Supplemental Digital Content is available in the text
Keywords: health information technology capabilities, outcome measure, patient engagement capability, patient readmissions, public health reporting capability
Abstract
Health information technology (IT) is often proposed as a solution to fragmentation of care, and has been hypothesized to reduce readmission risk through better information flow. However, there are numerous distinct health IT capabilities, and it is unclear which, if any, are associated with lower readmission risk.
To identify the specific health IT capabilities adopted by hospitals that are associated with hospital-level risk-standardized readmission rates (RSRRs) through path analyses using structural equation modeling.
This STROBE-compliant retrospective cross-sectional study included non-federal U.S. acute care hospitals, based on their adoption of specific types of health IT capabilities self-reported in a 2013 American Hospital Association IT survey as independent variables. The outcome measure included the 2014 RSRRs reported on Hospital Compare website.
A 54-indicator 7-factor structure of hospital health IT capabilities was identified by exploratory factor analysis, and corroborated by confirmatory factor analysis. Subsequent path analysis using Structural equation modeling revealed that a one-point increase in the hospital adoption of patient engagement capability latent scores (median path coefficient ß = −0.086; 95% Confidence Interval, −0.162 to −0.008), including functionalities like direct access to the electronic health records, would generally lead to a decrease in RSRRs by 0.086%. However, computerized hospital discharge and information exchange capabilities with other inpatient and outpatient providers were not associated with readmission rates.
These findings suggest that improving patient access to and use of their electronic health records may be helpful in improving hospital performance on readmission; however, computerized hospital discharge and information exchange among clinicians did not seem as beneficial – perhaps because of the quality or timeliness of information transmitted. Future research should use more recent data to study, not just adoption of health IT capabilities, but also whether their usage is associated with lower readmission risk. Understanding which capabilities impact readmission risk can help policymakers and clinical stakeholders better focus their scarce resources as they invest in health IT to improve care delivery.
1. Introduction
Through the Health Information Technology for Economic and Clinical Health Act, the United States (US) government has provided more than $27 billion to subsidize the adoption of health Information Technology (IT) capabilities, under the premise that improved information capture and transfer across various care settings will improve patient outcomes.[1–3]
Health IT capabilities vary widely and include functionalities that support quality of hospital discharge, patient engagement, public health reporting of immunizations, disease surveillance, specialized registries, and clinical information sharing electronically with patients and providers inside and outside hospital systems.[4–14] Each of the capabilities may play a distinct role in influencing readmission risk; in turn these roles may be additive or synergistic. For instance, being able to exchange data with clinicians outside the health system may help outpatient clinicians with post-discharge follow up and medication reconciliation. However, adverse events leading to readmissions may still occur if patients do not have direct access to electronic health records systems in order to best adhere to prescribed treatment and engage in their own care.
Early research linking health IT capabilities and reduced readmission rates has yielded mixed and inconclusive evidence.[15–19] For instance, in a study of 2406 hospitals, Jones and colleagues found that hospital participation in health information exchange had no impact on 30-day risk adjusted readmission rates, although expanded use of electronic documentation was found to be associated with moderately reduced readmission rates for pneumonia and heart failure.[16] By contrast, Ben-Assuli and colleagues found that electronic health records and health information exchange usage is associated with lower readmission rates,[17] while Ryan and colleagues have found the adoption and meaningful use of health IT to be among the reforms that led to greater reduction of readmissions.[20,21] At the same time, research by other experts continued to yield mixed evidence.[19] Despite these recent positive results, the specific health IT capabilities that are most associated with reduced readmission risk remain unclear, suggesting that the relationships between these variables are complex.
Our aim was to understand which health IT capabilities, specifically, contribute to lower readmission risk. First, using nationwide hospital IT adoption data, we identified and confirmed a set of factors representing types of health IT capability using factor analysis. We then applied structural equation modeling to determine the association of these factors with risk-standardized hospital readmission rates.
By understanding which capabilities are associated with lower readmission risk, policymakers and clinical stakeholders can craft and execute better strategies to maximize their utilization, as they work to minimize 30-day readmissions, which are detrimental to patient health, in addition to being costly.
2. Methods
2.1. Data sources
We used data from two sources: the 2013 American Hospital Association (AHA) annual IT supplement survey, and the 2014 Centers for Medicare and Medicaid Services (CMS) Hospital Compare database.[22–24] The 2013 AHA IT supplement survey was administered between November 2013 and February 2014, and consists of self-reported answers to questions about a variety of health IT capabilities adopted by hospitals.[23] The 2014 CMS Hospital Compare database includes the 30-day hospital-wide risk-standardized readmission rates (RSRRs), which were calculated using the Medicare administrative claims data and enrollment information of Medicare fee-for-service beneficiaries between July 2014 and June 2015, ensuring that outcomes were being captured after health IT adoption by hospitals was measured.
2.2. Study variables
From the AHA IT supplement survey, we identified 55 survey items, also referred to as indicators, to conduct the exploratory and confirmatory factor analyses (EFA and CFA) in order to derive and validate specific factors representing hospital health IT capabilities that were plausibly clinically important to reducing readmissions. These items were selected from various sections of the AHA IT supplement survey, including meaningful use functionalities (topic 2, 19 items), health information exchange functionalities (topic 3, 24 items), and patient engagement functionalities (topics 7 and 8, 8 and 4 items, respectively).
For items identified from topics 2, 3, and 7, the response options were “Yes,” “No,” and “Do Not Know.”For missing data, we conducted multiple imputations based on the assumption that data in these items are missing at random; however, we treated “Do Not Know” as “No.”On the other hand, after carefully reviewed the wording of and responses to items in topic 8, the pattern of missing values could not be assumed to be missing at random. We treated the missingness in these items as “Do Not Know.”
From the 2016 CMS Hospital Compare database, we used the hospital-wide RSRRs as the outcome variable to conduct path analyses using structural equation model (SEM) to determine the association between hospital health IT capabilities and readmission risk. RSRRs are calculated by CMS as ratios of predicted over expected readmission risk for each hospital, and are multiplied by the national mean for interpretability.[25]
2.3. Study sample
We included all non-federal acute care hospitals that responded to the 2013 AHA IT supplemental survey and that had hospital-wide RSRRs reported in Hospital Compare. We excluded federal hospitals because they are not included in Hospital Compare.
2.4. Statistical analysis
The analyses to determine the specific types of health IT capabilities that are associated with lower hospital-wide RSRRs were conducted in four phases. In the first phase, we used the fully conditional specification logistic regression method to impute missing data to items selected from topics 2, 3, and 7 as they are binary. We first attempted to use only one random-split sample to conduct the EFA based on the tetrachoric correlation matrix. However, the EFA model failed to converge. To address this, we conducted five imputations because they produce fairly accurate estimates with a standard deviation wider than the one of estimates based on infinite imputations by about 5%, as suggested by Rubin.[26] For each of the five datasets created with imputed missing values, we randomly split it into 2 halves for 200 times, creating1000 derivation sets, and 1000 verification sets.
Using the hospital Medicare Provider Identification (ID) numbers, we merged the 1000 verification sets with the 2014 dataset of hospital-wide RSRRs, creating 1000 merged sets (see Fig. 1). All of the above datasets exceeded the minimum sample size standard of 10 respondents per observed variable, or 550 hospitals for the 55survey items in this study.[27]
Figure 1.
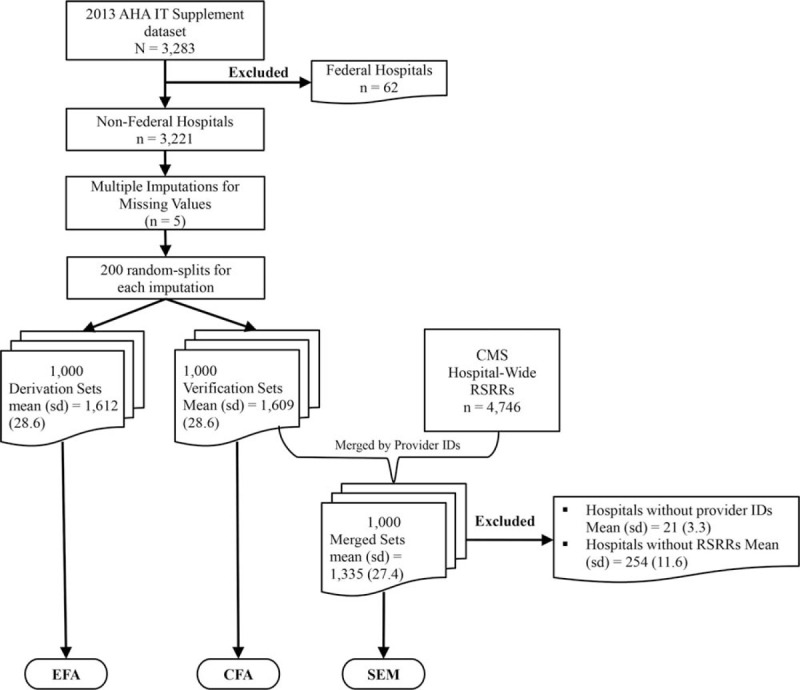
Flowchart of hospitals in study.
In the second phase, we used the 1000 derivation sets to conduct EFA to identify the underlying factor structure based on the tetrachoric correlations among the 55 items, since they are binary. We employed the oblique (Promax) rotation method because we did not assume that the factors were independent.[28]
Given the high number of replications involved in the factor analyses, we conducted the Shapiro-Wilk Test to evaluate normality, and found that the variable loadings on some factors were not normally distributed across replications. Therefore, to summarize our results, we calculated and examined the medians and interquartile ranges (IQR) of the variable loadings on each factor across all replications. We used the factor loading medians and frequencies to identify the variables to retain.
In the third phase, we used the validation sets to perform CFA to validate the factor structure discovered by the EFA. To address non-normality associated with the binary variables, we selected the maximum likelihood Satorra-Bentler estimation method, involving scaled model fit chi-square χ2statistics and the sandwich-type standard error estimates, both suggested by Satorra and Bentler.[29] Validated factors represented categories of health IT capabilities adopted by US hospitals. We then labeled them to reflect the attributes of the variables that loaded most strongly on them.
In the fourth phase, we conducted path analyses employing the SEM technique, using the maximum likelihood Satorra-Bentler estimation method discussed above. The advantage of the SEM technique is that we could use the latent factors of hospital health IT capabilities directly as the independent variables to predict the outcome variable, the hospital-wide RSRRs, accounting for measurement error to reduce potential bias in the estimates due to unreliability that may exist in the observed variables.
All statistical analyses in this study were conducted using SAS software version 9.4 (SAS Institute, Inc., Cary, NC). Specifically, we used procedure FACTOR for the EFA and procedure covariance analysis of linear structural equation for the CFA and SEM. As this study did not involve human subjects, institutional review board approval was not required.
To assess the general fits of CFA and SEM models, due to data non-normality we examined the medians and IQRs of Standardized Root Mean Square Residual (<0.05), Relative Root Mean Square Error (<0.08), and Bentler Comparative Fit Index (≥ 0.90).[30–35] If the median values of most of the above indexes indicate acceptable model fit, it means that the data support the derived factor structure of health IT capabilities adopted by US hospitals.[31]
3. Study results
3.1. Study sample
As displayed in Figure 1, there were 3,283 hospitals in the 2013 AHA annual survey IT supplement dataset. Of these hospitals, 62 were federal hospitals and were excluded. Among the 3,221 non-federal hospitals remaining, 37% were in rural areas; 28% were teaching hospitals; 50% were relatively small hospitals with less than 100 beds (including 23% critical access hospitals), 14% were relatively large hospitals with more than 400 beds, and the rest (36%) were medium-sized hospitals. Means and standard deviations (SD) are reported in Figure 1 because non-normality is not an issue for the distributions of data across the 1000 pairs of randomly-split samples, as confirmed by the results of the Shapiro–Wilk test (P = .73). After excluding those without hospital Medicare Provider IDs and RSRRs, a mean of 1,335 hospitals (SD = 27.4) were linked to the CMS Hospital Compare database, representing our final analytic dataset.
3.2. Missing data imputation phase
Of the 3,221 non-federal hospitals in the 2013 AHA IT Supplement dataset, the fully conditional specification missing data imputation procedure followed by the randomized split of each of the five imputed datasets into halves for 200 times yielded 1000 derivation sets with a mean (SD) of 1612 (SD = 28.6) hospitals, 1000 verification sets with a mean (SD) of 1609 (SD = 28.6) hospitals, and 1000 merged sets with a mean (SD) of 1335 (27.4) hospitals, as shown in Figure 1.
3.3. Derivation phase
The 1000 derivation sets were used to conduct the EFA. The estimation of the tetrachoric correlation matrix converged for 619 of them. For the factor structure, we reported medians and IQRs because the Shapiro-Wilk test revealed P values of <.05 for more than half of the variables that loaded on the seven factors, demonstrating non-normality. On the basis of the median loading values and IQRs for the factor structure suggested by EFA (see Appendix A), and the loading frequencies (see Appendix B), we retained 54 survey items with high loadings, and deleted the one with low median factor loading and frequency.
3.4. Validation phase
The 1000 verification sets were used to carry out CFA to assess the validity of the 7-factor structure of hospital health IT capabilities. The median values and IQRs of each fit index across the 1000 sets for the CFA model are reported in Table 1. The CFA and SEM models show acceptable or near acceptable fit (standardized root mean square residual <0.05, relative root mean square error <0.08, and comparative fit indexs close to commonly accepted value of 0.9).
Table 1.
Fit Indexes for CFA and SEM Models.
| Median (IQR) Fit Indices of the 1000 Replications | |||||
| Models | RMSER 95% CI | ||||
| SRMR | RMSER | Lower | Upper | CFI | |
| CFA | 0.049 (0.001) | 0.062 (0.001) | 0.061 (0.001) | 0.063 (0.001) | 0.890 (0.005) |
| SEM | 0.051 (0.002) | 0.060 (0.001) | 0.059 (0.001) | 0.062 (0.001) | 0.875 (0.006) |
CFA = confirmatory Factor Analysis, CFI = Bentler's comparative fit index, CI = confidence Interval, IQR = Interquartile Range, RMSER = Relative root mean square error, SEM = structural equation modeling, SRMR = standardized root mean square Residual.
The factor structure validated by the CFA is shown in Appendix C. As depicted there, we labeled the first factor, computerized discharge capability, because the sixteen observed variables that successfully loaded on it represent features, including being able to generate updated medication lists and orders at admission and at discharge, generate discharge instructions for patients, create and transmit discharge summaries for appropriate care transitions. The second factor we labeled, public health reporting because the three variables that underlie it reflect features such as hospitals’ electronic abilities to submit data to immunization registries or information systems, lab results and syndromic surveillance data to public health agencies.
The third factor was assigned the label of external hospital exchange because the six variables that loaded on it represent hospitals’ abilities to electronically exchange different types of patient data with other hospitals outside their system. The fourth factor was marked internal hospital exchange because the six variables that loaded on it represent hospitals’ abilities to electronically exchange different types of patient data with hospitals inside their system.
The fifth factor was labeled external ambulatory exchange because the six variables that loaded on it reflect hospitals’ abilities to electronically exchange different types of patient data with ambulatory providers outside their system. The sixth factor was labeled internal ambulatory exchange because the six variables that loaded on it reflect hospitals’ abilities to electronically exchange different types of patient data with ambulatory providers inside their system.
The seventh or last factor was labeled patient engagement, because the eleven variables that loaded on it all relate to patient interaction with the electronic health records: accessing health information electronically; being able to view, download, and transmit health/medical records online to a third party; requesting refills for prescriptions online; amending their health record; and engaging in secure messaging with providers.
We referred to the seven factors as specific types of health IT capabilities, and used them to develop the research framework in Figure 2 below, which displays the paths that are under study. Next, we tested these paths using SEM.
Figure 2.
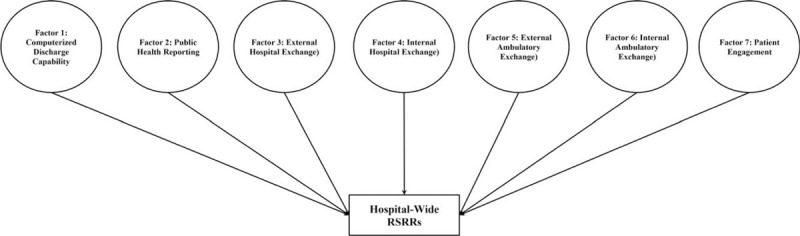
Research Framework.
3.5. Structural equation modeling (SEM) phase
The 1000 merged sets were used to conduct path analyses employing the SEM technique. The summarized path analysis results, as reported in Figure 3, revealed that, among the seven health IT capabilities validated by CFA, the patient engagement capability (Factor 7) had the general tendency to be negatively associated with hospital-wide RSRRs with a median path coefficient (ß) of −0.086 (95% confidence interval, −0.162 to −0.008). By contrast, the hospital public health reporting capability (Factor 2) generally tended to have a positive association with RSRRs with a median path coefficient (ß) of 0.110 (95% confidence interval, 0.015 to 0.212). On the other hand, the remaining five health IT capabilities, including the computerized hospital discharge (Factor 1) and information exchange capabilities (Factors 3–6) were found not to be associated with RSRRs, as shown in Figure 3. However, as displayed in Table 2, the seven factors were found to be positively correlated with one another.
Figure 3.
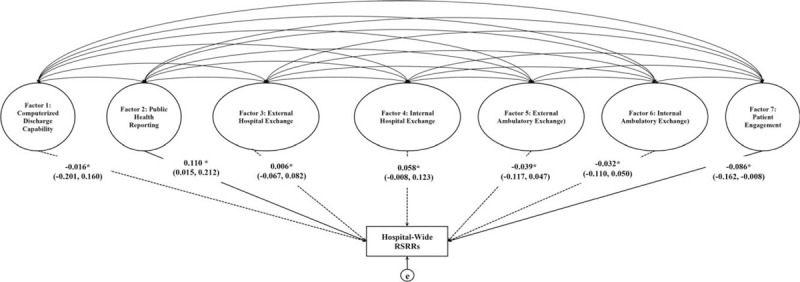
Summarized results of path analyses using SEM. ∗ß = median path coefficient across 1000 sets for each individual path. 95% Confidence Intervals (CI) reported in parentheses. The solid arrow-ended lines denote health IT capabilities that in general tended to be associated with lower hospital-wide RSRRs. If the 95% CI includes zero, then the path is not statistically significantly from zero, which is denoted as dashed lines in the diagram.
Table 2.
Factor correlation matrix.
| Median (IQR) Correlations of the 1000 Replications | ||||||||
| Factor | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| 1 | Computerized Discharge Capability | 0.501 (0.025) | 0.196 (0.030) | 0.197 (0.033) | 0.247 (0.033) | 0.229 (0.031) | 0.370 (0.021) | |
| 2 | Public Health Reporting | 0.170 (0.030) | 0.173 (0.029) | 0.172 (0.032) | 0.202 (0.031) | 0.258 (0.028) | ||
| 3 | External Hospital Exchange | 0.210 (0.026) | 0.228 (0.023) | 0.548 (0.025) | 0.346 (0.027) | |||
| 4 | Internal Hospital Exchange | 0.237 (0.030) | 0.187 (0.029) | 0.331 (0.023) | ||||
| 5 | External Ambulatory Exchange | 0.431 (0.025) | 0.305 (0.024) | |||||
| 6 | Internal Ambulatory Exchange | 0.347 (0.027) | ||||||
| 7 | Patient Engagement | |||||||
4. Discussion
Through a series of factor analyses on 2013 hospital IT adoption data, we derived and validated seven clinically important hospital health IT capabilities (computerized discharge capability, public health reporting, electronic exchange with hospitals in and out of the health system, electronic exchange with ambulatory providers in and out of the health system, and patient engagement) and found that only the patient engagement domain was associated with lower hospital readmission rates.
By engaging with their health information and with providers online, patients may be able to better understand their clinical information, adhere to the treatment plan and manage their medical conditions post-discharge.[36,37,38,39,40,41] For example, a recent study by Reed and colleagues[42] revealed that, after portal access, patients with diabetes used outpatient visits more, and the emergency departments less. As in our study, this favorable outcome is explained by the availability of, not only of patient electronic access, but also of advanced features such as “interactive tools, including viewing lab results and visit summaries, secure email messaging with health care providers, ordering medication refills, and appointment scheduling.”[42](p2)
However, we found that computerized hospital discharge and electronic information exchange capabilities had no associations with readmission rates. A plausible explanation for this unexpected finding might be because the clinical information transmitted is untimely or unusable due to low quality[7] or lack of interoperability if it is not structured in a standardized format that would allow for easy integration into recipient health IT system. We were surprised by the association of public health reporting capability with increased readmission rates. One explanation for this finding might be because the public health agencies may not have the capability to receive the data sent to them electronically by hospitals, as found by Holgrem and colleagues using 2018 data.[43]
These gaps in interoperability between the data sharing systems used by public health agencies and hospitals may adversely impact readmission risk.[43,44] We expect these gaps to be even more profound in 2013, when study data were collected, but also a period in which hospital adoption of health IT was in its infancy. Another explanation is that, as public health reporting electronically requires a very sophisticated capability, it may only be present in large health systems which tend to have higher readmission rates.
We find that, even when patient discharge and public health reporting are carried out properly, clinician decision making is effective, all enabled by appropriate health IT capabilities (i.e. flow of vital health information between providers during care transitions is timely, complete, and error-free, resulting in an informed treatment plan), that may not be enough to reduce readmission risk. Patient engagement[45] is also needed, which can be enabled through several different types of patient-facing technologies,[46] including Personal Health Records, patient portals, and secure messaging, which loaded strongly on related factor (see Appendix C), meaning they are part of the building blocks unique to the patient engagement capability factor that has been found to be associated with lower readmission risk.
These technologies can give patients electronic access to their health information so they can view and understand the discharge instructions, medications, interact online with their providers, make informed decisions about their care, identify and help correct record inaccuracies, adhere to the prescribed treatment plan, and more actively participate in their healthcare decisions. However, recent research by Sharma and colleagues and Lin et al. found that patient portal access is still underused,[12,47] suggesting there remains a need for policymakers and other stakeholders to intervene and incentivize portal adoption and use in order to realize greater reduction in readmission risk. Given the positive correlation among the seven factors, policies that focus on the adoption and use of patient engagement capability may not only lead to lower readmission risk, but are likely also improve adoption of the other six capabilities.
4.1. Study limitations and recommendations for future research
Our study used a large national dataset and multiple measures of health IT capability to better capture with acceptable model fit the complexities in the relationships between multifunctional health IT capabilities and readmission rates.
Despite the above strengths, our study has several limitations. First, it is cross-sectional; thus, we cannot draw causal inferences from the results. Second, our data source for the health IT capability measures is a survey, whose responses have not been validated directly. However, the factor structure used to examine the associations with RSRRs was validated by the confirmatory factor analysis we conducted.
Third, the data used for the health IT capability measures were collected in 2013, which represent only a single snapshot in time. Fourth, we did not observe hospital usage of adopted capabilities, which would influence the readmission rates more directly. Lastly, generalizability of study findings may be limited to non-federal acute care US hospitals.
Future studies should use more recent data on the adoption and use of health IT capabilities to conduct a more comprehensive examination of their impact on hospital readmission risk. Our model should be expanded in future research to examine other health IT capabilities such as telehealth, mHealth, remote monitoring, interoperability, and artificial intelligence, and their direct and indirect association with RSRRs. Also, future research should use panel data to see whether and how the associations studied here between health IT capabilities and readmission rates change over time to account for the lagged effects of health IT capabilities.
5. Conclusions
While readmission is 1 of the biggest challenges facing US healthcare, affecting millions of patients every year and costing billions of dollars, this study provides evidence of general tendency that it can be impacted in favorable ways by hospital adoption of patient access capability. For policymakers, providers, and payers, this finding suggests that enhancing hospital adoption of patient engagement capability may help improve hospital performance on readmission. However, for hospital adoption of public health reporting capability, more research is needed to determine how interoperability between the data sharing systems used by public health agencies and hospitals[43] may impact its relationship with readmission risk.
Acknowledgments
The authors thank Jane Padikkala, MPH, for scheduling the research project meetings, tracking action item completions, and assisting with citation formatting; and Shawn Hoke, BA, for his assistance with the data acquisition from Health Forum, LLC.
Author contributions
Conceptualization: Gerald Elysee, Huihui Yu, Jeph Herrin, Leora I. Horwitz.
Data curation: Huihui Yu.
Formal analysis: Huihui Yu.
Funding acquisition: Leora I. Horwitz.
Investigation: Gerald Elysee, Huihui Yu, Jeph Herrin, Leora I. Horwitz.
Methodology: Gerald Elysee, Huihui Yu, Jeph Herrin, Leora I. Horwitz.
Project administration: Gerald Elysee.
Resources: Leora I. Horwitz.
Software: Leora I. Horwitz.
Supervision: Leora I. Horwitz.
Validation: Gerald Elysee, Huihui Yu, Jeph Herrin, Leora I. Horwitz.
Visualization: Gerald Elysee, Huihui Yu, Jeph Herrin, Leora I. Horwitz.
Writing – original draft: Gerald Elysee, Huihui Yu, Jeph Herrin, Leora I. Horwitz.
Writing – review and editing: Gerald Elysee, Huihui Yu, Jeph Herrin, Leora I. Horwitz.
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: AHA = American hospital association, CFA = confirmatory factor analysis, CMS = centers for medicare and medicaid services, EFA = exploratory factor analysis, IQR = interquartile range, IT = information technology, RSRRs = hospital-level risk-standardized readmission rates, SEM = structural equation modeling.
How to cite this article: Elysee G, Yu H, Herrin J, Horwitz LI. Association between 30-day readmission rates and health information technology capabilities in US hospitals. Medicine. 2021;100:8(e24755).
Study was funded by the Agency for Healthcare Research and Quality (R01HS022882). AHRQ had no role in the design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the AHRQ.
The authors have no conflicts of interest to disclose.
The data that support the findings of this study are available from a third party, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are available from the authors upon reasonable request and with permission of the third party.
References
- [1].Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144:742–52. [DOI] [PubMed] [Google Scholar]
- [2].Gold M, McLaughlin C. Assessing HITECH Implementation and Lessons: 5 Years Later. Milbank Q 2016;94:654–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hessels A, Flynn L, Cimiotti JP, et al. Impact of heath information technology on the quality of patient care. On-line J Nurs informatics 2015. 19.http://www.himss.org/impact-heath-information-technology-quality-patient-care [PMC free article] [PubMed] [Google Scholar]
- [4].Kripalani S, Jackson AT, Schnipper JL, et al. Promoting effective transitions of care at hospital discharge: A review of key issues for hospitalists. J Hosp Med 2007;2:314–23. [DOI] [PubMed] [Google Scholar]
- [5].Kripalani S, Theobald CN, Anctil B, et al. Reducing Hospital Readmission Rates: Current Strategies and Future Directions. Annu Rev Med 2014;65:471–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Alper E, O’Malley TA, Greenwald J. Hospital discharge and readmission. UpToDate 2019;https://www.uptodate.com/contents/search?search=Hospital%20Discharge%20and%20Readmission&x=0&y=0https://www.uptodate.com/contents/search?search=Hospital%20Discharge%20and%20Readmission&x=0&y=0. Accessed February 3, 2021. [Google Scholar]
- [7].Al-Damluji MS, Dzara K, Hodshon B, et al. Association of discharge summary quality with readmission risk for patients hospitalized with heart failure exacerbation. Circ Cardiovasc Qual Outcomes 2015;8:109–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med 2013;173:1715–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].O’Leary KJ, Liebovitz DM, Feinglass J, et al. Creating a better discharge summary: Improvement in quality and timeliness using an electronic discharge summary. J Hosp Med 2009;4:219–25. [DOI] [PubMed] [Google Scholar]
- [10].Ammenwerth E, Schnell-Inderst P, Machan C, et al. The Effect of Electronic Prescribing on Medication Errors and Adverse Drug Events: A Systematic Review. Journal of the American Medical Informatics Association 2008;15:585–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kaushal R, Kern LM, Barrón Y, et al. Electronic prescribing improves medication safety in community-based office practices. J Gen Intern Med 2010;25:530–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Sharma AE, Rivadeneira NA, Barr-Walker J, et al. Patient Engagement In Health Care Safety: An Overview Of Mixed-Quality Evidence. Health Aff 2018;37:1813–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Norton PT, Rodriguez HP, Shortell SM, et al. Organizational influences on healthcare system adoption and use of advanced health information technology capabilities. Am J Manag Care 2019;25:e21–5. [PMC free article] [PubMed] [Google Scholar]
- [14].Mehta RL, Baxendale B, Roth K, et al. Assessing the impact of the introduction of an electronic hospital discharge system on the completeness and timeliness of discharge communication: a before and after study. BMC Health Serv Res 2017;17:doi:10.1186/s12913-017-2579-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff 2011;30:464–71. [DOI] [PubMed] [Google Scholar]
- [16].Jones SS, Friedberg MW, Schneider EC. Health information exchange, Health Information Technology use, and hospital readmission rates. AMIA Annu Symp Proc 2011;2011:644–53. [PMC free article] [PubMed] [Google Scholar]
- [17].Ben-Assuli O, Shabtai I, Leshno M. The impact of EHR and HIE on reducing avoidable admissions: controlling main differential diagnoses. BMC Med Inform Decis Mak 2013;13: doi:10.1186/1472-6947-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Jones SS, Rudin RS, Perry T, et al. Health information technology: an updated systematic review with a focus on meaningful use. Ann Intern Med 2014;106:48–54. [DOI] [PubMed] [Google Scholar]
- [19].Yanamadala S, Morrison D, Curtin C, et al. Electronic health records and quality of care an observational study modeling impact on mortality, readmissions, and complications. In: Medicine (United States) 2016;95:e3332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ryan AM, Krinsky S, Adler-Milstein J, et al. Association between hospitals’ engagement in value-based reforms and readmission reduction in the hospital readmission reduction program. JAMA Intern Med 2017;177:862–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kruse CS, Beane A. Health information technology continues to show positive effect on medical outcomes: systematic review. J Med Internet Res 2018;20:e41.doi:10.2196/jmir.8793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Centers for Medicare & Medicaid Services. 2016 Hospital Compare downloadable database. Centers for Medicare & Medicaid Services. Available at: https://data.cms.gov/provider-data/sites/default/files/archive/Hospitals/2016/hos_revised_flatfiles_archive_05_2016.zip. Accessed July 19, 2019. [Google Scholar]
- [23].American Hospital Association IT Supplement Survey. 2013 American Hospital Association IT Supplement Survey. AHA annual survey information technology supplement: Survey questionnaire. https://www.ahadataviewer.com/Global/IT surveys/2013 AHA Annual Survey IT Supplement Survey.pdf. Published 2013. Accessed July 19, 2019. [Google Scholar]
- [24].American Hospital. Association IT Supplement Survey. 2013 AHA annual survey information technology supplement: Custom Database. Am Hosp Assoc IT Suppl Surv Cust Database 2013. [Google Scholar]
- [25].Horwitz LI, Partovian C, Lin Z, et al. Development and use of an administrative claims measure for profiling hospital-wide performance on 30-day unplanned readmission. Ann Intern Med 2014. 161(10_Supplement):S66. doi:10.7326/m13-3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Rubin BD. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley; 1987. [Google Scholar]
- [27].Everitt BS. Multivariate analysis: the need for data, and other problems. Br J Psychiatry 1975;126:237–40. [DOI] [PubMed] [Google Scholar]
- [28].Brown, Dean J. Choosing the right type of rotation in PCA and EFA. JALT Test Eval SIG Newsl 2009;13:20–5. [Google Scholar]
- [29].Satorra A, Bentler PM. Corrections to test statistics and standard errors in covariance structure analysis. In: Latent Variables Analysis: Applications for Developmental Research. 1994;Thousand Oaks, CA: SAGE Publications Ltd, 399–419. [Google Scholar]
- [30].Froehle CM, Roth AV. New measurement scales for evaluating perceptions of the technology-mediated customer service experience. J Oper Manag 2004;22:1–21. [Google Scholar]
- [31].Schumacker RE, Lomax RG. A Beguiner's guide to structural equation modeling 3rd edition 2010. 1–510. [Google Scholar]
- [32].Mak BL, Sockel H. A confirmatory factor analysis of IS employee motivation and retention. Inf Manag 2001;38:265–76. [Google Scholar]
- [33].Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model 1999;6:1–55. [Google Scholar]
- [34].Hu LT, Bentler PM. Fit Indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Methods 1998;3:424–53. [Google Scholar]
- [35].Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med 2009;4:211. [DOI] [PubMed] [Google Scholar]
- [36].Irizarry T, Shoemake J, Nilsen ML, et al. Patient portals as a tool for health care engagement: a mixed-method study of older adults with varying levels of health literacy and prior patient portal use. J Med Internet Res 2017;19:e99.doi:10.2196/jmir.7099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Institute of Medicine Crossing the quality chasm: a new health system for the 21st century - institute of medicine 2001. 1–360. doi:10.17226/10027. [PubMed] [Google Scholar]
- [38].Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff 2013;32:207–14. [DOI] [PubMed] [Google Scholar]
- [39].Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res 2015;17:e44.doi:10.2196/jmir.3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Griffin A, Skinner A, Thornhill J, et al. Patient Portals: Who uses them? What features do they use? And do they reduce hospital readmissions? Appl Clin Inform 2016;7:489–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kaplan B, Brennan PF. Consumer informatics supporting patients as co-producers of quality. J Am Med Informatics Assoc 2001;8:309–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Reed ME, Huang J, Brand RJ, et al. Patients with complex chronic conditions: health care use and clinical events associated with access to a patient portal. PLoS One 2019;14:e0217636.doi:10.1371/journal.pone.0217636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Holmgren AJ, Apathy NC, Adler-Milstein J. Barriers to hospital electronic public health reporting and implications for the COVID-19 pandemic. J Am Med Informatics Assoc 2020;27:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Dixon BE, Vreeman DJ, Grannis SJ. The long road to semantic interoperability in support of public health: experiences from two states. J Biomed Inform 2014;49:3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Bao C, Bardhan IR, Singh H, et al. Patient-provider engagement and its impact on health outcomes: a longitudinal study of patient portal use. MIS Q Manag Inf Syst 2020;44:699–723. [Google Scholar]
- [46].Ahern DK, Woods SS, Lightowler MC, et al. Promise of and potential for patient-facing technologies to enable meaningful use. Am J Prev Med 2011;40: 5, Supplement 2: S162–72. [DOI] [PubMed] [Google Scholar]
- [47].Lin SC, Lyles CR, Sarkar U, et al. Are Patients Electronically Accessing Their Medical Records? Evidence From National Hospital Data. Health Aff 2019;38:1850–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


