist, SABA: Short-acting bronchodilator
Assessing symptom control
This implies a periodical assessment of asthma control combined with adjustments (if needed) of treatment based on the level of control. It is strongly recommended to use asthma treatment in a stepwise approach with the ultimate goal of achieving “optimal” control with “minimal” amount of medications and dosage.[316] Adherence to the prescribed medications and the proper use of their devices are recommended to be addressed before any modification of the treatment plan. Asthma control reflects the adequacy of management by describing the clinical status of a child as controlled, partially controlled, or uncontrolled. Focusing on asthma control may improve patient perceptions and expectations that improve symptoms reported by children and their caregivers and subsequently treatment decisions by clinicians.[317] In children, assessment of asthma control is recommended to cover the domains of physicians and patient/caregiver.
Physician assessment of control
Asthma symptom control has been estimated by physician assessment during clinic visit and/or perception of patients and their caregivers toward asthma control. During each clinic visit, the physician is recommended to assess disease. Different numerical tools have been developed and validated to objectively assess asthma control utilizing patients and their caregiver perception. However, as these tools have some limitations, they are recommended to be used as a complimentary tool rather than replacing physician assessment.[318]
Patient/caregiver assessment of control
The SINA expert panel recommends utilizing one of the following questionnaires based on age. The questionnaire is completed by patients and/or their caregiver before physician evaluation based on the age of the child:
Age group 5–12 years - The childhood-asthma control test (C-ACT)
The C-ACT is a validated test for children aged 5–12 years [Box 9.5]. C-ACT is a two-part questionnaire with a total of seven questions. The first part is to be answered by the patient and the second part by the caregiver. The final C-ACT score is made up of the sum of the scores of the two parts, ranging from 0 (poorest asthma control) to 27 (optimal asthma control). A score of ≤19 points suggests that a child's asthma is not adequately controlled.[319]
Box 9.5.
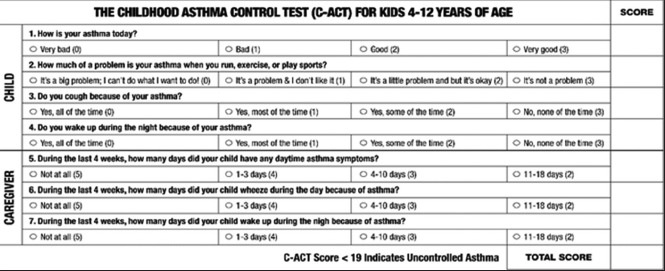
The childhood asthma control test
Age group less than 5 years - The respiratory and asthma control in kids (TRACK)
The TRACK is a validated test for children aged <5 years [Box 9.6]. It is a five-item standardized questionnaire, with four questions that address the impairment domain and one question that addresses the risk domain of asthma control. Each item is scored from 0 to 20 points on a 5-point Likert-type scale for a total score ranging from 0 to 100. Higher scores would indicate better respiratory and asthma control; a score of <80 points suggests that a child's asthma is not controlled.[320]
Box 9.6.
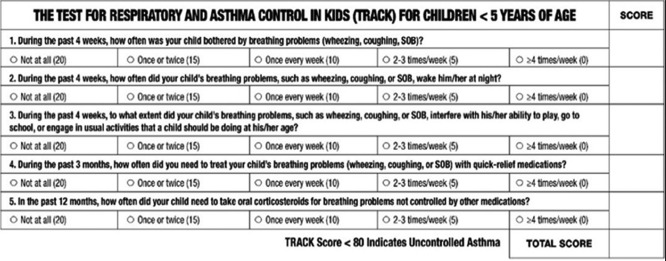
The test for respiratory and asthma control in kids
-
Controller therapy is a group of medications used on a regular basis to keep asthma under control and prevent future risk of adverse outcomes. The following are considerations for this category:
- There are insufficient data to recommend short courses of high-dose ICS in children with mild intermittent asthma attacks (Evidence B).[324] Safety of this approach has not been established
- The clinical benefits of intermittent inhaled or systemic steroid for children with intermittent and viral-induced wheezing remain controversial. This practice is recommended to be discouraged until clear evidence-based practices are available on this strategy of asthma management (Evidence C)[327,328]
- Chronic use of ICS for more than 3 months in prepubertal-aged children can suppress growth velocity which is dose dependent. However, asthmatic children when treated with low-dose ICS attain normal adult height but at a later age (Evidence A).[329,330] Any potential adverse effects of ICS need to be weighed against the well-established benefit to control persistent asthma. More details of the use of ICS in children are available in Medication Appendix
- Children commenced on LTRA should be followed during the early phase of initiation for the development of neuropsychiatric adverse drug reactions (such as anxiety, irritability, aggressiveness, and sleep disturbances) which warrant cessation of therapy in almost 1 out of 6 children. Patient and/or caregiver should be educated on this potential.[331,332,333]
-
Reliever therapy is a group of medications used to rescue asthmatic patient during exacerbation to relief acute symptoms of asthma. The following are considerations for this category:
- Oral bronchodilator therapy is not recommended to be prescribed due to slower onset of action and higher side effects[334]
- LABA should not be used alone as maintenance monotherapy in children (Evidence A).[335] LABA should be used only in combination with ICS. There are different combinations available in the Saudi market as shown in Medication Appendix.
-
Devices are important to select the best device for optimal treatment delivery [Box 9.7].
- Use of valved-holding spacer, with mouthpiece when possible, is recommended when an MDI is prescribed (Evidence B).[336] Breath-actuated devices (e.g., dry powder inhalers) represent an effective and simpler option for maintenance therapy in children 5–12 years of age (Evidence C).[337,338] For more information about medications, refer to Medication Appendix
- Nebulizers are not superior to MDI delivered by spacer in both acute and chronic asthma management (Evidence A).[339]
Box 9.7.
Choosing an inhaler device for children
| Age | Preferred device | Alternative device |
|---|---|---|
| <4 years | MDI + spacer with face mask | Nebulizer with face mask |
| 4-6 years | MDI + spacer with mouthpiece | Nebulizer with mouthpiece |
| More than 6 years | Dry powder inhaler, breath actuated pressurized MDI, MDI + spacer with mouthpiece | Nebulizer with mouthpiece |
MDI: Metered-dose inhaler
Role of patient education
Patient education is recommended to be an integral part of asthma management strategy in children. It is recommended to involve the basic knowledge of the disease pathophysiology, identifying and avoiding triggering factors, environmental controls (especially cigarette smoke exposures), proper use of treatment devices, and recognition of worsening asthma symptoms and the optimal time to seek advice.[340,341] Proper asthma education can lead to a significant reduction in ED visits and hospitalizations, improve self-management of asthma attacks, and an overall reduction in the cost of asthma care [Box 9.8].[342]
Box 9.8.
Goals and objectives of caregiver to be covered during patient education session about asthma
| Goals | Outcome |
|---|---|
| Developing partnership and common goals Sharing understandable information Addressing relevant concerns and expectations Continuity and consistency in providing education |
Understand asthma risk by explaining in a simplified pathophysiology term Acknowledge role of prevention and importance of avoiding triggers Recognize difference between “controller” and “reliever” treatment Address adverse events of medications Explain devices use and importance of compliance with treatment plans Recognize worsening asthma and explain action plan Define comorbid conditions and provide recommendations |
Setting asthma action plans
An action plan that documents medications, doses, and device technique should be provided to patients and their caregivers. The action plan is also recommended to include information for patient and caregiver on how to recognize worsening of asthma symptoms and advices of treatment modification in these situations [Box 9.9].
Box 9.9.
Components of asthma management action plan
| Item | Description |
|---|---|
| Patient identification | Name, medical record number, age, and weight |
| List of patient’s medications | Dosage, frequency, controller versus rescuer medications |
| Recognition of asthma control status | In simple terms and color coded |
| Suggested action based on asthma control status | |
| How to use inhalational devices | Use illustrations |
| When and how to seek medical advice | Access to emergency care or call center |
| Others | How to clean and advices on environmental control inhalers and spacer |
Prevention
Asthma attacks can be triggered by a variety of factors including allergens, viral infection, pollutants, and drugs. Eliminating these exposures improves the control of asthma and reduces medication needs. Parents/caregivers of children with asthma should be strictly advised not to smoke at home at all.[314,343] Breastfeeding and Vitamin D supplementation may decrease the chance of developing early wheezing episodes, while probiotics benefit is still doubtful in preventing allergic disease.[344,345,346] A study on early life use of probiotic supplementation did not show significant impact to prevent asthma or eczema at the age of 2 years for children at high risk.[347] School-based programs that target asthma self-management are associated with improved asthma outcomes, fewer ED visits, fewer hospitalizations, and fewer days of reduced activity.[348]
Precautions during viral pandemics
During the occurrence of viral infection pandemics, precautions related to infection-control measures that include hand-washing, social distancing, optimizing asthma control, and minimizing use of nebulization as the mean of drug delivery to reduce the risk of droplet generation are of extreme importance. Referral to specific guidelines by local and international experts on this task is recommended. The SINA has released specific advices on asthma management of adult and children during the COVID-19 pandemic.[349,350] Expert SINA panel advises to continue routine care for patient with acute exacerbation of bronchial asthma and to follow the regular clinical guideline including early.
Outpatient management of asthma in children
Management of asthma should be adjusted continuously based on asthma control. If current treatment did not achieve control, then treatment is recommended to be stepped up until control is achieved. Whenever control is maintained for at least 3 months, then treatment can be stepped down. This stepwise approach is essential to maintain optimum control with lowest step to maximize safety and minimize cost. The SINA panel recommends ensuring consistency in the approach of asthma in adults, adolescents, and children. Therefore, outpatient treatment will be described in three phases: initiation, adjustment, and maintenance. The recommendations in the following sections are further stratified based on age groups: <5 years and ≥5 years.
Initiation of asthma treatment in children
Before initiating asthma treatment in children, it is recommended to ensure availability of initial clinical assessment data, such as the status of asthma control, assessing for risk factors, obtaining C-CAT score for children aged ≥5 years, and obtaining TRACK score for children <5 years. It is also recommended to provide teaching of inhalers technique and action plan. The SINA panel recommends placing the child on one of the steps based on the common clinical scenarios described below:
-
Step 1: The following are considerations to initiate asthma treatment at Step 1:
- SABA as needed (such as salbutamol) for a child with minimal symptoms (less than twice a week) that qualify for a controlled status based on physician assessment that is equivalent to a C-ACT score of ≥20 or TRACK score of >80
- An alternative option for children aged >5 years is as-needed use of ICS whenever SABA is required or daily low-dose use of ICS.[333]
-
Step 2: Personalizing the treatment options for children in step 2 is stratified based on asthma phenotype, assessment of aeroallergen sensitization, and determining the eosinophil count. Positive sensitization and high eosinophil count may favor ICS as a primary controller intervention.[354] The following are recommended:
- For child aged >5 years, daily low-dose ICS is the preferred option; however, daily LTRA or as-needed use of ICS whenever SABA is required is an alternative and less effective controller option for step 2[110]
- Low-dose ICS for a child <5 years with a history of asthma attack in the past year or has ever been admitted to the ICU[361]
- In addition to a low-to-moderate dose of ICS, a short course of oral prednisolone is recommended to be considered for a child aged 5–12 years with early signs of asthma attack at presentation
Step 3: For a child <5 years with more persistent symptoms that are considered to be an uncontrolled status based on physician assessment, it is recommended to commence treatment on double dose of ICS.[362,363]
Adjustment of asthma treatment in children
Before treatment adjustments, it is recommend to assess adherence to treatment, proper device use, control of environment, and confirmation of the diagnosis, especially if there is a failure to respond to therapy.[364] For a child seen in the clinic for the first time while on controller treatment, the managing physician should ensure that the child is receiving the appropriate treatment based on the recommendations given in the section on treatment initiation. Adjustment of therapy is recommended after 1–3 months depending on the level of asthma control upon presentation and the C-ACT score for children aged 5–12 years or TRACK score for children aged <5 years. Based on the clinical assessment and the level of asthma control, the following are recommended:
A child with uncontrolled asthma: escalation of treatment to at least the next step
A child with controlled asthma: treatment is recommended to be maintained at the same step; however, stepping down may be considered during low seasons for asthma attacks.
The SINA panel recommends the following concepts of treatment adjustment based on age in the following section.
Children aged 5–12 years
If control is not achieved after initiation of therapy for a child aged 5–12 years, the following are recommended [Box 9.10]:
Box 9.10.
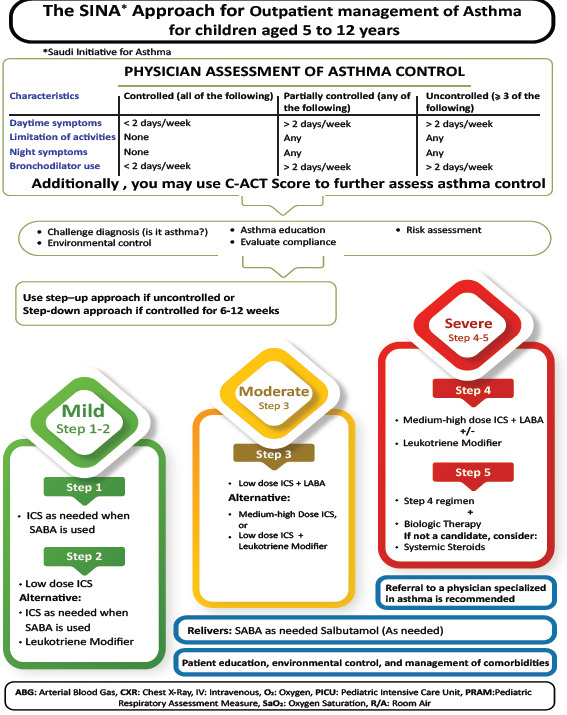
Outpatient management of asthma for children aged 5–12 years
Uncontrolled asthma at step 1: The preferred option is escalating to step 2 with low-dose ICS (step 2) (Evidence A).[321,322] Alternatively, either daily LTRA or as needed, use of ICS whenever SABA is required is a less effective option for step 2 in this age group[110]
Uncontrolled asthma at step 2: Escalation of treatment to step 3 by adding LABA to low-dose ICS (Evidence A).[133] Alternatively, LTRA can be added to low-dose ICS or the dose of ICS escalated to moderate dose (Evidence A)[365,366,367,368,369,370]
Uncontrolled asthma at step 3: It is recommended to escalate to step 4 by changing the combination inhaler to medium dose of ICS/LABA (step 4). LTRA may be added to this combination if control is not achieved. Whenever there is a difficulty to control asthma at step 4, it is strongly recommended to refer a patient to a physician specialized in asthma for further evaluation
-
Uncontrolled asthma at step 4: At this step, it is recommended to refer the child to a physician specialized in asthma as there is growing evidence to support other lines of biological therapy for children with uncontrolled asthma at step 4.[371,372] The following are the SINA recommendations for biological therapy at step 5 for this age group:
- Anti-IgE therapy is a well-established therapy in children aged ≥6 years with uncontrolled asthma at step 4 who fulfill the following criteria: children with severe persistent allergic asthma with frequent daytime symptoms or night-time awakenings, and who have multiple documented severe asthma attacks despite daily combination of high-dose ICS and LABA (Evidence A).[373,374] However, this line of management is recommended to be restricted to physicians specialized in asthma (Evidence C)[371,372]
- Mepolizumab is an anti-IL-5 agent approved for children aged ≥6 years (Evidence A)[375,376] that is indicated when eosinophil level is ≥150 cells/μL at treatment initiation or ≥300 cells/μL at any time in the prior 12 months. The dose of 40 mg for patients 6–11 years of age is subcutaneous every 4 weeks
Specific immunotherapy in pediatrics: They are limited data, but it can be used for children >5 years of age and was shown to reduce long-term asthma medication use and improve FEV1 as detailed in immunotherapy subsection.[190] It should be initiated by an asthma and allergy specialist.
Children aged <5 years
If control is not achieved after initiation of therapy for a child aged 5–12 years, the following are recommended [Box 9.11]:
Box 9.11.
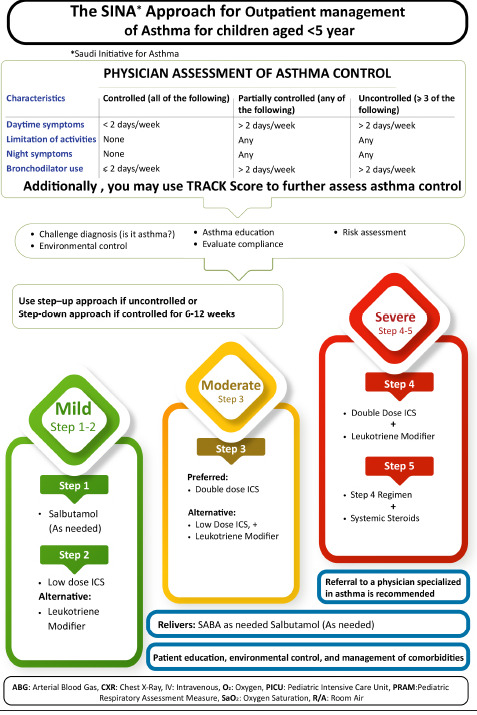
Outpatient management of asthma for children aged <5 years
Uncontrolled asthma at step 1: The preferred option is to escalate to step 2 with low-dose ICS (Evidence A)[321,322]
Uncontrolled asthma at step 2: It is recommended to escalate treatment to step 3. The recommended option is to double the dose of ICS (Evidence A).[368,377,378] Alternatively, adding LTRA to low-dose ICS is another option although this is considered as less effective[362,363]
Uncontrolled asthma at step 3: It is recommended to escalate treatment to step 4 by the addition of LTRA to moderate-dose ICS (Evidence B).[379,380,381] There is no evidence to support the use of LABA for patients younger than 5 years
Uncontrolled asthma at step 4: it is strongly recommended to refer patient to a physician specialized in asthma for further evaluation and options in step 5. However, to date, there is no evidence to support the use of either LABA or biological therapy in children <5 years. It is recommended to provide the caregiver an asthma action plan and a follow-up visit in 1–3 months depending on clinical status. Uncontrolled asthma in preschool children can lead to developmental disadvantages due to the negative impact of uncontrolled asthma on their social interaction and sleep. Caregivers of preschool children should be educated that asthma control is an achievable target and affected children should not be prevented from engagement in age-appropriate activities.
Maintenance of asthma treatment in children
On follow-up, it is recommended to perform a full clinical assessment including asthma control status and obtaining C-ACT score for children aged 5–12 years or TRACK score for children aged <5 years. Patient is recommended to be clinically assessed regarding medications and doses, compliance to treatment, accuracy of inhalers technique, and any related environmental factors. Based on clinical assessment and asthma control status, the SINA panel recommends the following:
Step up treatment for children who are uncontrolled based on physician assessment and complemented by a C-ACT score of ≤19 for a child aged 5–12 years or TRACK score of ≤80 for a child aged <5 years. It is recommended to rule out any modifiable factors preventing reaching optimal asthma control
Maintain treatment for children who reached controlled status based on physician assessment complemented by a C-ACT score of ≥20 for a child aged 5–12 years or TRACK score of >80 for a child aged <5 years
Consider stepping down treatment for children who are controlled for at least 3 months.
Reduction in therapy is recommended to be gradual and closely monitored based on clinical judgment complemented by either C-ACT or TRACK score. Furthermore, close monitoring on treatment stepping down is recommended for patient who has risk of asthma attack, especially during seasonal variation or for those with prior acute asthma attack in the past year or history of ICU admission.
The SINA expert panel recommends the following concepts for stepping down treatment based on age.
Children aged 5–12 years [Box 9.10]
If the patient is on ICS as monotherapy, the dose of ICS may be reduced by 25%–50% every 3–6 months to the lowest possible dose that is required to maintain control (Evidence B).[177,178,179] It should be clearly explained to the patient and/or caregiver that asthma control may deteriorate if treatment is abruptly discontinued.[180] In such a situation, an action plan that contains instruction on resuming controller therapy if asthma symptoms recurred are recommended to be provided to patients and their caregiver.
If the patient is on combination of ICS/LABA at step 3 or 4, abrupt discontinuation of LABA may lead to deterioration of asthma control[181]
If the patient is on a combination of ICS with LABA or LTRA, taper ICS to the lowest possible dose (Evidence B).[182,183] If control is maintained, LABA or LTRA may then be discontinued (Evidence D)[182]
For significant local side effects of ICS, consider a change in therapy, reduction in the dose, or frequency of ICS (if possible), advice for a vigorous mouth washing after inhalation, enforce use of MDI with spacer, and/or enforce use of appropriate local antifungal therapy for severe oral thrush[184]
For patients on continuous oral steroids, the dose is recommended to be tapered to the lowest dose and preferably to every other day (Evidence D). It is recommended to refer the child to a specialized physician in asthma management.
Children aged <5 years [Box 9.11]
The need for continuation of ICS should be regularly assessed as wheeze improves in a significant portion of children[382]
If the patient is on ICS as monotherapy, the dose of ICS may be reduced by 25%–50% every 3–6 months to the lowest possible dose that is required to maintain control (Evidence B).[177,178] It is recommended to be clearly explained to the caregiver that asthma control may deteriorate if treatment is abruptly discontinued.[180] If asthma symptom is recurred, an action plan that contains instruction on resuming controller therapy is recommended to be provided to patients and their caregiver. Consultation with a healthcare provider is recommended if control is not achieved
For significant side effects, consider a change in therapy, reduction in the dose, or frequency of ICS (if possible), advice for a mouth washing after inhalation if possible, enforce use of MDI with spacer, and/or enforce use of appropriate local antifungal therapy for severe oral thrush[184]
Uncontrolled asthma in preschool children can lead to developmental disadvantages due to the negative impact of uncontrolled asthma on their social interaction and sleep. Caregivers of preschool children are recommended to be educated that asthma control is an achievable target and affected children should not be prevented from engagement in age-appropriate activities.
Referral to an asthma specialist
Referral to an asthma specialist for consultation or comanagement is recommended in the following situations:
There is uncertainty regarding the diagnosis
There is difficulty achieving or maintaining control of asthma
Biological therapy or immunotherapy is being considered
The patient requires step 4 care or higher
The patient has had an asthma attack requiring a hospitalization or two or more OCSs in the past 12 months.
Section 10: Management of Acute Asthma in Children
Early recognition of acute asthma
Recognition of early signs of acute asthma is essential especially for those <5 years. Early symptoms of acute asthma include (Evidence D):
An attack of shortness of breath with wheeze or increase of shortness of breath with wheeze
Cough, especially at night although this is nonspecific
Impairment of daily activity
An increased need for or poor response to SABA
For a child <2 years, the presence of lethargy and poor feeding should raise the suspicion of acute asthma attack. However, viral bronchiolitis is a common differential diagnosis in this age group during winter season.
In a child aged 2–5 years, the combination of the above features can predict approximately 70% of acute asthma attacks with low false-positive rate.[383] Moreover, upper respiratory tract infection (URTI) may frequently precede acute asthma attack in children. Clinical assessment is essential in children as the utilization of objective measure such as PFT is problematic, especially in the younger age groups.
Initial management of acute asthma at home
The SINA panel recommends the management of a child with asthma to include an action plan that enables the caregiver to recognize worsening of asthma and the advices for initial treatment. The action plan is recommended to include features that mandate the need for urgent medical care that includes acute distress of the child, difficulty to complete few words in one breath, and poor response to SABA treatment at home.
In the case of acute attack, initial management at home by the caregiver is recommended to be started with salbutamol inhaler 2–4 puffs by a spacer that may be repeated every 20 min for a total of three doses. If the child improves, asthma therapy is recommended to be stepped up as per instructions in the action plan and medical advice should be sought as soon as possible.
Immediate transfer to hospital
If the child does not adequately improve within or after the initial period, urgent medical care is recommended. [Box 10.1] shows the indications for immediate transfer to hospital for children with acute asthma exacerbation.
Box 10.1.
Description of indications for immediate transfer to hospital for children with acute asthma exacerbation
| Indications | Description |
|---|---|
| Features of severe symptoms | Unable to speak and/or risk to chock with food or drink Bluish discoloration of lips and tongue (cyanosis)Rapid breathing >40/min for children <5 years of age Silent chest |
| Lack of response to rescuer treatment | Lack of response after 1-2 h of proper technique and dosage |
| Limitation to deliver acute treatment | Social, family, or environmental reasons |
During the transfer to hospital, rescuer treatment (inhaled SABA) should be provided as well as oxygen supply (to maintain saturation >94%). In addition to consideration to give the first dose of systemic corticosteroid, instant communication with specialized call center is recommended to provide the required consultations.
Assessment of asthma severity in the emergency department
Assessment of acute asthma severity in children has an important role in various components of acute asthma management, such as pharmacological interventions, need for hospitalization, and need for ICU admission. The assessment of acute asthma severity in young children is also important for clinical decision-making and evaluation of treatment effectiveness.[67,102,384,385,386,387] This is supported by the fact that PFT measurement is not feasible as more than half of asthma attacks in children presented to EDs for children <5 years.[388]
Pediatric respiratory assessment measure (PRAM) has been found to be feasible, valid, responsive, and reliable tool to determine acute asthma severity in children aged 2–17 years.[388,389] The PRAM represents a useful means to record clinical signs in a standardized fashion [Box 10.2].[67] The PRAM score is a 12-point score consisting of oxygen saturation, suprasternal retractions, scalene muscle contraction, air entry, and wheezing.[386] Clinical pathways based on PRAM for inpatient asthma management have been shown to decrease the length of stay and bronchodilator use with no adverse outcomes or increased acute care encounters.[390,391] The SINA panel recommends measuring PRAM score for asthmatic patients in emergency as it can categorize the risk of hospitalization:
Box 10.2.
The pediatric respiratory assessment measure score
| Sign | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Suprasternal retraction | Absent | Present | ||
| Scalene muscle contraction | Absent | Present | ||
| Air entry | Normal | Decreased at bases | Widespread decreased | Absent/minimal |
| Wheezing | Absent | Expiratory only | Inspiratory and expiratory | Audible without stethoscope/silent chest with minimal air entry |
| O2 saturation (%) | ≥95 | 92-94 | <92 |
Total score of 1–3: low risk with a chance of <10% for hospital admission
Total score of 4–7: moderate risk with a chance of 10%–50% for hospital admission
Total score of 8–12: high risk with a chance of >50% for hospital admission.
Management of acute asthma in the emergency department
Management of acute asthma exacerbation in the ED should target the following goals:[392]
Rapid reversal of bronchospasm
Correction of hypoxemia if present
Reducing the need for hospitalization
Preventing recurrence of the attack after discharge.
After performing the necessary clinical assessment, the SINA expert recommends the utilization of PRAM as a tool to assess patients in the ED and guide further management as well. The PRAM score should be obtained at the initial assessment and after initiation of treatment as well. After initial clinical assessment and starting initial appropriate therapy, managing physician is recommended to focus on obtained history to identify risk factors for ICU admission, including:[393]
Previous life-threatening asthma attack
Previous ICU admission
Previous intubation
Deterioration while already on systemic steroid.
In addition, managing physician is recommended to be aware of the following clinical features of severe or life-threatening asthma that required immediate medical attention:
Child is unable to speak or drink
Central cyanosis
Confusion or drowsiness
Significant subcostal or subglottic retraction
Oxygen saturation <92%
Silent chest on auscultation
Tachycardia.
Implementation of clinical pathway that utilizes PRAM score for acute asthma management in children with moderate-to-severe asthma attacks markedly decreases the rate of hospitalization without increasing the rate of return to emergency care (Evidence B) [Box 10.3].[391,394,395,396] This has been supported by a study showing that PRAM score after 3 h of initial management was associated with a significant improvement in the prediction of admission rate compared to pure clinical judgment at triage.[389] Ancillary investigation that includes CXR and ABG is not routinely recommended.[393] ABG is indicated in severe bronchial asthma that failed to respond to maximum therapy and required ICU admission. However, CXR is recommended in the following conditions:
Box 10.3.
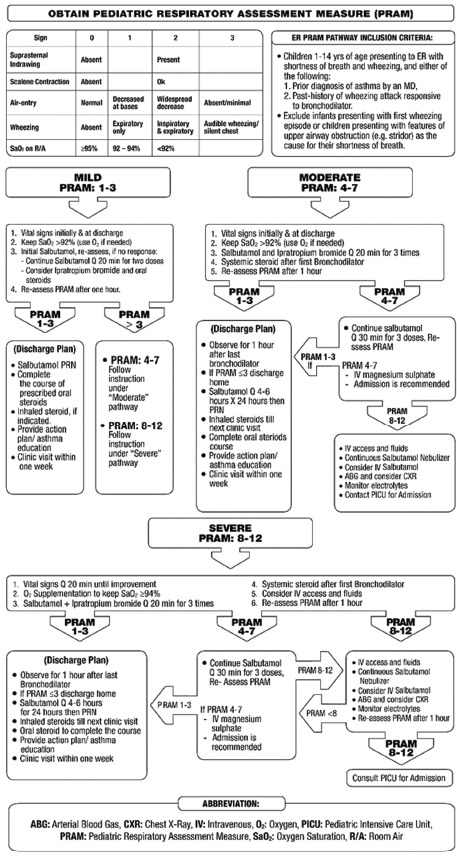
Assessment and treatment of acute asthma in children
Suspected bacterial pneumonia that presents with fever >39°C and presence of focal finding of decreased breath sound and crackles
To rule out bronchial asthma complications such as pneumothorax
Severe disease that does not respond to maximum treatment
Uncertainty about the diagnosis
Hypoxemia apparently disproportionate to the attack severity.
Viral infection is the usual cause of asthma attacks in children, and thus, routine use of antibiotics is strongly discouraged.[397] Antibiotics are recommended when bacterial pneumonia is clinically suspected.[394,395]
Acute asthma management based on pediatric respiratory assessment measure
The SINA panel recommends managing asthma based on PRAM score obtained at initial assessment:
Mild - Pediatric respiratory assessment measure score of 1–3
the initial management includes
Obtain vital signs initially and at discharge
Prescribe appropriate oxygen dose to keep saturation ≥92%
-
Salbutamol dose based on weight:[339,398]
- Less than 20 kg: 5 puffs by MDI/spacer or 2.5 mg by nebulizer
- 20 kg or more: 10 puffs by MDI/spacer or 5 mg by nebulizer titrate MDI dose based on response)
- In mild cases, SABA with spacer is not inferior to nebulized SABA.
Ipratropium bromide may be considered at a dose of 4 puffs by MDI with spacer or 250 mcg by nebulizer every 20 min for the 1st h only[399]
Consider oral steroids if there is no response to the first dose of salbutamol. Prednisolone dose is 1–2 mg/kg up to a maximum dose based on age. The maximum dose is 20 mg for children aged <2 years, 30 mg for children aged 2–5 years, and 60 mg for children aged 5–12 years. Dexamethasone dose of 0.6 mg/kg up to maximum dose of 16 mg[400]
Re-assess PRAM after 1 h.
Management after initial treatment based on pediatric respiratory assessment measure score
-
PRAM score is 1–3: The management includes:
- The child may be discharged on salbutamol inhaler and ICS inhaler with a spacer
- If oral steroids course is given initially, dexamethasone is recommended for extra 1 day and prednisolone for a total of 3–5 days
- It is recommended to offer the child an action plan, education on inhalers technique, and a follow-up visit within 1 week to the appropriate clinic
PRAM score is 4–7: Treat as a moderate asthma attack (see below)
PRAM score is 8–12: Treat as a severe asthma attack (see below).
Moderate - Pediatric respiratory assessment measure score of 4–7
The management includes:
Obtain vital signs
Prescribe appropriate oxygen dose to keep saturation ≥92%
The combination of salbutamol and ipratropium bromide has been shown to be effective in this situation (Evidence B)[398]
Systemic steroids after the first dose of SABA. Prednisolone dose is 1–2 mg/kg up to a maximum dose based on age. The maximum dose is 20 mg for children aged <2 years, 30 mg for children aged 2–5 years, and 60 mg for children aged 5–12 years. Dexamethasone dose of 0.6 mg/kg up to maximum dose 16 mg.[400,402]
Re-assess PRAM after 1 h
If PRAM score after 1 h is 1–3, observe for another hour.
Management after initial treatment based on pediatric respiratory assessment measure score
-
PRAM score is 1–3
- The child may be discharged on salbutamol inhaler with a spacer and ICS if the patient is not already on controller treatment
- Complete the course of oral steroids. Dexamethasone is recommended for extra 1 day and prednisolone for total of 3–5 days, both as once daily dose
- It is recommended to offer the child an action plan, education on inhalers technique, and a follow-up visit within 1 week to the appropriate clinic.
-
PRAM score is 4–7: It is recommended to continue treatment with salbutamol every 30 min for three doses and to assess PRAM score every 30 min. Further evaluation is based on the PRAM re-assessment:
- If PRAM score improves to 1–3, the child can be managed as above.
PRAM score is 8–12: treat as severe asthma attacks (see below).
Severe - Pediatric respiratory assessment measure score of 8–12
The management includes:
Obtain vital signs every 20 min until improvement
Prescribe appropriate oxygen dose to keep saturation ≥94%.
Salbutamol nebulizer at a dose of 2.5 mg for those weighted <20 kg or 5 mg for those weighted ≥20 kg and ipratropium bromide at a dose of 250 mcg by nebulizer every 20 min for the 1st h.[398,399,401,399] This combination has been shown to be effective in this situation (Evidence B)[398]
Systemic steroids after the first dose of SABA. Prednisolone dose is 1–2 mg/kg up to a maximum dose based on age. The maximum dose is 20 mg for children aged <2 years, 30 mg for children aged 2–5 years, and 60 mg for children aged 5–12 years. Dexamethasone dose of 0.6 mg/kg up to maximum dose 16 mg[400,402]
Re-assess PRAM after 1 h
Consider IV access and appropriate IV fluids
If PRAM score after 1 h is 1–3, Observe for another hour.
Management after initial treatment based on pediatric respiratory assessment measure score
-
PRAM score is 1–3
- The child may be discharged on salbutamol inhaler with a spacer and ICS if the patient is not already on controller treatment
- It is recommended to offer the child/caregiver an action plan, education on inhalers technique, and a follow-up visit within 1 week to the appropriate clinic.
-
PRAM score is 4–7: It is recommended to continue treatment with salbutamol every 30 min for three doses and to assess PRAM score every 30 min. Further evaluation is based on PRAM re-assessment:
- If PRAM score improves to 1–3, the child can be managed as above
-
PRAM score is 8–12: Deterioration of clinical status despite adequate treatment in the initial period warrants special care and attention. It is recommended to:
- Establish IV access and to start on appropriate IV fluids
- If PRAM score does not improve, IV magnesium sulfate is recommended as a single dose of 40–50 mg/kg to a maximum of 2 g by slow IV infusion over 20–30 min
- ABG, CXR, and electrolyte are recommended to be obtained and the pediatrics critical care or equivalent service must be consulted.
Advice related to coronavirus 2019 pandemic
Based on the available evidence at the time of preparing this document, asthma is not considered to be a strong risk factor for severe COVID-19 disease.[408,409] The expert SINA panel advises to continue routine care for patient with acute exacerbation of bronchial asthma and to follow the regular clinical guideline including early administration of systemic glucocorticoid therapy if indicated. The SINA expert panel recommends the avoidance of nebulization unless clinically indicated as it is considered an aerosol-generating procedure that may lead to disease spread.[409] It is recommended to commence therapy with MDI with spacer and switch to nebulizer therapy only if child has moderate-to-severe disease with poor response to MDI under strict precaution measures as per hospital.
Section 11: Appendix of Medications Used in Asthma Treatment
The objective of asthma treatment is to achieve and maintain control of the disease. Medications used to treat asthma can be classified as controllers or relievers. Controllers are medications taken daily on a long-term basis to keep asthma under clinical control.[410] Relievers are medications used on an “as-needed basis” that acts quickly to reverse bronchoconstriction and relieve symptoms.
Anti-inflammatory controller medications
Inhaled corticosteroids
ICSs are currently the most effective anti-inflammatory medications for the treatment of asthma.[47,107,411] They reduce symptoms, improve quality of life, improve lung function, decrease AH, control airway inflammation, reduce frequency and severity of asthma attacks, and reduce asthma mortality. Early initiation of low-dose ICS in asthma leads to improvement in lung functions.[123] When they are discontinued prematurely or abruptly, deterioration of clinical control follows within weeks to months in most patients. ICSs differ in their potency and bioavailability. Most of the benefits from ICS are achieved in adults and children at relatively low doses [Boxes 11.1 and 11.2].[1] Exposure to tobacco smoking or vaping, including secondary and tertiary, reduces the responsiveness to ICS. To reach control, add-on therapy with another class of controller is preferred to increase the dose of ICS.[141,412]
Box 11.1.
List of inhaled corticosteroids for adults and adolescent and daily recommended doses*
| Drug (doses in mcg)** | Low dose | Medium dose | High dose |
|---|---|---|---|
| Beclomethasone dipropionate (standard particles, HFA) | 200-500 | >500-1000 | >1000 |
| Beclomethasone dipropionate (extra fine particles, HFA) | 100-200 | >200-400 | >400 |
| Budesonide (DPI) | 200-400 | >400-800 | >800 |
| Ciclesonide (Extra fine particles, HFA) | 80-160 | >160-320 | >320 |
| Fluticasone propionate (DPI and HFA) | 100-250 | >250-500 | >500 |
| Mometasone furoate (DPI) | 100 | 100 | 200 |
*Adapted from reference,[1] **Based on availability in the Saudi Market for children. DPI: Dry powder inhaler, HFA: Chlorofluoroalkane propellant
Box 11.2.
List of inhaled corticosteroids inhalers and daily recommended doses*
| Drug (doses in mcg)** | <5 years Low dose | Children above 5 years |
||
|---|---|---|---|---|
| Low dose | Medium dose | High dose | ||
| Beclomethasone dipropionate (standard particles, HFA) | 100 | 200-500 | >500-1000 | >1000 |
| Beclomethasone dipropionate (extra fine particles, HFA) | 50 | 100-200 | >200-400 | >400 |
| Budesonide | 200 | 200-400 | >400-800 | >800 |
| Budesonide (Nebules) | 500 | 250-500 | >500-1000 | >1000 |
| Ciclesonide | Not applicable | 80-160 | >160-320 | >320 |
| Fluticasone propionate (DPI) | Not applicable | 100-250 | >250-500 | >500 |
| Fluticasone propionate (HFA) | 50 | 100-250 | >250-500 | >500 |
| Mometasone furoate | 100 | 200-400 | 200-400 | >400 |
*Adapted from reference,[1] **Based on availability in the Saudi market for children. DPI: Dry powder inhaler, HFA: chlorofluoroalkane propellant
Local adverse effects can occur and include oropharyngeal candidiasis and dysphonia; with MDI, these effects are reduced by using a spacer device. Mouth and throat washing after inhalation may reduce oral candidiasis. The small risk of adverse events from the use of ICS is well balanced by their efficacy.[413] Therefore, low–medium dose of ICS is generally safe and well tolerated in adults and children. Formulations with small size particles are believed to be more effective and safer as it leads to better deposition in the peripheral small airways.[414,415] Some studies have shown that ciclesonide had relatively lower local and systemic side effects, especially in children.[416] Systemic side effects are occasionally reported with high doses and long-term treatment.
Special considerations for use of inhaled corticosteroids in children
Growth retardation may be seen with all ICSs when a high-dose ICS is chronically used. Systematic reviews showed a reduction may affect height velocity in prepubertal children over 12 months' use of low-to-medium dose of ICS, especially during the 1st year of life.[417] Although this effect was statistically significant and sustained during adult life, it is not clear if that will be of significant clinical impact.[418,419] For instance, the use of moderate-dose ICS resulted in 1.2 cm reduction in the final adult height after more than 4 years use.[420] Moreover, more studies demonstrated the negative impact of medium-to-high-dose ICS on bone mineralization.[421,422,423] However, it is crucial to remember that long-term use of ICS is safer than frequent bursts of oral corticosteroids on bone mineralization. Adequate nutrition with sufficient intake of calcium and Vitamin D can blunt these effects.[424] In summary, the potential adverse effects of ICS need to be weighed against the well-established benefit to control persistent asthma. Therefore, it is important to target the lowest possible ICS dose that maintains adequate asthma control.
Leukotriene modifiers
Leukotriene-modifying agents reduce airway inflammation and improve asthma symptoms and lung function, but with a less consistent effect on asthma attacks, especially when compared to ICS. They may be used as an alternative treatment to ICS for patients with mild asthma, especially in those who have clinical rhinitis. Some patients with ASA-sensitive asthma respond well to the LTRA. However, when used alone as a controller, their effects are generally less than that of low-dose ICS. When added to ICS, LTRA may reduce the dose of ICS required by patients with uncontrolled asthma and may improve asthma control.[425,426] LTRAs are generally well tolerated, however; it is recommended to be aware of the FDA warning about serious behavior and mood-related changes with Montelukast.[161] In children, studies have shown that LTRA may be useful for reducing the number of asthma attacks induced by viruses and for reducing bronchial inflammation in atopic children.[427,428,429,430] There are no clinical data to support their use under the age of 6 months.[161]
Other controller medications
Long-acting inhaled β2-agonists
The commonly used long-acting inhaled β2-agonists, formoterol and salmeterol, are used on a twice daily basis. Vilanterol, indacaterol, and olodaterol are LABA agents with a 24-h duration of action.[431,432,433,434,435,436,437] Due to lack of anti-inflammatory effect, LABA should not be used alone as monotherapy in asthma as this can lead to increased mortality, and indeed, they should only be prescribed in combination in the same device with ICS. When used in combination with ICS, there are improvement in symptoms, decreased nocturnal asthma, improved lung function, decreased use of inhaled β2-agonists, reduced number of asthma attacks, and better control at a lower dose of ICSs. LABA provides longer protection to prevent exercise-induced bronchospasm than short-acting inhaled β2-agonists (SABA).[438] Their side effects are limited to tachycardia, tremor, headaches, muscle cramps, and sometimes hypokalemia. Regular use of LABA combined with ICSs may lead to a reduction in their side effects. Furthermore, patients rarely develop tolerance to LABA. The effect of LABA has not been adequately studied in children of <5 years.
Long-acting antimuscarinic agents
LAMAs inhibit the effect of acetylcholine on M3 receptors, thus producing bronchodilation. LAMAs are classically used for the treatment of COPD patients. When studies in asthma patients, the users of LAMAs (tiotropium bromide, aclidinium bromide, umeclidinium bromide, and glycopyrronium) were found to be of higher age at asthma onset, higher annual exacerbation rates, and worst asthma control.[439,440] Tiotropium bromide is the first LAMA extended for use in asthma. Its bronchodilation duration of action of more than 24 h allows for single daily dosing.[441,442] The earlier studies on tiotropium were conducted using the Handihaler© device, while the more recent studies were conducted using the new Respimat device. To date, tiotropium is mainly available in the Saudi Market in the Handihaler device in an 18-mcg capsule format while the Respimat device has not been widely available. Tiotropium was shown to be an effective stepping up strategy when added to a combination of ICS/LABA[443] and not inferior to LABA as an add-on to a medium-dose ICS.[147,148,157,444] Adding LAMA can significantly improve lung function in uncontrolled cases and reduce attacks (Evidence A).[146,156,157] Recently, once a day, triple therapy of umeclidinium bromide, fluticasone bromide, and vilanterol received the USA FDA approval for the treatment of asthma.[445] The main side effect of LAMA is dryness of mouth, although mild prostatic symptoms have been reported.
Theophylline
Theophylline is a weak bronchodilator with the modest anti-inflammatory properties. It may provide benefits as an add-on therapy in patients who do not achieve control with ICS alone but is less effective than LABA or LTRA. Theophylline is not recommended for use as monotherapy in asthma treatment. Low-dose theophylline (300 mg/day) may have a role in improving steroid resistance in patients with severe asthma requiring high-dose ICS.[446,447] Side effects include gastrointestinal symptoms, cardiac arrhythmias, seizures, and even death. Nausea and vomiting are the early symptoms of toxicity. Liver disease and CHF may increase the risk of toxicity. Use of lower doses may decrease these side effects. Theophylline has drug interaction with quinolones and some macrolides that may increase the risk of toxicity. Currently, it is very rarely used in treating asthma.
Oral β2-agonists
The side effect profile is much higher than that of inhaled β2-agonists. Therefore, their use is highly discouraged in asthma management. Oral route is not recommended in children.
Cromones
Cromones (sodium cromoglycate and nedocromil sodium) are not recommended for preschool children. They have limited role in the long-term treatment of older children. Evidence showed that low-dose ICS is superior to cromones in the management of asthma.[448] They are no longer available as an option to treat asthma.
Combination therapy with inhaled corticosteroids and long-acting bronchodilator
Fixed combination of ICS and LABA is considered more convenient for patients. Combination therapy is generally safe and did not result in a significantly higher risk of serious asthma-related events than treatment with an inhaled glucocorticoid alone but resulted in significantly fewer asthma attacks.[135] They increase adherence and ensure that LABA is always accompanied by ICS. Although salmeterol and formoterol provide a similar duration of bronchodilation and protection against bronchoconstriction, formoterol has a more rapid onset of action than salmeterol. Therefore, combination inhalers containing formoterol may be used for both rescue and maintenance of control.[112,135] Recent studies compared as-needed budesonide–formoterol with as-needed SABA alone or in combination with daily maintenance budesonide in mild asthmatics showed that budesonide–formoterol used as needed was noninferior to budesonide maintenance therapy for severe exacerbations but at 17% to 25% the dose of ICS in the maintenance therapy at the expense of a small, but significant, change in asthma control score in favor of budesonide maintenance therapy. ICSs are now recommended to start from step 1 either as ICS (evidence mainly in budesonide) formoterol combination on as-needed basis or in a separate inhaler every time rescue treatment SABA is needed.[113,114,449] Fixed combination inhalers of ICS and LABA are available in different devices in the Saudi Market [Box 11.3].[450,451,452,453] Once-a-day dry powder combination of ICS/LABA with fluticasone furoate and vilanterol (Relvar) is available in two strengths of 100/25 and 200/25 mcg with dispensed equivalent dose of 92/22 and 184/22 mcg, respectively.[139,140] The dose of fluticasone furoate of 100 mcg is approximately equivalent to fluticasone propionate 250 mcg.[454] Such a combination has a potential adherence advantage while maintaining the same safety as the combination of fluticasone propionate and salmeterol.[455]
Box 11.3.
List of fixed combinations of inhaled steroid and long-acting β2 agonists
| Inhaled steroid (doses in mcg) | Long-acting β2 agonist (doses in mcg) | Brand name | Device type | Device name |
|---|---|---|---|---|
| Beclomethasone (100) | Formoterol (6) | Foster® | MDI | |
| Budesonide (80,160, 320) | Formoterol (4.5, 9) | Symbicort® | DPI | Turbuhaler™ |
| Budesonide (200, 400) | Formoterol (6, 12) | Pulmoton® | DPI | Elpenhaler™ |
| Fluticasone propionate (50, 125, 250) | Salmeterol (25) | Seretide® | MDI | Evohaler™ |
| Fluticasone propionate (100, 250, 500) | Salmeterol (50) | Seretide® | DPI | Diskus™ |
| Fluticasone furoate (100, 200) | Vilanterol (25) | Relvar® | DPI** | Ellipta™ |
| Fluticasone propionate (50,125,250) | Formoterol (5,10) | Flutiform® | MDI | |
| Fluticasone propionate (250, 500) | Salmeterol (50) | Rolenium® | DPI | Elpenhaler™ |
| Mometasone furoate (100) | Formoterol (5) | Dulera® | MDI |
*Based on availability in the Saudi market for children, **Once-a-day combination. MDI: Metered dose inhaler, DPI: Dry powder inhaler
Triple therapy with inhaled corticosteroids, long-acting bronchodilator, and long-acting antimuscarinic agent
Fixed combination inhalation devices are considered more convenient for patients.[456] Triple therapy of ICS, LABA, and LAMA was first introduced for COPD treatment. The first approved triple therapy for asthma is the once-a-day combination of fluticasone furoate, umeclidinium, and vilanterol (Trelegy Ellipta®). It is available in two formats where one inhalation contains fluticasone furoate 100 mcg, umeclidinium 62.5 mcg, and vilanterol 25 mcg or one inhalation contains fluticasone furoate 200 mcg, umeclidinium 62.5 mcg, and vilanterol 25 mcg. In patients with uncontrolled moderate or severe asthma on a combination of ICS/LABA, adding umeclidinium was found to be an effective treatment option with favorable risk–benefit profile as it led to improved FEV1 and asthma symptoms but did not result in significant reduction in moderate and/or severe exacerbations.[155] A higher dose of fluticasone furoate (200 mcg) primarily reduced the rate of exacerbations, particularly in patients with raised biomarkers of type 2 airway inflammation. Other triple therapy combinations are approved for COPD treatment but not yet for asthma, such as the combination of budesonide 320 mcg, glycopyrronium 14.6 mcg, and formoterol fumarate 9.6 mcg (Breztri Aerosphere®) and the combination of mometasone furoate 160 mcg, glycopyrronium bromide 63 mcg, and indacaterol 150 mcg (Enerzair Breezhaler®).
Systemic corticosteroids
Long-term oral steroid therapy (excluding short courses for acute attacks of asthma for a period of 1–2 weeks) may be required to control difficult-to-treat asthma despite maximum standard therapy when biological agents cannot be used. The dose should be reduced to the lowest possible and other controllers are recommended to be maximized to minimize the side effects from the OCSs. Its use is limited by the risk of significant adverse effects. Use of intramuscular long-acting steroids is highly discouraged because of the increased risk of side effects. The side effects include osteoporosis, hypertension, diabetes, adrenal insufficiency, obesity, cataracts, glaucoma, skin thinning, and muscle weakness. Sudden withdrawal can elicit adrenal failure; therefore, gradual withdrawal is recommended. In patients prescribed long-term systemic corticosteroids, prophylactic treatment for osteoporosis is recommended. If available, biological therapy should be considered in these patients to decrease the corticosteroid burden.
Reliever medications
Relievers are medications used on an “as-needed basis” and act quickly to reverse bronchoconstriction and relieve symptoms.
Rapid-onset inhaled β2-agonists
SABAs, such as salbutamol, have been traditionally used for relief of symptoms of acute attacks of asthma and for the pretreatment of exercise-induced bronchoconstriction. Use of MDI with a chamber is as effective as the nebulized route in the treatment of acute episodes of wheeze in children.[457] Regular long-term use of SABA is not recommended. ICS/formoterol combination inhalers can be used alone on as-needed basis in patients with mild asthma or in combination with regular regimen in as-needed maintenance and reliever therapy approach in more symptomatic patients.[112,113,114] Vilanterol is another LABA used once a day that has a fast onset of action within 15 min and long half-life; hence, the patient should be advised to only use it once a day on a regular basis and not a rescue medication.[139,140] In acute asthma, inhaled salbutamol is the preferred choice.[458,459] Repeated doses are recommended to be given at 15–20 min intervals. Alternatively, continuous nebulization (salbutamol at 5–10 mg/h) could be used for 1 h if there is an inadequate response to initial treatment. However, a meta-analysis of randomized controlled trials of adults with acute asthma found no significant differences between the continuous or intermittent methods in terms of pulmonary function or hospital admission; nevertheless, patients treated by continuous nebulization had fewer side effects.[460] In patients who are able to use the inhaler devices, 6–12 puffs of MDI with a spacer is equivalent to 5 mg of salbutamol by nebulizer. As the inhaled route has a faster onset of action and fewer adverse effects, the use of IV β2-agonists in the initial treatment of patients with acute severe asthma is not generally recommended.[461] IV therapy should not be considered routinely if ever and only used cautiously if the response to the inhaled drug is poor or if the patient cannot tolerate the inhaled route.
Anticholinergics
Anticholinergics are less effective than SABA in asthma. However, when used in combination with SABA in acute asthma, they provide an additional benefit.[398] They can also be an alternative bronchodilator for patients who experience adverse effects, such as tachycardia, arrhythmia, and tremor from rapid-acting β2-agonists. Their side effects include dryness of the mouth and a bitter taste.
In moderate-to-severe acute asthma, combining ipratropium bromide with salbutamol was shown to have additional bronchodilation effect and faster improvement in lung function, compared to salbutamol alone.[462,463] A systematic review showed that the combination therapy has an added benefit in reducing hospitalizations.[464] Combining both agents led to reduction in hospital admission rates by 38%–57%, improvement in lung function, and substantial cost-saving.[463,465,466] No evidence of benefit for length of hospital stay and other markers of response when inhaled anticholinergics is added to short-acting β2-agonists in hospitalized asthmatic children with acute attacks.[467] The adult dosing of nebulized ipratropium bromide is 500 μg every 20 min for three doses, then as needed. Alternatively, ipratropium bromide can be administered by MDI at a dose of 4–8 puffs (80–160 μg) every 20 min, then as needed for up to 3 h.
Theophylline
There is no evidence supporting the routine use of theophylline in treating acute asthma and its routine use is discouraged. Similarly, routine use of IV aminophylline in acute asthma is strongly discouraged as there is no evidence to show added benefit and the drug has high levels of toxicity and side effects.[468]
Intravenous magnesium sulfate
In a systematic review, magnesium sulfate was shown to reduce hospitalizations in patients with severe or life-threatening asthma attacks that failed to respond to initial treatment.[469] A single dose of IV magnesium sulfate at a dose of 1–2 g over 20 min is safe and effective in acute severe asthma.[470]
Aerosol devices used in asthma
Medication aerosol can be delivered using three devices.
Small-volume nebulizer
Small-volume nebulizer (SVN) is the most popular for patients and clinicians in acute asthma. SVNs are predominately powered by a compressed gas (air or oxygen) to convert one or more drug solutions or suspensions at any concentrations and dose into aerosols. One of its main advantages is that it requires minimal patient cooperation and is therefore suitable for all ages, with normal breathing and no inspiratory pause required. One of its main disadvantages is importability, time to deliver the medication (10–25 min), and potential of contamination. There are high-output aerosol nebulizers that have an output rate of 30–50 mL/h and a flow rate of 10–15 L/min. It provides up to 8 h of continuous nebulization and has a 240 mL reservoir.
Pressurized metered-dose inhaler
It is a prepressurized inhaler with medication and a propellant, which when actuated will give one dose of the drug for a single inspiration. An MDI typically requires slow inspiratory flow (≤30 L/min). One of its main advantages is that it is premixed and the ability to provide multiple doses in a short period of time. It is also small and portable with limited contamination. Disadvantages include the need of patient training to coordinate inhalation with actuation, and if this is not done properly, there is a potential of high deposition of drug in the oropharynx and poor drug delivery. Furthermore, because it does not have dose counter, it is difficult to determine the dose remaining in the canister. Compared to the older chlorofluorocarbon propellant formulations, hydrofluroalkane formulations provide smaller particle size aerosols with less oral deposition, hence less oral side effects and greater proportion of lung deposition.
Dry powder inhaler
It is not pressurized (no propellant) and therefore requires high inspiratory flows (60–90 L/min) to disperse a full dose. In addition to its portability, advantages include easier inhaler technique and a built-in dose counter. Disadvantages include the need for adequate inspiratory flow to disperse a full dose. If not used properly, high oropharyngeal impaction may occur and exhaled humidity into mouthpiece might affect the function of some devices. Therefore, it may not be suitable for very young or very old patients. The commonly available devices in Saudi Arabia include Turbohaler, Diskus, Handihaler, Easi-Breathe, Ellipta, Easyhaler, and Nexthaler devices.
Breath-actuated inhalers
These inhalers automatically release a spray of medication when a person begins to inhale. They are easy to use and improve asthma control and compliance to medications.[471,472,473,474]
Biologics in asthma treatment
The recent progress in biologic therapy in asthma has made a step forward toward the practice of precision medicine for asthma patients. To date, there are no head-to-head studies to compare the available biologics with each other, neither between those with different targets nor between anti-IL-5 therapies themselves. In addition, due to a wide variability of the published clinical trials' inclusion criteria and analysis methodologies, it is also difficult to compare the efficacy of these therapies based on existing studies. This section describes the biologic agents that received appropriate approvals.[475]
Anti-immunoglobulin E
Omalizumab is a recombinant humanized monoclonal antibody against soluble IgE. It prevents binding of IgE to its high affinity receptor and subsequently lowers its expression and the activation of mast cells, basophils, and dendritic cells. Omalizumab is indicated for patients ≥6 years of age with severe allergic asthma (at least one positive aeroallergen on skin prick testing or an elevated specific aeroallergen IgE level) uncontrolled on high-dose ICS combined with LABA and other controllers and who have an IgE level of within therapeutic range. It was shown to reduce attacks, reduce hospitalizations, and allow stepping down of ICS dose.[476,477] Baseline IgE level does not predict response but is necessary, in addition to the weight, to calculate the dose that is administrated every 2–4 weeks.[478] However, the higher eosinophil count or FeNO, the better the response. Omalizumab also significantly reduces exacerbation rate in patients with severe eosinophilic asthma.[479] Repeating IgE level is not recommended to monitor the response as the level could go higher upon commencing anti-IgE therapy. Anti-IgE therapy is recommended to be stopped if no clinical response is observed in 4 months. The side effects include pain and bruising at injection site and very rarely anaphylaxis (0.1%). This drug requires careful monitoring and should only be initially prescribed by an expert physician in asthma treatment. There is an extensive experience with omalizumab of more than 15 years. It is classified as Category B for use in pregnant women based on the current cumulative experience. Therefore, it is not recommended to start omalizumab during pregnancy but can be continued for those who already use it if the benefit outweighs the risk.
Anti-interleukin 5
IL-5 is critical for eosinophil maturation, survival, and movement from the bone marrow to systemic circulation. Anti-IL-5 monoclonal antibodies treatment is directed to patients with severe eosinophilic asthma with two or more exacerbations in the past year and who have peripheral blood eosinophils count according to the specific anti-IL-5 agent. Anti-IL-5 therapy reduces exacerbations by 40%–60%, improves lung function, and allows for about 50% reduction in oral glucocorticoids maintenance treatment.[170,480,481] Patients with more severe disease and higher eosinophil counts are expected to benefit more.[482] Anti-IL-5 and anti-IL-5 receptor therapy reduced attacks by almost half and improved lung function in patients with severe, uncontrolled eosinophilic asthma, regardless of the serum IgE concentrations and atopy status.[483] As there are currently no data to guide when to stop anti-IL-5 therapy, the treatment may be continued for at least 4 months to judge efficacy and if effective at least 12 months before stopping and re-evaluation (Evidence D).[171] These medications should be avoided in patients with active helminthic infection. There are insufficient data regarding its use during pregnancy. There are currently three different anti-IL-5 medications in clinical use:
Mepolizumab binds circulating IL-5. Based on clinical trials, blood eosinophils should be >150/μL within the last 6 weeks or >300/μL within the last 12 months before starting. It is given as subcutaneous injections every 4 weeks at doses of 100 mg for patients ≥12 years and 40 mg for patients 6–11 years of age. Severe herpes zoster has been reported very rarely in some patients. Consider varicella vaccine before starting if clinically indicated
Reslizumab binds circulating IL-5. Based on clinical trials, blood eosinophils should be >400/μL before starting. It is approved for patients ≥18 years. It is given as monthly IV infusion at a dose of 3 mg/kg over 20–50 min.[484] Oropharyngeal pain and elevated creatine phosphokinase were reported in less than 10% and anaphylaxis was reported in 0.3% of patients. Since the dose is weight adjusted, reslizumab could be more efficacious when fixed dose mepolizumab is not adequate[485]
Benralizumab binds to the α chain of IL-5 receptor, leading to eosinophil apoptosis.[172] In addition, it induces antibody-mediated cell cytotoxicity and therefore has a prolonged effect in reducing eosinophils. Based on clinical trials, blood eosinophils counts is recommended to be >300/μL.[486] OCS reduction up to 75% from baseline was demonstrated in patients with baseline eosinophils counts >150/μL.[487] When there is suboptimal response to mepolizumab, evidence showed that benralizumab therapy may lead to significant clinical benefit in patients with severe eosinophilic asthma with reductions in exacerbation frequency and OCS exposure, alongside improvements in patient-reported outcome measures.[488,489] It is given at a dose of 30 mg subcutaneously once every 4 weeks for the first 3 doses and once every 8 weeks thereafter. It is indicated for patients ≥12 years. For patients with prolonged OCS use with baseline eosinophils counts >150/μL, it is indicated when in a patient ≥18 years.
Anti-interleukin 4 receptor α
Dupilumab is a monoclonal antibody against the α chain of the IL-4 receptor. This chain is shared with the IL-13 receptor. Therefore, this biologic impedes the signaling of both IL-4 and IL-13, two important cytokines in the development of IgE-producing B-cells, induction of airway smooth muscle hyperreactivity, eosinophil tissue chemotaxis, airway mucus production, and subepithelial fibrosis. Dupilumab is indicated in severe eosinophilic asthma (blood eosinophils ≥150/μL or FeNO ≥25 ppb) and oral steroid-dependent severe asthma regardless of blood eosinophils count, although patients with eosinophil count 300/μL had significantly more benefit. It is approved for patients ≥12 years of age. It improves asthma control, quality of life, and lung function and reduces the use of OCS and the rate of asthma attacks.[490] The dose is 400 mg SC once then 200 mg every 2 weeks for the eosinophilic asthma phenotype and 600 mg once then 300 mg every 2 weeks for the oral steroid-dependent asthma or if there are comorbid conditions responsive to dupilumab such as moderate-to-severe atopic dermatitis or chronic rhinosinusitis with nasal polyposis.[174] Adverse effects include URTIs and injection site reaction. Transient eosinophilia has been observed in some patients in the first 3 months of treatment. It is recommended not to start dupilumab in patients with blood eosinophil count >1500/μL. Furthermore, conjunctivitis has been noted in 10% of patients in the atopic dermatitis studies, but not in the asthma studies.[491] Patients on dupilumab should avoid live vaccines.
Thymic stromal lymphopoietin inhibitors
Tezepelumab is a human monoclonal antibody specific for the epithelial-cell–derived TSLP that is studied for the treatment of asthma and atopic dermatitis. Phase II randomized controlled trials showed that tezepelumab led to lower rates of clinically significant asthma exacerbations than those who received placebo, independent of baseline blood eosinophil counts.[492,493] It is not yet approved for asthma treatment; however, there are ongoing phase III trials to assess its safety in adults and adolescents with severe, uncontrolled asthma and also to assess its efficacy in reducing OCS use in adults with oral corticosteroid-dependent asthma.[494,495] Prepublication data showed that tezepelumab was well tolerated and met the primary end point of a statistically significant and clinically meaningful reduction of annualized asthma exacerbation rate for patients on medium–high ICS with or without OCS.[496]
Financial support and sponsorship
The SINA received financial and logistic support from the STS.
Conflicts of interest
The SINA is fully sponsored by the STS.
Disclaimer
These guidelines for the diagnosis and management of asthma in adults and children, developed by the SINA panel, are not meant to replace clinical judgments of physicians but to be used as tools to help the practicing physicians to manage asthma patients. Although a lot of effort was exerted to ensure the accurate names and doses of medications, the authors encourage the readers to refer to the relevant information of specific drugs for further clarification.
Acknowledgment
The panel would also like to thank the following consultant reviewers for previous versions (2009, 2012, 2016, and 2019 versions) for their valuable reviews: Prof. Mark FitzGerald and Prof. Sheldon Spier from the University of British Columbia, Vancouver, British Columbia, Canada; Prof. Qutayba Hamid and Prof. Ronald Olivenstein from the Meakins-Christie Laboratories, McGill University, Montreal, Quebec, Canada; Prof. Eric Bateman from the University of Cape Town Lung Institute, Cape Town, South Africa; and Prof. Andrew Bush, Imperial College, National Heart and Lung Institute, London, United Kingdom.
References
- 1.Asthma GIf. The Global Strategy for Asthma Management and Prevention. 2020 [Google Scholar]
- 2.Al Ghobain MO, Algazlan SS, Oreibi TM. Asthma prevalence among adults in Saudi Arabia. Saudi Med J. 2018;39:179–84. doi: 10.15537/smj.2018.2.20974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohamed Hussain S, Ayesha Farhana S, Mohammed Alnasser S. Time trends and regional variation in prevalence of asthma and associated factors in Saudi Arabia: A systematic review and meta-analysis. Biomed Res Int. 2018;2018:8102527. doi: 10.1155/2018/8102527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alatawi A, Alanazi M. Barriers of asthma care among asthmatic children in Saudi Arabia: Maternal perspectives. Open J Pediatr. 2020;10:302. [Google Scholar]
- 5.Taminskiene V, Alasevicius T, Valiulis A, Vaitkaitiene E, Stukas R, Hadjipanayis A, et al. Quality of life of the family of children with asthma is not related to asthma severity. Eur J Pediatr. 2019;178:369–76. doi: 10.1007/s00431-018-3306-8. [DOI] [PubMed] [Google Scholar]
- 6.Al-Moamary MS, Al-Hajjaj MS, Idrees MM, Zeitouni MO, Alanezi MO, Al-Jahdali HH, et al. The Saudi Initiative for Asthma. Ann Thorac Med. 2009;4:216–33. doi: 10.4103/1817-1737.56001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Moamary MS, Alhaider SA, Al-Hajjaj MS, Al-Ghobain MO, Idrees MM, Zeitouni MO, et al. The Saudi Initiative for Asthma - 2012 Update: Guidelines for the diagnosis and management of asthma in adults and children. Ann Thorac Med. 2012;7:175–204. doi: 10.4103/1817-1737.102166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Moamary MS, Alhaider SA, Idrees MM, Al Ghobain MO, Zeitouni MO, Al-Harbi AS, et al. The Saudi Initiative for Asthma - 2016 update: Guidelines for the diagnosis and management of asthma in adults and children. Ann Thorac Med. 2016;11:3–42. doi: 10.4103/1817-1737.173196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Moamary MS, Alhaider SA, Alangari AA, Al Ghobain MO, Zeitouni MO, Idrees MM, et al. The Saudi Initiative for Asthma - 2019 Update: Guidelines for the diagnosis and management of asthma in adults and children. Ann Thorac Med. 2019;14:3–48. doi: 10.4103/atm.ATM_327_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asthma GIf. The Global Strategy for Asthma Management and Prevention. 2020. [Last accessed on 2020 Oct 22]. Available from: www.ginasthma.org .
- 11.Jadad AR, Moher M, Browman GP, Booker L, Sigouin C, Fuentes M, et al. Systematic reviews and meta-analyses on treatment of asthma: Critical evaluation. BMJ. 2000;320:537–40. doi: 10.1136/bmj.320.7234.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Jahdali HH, Al-Hajjaj MS, Alanezi MO, Zeitoni MO, Al-Tasan TH. Asthma control assessment using asthma control test among patients attending 5 tertiary care hospitals in Saudi Arabia. Saudi Med J. 2008;29:714–7. [PubMed] [Google Scholar]
- 13.Loftus PA, Wise SK. Epidemiology of asthma. Curr Opin Otolaryngol Head Neck Surg. 2016;24:245–9. doi: 10.1097/MOO.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 14.Al-Harbi S, Al-Harbi AS, Al-Khorayyef A, Al-Qwaiee M, Al-Shamarani A, Al-Aslani W, et al. Awareness regarding childhood asthma in Saudi Arabia. Ann Thorac Med. 2016;11:60–5. doi: 10.4103/1817-1737.173194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammad MA, Alakhali KM, Manal Hattan M, Noor DA, Syed Azhar Syed Sulaiman S, Kharshid AM, et al. Asthma in Saudi Arabia: Risk factors and pharmacotherapy. Indo Am J Pharm Res. 2016;6:6814–21. [Google Scholar]
- 16.BinSaeed AA. Caregiver knowledge and its relationship to asthma control among children in Saudi Arabia. J Asthma. 2014;51:870–5. doi: 10.3109/02770903.2014.906608. [DOI] [PubMed] [Google Scholar]
- 17.BinSaeed AA, Torchyan AA, Alsadhan AA, Almidani GM, Alsubaie AA, Aldakhail AA, et al. Determinants of asthma control among children in Saudi Arabia. J Asthma. 2014;51:435–9. doi: 10.3109/02770903.2013.876649. [DOI] [PubMed] [Google Scholar]
- 18.Ahmed AE, Al-Jahdali H, Al-Harbi A, Khan M, Ali Y, Al Shimemeri A, et al. Factors associated with poor asthma control among asthmatic patient visiting emergency department. Clin Respir J. 2014;8:431–6. doi: 10.1111/crj.12090. [DOI] [PubMed] [Google Scholar]
- 19.Al-Jahdali H, Anwar A, Al-Harbi A, Baharoon S, Halwani R, Al Shimemeri A, et al. Factors associated with patient visits to the emergency department for asthma therapy. BMC Pulm Med. 2012;12:80. doi: 10.1186/1471-2466-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Zahrani JM, Ahmad A, Al-Harbi A, Khan AM, Al-Bader B, Baharoon S, et al. Factors associated with poor asthma control in the outpatient clinic setting. Ann Thorac Med. 2015;10:100–4. doi: 10.4103/1817-1737.152450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al Ghobain MO, AlNemer M, Khan M. Assessment of knowledge and education relating to asthma during pregnancy among women of childbearing age. Asthma Res Pract. 2018;4:2. doi: 10.1186/s40733-017-0038-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al Ghamdi BR, Koshak EA, Ageely HM, Omer FM, Awadalla NJ, Mahfouz AA. Prevalence and factors associated with adult bronchial asthma in Aseer region, Southwestern Saudi Arabia. Ann Thorac Med. 2019;14:278–84. doi: 10.4103/atm.ATM_67_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okada H, Kuhn C, Feillet H, Bach JF. The 'hygiene hypothesis' for autoimmune and allergic diseases: An update. Clin Exp Immunol. 2010;160:1–9. doi: 10.1111/j.1365-2249.2010.04139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al Ghobain MO, Al-Hajjaj MS, Al Moamary MS. Asthma prevalence among 16- to 18-year-old adolescents in Saudi Arabia using the ISAAC questionnaire. BMC Public Health. 2012;12:239. doi: 10.1186/1471-2458-12-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nahhas M, Bhopal R, Anandan C, Elton R, Sheikh A. Prevalence of allergic disorders among primary school-aged children in Madinah, Saudi Arabia: Two-stage cross-sectional survey. PLoS One. 2012;7:e36848. doi: 10.1371/journal.pone.0036848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moradi-Lakeh M, El Bcheraoui C, Daoud F, Tuffaha M, Kravitz H, Al Saeedi M, et al. Prevalence of asthma in Saudi adults: Findings from a national household survey, 2013. BMC Pulm Med. 2015;15:77. doi: 10.1186/s12890-015-0080-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alqahtani JM. Atopy and allergic diseases among Saudi young adults: A cross-sectional study. J Int Med Res. 2020;48:300060519899760. doi: 10.1177/0300060519899760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Horaib YF, ALAmri ES, Al-Anazi W, Sharahili EA, Alolayah AM, Alrobian MA. The prevalence of asthma and its related risk factors among the children in Riyadh, Saudi Arabia. Egypt J Hosp Med. 2018;70:965–73. [Google Scholar]
- 29.Torchyan AA, editor. Asthma Control in Saudi Arabia: Gender implications. New York, USA: Allergy & Asthma Proceedings; 2017. [DOI] [PubMed] [Google Scholar]
- 30.Al-Jahdali H, Wali S, Salem G, Al-Hameed F, Almotair A, Zeitouni M, et al. Asthma control and predictive factors among adults in Saudi Arabia: Results from the Epidemiological Study on the Management of Asthma in Asthmatic Middle East Adult Population study. Ann Thorac Med. 2019;14:148–54. doi: 10.4103/atm.ATM_348_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lovinsky-Desir S, Deshpande DR, De A, Murray L, Stingone JA, Chan A, et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020;146:1027–34.e4. doi: 10.1016/j.jaci.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.ATS Statement–Snowbird workshop on standardization of spirometry. Am Rev Respir Dis. 1979;119:831–8. doi: 10.1164/arrd.1979.119.5.831. [DOI] [PubMed] [Google Scholar]
- 33.Gold JA, Wong KK, Szablewski CM, Patel PR, Rossow J, da Silva J, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 - Georgia, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:545–50. doi: 10.15585/mmwr.mm6918e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052–9. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khan M, Khan MN, Mustagir MG, Rana J, Islam MS, Kabir MI. Effects of pre-existing morbidities on occurrence of death among COVID-19 disease patients: A systematic review and meta-analysis. Journal of global health. 2020;20:1–14. doi: 10.7189/jogh.10.020503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pavord ID, Beasley R, Agusti A, Anderson GP, Bel E, Brusselle G, et al. After asthma: Redefining airways diseases. Lancet. 2018;391:350–400. doi: 10.1016/S0140-6736(17)30879-6. [DOI] [PubMed] [Google Scholar]
- 37.Del Giacco SR, Bakirtas A, Bel E, Custovic A, Diamant Z, Hamelmann E, et al. Allergy in severe asthma. Allergy. 2017;72:207–20. doi: 10.1111/all.13072. [DOI] [PubMed] [Google Scholar]
- 38.Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol. 2015;16:45–56. doi: 10.1038/ni.3049. [DOI] [PubMed] [Google Scholar]
- 39.Brusselle GG, Maes T, Bracke KR. Eosinophils in the spotlight: Eosinophilic airway inflammation in nonallergic asthma. Nat Med. 2013;19:977–9. doi: 10.1038/nm.3300. [DOI] [PubMed] [Google Scholar]
- 40.Amelink M, de Nijs SB, de Groot JC, van Tilburg PM, van Spiegel PI, Krouwels FH, et al. Three phenotypes of adult-onset asthma. Allergy. 2013;68:674–80. doi: 10.1111/all.12136. [DOI] [PubMed] [Google Scholar]
- 41.Israel E, Reddel HK. Severe and difficult-to-treat asthma in adults. N Engl J Med. 2017;377:965–76. doi: 10.1056/NEJMra1608969. [DOI] [PubMed] [Google Scholar]
- 42.Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018;391:783–800. doi: 10.1016/S0140-6736(17)33311-1. [DOI] [PubMed] [Google Scholar]
- 43.Park JA, Sharif AS, Tschumperlin DJ, Lau L, Limbrey R, Howarth P, et al. Tissue factor-bearing exosome secretion from human mechanically stimulated bronchial epithelial cells in vitro and in vivo. J Allergy Clin Immunol. 2012;130:1375–83. doi: 10.1016/j.jaci.2012.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brightling CE, Gupta S, Gonem S, Siddiqui S. Lung damage and airway remodelling in severe asthma. Clin Exp Allergy. 2012;42:638–49. doi: 10.1111/j.1365-2222.2011.03917.x. [DOI] [PubMed] [Google Scholar]
- 45.Bergeron C, Al-Ramli W, Hamid Q. Remodeling in asthma. Proc Am Thorac Soc. 2009;6:301–5. doi: 10.1513/pats.200808-089RM. [DOI] [PubMed] [Google Scholar]
- 46.Grainge CL, Lau LC, Ward JA, Dulay V, Lahiff G, Wilson S, et al. Effect of bronchoconstriction on airway remodeling in asthma. N Engl J Med. 2011;364:2006–15. doi: 10.1056/NEJMoa1014350. [DOI] [PubMed] [Google Scholar]
- 47.Alangari AA. Corticosteroids in the treatment of acute asthma. Ann Thorac Med. 2014;9:187–92. doi: 10.4103/1817-1737.140120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.O'Byrne PM, Pedersen S, Lamm CJ, Tan WC, Busse WW. START Investigators Group. Severe exacerbations and decline in lung function in asthma. Am J Respir Crit Care Med. 2009;179:19–24. doi: 10.1164/rccm.200807-1126OC. [DOI] [PubMed] [Google Scholar]
- 49.O'Brian AL, Lemanske RF, Jr, Evans MD, Gangnon RE, Gern JE, Jackson DJ. Recurrent severe exacerbations in early life and reduced lung function at school age. J Allergy Clin Immunol. 2012;129:1162–4. doi: 10.1016/j.jaci.2011.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Russell RJ, Brightling C. Pathogenesis of asthma: Implications for precision medicine. Clin Sci (Lond) 2017;131:1723–35. doi: 10.1042/CS20160253. [DOI] [PubMed] [Google Scholar]
- 51.Stempel DA, McLaughin TP, Stanford RH, Fuhlbrigge AL. Patterns of asthma control: A 3-year analysis of patient claims. J Allergy Clin Immunol. 2005;115:935–9. doi: 10.1016/j.jaci.2005.01.054. [DOI] [PubMed] [Google Scholar]
- 52.Bloom CI, Palmer T, Feary J, Quint JK, Cullinan P. exacerbation patterns in adults with asthma in England. A population-based study. Am J Respir Crit Care Med. 2019;199:446–53. doi: 10.1164/rccm.201808-1516OC. [DOI] [PubMed] [Google Scholar]
- 53.Alharbi M, Almutairi A, Alotaibi D, Alotaibi A, Shaikh S, Bahammam AS. The prevalence of asthma in patients with obstructive sleep apnoea. Prim Care Respir J. 2009;18:328–30. doi: 10.4104/pcrj.2009.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bonsignore MR, Baiamonte P, Mazzuca E, Castrogiovanni A, Marrone O. Obstructive sleep apnea and comorbidities: A dangerous liaison. Multidiscip Respir Med. 2019;14:8. doi: 10.1186/s40248-019-0172-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Price D. Asthma and allergic rhinitis: Linked in treatment and outcomes. Ann Thorac Med. 2010;5:63–4. doi: 10.4103/1817-1737.62467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rogliani P, Sforza M, Calzetta L. The impact of comorbidities on severe asthma. Curr Opin Pulm Med. 2020;26:47–55. doi: 10.1097/MCP.0000000000000640. [DOI] [PubMed] [Google Scholar]
- 57.Naclerio R, Ansotegui IJ, Bousquet J, Canonica GW, D'Amato G, Rosario N, et al. International expert consensus on the management of allergic rhinitis (AR) aggravated by air pollutants: Impact of air pollution on patients with AR: Current knowledge and future strategies. World Allergy Organ J. 2020;13:100106. doi: 10.1016/j.waojou.2020.100106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Al-Mobeireek AF, Al-Sarhani A, Al-Amri S, Bamgboye E, Ahmed SS. Chronic cough at a non-teaching hospital: Are extrapulmonary causes overlooked? Respirology. 2002;7:141–6. doi: 10.1046/j.1440-1843.2002.00378.x. [DOI] [PubMed] [Google Scholar]
- 59.Al-Otair H, Bahammam AS. Unusual cause of respiratory distress misdiagnosed as refractory asthma. Ann Thorac Med. 2006;1:28–30. [Google Scholar]
- 60.Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med. 1995;152:1107–36. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 61.Cowie RL, Underwood MF, Field SK. Asthma symptoms do not predict spirometry. Can Respir J. 2007;14:339–42. doi: 10.1155/2007/816132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yi F, Han L, Liu B, Zhang X, Xue Y, Luo W, et al. Determinants of response to bronchodilator in patients with cough variant asthma- A randomized, single-blinded, placebo-controlled study. Pulm Pharmacol Ther. 2020;61:101903. doi: 10.1016/j.pupt.2020.101903. [DOI] [PubMed] [Google Scholar]
- 63.Song WJ, Kim HJ, Shim JS, Won HK, Kang SY, Sohn KH, et al. Diagnostic accuracy of fractional exhaled nitric oxide measurement in predicting cough-variant asthma and eosinophilic bronchitis in adults with chronic cough: A systematic review and meta-analysis. J Allergy Clin Immunol. 2017;140:701–9. doi: 10.1016/j.jaci.2016.11.037. [DOI] [PubMed] [Google Scholar]
- 64.Lux H, Lenz K, Budnik LT, Baur X. Performance of specific immunoglobulin E tests for diagnosing occupational asthma: A systematic review and meta-analysis. Occup Environ Med. 2019;76:269–78. doi: 10.1136/oemed-2018-105434. [DOI] [PubMed] [Google Scholar]
- 65.Humbert M, Holgate S, Boulet LP, Bousquet J. Asthma control or severity: That is the question. Allergy. 2007;62:95–101. doi: 10.1111/j.1398-9995.2006.01308.x. [DOI] [PubMed] [Google Scholar]
- 66.Halvorsen T, Walsted ES, Bucca C, Bush A, Cantarella G, Friedrich G, et al. Inducible laryngeal obstruction: An official joint European Respiratory Society and European Laryngological Society statement. Eur Respir J. 2017;50:1–15. doi: 10.1183/13993003.02221-2016. [DOI] [PubMed] [Google Scholar]
- 67.Cope SF, Ungar WJ, Glazier RH. International differences in asthma guidelines for children. Int Arch Allergy Immunol. 2009;148:265–78. doi: 10.1159/000170380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Apps LD, Chantrell S, Majd S, Eglinton E, Singh SJ, Murphy AC, et al. Patient perceptions of living with severe asthma: Challenges to effective management. J Allergy Clin Immunol Pract. 2019;7:2613–21.e1. doi: 10.1016/j.jaip.2019.04.026. [DOI] [PubMed] [Google Scholar]
- 69.Neffen H, Chahuàn M, Hernández DD, Vallejo-Perez E, Bolivar F, Sánchez MH, et al. Key factors associated with uncontrolled asthma - The asthma control in Latin America study. J Asthma. 2020;57:113–22. doi: 10.1080/02770903.2018.1553050. [DOI] [PubMed] [Google Scholar]
- 70.Asthma GIf. GINA Global Strategy for Asthma Management and Prevention. 2020 [Google Scholar]
- 71.Koolen BB, Pijnenburg MW, Brackel HJ, Landstra AM, van den Berg NJ, Merkus PJ, et al. Comparing Global Initiative for Asthma (GINA) criteria with the Childhood Asthma Control Test (C-ACT) and Asthma Control Test (ACT) Eur Respir J. 2011;38:561–6. doi: 10.1183/09031936.00173710. [DOI] [PubMed] [Google Scholar]
- 72.Vermeulen F, de Meulder I, Paesmans M, Muylle I, Bruyneel M, Ninane V. Asthma control measurement using five different questionnaires: A prospective study. Respir Med. 2013;107:1314–21. doi: 10.1016/j.rmed.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 73.Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma control test: Reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117:549–56. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 74.Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, et al. Development of the asthma control test: A survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59–65. doi: 10.1016/j.jaci.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 75.Lababidi H, Hijaoui A, Zarzour M. Validation of the Arabic version of the asthma control test. Ann Thorac Med. 2008;3:44–7. doi: 10.4103/1817-1737.39635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Alanezi M, Al-Jahdali HH, Al-Hajjaj MS, Zeitoni MO, Al-Tasan TH. Levels of acceptance of asthma control test questionnaire among Saudi patients attending 5 tertiary care hospitals in Saudi Arabia. Saudi Med J. 2009;30:546–9. [PubMed] [Google Scholar]
- 77.Al Moamary MS, Al-Kordi AG, Al Ghobain MO, Tamim HM. Utilization and responsiveness of the asthma control test (ACT) at the initiation of therapy for patients with asthma: A randomized controlled trial. BMC Pulm Med. 2012;12:14. doi: 10.1186/1471-2466-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schatz M, Kosinski M, Yarlas AS, Hanlon J, Watson ME, Jhingran P. The minimally important difference of the asthma control test. J Allergy Clin Immunol. 2009;124:719–23e1. doi: 10.1016/j.jaci.2009.06.053. [DOI] [PubMed] [Google Scholar]
- 79.Miller MK, Lee JH, Miller DP, Wenzel SE. TENOR Study Group. Recent asthma exacerbations: A key predictor of future exacerbations. Respir Med. 2007;101:481–9. doi: 10.1016/j.rmed.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 80.Amnuaypattanapon K, Limjindaporn C, Srivilaithon W, Dasanadeba I. Characteristics and outcomes of treatment in status asthmaticus patients at emergency department. Asian Pac J Allergy Immunol. 2019;37:87–93. doi: 10.12932/AP-261217-0224. [DOI] [PubMed] [Google Scholar]
- 81.Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. An official American Thoracic Society/European Respiratory Society statement: Asthma control and exacerbations: Standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009;180:59–99. doi: 10.1164/rccm.200801-060ST. [DOI] [PubMed] [Google Scholar]
- 82.Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB, et al. A new perspective on concepts of asthma severity and control. Eur Respir J. 2008;32:545–54. doi: 10.1183/09031936.00155307. [DOI] [PubMed] [Google Scholar]
- 83.Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43:343–73. doi: 10.1183/09031936.00202013. [DOI] [PubMed] [Google Scholar]
- 84.Al-Jahdali HH, Al-Zahrani AI, Al-Otaibi ST, Hassan IS, Al-Moamary MS, Al-Duhaim AS, et al. Perception of the role of inhaled corticosteroids and factors affecting compliance among asthmatic adult patients. Saudi Med J. 2007;28:569–73. [PubMed] [Google Scholar]
- 85.Noibi S, Mohy A, Gouhar R, Shaker F, Lukic T, Al-Jahdali H. Asthma control factors in the Gulf Cooperation Council (GCC) countries and the effectiveness of ICS/LABA fixed dose combinations: A dual rapid literature review. BMC Public Health. 2020;20:1211. doi: 10.1186/s12889-020-09259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Janežič A, Locatelli I, Kos M. Inhalation technique and asthma outcomes with different corticosteroid-containing inhaler devices. J Asthma. 2020;57:654–62. doi: 10.1080/02770903.2019.1591442. [DOI] [PubMed] [Google Scholar]
- 87.Hussain FN, Paravattil B. Assessment of educational inhaler technique interventions among community pharmacists: A systematic review. Integr Pharm Res Pract. 2020;9:23–31. doi: 10.2147/IPRP.S239215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Musharrafieh U, Tamim H, Houry R, AlBuhairan F. A nationwide study of asthma correlates among adolescents in Saudi Arabia. Asthma Res Pract. 2020;6:3. doi: 10.1186/s40733-020-00056-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Barnes NC. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma Control study. Am J Respir Crit Care Med. 2004;170:830–1. doi: 10.1164/rccm.2408006. [DOI] [PubMed] [Google Scholar]
- 90.Gibson PG, Powell H. Written action plans for asthma: An evidence-based review of the key components. Thorax. 2004;59:94–9. doi: 10.1136/thorax.2003.011858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dailah H. A Self-Management Program for Adults with Asthma in Saudi Arabia. The University of Salford, Manchester, UK: University of Salford; 2020. [Google Scholar]
- 92.Richmond RS, Connolly M. A delineation of self-management and associated concepts. Int J Healthc Manag. 2020:1–13. https://doi.org/10.1080/20479700.2020.1810963. [Google Scholar]
- 93.Zaraket R, Al-Tannir MA, Bin Abdulhak AA, Shatila A, Lababidi H. Parental perceptions and beliefs about childhood asthma: A cross-sectional study. Croat Med J. 2011;52:637–43. doi: 10.3325/cmj.2011.52.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Al-Binali AM, Mahfouz AA, Al-Fifi S, Naser SM, Al-Gelban KS. Asthma knowledge and behaviours among mothers of asthmatic children in Aseer, South-West Saudi Arabia. East Mediterr Health J. 2010;16:1153–8. [PubMed] [Google Scholar]
- 95.Al-Yami SM, Mohajer KA, Al-Jeraisy MI, Batarfi AM, Abolfotouh MA. Recurrent visits and admissions of children with asthma in Central Saudi Arabia. Saudi Med J. 2010;31:921–4. [PubMed] [Google Scholar]
- 96.Basyouni MH, BinDhim NF, Saini B, Williams KA. Online health information needs for patients with asthma in Saudi Arabia. J Consum Health Internet. 2015;19:13–24. [Google Scholar]
- 97.Al-Shimemeri A, Al-Ghadeer H, Giridhar H, Al-Jahdali M, Al-Moamary M, Khan J. Impact of an extensive asthma education campaign for physicians on their drug prescription practices. Ann Thorac Med. 2006;1:20–5. [Google Scholar]
- 98.Khdour MR, Elyan SO, Hallak HO, Jarab AS, Mukattash TL, Astal A. Pharmaceutical care for adult asthma patients: A controlled intervention one-year follow-up study. Basic Clin Pharmacol Toxicol. 2020;126:332–40. doi: 10.1111/bcpt.13344. [DOI] [PubMed] [Google Scholar]
- 99.Dardouri M, Sahli J, Ajmi T, Mtiraoui A, Bouguila J, Mallouli M. Factors associated with acute health care use in children and adolescents with asthma. Compr Child Adolesc Nurs. 2020:1–2. doi: 10.1080/24694193.2020.1742249. [DOI] [PubMed] [Google Scholar]
- 100.Alotaibi G. Status of respiratory care profession in Saudi Arabia: A national survey. Ann Thorac Med. 2015;10:55–60. doi: 10.4103/1817-1737.146878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gold DR, Adamkiewicz G, Arshad SH, Celedón JC, Chapman MD, Chew GL, et al. NIAID, NIEHS, NHLBI, and MCAN Workshop Report: The indoor environment and childhood asthma-implications for home environmental intervention in asthma prevention and management. J Allergy Clin Immunol. 2017;140:933–49. doi: 10.1016/j.jaci.2017.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Alangari AA, Riaz M, Mahjoub MO, Malhis N, Al-Tamimi S, Al-Modaihsh A. The effect of sand storms on acute asthma in Riyadh, Saudi Arabia. Ann Thorac Med. 2015;10:29–33. doi: 10.4103/1817-1737.146857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zeitouni MO, Al Barrak AM, Al-Moamary MS, Alharbi NS, Idrees MM, Al Shimemeri AA, et al. The Saudi Thoracic Society guidelines for influenza vaccinations. Ann Thorac Med. 2015;10:223–30. doi: 10.4103/1817-1737.167065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kyung Y, Choi MH, Lee JS, Lee JH, Jo SH, Kim SH. Influencing factors for influenza vaccination among south korean adolescents with asthma based on a nationwide cross-sectional study. Int Arch Allergy Immunol. 2020;181:434–45. doi: 10.1159/000506336. [DOI] [PubMed] [Google Scholar]
- 105.Grohskopf LA, Alyanak E, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices - United States, 2019-20 Influenza Season. MMWR Recomm Rep. 2019;68:1–21. doi: 10.15585/mmwr.rr6803a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Alharbi NS, Al-Barrak AM, Al-Moamary MS, Zeitouni MO, Idrees MM, Al-Ghobain MO, et al. The Saudi Thoracic Society Pneumococcal Vaccination Guidelines-2016. Ann Thorac Med. 2016;11:93–102. doi: 10.4103/1817-1737.177470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen YZ, Ohlsson SV, et al. Early intervention with budesonide in mild persistent asthma: A randomised, double-blind trial. Lancet. 2003;361:1071–6. doi: 10.1016/S0140-6736(03)12891-7. [DOI] [PubMed] [Google Scholar]
- 108.Barnes PJ, Pedersen S. Efficacy and safety of inhaled corticosteroids in asthma. Report of a workshop held in Eze, France, October 1992. Am Rev Respir Dis. 1993;148:S1–26. doi: 10.1164/ajrccm/148.4_Pt_2.S1. [DOI] [PubMed] [Google Scholar]
- 109.Berger WE. Levalbuterol: Pharmacologic properties and use in the treatment of pediatric and adult asthma. Ann Allergy Asthma Immunol. 2003;90:583–91. doi: 10.1016/S1081-1206(10)61859-5. [DOI] [PubMed] [Google Scholar]
- 110.Martinez FD, Chinchilli VM, Morgan WJ, Boehmer SJ, Lemanske RF, Jr, Mauger DT, et al. Use of beclomethasone dipropionate as rescue treatment for children with mild persistent asthma (TREXA): A randomised, double-blind, placebo-controlled trial. Lancet. 2011;377:650–7. doi: 10.1016/S0140-6736(10)62145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sumino K, Bacharier LB, Taylor J, Chadwick-Mansker K, Curtis V, Nash A, et al. A pragmatic trial of symptom-based inhaled corticosteroid use in African-American children with mild asthma. J Allergy Clin Immunol Pract. 2020;8:176–85.e2. doi: 10.1016/j.jaip.2019.06.030. [DOI] [PubMed] [Google Scholar]
- 112.O'Byrne PM, Bisgaard H, Godard PP, Pistolesi M, Palmqvist M, Zhu Y, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. Am J Respir Crit Care Med. 2005;171:129–36. doi: 10.1164/rccm.200407-884OC. [DOI] [PubMed] [Google Scholar]
- 113.Bateman ED, Reddel HK, O'Byrne PM, Barnes PJ, Zhong N, Keen C, et al. As-needed budesonide-formoterol versus maintenance budesonide in mild asthma. N Engl J Med. 2018;378:1877–87. doi: 10.1056/NEJMoa1715275. [DOI] [PubMed] [Google Scholar]
- 114.O'Byrne PM, FitzGerald JM, Bateman ED, Barnes PJ, Zhong N, Keen C, et al. Inhaled combined budesonide-formoterol as needed in mild asthma. N Engl J Med. 2018;378:1865–76. doi: 10.1056/NEJMoa1715274. [DOI] [PubMed] [Google Scholar]
- 115.Beasley R, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox RJ, et al. Controlled trial of budesonide-formoterol as needed for mild asthma. N Engl J Med. 2019;380:2020–30. doi: 10.1056/NEJMoa1901963. [DOI] [PubMed] [Google Scholar]
- 116.Turner MO, Noertjojo K, Vedal S, Bai T, Crump S, Fitzgerald JM. Risk factors for near-fatal asthma. A case-control study in hospitalized patients with asthma. Am J Respir Crit Care Med. 1998;157:1804–9. doi: 10.1164/ajrccm.157.6.9708092. [DOI] [PubMed] [Google Scholar]
- 117.Graff S, Demarche S, Henket M, Paulus V, Louis R, Schleich F. Increase in blood eosinophils during follow-up is associated with lung function decline in adult asthma. Respir Med. 2019;152:60–6. doi: 10.1016/j.rmed.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 118.Wilson AM, Dempsey OJ, Sims EJ, Lipworth BJ. A comparison of topical budesonide and oral montelukast in seasonal allergic rhinitis and asthma. Clin Exp Allergy. 2001;31:616–24. doi: 10.1046/j.1365-2222.2001.01088.x. [DOI] [PubMed] [Google Scholar]
- 119.Pols DH, Wartna JB, Moed H, van Alphen EI, Bohnen AM, Bindels PJ. Atopic dermatitis, asthma and allergic rhinitis in general practice and the open population: A systematic review. Scand J Prim Health Care. 2016;34:143–50. doi: 10.3109/02813432.2016.1160629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Qazi A, Armour C, Saini B. Perspectives of general practitioners about a collaborative asthma care model in primary care. J Asthma. 2020:1–3. doi: 10.1080/02770903.2020.1823408. [DOI] [PubMed] [Google Scholar]
- 121.Hardy J, Baggott C, Fingleton J, Reddel HK, Hancox RJ, Harwood M, et al. Budesonide-formoterol reliever therapy versus maintenance budesonide plus terbutaline reliever therapy in adults with mild to moderate asthma (PRACTICAL): A 52-week, open-label, multicentre, superiority, randomised controlled trial. Lancet. 2019;394:919–28. doi: 10.1016/S0140-6736(19)31948-8. [DOI] [PubMed] [Google Scholar]
- 122.Papi A, Canonica GW, Maestrelli P, Paggiaro P, Olivieri D, Pozzi E, et al. Rescue use of beclomethasone and albuterol in a single inhaler for mild asthma. N Engl J Med. 2007;356:2040–52. doi: 10.1056/NEJMoa063861. [DOI] [PubMed] [Google Scholar]
- 123.Selroos O. Effect of disease duration on dose-response of inhaled budesonide in asthma. Respir Med. 2008;102:1065–72. doi: 10.1016/j.rmed.2007.12.029. [DOI] [PubMed] [Google Scholar]
- 124.Sharma S, Harish R, Dutt N, Digra KK. To evaluate the efficacy of nebulized budesonide compared to oral prednisolone in the management of moderate exacerbation of acute asthma. Int J Contemp Pediatr. 2017;4:1278–83. [Google Scholar]
- 125.Sont JK. How do we monitor asthma control? Allergy. 1999;54(Suppl 49):68–73. doi: 10.1111/j.1398-9995.1999.tb04391.x. [DOI] [PubMed] [Google Scholar]
- 126.O'Byrne PM, Jenkins C, Bateman ED. The paradoxes of asthma management: Time for a new approach? Eur Respir J. 2017;50:1701103. doi: 10.1183/13993003.01103-2017. DOI: 10.1183/13993003.01103-2017. [DOI] [PubMed] [Google Scholar]
- 127.Fingleton J, Hardy J, Baggott C, Pilcher J, Corin A, Hancox RJ, et al. Description of the protocol for the PRACTICAL study: A randomised controlled trial of the efficacy and safety of ICS/LABA reliever therapy in asthma. BMJ Open Respir Res. 2017;4:e000217. doi: 10.1136/bmjresp-2017-000217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Reddel HK, Busse WW, Pedersen S, Tan WC, Chen YZ, Jorup C, et al. Should recommendations about starting inhaled corticosteroid treatment for mild asthma be based on symptom frequency: A post-hoc efficacy analysis of the START study. Lancet. 2017;389:157–66. doi: 10.1016/S0140-6736(16)31399-X. [DOI] [PubMed] [Google Scholar]
- 129.Dusser D, Montani D, Chanez P, de Blic J, Delacourt C, Deschildre A, et al. Mild asthma: An expert review on epidemiology, clinical characteristics and treatment recommendations. Allergy. 2007;62:591–604. doi: 10.1111/j.1398-9995.2007.01394.x. [DOI] [PubMed] [Google Scholar]
- 130.Powell H, Gibson PG. Initial starting dose of inhaled corticosteroids in adults with asthma: A systematic review. Thorax. 2004;59:1041–5. doi: 10.1136/thx.2004.023754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Drazen JM, Israel E, O'Byrne PM. Treatment of asthma with drugs modifying the leukotriene pathway. N Engl J Med. 1999;340:197–206. doi: 10.1056/NEJM199901213400306. [DOI] [PubMed] [Google Scholar]
- 132.Reddel HK, Busse WW, Pedersen S, Tan WC, Chen YZ, Jorup C, et al. Should recommendations about starting inhaled corticosteroid treatment for mild asthma be based on symptom frequency: A post-hoc efficacy analysis of the START study. Lancet. 2017;389:157–66. doi: 10.1016/S0140-6736(16)31399-X. [DOI] [PubMed] [Google Scholar]
- 133.O'Byrne PM, Barnes PJ, Rodriguez-Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: The OPTIMA randomized trial. Am J Respir Crit Care Med. 2001;164:1392–7. doi: 10.1164/ajrccm.164.8.2104102. [DOI] [PubMed] [Google Scholar]
- 134.Cates CJ, Schmidt S, Ferrer M, Sayer B, Waterson S. Inhaled steroids with and without regular salmeterol for asthma: Serious adverse events. Cochrane Database Syst Rev. 2018;12:CD006922. doi: 10.1002/14651858.CD006922.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Busse WW, Bateman ED, Caplan AL, Kelly HW, O'Byrne PM, Rabe KF, et al. Combined analysis of asthma safety trials of long-acting β2-agonists. N Engl J Med. 2018;378:2497–505. doi: 10.1056/NEJMoa1716868. [DOI] [PubMed] [Google Scholar]
- 136.Chowdhury BA, Dal Pan G. The FDA and safe use of long-acting beta-agonists in the treatment of asthma. N Engl J Med. 2010;362:1169–71. doi: 10.1056/NEJMp1002074. [DOI] [PubMed] [Google Scholar]
- 137.Koshak EA. New FDA safety warnings for LABAs: A call for asthma guidelines revisit for solo beta agonist. Ann Thorac Med. 2010;5:65–6. doi: 10.4103/1817-1737.62468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Bateman ED, Bousquet J, Keech ML, Busse WW, Clark TJ, Pedersen SE. The correlation between asthma control and health status: The GOAL study. Eur Respir J. 2007;29:56–62. doi: 10.1183/09031936.00128505. [DOI] [PubMed] [Google Scholar]
- 139.O'Byrne PM, Bleecker ER, Bateman ED, Busse WW, Woodcock A, Forth R, et al. Once-daily fluticasone furoate alone or combined with vilanterol in persistent asthma. Eur Respir J. 2014;43:773–82. doi: 10.1183/09031936.00064513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Woodcock A, Bleecker ER, Lötvall J, O'Byrne PM, Bateman ED, Medley H, et al. Efficacy and safety of fluticasone furoate/vilanterol compared with fluticasone propionate/salmeterol combination in adult and adolescent patients with persistent asthma: A randomized trial. Chest. 2013;144:1222–9. doi: 10.1378/chest.13-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Szefler SJ, Martin RJ, King TS, Boushey HA, Cherniack RM, Chinchilli VM, et al. Significant variability in response to inhaled corticosteroids for persistent asthma. J Allergy Clin Immunol. 2002;109:410–8. doi: 10.1067/mai.2002.122635. [DOI] [PubMed] [Google Scholar]
- 142.Powell H, Gibson PG. Inhaled corticosteroid doses in asthma: An evidence-based approach. Med J Aust. 2003;178:223–5. doi: 10.5694/j.1326-5377.2003.tb05167.x. [DOI] [PubMed] [Google Scholar]
- 143.Zeiger RS, Szefler SJ, Phillips BR, Schatz M, Martinez FD, Chinchilli VM, et al. Response profiles to fluticasone and montelukast in mild-to-moderate persistent childhood asthma. J Allergy Clin Immunol. 2006;117:45–52. doi: 10.1016/j.jaci.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 144.Vaquerizo MJ, Casan P, Castillo J, Perpiña M, Sanchis J, Sobradillo V, et al. Effect of montelukast added to inhaled budesonide on control of mild to moderate asthma. Thorax. 2003;58:204–10. doi: 10.1136/thorax.58.3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Joos S, Miksch A, Szecsenyi J, Wieseler B, Grouven U, Kaiser T, et al. Montelukast as add-on therapy to inhaled corticosteroids in the treatment of mild to moderate asthma: A systematic review. Thorax. 2008;63:453–62. doi: 10.1136/thx.2007.081596. [DOI] [PubMed] [Google Scholar]
- 146.Kerstjens HA, van den Berge M. Regular treatment for moderate asthma: Guidelines hold true. Lancet Respir Med. 2015;3:88–9. doi: 10.1016/S2213-2600(14)70297-8. [DOI] [PubMed] [Google Scholar]
- 147.Beeh KM, Moroni-Zentgraf P, Ablinger O, Hollaenderova Z, Unseld A, Engel M, et al. Tiotropium Respimat® in asthma: A double-blind, randomised, dose-ranging study in adult patients with moderate asthma. Respir Res. 2014;15:61. doi: 10.1186/1465-9921-15-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tian JW, Chen JW, Chen R, Chen X. Tiotropium versus placebo for inadequately controlled asthma: A meta-analysis. Respir Care. 2014;59:654–66. doi: 10.4187/respcare.02703. [DOI] [PubMed] [Google Scholar]
- 149.Peters SP, Kunselman SJ, Icitovic N, Moore WC, Pascual R, Ameredes BT, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med. 2010;363:1715–26. doi: 10.1056/NEJMoa1008770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Bateman ED, Kornmann O, Schmidt P, Pivovarova A, Engel M, Fabbri LM. Tiotropium is noninferior to salmeterol in maintaining improved lung function in B16-Arg/Arg patients with asthma. J Allergy Clin Immunol. 2011;128:315–22. doi: 10.1016/j.jaci.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 151.Smith LJ. Anticholinergics for patients with asthma? N Engl J Med. 2010;363:1764–5. doi: 10.1056/NEJMe1009429. [DOI] [PubMed] [Google Scholar]
- 152.Sobieraj DM, Baker WL, Nguyen E, Weeda ER, Coleman CI, White CM, et al. Association of inhaled corticosteroids and long-acting muscarinic antagonists with asthma control in patients with uncontrolled, persistent asthma: A systematic review and meta-analysis. JAMA. 2018;319:1473–84. doi: 10.1001/jama.2018.2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Al-Hajjaj MS. Difficult-to-treat asthma, is it really difficult? Ann Thorac Med. 2011;6:1–2. doi: 10.4103/1817-1737.74268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Pauwels RA, Löfdahl CG, Postma DS, Tattersfield AE, O'Byrne P, Barnes PJ, et al. Effect of inhaled formoterol and budesonide on exacerbations of asthma. Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. N Engl J Med. 1997;337:1405–11. doi: 10.1056/NEJM199711133372001. [DOI] [PubMed] [Google Scholar]
- 155.Lee LA, Bailes Z, Barnes N, Boulet LP, Edwards D, Fowler A, et al. Efficacy and safety of once-daily single-inhaler triple therapy (FF/UMEC/VI) versus FF/VI in patients with inadequately controlled asthma (CAPTAIN): A double-blind, randomised, phase 3A trial. Lancet Respir Med. 2020. https://doi.org/10.1016/S2213-2600(20)30389-1 . [DOI] [PubMed]
- 156.Kerstjens HA, Disse B, Schröder-Babo W, Bantje TA, Gahlemann M, Sigmund R, et al. Tiotropium improves lung function in patients with severe uncontrolled asthma: A randomized controlled trial. J Allergy Clin Immunol. 2011;128:308–14. doi: 10.1016/j.jaci.2011.04.039. [DOI] [PubMed] [Google Scholar]
- 157.Kerstjens HA, Engel M, Dahl R, Paggiaro P, Beck E, Vandewalker M, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med. 2012;367:1198–207. doi: 10.1056/NEJMoa1208606. [DOI] [PubMed] [Google Scholar]
- 158.Rodrigo GJ, Neffen H. Efficacy and safety of tiotropium in school-age children with moderate-to-severe symptomatic asthma: A systematic review. Pediatr Allergy Immunol. 2017;28:573–8. doi: 10.1111/pai.12759. [DOI] [PubMed] [Google Scholar]
- 159.American Lung Association Asthma Clinical Research Centers. Clinical trial of low-dose theophylline and montelukast in patients with poorly controlled asthma. Am J Respir Crit Care Med. 2007;175:235–42. doi: 10.1164/rccm.200603-416OC. [DOI] [PubMed] [Google Scholar]
- 160.Price DB, Hernandez D, Magyar P, Fiterman J, Beeh KM, James IG, et al. Randomised controlled trial of montelukast plus inhaled budesonide versus double dose inhaled budesonide in adult patients with asthma. Thorax. 2003;58:211–6. doi: 10.1136/thorax.58.3.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.US FDA. FDA Requires Boxed Warning about Serious Mental Health Side Effects for Asthma and Allergy Drug Montelukast (Singulair); Advises Restricting Use for Allergic Rhinitis. 2020 [Google Scholar]
- 162.Rivington RN, Boulet LP, Côté J, Kreisman H, Small DI, Alexander M, et al. Efficacy of uniphyl, salbutamol, and their combination in asthmatic patients on high-dose inhaled steroids. Am J Respir Crit Care Med. 1995;151:325–32. doi: 10.1164/ajrccm.151.2.7842186. [DOI] [PubMed] [Google Scholar]
- 163.Kearns N, Maijers I, Harper J, Beasley R, Weatherall M. Inhaled corticosteroids in acute asthma: A systemic review and meta-analysis. J Allergy Clin Immunol Pract. 2020;8:605–17.e6. doi: 10.1016/j.jaip.2019.08.051. [DOI] [PubMed] [Google Scholar]
- 164.Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med. 2004;170:836–44. doi: 10.1164/rccm.200401-033OC. [DOI] [PubMed] [Google Scholar]
- 165.Skiepko R, Ziętkowski Z, Lukaszyk M, Budny W, Skiepko U, Milewski R, et al. Changes in blood eosinophilia during omalizumab therapy as a predictor of asthma exacerbation. Postepy Dermatol Alergol. 2014;31:305–9. doi: 10.5114/pdia.2014.40973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Massanari M, Holgate ST, Busse WW, Jimenez P, Kianifard F, Zeldin R. Effect of omalizumab on peripheral blood eosinophilia in allergic asthma. Respir Med. 2010;104:188–96. doi: 10.1016/j.rmed.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 167.Bousquet J, Rabe K, Humbert M, Chung KF, Berger W, Fox H, et al. Predicting and evaluating response to omalizumab in patients with severe allergic asthma. Respir Med. 2007;101:1483–92. doi: 10.1016/j.rmed.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 168.Bousquet J, Siergiejko Z, Swiebocka E, Humbert M, Rabe KF, Smith N, et al. Persistency of response to omalizumab therapy in severe allergic (IgE-mediated) asthma. Allergy. 2011;66:671–8. doi: 10.1111/j.1398-9995.2010.02522.x. [DOI] [PubMed] [Google Scholar]
- 169.Poon AH, Hamid Q. Personalized medicine for asthma: Are we there yet? Ann Thorac Med. 2012;7:55–6. doi: 10.4103/1817-1737.94519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, et al. Mepolizumab for severe eosinophilic asthma (DREAM): A multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380:651–9. doi: 10.1016/S0140-6736(12)60988-X. [DOI] [PubMed] [Google Scholar]
- 171.Bousquet J, Brusselle G, Buhl R, Busse WW, Cruz AA, Djukanovic R, et al. Care pathways for the selection of a biologic in severe asthma. Eur Respir J. 2020;50:1701782. doi: 10.1183/13993003.01782-2017. DOI:10.1183/13993003.01782-2017. Available at: Care pathways for the selection of a biologic in severe asthma (ersjournals.com) [DOI] [PubMed] [Google Scholar]
- 172.Nair P, Wenzel S, Rabe KF, Bourdin A, Lugogo NL, Kuna P, et al. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med. 2017;376:2448–58. doi: 10.1056/NEJMoa1703501. [DOI] [PubMed] [Google Scholar]
- 173.Kostikas K, Brindicci C, Patalano F. blood eosinophils as biomarkers to drive treatment choices in asthma and COPD. Curr Drug Targets. 2018;19:1882–96. doi: 10.2174/1389450119666180212120012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Cockcroft DW. Asthma. Can J Respir Crit Care Sleep Med. 2020;4(Sup 1):S18–20. [Google Scholar]
- 175.Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2013:erj02020–2013. doi: 10.1183/09031936.00202013. [DOI] [PubMed] [Google Scholar]
- 176.Ignacio-Garcia JM, Gonzalez-Santos P. Asthma self-management education program by home monitoring of peak expiratory flow. Am J Respir Crit Care Med. 1995;151:353–9. doi: 10.1164/ajrccm.151.2.7842191. [DOI] [PubMed] [Google Scholar]
- 177.Hawkins G, McMahon AD, Twaddle S, Wood SF, Ford I, Thomson NC. Stepping down inhaled corticosteroids in asthma: Randomised controlled trial. BMJ. 2003;326:1115. doi: 10.1136/bmj.326.7399.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Powell H, Gibson PG. High dose versus low dose inhaled corticosteroid as initial starting dose for asthma in adults and children. Cochrane Database Syst Rev. 2004:CD004109. doi: 10.1002/14651858.CD004109.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Boulet LP, Drollmann A, Magyar P, Timar M, Knight A, Engelstätter R, et al. Comparative efficacy of once-daily ciclesonide and budesonide in the treatment of persistent asthma. Respir Med. 2006;100:785–94. doi: 10.1016/j.rmed.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 180.Rank MA, Hagan JB, Park MA, Podjasek JC, Samant SA, Volcheck GW, et al. The risk of asthma exacerbation after stopping low-dose inhaled corticosteroids: A systematic review and meta-analysis of randomized controlled trials. J Allergy Clin Immunol. 2013;131:724–9. doi: 10.1016/j.jaci.2012.11.038. [DOI] [PubMed] [Google Scholar]
- 181.Brozek JL, Kraft M, Krishnan JA, Cloutier MM, Lazarus SC, Li JT, et al. Long-acting β2-agonist step-off in patients with controlled asthma. Arch Intern Med. 2012;172:1365–75. doi: 10.1001/archinternmed.2012.3250. [DOI] [PubMed] [Google Scholar]
- 182.Masoli M, Weatherall M, Holt S, Beasley R. Budesonide once versus twice-daily administration: Meta-analysis. Respirology. 2004;9:528–34. doi: 10.1111/j.1440-1843.2004.00635.x. [DOI] [PubMed] [Google Scholar]
- 183.Bateman ED, Fairall L, Lombardi DM, English R. Budesonide/formoterol and formoterol provide similar rapid relief in patients with acute asthma showing refractoriness to salbutamol. Respir Res. 2006;7:13. doi: 10.1186/1465-9921-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Randell TL, Donaghue KC, Ambler GR, Cowell CT, Fitzgerald DA, van Asperen PP. Safety of the newer inhaled corticosteroids in childhood asthma. Paediatr Drugs. 2003;5:481–504. doi: 10.2165/00128072-200305070-00005. [DOI] [PubMed] [Google Scholar]
- 185.Cox L, Nelson H, Lockey R, Calabria C, Chacko T, Finegold I, et al. Allergen immunotherapy: A practice parameter third update. J Allergy Clin Immunol. 2011;127:S1–55. doi: 10.1016/j.jaci.2010.09.034. [DOI] [PubMed] [Google Scholar]
- 186.Dhami S, Kakourou A, Asamoah F, Agache I, Lau S, Jutel M, et al. Allergen immunotherapy for allergic asthma: A systematic review and meta-analysis. Allergy. 2017;72:1825–48. doi: 10.1111/all.13208. [DOI] [PubMed] [Google Scholar]
- 187.Dominguez-Ortega J, Delgado J, Blanco C, Prieto L, Arroabarren E, Cimarra M, et al. Specific allergen immunotherapy for the treatment of allergic asthma: A review of current evidence. J Investig Allergol Clin Immunol. 2017;27:1–35. doi: 10.18176/jiaci.0149. [DOI] [PubMed] [Google Scholar]
- 188.Demoly P, Makatsori M, Casale TB, Calderon MA. The potential role of allergen immunotherapy in stepping down asthma treatment. J Allergy Clin Immunol Pract. 2017;5:640–8. doi: 10.1016/j.jaip.2016.11.024. [DOI] [PubMed] [Google Scholar]
- 189.Jacobsen L, Niggemann B, Dreborg S, Ferdousi HA, Halken S, Høst A, et al. Specific immunotherapy has long-term preventive effect of seasonal and perennial asthma: 10-year follow-up on the PAT study. Allergy. 2007;62:943–8. doi: 10.1111/j.1398-9995.2007.01451.x. [DOI] [PubMed] [Google Scholar]
- 190.Rice JL, Diette GB, Suarez-Cuervo C, Brigham EP, Lin SY, Ramanathan M, Jr, et al. Allergen-specific immunotherapy in the treatment of pediatric asthma: A systematic review. Pediatrics. 2018;141:e20173833. doi: 10.1542/peds.2017-3833. [DOI] [PubMed] [Google Scholar]
- 191.Elliott J, Kelly SE, Johnston A, Skidmore B, Gomes T, Wells GA. Allergen immunotherapy for the treatment of allergic rhinitis and/or asthma: An umbrella review. CMAJ Open. 2017;5:E373–85. doi: 10.9778/cmajo.20160066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Currie GP, Douglas JG, Heaney LG. Difficult to treat asthma in adults. BMJ. 2009;338:b494. doi: 10.1136/bmj.b494. [DOI] [PubMed] [Google Scholar]
- 193.Brożek JL, Bousquet J, Agache I, Agarwal A, Bachert C, Bosnic-Anticevich S, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) Guidelines-2016 revision. J Allergy Clin Immunol. 2017;140:950–8. doi: 10.1016/j.jaci.2017.03.050. [DOI] [PubMed] [Google Scholar]
- 194.Sullivan SD, Rasouliyan L, Russo PA, Kamath T, Chipps BE. TENOR Study Group. Extent, patterns, and burden of uncontrolled disease in severe or difficult-to-treat asthma. Allergy. 2007;62:126–33. doi: 10.1111/j.1398-9995.2006.01254.x. [DOI] [PubMed] [Google Scholar]
- 195.Serra-Batlles J, Plaza V, Morejón E, Comella A, Brugués J. Costs of asthma according to the degree of severity. Eur Respir J. 1998;12:1322–6. doi: 10.1183/09031936.98.12061322. [DOI] [PubMed] [Google Scholar]
- 196.Chen H, Blanc PD, Hayden ML, Bleecker ER, Chawla A, Lee JH, et al. Assessing productivity loss and activity impairment in severe or difficult-to-treat asthma. Value Health. 2008;11:231–9. doi: 10.1111/j.1524-4733.2007.00229.x. [DOI] [PubMed] [Google Scholar]
- 197.Tiwari A, Guglani V, Jat KR. Ketamine versus aminophylline for acute asthma in children: A randomized, controlled trial. Ann Thorac Med. 2016;11:283–8. doi: 10.4103/1817-1737.191874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Porsbjerg C, Ulrik C, Skjold T, Backer V, Laerum B, Lehman S, et al. Nordic consensus statement on the systematic assessment and management of possible severe asthma in adults. Eur Clin Respir J. 2018;5:1440868. doi: 10.1080/20018525.2018.1440868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Lee JH, Haselkorn T, Borish L, Rasouliyan L, Chipps BE, Wenzel SE. Risk factors associated with persistent airflow limitation in severe or difficult-to-treat asthma: Insights from the TENOR study. Chest. 2007;132:1882–9. doi: 10.1378/chest.07-0713. [DOI] [PubMed] [Google Scholar]
- 200.Sturdy PM, Victor CR, Anderson HR, Bland JM, Butland BK, Harrison BD, et al. Psychological, social and health behaviour risk factors for deaths certified as asthma: A national case-control study. Thorax. 2002;57:1034–9. doi: 10.1136/thorax.57.12.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Butler C, Heaney LG. Risk factors of frequent exacerbations in difficult-to-treat asthma. Eur Respir J. 2006;27:1324–5. doi: 10.1183/09031936.06.00022606. [DOI] [PubMed] [Google Scholar]
- 202.Gaga M, Papageorgiou N, Yiourgioti G, Karydi P, Liapikou A, Bitsakou H, et al. Risk factors and characteristics associated with severe and difficult to treat asthma phenotype: An analysis of the ENFUMOSA group of patients based on the ECRHS questionnaire. Clin Exp Allergy. 2005;35:954–9. doi: 10.1111/j.1365-2222.2005.02281.x. [DOI] [PubMed] [Google Scholar]
- 203.Sullivan SD, Wenzel SE, Bresnahan BW, Zheng B, Lee JH, Pritchard M, et al. Association of control and risk of severe asthma-related events in severe or difficult-to-treat asthma patients. Allergy. 2007;62:655–60. doi: 10.1111/j.1398-9995.2007.01383.x. [DOI] [PubMed] [Google Scholar]
- 204.Robinson DS, Campbell DA, Durham SR, Pfeffer J, Barnes PJ, Chung KF, et al. Systematic assessment of difficult-to-treat asthma. Eur Respir J. 2003;22:478–83. doi: 10.1183/09031936.03.00017003. [DOI] [PubMed] [Google Scholar]
- 205.Natarajan S, Subramanian P. Allergic bronchopulmonary aspergillosis: A clinical review of 24 patients: Are we right in frequent serologic monitoring? Ann Thorac Med. 2014;9:216–20. doi: 10.4103/1817-1737.140130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Jani AL, Hamilos DL. Current thinking on the relationship between rhinosinusitis and asthma. J Asthma. 2005;42:1–7. doi: 10.1081/jas-200044744. [DOI] [PubMed] [Google Scholar]
- 207.Koczulla AR, Vogelmeier CF, Garn H, Renz H. New concepts in asthma: Clinical phenotypes and pathophysiological mechanisms. Drug Discov Today. 2017;22:388–96. doi: 10.1016/j.drudis.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 208.Saji J, Arai M, Yamamoto T, Mineshita M, Miyazawa T. Efficacy of omalizumab in patients with severe asthma using the asthma health questionnaire and asthma control test. Arerugi. 2014;63:1338–47. [PubMed] [Google Scholar]
- 209.Storms W, Bowdish MS, Farrar JR. Omalizumab and asthma control in patients with moderate-to-severe allergic asthma: A 6-year pragmatic data review. Allergy Asthma Proc. 2012;33:172–7. doi: 10.2500/aap.2012.33.3527. [DOI] [PubMed] [Google Scholar]
- 210.Heaney LG, Brightling CE, Menzies-Gow A, Stevenson M, Niven RM. British Thoracic Society Difficult Asthma Network. Refractory asthma in the UK: Cross-sectional findings from a UK multicentre registry. Thorax. 2010;65:787–94. doi: 10.1136/thx.2010.137414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Adcock IM, Lane SJ, Brown CR, Peters MJ, Lee TH, Barnes PJ. Differences in binding of glucocorticoid receptor to DNA in steroid-resistant asthma. J Immunol. 1995;154:3500–5. [PubMed] [Google Scholar]
- 212.Barnes PJ. Corticosteroid resistance in airway disease. Proc Am Thorac Soc. 2004;1:264–8. doi: 10.1513/pats.200402-014MS. [DOI] [PubMed] [Google Scholar]
- 213.Ayres JG. Pseudo-steroid resistant asthma. Thorax. 1999;54:956. doi: 10.1136/thx.54.10.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Campbell JD, Blough DK, Sullivan SD. Comparison of guideline-based control definitions and associations with outcomes in severe or difficult-to-treat asthma. Ann Allergy Asthma Immunol. 2008;101:474–81. doi: 10.1016/S1081-1206(10)60285-2. [DOI] [PubMed] [Google Scholar]
- 215.Gibson PG, Yang IA, Upham JW, Reynolds PN, Hodge S, James AL, et al. Effect of azithromycin on asthma exacerbations and quality of life in adults with persistent uncontrolled asthma (AMAZES): A randomised, double-blind, placebo-controlled trial. Lancet. 2017;390:659–68. doi: 10.1016/S0140-6736(17)31281-3. [DOI] [PubMed] [Google Scholar]
- 216.d'Hooghe JN, Ten Hacken NH, Weersink EJ, Sterk PJ, Annema JT, Bonta PI. Emerging understanding of the mechanism of action of bronchial thermoplasty in asthma. Pharmacol Ther. 2018;181:101–7. doi: 10.1016/j.pharmthera.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 217.Iyer VN, Lim KG. Bronchial thermoplasty: Where there is smoke, there is fire. Allergy Asthma Proc. 2015;36:251–5. doi: 10.2500/aap.2015.36.3857. [DOI] [PubMed] [Google Scholar]
- 218.Michaud G, Ernst A. Counterpoint: Efficacy of bronchial thermoplasty for patients with severe asthma. Is there sufficient evidence? Not yet. Chest. 2011;140:576–7. doi: 10.1378/chest.11-1390. [DOI] [PubMed] [Google Scholar]
- 219.Wu Q, Xing Y, Zhou X, Wang D. Meta-analysis of the efficacy and safety of bronchial thermoplasty in patients with moderate-to-severe persistent asthma. J Int Med Res. 2011;39:10–22. doi: 10.1177/147323001103900102. [DOI] [PubMed] [Google Scholar]
- 220.Dharmage SC, Perret JL, Custovic A. Epidemiology of asthma in children and adults. Front Pediatr. 2019;7:246. doi: 10.3389/fped.2019.00246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Suruki RY, Daugherty JB, Boudiaf N, Albers FC. The frequency of asthma exacerbations and healthcare utilization in patients with asthma from the UK and USA. BMC Pulm Med. 2017;17:74. doi: 10.1186/s12890-017-0409-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Alahmadi TS, Banjari MA, Alharbi AS. The prevalence of childhood asthma in Saudi Arabia. Int J Pediatr Adolesc Med. 2019;6:74–7. doi: 10.1016/j.ijpam.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Ali F, Behbehani N, Alomair N, Taher A. Fatal and near-fatal thunderstorm asthma epidemic in a desert country. Ann Thorac Med. 2019;14:155–60. doi: 10.4103/atm.ATM_258_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Serrano-Pariente J, Plaza V. Near-fatal asthma: A heterogeneous clinical entity. Curr Opin Allergy Clin Immunol. 2017;17:28–35. doi: 10.1097/ACI.0000000000000333. [DOI] [PubMed] [Google Scholar]
- 225.D'Amato G, Vitale C, Lanza M, Sanduzzi A, Molino A, Mormile M, et al. Near fatal asthma: Treatment and prevention. Eur Ann Allergy Clin Immunol. 2016;48:116–22. [PubMed] [Google Scholar]
- 226.Al-Dorzi HM, Al-Shammary HA, Al-Shareef SY, Tamim HM, Shammout K, Al Dawood A, et al. Risk factors, management and outcomes of patients admitted with near fatal asthma to a tertiary care hospital in Riyadh. Ann Thorac Med. 2014;9:33–8. doi: 10.4103/1817-1737.124441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Fergeson JE, Patel SS, Lockey RF. Acute asthma, prognosis, and treatment. J Allergy Clin Immunol. 2017;139:438–47. doi: 10.1016/j.jaci.2016.06.054. [DOI] [PubMed] [Google Scholar]
- 228.Al-Dawood KM. Pattern and risk factors associated with hospital emergency visits among schoolboys with bronchial asthma in Al-Khobar. Ann Saudi Med. 2002;22:29–33. doi: 10.5144/0256-4947.2002.29. [DOI] [PubMed] [Google Scholar]
- 229.Courtney AU, McCarter DF, Pollart SM. Childhood asthma: Treatment update. Am Fam Physician. 2005;71:1959–68. [PubMed] [Google Scholar]
- 230.Bai TR, Cooper J, Koelmeyer T, Paré PD, Weir TD. The effect of age and duration of disease on airway structure in fatal asthma. Am J Respir Crit Care Med. 2000;162:663–9. doi: 10.1164/ajrccm.162.2.9907151. [DOI] [PubMed] [Google Scholar]
- 231.Perrin K, Wijesinghe M, Healy B, Wadsworth K, Bowditch R, Bibby S, et al. Randomised controlled trial of high concentration versus titrated oxygen therapy in severe exacerbations of asthma. Thorax. 2011;66:937–41. doi: 10.1136/thx.2010.155259. [DOI] [PubMed] [Google Scholar]
- 232.Geng W, Batu W, You S, Tong Z, He H. High-flow nasal cannula: A promising oxygen therapy for patients with severe bronchial asthma complicated with respiratory failure. Can Respir J. 2020;2020:2301712. doi: 10.1155/2020/2301712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Donohue JF, Wise R, Busse WW, Garfinkel S, Zubek VB, Ghafouri M, et al. Efficacy and safety of ipratropium bromide/albuterol compared with albuterol in patients with moderate-to-severe asthma: A randomized controlled trial. BMC Pulm Med. 2016;16:65. doi: 10.1186/s12890-016-0223-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Memon BN, Parkash A, Ahmed Khan KM, Gowa MA, Bai C. Response to nebulized salbutamol versus combination with ipratropium bromide in children with acute severe asthma. J Pak Med Assoc. 2016;66:243–6. [PubMed] [Google Scholar]
- 235.Normansell R, Kew KM, Mansour G. Different oral corticosteroid regimens for acute asthma. Cochrane Database Syst Rev. 2016:CD011801. doi: 10.1002/14651858.CD011801.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Kolbe J, Fergusson W, Vamos M, Garrett J. Case-control study of severe life threatening asthma (SLTA) in adults: Demographics, health care, and management of the acute attack. Thorax. 2000;55:1007–15. doi: 10.1136/thorax.55.12.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Barnard A. Management of an acute asthma attack. Aust Fam Physician. 2005;34:531–4. [PubMed] [Google Scholar]
- 238.Griffiths B, Kew KM. Intravenous magnesium sulfate for treating children with acute asthma in the emergency department. Cochrane Database Syst Rev. 2016;4:CD011050. doi: 10.1002/14651858.CD011050.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Mitchell I, Tough SC, Semple LK, Green FH, Hessel PA. Near-fatal asthma: A population-based study of risk factors. Chest. 2002;121:1407–13. doi: 10.1378/chest.121.5.1407. [DOI] [PubMed] [Google Scholar]
- 240.Plaza V, Serrano J, Picado C, Sanchis J. High Risk Asthma Research Group. Frequency and clinical characteristics of rapid-onset fatal and near-fatal asthma. Eur Respir J. 2002;19:846–52. doi: 10.1183/09031936.02.00241502. [DOI] [PubMed] [Google Scholar]
- 241.Bousquet J, Jutel M, Akdis CA, Klimek L, Pfaar O, Nadeau KC, et al. ARIA-EAACI statement on asthma and COVID-19 (June 2, 2020) Allergy. 2020 doi: 10.1111/all.14471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Warren A, Chiu YD, Villar SS, Fowles JA, Symes N, Barker J, et al. Outcomes of the NHS England National Extracorporeal Membrane Oxygenation Service for adults with respiratory failure: A multicentre observational cohort study. Br J Anaesth. 2020;125:259–66. doi: 10.1016/j.bja.2020.05.065. [DOI] [PubMed] [Google Scholar]
- 243.Gaude GS. Pulmonary manifestations of gastroesophageal reflux disease. Ann Thorac Med. 2009;4:115–23. doi: 10.4103/1817-1737.53347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Havemann BD, Henderson CA, El-Serag HB. The association between gastro-oesophageal reflux disease and asthma: A systematic review. Gut. 2007;56:1654–64. doi: 10.1136/gut.2007.122465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Houghton LA, Lee AS, Badri H, DeVault KR, Smith JA. Respiratory disease and the oesophagus: Reflux, reflexes and microaspiration. Nat Rev Gastroenterol Hepatol. 2016;13:445–60. doi: 10.1038/nrgastro.2016.91. [DOI] [PubMed] [Google Scholar]
- 246.Asano K, Suzuki H. Silent acid reflux and asthma control. N Engl J Med. 2009;360:1551–3. doi: 10.1056/NEJMe0900117. [DOI] [PubMed] [Google Scholar]
- 247.Cruz AA, Popov T, Pawankar R, Annesi-Maesano I, Fokkens W, Kemp J, et al. Common characteristics of upper and lower airways in rhinitis and asthma: ARIA update, in collaboration with GA(2)LEN. Allergy. 2007;62(Suppl 84):1–41. doi: 10.1111/j.1398-9995.2007.01551.x. [DOI] [PubMed] [Google Scholar]
- 248.Gleadhill C, Speth MM, Gengler I, Phillips KM, Hoehle LP, Caradonna DS, et al. Chronic rhinosinusitis disease burden is associated with asthma-related emergency department usage. Eur Arch Otorhinolaryngol. 2020:1–7. doi: 10.1007/s00405-020-06259-2. [DOI] [PubMed] [Google Scholar]
- 249.Hansbro PM, Kim RY, Starkey MR, Donovan C, Dua K, Mayall JR, et al. Mechanisms and treatments for severe, steroid-resistant allergic airway disease and asthma. Immunol Rev. 2017;278:41–62. doi: 10.1111/imr.12543. [DOI] [PubMed] [Google Scholar]
- 250.Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141:1169–79. doi: 10.1016/j.jaci.2018.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Desai AG, Togias A, Schechter C, Fisher B, Parow A, Skloot G. Peripheral airways dysfunction in obesity reflects increased bronchomotor tone. J Allergy Clin Immunol. 2015;135:820–2. doi: 10.1016/j.jaci.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 252.Scott HA, Gibson PG, Garg ML, Pretto JJ, Morgan PJ, Callister R, et al. Dietary restriction and exercise improve airway inflammation and clinical outcomes in overweight and obese asthma: A randomized trial. Clin Exp Allergy. 2013;43:36–49. doi: 10.1111/cea.12004. [DOI] [PubMed] [Google Scholar]
- 253.Moreira A, Bonini M, Garcia-Larsen V, Bonini S, Del Giacco SR, Agache I, et al. Weight loss interventions in asthma: EAACI evidence-based clinical practice guideline (Part I) Allergy. 2013;68:425–39. doi: 10.1111/all.12106. [DOI] [PubMed] [Google Scholar]
- 254.Boulet LP, Turcotte H, Martin J, Poirier P. Effect of bariatric surgery on airway response and lung function in obese subjects with asthma. Respir Med. 2012;106:651–60. doi: 10.1016/j.rmed.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 255.Cao Y, Lin SH, Zhu D, Xu F, Chen ZH, Shen HH, et al. WeChat public account use improves clinical control of cough-variant asthma: A randomized controlled trial. Med Sci Monit. 2018;24:1524–32. doi: 10.12659/MSM.907284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Achilleos A. Evidence-based evaluation and management of chronic cough. Med Clin North Am. 2016;100:1033–45. doi: 10.1016/j.mcna.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 257.Morice AH, McGarvey L, Pavord I. British Thoracic Society Cough Guideline Group. Recommendations for the management of cough in adults. Thorax. 2006;61(Suppl 1):i1–24. doi: 10.1136/thx.2006.065144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Spector SL, Tan RA. Effectiveness of montelukast in the treatment of cough variant asthma. Ann Allergy Asthma Immunol. 2004;93:232–6. doi: 10.1016/S1081-1206(10)61493-7. [DOI] [PubMed] [Google Scholar]
- 259.Desai D, Brightling C. Cough due to asthma, cough-variant asthma and non-asthmatic eosinophilic bronchitis. Otolaryngol Clin North Am. 2010;43:123–30, x. doi: 10.1016/j.otc.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 260.Diver S, Russell RJ, Brightling CE. Cough and Eosinophilia. J Allergy Clin Immunol Pract. 2019;7:1740–7. doi: 10.1016/j.jaip.2019.04.048. [DOI] [PubMed] [Google Scholar]
- 261.Weiler JM, Brannan JD, Randolph CC, Hallstrand TS, Parsons J, Silvers W, et al. Exercise-induced bronchoconstriction update-2016. J Allergy Clin Immunol. 2016;138:1292–5.e36. doi: 10.1016/j.jaci.2016.05.029. [DOI] [PubMed] [Google Scholar]
- 262.Dreßler M, Friedrich T, Lasowski N, Herrmann E, Zielen S, Schulze J. Predictors and reproducibility of exercise-induced bronchoconstriction in cold air. BMC Pulm Med. 2019;19:94. doi: 10.1186/s12890-019-0845-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Parsons JP, Hallstrand TS, Mastronarde JG, Kaminsky DA, Rundell KW, Hull JH, et al. An official American Thoracic Society clinical practice guideline: Exercise-induced bronchoconstriction. Am J Respir Crit Care Med. 2013;187:1016–27. doi: 10.1164/rccm.201303-0437ST. [DOI] [PubMed] [Google Scholar]
- 264.Lazarinis N, Jørgensen L, Ekström T, Bjermer L, Dahlén B, Pullerits T, et al. Combination of budesonide/formoterol on demand improves asthma control by reducing exercise-induced bronchoconstriction. Thorax. 2014;69:130–6. doi: 10.1136/thoraxjnl-2013-203557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Laidlaw TM, Boyce JA. Aspirin-exacerbated respiratory disease--New prime suspects. N Engl J Med. 2016;374:484–8. doi: 10.1056/NEJMcibr1514013. [DOI] [PubMed] [Google Scholar]
- 266.Rajan JP, Wineinger NE, Stevenson DD, White AA. Prevalence of aspirin-exacerbated respiratory disease among asthmatic patients: A meta-analysis of the literature. J Allergy Clin Immunol. 2015;135:676–81.e1. doi: 10.1016/j.jaci.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 267.Szczeklik A, Stevenson DD. Aspirin-induced asthma: Advances in pathogenesis, diagnosis, and management. J Allergy Clin Immunol. 2003;111:913–21. doi: 10.1067/mai.2003.1487. [DOI] [PubMed] [Google Scholar]
- 268.White AA, Stevenson DD. Aspirin-exacerbated respiratory disease. N Engl J Med. 2018;379:1060–70. doi: 10.1056/NEJMra1712125. [DOI] [PubMed] [Google Scholar]
- 269.Woessner KM, Simon RA, Stevenson DD. The safety of celecoxib in patients with aspirin-sensitive asthma. Arthritis Rheum. 2002;46:2201–6. doi: 10.1002/art.10426. [DOI] [PubMed] [Google Scholar]
- 270.Cahill KN, Boyce JA. Aspirin-exacerbated respiratory disease: Mediators and mechanisms of a clinical disease. J Allergy Clin Immunol. 2017;139:764–6. doi: 10.1016/j.jaci.2016.09.025. [DOI] [PubMed] [Google Scholar]
- 271.Park JS, Jang AS, Park SW, Lee YM, Uh ST, Kim YH, et al. Protection of leukotriene receptor antagonist against aspirin-induced bronchospasm in asthmatics. Allergy Asthma Immunol Res. 2010;2:48–54. doi: 10.4168/aair.2010.2.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Cohen JM, Bateman BT, Huybrechts KF, Mogun H, Yland J, Schatz M, et al. Poorly controlled asthma during pregnancy remains common in the United States. J Allergy Clin Immunol Pract. 2019;7:2672–80.e10. doi: 10.1016/j.jaip.2019.05.043. [DOI] [PubMed] [Google Scholar]
- 273.Bonham CA, Patterson KC, Strek ME. Asthma outcomes and management during pregnancy. Chest. 2018;153:515–27. doi: 10.1016/j.chest.2017.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Blais L, Kettani FZ, Forget A, Beauchesne MF, Lemière C. Asthma exacerbations during the first trimester of pregnancy and congenital malformations: Revisiting the association in a large representative cohort. Thorax. 2015;70:647–52. doi: 10.1136/thoraxjnl-2014-206634. [DOI] [PubMed] [Google Scholar]
- 275.Murphy VE, Gibson PG, Smith R, Clifton VL. Asthma during pregnancy: Mechanisms and treatment implications. Eur Respir J. 2005;25:731–50. doi: 10.1183/09031936.05.00085704. [DOI] [PubMed] [Google Scholar]
- 276.Holland SM, Thomson KD. Acute severe asthma presenting in late pregnancy. Int J Obstet Anesth. 2006;15:75–8. doi: 10.1016/j.ijoa.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 277.Hanania NA, Belfort MA. Acute asthma in pregnancy. Crit Care Med. 2005;33:S319–24. doi: 10.1097/01.ccm.0000182789.14710.a1. [DOI] [PubMed] [Google Scholar]
- 278.Smy L, Chan AC, Bozzo P, Koren G. Is it safe to use inhaled corticosteroids in pregnancy? Can Fam Physician. 2014;60:809. [PMC free article] [PubMed] [Google Scholar]
- 279.Rahimi R, Nikfar S, Abdollahi M. Meta-analysis finds use of inhaled corticosteroids during pregnancy safe: A systematic meta-analysis review. Hum Exp Toxicol. 2006;25:447–52. doi: 10.1191/0960327106het647oa. [DOI] [PubMed] [Google Scholar]
- 280.Gluck JC, Gluck PA. The effect of pregnancy on the course of asthma. Immunol Allergy Clin North Am. 2006;26:63–80. doi: 10.1016/j.iac.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 281.Sevelsted A, Stokholm J, Bisgaard H. Risk of asthma from cesarean delivery depends on membrane rupture. J Pediatr. 2016;171:38–42.e4. doi: 10.1016/j.jpeds.2015.12.066. [DOI] [PubMed] [Google Scholar]
- 282.Vallera C, Choi LO, Cha CM, Hong RW. Uterotonic medications: Oxytocin, methylergonovine, carboprost, misoprostol. Anesthesiol Clin. 2017;35:207–19. doi: 10.1016/j.anclin.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 283.Arora N, Mahajan K, Jana N, Maiti TK, Mandal D, Pandey R. Successful pregnancy outcome among women with end-stage renal disease requiring haemodialysis. J Indian Med Assoc. 2009;107:237–8. [PubMed] [Google Scholar]
- 284.Perlow JH, Montgomery D, Morgan MA, Towers CV, Porto M. Severity of asthma and perinatal outcome. Am J Obstet Gynecol. 1992;167:963–7. doi: 10.1016/s0002-9378(12)80020-2. [DOI] [PubMed] [Google Scholar]
- 285.Levy ML, Nicholson PJ. Occupational asthma case finding: A role for primary care. Br J Gen Pract. 2004;54:731–3. [PMC free article] [PubMed] [Google Scholar]
- 286.Baur X, Aasen TB, Burge PS, Heederik D, Henneberger PK, Maestrelli P, et al. The management of work-related asthma guidelines: A broader perspective. Eur Respir Rev. 2012;21:125–39. doi: 10.1183/09059180.00004711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Legiest B, Nemery B. Management of work-related asthma: Guidelines and challenges. Eur Respir Rev. 2012;21:79–81. doi: 10.1183/09059180.00002912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Al Ghobain M, Al-Hajjaj MS, Wali SO. Prevalence of chronic obstructive pulmonary disease among smokers attending primary healthcare clinics in Saudi Arabia. Ann Saudi Med. 2011;31:129–33. doi: 10.4103/0256-4947.77485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: What are its features and how important is it? Thorax. 2009;64:728–35. doi: 10.1136/thx.2008.108027. [DOI] [PubMed] [Google Scholar]
- 290.Kauppi P, Kupiainen H, Lindqvist A, Tammilehto L, Kilpeläinen M, Kinnula VL, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011;48:279–85. doi: 10.3109/02770903.2011.555576. [DOI] [PubMed] [Google Scholar]
- 291.Hardin M, Silverman EK, Barr RG, Hansel NN, Schroeder JD, Make BJ, et al. The clinical features of the overlap between COPD and asthma. Respir Res. 2011;12:127. doi: 10.1186/1465-9921-12-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 Update. An official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200:e70–88. doi: 10.1164/rccm.201908-1590ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Naja AS, Permaul P, Phipatanakul W. Taming asthma in school-aged children: A comprehensive review. J Allergy Clin Immunol Pract. 2018;6:726–35. doi: 10.1016/j.jaip.2018.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Denlinger LC, Sorkness CA, Chinchilli VM, Lemanske RF., Jr Guideline-defining asthma clinical trials of the National Heart, Lung, and Blood Institute's Asthma Clinical Research Network and Childhood Asthma Research and Education Network. J Allergy Clin Immunol. 2007;119:3–11. doi: 10.1016/j.jaci.2006.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Ferrante G, La Grutta S. The burden of pediatric asthma. Front Pediatr. 2018;6:186. doi: 10.3389/fped.2018.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Almakrami IH, Alzahrani EA, Alqarni SA. Assessment of knowledge and adherence of pediatric residents to Saudi initiative asthma (SINA) guidelines in Saudi Arabia. The Egyptian Journal of Hospital Medicine. 70(4):686–691. [Google Scholar]
- 297.Yang CL, Simons E, Foty RG, Subbarao P, To T, Dell SD. Misdiagnosis of asthma in schoolchildren. Pediatr Pulmonol. 2017;52:293–302. doi: 10.1002/ppul.23541. [DOI] [PubMed] [Google Scholar]
- 298.Danvers L, Lo DK, Gaillard EA. The role of objective tests to support a diagnosis of asthma in children. Paediatr Respir Rev. 2020;33:52–7. doi: 10.1016/j.prrv.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 299.Kann K, Long B, Koyfman A. Clinical mimics: An emergency medicine-focused review of asthma mimics. J Emerg Med. 2017;53:195–201. doi: 10.1016/j.jemermed.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 300.Hederos CA, Janson S, Andersson H, Hedlin G. Chest X-ray investigation in newly discovered asthma. Pediatr Allergy Immunol. 2004;15:163–5. doi: 10.1046/j.1399-3038.2003.00098.x. [DOI] [PubMed] [Google Scholar]
- 301.Gauthier MC, Fajt ML. Is It Asthma? Recognizing Asthma Mimics. Difficult To Treat Asthma. New York, USA: Springer; 2020. pp. 25–38. [Google Scholar]
- 302.Alfonso J, Pérez S, Bou R, Amat A, Ruiz I, Mora A, et al. Asthma prevalence and risk factors in school children: The RESPIR longitudinal study. Allergol Immunopathol (Madr) 2020;48:223–31. doi: 10.1016/j.aller.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 303.Al-Shamrani A, Bagais K, Alenazi A, Alqwaiee M, Al-Harbi AS. Wheezing in children: Approaches to diagnosis and management. Int J Pediatr Adolesc Med. 2019;6:68–73. doi: 10.1016/j.ijpam.2019.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Chipps BE, Bacharier LB, Harder JM. Phenotypic expressions of childhood wheezing and asthma: Implications for therapy. J Pediatr. 2011;158:878–84e1. doi: 10.1016/j.jpeds.2011.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Fahy JV, O'Byrne PM. “Reactive airways disease”.A lazy term of uncertain meaning that should be abandoned. Am J Respir Crit Care Med. 2001;163:822–3. doi: 10.1164/ajrccm.163.4.2005049. [DOI] [PubMed] [Google Scholar]
- 306.Weinberger MI, Sirey JA, Bruce ML, Heo M, Papademetriou E, Meyers BS. Predictors of major depression six months after admission for outpatient treatment. Psychiatr Serv. 2008;59:1211–5. doi: 10.1176/appi.ps.59.10.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Weinberger M. Pediatric asthma and related allergic and nonallergic diseases: Patient-oriented evidence-based essentials that matter. Pediatric Health. 2008;2:631–50. [Google Scholar]
- 308.Bubshait DK, Albuali WH, Yousef AA, Obeid OE, Alkharsah KR, Hassan MI, et al. Clinical description of human bocavirus viremia in children with LRTI, Eastern Province, Saudi Arabia. Ann Thorac Med. 2015;10:146–9. doi: 10.4103/1817-1737.151437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Just J, Gouvis-Echraghi R, Couderc R, Guillemot-Lambert N, Saint-Pierre P. Novel severe wheezy young children phenotypes: Boys atopic multiple-trigger and girls nonatopic uncontrolled wheeze. J Allergy Clin Immunol. 2012;130:103–10e8. doi: 10.1016/j.jaci.2012.02.041. [DOI] [PubMed] [Google Scholar]
- 310.Savenije OE, Kerkhof M, Koppelman GH, Postma DS. Predicting who will have asthma at school age among preschool children. J Allergy Clin Immunol. 2012;130:325–31. doi: 10.1016/j.jaci.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 311.Guilbert TW, Morgan WJ, Zeiger RS, Bacharier LB, Boehmer SJ, Krawiec M, et al. Atopic characteristics of children with recurrent wheezing at high risk for the development of childhood asthma. J Allergy Clin Immunol. 2004;114:1282–7. doi: 10.1016/j.jaci.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 312.Castro-Rodriguez JA. The Asthma Predictive Index: A very useful tool for predicting asthma in young children. J Allergy Clin Immunol. 2010;126:212–6. doi: 10.1016/j.jaci.2010.06.032. [DOI] [PubMed] [Google Scholar]
- 313.Chang TS, Lemanske RF, Jr, Guilbert TW, Gern JE, Coen MH, Evans MD, et al. Evaluation of the modified asthma predictive index in high-risk preschool children. J Allergy Clin Immunol Pract. 2013;1:152–6. doi: 10.1016/j.jaip.2012.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Pedersen SE, Hurd SS, Lemanske RF, Jr, Becker A, Zar HJ, Sly PD, et al. Global strategy for the diagnosis and management of asthma in children 5 years and younger. Pediatr Pulmonol. 2011;46:1–7. doi: 10.1002/ppul.21321. [DOI] [PubMed] [Google Scholar]
- 315.Yousef AA, Al-Shamrani AS, Al-Haider SA, Said YS, Al Harbi S, Al-Harbi AS. Pediatric pulmonary services in Saudi Arabia. Ann Thorac Med. 2013;8:224–8. doi: 10.4103/1817-1737.118502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Yawn BP, Brenneman SK, Allen-Ramey FC, Cabana MD, Markson LE. Assessment of asthma severity and asthma control in children. Pediatrics. 2006;118:322–9. doi: 10.1542/peds.2005-2576. [DOI] [PubMed] [Google Scholar]
- 317.Bakel LA, Hamid J, Ewusie J, Liu K, Mussa J, Straus S, et al. International Variation in Asthma and Bronchiolitis Guidelines. Pediatrics. 2017;140:e20170092. doi: 10.1542/peds.2017-0092. [DOI] [PubMed] [Google Scholar]
- 318.Liu AH, Zeiger R, Sorkness C, Mahr T, Ostrom N, Burgess S, et al. Development and cross-sectional validation of the childhood asthma control test. J Allergy Clin Immunol. 2007;119:817–25. doi: 10.1016/j.jaci.2006.12.662. [DOI] [PubMed] [Google Scholar]
- 319.Liu AH, Zeiger RS, Sorkness CA, Ostrom NK, Chipps BE, Rosa K, et al. The Childhood Asthma Control Test: Retrospective determination and clinical validation of a cut point to identify children with very poorly controlled asthma. J Allergy Clin Immunol. 2010;126:267–73. 273.e1. doi: 10.1016/j.jaci.2010.05.031. [DOI] [PubMed] [Google Scholar]
- 320.Zeiger RS, Mellon M, Chipps B, Murphy KR, Schatz M, Kosinski M, et al. Test for Respiratory and Asthma Control in Kids (TRACK): Clinically meaningful changes in score. J Allergy Clin Immunol. 2011;128:983–8. doi: 10.1016/j.jaci.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 321.Bisgaard H, Allen DB, Milanowski J, Kalev I, Willits L, Davies P. Twelve-month safety and efficacy of inhaled fluticasone propionate in children aged 1 to 3 years with recurrent wheezing. Pediatrics. 2004;113:e87–94. doi: 10.1542/peds.113.2.e87. [DOI] [PubMed] [Google Scholar]
- 322.Leflein JG, Szefler SJ, Murphy KR, Fitzpatrick S, Cruz-Rivera M, Miller CJ, et al. Nebulized budesonide inhalation suspension compared with cromolyn sodium nebulizer solution for asthma in young children: Results of a randomized outcomes trial. Pediatrics. 2002;109:866–72. doi: 10.1542/peds.109.5.866. [DOI] [PubMed] [Google Scholar]
- 323.Simons E. Use of beclomethasone dipropionate as rescue Treatment for Children With Mild Persistent Asthma (TREXA): A randomized, double-blind, placebo-controlled trial. Pediatrics. 2011;128(Supp 3):S131–S2. doi: 10.1016/S0140-6736(10)62145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Dufour V, Millon L, Faucher JF, Bard E, Robinet E, Piarroux R, et al. Effects of a short-course of amoxicillin/clavulanic acid on systemic and mucosal immunity in healthy adult humans. Int Immunopharmacol. 2005;5:917–28. doi: 10.1016/j.intimp.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 325.Adams NP, Bestall JB, Jones PW. Inhaled beclomethasone versus placebo for chronic asthma. Cochrane Database Syst Rev. 2000:CD002738. doi: 10.1002/14651858.CD002738. [DOI] [PubMed] [Google Scholar]
- 326.Jackson DJ, Bacharier LB, Mauger DT, Boehmer S, Beigelman A, Chmiel JF, et al. Quintupling inhaled glucocorticoids to prevent childhood asthma exacerbations. N Engl J Med. 2018;378:891–901. doi: 10.1056/NEJMoa1710988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Bacharier LB, Phillips BR, Zeiger RS, Szefler SJ, Martinez FD, Lemanske RF, Jr, et al. Episodic use of an inhaled corticosteroid or leukotriene receptor antagonist in preschool children with moderate-to-severe intermittent wheezing. J Allergy Clin Immunol. 2008;122:1127–35e8. doi: 10.1016/j.jaci.2008.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Reddel HK, Foster JM. Inconclusive evidence about the efficacy of diverse strategies for intermittent versus daily inhaled corticosteroids for persistent asthma in adults and children. Evid Based Med. 2014;19:e2. doi: 10.1136/eb-2013-101249. [DOI] [PubMed] [Google Scholar]
- 329.Zhang L, Pruteanu AI, Prietsch SO, Chauhan BF, Ducharme FM. Cochrane in context: Inhaled corticosteroids in children with persistent asthma: Effects on growth and dose-response effects on growth. Evid Based Child Health. 2014;9:1047–51. doi: 10.1002/ebch.1984. [DOI] [PubMed] [Google Scholar]
- 330.Pruteanu AI, Chauhan BF, Zhang L, Prietsch SO, Ducharme FM. Inhaled corticosteroids in children with persistent asthma: Dose-response effects on growth. Evid Based Child Health. 2014;9:931–1046. doi: 10.1002/ebch.1989. [DOI] [PubMed] [Google Scholar]
- 331.Benard B, Bastien V, Vinet B, Yang R, Krajinovic M, Ducharme FM. Neuropsychiatric adverse drug reactions in children initiated on montelukast in real-life practice. Eur Respir J. 2017;50:1700148. doi: 10.1183/13993003.00148-2017. [DOI] [PubMed] [Google Scholar]
- 332.Urdaneta E. Neuropsychiatric adverse drug reactions in children initiated on montelukast in real-life practice. Eur Respir J. 2017;50:1700148. doi: 10.1183/13993003.01984-2017. [DOI] [PubMed] [Google Scholar]
- 333.Glockler-Lauf SD, Finkelstein Y, Zhu J, Feldman LY, To T. Montelukast and neuropsychiatric events in children with asthma: A nested case-control study. J Pediatr. 2019;209:176–82.e4. doi: 10.1016/j.jpeds.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 334.Bonner S, Matte T, Rubin M, Fagan JK, Ahern J, Evans D. Oral beta2-agonist use by preschool children with asthma in East and Central Harlem, New York. J Asthma. 2006;43:31–5. doi: 10.1080/02770900500446989. [DOI] [PubMed] [Google Scholar]
- 335.Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF, Jr, Sorkness CA, et al. Long-acting beta2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA. 2001;285:2583–93. doi: 10.1001/jama.285.20.2583. [DOI] [PubMed] [Google Scholar]
- 336.Deerojanawong J, Manuyakorn W, Prapphal N, Harnruthakorn C, Sritippayawan S, Samransamruajkit R. Randomized controlled trial of salbutamol aerosol therapy via metered dose inhaler-spacer vs. jet nebulizer in young children with wheezing. Pediatr Pulmonol. 2005;39:466–72. doi: 10.1002/ppul.20204. [DOI] [PubMed] [Google Scholar]
- 337.Drblik S, Lapierre G, Thivierge R, Turgeon J, Gaudreault P, Cummins-McManus B, et al. Comparative efficacy of terbutaline sulphate delivered by Turbuhaler dry powder inhaler or pressurised metered dose inhaler with Nebuhaler spacer in children during an acute asthmatic episode. Arch Dis Child. 2003;88:319–23. doi: 10.1136/adc.88.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Vincken W, Levy ML, Scullion J, Usmani OS, Dekhuijzen PN, Corrigan CJ. Spacer devices for inhaled therapy: Why use them, and how. ERJ Open Res. 2018;4:1–10. doi: 10.1183/23120541.00065-2018. (00065-2018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Castro-Rodriguez JA, Rodrigo GJ. Beta-agonists through metered-dose inhaler with valved holding chamber versus nebulizer for acute exacerbation of wheezing or asthma in children under 5 years of age: A systematic review with meta-analysis. J Pediatr. 2004;145:172–7. doi: 10.1016/j.jpeds.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 340.Welsh EJ, Hasan M, Li P. Home-based educational interventions for children with asthma. Cochrane Database Syst Rev. 2011:CD008469. doi: 10.1002/14651858.CD008469.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Wolf FM, Guevara JP, Grum CM, Clark NM, Cates CJ. Educational interventions for asthma in children. Cochrane Database Syst Rev. 2003:CD000326. doi: 10.1002/14651858.CD000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Wood MR, Bolyard D. Making education count: The nurse's role in asthma education using a medical home model of care. J Pediatr Nurs. 2011;26:552–8. doi: 10.1016/j.pedn.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 343.Becker A, Lemière C, Bérubé D, Boulet LP, Ducharme FM, FitzGerald M, et al. Summary of recommendations from the Canadian Asthma Consensus guidelines, 2003. CMAJ. 2005;173:S3–11. [PMC free article] [PubMed] [Google Scholar]
- 344.Nurmatov U, Devereux G, Sheikh A. Nutrients and foods for the primary prevention of asthma and allergy: Systematic review and meta-analysis. J Allergy Clin Immunol. 2011;127:724. doi: 10.1016/j.jaci.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 345.Pelucchi C, Chatenoud L, Turati F, Galeone C, Moja L, Bach JF, et al. Probiotics supplementation during pregnancy or infancy for the prevention of atopic dermatitis: A meta-analysis. Epidemiology. 2012;23:402–14. doi: 10.1097/EDE.0b013e31824d5da2. [DOI] [PubMed] [Google Scholar]
- 346.Kozyrskyj AL, Pawlowski AN. Maternal distress and childhood wheeze: Mechanisms and context. Am J Respir Crit Care Med. 2013;187:1160–2. doi: 10.1164/rccm.201304-0649ED. [DOI] [PubMed] [Google Scholar]
- 347.Cabana MD, McKean M, Caughey AB, Fong L, Lynch S, Wong A, et al. Early probiotic supplementation for eczema and asthma prevention: A randomized controlled trial. Pediatrics. 2017;140:e20163000. doi: 10.1542/peds.2016-3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Kneale D, Harris K, McDonald VM, Thomas J, Grigg J. Effectiveness of school-based self-management interventions for asthma among children and adolescents: Findings from a Cochrane systematic review and meta-analysis. Thorax. 2019;74:432–8. doi: 10.1136/thoraxjnl-2018-211909. [DOI] [PubMed] [Google Scholar]
- 349.Asthma SIf. Advisory from the Saudi Initiative for Asthma during COVID-19. 2020 [Google Scholar]
- 350.Al-Shamrani A, Al-Harbi AS, Alhaider SA, Alharbi S, Al-Harbi NS, Alanazi A, et al. Approach to childhood asthma in the era of COVID-19: The official statement endorsed by the Saudi Pediatric Pulmonology Association (SPPA) Int J Pediatr Adolesc Med. 2020;7:103–6. doi: 10.1016/j.ijpam.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Ducharme FM, Lemire C, Noya FJ, Davis GM, Alos N, Leblond H, et al. Preemptive use of high-dose fluticasone for virus-induced wheezing in young children. N Engl J Med. 2009;360:339–53. doi: 10.1056/NEJMoa0808907. [DOI] [PubMed] [Google Scholar]
- 352.Bisgaard H, Hermansen MN, Loland L, Halkjaer LB, Buchvald F. Intermittent inhaled corticosteroids in infants with episodic wheezing. N Engl J Med. 2006;354:1998–2005. doi: 10.1056/NEJMoa054692. [DOI] [PubMed] [Google Scholar]
- 353.Papi A, Nicolini G, Baraldi E, Boner AL, Cutrera R, Rossi GA, et al. Regular vs prn nebulized treatment in wheeze preschool children. Allergy. 2009;64:1463–71. doi: 10.1111/j.1398-9995.2009.02134.x. [DOI] [PubMed] [Google Scholar]
- 354.Fitzpatrick AM, Jackson DJ, Mauger DT, Boehmer SJ, Phipatanakul W, Sheehan WJ, et al. Individualized therapy for persistent asthma in young children. J Allergy Clin Immunol. 2016;138:1608–18.e12. doi: 10.1016/j.jaci.2016.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Guilbert TW, Morgan WJ, Zeiger RS, Mauger DT, Boehmer SJ, Szefler SJ, et al. Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med. 2006;354:1985–97. doi: 10.1056/NEJMoa051378. [DOI] [PubMed] [Google Scholar]
- 356.Nielsen KG, Bisgaard H. The effect of inhaled budesonide on symptoms, lung function, and cold air and methacholine responsiveness in 2- to 5-year-old asthmatic children. Am J Respir Crit Care Med. 2000;162:1500–6. doi: 10.1164/ajrccm.162.4.2002019. [DOI] [PubMed] [Google Scholar]
- 357.Szefler SJ, Baker JW, Uryniak T, Goldman M, Silkoff PE. Comparative study of budesonide inhalation suspension and montelukast in young children with mild persistent asthma. J Allergy Clin Immunol. 2007;120:1043–50. doi: 10.1016/j.jaci.2007.08.063. [DOI] [PubMed] [Google Scholar]
- 358.Knorr B, Franchi LM, Bisgaard H, Vermeulen JH, LeSouef P, Santanello N, et al. Montelukast, a leukotriene receptor antagonist, for the treatment of persistent asthma in children aged 2 to 5 years. Pediatrics. 2001;108:E48. doi: 10.1542/peds.108.3.e48. [DOI] [PubMed] [Google Scholar]
- 359.Bisgaard H. Leukotriene modifiers in pediatric asthma management. Pediatrics. 2001;107:381–90. doi: 10.1542/peds.107.2.381. [DOI] [PubMed] [Google Scholar]
- 360.Ducharme FM, Hicks GC. Anti-leukotriene agents compared to inhaled corticosteroids in the management of recurrent and/or chronic asthma in adults and children. Cochrane Database Syst Rev. 2002:CD002314. doi: 10.1002/14651858.CD002314. [DOI] [PubMed] [Google Scholar]
- 361.O'Byrne P, Fabbri LM, Pavord ID, Papi A, Petruzzelli S, Lange P. Asthma progression and mortality: The role of inhaled corticosteroids. Eur Respir J. 2019;54:1900491. doi: 10.1183/13993003.00491-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Chauhan BF, Ducharme FM. Addition to inhaled corticosteroids of long-acting beta2-agonists versus anti-leukotrienes for chronic asthma. Cochrane Database Syst Rev. 2014:CD003137. doi: 10.1002/14651858.CD003137.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Chong JK, Chauhan BF. Addition of antileukotriene agents to inhaled corticosteroids in children with persistent asthma. Paediatr Child Health. 2014;19:473–4. doi: 10.1093/pch/19.9.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Halwani R, Vazquez-Tello A, Horanieh N, Dulgom S, Al-Aseri Z, Al-Khamis N, et al. Risk factors hindering asthma symptom control in Saudi children and adolescents. Pediatr Int. 2017;59:661–8. doi: 10.1111/ped.13268. [DOI] [PubMed] [Google Scholar]
- 365.Shrewsbury S, Pyke S, Britton M. Meta-analysis of increased dose of inhaled steroid or addition of salmeterol in symptomatic asthma (MIASMA) BMJ. 2000;320:1368–73. doi: 10.1136/bmj.320.7246.1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Matz J, Emmett A, Rickard K, Kalberg C. Addition of salmeterol to low-dose fluticasone versus higher-dose fluticasone: An analysis of asthma exacerbations. J Allergy Clin Immunol. 2001;107:783–9. doi: 10.1067/mai.2001.114709. [DOI] [PubMed] [Google Scholar]
- 367.Vaessen-Verberne AA, van den Berg NJ, van Nierop JC, Brackel HJ, Gerrits GP, Hop WC, et al. Combination therapy salmeterol/fluticasone versus doubling dose of fluticasone in children with asthma. Am J Respir Crit Care Med. 2010;182:1221–7. doi: 10.1164/rccm.201002-0193OC. [DOI] [PubMed] [Google Scholar]
- 368.Verberne AA, Frost C, Duiverman EJ, Grol MH, Kerrebijn KF. Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. The Dutch Asthma Study Group. Am J Respir Crit Care Med. 1998;158:213–9. doi: 10.1164/ajrccm.158.1.9706048. [DOI] [PubMed] [Google Scholar]
- 369.Ducharme FM, Ni Chroinin M, Greenstone I, Lasserson TJ. Addition of long-acting beta2-agonists to inhaled corticosteroids versus same dose inhaled corticosteroids for chronic asthma in adults and children. Cochrane Database Syst Rev. 2010:CD005535. doi: 10.1002/14651858.CD005535.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Ducharme FM, Ni Chroinin M, Greenstone I, Lasserson TJ. Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma. Cochrane Database Syst Rev. 2010:CD005533. doi: 10.1002/14651858.CD005533.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Deschildre A, Marguet C, Langlois C, Pin I, Rittié JL, Derelle J, et al. Real-life long-term omalizumab therapy in children with severe allergic asthma. Eur Respir J. 2015;46:856–9. doi: 10.1183/09031936.00008115. [DOI] [PubMed] [Google Scholar]
- 372.Licari A, Marseglia A, Caimmi S, Castagnoli R, Foiadelli T, Barberi S, et al. Omalizumab in children. Paediatr Drugs. 2014;16:491–502. doi: 10.1007/s40272-014-0107-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Kulus M, Hébert J, Garcia E, Fowler Taylor A, Fernandez Vidaurre C, Blogg M. Omalizumab in children with inadequately controlled severe allergic (IgE-mediated) asthma. Curr Med Res Opin. 2010;26:1285–93. doi: 10.1185/03007991003771338. [DOI] [PubMed] [Google Scholar]
- 374.Lanier B, Bridges T, Kulus M, Taylor AF, Berhane I, Vidaurre CF. Omalizumab for the treatment of exacerbations in children with inadequately controlled allergic (IgE-mediated) asthma. J Allergy Clin Immunol. 2009;124:1210–6. doi: 10.1016/j.jaci.2009.09.021. [DOI] [PubMed] [Google Scholar]
- 375.Gupta A, Pouliquen I, Austin D, Price RG, Kempsford R, Steinfeld J, et al. Subcutaneous mepolizumab in children aged 6 to 11 years with severe eosinophilic asthma. Pediatr Pulmonol. 2019;54:1957–67. doi: 10.1002/ppul.24508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Gupta A, Ikeda M, Geng B, Azmi J, Price RG, Bradford ES, et al. Long-term safety and pharmacodynamics of mepolizumab in children with severe asthma with an eosinophilic phenotype. J Allergy Clin Immunol. 2019;144:1336–42.e7. doi: 10.1016/j.jaci.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 377.Ni Chroinin M, Greenstone I, Lasserson TJ, Ducharme FM. Addition of inhaled long-acting beta2-agonists to inhaled steroids as first line therapy for persistent asthma in steroid-naive adults and children. Cochrane Database Syst Rev. 2009:CD005307. doi: 10.1002/14651858.CD005307.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Ni Chroinin M, Lasserson TJ, Greenstone I, Ducharme FM. Addition of long-acting beta-agonists to inhaled corticosteroids for chronic asthma in children. Cochrane Database Syst Rev. 2009:CD007949. doi: 10.1002/14651858.CD007949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Ducharme FM. Anti-leukotrienes as add-on therapy to inhaled glucocorticoids in patients with asthma: Systematic review of current evidence. BMJ. 2002;324:1545. doi: 10.1136/bmj.324.7353.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Phipatanakul W, Cronin B, Wood RA, Eggleston PA, Shih MC, Song L, et al. Effect of environmental intervention on mouse allergen levels in homes of inner-city Boston children with asthma. Ann Allergy Asthma Immunol. 2004;92:420–5. doi: 10.1016/S1081-1206(10)61777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Simons FE, Villa JR, Lee BW, Teper AM, Lyttle B, Aristizabal G, et al. Montelukast added to budesonide in children with persistent asthma: A randomized, double-blind, crossover study. J Pediatr. 2001;138:694–8. doi: 10.1067/mpd.2001.112899. [DOI] [PubMed] [Google Scholar]
- 382.Goksör E, Amark M, Alm B, Gustafsson PM, Wennergren G. Asthma symptoms in early childhood--What happens then? Acta Paediatr. 2006;95:471–8. doi: 10.1080/08035250500499440. [DOI] [PubMed] [Google Scholar]
- 383.Swern AS, Tozzi CA, Knorr B, Bisgaard H. Predicting an asthma exacerbation in children 2 to 5 years of age. Ann Allergy Asthma Immunol. 2008;101:626–30. doi: 10.1016/S1081-1206(10)60226-8. [DOI] [PubMed] [Google Scholar]
- 384.Ducharme FM, Chalut D, Plotnick L, Savdie C, Kudirka D, Zhang X, et al. The pediatric respiratory assessment measure: A valid clinical score for assessing acute asthma severity from toddlers to teenagers. J Pediatr. 2008;152:476–80. 480.e1. doi: 10.1016/j.jpeds.2007.08.034. [DOI] [PubMed] [Google Scholar]
- 385.Parkin PC, Macarthur C, Saunders NR, Diamond SA, Winders PM. Development of a clinical asthma score for use in hospitalized children between 1 and 5 years of age. J Clin Epidemiol. 1996;49:821–5. doi: 10.1016/0895-4356(96)00027-3. [DOI] [PubMed] [Google Scholar]
- 386.Chalut DS, Ducharme FM, Davis GM. The Preschool Respiratory Assessment Measure (PRAM): A responsive index of acute asthma severity. J Pediatr. 2000;137:762–8. doi: 10.1067/mpd.2000.110121. [DOI] [PubMed] [Google Scholar]
- 387.Al-Muhsen S, Horanieh N, Dulgom S, Aseri ZA, Vazquez-Tello A, Halwani R, et al. Poor asthma education and medication compliance are associated with increased emergency department visits by asthmatic children. Ann Thorac Med. 2015;10:123–31. doi: 10.4103/1817-1737.150735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Birken CS, Parkin PC, Macarthur C. Asthma severity scores for preschoolers displayed weaknesses in reliability, validity, and responsiveness. J Clin Epidemiol. 2004;57:1177–81. doi: 10.1016/j.jclinepi.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 389.Alnaji F, Zemek R, Barrowman N, Plint A. PRAM score as predictor of pediatric asthma hospitalization. Acad Emerg Med. 2014;21:872–8. doi: 10.1111/acem.12422. [DOI] [PubMed] [Google Scholar]
- 390.Jarvis SW, Kovacs C, Badriyah T, Briggs J, Mohammed MA, Meredith P, et al. Development and validation of a decision tree early warning score based on routine laboratory test results for the discrimination of hospital mortality in emergency medical admissions. Resuscitation. 2013;84:1494–9. doi: 10.1016/j.resuscitation.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 391.Johnson KB, Blaisdell CJ, Walker A, Eggleston P. Effectiveness of a clinical pathway for inpatient asthma management. Pediatrics. 2000;106:1006–12. [PubMed] [Google Scholar]
- 392.Banasiak NC. Childhood asthma practice guideline part three: Update of the 2007 National Guidelines for the Diagnosis and Treatment of Asthma. The National Asthma Education and Prevention Program. J Pediatr Health Care. 2009;23:59–61. doi: 10.1016/j.pedhc.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 393.Ortiz-Alvarez O, Mikrogianakis A. Canadian Paediatric Society, Acute Care Committee. Managing the paediatric patient with an acute asthma exacerbation. Paediatr Child Health. 2012;17:251–62. doi: 10.1093/pch/17.5.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Norton SP, Pusic MV, Taha F, Heathcote S, Carleton BC. Effect of a clinical pathway on the hospitalisation rates of children with asthma: A prospective study. Arch Dis Child. 2007;92:60–6. doi: 10.1136/adc.2006.097287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Lougheed MD, Olajos-Clow JG. Asthma care pathways in the emergency department. Curr Opin Allergy Clin Immunol. 2010;10:181–7. doi: 10.1097/ACI.0b013e328339731d. [DOI] [PubMed] [Google Scholar]
- 396.Browne GJ, Giles H, McCaskill ME, Fasher BJ, Lam LT. The benefits of using clinical pathways for managing acute paediatric illness in an emergency department. J Qual Clin Pract. 2001;21:50–5. doi: 10.1046/j.1440-1762.2001.00405.x. [DOI] [PubMed] [Google Scholar]
- 397.Graham VA, Milton AF, Knowles GK, Davies RJ. Routine antibiotics in hospital management of acute asthma. Lancet. 1982;1:418–20. doi: 10.1016/s0140-6736(82)91619-1. [DOI] [PubMed] [Google Scholar]
- 398.Everard ML, Bara A, Kurian M, Elliott TM, Ducharme F, Mayowe V. Anticholinergic drugs for wheeze in children under the age of two years. Cochrane Database Syst Rev. 2005:CD001279. doi: 10.1002/14651858.CD001279.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Griffiths B, Ducharme FM. Combined inhaled anticholinergics and short-acting beta2-agonists for initial treatment of acute asthma in children. Cochrane Database Syst Rev. 2013:CD000060. doi: 10.1002/14651858.CD000060.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Rowe BH, Spooner CH, Ducharme FM, Bretzlaff JA, Bota GW. Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst Rev. 2001:CD000195. doi: 10.1002/14651858.CD000195. [DOI] [PubMed] [Google Scholar]
- 401.Griffiths B, Ducharme FM. Combined inhaled anticholinergics and short-acting beta2-agonists for initial treatment of acute asthma in children. Paediatr Respir Rev. 2013;14:234–5. doi: 10.1016/j.prrv.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 402.Rowe BH, Spooner C, Ducharme FM, Bretzlaff JA, Bota GW. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. 2001:CD002178. doi: 10.1002/14651858.CD002178. [DOI] [PubMed] [Google Scholar]
- 403.Cheuk DK, Chau TC, Lee SL. A meta-analysis on intravenous magnesium sulphate for treating acute asthma. Arch Dis Child. 2005;90:74–7. doi: 10.1136/adc.2004.050005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Powell CV, Kolamunnage-Dona R, Lowe J, Boland A, Petrou S, Doull I, et al. MAGNEsium Trial In Children (MAGNETIC): A randomised, placebo-controlled trial and economic evaluation of nebulised magnesium sulphate in acute severe asthma in children. Health Technol Assess. 2013;17:v. doi: 10.3310/hta17450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Powell C, Kolamunnage-Dona R, Lowe J, Boland A, Petrou S, Doull I, et al. Magnesium sulphate in acute severe asthma in children (MAGNETIC): A randomised, placebo-controlled trial. Lancet Respir Med. 2013;1:301–8. doi: 10.1016/S2213-2600(13)70037-7. [DOI] [PubMed] [Google Scholar]
- 406.Camargo CA, Jr, Spooner CH, Rowe BH. Continuous versus intermittent beta-agonists in the treatment of acute asthma. Cochrane Database Syst Rev. 2003:CD001115. doi: 10.1002/14651858.CD001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Scarfone RJ, Fuchs SM, Nager AL, Shane SA. Controlled trial of oral prednisone in the emergency department treatment of children with acute asthma. Pediatrics. 1993;92:513–8. [PubMed] [Google Scholar]
- 408.Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75:1730–41. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 409.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Creticos PS. Treatment options for initial maintenance therapy of persistent asthma: A review of inhaled corticosteroids and leukotriene receptor antagonists. Drugs. 2003;63(Suppl 2):1–20. doi: 10.2165/00003495-200363002-00002. [DOI] [PubMed] [Google Scholar]
- 411.Lemanske RF, Jr, Sorkness CA, Mauger EA, Lazarus SC, Boushey HA, Fahy JV, et al. Inhaled corticosteroid reduction and elimination in patients with persistent asthma receiving salmeterol: A randomized controlled trial. JAMA. 2001;285:2594–603. doi: 10.1001/jama.285.20.2594. [DOI] [PubMed] [Google Scholar]
- 412.Masoli M, Weatherall M, Holt S, Beasley R. Moderate dose inhaled corticosteroids plus salmeterol versus higher doses of inhaled corticosteroids in symptomatic asthma. Thorax. 2005;60:730–4. doi: 10.1136/thx.2004.039180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Fouda MA, Al-Kassimi FA. Budesonide and fluticasone and adrenal suppression. Ann Thorac Med. 2012;7:253. doi: 10.4103/1817-1737.102188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Leach C, Colice GL, Luskin A. Particle size of inhaled corticosteroids: Does it matter? J Allergy Clin Immunol. 2009;124:S88–93. doi: 10.1016/j.jaci.2009.09.050. [DOI] [PubMed] [Google Scholar]
- 415.Menzies D, Nair A, Hopkinson P, McFarlane L, Lipworth BJ. Differential anti-inflammatory effects of large and small particle size inhaled corticosteroids in asthma. Allergy. 2007;62:661–7. doi: 10.1111/j.1398-9995.2007.01376.x. [DOI] [PubMed] [Google Scholar]
- 416.Kramer S, Rottier BL, Scholten RJ, Boluyt N. Ciclesonide versus other inhaled corticosteroids for chronic asthma in children. Cochrane Database Syst Rev. 2013:CD010352. doi: 10.1002/14651858.CD010352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Pruteanu AI, Chauhan BF, Zhang L, Prietsch SO, Ducharme FM. Inhaled corticosteroids in children with persistent asthma: Dose-response effects on growth. Cochrane Database Syst Rev. 2014:CD009878. doi: 10.1002/14651858.CD009878.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Raissy HH, Blake K. Does use of inhaled corticosteroid for management of asthma in children make them shorter adults? Pediatr Allergy Immunol Pulmonol. 2013;26:99–101. doi: 10.1089/ped.2013.0244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Hossny E, Rosario N, Lee BW, Singh M, El-Ghoneimy D, Soh JY, et al. The use of inhaled corticosteroids in pediatric asthma: Update. World Allergy Organ J. 2016;9:26. doi: 10.1186/s40413-016-0117-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Hoover RM, Erramouspe J, Bell EA, Cleveland KW. Effect of inhaled corticosteroids on long-term growth in pediatric patients with asthma and allergic rhinitis. Ann Pharmacother. 2013;47:1175–81. doi: 10.1177/1060028013503125. [DOI] [PubMed] [Google Scholar]
- 421.Kelly HW, Van Natta ML, Covar RA, Tonascia J, Green RP, Strunk RC, et al. Effect of long-term corticosteroid use on bone mineral density in children: A prospective longitudinal assessment in the childhood Asthma Management Program (CAMP) study. Pediatrics. 2008;122:e53–61. doi: 10.1542/peds.2007-3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Sidoroff VH, Ylinen MK, Kröger LM, Kröger HP, Korppi MO. Inhaled corticosteroids and bone mineral density at school age: A follow-up study after early childhood wheezing. Pediatr Pulmonol. 2015;50:1–7. doi: 10.1002/ppul.22968. [DOI] [PubMed] [Google Scholar]
- 423.Stelmach I, Olszowiec-Chlebna M, Jerzynska J, Grzelewski T, Stelmach W, Majak P. Inhaled corticosteroids may have a beneficial effect on bone metabolism in newly diagnosed asthmatic children. Pulm Pharmacol Ther. 2011;24:414–20. doi: 10.1016/j.pupt.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 424.Altintas DU, Karakoc GB, Can S, Yilmaz M, Kendirli SG. The effects of long term use of inhaled corticosteroids on linear growth, adrenal function and bone mineral density in children. Allergol Immunopathol (Madr) 2005;33:204–9. doi: 10.1157/13077744. [DOI] [PubMed] [Google Scholar]
- 425.Bjermer L, Diamant Z. The use of leukotriene receptor antagonists (LTRAs) as complementary therapy in asthma. Monaldi Arch Chest Dis. 2002;57:76–83. [PubMed] [Google Scholar]
- 426.Idrees MM, Al Moamary MS. Blocking leukotrienes optimize asthma control: The BLOC survey. Ann Thorac Med. 2007;2:99–102. doi: 10.4103/1817-1737.33696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Bisgaard H. Study Group on Montelukast and Respiratory Syncytial Virus. A randomized trial of montelukast in respiratory syncytial virus postbronchiolitis. Am J Respir Crit Care Med. 2003;167:379–83. doi: 10.1164/rccm.200207-747OC. [DOI] [PubMed] [Google Scholar]
- 428.Straub DA, Minocchieri S, Moeller A, Hamacher J, Wildhaber JH. The effect of montelukast on exhaled nitric oxide and lung function in asthmatic children 2 to 5 years old. Chest. 2005;127:509–14. doi: 10.1378/chest.127.2.509. [DOI] [PubMed] [Google Scholar]
- 429.Straub DA, Moeller A, Minocchieri S, Hamacher J, Sennhauser FH, Hall GL, et al. The effect of montelukast on lung function and exhaled nitric oxide in infants with early childhood asthma. Eur Respir J. 2005;25:289–94. doi: 10.1183/09031936.05.00031904. [DOI] [PubMed] [Google Scholar]
- 430.Bisgaard H, Zielen S, Garcia-Garcia ML, Johnston SL, Gilles L, Menten J, et al. Montelukast reduces asthma exacerbations in 2- to 5-year-old children with intermittent asthma. Am J Respir Crit Care Med. 2005;171:315–22. doi: 10.1164/rccm.200407-894OC. [DOI] [PubMed] [Google Scholar]
- 431.Lötvall J, Bateman ED, Bleecker ER, Busse WW, Woodcock A, Follows R, et al. 24-h duration of the novel LABA vilanterol trifenatate in asthma patients treated with inhaled corticosteroids. Eur Respir J. 2012;40:570–9. doi: 10.1183/09031936.00121411. [DOI] [PubMed] [Google Scholar]
- 432.Casarosa P, Kollak I, Kiechle T, Ostermann A, Schnapp A, Kiesling R, et al. Functional and biochemical rationales for the 24-hour-long duration of action of olodaterol. J Pharmacol Exp Ther. 2011;337:600–9. doi: 10.1124/jpet.111.179259. [DOI] [PubMed] [Google Scholar]
- 433.Pearlman DS, Greos L, LaForce C, Orevillo CJ, Owen R, Higgins M. Bronchodilator efficacy of indacaterol, a novel once-daily beta2-agonist, in patients with persistent asthma. Ann Allergy Asthma Immunol. 2008;101:90–5. doi: 10.1016/S1081-1206(10)60840-X. [DOI] [PubMed] [Google Scholar]
- 434.Sugihara N, Kanada S, Haida M, Ichinose M, Adachi M, Hosoe M, et al. 24-h bronchodilator efficacy of single doses of indacaterol in Japanese patients with asthma: A comparison with placebo and salmeterol. Respir Med. 2010;104:1629–37. doi: 10.1016/j.rmed.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 435.Cazzola M, Segreti A, Matera MG. Novel bronchodilators in asthma. Curr Opin Pulm Med. 2010;16:6–12. doi: 10.1097/MCP.0b013e32833303d2. [DOI] [PubMed] [Google Scholar]
- 436.Cazzola M, Matera MG. Novel long-acting bronchodilators for COPD and asthma. Br J Pharmacol. 2008;155:291–9. doi: 10.1038/bjp.2008.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.LaForce C, Korenblat P, Osborne P, Dong F, Higgins M. 24-hour bronchodilator efficacy of single doses of indacaterol in patients with persistent asthma: Comparison with placebo and formoterol. Curr Med Res Opin. 2009;25:2353–9. doi: 10.1185/03007990903143143. [DOI] [PubMed] [Google Scholar]
- 438.Cates CJ, Cates MJ. Regular treatment with formoterol for chronic asthma: Serious adverse events. Cochrane Database Syst Rev. 2012:CD006923. doi: 10.1002/14651858.CD006923.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Puggioni F, Heffler EM, Canonica GW, Latorre M, Blasi F, Paggiaro P, et al. Long-acting anti-muscarinic agents (LAMA) frequency of use and clinical features of patients with severe asthma in real-life setting: Data from the Severe Asthma Network in Italy (SANI) registry. Eur Respiratory Soc. 2019;54:suppl 63. [Google Scholar]
- 440.Matera MG, Belardo C, Rinaldi M, Rinaldi B, Cazzola M. Emerging muscarinic receptor antagonists for the treatment of asthma. Expert Opin Emerg Drugs. 2020;25:123–30. doi: 10.1080/14728214.2020.1758059. [DOI] [PubMed] [Google Scholar]
- 441.van Noord JA, Bantje TA, Eland ME, Korducki L, Cornelissen PJ. A randomised controlled comparison of tiotropium nd ipratropium in the treatment of chronic obstructive pulmonary disease. The Dutch Tiotropium Study Group. Thorax. 2000;55:289–94. doi: 10.1136/thorax.55.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Maesen FP, Smeets JJ, Sledsens TJ, Wald FD, Cornelissen PJ. Tiotropium bromide, a new long-acting antimuscarinic bronchodilator: A pharmacodynamic study in patients with chronic obstructive pulmonary disease (COPD). Dutch Study Group. Eur Respir J. 1995;8:1506–13. [PubMed] [Google Scholar]
- 443.Fardon T, Haggart K, Lee DK, Lipworth BJ. A proof of concept study to evaluate stepping down the dose of fluticasone in combination with salmeterol and tiotropium in severe persistent asthma. Respir Med. 2007;101:1218–28. doi: 10.1016/j.rmed.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 444.Rodrigo GJ, Castro-Rodríguez JA. What is the role of tiotropium in asthma.: A systematic review with meta-analysis? Chest. 2015;147:388–96. doi: 10.1378/chest.14-1698. [DOI] [PubMed] [Google Scholar]
- 445.GSK. FDA approves Trelegy Ellipta as the First Once-Daily Single Inhaler Triple Therapy for the Treatment of Both Asthma and COPD in the US. 2020. [Last accessed on 2020 Nov 21]. Available from: https://us.gsk.com/en-us/media/press-releases/fda-approves-trelegy-ellipta-as-the-first-once-daily-single-inhaler-triple-therapy-for-the-treatment-of-both-asthma-and-copd-in-the-us/
- 446.Elias JA, Lee CG, Zheng T, Ma B, Homer RJ, Zhu Z. New insights into the pathogenesis of asthma. J Clin Invest. 2003;111:291–7. doi: 10.1172/JCI17748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Hamid Q, Tulic MK. New insights into the pathophysiology of the small airways in asthma. Ann Thorac Med. 2007;2:28–33. doi: 10.4103/1817-1737.30361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.Sridhar AV, McKean M. Nedocromil sodium for chronic asthma in children. Cochrane Database Syst Rev. 2006:CD004108. doi: 10.1002/14651858.CD004108.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.O'Byrne PM, FitzGerald JM, Zhong N, Bateman E, Barnes PJ, Keen C, et al. The SYGMA programme of phase 3 trials to evaluate the efficacy and safety of budesonide/formoterol given 'as needed' in mild asthma: Study protocols for two randomised controlled trials. Trials. 2017;18:12. doi: 10.1186/s13063-016-1731-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450.Huchon G, Magnussen H, Chuchalin A, Dymek L, Gonod FB, Bousquet J. Lung function and asthma control with beclomethasone and formoterol in a single inhaler. Respir Med. 2009;103:41–9. doi: 10.1016/j.rmed.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 451.Nolte H, Pavord I, Backer V, Spector S, Shekar T, Gates D, et al. Dose-dependent anti-inflammatory effect of inhaled mometasone furoate/formoterol in subjects with asthma. Respir Med. 2013;107:656–64. doi: 10.1016/j.rmed.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 452.Grekas N, Athanassiou K, Papataxiarchou K, Rizea Savu S, Silvestro L. Pharmacokinetic study for the establishment of bioequivalence of two inhalation treatments containing budesonide plus formoterol. J Pharm Pharmacol. 2014;66:1677–85. doi: 10.1111/jphp.12303. [DOI] [PubMed] [Google Scholar]
- 453.Bodzenta-Lukaszyk A, Pulka G, Dymek A, Bumbacea D, McIver T, Schwab B, et al. Efficacy and safety of fluticasone and formoterol in a single pressurized metered dose inhaler. Respir Med. 2011;105:674–82. doi: 10.1016/j.rmed.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 454.Bateman ED, O'Byrne PM, Busse WW, Lötvall J, Bleecker ER, Andersen L, et al. Once-daily fluticasone furoate (FF)/vilanterol reduces risk of severe exacerbations in asthma versus FF alone. Thorax. 2014;69:312–9. doi: 10.1136/thoraxjnl-2013-203600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Busse WW, O'Byrne PM, Bleecker ER, Lötvall J, Woodcock A, Andersen L, et al. Safety and tolerability of the novel inhaled corticosteroid fluticasone furoate in combination with the β2 agonist vilanterol administered once daily for 52 weeks in patients >=12 years old with asthma: A randomised trial. Thorax. 2013;68:513–20. doi: 10.1136/thoraxjnl-2012-202606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Jabbal S, Kuo CR, Lipworth B. Randomized controlled trial of triple versus dual inhaler therapy on small airways in smoking asthmatics. Clin Exp Allergy. 2020;50:1140–7. doi: 10.1111/cea.13702. [DOI] [PubMed] [Google Scholar]
- 457.Cates CJ, Crilly JA, Rowe BH. Holding chambers (spacers) versus nebulisers for beta-agonist treatment of acute asthma. Cochrane Database Syst Rev. 2006:CD000052. doi: 10.1002/14651858.CD000052.pub2. [DOI] [PubMed] [Google Scholar]
- 458.McFadden ER., Jr Critical appraisal of the therapy of asthma--an idea whose time has come. Am Rev Respir Dis. 1986;133:723–4. doi: 10.1164/arrd.1986.133.5.723. [DOI] [PubMed] [Google Scholar]
- 459.Rossing TH, Fanta CH, Goldstein DH, Snapper JR, McFadden ER., Jr Emergency therapy of asthma: Comparison of the acute effects of parenteral and inhaled sympathomimetics and infused aminophylline. Am Rev Respir Dis. 1980;122:365–71. doi: 10.1164/arrd.1980.122.3.365. [DOI] [PubMed] [Google Scholar]
- 460.Rodrigo GJ, Rodrigo C. Continuous vs intermittent beta-agonists in the treatment of acute adult asthma: A systematic review with meta-analysis. Chest. 2002;122:160–5. doi: 10.1378/chest.122.1.160. [DOI] [PubMed] [Google Scholar]
- 461.Travers AH, Rowe BH, Barker S, Jones A, Camargo CA., Jr The effectiveness of IV beta-agonists in treating patients with acute asthma in the emergency department: A meta-analysis. Chest. 2002;122:1200–7. doi: 10.1378/chest.122.4.1200. [DOI] [PubMed] [Google Scholar]
- 462.Lanes SF, Garrett JE, Wentworth CE, 3rd, Fitzgerald JM, Karpel JP. The effect of adding ipratropium bromide to salbutamol in the treatment of acute asthma: A pooled analysis of three trials. Chest. 1998;114:365–72. doi: 10.1378/chest.114.2.365. [DOI] [PubMed] [Google Scholar]
- 463.Stoodley RG, Aaron SD, Dales RE. The role of ipratropium bromide in the emergency management of acute asthma exacerbation: A metaanalysis of randomized clinical trials. Ann Emerg Med. 1999;34:8–18. doi: 10.1016/s0196-0644(99)70266-0. [DOI] [PubMed] [Google Scholar]
- 464.Rodrigo G, Rodrigo C, Burschtin O. A meta-analysis of the effects of ipratropium bromide in adults with acute asthma. Am J Med. 1999;107:363–70. doi: 10.1016/s0002-9343(99)00243-0. [DOI] [PubMed] [Google Scholar]
- 465.Rodrigo GJ, Rodrigo C. First-line therapy for adult patients with acute asthma receiving a multiple-dose protocol of ipratropium bromide plus albuterol in the emergency department. Am J Respir Crit Care Med. 2000;161:1862–8. doi: 10.1164/ajrccm.161.6.9908115. [DOI] [PubMed] [Google Scholar]
- 466.Rodrigo GJ, Rodrigo C. The role of anticholinergics in acute asthma treatment: An evidence-based evaluation. Chest. 2002;121:1977–87. doi: 10.1378/chest.121.6.1977. [DOI] [PubMed] [Google Scholar]
- 467.Vézina K, Chauhan BF, Ducharme FM. Inhaled anticholinergics and short-acting beta(2)-agonists versus short-acting beta2-agonists alone for children with acute asthma in hospital. Cochrane Database Syst Rev. 2014:CD010283. doi: 10.1002/14651858.CD010283.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.Parameswaran K, Belda J, Rowe BH. Addition of intravenous aminophylline to beta2-agonists in adults with acute asthma. Cochrane Database Syst Rev. 2000:CD002742. doi: 10.1002/14651858.CD002742. [DOI] [PubMed] [Google Scholar]
- 469.Silverman RA, Osborn H, Runge J, Gallagher EJ, Chiang W, Feldman J, et al. IV magnesium sulfate in the treatment of acute severe asthma: A multicenter randomized controlled trial. Chest. 2002;122:489–97. doi: 10.1378/chest.122.2.489. [DOI] [PubMed] [Google Scholar]
- 470.Rowe BH, Bretzlaff JA, Bourdon C, Bota GW, Camargo CA., Jr Magnesium sulfate for treating exacerbations of acute asthma in the emergency department. Cochrane Database Syst Rev. 2000:CD001490. doi: 10.1002/14651858.CD001490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.Nair A, Menzies D, Barnes M, Burns P, McFarlane L, Lipworth BJ. Respirable dose delivery of fluticasone propionate from a small valved holding chamber, a compact breath actuated integrated vortex device and a metered dose inhaler. Br J Clin Pharmacol. 2008;66:20–6. doi: 10.1111/j.1365-2125.2008.03153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Giraud V, Allaert FA, Roche N. Inhaler technique and asthma: Feasability and acceptability of training by pharmacists. Respir Med. 2011;105:1815–22. doi: 10.1016/j.rmed.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 473.Giraud V, Allaert FA. Improved asthma control with breath-actuated pressurized metered dose inhaler (pMDI): The SYSTER survey. Eur Rev Med Pharmacol Sci. 2009;13:323–30. [PubMed] [Google Scholar]
- 474.Donnell D. Inhaled corticosteroid delivery systems: Clinical role of a breath-actuated device. Eur Rev Med Pharmacol Sci. 2001;5:7–16. [PubMed] [Google Scholar]
- 475.Drazen JM, Harrington D. New Biologics for Asthma. N Engl J Med. 2018;378:2533–4. doi: 10.1056/NEJMe1806037. [DOI] [PubMed] [Google Scholar]
- 476.Hanania NA, Wenzel S, Rosén K, Hsieh HJ, Mosesova S, Choy DF, et al. Exploring the effects of omalizumab in allergic asthma: An analysis of biomarkers in the EXTRA study. Am J Respir Crit Care Med. 2013;187:804–11. doi: 10.1164/rccm.201208-1414OC. [DOI] [PubMed] [Google Scholar]
- 477.Normansell R, Walker S, Milan SJ, Walters EH, Nair P. Omalizumab for asthma in adults and children. Cochrane Database Syst Rev. 2014:CD003559. doi: 10.1002/14651858.CD003559.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Lowe PJ, Georgiou P, Canvin J. Revision of omalizumab dosing table for dosing every 4 instead of 2 weeks for specific ranges of bodyweight and baseline IgE. Regul Toxicol Pharmacol. 2015;71:68–77. doi: 10.1016/j.yrtph.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 479.Agache I, Beltran J, Akdis C, Akdis M, Canelo-Aybar C, Canonica GW, et al. Efficacy and safety of treatment with biologicals (benralizumab, dupilumab, mepolizumab, omalizumab and reslizumab) for severe eosinophilic asthma. A systematic review for the EAACI Guidelines - recommendations on the use of biologicals in severe asthma. Allergy. 2020;75:1023–42. doi: 10.1111/all.14221. [DOI] [PubMed] [Google Scholar]
- 480.Ortega HG, Yancey SW, Mayer B, Gunsoy NB, Keene ON, Bleecker ER, et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: A secondary analysis of the DREAM and MENSA studies. Lancet Respir Med. 2016;4:549–56. doi: 10.1016/S2213-2600(16)30031-5. [DOI] [PubMed] [Google Scholar]
- 481.Bel EH, Wenzel SE, Thompson PJ, Prazma CM, Keene ON, Yancey SW, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med. 2014;371:1189–97. doi: 10.1056/NEJMoa1403291. [DOI] [PubMed] [Google Scholar]
- 482.FitzGerald JM, Bleecker ER, Menzies-Gow A, Zangrilli JG, Hirsch I, Metcalfe P, et al. Predictors of enhanced response with benralizumab for patients with severe asthma: Pooled analysis of the SIROCCO and CALIMA studies. Lancet Respir Med. 2018;6:51–64. doi: 10.1016/S2213-2600(17)30344-2. [DOI] [PubMed] [Google Scholar]
- 483.Chipps BE, Newbold P, Hirsch I, Trudo F, Goldman M. Benralizumab efficacy by atopy status and serum immunoglobulin E for patients with severe, uncontrolled asthma. Ann Allergy Asthma Immunol. 2018;120:504–11.e4. doi: 10.1016/j.anai.2018.01.030. [DOI] [PubMed] [Google Scholar]
- 484.Castro M, Zangrilli J, Wechsler ME, Bateman ED, Brusselle GG, Bardin P, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: Results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med. 2015;3:355–66. doi: 10.1016/S2213-2600(15)00042-9. [DOI] [PubMed] [Google Scholar]
- 485.Mukherjee M, Aleman Paramo F, Kjarsgaard M, Salter B, Nair G, LaVigne N, et al. Weight-adjusted intravenous reslizumab in severe asthma with inadequate response to fixed-dose subcutaneous mepolizumab. Am J Respir Crit Care Med. 2018;197:38–46. doi: 10.1164/rccm.201707-1323OC. [DOI] [PubMed] [Google Scholar]
- 486.Busse WW, Bleecker ER, FitzGerald JM, Ferguson GT, Barker P, Sproule S, et al. Long-term safety and efficacy of benralizumab in patients with severe, uncontrolled asthma: 1-year results from the BORA phase 3 extension trial. Lancet Respir Med. 2019;7:46–59. doi: 10.1016/S2213-2600(18)30406-5. [DOI] [PubMed] [Google Scholar]
- 487.Chupp G, Lugogo NL, Kline JN, Ferguson GT, Hirsch I, Goldman M, et al. Rapid onset of effect of benralizumab on morning peak expiratory flow in severe, uncontrolled asthma. Ann Allergy Asthma Immunol. 2019;122:478–85. doi: 10.1016/j.anai.2019.02.016. [DOI] [PubMed] [Google Scholar]
- 488.Kavanagh J, Roxas C, Green L, Thomson L, d'Ancona G, Fernandes M, et al. S53 Response to benralizumab after sub-optimal response to mepolizumab in severe eosinophilic asthma. New York, USA: BMJ Publishing Group Ltd; 2019. [DOI] [PubMed] [Google Scholar]
- 489.Kavanagh J, Green L, Fernandes M, Roxas C, Kent B, Jackson D, et al. B21 severe asthma: Clinical and mechanistic studies. New York, USA: American Thoracic Society; 2019. Response to benralizumab after sub-optimal response to mepolizumab in oral corticosteroid dependent severe eosinophilic asthma; pp. A2675–A. [Google Scholar]
- 490.Agache I, Rocha C, Beltran J, Song Y, Posso M, Solà I, et al. Efficacy and safety of treatment with biologicals (benralizumab, dupilumab and omalizumab) for severe allergic asthma: A systematic review for the EAACI Guidelines - Recommendations on the use of biologicals in severe asthma. Allergy. 2020;75:1043–57. doi: 10.1111/all.14235. [DOI] [PubMed] [Google Scholar]
- 491.Peters MC, Wenzel SE. Intersection of biology and therapeutics: Type 2 targeted therapeutics for adult asthma. Lancet. 2020;395:371–83. doi: 10.1016/S0140-6736(19)33005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 492.Corren J, Parnes JR, Wang L, Mo M, Roseti SL, Griffiths JM, et al. Tezepelumab in Adults with Uncontrolled Asthma. N Engl J Med. 2017;377:936–46. doi: 10.1056/NEJMoa1704064. [DOI] [PubMed] [Google Scholar]
- 493.Simpson EL, Parnes JR, She D, Crouch S, Rees W, Mo M, et al. Tezepelumab, an anti-thymic stromal lymphopoietin monoclonal antibody, in the treatment of moderate to severe atopic dermatitis: A randomized phase 2a clinical trial. J Am Acad Dermatol. 2019;80:1013–21. doi: 10.1016/j.jaad.2018.11.059. [DOI] [PubMed] [Google Scholar]
- 494.Wechsler ME, Colice G, Griffiths JM, Almqvist G, Skärby T, Piechowiak T, et al. SOURCE: A phase 3, multicentre, randomized, double-blind, placebo-controlled, parallel group trial to evaluate the efficacy and safety of tezepelumab in reducing oral corticosteroid use in adults with oral corticosteroid dependent asthma. Respir Res. 2020;21:264. doi: 10.1186/s12931-020-01503-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 495.Menzies-Gow A, Colice G, Griffiths JM, Almqvist G, Ponnarambil S, Kaur P, et al. NAVIGATOR: A phase 3 multicentre, randomized, double-blind, placebo-controlled, parallel-group trial to evaluate the efficacy and safety of tezepelumab in adults and adolescents with severe, uncontrolled asthma. Respir Res. 2020;21:266. doi: 10.1186/s12931-020-01526-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 496.Kemp A. Tezepelumab NAVIGATOR Phase III Trial Met Primary Endpoint of a Statistically Significant and Clinically Meaningful Reduction in Exacerbations in a Broad Population of Patients with Severe Asthma. AstraZeneca. 2020. [Last accessed on 2020 Nov 22]. Available from: https://www.astrazeneca.com/media-centre/press-releases/2020/tezepelumab-navigator-phase-iii-trial-met-primary-endpoint.html .


